Spondylodiscitis After Surgery for Pelvic Organ Prolapse: Description of a Rare Complication and Systematic Review of the Literature
- 1Department of Gynecology and Obstetrics, Institute for Maternal and Child Health Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) “Burlo Garofolo”, Trieste, Italy
- 2University Clinical Department of Medical, Surgical and Health Sciences, University of Trieste, Trieste, Italy
- 3Department of Obstetrics and Gynecology, ‘Filippo Del Ponte' Hospital, University of Insubria, Varese, Italy
Background: Spondylodiscitis can be a rare complication of gynecological surgery, typically of procedures involving the sacrum and the sacrospinous ligament. This report presents a case of spondylodiscitis arising after a laparoscopic sacrocolpopexy with a mesh. We also review the literature finding 52 cases of spondylodiscitis following sacrocolpopexy and (or) rectopexy with or without a mesh.
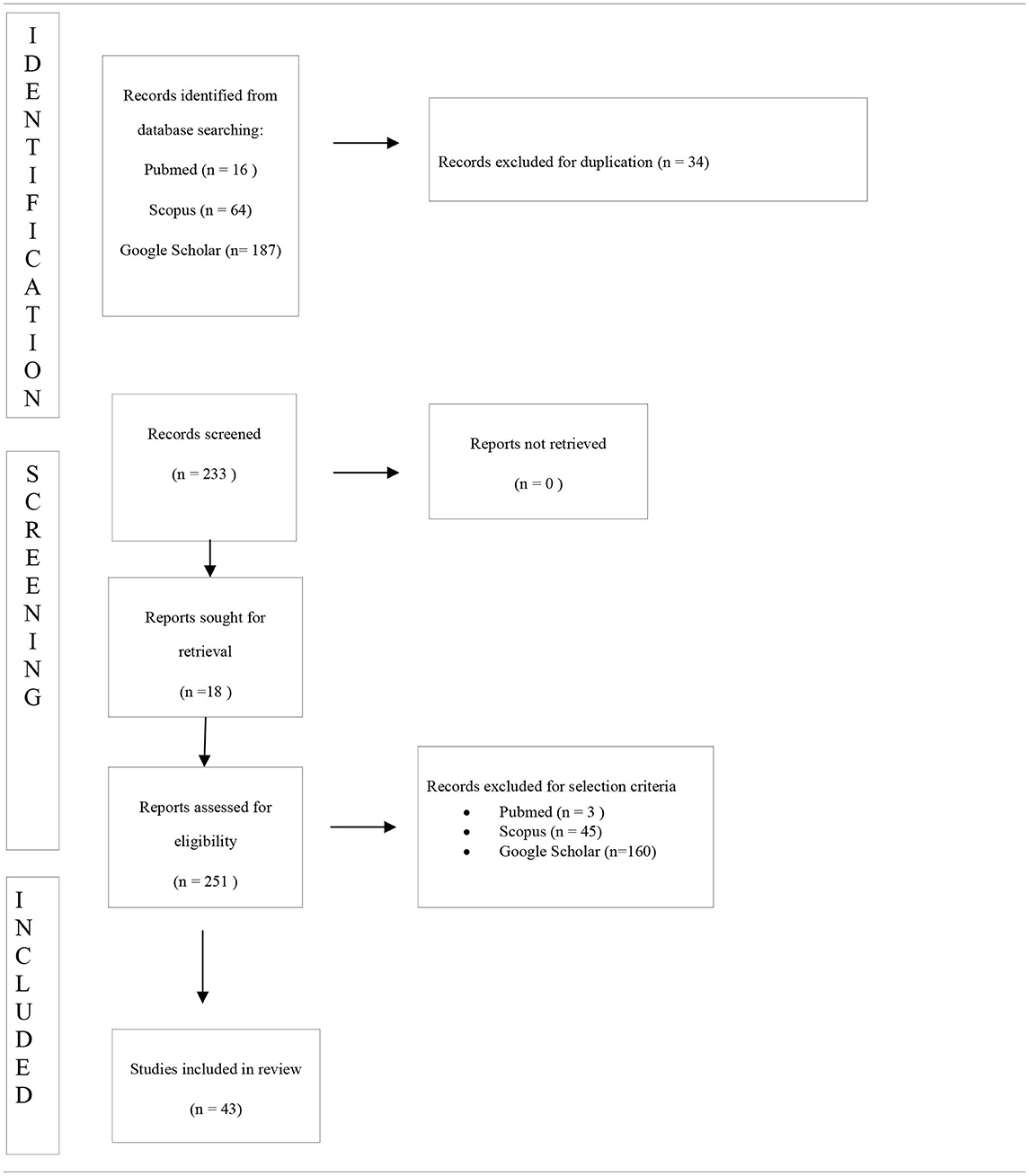
Methods: We performed a comprehensive search from the electronic databases MEDLINE (Pubmed), Scopus, Web of Science, Embase, CINAHL, and Google Scholar from 1990 to February 2021 in order to identify case reports or case series reporting on spondylodiscitis after rectopexy or sacrocolpopexy.
Results: We identified 52 total postoperative spondylodiscitis. We examined the mean age of patients, the surgical history, the time from initial surgery to spondylodiscitis, the presenting symptoms, the diagnostic tools, the medical and surgical treatment, the type of mesh used, the surgical access, and the possible causes of spondylodiscitis.
Conclusions: Diagnosis of spondylodiscitis may be challenging. From our review emerges that recurrent pelvic pain and lumbosciatalgia may be signals of lumbar spondylodiscitis. Magnetic resonance is the gold standard examination for spondylodiscitis. Surgical practice needs to be improved further in order to establish the best procedure to minimize the incidence of this complication. Awareness of symptoms, timely diagnosis, and treatment are fundamental to prevent irreversible complications.
