Abstract
Coronavirus disease 2019 (COVID-19) is a highly contagious disease that appeared in China in December 2019 and spread rapidly around the world. Several patients with severe COVID-19 infection can develop a coagulopathy according to the ISTH criteria for disseminated intravascular coagulopathy (DIC) with fulminant activation of coagulation, resulting in widespread microvascular thrombosis and consumption of coagulation factors. We conducted a meta-analysis in order to explore differences in coagulopathy indices in patients with severe and non-severe COVID-19. An electronic search was performed within PubMed, Google Scholar and Scopus electronic databases between December 2019 (first confirmed Covid-19 case) up to April 6th, 2020. The primary endpoint was the difference of D-dimer values between Non-Severe vs Severe disease and Survivors vs Non-Survivors. Furthermore, results on additional coagulation parameters (platelet count, prothrombin time, activated partial thromboplastin time) were also analyzed. The primary analysis showed that mean d-dimer was significantly lower in COVID-19 patients with non-severe disease than in those with severe (SMD − 2.15 [− 2.73 to − 1.56], I2 98%, P < 0.0001). Similarly, we found a lower mean d-dimer in Survivors compared to Non-Survivors (SMD − 2.91 [− 3.87 to − 1.96], I2 98%, P < 0.0001). Additional analysis of platelet count showed higher levels of mean PLT in Non-Severe patients than those observed in the Severe group (SMD 0.77 [0.32 to 1.22], I2 96%, P < 0.001). Of note, a similar result was observed even when Survivors were compared to Non-Survivors (SMD 1.84 [1.16 to 2.53], I2 97%, P < 0.0001). Interestingly, shorter mean PT was found in both Non-Severe (SMD − 1.34 [− 2.06 to − 0.62], I2 98%, P < 0.0002) and Survivors groups (SMD − 1.61 [− 2.69 to − 0.54], I2 98%, P < 0.003) compared to Severe and Non-Survivor patients. In conclusion, the results of the present meta-analysis demonstrate that Severe COVID-19 infection is associated with higher D-dimer values, lower platelet count and prolonged PT. This data suggests a possible role of disseminated intravascular coagulation in the pathogenesis of COVID-19 disease complications.
Similar content being viewed by others
Introduction
Coronavirus Disease 2019 (COVID-19), caused by a novel coronavirus (SARS-CoV-2), is a highly contagious disease that appeared in Wuhan, Hubei province of China in December 2019 and spread rapidly in China and even around the world1.
Most of the infected patients have mild symptoms including fever, fatigue and cough. Nevertheless, in severe cases, patients can progress rapidly and develop the acute respiratory distress syndrome, septic shock, metabolic acidosis and coagulopathy2.
Although COVID-19 has a relatively low mortality rate, it can be highly deadly and lethal, especially in high-risk patients, and to date, there is no specific treatment available for this new disease. Therefore, it is mandatory to identify potential risk factors for predicting disease progression and severity. Coagulation abnormalities have been already detected in other severe coronavirus infections. Prolonged activated partial-thromboplastin time, elevated D-dimer and thrombocytopenia have been described in patients with SARS-CoV1. Moreover, even if less data is available about MERS-CoV, DIC was often associated with fatal cases of this very severe form of pneumonia3. Similarly, several patients with severe COVID-19 infection can develop a coagulopathy according to the International Society on Thrombosis and Haemostasis (ISTH) criteria for disseminated intravascular coagulopathy (DIC) with fulminant activation of coagulation4, resulting in widespread microvascular thrombosis and consumption of coagulation factors (Fig. 1).
Pathogenesis of disseminated intravascular coagulation. DIC is characterized by systemic activation of blood coagulation, which results in generation and deposition of fibrin, leading to microvascular thrombi contributing to multi-organ dysfunction. Furthermore, consumption of clotting factors and platelets can result in life-threatening hemorrhage.
SARS-CoV-2 infection has been in fact associated with pulmonary embolism5, deep vein thrombosis and microthrombi formation6. The pro-inflammatory environment resulting from the infection causes an endothelial dysfunction that could be responsible of an imbalance between pro-thrombotic and anti-thrombotic factors. The resulting hyper thrombotic state carries unique hallmarks, in a certain grade overlapping with DIC, that need to be fully discovered yet. The attention on this aspect is so high that it has been postulated that the COVID-19, previously considered mainly as a respiratory disease, could be instead defined in his most severe form an endothelial disease7.
D-dimer is a soluble fibrin degradation product deriving from the plasmin-mediated degradation of cross-linked fibrin can be considered a biomarker of activation of coagulation and fibrinolysis8. D-Dimer has been found increased in COVID-19 patients9, and Zhou et al. demonstrated that the d-dimer levels on admission greater than 1 μg/mL were associated with an increase of in-hospital death10. Moreover, Xiang et al. demonstrated in a metanalysis including 16 observational studies higher mortality rate in patients with COVID-19-related coagulopathy (RR 10.86, 2.86 to 41.24, P < 0.001)11. Thus, the data related to coagulation parameters in different stages of COVID-19 disease may be of paramount importance to consider therapeutic prophylaxis or anticoagulation.
