Hypospadias is a congenital defect defined as a malformation of the male urethrathat is abnormally located at the lower extremity of the glans penis, on the underside of the penis or at the junction of the penis and scrotum. Therefore, hypospadias can be classified into anterior, medial and posterior.
The severity of hypospadias will depend on the location of the urethral opening. In either case, the male will have trouble having sex and ejaculating, so pregnancy in a natural way will be complicated.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 2.1.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 7.
- 8.
- 9.
Definition
Hypospadias is an anomaly that appears from birth (congenital) characterized by having the opening of the urethra in a place other than the tip of the penis. Hypospadias is also usually associated with a malformation of the foreskin and a curvature of the penis toward the belly. This type of penis is called congenital curved penis.
Because of this curvature of the penis, hypospadias is considered a cause of sexual dysfunction, as it can mechanically make sexual intercourse impossible. In addition, as a consequence of the abnormal position of the urethral orifice, ejaculation in the vagina is also impeded.
The frequency of occurrence of hypospadias is between 1 and 8 newborns out of 1000.
Hypospadias has both aesthetic and functional consequences. Once the child is older, this malformation can even have psychological consequences.
On the other hand, hypospadias can sometimes be accompanied by other types of malformations that can compromise male fertility such as cryptorchidism, presence of hidden testes and even the diagnosis of sexual ambiguity or pseudohermaphroditism should be ruled out.
Types
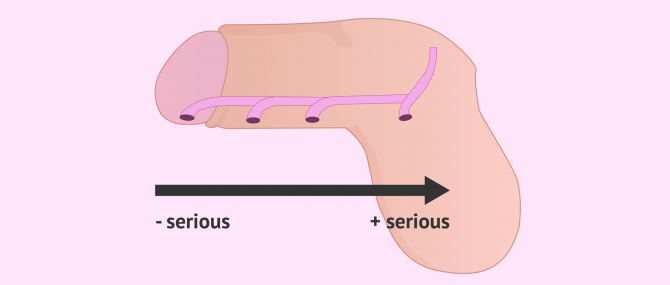
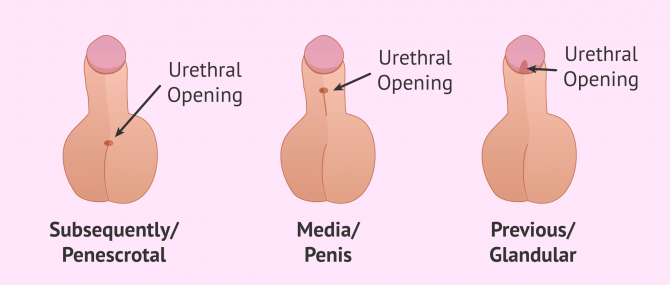
There are different types of hypospadias depending on the location of the urethral opening. The further the urethral opening is located from the glans penis, the greater the severity of hypospadias. In this way, they are distinguished:
- Posterior hypospadias
- is the most severe form. This type of hypospadias appears in 20% of cases and the urethral orifice is very distal to the glans, in the area between the scrotum and the penis or at the base of the penis. In addition, posterior hypospadias is accompanied by a very curved penis. This type of hypospadias is also known as penescrotal hypospadias.
- Hypospadias media (penile)
- constitutes 10% of cases and is of medium severity. Here the orifice is located in the middle part of the penis, usually on the underside. This causes a certain curvature of the penis towards the belly.
- Anterior hypospadias
- also called glandular hypospadias. This is the most common type, occurring in 70% of cases. In addition, this form of hypospadias is the mildest, as the urinary meatus is close to the glans penis. In addition, the penis looks aesthetically normal and has virtually no curvature.
The problems associated with hypospadias will be more severe the further back the urethral opening is located.
Causes of the hypospadias
The exact reason for hypospadias is not known. However, most studies seem to indicate that this abnormality in the position of the urethral opening is caused by genetic factors in combination with environmental factors and certain medications. In addition, this malformation is under the dependence of androgens. Thus, among the causes that could lead to hypospadias, a genetic mutation that causes a deficiency in androgen receptors may be involved.
This mutation can be inherited in some cases when there is already a family member with hypospadias. It is estimated that it is 20% more likely to appear in other members of the same family.
It is also thought that disruption of embryonic androgen receptors by environmental factors may be one of the culprits. As well as some type of hormonal treatment during the first month or trimester of pregnancy or some type of alteration in the synthesis of testosterone.
Risk Factors
Some factors that appear to increase a child's risk of developing hypospadias include the following:
- Mothers over 35 years of age and with high body mass index (BMI).
- Women pregnant through assisted reproduction techniques.
- Administration of certain hormones before and during pregnancy.
However, the presence of these factors does not mean that the baby will have hypospadias. These are only factors that have been studied and appear to increase risk.
