Abstract
Neuroendocrine neoplasms (NENs) can develop in almost any organ and span a spectrum from well-differentiated and indolent neuroendocrine tumours (NETs) to poorly differentiated and highly aggressive neuroendocrine carcinomas (NECs), including small-cell lung cancer (SCLC). These neoplasms are thought to primarily derive from neuroendocrine precursor cells located throughout the body and can also arise through neuroendocrine transdifferentiation of organ-specific epithelial cell types. Hence, NENs constitute a group of tumour types that share key genomic and phenotypic characteristics irrespective of their site of origin, albeit with some organ-specific differences. The establishment of representative preclinical models for several of these disease entities together with analyses of human tumour specimens has provided important insights into crucial aspects of their biology with therapeutic implications. In this Review, we provide a comprehensive overview of the current understanding of NENs of the gastrointestinal system and lung from clinical and biological perspectives. Research on NENs has typically been siloed by the tumour site of origin, and a cross-cutting view might enable advances in one area to accelerate research in others. Therefore, we aim to emphasize that a better understanding of the commonalities and differences of NENs arising in different organs might more effectively inform clinical research to define therapeutic targets and ultimately optimize patient care.
Key points
-
Neuroendocrine neoplasms are categorized as either neuroendocrine tumours (NETs) or neuroendocrine carcinomas (NECs) characterized by markedly different proliferative rates.
-
Slow-growing NETs share key biological characteristics across different sites of origin.
-
NECs are aggressive cancers that almost always have inactivation of the tumour-suppressor genes TP53 and RB1.
-
NECs across sites of origin have been subtyped based on overlapping sets of key transcription factors.
-
Despite fundamental biological similarities, both NETs and NECs have some characteristics, including mutational spectra, that are reflective of their organ of origin.
-
Further understanding of these differences and commonalities could accelerate therapeutic research for patients with neuroendocrine neoplasms.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Bedard, P. L., Hyman, D. M., Davids, M. S. & Siu, L. L. Small molecules, big impact: 20 years of targeted therapy in oncology. Lancet 395, 1078–1088 (2020).
Flaherty, K. T., Le, D. T. & Lemery, S. Tissue-agnostic drug development. Am. Soc. Clin. Oncol. Educ. Book 37, 222–230 (2017).
FDA. FDA Approves Entrectinib for NTRK Solid Tumors and ROS-1 NSCLC https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-entrectinib-ntrk-solid-tumors-and-ros-1-nsclc (2019).
FDA. FDA Approves Larotrectinib for Solid Tumors with NTRK Gene Fusions https://www.fda.gov/drugs/fda-approves-larotrectinib-solid-tumors-ntrk-gene-fusions (2018).
FDA. FDA Approves Pembrolizumab for Adults and Children with TMB-H Solid Tumors https://www.fda.gov/drugs/drug-approvals-and-databases/fda-approves-pembrolizumab-adults-and-children-tmb-h-solid-tumors (2020).
FDA. FDA Grants Accelerated Approval to Pembrolizumab for First Tissue/site Agnostic Indication https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-pembrolizumab-first-tissuesite-agnostic-indication (2017).
FDA. FDA Grants Accelerated Approval to Dostarlimab-gxly for dMMR Advanced Solid Tumors https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-dostarlimab-gxly-dmmr-advanced-solid-tumors (2022).
Rindi, G. et al. A common classification framework for neuroendocrine neoplasms: an International Agency for Research on Cancer (IARC) and World Health Organization (WHO) expert consensus proposal. Mod. Pathol. 31, 1770–1786 (2018).
Yao, J. C. et al. One hundred years after ‘carcinoid’: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J. Clin. Oncol. 26, 3063–3072 (2008).
Dasari, A. et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 3, 1335–1342 (2017).
Frilling, A. et al. Neuroendocrine tumor disease: an evolving landscape. Endocr. Relat. Cancer 19, R163–R185 (2012).
Williams, E. D. & Sandler, M. The classification of carcinoid tumours. Lancet 1, 238–239 (1963).
WHO Classification of Tumours Editorial Board. Digestive System Tumours: WHO Classification of Tumours, 5th Edition (International Agency for Research on Cancer, 2019).
