Oro-Dental Health and Primary Nephrotic Syndrome among Vietnamese Children
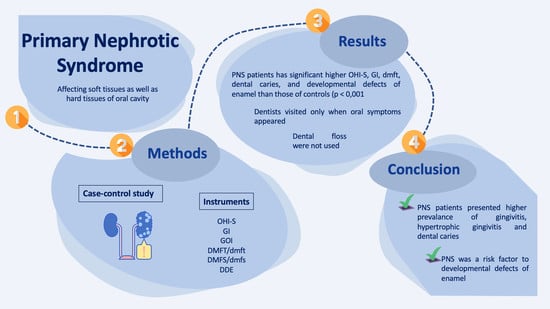
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Oral Examination
2.2.1. Simplified Oral Hygiene Index (OHI-S)
2.2.2. The Gingival Index (GI)
2.2.3. The Gingival Overgrowth Index (GOI)
2.2.4. Decayed, Missing, and Filled Teeth (dmft/DMFT)
2.2.5. Developmental Defects of Enamel
2.3. Questionnaire for Parents’ Knowledge of Oral Health and Oral Hygiene Care for Children with Systemic Diseases
2.4. Statistical Analysis
3. Results
3.1. Medication Characteristics
3.2. The Percentage of Gingivitis, Gingivitis Overgrowth, Dental Caries, and DDE
3.3. OHI-S and dmft/DMFT Indices
3.4. Oral Health Behaviors
4. Discussion
4.1. Gingivitis and Hypertrophic Gingivitis
4.2. Caries
4.3. DDE
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Variables | PNS (N = 407) | Non-PNS (N = 407) |
| 1. At the first diagnosis of NPS of your child, did the doctor mention related issues of oral health? n (%) | ||
| No | 369 (90.7%) | - |
| Yes | 38 (9.3%) | - |
| 2. Do you recognize the relationship between oral health and PNS? n (%) | ||
| No | 367 (90.2%) | - |
| Yes, but not fully informed | 33 (8.1%) | - |
| Yes, fully informed | 7 (1.7%) | - |
| 3. Did the dentist of your child recognize his/her NPS? n (%) | ||
| No | 143 (65.6%) | - |
| Yes, but he did not mention anything else | 56 (25.7%) | - |
| Yes, and he reminded us of some issues | 19 (8.7%) | - |
| 4. How often does your child visit a dentist? n (%) | ||
| Never or when having problems | 201 (49.4) | 26 (6.4) |
| Less than once/year | 102 (25.1) | 28 (6.9) |
| Once/year | 51 (12.5) | 239 (58.7) |
| 2 times/year | 35 (8.6) | 89 (21.9) |
| More than 2 times/year | 18 (4.4) | 25 (6.1) |
| 5. How often does your child brush his/her teeth? n (%) | ||
| Never | 13 (3.2) | 1 (0.3) |
| Once/day | 167 (41.0) | 82 (20.1) |
| Twice/day | 222 (54.6) | 320 (78.6) |
| More than 2 times/day | 5 (1.2) | 4 (1.0) |
| 6. Does your child have a toothbrush of his/her own? n (%) | ||
| No | 4 (1.0) | 1 (0.25) |
| Yes, a hard one | 18 (4.5) | 64 (15.0) |
| Yes, a soft one | 377 (93.5) | 344 (84.5) |
| Do not remember/Do not know | 4 (1.0) | 1 (0.25) |
| 7. How long does it take whenever your child brushes their teeth? n (%) | ||
| Less than 3 min | 366 (90.8) | 352 (88.0) |
| 3–5 min | 5 (1.3) | 27 (6.8) |
| Do not remember/Do not know | 32 (7.9) | 21 (5.2) |
| 8. How does your child brush her/his teeth every day? n (%) | ||
| Circular and Slow | 26 (6.5) | 126 (31.0) |
| Top–bottom and Slow | 18 (4.5) | 127 (31.3) |
| Across and Fast | 358 (89.1) | 152 (37.4) |
| Across and Slow | 0 | 1 (0.3) |
| 9. How often do you check the dental hygiene of your child? n (%) | ||
| Never | 277 (68.2) | 192 (47.2) |
| 1–3 times/week | 78 (18.7) | 159 (39.1) |
| Daily | 53 (13.1) | 56 (13.7) |
| 10. How often does your child use dental floss? n (%) | ||
| Never | 394 (96.7) | 135 (33.2) |
| Once/month | 5 (1.2) | 38 (9.3) |
| Once/week | 2 (0.5) | 33 (8.1) |
| Once/day | 3 (0.8) | 98 (24.1) |
| Every time | 3 (0.8) | 103 (25.3) |
| 11. Does your child have fluoride supplements? n (%) | ||
