You may think of your period as just one week every month when you’re dealing with vaginal bleeding, abdominal cramping and other potentially annoying symptoms — but there’s more to it than that.
Your menstrual cycle is the process your body undergoes to prepare for a potential pregnancy, and it’s made up of several phases during which different things occur in order to facilitate conception. If everything is working properly, the menstrual cycle phases repeat month after month, year after year, from adolescence to menopause.
When you actually dig into the science of what makes a period occur and the phases of a menstrual cycle, it’s quite fascinating. “To get a predictable month-to-month bleeding episode that seems the same each and every time requires coordination,” says Kristen A. Matteson, M.D., M.P.H., director of the Division of Research in the Department of Obstetrics & Gynecology at UMass Memorial Medical Center. “It’s like a universal, coordinated, full-uterine event. The reason I say that is you need a lot of complicated systems to work all together to produce that. When anything is a little bit off — so stress or medications or any other issues — you can have irregularities in your menstrual period.”
Consider this: For ovulation and menstruation to occur, the hypothalamus and pituitary gland in the brain must send signals to an ovary, which must return signals to the brain and also send messages to the lining of the uterus. “The thing I tell patients is that the lining of the uterus only does what the ovaries tell it to do,” says Dr. Matteson. “So if the signals from the ovary aren’t coming in their pre-programmed, typical fashion, that leads you to have abnormalities in your menstrual cycles.”
The good news is the more we learn about the menstrual cycle phases, pay attention to the patterns in our bodies and talk to one another about our periods, the better off we all will be. When you know what’s supposed to happen, you can figure out when something is amiss and address it with a physician.
Menstrual cycle phases
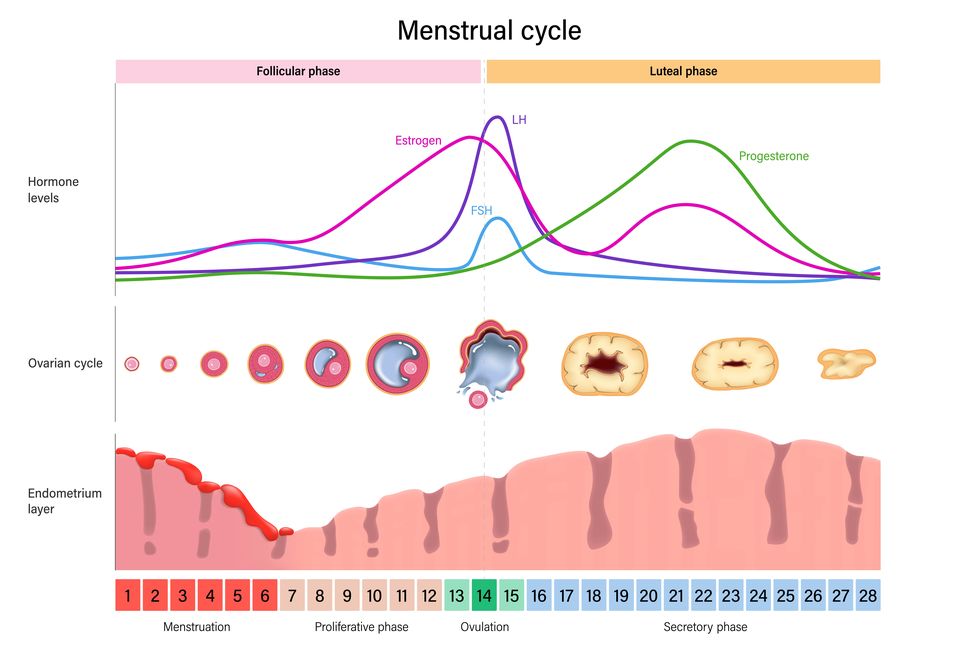
The menstrual cycle is divided into two phases: the follicular phase and the luteal phase. Within each phase, different things happen concurrently in the uterus and ovaries.
Everything that happens in the uterus (such as the uterine lining shedding or getting ready for a fertilized egg to be implanted) is part of the uterine cycle while everything that happens in the ovaries (including follicle preparation and hormone secretion) is considered to be part of the ovarian cycle.
FAQs
How long does a typical menstrual cycle last?
“The cycle is the number of days from the first day of one bleeding episode to the first day of the next,” says Dr. Matteson. The average cycle lasts 28 days, but that number varies from one person to the next. Some people regularly have a cycle that spans only 21 days while others have a 35-day cycle. This variation occurs because the follicular phase can be longer or shorter, but the luteal phase is usually around 14 days for everyone who menstruates. Irregular cycles are those that vary by more than seven to nine days from cycle to cycle (like a 25-day cycle followed by a 40-day cycle).
How do you track your period?
Grab a calendar or download a period-tracking app and denote the first day of your last menstrual cycle as well as any symptoms you experience and how heavy your bleeding is. “I think the data you get from an app is only as good as what you put in it,” says Dr. Matteson. “It can help you provide detailed information to your health care provider who can then walk through it and say, ‘Oh, I think this is what’s happening with your bleeding. These are the investigations that we should do to see what’s going on.’”
What causes irregular menstrual cycles?
First, age is a factor. After menarche (a person’s first period) and during perimenopause (the transitional time before menopause officially occurs), cycles can be anovulatory, meaning ovulation doesn’t occur. Essentially, when an egg isn’t released, there are no hormones released that tell the uterus what to do. “When this happens there is no monthly period that follows,” says Dr. King. “When a girl is young, the brain — specifically the hypothalamus and pituitary gland — is still developing so it can take some time for the cycle patterns to become regular and monthly. On the other end of the spectrum, during perimenopause, the cycle irregularity and anovulation is due to limited follicles in the ovaries that are available to ovulate.” Sometimes, notes Dr. Matteson, the uterine lining keeps building up and becomes unstable. “So then one area of the lining of the uterus will start to shed and as that area starts healing on its own, another area may start to shed so you get unpredictable bleeding,” she explains.
Because such a complex chain of events must occur for a regular menstrual cycle to occur, there are lots of other things beyond menarche and perimenopause that can also cause it to go haywire, according to Dr. Matteson. Those include structural issues (such as fibroids, polyps or tumors) and non-structural problems (for example, blood clotting disorders, stress, thyroid diseases, polycystic ovarian syndrome, medications, excess exercise or certain contraceptives).
When to see your doctor
If you have concerns about late or missed periods, bleeding duration or heaviness, menstrual cramp intensity or changes in any of the above, it’s smart to schedule a visit with a gynecologist ASAP. For instance, debilitating cramps that interfere with your daily routine or bleeding that occurs after you’ve entered menopause (which is defined by 12 months without any bleeding) both warrant a trip to the doctor.
That said, you should have an annual checkup even if you’re not worried about anything. “I think all individuals who menstruate should see a gynecologist each year to just check in because I think gynecologists ask the questions about menstrual cycles and periods and other reproductive health issues that can help screen for when there might be a problem,” says Dr. Matteson.
Kaitlyn Phoenix is a deputy editor in the Hearst Health Newsroom, where she reports, writes and edits research-backed health content for Good Housekeeping, Prevention and Woman's Day. She has more than 10 years of experience talking to top medical professionals and poring over studies to figure out the science of how our bodies work. Beyond that, Kaitlyn turns what she learns into engaging and easy-to-read stories about medical conditions, nutrition, exercise, sleep and mental health. She also holds a B.S. in magazine journalism from Syracuse University.