Mild traumatic brain injury: How long does post-concussion syndrome last?
How long does post-concussion syndrome last?
(Punchline: It depends. On what? Keep reading.)
This is a question best answered by first explaining what post-concussion syndrome (PCS) is.
For starters, the medical community is moving away from the term PCS, and is adding an extra "P." This makes the abbreviation PPCS, which stands for Persistent Post-Concussion Symptoms.
While the semantics can be confusing and annoying, PPCS better describes what is going on: You had a concussion. The symptoms are persisting beyond what is considered normal — persistent post-concussion symptoms.
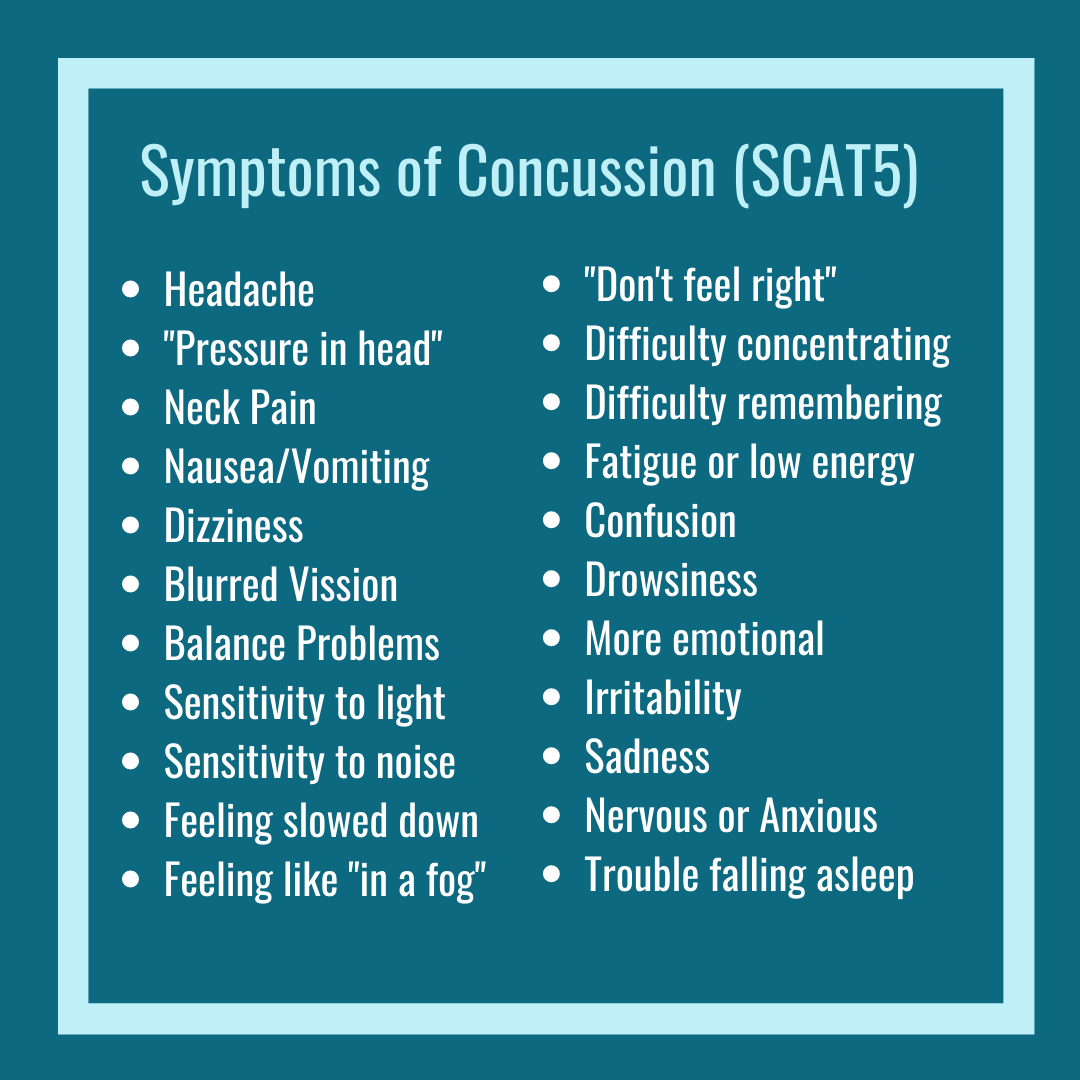
These are the symptoms included in the sideline Sports Concussion Assessment Tool 5th Edition (SCAT-5).
It's 2020. What is normal, anyway?
A concussion, also called a mild traumatic brain injury (mTBI), is a transient and functional injury to the brain.
Said differently, a concussion does not damage your brain. A concussion causes a temporary disturbance in normal function. How fleeting, you ask? You're full of great questions!
