Potential Benefits of Bovine Colostrum in Pediatric Nutrition and Health
Abstract
:1. Introduction
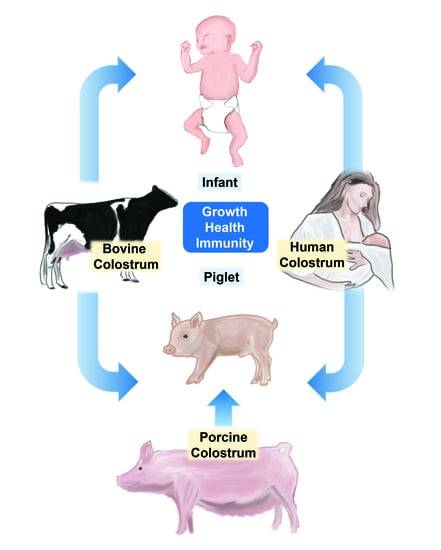
2. Composition and Function of Colostrum in Humans and Animals
2.1. Macronutrients
2.2. Immunoglobulins
2.3. Lactoferrin, Lysozyme, and α-Lactalbumin
2.4. Milk Fat Globule Membranes
2.5. Oligosaccharides
2.6. Insight into Novel Milk Components
3. Bovine Colostrum for Growth, Development and Immunity
3.1. Healthy Term Infants and Animal Models
3.2. Preterm Infants and Animal Models
3.3. Growth-Restricted Infants, Children, or Animal Models
4. Bovine Colostrum to Prevent or Treat Specific Pediatric Diseases
4.1. Gut and Lung Infections in Children and Animal Models
4.2. Necrotizing Enterocolitis in Preterm Infants and Animal Models
4.3. Fetal Infection and Neonatal Sepsis in Infants and Animal Models
4.4. Inflammatory Bowel Disease in Adolescents or Animal Models
4.5. Short-Bowel Syndrome in Infants or Animal Models
4.6. Chemotherapy-Induced Mucositis
5. Processing of Bovine Colostrum for Use in Pediatrics
6. Product Consistency and Quality
7. Possible Health Risks of Using Bovine Colostrum in Pediatrics
7.1. Cow’s Milk Allergy
7.2. Recommended Safe and Effective Intake Levels
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hammon, H.M.; Liermann, W.; Frieten, D.; Koch, C. Review: Importance of colostrum supply and milk feeding intensity on gastrointestinal and systemic development in calves. Animal 2020, 14, s133–s143. [Google Scholar] [CrossRef] [Green Version]
- Wall, S.K.; Gross, J.J.; Kessler, E.C.; Villez, K.; Bruckmaier, R.M. Blood-derived proteins in milk at start of lactation: Indicators of active or passive transfer. J. Dairy Sci. 2015, 98, 7748–7756. [Google Scholar] [CrossRef] [Green Version]
- Playford, R.J.; Weiser, M.J. Bovine Colostrum: Its Constituents and Uses. Nutrients 2021, 13, 265. [Google Scholar] [CrossRef] [PubMed]
- Ballard, O.; Morrow, A.L. Human milk composition: Nutrients and bioactive factors. Pediatr. Clin. North Am. 2013, 60, 49–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldman, A.S. Evolution of the mammary gland defense system and the ontogeny of the immune system. J. Mammary Gland. Biol. Neoplasia 2002, 7, 277–289. [Google Scholar] [CrossRef]
- Stevens, E.E.; Patrick, T.E.; Pickler, R. A history of infant feeding. J. Perinat. Educ. 2009, 18, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Riley, L.K.; Rupert, J.; Boucher, O. Nutrition in Toddlers. Am. Fam. Physician 2018, 98, 227–233. [Google Scholar] [PubMed]
- Clark, D.C.; Cifelli, C.J.; Pikosky, M.A. Growth and Development of Preschool Children (12–60 Months): A Review of the Effect of Dairy Intake. Nutrients 2020, 12, 3556. [Google Scholar] [CrossRef]
- Lucas, A. Scientific Evidence for Breastfeeding. Nestle Nutr. Inst. Workshop Ser. 2019, 90, 1–12. [Google Scholar] [CrossRef]
- Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 2012, 129, e827–e841. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maffei, D.; Schanler, R.J. Human milk is the feeding strategy to prevent necrotizing enterocolitis! Semin. Perinatol. 2017, 41, 36–40. [Google Scholar] [CrossRef] [Green Version]
- Quigley, M.; Embleton, N.D.; McGuire, W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst. Rev. 2018, 6, Cd002971. [Google Scholar] [CrossRef] [PubMed]
- Ananthan, A.; Balasubramanian, H.; Rao, S.; Patole, S. Human Milk-Derived Fortifiers Compared with Bovine Milk-Derived Fortifiers in Preterm Infants: A Systematic Review and Meta-Analysis. Adv. Nutr. 2020, 11, 1325–1333. [Google Scholar] [CrossRef]
- Høst, A.; Halken, S. Cow’s milk allergy: Where have we come from and where are we going? Endocr. Metab. Immune Disord. Drug Targets 2014, 14, 2–8. [Google Scholar] [CrossRef]
- Burris, A.D.; Burris, J.; Järvinen, K.M. Cow’s Milk Protein Allergy in Term and Preterm Infants: Clinical Manifestations, Immunologic Pathophysiology, and Management Strategies. NeoReviews 2020, 21, e795–e808. [Google Scholar] [CrossRef]
- Michelet, M.; Schluckebier, D.; Petit, L.M.; Caubet, J.C. Food protein-induced enterocolitis syndrome—A review of the literature with focus on clinical management. J. Asthma Allergy 2017, 10, 197–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Canvasser, J.; Hair, A.B.; Kim, J.H.; Taylor, S.N. Parent and Provider Perspectives on the Imprecise Label of “Human Milk Fortifier” in the NICU. Nutrients 2020, 12, 720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korhonen, H.; Marnila, P.; Gill, H.S. Bovine milk antibodies for health. Br. J. Nutr. 2000, 84 (Suppl. S1), S135–S146. [Google Scholar] [CrossRef] [Green Version]
- Ulfman, L.H.; Leusen, J.H.W.; Savelkoul, H.F.J.; Warner, J.O.; van Neerven, R.J.J. Effects of Bovine Immunoglobulins on Immune Function, Allergy, and Infection. Front. Nutr. 2018, 5, 52. [Google Scholar] [CrossRef] [PubMed]
- Rathe, M.; Müller, K.; Sangild, P.T.; Husby, S. Clinical applications of bovine colostrum therapy: A systematic review. Nutr. Rev. 2014, 72, 237–254. [Google Scholar] [CrossRef]
- Playford, R.J.; Macdonald, C.E.; Johnson, W.S. Colostrum and milk-derived peptide growth factors for the treatment of gastrointestinal disorders. Am. J. Clin. Nutr. 2000, 72, 5–14. [Google Scholar] [CrossRef]
- Stelwagen, K.; Carpenter, E.; Haigh, B.; Hodgkinson, A.; Wheeler, T.T. Immune components of bovine colostrum and milk. J. Anim. Sci. 2009, 87, 3–9. [Google Scholar] [CrossRef] [Green Version]
- Hurley, W.L.; Theil, P.K. Perspectives on immunoglobulins in colostrum and milk. Nutrients 2011, 3, 442–474. [Google Scholar] [CrossRef]
- Puppel, K.; Golebiewski, M.; Grodkowski, G.; Slosarz, J.; Kunowska-Slosarz, M.; Solarczyk, P.; Lukasiewicz, M.; Balcerak, M.; Przysucha, T. Composition and Factors Affecting Quality of Bovine Colostrum: A Review. Animals 2019, 9, 1070. [Google Scholar] [CrossRef] [Green Version]
- Davis, T.A.; Nguyen, H.V.; Garcia-Bravo, R.; Fiorotto, M.L.; Jackson, E.M.; Reeds, P.J. Amino acid composition of the milk of some mammalian species changes with stage of lactation. Br. J. Nutr. 1994, 72, 845–853. [Google Scholar] [CrossRef] [Green Version]
- Lonnerdal, B.; Erdmann, P.; Thakkar, S.K.; Sauser, J.; Destaillats, F. Longitudinal evolution of true protein, amino acids and bioactive proteins in breast milk: A developmental perspective. J. Nutr. Biochem. 2017, 41, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahern, G.J.; Hennessy, A.A.; Ryan, C.A.; Ross, R.P.; Stanton, C. Advances in Infant Formula Science. Annu. Rev. Food Sci. Technol. 2019, 10, 75–102. [Google Scholar] [CrossRef] [PubMed]
- Godden, S.M.; Lombard, J.E.; Woolums, A.R. Colostrum Management for Dairy Calves. Vet. Clin. N. Am. Food Anim. Pract. 2019, 35, 535–556. [Google Scholar] [CrossRef]
- West, D.W.D.; Mitchell, C.J. Tracking the Fate of Milk Proteins: Better in Whole or in Part? J. Nutr. 2020, 150, 2001–2002. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.R.; Ling, P.R.; Blackburn, G.L. Review of Infant Feeding: Key Features of Breast Milk and Infant Formula. Nutrients 2016, 8, 279. [Google Scholar] [CrossRef] [Green Version]
- Bhat, M.Y.; Dar, T.A.; Singh, L.R. Casein Proteins: Structural and Functional Aspects. In Milk Proteins—From Structure to Biological Properties and Health Aspects; InTech: Rijeka, Croatia, 2016. [Google Scholar] [CrossRef] [Green Version]
- Dupont, D.; Tomé, D. Milk proteins: Digestion and absorption in the gastrointestinal tract. In Milk Proteins; Academic Press: Cambridge, MA, USA, 2020; pp. 701–714. [Google Scholar] [CrossRef]
- Boirie, Y.; Dangin, M.; Gachon, P.; Vasson, M.P.; Maubois, J.L.; Beaufrere, B. Slow and fast dietary proteins differently modulate postprandial protein accretion. Proc. Natl. Acad. Sci. USA 1997, 94, 14930–14935. [Google Scholar] [CrossRef] [Green Version]
- Bourlieu, C.; Ménard, O.; Bouzerzour, K.; Mandalari, G.; Macierzanka, A.; Mackie, A.R.; Dupont, D. Specificity of Infant Digestive Conditions: Some Clues for Developing Relevant In Vitro Models. Crit. Rev. Food Sci. Nutr. 2014, 54, 1427–1457. [Google Scholar] [CrossRef] [PubMed]
- Welch-Jernigan, R.J.; Abrahamse, E.; Stoll, B.; Smith, O.; Wierenga, P.A.; van de Heijning, B.J.M.; Renes, I.B.; Burrin, D.G. Postprandial Amino Acid Kinetics of Milk Protein Mixtures are Affected by Composition, But Not Denaturation, in Neonatal Piglets. Curr. Dev. Nutr. 2019, 3, nzy102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chatterton, D.E.; Nguyen, D.N.; Bering, S.B.; Sangild, P.T. Anti-inflammatory mechanisms of bioactive milk proteins in the intestine of newborns. Int. J. Biochem. Cell Biol. 2013, 45, 1730–1747. [Google Scholar] [CrossRef] [PubMed]
- Lönnerdal, B. Biological effects of novel bovine milk fractions. Nestle Nutr. Workshop Ser. Paediatr. Program. 2011, 67, 41–54. [Google Scholar] [CrossRef] [Green Version]
- Wada, Y.; Lönnerdal, B. Bioactive peptides derived from human milk proteins—Mechanisms of action. J. Nutr. Biochem. 2014, 25, 503–514. [Google Scholar] [CrossRef]
- Korhonen, H.; Marnila, P.; Gill, H.S. Milk immunoglobulins and complement factors. Br. J. Nutr. 2000, 84 (Suppl. S1), S75–S80. [Google Scholar] [CrossRef] [Green Version]
- Cakebread, J.A.; Humphrey, R.; Hodgkinson, A.J. Immunoglobulin A in Bovine Milk: A Potential Functional Food? J. Agric. Food Chem. 2015, 63, 7311–7316. [Google Scholar] [CrossRef]
- Klobasa, F.; Werhahn, E.; Butler, J.E. Composition of sow milk during lactation. J. Anim. Sci. 1987, 64, 1458–1466. [Google Scholar] [CrossRef]
- Hedegaard, C.J.; Heegaard, P.M. Passive immunisation, an old idea revisited: Basic principles and application to modern animal production systems. Vet. Immunol. Immunopathol. 2016, 174, 50–63. [Google Scholar] [CrossRef] [Green Version]
- Malek, A.; Sager, R.; Kuhn, P.; Nicolaides, K.H.; Schneider, H. Evolution of maternofetal transport of immunoglobulins during human pregnancy. Am. J. Reprod. Immunol. 1996, 36, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Palmeira, P.; Quinello, C.; Silveira-Lessa, A.L.; Zago, C.A.; Carneiro-Sampaio, M. IgG placental transfer in healthy and pathological pregnancies. Clin. Dev. Immunol. 2012, 2012, 985646. [Google Scholar] [CrossRef]