Introduction
Pelvic organ prolapse results from laxities of the ligaments, fascia, and muscles supporting the pelvic organs (1). Rectopexy and sacrocolpopexy are established surgical techniques to restore anatomy and organ function. The promontory of the sacrum is widely used as the proximal fixation point for laparotomic or laparoscopic- or robotic-assisted recto- and sacrocolpopexy as well for other surgical techniques (2). Depending on the technique, the organ fixation is performed either by direct sutures or by using a mesh that is sutured or tacked to the promontory of the sacrum. We report a case of spondylodiscitis arising as a complication of a laparoscopic sacrocolpopexy with a mesh. The spondylodiscitis had not been recognized immediately and the diagnosis was reached only after a magnetic resonance was performed for the recurrence of pelvic pain and lumbosciatalgia. The report also discusses 52 cases available in literature of spondylodiscitis following sacrocolpopexy and (or) rectopexy with or without a mesh. We evaluate the current knowledge for the diagnosis and management of spondylodiscitis after surgery.
Case
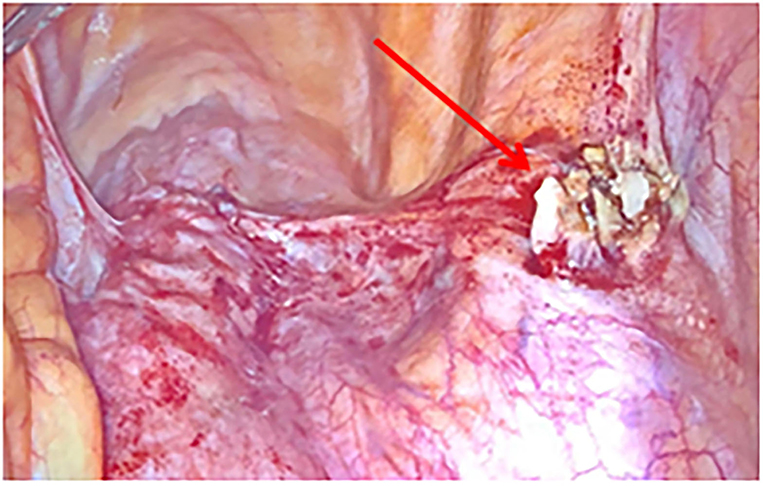
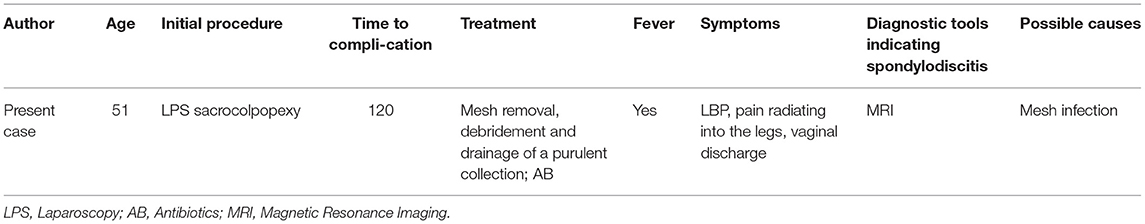
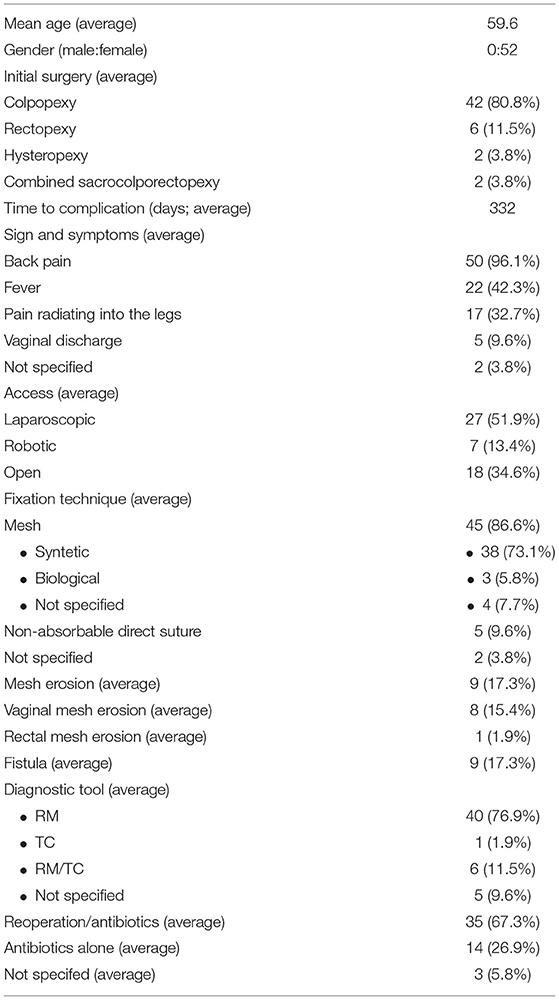
A 51-years-old woman with three previous vaginal deliveries suffered from stage IV uterine and bladder prolapse for 1 year and it worsened in the last 6 months. In May 2020, at the Gynecology Department of the Institute for Maternal and Child Health “IRCCS Burlo Garofolo” of Trieste, the patient underwent laparoscopic hysterectomy; adnexectomy and sacrocolpopexy were performed using a polypropylene mesh anchored with tacks. The postoperative course was initially uneventful and the patient was then discharged on the third postoperative day. One week later, she started to suffer from pelvic pain and approached the emergency department. The transvaginal gynecological ultrasound performed showed a rectovaginal hematic effusion of 80 cc. The woman required hospitalization. Her blood exams were normal except for leukocytosis. She was afebrile and received an intravenous empirical antibiotic treatment with Gentamicin 5 mg/Kg/die and Clindamycin 600 mg x3/die, pending the outcome of blood cultures, which later turned out to be negative. Blood routine examination was normal. After 7 days of antibiotic therapy, the pelvic pain disappeared; the woman became asymptomatic and was discharged. Eighty-three days after the laparoscopic sacrocolpopexy, the patient manifested painful symptoms again and she returned to the emergency room complaining of pelvic pain, back pain, and lumbosciatalgia. A lumbosacral magnetic resonance was performed. The exam showed a signal alteration in the L5-S1 vertebrae with a marked edema of the perivertebral tissues. The patient was therefore hospitalized for the third time at the Gynecology department. Laboratory findings included a white blood cell count of 10,920/ml and C-reactive protein of 54 mg/l. The blood cultures performed resulted in negative again. A magnetic resonance of the pelvis was carried out to complete the study of the lumbosacral district: it confirmed an inflammation of L5-S1 vertebrae, suggesting a spondylodiscitis (Figure 1). Intravenous antibiotic therapy with clindamycin 600 mgx3/die and Gentamicin 5 mg/kg/die started on hospitalization