CardioSmart Corner | Pregnancy and Heart Disease: Helping Patients Know the Risks?
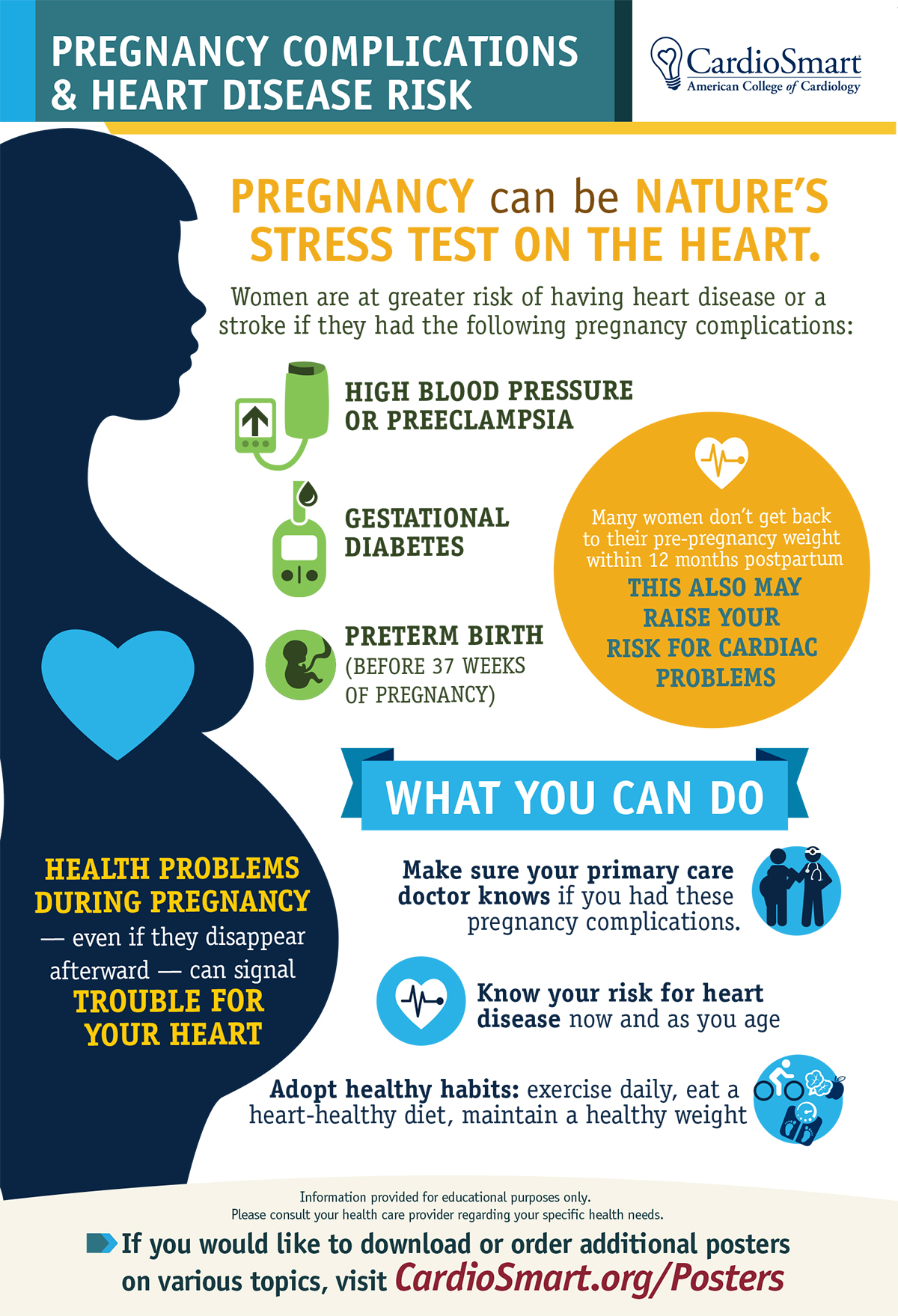
In many ways, pregnancy is a bit like nature’s stress test on the heart. As soon as a woman becomes pregnant, a cascade of changes begins in the body, including a dramatic rise in blood flow and extra workload on the heart.
These are all healthy and normal parts of helping to nourish the growing baby, and most moms-to-be won’t have any heart troubles during pregnancy. However, for a growing number of women, pregnancy may bring about new, often temporary spikes in blood pressure (gestational hypertension or preeclampsia) or blood sugar levels (gestational diabetes).
While these conditions typically go away soon after childbirth, sometimes they don’t and having them at all has been linked to a greater risk of cardiovascular disease or stroke later in life. For example, having had preeclampsia doubles the risk of having a future heart attack or stroke and quadruples the risk of high blood pressure, according to experts. In addition, preterm birth regardless of the reason may also be a red flag for future cardiovascular issues.
"More awareness and action on behalf of both cardiovascular professionals and patients are needed."
Because these conditions disappear after pregnancy, they can be quickly forgotten. Often no one talks about or follows up on a woman’s increased and ongoing cardiovascular risk. More awareness and action on behalf of both cardiovascular professionals and patients are needed.
CardioSmart has a number of new tools (including the infographic here) to help with this awareness building. Send your patients to CardioSmart.org for tips on understanding pregnancy and heart disease.
AHA, ACOG Issue Advisory on CVD Risk Factors in Women
The American Heart Association (AHA) and the American College of Obstetricians and Gynecologists (ACOG) recently issued a Presidential Advisory to raise awareness of cardiovascular disease risk factors among women.
The majority of women consider their obstetrician/gynecologist to be their primary physician during the childbearing years – an important time period for atherosclerotic CVD (ASCVD) risk assessment and primary prevention. Additionally, cardiologists need to be aware of sex-specific ASCVD risk factors, including those related to pregnancy and hormonal influences like polycystic ovarian syndrome, functional hypothalamic amenorrhea, unsuccessful fertility therapy, menopausal status and hormone use.
Among many things, the advisory also highlights pregnancy complications associated with increased future risk of ASCVD, such as preeclampsia, gestational diabetes, gestational hypertension, preterm delivery, and low-for-estimated-gestational age birth weight. It also suggests that postpartum follow-up visits and well-woman visits should be an opportunity for ASCVD risk assessment, counseling and risk reduction.
Keywords: ACC Publications, Cardiology Magazine, Infant, Newborn, Pregnancy, Hypertension, Pregnancy-Induced, Diabetes, Gestational, Risk Factors, Pre-Eclampsia, Blood Pressure, Blood Glucose, Premature Birth, Birth Weight, Polycystic Ovary Syndrome, Exercise Test, Workload, Follow-Up Studies, Amenorrhea, Gestational Age, Risk Assessment, Parturition, Postpartum Period, Myocardial Infarction, Stroke, Heart Diseases, Risk Reduction Behavior, Primary Prevention, Fertility, Counseling
< Back to Listings