What Are The Most Common Causes of Acute Pancreatitis
On This Page: Acute Pancreatitis
Jump To Section
- Exocrine Acute Pancreatitis
- What is Acute Pancreatitis?
- The Main Causes of Acute Pancreatitis
- Other Causes of Acute Pancreatitis
- Symptoms of Acute Pancreatitis
- Acute Pancreatitis Risk Factors
- Diet Considerations For those with Acute Pancreatitis
- Management, Treatment, and Pain Control of Acute Pancreatitis
Acute Pancreatitis
January 2022
Exocrine Acute Pancreatitis
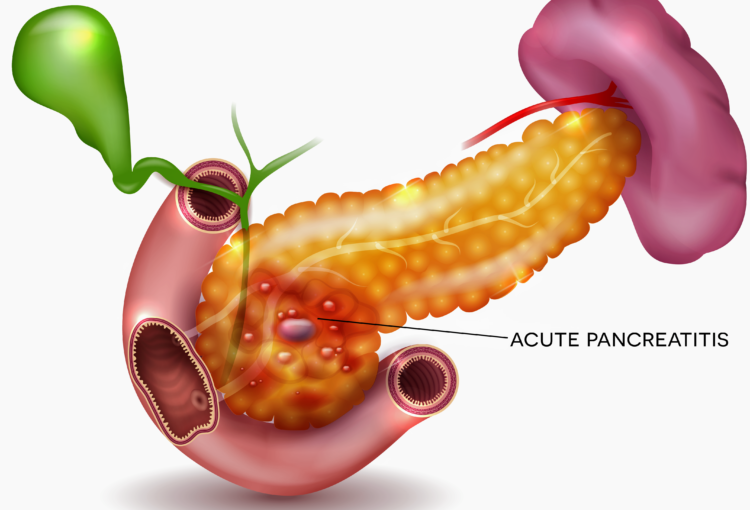
Sometimes referred to as “exocrine acute pancreatitis“, acute pancreatitis can be described as a severe inflammation of pancreas that brings intense pain. Acute pancreatitis can strike suddenly, particularly after eating a meal and associated changes in blood sugar levels. Since the pancreas is sandwiched between the back of the stomach and the spine, the intense pain will come from the mid-abdomen stomach area and the pain will usually radiate to the back.
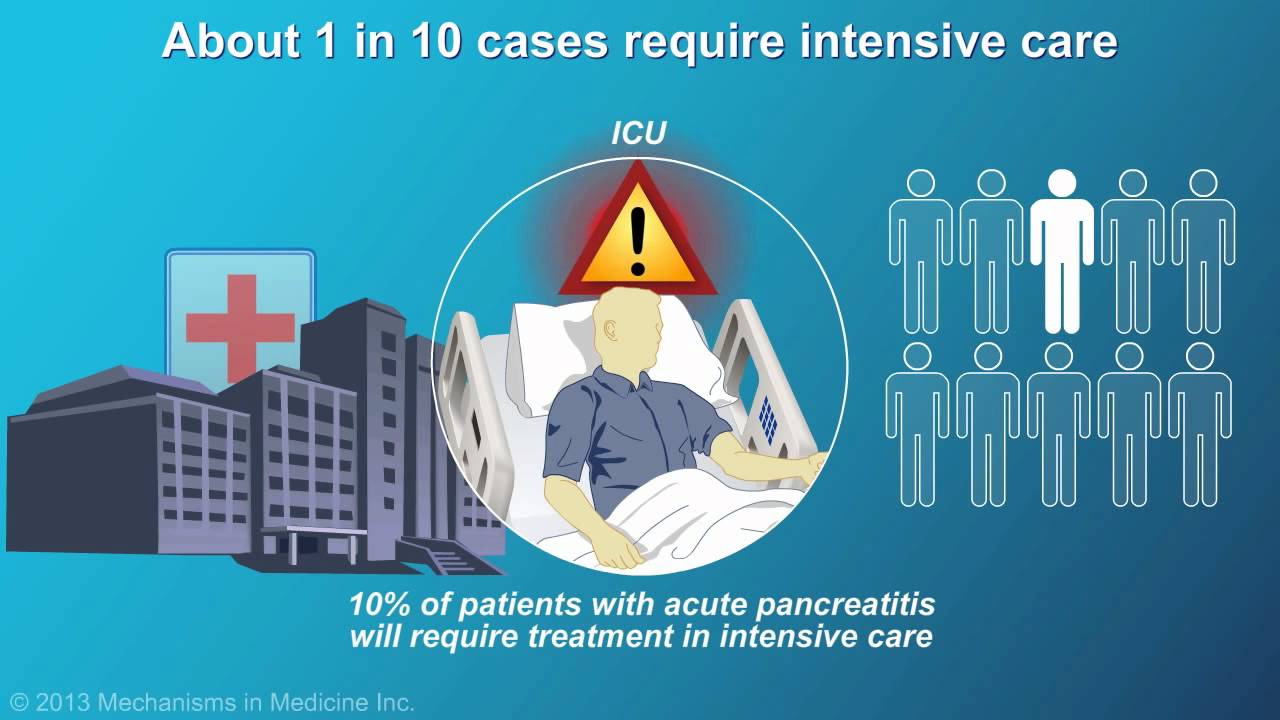
Although acute pancreatitis can recur, most of the time it is a single occurrence depending upon the original cause. The national pancreas foundation notes that it can become deadly with a mortality rate of up to 10% although most bouts can be controlled over a few days in the hospital with proper treatment. Acute Pancreatitis is very similar to Chronic Pancreatitis. Although both can be extremely painful pancreatic diseases, the chronic version is most often recurring and can progressively reach a point of complete destruction of the pancreas.
What is Acute Pancreatitis?
Acute pancreatitis is a very painful inflammation of the pancreas. It occurs in the “Exocrine Portion” of the pancreas which produces digestive enzymes and digestive juices. When the enzymes are initially created, they remain in an “inactive” state while still in the pancreas. Remaining in their inactive state means they are incapable of digesting food until they enter the the small intestine via the pancreatic duct where they “activated” to begin the digestive process within the small intestine. The digestive process breaks-down food into the nutrients of fats, proteins, and carbohydrates which are transformed in sugar (glucose).