WHO Classification of Tumours Editorial Board. Thoracic Tumours: WHO Classification of Tumours, 5th Edition (International Agency for Research on Cancer, 2021).
Stelwagen, J., de Vries, E. G. E. & Walenkamp, A. M. E. Current treatment strategies and future directions for extrapulmonary neuroendocrine carcinomas: a review. JAMA Oncol. 7, 759–770 (2021).
Chang, M. T. et al. Small-cell carcinomas of the bladder and lung are characterized by a convergent but distinct pathogenesis. Clin. Cancer Res. 24, 1965–1973 (2018).
Gluckman, C. R. & Metz, D. C. Gastric neuroendocrine tumors (Carcinoids). Curr. Gastroenterol. Rep. 21, 13 (2019).
Perri, G., Prakash, L. R. & Katz, M. H. G. Pancreatic neuroendocrine tumors. Curr. Opin. Gastroenterol. 35, 468–477 (2019).
Naraev, B. G. et al. Management of diarrhea in patients with carcinoid syndrome. Pancreas 48, 961–972 (2019).
Robelin, P. et al. Characterization, prognosis, and treatment of patients with metastatic lung carcinoid tumors. J. Thorac. Oncol. 14, 993–1002 (2019).
Hermans, B. C. M. et al. Unique metastatic patterns in neuroendocrine neoplasms of different primary origin. Neuroendocrinology 111, 1111–1120 (2021).
Riihimäki, M., Hemminki, A., Sundquist, K., Sundquist, J. & Hemminki, K. The epidemiology of metastases in neuroendocrine tumors. Int. J. Cancer 139, 2679–2686 (2016).
Rekhtman, N. et al. Stage IV lung carcinoids: spectrum and evolution of proliferation rate, focusing on variants with elevated proliferation indices. Mod. Pathol. 32, 1106–1122 (2019).
Moertel, C. G., Weiland, L. H., Nagorney, D. M. & Dockerty, M. B. Carcinoid tumor of the appendix: treatment and prognosis. N. Engl. J. Med. 317, 1699–1701 (1987).
Grozinsky-Glasberg, S. et al. Current size criteria for the management of neuroendocrine tumors of the appendix: are they valid? Clinical experience and review of the literature. Neuroendocrinology 98, 31–37 (2013).
Raymond, E. et al. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N. Engl. J. Med. 364, 501–513 (2011).
Cives, M. & Strosberg, J. R. Gastroenteropancreatic neuroendocrine tumors. CA Cancer J. Clin. 68, 471–487 (2018).
Rudin, C. M., Brambilla, E., Faivre-Finn, C. & Sage, J. Small-cell lung cancer. Nat. Rev. Dis. Prim. 7, 3 (2021).
Ko, J., Winslow, M. M. & Sage, J. Mechanisms of small cell lung cancer metastasis. EMBO Mol. Med. 13, e13122 (2021).
Smith, J. D., Reidy, D. L., Goodman, K. A., Shia, J. & Nash, G. M. A retrospective review of 126 high-grade neuroendocrine carcinomas of the colon and rectum. Ann. Surg. Oncol. 21, 2956–2962 (2014).
Garcia-Carbonero, R. et al. ENETS consensus guidelines for high-grade gastroenteropancreatic neuroendocrine tumors and neuroendocrine carcinomas. Neuroendocrinology 103, 186–194 (2016).
Yatabe, Y. et al. Best practices recommendations for diagnostic immunohistochemistry in lung cancer. J. Thorac. Oncol. 14, 377–407 (2019).
Cree, I. A. et al. Counting mitoses: SI(ze) matters! Mod. Pathol. 34, 1651–1657 (2021).
Travis, W. D. et al. Survival analysis of 200 pulmonary neuroendocrine tumors with clarification of criteria for atypical carcinoid and its separation from typical carcinoid. Am. J. Surg. Pathol. 22, 934–944 (1998).
Beasley, M. B. et al. Pulmonary atypical carcinoid: predictors of survival in 106 cases. Hum. Pathol. 31, 1255–1265 (2000).
