Even Though Acne and Rosacea Sometimes Look Similar, They Are Two Separate Diseases

The Essential Info
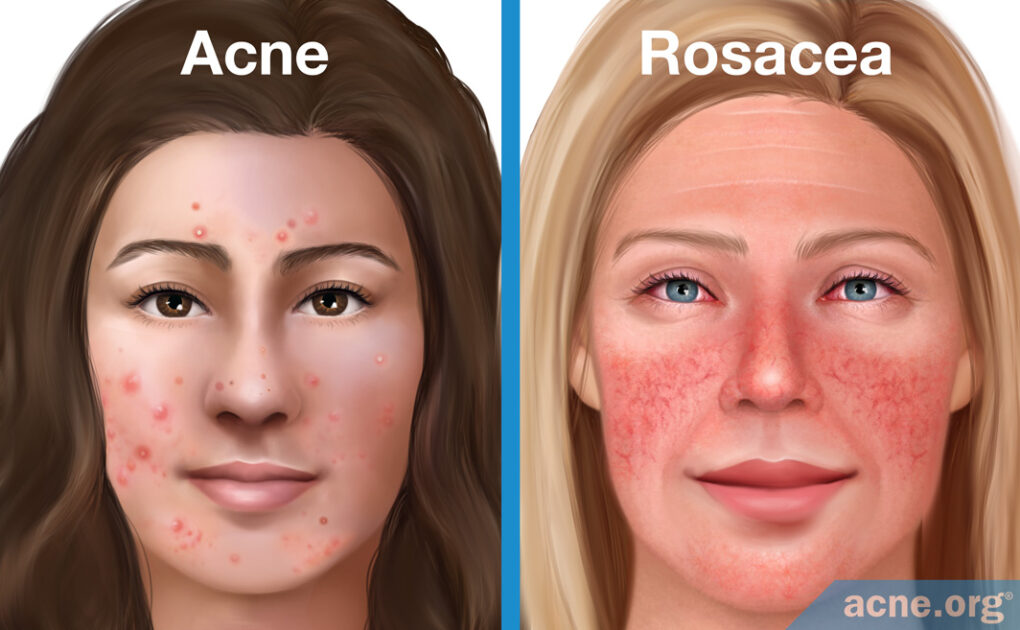
Acne and rosacea are different diseases, but are sometimes confused with one another because they both can show up on the face and can come with similar lesions.
Similarities:
- Both are inflammatory skin diseases that range from mild to severe and commonly affect the face.
- Both can come with similar lesions (papules and pustules).
- There is some overlap in medications, such as topical retinoids.
Differences:
- Acne affects mostly adolescents, whereas rosacea affects mostly people between 30-50 years old.
- Acne is much more common.
- Acne affects the face and body, and rosacea only affects the face.
- Rosacea can show up in various ways, called subtypes, that look very different. For instance, some people have papules and pustules, and other people have broken capillaries instead, or thickened skin around the nose.

The Science
- Acne vs. Rosacea
- Causes of Acne and Rosacea
- Clinical Manifestations of Acne
- Clinical Manifestations of Rosacea
- Treatment of Acne and Rosacea
Both acne and rosacea are common skin diseases that affect millions of people worldwide. Although they are separate conditions, people sometimes cannot distinguish between them. This misunderstanding occurs for two related reasons:
- Sometimes the lesions of facial acne and rosacea look similar, for instance, both diseases can come with papules and pustules.
- Because some lesions of acne and rosacea can look similar, historically, researchers referred to one of the subtypes of rosacea as “acne rosacea.”