If the normal digestion process fails, the digestive enzymes can prematurely activate while still in the pancreas, or the activated enzymes that have entered the small intestine can push the fluids back into the pancreatic duct. Severe inflammation is caused when the prematurely activated enzymes actually begin to digest the pancreas itself. The malfunction of the normal process will cause “Acute Pancreatitis”. Sometimes just a limited amount of activated digestive enzymes remain the the small intestine and malnutrition ensues when only small portions of food are broken-down into nutrients. This malfunction can heighten the risk of becoming pancreatic cancer.
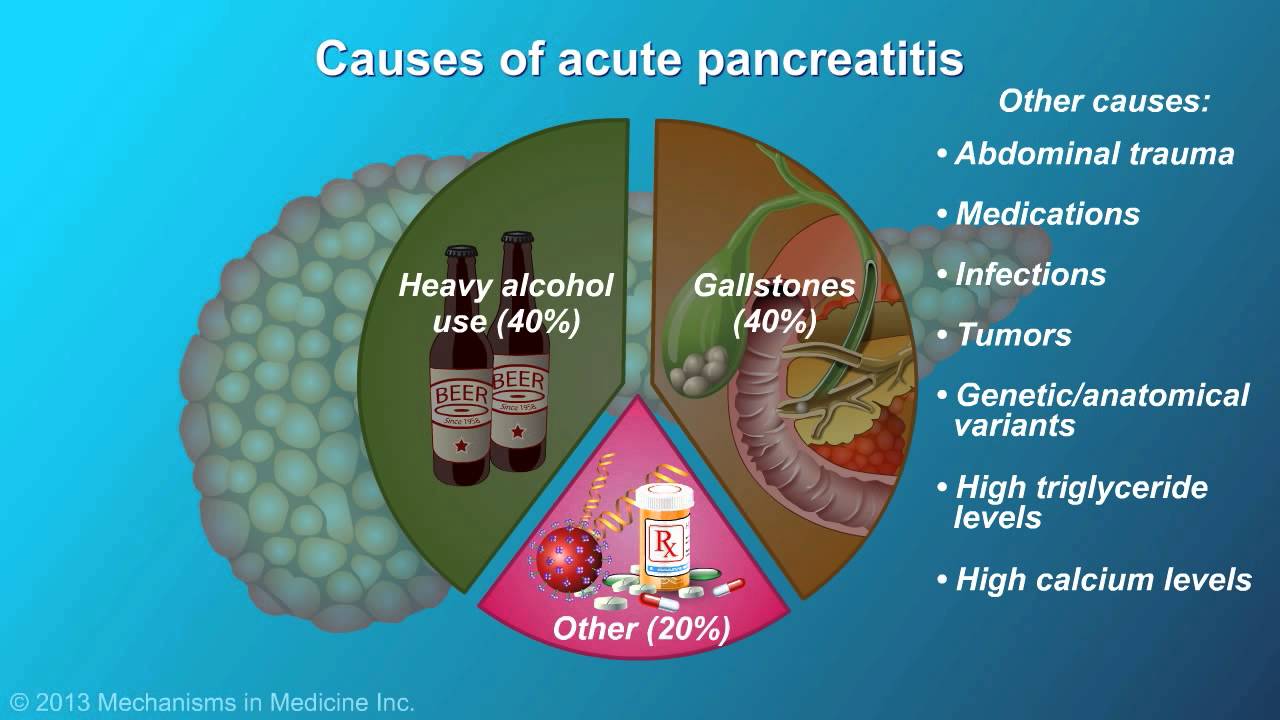
The Main Causes of Acute Pancreatitis
The most common causes of acute pancreatitis are gallstones and heavy alcohol use are the primary causes of acute pancreatitis, together accounting for about 80% of cases. Gallstones, a disorder of the gallbladder, can obstruct the common bile duct, which also serves as the channel for pancreatic enzymes. This obstruction leads to the accumulation and activation of digestive enzymes within the pancreas, which instead of allowing your body to digest food, causes the pancreas to digest itself and resulting in inflammation. Heavy alcohol use is another major cause. Although the exact mechanism is unclear, it’s hypothesized that alcohol or its byproducts may trigger an inflammatory response or activate digestive enzymes within the pancreas. Scientists estimate that heavy alcohol use is responsible for about half of both acute and chronic pancreatitis cases.
The relationship between alcohol and pancreatitis is particularly complex. While the precise reasons for alcohol-induced pancreatitis remain a subject of study, the detrimental effects of alcohol on the pancreas are evident. Prolonged heavy drinking can lead to repeated instances of acute pancreatitis, which over time may evolve into chronic pancreatitis. This transition underscores the importance of managing alcohol consumption as a preventive measure against the development of pancreatitis. The impact of gallstones is more direct, with physical blockage causing immediate distress to the pancreas, often necessitating medical intervention to resolve the blockage and alleviate the condition.