| No | 42 (10.3) | 10 (2.5) |
| Yes, with fluoride in toothpaste | 359 (88.2) | 390 (95.8) |
| Yes, with fluoride salt | 5 (1.2) | 3 (0.7) |
| Yes, with fluoride oral pill | 0 | 2 (0.5) |
| 12. Has your child ever had toothaches? n (%) | ||
| No | 191 (46.9) | 225 (55.3) |
| Yes | 209 (51.4) | 139 (34.2) |
| Do not remember/Do not know | 7 (1.7) | 43 (10.6) |
| 13. How often do you note gum bleeding? n (%) | ||
| Never | 234 (57.6) | 270 (66.3) |
| 1/week | 83 (20.4) | 41 (10.1) |
| 1/day | 42 (10.3) | 59 (14.5) |
| Every time | 8 (2.0) | 4 (1.0) |
| Do not remember/Do not know | 39 (9.6) | 33 (8.1) |
| 14. How often does your child eat sweets? n (%) | ||
| Never | 70 (17.2) | 7 (1.7) |
| 1/day | 79 (19.4) | 68 (16.7) |
| 2/day | 135 (33.2) | 143 (35.1) |
| 3/day | 102 (25.1) | 84 (20.6) |
| More often/day | 19 (4.7) | 104 (25.6) |
| Do not remember/Do not know | 2 (0.5) | 1 (0.3) |
| 15. How many sweetened beverages does your child consume? n (%) | ||
| None | 112 (27.5) | 30 (7.4) |
| Less than 0.5 L/day | 229 (56.3) | 253 (62.2) |
| 0.5–1 L/day | 63 (15.5) | 114 (28.0) |
| More than 1 L/day | 2 (0.5) | 3 (0.7) |
| Do not remember/Do not know | 1 (0.3) | 7 (1.7) |
| 16. How often did your child consume sweetened tea, lemonade, or juices during his/her early childhood (aged 0–4)? n (%) | ||
| Never | 69 (16.9) | 16 (3.9) |
| 1/week | 72 (17.7) | 50 (12.3) |
| 1/day | 117 (28.7) | 129 (31.7) |
| 2/day | 91 (22.4) | 92 (22.6) |
| More often | 21 (5.2) | 99 (24.3) |
| Do not remember/Do not know | 37 (9.1) | 21 (5.2) |
References
- Orth, S.R.; Ritz, E. The nephrotic syndrome. N. Engl. J. Med. 1998, 338, 1202–1211. [Google Scholar] [CrossRef]
- Eddy, A.A.; Symons, J.M. Nephrotic syndrome in childhood. Lancet 2003, 362, 629–639. [Google Scholar] [CrossRef]
- Chanchlani, R.; Parekh, R.S. Ethnic differences in childhood nephrotic syndrome. Front. Pediatrics 2016, 4, 39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seymour, R.A.; Thomason, J.M.; Nolan, A. Oral lesions in organ transplant patients. J. Oral Pathol. Med. 1997, 26, 297–304. [Google Scholar] [CrossRef] [PubMed]
- El-Husseini, A.; El-Basuony, F.; Mahmoud, I.; Sheashaa, H.; Sabry, A.; Hassan, R.; Taha, N.; Hassan, N.; Sayed-Ahmad, N.; Sobh, M. Long-term effects of cyclosporine in children with idiopathic nephrotic syndrome: A single-centre experience. Nephrol. Dial. Transplant. 2005, 20, 2433–2438. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wright, G.; Welbury, R.; Hosey, M. Cyclosporin-induced gingival overgrowth in children. Int. J. Paediatr. Dent. 2005, 15, 403–411. [Google Scholar] [CrossRef] [PubMed]
- Weraarchakul, W.; Weraarchakul, W. Oral Health Status in Pediatric Patients with Renal Disease at Srinagarind Hospital, Khon Kaen University, Thailand. J. Med. Assoc. Thai. 2015, 98, S185–S191. [Google Scholar]
- Subramaniam, P.; Gupta, M.; Mehta, A. Oral health status in children with renal disorders. J. Clin. Pediatric Dent. 2012, 37, 89–93. [Google Scholar] [CrossRef]
- McGaw, W.T.; Porter, H. Cyclosporine-induced gingival overgrowth: An ultrastructural stereologic study. Oral Surg. Oral Med. Oral Pathol. 1988, 65, 186–190. [Google Scholar] [CrossRef]
