VIRUSES AND FUNGI ASSOCIATED WITH RESPIRATORY TRACT INFECTION
CHAPTER ONE
VIRUSES ASSOCIATED WITH RESPIRATORY TRACT INFECTION
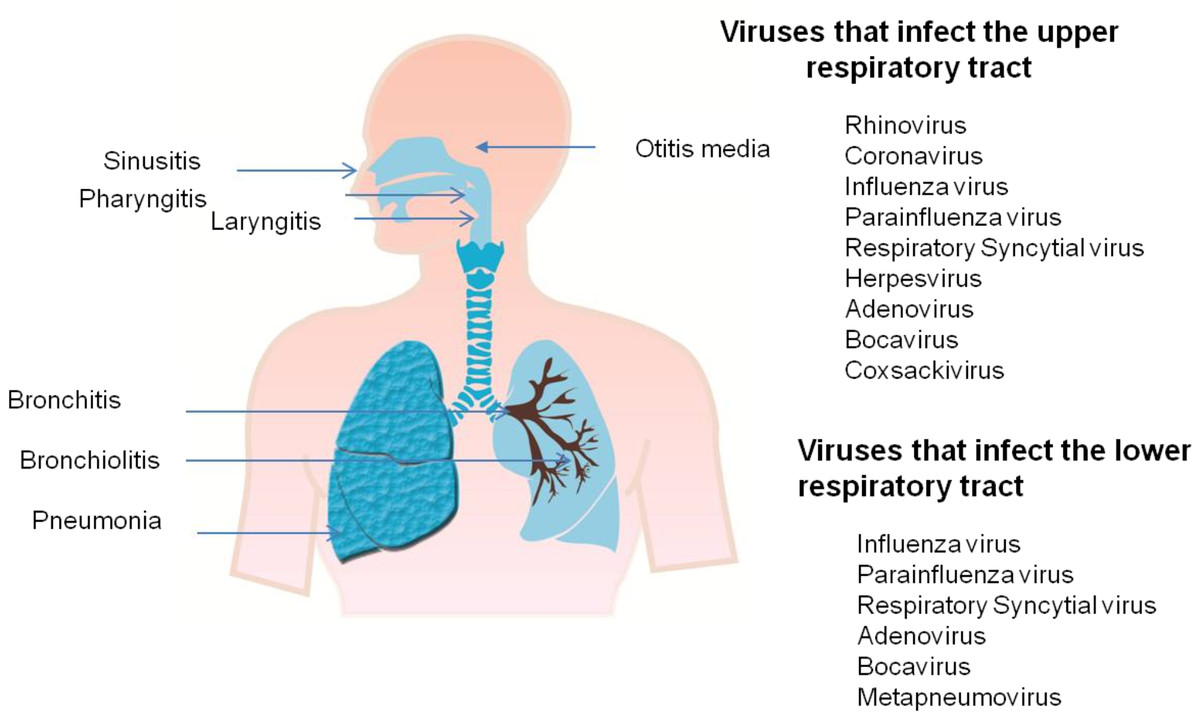
The respiratory tract is made up of the upper and lower respiratory parts. The upper respiratory system includes the nose, nasal cavity, pharynx, and larynx with subglottic area of trachea. In the normal circumstances, air enters the respiratory system through nostrils where it is filtered, humidified, and warmed inside the nasal cavity. Conditioned air passes through pharynx, larynx, and trachea and then enters in lower respiratory system. Dysfunction of any part of upper respiratory tract may change quality of inhaled air and consequently, may impair function of tracheobronchial tree and lung.
Upper respiratory tract infections are the most common infections in the population. They are the leading cause for people missing work or school and, thus, have important social implications. They range from mild, self-limiting disease like common cold, syndrome of the nasopharynx to serious, life-threatening illnesses, such as epiglottitis. Most of these infections are of viral origin, involving more or less all the parts of upper respiratory system and associated structures, such as paranasal sinuses and middle ear. Common upper respiratory tract infections include rhinitis (inflammation of the nasal mucosa), rhinosinusitis or sinusitis (inflammation of the nares and paranasal sinuses, including frontal, ethmoid, maxillary, and sphenoid), nasopharyngitis (rhinopharyngitis or the common cold—inflammation of the nares pharynx, hypopharynx, uvula, and tonsils), pharyngitis (inflammation of the pharynx, hypopharynx, uvula, and tonsils), epiglottitis (inflammation of the superior portion of the larynx and supraglottic area), laryngitis (inflammation of the larynx), laryngotracheitis (inflammation of the larynx, trachea, and subglottic area), and tracheitis (inflammation of the trachea and subglottic area).