Other Causes of Acute Pancreatitis
Beyond gallstones and alcohol, there are several other causes of acute pancreatitis, though they are less prevalent, accounting for around 20% of cases. These include infections, particularly viral ones, autoimmune diseases, hereditary pancreatitis due to a family history of pancreatic abnormalities, complications related to cystic fibrosis, elevated blood levels of triglycerides (hypertriglyceridemia), and high blood calcium levels (hypercalcemia). Other factors like reduced blood supply to the pancreas (ischemia), cancer, traumatic injuries to the pancreas, and certain medications that irritate the pancreas can also trigger acute pancreatitis.
In some cases, the cause of acute pancreatitis remains unidentified. This uncertainty can complicate treatment and management, as understanding the underlying cause is crucial for targeted interventions. The diversity of these causes highlights the complexity of the pancreas’s role in the body and its susceptibility to a range of disturbances. From genetic predispositions to environmental factors like medication reactions, the potential triggers for acute pancreatitis are varied, making it a challenging condition to both predict and manage effectively.
Acute Pancreatitis Symptoms
The hallmark symptom of acute pancreatitis is intense abdominal pain, which might be moderate to severe and often radiates to the back. This pain can have a penetrating quality and is generally more severe in acute cases. The abdomen may be tender to touch. Chronic pancreatitis presents a different pattern of pain, which may vary in intensity and often does not completely subside, becoming more noticeable after eating. Other symptoms of acute pancreatitis include nausea, vomiting, an accelerated heart rate, rapid, shallow breathing, and fever, reflecting the body’s response to the inflammation of the pancreas.