- Kaczmarek, U.; Wrzyszcz-Kowalczyk, A.; Jankowska, K.; Prościak, K.; Mysiak-Dębska, M.; Przywitowska, I.; Makulska, I. Oral health conditions in children with idiopathic nephrotic syndrome: A cross-sectional study. BMC Oral Health 2020, 20, 213. [Google Scholar] [CrossRef] [PubMed]
- Güzel, K.G.U.; Yilmaz, D.; Abacigil, F.; Pirinçci, S. Oral aspects in children with nephrotic syndrome. Turk. Klin. Dishekim. Bilimleri Derg. 2018, 24, 183–189. [Google Scholar] [CrossRef] [Green Version]
- Babu, N.V.; Jana, S. Assessment of oral health status in children suffering from nephrotic syndrome. Int. J. Sci. Study 2014, 2, 19–23. [Google Scholar]
- Salamone, K.; Yacoub, E.; Mahoney, A.-M.; Edward, K.-L. Oral care of hospitalised older patients in the acute medical setting. Nurs. Res. Pract. 2013, 2013, 827670. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Son, T.; Huong, N.; My Hanh, T.; Chieu, H.; Thuy Linh, L. Dental Caries Status and Relevant Factors in Children with Primary Nephrotic Syndrome in National Children Hospital, Vietnam. Int. J. Oral Craniofac. Sci. 2018, 4, 001–004. [Google Scholar]
- Piróg, A.; Michałek-Pasternak, E.; Mizerska-Wasiak, M.; Pańczyk-Tomaszewska, M.; Domagała, J.; Roszkowska-Blaim, M.; Olczak-Kowalczyk, D.; Poplawski, M. The incidence and intensity of dental caries in children with nephritic syndrome. Nowa Stomatol. 2012, 20, PMC7391815. [Google Scholar]
- Martins, C.; Siqueira, W.L.; Primo, L.S.G. Oral and salivary flow characteristics of a group of Brazilian children and adolescents with chronic renal failure. Pediatric Nephrol. 2008, 23, 619–624. [Google Scholar] [CrossRef] [PubMed]
- Dem, P.V.; Huong, N.T.; Lien, N.T.T.; Kien, N.T.; Nam, T.T.; Huonh, N.T.Q. Outcomes of Cyclosporine A Treatment in Children with Steroid Resistant Nephrotic Syndrome at Vietnam National Children’s Hospital. VNU J. Sci. Med Pharm. Sci. 2018, 34. (In Vietnamese) [Google Scholar] [CrossRef]
- Lombel, R.; Gipson, D.; Hodson, E. Kidney disease: Improving global outcomes. Treat. Steroid Sensitive Nephrotic Syndr. New Guidel. KDIGO. PediatrNephrol 2013, 28, 415–426. [Google Scholar]
- Kliegman, R.M.; St. Geme, J. Nephrotic Syndrome. In Nelson Textbook of Pediatrics, 21st ed.; Elsevier: Amsterdam, The Netherlands, 2019; Volume 2. [Google Scholar]
- Jc, G. The Simplified Oral Hygiene Index. J. Am. Dent. Assoc. 1964, 68, 7–13. [Google Scholar]
- Löe, H.; Silness, J. Periodontal disease in pregnancy I. Prevalence and severity. Acta Odontol. Scand. 1963, 21, 533–551. [Google Scholar] [CrossRef]
- Miranda, J.; Brunet, L.; Roset, P.; Farré, M.; Mendieta, C. Reliability of two measurement indices for gingival enlargement. J. Periodontal Res. 2012, 47, 776–782. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.E.; Baez, R.J.; World Health Organization. Oral Health Surveys: Basic Methods; WHO: New York, NY, USA, 2013. [Google Scholar]
- Ismail, A.I.; Pitts, N.B.; Tellez, M. The International Caries Classification and Management System (ICCMS™) an example of a caries management pathway. BMC Oral Health 2015, 15, S9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Group, F.W. A review of the developmental defects of enamel index (DDE Index): Commission on Oral Health, Research & Epidemiology. Int. Dent. J. 1992, 42, 411–426. [Google Scholar]
