Plantar Fasciitis Infographic
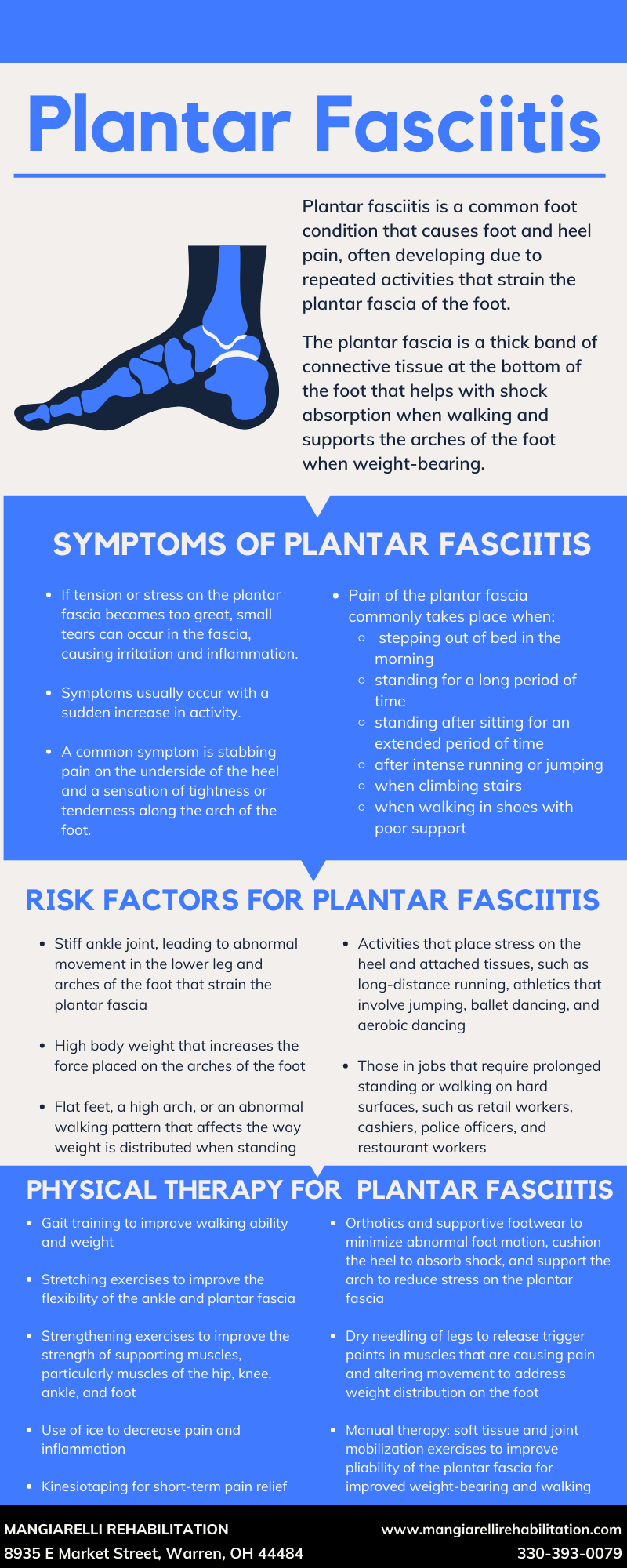
April is #FootHealthAwarenessMonth. Maintaining good foot health is essential for an active life. Our feet are the foundation for the rest of our body, carrying four to six times our body weight across the ankle joint when climbing stairs or walking a steep incline. If the foot is not mechanically healthy, this can negatively affect your knees, hips, and lower back. Plantar fasciitis is a common foot condition that causes foot and heel pain and affects two million Americans annually.
Plantar fasciitis frequently develops due to repeated activities that strain the plantar fascia of the foot. The plantar fascia is a thick band of connective tissue at the bottom of the foot that runs from the bottom of the heel bone and connects to the toes at the ball of the foot. The plantar fascia helps with shock absorption when walking and supports the arches of the foot when weight-bearing. When too much tension and stress are placed on the plantar fascia, small tears can occur, and repeated stretching and tearing irritates and inflames the fascia. Weakness or dysfunction of foot muscles and tendons increase the demand for stabilization on the plantar fascia, which can lead to heel pain. Dysfunction of hip or leg muscles can also change a person’s gait and weight-bearing distribution, which may also lead to pain and irritation of the plantar fascia.
Common plantar fasciitis symptoms are stabbing pain on the underside of the heel and a sensation of tightness or tenderness along the arch of the foot. Increased pain of the plantar fascia is common when stepping out of bed in the morning, standing for a long period of time, standing after sitting for an extended period of time, after intense running or jumping, when climbing stairs, or when walking in shoes with poor support.
Research has shown that physical therapy care for plantar fasciitis leads to recovery, fewer overall healthcare visits, and a lower cost of care than other medical interventions. Physical therapy treatment for plantar fasciitis is tailored to the patient’s condition and the factors that contributed to the foot and heel pain. After a thorough evaluation, the physical therapist may use any number of the following treatments to relieve pain and restore function to the foot and heel:
Gait training to enhance walking ability and ensure proper weight distribution
Stretching exercises to improve flexibility of the ankle and plantar fascia
Strengthening exercises to improve muscle strength of ankle, foot, knee, and hip
Use of ice to decrease pain and inflammation
Kinesiotaping for short-term pain relief
Orthotics and supportive footwear to minimize abnormal foot movement, cushion the heel to absorb shock, and support the arch of the foot to reduce the stress on the plantar fascia
Dry needling of leg muscles to release trigger points in muscles that are causing pain and altering movement in order to improve weight distribution on the foot
Manual therapy: soft tissue and joint mobilization to improve the pliability of the plantar fascia for improved walking ability and weight-bearing
Plantar fasciitis is a common repetitive strain injury in runners, walkers, hikers, and those that stand for the majority of their job (such as cashiers, retail workers, police officers, and restaurant workers). Physical therapy provides an effective and non-invasive treatment for plantar fasciitis to reduce pain and restore function to the foot and heel.