Weight loss without trying could indicate the pancreas is not producing enough digestive enzymes. If your stool shows an unusual amount of partly digested food would be an early warning sign. Nausea, especially when accompanied with vomiting and oily and smelly stool (steatorrhea) can also be a symptoms of acute pancreatitis. If symptoms and pain persist, seek immediate medical intervention.
Acute pancreatitis is considered a serious and deadly disease and generally requires immediate medical intervention with hospital admission to confirm an acute pancreatitis diagnosis. If confirmed, vitally necessary treatments could begin immediately. Studies show there is a link between acute pancreatitis and pancreatic cancer. It must be detected as early as possible when it is most treatable.
Acute Pancreatitis Risk Factors
Among the risk factors of acute pancreatitis is increasing age and abuse of alcoholic beverages. Some studies show that Type 2 Diabetes and Celiac Disease can increase the risk of acute pancreatitis 3-fold versus the general population. Obesity not only is considered a risk factor but being significantly overweight could increase the severity of intense pain and symptoms.
The identification and management of these risk factors are essential in preventing the onset and recurrence of acute pancreatitis. Regular monitoring and control of alcohol intake, coupled with the management of conditions like gallstones, can significantly reduce the risk of developing pancreatitis. Additionally, understanding these risk factors helps in the early detection and diagnosis of the condition, allowing for timely and more effective treatment. This is particularly important given the potentially severe complications associated with acute pancreatitis, including the risk of developing chronic pancreatitis and other related health issues.
Diet Considerations For those with Acute or Chronic Pancreatitis
Dietary management plays a critical role in both the treatment and prevention of acute and chronic pancreatitis. During acute episodes, patients may be advised to refrain from eating or drinking for a certain period, with nutrition provided through a feeding tube to rest the pancreas and reduce inflammation. Once patients are able to eat again, they are typically prescribed a healthy, low-fat diet comprising small, frequent meals. This dietary approach is crucial in reducing the workload on the pancreas and preventing exacerbation of the condition.
Long-term dietary considerations for pancreatitis involve maintaining a low-fat, nutrient-rich eating plan. Adequate hydration is essential, and caffeine intake should be limited. Alcohol consumption is strongly discouraged in all patients with pancreatitis, even in mild cases, due to its damaging effect on the pancreas. A diet high in fat and calories can lead to elevated blood fat levels, further increasing the risk of pancreatitis. Adherence to a balanced, low-fat diet not only aids in the recovery process and supporting the immune system but also plays a significant role in reducing the likelihood of pancreatitis recurrence and in managing chronic pancreatitis effectively.
Management, Treatment, and Pain Control of Acute Pancreatitis
Acute pancreatitis is a severe inflammatory condition of the pancreas, which, while serious, often resolves with proper treatment and management. Treatment strategies are centered around hospitalization to manage symptoms and potential complications. No specific medicine exists to directly treat pancreatitis, but pain management is a crucial aspect of care. Medications, including pain medicines, are often administered to control the severe pain associated with the condition. Intravenous (IV) fluids are also a standard part of the treatment protocol.
Additionally, enzyme pills may be prescribed to aid in digestion, particularly if there is malabsorption. Vitamins A, D, E, K, and sometimes vitamin B-12 shots are provided if needed, addressing nutritional deficiencies that might occur due to the pancreas’s impaired function. In cases where chronic pancreatitis leads to diabetes, appropriate treatments for diabetes are also integrated into the care plan.
Recovery from acute pancreatitis often occurs within a few days with supportive care, including rest, hydration, and pain relief. However, severe cases can lead to serious, potentially life-threatening health complications. It’s important to note that chronic pancreatitis, while related, is a long-term, progressive condition that requires ongoing management.
It’s important to note that acute pancreatitis may be caused by more serious issues. Cysts, pseudocysts, tumors, endocrine dysfunction, and other diseases of the pancreas may result in exocrine pancreatic insufficiency. The true cause of pancreatitis is best determined by your healthcare provider, and may only be revealed through biopsy, endoscopic ultrasound/endoscopy, blood tests, a CT scan, or other imaging tests.
In summary, acute pancreatitis requires immediate and comprehensive medical intervention, focusing on symptom management, pain relief, hydration, nutritional support, and specific treatments like endoscopic therapy for underlying causes like gallstones. With prompt and appropriate care, most individuals with acute pancreatitis can recover fully, though the severity of the condition can vary significantly.