- Koerdt, S.; Hartz, J.; Hollatz, S.; Frohwitter, G.; Kesting, M.R.; Ewert, P.; Oberhoffer, R.; Deppe, H. Dental prevention and disease awareness in children with congenital heart disease. Clin. Oral Investig. 2018, 22, 1487–1493. [Google Scholar] [CrossRef] [PubMed]
- Mola, K.; Shimelis, D. Pattern and outcome of renal diseases in hospitalized children in Tikur anbessa specialized teaching hospital, Addis Ababa, Ethiopia. Ethiop. Med. J. 2016, 54, 117–123. [Google Scholar] [PubMed]
- Ali, E.-T.M.; Rahman, A.H.; Karrar, Z.A. Pattern and outcome of renal diseases in hospitalized children in Khartoum State, Sudan. Sudan. J. Paediatr. 2012, 12, 52. [Google Scholar]
- Barnett, H.; Edelmann, C.; Greifer, I. The primary nephrotic syndrome in children. Identification of patients with minimal change nephrotic syndrome from initial response to prednisone. A report of the international study of kidney disease in children. J. Pediatr. 1981, 98, 561–564. [Google Scholar]
- Kumar, J.; Gulati, S.; Sharma, A.P.; Sharma, R.K.; Gupta, R.K. Histopathological spectrum of childhood nephrotic syndrome in Indian children. Pediatric Nephrol. 2003, 18, 657–660. [Google Scholar] [CrossRef] [PubMed]
- Van Boeckel, T.P.; Gandra, S.; Ashok, A.; Caudron, Q.; Grenfell, B.T.; Levin, S.A.; Laxminarayan, R. Global antibiotic consumption 2000 to 2010: An analysis of national pharmaceutical sales data. Lancet Infect. Dis. 2014, 14, 742–750. [Google Scholar] [CrossRef]
- Okeke, I.N.; Laxminarayan, R.; Bhutta, Z.A.; Duse, A.G.; Jenkins, P.; O’Brien, T.F.; Pablos-Mendez, A.; Klugman, K.P. Antimicrobial resistance in developing countries. Part I: Recent trends and current status. Lancet Infect. Dis. 2005, 5, 481–493. [Google Scholar] [CrossRef]
- Olczak-Kowalczyk, D.; Pyrżak, B.; Dąbkowska, M.; Pańczyk-Tomaszewska, M.; Miszkurka, G.; Rogozińska, I.; Swoboda-Kopeć, E.; Gozdowski, D.; Kalińska, A.; Piróg, A. Candida spp. and gingivitis in children with nephrotic syndrome or type 1 diabetes. BMC Oral Health 2015, 15, 57. [Google Scholar] [CrossRef] [Green Version]
- Andrade, M.R.T.C.; Salazar, S.L.A.; de Sá, L.F.R.; Portela, M.; Ferreira-Pereira, A.; Soares, R.M.A.; Leão, A.T.T.; Primo, L.G. Role of saliva in the caries experience and calculus formation of young patients undergoing hemodialysis. Clin. Oral Investig. 2015, 19, 1973–1980. [Google Scholar] [CrossRef]
- Davidovich, E.; Davidovits, M.; Peretz, B.; Shapira, J.; Aframian, D.J. The correlation between dental calculus and disturbed mineral metabolism in paediatric patients with chronic kidney disease. Nephrol. Dial. Transpl. 2009, 24, 2439–2445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakhjavani, Y.B.; Bayramy, A. The dental and oral status of children with chronic renal failure. J. Indian Soc. Pedod. Prev. Dent. 2007, 25, 7. [Google Scholar] [CrossRef] [PubMed]