In most cases, these diseases are self-limiting and can be managed at home. The more severe cases or those with complications need to seek medical help. In general, symptomatic therapy is sufficient (analgesics, antipyretics, anticholinergic agents, antihistamines, antitussives, adrenergic agonists, corticosteroids, decongestants), in some instances antibiotics, or some traditional way of cure are also used. Rarely, surgical intervention or in most serious cases, care in the intensive care unit (ICU) is necessary.
Acute Viral Pharyngitis
Pharyngitis is caused by inflammation and swelling of pharyngeal mucosa. The main symptom of acute pharyngitis is a sore throat. Similar to other upper respiratory infections, the most common cause of acute pharyngitis is a viral infection in settings of common cold or flu. The most common pathogens are rhinovirus, and influenza A and B. Some other viruses can cause specific forms of pharyngitis, such as enteroviruses, Epstein-Barr virus (EBV), and HIV. Herpangina is a painful pharyngitis caused by various enteroviruses like Coxsackie virus A16, Coxsackie virus B, enterovirus 71, echovirus, parechovirus 1, adenovirus, and herpes simplex virus.
Laryngitis
Laryngitis is an acute or chronic inflammation of laryngeal structures. Rhinovirus, Influenza A, B, C, Adenoviruses, Parainfluenza viruses, RSV, Measles, Varicella-zoster are implicated as causative organisms for laryngitis.
The major viruses implicated in both upper and lower respiratory tract infections include:
1) Picornaviruses
The family of Picornaviruses is a group of small, nonenveloped viruses with single-stranded positive-sense RNA genome. The group is divided into the following Nine genera: entero-, hepato-, kobu-, parecho-, rhino-, aphto-, cardio-, erbo-, and teschoviruses. In terms of causing respiratory illnesses to humans, the most important viruses are rhino-, entero-, and parechoviruses. These three human picornaviruses are discussed in detail in the text below.
a) Rhinoviruses
Rhinoviruses are the largest group of picornaviruses, including 101 different serotypes. Rhinoviruses are the predominant cause of the common cold all over the world and in all age groups. Rhinoviruses occur relatively more often in children than in adults. The optimal temperature for growth is 33°C to 35°C in vitro, and the nose and nasopharynx are the primary sites for replication. The infectious dose for humans is very small and the infection proceeds rapidly, with the incubation period being as short as 8 to 12 hours. Inflammatory responses of the host tend to prolong symptoms of infection even after virus replication has diminished. Usually rhinovirus infection results in a mild illness characterized by a runny and stuffy nose, a sore throat, and coughing and hoarseness. Although rhinoviruses are generally thought to cause only mild upper respiratory infections, they are also associated with acute lower respiratory tract infections, wheezing, bronchiolitis, and pneumonia in children.
b) Enteroviruses
Enteroviruses are picornaviridae with three serotypic groups: poliovirus, coxsackievirus and enteric cytopathic human orphan(ECHO) virus (echovirus). Enteroviruses are unenveloped, icosahedral, positive-sense RNA viruses that encode for four proteins.
Pathogenesis
· The virus enters cells by a specific receptor that differs for different virus types, therefore defining tissue tropism.
· The virus is usually acquired via the intestinal tract, causing subsequent viraemia and invasion of reticuloendothelial cells.
· Secondary viraemia leads to invasion of target organs (e.g. meninges, spinal cord, brain or myocardium).
· Poliovirus appears to spread along nerve fibres; if significant multiplication occurs within the dorsal root ganglia, the nerve fibre may die, with resultant motor paralysis.
Epidemiology
· Enteroviruses are spread by the faecal–oral route.
· In developing countries infection occurs early in life; it occurs later in industrialized countries.
· Infection can occur in parents and carers of infants who have received the live vaccine.
