What is white lung syndrome? Here's what to know about pneumonia
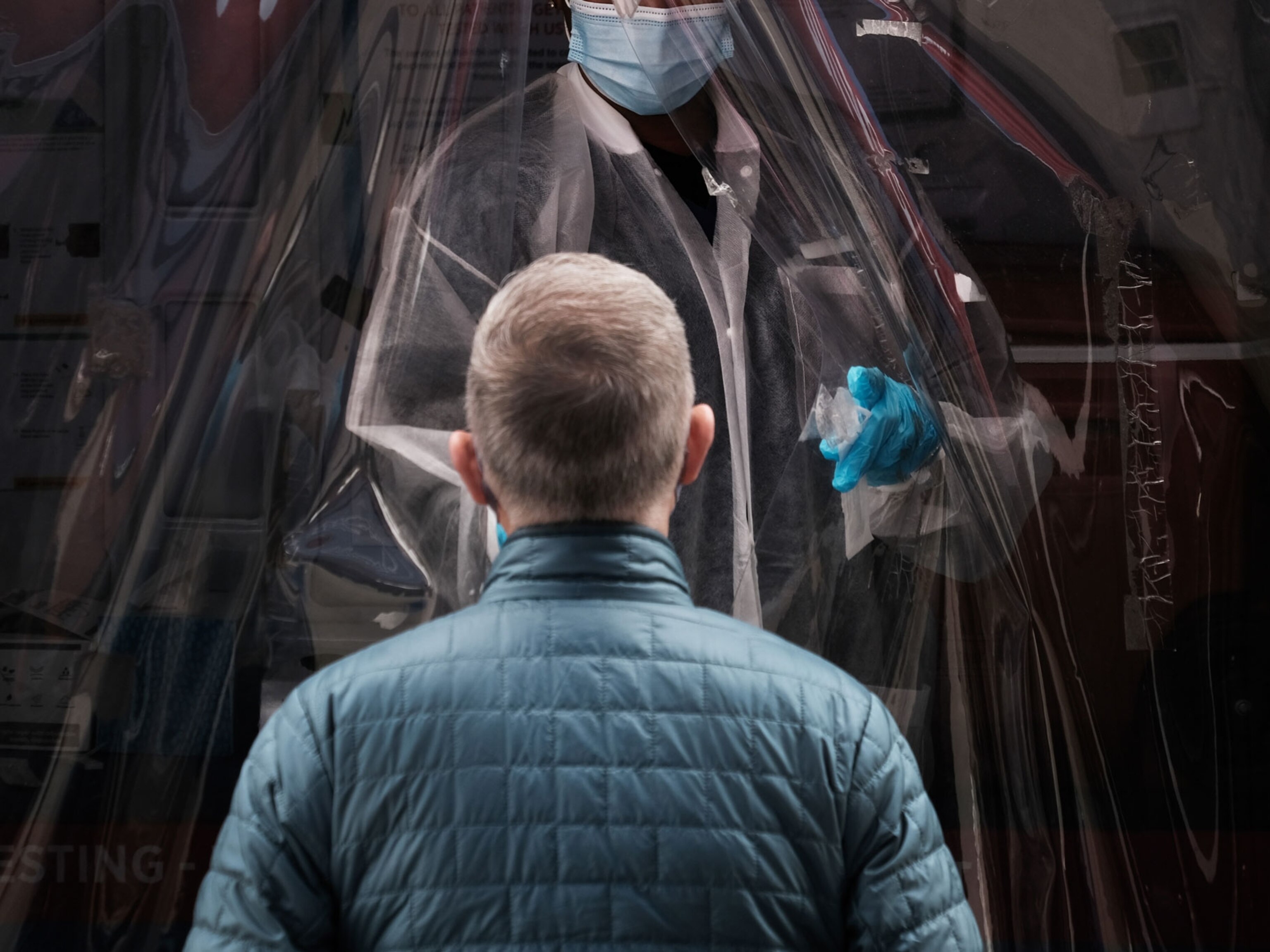
Experts say a recent outbreak in Ohio is likely just typical pediatric pneumonia. They spoke to Nat Geo about the different types of pneumonia, plus the risks and treatments.