and ended after 14 days. After a multidisciplinary discussion, the medical staff decided that the situation required a revision surgery. Therefore, the patient underwent a second operation 91 days after the laparoscopic sacrocolpopexy. Mesh removal with two metallic tacks, debridement, and drainage of a purulent collection were performed (Figure 2). Furthermore, in those same days, the patient experienced foul-smelling vaginal discharge and had a fever. The intraoperative microbiological samples showed the presence of several colonies of Staphylococcus Aureus resistente alla meticillina (MRSA) and Peptostreptococcus asaccharolyticus. An intravenous targeted antibiotic therapy with vancomycin 2 g/die and rifampicin 600 mg/die was started. Three days later, the patient underwent a CT scan that showed a voluminous collection of pus in the abdominal cavity, concentrated in particular in the pelvis between the vagina and the rectum. Moreover, the CT scan showed a fistula with a median length of about 4 centimeters between the pelvic purulent collection and the vaginal vault (Figure 3). The patient was discharged 21 days after the reoperation. Oral antibiotics (sulfamethoxazole/trimethoprim 160/800 mg cp, 2 cp ×2/die and rifampicin 600 mg/die) were administered to treat the spondylodiscitis for six more weeks. At discharge, the patient was asymptomatic. She underwent a further magnetic resonance performed 121 days after the laparoscopic sacrocolpopexy: the exam showed a volumetric decrease of the pus collection in the pelvis and a persistence of the fistula reaching the vaginal vault. The woman had no pelvic pain, back pain, lumbosciatalgia, or any other symptoms (Table 1). The patient received a close follow-up at our center. Gynecological visits and pelvic ultrasounds were performed monthly. Six months after the second surgical procedure, the woman reported feeling well and denied having any symptoms. Two more pelvic magnetic resonances were performed, respectively, 92 and 169 days after the second surgery, showing a progressive decrease of the purulent collection and a spontaneous resolution of the fistula (Figure 4).

Figure 1. Pelvic MRI: enhancement of soft tissues surrounding the L5-S1 vertebrae (arrow). MRI, magnetic resonance imaging.
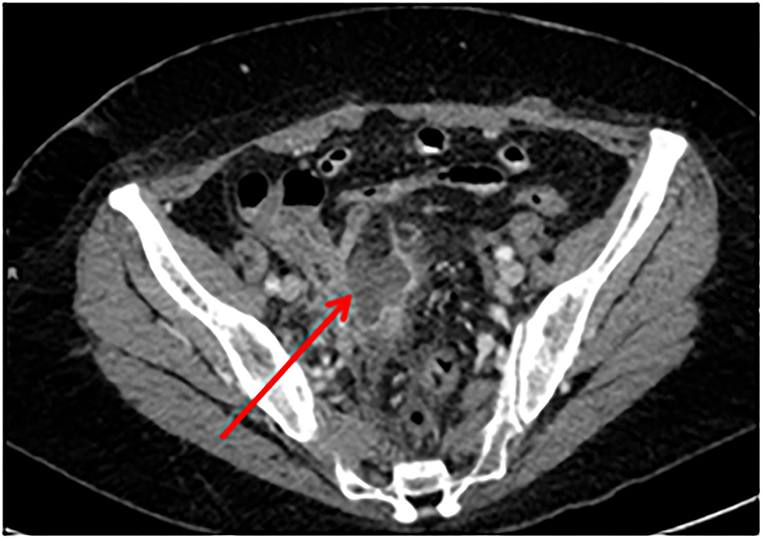
Figure 3. CT: purulent collection of the pelvis between the vagina and the rectum (arrow). CT, computed tomography.
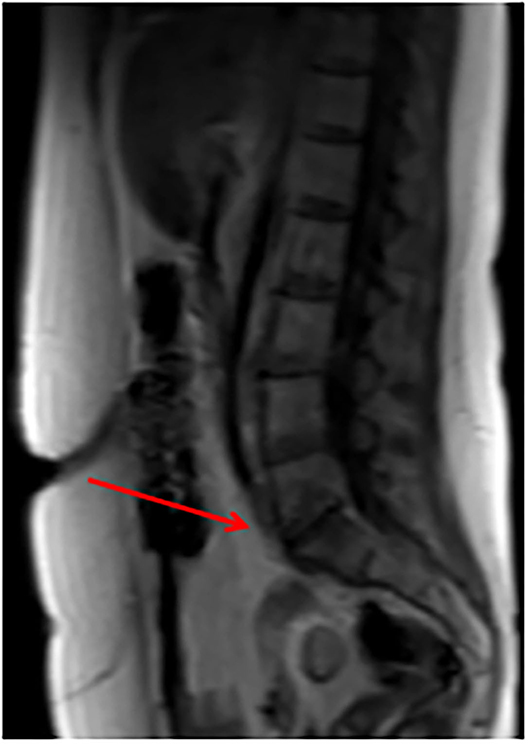
Figure 4. Pelvic MRI 169 days after the second surgery showing a progressive decrease of the purulent collection and a spontaneous resolution of the fistula.
Methods
This retrospective observational descriptive study was approved by our Institutional review board (IRB-Burlo RC 08/2020).
Eligibility Criteria
We performed a comprehensive search from the electronic databases MEDLINE (Pubmed), Scopus, Web of Science, Embase, CINAHL, and Google Scholar from 1990 to February 2021 in order to identify case reports or case series reporting on spondylodiscitis after rectopexy or sacrocolpopexy. We examined in literature the mean age of patients, the surgical history, the time from initial surgery to spondylodiscitis, the presenting symptoms, the medical and surgical treatment, the diagnostic tools, the type of mesh used, the surgical access, and the possible causes of spondylodiscitis.