Despite these similarities, acne and rosacea are not the same disease.1,2
Acne vs. Rosacea
Similarities
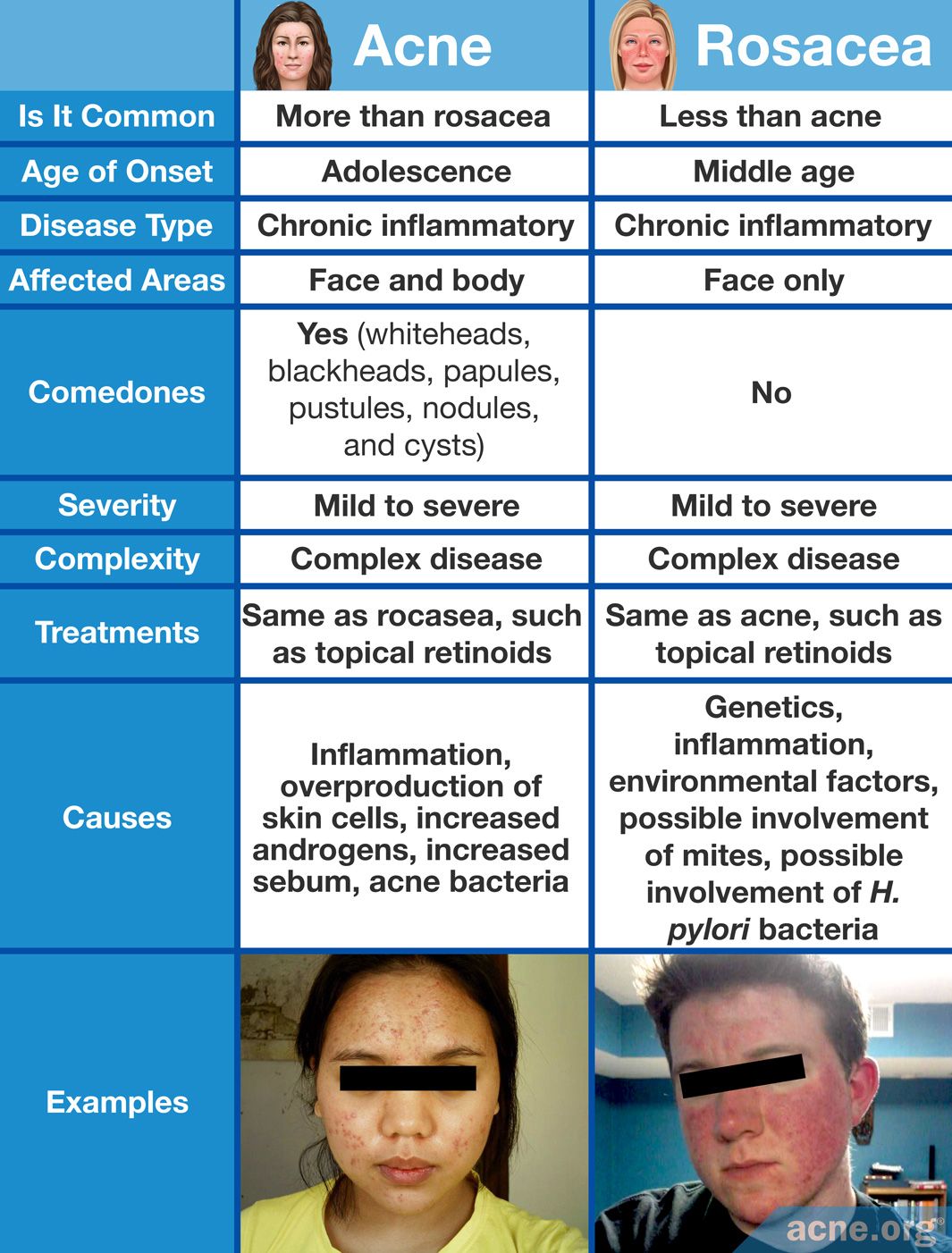
- They are both common.
- Both are chronic inflammatory skin diseases.
- They can produce red, inflamed lesions called papules and pustules on the face.
- They both respond to some of the same medications, such as topical retinoids.
- Both can vary from mild to severe.
- They are both complex conditions that involve multiple factors, and scientists still possess an incomplete understanding of each disease.1,3-6
Differences
- Acne
- More common than rosacea.
- Acne is the most common skin disease in the Western world, and researchers estimate that in the United States alone, it affects between 17 and 45 million people.
- Usually appears in adolescence, though it often persists into adulthood and can even appear for the first time in adulthood.
- Affects the face and body.
- Can produce closed and open comedones (whiteheads and blackheads), papules, pustules, nodules, and cysts.
- Can be more or less severe, but ultimately presents itself the same, regardless of the person afflicted.3,4
- More common than rosacea.
- Rosacea
- Is common, but not as common as acne.
- The National Rosacea Society estimates that approximately 16 million Americans suffer from rosacea.
- Usually appears in middle age, between the ages of 30 and 50.
- Affects only the face, typically the central region (nose, cheeks, and forehead).
- Does not produce comedones.
- Presents itself in a variety of ways that differ from person to person.1,3,7,8
- Is common, but not as common as acne.
