Authors: Ahmed Elsherif 1 ; Michelle Wyatt 2
Peer Reviewers: Stanley Oiseth 3 ; Joseph Alpert 4
Affiliations: 1 Suez Canal University; 2 Medical Editor at Lecturio; 3 Chief Medical Editor at Lecturio; 4 Tucson University, Arizona
This article is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition.
Vital Signs
Vital signs are necessary for every patient you clinically examine, including heart rate Heart rate The number of times the heart ventricles contract per unit of time, usually per minute. Cardiac Physiology (HR), respiratory rate Respiratory rate The number of times an organism breathes with the lungs (respiration) per unit time, usually per minute. Pulmonary Examination ( RR RR Relative risk (RR) is the risk of a disease or condition occurring in a group or population with a particular exposure relative to a control (unexposed) group. Measures of Risk), and blood pressure (BP). In most situations, these are measured with basic equipment (a watch, a sphygmomanometer, and a stethoscope) and are part of a physician’s basic skills.
It is essential to learn how to perform these examinations correctly and the basic rules associated with each measurement. Even if the hospital or clinic staff provide the patient’s BP readings, most physicians Physicians Individuals licensed to practice medicine. Clinician–Patient Relationship in clinical practice will repeat some of the vital sign measurements. Automated and validated oscillometric BP monitors are preferred to stethoscope-based manual methods.
The patient should be resting comfortably, lying supine (for hospitalized patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship in bed), or sitting in any other situation (at home or in the clinic). [2] Before checking their BP, the patient should have rested for 3 to 5 minutes (not run in from the parking lot or just had a blood draw). Wash your hands and explain to the patient what you are doing. Do not perform the exam through clothing—use a bare arm Arm The arm, or "upper arm" in common usage, is the region of the upper limb that extends from the shoulder to the elbow joint and connects inferiorly to the forearm through the cubital fossa. It is divided into 2 fascial compartments (anterior and posterior). Arm: Anatomy. Do not use an arm Arm The arm, or "upper arm" in common usage, is the region of the upper limb that extends from the shoulder to the elbow joint and connects inferiorly to the forearm through the cubital fossa. It is divided into 2 fascial compartments (anterior and posterior). Arm: Anatomy with a medical problem or on the same side as a mastectomy Mastectomy Surgical procedure to remove one or both breasts. Fat Necrosis of the Breast.
Observation
With the anterior chest exposed, observe your patient’s thorax and the rest of their body. Look at the eyes, upper and lower extremities, and neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology as well.
Thorax
- Scars from prior cardiac surgery Cardiac surgery Cardiac surgery is the surgical management of cardiac abnormalities and of the great vessels of the thorax. In general terms, surgical intervention of the heart is performed to directly restore adequate pump function, correct inherent structural issues, and reestablish proper blood supply via the coronary circulation. Cardiac Surgery. A vertical scar Scar Dermatologic Examination on the sternum Sternum A long, narrow, and flat bone commonly known as breastbone occurring in the midsection of the anterior thoracic segment or chest region, which stabilizes the rib cage and serves as the point of origin for several muscles that move the arms, head, and neck. Chest Wall: Anatomy is an indication of prior open-heart surgery.
- Chest deformities include pectus excavatum Pectus Excavatum Cardiovascular Examination (a sunken sternum Sternum A long, narrow, and flat bone commonly known as breastbone occurring in the midsection of the anterior thoracic segment or chest region, which stabilizes the rib cage and serves as the point of origin for several muscles that move the arms, head, and neck. Chest Wall: Anatomy and ribs Ribs A set of twelve curved bones which connect to the vertebral column posteriorly, and terminate anteriorly as costal cartilage. Together, they form a protective cage around the internal thoracic organs. Chest Wall: Anatomy may be a sign of a connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology disease such as Marfan syndrome Marfan syndrome Marfan syndrome is a genetic condition with autosomal dominant inheritance. Marfan syndrome affects the elasticity of connective tissues throughout the body, most notably in the cardiovascular, ocular, and musculoskeletal systems. Marfan Syndrome) and pectus carinatum Pectus carinatum A developmental anomaly characterized by abnormal anterior protrusion of the sternum and adjacent costal cartilage. Cardiovascular Examination (“ pigeon chest Pigeon chest A developmental anomaly characterized by abnormal anterior protrusion of the sternum and adjacent costal cartilage. Cardiovascular Examination,” a protrusion of the sternum Sternum A long, narrow, and flat bone commonly known as breastbone occurring in the midsection of the anterior thoracic segment or chest region, which stabilizes the rib cage and serves as the point of origin for several muscles that move the arms, head, and neck. Chest Wall: Anatomy and ribs Ribs A set of twelve curved bones which connect to the vertebral column posteriorly, and terminate anteriorly as costal cartilage. Together, they form a protective cage around the internal thoracic organs. Chest Wall: Anatomy).


Eyes
- Yellow plaques around the eyes and eyelids Eyelids Each of the upper and lower folds of skin which cover the eye when closed. Blepharitis, called xanthelasmas Xanthelasmas Lipid Disorders, may signify hypercholesterolemia Hypercholesterolemia A condition with abnormally high levels of cholesterol in the blood. It is defined as a cholesterol value exceeding the 95th percentile for the population. Lipid Disorders. Although sometimes seen in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship without hyperlipidemia, xanthelasmas Xanthelasmas Lipid Disorders can be a sign of a risk factor for cardiovascular disease.
- Roth spots Roth spots Endocarditis are observed on the retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy with an ophthalmoscope Ophthalmoscope Ophthalmic Exam and appear as a red ring surrounding a white center. These are only seen in about 2% of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with infective endocarditis Infective endocarditis Infective endocarditis (IE) is caused by infection or inflammation of the inner lining of the heart (endocardium), most commonly affecting the heart valves. Endocarditis but are a classic sign that medical students are often tested on. [3]

Xanthelasma palpebrarum, a type of xanthoma, affecting the upper and lower eyelids
Image: “ File:Xanthelasma” by Klaus D. Peter. License: CC BY 3.0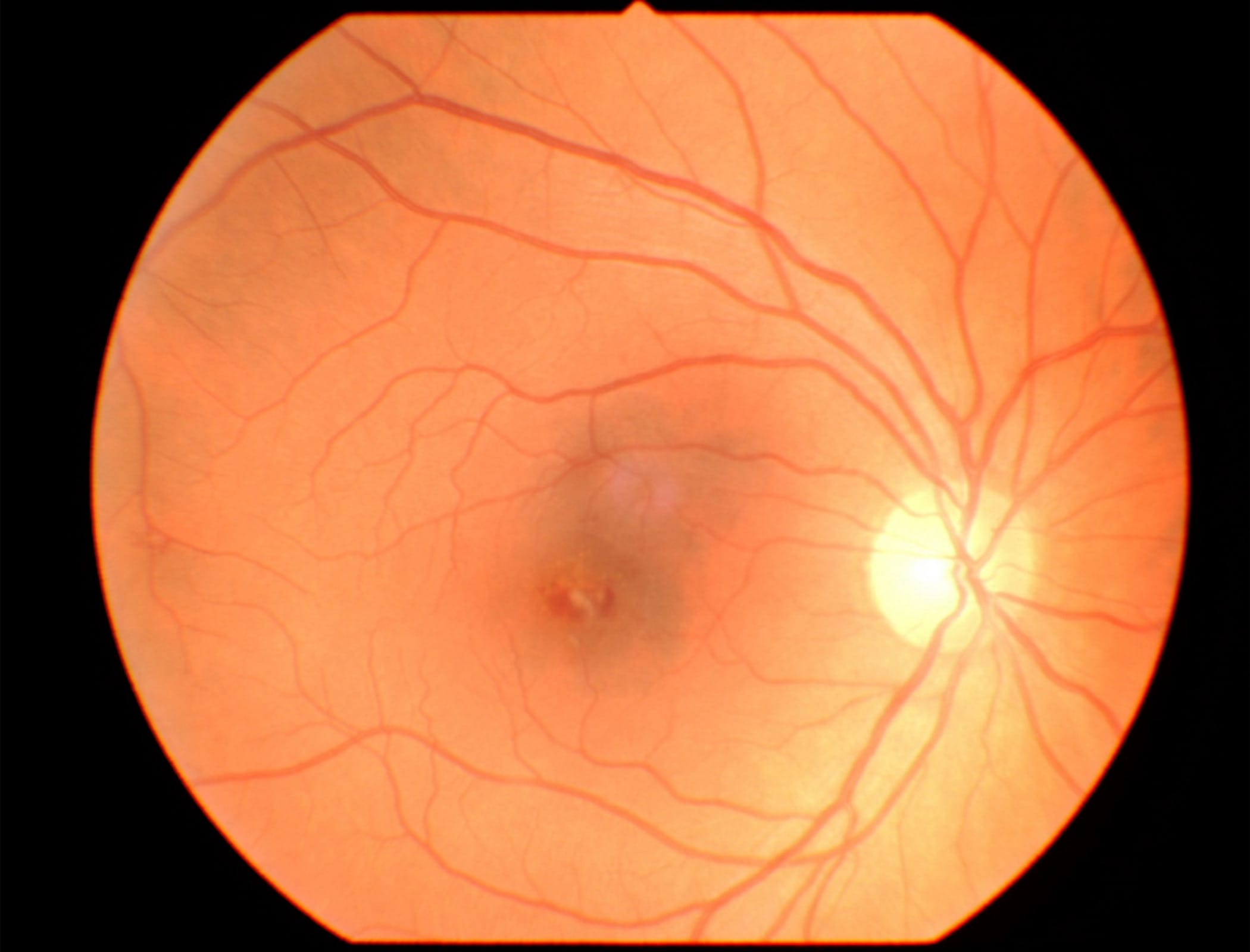
Upper and Lower Extremities
Clubbing Clubbing Cardiovascular Examination of the fingers or toes manifests with the distal part of the digit appearing flatter and broader. This is a sign of lung disease or chronic hypoxemia Hypoxemia Neonatal Respiratory Distress Syndrome but may occasionally be seen in individuals without these conditions.