Information Sources
Pubmed, Scopus, Web of Science, Embase, CINAHL, and Google Scholar were searched up to February 2021. The manuscripts considered were published in 1990. Only articles in English were included in the search. The research strategy adopted included different combinations of the following terms: (spondylodiscitis) AND (colpopexy or rectopexy) AND (prolapse). We identified 16 manuscripts from Pubmed database, 64 from Scopus database, and 187 manuscripts from Google Scholar database.
Study Selection
All studies identified were listed by title, authors, and year of publication. We have followed the PRISMA checklist. The PRISMA flow diagram of the selection process is provided in Table 2. Two independent investigators screened the title and abstracts based on the predefined eligibility criteria. The same two authors reviewed independently the full text of papers identifying those to be included in the review. Discrepancies were resolved by consensus. Thirty-four manuscripts were excluded for duplication. Two-hundred-eight works were excluded for selection criteria. Eighteen manuscripts were detected through the references of the works that had been identified with the research on MEDLINE (PubMed), Scopus, Web of Science, Embase, CINAHL, and Google Scholar.
Assessment of Methodological Quality
The methodological quality of the included studies was assessed using the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for case reports and case series (Supplementary Material).
Assessment of Risk of Bias
The main risk of bias of the presented work is that almost all papers selected in the literature are case reports.
Data Analysis
Studies included are almost all case reports due to the rarity of this evenience. For this reason, we presented data in a descriptive manner.
Results
We describe our clinical case, and then we perform a literature review with MEDLINE (PubMed), Scopus, Web of Science, Embase, CINAHL, and Google Scholar.
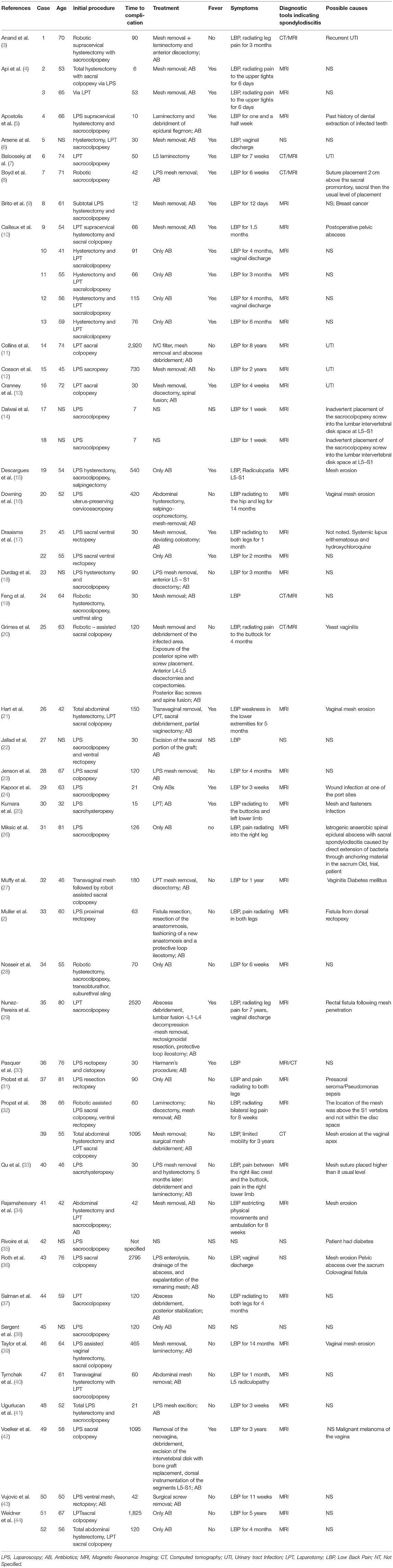
We found 41 manuscripts about spondylodiscitis following sacral colpopexy or rectopexy or combined sacro/rectopexy and two reports of spondylodiscitis following a sacrohysteropexy. Summary of the characteristics is presented in Table 3. Fifty-two women with a median age of 59.6 years were diagnosed with spondylodiscitis after a median of 332 days from the initial surgery. Initial surgery consisted of sacrocolpopexy (n = 42; 80.8%), rectopexy (n = 6; 11.5%), hysteropexy (n = 2; 3.8%), and combined sacrocolporectopexy (n = 2; 3.8%). The most common surgery technique used was laparoscopic access (n =27; 51.9%), followed by open access in 34.6% of cases (n = 18), and robotic access in the minority of cases (n = 7; 13.4%). Pexy was performed using synthetic meshes (n = 38; 73.1%), biologic meshes (n = 3; 5.8%), in four cases (7.7%), the type of mesh used was not specified. Direct sutures were used in five cases (9.6%) and the type of technique used was not specified in two cases (3.8%). All patients complained of back pain (n = 50; in two cases, the symptoms were not specified), almost half of the patients (42.3%, n = 22) had fever. Other common presenting symptoms were pain radiation into the legs (n = 17; 32.7%) and vaginal discharge (n = 5; 9.6%). A mesh erosion (n = 9; 17.3%) or a fistula formation (n = 8; 15.4%) was detected in a minority of cases. The gold standard for diagnosis of postoperative spondylodiscitis is pelvic magnetic resonance. Most of the cases analyzed by our review have been diagnosed performing a pelvic resonance (n = 40; 76.9%), in one case, the diagnosis was reached using a CT scan. Six women underwent both exams, while in five patients, the diagnostic tool chosen was not specified (Tables 3, 4). Antibiotics alone were effective in only 14 cases (26.9%), whereas 67.3% of the patients (n = 35) had to undergo additional surgical treatment.