This study aims to summarize all available data on coagulation parameters in COVID-19 patients, particularly platelet count, Prothrombin Time (PT), D-dimer, and fibrinogen as suggested from the ISTH Interim Guidance on recognition and management of coagulopathy in COVID‐1912, and to perform a meta-analysis to assess differences in coagulopathy indices in different stages of COVID-19 disease.
Methods
Search strategy and study selection
An electronic search was performed within PubMed, Google Scholar and Scopus electronic databases between December 2019 (first confirmed Covid-19 case) up to April 6th, 2020. The following keywords were used for the search: “laboratory” or “coagulation” and “COVID-19” or “Coronavirus” or “SARS-CoV-2”. The English language was a limiting criterium for our analysis. All reports, including the search terms, were independently screened by two investigators for relevance and eligibility (I.L. and A.P.). Additionally, references from relevant articles were also manually scanned for additional studies. Where data were not available in the published study reports, authors were contacted, whenever possible, to supply missing information by email. The authors discussed their evaluation, and any disagreement was resolved through discussion and re-reading.
Inclusion and exclusion criteria
Studies were considered eligible if the following statements were applying (a) they involved a study population with COVID-19 confirmed infection; (b) studies that stratify the risk of severe or fatal COVID-19; (c) they reported information on the difference of D-dimer values between two groups. Exclusion criteria were (just one was sufficient for study exclusion): non-original articles or articles with the number of patients less than 10, a duplicate publication with the same endpoint, endpoint measure not specified.
Endpoints
The primary endpoint was the difference of D-dimer values between Non-Severe vs Severe disease and Survivors vs Non-Survivors. Moreover, results on additional coagulation parameters (platelets count, prothrombin time, activated partial thromboplastin time) were also analyzed.
Data abstraction and management
Baseline characteristics and laboratory data were abstracted from the single studies through carefully scanning of the full article by two independent reviewers (I.L. and AP). Divergences were resolved by consensus. Moreover, the following data was extracted: year of publication, location, number of study patients, source type, peer-review process, study design, study groups. Selection and data abstraction were performed according to the MOOSE (Meta-analyses Of Observational Studies in Epidemiology) and PRISMA Checklist (Supplemental Tables S1, S2). The quality analysis of the selected studies was performed using the Agency for Healthcare Research and Quality (AHRQ) for cross-sectional study form (Supplemental Table S3).
Statistical analysis
Mean and standard deviation were calculated from median and interquartile range (IQR), according to the formula reported by Wan et al.13 The summary measure used was the Standardized Mean Difference (SMD) with 95% confidence. Random-effects meta-analysis was used because high variability between studies was expected. Heterogeneity was evaluated using the I2 statistic. Cut-off values of 25%, 50%, and 75% indicated low, moderate, and high heterogeneity, respectively. Next, to explore potential sources of heterogeneity, we conducted a subgroup analysis between peer-reviewed/non-peer-reviewed articles. Finally, sensitivity analyses were performed by systematically removing each study, in turn, to explore its effect on outcome as previously described14,15. Publication bias was evaluated by the Egger test. Forest plots were used to graphically display the results of the meta-analysis, as already previously described16,17. All Analyses were performed using R Statistical Software (version 3.6.3; R Foundation for Statistical Computing, Vienna, Austria).
Results
Search results
Our search retrieved a total of 3439 entries, which were reduced to 3252 studies after duplicates removed. After the screening of 322 records, 290 studies were then excluded because they were not related to our research question. In the assessment of eligibility, further 20 studies were excluded because of: duplicate publication; outcome not reported; not original articles. Finally, a total of 35 studies were available for the analysis, including 6427 patients9,10,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50. The study selection procedure is reported in detail in Fig. 2.
Data on included studies
Since randomized trials were not currently available, only retrospective studies were included in the present meta-analysis. Table 1 summarizes the most relevant characteristics of the selected studies. Sixteen studies were peer-reviewed9,10,18,19,20,21,22,23,24,25,26,27,28,29,30,31, 19 were non-peer-reviewed32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50. Not surprisingly, quality assessment revealed a non-high study quality (Supplemental Table S1). Across the studies, patients were predominantly male and approximately one-fourth of patients had a history of cardiovascular disease. More details on patients’ characteristics are provided in Table 2.
Meta-analysis results
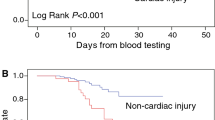
The primary analysis showed that mean d-dimer is significantly lower in COVID-19 patients with non-severe disease than in those with severe infection (SMD − 2.15 [− 2.73 to − 1.56], I2 98%, P < 0.0001) (Fig. 3, panel A). Similarly, we found a much lower mean d-dimer in Survivors compared to Non-Survivors (SMD − 2.91 [− 3.87 to − 1.96], I2 98%, P < 0.0001) (Fig. 3, panel B).
