Ilioinguinal Nerve Entrapment
Table of Contents
What is an Ilioinguinal Nerve Entrapment?
Ilioinguinal nerve entrapment refers to a condition where the ilioinguinal nerve, which runs through the abdominal and groin area, becomes compressed or irritated, leading to pain, discomfort, or other sensations in the region supplied by the nerve.
The pain might radiate down the leg or be localized to specific areas. Activities such as standing, walking, or any movement that engages the lower abdominal muscles may exacerbate the discomfort.
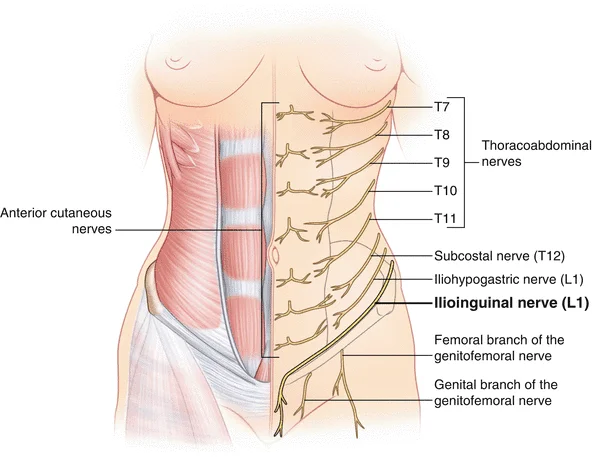
Anatomy
The ilioinguinal nerve is a branch of the first lumbar nerve (L1) that originates from the spinal cord. It passes through the psoas major muscle in the abdomen and travels obliquely downward toward the inguinal ligament, which is located in the lower abdomen near the groin.
As the ilioinguinal nerve courses downward, it exits the abdomen through the inguinal canal, which is a passage in the lower abdominal wall. It continues its path along the inguinal canal, providing sensory innervation to the skin of the upper inner thigh, the mons pubis, and the genitalia.
Due to its path and proximity to structures like the inguinal ligament and inguinal canal, the ilioinguinal nerve can be susceptible to entrapment or compression, leading to pain or other sensory disturbances in its distribution area. This can occur due to various reasons, such as anatomical variations, trauma, or surgical procedures in the pelvic or groin area.
Causes of Ilioinguinal Nerve Entrapment
- Hernias: A hernia in the groin area can put pressure on the ilioinguinal nerve, leading to entrapment and subsequent pain or discomfort.
- Surgery: Surgical procedures in the abdominal or groin area can sometimes lead to nerve irritation or damage.
- Injury or Trauma: Direct injury or trauma to the abdominal or groin area can cause nerve compression or irritation.
- Repetitive Strain: Activities that involve repetitive movements or strain on the abdominal muscles and groin can contribute to nerve compression over time.
- Inflammation: Inflammatory conditions like infections or inflammation of nearby structures can potentially affect the nerve.
- Tight Clothing: Wearing tight clothing or belts that put pressure on the groin area might contribute to nerve entrapment.
- Anatomical Variations: Individual anatomical differences can make certain people more susceptible to ilioinguinal nerve entrapment.
- Inguinal Hernia: A hernia in the groin area can cause similar pain and discomfort, especially during physical activities or when coughing or sneezing.
- Femoral Nerve Entrapment: Compression or irritation of the femoral nerve can lead to pain and sensory changes in the front of the thigh, which might be mistaken for ilioinguinal nerve issues.
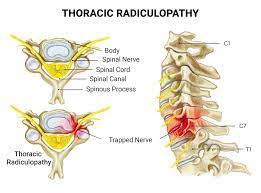
- Lumbar Radiculopathy: Nerve compression in the lower back (lumbar spine) can cause pain, numbness, and tingling that might radiate down the leg, resembling ilioinguinal nerve entrapment.
- Hip Joint Problems: Conditions affecting the hip joint, like hip osteoarthritis or labral tears can cause groin pain similar to nerve-related issues.
- Referred Pain: Issues in nearby structures, such as the urinary tract or reproductive organs, can cause referred pain that’s felt in the groin and abdominal area.
- Sports Hernia: Also known as athletic pubalgia, this condition involves soft tissue injuries in the groin area and can cause pain similar to nerve entrapment.
- Muscle Strain: Strain or injury to muscles in the groin region can lead to pain and discomfort similar to nerve-related symptoms.
- Appendicitis: Inflammation of the appendix can cause pain that initially starts in the belly button and might be mistaken for ilioinguinal nerve issues.
- Irritable Bowel Syndrome (IBS): This gastrointestinal disorder can cause abdominal pain and discomfort that might be localized in the groin area.
- Pelvic Floor Dysfunction: Issues with the muscles and ligaments of the pelvic floor can lead to pain and discomfort that might be felt in the groin region.
Symptoms of Ilioinguinal Nerve Entrapment
- Pain: Sharp or burning pain in the groin, lower abdomen, or upper thigh area.
- Numbness or Tingling: Sensations of numbness, tingling, or pins-and-needles in the same regions.
- Radiating Pain: Pain that travels down the inner thigh or along the path of the ilioinguinal nerve.
- Sensitivity: Increased sensitivity or discomfort when touching or applying pressure to the affected area.