Discussions
Surgeons should be aware of the potential risk of spondylodiscitis caused by a sacrocolpopexy and (or) rectopexy with and without the use of a mesh. Sacrocolpopexy is described to be one of the safest procedures for the surgical treatment of prolapse (6). Monofilament polypropylene mesh is the graft of choice (45). In literature, there are 52 cases of lumbar spondylodiscitis as a result of sacrocolpopexy and (or) rectopexy or sacrohysteropexy performed using synthetic meshes (n = 38), biologic meshes (n = 3), direct sutures (n = 5), with four cases where the type of mesh used is not specified and two cases where the technique is not mentioned (6). The characteristics of patients are summarized in Tables 3, 4. The mesh is placed on the ventral side of the vagina and fixated with stitches or tacks on the sacral promontory (1). Qu et al. reported that the possible causes of spondylodiscitis are mainly related to the mesh (32%) and to other infections (29%), including urinary tract infections, vaginitis, postoperative pelvic abscess, wound infection, dental extraction of infected teeth in one case (33), while the other causes of spondylodiscitis are not known. In their manuscript, mesh-related causes of spondylodiscitis include vaginal mesh erosion, mesh penetration into the rectum (one case), and suture placement on the sacral anterior ligament at a higher level than the usual fixation (33). Mesh erosion after ventral rectopexy and sacropexy varies greatly across studies and are reported rates between 1.3 and 6%. The deterioration of the mesh may predispose to infections, leading to the migration of bacteria from the vagina or rectus to the prothesis and its fixation site (46). Sacral colpopexy can be performed with open, laparoscopic, or robotic– assisted techniques. Our research revealed that 51.9% of cases underwent a laparoscopic colpopexy. An open access was adopted in 18 cases (34.6%) and a robotic-assisted surgery was performed in a minority of patients (seven cases; 13.4%). This may suggest laparoscopy as a risk factor for spondylodiscitis. Nevertheless, it should be taken into account that laparoscopy is the preferred technique for this type of surgery (45).
Interestingly, the study by Unger et al. compared the results between laparoscopic sacrocolpopexy and robotic-assisted sacrocolpopexy in 406 women. The rate of postoperative osteomyelitis was similar between the two groups (47). Grevez et al. reported the absence of postoperative spondylodiscitis among the 20 cases of abdominal promontofixation analyzed in their systematic review (48). The different haptic feedback of the three surgical techniques could be the key to explain these data. A decreased haptic feedback could elevate the risk of penetration deeper into the anterior longitudinal ligament, which allows bacteria to directly access the bone or disc. There are insufficient and conflicting data about the possible risk associated with performing hysterectomy (total or subtotal) or uterus preservation during sacrocolpopexy. The issue of uterine preservation or excision during the procedure requires further clarification (45). The most common type of mesh used is the polypropylene (45). From our data emerges that 73.1% of postoperative spondylodiscitis arises after a surgical prolapse correction with a synthetic prosthesis. It can be hypothesized that synthetic grafts can be a vehicle for germs colonization and their subsequent spreading into the disc and the bone. However, a bias could be represented by the almost exclusive use of this type of synthetic grafts in all sacrocolpopexy. So, we cannot generalize considering them as a risk factor for spondylodiscitis. It is known that the origin of spondylodiscitis is multifactorial and it can occur with classic sutures (6). The mesh can be anchored using stitches of different types (also barbed one) (49) or tacks. It could be supposed that tacks could penetrate more easily into the anterior longitudinal ligament exceeding its thickness and leading to spondylodiscitis. The majority of articles do not describe the way of mesh fixation to the anterior longitudinal ligament. The lack of data does not allow to have certain information about this aspect and to understand which is the best tool of fixation. However, surgeons are able to minimize the risk of spondylodiscitis by carefully placing the presacral fixation, putting stitches or tacks into the anterior longitudinal ligament avoiding the disc space (49). The surgeon has to keep in mind that the anterior longitudinal ligament is only 1–2 mm thick and this could lead to an easy perforation of it (50). Furthermore, mesh suture load into the vaginal wall should be minimized in order to decrease the risk of organism migration between the mucocutaneous layer and the mesh (51). From our review emerged that the onset of spondylodiscitis varies greatly, from 1 month to 8 years after surgery. In 76.9% of cases (40 cases), spondylodiscitis occurred within 1 year after surgery. The mean time of presentation of this postoperative complication is 332 days. This could be explained by fewer painful symptoms, which delay the diagnosis of complications. All patients complained of back pain (n = 50; in two cases, symptoms were not specified), pain radiating into the legs, and consecutive motor weakness and sensory changes are only found in a minority (n = 17; 35%). Less than half of the patients (n = 22; 42.3%) have fever. Some women declare also vaginal discharge (n = 5; 9.6%). Pelvic magnetic resonance appears to be the gold standard for the diagnosis of spondylodiscitis. It is the diagnostic tool used in the majority of clinical cases (n = 40; 76.9%). The magnetic resonance demonstrates to be the most sensitive (93–96%) and specific (92–97%) imaging modality for the diagnosis of spondylodiscitis. On the other hand, CT gives a more detailed image of bone destruction (second choice) (20). In the presence of typical clinical symptoms, imaging studies of the lower spinal cord should be performed without delay. The diagnostic process should require blood and urine cultures completed by a gynecological evaluation to exclude vaginal infections (20). From the review of Mavrogenis et al., it emerges that Staphylococcus aureus has become the most frequent bacterium responsible for vertebral infections, accounting for 20–84% of all cases (52). Additionally, Enterobacteriaceae spp. are implicated in 7–33% of pyogenic vertebral infections. Escherichia coli is the most common pathogen in this group, followed by Proteus and Klebsiella. Streptococci and Enterococci are common causes responsible for 5% to 20% of cases, whereas, anaerobes are isolated in <4% (20, 52–56). When blood cultures are negative, CT-guided biopsy is recommended (20). Our comprehensive research revealed that in many cases, the conservative treatment with antibiotics is not enough and surgical therapy is needed in 67.3% of the cases (Table 4). A possible explanation could be that prosthetic material acts as an infection route and reservoir for bacteria, as reported by Muller et al. and Qu et al. in their reviews. Surgical treatment usually includes mesh removal, laminectomy, discectomy, and spine-stabilizing procedures (these last in case of either nerve compression or spinal instability) (2, 33). Intravenous antibiotic therapy is recommended for 4–8 weeks; after that, a 3-month course of oral antibiotic therapy should follow (2).
