Quadriplegia
Table of Contents
What is Quadriplegia?
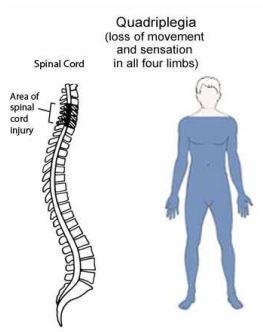
Quadriplegia is a type of paralysis that starts at the neck and spreads to the entire body, including all of the limbs. Numerous factors can lead to quadriplegia, but the most common one is a spinal cord injury in the neck.
Tetraplegia, often known as quadriplegia (the word “quad” originates from the Latin for “four”), is a form of paralysis that affects the torso in addition to all four limbs. Many tetraplegics are fully immobile, and the majority of them experience severe paralysis below the neck.
This kind of paralysis is generally caused by damage high up in the spinal cord, typically in the cervical spine between C1 and C7. The intensity of the injury will expand the damage’s scope. In fact, spinal cord lesions to the C1 and C2 vertebrae commonly result in rapid death because they impair the capacity to control respiration and other essential processes.
The majority of quadriplegics have totally healthy (though slightly atrophied) arms and legs, contrary to what you might think as you may presume that harm to the arms and legs is necessary for complete paralysis. Instead, the problem usually begins in the brain, spinal cord, or both. The spinal cord is used to carry signals to and from the brain, and once the brain processes them, fresh signals are sent out by the spinal cord. Therefore, a spinal cord injury prevents the brain from sending and receiving messages, whereas a brain injury inhibits the brain’s ability to comprehend these signals.
Think of it as being similar to a computer: the CPU and motherboard are the brains that receive and process signals, and the cables that connect the motherboard to the keyboard, mouse, printer, monitor, etc. are the nerves in the spinal cord that connect to the various sections of the body. If the wires are cut or even slightly damaged, the computer may not operate properly. A similar result could also occur if the CPU is damaged.
Type of Spinal cord Injury:
There are five different types of spinal cord injuries:
- Complete spinal cord injury A: this is the most extreme type of injury. The patient has loss of sensation with motor function below the level of injury.
- Incomplete spinal cord injury B: the patient has some sensations. Motor function is limited below the injury.
- Incomplete spinal cord injury C: the patient has some sensation and muscle control, but the muscles are weak and non-functional.
- Incomplete spinal cord injury D: muscles are 75% functional.
- Incomplete spinal cord injury E: minor injury. The patient has almost normal sensations and strength.
Quadriplegia Symptoms
Paralysis may be total or partial. It depends on level of injury and severity of injury of the spinal cord. Other problems may be:
- Loss of bladder or bowel control—incontinence
Loss of sexual function
Trouble breathing
Problems sitting upright
Inactivity can lead to other problems, such as: - Pressure sores
Abnormal muscle tightness (Spastic Quadriplegia)
Pneumonia
Urinary tract infection
Weakened bones
Chronic pain
People may also become depressed because of: - Lack of social and emotional support
Being more dependent on others
The basic symptoms of quadriplegia include:
- Numbness/loss of feeling in the body, particularly in the arms and legs;
- Paralysis of the arms and legs (and major muscles in the torso);
- Urinary retention and bowel dysfunction caused by lack of muscle control;
- Difficulty breathing (some quadriplegics require assisted breathing devices); and
- Trouble sitting upright (because of an inability to balance).
The result of damage below the neck is paraplegia. When there is damage to the skull or neck, quadriplegia results.
Causes of Quadriplegia
Trauma, such as a sports injury, vehicle accident, or fall, is the most frequent cause.
Damage to the brain, cervical spine, or spinal cord can result in quadriplegia. The most frequent cause of spinal injuries is car accidents, while tumors and spinal illnesses can also result in damage. Multiple sclerosis, Guillain-Barré syndrome, and transverse myelitis are among the illnesses that can result in quadriplegia.
Children may have the injuries either before, during, or after delivery. Lack of oxygen in the brain as a result of inadequate oxygen delivery is the most frequent reason. It’s possible that an infectious condition or problems during labor are to cause for the shortage of oxygen.