Sorbye, H. et al. Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the NORDIC NEC study. Ann. Oncol. 24, 152–160 (2013).
Baine, M. K. & Rekhtman, N. Multiple faces of pulmonary large cell neuroendocrine carcinoma: update with a focus on practical approach to diagnosis. Transl. Lung Cancer Res. 9, 860–878 (2020).
Febres Aldana, C. A. et al. Rb tumor suppressor in small cell lung cancer: combined genomic and immunohistochemical analysis with a description of a distinct Rb-proficient subset. Clin. Cancer Res. https://doi.org/10.1158/1078-0432.CCR-22-1115 (2022).
Dasari, A., Mehta, K., Byers, L. A., Sorbye, H. & Yao, J. C. Comparative study of lung and extrapulmonary poorly differentiated neuroendocrine carcinomas: a SEER database analysis of 162,983 cases. Cancer 124, 807–815 (2018).
Ito, T. et al. Epidemiological trends of pancreatic and gastrointestinal neuroendocrine tumors in Japan: a nationwide survey analysis. J. Gastroenterol. 50, 58–64 (2015).
Tsai, H.-J. et al. The epidemiology of neuroendocrine tumors in Taiwan: a nation-wide cancer registry-based study. PLoS One 8, e62487 (2013).
Leoncini, E., Carioli, G., la Vecchia, C., Boccia, S. & Rindi, G. Risk factors for neuroendocrine neoplasms: a systematic review and meta-analysis. Ann. Oncol. 27, 68–81 (2016).
Giraldi, L. et al. Risk factors for pancreas and lung neuroendocrine neoplasms: a case-control study. Endocrine 71, 233–241 (2021).
Varghese, A. M. et al. Small-cell lung cancers in patients who never smoked cigarettes. J. Thorac. Oncol. 9, 892–896 (2014).
Tlemsani, C. et al. Whole-exome sequencing reveals germline-mutated small cell lung cancer subtype with favorable response to DNA repair-targeted therapies. Sci. Transl. Med. 13, eabc7488 (2021).
Mukherjee, S. et al. Germline pathogenic variants impact clinicopathology of advanced lung cancer. Cancer Epidemiol. Biomark. Prev. 31, 1450–1459 (2022).
Quintanal-Villalonga, Á. et al. Lineage plasticity in cancer: a shared pathway of therapeutic resistance. Nat. Rev. Clin. Oncol. 17, 360–371 (2020).
Sequist, L. V. et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci. Transl. Med. 3, 75ra26 (2011).
Rickman, D. S., Beltran, H., Demichelis, F. & Rubin, M. A. Biology and evolution of poorly differentiated neuroendocrine tumors. Nat. Med. 23, 1–10 (2017).
Nadal, R., Schweizer, M., Kryvenko, O. N., Epstein, J. I. & Eisenberger, M. A. Small cell carcinoma of the prostate. Nat. Rev. Urol. 11, 213–219 (2014).
Quintanal-Villalonga, A. et al. Multiomic analysis of lung tumors defines pathways activated in neuroendocrine transformation. Cancer Discov. 11, 3028–3047 (2021).
Quintanal-Villalonga, A. et al. Comprehensive molecular characterization of lung tumors implicates AKT and MYC signaling in adenocarcinoma to squamous cell transdifferentiation. J. Hematol. Oncol. 14, 170 (2021).
Shamir, E. R. et al. Identification of high-risk human papillomavirus and Rb/E2F pathway genomic alterations in mutually exclusive subsets of colorectal neuroendocrine carcinoma. Mod. Pathol. 32, 290–305 (2019).
Yachida, S. et al. Comprehensive genomic profiling of neuroendocrine carcinomas of the gastrointestinal system. Cancer Discov. 12, 692–711 (2022).
Kraft, S., Faquin, W. C. & Krane, J. F. HPV-associated neuroendocrine carcinoma of the oropharynx: a rare new entity with potentially aggressive clinical behavior. Am. J. Surg. Pathol. 36, 321–330 (2012).