The strength of our study is the long period of time overviewed in literature: we analyzed the cases of postoperative spondylodiscitis arised in the last 30 years. All the studies selected during the eligibility phase (according to the PRISMA guidelines) have been further evaluated by manual comparison of populations, study settings, and authors to exclude overlapping cases. However, the limitation of our study is the retrospective nature of it, and the main risk of bias is represented by the presence of almost all case reports among the papers selected.
Although spondylodiscitis remains a rare evenience, it can lead to irreversible complications. Indications to surgical treatment include doubtful diagnosis, progressive neurological deficits, progressive spinal deformity, failure to respond to treatment, and unresolved pain. Today, the time spanning from the initial procedure to the diagnosis of spondylodiscitis varies greatly and ranges from 6 days to 8 years. A reasonable level of suspicion and a certain degree of multidisciplinary approach are fundamental for a prompt diagnosis and a successful treatment.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Written informed consent was obtained from the relevant individual for the publication of any potentially identifiable images or data included in this article.
Author Contributions
GS and GT: conceptualization and writing—original draft preparation. GS, GT, and GR: methodology. GT and AL: software. GS, FR, and GR: validation. GT and FR: formal analysis. GS, FM, and GD: investigation. GS, GD, FM, and GR: data curation. GS, FR, AL, and GT: writing—review and editing. AL: visualization. FR and GR: supervision. FM and GD: project administration. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by a grant from the Institute for Maternal and Child Health IRCCS Burlo Garofolo (RC 08/2020).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2021.741311/full#supplementary-material
References
1. Brubaker L, Maher C, Jacquetin B, Rajamaheswari N, Von Theobald P, Norton P. Surgery for pelvic organ prolapse. Female Pelvic Med Reconstr Surg. (2010) 16:9–19. doi: 10.1097/SPV.0b013e3181ce959c
2. Muller PC, Berchtold C, Kuemmerli C, Ruzza C, Graggen KZ, Steinemann DC. Spondylodiscitis after minimally invasive recto- and colpo-sacropexy: report of a case and systemic review of the literature. Journal of Minimal Access Surgery. (2019) 16:5–12. doi: 10.4103/jmas.JMAS_235_18
3. Anand M, Tanouy SL, Gebhart JB. Vesicosacrofistulization after robotically assisted laparoscopic sacrocolpopexy. Female Pelvic Med Reconstr Surg. (2014) 20:180–3. doi: 10.1097/SPV.0000000000000033
4. Api M, Kayatas S, Boza A. Spondylodiscitis following sacral colpopexy procedure: is it an infection or graft rejection? Eur J Obstet Gynecol Reprod Biol. (2015) 194:43–8. doi: 10.1016/j.ejogrb.2015.08.003
5. Apostolis CA, Heiselman C. Sacral osteomyelitis after laparoscopic sacral colpopexy performed after a recent dental extraction: a case report. Female Pelvic Med Reconstr Surg. (2014) 20:e5–7. doi: 10.1097/SPV.0000000000000092
6. Arsene E, Giraudet G, Lucot JP, Rubod C, Cosson M. Sacral colpopexy: long-term mesh complications requiring reoperation(s). Int Urogynecol J. (2015) 26:353–8. doi: 10.1007/s00192-014-2514-7
7. Beloosesky Y, Grinblat J, Dekel A, Rabinerson D. Vertebral osteomyelitis after abdominal colposacropexy. Acta Obstet Gynecol Scand. (2002) 81:567–8. doi: 10.1034/j.1600-0412.2002.810617.x
8. Boyd B, Pratt T, Mishra K. Fungal lumbosacral osteomyelitis after robotic-assested laparoscopic sacrocolpopexy. Female Pelvic Med Reconstr Surg. (2018) 24:e.46–8. doi: 10.1097/SPV.0000000000000612
9. Brito LG, Giraudet G, Lucot JP, Cosson M. Spondylodiscitis after sacrocolpopexy. Eur J Obstet Gynecol Reprod Biol. (2015) 187:72. doi: 10.1016/j.ejogrb.2015.02.024
10. Cailleux N, Daragon A, Laine F, Deshayes P, Le Loët X, Duva C, et al. Infectious spondylodiscitis after a cure for genital prolapse 5 cases. J Gynecol Obstet Biol Reprod. (1991) 20:1074–8.
11. Collins SA, Tulikangas PK, LaSala CA, Lind LR. Complex sacral abscess 8 years after abdominal sacral colpopexy. Obstet Gynecol. (2011) 118:451–4. doi: 10.1097/AOG.0b013e3182234e7c
12. Cosson M, Narducci F, Querleu D, Crépin G. Experimental use of laparoscopic material: report of a case of spondylodiscitis after laparoscopic sacropexy with taker. Ann Chir. (2001) 126:554–6. doi: 10.1016/S0003-3944(01)00554-5
13. Cranney A, Feibel R, Toye BW, Karsh J. Osteomyelitis subsequent to abdominal-vaginal sacropexy. J Rheumatol. (1994) 21:1769–70.