Quadriplegia could have a variety of causes. The spinal cord is most frequently damaged in the cervical vertebrae, or the C1–C7 segments of the spine that are closest to the skull, as was already mentioned. The following are the leading causes of spinal cord injuries (SCIs), according to data from a 2019 National Spinal Cord Injury Statistical Centre (NSCISC) report:
- Auto Accidents (32.2%)
- Falls (22.9%)
- Gunshot Wounds (15.2%)
- Motorcycle Accidents (6.2%)
- Diving (5.7%)
- Medical/Surgical Complications (2.9%)
- Being Hit by a Flying/Falling Object (2.7%)
- Bicycle Accidents (1.7%)
- Pedestrian Accidents (1.5%)
Brain damage, such as that caused by a traumatic brain injury (TBI), is another potential factor in tetraplegia or quadriplegia. A person’s temperament or capacity to think can alter as a result of brain damage, among other unanticipated consequences.
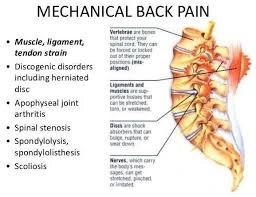
Vertebrae Damage
One of the main reasons for quadriplegia is damage to the spinal cord. Quadriplegia is specifically caused by injury to the cervical region of the spinal cord. Quadriplegia is uncommonly caused by damage to the lower portions of the spine (such as the thoracic or lumbar spinal column), which generally causes paraplegia.
The severity of the effects usually increases with the location of the damage to the cervical spine. Here are a few succinct descriptions of harm to certain cervical spine vertebrae:
C1, C2, C3 Damage
Damage to the vertebrae closest to the skull (the C1, C2, and C3 vertebrae) on the spinal column is more likely to be deadly than damage to the vertebrae further down. C1 and C2 injuries are regarded as very severe since they frequently result in death and may cause breathing difficulties.
Damage at this level is quite likely to cause near-total paralysis in the case of a complete SCI and may call for specialized breathing apparatuses.
C4 Damage
loss of diaphragm control, requiring the use of a ventilator or other breathing devices
Arms, torso, and leg paralysis or restricted range of motion
Bowel and bladder control issues
C5 Damage
The vocal cords may be impacted by damage to the C5 vertebra, which may also cause paralysis in the hands, wrists, and legs.
A person with a C5 spinal injury might have trouble speaking, but they might still be able to breathe on their own.
C6 Damage
It is less likely that injury to the spinal cord below C6 will result in total loss of arm function. An individual with a C6 injury might:
Be unable to move your legs, torso, or hands.
Be unable to manage their bowels or bladder
You have trouble speaking normally
C7 Damage
Quadriplegia due to C7 injury is uncommon without additional aggravating conditions. Instead, those who survive C7 SCI may develop paralysis and/or feel a burning agony in their shoulders, back, and arms.
Conditions that Can Be Inherited and Lead to Quadriplegia
Quadriplegia (and other types of paralysis) can also be brought on by particular illnesses or genetic problems.
The following two conditions can result in quadriplegia:
ALS, or Amyotrophic Lateral Sclerosis. is a well-known illness that renders paralysis permanent. There are two types of ALS, sporadic and familial, according to ALS.org. Despite the fact that sporadic ALS makes up the majority of cases.
A muscle disorder. In contrast to common causes of quadriplegia, muscular dystrophy is not brought on by nervous system impairment.
A muscular dystrophy is a group of diseases that cause progressive weakness and loss of muscle mass. Although messages continue to reach the muscles and nerves, as the illness worsens, the muscles themselves lose the capacity to react to the impulses. As different muscles lose their bulk and strength, this may initially result in a loss of capacity to walk, followed by difficulties moving the arms and breathing. Even without nerve injury, this produces results akin to partial quadriplegia.
Quadriplegia Risk Factors
It’s critical to understand the causes of quadriplegia. What are some of the risk factors, though, that can make someone a quadriplegic? Let’s define a quadriplegia risk factor first.