Causes of Acne and Rosacea
Acne
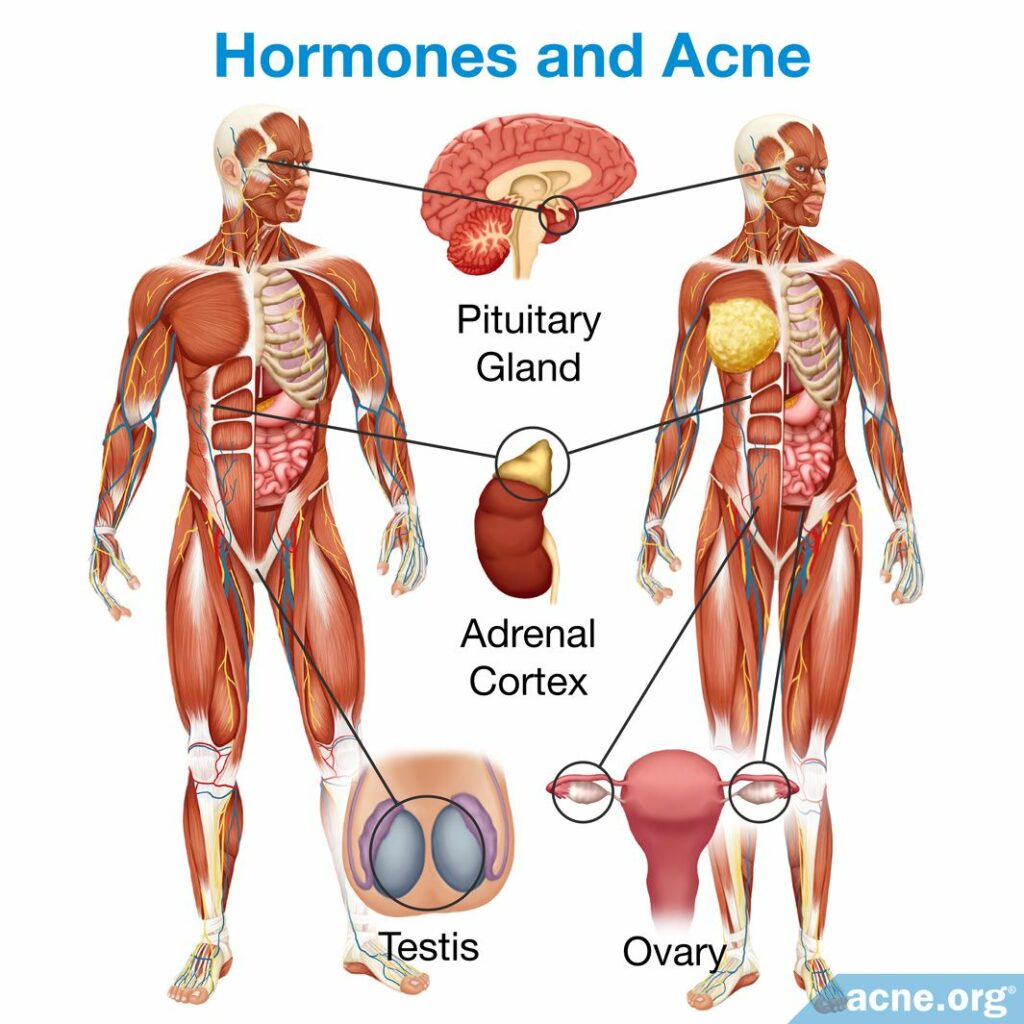
Acne is a disease of the skin pore. It often begins during puberty, which is when the body starts to increase production of androgens (male hormones that are present in both males and females). High levels of androgens stimulate the skin oil glands to produce more sebum (skin oil), an excess of which can lead to acne. Acne that develops in adulthood is also often linked to high levels of androgens, especially in women.4,5
Acne is at least partly genetic in nature, but scientists still do not understand the underlying cause(s) of acne. They believe that five processes take place in the formation of acne lesions. The order in which they occur is still a matter of debate among researchers.
- Inflammation
- Overproduction of skin cells that form comedones
- Increased production of androgens, which increases skin oil production
- Increased production of sebum
- Colonization of the pore by C. acnes, a type of bacteria that is associated with acne3-5
Rosacea
Researchers do not know what causes rosacea, though there appears to be a strong genetic component.3,5 According to a 2017 article in Dermatology and Therapy:

“Although environmental factors contribute to the development of rosacea, there is also a strong genetic component.”5 In addition, although rosacea can affect anyone, it is more common in fair-skinned people of Celtic, Northern European, and Eastern European heritage.1,7
Scientists have proposed several theories about what might play a role in the development of rosacea.
- Vascular (blood vessel) dysfunction
In rosacea, blood vessels of the face dilate and cause redness and flushing. Some scientists believe that this happens because the blood vessels react abnormally to a variety of stimuli, including heat and hormones. - Ultraviolet (UV) radiation from the sun
Rosacea affects the parts of the face that are exposed to the sun. In addition, rosacea tends to appear later in life and affects mostly people with fair skin, who are prone to sunburns. There is some evidence that chronic skin damage from the sun is a risk factor for developing rosacea. - Inflammation
Inflammation is a core component of rosacea, but the cause of the inflammation is unknown. - Demodex
Demodex mites are microscopic creatures that normally live harmlessly in hair follicles. Some researchers propose that they might be more numerous in people with rosacea, and that rosacea patients might be hypersensitive to them and therefore experience immune reactions and inflammation when exposed to the mites. - An intestinal strain of bacteria called H. pylori
Rosacea is associated with some gastrointestinal diseases, such as gastritis (inflammation of the stomach), which are sometimes caused by H. pylori. In addition, studies suggest that some people with rosacea improve after taking medication that kills this bacteria. However, other studies show no association between rosacea and H. pylori.6,7
Despite the proposed theories, the fact that rosacea symptoms vary has led many researchers to believe that there is no single cause.

As a 2008 article in the Spanish journal Actas Dermo-Sifiliográficas noted, “Due to the clinical variability of the disease, it is likely that there is no single cause and that there are multiple pathophysiologic mechanisms involved. Analysis of the theories proposed to explain the pathophysiology of rosacea has produced inconsistent data in all cases.”7
Clinical Manifestations of Acne
Age and gender
Acne can affect anyone and can appear at any time in life, though it is more common in adolescents. During the teenage years, acne is more common in males and is more common in females after the age of 20.3
Symptoms
The primary symptom of acne is lesions on the face, back, chest, and/or shoulders. There are five types of acne lesions.
