Abbreviations
- AR: aortic regurgitation
- PMI: point of maximal impulse
- TTE: trans-thoracic echocardiography
- TEE: trans-esophageal echocardiography
- PND: paroxysmal nocturnal dyspnea
- PR: pulmonic regurgitation
- ACEI: angiotensin converting enzyme inhibitor
- ARB: angiotensin receptor blocker
- ARNI: angiotensin receptor neprilysin inhibitor
Introduction
- Aortic valve regurgitation can be thought of as two entities based on chronicity: acute and chronic.
- Both acute and chronic AR result in a volume overloaded state, with resulting hemodynamic disturbances.
- In chronic AR, the left ventricle can gradually adapt to an increased volume state.
- In acute AR, the left ventricle can’t quickly adapt to the regurgitant volume, leading to dramatic hemodynamic consequences.
Acute AR
- Etiologies:
- Endocarditis
- Aortic dissection
- Blunt chest trauma
- Prosthetic valve failure
- Complication of transcatheter procedure
- Pathophysiology
- In acute AR, there is a sudden increase in regurgitant volume placed upon an LV that has not had time to adapt.
- Diastolic pressures quickly rise, and the patient experiences:
- Congestion (acute pulmonary edema)
- Poor forward flow/hypoperfusion (acute cardiogenic shock)
- Clinical Presentation:
- Acute cardiogenic shock and flash pulmonary edema
- Physical Exam:
- Vital signs: wide pulse pressure, tachycardia
- Reduced S1 (early mitral valve closure); S3, S4 from high filling pressures and reduced LV compliance
- Brief decrescendo early diastolic murmur (rapid equilibration of pressures)
- Austin-Flint Rumble – low pitch diastolic murmur best heard in the apex (caused by aortic regurgitation jet abutting the anterior mitral valve leaflet or endocardium)
- Systolic murmur
- Due to increased stroke volume (much of it regurgitated blood)
- Poor forward flow (reduced capillary refill, cold extremities, decreased level of consciousness)
- Pulmonary hypertension signs
Rapid diagnosis is vital:
- CT chest if suspected aortic dissection
- Echo (TTE or TEE)
- Consider point-of-care cardiac ultrasound
Management:
- Urgent surgery to correct the underlying cause
- Temporising measures:
- Increased inotropy – dobutamine/milrinone (increases stroke volume)
- Afterload reduction (promotes forward flow, reduces regurgitation) an easily-titratable arterial vasodilator is IV nitroprusside
- IABP is contraindicated in acute severe AR because diastolic inflation will worsen regurgitation
Chronic AR - Introduction
Etiology
Consider the origin of aortic regurgitation as arising from either the aortic valve or the level of the aorta.
- Aortic valve:
- Bicuspid aortic valve (most common cause of severe AR in high income countries)
- Rheumatic disease (low income countries)
- Degenerative (calcific – most common cause of mild/moderate AR)
- Endocarditis
- Aorta:
- Aortic dilation (numerous underlying causes; see separate post on aortopathy)
- Aortic dissection
Hemodynamics
- Chronic AR is a volume overload state of the left ventricle.
- With continued regurgitation, there is progressive dilation of the LV, leading to an eventual drop in LV ejection fraction and heart failure symptoms.
- It is important to intervene on the valve before there is a drop in LV systolic function (i.e. decompensation).
Chronic AR - History & Physical
History
- Symptoms are those of chronic heart failure: exertional dyspnea and exercise intolerance, leg swelling, and orthopnea/PND.
Physical
- Vitals:
- Wide pulse pressure (with low diastolic BP)
- Bounding pulses with carotid thrill
- Pulsus bisferiens (double-pulse)
- Palpation
- PMI: laterally displaced, hyperdynamic, enlarged (LV enlargement)
- Palpable S3
- Auscultation:
- High specificity of detecting AR, low sensitivity
- Diastolic decrescendo murmur, best assessed with patient seated, leaning forward, and at end expiration
- Murmur intensity and duration correlate to severity (shorter duration = more severe, rapid equalization of pressures)
- Radiation of the murmur:
- Left parasternal region – suggests valvular pathology
- Right parasternal region – suggests aortic pathology
- S3 – volume overloaded ventricle
- Systolic ejection murmur due to increased stroke volume
- Austin-Flint murmur (see above)
- Distinguish AR from PR -> murmur starting from A2, peripheral signs, PR murmur increases during inspiration
- Peripheral signs (in severe chronic AR):
- Corrigan’s (water hammer) pulse: visibly pulsating carotid artery with collapse
- de Musset’s sign: head bob with each beat
- Muller’s sign: pulsation of the uvula with each beat
- Quincke’s pulse: pulsating capillaries upon gentle pressure at the distal nail-bed
- Traube’s sign: loud “pistol shot” sound heart in diastole with gentle auscultation over the femoral artery
- Duroziez’s sign: “to-and-fro” bruit over femoral artery with pressure applied
- Excellent review of physical exam (important for OSCEs)
Chronic AR - Investigations
Echo (TTE) is vital to diagnosis and monitoring.
Echo allows for assessment of valve morphology, severity and mechanism of AR, presence of aortic dilation, and LV size and function.
Bicuspid aortic valve patients need an assessment of the entire aorta with a CT scan.
Monitoring in asymptomatic patients
- The goal of monitoring asymptomatic patients with chronic AR is to identify them at the optimal moment for surgery: before there is a decompensation in LV function.
- After first diagnosis, clinical follow-up +/- echo at 3-6 months is recommended to ensure interval stability.
- With mild-to-moderate AR, echo every 2 years is recommended.
- If echo shows a dilated ascending aorta (> 40mm), CT or cardiac MRI should also be performed.
Chronic AR - Management
- Management of chronic aortic regurgitation centres on intervening on the aortic valve before there is potentially irreversible LV dysfunction.
- Medical therapy:
- Treat hypertension to target sBP <140mmHg. (Class 1)
- Treat LV systolic dysfunction with standard heart failure medications (ACEI/ARB/ARNI etc.)
- Although afterload reduction theoretically improves hemodynamics by improving forward flow and reducing regurgitation, there is no evidence that it improves the natural history of AR, and should not be a substitute for surgery.
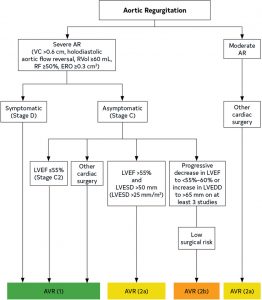
- Surgical Valve Intervention:
- Indications for surgery:
- Severe AR + Symptoms [I]
- Severe AR + LV systolic dysfunction (LVEF < 55%) [I]
- Severe AR + LV dilation (LV End-systolic Dimension > 50mm or indexed > 25mm/m2) [IIA]
- Severe AR + progressive LV dilation or reduction in LVEF [IIB]
- At least moderate AR + undergoing other surgery [I – severe, IIA moderate]
- Transaortic valve replacement (TAVR) is not used for isolated chronic AR due to dilation of aortic annulus that can cause paravalvular leak and a lack of leaflet calcification to anchor the valve.
- Indications for surgery:
Authors
- Primary Author: Dr. Matthew Church (MD, FRCPC, Cardiology Fellow), Dr. Pavel Antiperovitch (MD, FRCPC Cardiologist)
- Reviewer: Dr. Atul Jaidka (MD, FRCPC, Cardiology Fellow)
- Copy Editor: Megha Shetty (MD Student)
- Last Updated: Dec. 19, 2021
- Comments or questions please email feedback@cardioguide.ca