- Paresthesia - (https://en.wikipedia.org/wiki/paresthesia)
- Numbness (paresthesia and neuropathy) - (https://mpkb.org/home/symptoms/neurological/paresthesia)
- What is Paresthesia? - (http://www.newhealthguide.org/paresthesia.html)
- Paresthesias: A Practical Diagnostic Approach - (http://www.chiro.org/chirozine/full/paresthesias.shtml)
- What is Paresthesia - Sign, Symptoms, Causes and Treatment - (http://www.paincare.org/what-is-paresthesia-symptoms-causes-and-treatment/)
What is Paresthesias?
Many of us often experience an odd sensation like sudden burning of our feet, or numbness in our legs when we get up after sitting cross-legged for long. Or at times, we feel something is crawling up our skin or our hands have suddenly become very itchy. These sensations come and go in most of us. In some people, it stays. When it does, it indicates a deeper problem that should not be ignored. It indicates some form of nerve damage and the presenting condition is called paresthesia.
Paresthesia is not a disease in itself; it is a cluster of symptoms and present in a number of diseases. It represents an altered nerve sensation in the form of burning, prickling, numbness, itching and even severe intolerable pain at times in the absence of a stimulus.
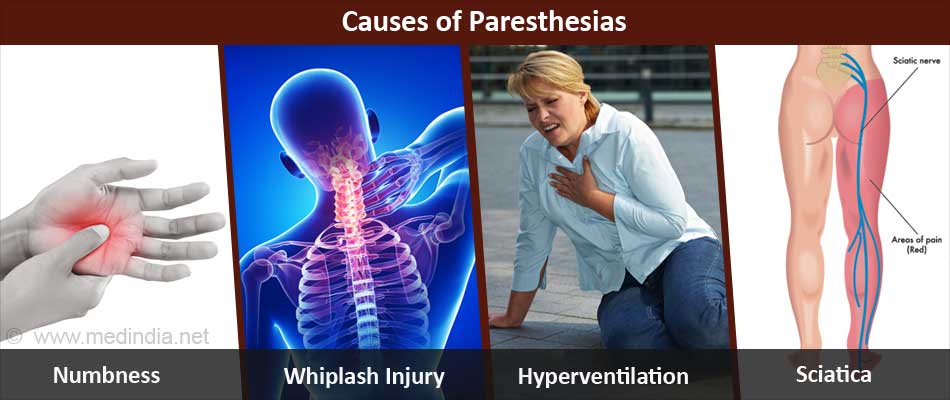
What are the Causes of Paresthesias?
Paresthesias can have a wide variety of causes. Temporary paresthesias can occur due to the following reasons:
a. Obdormition: Numbness caused due to prolonged pressure on a nerve. The sensation disappears on relieving pressure on the nerve.
b. Whiplash injury: Commonly occurs in upper limbs due to any soft tissueinjury in the cervical (neck) region. It is self-limiting and generally heals over a period of 6 months.
c. Hyperventilation syndrome: Many patients complain of transient paresthesias within 3 to 4 minutes of hyperventilation. This occurs due to electrolyte imbalances.
d. Panic Attack: Many people complain of odd sensations around the mouth, hands and feet during a panic attack. Presence of paresthesia indicates the severity of the panic attack.
e. Acute arterial occlusion: Sudden loss of blood circulation to a body part can result in 5 cardinal symptoms; namely, pallor, pain, pulselessness, paralysis and paresthesia.
Paresthesias that persist for a long time can occur due to the following underlying pathologies:
I. Central Nervous System disorders:
a. Stroke: Paresthesias are characteristically present in post-stroke patients and in some cases could be the only presenting symptom.
b. Intracerebral (brain) hemorrhage: Paresthesia can present in most cases of bleeding within the cerebrum.
c. Brain tumor: A sudden numbness accompanied by headache, nausea or vomiting could point towards a brain tumor and requires thorough evaluation.
d. Multiple sclerosis: One of the most significant symptoms presented by these patients is painful paresthesias which get triggered by any activity.
e. Vitamin B12 deficiency: Severe deficiency of this vitamin can cause paresthesias that get promptly relieved on replenishing its stores in the body by aggressive supplementation.
f. Head trauma: Many head injury patients complain of paresthesias in the face, especially in the area of distribution of the trigeminal nerve.
II. Peripheral Nervous System disorders:
a. Entrapment Neuropathy: Numbness and pain are the characteristic symptoms presented by these patients. The most common type is carpal tunnel syndrome wherein the median nerve that supplies part of the forearm, wrist and hand regions gets compressed within the carpal tunnel (an anatomical region in the wrist area).
b. Sciatica: A prolapsed intervertebral disc can compress the sciatic nerve causing pain, numbness and weakness in the lower limbs.
c. Circulatory disorders: Chronic peripheral arterial disease can also result in abnormal sensations due to poor blood circulation. These are most commonly felt in the extremities and begin from the tips of toes and fingers where the blood supply is first compromised.
d. Diabetes: One of the most common causes of the nerve symptoms of paresthesias is poor blood sugar control. Paradoxically, hypoglycemia (low blood sugar) can also present as paresthesias.
e. Alcoholism: Another common cause, paresthesias indicate a complication of alcoholism called toxic neuropathy.
f. Herpes zoster infection: Post herpetic neuralgia is a painful chronic condition presenting as paresthesias that significantly affect the quality of life of the patient.
The other common etiologies of paresthesia include thyroid disorders, HIV infection, leprosy, uremia, porphyrias, arthritis, burns, and frostbite.
What are the Types of Paresthesias?
Paresthesias is classified based on the time the odd sensation lasts.