Stoler, M. H., Mills, S. E., Gersell, D. J. & Walker, A. N. Small-cell neuroendocrine carcinoma of the cervix. A human papillomavirus type 18-associated cancer. Am. J. Surg. Pathol. 15, 28–32 (1991).
Capella, C. et al. Primary gastric Merkel cell carcinoma harboring DNA polyomavirus: first description of an unusual high-grade neuroendocrine carcinoma. Hum. Pathol. 45, 1310–1314 (2014).
Yang, C. et al. Lung-only melanoma: UV mutational signature supports origin from occult cutaneous primaries and argues against the concept of primary pulmonary melanoma. Mod. Pathol. 33, 2244–2255 (2020).
Hartley, C. P., Steinmetz, H. B., Memoli, V. A. & Tafe, L. J. Small cell neuroendocrine carcinomas of the lung do not harbor high-risk human papillomavirus. Hum. Pathol. 46, 577–582 (2015).
Bishop, J. A. et al. HPV analysis in distinguishing second primary tumors from lung metastases in patients with head and neck squamous cell carcinoma. Am. J. Surg. Pathol. 36, 142–148 (2012).
George, J. et al. Comprehensive genomic profiles of small cell lung cancer. Nature 524, 47–53 (2015).
Scarpa, A. et al. Whole-genome landscape of pancreatic neuroendocrine tumours. Nature 543, 65–71 (2017).
Francis, J. M. et al. Somatic mutation of CDKN1B in small intestine neuroendocrine tumors. Nat. Genet. 45, 1483–1486 (2013).
van Riet, J. et al. The genomic landscape of 85 advanced neuroendocrine neoplasms reveals subtype-heterogeneity and potential therapeutic targets. Nat. Commun. 12, 4612 (2021).
Kawasaki, K. et al. An organoid biobank of neuroendocrine neoplasms enables genotype-phenotype mapping. Cell 183, 1420–1435 (2020).
Crona, J. & Skogseid, B. GEP- NETS UPDATE: genetics of neuroendocrine tumors. Eur. J. Endocrinol. 174, R275–R290 (2016).
Brandi, M. L. et al. Multiple endocrine neoplasia type 1: latest insights. Endocr. Rev. 42, 133–170 (2021).
Choueiri, T. K. & Kaelin, W. G. Targeting the HIF2-VEGF axis in renal cell carcinoma. Nat. Med. 26, 1519–1530 (2020).
Schmelzle, T. & Hall, M. N. TOR, a central controller of cell growth. Cell 103, 253–262 (2000).
Kresak, J. L. & Walsh, M. Neurofibromatosis: a review of NF1, NF2, and Schwannomatosis. J. Pediatr. Genet. 5, 98–104 (2016).
Fernandez-Cuesta, L. et al. Frequent mutations in chromatin-remodelling genes in pulmonary carcinoids. Nat. Commun. 5, 3518 (2014).
Jiao, Y. et al. DAXX/ATRX, MEN1, and mTOR pathway genes are frequently altered in pancreatic neuroendocrine tumors. Science 331, 1199–1203 (2011).
Swarts, D. R. A. et al. MEN1 gene mutation and reduced expression are associated with poor prognosis in pulmonary carcinoids. J. Clin. Endocrinol. Metab. 99, E374–E378 (2014).
George, J. et al. Integrative genomic profiling of large-cell neuroendocrine carcinomas reveals distinct subtypes of high-grade neuroendocrine lung tumors. Nat. Commun. 9, 1048 (2018).
Cancer Genome Atlas Research Network. Comprehensive molecular profiling of lung adenocarcinoma. Nature 511, 543–550 (2014).
Mu, P. et al. SOX2 promotes lineage plasticity and antiandrogen resistance in TP53- and RB1-deficient prostate cancer. Science 355, 84–88 (2017).
Aggarwal, R., Zhang, T., Small, E. J. & Armstrong, A. J. Neuroendocrine prostate cancer: subtypes, biology, and clinical outcomes. J. Natl Compr. Canc Netw. 12, 719–726 (2014).
Aggarwal, R. et al. Clinical and genomic characterization of treatment-emergent small-cell neuroendocrine prostate cancer: a multi-institutional prospective study. J. Clin. Oncol. 36, 2492–2503 (2018).