Cyanosis Cyanosis A bluish or purplish discoloration of the skin and mucous membranes due to an increase in the amount of deoxygenated hemoglobin in the blood or a structural defect in the hemoglobin molecule. Pulmonary Examination, a bluish discoloration of the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and mucous membranes, implies poor perfusion. The presence of at least 3 g/dL of reduced or deoxygenated hemoglobin ( Hb Hb The oxygen-carrying proteins of erythrocytes. They are found in all vertebrates and some invertebrates. The number of globin subunits in the hemoglobin quaternary structure differs between species. Structures range from monomeric to a variety of multimeric arrangements. Gas Exchange) corresponds to an O2 saturation of < 85% if the patient is not anemic. The lower the Hb Hb The oxygen-carrying proteins of erythrocytes. They are found in all vertebrates and some invertebrates. The number of globin subunits in the hemoglobin quaternary structure differs between species. Structures range from monomeric to a variety of multimeric arrangements. Gas Exchange level, the lower the O2 saturation needed before cyanosis Cyanosis A bluish or purplish discoloration of the skin and mucous membranes due to an increase in the amount of deoxygenated hemoglobin in the blood or a structural defect in the hemoglobin molecule. Pulmonary Examination can be appreciated. Cyanosis Cyanosis A bluish or purplish discoloration of the skin and mucous membranes due to an increase in the amount of deoxygenated hemoglobin in the blood or a structural defect in the hemoglobin molecule. Pulmonary Examination does not appear at a Hb Hb The oxygen-carrying proteins of erythrocytes. They are found in all vertebrates and some invertebrates. The number of globin subunits in the hemoglobin quaternary structure differs between species. Structures range from monomeric to a variety of multimeric arrangements. Gas Exchange level of 10 g/dL until the O2 saturation is ~ 70%. If you see cyanosis Cyanosis A bluish or purplish discoloration of the skin and mucous membranes due to an increase in the amount of deoxygenated hemoglobin in the blood or a structural defect in the hemoglobin molecule. Pulmonary Examination in a severely anemic patient, this means that the concentration of Hb Hb The oxygen-carrying proteins of erythrocytes. They are found in all vertebrates and some invertebrates. The number of globin subunits in the hemoglobin quaternary structure differs between species. Structures range from monomeric to a variety of multimeric arrangements. Gas Exchange is very low, and the patient is critically ill. Cyanosis Cyanosis A bluish or purplish discoloration of the skin and mucous membranes due to an increase in the amount of deoxygenated hemoglobin in the blood or a structural defect in the hemoglobin molecule. Pulmonary Examination can be detected in the extremities (peripheral cyanosis Cyanosis A bluish or purplish discoloration of the skin and mucous membranes due to an increase in the amount of deoxygenated hemoglobin in the blood or a structural defect in the hemoglobin molecule. Pulmonary Examination) or the lips Lips The lips are the soft and movable most external parts of the oral cavity. The blood supply of the lips originates from the external carotid artery, and the innervation is through cranial nerves. Lips and Tongue: Anatomy ( central cyanosis Central Cyanosis Tricuspid Valve Atresia (TVA), which is more serious). [4]
Infective endocarditis Infective endocarditis Infective endocarditis (IE) is caused by infection or inflammation of the inner lining of the heart (endocardium), most commonly affecting the heart valves. Endocarditis lesions on the hands and feet
Osler nodes Osler nodes Endocarditis are raised, painful, red lesions on the hands and feet. They are caused by immune complex deposition. Janeway lesions Janeway lesions Endocarditis are small, red, and painless. They are caused by microemboli.[5] Splinter hemorrhages Splinter hemorrhages Endocarditis manifest as short dark lines beneath the nails and are also caused by microemboli.

Jugular Venous Distention
The cardiovascular exam includes observing the right internal jugular vein Internal jugular vein Parapharyngeal Abscess (IJV). This test helps evaluate right heart function and central venous pressure Central venous pressure The blood pressure in the central large veins of the body. It is distinguished from peripheral venous pressure which occurs in an extremity. Central Venous Catheter.
Examination:
- Elevate the patient’s head between 15° and 30° while lying supine.
- Identify the right IJV. This may take some practice. It crosses deep to the sternocleidomastoid Sternocleidomastoid Muscles of the Neck: Anatomy muscle and anterior to the right ear. Ask the patient to turn their head to the left or perform a Valsalva maneuver Valsalva maneuver Forced expiratory effort against a closed glottis. Rectal Prolapse. The hepatojugular reflux maneuver can also help find the internal jugular vein Internal jugular vein Parapharyngeal Abscess. Apply firm pressure to the right upper quadrant Right upper quadrant Anterior Abdominal Wall: Anatomy of the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy for a few seconds, and the IJV will fill with blood. A penlight Penlight Ophthalmic Exam can be very useful while trying to find the IJV.
- Measure the top of the IJV fluid level in cm above the Angle of Louis ( sternal angle Sternal angle Chest Wall: Anatomy). A normal measurement is a vertical height 3 cm above the sternal angle Sternal angle Chest Wall: Anatomy.

Palpation
The palpation Palpation Application of fingers with light pressure to the surface of the body to determine consistency of parts beneath in physical diagnosis; includes palpation for determining the outlines of organs. Dermatologic Examination portion of the cardiovascular exam includes evaluating the peripheral pulses in the neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess (for carotid pulses) and extremities; it also palpation Palpation Application of fingers with light pressure to the surface of the body to determine consistency of parts beneath in physical diagnosis; includes palpation for determining the outlines of organs. Dermatologic Examination of the point of maximum impulse (PMI) on the anterior chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy. A relatively strong vibration Vibration A continuing periodic change in displacement with respect to a fixed reference. Neurological Examination is created when the ventricles contract, transmitted down the apex of the heart and into the chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy. The PMI is located at the 5th intercostal space in the left midclavicular line in a healthy individual.
Evaluation of the Extremities
Temperature
Evaluate the extremities for temperature. Gently touch the hands and feet and note their temperatures. A well-perfused extremity will be slightly warm or at body temperature Body Temperature The measure of the level of heat of a human or animal. Heatstroke. A cold extremity indicates poor perfusion or blood being shunted away from the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions. A warm extremity suggests a reduction of vascular resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing and may be a sign of septic shock Septic shock Sepsis associated with hypotension or hypoperfusion despite adequate fluid resuscitation. Perfusion abnormalities may include, but are not limited to lactic acidosis; oliguria; or acute alteration in mental status. Sepsis and Septic Shock in a patient with severe hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension.
Peripheral Pulses
There are a variety of pulse points with which you should be familiar. Some are regularly used (radial pulse, carotid pulse Carotid Pulse Cardiovascular Examination), and some are infrequently used (femoral pulse). A thorough cardiac exam requires an evaluation of all peripheral pulses. Always compare the pulses on both sides of the body to detect differences in strength.
- Carotid artery
- Radial artery Radial Artery The direct continuation of the brachial trunk, originating at the bifurcation of the brachial artery opposite the neck of the radius. Its branches may be divided into three groups corresponding to the three regions in which the vessel is situated, the forearm, wrist, and hand. Forearm: Anatomy
- Femoral artery Femoral Artery The main artery of the thigh, a continuation of the external iliac artery. Femoral Region and Hernias: Anatomy
- Popliteal artery Popliteal Artery The continuation of the femoral artery coursing through the popliteal fossa; it divides into the anterior and posterior tibial arteries. Popliteal Fossa: Anatomy
- Posterior tibial artery
- Dorsalis pedis artery Dorsalis pedis artery Foot: Anatomy
Peripheral Edema Peripheral edema Peripheral edema is the swelling of the lower extremities, namely, legs, feet, and ankles. Edema
Palpating the extremities is the preferred method for quantifying peripheral edema Peripheral edema Peripheral edema is the swelling of the lower extremities, namely, legs, feet, and ankles. Edema. The two types of edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema are pitting and non-pitting edema Non-pitting edema Edema caused by excess colloid without excess fluid Edema.[6]
Pitting edema Pitting edema Edema caused by excess fluid without excess colloid. Leaves “pits” due to fluid displacement when pressure is applied to the area Edema refers to the depressed or indented area that results from pressure applied over an area of swollen/edematous tissue. It is caused by the displacement Displacement The process by which an emotional or behavioral response that is appropriate for one situation appears in another situation for which it is inappropriate. Defense Mechanisms of thin, watery, protein-poor (transudative) interstitial fluid Interstitial fluid Body Fluid Compartments. Although it can affect any part of the body, pitting edema Pitting edema Edema caused by excess fluid without excess colloid. Leaves “pits” due to fluid displacement when pressure is applied to the area Edema usually occurs in the legs, feet, and ankles due to venous insufficiency caused by congestive heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR). Edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema associated with decreased plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products oncotic pressure Oncotic Pressure Edema (e.g., low serum albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests associated with liver failure Liver failure Severe inability of the liver to perform its normal metabolic functions, as evidenced by severe jaundice and abnormal serum levels of ammonia; bilirubin; alkaline phosphatase; aspartate aminotransferase; lactate dehydrogenases; and albumin/globulin ratio. Autoimmune Hepatitis or malnutrition Malnutrition Malnutrition is a clinical state caused by an imbalance or deficiency of calories and/or micronutrients and macronutrients. The 2 main manifestations of acute severe malnutrition are marasmus (total caloric insufficiency) and kwashiorkor (protein malnutrition with characteristic edema). Malnutrition in children in resource-limited countries) does not change with dependency.
Non-pitting or “brawny” edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema is observed when applied pressure does not leave an indentation. It is usually caused by compression Compression Blunt Chest Trauma or compromise of lymphatic drainage ( lymphedema Lymphedema Edema due to obstruction of lymph vessels or disorders of the lymph nodes. Lymphatic Filariasis (Elephantiasis)) and can also be seen in myxedema Myxedema A condition characterized by a dry, waxy type of swelling (edema) with abnormal deposits of mucopolysaccharides in the skin and other tissues. It is caused by a deficiency of thyroid hormones. The skin becomes puffy around the eyes and on the cheeks. The face is dull and expressionless with thickened nose and lips. Edema of hypothyroidism Hypothyroidism Hypothyroidism is a condition characterized by a deficiency of thyroid hormones. Iodine deficiency is the most common cause worldwide, but Hashimoto's disease (autoimmune thyroiditis) is the leading cause in non-iodine-deficient regions. Hypothyroidism. The non-compressible subcutaneous tissue Subcutaneous tissue Loose connective tissue lying under the dermis, which binds skin loosely to subjacent tissues. It may contain a pad of adipocytes, which vary in number according to the area of the body and vary in size according to the nutritional state. Soft Tissue Abscess contains proteinaceous and possibly organizing collagenous substances.
Pitting edema Pitting edema Edema caused by excess fluid without excess colloid. Leaves “pits” due to fluid displacement when pressure is applied to the area Edema refers to the depressed or indented area that results from pressure applied over an area of swollen/edematous subcutaneous tissue. It is caused by the displacement Displacement The process by which an emotional or behavioral response that is appropriate for one situation appears in another situation for which it is inappropriate. Defense Mechanisms of thin, watery, protein-poor (transudative) interstitial fluid Interstitial fluid Body Fluid Compartments. Although it can affect any part of the body, pitting edema Pitting edema Edema caused by excess fluid without excess colloid. Leaves “pits” due to fluid displacement when pressure is applied to the area Edema usually occurs in the legs, feet, and ankles when due to venous insufficiency caused by congestive heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR). Edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema associated with decreased plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products oncotic pressure Oncotic Pressure Edema (e.g., low serum albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests associated with liver failure Liver failure Severe inability of the liver to perform its normal metabolic functions, as evidenced by severe jaundice and abnormal serum levels of ammonia; bilirubin; alkaline phosphatase; aspartate aminotransferase; lactate dehydrogenases; and albumin/globulin ratio. Autoimmune Hepatitis or malnutrition Malnutrition Malnutrition is a clinical state caused by an imbalance or deficiency of calories and/or micronutrients and macronutrients. The 2 main manifestations of acute severe malnutrition are marasmus (total caloric insufficiency) and kwashiorkor (protein malnutrition with characteristic edema). Malnutrition in children in resource-limited countries) does not change with dependency. Non-pitting or “brawny” edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema is observed when applied pressure does not leave an indentation. It is usually caused by compression Compression Blunt Chest Trauma or compromise of lymphatic drainage, and can also be seen in myxedema Myxedema A condition characterized by a dry, waxy type of swelling (edema) with abnormal deposits of mucopolysaccharides in the skin and other tissues. It is caused by a deficiency of thyroid hormones. The skin becomes puffy around the eyes and on the cheeks. The face is dull and expressionless with thickened nose and lips. Edema of hypothyroidism Hypothyroidism Hypothyroidism is a condition characterized by a deficiency of thyroid hormones. Iodine deficiency is the most common cause worldwide, but Hashimoto's disease (autoimmune thyroiditis) is the leading cause in non-iodine-deficient regions. Hypothyroidism. The non-compressible subcutaneous tissue Subcutaneous tissue Loose connective tissue lying under the dermis, which binds skin loosely to subjacent tissues. It may contain a pad of adipocytes, which vary in number according to the area of the body and vary in size according to the nutritional state. Soft Tissue Abscess contains proteinaceous and possibly organizing collagenous or myxomatous substances.
