Making a diagnosis of a salivary gland disorder can be difficult. Common presentations, such as a painful or swollen gland, can be caused by numerous disorders of strikingly variable severity and consequences, including inflammatory, infectious, and neoplastic conditions, for which treatment can differ significantly, and referral for specialty care is sometimes necessary.
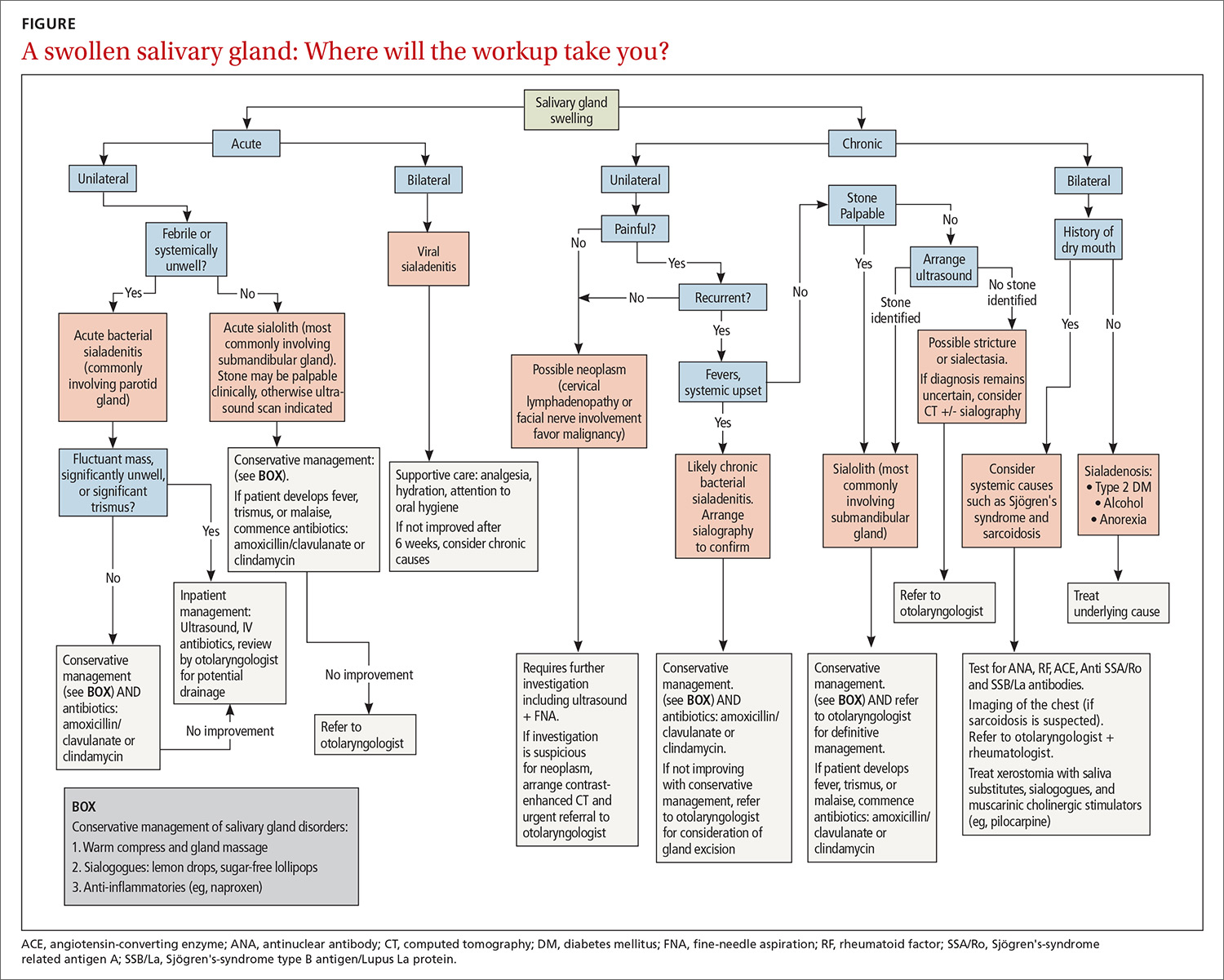
Yet it is the patient’s presentation that can aid you in making the diagnosis that will guide management. Consider that acute symptoms often result from infection, for example, and chronic or recurrent symptoms are caused more often by obstructive or nonobstructive inflammatory conditions and neoplasms. Diagnosis of an apparent neoplasm, prompted by clinical findings, is made using imaging and fine-needle aspiration (FNA) biopsy. Acute infection usually resolves with antibiotics and supportive management; calculi that cause persistent symptoms warrant referral for consideration of stone or gland removal; and malignant neoplasms usually require excision as well as neck dissection and chemotherapy or radiotherapy, or both—calling for multidisciplinary care.