It’s vital to understand that a risk factor differs from a cause in that it might not directly cause a certain condition to occur. A risk factor may only increase the likelihood that a condition, such as a quadriplegia, will manifest or make it more likely that someone will experience an injury that will result in quadriplegia.
Consider someone falling down a tall ladder to illustrate the distinction between a cause and a risk factor. The faller becomes quadriplegic after the collision destroys their cervical spine and they lose feeling in their arms and legs.
Risk factors for SCIs and TBIs that result in the development of quadriplegia include the following:
Gender. Males are more likely than females to experience an SCI. In reality, the 2019 NSCISC data revealed that whereas 27,453 men experienced SCIs from a variety of causes throughout that time, just 6,672 women did. Injuries that result in quadriplegia may therefore be more likely to occur in men.
Age. Over time, the precise age at which a person is most at risk for an SCI or TBI has changed. The mean “age at injury” (the age of the SCI survivor at the time of their injury), according to NSCISC, was around 28 years old in the late 1970s. The mean age at injury had risen to about 43 years old between 2015 and 2019. Additionally, people’s susceptibility to severe SCIs and TBIs increases with age, especially if they have osteoporosis or other disorders that affect their bone health.
Risky Actions. You run a higher risk of having a spinal cord or brain injury that results in complete paralysis if you dive, drive recklessly (or without seatbelts), or play high-contact sports.
Career Option. Professional athletes in high-contact sports, police officers, and construction workers all have an elevated risk of injury from workplace violence or accidents. They thus run a higher than normal chance of developing quadriplegia as a result.
Family medical background. You face a higher risk of contracting an illness like ALS (also known as Lou Gehrig’s disease) and losing control of your arms and legs if it runs in your family.
Quadriplegia Prevention
It is feasible to prevent quadriplegia to some extent by being aware of the main risk factors. It’s crucial to remember that not all risks can be completely avoided. Quadriplegia can happen to anyone due to a slip and fall, a hereditary illness, or an act of violence committed at random.
The following are some fundamental actions for reducing quadriplegia risk factors:
Having Congenital Diseases Tested. It’s vital to talk to your doctor about your family’s medical history and get screened for any disorders that could run in your family.
Early detection of ALS or other illnesses’ symptoms can have a significant impact on your treatment.
Wearing the proper safety gear.
Wearing the proper safety equipment is crucial whenever possible, whether it be in high-risk job environments, motorcycle sports, or on motorcycles.
Although a concussion is still serious and requires medical attention, wearing a hard hat or helmet could be the difference between severe open head wounds and one!
Avoiding Dangerous Behaviour.
Avoiding actions that could cause substantial bodily harm includes not drinking and driving, diving (particularly in shallow water), and other such activities.
When unsafe circumstances cannot be avoided, the best safety equipment should be employed.
Maintaining a Regular Exercise and Diet Plan.
The state of your bones and muscles can significantly affect how bad an injury will get.
In someone with bone and joint diseases, an impact that would only cause pain in someone with a healthy musculoskeletal system could break bones.
Although it might not be able to stop diseases like osteoporosis, which have a detrimental impact on bone strength, a diet and exercise routine can assist promote bone health.
History of specific genetic nerve illnesses in the family
Cancer history may put pressure on the spinal cord.
Types of Quadriplegia
Many people believe that all quadriplegics are the same and are completely incapable of moving their arms or legs. Quadriplegia comes in a variety of forms, including partial, complete, and spastic quadriplegia, all of which differ significantly from one another.
Incomplete Quadriplegia
In contrast to a person who is completely paralyzed, an “incomplete quadriplegic” may still have some sensation and/or function in their arms or legs. This could apply to incomplete or “partial” SCI, some TBIs, and some inherited quadriplegia-causing diseases.
Depending on the underlying cause, some quadriplegia therapies and exercises may help some persons with incomplete quadriplegia regain some control over their limbs. Others, however, can experience the progression of their illness from incomplete quadriplegia to complete quadriplegia.
Complete Quadriplegia
A complete lack of control over the arms and legs is a feature of complete quadriplegia. With the exception of their head, a person is completely immobile due to this almost complete kind of paralysis.