- Lynch, R.J. The primary and mixed dentition, post-eruptive enamel maturation and dental caries: A review. Int. Dent. J. 2013, 63, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Nunn, J.H.; Sharp, J.; Lambert, H.J.; Plant, N.D.; Coulthard, M.G. Oral health in children with renal disease. Pediatric Nephrol. 2000, 14, 997–1001. [Google Scholar] [CrossRef] [PubMed]
- Bublitz, A.; Machat, E.; Schärer, K.; Komposch, G.; Mehls, O. Changes in dental development in paediatric patients with chronic kidney disease. Proc. Eur. Transpl. Assoc. 1981, 18, 517–523. [Google Scholar]
- Koch, M.J.; Bührer, R.; Pioch, T.; Schärer, K. Enamel hypoplasia of primary teeth in chronic renal failure. Pediatric Nephrol. 1999, 13, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Kazoullis, S.; Seow, W.K.; Holcombe, T.; Newman, B.; Ford, D. Common dental conditions associated with dental erosion in schoolchildren in Australia. Pediatric Dent. 2007, 29, 33–39. [Google Scholar]
| Group | Gender | Age | |||
|---|---|---|---|---|---|
| Male | Female | 3–6 | 7–12 | 13–18 | |
| PNS | 309 | 98 | 123 | 210 | 74 |
| Control | 309 | 98 | 123 | 210 | 74 |
| Total | 618 | 196 | 246 | 420 | 148 |
| Oral Diseases | PNS (n (%)) | Non-PNS (n (%)) | Odds Ratio | 95% Confidence Interval | p-Value |
|---|---|---|---|---|---|
| Gingivitis | 281 (79.0%) | 203 (49.9%) | 1.301 | 1.112–1.523 | 0.001 |
| Mild | 209 (51.3%) | 139 (34.1%) | |||
| Moderate | 57 (14.0%) | 64 (15.8%) | |||
| Severe | 15 (3.7%) | 0 (0%) | 10 | 3.611–27.693 | 0.000001 |
| Gingivitis overgrowth | 68 (16.7%) | 5 (1.2%) | 14.25 | 5.219–38.908 | 0.000001 |
| Mild | 48 (11.8%) | 4 (1.0%) | |||
| Moderate | 17 (4.2%) | 1 (0.2%) | |||
| Severe | 3 (0.7%) | 0 (0%) | 0.992 | 0.984–1.001 | 0.249 |
| Dental caries | 320 (78.6%) | 257 (63.1%) | 2.15 | 1.57–2.93 | 0.0005 |
| DDE | 45 (11.1%) | 11 (2.7%) | 4.49 | 2.29–8.81 | 0.0003 |
| Variables | PNS | Non-PNS | p-Value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| DI-S | 1.22 | 0.66 | 0.84 | 0.71 | 0.0006 |
| CI-S | 0.53 | 0.76 | 0.28 | 0.45 | 0.0007 |
| OHI-S | 1.75 | 1.20 | 1.13 | 1.04 | 0.0006 |
| dt | 5.21 | 4.32 | 3.63 | 4.07 | 0.0006 |
| mt | 0.14 | 0.53 | 0.14 | 0.78 | 0.285 |
| ft | 0.24 | 0.81 | 0.40 | 1.25 | 0.845 |
| dmft | 5.58 | 4.41 | 4.17 | 4.33 | 0.0008 |
| DT | 1.26 | 1.75 | 1.54 | 2.23 | 0.721 |
| MT | 0.02 | 0.18 | 0.01 | 0.13 | 0.449 |
| FT | 0.08 | 0.49 | 0.16 | 0.65 | 0.09 |
| DMFT | 1.36 | 1.89 | 1.71 | 2.36 | 0.511 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luong, H.M.; Nguyen, T.T.; Tran, H.-T.; Tran, P.T.; Nguyen, P.-N.; Nguyen, H.T.; Nguyen, D.M.; Duc, H.T.T.; Tong, S.M. Oro-Dental Health and Primary Nephrotic Syndrome among Vietnamese Children. Children 2021, 8, 494. https://doi.org/10.3390/children8060494
Luong HM, Nguyen TT, Tran H-T, Tran PT, Nguyen P-N, Nguyen HT, Nguyen DM, Duc HTT, Tong SM. Oro-Dental Health and Primary Nephrotic Syndrome among Vietnamese Children. Children. 2021; 8(6):494. https://doi.org/10.3390/children8060494
Chicago/Turabian StyleLuong, Hang Minh, Tra Thu Nguyen, Huy-Thinh Tran, Phung Thi Tran, Phuong-Nga Nguyen, Huong Thu Nguyen, Duc Minh Nguyen, Hanh Tran Thi Duc, and Son Minh Tong. 2021. "Oro-Dental Health and Primary Nephrotic Syndrome among Vietnamese Children" Children 8, no. 6: 494. https://doi.org/10.3390/children8060494