- Van den Berg, J.P.; Westerbeek, E.A.; van der Klis, F.R.; Berbers, G.A.; van Elburg, R.M. Transplacental transport of IgG antibodies to preterm infants: A review of the literature. Early Hum. Dev. 2011, 87, 67–72. [Google Scholar] [CrossRef]
- Lee, J.; Kim, H.S.; Jung, Y.H.; Choi, K.Y.; Shin, S.H.; Kim, E.K.; Choi, J.H. Oropharyngeal colostrum administration in extremely premature infants: An RCT. Pediatrics 2015, 135, e357–e366. [Google Scholar] [CrossRef] [Green Version]
- Goldblum, R.M.; Schanler, R.J.; Garza, C.; Goldman, A.S. Human milk feeding enhances the urinary excretion of immunologic factors in low birth weight infants. Pediatr. Res. 1989, 25, 184–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Axelsson, I.; Jakobsson, I.; Lindberg, T.; Polberger, S.; Benediktsson, B.; Raiha, N. Macromolecular absorption in preterm and term infants. Acta Paediatr. 1989, 78, 532–537. [Google Scholar] [CrossRef] [PubMed]
- Simister, N.E. Placental transport of immunoglobulin G. Vaccine 2003, 21, 3365–3369. [Google Scholar] [CrossRef]
- Van de Perre, P. Transfer of antibody via mother’s milk. Vaccine 2003, 21, 3374–3376. [Google Scholar] [CrossRef]
- Sangild, P.T. Uptake of colostral immunoglobulins by the compromised newborn farm animal. Acta Vet. Scandinavica. Suppl. 2003, 98, 105–122. [Google Scholar] [CrossRef]
- Sangild, P.T. Gut responses to enteral nutrition in preterm infants and animals. Exp. Biol. Med. 2006, 231, 1695–1711. [Google Scholar] [CrossRef]
- Westrom, B.; Arevalo Sureda, E.; Pierzynowska, K.; Pierzynowski, S.G.; Perez-Cano, F.J. The Immature Gut Barrier and Its Importance in Establishing Immunity in Newborn Mammals. Front. Immunol. 2020, 11, 1153. [Google Scholar] [CrossRef]
- Stirling, C.M.; Charleston, B.; Takamatsu, H.; Claypool, S.; Lencer, W.; Blumberg, R.S.; Wileman, T.E. Characterization of the porcine neonatal Fc receptor--potential use for trans-epithelial protein delivery. Immunology 2005, 114, 542–553. [Google Scholar] [CrossRef]
- Drew, M.D.; Owen, B.D. The provision of passive immunity to colostrum-deprived piglets by bovine or porcine serum immunoglobulins. Can. J. Anim Sci. 1988, 68, 1277–1284. [Google Scholar] [CrossRef]
- Pyzik, M.; Sand, K.M.K.; Hubbard, J.J.; Andersen, J.T.; Sandlie, I.; Blumberg, R.S. The Neonatal Fc Receptor (FcRn): A Misnomer? Front. Immunol. 2019, 10, 1540. [Google Scholar] [CrossRef]
- Shah, U.; Dickinson, B.L.; Blumberg, R.S.; Simister, N.E.; Lencer, W.I.; Walker, W.A. Distribution of the IgG Fc receptor, FcRn, in the human fetal intestine. Pediatr. Res. 2003, 53, 295–301. [Google Scholar] [CrossRef]
- Yoshida, M.; Kobayashi, K.; Kuo, T.T.; Bry, L.; Glickman, J.N.; Claypool, S.M.; Kaser, A.; Nagaishi, T.; Higgins, D.E.; Mizoguchi, E.; et al. Neonatal Fc receptor for IgG regulates mucosal immune responses to luminal bacteria. J. Clin. Investig. 2006, 116, 2142–2151. [Google Scholar] [CrossRef]
- Hodgkinson, A.J.; Cakebread, J.; Callaghan, M.; Harris, P.; Brunt, R.; Anderson, R.C.; Armstrong, K.M.; Haigh, B. Comparative innate immune interactions of human and bovine secretory IgA with pathogenic and non-pathogenic bacteria. Dev. Comp. Immunol. 2017, 68, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Jensen, A.R.; Elnif, J.; Burrin, D.G.; Sangild, P.T. Development of intestinal immunoglobulin absorption and enzyme activities in neonatal pigs is diet dependent. J. Nutr. 2001, 131, 3259–3265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nash, G.S.; MacDermott, R.P.; Schloemann, S.; Bertovich, M.J.; O’Neal, J.; Porter, L.; Kulczycki, A. Bovine IgG1, but not IgG2, binds to human B cells and inhibits antibody secretion. Immunology 1990, 69, 361–366. [Google Scholar] [PubMed]
- Bagwe-Parab, S.; Yadav, P.; Kaur, G.; Tuli, H.S.; Buttar, H.S. Therapeutic Applications of Human and Bovine Colostrum in the Treatment of Gastrointestinal Diseases and Distinctive Cancer Types: The Current Evidence. Front. Pharmacol. 2020, 11, 01100. [Google Scholar] [CrossRef] [PubMed]
- Detzel, C.J.; Horgan, A.; Henderson, A.L.; Petschow, B.W.; Warner, C.D.; Maas, K.J.; Weaver, E.M. Bovine immunoglobulin/protein isolate binds pro-inflammatory bacterial compounds and prevents immune activation in an intestinal co-culture model. PLoS ONE 2015, 10, e0120278. [Google Scholar] [CrossRef] [Green Version]
- Arrouk, R.; Herdes, R.E.; Karpinski, A.C.; Hyman, P.E. Serum-derived bovine immunoglobulin for children with diarrhea-predominant irritable bowel syndrome. Pediatr. Health Med. Ther. 2018, 9, 129–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asmuth, D.M.; Hinkle, J.E.; LaMarca, A.; Fichtenbaum, C.J.; Somsouk, M.; Utay, N.S.; Shaw, A.L.; Petschow, B.W.; Detzel, C.J.; Weaver, E.M. Evaluation of oral serum-derived bovine immunoglobulins in HIV-infected patients with chronic idiopathic diarrhea. HIV Clin. Trials 2017, 18, 205–213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petschow, B.W.; Blikslager, A.T.; Weaver, E.M.; Campbell, J.M.; Polo, J.; Shaw, A.L.; Burnett, B.P.; Klein, G.L.; Rhoads, J.M. Bovine immunoglobulin protein isolates for the nutritional management of enteropathy. World J. Gastroenterol. 2014, 20, 11713–11726. [Google Scholar] [CrossRef] [PubMed]
- Petschow, B.W.; Burnett, B.; Shaw, A.L.; Weaver, E.M.; Klein, G.L. Serum-derived bovine immunoglobulin/protein isolate: Postulated mechanism of action for management of enteropathy. Clin. Exp. Gastroenterol. 2014, 7, 181–190. [Google Scholar] [CrossRef] [Green Version]
- Van Arsdall, M.; Haque, I.; Liu, Y.; Rhoads, J.M. Is There a Role for the Enteral Administration of Serum-Derived Immunoglobulins in Human Gastrointestinal Disease and Pediatric Critical Care Nutrition? Adv. Nutr. 2016, 7, 535–543. [Google Scholar] [CrossRef] [Green Version]
- Montagne, P.; Culliere, M.L.; Bene, M.C.; Faure, G. Changes in lactoferrin and lysozyme levels in human milk during the first twelve weeks of lactation. In Bioactive Components of Human Milk; Springer: Boston, MA, USA, 2001. [Google Scholar]
- Donovan, S.M.; Odle, J. Growth factors in milk as mediators of infant development. Annu. Rev. Nutr. 1994, 14, 147–167. [Google Scholar] [CrossRef]
- Gislason, J.; Iyer, S.; Hutchens, T.W.; Lonnerdal, B. Lactoferrin receptors in piglet small intestine: Lactoferrin binding properties, ontogeny, and regional distribution in the gastrointestinal tract. J. Nutr. Biochem. 1993, 4, 528–533. [Google Scholar] [CrossRef]
- Donovan, S.M. The Role of Lactoferrin in Gastrointestinal and Immune Development and Function: A Preclinical Perspective. J. Pediatr. 2016, 173, S16–S28. [Google Scholar] [CrossRef]
- Zhang, J.L.; Han, X.; Shan, Y.J.; Zhang, L.W.; Du, M.; Liu, M.; Yi, H.X.; Ma, Y. Effect of bovine lactoferrin and human lactoferrin on the proliferative activity of the osteoblast cell line MC3T3-E1 in vitro. J. Dairy Sci. 2018, 101, 1827–1833. [Google Scholar] [CrossRef] [Green Version]
- Embleton, N.D.; Berrington, J.E. Clinical Trials of Lactoferrin in the Newborn: Effects on Infection and the Gut Microbiome. Nestle Nutr. Inst. Workshop Ser. 2020, 94, 141–151. [Google Scholar] [CrossRef]
- Manzoni, P.; Meyer, M.; Stolfi, I.; Rinaldi, M.; Cattani, S.; Pugni, L.; Romeo, M.G.; Messner, H.; Decembrino, L.; Laforgia, N.; et al. Bovine lactoferrin supplementation for prevention of necrotizing enterocolitis in very-low-birth-weight neonates: A randomized clinical trial. Early Hum. Dev. 2014, 90, S60–S65. [Google Scholar] [CrossRef]
- Manzoni, P.; Dall’Agnola, A.; Tomé, D.; Kaufman, D.A.; Tavella, E.; Pieretto, M.; Messina, A.; De Luca, D.; Bellaiche, M.; Mosca, A.; et al. Role of Lactoferrin in Neonates and Infants: An Update. Am. J. Perinatol. 2018, 35, 561–565. [Google Scholar] [CrossRef]
- Pammi, M.; Suresh, G. Enteral lactoferrin supplementation for prevention of sepsis and necrotizing enterocolitis in preterm infants. Cochrane Database Syst. Rev. 2020, 3, CD007137. [Google Scholar] [CrossRef]
- Actor, J.K.; Hwang, S.; Kruzel, M.L. Lactoferrin as a natural immune modulator. Curr. Pharm. Des. 2009, 15, 1956–1973. [Google Scholar] [CrossRef] [Green Version]
- Afrazi, A.; Sodhi, C.P.; Richardson, W.; Neal, M.; Misty, G.; Siggers, R.; Hackman, D.J. New insights into pathogenesis and treatment of necrotizing enterocolitis: Toll-like receptors and beyond. Pediatr. Res. 2011, 69, 183–188. [Google Scholar] [CrossRef]
- Comstock, S.S.; Reznikov, E.A.; Contractor, N.; Donovan, S.M. Dietary bovine lactoferrin alters mucosal and systemic immune cell responses in neonatal piglets. J. Nutr. 2014, 144, 525–532. [Google Scholar] [CrossRef]
- Nguyen, D.N.; Jiang, P.; Stensballe, A.; Bendixen, E.; Sangild, P.T.; Chatterton, D.E. Bovine lactoferrin regulates cell survival, apoptosis and inflammation in intestinal epithelial cells and preterm pig intestine. J. Proteom. 2016, 139, 95–102. [Google Scholar] [CrossRef]
- Nguyen, D.N.; Li, Y.; Sangild, P.T.; Bering, S.B.; Chatterton, D.E. Effects of bovine lactoferrin on the immature porcine intestine. Br. J. Nutr. 2014, 111, 321–331. [Google Scholar] [CrossRef] [Green Version]
- Layman, D.K.; Lonnerdal, B.; Fernstrom, J.D. Applications for alpha-lactalbumin in human nutrition. Nutr. Rev. 2018, 76, 444–460. [Google Scholar] [CrossRef]
- Krissansen, G.W. Emerging health properties of whey proteins and their clinical implications. J. Am. Coll. Nutr. 2007, 26, 713s–723s. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, C.H.; Hui, Y.; Nguyen, D.N.; Ahnfeldt, A.M.; Burrin, D.G.; Hartmann, B.; Heckmann, A.B.; Sangild, P.T.; Thymann, T.; Bering, S.B. Alpha-Lactalbumin Enriched Whey Protein Concentrate to Improve Gut, Immunity and Brain Development in Preterm Pigs. Nutrients 2020, 12, 245. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.; Padhi, E.; Hasegawa, Y.; Larke, J.; Parenti, M.; Wang, A.; Hernell, O.; Lonnerdal, B.; Slupsky, C. Compositional Dynamics of the Milk Fat Globule and Its Role in Infant Development. Front. Pediatr. 2018, 6, 313. [Google Scholar] [CrossRef] [Green Version]
- Koletzko, B. Human Milk Lipids. Ann. Nutr. Metab. 2016, 69 (Suppl. S2), 27–40. [Google Scholar] [CrossRef] [Green Version]