Park, J. W. et al. Reprogramming normal human epithelial tissues to a common, lethal neuroendocrine cancer lineage. Science 362, 91–95 (2018).
Lim, J. S. et al. Intratumoural heterogeneity generated by Notch signalling promotes small-cell lung cancer. Nature 545, 360–364 (2017).
Yoshida, K. et al. Tobacco smoking and somatic mutations in human bronchial epithelium. Nature 578, 266–272 (2020).
Cortés-Ciriano, I. et al. Comprehensive analysis of chromothripsis in 2,658 human cancers using whole-genome sequencing. Nat. Genet. 52, 331–341 (2020).
Kawasaki, K. et al. Chromosome engineering of human colon-derived organoids to develop a model of traditional serrated adenoma. Gastroenterology 158, 638–651 (2020).
Kloosterman, W. P. et al. A systematic analysis of oncogenic gene fusions in primary colon cancer. Cancer Res. 77, 3814–3822 (2017).
Venizelos, A. et al. The molecular characteristics of high-grade gastroenteropancreatic neuroendocrine neoplasms. Endocr. Relat. Cancer 29, 1–14 (2021).
Chen, L. et al. Genetic characteristics of colorectal neuroendocrine carcinoma: more similar to colorectal adenocarcinoma. Clin. Colorectal Cancer 20, 177–185 (2021).
Rekhtman, N. et al. Next-generation sequencing of pulmonary large cell neuroendocrine carcinoma reveals small cell carcinoma-like and non-small cell carcinoma-like subsets. Clin. Cancer Res. 22, 3618–3629 (2016).
Rudin, C. M. et al. Molecular subtypes of small cell lung cancer: a synthesis of human and mouse model data. Nat. Rev. Cancer 19, 289–297 (2019).
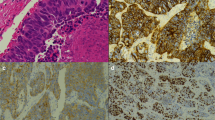
Baine, M. K. et al. SCLC subtypes defined by ASCL1, NEUROD1, POU2F3, and YAP1: a comprehensive immunohistochemical and histopathologic characterization. J. Thorac. Oncol. 15, 1823–1835 (2020).
Gay, C. M. et al. Patterns of transcription factor programs and immune pathway activation define four major subtypes of SCLC with distinct therapeutic vulnerabilities. Cancer Cell 39, 346–360 (2021).
Rekhtman, N. Lung neuroendocrine neoplasms: recent progress and persistent challenges. Mod. Pathol. 35, 36–50 (2022).
Plasschaert, L. W. et al. A single-cell atlas of the airway epithelium reveals the CFTR-rich pulmonary ionocyte. Nature 560, 377–381 (2018).
Elmentaite, R. et al. Cells of the human intestinal tract mapped across space and time. Nature 597, 250–255 (2021).
Baine, M. K. et al. POU2F3 in SCLC: clinicopathologic and genomic analysis with a focus on its diagnostic utility in neuroendocrine-low SCLC. J. Thorac. Oncol. https://doi.org/10.1016/j.jtho.2022.06.004 (2022).
Mollaoglu, G. et al. MYC drives progression of small cell lung cancer to a variant neuroendocrine subtype with vulnerability to aurora kinase inhibition. Cancer Cell 31, 270–285 (2017).
Wu, Q. et al. YAP drives fate conversion and chemoresistance of small cell lung cancer. Sci. Adv. 7, eabg1850 (2021).
Chan, J. M. et al. Signatures of plasticity, metastasis, and immunosuppression in an atlas of human small cell lung cancer. Cancer Cell 39, 1479–1496 (2021).
Ireland, A. S. et al. MYC drives temporal evolution of small cell lung cancer subtypes by reprogramming neuroendocrine fate. Cancer Cell 38, 60–78 (2020).
Cejas, P. et al. Subtype heterogeneity and epigenetic convergence in neuroendocrine prostate cancer. Nat. Commun. 12, 5775 (2021).
Brady, N. J. et al. Temporal evolution of cellular heterogeneity during the progression to advanced AR-negative prostate cancer. Nat. Commun. 12, 3372 (2021).