Procedure: Press firmly on the affected area for 5 seconds—usually the lower leg Leg The lower leg, or just "leg" in anatomical terms, is the part of the lower limb between the knee and the ankle joint. The bony structure is composed of the tibia and fibula bones, and the muscles of the leg are grouped into the anterior, lateral, and posterior compartments by extensions of fascia. Leg: Anatomy (on the medial ankle or anterior tibia Tibia The second longest bone of the skeleton. It is located on the medial side of the lower leg, articulating with the fibula laterally, the talus distally, and the femur proximally. Knee Joint: Anatomy). Pitting is measured by the table below:
| Trace | Barely detectable impression when a finger is pressed into the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions |
| 1+ | Mild pitting edema Pitting edema Edema caused by excess fluid without excess colloid. Leaves “pits” due to fluid displacement when pressure is applied to the area Edema, disappears rapidly |
| 2+ | Moderate indentation, persists for more than a few seconds |
| 3+ | Moderately severe pitting, more profound and persists longer than 2+ |
| 4+ | Severe pitting that persists for over a minute |
Although all clinicians use this scale Scale Dermatologic Examination, there is no agreed-upon definition of these grades. Some sources use 0.5 cm to 2 cm for 1+ to 4+, others use 2mm to 8 mm, and some use times for rebound from 15 seconds to 2 minutes. However, this scale Scale Dermatologic Examination is still useful because it documents relative changes in edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema on repeat exams. [7,8]
Point of Maximal Impulse (PMI)
Procedure:
- Place the palm of your right hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy on the chest. With the heel of your palm at the left lower sternal border, your fingers should wrap around the patient’s ribs Ribs A set of twelve curved bones which connect to the vertebral column posteriorly, and terminate anteriorly as costal cartilage. Together, they form a protective cage around the internal thoracic organs. Chest Wall: Anatomy laterally.
- Apply some pressure to the chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy until you feel the heartbeat in your palm.
- Identify the point of maximum impulse on the chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy. It will be a small area, no larger than 2–3 cm wide.
Obesity Obesity Obesity is a condition associated with excess body weight, specifically with the deposition of excessive adipose tissue. Obesity is considered a global epidemic. Major influences come from the western diet and sedentary lifestyles, but the exact mechanisms likely include a mixture of genetic and environmental factors. Obesity will make this part of the exam difficult. The PMI of a healthy person with a normal and healthy heart will be located near the 5th intercostal space, along the midclavicular line. The PMI of a dilated or hypertrophied left ventricle will be displaced laterally.
Thrill
A thrill–a vibration Vibration A continuing periodic change in displacement with respect to a fixed reference. Neurological Examination associated with turbulent blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure– may be detected if valvular disease is present. This is through a damaged or malformed valve. Thrills are located near the area in which the valves are auscultated.
Auscultation
The detection and recognition of heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds play an important role in diagnosing various cardiac and valvular conditions. Because familiarity with heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds has such profound and practical importance, students undertaking the USMLE are expected to have a good understanding of their pathophysiology and their clinical applications.
Auscultation is best performed on bare skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions. Always be sure to maintain your patient’s modesty while examining on the chest.
Heart Sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds
On auscultation, 2 heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds are heard from a normal heart, known as “ S1 S1 Heart Sounds” and “ S2 S2 Heart Sounds,” or the first and second heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds. They reflect the turbulence created when the heart valves close. Two extra heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds may also be heard, called the third and fourth heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds, “ S3 S3 Heart Sounds” and “ S4 S4 Heart Sounds” may be heard in both normal and abnormal conditions. [9] A murmur consists of a blowing, whooshing, or rasping sound heard during a heartbeat as blood flows through the heart’s chambers and valves or blood vessels near the heart. It can be a sign of a benign Benign Fibroadenoma/physiologic or pathologic condition.
Murmurs
A murmur is a sound that is produced by turbulent blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure across a heart valve. The turbulent flow Turbulent flow Vascular Resistance, Flow, and Mean Arterial Pressure can occur for two reasons; blood flowing across an abnormal heart valve or increased blood flowing across a normal heart valve. Heart murmurs Heart murmurs Heart sounds caused by vibrations resulting from the flow of blood through the heart. Heart murmurs can be examined by heart auscultation, and analyzed by their intensity (6 grades), duration, timing (systolic, diastolic, or continuous), location, transmission, and quality (musical, vibratory, blowing, etc). Heart Sounds may be classified as physiological or innocent murmurs or pathologic murmurs based on their etiology. [20]
- A physiological or innocent murmur is heard when there is increased turbulent
blood flow
Blood flow
Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute).
Vascular Resistance, Flow, and Mean Arterial Pressure across a normal valve, as can happen in
patients
Patients
Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures.
Clinician–Patient Relationship with
fever
Fever
Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin.
Fever,
thyrotoxicosis
Thyrotoxicosis
A hypermetabolic syndrome caused by excess thyroid hormones which may come from endogenous or exogenous sources. The endogenous source of hormone may be thyroid hyperplasia; thyroid neoplasms; or hormone-producing extrathyroidal tissue. Thyrotoxicosis is characterized by nervousness; tachycardia; fatigue; weight loss; heat intolerance; and excessive sweating.
Thyrotoxicosis and Hyperthyroidism, or
anemia
Anemia
Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology.
Anemia: Overview and Types and during exercise. The key features of innocent murmurs can be summarized by the “Seven S’s”:
- Sensitive (changes with body position or with respiration Respiration The act of breathing with the lungs, consisting of inhalation, or the taking into the lungs of the ambient air, and of exhalation, or the expelling of the modified air which contains more carbon dioxide than the air taken in. Nose Anatomy (External & Internal))
- Short duration (not holosystolic)
- Single (no associated clicks Clicks A high-pitched sound occurring at the point of maximal opening of the valves Heart Sounds or gallops)
- Small (murmur limited to a small area and not radiating away from this area)
- Soft (low amplitude)
- Sweet (not harsh sounding)
- Systolic (occurs during and is limited to systole Systole Period of contraction of the heart, especially of the heart ventricles. Cardiac Cycle)
- A pathologic murmur occurs when there is turbulent blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure across an abnormal valve. This can be due to either stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) or insufficiency.
Valvular abnormalities
Stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS)
Stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) is the abnormal narrowing of a valve orifice, commonly seen when age-related calcific deposits (“degenerative calcification”) occur in the aortic valve Aortic valve The valve between the left ventricle and the ascending aorta which prevents backflow into the left ventricle. Heart: Anatomy. Stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) is also seen in a mitral valve Mitral valve The valve between the left atrium and left ventricle of the heart. Heart: Anatomy damaged by scar Scar Dermatologic Examination tissue from healed rheumatic heart disease Rheumatic Heart Disease Cardiac manifestation of systemic rheumatological conditions, such as rheumatic fever. Rheumatic heart disease can involve any part the heart, most often the heart valves and the endocardium. Rheumatic Fever (RHD), mostly seen in developing countries, or by myxomatous disease and fibroelastic deficiency Fibroelastic deficiency Mitral Valve Prolapse, more common in developed countries.
Regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD)
Regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) refers to the abnormal backward flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure of blood from a high-pressure chamber to a low-pressure chamber, often due to an incompetent valve (i.e., a valve that cannot close properly). An example is valvular aortic regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) ( AR AR Aortic regurgitation (AR) is a cardiac condition characterized by the backflow of blood from the aorta to the left ventricle during diastole. Aortic regurgitation is associated with an abnormal aortic valve and/or aortic root stemming from multiple causes, commonly rheumatic heart disease as well as congenital and degenerative valvular disorders. Aortic Regurgitation), most commonly due to congenital or degenerative abnormalities of the aortic leaflets, aortic root, and ascending aorta Ascending aorta Mediastinum and Great Vessels: Anatomy in developed countries. At the same time, RHD remains the most common cause of severe AR AR Aortic regurgitation (AR) is a cardiac condition characterized by the backflow of blood from the aorta to the left ventricle during diastole. Aortic regurgitation is associated with an abnormal aortic valve and/or aortic root stemming from multiple causes, commonly rheumatic heart disease as well as congenital and degenerative valvular disorders. Aortic Regurgitation worldwide. [10.11]
Origins and Timing of the Heart Sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds
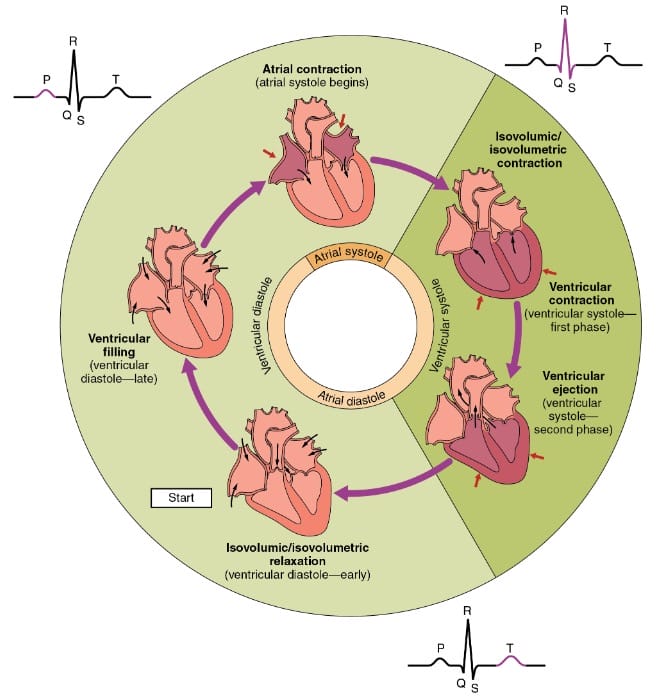
First and Second Heart Sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds
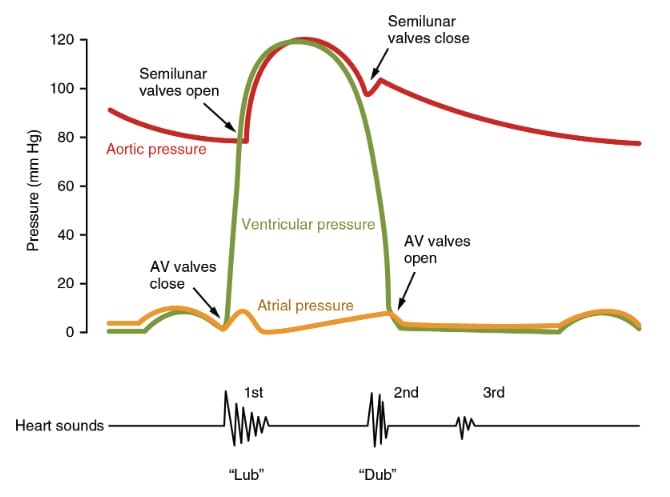
The closure of the heart valves produces vibrations that are picked up as the two heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds.