- Manoni, M.; Di Lorenzo, C.; Ottoboni, M.; Tretola, M.; Pinotti, L. Comparative Proteomics of Milk Fat Globule Membrane (MFGM) Proteome across Species and Lactation Stages and the Potentials of MFGM Fractions in Infant Formula Preparation. Foods 2020, 9, 1251. [Google Scholar] [CrossRef] [PubMed]
- Brink, L.R.; Lonnerdal, B. Milk fat globule membrane: The role of its various components in infant health and development. J. Nutr. Biochem. 2020, 85, 108465. [Google Scholar] [CrossRef]
- Hernell, O.; Lonnerdal, B.; Timby, N. Milk Fat Globule Membranes: Effects on Microbiome, Metabolome, and Infections in Infants and Children. Nestle Nutr. Inst. Workshop Ser. 2020, 94, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, K.; Hosozawa, M.; Kudo, N.; Yoshikawa, N.; Hisata, K.; Shoji, H.; Shinohara, K.; Shimizu, T. The pilot study: Sphingomyelin-fortified milk has a positive association with the neurobehavioural development of very low birth weight infants during infancy, randomized control trial. Brain Dev. 2013, 35, 45–52. [Google Scholar] [CrossRef]
- Henriksen, N.L.; Aasmul-Olsen, K.; Venkatasubramanian, R.; Nygaard, M.K.E.; Sprenger, R.R.; Heckmann, A.B.; Ostenfeld, M.S.; Ejsing, C.S.; Eskildsen, S.F.; Müllertz, A.; et al. Dairy-Derived Emulsifiers in Infant Formula Show Marginal Effects on the Plasma Lipid Profile and Brain Structure in Preterm Piglets Relative to Soy Lecithin. Nutrients 2021, 13, 718. [Google Scholar] [CrossRef]
- Palmano, K.; Rowan, A.; Guillermo, R.; Guan, J.; McJarrow, P. The role of gangliosides in neurodevelopment. Nutrients 2015, 7, 3891–3913. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rueda, R.; Maldonado, J.; Narbona, E.; Gil, A. Neonatal dietary gangliosides. Early Hum. Dev. 1998, 53, S135–S147. [Google Scholar] [CrossRef]
- Greenspon, J.; Li, R.; Xiao, L.; Rao, J.N.; Sun, R.; Strauch, E.D.; Shea-Donohue, T.; Wang, J.Y.; Turner, D.J. Sphingosine-1-phosphate regulates the expression of adherens junction protein E-cadherin and enhances intestinal epithelial cell barrier function. Dig. Dis. Sci. 2011, 56, 1342–1353. [Google Scholar] [CrossRef] [Green Version]
- Hernell, O.; Timby, N.; Domellof, M.; Lonnerdal, B. Clinical Benefits of Milk Fat Globule Membranes for Infants and Children. J. Pediatr. 2016, 173, S60–S65. [Google Scholar] [CrossRef] [Green Version]
- Spitsberg, V.L. Invited Review: Bovine Milk Fat Globule Membrane as a Potential Nutraceutical. J. Dairy Sci. 2005, 88, 2289–2294. [Google Scholar] [CrossRef]
- Bhinder, G.; Allaire, J.M.; Garcia, C.; Lau, J.T.; Chan, J.M.; Ryz, N.R.; Bosman, E.S.; Graef, F.A.; Crowley, S.M.; Celiberto, L.S.; et al. Milk Fat Globule Membrane Supplementation in Formula Modulates the Neonatal Gut Microbiome and Normalizes Intestinal Development. Sci. Rep. 2017, 7, 45274. [Google Scholar] [CrossRef]
- Timby, N.; Domellof, M.; Holgerson, P.L.; West, C.E.; Lonnerdal, B.; Hernell, O.; Johansson, I. Oral Microbiota in Infants Fed a Formula Supplemented with Bovine Milk Fat Globule Membranes—A Randomized Controlled Trial. PLoS ONE 2017, 12, e0169831. [Google Scholar] [CrossRef]
- Urashima, T.; Taufik, E.; Fukuda, K.; Asakuma, S. Recent advances in studies on milk oligosaccharides of cows and other domestic farm animals. Biosci. Biotechnol. Biochem. 2013, 77, 455–466. [Google Scholar] [CrossRef] [Green Version]
- Albrecht, S.; Lane, J.A.; Mariño, K.; Al Busadah, K.A.; Carrington, S.D.; Hickey, R.M.; Rudd, P.M. A comparative study of free oligosaccharides in the milk of domestic animals. Br. J. Nutr. 2014, 111, 1313–1328. [Google Scholar] [CrossRef]
- Gopal, P.K.; Gill, H.S. Oligosaccharides and glycoconjugates in bovine milk and colostrum. Br. J. Nutr. 2000, 84 (Suppl. S1), S69–S74. [Google Scholar] [CrossRef] [Green Version]
- Donovan, S.M.; Comstock, S.S. Human Milk Oligosaccharides Influence Neonatal Mucosal and Systemic Immunity. Ann. Nutr. Metab. 2016, 69 (Suppl. S2), 42–51. [Google Scholar] [CrossRef]
- Pacheco, A.R.; Barile, D.; Underwood, M.A.; Mills, D.A. The impact of the milk glycobiome on the neonate gut microbiota. Annu. Rev. Anim. Biosci. 2015, 3, 419–445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smilowitz, J.T.; Lebrilla, C.B.; Mills, D.A.; German, J.B.; Freeman, S.L. Breast milk oligosaccharides: Structure-function relationships in the neonate. Annu. Rev. Nutr. 2014, 34, 143–169. [Google Scholar] [CrossRef] [Green Version]
- Bode, L.; Jantscher-Krenn, E. Structure-function relationships of human milk oligosaccharides. Adv. Nutr. (Bethesda Md.) 2012, 3, 383S–391S. [Google Scholar] [CrossRef]
- Newburg, D.S. Neonatal protection by an innate immune system of human milk consisting of oligosaccharides and glycans. J. Anim. Sci. 2009, 87, 26–34. [Google Scholar] [CrossRef]
- Aldredge, D.L.; Geronimo, M.R.; Hua, S.; Nwosu, C.C.; Lebrilla, C.B.; Barile, D. Annotation and structural elucidation of bovine milk oligosaccharides and determination of novel fucosylated structures. Glycobiology 2013, 23, 664–676. [Google Scholar] [CrossRef]
- Wang, B.; Yu, B.; Karim, M.; Hu, H.; Sun, Y.; McGreevy, P.; Petocz, P.; Held, S.; Brand-Miller, J. Dietary sialic acid supplementation improves learning and memory in piglets. Am. J. Clin. Nutr. 2007, 85, 561–569. [Google Scholar] [CrossRef] [Green Version]
- Harmsen, H.J.; Wildeboer-Veloo, A.C.; Raangs, G.C.; Wagendorp, A.A.; Klijn, N.; Bindels, J.G.; Welling, G.W. Analysis of intestinal flora development in breast-fed and formula-fed infants by using molecular identification and detection methods. J. Pediatr. Gastroenterol. Nutr. 2000, 30, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Morrin, S.T.; Lane, J.A.; Marotta, M.; Bode, L.; Carrington, S.D.; Irwin, J.A.; Hickey, R.M. Bovine colostrum-driven modulation of intestinal epithelial cells for increased commensal colonisation. Appl. Microbiol. Biotechnol. 2019, 103, 2745–2758. [Google Scholar] [CrossRef]
- Davis, E.C.; Wang, M.; Donovan, S.M. The role of early life nutrition in the establishment of gastrointestinal microbial composition and function. Gut Microbes 2017, 8, 143–171. [Google Scholar] [CrossRef] [PubMed]
- Lane, J.A.; Mariño, K.; Naughton, J.; Kavanaugh, D.; Clyne, M.; Carrington, S.D.; Hickey, R.M. Anti-infective bovine colostrum oligosaccharides: Campylobacter jejuni as a case study. Int. J. Food Microbiol. 2012, 157, 182–188. [Google Scholar] [CrossRef]
- Angeloni, S.; Ridet, J.L.; Kusy, N.; Gao, H.; Crevoisier, F.; Guinchard, S.; Kochhar, S.; Sigrist, H.; Sprenger, N. Glycoprofiling with micro-arrays of glycoconjugates and lectins. Glycobiology 2005, 15, 31–41. [Google Scholar] [CrossRef]
- Lane, J.A.; O’Callaghan, J.; Carrington, S.D.; Hickey, R.M. Transcriptional response of HT-29 intestinal epithelial cells to human and bovine milk oligosaccharides. Br. J. Nutr. 2013, 110, 2127–2137. [Google Scholar] [CrossRef] [PubMed]
- Comstock, S.S.; Wang, M.; Hester, S.N.; Li, M.; Donovan, S.M. Select human milk oligosaccharides directly modulate peripheral blood mononuclear cells isolated from 10-d-old pigs. Br. J. Nutr. 2014, 111, 819–828. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, M.; Monaco, M.H.; Wang, M.; Comstock, S.S.; Kuhlenschmidt, T.B.; Fahey, G.C., Jr.; Miller, M.J.; Kuhlenschmidt, M.S.; Donovan, S.M. Human milk oligosaccharides shorten rotavirus-induced diarrhea and modulate piglet mucosal immunity and colonic microbiota. ISME J. 2014, 8, 1609–1620. [Google Scholar] [CrossRef] [Green Version]
- Comstock, S.S.; Li, M.; Wang, M.; Monaco, M.H.; Kuhlenschmidt, T.B.; Kuhlenschmidt, M.S.; Donovan, S.M. Dietary Human Milk Oligosaccharides but Not Prebiotic Oligosaccharides Increase Circulating Natural Killer Cell and Mesenteric Lymph Node Memory T Cell Populations in Noninfected and Rotavirus-Infected Neonatal Piglets. J. Nutr. 2017, 147, 1041–1047. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Short, D.M.; Moore, D.A.; Sischo, W.M. A Randomized Clinical Trial Evaluating the Effects of Oligosaccharides on Transfer of Passive Immunity in Neonatal Dairy Calves. J. Vet. Intern. Med. 2016, 30, 1381–1389. [Google Scholar] [CrossRef]
- Bode, L. Human Milk Oligosaccharides in the Prevention of Necrotizing Enterocolitis: A Journey from in vitro and in vivo Models to Mother-Infant Cohort Studies. Front. Pediatr. 2018, 6, 385. [Google Scholar] [CrossRef]
- Cilieborg, M.S.; Sangild, P.T.; Jensen, M.L.; Østergaard, M.V.; Christensen, L.; Rasmussen, S.O.; Mørbak, A.L.; Jørgensen, C.B.; Bering, S.B. α1,2-Fucosyllactose Does Not Improve Intestinal Function or Prevent Escherichia coli F18 Diarrhea in Newborn Pigs. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 310–318. [Google Scholar] [CrossRef] [Green Version]
- Cilieborg, M.S.; Bering, S.B.; Østergaard, M.V.; Jensen, M.L.; Krych, Ł.; Newburg, D.S.; Sangild, P.T. Minimal short-term effect of dietary 2′-fucosyllactose on bacterial colonisation, intestinal function and necrotising enterocolitis in preterm pigs. Br. J. Nutr. 2016, 116, 834–841. [Google Scholar] [CrossRef] [Green Version]
- Obelitz-Ryom, K.; Rendboe, A.K.; Nguyen, D.N.; Rudloff, S.; Brandt, A.B.; Nielsen, D.S.; Heckmann, A.B.; Chichlowski, M.; Sangild, P.T.; Thymann, T.; et al. Bovine Milk Oligosaccharides with Sialyllactose for Preterm Piglets. Nutrients 2018, 10, 1489. [Google Scholar] [CrossRef] [Green Version]
- Rasmussen, S.O.; Martin, L.; Østergaard, M.V.; Rudloff, S.; Roggenbuck, M.; Nguyen, D.N.; Sangild, P.T.; Bering, S.B. Human milk oligosaccharide effects on intestinal function and inflammation after preterm birth in pigs. J. Nutr. Biochem. 2017, 40, 141–154. [Google Scholar] [CrossRef]
- Bering, S.B. Human Milk Oligosaccharides to Prevent Gut Dysfunction and Necrotizing Enterocolitis in Preterm Neonates. Nutrients 2018, 10, 1461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masi, A.C.; Embleton, N.D.; Lamb, C.A.; Young, G.; Granger, C.L.; Najera, J.; Smith, D.P.; Hoffman, K.L.; Petrosino, J.F.; Bode, L.; et al. Human milk oligosaccharide DSLNT and gut microbiome in preterm infants predicts necrotising enterocolitis. Gut 2020. [Google Scholar] [CrossRef]