Tully, K. M. et al. Radioimmunotherapy targeting delta-like ligand 3 in small cell lung cancer exhibits antitumor efficacy with low toxicity. Clin. Cancer Res. 28, 1391–1401 (2022).
Korsen, J. A. et al. Delta-like ligand 3-targeted radioimmunotherapy for neuroendocrine prostate cancer. Proc. Natl Acad. Sci. USA 119, e2203820119 (2022).
Ferone, G., Lee, M. C., Sage, J. & Berns, A. Cells of origin of lung cancers: lessons from mouse studies. Genes Dev. 34, 1017–1032 (2020).
Ouadah, Y. et al. Rare pulmonary neuroendocrine cells are stem cells regulated by Rb, p53, and Notch. Cell 179, 403–416 (2019).
Shimokawa, M. et al. Visualization and targeting of LGR5+ human colon cancer stem cells. Nature 545, 187–192 (2017).
Derks, J. L. et al. Clinical-pathologic challenges in the classification of pulmonary neuroendocrine neoplasms and targets on the horizon for future clinical practice. J. Thorac. Oncol. 16, 1632–1646 (2021).
Cives, M. et al. The tumor microenvironment in neuroendocrine tumors: biology and therapeutic implications. Neuroendocrinology 109, 83–99 (2019).
Bischoff, P. et al. The single-cell transcriptional landscape of lung carcinoid tumors. Int. J. Cancer 150, 2058–2071 (2022).
Stankovic, B. et al. The immune microenvironment in typical carcinoid lung tumour, a brief report of four cases. Scand. J. Immunol. 92, e12893 (2020).
da Silva, A. et al. Characterization of the neuroendocrine tumor immune microenvironment. Pancreas 47, 1123–1129 (2018).
Ferrata, M. et al. PD-L1 expression and immune cell infiltration in gastroenteropancreatic (GEP) and non-GEP neuroendocrine neoplasms with high proliferative activity. Front. Oncol. 9, 343 (2019).
Roberts, J. A., Gonzalez, R. S., Das, S., Berlin, J. & Shi, C. Expression of PD-1 and PD-L1 in poorly differentiated neuroendocrine carcinomas of the digestive system: a potential target for anti-PD-1/PD-L1 therapy. Hum. Pathol. 70, 49–54 (2017).
Tsunokake, J. et al. Tumor microenvironment in mixed neuroendocrine non-neuroendocrine neoplasms: interaction between tumors and immune cells, and potential effects of neuroendocrine differentiation on the tumor microenvironment. Cancers 14, 2152 (2022).
Marion-Audibert, A.-M. et al. Low microvessel density is an unfavorable histoprognostic factor in pancreatic endocrine tumors. Gastroenterology 125, 1094–1104 (2003).
Terris, B. et al. Expression of vascular endothelial growth factor in digestive neuroendocrine tumours. Histopathology 32, 133–138 (1998).
Calbo, J. et al. A functional role for tumor cell heterogeneity in a mouse model of small cell lung cancer. Cancer Cell 19, 244–256 (2011).
Kwon, M. et al. Paracrine signaling between tumor subclones of mouse SCLC: a critical role of ETS transcription factor Pea3 in facilitating metastasis. Genes Dev. 29, 1587–1592 (2015).
Denny, S. K. et al. Nfib promotes metastasis through a widespread increase in chromatin accessibility. Cell 166, 328–342 (2016).
Yang, D. et al. Axon-like protrusions promote small cell lung cancer migration and metastasis. eLife 8, e50616 (2019).
Best, S. A. et al. Harnessing natural killer immunity in metastatic SCLC. J. Thorac. Oncol. 15, 1507–1521 (2020).
Chen, H.-Z. et al. Genomic and transcriptomic characterization of relapsed SCLC through rapid research autopsy. JTO Clin. Res. Rep. 2, 100164 (2021).
Nguyen, B. et al. Genomic characterization of metastatic patterns from prospective clinical sequencing of 25,000 patients. Cell 185, 563–575 (2022).
Yao, J. C. et al. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet 387, 968–977 (2016).
Rinke, A. et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J. Clin. Oncol. 27, 4656–4663 (2009).