- Muscle Weakness: Weakness in the abdominal muscles or hip flexors on the same side.
- Worsening with Movement: Pain may worsen with certain movements, such as bending, lifting, or walking.
- Coughing or Sneezing Pain: Increased pain during activities that put pressure on the abdomen, like coughing or sneezing.
Risk Factor
- Surgery: Procedures involving the pelvic or inguinal area, such as hernia repair, can sometimes lead to nerve entrapment.
- Hernias: Inguinal hernias or other abdominal wall hernias may increase the risk due to their proximity to the ilioinguinal nerve.
- Trauma: Injuries to the pelvic or groin region could potentially lead to nerve entrapment.
- Repetitive Strain: Activities or occupations that involve frequent and repetitive movements of the hip or groin area might contribute.
- Anatomy: Variations in anatomical structures, like the course of the nerve or the presence of anatomical anomalies, could increase the risk.
- Obesity: Excess weight can potentially put pressure on nerves in the pelvic region, increasing the risk of entrapment.
- Pregnancy: The changes in the pelvic area during pregnancy can sometimes affect nerve positioning.
- Genetics: Some individuals might be more genetically predisposed to nerve-related issues.
Diagnosis
The diagnosis of ilioinguinal nerve entrapment typically involves a combination of medical history, physical examination, and possibly imaging studies.
- Medical History:* Your healthcare provider will ask you about your symptoms, when they started, and any relevant medical history or events that might have contributed.
- Physical Examination: The doctor will perform a physical examination to assess the affected area, looking for signs of pain, tenderness, muscle weakness, and any other abnormalities.
- Provocative Tests: Specific tests might be performed to reproduce or worsen your symptoms, helping to identify the involvement of the ilioinguinal nerve.
- Imaging: In some cases, imaging studies like ultrasound, MRI, or CT scan may be ordered to visualize the affected area and rule out other potential causes of your symptoms.
- Nerve Blocks: Nerve blocks, where a local anesthetic is injected near the nerve, can be used as both a diagnostic tool and a temporary treatment to confirm the nerve’s involvement.
- Electrodiagnostic Tests: Electromyography (EMG) and nerve conduction studies (NCS) can help assess nerve function and identify any abnormalities.
Medical Treatment
- Pain Management: Over-the-counter pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), might help manage pain and inflammation
- Medications: In some cases, your doctor might prescribe medications like muscle relaxants or nerve pain medications to alleviate symptoms.
Physiotherapy Treatment
A physical therapist can guide you through exercises to strengthen and stretch the affected muscles, potentially relieving pressure on the nerve. Physiotherapy can play a crucial role in managing ilioinguinal nerve entrapment by addressing muscle imbalances, improving mobility, and reducing nerve compression.
- Stretching Exercises: Gentle stretching of the hip flexors, abdominal muscles, and surrounding muscles can help alleviate tension and pressure on the ilioinguinal nerve.
- Strengthening Exercises: Strengthening weak muscles, especially the core and hip muscles, can provide better support to the affected area and help prevent further nerve irritation.
- Manual Therapy: Techniques such as soft tissue mobilization, myofascial release, and joint mobilizations can help relax muscles and improve tissue flexibility.
- Nerve Gliding Exercises: Specific exercises that involve controlled movements of the affected nerve can help prevent adhesions and improve nerve mobility.
- Posture Correction: Correcting poor posture can relieve pressure on the nerve and promote better alignment of the spine and pelvis.
- Modalities: Modalities like ultrasound, electrical stimulation, or cold packs might be used to reduce pain and inflammation.
- Functional Training: Your physiotherapist can guide you through exercises that mimic real-life movements to ensure the affected area functions well during daily activities.
- Activity Modification: Your physiotherapist may provide guidance on modifying certain activities to avoid exacerbating symptoms.
- Education: Learning about proper body mechanics, ergonomics, and self-care strategies can empower you to manage symptoms effectively.
Exercise
Hip Flexor Stretch:

- Kneel on one knee with the other leg in front, foot flat on the floor.
- Normally push your hips forward until you feel a stretch in the front of your hip.
- Hold a muscle stretch for 20-30 seconds and repeat on both sides.
Piriformis Stretch:

- Lie on your back, and cross one ankle over the opposite knee joint.
- Gently pull the crossed knee toward your chest until you feel a stretch in your buttocks.
- Hold for 20-30 seconds and switch sides.
Supine Leg Slides:
- Lie on your back with your knee flexed and feet flat on the ground.
- Slowly slide one foot out and back while keeping your core engaged.
- Repeat on the other side, alternating for 10-15 time repetitions.
Standing Pelvic Tilt:
- Standing position with your back against a wall and your feet hip-width apart.
- Gently press your lower back into the wall, engaging your abdominal muscles.
- Hold this position for five to 10 seconds, then release the position. Repeat 10-15 times.
- Lie on your side with knees flexed and feet together.
- Keeping your feet touching, lift your top knee while maintaining your pelvis stable.
- Lower the knee back down. Perform 10-15 reps on each side.
Wall Angels:
- Stand with your back against a wall, arms flexed at 90 degrees, and palms facing forward.
- Slowly slide your arms up and down the wall while maintaining contact with your elbow joint, wrist joint, and hands.
- Perform 10-15 reps to improve shoulder muscle and upper back muscle mobility.
Bridge Exercise:

- Lie on your back with your knees flexed and feet flat on the ground.
- Lift your hips off the floor.
- Hold this position for 5 to 10 seconds, then lower your hips. Repeat 10-15 times.
Seated Forward Bend:

- Sit on the floor with your legs straight in front of the patient.
- Slowly bend forward at your hips, reaching your hands toward the patient’s feet.
- Hold the stretch for a few seconds while breathing deeply.
Cat-Cow Stretch:

- Start on the patient’s hands and knees in a tabletop position.
- Inhale as you arch your back and lift your head area(cow pose), then exhale as you round your back and tuck your chin(cat pose).
- Repeat the movement for 10-15 cycles.
Standing Hip Abduction:

- Stand upright, holding onto a stable object surface for support.
- Lift one leg out to the other side, keeping it straight, and then lower it back down.
- Perform 10-15 repetitions on both legs.
Lying Leg Raise:
- Lie on the patient’s back with one leg straight and the other leg flexed.
- Lift the straight leg a few inches off the ground, engaging your core.
- Lower the leg back down. Perform 10-15 reps on each leg.
Standing Hip Extension:
- Stand upright, holding onto a stable object surface for support.
- Extend one leg straight behind you, squeezing your glute muscle at the top.
- Lower the leg back down. Do 10-15 repetitions on both legs.
Child’s Pose Stretch:

