Was the International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) needed? The short answer is yes. Will it change practice? The answer should be no if your practice was already consistent with recent international guidance for chronic coronary syndrome.1–3 Coronary revascularisation should be considered if patients have recurrent symptoms of angina not controlled by optimal medical therapy (OMT). However, the timing of when to offer revascularisation – and whether it offers benefits beyond symptom control – has remained in question. While guidance has emphasised OMT, there are wide disparities in how the guidance is interpreted and applied between specialities, hospitals and countries. Real-world practice demonstrates there is often routine revascularisation for those with demonstrable ischaemia on non-invasive testing and medication titration has remained limited. To understand whether this is the right approach, a randomised controlled study was carried out to compare a routine early invasive strategy with a strategy of medical therapy alone.
The headline message of the ISCHEMIA trial was that an invasive strategy was no better than medication for reduction in cardiovascular events. While this headline suggests conclusion of the debate, it is simplistic and misses the nuanced learning from the study. Albeit clearly an ambitious, large and costly study, questions remain on whether the study design was the most definitive approach. There are also concerns on whether the selected cohort represents the wider population of patients with chronic coronary syndromes. In this editorial, we will consider the ISCHEMIA study, along with older data, from the viewpoint of the interventionalist.
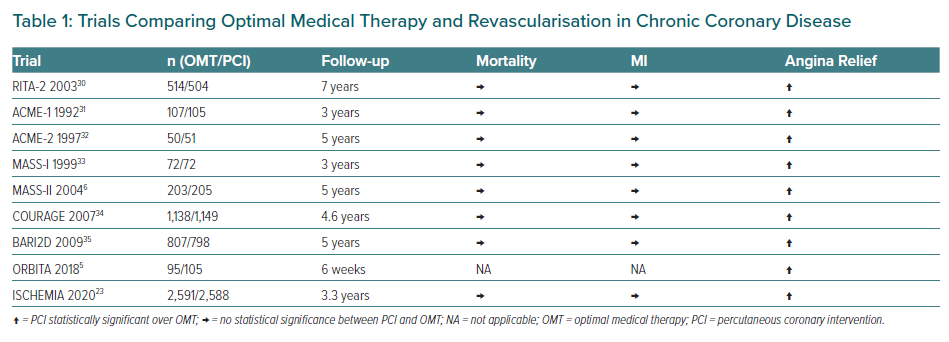
Ischaemic heart disease (IHD) remains the leading cause of mortality and morbidity worldwide, causing more than 9 million deaths per year globally.4 Management requires a combination of medical therapy with or without revascularisation. Since both MI and chronic ischaemia have deleterious clinical events through vessel occlusion, it is intuitive to think that relieving severe coronary stenoses and thus improving blood flow would improve outcomes in IHD. Percutaneous coronary intervention (PCI) studies show that coronary intervention successfully removes or reduces ischaemia. This includes modern studies such as the double-blind, randomised controlled trial ORBITA.5 Older studies using coronary artery bypass surgery, albeit before the advent of medical therapy, had shown a reduction in mortality.6–9 Older PCI studies had suggested percutaneous revascularisation reduced cardiovascular mortality and MI.10 However, more recent studies have failed to show a mortality benefit. This includes large randomised controlled studies, such as COURAGE, BARI2D and FAME 2.11–13 Table 1 shows a summary of the key studies from 1992 to 2020.
Does Ischaemia Matter?
Previous interventional studies included patients based on severity of angiographic stenosis without confirmation of ischaemia. Invasive pressure wire studies have repeatedly demonstrated angiographic appearance relates poorly to ischaemia.11 It is likely that prior studies will have included patients without ischaemia and thus revascularisation would give minimal benefit; such recruitment would dilute signals of benefit. Those studies that did seek ischaemia demonstrated only relatively limited levels of it.14 This issue with prior studies formed the basis of the ISCHEMIA study, which originally aimed to recruit patients with moderate to severe levels of ischaemia.
This is a valid study design strategy as it addresses the tightly held belief that forms the basis of the central paradigm in the management of IHD.15 Patients with angina are typically referred for non-invasive ischaemia testing according to the local availability (tests range from those with limited sensitivity and specificity, such as exercise stress ECG testing, to those with higher accuracy such as stress perfusion myocardial resonance imaging or PET). In some countries, repeated annual ischaemia testing generates a lot of routine elective activity.16,17 However, data relating ischaemia – or its improvement following revascularisation – with hard clinical events remain limited.