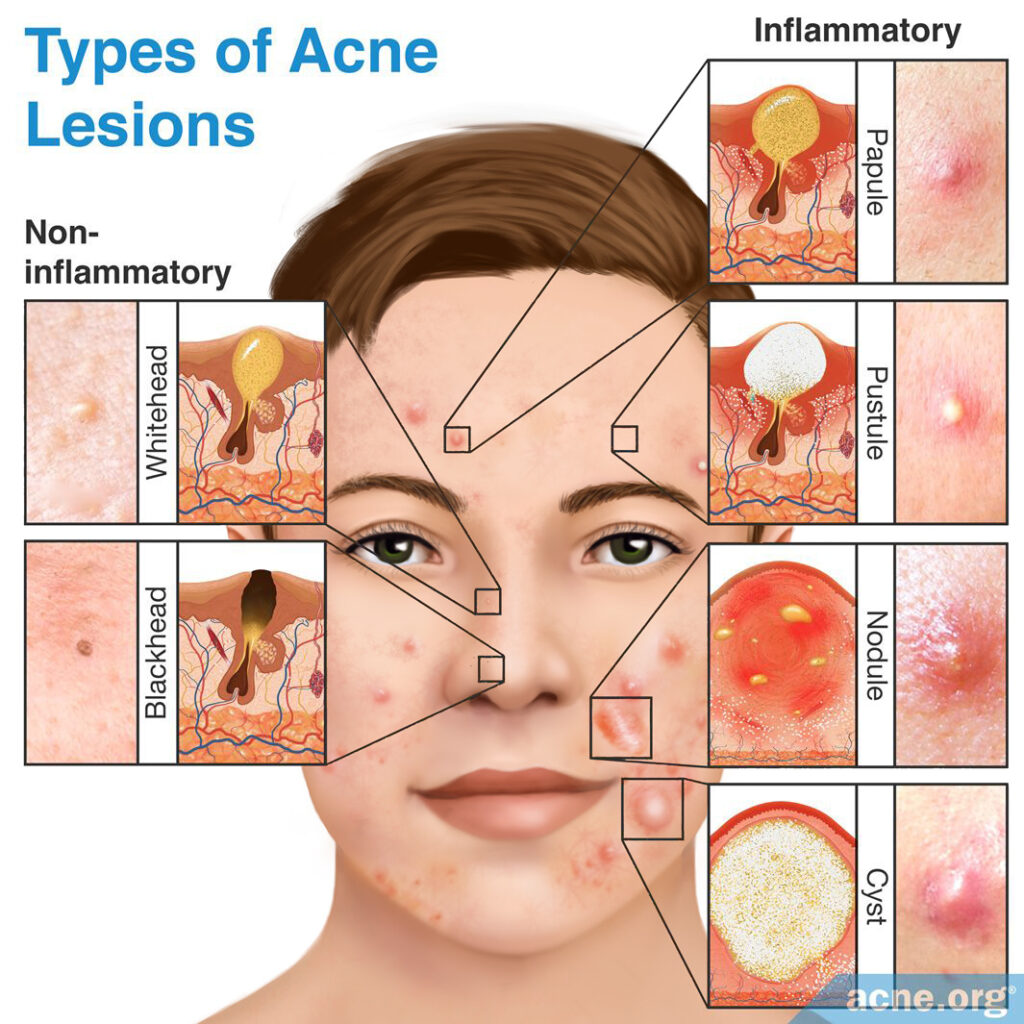
- Comedones – can be open or closed, but neither is inflamed nor red.
- Papules – red, inflamed bumps.
- Pustules – inflamed, red bumps with a white or yellow center, often called “pimples” or “zits”.
- Nodules – severe lesions that are large, inflamed, painful, and solid.
- Cysts – severe lesions that are large, inflamed, painful, and filled with pus.3
Scientists classify acne into different types, according to the type of lesions present.
- Comedonal acne: Whiteheads and blackheads
- Inflammatory acne: Papules and pustules
- Nodulocystic acne: Nodules and cysts9
Triggers
Stress and mechanical irritation of the skin can trigger an acne breakout. We still do not know whether diet, specifically a high-glycemic diet, or dairy intake can increase acne symptoms.
