A 24-year-old white male presented with a 2-year history of changes to his nails. He stated that the white discoloration had never completely resolved but improved from time to time with the nails appearing to "grow out normally." He complained of intermittent tenderness at the lateral and proximal nail folds from occasional "infections" that he characterized as increased redness and pus. He worked as an administrative supervisor in a machine shop and he rarely was exposed to cutting oils. Hobbies included mechanical work on his car. The patient had a several-year history of anxiety symptoms that caused interruption of his sleep patterns. He admitted to biting his fingernails and to tapping his fingernails repeatedly on flat surfaces like a desk on most days. He admitted to constantly picking at the proximal nail fold and hyponychium of the involved fingers. The patient did notice worsening of his fingernails during stressful periods in his life. Past medical history was otherwise negative. He denied medications including chemotherapy and underlying illnesses including thyroid disease. Review of systems was negative. There was no evidence of liver or renal disease. No history of possible arsenic exposure. Family history was negative for skin and nail disease. On physical exam, the patient appeared anxious but otherwise normal. He was directly observed tapping his nails on the armrest of the chair and picking at his nails during the exam. Patient otherwise had normal teeth, hair, and skin. On exam of the nails, multiple transverse white curvilinear bands were noted. The bands were separated by normal pink nail color (Figure 1). The proximal, distal, and lateral nail folds were noted to be slightly erythematous, frayed, and jagged (Figure 2). The cuticle was noted to be frayed and almost absent. The distal nail plate was ragged on the right nail. No frank signs of infection could be appreciated. Potassium hydroxide test was negative. The patient was referred to psychiatry to manage the anxiety symptoms.
Multiple transverse bands of white discoloration noted to involve almost all nails.
Close-up view of thumbnails; notice ragged proximal, lateral, and distal nail folds and slight erythema but no frank infection.
Transverse leukonychia is defined as bands or lines of white discoloration in the nail.[1] It has been described in association with repeated trauma including cryotherapy, key punching, and salt immersion; systemic illnesses; and medications including chemotherapeutic agents.[1,2,3] We report a case of transverse leukonychia in a patient with a nervous tic involving his nails.
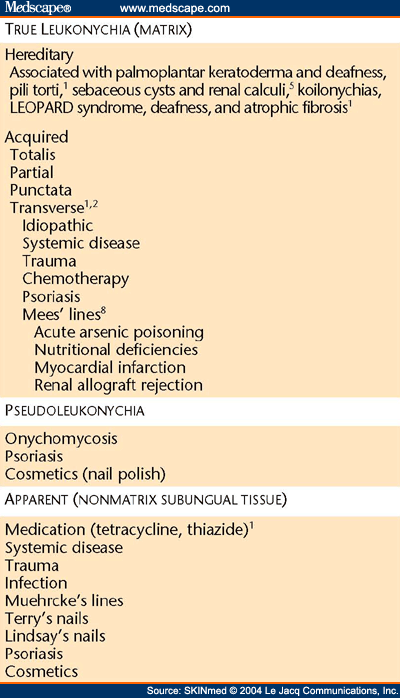
Multiple authors have attempted to classify leukonychia. Leukonychia is defined as whitening or apparent whitening of the nail plate.[1] One classification scheme divides leukonychia into true, apparent, and pseudo-leukonychia.[4] In true leukonychia, the white discoloration is caused by pathology that lies in the matrix. In apparent leukonychia, the pathology is in the subungual tissue. Pseudo-leukonychia results from an exogenous source such as fungal infection, keratin granulation from nail polish, and psoriasis ( Table 1 ).
True leukonychia is further divided into inherited and acquired.[1] Acquired leukonychia is then divided based on where the nail plate is involved: superficial, intermediate, or indeterminate. True leukonychia has also been divided according to distribution of the white pattern. These include leukonychia punctata (white spots), transverse leukonychia (bands or lines), leukonychia partialis (incompletely white), and leukonychia totalis (total discoloration).[1,2,4]
Hereditary leukonychia has been observed to have an autosomal dominant pattern either alone or in association with a clinical syndrome. It has been associated with pili torti,[1] sebaceous cysts and renal calculi,[5] palmoplantar keratoderma and deafness, knuckle pads and deafness,[6] palmoplantar keratoderma and atrophic fibrosis, congenital hypoparathyroidism, koilonychias (spoon nails), and LEOPARD syndrome.[1]
Acquired leukonychia is caused by nail matrix disturbance during systemic disease, trauma, or poisoning. Acquired leukonychia usually presents as punctata or transverse striae.[7] Mees' lines are considered to be a true leukonychia. They present as white transverse lines. They have been associated with acute arsenic poisoning, pellagra, malnutrition, typhoid fever, Hodgkin's disease, renal failure, renal allograft rejection, and myocardial infarction.[8]
We describe a case of transverse leukonychia that we believe to be caused by repeated microtrauma to the nail matrix. White spots and transverse streaks have been explained by repeated microtrauma to the nail matrix.[2] The white color is caused by a structural abnormality of the nail material that decreases transmission of incident light.[2] Others have reported abnormal keratinization in the areas of the white bands. One group performed biopsies of toenails with transverse leukonychia presumed to be caused by microtrauma. They noted an abnormal parakeratotic strip in the lower third of the nail plate that was strongly eosinophilic in some foci close to the subungual keratin. The affected onychocytes differed from those of the normally keratinized nail plate, in which they were larger and globular in shape. Disorganization and perinuclear vacuolization of the onychocytes could be noted by hematoxylin-eosin stain and periodic acid Schiff.[2]
We believe microtrauma caused by the repeated tapping of the free nail edge on hard surfaces led to damage to the onychocytes in the nail matrix. In our patient, the clinical appearance of the curvilinear bands followed the course of the lunula, leading us to believe the damage started at the nail matrix. The nails returned to normal in approximately 100 days when the patient stopped tapping.
LCDR Kimberly L. Maino, MC, USNR, 8901 Wisconsin Avenue, National Naval Medical Center, Dermatology Service, Bethesda, MD 20899. E-mail: drmaino@aol.com.
Skinmed. 2004;3(1) © 2004 Le Jacq Communications, Inc.
Cite this: Traumatic Transverse Leukonychia - Medscape - Jan 01, 2004.