Large observational studies have suggested limited value to routine revascularisation for ischaemia.18,19 On the other hand, a propensity-matched analysis in 39,131 Canadian patients with stable IHD undergoing early revascularisation (n=23,992) or treated conservatively (n=15,139) found, over 4 years of follow-up, a significant reduction in death and MI with revascularisation.20 The relationship between ischaemia and exercise capacity was also questioned in the small but well performed randomised placebo-controlled PCI study ORBITA. Although ORBITA demonstrated clear improvements in both invasive and non-invasive markers of ischaemia, there was no demonstrable improvement in treadmill exercise time between those treated with sham-PCI and those with true relief of the coronary stenosis. This was measured at 6 weeks and whilst there are those who suggest a longer follow-up would have altered outcomes, this is difficult to imagine since PCI relieves the stenosis and ischaemia immediately. At the end of the study, after blinding was removed, 80% of those in the sham arm chose to have coronary intervention. Many claim this is crossover: it is not. The patients had been advised to have PCI by their usual care practitioners before volunteering to participate in the study. They had expected to have PCI and their participation was prefaced with the expectation that they would get it within the usual waiting time built into the local healthcare system.
Does the Mode of Revascularisation Matter?
The debate over revascularisation approaches – specifically PCI versus coronary artery bypass grafting (CABG) – has remained fractious. In many ways, it was always a sign of great hubris that the two very different techniques are compared at all. CABG offers an entirely separate conduit to perfuse the myocardium beyond the stenosis while PCI offers a focal solution to a single narrowing. Intravascular imaging and physiology often reveal that coronary disease is rarely focal, undermining the PCI strategy. Inadequate technique undermines the longevity of a given stent. Older studies, such as COURAGE, will have used older PCI techniques and had older stent technologies more prone to failure. These events are more notable and are often clinically detected. While CABG provides a more optimal solution in many anatomical settings, such as those with a high SYNTAX score, the acceleration of native disease and high failure rates in saphenous vein grafts mean that many patients are left with chronic ischaemia with or without significant cardiac events.21,22 Graft attrition is not always clinically detectable.
Even allowing for the very different mechanistic approaches, there are many technical or patient factors to favour one over the other, and these factors can drive outcome differences. In a study such as ISCHEMIA, where the mode of revascularisation was selected by the physician based on normal clinical criteria, one can draw limited value from comparing the mode of revascularisation.
Importantly, ISCHEMIA excluded patients that would typically be referred for revascularisation with CABG such as patients with significant left main stem (LMS) disease or patients with severe coronary disease with left ventricular impairment.23 Although PCI and CABG were analysed as the same treatment in ISCHEMIA, patients that would have been referred for CABG in the real world based on evidence based guidance were excluded from the study.
What Does the ISCHEMIA Trial Add?
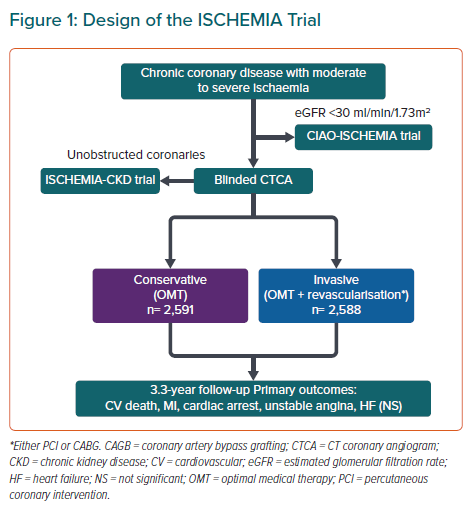
ISCHEMIA represents the culmination of an audacious and admirable research efforts of an international team, lasting more than 10 years, with more than US$100 million of National Institutes of Health funding. The design emphasised the use of careful core laboratory validation of ischaemia testing. It randomised chronic coronary syndrome patients with moderate to severe ischaemia to early invasive investigation or OMT after a CT coronary angiogram (CTCA) as detailed in Figure 1.
Importantly, invasive assessment did not mean mandatory invasive treatment and physicians were free to treat according to the invasive findings and this included medical therapy, PCI or CABG. Physicians were encouraged to use the latest technologies, including pressure wires, but uptake remained low. This may be because of resource issues and because patients already had positive ischaemia tests to enter the study.
The total number of patients enrolled in the trial was 5,179 (2,588 in the invasive group and 2,591 in the medical therapy group). Median duration of follow-up was 3.2 years and median patient age 64 years; 23% were women and 41% had diabetes. A total of 54% of participants had severe baseline inducible ischaemia on stress testing – this included ECG exercise stress testing, which was added to the study because of slow recruitment. Exclusion criteria included significant LMS stenosis (blinded CTCA), chronic kidney disease (CKD), significant symptom burden, severe left ventricular impairment or heart failure or recent revascularisation with 12 months.