The first heart sound, S1 S1 Heart Sounds, corresponds to the closure of the atrioventricular valves—the tricuspid and mitral valves of the heart. S1 S1 Heart Sounds represents the start of ventricular systole Ventricular systole Cardiac Cycle. The closure of the mitral valves precedes the closure of the tricuspid valves, but this is only minimally different so that S1 S1 Heart Sounds is usually heard as a single sound. S1 S1 Heart Sounds is best heard at the apex of the heart, which points to the left of the body and is located near the PMI in a healthy individual).
The second heart sound, S2 S2 Heart Sounds, corresponds to the closure of the semilunar valves—the aortic and pulmonary valves of the heart. S2 S2 Heart Sounds signifies the end of ventricular systole Ventricular systole Cardiac Cycle and the beginning of diastole Diastole Post-systolic relaxation of the heart, especially the heart ventricles. Cardiac Cycle. S2 S2 Heart Sounds is shorter, softer, and slightly higher pitched than the first heart sound. A reduced or absent S2 S2 Heart Sounds indicates pathology due to an abnormal aortic or pulmonic valve.
The pulmonary component of S2 S2 Heart Sounds is called P2, and the aortic component is called A2.
It is important to clearly identify S1 S1 Heart Sounds and S2 S2 Heart Sounds because it helps distinguish systolic from diastolic murmurs Diastolic Murmurs Heart Sounds and other events in the cardiac cycle Cardiac cycle The cardiac cycle describes a complete contraction and relaxation of all 4 chambers of the heart during a standard heartbeat. The cardiac cycle includes 7 phases, which together describe the cycle of ventricular filling, isovolumetric contraction, ventricular ejection, and isovolumetric relaxation. Cardiac Cycle. Here are three clues to help distinguish them: the time between S1 S1 Heart Sounds and S2 S2 Heart Sounds ( systole Systole Period of contraction of the heart, especially of the heart ventricles. Cardiac Cycle) is shorter than the time between S2 S2 Heart Sounds and the next S1 S1 Heart Sounds ( diastole Diastole Post-systolic relaxation of the heart, especially the heart ventricles. Cardiac Cycle); S1 S1 Heart Sounds is usually louder than S2 S2 Heart Sounds (useful if tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children interferes with the interpretation), and S1 S1 Heart Sounds is synchronized with the carotid pulse Carotid Pulse Cardiovascular Examination. [12, 13]
Splitting Splitting Defense Mechanisms of the Second Heart Sound
Physiologic Splitting Splitting Defense Mechanisms of S2 S2 Heart Sounds:
Both the aortic and pulmonic valves will close when the pressure above them is higher than the pressure in the ventricle below. The pulmonic valve closes later than the aortic valve Aortic valve The valve between the left ventricle and the ascending aorta which prevents backflow into the left ventricle. Heart: Anatomy because of two main factors. The first is that the vascular resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing in the pulmonary artery Pulmonary artery The short wide vessel arising from the conus arteriosus of the right ventricle and conveying unaerated blood to the lungs. Lungs: Anatomy is lower than that in the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy, so blood continues flowing into the pulmonary artery Pulmonary artery The short wide vessel arising from the conus arteriosus of the right ventricle and conveying unaerated blood to the lungs. Lungs: Anatomy after the aortic valve Aortic valve The valve between the left ventricle and the ascending aorta which prevents backflow into the left ventricle. Heart: Anatomy closes. In 70% of normal adults, this difference can be heard as splitting Splitting Defense Mechanisms of the second heart sound. Additionally, during inspiration Inspiration Ventilation: Mechanics of Breathing, more blood fills the right ventricle leading to a slightly longer ejection time of the right ventricle, adding to the delayed pulmonic valve closure and to the length of the S2 S2 Heart Sounds split. A2 is heard widely all over the chest. P2 is usually soft and only heard at the pulmonic region (second intercostal space, left sternal border), but even here, A2 is louder.
Abnormal (Pathologic) Splitting Splitting Defense Mechanisms of S2 S2 Heart Sounds:
- Wider-than-normal splitting Splitting Defense Mechanisms of S2 S2 Heart Sounds is an exaggerated (persistent) physiological split that is more pronounced during inspiration Inspiration Ventilation: Mechanics of Breathing. Wide splitting Splitting Defense Mechanisms is caused by delayed pulmonic valve closure, such as in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with pulmonic stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) or right bundle branch block Right bundle branch block Bundle Branch and Fascicular Blocks, or early closure of the aortic valve Aortic valve The valve between the left ventricle and the ascending aorta which prevents backflow into the left ventricle. Heart: Anatomy caused by mitral regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD).
- Fixed splitting Splitting Defense Mechanisms of S2 S2 Heart Sounds: wide splitting Splitting Defense Mechanisms that does not vary with respiration Respiration The act of breathing with the lungs, consisting of inhalation, or the taking into the lungs of the ambient air, and of exhalation, or the expelling of the modified air which contains more carbon dioxide than the air taken in. Nose Anatomy (External & Internal), often due to prolonged right ventricular systole Ventricular systole Cardiac Cycle, seen in atrial septal defect Atrial Septal Defect Atrial septal defects (ASDs) are benign acyanotic congenital heart defects characterized by an opening in the interatrial septum that causes blood to flow from the left atrium (LA) to the right atrium (RA) (left-to-right shunt). Atrial Septal Defect (ASD) or advanced right ventricular failure.
- Reversed or paradoxical splitting Splitting Defense Mechanisms of S2 S2 Heart Sounds: Aortic valve Aortic valve The valve between the left ventricle and the ascending aorta which prevents backflow into the left ventricle. Heart: Anatomy closure delayed due to aortic stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS)) or conduction disease ( left bundle branch block Left bundle branch block Bundle Branch and Fascicular Blocks). Normal inspiratory delay of P2 usually makes the split disappear.
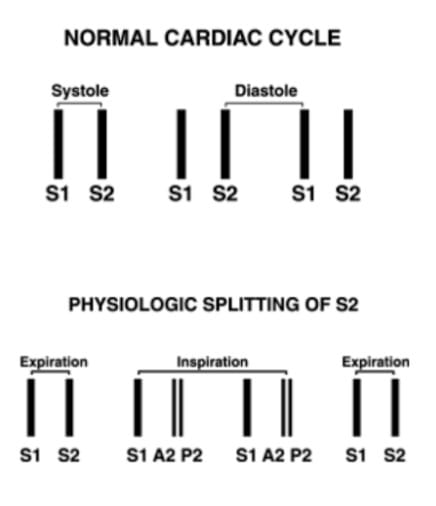
Normal cardiac cycle and splitting of S2
Image by Lecturio.High-yield fact:
Absent normal/physiologic splitting Splitting Defense Mechanisms of S2 S2 Heart Sounds can be seen in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with:
- Severe aortic stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) (seen most often in older adults)
- Ventricular septal defect Ventricular Septal Defect Tetralogy of Fallot (VSD) with Eisenmenger syndrome (in pediatric patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship)
Extra Heart Sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds
Third Heart Sound ( S3 S3 Heart Sounds)
“Extra” heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds include the third and fourth heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds called S3 S3 Heart Sounds and S4 S4 Heart Sounds. S3 S3 Heart Sounds is a mid-diastolic, low-pitched sound that occurs after S2 S2 Heart Sounds during the rapid passive filling of the ventricle. When there is an audible S3 S3 Heart Sounds, the heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds are described as having a gallop rhythm, resembling a galloping horse, especially at rapid heart rates, which sounds like the word “Kentucky.” S3 S3 Heart Sounds is also called a ventricular gallop.
A physiologic S3 S3 Heart Sounds is produced when there is rapid filling during diastole Diastole Post-systolic relaxation of the heart, especially the heart ventricles. Cardiac Cycle, as can happen in conditions that increase cardiac output Cardiac output The volume of blood passing through the heart per unit of time. It is usually expressed as liters (volume) per minute so as not to be confused with stroke volume (volume per beat). Cardiac Mechanics, such as thyrotoxicosis Thyrotoxicosis A hypermetabolic syndrome caused by excess thyroid hormones which may come from endogenous or exogenous sources. The endogenous source of hormone may be thyroid hyperplasia; thyroid neoplasms; or hormone-producing extrathyroidal tissue. Thyrotoxicosis is characterized by nervousness; tachycardia; fatigue; weight loss; heat intolerance; and excessive sweating. Thyrotoxicosis and Hyperthyroidism and pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care. It is also sometimes seen as a normal finding in children. On the other hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy, a pathologic S3 S3 Heart Sounds is produced when there is decreased compliance Compliance Distensibility measure of a chamber such as the lungs (lung compliance) or bladder. Compliance is expressed as a change in volume per unit change in pressure. Veins: Histology of the ventricle (dilatation or overload), arising from high left ventricular filling Ventricular filling Cardiac Cycle pressures and abrupt deceleration Deceleration A decrease in the rate of speed. Blunt Chest Trauma of blood as it flows into the ventricle at the end of the rapid filling phase of diastole Diastole Post-systolic relaxation of the heart, especially the heart ventricles. Cardiac Cycle. Causes include decreased myocardial contractility, heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR), ventricular volume overload from aortic or mitral regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD), hypertrophic cardiomyopathy Hypertrophic Cardiomyopathy Hypertrophic cardiomyopathy (HCM) is the most commonly inherited cardiomyopathy, which is characterized by an asymmetric increase in thickness (hypertrophy) of the left ventricular wall, diastolic dysfunction, and often left ventricular outflow tract obstruction. Hypertrophic Cardiomyopathy, and left-to-right shunts Left-to-right shunts Development of the Heart (e.g., patent ductus arteriosus Ductus arteriosus A fetal blood vessel connecting the pulmonary artery with the descending aorta. Patent Ductus Arteriosus (PDA), ventricular septal defect Ventricular Septal Defect Tetralogy of Fallot). Reduced right ventricular compliance Compliance Distensibility measure of a chamber such as the lungs (lung compliance) or bladder. Compliance is expressed as a change in volume per unit change in pressure. Veins: Histology can also cause a pathologic S3 S3 Heart Sounds, including right ventricular failure and constrictive pericarditis Constrictive pericarditis Inflammation of the pericardium that is characterized by the fibrous scarring and adhesion of both serous layers, the visceral pericardium and the parietal pericardium leading to the loss of pericardial cavity. The thickened pericardium severely restricts cardiac filling. Clinical signs include fatigue, muscle wasting, and weight loss. Pericarditis. [14,15]

The third heart sound (S3) is an extra heart sound which follows S2 and is caused by blood from the left atrium “colliding” with residual blood in the left ventricle. It is associated with heart failure.
Image by Lecturio.Fourth Heart Sound ( S4 S4 Heart Sounds)
The fourth heart sound ( S4 S4 Heart Sounds) is a late diastolic sound. It is a bit higher-pitched than S3 S3 Heart Sounds. An S4 S4 Heart Sounds sound can produce a gallop rhythm but with a cadence that matches the word “Tennessee.” It is never heard when there are no atrial contractions (it is absent in atrial fibrillation Atrial fibrillation Atrial fibrillation (AF or Afib) is a supraventricular tachyarrhythmia and the most common kind of arrhythmia. It is caused by rapid, uncontrolled atrial contractions and uncoordinated ventricular responses. Atrial Fibrillation). S4 S4 Heart Sounds is caused by decreased ventricular compliance Compliance Distensibility measure of a chamber such as the lungs (lung compliance) or bladder. Compliance is expressed as a change in volume per unit change in pressure. Veins: Histology; the most common causes of a left-sided S4 S4 Heart Sounds include hypertensive heart disease, aortic stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), and ischemic and hypertrophic cardiomyopathy Hypertrophic Cardiomyopathy Hypertrophic cardiomyopathy (HCM) is the most commonly inherited cardiomyopathy, which is characterized by an asymmetric increase in thickness (hypertrophy) of the left ventricular wall, diastolic dysfunction, and often left ventricular outflow tract obstruction. Hypertrophic Cardiomyopathy. As in pulmonary hypertension Pulmonary Hypertension Pulmonary hypertension (PH) or pulmonary arterial hypertension (PAH) is characterized by elevated pulmonary arterial pressure, which can lead to chronic progressive right heart failure. Pulmonary hypertension is grouped into 5 categories based on etiology, which include primary PAH, and PH due to cardiac disease, lung or hypoxic disease, chronic thromboembolic disease, and multifactorial or unclear etiologies. Pulmonary Hypertension and pulmonary stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), reduced right ventricular compliance Compliance Distensibility measure of a chamber such as the lungs (lung compliance) or bladder. Compliance is expressed as a change in volume per unit change in pressure. Veins: Histology can also cause a right-sided S4 S4 Heart Sounds.
