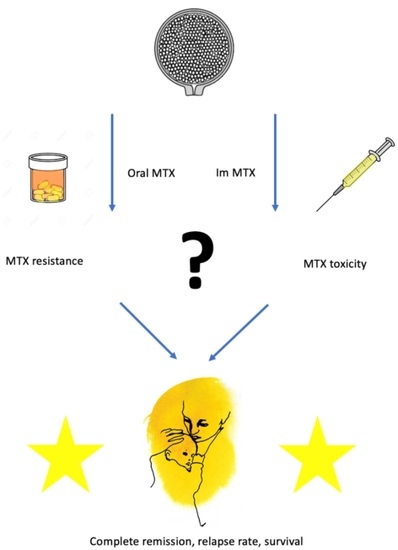
Differences in Administration of Methotrexate and Impact on Outcome in Low-Risk Gestational Trophoblastic Neoplasia
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Treatment Protocols
2.3. Outcome Variables
2.4. Statistical Analysis
3. Results
3.1. Oncological Outcomes
3.2. Risk of Methotrexate Resistance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Soper, J.T. Gestational Trophoblastic Disease: Current Evaluation and Management. Obstet. Gynecol. 2021, 137, 355–370. [Google Scholar] [CrossRef] [PubMed]
- Mangili, G.; Lorusso, D.; Brown, J.; Pfisterer, J.; Massuger, L.; Vaughan, M.; Ngan, H.Y.; Golfier, F.; Sekharan, P.K.; Charry, R.C.; et al. Trophoblastic disease review for diagnosis and management: A joint report from the International Society for the Study of Trophoblastic Disease, European Organisation for the Treatment of Trophoblastic Disease, and the Gynecologic Cancer InterGroup. Int. J. Gynecol. Cancer Off. J. Int. Gynecol. Cancer Soc. 2014, 24, S109–S116. [Google Scholar] [CrossRef] [PubMed]
- FIGO staging for gestational trophoblastic neoplasia 2000. FIGO Oncology Committee. Int. J. Gynaecol. Obstet. Off. Organ Int. Fed. Gynaecol. Obstet. 2002, 77, 285–287. [Google Scholar] [CrossRef]
- Lok, C.; van Trommel, N.; Massuger, L.; Golfier, F.; Seckl, M. Practical clinical guidelines of the EOTTD for treatment and referral of gestational trophoblastic disease. Eur. J. Cancer 2020, 130, 228–240. [Google Scholar] [CrossRef] [PubMed]
- May, T.; Goldstein, D.P.; Berkowitz, R.S. Current chemotherapeutic management of patients with gestational trophoblastic neoplasia. Chemother. Res. Pract. 2011, 2011, 806256. [Google Scholar] [CrossRef]
- Seckl, M.J.; Sebire, N.J.; Berkowitz, R.S. Gestational trophoblastic disease. Lancet 2010, 376, 717–729. [Google Scholar] [CrossRef]
- Ngan, H.Y.S.; Seckl, M.J.; Berkowitz, R.S.; Xiang, Y.; Golfier, F.; Sekharan, P.K.; Lurain, J.R.; Massuger, L. Update on the diagnosis and management of gestational trophoblastic disease. Int. J. Gynaecol. Obstet. Off. Organ Int. Fed. Gynaecol. Obstet. 2018, 143 (Suppl. S2), 79–85. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, D.P.; Berkowitz, R.S.; Horowitz, N.S. Optimal management of low-risk gestational trophoblastic neoplasia. Expert Rev. Anticancer Ther. 2015, 15, 1293–1304. [Google Scholar] [CrossRef]
- Seckl, M.J.; Sebire, N.J.; Fisher, R.A.; Golfier, F.; Massuger, L.; Sessa, C.; ESMO Guidelines Working Group. Gestational trophoblastic disease: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol./ ESMO 2013. [Google Scholar] [CrossRef]
- Lawrie, T.A.; Alazzam, M.; Tidy, J.; Hancock, B.W.; Osborne, R. First-line chemotherapy in low-risk gestational trophoblastic neoplasia. Cochrane Database Syst. Rev. 2016, 2016, Cd007102. [Google Scholar] [CrossRef] [Green Version]
- Lertkhachonsuk, A.A.; Israngura, N.; Wilailak, S.; Tangtrakul, S. Actinomycin d versus methotrexate-folinic acid as the treatment of stage I, low-risk gestational trophoblastic neoplasia: A randomized controlled trial. Int. J. Gynecol. Cancer Off. J. Int. Gynecol. Cancer Soc. 2009, 19, 985–988. [Google Scholar] [CrossRef] [PubMed]
- Yarandi, F.; Mousavi, A.; Abbaslu, F.; Aminimoghaddam, S.; Nekuie, S.; Adabi, K.; Hanjani, P. Five-Day Intravascular Methotrexate Versus Biweekly Actinomycin-D in the Treatment of Low-Risk Gestational Trophoblastic Neoplasia: A Clinical Randomized Trial. Int. J. Gynecol. Cancer Off. J. Int. Gynecol. Cancer Soc. 2016, 26, 971–976. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, G.; Caporali, R.; Todoerti, M.; Mattana, P. Methotrexate and Rheumatoid Arthritis: Current Evidence Regarding Subcutaneous Versus Oral Routes of Administration. Adv. Ther. 2016, 33, 369–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goodman, S.M.; Cronstein, B.N.; Bykerk, V.P. Outcomes related to methotrexate dose and route of administration in patients with rheumatoid arthritis: A systematic literature review. Clin. Exp. Rheumatol. 2015, 33, 272–278. [Google Scholar] [PubMed]