Interestingly, a significant proportion (34%) had no angina at baseline implying that they had non-invasive ischaemia testing for other reasons – perhaps work-up prior to other elective surgery. Rates of the primary outcome of cardiovascular death, MI, resuscitated cardiac arrest, hospitalisation for unstable angina or heart failure at 3.5 years were 13.3% in the invasive group versus 15.5% in the OMT group (p=0.34).23 There were also no differences in the primary outcome when stratified by subgroup, such as diabetes or single versus multivessel disease. Importantly, there was no association between degree of ischaemia and all-cause mortality. These results should be interpreted in the context of the short-term follow-up period. It is possible that the increased incidence of spontaneous MI in the OMT group may affect longer-term outcomes in favour of revascularisation. Indeed, a recent publication by the same group found that longer follow-up is needed to assess whether reduction of spontaneous MI in the revascularisation arm observed in their meta-analysis translates into improved patient outcomes.24
It is perhaps inevitable that these results led to striking headlines, such as “ISCHEMIA: invasive strategy no better than meds for CV events” and “ISCHEMIA: invasive treatment not better than meds in patients with stable ischemic heart disease”.25,26 However, it is worth noting that the randomisation was to early angiography and not to early invasive treatment per se. Eighty per cent had revascularisation, while 20% had treatment deferred. In the deferment group, two-thirds (66%) had normal coronary arteries, while a third had coronary vessels too severe for revascularisation. In the 80% who had revascularisation, 74% (around 1,532 patients) had PCI, while 26% (538) had bypass surgery. This is evident in the usage of dual antiplatelet therapy in the study: this peaks at 60%. Around 26% of patients in the medical arm underwent angiography with 21% being revascularised. It is also worth noting that of the PCI performed, only 93% was considered successful.
Those patients with the most symptoms did better in the invasive arm having undergone revascularisation. Angina relief and quality of life were statistically better with the invasive strategy, durable out to 3 years of follow-up. The probability of rendering patients angina-free was greater in the higher symptom burden group, reflected by lower Seattle Angina Questionnaire scores.
Both groups had similar numbers of non-fatal MI with the number of spontaneous MI higher in the conservative arm and a higher number of peri-procedural MIs in the invasive group. Although there was a higher number of peri-procedural MIs in the invasive group, it is important to note that this did not translate into mortality. Spontaneous infarctions however on the other hand confer a higher risk of subsequent death.27,28
ISCHEMIA-CKD, comprising 777 participants, was a pre-specified subgroup of the main study assessing those patients with CKD or end-stage renal failure. This is a higher-risk cohort of patients who are often under-treated because of concerns over kidney function. This subgroup also demonstrated no reduction in death or MI with routine invasive strategy compared to OMT in patients with severe CKD (i.e. estimated glomerular filtration rate <30 ml/min/1.73 m2).29
Application of ISCHEMIA in Real-world Practice
Patients remain the true winners in the ISCHEMIA debate. Those who meet the entry criteria – including a low symptom burden – can choose OMT, with an invasive strategy only required if there are on-going symptoms.
The study also shows an increase in spontaneous MI after the first year in the conservative arm. Therefore, early invasive strategy should remain available for those that cannot tolerate medical therapy or those with worsening symptoms despite optimal therapy.
Considering the safety of revascularisation and significant improvements seen in quality of life with interventions, we can make the argument to offer an invasive strategy early in the patient journey. In the past, cardiologists may have been eager to expedite invasive management of patients with low symptom burden but significant ischaemia. A key take away from ISCHEMIA study is that mortality in patients with chronic coronary syndromes is relatively low with OMT and treatment should be individualised to patients.
Those who do not meet the entry criteria should be treated as per established pathways. Unstable angina and acute coronary syndromes were not included in the study. Those with intolerable angina were also not included.
When using medical treatment, this should be as close to clinical studies to be able to claim results seen in studies. Outside of closely monitored research studies, this can be challenging to deliver. The ORBITA study had close one-to-one consultant supervision of medical therapy escalation – rarely possible in routine clinical practice.
As interventionalists, we should do our best to communicate these results effectively to our patients and colleagues when discussing treatment options. The discussion that revascularisation may not prolong your life, but prevent spontaneous MI, alleviate symptoms and improve quality of life, is one we should continue to have with our patients. It is very important to stress that this is set against trial setting medical therapy. There will always be the group of patients who were excluded from ISCHEMIA and a heart team approach should always be best practice. These patients represent a group considered at significant risk because of significant LMS disease, severe heart failure or CKD.
A key message for interventionalists and all physicians is that modifying the atherosclerotic disease process should be the cornerstone of management. Addressing cardiovascular risk factors with lifestyle modifications is an essential part of the treatment plan. The application of the ISCHEMIA trial results of moderate to severe ischaemia seen in chest pain clinics should strengthen the argument for initial optimal medical management offering an invasive strategy on an individual patient level. Results from longer term follow up of ISCHEMIA trial patients, ORBITA 2 and the debate of cost effectiveness of adding revascularisation to OMT is one that will need to be analysed more closely. This involves a more complex analysis quality-adjusted life years, burden on healthcare system and quality of life.
The ISCHEMIA trial should inform the cardiologist and physician how to better communicate treatment options to patients with chronic coronary syndromes. OMT is the cornerstone of patient management.