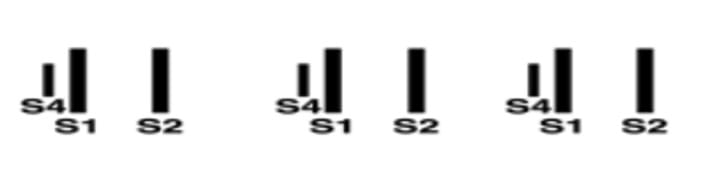
The fourth heart sound (S4) precedes S1 and is usually caused by atrial systolic contraction of blood into a poorly-compliant (“stiff”) left ventricle, as can be seen in systemic hypertension.
Image by Lecturio.It is possible for the third and fourth heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds to co-exist, which is called a quadruple rhythm. This indicates significantly impaired ventricular function. If S3 S3 Heart Sounds and S4 S4 Heart Sounds are superimposed when tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children is present, it produces a summation gallop. [16]
Murmurs
There are 8 possible features of heart murmurs Heart murmurs Heart sounds caused by vibrations resulting from the flow of blood through the heart. Heart murmurs can be examined by heart auscultation, and analyzed by their intensity (6 grades), duration, timing (systolic, diastolic, or continuous), location, transmission, and quality (musical, vibratory, blowing, etc). Heart Sounds to describe and document after auscultating a patient’s heart to formulate a diagnosis. The characteristics of a heart murmur are intensity (grade), quality Quality Activities and programs intended to assure or improve the quality of care in either a defined medical setting or a program. The concept includes the assessment or evaluation of the quality of care; identification of problems or shortcomings in the delivery of care; designing activities to overcome these deficiencies; and follow-up monitoring to ensure effectiveness of corrective steps. Quality Measurement and Improvement, pitch, timing, configuration (shape), location, and whether they are affected by maneuvers such as hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy grip, Valsalva, or squatting. For example, after examining a patient, a student may present this information: “The patient has a 2/6, harsh, low-pitched, systolic crescendo-decrescendo murmur heard loudest at the right upper sternal border that radiates to the neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess into both carotids,” which lets us know this patient most likely has valvular aortic stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS).[17]
Timing, Pitch, and Quality Quality Activities and programs intended to assure or improve the quality of care in either a defined medical setting or a program. The concept includes the assessment or evaluation of the quality of care; identification of problems or shortcomings in the delivery of care; designing activities to overcome these deficiencies; and follow-up monitoring to ensure effectiveness of corrective steps. Quality Measurement and Improvement
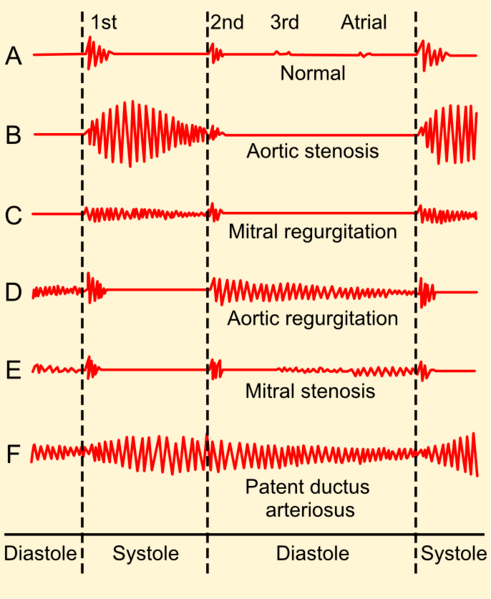
Systolic Murmurs Systolic Murmurs Heart murmurs which are systolic in timing. They occur between the first and the second heart sounds, between the closure of mitral valve and tricuspid valve and the closure of semilunar aortic and pulmonary valves. Systolic murmurs include ejection murmurs and regurgitant murmurs. Heart Sounds
Systolic murmurs Systolic Murmurs Heart murmurs which are systolic in timing. They occur between the first and the second heart sounds, between the closure of mitral valve and tricuspid valve and the closure of semilunar aortic and pulmonary valves. Systolic murmurs include ejection murmurs and regurgitant murmurs. Heart Sounds are produced during systole Systole Period of contraction of the heart, especially of the heart ventricles. Cardiac Cycle (contraction) of the ventricles, which is the period between S1 S1 Heart Sounds and S2 S2 Heart Sounds. These murmurs can be midsystolic (ejection), late systolic, or pansystolic. Systolic murmurs Systolic Murmurs Heart murmurs which are systolic in timing. They occur between the first and the second heart sounds, between the closure of mitral valve and tricuspid valve and the closure of semilunar aortic and pulmonary valves. Systolic murmurs include ejection murmurs and regurgitant murmurs. Heart Sounds can be either normal or abnormal.
Midsystolic ejection murmurs have their highest intensity in the middle of systole Systole Period of contraction of the heart, especially of the heart ventricles. Cardiac Cycle. They are often described as having a “crescendo-decrescendo” configuration or shape. This could be a physiological murmur caused by an increased flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure through a normal valve or indicate various pathologic conditions, such as aortic stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) or pulmonary stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS). In cases of congenital aortic or pulmonary stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), an early high-pitched systolic ejection click may also be heard, representing the sudden opening of these valves, which are still mobile.[18]
A late systolic murmur is when there is a gap between hearing S1 S1 Heart Sounds and the murmur. This can be caused by mitral regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD), as in the case of papillary muscle dysfunction or mitral valve Mitral valve The valve between the left atrium and left ventricle of the heart. Heart: Anatomy prolapse.
A pansystolic (holosystolic) murmur extends from S1 S1 Heart Sounds to S2 S2 Heart Sounds. The pitch and loudness of this murmur stay the same during systole Systole Period of contraction of the heart, especially of the heart ventricles. Cardiac Cycle. The murmur is caused by leakage from a high-pressure chamber to a low-pressure chamber. Causes of pansystolic murmurs include mitral or tricuspid regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) and ventricular septal defect Ventricular Septal Defect Tetralogy of Fallot.
High-yield fact:
A mid-systolic murmur in an asymptomatic individual is most likely physiological, unlike diastolic murmurs Diastolic Murmurs Heart Sounds, which are always pathological.
High-yield fact:
It is usually easier to auscultate a systolic murmur than a diastolic one because it tends to be louder, with a harsher sound, and does not require a special maneuver to accentuate it.
Diastolic Murmurs Diastolic Murmurs Heart Sounds
Diastolic murmurs Diastolic Murmurs Heart Sounds, as their name implies, occur during ventricular diastole Ventricular diastole Cardiac Cycle. They are always pathological. They are less common, softer, and more challenging to hear than systolic murmurs Systolic Murmurs Heart murmurs which are systolic in timing. They occur between the first and the second heart sounds, between the closure of mitral valve and tricuspid valve and the closure of semilunar aortic and pulmonary valves. Systolic murmurs include ejection murmurs and regurgitant murmurs. Heart Sounds. There are two basic types in adults. Early decrescendo (meaning the sound decreases in intensity from the beginning to the end of the murmur) diastolic murmurs Diastolic Murmurs Heart Sounds are caused by regurgitant flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure through an incompetent semilunar valve, usually the aortic. Rumbling diastolic murmurs in mid- or late diastole Diastole Post-systolic relaxation of the heart, especially the heart ventricles. Cardiac Cycle are most often caused by mitral stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS).
An early diastolic murmur starts with S2 S2 Heart Sounds and is a decrescendo murmur that is loudest at its commencement. It produces a high-pitched sound. Causes of an early diastolic murmur include aortic regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) or pulmonary regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD). The decrescendo quality Quality Activities and programs intended to assure or improve the quality of care in either a defined medical setting or a program. The concept includes the assessment or evaluation of the quality of care; identification of problems or shortcomings in the delivery of care; designing activities to overcome these deficiencies; and follow-up monitoring to ensure effectiveness of corrective steps. Quality Measurement and Improvement mirrors the peak in aortic and pulmonary pressures at the start of diastole Diastole Post-systolic relaxation of the heart, especially the heart ventricles. Cardiac Cycle.
Compared to early diastolic murmurs Diastolic Murmurs Heart Sounds, mid-and late diastolic murmurs Diastolic Murmurs Heart Sounds are lower-pitched and can be mitral or tricuspid stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) or atrial myxoma Myxoma A benign neoplasm derived from connective tissue, consisting chiefly of polyhedral and stellate cells that are loosely embedded in a soft mucoid matrix, thereby resembling primitive mesenchymal tissue. It occurs frequently intramuscularly where it may be mistaken for a sarcoma. It appears also in the jaws and the skin. Cardiac Myxoma (rare). They may be described as “rumbling” in quality Quality Activities and programs intended to assure or improve the quality of care in either a defined medical setting or a program. The concept includes the assessment or evaluation of the quality of care; identification of problems or shortcomings in the delivery of care; designing activities to overcome these deficiencies; and follow-up monitoring to ensure effectiveness of corrective steps. Quality Measurement and Improvement. In patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with mitral stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), the diastolic murmur may be preceded by a high-pitched opening snap Opening snap Mitral Stenosis which represents the abrupt opening of the stenosed mitral valve Mitral valve The valve between the left atrium and left ventricle of the heart. Heart: Anatomy.
Continuous Murmurs
Continuous murmurs occur during both systole Systole Period of contraction of the heart, especially of the heart ventricles. Cardiac Cycle and diastole Diastole Post-systolic relaxation of the heart, especially the heart ventricles. Cardiac Cycle without a pause. The sound is created by unidirectional flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure when there is communication Communication The exchange or transmission of ideas, attitudes, or beliefs between individuals or groups. Decision-making Capacity and Legal Competence between a high-pressure and a low-pressure source. The constant pressure gradient Pressure gradient Vascular Resistance, Flow, and Mean Arterial Pressure results in a continuous flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure. The most common causes are nonvalvular and include patent ductus arteriosus Ductus arteriosus A fetal blood vessel connecting the pulmonary artery with the descending aorta. Patent Ductus Arteriosus (PDA), an arteriovenous fistula Arteriovenous fistula An abnormal direct communication between an artery and a vein without passing through the capillaries. An a-v fistula usually leads to the formation of a dilated sac-like connection, arteriovenous aneurysm. The locations and size of the shunts determine the degree of effects on the cardiovascular functions such as blood pressure and heart rate. Vascular Surgery, and coarctation of the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy.[19] A venous hum is also a continuous sound that is benign Benign Fibroadenoma, common in children, and produced by turbulence of blood in the jugular veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology.
