![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
109 Cards in this Set
- Front
- Back
|
Define hyphae
|
Long strands of cells which may form mats like mycelium
|
|
|
What is the appearance of asceptate hyphae? Give an example of a group with asceptic hyphae
|
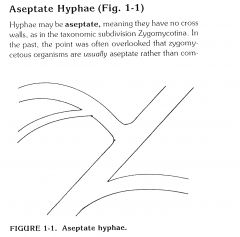
- contain no cross walls
- seen in Zygomycotina - |
|
|
Describe septate hyphae. Give an example of a group with this hyphae.
|
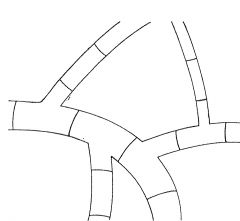
- most hyphae are septate
- Ascomycotina - Basidiomycotina - Deuteromycotina |
|
|
Define conidia
|
reproductive structures often seen on the end of aerial hyphae
|
|
|
Define superficial mycoses
|
- Top keratin-containing layers of skin or hair.
- Non-invasive - Sometimes described as 'basically asymptomatic' |
|
|
Define cutaneous infections
|
- deeper epidermal layers of skin, nails and hair,
- produces more tissue destruction and symptoms than superficial. |
|
|
What are the four superficial mycoses?
|

tinea nigra
Pityriasis versicolor Black piedra White Piedra |
|
|
What is the organism responsible for Black Piedra?
|

|
|
|
What is the organism responsible for white piedra?
|

trichosporon ovoides
|
|
|
Give examples of cutaneous infections in humans
|

Dermato- phytosis
Dermato-mycosis Candidiasis |
|
|
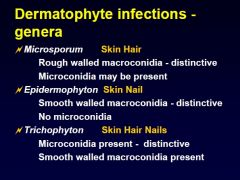
What are the causative agents of Dermatophytosis
|

Tricho-phyton spp.
Epidermo-phyton sp. Microsporum sp. |
|
|
What is Dermatomycosis
|
a cutaneous mycoses caused by fungi other than dermatophytes
|
|
|
List dermatophytes
|

trichophyton
epidermosphyton microsporum |
|
|
What is the causative agent of the mycosis Candidiasis
|
Candidia spp.
|
|
|
What are the two types of specimens in the mycology lab? what types of specimens are in this group?
|
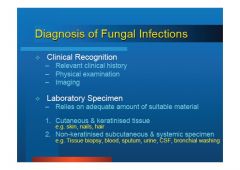
1. cutaneous and keratinised tissue (3)
-skin, hair, nails 2. non keratinised subcutaneous and systemic specimen (6) - tissue bx - blood, - sputum, - urine, - CSF, - bronchial washing |
|
|
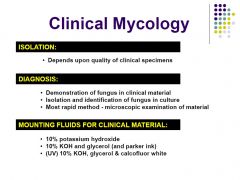
What is performed on all specimens. What is rate limiting step in clinical specimens?
|

- Microscopy and culture is performed on all specimens as direct microscopy does not rule out disease.
- enough specimen material |
|
|
How is isolation media and direct microscopy performed?
|
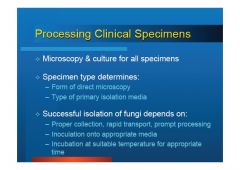
guided by specimen types - same as bacteriology
|
|
|
What are the factors which determine whether or not the isolation of fungi is successful?
|

1. proper collection
2. quick transport, quick processing 3. appropriate media 4. correct incubation conditions |
|
|
What is the Most rapid method for diagnosis?
|
- microscopic examination of material
|
|
|
what are the mounting fluids for clinical materials composed of?
|
- 10% potassium hydroxide
- 10% KOH and glycerol - (UV) 10% KOH, glycerol and calcoflour white |
|
|
How is collection performed for superficial and cutaneous infections?
|
from actively growing outer edge of lesion
|
|
|
How is collection performed for scalp infection
|
15-20 hair roots for collection
- due to infection being in the roots - spores are around hair and inside |
|
|
How is collection performed for nails?
|
scrape inside of nail and close to nail bed, while removing as much diseased tissue as possible
|
|
|
How is collection performed for feet?
|
Discard outer horny layer and scrape lower layer
also sample between 4th and 5th toes. |
|
|
How is collection performed for tinea
|