A short-lived sensation of our foot falling asleep or sensation of pins and needles in our soles for a few seconds is called temporary paresthesia. This most commonly occurs due to undue pressure on a nerve and the sensation disappears completely when the pressure is relieved.
When these odd sensations are experienced repeatedly and they last for longer periods of time, they indicate an underlying pathology. They are known as chronic paresthesias and they should be investigated further.
How do you Diagnose Paresthesia?
If paresthesia is associated with specific nerves it is referred to as a neuropathy. If it does not follow a specific nerve distribution it may be due to an upper neuron lesion. Performing a sensory examination will help to determine between upper and lower motor neuron lesions. Abnormal findings may suggest a specific nerve, nerve root or spinal cord lesion. Increased reflexes are suggestive of upper motor neuron disease, while decreased reflexes are suggestive of spinal nerve segment disease or peripheral nerve injury.
Diagnosis is based on history, physical examination and specific radiological studies.
a. Patient history: Information about the time of onset, duration and location of the paresthesias, as well as any pain or motor dysfunction associated with it have to be obtained from the patient. The patient should also be asked about past and current medical problems and medications, and any drug or toxic exposure.
b. Physical examination: The patient’s response to pain, touch, vibration, joint position and thermal sensation are measured using a sensory examination.

Pain sensation is generally tested with a pin or needle (for sharp pain), or with a wisp of cotton (for soft touch). This serves to map the area of involvement and may provide information as to a spinal cord lesion or a peripheral nerve abnormality.
Loss of vibratory sensation (checked using a tuning fork) occurs relatively early in a peripheral neuropathy such as those related to diabetes, alcoholism, vitamin B12 deficiency or dorsal column disease.
In proprioception testing, the patient closes their eyes and is asked to indicate whether the finger or toe that is being held is being moved up or down. If there is a loss of position sense, it is associated with a nerve root lesion, a peripheral nerve abnormality or dorsal column disease.
Thermal sensation is tested by putting the patients’ hand into test tubes containing water with varying degrees of temperature; patients with a normal thermal sensation should be able to distinguish between stimuli differing by a few degrees.
A neurologic examination can be done to reveal signs of a neuropathy or myelopathy that may have been the cause of the paresthesia.
Muscle groups should be assessed for strength and signs of atrophy. Any abnormalities of specific muscles are associated with specific nerve lesions.
c. Laboratory evaluation: This involves a complete blood cell count, a chemistry profile, and a urinalysis.
Neurophysiologic testing, such as nerve conduction studies, and electromyography, are useful in establishing a diagnosis (if laboratory tests are not satisfactory) and prognosis. They are helpful in checking for large-diameter nerve conduction problems. While they can be used for the evaluation of trauma or entrapment neuropathies, they do not differentiate between simulated sensory loss and neuropathy.
Imaging studies like magnetic resonance imaging (MRI) and computed tomography(CT scan) can be performed to rule out some causes from the central nervous system.
Specific tests can be done to accurately determine the cause of paresthesias. These include:
- MRI or a CT scan of the affected area for the evaluation of a suspected herniated disc, entrapment neuropathy or suspected lumbar compression
- Chest radiograph to rule out a lung tumor or tuberculosis
- Lumbar puncture to eliminate a diagnosis of tertiary syphilis, carcinomatous meningitis (cancer that spreads from the primary site to the meninges) or a central inflammatory cause
- Nerve biopsy to diagnose inflammation of muscular arteries, sarcoidosis (inflammatory disease affecting multiple organs) and amyloidosis (building up of abnormal amyloid fibrils)
- MRI angiography helpful in diagnosing vascular abnormalities
How do you Treat Paresthesias?
Success in treating paresthesias is completely hinged upon accurate diagnosis of the underlying cause. Unless the cause is not treated, nothing can offer relief.
If it is the limbs that have fallen asleep, exercises like stretching and massaging can help restore feeling.
If the paresthesia is a result of peripheral neuropathy due to diabetes it requires strict sugar control for alleviation of symptoms. Unless the blood sugar levels are not controlled well, no drug can provide complete relief.
If the symptoms do not subside in the above patients or if paresthesia occurs after treatments like chemotherapy, relief can be obtained by anti-inflammatory drugs like Aspirin and Ibuprofen; but long term usage of these medications is not encouraged. These drugs act by blocking the nerves that carry the sensation of pain to the brain thereby relieving the pain.
If patients do not respond to conventional anti-inflammatory drugs, they might require mild antidepressants like Amitryptaline for a short period of time under medical supervision only. Antidepressants can change the perception of a person about pain and thus provide relief.
For severe paresthesia, opium derivatives like Codeine are prescribed.
Some medications offered depend on the underlying cause and can include immunosuppressants like Prednisone, intravenous gamma globulin (IVIG), anticonvulsants such as Gabapentin and antiviral medications (if paresthesias is due to shingles).
Other therapies that might provide some relief are physiotherapy, acupuncture, nutritional therapy, aromatic oils and topical ointments.
How do you Prevent Paresthesias?
Paresthesias can be prevented in the real sense of the term only by seeking early medical care and complying with medications regularly. The presence of chronic paresthesia indicates poor control of a pre-existing medical condition. If the disease is under control, paresthesias might not occur.
Health Tips
- Chronic paresthesias indicate underlying nerve damage.
- People experiencing numbness in their soles should always wear special orthotic footwear and not move around with naked feet. They can unknowingly burn or hurt their feet.
- Patients should avoid holding anything heavy as they might lose the grip and hurt themselves.
- They should also avoid obstacles like climbing stairs.