The complete form of quadriplegia is typically seen as being more severe than the incomplete form.
Traumatic brain injuries or severe, full SCI in the cervical vertebrae are frequent causes of complete quadriplegia.
Although there are still quadriplegia therapy choices, recovery, and exercise will be more challenging for a complete quadriplegic than an incomplete quadriplegic.
Spastic Quadriplegia
Spinal cord and brain damage brought on by trauma or disease frequently have the side effect of spasticity (also known as spastic hypertonia). An individual who is a spastic quadriplegic can have muscle spasms in their paralyzed limbs even if they are unable to voluntarily control their arms or legs.
Spastic hypertonia in quadriplegics can cause hyperactive reflexes or uncontrollable muscle rigidity that makes it challenging to assume a calm posture.
Spasticity may result from neural infections, spinal cysts that developed after an SCI, or other blockages. For this reason, it’s crucial to have a skilled medical professional identify the root cause of the quadriplegia and suggest a suitable course of treatment.
Diagnosing Quadriplegia
The lack of limb function may lead some to believe that it is simple to determine if you have quadriplegia, but in certain cases, the reason for quadriplegia is not so obvious. Early diagnosis can increase your therapeutic options and enhance your general prognosis by treating the underlying causes.
To identify the various causes of quadriplegia, doctors may employ a variety of techniques, such as:
MRI images: MRI scans can be used by doctors to look for anomalies including brain tumors, cysts, and herniated discs in the spinal cord that might be obstructing brain impulses.
Lumbar Puncture (Spinal Taps): Cerebrospinal fluid from the spinal column may need to be removed for analysis and spinal health testing by medical professionals.
Blood test: To check for deficits or to look for genetic markers that might suggest an inherited congenital paralysis problem.
Electromyography (EMG) Tests: To help distinguish between muscle and nerve problems, doctors may do tests on nerve function.
Living with Quadriplegia
Living with quadriplegia can be extremely difficult and call on both the quadriplegic and those around them to make major lifestyle changes.
Quadriplegics frequently depend on helpers for daily tasks like eating, going to the toilet, and moving around since they lack control over their arms and legs. Quadriplegics may be able to steer some motorized wheelchairs with head gestures, but it might take some getting used to.
Due to their condition, quadriplegics will suffer major changes in their everyday activities and even their life expectancy.
Quadriplegia Life Expectancy
The life expectancy of people with quadriplegia may be lower than that of age-matched healthy individuals. For instance, a 15-year-old without an SCI has an average life expectancy of another 64.2 years, according to the NSCISC research. The life expectancy of a 15-year-old with a C1-C4 SCI, which might result in quadriplegia, is around 37.6 years, a decrease of more than 26 years!
Their average life expectancy will only be 19.5 years if the SCI makes them ventilator dependent (needing a respirator to breathe).
Naturally, not every quadriplegic is the same. With some effort, someone with quadriplegia can lead a healthy lifestyle that increases life expectancy. While coping with quadriplegia, it is also possible to have an active life and even accomplish amazing things. Occasionally used somatosensory evoked potentials
Effects of Quadriplegia
Infographic-Quadriplegia-Tetraplegia
In addition to the above list of quadriplegia’s primary symptoms, there are a number of additional side effects that the disorder can induce. Tetraplegia and quadriplegia frequently have the following effects:
The Growth of Wounds.
Sores might develop if a person is unable to shift or modify their position in a chair or bed for an extended period of time. Secondary infections may result from this in turn.
Legs with spasms.
It’s possible for some quadriplegics to have uncontrollable muscle spasms in their arms or legs. There could be incomplete nerve injury as a result of this or additional factors that caused the quadriplegia.
UTIs, or urinary tract infections.
Infections of the urinary tract (UTIs) are a frequent side effect of quadriplegia. Loss of bladder control makes it challenging to eliminate debris from the urethra, which increases the risk of infections.
muscle wasting.
Quadriplegics frequently have muscular atrophy, or the loss of muscle mass, in their arms and legs because they are unable to move. Physical therapy and other exercises can lessen this quadriplegia side effect.
Pain that is persistent.