- Kim, S.Y.; Yi, D.Y. Components of human breast milk: From macronutrient to microbiome and microRNA. Clin. Exp. Pediatr. 2020, 63, 301–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gu, Y.; Li, M.; Wang, T.; Liang, Y.; Zhong, Z.; Wang, X.; Zhou, Q.; Chen, L.; Lang, Q.; He, Z.; et al. Lactation-related microRNA expression profiles of porcine breast milk exosomes. PLoS ONE 2012, 7, e43691. [Google Scholar] [CrossRef]
- Zempleni, J.; Sukreet, S.; Zhou, F.; Wu, D.; Mutai, E. Milk-Derived Exosomes and Metabolic Regulation. Annu. Rev. Anim. Biosci. 2019, 7, 245–262. [Google Scholar] [CrossRef]
- Van Hese, I.; Goossens, K.; Vandaele, L.; Opsomer, G. Invited review: MicroRNAs in bovine colostrum—Focus on their origin and potential health benefits for the calf. J. Dairy Sci. 2020, 103, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Özdemir, S. Identification and comparison of exosomal microRNAs in the milk and colostrum of two different cow breeds. Gene 2020, 743, 144609. [Google Scholar] [CrossRef] [PubMed]
- Sun, Q.; Chen, X.; Yu, J.; Zen, K.; Zhang, C.Y.; Li, L. Immune modulatory function of abundant immune-related microRNAs in microvesicles from bovine colostrum. Protein Cell 2013, 4, 197–210. [Google Scholar] [CrossRef] [Green Version]
- O’Reilly, D.; Dorodnykh, D.; Avdeenko, N.V.; Nekliudov, N.A.; Garssen, J.; Elolimy, A.A.; Petrou, L.; Simpson, M.R.; Yeruva, L.; Munblit, D. Perspective: The Role of Human Breast-Milk Extracellular Vesicles in Child Health and Disease. Adv. Nutr. 2021, 12, 59–70. [Google Scholar] [CrossRef]
- Samuel, M.; Chisanga, D.; Liem, M.; Keerthikumar, S.; Anand, S.; Ang, C.S.; Adda, C.G.; Versteegen, E.; Jois, M.; Mathivanan, S. Bovine milk-derived exosomes from colostrum are enriched with proteins implicated in immune response and growth. Sci. Rep. 2017, 7, 5933. [Google Scholar] [CrossRef]
- Baier, S.R.; Nguyen, C.; Xie, F.; Wood, J.R.; Zempleni, J. MicroRNAs are absorbed in biologically meaningful amounts from nutritionally relevant doses of cow milk and affect gene expression in peripheral blood mononuclear cells, HEK-293 kidney cell cultures, and mouse livers. J. Nutr. 2014, 144, 1495–1500. [Google Scholar] [CrossRef]
- Ross, M.; Atalla, H.; Karrow, N.; Mallard, B.A. The bioactivity of colostrum and milk exosomes of high, average, and low immune responder cows on human intestinal epithelial cells. J. Dairy Sci. 2020, 104, 2499–2510. [Google Scholar] [CrossRef]
- Kirchner, B.; Buschmann, D.; Paul, V.; Pfaffl, M.W. Postprandial transfer of colostral extracellular vesicles and their protein and miRNA cargo in neonatal calves. PLoS ONE 2020, 15, e0229606. [Google Scholar] [CrossRef]
- Goudarzi, N.; Shabani, R.; Ebrahimi, M.; Baghestani, A.; Dehdashtian, E.; Vahabzadeh, G.; Soleimani, M.; Moradi, F.; Katebi, M. Comparative phenotypic characterization of human colostrum and breast milk-derived stem cells. Hum. Cell 2020, 33, 308–317. [Google Scholar] [CrossRef]
- Ghosh, A. Breast Milk Stem Cell Survival in Neonate’s Gut, Entery into Neonate Circulation and Adaption by the Body. Curr. Stem Cell Res. Ther. 2020, 15, 98–101. [Google Scholar] [CrossRef]
- Cacho, N.T.; Lawrence, R.M. Innate Immunity and Breast Milk. Front. Immunol. 2017, 8, 584. [Google Scholar] [CrossRef] [Green Version]
- Admyre, C.; Johansson, S.M.; Qazi, K.R.; Filén, J.J.; Lahesmaa, R.; Norman, M.; Neve, E.P.; Scheynius, A.; Gabrielsson, S. Exosomes with immune modulatory features are present in human breast milk. J. Immunol. 2007, 179, 1969–1978. [Google Scholar] [CrossRef]
- Martinez, J.A.; Ballew, M.P. Infant formulas. Pediatr. Rev. 2011, 32, 179–189. [Google Scholar] [CrossRef]
- Przyrembel, H.; Agostoni, C. Growing-up milk: A necessity or marketing? World Rev. Nutr. Diet. 2013, 108, 49–55. [Google Scholar] [CrossRef]
- Gomez, G.G.; Phillips, O.; Goforth, R.A. Effect of immunoglobulin source on survival, growth, and hematological and immunological variables in pigs. J. Anim. Sci. 1998, 76, 1–7. [Google Scholar] [CrossRef]
- Staak, C. Bovine colostrum and protection of young animals. Berl. Munch. Tierarztl. Wochenschr. 1992, 105, 219–224. [Google Scholar]
- Heidebrecht, H.J.; Weiss, W.J.; Pulse, M.; Lange, A.; Gisch, K.; Kliem, H.; Mann, S.; Pfaffl, M.W.; Kulozik, U.; von Eichel-Streiber, C. Treatment and Prevention of Recurrent Clostridium difficile Infection with Functionalized Bovine Antibody-Enriched Whey in a Hamster Primary Infection Model. Toxins 2019, 11, 98. [Google Scholar] [CrossRef] [Green Version]
- Lyerly, D.M.; Bostwick, E.F.; Binion, S.B.; Wilkins, T.D. Passive immunization of hamsters against disease caused by Clostridium difficile by use of bovine immunoglobulin G concentrate. Infect. Immun. 1991, 59, 2215–2218. [Google Scholar] [CrossRef] [Green Version]
- Satyaraj, E.; Reynolds, A.; Pelker, R.; Labuda, J.; Zhang, P.; Sun, P. Supplementation of diets with bovine colostrum influences immune function in dogs. Br. J. Nutr. 2013, 110, 2216–2221. [Google Scholar] [CrossRef] [Green Version]
- Casal, M.L.; Jezyk, P.F.; Giger, U. Transfer of colostral antibodies from queens to their kittens. Am. J. Vet. Res. 1996, 57, 1653–1658. [Google Scholar] [PubMed]
- Kirkden, R.D.; Broom, D.M.; Andersen, I.L. Invited review: Piglet mortality: Management solutions. J. Anim. Sci. 2013, 91, 3361–3389. [Google Scholar] [CrossRef]
- Blencowe, H.; Cousens, S.; Chou, D.; Oestergaard, M.; Say, L.; Moller, A.B.; Kinney, M.; Lawn, J. Born too soon: The global epidemiology of 15 million preterm births. Reprod. Health 2013, 10 (Suppl. S1), S2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lawn, J.E.; Blencowe, H.; Waiswa, P.; Amouzou, A.; Mathers, C.; Hogan, D.; Flenady, V.; Frøen, J.F.; Qureshi, Z.U.; Calderwood, C.; et al. Stillbirths: Rates, risk factors, and acceleration towards 2030. Lancet 2016, 387, 587–603. [Google Scholar] [CrossRef] [Green Version]
- Lee, A.C.; Katz, J.; Blencowe, H.; Cousens, S.; Kozuki, N.; Vogel, J.P.; Adair, L.; Baqui, A.H.; Bhutta, Z.A.; Caulfield, L.E.; et al. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob. Health 2013, 1, e26–e36. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Juhl, S.M.; Ye, X.; Shen, R.L.; Iyore, E.O.; Dai, Y.; Sangild, P.T.; Greisen, G.O. A Stepwise, Pilot Study of Bovine Colostrum to Supplement the First Enteral Feeding in Preterm Infants (Precolos): Study Protocol and Initial Results. Front. Pediatr. 2017, 5, 42. [Google Scholar] [CrossRef] [PubMed]
- Juhl, S.M.; Ye, X.; Zhou, P.; Li, Y.; Iyore, E.O.; Zhang, L.; Jiang, P.; van Goudoever, J.B.; Greisen, G.; Sangild, P.T. Bovine Colostrum for Preterm Infants in the First Days of Life: A Randomized Controlled Pilot Trial. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 471–478. [Google Scholar] [CrossRef]
- Jiang, P.P.; Muk, T.; Krych, L.; Nielsen, D.S.; Khakimov, B.; Li, Y.; Juhl, S.M.; Greisen, G.; Sangild, P.T. Gut colonization in preterm infants supplemented with bovine colostrum in the first week of life: An explorative pilot study. J. Parenter. Enter. Nutr. 2021. [Google Scholar] [CrossRef] [PubMed]
- Hutchens, T.W.; Henry, J.F.; Yip, T.T. Structurally intact (78-kDa) forms of maternal lactoferrin purified from urine of preterm infants fed human milk: Identification of a trypsin-like proteolytic cleavage event in vivo that does not result in fragment dissociation. Proc. Natl. Acad. Sci. USA 1991, 88, 2994–2998. [Google Scholar] [CrossRef] [Green Version]
- Burrin, D.; Sangild, P.T.; Stoll, B.; Thymann, T.; Buddington, R.; Marini, J.; Olutoye, O.; Shulman, R.J. Translational Advances in Pediatric Nutrition and Gastroenterology: New Insights from Pig Models. Annu. Rev. Anim. Biosci. 2020, 8, 321–354. [Google Scholar] [CrossRef] [Green Version]
- Sangild, P.T.; Thymann, T.; Schmidt, M.; Stoll, B.; Burrin, D.G.; Buddington, R.K. Invited review: The preterm pig as a model in pediatric gastroenterology. J. Anim. Sci. 2013, 91, 4713–4729. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Odle, J.; Lin, X.; Jacobi, S.K.; Kim, S.W.; Stahl, C.H. The suckling piglet as an agrimedical model for the study of pediatric nutrition and metabolism. Annu. Rev. Anim. Biosci. 2014, 2, 419–444. [Google Scholar] [CrossRef]
- Sangild, P.T.; Petersen, Y.M.; Schmidt, M.; Elnif, J.; Petersen, T.K.; Buddington, R.K.; Greisen, G.; Michaelsen, K.F.; Burrin, D.G. Preterm birth affects the intestinal response to parenteral and enteral nutrition in newborn pigs. J. Nutr. 2002, 132, 3786–3794. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bjornvad, C.R.; Schmidt, M.; Petersen, Y.M.; Jensen, S.K.; Offenberg, H.; Elnif, J.; Sangild, P.T. Preterm birth makes the immature intestine sensitive to feeding-induced intestinal atrophy. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2005, 289, R1212–R1222. [Google Scholar] [CrossRef] [PubMed]
- Sangild, P.T.; Siggers, R.H.; Schmidt, M.; Elnif, J.; Bjornvad, C.R.; Thymann, T.; Grondahl, M.L.; Hansen, A.K.; Jensen, S.K.; Boye, M.; et al. Diet- and colonization-dependent intestinal dysfunction predisposes to necrotizing enterocolitis in preterm pigs. Gastroenterology 2006, 130, 1776–1792. [Google Scholar] [CrossRef]
- Bjornvad, C.R.; Thymann, T.; Deutz, N.E.; Burrin, D.G.; Jensen, S.K.; Jensen, B.B.; Mølbak, L.; Boye, M.; Larsson, L.I.; Schmidt, M.; et al. Enteral feeding induces diet-dependent mucosal dysfunction, bacterial proliferation, and necrotizing enterocolitis in preterm pigs on parenteral nutrition. Am. J. Physiol. Gastrointest. Liver Physiol. 2008, 295, G1092–G1103. [Google Scholar] [CrossRef]
- Bæk, O.; Brunse, A.; Nguyen, D.N.; Moodley, A.; Thymann, T.; Sangild, P.T. Diet Modulates the High Sensitivity to Systemic Infection in Newborn Preterm Pigs. Front. Immunol. 2020, 11, 1019. [Google Scholar] [CrossRef] [PubMed]
- Brunse, A.; Worsøe, P.; Pors, S.E.; Skovgaard, K.; Sangild, P.T. Oral Supplementation With Bovine Colostrum Prevents Septic Shock and Brain Barrier Disruption During Bloodstream Infection in Preterm Newborn Pigs. Shock 2019, 51, 337–347. [Google Scholar] [CrossRef] [PubMed]