- Start on the patient’s hands and knees, then sit back on your heels with your arms stretched forward.
- Allow your forehead to rest on the ground and feel the stretch in your lower back and hips.
Quad Stretch:
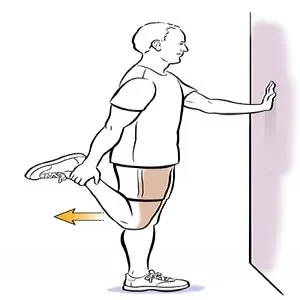
- Stand on one leg and grab your opposite ankle behind the patient’s.
- Gently pull your ankle toward your glutes muscle while keeping your knees together.
- Hold the stretch for 20-30 seconds on both legs.
Isometric Core Activation:
- Lie on your back with your knees flexed and feet flat on the ground.
- Press your lower back into the ground while engaging your core muscles.
- Hold the muscle contraction for a few seconds and release. Repeat 10-15 times.
Standing Hip Flexor Stretch:
- Stand upright and take a step forward with one leg, keeping the other leg behind the patient’s.
- normally lunge forward, bending the front knee, and tilting your pelvis slightly backward to feel a muscle stretch in the hip flexor of the back leg.
- Hold the muscle stretch for 20-30 seconds on each side.
Knee-to-Chest Stretch:
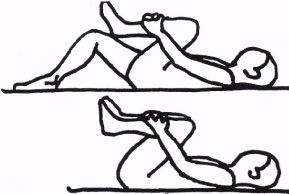
- Lie on your back and bring one knee toward the patient’s chest, holding it with your hands.
- Feel a gentle stretch in your lower back muscles and hip muscles.
- Hold the muscle stretch for 20-30 seconds on both sides.
Sitting Pelvic Tilt:

- Sit on a chair with feet flat on the ground and hands on your hips.
- Normally tilt your pelvis forward and backward while maintaining a neutral spine.
- Repeat this activity for 10-15 repetitions.
Side-Lying Leg Lift:
- Lie on the patient’s side with your legs straight.
- Raise the top leg upward while keeping it straight, then lower it back down.
- Perform 10-15 reps on both sides.
Standing Calf Stretch:

- Stand facing a wall, placing your hands against the wall for support.
- Step one foot back while keeping the heel on the floor, feeling the stretch in your calf muscle.
- Hold the muscle stretch for 20-30 seconds on each leg.
Seated Groin Stretch:

- The soles of your feet should touch as you sit down on the ground.
- Gently press down on the patient’s knees with your hands to feel a stretch in the patient’s groin area.
- Hold the muscle stretch for 20-30 seconds.
Trunk Rotation Stretch:

- Sit or lie down and bend your knee joint.
- Normally rotate your knees from side to side, allowing your lower back to rotate as well.
- Perform this activity for 10-15 reps on both sides.
Surgery
Surgery might be considered as a treatment option for ilioinguinal nerve entrapment when conservative approaches haven’t provided relief and the condition significantly impairs your quality of life. Surgical procedures aim to release the compressed or entrapped nerve, alleviate symptoms, and address any underlying causes. Surgical intervention might be considered if conservative measures don’t provide relief. Surgery aims to release the entrapped nerve or repair underlying issues like hernias. Here are a few surgical options that might be discussed
Nerve Decompression: This procedure involves surgically releasing any structures or tissues that are compressing the ilioinguinal nerve. The surgeon carefully identifies and frees the nerve from entrapment sites.
Hernia Repair: If a hernia is contributing to the nerve entrapment, a surgical repair of the hernia might be performed. During this procedure, the hernia is corrected, and the nerve is released if necessary.
Laparoscopic Surgery: Minimally invasive laparoscopic techniques may be used to release the entrapped nerve. This approach typically involves smaller incisions and quicker recovery compared to open surgery.
Neurectomy: In some cases, when other treatments have failed, a neurectomy might be considered. This involves surgically removing a segment of the ilioinguinal nerve. However, this procedure can result in permanent numbness in the affected area.
Exploratory Surgery: In situations where the exact cause of nerve entrapment is uncertain, exploratory surgery might be performed to identify and address the underlying issue.
Complication
- Pain: The most common symptom is pain in the distribution area of the nerve, which includes the upper inner thigh, mons pubis, and genitalia. The ache can vary in intensity from mild pain to severe pain.
- Sensory Disturbances: Patients might experience tingling, numbness, or altered sensation in the affected areas due to nerve dysfunction.
- Reduced Function: The pain and sensory disturbances can potentially limit movement and function in the affected leg and pelvic region.
- Quality of Life: Chronic pain and discomfort can significantly impact a person’s quality of life, affecting daily activities, sleep, and overall well-being.
- Inflammation: Nerve entrapment can lead to inflammation around the nerve, causing localized swelling and discomfort.
- Psychological Impact: Long-term pain and discomfort can lead to psychological distress, including anxiety and depression.
- Recurrent Symptoms: Even after treatments, there’s a possibility of recurrent symptoms if the underlying cause of nerve entrapment isn’t fully addressed.
Prevention
- Proper Technique and Posture: When engaging in activities that involve repetitive movements, ensure you use proper techniques and maintain good posture to minimize strain on the pelvic and inguinal areas.
- Avoid Excessive Strain: Be mindful of activities that put excessive strain on the groin or pelvic region, and take breaks or modify movements as needed.
- Weight Management: Maintaining a healthy weight can reduce pressure on the nerves in the pelvic area and decrease the risk of nerve entrapment.
- Post-Surgery Care: If you’ve had pelvic or inguinal surgery, follow post-operative instructions carefully to promote healing and reduce the risk of complications.
- Injury Prevention: Take precautions to prevent injuries to the pelvic region, such as using proper safety equipment during sports or activities.
- Listen to Your Body: If you experience any unusual sensations, pain, or discomfort in the pelvic or groin area, don’t ignore them. Seek medical attention if symptoms persist.
- Warm-up and Stretching: Before engaging in physical activities, warm up your muscles and perform gentle stretches to prepare your body for movement.
- Healthy Lifestyle: Maintain a healthy lifestyle with regular exercise, balanced nutrition, and proper hydration to support overall well-being.
Home Advice
- Rest and Avoid Aggravating Activities: Give your body time to rest and avoid activities that worsen your symptoms.
- Ice Packs: Applying ice packs wrapped in a cloth to the affected area for 15-20 minutes at a time can help reduce inflammation and provide temporary relief from pain.
- Over-the-Counter Pain Relief: Non-prescription pain relievers, like acetaminophen or ibuprofen (if not contraindicated for you), may help alleviate mild pain and discomfort. Remember to follow recommended dosages.
- Gentle Stretching: Some gentle and appropriate stretches can help alleviate tension and promote flexibility in the pelvic and groin area. Consult a physical therapist or healthcare provider for suitable stretches.
- Posture Correction: Maintain proper posture to avoid unnecessary strain on the affected area. Sit and stand position with a neutral spine position.
- Supportive Clothing: Wearing supportive clothing, such as a supportive belt or compression shorts, may help provide some relief by reducing pressure on the affected area.
- Mindfulness Techniques: Practices like deep breathing, meditation, or relaxation exercises can help manage pain and reduce the stress associated with discomfort.
- Warm Compresses: Alternating between warm and cold compresses may provide relief by relaxing muscles and reducing inflammation.
FAQ
What causes nerve entrapment?
Acute entrapment neuropathy is usually caused by an injury, such as a sprain or fracture, that moves bones or ligaments and causes them to compress the nerve. Chronic compression neuropathy is usually caused by repetitive motion that affects the area where the nerve passes through a narrow space.
What are the complications of an ilioinguinal nerve block?
Potential risks include, but are not limited to: vasovagal reaction (fainting), new or increased pain, infection, bleeding, permanent skin changes, allergic or unexpected drug reactions with minor or serious consequences, and unintended nerve damage.
What muscles does the ilioinguinal nerve supply?
The transverse abdominis muscles and internal oblique muscles are innervated by the ilioinguinal nerve. It provides sensory nerve to the region of the upper anteromedial region of the thigh.
What are the symptoms of ilioinguinal nerve entrapment?
Symptoms of ilioinguinal nerve entrapment may involve skin hyperesthesia or hypoesthesia along the inguinal ligament. The sensation may radiate to the lower abdomen area. The pain can be localized in the medial groin, labia majora, or the scrotum and inner thigh.
What are the risks of nerve block anesthesia?
Risks include block failure, bleeding, infection, damage to surrounding structures, permanent nerve damage, and intravenous absorption of the local anesthetic causing systemic toxicity.
What is the distribution of the ilioinguinal nerve?
The ilioinguinal nerve provides a skin nerve to the upper medial part of the thigh and: in men, also to the skin over the front of the scrotum and the root of the penis. in women, it also treats the skin of the front third of the labia and the base of the clitoris