Pain is frequently experienced by SCI and TBI survivors as a result of disrupted nerve connections. But it’s challenging to generalize about this side effect because everyone’s level of discomfort is different.
Bodily Awareness Challenges.
Naturally, a loss of feeling might make it difficult always to know where one’s limbs are.
This may obstruct your ability to perceive space.
Quadriplegics who cannot walk or exercise may gain weight quickly due to their reduced capacity to burn calories.
Challenges of quadriplegia
Due to the fact that quadriplegia affects the body from the neck down, it can greatly limit one’s independence.
A person with quadriplegia may go through the following depending on the severity of their paralysis:
The presence or absence of issues with arm and hand function the ability to communicate, swallow, or breathe on their own
Difficulty getting out of bed or a wheelchair without help or the use of a device difficulty carrying out daily activities like showering, dressing, and eating
Pressure ulcers, commonly known as bedsores or pressure sores, cause bone and muscle deterioration
Treatments
Although paralysis cannot be cured, some persons may eventually regain full or partial control over the paralyzed parts.
Currently, available therapies can:
- Lessen the long-term impact of injury to the central nervous
- Any disease’s development slowly
- Prevent and control extra issues
- Increase a person’s standard of living
Among the medical procedures for paraplegia and quadriplegia are:
Surgical procedures
The following basic causes of central nervous system injury may be treated by emergency surgery:
Edema surrounding the brain or spinal cord due to clogged or leaking arteries
Vertebral fractures or dislocations of spinal cord tumors
If a patient experiences paralysis-related consequences including pressure ulcers, muscular damage, or persistent pain, doctors may advise surgery.
Medications
The following medicines are some that doctors may suggest:
Antibiotics, to reduce the chance of infection corticosteroids, to lessen inflammation in the nerves
Blood-thinning medications to avoid blood clots
The rehabilitation procedure is a crucial step in the healing process.
Through repetitive motions, physical therapy focuses on rebuilding muscle strength and function. Physical therapists can suggest specific workouts and methods for maintaining an active lifestyle.
While occupational therapy teaches patients how to combine employment and self-care, speech therapy can help patients regain or retain their verbal communication skills.
Support and coping
A person’s quality of life can be substantially changed by paralysis. Researchers assessed the quality of life for 84 patients with traumatic paraplegia in a study published in 2016 (Trusted Source). Each participant was invited to fill out a questionnaire and participate in a face-to-face interview.
The study participants’ ratings for their physical health, psychological well-being, and social interactions were worse than those of the general population. However, because more than 90% of the participants were men, the study cohort was not typical of the broader population.
Those who are paralyzed or quadriplegic may gain from:
Educating oneself on the many rehabilitation and treatment choices and implementing adjustments that improve mobility, such as placing adaptable devices around the home
Exercising frequently and without reluctance requesting assistance from family, friends, and medical experts joining a local or online support group to interact with other paralyzed individuals
Physiotherapy Treatment
The severity and type of spinal cord injury determine the acute care and rehabilitation of SCI. The rehabilitation process often begins in the acute care setting for people with SCI, followed by extended care in a specialized Spinal Injury Unit.
People with SCI frequently need initial treatment in an intensive care unit. The duration of inpatient management can range from 8 to 24 weeks, with subsequent outpatient rehabilitation lasting 3 to 12 months. Annual medical and functional reviews are typically conducted after this.
A multidisciplinary approach is necessary for the complex and lifelong management of a person with SCI.
The person with a spinal cord injury should be able to lead as complete and independent a life as possible with the help of a functional, goal-oriented, multidisciplinary rehabilitation plan.
Under the direction of a Physiatrist or Rehabilitation Physician, a team of health and social care professionals, including physiotherapy, occupational therapist, speech and language therapist, rehabilitation nurses, social workers, and psychologists, decide on goals with the individual and create a discharge plan that is suitable for their level of injury and circumstances.
The following are the top five steps in managing people with SCI:
Evaluating disabilities, activity limits, and participation limitations
Setting objectives that take activity restrictions and participation restrictions into account
Identifying the main limitations that prevent goal achievement
Identifying and delivering physiotherapy treatments (pain management, cardiovascular fitness, joint Mobility, motor skill development, and strengthening)
Evaluating the effectiveness of therapies
Acute, Sub-acute, Chronic (Long Term), and Rehabilitation.