Intensity
If a murmur is heard, various dynamic maneuver tests are required to characterize it further. These maneuvers alter circulatory hemodynamics Hemodynamics The movement and the forces involved in the movement of the blood through the cardiovascular system. Vascular Resistance, Flow, and Mean Arterial Pressure and, in doing so, change the emphasis with different murmurs.
- Grade 1: Murmur is very soft and is initially not heard.
- Grade 2: Murmur is soft but can be readily heard by a skilled examiner.
- Grade 3: Murmur is easy to hear.
- Grade 4: Murmur is slightly loud and accompanied by a palpable thrill (these murmurs are always pathological).
- Grade 5: Murmur is very loud, and the accompanying thrill is easily palpable.
- Grade 6: Murmur is so loud that it is audible even without directly placing the stethoscope on the chest.
Note:
The intensity of the murmur doesn’t always correlate to the severity of the lesions, as a smaller VSD produces louder murmurs than a larger VSD.
High-yield fact:
- Murmurs of grade III and above are usually pathological.
- Thrills are palpable murmurs and only can be felt in murmurs of grade IV and above.
Location, Radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma, and Dynamic Maneuvers
Location
There are four locations on the chest that the stethoscope is placed over to listen to heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds and any abnormal findings. Auscultation can be carried out clockwise, starting with the aortic, then the pulmonic and mitral areas, followed by the tricuspid area.
To identify the difference between the two heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds on auscultation, palpation Palpation Application of fingers with light pressure to the surface of the body to determine consistency of parts beneath in physical diagnosis; includes palpation for determining the outlines of organs. Dermatologic Examination of the pulse (carotid or radial) while listening to the heart can be helpful. The pulse indicates systole Systole Period of contraction of the heart, especially of the heart ventricles. Cardiac Cycle, therefore corresponding to the first heart sound S1 S1 Heart Sounds. Knowing when systole Systole Period of contraction of the heart, especially of the heart ventricles. Cardiac Cycle and diastole Diastole Post-systolic relaxation of the heart, especially the heart ventricles. Cardiac Cycle occur is essential if an additional heart sound is heard for its timing in the cardiac cycle Cardiac cycle The cardiac cycle describes a complete contraction and relaxation of all 4 chambers of the heart during a standard heartbeat. The cardiac cycle includes 7 phases, which together describe the cycle of ventricular filling, isovolumetric contraction, ventricular ejection, and isovolumetric relaxation. Cardiac Cycle to be accurately described. [22]
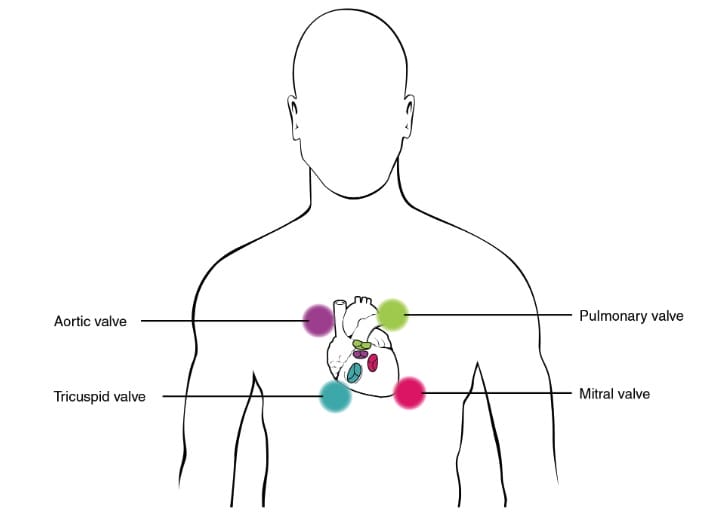
The aortic area is located in the second intercostal space, at the right sternal border. The diaphragm Diaphragm The diaphragm is a large, dome-shaped muscle that separates the thoracic cavity from the abdominal cavity. The diaphragm consists of muscle fibers and a large central tendon, which is divided into right and left parts. As the primary muscle of inspiration, the diaphragm contributes 75% of the total inspiratory muscle force. Diaphragm: Anatomy of the stethoscope can be placed at this site to listen for aortic stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS).
The pulmonic area is opposite the aortic area t the left second intercostal space, at the left sternal border. The diaphragm Diaphragm The diaphragm is a large, dome-shaped muscle that separates the thoracic cavity from the abdominal cavity. The diaphragm consists of muscle fibers and a large central tendon, which is divided into right and left parts. As the primary muscle of inspiration, the diaphragm contributes 75% of the total inspiratory muscle force. Diaphragm: Anatomy is placed here to listen for P2 and pulmonary flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure murmurs.
The mitral area is also referred to as the apex of the heart. It is located in the fifth intercostal space, in the midclavicular line. This area should be auscultated with both the bell and the diaphragm Diaphragm The diaphragm is a large, dome-shaped muscle that separates the thoracic cavity from the abdominal cavity. The diaphragm consists of muscle fibers and a large central tendon, which is divided into right and left parts. As the primary muscle of inspiration, the diaphragm contributes 75% of the total inspiratory muscle force. Diaphragm: Anatomy of the stethoscope. Low-pitched sounds, such as the diastolic murmur of mitral stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) and the third heart sound, can be better appreciated with the bell. The diaphragm Diaphragm The diaphragm is a large, dome-shaped muscle that separates the thoracic cavity from the abdominal cavity. The diaphragm consists of muscle fibers and a large central tendon, which is divided into right and left parts. As the primary muscle of inspiration, the diaphragm contributes 75% of the total inspiratory muscle force. Diaphragm: Anatomy can be used to detect high-pitched sounds, such as the fourth heart sound and mitral regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD).
The tricuspid area is located at the left sternal border in the fourth and fifth intercostal spaces Intercostal spaces Chest Wall: Anatomy. The diaphragm Diaphragm The diaphragm is a large, dome-shaped muscle that separates the thoracic cavity from the abdominal cavity. The diaphragm consists of muscle fibers and a large central tendon, which is divided into right and left parts. As the primary muscle of inspiration, the diaphragm contributes 75% of the total inspiratory muscle force. Diaphragm: Anatomy is placed at this site to listen for tricuspid regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD).
Erb’s point is located at the third intercostal space along the left sternal border, one intercostal space below the pulmonic area. It is the midpoint between the base and apex of the heart. Both the S1 S1 Heart Sounds and S2 S2 Heart Sounds sounds can be heard here, and all other heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds. It is often used to quickly assess heart rate Heart rate The number of times the heart ventricles contract per unit of time, usually per minute. Cardiac Physiology and determine if there is a pulse deficit (when not all heartbeats reach the periphery, e.g., in atrial fibrillation Atrial fibrillation Atrial fibrillation (AF or Afib) is a supraventricular tachyarrhythmia and the most common kind of arrhythmia. It is caused by rapid, uncontrolled atrial contractions and uncoordinated ventricular responses. Atrial Fibrillation, detected by simultaneously palpating the radial pulse). Aortic regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) is also heard best here (if not due to aortic root dilatation).
Radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma
Know that even when a murmur is heard more clearly in a specific location, it might not always help determine its origin because a murmur can radiate away its site of origin. For example, a mitral regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) ( MR MR Calculated as the ratio of the total number of people who die due to all causes over a specific time period to the total number of people in the selected population. Measures of Health Status) murmur is best heard in the mitral area, but it may also be heard anywhere else on the chest. The murmur of MR MR Calculated as the ratio of the total number of people who die due to all causes over a specific time period to the total number of people in the selected population. Measures of Health Status is also characterized by its radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma to the left axilla Axilla The axilla is a pyramid-shaped space located between the upper thorax and the arm. The axilla has a base, an apex, and 4 walls (anterior, medial, lateral, posterior). The base of the pyramid is made up of the axillary skin. The apex is the axillary inlet, located between the 1st rib, superior border of the scapula, and clavicle. Axilla and Brachial Plexus: Anatomy. The systolic ejection murmur of aortic valve Aortic valve The valve between the left ventricle and the ascending aorta which prevents backflow into the left ventricle. Heart: Anatomy origin characteristically radiates to the neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess/ carotid arteries Carotid Arteries Either of the two principal arteries on both sides of the neck that supply blood to the head and neck; each divides into two branches, the internal carotid artery and the external carotid artery. Carotid Arterial System: Anatomy.
Dynamic Maneuvers
Performing dynamic maneuvers means altering heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds by changing circulatory hemodynamics Hemodynamics The movement and the forces involved in the movement of the blood through the cardiovascular system. Vascular Resistance, Flow, and Mean Arterial Pressure. These can distinguish the clinical cause of similar auscultatory findings and are frequently tested on board exams. It is essential to understand the physiologic alterations produced by certain maneuvers.
If a murmur is heard, various dynamic maneuver tests can characterize it further. These maneuvers alter circulatory hemodynamics Hemodynamics The movement and the forces involved in the movement of the blood through the cardiovascular system. Vascular Resistance, Flow, and Mean Arterial Pressure and, in doing so, change the emphasis with different murmurs.
Respiration Respiration The act of breathing with the lungs, consisting of inhalation, or the taking into the lungs of the ambient air, and of exhalation, or the expelling of the modified air which contains more carbon dioxide than the air taken in. Nose Anatomy (External & Internal) can be used to differentiate between right-sided and left-sided murmurs. Inspiration Inspiration Ventilation: Mechanics of Breathing has the effect of increasing venous return, and as there is an increase in blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure to the right side of the heart, right-sided murmurs are accentuated. On the other hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy, expiration Expiration Ventilation: Mechanics of Breathing causes left-sided murmurs to become louder.
Another respiratory maneuver is deep expiration Expiration Ventilation: Mechanics of Breathing. As the patient leans forward and is in deep expiration Expiration Ventilation: Mechanics of Breathing, the base of the heart is brought closer to the chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy. In this maneuver, the murmur of aortic regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD), not caused by a dilated aortic root, can be appreciated at Erb’s point, which is the point between the base and the apex of the heart.
- The Valsalva Maneuver Valsalva maneuver Forced expiratory effort against a closed glottis. Rectal Prolapse
This is a well-known and often-used dynamic maneuver involving forcible exhalation against a closed glottis Glottis The vocal apparatus of the larynx, situated in the middle section of the larynx. Glottis consists of the vocal folds and an opening (rima glottidis) between the folds. Larynx: Anatomy after full inspiration Inspiration Ventilation: Mechanics of Breathing for 10-20 seconds, causing increased intrathoracic pressure.[21]The normal systolic blood pressure ( SBP SBP Ascites) response follows four phases (two phases while the glottis Glottis The vocal apparatus of the larynx, situated in the middle section of the larynx. Glottis consists of the vocal folds and an opening (rima glottidis) between the folds. Larynx: Anatomy is closed and two after the start of breathing normally):
Phase I (onset of the strain phase) is a very short phase at the start of the maneuver. The intrathoracic pressure increases, causing an increase in cardiac output Cardiac output The volume of blood passing through the heart per unit of time. It is usually expressed as liters (volume) per minute so as not to be confused with stroke volume (volume per beat). Cardiac Mechanics and blood pressure (due to compression Compression Blunt Chest Trauma). There is also a pressure increase in the chest and abdomen blood vessels (including the superior and inferior vena cavae) and the cardiac chambers. This increase in pressure is associated with a reciprocal decrease in heart rate Heart rate The number of times the heart ventricles contract per unit of time, usually per minute. Cardiac Physiology due to the baroreceptor reflex Baroreceptor reflex A response by the baroreceptors to increased blood pressure. Increased pressure stretches blood vessels which activates the baroreceptors in the vessel walls. The net response of the central nervous system is a reduction of central sympathetic outflow. This reduces blood pressure both by decreasing peripheral vascular resistance and by lowering cardiac output. Because the baroreceptors are tonically active, the baroreflex can compensate rapidly for both increases and decreases in blood pressure. Vascular Resistance, Flow, and Mean Arterial Pressure.