Discard outer horny layer and scrape lower layer
also sample between 4th and 5th toes. |
|
|
What is the specimen collection procedure for skin scrapings
|

- alcohol swab
- advancing border sample - rolling of swab over lesions |
|
|
What is the specimen collection procedure for hair samples
|

pluck from shaft
|
|
|
What is the specimen collection procedure for nail samples
|

alcohol
deep scrape to sample tissue recently invaded. |
|
|
What is the turnover time for microscopy?
|
<24hrs
|
|
|
What is the turn around time for culture?
|
1-4 weeks
|
|
|
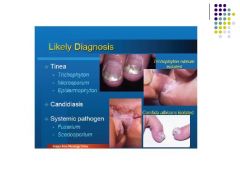
What are the likely dx for tinea?
|
TEM
Trichophyton epidermophyton microsporum |
|
|
What are possible dx for systemic pathogens?
|
Fusarium
Scedosporium |
|
|
What are the three dermatophyte genera?
|
TEM
|
|
|
How can dermatophyte genera be made distinct from one another?
|

TEM
|
|
|
Which of the three genera of dermatophytes can infect nails?
|
Trichophyton
|
|
|
Describe the shape and cells in each of the dermatophyte genera
|

|
|
|
Which genera in dermatophytes have thick walls?
|

Microsporum can have thick or thin walls.
|
|
|
Which dermatophyte has macroconidia shaped like a
(a) pencil (b) eliptical/spindle (c) club |

trichophyton
microsporum epidermophyton |
|
|
Define arthrophilic and an example of such an infection
|
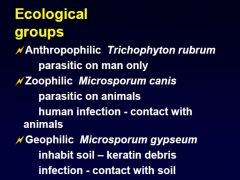
Trichophyton rubrum
only affecting parastisim in humans |
|
|
What are zoophilic infections? give an example
|
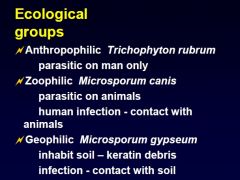
human infection is from contact with animals. an exampls is microsporum canis
|
|
|
What is a geophilic infection? give an example
|
an infection transferred through soil or contact with soil. Microsporum gypseum is an example.
|
|
|
Explain host specificity - give an example
|

T. concentricum Infections among Europeans are rare. Distribution is restricted to the Pacific Islands of Oceania, South East Asia and Central and South America.
|
|
|
How do we diagnose dermatophytes?
|
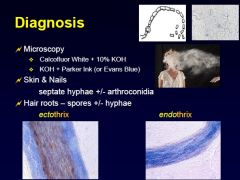
Use calcofluor white + 10% KOH
OR --> KOH + Parker ink look for septae and arthroconidia in skin & nails look for spores and hyphae in hair roots |
|
|
define ectothrix
|