Rehabilitation strategies throughout the acute and subacute periods of therapy provide a greater emphasis on preventing subsequent problems, encouraging neuro healing, resolving underlying deficits, and maximizing function. Approaches that are compensatory or supportive are frequently used during the chronic phase.
Acute Phase
All members of the multidisciplinary team are involved in preventing complications brought on by spinal instability or neurological deterioration. In the initial stages following an accident, physical therapy management focuses primarily on the prevention and treatment of respiratory and circulatory issues, as well as reducing the effects of immobilization on the person, such as the development of pressure ulcers and contractures.
Objectives
Following are some treatment goals for the acute phase:
To implement a preventative respiratory regimen to manage respiratory issues and any sequelae from the spinal cord injury or related disorders, such as reducing the likelihood of atelectasis and improving secretion clearance to, whenever possible, establish an independent respiratory status.
To monitor and manage the neurological status, maintain and strengthen all innervated muscle groups.
To facilitate functional patterns of activity, to maintain the full range of motion of all joints within the limitations determined by the stability of the fracture, to support and educate the patient, carers, family, and staff
Respiratory Performance
Hypoventilation, atelectasis, secretory retention, and pneumonia are examples of frequent secondary consequences.
Due to a disruption in the spinal cord related to the neurological level of the SCI, respiratory function is impacted.
C3-5 Diaphragm, C3-8 Scalenes, C5-T1 Pectoralis, T1-11 Intercostalis, and T6-12 Abdominals are the levels of innervations.
While most people with C4 tetraplegia can breathe on their own, those with C1-3 tetraplegia need mechanical ventilation.
Despite being able to breathe on their own, people with SCI C4 to T12 may still have diminished vital capacity and have trouble raising intra-abdominal pressure for a productive cough or other forced-expiratory methods (FETs).
Secretion clearing and more vigorous ventilatory procedures should always be a part of physical therapy therapies.
Techniques for clearing secretions include suctioning, postural drainage, vibrations, and shaking.
Abdominal binders, posture, deep breathing exercises, incentive spirometry, and inspiratory muscle training are treatments to increase ventilation. Bi-level positive airway pressure (BPAP) and continuous positive airway pressure (CPAP) are two additional pieces of medical equipment frequently used to enhance ventilation.
All-joint range of motion (FROM) preserving and boosting the strength of innervated muscles
Clinical studies have shown that functional strength training and progressive resistance training are effective ways to maintain and strengthen innervated muscle groups.
Dosage for progressive resistance training (strengthening):
8–12 rep sets, with one–three sets in between, with a one–minute break
2-3 times per week, load 60-70% of one rep maximum
Reduce the load and up the repetitions to focus on endurance. to immobility and improper placement, a reduced range of motion (ROM) can cause contractures as well as an increase in tone and spasticity.
Passive stretches, placement in the lengthened posture, and other standard hypertonic treatment methods like compression, heat, and continuous deep pressure should all be used in the course of treatment.
Quadriplegia Exercises
Exercises for quadriplegics can help prevent sores, prevent muscle atrophy from inactivity, and relieve the pain caused by spastic muscles. Additionally, it can support both physical and emotional health.
However, for those who are unable to move their arms or legs independently, exercise is intrinsically challenging.
It may be beneficial in this situation to visit an activity-based therapy facility where trainers can suggest safe activities or assist people with paralysis in moving their uncontrollable limbs. In addition to the exercises performed at the facility, certain therapists might be able to advise lifestyle modifications that are crucial for your health and well-being.
Pressure ulcer prevention
When resting supine, the occiput, scapulas, sacrum, and heels are vulnerable to pressure ulcers. While the malleoli and greater trochanter are more vulnerable to side-lying.
Interventions in the acute phase include diet, monitoring, and passive pressure treatment techniques such as frequent rolling and mobilizing programs.
Individuals will later be taught how to use frequent self-lift techniques to release pressure during the sub-acute and long-term stages.