Clinical Manifestations of Rosacea
Age and gender
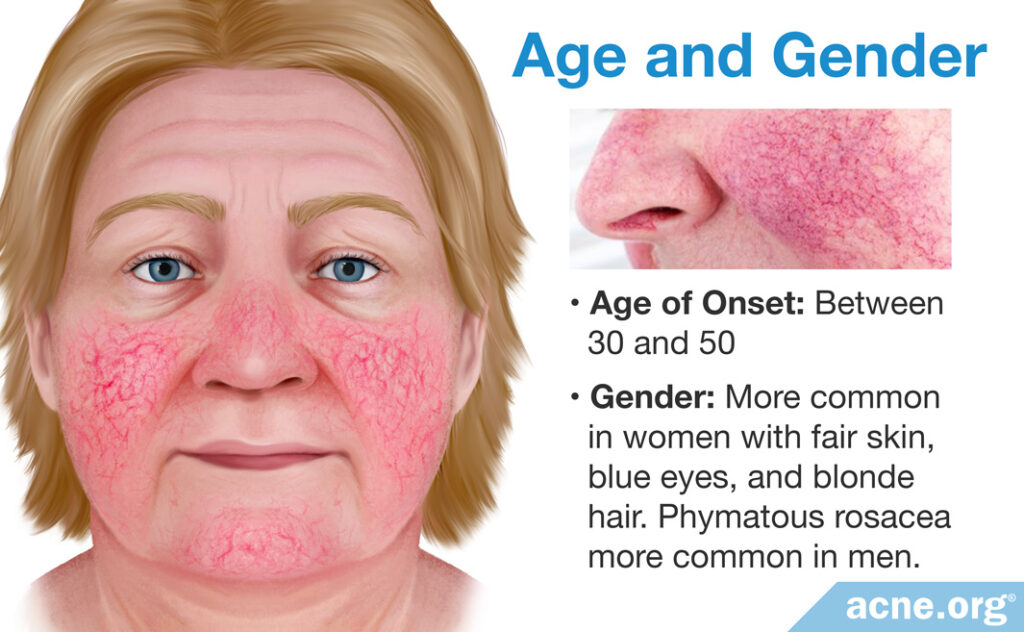
Rosacea usually begins in middle age, between the ages of 30 and 50. While it can affect anyone, it typically shows up in women with fair skin, blue eyes, and blonde hair. Although rosacea is more common in women, one subtype called phymatous rosacea is more common in men.1,6
Symptoms
Because rosacea can present a variety of symptoms, scientists classified it into four subtypes that correspond to the most common groupings of symptoms.
- Subtype 1: Erythematotelangiectatic rosacea
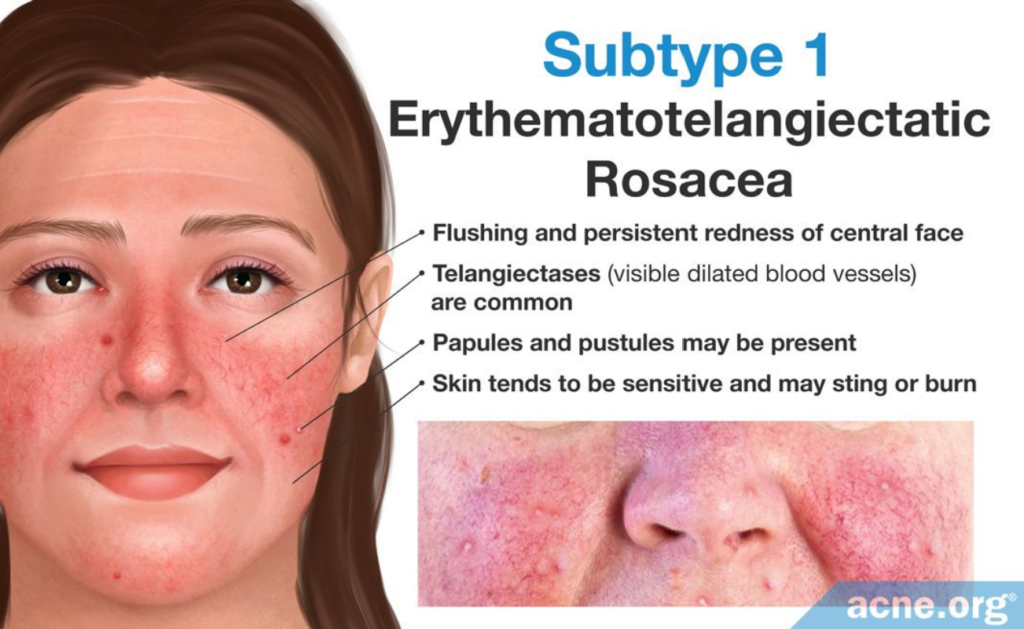
The primary symptoms of this subtype are flushing and persistent redness of the central face. Telangiectases (visible dilated blood vessels) are common, but are not necessary for diagnosis. Papules and pustules may also be present, and the skin tends to be sensitive and may sting or burn at times. - Subtype 2: Papulopustular rosacea
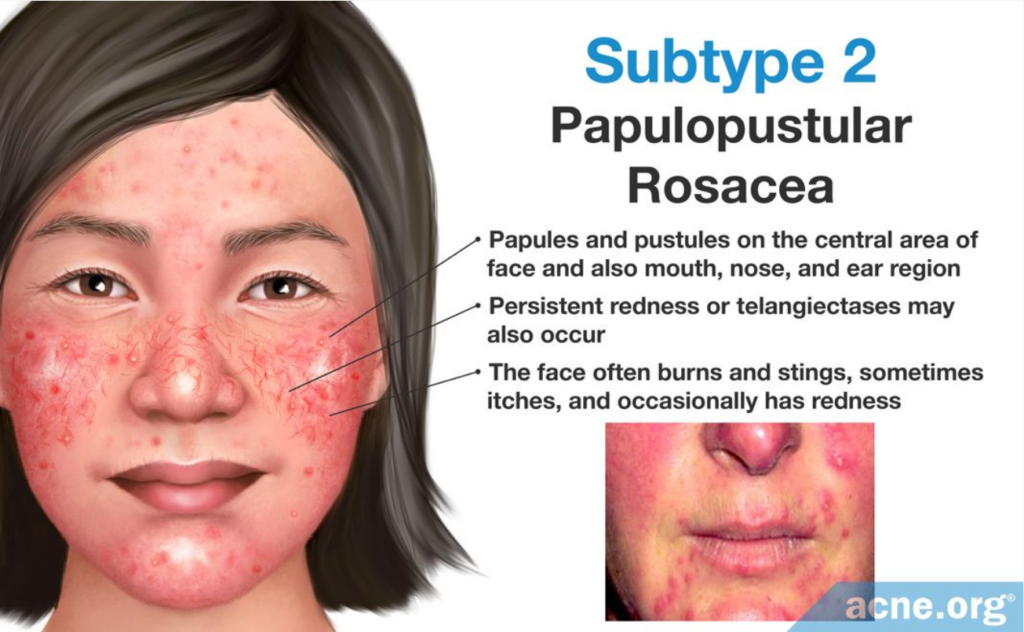
The primary symptom of this subtype is papules and pustules that come and go on the central area of the face. These lesions may resemble acne and may also be present around the mouth, nose, and in the ear region. Persistent redness or telangiectases may also occur. The face often burns and stings, sometimes itches, and occasionally has redness. - Subtype 3: Phymatous rosacea
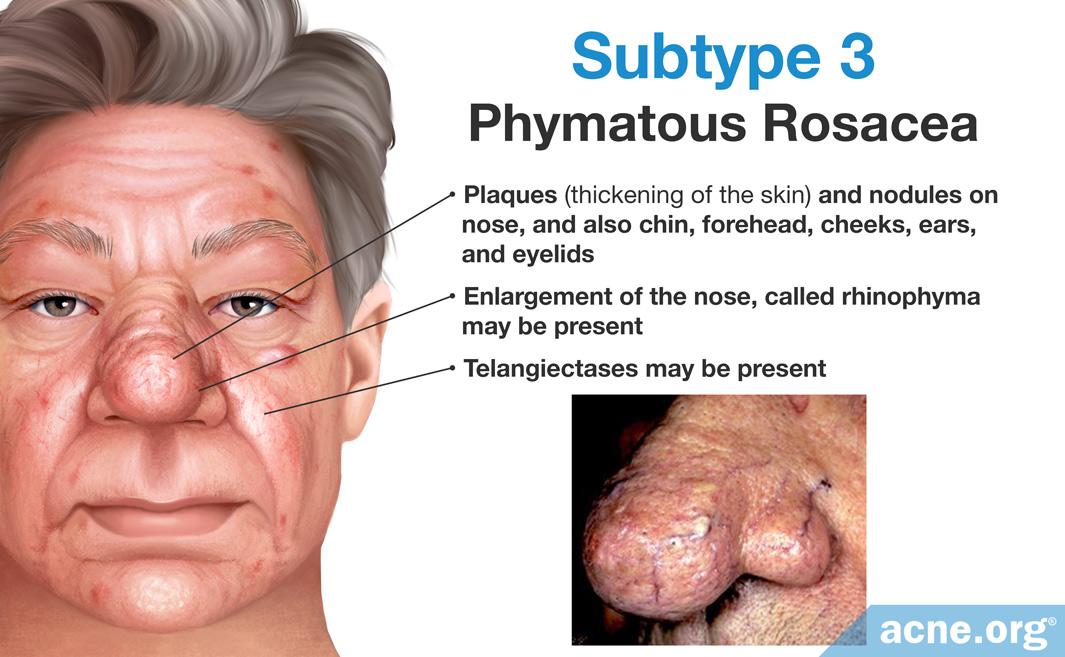
The primary symptoms of this subtype are plaques (thickening of the skin) and nodules on the skin. These symptoms typically affect the nose, but can also affect the chin, forehead, cheeks, ears, and eyelids. Enlargement of the nose called rhinophyma and telangiectases may also be present. This subtype is most common in men, and left untreated, it can worsen and cause severe facial disfigurement. - Subtype 4: Ocular rosacea