14. Dalwai R, Menon KV, Kumar RJ. Pyogenic diskitis of the L5-S1 disk space following inadvertent placement of a sacrocolpopexy screw. Int J Gynaecol Obstet. (2010) 111:268–9. doi: 10.1016/j.ijgo.2010.07.012
15. Descargues G, Bouzouita A, Grise P. Infectious spondylodiscitis after a laparoscopic sacrocolpopexy: about one case. Gynecol Obstet Fertil. (2009) 37:183–5. doi: 10.1016/j.gyobfe.2008.11.013
16. Downing KT. Vertebral osteomyelitis and epidural abscess after laparoscopic uterus-preserving cervicosacropexy. J Minim Invasive Gynecol. (2008) 15:370–2. doi: 10.1016/j.jmig.2007.12.006
17. Draaisma WA, van Eijck MM, Vos J, Consten EC. Lumbar discitis after laparoscopic ventral rectopexy for rectal prolapse. Int J Colorectal Dis. (2011) 26:255–6. doi: 10.1007/s00384-010-0971-0
18. Durdag GD, Alemdaroglu S, Durdag E, Simsek SY, Turunc T, Yetkinel S, et al. Lumbosacral discitis as a rare colpication of laparoscopic sacrocolpopexy. Int Urogynecol Assoc. (2020) 31:2431–3. doi: 10.1007/s00192-020-04331-3
19. Feng TS, Thum DJ, Anger JT, Eilber KS. Sacral osteomyelitis after robotic sacrocolpopexy. Female Pelvic Med Reconstr Surg. (2016) 22:e6–7. doi: 10.1097/SPV.0000000000000219
20. Grimes CL, Tan-Kim J, Garfi SR, Nager CW. Sacral colpopexy followed by refractory candida albicans osteomyelitis and discitis requiring extensive spinal surgery. Obstet Gynecol. (2012) 120:464–8. doi: 10.1097/AOG.0b013e318256989e
21. Hart SR, Weiser EB. Abdominal sacral colpopexy mesh erosion resulting in a sinus tract formation and sacral abscess. Obstet Gynecol. (2004) 103:1037–40. doi: 10.1097/01.AOG.0000121829.55491.0d
22. Jallad C, Ridgeway B, Paraiso MFR, Gurland B, Cecile AU. Long-term outcomes after ventral rectopexy with sacrocolpo- or hysteropexy for the treatment of concurrent rectal and pelvic organ prolapse. Female Pelvic Med Reconstruct Surg. (2017) 24:336–40. doi: 10.1097/SPV.0000000000000444
23. Jenson AV, Scranton R, Antosh DD, Simpson RK. Lumbosacral osteomyelitis and discitis with phlegmon following laparoscopic sacral colpopexy. Cureus. (2016) 8:e671. doi: 10.7759/cureus.671
24. Kapoor B, Toms A, Hooper P, Fraser AM, Cox CW. Infective lumbar discitis following laparascopic sacrocolpopexy. J R Coll Surg Edinb. (2002) 47:709–10.
25. Kumara DMA, Jayasekara M, Caldera M. Lumbosacral discitis following laparoscopic sacrohysteropex. Sri Lanka J Obstetr Gynaecol. (2020) 42:115–9. doi: 10.4038/sljog.v42i3.7940
26. Miksic N.G, Dujic MK, Marko JR, Vorsik M, But I. Bacteroides fragilis sacral spondylodiscitis and epidural abscess after sacrocolpopexy: a case report and literature review. J Int Med Res. (2019) 47:4568–74. doi: 10.1177/0300060519866270
27. Muffly TM, Diwadkar GB, Paraiso MF. Lumbosacral osteomyelitis after robot-assisted total laparoscopic hysterectomy and sacral colpopexy. Int Urogynecol J. (2010) 21:1569–71. doi: 10.1007/s00192-010-1187-0
28. Nosseir SB, Kim YH, Lind LR, Winkler HA. Sacral osteomyelitis after robotically assisted laparoscopic sacral colpopexy. Obstet Gynecol. (2010) 116 (Suppl. 2):513–5. doi: 10.1097/AOG.0b013e3181e10ea6
29. Núñez-Pereira S, Huhmann NV, Rheinwalt KP, Bullmann V. Lumbosacral spondylodiscitis due to rectal fistula following mesh penetration 7 years after colpopexy. Int J Surg Case Rep. (2016) 24:219–22. doi: 10.1016/j.ijscr.2016.04.047
30. Pasquer A, Djeudji F, Pechoux A, Barth X. Spondylodiscitis after rectopexy: diagnostic of a rare complication. Tech Coloproctol. (2017) 21:63–4. doi: 10.1007/s10151-016-1566-8
31. Probst P, Knoll SN, Breitenstein S, Karrer U. Vertebral discitis after laparoscopic resection rectopexy: a rare differential diagnosis. J Surg Case Rep. (2014) 2014:rju075. doi: 10.1093/jscr/rju075
32. Propst K, Tunitsky-Bitton E, Schimpf MO, Ridgeway B. Pyogenic spondylodiscitis associated with sacral colpopexy and rectopexy: report of two cases and evaluation of the literature. Int Urogynecol J. (2014) 25:21–31. doi: 10.1007/s00192-013-2138-3
33. Qu DC, Chen HB, Yang MM, Zhou HG. Management of lumbar spondylodiscitis developing after laparoscopic sacrohysteropexy with a mesh. A case report and review of the literature. Medicine. (2019) 98:e18252. doi: 10.1097/MD.0000000000018252
34. Rajamaheswari N, Agarwal S, Seethalakshmi K. Lumbosacral spondylodiscitis: an unusual complication of abdominal sacrocolpopexy. Int Urogynecol J. (2012) 23:375–7. doi: 10.1007/s00192-011-1547-4
35. Rivoire C, Botchorishvili R, Canis M, Jardon K, Rabischong B, Wattiez A, et al. Complete laparoscopic treatment of genital prolapsed with meshes including vaginal promontofixation and anterior repair: a serious of 138 patients. J Minimal Invasive Gynecol. (2007) 14:712–8. doi: 10.1016/j.jmig.2007.06.017
36. Roth TM, Reight I. Laparoscopic mesh explantation and drainage of sacral abscess remote from transvaginal excision of exposed sacral colpopexy mesh. Int Urogynecol J. (2012) 23:953–5. doi: 10.1007/s00192-011-1630-x