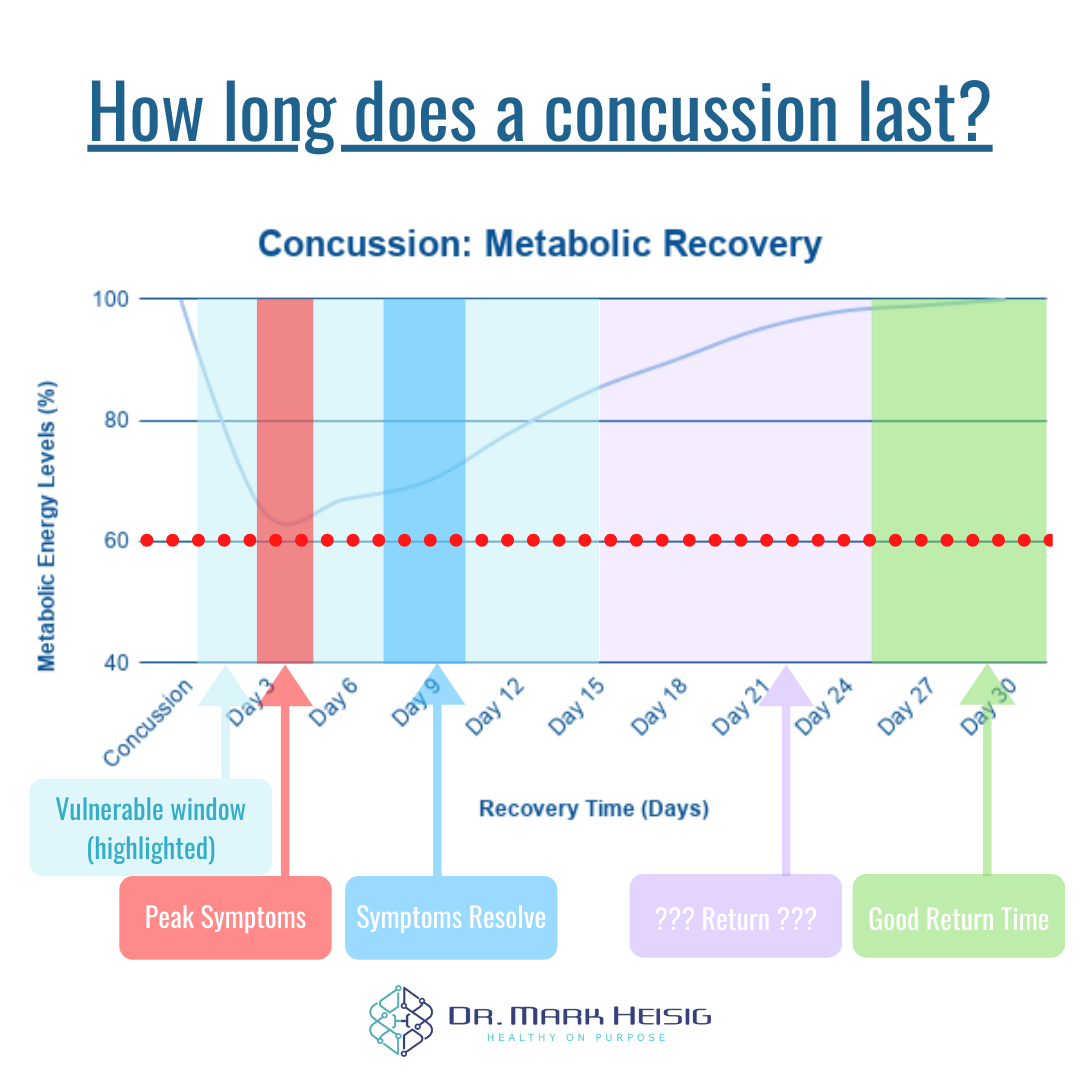
Concussion symptoms usually peak (are worst) 3-5 days after the injury.
Concussion symptoms typically go away in 7-10 days after the injury.
So, even in 2020, a typical concussion timeline would include your symptoms going away after approximately 7-10 days.
That does not mean you're off the hook, however! Your brain energy metabolism takes about 21-30 days before it's back up to speed. That is why it's essential to have a concussion-literate doctor on your team to make sure you return to school/work, sport, or life at the appropriate time.
What if symptoms don't go away in 7-10 days?
That's when we start to consider you an (ideally, temporary) member of the PPCS category. You had a concussion/mTBI - your symptoms are persisting.
There are no shiny new guidelines on PPCS quite yet; however, the new guidelines will likely be the same PCS guidelines (with an extra "P").
A few of the definitions stated that you have to have more than three symptoms for more than three months after your injury - and these symptoms have to interfere with your daily life.
According to the sport-centered Berlin Concussion Consensus, you had to have symptoms for longer than 14-30 days. And this makes more sense. After all, why would you wait to suffer from symptoms for over 90 days when the projected symptom recovery is 7-10 days?
Adults with symptoms longer than 14 days (2 weeks) are considered to have PPCS.
Children with symptoms longer than 30 days (1 month) are considered to have PPCS.
That said, if you have symptoms longer than 7-10 days in my practice, we evaluate you for reasons for delayed recovery right away. There's nothing to gain by either of us from delaying your recovery.