- Cipriani, P.; Ruscitti, P.; Carubbi, F.; Liakouli, V.; Giacomelli, R. Methotrexate in rheumatoid arthritis: Optimizing therapy among different formulations. Current and emerging paradigms. Clin. Ther. 2014, 36, 427–435. [Google Scholar] [CrossRef]
- Barter, J.F.; Soong, S.J.; Hatch, K.D.; Orr, J.W., Jr.; Partridge, E.C.; Austin, J.M., Jr.; Shingleton, H.M. Treatment of nonmetastatic gestational trophoblastic disease with oral methotrexate. Am. J. Obstet. Gynecol. 1987, 157, 1166–1168. [Google Scholar] [CrossRef]
- Farley, J.H.; Heathcock, R.B.; Branch, W.; Larsen, W.; Homas, D. Treatment of metastatic gestational choriocarcinoma with oral methotrexate in a combat environment. Obstet. Gynecol. 2005, 105, 1250–1254. [Google Scholar] [CrossRef]
- Patsner, B. Successful treatment of persistent partial mole with oral methotrexate therapy. Gynecol. Oncol. 1992, 46, 233–234. [Google Scholar] [CrossRef]
- Barter, J.F.; Soong, S.J.; Hatch, K.D.; Orr, J.W., Jr.; Partridge, E.C.; Austin, J.M., Jr.; Shingleton, H.M. Treatment of nonmetastatic gestational trophoblastic disease with sequential intramuscular and oral methotrexate. Gynecol. Oncol. 1989, 33, 82–84. [Google Scholar] [CrossRef]
- Faaborg, L.; Niemann, I.; Ostenfeld, E.B.; Hansen, E.S.; Sunde, L.; Lindegaard, J.C. A 30-year experience in using oral methotrexate as initial treatment for gestational trophoblastic neoplasia regardless of risk group. Acta Oncol. 2016, 55, 234–239. [Google Scholar] [CrossRef] [Green Version]
- McNeish, I.A.; Strickland, S.; Holden, L.; Rustin, G.J.; Foskett, M.; Seckl, M.J.; Newlands, E.S. Low-risk persistent gestational trophoblastic disease: Outcome after initial treatment with low-dose methotrexate and folinic acid from 1992 to 2000. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2002, 20, 1838–1844. [Google Scholar] [CrossRef] [PubMed]
- Clark, J.J.; Slater, S.; Seckl, M.J. Treatment of gestational trophoblastic disease in the 2020s. Curr. Opin. Obs. Gynecol. 2021, 33, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Chapman-Davis, E.; Hoekstra, A.V.; Rademaker, A.W.; Schink, J.C.; Lurain, J.R. Treatment of nonmetastatic and metastatic low-risk gestational trophoblastic neoplasia: Factors associated with resistance to single-agent methotrexate chemotherapy. Gynecol. Oncol. 2012, 125, 572–575. [Google Scholar] [CrossRef]
- McGrath, S.; Short, D.; Harvey, R.; Schmid, P.; Savage, P.M.; Seckl, M.J. The management and outcome of women with post-hydatidiform mole ‘low-risk’ gestational trophoblastic neoplasia, but hCG levels in excess of 100 000 IU l(-1). Br. J. Cancer 2010, 102, 810–814. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, F.; Grew, T.; Everard, J.; Ellis, L.; Winter, M.C.; Tidy, J.; Hancock, B.W.; Coleman, R.E. The outcome of patients with low risk gestational trophoblastic neoplasia treated with single agent intramuscular methotrexate and oral folinic acid. Eur. J. Cancer 2013, 49, 3184–3190. [Google Scholar] [CrossRef]
- Taylor, F.; Short, D.; Winter, M.C.; Tidy, J.; Savage, P.M.; Sarwar, N.; Hancock, B.W.; Seckl, M.J.; Coleman, R.E. A retrospective study to evaluate single agent methotrexate treatment in low risk gestational choriocarcinoma in the United Kingdom. Gynecol. Oncol. 2015, 136, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Powles, T.; Savage, P.M.; Stebbing, J.; Short, D.; Young, A.; Bower, M.; Pappin, C.; Schmid, P.; Seckl, M.J. A comparison of patients with relapsed and chemo-refractory gestational trophoblastic neoplasia. Br. J. Cancer 2007, 96, 732–737. [Google Scholar] [CrossRef] [Green Version]