Clinical features
Polio may present as a minor illness (abortive polio), as aseptic meningitis (non-paralytic polio), with lower motor neurone damage and paralysis (paralytic polio), or as a late recrudescence of muscle wasting that occurs sometimes decades after the initial paralytic polio (progressive postpoliomyelitis muscle atrophy). In paralytic polio, muscle involvement is maximal within a few days after commencement of the paralysis; recovery may occur within 6 months.
· Aseptic meningitis and, rarely, severe focal encephalitis or general infection may present in neonates.
· Herpangina, a self-limiting, painful, vesicular pharyngeal infection, is caused by some types of coxsackievirus.
· Coxsackie B causes acute myocarditis.
· Hand, foot and mouth disease is characterized by a vesicular rash of the palms, mouth and soles that heals without crusting.
Treatment and Prevention
¾ Treatment is supportive care but pleconaril shows benefit in the treatment of enteroviral meningitis. Artificial ventilation may be required in the case of polio.
¾ Two vaccines are available: the oral live attenuated Sabin and the killed parenteral Salk vaccine. Now that polio is limited to a few countries, the inactivated poliovirus vaccine (IPV) is used.
2) Respiratory syncytial viruses
Human RSV is an enveloped, single-stranded negative-sense RNA virus with two distinct serotypes, types A and B. RSV belong to the genus Pneumovirus within the family of Paramyxoviridae. RSV infections are present in all age groups, but they predominate in children and especially in infants. Treatment for RSV infection is based on symptomatic relief and humidification. Severe cases may require hospitalization and humidified oxygen. Severely ill, immunocompromised patients may benefit from aerosolized ribavirin. There is no currently available vaccine.
3) Influenza viruses
Influenza viruses are enveloped RNA viruses with three types: A, B, and C. Influenza A virus is the most important and can be further subtyped according to the composition of the envelope proteins (hemagglutinin and neuraminidase). The natural hosts for influenza A viruses are aquatic birds and various mammals, such as humans, pigs, and horses. Influenza B infections occur mainly in humans. Influenza C is mostly a human virus. Transmission of influenza viruses occurs mainly by inhalation of small-particle aerosols or by direct contact. Viruses are rapidly spread to the trachea, bronchi, and lower airways. Most often influenza virus infections are associated with a characteristic clinical picture, including cough, high fever, pharyngitis, myalgia, and headache. Both inactivated and live attenuated vaccines have been developed for influenza viruses, but in annual vaccinations inactivated vaccines are used.
Treatment, prevention and control
Treatment is usually symptomatic; secondary bacterial infections require appropriate antibiotics. Inactivated viral vaccines are prepared from the currently circulating viruses each year. Vaccination provides 70% protection and is recommended for individuals at risk of severe disease, such as those with cardiopulmonary disease or asthma. Influenza can be treated with the neuraminidase inhibitors zanamivir and oseltamivir, which shorten the duration of symptoms.
4) Coronaviruses
Human coronaviruses are large enveloped RNA viruses. There are three groups of coronaviruses. The diagnosis of coronaviruses has previously been laborious because viral culture is difficult. The epidemiology and clinical picture of these diseases have been based mainly on serologic studies. Clinical expression has mainly been associated with mild upper respiratory infections. No treatment or prevention exists for coronavirus infections. Interferons and several proteinase inhibitors have been studied for treatment of infections, but none of these are in clinical use.
5) Adenoviruses
Adenoviruses are unenveloped, icosahedral, double-stranded DNA viruses that possess species-specific, group-specific and type-specific antigens. There are more than 50 serotypes of human adenoviruses, which are divided into six groups (A–F) on the basis of their genomic homology. Most adenoviruses are considered to be respiratory pathogens, although diseases involving the gastrointestinal tract, urinary bladder, liver, pancreas, and central nervous system have also been described. Adenovirus types 40 and 41 are known to cause only gastroenteritis. Adenoviruses infrequently cause common colds, and respiratory infections caused by these viruses tend to be severe, characterized by high and prolonged fever and strong inflammatory response. Adenoviruses are usually transmitted by the fecal-oral route or by aerosols. Infection often begins in the eyes, nasopharynx, or lungs and then spreads to other organs. Cells may also become persistently infected, resulting in viral shedding years after infection. During respiratory infections caused by adenoviruses the major symptoms and signs are rhinitis, nasal congestion, fever, cough, conjunctivitis, and tonsillitis.