An outbreak of pediatric pneumonia cases in Cleveland, Ohio, was not caused by a novel respiratory virus, according to a press release issued by the Warren County Health District; more likely these were just “typical pediatric pneumonia cases.”
Although several media outlets have started referring to these cases as “white lung syndrome,” that is “not a medical term,” says Tianshi David Wu, a pulmonologist at Baylor College of Medicine.
The term “white lung syndrome” refers to the whiteness that appears on an x-ray of the lungs of a patient with pneumonia. Normally, lungs appear dark on an x-ray, but when inflammation or mucus is present, these can appear as white patches or spots and is a hallmark often used to diagnose pneumonia. “What people have called white lung syndrome appears to be just standard pneumonia,” Wu says.
Pneumonia is the world’s leading cause of death for children under the age of five, and the leading cause of hospitalization for adults in the United States, with over one million admissions per year; about 40,000 Americans die from the disease annually. Pneumonia, which can range from mild to life-threatening, is caused by inflammation within the tiny air sacs in the lungs. It can lead to deadly consequences—including a lack of oxygen and blood infections—if left untreated.
National Geographic spoke with several experts to gain a better understanding of the various types of pneumonia, and the risks of contracting different forms of the disease.
How is it diagnosed?
Pneumonia is an infection of the lower airways, specifically the tiny air sacs, called alveoli, which serves as the exchange point for delivering oxygen to the blood, and removing carbon dioxide. This infection can be triggered by various factors that initiate in the upper airway and then travel into the deeper parts of the lungs.
Some of the common symptoms for pneumonia include cough, shortness of breath, chest pain, and general fatigue. To diagnose pneumonia, a doctor will use a stethoscope to check a patient’s breathing, listening for a characteristic crackling sound, similar to the sound of crumpling paper, Wu says. “That’s all that’s needed to diagnose pneumonia,” Wu says, adding that if a doctor is still unsure, they can also order an x-ray of the lungs, which will confirm the diagnosis.
Four types of pneumonia
The four main types of pneumonia that are characterized based on the cause: bacterial, viral, fungal, and hospital-acquired.
For the most part, “there’s no way to tell if a pneumonia is being caused by a bacterium, a virus, or a fungi just by examination,” Wu says. “Most pneumonias don’t ultimately get a diagnosis” of what is causing it. Instead, doctors will treat pneumonia based on a patient’s symptoms and their medical history, using this information to determine the best course of treatment.
Bacterial pneumonia, which is the most common type, is caused by bacteria, which means that it is easily treated with an antibiotic. For many patients, treating pneumonia with an antibiotic will help resolve their symptoms, and help them start to feel better within days of starting treatment. “The earlier the treatment, the better,” Wu says. There is also a vaccine that protects against the most prominent bacterial strain that causes pneumonia, and is approved for certain groups, including patients over the age of 65 and those with certain pre-existing conditions.
Viral pneumonia, which is less common, is caused by a virus, such as influenza, SARS-CoV-2—‑the virus that causes COVID-19—or RSV, a respiratory virus that usually causes mild, cold-like symptoms. Many of these viral infections begin in the upper airways, then travel down into the lungs.
A viral infection can also lead to bacterial pneumonia by weakening a patient’s immune system, leaving them vulnerable to a secondary infection. Although no virus can be treated with an antibiotic, there are vaccines that can help prevent infection: the yearly flu shot, COVID vaccine, and for those who are eligible, the new RSV vaccine.
Fungal pneumonias are rare, and usually found in patients with pre-existing conditions, such as a compromised immune system. Fungal pneumonias tend to affect people with autoimmune disorders, patients who are undergoing chemotherapy, or other chronic conditions that can affect a person’s immune system, says Lucas Kimmig, a pulmonologist at University of Chicago Medicine. Fungal pneumonias require a different treatment strategy and can often be more serious, due to both the complications of pneumonia, as well as the patient’s other underlying conditions.
Hospital-acquired pneumonias are considered a separate category because a hospital environment often exposes patients to a different set of bacteria, including strains that are more likely to be resistant to antibiotics. A case of pneumonia that was acquired in a hospital setting can affect how doctors treat the condition. “They’re at risk for some different bugs that we don’t usually see in the outpatient setting,” Kimmig says. “That affects the antibiotic choice.”
