by Rosemarie Tremblay-LeMay MD FRCPC
May 1, 2024
Hemolytic anemia is a condition in which the body’s immune system attacks and damages red blood cells (RBCs) in the blood. The damaged RBCs are either removed in the spleen or liver or destroyed in the blood. This process is called immune hemolysis, and over time, it leads to low levels of RBCs in the blood.
What causes hemolytic anemia?
Conditions that can cause hemolytic anemia include autoimmune diseases such as lupus, blood cancers such as non-Hodgkin’s lymphoma, and chronic infections such as HIV and tuberculosis.
Types of hemolytic anemia
Doctors separate hemolytic anemia into two groups – autoimmune hemolysis and alloimmune hemolysis – based on the trigger that initiates the disease.
Autoimmune hemolysis
Autoimmune hemolysis develops when the immune system fails to recognize RBCs as a normal part of the body and attacks them. This is called an autoimmune reaction. Similarly, the antibodies that stick to RBCs are called autoantibodies. Many conditions can lead to autoimmune hemolysis including lymphoma, infections (in particular HIV, Mycoplasma pneumoniae), and certain medications. Other autoimmune diseases such as systemic lupus erythematosus can also produce antibodies against RBCs resulting in immune hemolysis.

Some autoantibodies stick to RBCs at the normal internal temperature of the body. These autoantibodies cause a type of anemia called warm autoimmune hemolytic anemia. In contrast, some autoantibodies can only stick to RBCs at lower temperatures normally occurring in the hands and feet. These autoantibodies cause a type of anemia called cold agglutinin-mediated autoimmune hemolytic anemia.
A disease called paroxysmal cold hemoglobinuria that mostly happens in children after an infection is also due to a special type of antibody that sticks to RBCs in colder temperatures of the extremities and will activate the immune system when it comes back to warmer areas of the body.

Alloimmune hemolysis
Immune hemolysis can also be caused when proteins not normally found in the body enter the bloodstream. Once detected by the body, the foreign proteins trigger an alloimmune reaction (“allo” means other).
An alloimmune reaction can occur when a baby inherits blood proteins (RhD or ABO) from the father that are different from the mother. An alloimmune reaction can also occur when a person receives a blood transfusion that is not compatible with their blood group. Fortunately, both of these situations are now rare, thanks to preventative medications and strict testing.
How do doctors test for immune hemolysis?
Doctors can test for immune hemolysis by looking for autoantibodies in the blood.
Two kinds of tests can be performed to look for autoantibodies:
- Direct antiglobulin test
- Indirect antiglobulin test
Other blood tests can look for substances released from damaged RBCs, such as indirect bilirubin and lactate dehydrogenase (LDH). A specialized protein called haptoglobin may also be measured. Haptoglobin sticks to free hemoglobin in the blood to remove it. Because the amount of free hemoglobin in the blood goes up when RBCs are damaged or destroyed inside the vessels, intravascular hemolysis causes the level of haptoglobin to go down.
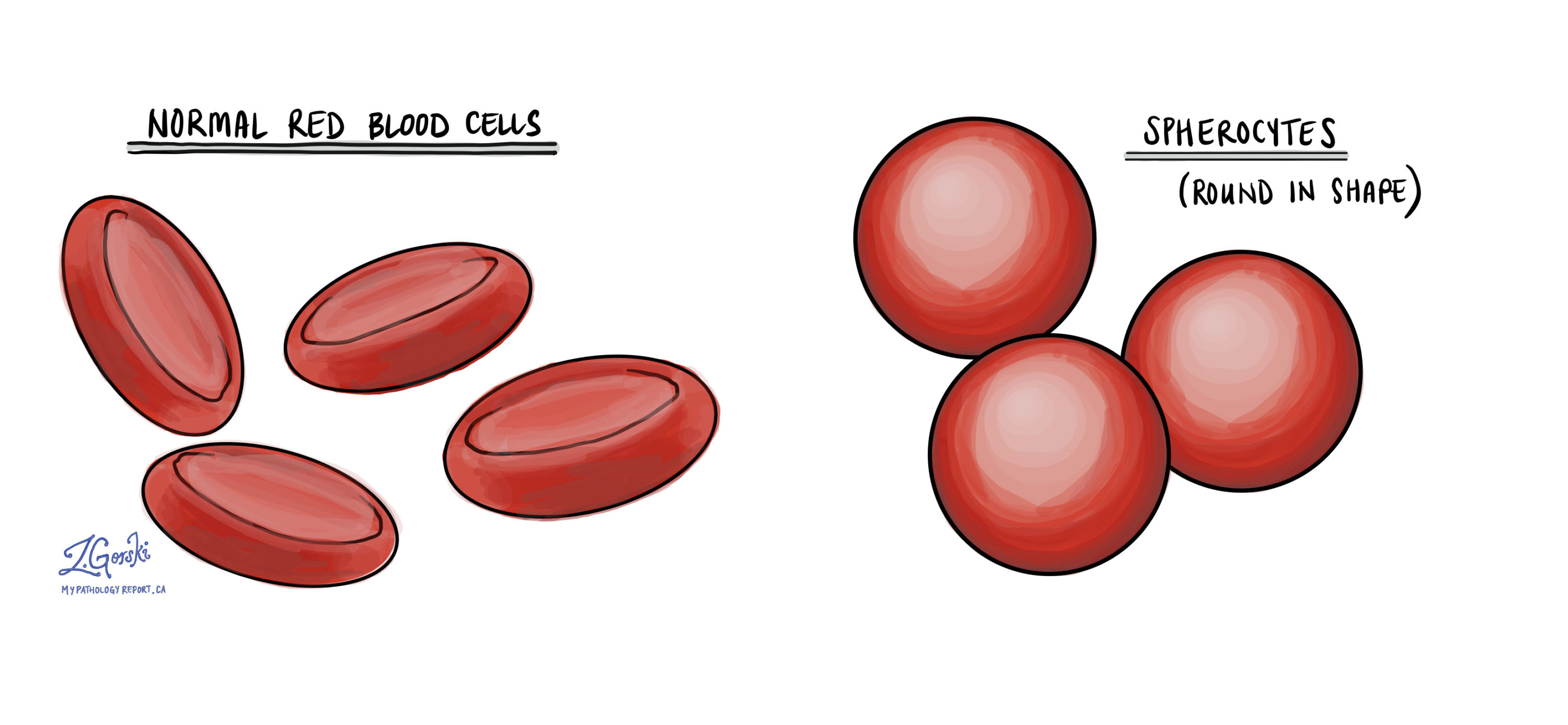
When a blood sample is examined under the microscope, your pathologist may see an increased number of young (immature) RBCs. Immature RBCs are larger and more purple, while very immature RBCs still have a nucleus. A type of RBC called spherocyte, which is very round and darker than normal RBCs, can also be seen.
About this article
Doctors wrote this article to help you read and understand your pathology report. Contact us if you have any questions about this article or your pathology report. Read this article for a more general introduction to the parts of a typical pathology report.