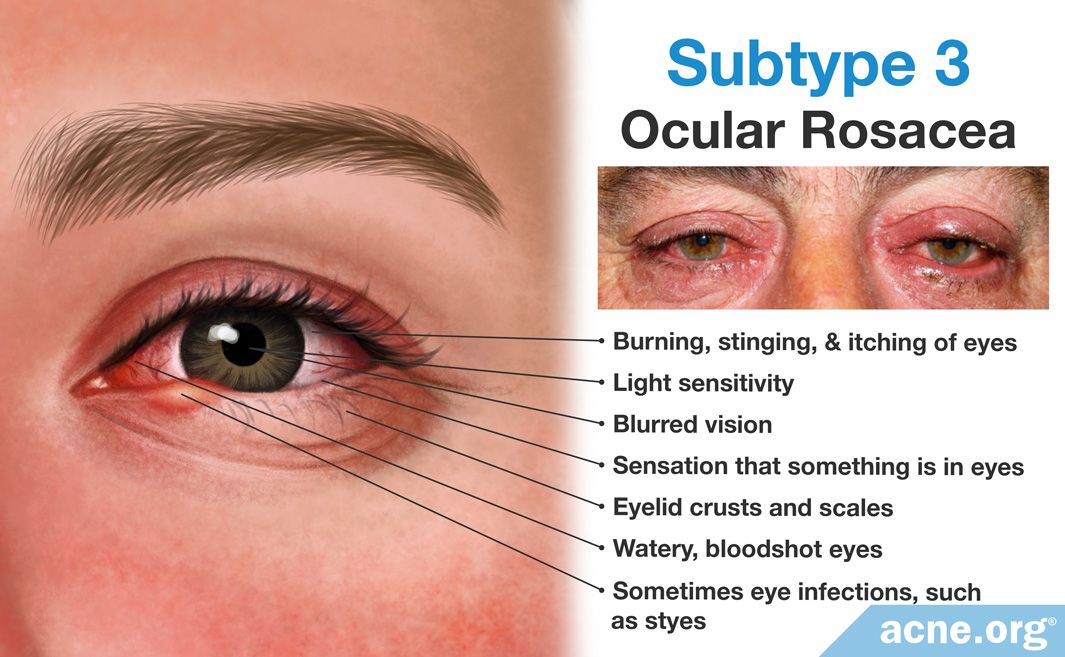
This subtype primarily affects the eyes, including the eyelids, conjunctiva, and cornea. Primary symptoms include watery, bloodshot eyes, burning, stinging, and itching of the eyes, light sensitivity, blurred vision, the sensation that something is in the eyes, eyelid crusts and scales, and sometimes eye infections, such as styes. Ocular rosacea usually occurs alongside skin symptoms, but it can appear by itself as well.6,7,10
It is common for rosacea sufferers to experience more than one subtype of rosacea, and many such people also deal with other skin disorders, such as dermatitis, acne, and psoriasis, at the same time. In addition, many people with rosacea experience dry, sensitive skin.7,11
Triggers
Rosacea is associated with several triggers that can contribute to symptom flares. The list of possible triggers is long, and each individual responds differently to them. Some of the most common triggers include sun exposure, stress, heat, and wind. The National Rosacea Society maintains two lists of common triggers:
Treatment of Acne and Rosacea
Acne
While acne affects 25 – 50% of adults, it often subsides after adolescence, with or without treatment. Treatment depends on the severity and type of lesions.
- For comedonal acne, the first-line therapy is often a topical retinoid medication, such as tretinoin, adapalene, or tazarotene. Azelaic acid and salicylic acid are also used for comedonal acne.