Why is pneumonia so serious?
The risk of pneumonia is that, if left untreated, it can cause serious complications, and can spread to other parts of the body.
“If there is a bacteria or a virus that infects the lungs, there’s really no way to get it out,” says Jason Turowski, a pulmonologist at the Cleveland Clinic. “That infection can rage and rage.”
The primary risk of pneumonia is that it can damage the lungs, affecting a person’s ability to get the oxygen they need. This damage usually happens because inflammation can cause a buildup of inflammatory cells in the tiny sacs of the lung that prevents oxygen from getting delivered, and carbon dioxide from getting released. “It’s causing an injury that doesn’t enable you to get the vital oxygen you need and to release the carbon dioxide your body’s making,” Turowski says.
The secondary risk is that the infection can spread to other parts of the body, such as the space between the lung and the chest wall, or into the bloodstream. When this infection starts to spread to other parts of the body, this can turn into a condition called sepsis, which is an out-of-control, systemic response to an infection. Sepsis can quickly grow into a life-threatening condition that often results in death.
Who is most at risk for developing pneumonia?
The people who are at the highest risk for developing serious complications from pneumonia include children under the age of five, adults over the age of 65, and people with pre-existing conditions, such as heart and lung disease, or a weakened immune system due to chemotherapy or organ transplantation.
Other risk factors include having uncontrolled diabetes or smoking or drinking heavily.
“Most forms of pneumonia end up being mild and self-limiting,” Wu says. “If it is severe enough to be hospitalized, there are probably other things going on.”
Warning signs pneumonia is worsening
For patients who have been diagnosed with pneumonia, and are recovering at home, some of the major warning signs that they may need to seek out additional medical care include a worsening in their condition, even after treatment, whether it’s a fever that won’t go away, chest pain or shortness of breath that won’t resolve, or rapid breathing, which can indicate a failure to get enough oxygen.
“It’s important to always contact your doctor when something feels different,” Turowski says. “When we’re involved early, we can guide you, and if we get a follow up call, that I’m getting worse, then we can help get things ready for you in the hospital.”
You May Also Like
Go Further
Animals
- Behind the scenes at America’s biggest birding festivalBehind the scenes at America’s biggest birding festival
- How scientists are piecing together a sperm whale ‘alphabet’How scientists are piecing together a sperm whale ‘alphabet’
- Orangutan seen using plants to heal wound for first timeOrangutan seen using plants to heal wound for first time
- What La Palma's 'lava tubes' tell us about life on other planetsWhat La Palma's 'lava tubes' tell us about life on other planets
Environment
- The northernmost flower living at the top of the worldThe northernmost flower living at the top of the world
- This beautiful floating flower is wreaking havoc on NigeriaThis beautiful floating flower is wreaking havoc on Nigeria
- What the Aral Sea might teach us about life after disasterWhat the Aral Sea might teach us about life after disaster
- What La Palma's 'lava tubes' tell us about life on other planetsWhat La Palma's 'lava tubes' tell us about life on other planets
- How fungi form ‘fairy rings’ and inspire superstitionsHow fungi form ‘fairy rings’ and inspire superstitions
History & Culture
- This thriving society vanished into thin air. What happened?This thriving society vanished into thin air. What happened?
- These were the real rules of courtship in the ‘Bridgerton’ eraThese were the real rules of courtship in the ‘Bridgerton’ era
Science
- Is the 5-second rule true? Science finally has an answer.
- Science
- Gory Details
Is the 5-second rule true? Science finally has an answer. - E-bikes are good for the environment—but what about your health?E-bikes are good for the environment—but what about your health?
- Why trigger points cause so much pain—and how you can relieve itWhy trigger points cause so much pain—and how you can relieve it
Travel
- The best LGBTQ-friendly destinations for every travelerThe best LGBTQ-friendly destinations for every traveler
- 6 of the best active pursuits on Cape Cod and the Islands
- Paid Content
6 of the best active pursuits on Cape Cod and the Islands - The key to better mindfulness may be your public gardenThe key to better mindfulness may be your public garden