- Ren, S.; Hui, Y.; Obelitz-Ryom, K.; Brandt, A.B.; Kot, W.; Nielsen, D.S.; Thymann, T.; Sangild, P.T.; Nguyen, D.N. Neonatal gut and immune maturation is determined more by postnatal age than by postconceptional age in moderately preterm pigs. Am. J. Physiol. Gastrointest. Liver Physiol. 2018, 315, G855–G867. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hansen, C.F.; Thymann, T.; Andersen, A.D.; Holst, J.J.; Hartmann, B.; Hilsted, L.; Langhorn, L.; Jelsing, J.; Sangild, P.T. Rapid gut growth but persistent delay in digestive function in the postnatal period of preterm pigs. Am. J. Physiol. Gastrointest. Liver Physiol. 2016, 310, G550–G560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersen, A.D.; Sangild, P.T.; Munch, S.L.; van der Beek, E.M.; Renes, I.B.; Ginneken, C.; Greisen, G.O.; Thymann, T. Delayed growth, motor function and learning in preterm pigs during early postnatal life. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2016, 310, R481–R492. [Google Scholar] [CrossRef] [Green Version]
- Bergström, A.; Kaalund, S.S.; Skovgaard, K.; Andersen, A.D.; Pakkenberg, B.; Rosenørn, A.; van Elburg, R.M.; Thymann, T.; Greisen, G.O.; Sangild, P.T. Limited effects of preterm birth and the first enteral nutrition on cerebellum morphology and gene expression in piglets. Physiol. Rep. 2016, 4, e12871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cao, M.; Andersen, A.D.; Van Ginneken, C.; Shen, R.L.; Petersen, S.O.; Thymann, T.; Jing, J.; Sangild, P.T. Physical activity level is impaired and diet dependent in preterm newborn pigs. Pediatr. Res. 2015, 78, 137–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holme Nielsen, C.; Bladt Brandt, A.; Thymann, T.; Obelitz-Ryom, K.; Jiang, P.; Vanden Hole, C.; van Ginneken, C.; Pankratova, S.; Sangild, P.T. Rapid Postnatal Adaptation of Neurodevelopment in Pigs Born Late Preterm. Dev. Neurosci. 2018, 40, 586–600. [Google Scholar] [CrossRef]
- Jensen, M.L.; Sangild, P.T.; Lykke, M.; Schmidt, M.; Boye, M.; Jensen, B.B.; Thymann, T. Similar efficacy of human banked milk and bovine colostrum to decrease incidence of necrotizing enterocolitis in preterm piglets. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2013, 305, R4–R12. [Google Scholar] [CrossRef] [Green Version]
- Rasmussen, S.O.; Martin, L.; Østergaard, M.V.; Rudloff, S.; Li, Y.; Roggenbuck, M.; Bering, S.B.; Sangild, P.T. Bovine colostrum improves neonatal growth, digestive function, and gut immunity relative to donor human milk and infant formula in preterm pigs. Am. J. Physiol. Gastrointest. Liver Physiol. 2016, 311, G480–G491. [Google Scholar] [CrossRef] [Green Version]
- Oosterloo, B.C.; Premkumar, M.; Stoll, B.; Olutoye, O.; Thymann, T.; Sangild, P.T.; Burrin, D.G. Dual purpose use of preterm piglets as a model of pediatric GI disease. Vet. Immunol. Immunopathol. 2014, 159, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Bæk, O.; Cilieborg, M.S.; Bering, S.B.; Nguyen, D.N.; Thymann, T.; Sangild, P.T. Sex-specific survival, growth, immunity and organ development in preterm pigs as models for immature newborns. Front. Pediatr. 2021, 9, 63. [Google Scholar] [CrossRef] [PubMed]
- Meder, U.; Tarjanyi, E.; Kovacs, K.; Szakmar, E.; Cseko, A.J.; Hazay, T.; Belteki, G.; Szabo, M.; Jermendy, A. Cerebral oxygenation in preterm infants during maternal singing combined with skin-to-skin care. Pediatr. Res. 2020. [Google Scholar] [CrossRef]
- Brunse, A.; Peng, Y.; Li, Y.; Lykkesfeldt, J.; Sangild, P.T. Co-bedding of preterm newborn pigs reduces necrotizing enterocolitis incidence independent of vital functions and cortisol levels. Front. Pediatr. 2021, 9, 216. [Google Scholar] [CrossRef] [PubMed]
- Reed, R.C.; Johnson, D.E.; Nie, A.M. Preterm Infant Skin Structure Is Qualitatively and Quantitatively Different from That of Term Newborns. Pediatr. Dev. Pathol. 2021, 24, 96–102. [Google Scholar] [CrossRef]
- Li, J.; Xu, Y.W.; Jiang, J.J.; Song, Q.K. Bovine colostrum and product intervention associated with relief of childhood infectious diarrhea. Sci. Rep. 2019, 9, 3093. [Google Scholar] [CrossRef]
- Barakat, S.H.; Meheissen, M.A.; Omar, O.M.; Elbana, D.A. Bovine Colostrum in the Treatment of Acute Diarrhea in Children: A Double-Blinded Randomized Controlled Trial. J. Trop. Pediatr. 2020, 66, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Premkumar, M.H.; Massieu, L.A.; Anderson, D.M.; Gokulakrishnan, G. Human Milk Supplements: Principles, Practices, and Current Controversies. Clin. Perinatol. 2020, 47, 355–368. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Li, Y.; Nguyen, D.N.; Mortensen, M.S.; van den Akker, C.H.P.; Skeath, T.; Pors, S.E.; Pankratova, S.; Rudloff, S.; Sørensen, S.J.; et al. Nutrient Fortification of Human Donor Milk Affects Intestinal Function and Protein Metabolism in Preterm Pigs. J. Nutr. 2018, 148, 336–347. [Google Scholar] [CrossRef] [Green Version]
- Sun, J.; Li, Y.; Pan, X.; Nguyen, D.N.; Brunse, A.; Bojesen, A.M.; Rudloff, S.; Mortensen, M.S.; Burrin, D.G.; Sangild, P.T. Human Milk Fortification with Bovine Colostrum Is Superior to Formula-Based Fortifiers to Prevent Gut Dysfunction, Necrotizing Enterocolitis, and Systemic Infection in Preterm Pigs. J. Parenter. Enter. Nutr. 2019, 43, 252–262. [Google Scholar] [CrossRef] [PubMed]
- Boudry, C.; Buldgen, A.; Portetelle, D.; Collard, A.; Théwis, A.; Dehoux, J.P. Effects of oral supplementation with bovine colostrum on the immune system of weaned piglets. Res. Vet. Sci. 2007, 83, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Boudry, C.; Dehoux, J.P.; Wavreille, J.; Portetelle, D.; Théwis, A.; Buldgen, A. Effect of a bovine colostrum whey supplementation on growth performance, faecal Escherichia coli population and systemic immune response of piglets at weaning. Animal 2008, 2, 730–737. [Google Scholar] [CrossRef] [Green Version]
- Poulsen, A.R.; de Jonge, N.; Sugiharto, S.; Nielsen, J.L.; Lauridsen, C.; Canibe, N. The microbial community of the gut differs between piglets fed sow milk, milk replacer or bovine colostrum. Br. J. Nutr. 2017, 117, 964–978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sugiharto, S.; Poulsen, A.S.; Canibe, N.; Lauridsen, C. Effect of bovine colostrum feeding in comparison with milk replacer and natural feeding on the immune responses and colonisation of enterotoxigenic Escherichia coli in the intestinal tissue of piglets. Br. J. Nutr. 2015, 113, 923–934. [Google Scholar] [CrossRef] [Green Version]
- Huguet, A.; Le Dividich, J.; Le Huërou-Luron, I. Improvement of growth performance and sanitary status of weaned piglets fed a bovine colostrum-supplemented diet. J. Anim. Sci. 2012, 90, 1513–1520. [Google Scholar] [CrossRef]
- Lallès, J.P.; Bosi, P.; Janczyk, P.; Koopmans, S.J.; Torrallardona, D. Impact of bioactive substances on the gastrointestinal tract and performance of weaned piglets: A review. Animal 2009, 3, 1625–1643. [Google Scholar] [CrossRef] [Green Version]
- Hilpert, H.; Brussow, H.; Mietens, C.; Sidoti, J.; Lerner, L.; Werchau, H. Use of bovine milk concentrate containing antibody to rotavirus to treat rotavirus gastroenteritis in infants. J. Infect. Dis. 1987, 156, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Mitra, A.K.; Mahalanabis, D.; Ashraf, H.; Unicomb, L.; Eeckels, R.; Tzipori, S. Hyperimmune cow colostrum reduces diarrhoea due to rotavirus: A double-blind, controlled clinical trial. Acta Paediatr. 1995, 84, 996–1001. [Google Scholar] [CrossRef] [PubMed]
- Sarker, S.A.; Casswall, T.H.; Mahalanabis, D.; Alam, N.H.; Albert, M.J.; Brussow, H.; Fuchs, G.J.; Hammerstrom, L. Successful treatment of rotavirus diarrhea in children with immunoglobulin from immunized bovine colostrum. Pediatr. Infect. Dis. J. 1998, 17, 1149–1154. [Google Scholar] [CrossRef]
- Ylitalo, S.; Uhari, M.; Rasi, S.; Pudas, J.; Leppaluoto, J. Rotaviral antibodies in the treatment of acute rotaviral gastroenteritis. Acta Paediatr. 1998, 87, 264–267. [Google Scholar] [CrossRef]
- Mietens, C.; Keinhorst, H.; Hilpert, H.; Gerber, H.; Amster, H.; Pahud, J.J. Treatment of infantile E. coli gastroenteritis with specific bovine anti-E. coli milk immunoglobulins. Eur. J. Pediatr. 1979, 132, 239–252. [Google Scholar] [CrossRef] [PubMed]
- Casswall, T.H.; Sarker, S.A.; Faruque, S.M.; Weintraub, A.; Albert, M.J.; Fuchs, G.J.; Alam, N.H.; Dahlstrom, A.K.; Link, H.; Brussow, H.; et al. Treatment of enterotoxigenic and enteropathogenic Escherichia coli-induced diarrhoea in children with bovine immunoglobulin milk concentrate from hyperimmunized cows: A double-blind, placebo-controlled, clinical trial. Scand. J. Gastroenterol. 2000, 35, 711–718. [Google Scholar] [CrossRef]
- Huppertz, H.I.; Rutkowski, S.; Busch, D.H.; Eisebit, R.; Lissner, R.; Karch, H. Bovine colostrum ameliorates diarrhea in infection with diarrheagenic Escherichia coli, shiga toxin-producing E. Coli, and E. coli expressing intimin and hemolysin. J. Pediatr. Gastroenterol. Nutr. 1999, 29, 452–456. [Google Scholar] [CrossRef] [PubMed]
- Ashraf, H.; Mahalanabis, D.; Mitra, A.K.; Tzipori, S.; Fuchs, G.J. Hyperimmune bovine colostrum in the treatment of shigellosis in children: A double-blind, randomized, controlled trial. Acta Paediatr. 2001, 90, 1373–1378. [Google Scholar] [CrossRef]
- Ebina, T.; Sato, A.; Umezu, K.; Ishida, N.; Ohyama, S.; Ohizumi, A.; Aikawa, K.; Katagiri, S.; Katsushima, N.; Imai, A.; et al. Prevention of rotavirus infection by cow colostrum antibody against human rotaviruses. Lancet 1983, 2, 1029–1030. [Google Scholar] [CrossRef]
- Davidson, G.P.; Whyte, P.B.; Daniels, E.; Franklin, K.; Nunan, H.; McCloud, P.I.; Moore, A.G.; Moore, D.J. Passive immunisation of children with bovine colostrum containing antibodies to human rotavirus. Lancet 1989, 2, 709–712. [Google Scholar] [CrossRef]
- Turner, R.B.; Kelsey, D.K. Passive immunization for prevention of rotavirus illness in healthy infants. Pediatr. Infect. Dis. J. 1993, 12, 718–722. [Google Scholar] [CrossRef]
- Brunser, O.; Espinoza, J.; Figueroa, G.; Araya, M.; Spencer, E.; Hilpert, H.; Link-Amster, H.; Brussow, H. Field trial of an infant formula containing anti-rotavirus and anti-Escherichia coli milk antibodies from hyperimmunized cows. J. Pediatr. Gastroenterol. Nutr. 1992, 15, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Den Hartog, G.; Jacobino, S.; Bont, L.; Cox, L.; Ulfman, L.H.; Leusen, J.H.; van Neerven, R.J. Specificity and Effector Functions of Human RSV-Specific IgG from Bovine Milk. PLoS ONE 2014, 9, e112047. [Google Scholar] [CrossRef] [Green Version]