Endothrix refers to dermatophyte infections of the hair that invade the hair shaft and internalize into the hair cell. This is in contrast to exothrix (ectothrix), where a dermatophyte infection remains confined to the hair surface
|
|
|
define endothrix
|
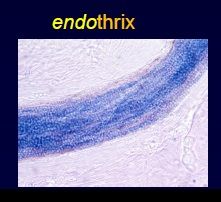
Endothrix refers to dermatophyte infections of the hair that invade the hair shaft and internalize into the hair cell. This is in contrast to exothrix (ectothrix), where a dermatophyte infection remains confined to the hair surface
|
|
|
Why is microscopy so important in fungi?
|
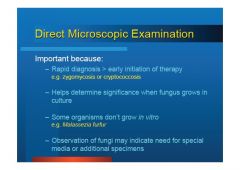
1. In case it was zygomycosis or cryptococcus
2. Some organisms do not grow in culture 3. will direct the selection of primary isolation media - special media or additional specimens 4. Helps determine the significance when it does grow in culture |
|
|
Describe the calcofluor white + 10% KOH
|
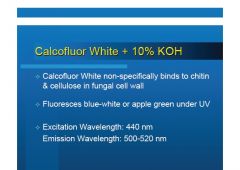
- UV fluorescence
- %10 chitin and cellulose binding for the fungal wall. - sensitive |
|
|
Describe KOH and Parker Ink
|
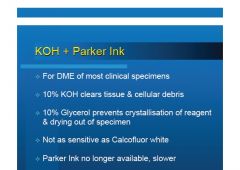
- no longer available
- was used most often for direct microscopy - not as sensitive as calcofluor |
|
|
What does 10% KOh do?
|
clears tissue and cell debris
|
|
|
What does 10% glycerol do?
|
- prevents crystallisation of reagent
- dyring out of specimen |
|
|
What is the differential characteristic of DTM?
|
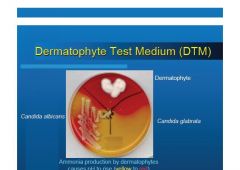
Dermatophytes produce ammonia which causes a pH change and goes from yellow to red.
|
|
|
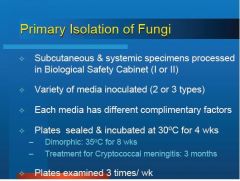
Explain the basic primary isolation conditions for fungi
|
- Biosafety cabinets for subcutaneous and systemic fungi (I or II)
- microscopy is performed (Calcofluor + 10% KOH) - 2 to 3 types of media is innoculated - 30 C for 4 weeks - Dimorphic 35 C for 8 weeks - examined 3x weeks |
|
|
How long is the treatment for cryptococcus meningitis
|
3 months
|
|
|
How is Direct Microscopic Examination performed?
|
**
|
|
|
What is the primary isolation media specifically for Dermatophytes?
|

|
|
|
What does DTM contain?
|

|
|
|
Describe the Isolation of Fungi
|
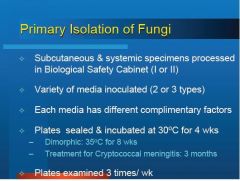
SICI
Safety: subcutaneous and systemic specimens must be processed in Biological safety cabinets Innoculation: variety 2-3 types of media are innoculated. Complimentary: complimentary factors in the media are combined to isolate the fungi Incubation: sealed and incubated at 30 C for 4 weeks, dimorphic at 35C for 8 weeks. |
|
|
List types of PIM for fungi
|
Media:
1. No antimicrobials - SDA 2. Antibiotics innoculated - SABP: SDA + blood + polymixin B - SABD: SDA + BHI + chloramphenicol + gentamicin 3. Antibiotic and Antifungals - Mycose/MD: mycobiotic afar + chloramphenicol, gentamicin & cycloheximide. 4. CandidaCHROM |
|
|
What is observed in culture?
|
1. Surface colour and reverse colour
2. Typography 3. texture 4. growth rate |
|
|
What temperature do pathogenic dermatophytes grow at?
|
35C
|
|
|
How is identification mainly derived?
|
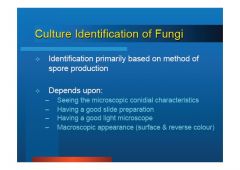
method of spore production
|
|
|
Identification of Fungi depends on what main characteristics
|
1. ability to visualise microscopic conidial features
2. Having a good slide preparation 3. Having a good microscope 4. Macroscopic appearance also assists in Id of fungi (IE: surface and reverse colour) |
|
|
How is Microscopy culture performed?
|
cellotape preparation
|
|
|
What is observed in microscopy culture?
|
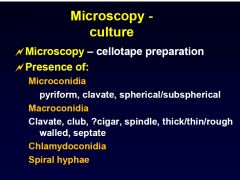
1. Microconidia shape,
2. Macroconidia shape, thickness of walls, sepate/non spetate 3. Observation of chlamydoconidia defn: thick walled thallic spores formed within the vegetative hyphae for survival. 4. Unique characteristics like spiral hyphae in Trichophyton mentagrophytes |
|
What is the following?
|
pyriform microconidia
|
|
What is the following?
|
sub sperical microconidia
|
|
What is the following?
|
spherical microconidia
|
|