Prevention and control
Outbreaks must be managed according to infection control practices (both respiratory and contact). Outbreaks of ocular infection at swimming pools are prevented by adequate chlorination. Transmission between patients undergoing ophthalmic examination can be prevented by single-use equipment, adequate decontamination of equipment and appropriate hygiene by healthcare staff.
6) Parainfluenza viruses
This is a fragile, enveloped paramyxovirus (150–300 nm) containing a single strand of negative-sense RNA. It has four types that share antigenic determinants.
Pathogenesis and epidemiology: The virus attaches to host cells, where the envelope fuses with the host cell membrane. The virus multiplies throughout the tracheobronchial tree. Infection, which is transmitted by the respiratory route, peaks in the winter, with the highest attack rates occurring in children under 3 years old.
Clinical features
In this common, self-limiting condition, which usually lasts 4–5 days, children are distressed, coryzal and febrile. In young children, hoarse coughing often alternates with hoarse crying and is associated with inspiratory stridor secondary to laryngeal obstruction (croup). Rarely, bronchiolitis, bronchopneumonia or acute epiglottitis may develop, signaled by reduced air entry and cyanosis.
Diagnosis and treatment
Diagnosis is clinical. Direct immunofluorescence gives rapid results; viral isolation and reverse transcriptase nucleic acid amplification tests (NAATs) are available as part of a respiratory virus screen. Treatment is symptomatic (e.g. paracetamol and humidification). Severe infection can be treated with ribavirin and humidified oxygen.
Metapneumovirus
Human metapneumovirus is a recently discovered respiratory virus. This virus was identified as a new member of the Metapneumovirus genus based on sequence homology and given the name human metapneumovirus.
GENERAL PRINCIPLES OF MANAGEMENT
The primary initial concern is ensuring an adequate airway. Other adjunctive measures, such as highly humidified air and oxygen, may also provide relief in acute diseases involving the structures in and around the larynx. In proved or suspected bacterial infections, specific antimicrobic therapy is required; other treatment, such as antitoxin administration in diphtheria, may also be necessary. Viral infections of the upper respiratory tract can only be treated symptomatically. Vaccination against some of the viral particles can be very effective.
If invasive Candida infection is present, topical and/or systemic antifungal therapy is sometimes necessary.
CHAPTER TWO
FUNGI ASSOCIATED WITH RESPIRATORY TRACT INFECTION
Fungal infections of the lung are less common than bacterial and viral infections but pose significant problems in diagnosis and treatment. They mainly affect people living in certain geographic areas and those with immune deficiency. Their virulence varies from causing no symptoms to causing death.
Epidemiology, prevalence, economic burden, vulnerable populations
Rates of invasive fungal infections have surged during recent decades, largely because of the increasing size of the population at risk. This population includes patients who are immunosuppressed because of diseases, such as cancers of immune cells of the blood, bone marrow, and lymph nodes, and those with human immunodeficiency virus (HIV) infection. It also includes patients taking immunosuppressive drugs, which are given to avoid rejection of transplanted organs or stem cells and as treatment for autoimmune diseases, such as rheumatoid arthritis. Immunosuppressive drugs are also given to reduce inflammation. For example, corticosteroids are often prescribed for many different lung diseases. A new class of potent immunosuppressive agents includes compounds that block regulatory molecules produced by the immune system called cytokines. One of these cytokines, tumor necrosis factor, is key to many of the body’s immune processes. In addition, patients with chronic debilitating diseases, who are in an immune-deficient state, make an attractive host for invasive fungi.