- Lybol, C.; Sweep, F.C.; Harvey, R.; Mitchell, H.; Short, D.; Thomas, C.M.; Ottevanger, P.B.; Savage, P.M.; Massuger, L.F.; Seckl, M.J. Relapse rates after two versus three consolidation courses of methotrexate in the treatment of low-risk gestational trophoblastic neoplasia. Gynecol. Oncol. 2012, 125, 576–579. [Google Scholar] [CrossRef]
- Maestá, I.; Nitecki, R.; Horowitz, N.S.; Goldstein, D.P.; de Freitas Segalla Moreira, M.; Elias, K.M.; Berkowitz, R.S. Effectiveness and toxicity of first-line methotrexate chemotherapy in low-risk postmolar gestational trophoblastic neoplasia: The New England Trophoblastic Disease Center experience. Gynecol. Oncol. 2018, 148, 161–167. [Google Scholar] [CrossRef] [Green Version]
- Campbell, J.M.; Bateman, E.; Stephenson, M.D.; Bowen, J.M.; Keefe, D.M.; Peters, M.D. Methotrexate-induced toxicity pharmacogenetics: An umbrella review of systematic reviews and meta-analyses. Cancer Chemother. Pharm. 2016, 78, 27–39. [Google Scholar] [CrossRef]



| IM MTX | ORAL MTX | p-Value | |
|---|---|---|---|
| n = 107 | n = 63 | ||
| Karolinska, Sweden, n = 109 | 107 | 2 | |
| Aarhus, Denmark, n = 61 | 0 | 61 | |
| Age, years, median (IQR) | 32.1 (27.6–38.4) | 30.0 (26.0–34.0) | <0.05 1 |
| hCG at start of treatment, median (IQR) | 6370 (778–20,161) | 2486 (230–21,000) | 0.29 1 |
| Parity, median (range) | 0 (0–3) | 1 (0–3) | 0.50 1 |
Risk score, median (range)
| 2 (0–6) 11 (10.3) | 2 (0–6) 11 (17.5) | 0.45 1 0.24 2 |
| Histology n (%) | |||
| 87 (81.3) | 53 (84.1) | 1.00 2 |
| 12 (11.2) | 4 (6.3) | 1.00 2 |
| 3 (2.8) | 0 (0) | - |
| 4 (3.7) | 4 (6.3) | 1.00 2 |
| 1 (0.9) | 2 (3.2) | 1.00 2 |
| IM MTX | ORAL MTX | p-Value 3 | |
|---|---|---|---|
| n = 107 | n = 63 | ||
| Days to hCG normalization 1 | 41 (27–69) | 42 (22–57.5) | 0.5 |
| median (IQR) | |||
| Number of consolidation courses 1 | 2 (0–4) | 1 (0–3) | <0.01 |
| median (range) | |||
| MTX-resistance, n (%) | 37 (34.6) | 34 (54) | 0.01 |
| Complete remission, n (%) | 106 (99.1) 2 | 63 (100) | 0.44 |
| Relapse after MTX < 1 year, n (%) | 3 (2.8) | 1 (1.6) | 0.29 |
| Relapse after MTX > 1 year, n (%) | 2 (1.9) | 0 | 0.12 |
| Variables | Category | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|---|
| OR | p-Value | 95% CI | OR | p-Value | 95% CI | ||
| Type of treatment | Oral vs. im | 2.22 | 0.01 | 1.18–4.19 | 2.21 | 0.02 | 1.15–4.21 |
| Histological diagnosis | 1. Postmolar | 0.62 | 0.60 | ||||
| 2. Choriocarcinoma | 2.89 | 0.39 | 0.26–32.57 | 3.47 | 0.32 | 0.30–40.8 | |
| 3. Unknown | 1.45 | 0.61 | 0.35–5.99 | 1.22 | 0.79 | 0.28–5.42 | |
| Risk score | 5–6 vs. <5 | 2.24 | 0.08 | 0.90–5.58 | 1.96 | 0.16 | 0.77–5.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wallin, E.; Niemann, I.; Faaborg, L.; Fokdal, L.; Joneborg, U. Differences in Administration of Methotrexate and Impact on Outcome in Low-Risk Gestational Trophoblastic Neoplasia. Cancers 2022, 14, 852. https://doi.org/10.3390/cancers14030852
Wallin E, Niemann I, Faaborg L, Fokdal L, Joneborg U. Differences in Administration of Methotrexate and Impact on Outcome in Low-Risk Gestational Trophoblastic Neoplasia. Cancers. 2022; 14(3):852. https://doi.org/10.3390/cancers14030852
Chicago/Turabian StyleWallin, Emelie, Isa Niemann, Louise Faaborg, Lars Fokdal, and Ulrika Joneborg. 2022. "Differences in Administration of Methotrexate and Impact on Outcome in Low-Risk Gestational Trophoblastic Neoplasia" Cancers 14, no. 3: 852. https://doi.org/10.3390/cancers14030852