Caplin, M. E. et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N. Engl. J. Med. 371, 224–233 (2014).
Yao, J. C. et al. Everolimus for advanced pancreatic neuroendocrine tumors. N. Engl. J. Med. 364, 514–523 (2011).
Caplin, M. E. et al. Lanreotide autogel/depot in advanced enteropancreatic neuroendocrine tumours: final results of the CLARINET open-label extension study. Endocrine 71, 502–513 (2021).
Singh, S., Poon, R., Wong, R. & Metser, U. 68Ga PET imaging in patients with neuroendocrine tumors: a systematic review and meta-analysis. Clin. Nucl. Med. 43, 802–810 (2018).
Reubi, J. C. et al. Detection of somatostatin receptors in surgical and percutaneous needle biopsy samples of carcinoids and islet cell carcinomas. Cancer Res. 50, 5969–5977 (1990).
Susini, C. & Buscail, L. Rationale for the use of somatostatin analogs as antitumor agents. Ann. Oncol. 17, 1733–1742 (2006).
Strosberg, J. et al. Phase 3 trial of 177Lu-Dotatate for midgut neuroendocrine tumors. N. Engl. J. Med. 376, 125–135 (2017).
Cives, M. et al. The role of cytotoxic chemotherapy in well-differentiated gastroenteropancreatic and lung neuroendocrine tumors. Curr. Treat. Options Oncol. 20, 72 (2019).
Moertel, C. G., Hanley, J. A. & Johnson, L. A. Streptozocin alone compared with streptozocin plus fluorouracil in the treatment of advanced islet-cell carcinoma. N. Engl. J. Med. 303, 1189–1194 (1980).
Strosberg, J. R. et al. First-line chemotherapy with capecitabine and temozolomide in patients with metastatic pancreatic endocrine carcinomas. Cancer 117, 268–275 (2011).
Fine, R. L. et al. Capecitabine and temozolomide (CAPTEM) for metastatic, well-differentiated neuroendocrine cancers: the pancreas center at Columbia University experience. Cancer Chemother. Pharmacol. 71, 663–670 (2013).
Filosso, P. L. et al. Multidisciplinary management of advanced lung neuroendocrine tumors. J. Thorac. Dis. 7, S163–S171 (2015).
Forde, P. M. et al. Systemic therapy, clinical outcomes, and overall survival in locally advanced or metastatic pulmonary carcinoid: a brief report. J. Thorac. Oncol. 9, 414–418 (2014).
Horn, L. et al. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N. Engl. J. Med. 379, 2220–2229 (2018).
Paz-Ares, L. et al. Durvalumab plus platinum-etoposide versus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): a randomised, controlled, open-label, phase 3 trial. Lancet 394, 1929–1939 (2019).
Paz-Ares, L. et al. Durvalumab, with or without tremelimumab, plus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer: 3-year overall survival update from CASPIAN. ESMO Open 7, 100408 (2022).
Moertel, C. G., Kvols, L. K., O’Connell, M. J. & Rubin, J. Treatment of neuroendocrine carcinomas with combined etoposide and cisplatin. Evidence of major therapeutic activity in the anaplastic variants of these neoplasms. Cancer 68, 227–232 (1991).
Mitry, E. et al. Treatment of poorly differentiated neuroendocrine tumours with etoposide and cisplatin. Br. J. Cancer 81, 1351–1355 (1999).
Zhang, P. et al. Etoposide and cisplatin versus irinotecan and cisplatin as the first-line therapy for patients with advanced, poorly differentiated gastroenteropancreatic neuroendocrine carcinoma: a randomized phase 2 study. Cancer 126, 2086–2092 (2020).
Li, R. et al. Multi-omics profiling of primary small cell carcinoma of the esophagus reveals RB1 disruption and additional molecular subtypes. Nat. Commun. 12, 3785 (2021).
Selenica, P. et al. APOBEC mutagenesis, kataegis, chromothripsis in EGFR-mutant osimertinib-resistant lung adenocarcinomas. Ann. Oncol. https://doi.org/10.1016/j.annonc.2022.09.151 (2022).