Massive population growth, urban development, and climate change are also factors that have increased the prevalence of fungal infections in certain areas and are putting more people at risk of becoming infected with the fungi that is endemic to where they live. Generally speaking, invasive fungal infections (termed mycoses) can be divided into two broad categories: the opportunistic and the endemic mycoses. Opportunistic fungal infections involve ubiquitous fungi and occur predominantly in individuals whose immune systems are compromised. These infections do not follow any particular geographic distribution and are seen with increasing frequency worldwide. Invasive pulmonary aspergillosis and systemic candidiasis are the most prevalent opportunistic fungal infections. Mold infections that were once considered rare are now emerging as significant infectious complications of the severely immune compromised. The fungus aspergillus is the leading cause of infection-related death in stem cell transplant recipients. Allergic lung diseases can also develop in otherwise healthy subjects who are repeatedly exposed to environmental molds. On the other hand, endemic fungal infections follow distinct geographic distributions that are determined by soil and climate conditions optimal for the fungi’s growth. North America and Africa are home to three of the major endemic mycoses: histoplasmosis, blastomycosis, and coccidioidomycosis. Their prevalence varies by region.
These three endemic fungal diseases share many characteristics. Illness is acquired by inhaling aerosolized spores. Healthy individuals who contract these diseases generally experience few symptoms, or, if they become ill, recover quickly on their own. In contrast, the infections can be life-threatening in patients with depressed immunity, especially those with acquired immune deficiency syndrome (AIDS) and those receiving immunosuppressive medications. The infections can persist and cause other lung diseases, such as emphysema, to worsen.
Candida spp.
C. albicans is the most frequent species isolated from respiratory samples followed by C. parapsilosis, C. tropicalis and C. glabrata. Despite the frequent isolation of Candida spp. from respiratory samples, isolation in non-neutropenic patients is not considered diagnosis of pneumonia regardless the species isolated. Pneumonia by Candida spp. is exceptional in non-neutropenic patients
Aspergillus spp.
In contrast to Candida, the genus Aspergillus acquires relevance in the respiratory infection of the critically ill patient. Aspergillus fumigatus is the most frequent species causing invasive pulmonary aspergillosis (IPA). Conidia of Aspergillus are easily aerosolized, being transmission by air nearly universal. A fumigatus presents rapid replication and small size conidia, thus favoring its frequency as etiological agent of IPA. Humans continuously inhale Aspergillus conidia but, in general, they are efficiently eliminated by the immune system.
Other Mucorales
Mucormycosis is an opportunistic acute infection caused by fungi from the order Mucorales of the Zygomycetes class. Within this family, most frequent genera are Rhizopus, Mucor and Lichtheimia (before Absidia). Spores of these microorganisms enter the organism through inhalation or through open wounds. The most frequent clinical presentation is rhinocerebral mucormycosis followed by pulmonary infection.
Pathophysiology, causes: genetic, environment, microbes
Most pulmonary fungal infections occur after inhalation of fungi that have been aerosolized because their natural habitat was disturbed. Once in the lungs’ alveoli (air sacs), the fungus is engulfed by macrophages and other cells involved in the primary immune response. Macrophages are usually able to neutralize and destroy the pathogens that they attack, but many fungi have developed a way to disable the macrophage’s weapons, and some fungi have actually developed the ability to grow and multiply inside macrophages.
Secondary or adaptive immunity cells are called to the site of infection, and in healthy individuals, this action can usually control the infection’s spread. The fungus is contained, but the sites of initial infection can remain as granulomas, collections of different types of immune cells. The granulomas later degenerate to scars and often calcify. Calcified granulomas may be seen years later on x-ray images. When cellular immunity is impaired, as it is, for instance, in AIDS, infection with an endemic fungus cannot be controlled. Almost any organ can be involved as the infection spreads throughout the body. The presence of structural lung disease, such as emphysema, impairs the clearance of the infection and allows a chronic condition to take hold. White blood cells (especially neutrophils) are critical to fight certain fungal infections such as those due to the fungus Aspergillus.
Prevention, treatment and prognosis
There is no fungal vaccine is available for clinical use. Today, the most effective way of preventing fungal infections in individuals at risk is by avoiding activities that are associated with exposure to the fungi. Antifungal medication to prevent infection is recommended only in patients with severe immunosuppression, especially since it may lead to the emergence of fungi that are resistant to these medications. Three antifungal classes are available for the treatment of fungal infections: polyenes, azoles and echinocandins. Polyenes, mainly amphotericin B, are fungicidal and present the widest spectrum of activity, with resistance to these agents only reported in Candida lusitaniae and A. terreus.