- Loss, G.; Depner, M.; Ulfman, L.H.; van Neerven, R.J.; Hose, A.J.; Genuneit, J.; Karvonen, A.M.; Hyvärinen, A.; Kaulek, V.; Roduit, C.; et al. Consumption of unprocessed cow’s milk protects infants from common respiratory infections. J. Allergy Clin. Immunol. 2015, 135, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Von Mutius, E.; Vercelli, D. Farm living: Effects on childhood asthma and allergy. Nat. Rev. Immunol. 2010, 10, 861–868. [Google Scholar] [CrossRef]
- Roselli, M.; Britti, M.S.; Le Huërou-Luron, I.; Marfaing, H.; Zhu, W.Y.; Mengheri, E. Effect of different plant extracts and natural substances (PENS) against membrane damage induced by enterotoxigenic Escherichia coli K88 in pig intestinal cells. Toxicol. In Vitro 2007, 21, 224–229. [Google Scholar] [CrossRef]
- De Waard, M.; Li, Y.; Zhu, Y.; Ayede, A.I.; Berrington, J.; Bloomfield, F.H.; Busari, O.O.; Cormack, B.E.; Embleton, N.D.; van Goudoever, J.B.; et al. Time to Full Enteral Feeding for Very Low-Birth-Weight Infants Varies Markedly Among Hospitals Worldwide But May Not Be Associated With Incidence of Necrotizing Enterocolitis: The NEOMUNE-NeoNutriNet Cohort Study. J. Parenter. Enter. Nutr. 2019, 43, 658–667. [Google Scholar] [CrossRef] [PubMed]
- Sadeghirad, B.; Morgan, R.L.; Zeraatkar, D.; Zea, A.M.; Couban, R.; Johnston, B.C.; Florez, I.D. Human and Bovine Colostrum for Prevention of Necrotizing Enterocolitis: A Meta-analysis. Pediatrics 2018, 142. [Google Scholar] [CrossRef]
- Ahnfeldt, A.M.; Hyldig, N.; Li, Y.; Kappel, S.S.; Aunsholdt, L.; Sangild, P.T.; Zachariassen, G. FortiColos—A multicentre study using bovine colostrum as a fortifier to human milk in very preterm infants: Study protocol for a randomised controlled pilot trial. Trials 2019, 20, 279. [Google Scholar] [CrossRef]
- Brooks, H.J.; McConnell, M.A.; Corbett, J.; Buchan, G.S.; Fitzpatrick, C.E.; Broadbent, R.S. Potential prophylactic value of bovine colostrum in necrotizing enterocolitis in neonates: An in vitro study on bacterial attachment, antibody levels and cytokine production. FEMS Immunol. Med. Microbiol. 2006, 48, 347–354. [Google Scholar] [CrossRef] [Green Version]
- Balachandran, B.; Dutta, S.; Singh, R.; Prasad, R.; Kumar, P. Bovine Colostrum in Prevention of Necrotizing Enterocolitis and Sepsis in Very Low Birth Weight Neonates: A Randomized, Double-blind, Placebo-controlled Pilot Trial. J. Trop. Pediatr. 2017, 63, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Ismail, R.I.H.; Awad, H.A.; Imam, S.S.; Gad, G.I.; Aboushady, N.M.; Abdou, R.M.; Eissa, D.S.; Azzam, N.T.; Barakat, M.M.; Yassin, M.M.; et al. Gut priming with bovine colostrum and T regulatory cells in preterm neonates: A randomized controlled trial. Pediatr. Res. 2021. [Google Scholar] [CrossRef]
- Eibl, M.M.; Wolf, H.M.; Furnkranz, H.; Rosenkranz, A. Prevention of necrotizing enterocolitis in low-birth-weight infants by IgA-IgG feeding. N. Engl. J. Med. 1988, 319, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, G.; Tudehope, D.; Baumann, K.; Jeffery, H.; Gill, A.; Cole, M.; Drew, J.; McPhee, A.; Ratcliffe, J.; Reynolds, G.; et al. Enteral human IgG for prevention of necrotising enterocolitis: A placebo-controlled, randomised trial. Lancet 2001, 357, 2090–2094. [Google Scholar] [CrossRef]
- Rubaltelli, F.F.; Benini, F.; Sala, M. Prevention of necrotizing enterocolitis in neonates at risk by oral administration of monomeric IgG. Dev. Pharmacol. Ther. 1991, 17, 138–143. [Google Scholar] [CrossRef]
- Fast, C.; Rosegger, H. Necrotizing enterocolitis prophylaxis: Oral antibiotics and lyophilized enterobacteria vs. oral immunoglobulins. Acta Paediatr. 1994, 83, 86–90. [Google Scholar] [CrossRef]
- Richter, D.; Bartmann, P.; Pohlandt, F. Prevention of necrotizing enterocolitis in extremely low birth weight infants by IgG feeding? Eur. J. Pediatr. 1998, 157, 924–925. [Google Scholar] [CrossRef] [PubMed]
- Foster, J.P.; Seth, R.; Cole, M.J. Oral immunoglobulin for preventing necrotizing enterocolitis in preterm and low birth weight neonates. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef] [Green Version]
- Siggers, J.; Sangild, P.T.; Jensen, T.K.; Siggers, R.H.; Skovgaard, K.; Støy, A.C.; Jensen, B.B.; Thymann, T.; Bering, S.B.; Boye, M. Transition from parenteral to enteral nutrition induces immediate diet-dependent gut histological and immunological responses in preterm neonates. Am. J. Physiol. Gastrointest. Liver Physiol. 2011, 301, G435–G445. [Google Scholar] [CrossRef]
- Danielsen, M.; Thymann, T.; Jensen, B.B.; Jensen, O.N.; Sangild, P.T.; Bendixen, E. Proteome profiles of mucosal immunoglobulin uptake in inflamed porcine gut. Proteomics 2006, 6, 6588–6596. [Google Scholar] [CrossRef] [PubMed]
- Che, L.; Thymann, T.; Bering, S.B.; Le Huerou-Luron, I.; D’inca, R.; Zhang, K.; Sangild, P.T. IUGR does not predispose to necrotizing enterocolitis or compromise postnatal intestinal adaptation in preterm pigs. Pediatr. Res. 2010, 67, 54–59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cilieborg, M.S.; Boye, M.; Mølbak, L.; Thymann, T.; Sangild, P.T. Preterm birth and necrotizing enterocolitis alter gut colonization in pigs. Pediatr. Res. 2011, 69, 10–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cilieborg, M.S.; Boye, M.; Thymann, T.; Jensen, B.B.; Sangild, P.T. Diet-dependent effects of minimal enteral nutrition on intestinal function and necrotizing enterocolitis in preterm pigs. J. Parenter. Enter. Nutr. 2011, 35, 32–42. [Google Scholar] [CrossRef]
- Li, Y.; Jensen, M.L.; Chatterton, D.E.; Jensen, B.B.; Thymann, T.; Kvistgaard, A.S.; Sangild, P.T. Raw bovine milk improves gut responses to feeding relative to infant formula in preterm piglets. Am. J. Physiol. Gastrointest. Liver Physiol. 2014, 306, G81–G90. [Google Scholar] [CrossRef]
- Li, Y.; Østergaard, M.V.; Jiang, P.; Chatterton, D.E.; Thymann, T.; Kvistgaard, A.S.; Sangild, P.T. Whey protein processing influences formula-induced gut maturation in preterm pigs. J. Nutr. 2013, 143, 1934–1942. [Google Scholar] [CrossRef] [Green Version]
- Møller, H.K.; Thymann, T.; Fink, L.N.; Frokiaer, H.; Kvistgaard, A.S.; Sangild, P.T. Bovine colostrum is superior to enriched formulas in stimulating intestinal function and necrotising enterocolitis resistance in preterm pigs. Br. J. Nutr. 2011, 105, 44–53. [Google Scholar] [CrossRef] [Green Version]
- Oste, M.; Van Ginneken, C.J.; Van Haver, E.R.; Bjornvad, C.R.; Thymann, T.; Sangild, P.T. The intestinal trophic response to enteral food is reduced in parenterally fed preterm pigs and is associated with more nitrergic neurons. J. Nutr. 2005, 135, 2657–2663. [Google Scholar] [CrossRef] [Green Version]
- Oste, M.; Van Haver, E.; Thymann, T.; Sangild, P.; Weyns, A.; Van Ginneken, C.J. Formula induces intestinal apoptosis in preterm pigs within a few hours of feeding. J. Parenter. Enter. Nutr. 2010, 34, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Shen, R.L.; Thymann, T.; Østergaard, M.V.; Støy, A.C.; Krych, Ł.; Nielsen, D.S.; Lauridsen, C.; Hartmann, B.; Holst, J.J.; Burrin, D.G.; et al. Early gradual feeding with bovine colostrum improves gut function and NEC resistance relative to infant formula in preterm pigs. Am. J. Physiol. Gastrointest. Liver Physiol. 2015, 309, G310–G323. [Google Scholar] [CrossRef]
- Siggers, J.; Ostergaard, M.V.; Siggers, R.H.; Skovgaard, K.; Mølbak, L.; Thymann, T.; Schmidt, M.; Møller, H.K.; Purup, S.; Fink, L.N.; et al. Postnatal amniotic fluid intake reduces gut inflammatory responses and necrotizing enterocolitis in preterm neonates. Am. J. Physiol. Gastrointest. Liver Physiol. 2013, 304, G864–G875. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siggers, R.H.; Thymann, T.; Jensen, B.B.; Mølbak, L.; Heegaard, P.M.; Schmidt, M.; Buddington, R.K.; Sangild, P.T. Elective cesarean delivery affects gut maturation and delays microbial colonization but does not increase necrotizing enterocolitis in preterm pigs. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2008, 294, R929–R938. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sty, A.C.; Sangild, P.T.; Skovgaard, K.; Thymann, T.; Bjerre, M.; Chatterton, D.E.; Purup, S.; Boye, M.; Heegaard, P.M. Spray Dried, Pasteurised Bovine Colostrum Protects Against Gut Dysfunction and Inflammation in Preterm Pigs. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 280–287. [Google Scholar] [CrossRef] [Green Version]
- Støy, A.C.; Heegaard, P.M.; Thymann, T.; Bjerre, M.; Skovgaard, K.; Boye, M.; Stoll, B.; Schmidt, M.; Jensen, B.B.; Sangild, P.T. Bovine colostrum improves intestinal function following formula-induced gut inflammation in preterm pigs. Clin. Nutr. 2014, 33, 322–329. [Google Scholar] [CrossRef]
- Van Haver, E.R.; de Vooght, L.; Oste, M.; Sangild, P.T.; Thymann, T.; Weyns, A.L.; van Ginneken, C.J. Postnatal and diet-dependent increases in enteric glial cells and VIP-containing neurones in preterm pigs. Neurogastroenterol. Motil. 2008, 20, 1070–1079. [Google Scholar] [CrossRef]
- Van Haver, E.R.; Oste, M.; Thymann, T.; Sys, S.U.; Lamers, W.H.; Weyns, A.L.; Sangild, P.T.; van Ginneken, C.J. Enteral feeding reduces endothelial nitric oxide synthase in the caudal intestinal microvasculature of preterm piglets. Pediatr. Res. 2008, 63, 137–142. [Google Scholar] [CrossRef] [Green Version]
- Van Haver, E.R.; Sangild, P.T.; Oste, M.; Siggers, J.L.; Weyns, A.L.; Van Ginneken, C.J. Diet-dependent mucosal colonization and interleukin-1beta responses in preterm pigs susceptible to necrotizing enterocolitis. J. Pediatr. Gastroenterol. Nutr. 2009, 49, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Willems, R.; Krych, L.; Rybicki, V.; Jiang, P.; Sangild, P.T.; Shen, R.L.; Hensel, K.O.; Wirth, S.; Postberg, J.; Jenke, A.C. Introducing enteral feeding induces intestinal subclinical inflammation and respective chromatin changes in preterm pigs. Epigenomics 2015, 7, 553–565. [Google Scholar] [CrossRef] [Green Version]
- Ren, S.; Hui, Y.; Goericke-Pesch, S.; Pankratova, S.; Kot, W.; Pan, X.; Thymann, T.; Sangild, P.T.; Nguyen, D.N. Gut and immune effects of bioactive milk factors in preterm pigs exposed to prenatal inflammation. Am. J. Physiol. Gastrointest. Liver Physiol. 2019, 317, G67–G77. [Google Scholar] [CrossRef]