Describe the following
|
clavate microconidia
|
|

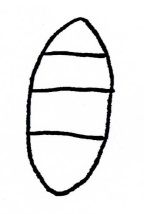
Describe the above morphology
|
ellipsoidal macroconidia
|
|
Describe the above
|
clavate of bullet shaped macroconidia
|
|
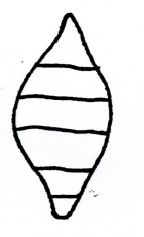
Describe the above
|
spindle shaped macroconidia
|
|
Describe the above
|
cigar shaped macroconidia
|
|

Describe the above
|

irregular shaped macroconidia
|
|
|
How can macroconidia be described?
|
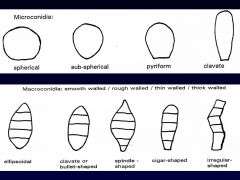
1. wall thickness, wall texture
2. macroconidia shape |
|
|
How can microconidia be described?
|
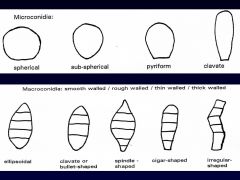
shape
|
|
Identify the above
|
characteristic smooth, thin-walled macroconidia, cigar shaped
|
|

Identify the above
|

chlamydoconidium
|
|

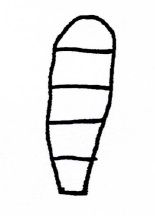
Identify the above morphology
|

thick walled spindle shaped macroconidia
|
|
Identify the morphology of the above
|
macroconidia are irregular, spindle-shaped, with rough thick walls
Microconidia are pyriform to clavate in shape |
|
Identify the morphology of the above
|
ovoid to pyriform macroconidia with 1-3 cells,
relatively thin, finely rough walls, and broad truncate bases |
|
|
What are the four essential steps to the successful isolation of fungi?
|

1. clinical suspicion of fungi by GP/ physician
2. Proper collection and transport 3. isolation through innoculation on to correct media and incubation conditions, followed by appropriate staining 4. informed and skilled microscopic examination |
|

Identify
|

slender clavate to pyroform microconidia. barb wire like - Trichophyton rubrum
|
|
Identify
|
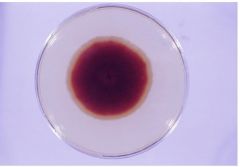
T. rubrum - white suede like to downy with a characteristic deep wine reverse pigment.
|
|

Identify
|
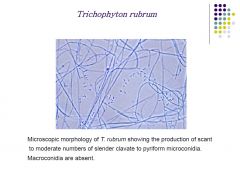
T. rubrum - scant to moderate number o
|
|
|
What are the clinical symptoms, locations and terms for T. rubrum?
|