37. Salman MM, Hancock AL, Hussein AA, Hartwell R. Lumbosacral spondylodiscitis: an unreported complication of sacrocolpopexy using mesh. BJOG. (2003) 110:537–8. doi: 10.1046/j.1471-0528.2003.02012.x
38. Sergent F, Resch B, Loisel C, Bisson V, Schaal JP, Marpeau L. Mid – term outcome of laparoscopic sacrocolpopexy with anterior and posterior polyester mesh for treatment of genitor – urinary prolapsed. Eur J Obstetr Gynecol Reprod Biol. (2011) 156:217–22. doi: 10.1016/j.ejogrb.2011.01.022
39. Taylor GB, Moore RD, Miklos JR. Osteomyelitis secondary to sacral colpopexy mesh erosion requiring laminectomy. Obstet Gynecol. (2006) 107:475–7. doi: 10.1097/01.AOG.0000187949.87223.06
40. Tymchak ZA, Epp A, Fourney DR. Lumbosacral discitis-osteomyelitis after mesh abdominosacrocolpopexy. Spine J. (2015) 15:194–5. doi: 10.1016/j.spinee.2014.08.004
41. Ugurlucan FG, Yasa C, Demir O, Basaran S, Bakir B, Yalcin O. Long-term follow up of a patient with spondylodiscitis after laparoscopic sacrocolpopexy: an unusual complication with a review of the literature. Urol int. (2018) 103:364–8. doi: 10.1159/000494370
42. Voelker A, Hoeckel M, Heyde CE. Lumbosacral spondylodiscitis after sacral colpopexy of a sigmoid neovagina in a patient with vaginal melanoma. Surg Infect. (2012) 13:134–5. doi: 10.1089/sur.2011.083
43. Vujovic Z, Cuarana E, Campbell KL, Valentine N, Koch S, Ziyaie D, et al. Lumbosacral discitis following laparoscopic ventral mesh rectopexy: a rare but potentially serious complication. Tech Coloproctol. (2015) 19:263–5. doi: 10.1007/s10151-015-1279-4
44. Weidner AC, Cundiff GW, Harris RL, Addison WA. Sacral osteomyelitis: an unusual complication of abdominal sacral colpopexy. Obstet Gynecol. (1997) 90:689–91. doi: 10.1016/S0029-7844(97)00306-2
45. Costantini E, Brubaker L, Cervigni M, Matthews CA, O' Reilly BA, Rizk D, et al. Sacrocolpopexy for pelvic organ prolapsed: evidence-based review and recommendations. Obstetr Ginecol. (2016) 205:60–5. doi: 10.1016/j.ejogrb.2016.07.503
46. Consten EC, van Iersel JJ, Verheijen PM, Broeders IA, Wolthuis AM, D'Hoore A, et al. Long-term outcome after laparoscopic ventral mesh rectopexy: an observational study of 919 consecutive patients. Ann Surg. (2015) 262:742–7. doi: 10.1097/SLA.0000000000001401
47. Unger CA, Paraiso MF, Jelovsek JE, Barber MD, Ridgeway B. Perioperative adverse events after minimally invasive abdominal sacrocolpopexy. Am J Obstetr Gynecol. (2014) 211:547.e1–8. doi: 10.1016/j.ajog.2014.07.054
48. Grevez T, Vanalderwerelt V, Bruyère F. Infectious complications of promontofixation, a systematic review of literature. Med Mal Infect. (2020) 51:107–113. doi: 10.1016/j.medmal.2020.10.004
49. Stabile G, Romano F, De Santo D, Sorrentino F, Nappi L, Cracco F, et al. Bowel occlusion following the use of barbed sutures in abdominal surgery: case report and literature review. Front Surg. (2021) 8:626505. doi: 10.3389/fsurg.2021.626505
50. Romano F, Sartore A, Mordeglia D, Di Lorenzo G, Stabile G, Ricci G. Laparoscopic monolateral suspension for vaginal vault prolapse: a report of an exit surgical strategy during sacralcolpopexy. BMC Surg. (2020) 20:199. doi: 10.1186/s12893-020-00861-1
51. White AB, Carrick KS, Corton MM, McIntie DD, Word RA, Rahn DD, et al. Optimal location and orientation of suture placement in abdominal sacrocolpopexy. Obstetr Gynecol. (2009) 113:1098–103. doi: 10.1097/AOG.0b013e31819ec4ee
52. Mavrogenis AF, Megaloikomonos PD, Igoumenou VG, Panagopoulos GN, Giannitsioti E, Papadopoulos A, et al. Spondilodiscitis revisited. EFORT Open Rev. (2017) 2:447–61. doi: 10.1302/2058-5241.2.160062
53. Gray TG, Radley SC, Mc Vey S, Green J, Saxena A, Patel D. Pelvic organ prolapse. Urol Principles Pract. (2020) 1:487–97. doi: 10.1007/978-3-030-28599-9_29
54. Aagaard T, Roed C, Dragsted C, Skinhoj P. Microbiological and therapeutic challenges in infectious spondylodiscitis: a cohort study of 100 cases, 2006-2011. Scand J Infect Dis. (2012) 45:417–24. doi: 10.3109/00365548.2012.753160
55. Cottle L, Riordan T. Infectious spondylodiscitis. J Infect. (2008) 56:401–12. doi: 10.1016/j.jinf.2008.02.005
Keywords: spondylodiscitis, sacrocolpopexy, rectopexy, prolapse, mesh
Citation: Stabile G, Romano F, Topouzova GA, Mangino FP, Di Lorenzo G, Laganà AS, De Manzini N and Ricci G (2021) Spondylodiscitis After Surgery for Pelvic Organ Prolapse: Description of a Rare Complication and Systematic Review of the Literature. Front. Surg. 8:741311. doi: 10.3389/fsurg.2021.741311
Received: 14 July 2021; Accepted: 27 September 2021;
Published: 29 October 2021.
Edited by:
Stefano Cianci, University of Messina, ItalyReviewed by:
Silvia Zermano, University of Udine, ItalyAndrea Lombisani, Catholic University of the Sacred Heart, Italy
Copyright © 2021 Stabile, Romano, Topouzova, Mangino, Di Lorenzo, Laganà, De Manzini and Ricci. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guglielmo Stabile, guglielmost@gmail.com
 Guglielmo Stabile
Guglielmo Stabile Federico Romano
Federico Romano Ghergana A. Topouzova2
Ghergana A. Topouzova2  Antonio Simone Laganà
Antonio Simone Laganà Giuseppe Ricci
Giuseppe Ricci