- Li, Y.; Pan, X.; Nguyen, D.N.; Ren, S.; Moodley, A.; Sangild, P.T. Bovine Colostrum Before or After Formula Feeding Improves Systemic Immune Protection and Gut Function in Newborn Preterm Pigs. Front. Immunol. 2019, 10, 3062. [Google Scholar] [CrossRef] [Green Version]
- Yan, X.; Sangild, P.T.; Peng, Y.; Li, Y.; Bering, S.B.; Pan, X. Supplementary bovine colostrum feeding to formula-fed preterm pigs improves gut function and reduces necrotizing enterocolitis. J. Pediatr. Gastroenterol. Nutr. 2021. [Google Scholar] [CrossRef]
- Buddington, R.K.; Bering, S.B.; Thymann, T.; Sangild, P.T. Aldohexose malabsorption in preterm pigs is directly related to the severity of necrotizing enterocolitis. Pediatr. Res. 2008, 63, 382–387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oste, M.; De Vos, M.; Van Haver, E.; Van Brantegem, L.; Thymann, T.; Sangild, P.; Weyns, A.; Van Ginneken, C. Parenteral and enteral feeding in preterm piglets differently affects extracellular matrix proteins, enterocyte proliferation and apoptosis in the small intestine. Br. J. Nutr. 2010, 104, 989–997. [Google Scholar] [CrossRef] [Green Version]
- Puiman, P.J.; Jensen, M.; Stoll, B.; Renes, I.B.; de Bruijn, A.C.; Dorst, K.; Schierbeek, H.; Schmidt, M.; Boehm, G.; Burrin, D.G.; et al. Intestinal threonine utilization for protein and mucin synthesis is decreased in formula-fed preterm pigs. J. Nutr. 2011, 141, 1306–1311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cilieborg, M.S.; Boye, M.; Sangild, P.T. Bacterial colonization and gut development in preterm neonates. Early Hum. Dev. 2012, 88 (Suppl. S1), S41–S49. [Google Scholar] [CrossRef] [PubMed]
- Wolfs, T.G.; Jellema, R.K.; Turrisi, G.; Becucci, E.; Buonocore, G.; Kramer, B.W. Inflammation-induced immune suppression of the fetus: A potential link between chorioamnionitis and postnatal early onset sepsis. J. Matern. Fetal Neonatal Med. 2012, 25 (Suppl. S1), 8–11. [Google Scholar] [CrossRef] [PubMed]
- Ophelders, D.; Gussenhoven, R.; Klein, L.; Jellema, R.K.; Westerlaken, R.J.J.; Hütten, M.C.; Vermeulen, J.; Wassink, G.; Gunn, A.J.; Wolfs, T. Preterm Brain Injury, Antenatal Triggers, and Therapeutics: Timing Is Key. Cells 2020, 9, 1871. [Google Scholar] [CrossRef]
- Gussenhoven, R.; Westerlaken, R.J.J.; Ophelders, D.; Jobe, A.H.; Kemp, M.W.; Kallapur, S.G.; Zimmermann, L.J.; Sangild, P.T.; Pankratova, S.; Gressens, P.; et al. Chorioamnionitis, neuroinflammation, and injury: Timing is key in the preterm ovine fetus. J. Neuroinflamm. 2018, 15, 113. [Google Scholar] [CrossRef] [PubMed]
- Cilieborg, M.S.; Schmidt, M.; Skovgaard, K.; Boye, M.; Weber, N.R.; Heegaard, P.M.; Burrin, D.G.; Sangild, P.T. Fetal lipopolysaccharide exposure modulates diet-dependent gut maturation and sensitivity to necrotising enterocolitis in pre-term pigs. Br. J. Nutr. 2011, 106, 852–861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coggins, S.A.; Laskin, B.; Harris, M.C.; Grundmeier, R.W.; Passarella, M.; McKenna, K.J.; Srinivasan, L. Acute Kidney Injury Associated with Late-Onset Neonatal Sepsis: A Matched Cohort Study. J. Pediatr. 2021, 231, 185–192. [Google Scholar] [CrossRef]
- Gao, X.; Li, Y.; Olin, A.B.; Nguyen, D.N. Fortification with bovine colostrum enhances antibacterial activity of human milk. J. Parenter. Enter. Nutr. 2020. [Google Scholar] [CrossRef]
- Harbeson, D.; Francis, F.; Bao, W.; Amenyogbe, N.A.; Kollmann, T.R. Energy Demands of Early Life Drive a Disease Tolerant Phenotype and Dictate Outcome in Neonatal Bacterial Sepsis. Front. Immunol. 2018, 9, 1918. [Google Scholar] [CrossRef]
- Trend, S.; Strunk, T.; Hibbert, J.; Kok, C.H.; Zhang, G.; Doherty, D.A.; Richmond, P.; Burgner, D.; Simmer, K.; Davidson, D.J.; et al. Antimicrobial protein and Peptide concentrations and activity in human breast milk consumed by preterm infants at risk of late-onset neonatal sepsis. PLoS ONE 2015, 10, e0117038. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Nguyen, D.N.; de Waard, M.; Christensen, L.; Zhou, P.; Jiang, P.; Sun, J.; Bojesen, A.M.; Lauridsen, C.; Lykkesfeldt, J.; et al. Pasteurization Procedures for Donor Human Milk Affect Body Growth, Intestinal Structure, and Resistance against Bacterial Infections in Preterm Pigs. J. Nutr. 2017, 147, 1121–1130. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, D.N.; Currie, A.; Ren, S.; Bering, S.; Sangild, P. Heat treatment and irradiation reduce anti-bacterial and immune-modulatory properties of bovine colostrum. J. Funct. Foods 2019, 57, 182–189. [Google Scholar] [CrossRef]
- Playford, R.J.; Garbowsky, M.; Marchbank, T. Pasteurized Chicken Egg Powder Stimulates Proliferation and Migration of AGS, RIE1, and Caco-2 Cells and Reduces NSAID-Induced Injury in Mice and Colitis in Rats. J. Nutr. 2020, 150, 1434–1442. [Google Scholar] [CrossRef] [PubMed]
- Ye, Y.; Manne, S.; Treem, W.R.; Bennett, D. Prevalence of Inflammatory Bowel Disease in Pediatric and Adult Populations: Recent Estimates from Large National Databases in the United States, 2007–2016. Inflamm. Bowel Dis. 2020, 26, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Cucinotta, U.; Romano, C.; Dipasquale, V. Diet and Nutrition in Pediatric Inflammatory Bowel Diseases. Nutrients 2021, 13, 655. [Google Scholar] [CrossRef] [PubMed]
- Khan, Z.; Macdonald, C.; Wicks, A.C.; Holt, M.P.; Floyd, D.; Ghosh, S.; Wright, N.A.; Playford, R.J. Use of the ‘nutriceutical’, bovine colostrum, for the treatment of distal colitis: Results from an initial study. Aliment. Pharmacol. Ther. 2002, 16, 1917–1922. [Google Scholar] [CrossRef]
- Bodammer, P.; Kerkhoff, C.; Maletzki, C.; Lamprecht, G. Bovine colostrum increases pore-forming claudin-2 protein expression but paradoxically not ion permeability possibly by a change of the intestinal cytokine milieu. PLoS ONE 2013, 8, e64210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Filipescu, I.E.; Leonardi, L.; Menchetti, L.; Guelfi, G.; Traina, G.; Casagrande-Proietti, P.; Piro, F.; Quattrone, A.; Barbato, O.; Brecchia, G. Preventive effects of bovine colostrum supplementation in TNBS-induced colitis in mice. PLoS ONE 2018, 13, e0202929. [Google Scholar] [CrossRef]
- Sangild, P.T.; Ney, D.M.; Sigalet, D.L.; Vegge, A.; Burrin, D. Animal models of gastrointestinal and liver diseases. Animal models of infant short bowel syndrome: Translational relevance and challenges. Am. J. Physiol. Gastrointest. Liver Physiol. 2014, 307, G1147–G1168. [Google Scholar] [CrossRef]
- Aunsholt, L.; Jeppesen, P.B.; Lund, P.; Sangild, P.T.; Ifaoui, I.B.; Qvist, N.; Husby, S. Bovine colostrum to children with short bowel syndrome: A randomized, double-blind, crossover pilot study. J. Parenter. Enter. Nutr. 2014, 38, 99–106. [Google Scholar] [CrossRef]
- Aunsholt, L.; Qvist, N.; Sangild, P.T.; Vegge, A.; Stoll, B.; Burrin, D.G.; Jeppesen, P.B.; Eriksen, T.; Husby, S.; Thymann, T. Minimal Enteral Nutrition to Improve Adaptation After Intestinal Resection in Piglets and Infants. J. Parenter. Enter. Nutr. 2018, 42, 446–454. [Google Scholar] [CrossRef]
- Aunsholt, L.; Thymann, T.; Qvist, N.; Sigalet, D.; Husby, S.; Sangild, P.T. Prematurity Reduces Functional Adaptation to Intestinal Resection in Piglets. J. Parenter. Enter. Nutr. 2015, 39, 668–676. [Google Scholar] [CrossRef]
- Vegge, A.; Thymann, T.; Lund, P.; Stoll, B.; Bering, S.B.; Hartmann, B.; Jelsing, J.; Qvist, N.; Burrin, D.G.; Jeppesen, P.B.; et al. Glucagon-like peptide-2 induces rapid digestive adaptation following intestinal resection in preterm neonates. Am. J. Physiol. Gastrointest. Liver Physiol. 2013, 305, G277–G285. [Google Scholar] [CrossRef] [Green Version]
- Nagy, E.S.; Paris, M.C.; Taylor, R.G.; Fuller, P.J.; Sourial, M.; Justice, F.; Bines, J.E. Colostrum protein concentrate enhances intestinal adaptation after massive small bowel resection in juvenile pigs. J. Pediatr. Gastroenterol. Nutr. 2004, 39, 487–492. [Google Scholar] [CrossRef]
- Pereira-Fantini, P.M.; Thomas, S.L.; Taylor, R.G.; Nagy, E.; Sourial, M.; Fuller, P.J.; Bines, J.E. Colostrum supplementation restores insulin-like growth factor -1 levels and alters muscle morphology following massive small bowel resection. J. Parenter. Enter. Nutr. 2008, 32, 266–275. [Google Scholar] [CrossRef]
- Paris, M.C.; Fuller, P.J.; Carstensen, B.; Nagy, E.; Taylor, R.G.; Sourial, M.; Holst, J.J.; Hartmann, B.; Binesm, J.E. Plasma GLP-2 levels and intestinal markers in the juvenile pig during intestinal adaptation: Effects of different diet regimens. Dig. Dis. Sci. 2004, 49, 1688–1695. [Google Scholar] [CrossRef] [PubMed]
- Sangild, P.T.; Shen, R.L.; Pontoppidan, P.; Rathe, M. Animal models of chemotherapy-induced mucositis: Translational relevance and challenges. Am. J. Physiol. Gastrointest. Liver Physiol. 2018, 314, G231–G246. [Google Scholar] [CrossRef] [PubMed]
- Rathe, M.; De Pietri, S.; Wehner, P.S.; Frandsen, T.L.; Grell, K.; Schmiegelow, K.; Sangild, P.T.; Husby, S.; Muller, K. Bovine Colostrum Against Chemotherapy-Induced Gastrointestinal Toxicity in Children With Acute Lymphoblastic Leukemia: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Parenter. Enter. Nutr. 2020, 44, 337–347. [Google Scholar] [CrossRef]
- Martin, J.; Howard, S.C.; Pillai, A.; Vogel, P.; Naren, A.P.; Davis, S.; Ringwald-Smith, K.; Buddington, K.; Buddington, R.K. The weaned pig as a model for Doxorubicin-induced mucositis. Chemotherapy 2014, 60, 24–36. [Google Scholar] [CrossRef] [PubMed]
- Shen, R.L.; Pontoppidan, P.E.; Rathe, M.; Jiang, P.; Hansen, C.F.; Buddington, R.K.; Heegaard, P.M.; Müller, K.; Sangild, P.T. Milk diets influence doxorubicin-induced intestinal toxicity in piglets. Am. J. Physiol. Gastrointest. Liver Physiol. 2016, 311, G324–G333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, R.L.; Rathe, M.; Jiang, P.; Pontoppidan, P.E.; Heegaard, P.M.; Müller, K.; Sangild, P.T. Doxorubicin-Induced Gut Toxicity in Piglets Fed Bovine Milk and Colostrum. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 698–707. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pontoppidan, P.E.; Shen, R.L.; Cilieborg, M.S.; Jiang, P.; Kissow, H.; Petersen, B.L.; Thymann, T.; Heilmann, C.; Muller, K.; Sangild, P.T. Bovine Colostrum Modulates Myeloablative Chemotherapy-Induced Gut Toxicity in Piglets. J. Nutr. 2015, 145, 1472–1480. [Google Scholar] [CrossRef] [PubMed]