CLINICAL SYMPTOMS:
- circular erythematous scaling border - soft wrinkled skin - brittle and discoloured nails - Tinea pedis, Tinea cruris - normally sees growth in 1 week |
|
|
What are the clinical symptoms, microscopic appearance and culture results for trichophyton mentagrophytes?
|
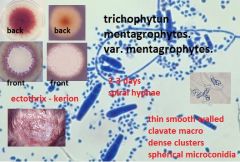
clinical:
- scaly, erythematous lesion, scaly. - kerion lesion of scalp with superlative foliculitis - ectothrix infection - does not fluoresce |
|
|
Describe yeasts
|
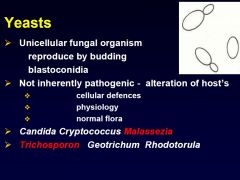
- unicellular
- blastoconidia reproduction - mother cell develops to blastoconidia and separates. - not inherently pathogenic - HME |
|
|
What are examples of yeasts that can become pathogenic?
|
Candida
Cryptococcus Malassezia Rhodotorula Trichosporon Geotrichhum |
|
|
What are the two main pathogenic yeasts?
|
Malassezia furfur
|
|
|
What does pathogenic Malassezia furfur cause?
|
pityriasis
|
|
|
Describe the clinical presentation of Malassezia furfur
|
- common
- mild - recurrent - pigmentation of redish, brown,white - affect upper trunk, arms and upper body - face legs and hands can be affected - common in the tropics - flaking of the skin/scaling - most commonly seen in caucausions --> hyperpidmentation of the trunk - depigmentation occurs in people of colour called pityriasis versicolor |
|
|
Describe the treatment for Malassezia furfur
|
imidiazoles
shampoos |
|
|
Describe the culure of malassezia furfur
|
- fluoresces under wood's lamp
- Dixon's media as it requires lipid base, or requires normal media + olive oil layer - 37C incubation |
|
|
Describe the microscopic appearance of malassezia furufr in microscopy and culture
|
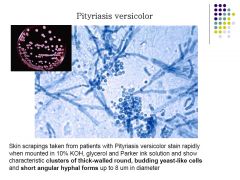
MICROSCOPY
- thick round oval cells - clusters - short angular hyphae forms CULTURE - small circular colonies pinkish |
|
|
Describe Dixon's agar
|
Specialised isolation medium containing glycerol-mono-oleate. oily based media.
|
|
|
What is the causative agent of white piedra
|
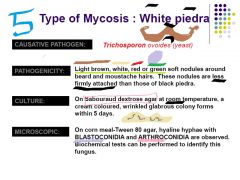
trichosporon ovoides
|
|
|
What is the clinical presentation of white piedra:?
|
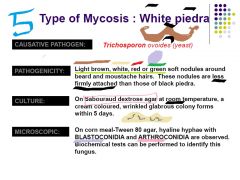
- light brown, green, red or white soft nodules around beard and moustache
- less firmly attached than black piedra |
|
|
What is the culture method for white piedra
|
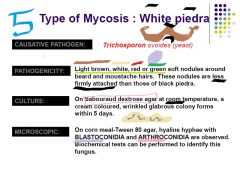
- SDA at room temperature
- white glabrous colonies within 5 days - wrinkled |
|
|
What is the microscopic appearance of trichosporon ovoides? How is white piedra dx?
|
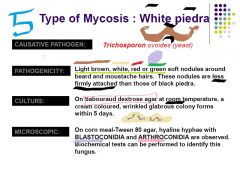
- corn meal-tween 80
- hyaline hyphae - blastoconidia - arthoconidia - biochemical tests |
|
|
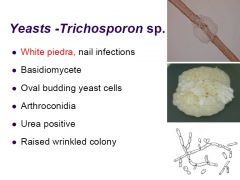
What are the main diagnostic features of Trichosporon sp.?
|
raised wrinkled colony
arthroconidia basidiomycete class urea positive oval budding yeast celle |
|
|
What class is Trichosporon?
|
Basidiomycete
|
|
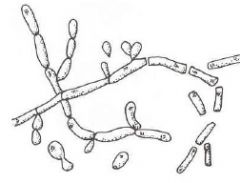
Identify
|
Trichosporon spp.
- oval budding yeast cells |
|

Identify
|
|
|

What other characteristics would we look for here
|
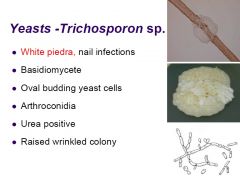
urease positive or negative?
culture that is raised and wrinkled colony arthroconidia oval budding yeast cells |
|
|
What is the causative agent of Tinea Nigra?
|
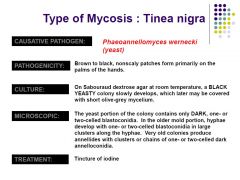
Phaeo -annello- myces wernicki
phaeannellomyces wernicki |
|
|
What is the clinical presentation of tinea nigra?
|
brown to black
non scaly patches hands |
|
|
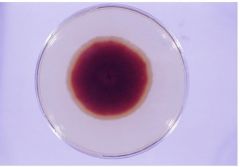
What cultural media and procedure is used to isolate tinea nigra. What are we likely to see?
|
SDA
room temp Black yeasty colony - initial slow growth short olive grey mycelium turn to olive as aerial mycelia develop |
|
|
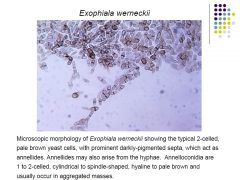
Describe the microscopic characteristics of phaeoannellomyces wernecki
|
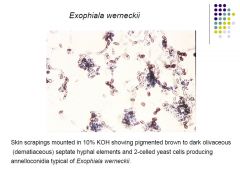
brown to dark
septate hyphae 2 celled yest cells annelloconidia |
|
|
Describe the microscopic characteristics of phaeoannellomyces wernecki
|
|