- For mild-to-moderate inflammatory acne, treatment includes topical benzoyl peroxide, topical retinoids, and/or topical antibiotics.
- For moderate-to-severe acne, treatment includes benzoyl peroxide, topical retinoids, oral antibiotics, or oral isotretinoin for severe acne that does not respond to other treatments. In women, oral contraceptives (birth control pills) or anti-androgens, such as spironolactone, are sometimes used for acne that is caused by high levels of androgens.3,14
Rosacea
Rosacea is a progressive disease with no cure, so treatment aims to control symptoms. Some people can use rosacea treatments intermittently and remain symptom-free for long periods of time, while other people need consistent treatment to keep symptoms under control. If left untreated, rosacea tends to worsen over time, so treatment is essential. Rosacea management depends on the particular symptoms and triggers and can include:
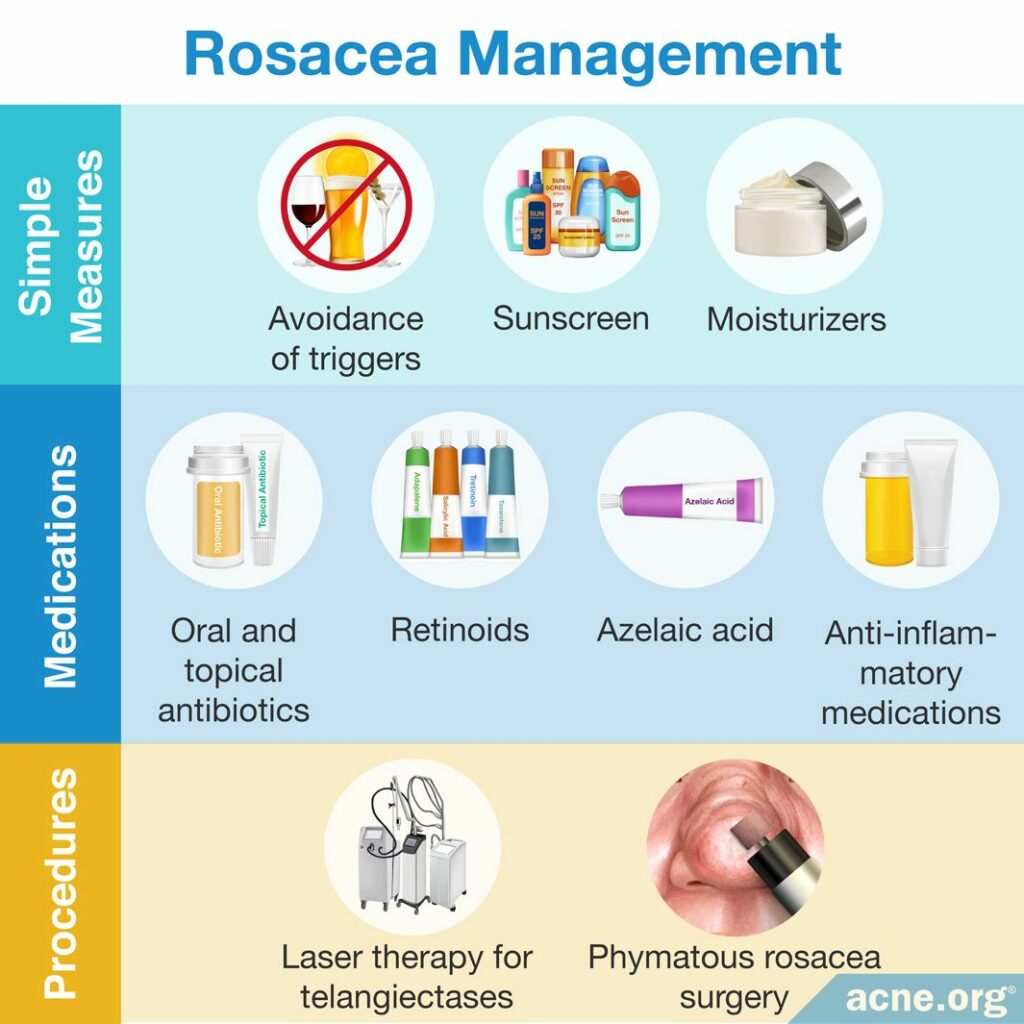
- Avoidance of triggers
- Sunscreen and sun-protective clothing
- Moisturizers and skincare products for dry, sensitive skin
- Topical antibiotics
- Oral antibiotics
- Topical or oral anti-inflammatory medications
- Retinoids
- Azelaic acid
- Laser therapy for telangiectases
- Surgery for phymatous rosacea5-7
References
- Jansen, T. & Plewig, G. Rosacea: classification and treatment. J R Soc Med 90, 144 – 150 (1997). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1296179/
- Acne or Rosacea? A Case of Mistaken Identity, https://www.rosacea.org/weblog/acne-or-rosacea-case-mistaken-identity