Sub-acute (Rehabilitation) Phase
Although it is better to address a person’s rehabilitation needs at a specialized Spinal Cord Injury Unit, rehabilitation frequently gets started in an acute or trauma hospital while the person is waiting to be transferred to a Spinal Injuries Unit.
The entire person must be taken into account throughout rehabilitation, including their physical, psychological, occupational, and social backgrounds. The purpose of the goal-directed, time-limited rehabilitation approach is to promote maximum independence and the best possible reintegration back into the person’s preferred community role and way of life.
The International Classification of Functioning, Disability, and Health (ICF) include several domains, including body function and structure, activity limitation, and participation, and physical therapy is a crucial part of the recovery process after spinal cord injury. Many interventions are aimed at preventing rather than treating impairments, activity limitations, and participation restrictions.
Management now has a primary emphasis on quality of life, which includes involvement in the community, productive employment, interpersonal connections, and leisure activities.
Objectives
The following are some of the rehabilitation phase’s treatment goals:
To develop an interdisciplinary approach that is patient-centered, thorough, and coordinated to treat physical motor function activities with early intervention and management to avoid subsequent issues
To increase a person’s independence in daily activities like eating, dressing, grooming, and mobility in order to achieve functional independence, whether through the use of physical or verbal aids.
This independence will help the person achieve and maintain successful reintegration into the community.
Physiotherapists use a variety of therapeutic techniques based on the severity and kind of the injury throughout recovery. For patients with high levels of tetraplegia, range of motion/stretching, strengthening, and transfers were the three most frequent individual therapy activities; for patients with low levels of tetraplegia, transfers took up more time than strengthening. Similar to this, transfers were the most popular individual physiotherapy exercises among paraplegic patients, followed by a range of motion/stretching and strengthening.
Variable motor tasks are performed differently by people with varying levels of SCI, so it’s crucial for physiotherapists to know what abilities are possible given the SCI level. To accomplish tasks as efficiently as possible, all motor tasks should be broken down into smaller tasks. Individuals must possess the necessary strength, balance, range of motion, and knowledge or ability for a particular motor activity in order to accomplish motor tasks successfully. Through consistent, progress-oriented training, all these objectives are achievable.
Bed mobility and transfers
Five motor skills can be attained by C6 and lower level SCI;
Moving from supine to long sitting by rolling (with the help of momentum) and elevating vertically while unsupported sitting (both short and long sitting) transfers.
These five motor skills are still achievable with minor changes even with C6 tetraplegia. C6 tetraplegia should externally rotate their shoulders and swing their arms across their bodies during rolling rather than overhead.
To maintain balance while sitting unsupported, C6 tetraplegics should externally rotate their shoulders and lock their elbows in extension. With hands placed anterior to the pelvis, passively extending the elbows, externally rotating the shoulders, and depressing the shoulders to bear weight can help people with C6 tetraplegia move objects vertically.
Wheelchair (WC) mobility
Tetraplegic patients with C1-4 need motorized toilets. Sip and puff, head array, or chin movements can all be used to regulate these WCs.
The majority of people with C5 tetraplegia operate powered toilets with hand motions.
The majority of people with C6–8 tetraplegia can independently move around with a manual WC; alternatively, they may utilize a hand-controlled WC.
A manual WC will let those with SCI lower than C8 independently move around.
People with SCI need to be introduced to their new kind of mobilization. To ensure safe and independent mobility, it’s crucial to practice turning, opening, and closing doors, moving up and down slopes, moving around and over obstacles and moving both indoors and outdoors.
The latest study’s findings imply the need for the structure and content of future fall prevention methods for wheelchair users. Participants with SCI predict the importance of initiatives that go beyond the tactics already available, according to the study’s findings. By gathering feedback from wheelchair users with SCI who live in the community, more study is needed to assess the effectiveness of certain fall prevention efforts.
Gait and standing
In patients with an AIS D spinal cord injury, gait training, strengthening, and balance exercises were the most frequently used physiotherapy techniques.
The most frequent group therapy activity across all severity levels and forms of spinal cord injury was general strengthening.