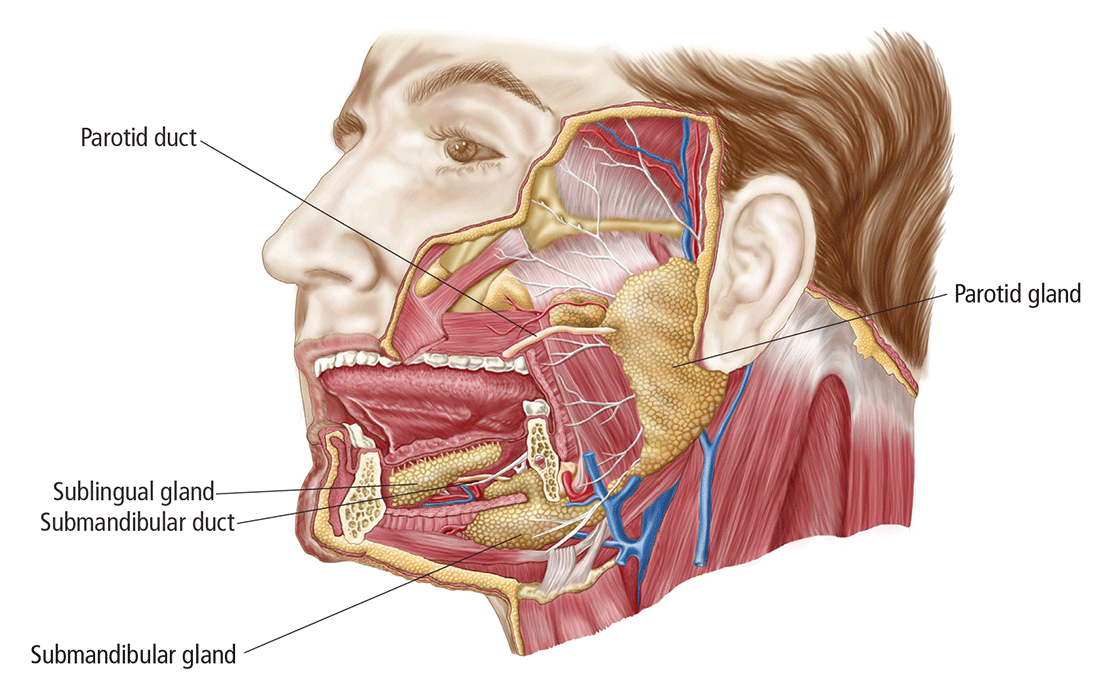
In this article, we clarify what can be an imprecise and perplexing path from the presentation to diagnosis to treatment of disorders of the salivary glands. To begin, see “Geography of the salivary glands,” for an overview of the location, structure, and corresponding ducts of the component salivary glands (parotid, submandibular, sublingual, and minor glands).
SIDEBAR
Geography of the salivary glands
The salivary glands comprise the major paired parotid, submandibular, and sublingual glands, as well as minor salivary glands that line the oropharyngeal mucosa. Secretion of saliva is modulated by both autonomic and humoral factors.
The parotid gland sits between the mastoid process, the ramus of the mandible, and the styloid process, extend- ing from the external auditory meatus superiorly to below the angle of the mandible and into the neck inferiorly. The gland is surrounded by a tough capsule. Embedded within the gland is the facial nerve, which divides into its 5 branches within the substance of the gland. The parotid (Stensen’s) duct passes anteriorly before turning medially to pierce the buccinator muscle, opening onto the mucous membrane of the cheek opposite the second upper molar.
The submandibular gland comprises (1) a large superficial part that fills the space between the mandible and the floor of the mouth and (2) a small deep part that wraps around the posterior border of the mylohyoid muscle. The submandibular (Wharton’s) duct runs anteriorly to open onto the floor of the mouth, alongside the frenulum.
The sublingual gland, the smallest of the major salivary glands, lies anteriorly in the floor of the mouth, with many small ducts opening either into the submandibular duct or directly into the mouth.
Basic secretory units of salivary glands are clusters of cells, each called an acinus. These cells secrete a fluid that contains water, electrolytes, mucous, and enzymes, all of which flow out of the acini into collecting ducts. The saliva produced by the parotid is mainly serous; by the submandibular gland, mixed; and by the sublingual and minor salivary glands, mucoid.
Presentation helps establish the differential Dx
Ask: Are the glands swollen?
Painless salivary gland swelling has a variety of causes, including neoplasm, sialadenosis, and the eating disorders bulimia and anorexia nervosa. There is significant overlap of presentations among those causes (FIGURE). Pain accompanying swelling is uncommon but not unheard of.
Neoplasms. Tumors of the salivary gland are relatively uncommon, constituting approximately 2% of head and neck neoplasms; most (80%) occur in the parotid gland, and most of those are benign.1 Although benign and malignant salivary gland neoplasms do not usually present with pain, pain can be associated with a neoplasm secondary to suppuration, hemorrhage into a mass, or infiltration of a malignancy into adjacent tissue.
Benign tumors. The majority of benign tumors are pleomorphic adenomas of the parotid, accounting for approximately 60% of salivary gland neoplasms.1,2 Tumors localized to the submandibular gland are often (in 50% of cases) malignant, however.3
Benign tumors are typically slow-growing and, generally, painless. On examination, they are well-circumscribed, mobile, and nontender. Patients presenting late with a large tumor might, however, experience pain secondary to stretching of the parotid capsule or compression of local structures.
Continue to: Ultrasonograhpy (US) is an excellent...