Tension Pneumothorax: Want to get something off your chest?
When covering the subject of chest injuries, pre-hospital treatment of a Tension Pneumothorax is a popular subject in remote medical classrooms, with instructors classically looking for a response from students centred around the textbook landmarks, ‘Mid-clavicular line, second intercostal space, just above the third rib’. However, in reality this invasive but potentially life-saving procedure isn’t as straightforward as citing a textbook and can be quite harrowing for the medic not practised in its use.
A Tension what?
Air (Pneumo) in the chest (thorax) under tension often occurs due to thoracic trauma (impact or penetration to the chest wall) but may be also present in a medical patient such as an asthmatic. Air leaks from the lung into the pleural cavity (the thin fluid filled space around the lung) when the patient breathes in, but is unable to escape when the patient breathes out due to what is quite often a one-way valve created by the lung tissue.
That rings a bell.
Normally referred to by the layman as a collapsed lung, Tension Pneumothorax is often thought of as a respiratory problem, the this is not the case. In actual fact, the human body can adequately compensate for the absence of one lung as has been proven in cancer patients. The current pontiff, Pope Francis, had a lung removed after an infection as a teenager. The problem with a Tension Pneumothorax lies with increased pressure in the chest (intra-thoracic pressure) as each inspiratory breath leads to air in the pleural space. As this builds, the heart and its vessels become restricted, leading to circulatory collapse.
How do I diagnose Tension Pneumothorax ?
There are plenty of signs and symptoms that may assist you in your diagnosis. Chest pain and respiratory distress will probably be present in a conscious patient along with an elevated heart rate (tachycardia) as it works harder under pressure to pump blood around the body. Associated with this may be an extended capillary refill time (CRT) and reduced saturation on your pulse-oximeter.
Patient deterioration can be rapid and you may feel resistance when ventilating with a bag-valve mask. The affected side of the chest may not be moving as much as the unaffected side (assuming it is a unit-lateral pneumothorax), decreased breath sounds when using a stethoscope and the affected side of the chest may be appear over-inflated. Percussion might lead to what is referred to as hyper-resonance (think a taught skin over a cavity of air sounding like a drum). However, the Royal College of Surgeons (Edinburgh) and a paper written in the Emergency Medical Journal consider this to be rare.
Time to act.
Restriction to venous return to the heart leads to hypotension (low blood pressure) and distension (enlargement) of the jugular veins in the neck along with the rare occurrence of deviation of the trachea towards the unaffected side. These are very late signs and may be a warning that your patient is about to arrest.
What do I do?
Although commercial decompression needles such as the Air Release System (ARS) and ThoraQuick devices have been introduced, using a 14G cannula to get that air out of the chest is still a recognised method. The problem lies with finding where to insert it using surface anatomy on a patient with even a suggestion of an increased Body Mass Index (BMI).
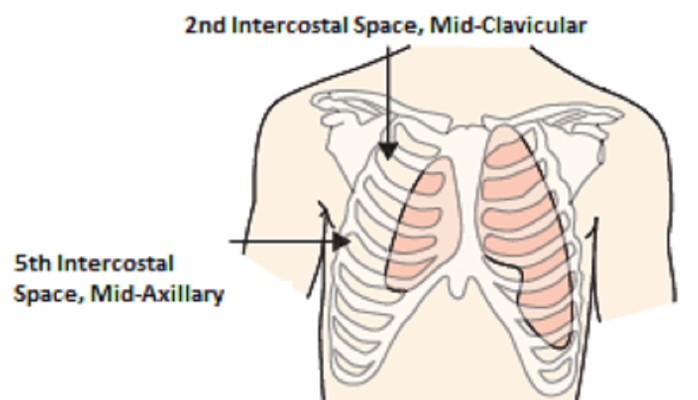
The traditional method takes a line from the centre of the clavicle (mid-clavicular line) on the affected side of the chest down to where you can feel the space between the second and third ribs (second intercostal space) and inserting the cannula above the third rib to avoid the neurovascular bundle (nerve and blood vessel) that supplies the intercostal muscle itself. Aspiration (drawing back on) of the syringe on insertion should mitigate blockage of the cannula and indicate to the practitioner they are in the pleural space. If this doesn’t work, flushing with 2ml of air or water can clear it.
Another method of finding this landmark can be to use the Angle of Louis on the sternum (the joint formed by the articulation of the manubrium and the body of the sternum) and draw a horizontal line across the chest wall to see where it would intersect with a vertical line from the male nipple (in a ‘normally’ shaped gentleman).
If this doesn’t work, the Royal College of Surgeons advocates a second attempt (with the correct training) just anterior (towards the front of the body) to the mid-axillary line (a line running down the side of the body from the centre of the armpit) at the fifth intercostal space. This site is arguably easier to find due to reduced chest wall thickness.
So, in a nutshell...
- Diagnose a Tension Pneumothorax;
- Prepare your equipment (alcohol wipe, decompression needle or 14G cannula, syringe);
- Find your insertion landmarks (2nd Intercostal Space, Mid-Clavicular or 5th Intercostal Space, Mid-Axillary);
- Clean the area of skin;
- Insert the needle just above the lower rib;
- When air is aspirated into the syringe, advance the cannula;
- Withdraw the needle and feel/listen for hiss of air;
- Secure the cannula; and
- Reassess the patient.
Some might insist on using an Asherman or Bolin chest seal to secure the cannula (which has now effectively turned a closed chest wound into an open one) but bear in mind that this might impede access to the cannula if it becomes blocked or insertion of another cannula at the same site. Other treatment methods include Thoracostomy (incision of the chest wall for drainage) and chest drain insertion but these are generally reserved for Level 6 PHEM practitioners.
Did you find this useful? Check out the Medsec 7 blog for more emergency medical tutorials covering drowning, pelvic injury and Epiglottis.
For more information on what pre-hospital medical courses Medsec 7 offers visit our website at www.medsec7.com or email our Clinical Lead: adambrind@medsec7.com.