Takayanagi, D. et al. Comparative analysis of genetic alterations, HPV-status, and PD-L1 expression in neuroendocrine carcinomas of the cervix. Cancers 13, 1215 (2021).
Meuwissen, R. et al. Induction of small cell lung cancer by somatic inactivation of both Trp53 and Rb1 in a conditional mouse model. Cancer Cell 4, 181–189 (2003).
Kawasaki, K., Fujii, M. & Sato, T. Gastroenteropancreatic neuroendocrine neoplasms: genes, therapies and models. Dis. Model. Mech. 11, dmm029595 (2018).
Caeser, R. et al. Genomic and transcriptomic analysis of a library of small cell lung cancer patient-derived xenografts. Nat. Commun. 13, 2144 (2022).
Kim, M. et al. Patient-derived lung cancer organoids as in vitro cancer models for therapeutic screening. Nat. Commun. 10, 3991 (2019).
Sachs, N. et al. Long-term expanding human airway organoids for disease modeling. EMBO J. 38, e100300 (2019).
April-Monn, S. L. et al. Three-dimensional primary cell culture: a novel preclinical model for pancreatic neuroendocrine tumors. Neuroendocrinology 111, 273–287 (2021).
Gao, H. et al. High-throughput screening using patient-derived tumor xenografts to predict clinical trial drug response. Nat. Med. 21, 1318–1325 (2015).
Vlachogiannis, G. et al. Patient-derived organoids model treatment response of metastatic gastrointestinal cancers. Science 359, 920–926 (2018).
Ooft, S. N. et al. Patient-derived organoids can predict response to chemotherapy in metastatic colorectal cancer patients. Sci. Transl. Med. 11, eaay2574 (2019).
Toshimitsu, K. et al. Organoid screening reveals epigenetic vulnerabilities in human colorectal cancer. Nat. Chem. Biol. 18, 605–614 (2022).
Cheng, D. T. et al. Memorial Sloan Kettering-integrated mutation profiling of actionable cancer targets (MSK-IMPACT): a hybridization capture-based next-generation sequencing clinical assay for solid tumor molecular oncology. J. Mol. Diagn. 17, 251–264 (2015).
Acknowledgements
The work of C.M.R. is supported by the US NIH National Cancer Institute (NCI) grants R35 CA263816 and U24 CA213274. Generation of the data for Fig. 3 was supported in part by the Marie-Josée and Henry R. Kravis Center for Molecular Oncology and the NCI Cancer Center Core Grant P30 CA008748. The authors gratefully acknowledge S. Tischfield and the members of the Molecular Diagnostics Service in the Department of Pathology at the Memorial Sloan Kettering Cancer Center for their assistance in drafting the figures for this manuscript.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding authors
Ethics declarations
Competing interests
C.M.R. has consulted regarding oncology drug development for AbbVie, Amgen, AstraZeneca, D2G, Daiichi Sankyo, Epizyme, Genentech/Roche, Ipsen, Jazz, Kowa, Lilly, Merck and Syros, and serves on the scientific advisory boards of Bridge Medicines, Earli, and Harpoon Therapeutics. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Clinical Oncology thanks P. Bunn; M. Falconi, who co-reviewed with V. Andreasi; G. Pelosi; and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
ClinicalTrials.gov: https://www.clinicaltrials.gov/ct2/home
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kawasaki, K., Rekhtman, N., Quintanal-Villalonga, Á. et al. Neuroendocrine neoplasms of the lung and gastrointestinal system: convergent biology and a path to better therapies. Nat Rev Clin Oncol 20, 16–32 (2023). https://doi.org/10.1038/s41571-022-00696-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41571-022-00696-0
This article is cited by
-
Decoding the basis of histological variation in human cancer
Nature Reviews Cancer (2024)
-
Neuroendokrine Tumoren der Lunge: State of the Art
Journal für Endokrinologie, Diabetologie und Stoffwechsel (2024)
-
Multiple bronchial carcinoids associated with Cowden syndrome
Endocrine (2024)
-
Niacin restriction with NAMPT-inhibition is synthetic lethal to neuroendocrine carcinoma
Nature Communications (2023)