Symptoms
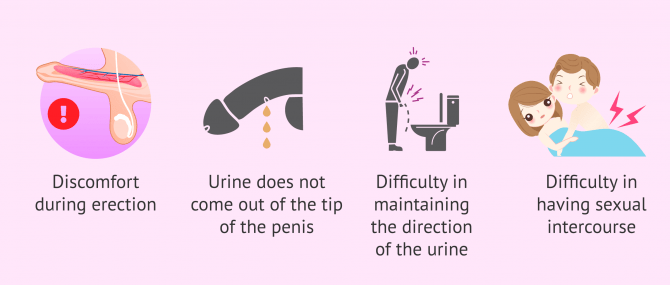
The symptoms of hypospadias depend on the severity of the hypospadias. In any case, the most common clinical manifestations associated with hypospadias are:
- Discomfort during erection.
- Urine does not come out of the tip of the penis.
- Difficulty maintaining urine direction
- Difficulty during sexual intercourse.
- Abnormal appearance of the foreskin.
As a result of ejaculation problems, the possibility of having children naturally can be complicated. In addition, it will also be difficult for sperm to reach the uterus during intercourse.
Diagnosis and Treatment
The way to diagnose hypospadias at birth is by physical examination of the baby. If the pediatrician is unsure of the diagnosis, further evaluation may be ordered.
Usually, the treatment of choice for hypospadias is the surgical option. Due to the psychological impact that this anomaly can have on the child, most specialists recommend the operation at an early age, before the age of 3.
Generally, if the hypospadias problem is corrected when the child is young, it does not need to influence adulthood.
In addition, a micropenis may appear as a result of the curvature of the penis towards the belly. Therefore, during surgery, if necessary, the curvature of the penis can be corrected along with the reconstruction of the urethra and foreskin. Sometimes penis growth can also be stimulated with hormone treatment.
As we have seen, there are different surgical techniques to solve hypospadias. It will be the specialist who will assess the case and decide which is the appropriate technique to address the different aspects to be treated, orifice, curvature of the penis and foreskin.
Hypospadias and fertility
The concentration of male hormones involved in sperm formation and associated with fertility in the male may decrease depending on the location of the urethral orifice.
In addition, hypospadias causes problems with ejaculation by preventing sperm from entering through the vagina. For these reasons, the probability of having a child with hypospadias is low.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
However, if this congenital malformation in the location of the urethral opening is treated correctly at an early age, it does not usually lead to problems in the reproductive health of the adult male.
FAQs from users
Does hypospadias cause male infertility?
Hypospadias causes problems in ejaculation, preventing the correct ejaculation of sperm in some cases, even after surgical correction.
If there is also a hormonal or karyotype alteration, there may be an alteration in the correct production of spermatozoa.
All of this means that the chances of having offspring are reduced.
How do I know if I have hypospadias?
Hypospadias is a birth defect that affects male babies. With this conditions, the urinary meatus is located in a place other than the external urethral orifice, such as the scrotum. There exist various types of hypospadias, from mild to most severe.
Is hypospadias hereditary?
The exact cause of hypospadias is not known exactly, but there is some link to genetics. For this reason, some studies show that hypospadias is hereditary.
Specifically, the genetic cause of hypospadias would be a mutation in a gene, leading to a lower concentration of androgen receptors. However, it is not possible to state that this congenital malformation in the location of the urethral opening is genetic.
Suggested for you
Hypospadias can lead to cryptorchidism in the male, which can cause problems in having offspring. If you would like to learn more about this testicular disorder, we recommend you visit the following article: Cryptorchidism - a testicular disorder that causes infertility.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
H J R van der Horst , L L de Wall. Hypospadias, all there is to know. Eur J Pediatr. 2017 Apr;176(4):435-441. doi: 10.1007/s00431-017-2864-5. Epub 2017 Feb 11.
Kate H Kraft, Aseem R Shukla, Douglas A Canning. Hypospadias. Urol Clin North Am. 2010 May;37(2):167-81. doi: 10.1016/j.ucl.2010.03.003.
Laura A Stokowski. Hypospadias in the neonate. Adv Neonatal Care. 2004 Aug;4(4):206-15. doi: 10.1016/j.adnc.2004.05.003.
Laurence Baskin. What Is Hypospadias? Clin Pediatr (Phila). 2017 May;56(5):409-418. doi: 10.1177/0009922816684613. Epub 2017 Jan 12.
I Rübben, R Stein. Hypospadias : Insights and challenges. Urologe A. 2017 Oct;56(10):1256-1265. doi: 10.1007/s00120-017-0498-x.
Marjan Joodi, Forouzan Amerizadeh, Seyed Mahdi Hassanian, Marjan Erfani, Majid Ghayour-Mobarhan, Gordon A Ferns, Majid Khazaei, Amir Avan. The genetic factors contributing to hypospadias and their clinical utility in its diagnosis. J Cell Physiol. 2019 May;234(5):5519-5523. doi: 10.1002/jcp.27350. Epub 2018 Sep 21.
S B Levitt, E F Reda. Hypospadias. Pediatr Ann. 1988 Jan;17(1):48-9, 53-4, 57. doi: 10.3928/0090-4481-19880101-09.
T Koyanagi, K Nonomura. Hypospadias. Nihon Hinyokika Gakkai Zasshi. 1990 Nov;81(11):1609-17. doi: 10.5980/jpnjurol1989.81.1609.
FAQs from users: 'Does hypospadias cause male infertility?', 'How do I know if I have hypospadias?' and 'Is hypospadias hereditary?'.
Authors and contributors