Amphotericin B is still used in the initial treatment of severe and central nervous system fungal infections. It is usually followed by a maintenance regimen using the new medications. Immunosuppressed patients should be educated about their risk for developing fungal infections and advised about activities they should avoid, symptoms of fungal disease, and when to report possible exposure or symptoms to their doctor. High-risk activities include demolition and renovation of old buildings, clearing shrubs and debris, and spelunking.
Azoles are fungistatic and despite their similar mechanism of action, differences in their chemical structure lead to drug-dependent activity profiles. All are active against yeasts, but while fluconazole is not active against filamentous fungi, itraconazole, voriconazole and posaconazole are active against Aspergillus. Posaconazole, only available by oral route, is the unique azole active against Mucorales.
Echinocandins are active against Aspergillus and Candida, without activity against Mucorales. They exhibit fungistatic activity against Aspergillus as salvage therapy.
When pulmonary mucormycosis is suspected, antifungal treatment should be initiated without delay.
For the most part, treatment of endemic pulmonary fungal infections is very effective, especially when patients are diagnosed and treated in a timely fashion. For the opportunistic fungal infections, the prognosis depends mostly on the immune state of the patient. Therapy is more likely to be effective if immunity is recovered. The most striking example is the impact of anti-retroviral therapy for HIV, which has greatly reduced the incidence and outcome of opportunistic fungal infections in patients infected with HIV. The most important immediate step in controlling fungal infections is to increase awareness among clinicians of the significance of these pathogens and the changing patient population at risk.
Conclusions
Aspergillus spp. is the main fungi responsible for fungal respiratory infections in the critically ill patient followed by far by fungi from the other Mucorales. In the critically ill patient, main risk factors for IPA are COPD and use of steroids. Aspergillus spp. is also the principal fungus causing respiratory infection in solid organ transplant recipients, mainly affecting lung transplant recipients followed by liver transplant recipients. Although risk factors may vary according to the type of transplantation, reintervention, need for renal replacement therapy or CMV infection are risk factors for IPA following solid organ transplantation. Pulmonary infection by Zygomycetes mainly affects neutropenic patients.
REFERENCES
Ben-Ami R., Lewis R.E., Kontoyiannis D.P.,(2009). Invasive mould infections in the setting of hematopoietic cell transplantation: current trends and new challenges. Curr Opin Infect Dis; 22:376–384.
Dasbach E.J., Davies GM., Teutsch S.M., (2000). Burden of aspergillosis-related hospitalizations in the United States. Clin Infect Dis; 31:1524–1528.
Espy M.J., Uhl J.R., Sloan L.M., (2006): Real-time PCR in clinical microbiology: Applications for routine laboratory testing. Clin Microbiol Rev; 19:165.
Girones R., (2006): Tracking viruses that contaminate environments. Microbe; 1:19.
Knipe D.M., Howley P.M., (2007): Fields Virology, 5th ed. Lippincott Williams & Wilkins; pp404-408.
Le J., Schiller D.S., (2010): Aerosolized delivery of antifungal agents. Curr Fungal Infect Rep; 4:96-102.
Petrikkos G, Skiada A, Lortholary O, Roilides E, Walsh TJ, Kontoyiannis DP. Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis 2012; 54 (Suppl 1):S23-34.
Segal BH. Aspergillosis. N Engl J Med 2009; 360:1870-84.
Smith JA, Kauffman CA. Pulmonary fungal infections. Respirology 2012; 17:913-26.
Tortorano A., Dho G., Prigitano A., Breda G., Grancini A., Emmi V., (2012): Invasive fungal infections in the intensive care unit: a multicentre, prospective, observational study in Italy (2006-2008). Mycoses; 55:73-9.
Vincent J., Rello J., Marshall J., Silva E., Anzueto A., Martin C., (2009): International study of the prevalence and outcomes of infection in intensive care units. JAMA; 302:2323-9.
Wilson L., Reyes C., Stolpman M., Speckman J., Allen K., Beney J.,(2002): The direct cost and incidence of systemic fungal infections. Value Health; 5:26–34.
Woolhouse M.E.J., (2006): Where do emerging pathogens come from? Microbe; 1:511. www.ketabdownload.