The ability to stand or walk depends on a variety of conditions, but even if independent standing is unlikely to ever be possible, there are several advantages to standing.
Orthostatic hypotension, bone mineral density, spasticity, and bladder, and bowel function are a few advantages. Utilizing aids like tilt tables, standing toilets, and/or standing frames, one can stand. Some paraplegics may be able to stand in parallel bars with the aid of knee-extension orthoses or splints.
Using orthoses and walking aids like knee-ankle-foot and hip-knee-ankle-foot orthoses, people with total paraplegia to partially paralyzed lower extremities can learn to walk again.
Other crucial elements of recovery are;
Cardiovascular fitness and pain management.
Long Term Phase
Depending on the severity and type of the lesion, people who have suffered a spinal cord injury may have a wide range of complex needs and long-term limitations in their ability to live independently, drive or use public transportation, go back to work or school, or engage in recreational and social activities. To satisfy the long-term and ongoing needs of people with spinal cord injuries, integrated community rehabilitation programs, and long-term support are necessary for successful long-term treatment. In order to coordinate care after initial rehabilitation and ensure ongoing individualized case management for patients with complex or ongoing needs, best practices in long-term management include active case management with case managers who have the necessary training, clinical expertise, and service knowledge.
Low self-efficacy of the patients/family members appears to be a risk factor for adjustment problems in people with spinal cord injuries, according to a prospective longitudinal study, which points to the need for screening of patients and their family members efficacy to help prevent personal and family adjustment problems.
Objectives
The following are among the long-term phase’s treatment goals:
to reach the high mobility goals necessary for community involvement and function recovery monitoring
to strengthen family and carer education
Quadriplegia Related other Therapies
There isn’t a precise treatment at the moment; it all depends on how severe the damage is and how the patient is doing. Different bodily components’ loss of sensitivity and function are addressed.
The major goals of treating spinal cord injuries are to stop more damage from occurring and to return the patient to an active lifestyle as quickly as feasible.
Some treatments may include:
- pulmonary care
- Skincare and skin management
- exercises that increase flexibility and power
Workplace therapy
Strategies for bladder and bowel control
Quadriplegia is often not curable with treatment, despite the fact that some quadriplegics notice significant improvements in their symptoms.
This means that very few quadriplegics will ever regain full control of their limbs and that no surgical technique, medication, or kind of rehabilitation will guarantee a return of function in the arms and legs.
Instead, quadriplegia therapies focus on enhancing the patient’s long-term outlook, lowering immediate dangers to their life and health, and “teaching” the brain and spinal cord how to compensate for the injury. Options for therapy include:
Operations on the spinal cord and brain to remove obstructions, stop bleeding, and control any edema.
medication to lower the chance of infection; also, you can take other medicines such as blood thinners or blood pressure pills.
Training on your legal rights under the Americans With Disabilities Act and other pertinent statutes, as well as information about quadriplegia. Some rehabilitation centers also provide instruction in occupational skills.
- Support and education for families.
- You can keep or restore your ability to talk by receiving speech and language therapy.
- You’ll need physical treatment to get back to work.
- Exercise treatment to maintain your body’s health at its best.
To cope with the social and psychological impacts of quadriplegia, seek out psychotherapy. Additionally, your doctor might suggest medications like antidepressants.
Involvement in support groups.
- Physical therapy: to build strength and become familiar with assistive technology
- Occupational therapy can help with self-care and daily tasks.
- Speech therapy can assist with speaking and swallowing.
- Psychological counseling to offer support.
Summary
Loss of sensation and movement in both legs, as well as occasionally a portion of the lower abdomen, is referred to as paraplegia. All four limbs and, sporadically, portions of the chest, belly, and back are affected by quadriplegia.
Both of these types of paralysis are frequently brought on by spinal cord injuries. Trauma, such as that received in a vehicle accident, or a medical issue, like a stroke, may be the root of the issue.
The physical health and general quality of life of a person can be significantly impacted by paralysis.
Although it cannot be cured, there are a number of therapies and management techniques that may allow some people to restore partial or full control over the affected areas.