Phase II (continued strain): SBP SBP Ascites decreases to below baseline due to decreased venous return as the strain is maintained. Most murmurs become softer, but the systolic murmur of hypertrophic cardiomyopathy Hypertrophic Cardiomyopathy Hypertrophic cardiomyopathy (HCM) is the most commonly inherited cardiomyopathy, which is characterized by an asymmetric increase in thickness (hypertrophy) of the left ventricular wall, diastolic dysfunction, and often left ventricular outflow tract obstruction. Hypertrophic Cardiomyopathy increases and the murmur of mitral valve Mitral valve The valve between the left atrium and left ventricle of the heart. Heart: Anatomy prolapse is heard. Heart rate Heart rate The number of times the heart ventricles contract per unit of time, usually per minute. Cardiac Physiology increases due to the baroreceptor response (reflex) to a decreased SBP SBP Ascites.
Phase III (“release phase” = normal breathing starts): Very short phase characterized by a rapid drop in SBP SBP Ascites and decreased left ventricular volume due to decreased intrathoracic pressure, which may cause syncope Syncope Syncope is a short-term loss of consciousness and loss of postural stability followed by spontaneous return of consciousness to the previous neurologic baseline without the need for resuscitation. The condition is caused by transient interruption of cerebral blood flow that may be benign or related to a underlying life-threatening condition. Syncope or pre-syncope/ dizziness Dizziness An imprecise term which may refer to a sense of spatial disorientation, motion of the environment, or lightheadedness. Lateral Medullary Syndrome (Wallenberg Syndrome). Right-sided murmurs are louder for a short interval. The heart rate Heart rate The number of times the heart ventricles contract per unit of time, usually per minute. Cardiac Physiology increases due to the baroreceptor reflex Baroreceptor reflex A response by the baroreceptors to increased blood pressure. Increased pressure stretches blood vessels which activates the baroreceptors in the vessel walls. The net response of the central nervous system is a reduction of central sympathetic outflow. This reduces blood pressure both by decreasing peripheral vascular resistance and by lowering cardiac output. Because the baroreceptors are tonically active, the baroreflex can compensate rapidly for both increases and decreases in blood pressure. Vascular Resistance, Flow, and Mean Arterial Pressure.
Phase IV (recovery or “ overshoot Overshoot Membrane Potential” phase): SBP SBP Ascites increases due to reflex sympathetic activation and increased stroke volume Stroke volume The amount of blood pumped out of the heart per beat, not to be confused with cardiac output (volume/time). It is calculated as the difference between the end-diastolic volume and the end-systolic volume. Cardiac Cycle. Heart rate Heart rate The number of times the heart ventricles contract per unit of time, usually per minute. Cardiac Physiology decreases due to the baroreceptor reflex Baroreceptor reflex A response by the baroreceptors to increased blood pressure. Increased pressure stretches blood vessels which activates the baroreceptors in the vessel walls. The net response of the central nervous system is a reduction of central sympathetic outflow. This reduces blood pressure both by decreasing peripheral vascular resistance and by lowering cardiac output. Because the baroreceptors are tonically active, the baroreflex can compensate rapidly for both increases and decreases in blood pressure. Vascular Resistance, Flow, and Mean Arterial Pressure.
The Valsalva maneuver Valsalva maneuver Forced expiratory effort against a closed glottis. Rectal Prolapse accentuates the murmurs of hypertrophic cardiomyopathy Hypertrophic Cardiomyopathy Hypertrophic cardiomyopathy (HCM) is the most commonly inherited cardiomyopathy, which is characterized by an asymmetric increase in thickness (hypertrophy) of the left ventricular wall, diastolic dysfunction, and often left ventricular outflow tract obstruction. Hypertrophic Cardiomyopathy and mitral valve Mitral valve The valve between the left atrium and left ventricle of the heart. Heart: Anatomy prolapse when listening at the left sternal edge.
- Squatting
Squatting is another dynamic maneuver that causes an increase in venous return. The patient quickly moves from a standing position to a squat in this test. This makes the murmurs of aortic stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) and mitral regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) louder, but the murmurs of hypertrophic cardiomyopathy Hypertrophic Cardiomyopathy Hypertrophic cardiomyopathy (HCM) is the most commonly inherited cardiomyopathy, which is characterized by an asymmetric increase in thickness (hypertrophy) of the left ventricular wall, diastolic dysfunction, and often left ventricular outflow tract obstruction. Hypertrophic Cardiomyopathy and mitral valve Mitral valve The valve between the left atrium and left ventricle of the heart. Heart: Anatomy prolapse become softer and shorter. When the patient does the opposite and stands quickly from a squatting position, then the opposite changes in murmurs occur.
- Isometric Exercise
Isometric exercise can also be used for eliciting certain types of murmurs. For this exercise, the patient sustains a handgrip for half a minute. This exercise increases afterload Afterload Afterload is the resistance in the aorta that prevents blood from leaving the heart. Afterload represents the pressure the LV needs to overcome to eject blood into the aorta. Cardiac Mechanics (or peripheral resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing). The murmur of mitral regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) is accentuated. The murmur of aortic stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) and hypertrophic cardiomyopathy Hypertrophic Cardiomyopathy Hypertrophic cardiomyopathy (HCM) is the most commonly inherited cardiomyopathy, which is characterized by an asymmetric increase in thickness (hypertrophy) of the left ventricular wall, diastolic dysfunction, and often left ventricular outflow tract obstruction. Hypertrophic Cardiomyopathy becomes softer, while the murmur of mitral valve Mitral valve The valve between the left atrium and left ventricle of the heart. Heart: Anatomy prolapse becomes shorter.
Summary Table
| Heart Sound | Causes |
| Normal Heart Sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds | |
| First heart sound ( S1 S1 Heart Sounds) | Closure of the mitral and tricuspid valves |
| Second heart sound ( S2 S2 Heart Sounds) | Closure of the aortic and pulmonary valves |
| Extra Heart Sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds | |
| Third heart sound ( S3 S3 Heart Sounds) | A physiological S3 S3 Heart Sounds is caused by rapid diastolic filling (e.g., pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care, thyrotoxicosis Thyrotoxicosis A hypermetabolic syndrome caused by excess thyroid hormones which may come from endogenous or exogenous sources. The endogenous source of hormone may be thyroid hyperplasia; thyroid neoplasms; or hormone-producing extrathyroidal tissue. Thyrotoxicosis is characterized by nervousness; tachycardia; fatigue; weight loss; heat intolerance; and excessive sweating. Thyrotoxicosis and Hyperthyroidism, and sometimes in children). A pathological S3 S3 Heart Sounds is caused by reduced compliance Compliance Distensibility measure of a chamber such as the lungs (lung compliance) or bladder. Compliance is expressed as a change in volume per unit change in pressure. Veins: Histology of the left ventricle (e.g., left ventricular failure, aortic regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD), mitral regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD), patent ductus arteriosus Ductus arteriosus A fetal blood vessel connecting the pulmonary artery with the descending aorta. Patent Ductus Arteriosus (PDA), and a ventricular septal defect Ventricular Septal Defect Tetralogy of Fallot) or reduced compliance Compliance Distensibility measure of a chamber such as the lungs (lung compliance) or bladder. Compliance is expressed as a change in volume per unit change in pressure. Veins: Histology of the right ventricle (right ventricular failure, constrictive pericarditis Constrictive pericarditis Inflammation of the pericardium that is characterized by the fibrous scarring and adhesion of both serous layers, the visceral pericardium and the parietal pericardium leading to the loss of pericardial cavity. The thickened pericardium severely restricts cardiac filling. Clinical signs include fatigue, muscle wasting, and weight loss. Pericarditis). |
| Fourth heart sound ( S4 S4 Heart Sounds) | Decreased ventricular compliance Compliance Distensibility measure of a chamber such as the lungs (lung compliance) or bladder. Compliance is expressed as a change in volume per unit change in pressure. Veins: Histology of the left ventricle (aortic stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), mitral regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD), hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, angina, myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction) or the right ventricle ( pulmonary hypertension Pulmonary Hypertension Pulmonary hypertension (PH) or pulmonary arterial hypertension (PAH) is characterized by elevated pulmonary arterial pressure, which can lead to chronic progressive right heart failure. Pulmonary hypertension is grouped into 5 categories based on etiology, which include primary PAH, and PH due to cardiac disease, lung or hypoxic disease, chronic thromboembolic disease, and multifactorial or unclear etiologies. Pulmonary Hypertension, pulmonary stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS)) |
| Systolic Murmurs Systolic Murmurs Heart murmurs which are systolic in timing. They occur between the first and the second heart sounds, between the closure of mitral valve and tricuspid valve and the closure of semilunar aortic and pulmonary valves. Systolic murmurs include ejection murmurs and regurgitant murmurs. Heart Sounds | |
| Midsystolic murmur | Increased flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure through a normal valve (physiologic or innocent murmur), aortic stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), pulmonary stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), hypertrophic cardiomyopathy Hypertrophic Cardiomyopathy Hypertrophic cardiomyopathy (HCM) is the most commonly inherited cardiomyopathy, which is characterized by an asymmetric increase in thickness (hypertrophy) of the left ventricular wall, diastolic dysfunction, and often left ventricular outflow tract obstruction. Hypertrophic Cardiomyopathy, atrial septal defect Atrial Septal Defect Atrial septal defects (ASDs) are benign acyanotic congenital heart defects characterized by an opening in the interatrial septum that causes blood to flow from the left atrium (LA) to the right atrium (RA) (left-to-right shunt). Atrial Septal Defect (ASD) |
| Late systolic murmur | Mitral regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) ( MR MR Calculated as the ratio of the total number of people who die due to all causes over a specific time period to the total number of people in the selected population. Measures of Health Status), due to papillary muscle dysfunction, mitral valve Mitral valve The valve between the left atrium and left ventricle of the heart. Heart: Anatomy prolapse, or infective endocarditis Infective endocarditis Infective endocarditis (IE) is caused by infection or inflammation of the inner lining of the heart (endocardium), most commonly affecting the heart valves. Endocarditis |
| Pansystolic murmur Pansystolic Murmur Transposition of the Great Vessels | Mitral regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD), tricuspid regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD), ventricular septal defect Ventricular Septal Defect Tetralogy of Fallot (VSD), aortopulmonary shunts |
| Diastolic murmurs Diastolic Murmurs Heart Sounds | |
| Early diastolic murmur | Aortic regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD), pulmonary regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) |
| Mid-diastolic murmur | Mitral stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), tricuspid stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), atrial myxoma Myxoma A benign neoplasm derived from connective tissue, consisting chiefly of polyhedral and stellate cells that are loosely embedded in a soft mucoid matrix, thereby resembling primitive mesenchymal tissue. It occurs frequently intramuscularly where it may be mistaken for a sarcoma. It appears also in the jaws and the skin. Cardiac Myxoma (rare), acute rheumatic fever Rheumatic fever Acute rheumatic fever (ARF) is an autoimmune inflammatory process that usually follows Streptococcal pharyngitis. Acute rheumatic fever usually occurs 2-4 weeks after an untreated infection and affects the heart, skin, joints, and nervous system. Rheumatic Fever murmur (Carey Coombs murmur of mitral valvulitis Valvulitis Rheumatic Fever) |
| Other | |
| Presystolic murmur | Mitral stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), tricuspid stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), atrial myxoma Myxoma A benign neoplasm derived from connective tissue, consisting chiefly of polyhedral and stellate cells that are loosely embedded in a soft mucoid matrix, thereby resembling primitive mesenchymal tissue. It occurs frequently intramuscularly where it may be mistaken for a sarcoma. It appears also in the jaws and the skin. Cardiac Myxoma |
| Continuous murmur | Patent ductus arteriosus Ductus arteriosus A fetal blood vessel connecting the pulmonary artery with the descending aorta. Patent Ductus Arteriosus (PDA), arteriovenous fistula Arteriovenous fistula An abnormal direct communication between an artery and a vein without passing through the capillaries. An a-v fistula usually leads to the formation of a dilated sac-like connection, arteriovenous aneurysm. The locations and size of the shunts determine the degree of effects on the cardiovascular functions such as blood pressure and heart rate. Vascular Surgery, venous hum |
Review Questions
- Where is the murmur of aortic
regurgitation
Regurgitation
Gastroesophageal Reflux Disease (GERD) heard best?