How long does PPCS last, then?
If you have symptoms lasting longer than 14-30 days, then it means you've got a roadblock.
*Pause for applause* Thank you, thank you! I know that was profound!
Jokes aside, in PPCS, there are very predictable roadblocks that can be in the way of your recovery. How long PPCS last, then, to some degree, is a matter of how quickly these roadblocks get identified and treated.
The 5 "Buckets" (roadblocks) of PPCS.
Concussion (mTBI) involved physical and metabolic changes due to the injury. Your head was either hit or whipped at a force at least 14X harder than needed for a whiplash injury. Which means you likely sustained a cervical ("whiplash") injury in addition to the concussion. And your brain went through an excitotoxic, inflammatory phase followed by a massive energy crisis.
Suppose you're not recovering from these symptoms in 7-10 days. In that case, it likely means that you are carrying one or more of the following heavy PPCS buckets.
Physiologic/Autonomic Bucket - This bucket relates to your blood flow. After a concussion, our sympathetic ("fight or flight") nervous system becomes more active. Simultaneously, we are less able to activate our parasympathetic ("rest and recover") nervous system. Problems in blood flow can lead to nearly every symptom experienced in concussion.
Metabolic/Hormonal Bucket - This bucket refers to your body and brain inflammation, as well as hormonal balance. Following a concussion, your gut can become inflamed, which leads to further brain inflammation. Additionally, the impact of the injury may have affected your pituitary gland. We often see growth hormone (GH) and testosterone (T) deficiencies after mild traumatic brain injuries. Like blood flow issues (above), having "inflammatory blood" or inadequate hormone levels can lead to many symptoms of mTBI.
Visual/Vestibular Bucket - This bucket correlates tightly to how you feel when you move through your world. Are things blurry? Are you dizzy? Foggy? Fatigued? Sure, these could be blood flow and metabolic issues. However, these could also be symptoms of a sensory mismatch between your eyes (vision) and ear (vestibular system). Your vestibular system is a tiny, fluid-filled system in your ear that detects your head movement through space - AND it provides information to your brain so that you can keep your eyes steady on a target while you move. This is why the world looks smooth and isn't choppy up and down while you walk or run. An impairment in how your eyes move or how your vestibular system perceives the world can keep you stuck.
Cervical Spine Bucket - This bucket is also very tightly linked to the visual/vestibular bucket. To feel clear-headed, move smoothly, and not feel dizzy, you need what you see to match what your vestibular system and spine are feeling. If one of those three systems is "off," then you will feel "off." Remember, the cervical spine (your neck) is how your head (and brain) is attached to your body. Concussions happen at 80-160g of force, while whiplash occurs at 4-5g of force (g-force, not grams). Most concussions also have a whiplash element that, if not treated, can contribute to many, many of your PPCS symptoms.
Mental/Emotional Bucket - This last bucket can be the most tricky because most of the onus gets placed on you as the patient. Mental and emotional health roadblocks like anxiety, depression, and PTSD are very common in concussion - and very closely associated with delayed recovery. Many concussion symptoms can be caused, not by a concussion, but by anxiety or depression, elevated stress levels, etc... Being honest and open with your concussion doctor and seeking an appropriate mental health professional can be huge.
How long do persistent post-concussion symptoms (PPCS) last?
The symptoms are as severe as the bucket is big.
The symptoms last as long as your body and brain hold the bucket(s).
Teaming up with a concussion-specialist can help you find your bucket(s). The goal, then, is to begin therapies and rehab that allows you to start to empty your buckets and ideally let them go.
A few important notes:
You may have sustained an mTBI that led to PPCS, and you achieve 100% recovery.
Someone else may have sustained a moderate or severe TBI, which led to PPCS (debatably not PPCS, but is simply their TBI), and may only achieve 70% recovery that requires ongoing maintenance.
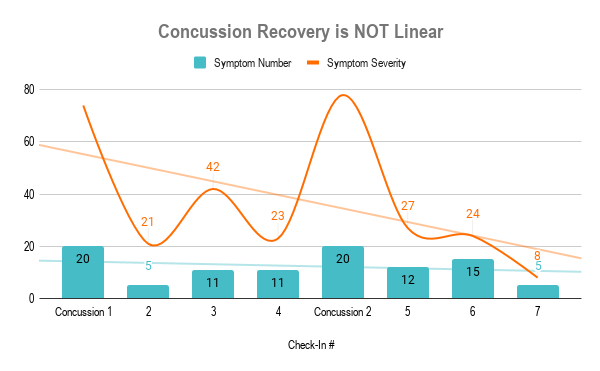
No recovery is linear or perfect. Recovery is often a roller coaster of ups, downs, wins, and losses. The ultimate result is you gaining more (if not all) of your life, work/school, or sport back.
Dr. Mark Heisig is a licensed naturopathic doctor with continuing mTBI education from The American Academy of Neurology (AAN), Complete Concussion. Management (CCMI) and The Carrick Institute. His office is located in Scottsdale, AZ.