- Goldberg, D. J. & Berlin, A. L. Acne and Rosacea: Epidemiology, Diagnosis and Treatment. 1st edn, (CRC Press, 2011). https://www.crcpress.com/Acne-and-Rosacea-Epidemiology-Diagnosis-and-Treatment/Goldberg-Berlin/p/book/9781840761504
- Williams, H. C., Dellavalle, R. P. & Garner, S. Acne vulgaris. Lancet 379, 361 – 372 (2012). https://www.ncbi.nlm.nih.gov/pubmed/21880356
- Picardo, M., Eichenfield, L. F. & Tan, J. Acne and rosacea. Dermatol Ther 7, 43 – 52 (2017). https://www.ncbi.nlm.nih.gov/pubmed/28150107
- Mikkelsen, C. S. et al. Rosacea: a clinical review. Dermatol Reports 8, 6387 (2016). https://www.ncbi.nlm.nih.gov/pubmed/27942368
- Barco, D. & Alomar, A. Rosacea. Actas Dermosifiliogr 99, 244 – 256 (2008). https://www.ncbi.nlm.nih.gov/pubmed/18394399
- Rosacea Now Estimated to Affect at Least 16 Million Americans. Rosacea Review: Newsletter of the National Rosacea Society (2010). https://www.rosacea.org/rr/2010/winter/article_1.php
- Feldman, S. et al. Diagnosis and treatment of acne. Am Fam Physician 69, 2123 – 2130 (2004). https://www.ncbi.nlm.nih.gov/pubmed/15152959
- Wilkin, J. et al. Standard grading system for rosacea: Report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol 46, 584 – 587 (2002). https://www.ncbi.nlm.nih.gov/pubmed/11907512
- Survey: Other Skin Conditions Often Present in Rosacea Patients. Rosacea Review: Newsletter of the National Rosacea Society (2013). https://www.rosacea.org/rr/2013/winter/article_3.php
- Factors That May Trigger Rosacea Flare-Ups, https://www.rosacea.org/patients/materials/triggers.php
- Rosacea Triggers Survey, https://www.rosacea.org/patients/materials/triggersgraph.php
- Graber, E. Treatment of acne vulgaris. http://www.uptodate.com/contents/treatment-of-acne-vulgaris