- At the left lower sternal border, with the patient in the left lateral decubitus position, after a short period of exercise
- At the right upper sternal border during systole Systole Period of contraction of the heart, especially of the heart ventricles. Cardiac Cycle and in the carotid arteries Carotid Arteries Either of the two principal arteries on both sides of the neck that supply blood to the head and neck; each divides into two branches, the internal carotid artery and the external carotid artery. Carotid Arterial System: Anatomy to assess for radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma
- At the left lower sternal border, with the patient sitting up, leaning forward, and holding their breath after expiration Expiration Ventilation: Mechanics of Breathing
- At the left lower sternal border, augmented by Valsalva maneuver Valsalva maneuver Forced expiratory effort against a closed glottis. Rectal Prolapse
- What distinguishes a grade 6 murmur from other grades in the Levine System?
- It is a murmur that is soft and difficult to hear.
- It can be heard without direct placement of the stethoscope.
- It has a palpable thrill accompanying it.
- It can only be heard by someone experienced in auscultation.
- What is the cause of the physiological
splitting
Splitting
Defense Mechanisms of the second heart sound?
- Closure of the mitral and tricuspid valves just before ventricular systole Ventricular systole Cardiac Cycle.
- Increase in venous return during inspiration Inspiration Ventilation: Mechanics of Breathing, causing the aortic valves to remain open for longer.
- Aortic regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) with retrograde leakage through the valve during diastole Diastole Post-systolic relaxation of the heart, especially the heart ventricles. Cardiac Cycle
- Delayed closure Delayed Closure Gastroschisis of the pulmonic valve due to lower pressures in the pulmonary circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment and increased venous return during inspiration Inspiration Ventilation: Mechanics of Breathing.
Answers: 1C, 2B, 3D
References
- Seitz, M.P., Minhas, S., Khouzam, A., Khouzam, N., & Harper, Y. (2021). The Face Is the Mirror of the Soul. The Cardiovascular Physical Exam Is Not Yet Dead. Current problems in cardiology, 46(3), 100644.
- Ogedegbe, G., & Pickering, T. (2010). Principles and techniques of blood pressure measurement. Cardiology clinics, 28(4), 571-86.
- Ceglowska. K, et al AL Amyloidosis. (2015). Bilateral Macular Roth Spots Roth spots Endocarditis as a Manifestation of Subacute Endocarditis Endocarditis Endocarditis is an inflammatory disease involving the inner lining (endometrium) of the heart, most commonly affecting the cardiac valves. Both infectious and noninfectious etiologies lead to vegetations on the valve leaflets. Patients may present with nonspecific symptoms such as fever and fatigue. Endocarditis. Case Reports in Ophthalmological Medicine, https://doi.org/10.1155/2015/493947
- Pandian, JD, Sebastian, IA, & Sidhu, A. (2019). Acute ischemic stroke Ischemic Stroke An ischemic stroke (also known as cerebrovascular accident) is an acute neurologic injury that occurs as a result of brain ischemia; this condition may be due to cerebral blood vessel occlusion by thrombosis or embolism, or rarely due to systemic hypoperfusion. Ischemic Stroke in secondary polycythemia Secondary Polycythemia Polycythemia Vera due to complex congenital cyanotic heart disease. BMJ case reports, 12(10), e231261.
- Long, B, & Koyfman, A. (2018). Infectious endocarditis Endocarditis Endocarditis is an inflammatory disease involving the inner lining (endometrium) of the heart, most commonly affecting the cardiac valves. Both infectious and noninfectious etiologies lead to vegetations on the valve leaflets. Patients may present with nonspecific symptoms such as fever and fatigue. Endocarditis: An update for emergency clinicians. The American journal of emergency medicine, 36(9), 1686-92.
- Siddall, E, Khatri, M, & Radhakrishnan, J. (2017). Capillary leak syndrome Capillary leak syndrome A condition characterized by recurring episodes of fluid leaking from capillaries into extravascular compartments causing hematocrit to rise precipitously. If not treated, generalized vascular leak can lead to generalized edema; shock; cardiovascular collapse; and multiple organ failure. Hematopoietic Growth Factors: etiologies, pathophysiology, and management. Kidney International, 92(1), 37-46.
- Besharat, S, Grol-Prokopczyk, H, Gao, S, Feng, C, Akwaa, F, & Gewandter, JS. (2021). Peripheral edema Peripheral edema Peripheral edema is the swelling of the lower extremities, namely, legs, feet, and ankles. Edema: A common and persistent health problem for older Americans. PloS one, 16(12), e0260742.
- Williams, K, Han, M, Hardin, S, George, S, & Yao, J. (2018). AERO: An Objective Peripheral Edema Peripheral edema Peripheral edema is the swelling of the lower extremities, namely, legs, feet, and ankles. Edema Measurement Device. Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual International Conference, 2018, 5914-7.
- Padilla-Ortiz, AL AL Amyloidosis, & Ibarra, D. (2018). Lung and Heart Sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds Analysis: State-of-the-Art and Future Trends. Critical reviews in biomedical engineering, 46(1), 33-52.
- Flint, N., Wunderlich, N.C., Shmueli, H., Ben-Zekry, S., Siegel, R.J., & Beigel, R. (2019). Aortic Regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD). Current cardiology reports, 21(7), 65.
- Akinseye, OA OA Osteoarthritis (OA) is the most common form of arthritis, and is due to cartilage destruction and changes of the subchondral bone. The risk of developing this disorder increases with age, obesity, and repetitive joint use or trauma. Patients develop gradual joint pain, stiffness lasting < 30 minutes, and decreased range of motion. Osteoarthritis, Pathak, A, & Ibebuogu, UN (2018). Aortic Valve Aortic valve The valve between the left ventricle and the ascending aorta which prevents backflow into the left ventricle. Heart: Anatomy Regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD): A Comprehensive Review. Current problems in cardiology, 43(8), 315-34.
- Chen, W, et al AL Amyloidosis. (2021). Deep Learning Methods for Heart Sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds Classification: A Systematic Review. Entropy Entropy The measure of that part of the heat or energy of a system which is not available to perform work. Entropy increases in all natural (spontaneous and irreversible) processes. Enzyme Kinetics (Basel, Switzerland), 23(6), 667.
- Plesinger, F, et al AL Amyloidosis.(2017). Heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds analysis using probability Probability Probability is a mathematical tool used to study randomness and provide predictions about the likelihood of something happening. There are several basic rules of probability that can be used to help determine the probability of multiple events happening together, separately, or sequentially. Basics of Probability assessment. Physiological measurement, 38(8), 1685-700.
- Sato, Y, Kawasaki, T, Honda, et al AL Amyloidosis. (2018). Third and Fourth Heart Sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds and Myocardial Fibrosis Fibrosis Any pathological condition where fibrous connective tissue invades any organ, usually as a consequence of inflammation or other injury. Bronchiolitis Obliterans in Hypertrophic Cardiomyopathy Hypertrophic Cardiomyopathy Hypertrophic cardiomyopathy (HCM) is the most commonly inherited cardiomyopathy, which is characterized by an asymmetric increase in thickness (hypertrophy) of the left ventricular wall, diastolic dysfunction, and often left ventricular outflow tract obstruction. Hypertrophic Cardiomyopathy. Circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment journal: official journal of the Japanese Circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment Society, 82(2), 509-16.
- Soto-Murillo, MA, Galván-Tejada, JI, et al AL Amyloidosis. (2021). Automatic Evaluation of Heart Condition According to the Sounds Emitted and Implementing Six Classification Methods. Healthcare (Basel, Switzerland), 9(3), 317.
- Abdollahpur, M, Ghaffari, A, Ghiasi, S, & Mollakazemi, MJ (2017). Detection of pathological heart sounds Heart sounds Heart sounds are brief, transient sounds produced by valve opening and closure and by movement of blood in the heart. They are divided into systolic and diastolic sounds. In most cases, only the first (S1) and second (S2) heart sounds are heard. These are high-frequency sounds and arise from aortic and pulmonary valve closure (S1), as well as mitral and tricuspid valve closure (S2). Heart Sounds. Physiological measurement, 38(8), 1616-30.
- Montinari, MR MR Calculated as the ratio of the total number of people who die due to all causes over a specific time period to the total number of people in the selected population. Measures of Health Status, & Minelli, S. (2019). The first 200 years of cardiac auscultation and future perspectives. Journal of multidisciplinary healthcare, 12, 183-9.
- Wang, J., You, T., Yi, K., et al AL Amyloidosis. (2020). Intelligent Diagnosis of Heart Murmurs Heart murmurs Heart sounds caused by vibrations resulting from the flow of blood through the heart. Heart murmurs can be examined by heart auscultation, and analyzed by their intensity (6 grades), duration, timing (systolic, diastolic, or continuous), location, transmission, and quality (musical, vibratory, blowing, etc). Heart Sounds in Children with Congenital Heart Disease. Journal of healthcare engineering, 2020, 9640821.
- Hoffman, JI (2018). The challenge in diagnosing coarctation of the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy. Cardiovascular journal of Africa, 29(4), 252-5.
- Austin, AV., Owens, et al AL Amyloidosis. (2022). Do “pathologic” cardiac murmurs in adolescents identify structural heart disease? An evaluation of 15,141 active adolescents for conditions that put them at risk of sudden cardiac death Sudden cardiac death Cardiac arrest is the sudden, complete cessation of cardiac output with hemodynamic collapse. Patients present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation/tachycardia, asystole, or pulseless electrical activity. Cardiac Arrest. British journal of sports medicine, 56(2), 88-94.
- Shindler, DM DM Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus. (2018). Effect of the Valsalva Maneuver Valsalva maneuver Forced expiratory effort against a closed glottis. Rectal Prolapse on the Second Heart Sound. Cardiology, 139(3), 159-60.
- Power, J.E., Toft, L.E.B., & Barrett, M. (2020). The Murmur Online Learning Experience ( MOLE Mole Nevi (singular nevus), also known as "moles," are benign neoplasms of the skin. Nevus is a non-specific medical term because it encompasses both congenital and acquired lesions, hyper- and hypopigmented lesions, and raised or flat lesions. Nevus/Nevi) Curriculum Improves Medical Students’ Ability to Correctly Identify Cardiac Murmurs. MedEdPORTAL: the journal of teaching and learning resources, 16, 10904.