- Pontoppidan, P.L.; Shen, R.L.; Petersen, B.L.; Thymann, T.; Heilmann, C.; Müller, K.; Sangild, P.T. Intestinal response to myeloablative chemotherapy in piglets. Exp. Biol. Med. 2014, 239, 94–104. [Google Scholar] [CrossRef]
- Chatterton, D.E.W.; Aagaard, S.; Hesselballe Hansen, T.; Nguyen, D.N.; De Gobba, C.; Lametsch, R.; Sangild, P.T. Bioactive proteins in bovine colostrum and effects of heating, drying and irradiation. Food Funct. 2020, 11, 2309–2327. [Google Scholar] [CrossRef]
- Elfstrand, L.; Lindmark-Månsson, H.; Paulsson, M.; Nyberg, L.; Åkesson, B. Immunoglobulins, growth factors and growth hormone in bovine colostrum and the effects of processing. Int. Dairy J. 2002, 12, 879–887. [Google Scholar] [CrossRef]
- Foster, D.M.; Poulsen, K.P.; Sylvester, H.J.; Jacob, M.E.; Casulli, K.E.; Farkas, B.E. Effect of high-pressure processing of bovine colostrum on immunoglobulin G concentration, pathogens, viscosity, and transfer of passive immunity to calves. J. Dairy Sci. 2016, 99, 8575–8588. [Google Scholar] [CrossRef] [Green Version]
- Navis, M.; Muncan, V.; Sangild, P.T.; Møller Willumsen, L.; Koelink, P.J.; Wildenberg, M.E.; Abrahamse, E.; Thymann, T.; van Elburg, R.M.; Renes, I.B. Beneficial Effect of Mildly Pasteurized Whey Protein on Intestinal Integrity and Innate Defense in Preterm and Near-Term Piglets. Nutrients 2020, 12, 1125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Navis, M.; Schwebel, L.; Soendergaard Kappel, S.; Muncan, V.; Sangild, P.T.; Abrahamse, E.; Aunsholt, L.; Thymann, T.; van Elburg, R.M.; Renes, I.B. Mildly Pasteurized Whey Protein Promotes Gut Tolerance in Immature Piglets Compared with Extensively Heated Whey Protein. Nutrients 2020, 12, 3391. [Google Scholar] [CrossRef]
- Lönnerdal, B.; Hernell, O. Effects of feeding ultrahigh-temperature (UHT)-treated infant formula with different protein concentrations or powdered formula, as compared with breast-feeding, on plasma amino acids, hematology, and trace element status. Am. J. Clin. Nutr. 1998, 68, 350–356. [Google Scholar] [CrossRef]
- Playford, R.J.; Cattell, M.; Marchbank, T. Marked variability in bioactivity between commercially available bovine colostrum for human use; implications for clinical trials. PLoS ONE 2020, 15, e0234719. [Google Scholar] [CrossRef]
- Klobasa, F.; Butler, J.E.; Habe, F. Maternal-neonatal immunoregulation: Suppression of de novo synthesis of IgG and IgA, but not IgM, in neonatal pigs by bovine colostrum, is lost upon storage. Am. J. Vet. Res. 1990, 51, 1407–1412. [Google Scholar]
- Agbokounou, A.M.; Ahounou, G.S.; Youssao Abdou Karim, I.; Mensah, G.A.; Koutinhouin, B.; Hornick, J.L. Effect of cow colostrum on the performance and survival rate of local newborn piglets in Benin Republic. Trop. Anim. Health Prod. 2017, 49, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhang, W.; Han, B.; Zhang, L.; Zhou, P. Changes in bioactive milk serum proteins during milk powder processing. Food Chem. 2020, 314, 126177. [Google Scholar] [CrossRef] [PubMed]
- Langhendries, J.P.; Hurrell, R.F.; Furniss, D.E.; Hischenhuber, C.; Finot, P.A.; Bernard, A.; Battisti, O.; Bertrand, J.M.; Senterre, J. Maillard reaction products and lysinoalanine: Urinary excretion and the effects on kidney function of preterm infants fed heat-processed milk formula. J. Pediatr. Gastroenterol. Nutr. 1992, 14, 62–70. [Google Scholar] [CrossRef]
- Cattaneo, S.; Masotti, F.; Pellegrino, L. Liquid infant formulas: Technological tools for limiting heat damage. J. Agric. Food Chem. 2009, 57, 10689–10694. [Google Scholar] [CrossRef] [PubMed]
- Cano-Sancho, G.; Alexandre-Gouabau, M.C.; Moyon, T.; Royer, A.L.; Guitton, Y.; Billard, H.; Darmaun, D.; Rozé, J.C.; Boquien, C.Y.; Le Bizec, B.; et al. Simultaneous exploration of nutrients and pollutants in human milk and their impact on preterm infant growth: An integrative cross-platform approach. Environ. Res. 2020, 182, 109018. [Google Scholar] [CrossRef]
- Andrew, S.M. Effect of composition of colostrum and transition milk from Holstein heifers on specificity rates of antibiotic residue tests. J. Dairy Sci. 2001, 84, 100–106. [Google Scholar] [CrossRef]
- an Wattum, J.J.; Leferink, T.M.; Wilffert, B.; Ter Horst, P.G.J. Antibiotics and lactation: An overview of relative infant doses and a systematic assessment of clinical studies. Basic Clin. Pharmacol. Toxicol. 2019, 124, 5–17. [Google Scholar] [CrossRef] [Green Version]
- Hair, A.B.; Blanco, C.L.; Moreira, A.G.; Hawthorne, K.M.; Lee, M.L.; Rechtman, D.J.; Abrams, S.A. Randomized trial of human milk cream as a supplement to standard fortification of an exclusive human milk-based diet in infants 750-1250 g birth weight. J. Pediatr. 2014, 165, 915–920. [Google Scholar] [CrossRef] [Green Version]
- Rechtman, D.J.; Lee, M.L.; Berg, H. Effect of environmental conditions on unpasteurized donor human milk. Breastfeed. Med. Off. J. Acad. Breastfeed. Med. 2006, 1, 24–26. [Google Scholar] [CrossRef]
- Salcedo, J.; Karav, S.; Le Parc, A.; Cohen, J.L.; de Moura Bell, J.; Sun, A.; Lange, M.C.; Barile, D. Applihairations of industrial treatments to donor human milk: Influence of pasteurization treatments, storage temperature, and time on human milk gangliosides. NPJ Sci. Food 2018, 2, 5. [Google Scholar] [CrossRef] [Green Version]
- Høst, A. Cow’s milk protein allergy and intolerance in infancy. Some clinical, epidemiological and immunological aspects. Pediatr. Allergy Immunol. 1994, 5, 5–36. [Google Scholar] [CrossRef]
- Barni, S.; Giovannini, M.; Mori, F. Epidemiology of non-IgE-mediated food allergies: What can we learn from that? Curr. Opin. Allergy Clin. Immunol. 2021, 21, 188–194. [Google Scholar] [CrossRef]
- Cianferoni, A. Food protein-induced enterocolitis syndrome epidemiology. Ann. Allergy Asthma Immunol. 2021, 126, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, N.; Okochi, M.; Matsushima, M.; Kato, R.; Takase, T.; Yoshida, Y.; Kawase, M.; Isobe, K.; Kawabe, T.; Honda, H. Peptide array-based analysis of the specific IgE and IgG4 in cow’s milk allergens and its use in allergy evaluation. Peptides 2009, 30, 1840–1847. [Google Scholar] [CrossRef] [PubMed]
- Villa, C.; Costa, J.; Oliveira, M.; Mafra, I. Bovine Milk Allergens: A Comprehensive Review. Compr. Rev. Food Sci. Food Saf. 2018, 17, 137–164. [Google Scholar] [CrossRef] [Green Version]
- Zachariassen, G.; Faerk, J.; Esberg, B.H.; Fenger-Gron, J.; Mortensen, S.; Christesen, H.T.; Halken, S. Allergic diseases among very preterm infants according to nutrition after hospital discharge. Pediatr. Allergy Immunol. 2011, 22, 515–520. [Google Scholar] [CrossRef]
- Thureen, P.J.; Melara, D.; Fennessey, P.V.; Hay, W.W., Jr. Effect of low versus high intravenous amino acid intake on very low birth weight infants in the early neonatal period. Pediatr. Res. 2003, 53, 24–32. [Google Scholar] [CrossRef]
- Hay, W.W., Jr. Strategies for feeding the preterm infant. Neonatology 2008, 94, 245–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clark, D.; Henderson, M.; Smith, M.; Dear, P.R. Plasma amino acid concentrations in parenterally fed preterm infants. Arch. Dis. Child. 1989, 64, 939–942. [Google Scholar] [CrossRef] [Green Version]
- Meyer, R.; Foong, R.X.; Thapar, N.; Kritas, S.; Shah, N. Systematic review of the impact of feed protein type and degree of hydrolysis on gastric emptying in children. BMC Gastroenterol. 2015, 15, 137. [Google Scholar] [CrossRef] [Green Version]
- Ghoneim, N.; Bauchart-Thevret, C.; Oosterloo, B.; Stoll, B.; Kulkarni, M.; de Pipaon, M.S.; Zamora, I.J.; Olutoye, O.O.; Berg, B.; Wittke, A.; et al. Delayed initiation but not gradual advancement of enteral formula feeding reduces the incidence of necrotizing enterocolitis (NEC) in preterm pigs. PLoS ONE 2014, 9, e106888. [Google Scholar] [CrossRef] [PubMed]
- Corvaglia, L.; Mariani, E.; Aceti, A.; Galletti, S.; Faldella, G. Extensively hydrolyzed protein formula reduces acid gastro-esophageal reflux in symptomatic preterm infants. Early Hum. Dev. 2013, 89, 453–455. [Google Scholar] [CrossRef]
- Ferreira, C.H.F.; Martinez, F.E.; Crott, G.C.; Belik, J. Gavage Feed Volume Determines the Gastric Emptying Rate in Preterm Infants. J. Pediatr. Gastroenterol. Nutr. 2018, 67, e43–e46. [Google Scholar] [CrossRef] [PubMed]
- Perrella, S.L.; Hepworth, A.R.; Gridneva, Z.; Simmer, K.N.; Hartmann, P.E.; Geddes, D.T. Gastric Emptying and Curding of Pasteurized Donor Human Milk and Mother’s Own Milk in Preterm Infants. J. Pediatr. Gastroenterol. Nutr. 2015, 61, 125–129. [Google Scholar] [CrossRef]
- Thymann, T.; Støy, C.A.; Bering, S.B.; Mølbak, L.; Sangild, P.T. Casein addition to a whey-based formula has limited effects on gut function in preterm pigs. J. Anim. Sci. 2012, 90 (Suppl. S4), 378–380. [Google Scholar] [CrossRef] [Green Version]
- Kappel, S.S.; Sangild, P.T.; Scheike, T.; Friborg, C.R.; Gormsen, M.; Aunsholt, L. Radiographic Imaging to Evaluate Food Passage Rate in Preterm Piglets as a Model for Preterm Infants. Front. Pediatr. 2020, 8, 624915. [Google Scholar] [CrossRef] [PubMed]
- Buddington, R.K.; Davis, S.L.; Buddington, K.K. The Risk of Necrotizing Enterocolitis Differs Among Preterm Pigs Fed Formulas With Either Lactose or Maltodextrin. J. Pediatr. Gastroenterol. Nutr. 2018, 66, e61–e66. [Google Scholar] [CrossRef]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sangild, P.T.; Vonderohe, C.; Melendez Hebib, V.; Burrin, D.G. Potential Benefits of Bovine Colostrum in Pediatric Nutrition and Health. Nutrients 2021, 13, 2551. https://doi.org/10.3390/nu13082551
Sangild PT, Vonderohe C, Melendez Hebib V, Burrin DG. Potential Benefits of Bovine Colostrum in Pediatric Nutrition and Health. Nutrients. 2021; 13(8):2551. https://doi.org/10.3390/nu13082551
Chicago/Turabian StyleSangild, Per Torp, Caitlin Vonderohe, Valeria Melendez Hebib, and Douglas G. Burrin. 2021. "Potential Benefits of Bovine Colostrum in Pediatric Nutrition and Health" Nutrients 13, no. 8: 2551. https://doi.org/10.3390/nu13082551