Forest plots of the standardized mean difference in d-dimer levels. (A) Non severe vs Severe patients. The black squares represent the pooled standardized mean difference effect size for each analysis while the left and right extremes of the squares represent the corresponding 95% confidence intervals for the pooled standardized mean difference effect size for each analysis. All analyses are based on a random-effects model. (B) Survivors vs Non-Survivors. The black squares represent the pooled standardized mean difference effect size for each analysis while the left and right extremes of the squares represent the corresponding 95% confidence intervals for the pooled standardized mean difference effect size for each analysis. All analyses are based on a random-effects model.
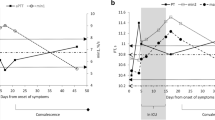
Additional analysis of platelet count showed higher mean PLT in Non-Severe patients than those observed in the Severe group (SMD 0.77 [0.32 to 1.22], I2 96%, P < 0.001) (Fig. 4, panel A). Of note, a similar result was observed even when Survivors were compared to Non-Survivors (SMD 1.84 [1.16 to 2.53], I2 97%, P < 0.0001) (Fig. 4, panel D).
Forest plots of the standardized mean difference in platelets count (PLT), prothrombin time (PT) and activated partial thromboplastin time (aPTT). (A–C) Forest plots of the standard mean difference in PLT count, PT and aPTT between Non Severe and Severe patients. (D–F) Forest plots of the standard mean difference in PLT count, PT and aPTT between Survivors and Non-Survivors.
Interestingly, shorter mean PT was found in both Non-Severe (SMD − 1.34 [− 2.06 to − 0.62], I2 98%, P < 0.0002) (Fig. 4, panel B) and Survivors groups (SMD − 1.61 [− 2.69 to − 0.54], I2 98%, P < 0.003) (Fig. 4, panel E) compared to Severe and Non-Survivor patients.
Whether no statistically significant differences were found in mean aPPT in both Non-Severe/Severe (SMD 0.39 [− 0.33 to 1.12], I2 98%, P = 0.28) and Survivors/Non-Survivors (SMD 0.58 [− 0.42 to 1.58], I2 97%, P = 0.26) (Fig. 4, panels C–F). Mean Fibrinogen was lower in both Non-Severe (SMD − 1.27 [− 1.86 to − 0.68], I2 92%, P < 0.0001) (Supplementary Fig. S3, panel A) and Survivor patients (SMD − 1.16 [− 2.29 to − 0.04], I2 94%, P = 0.04) (Supplementary Fig. S3, panel B). Even if few data was available in the studies included in our analysis regarding Fibrin Degradation Products (FDP) (Supplementary Fig. S4) and International Normalized Ratio (INR) (Supplementary Fig. S5) we found higher values for both parameters in Severe patients (SMD − 0.74 [− 1.46 to − 0.02], I2 89%, P = 0.04 and SMD − 2.38 [− 5.13 to 0.36], I2 98%, P = 0.08 respectively).
Subgroup and sensitivity analyses for the primary endpoint
As both peer-reviewed and non-peer-reviewed studies were included in this analysis (Table 1), we performed a subgroup analysis, revealing a similar result for both study types for the primary endpoint (peer-reviewed SMD − 1.90 [− 2.95 to − 0.84], I2 98%, P < 0.001; non-peer-reviewed SMD − 2.34 [− 3.0 to − 1.68], I2 97%, P < 0.0001) (Supplemental Fig. S1, panels A,B).
Moreover, sensitivity analysis performed by the leave-one-out approach showed that no single study had a substantial contribution to the pooled mean difference (Supplemental Fig. S2, panels A,B).
Metaregression analysis
To evaluate the possible confounding effect of age on D-Dimer levels we performed a metaregression analysis using as covariate the ratio of mean age between the two groups (severe/non severe). No significant correlation between age and D-Dimer levels (SE 0.386; P = 0.772) were found at this additional analysis. Similar results have been obtained accepting as covariate the ratio of days from onset of symptoms to hospitalization between the two groups (SE 0.491; P = 0.274; Supplemental Fig. S5).
Publication bias
No evidence of publication bias was found by Egger’s test. The P values were: P = 0.07 for D-dimer, 0.81 for PLT, 0.13 for PT, and 0.10 for aPTT.
Discussion
The major finding of the present meta-analysis is that higher levels of D-Dimer were found in patients with severe COVID-19. Finally, the mean platelet count is lower and mean prothrombin time more prolonged in Severe and Non-Survivor Covid-19 patients, supporting the concept that patients infected by COVID-19 may be at risk of developing disseminated intravascular coagulation (DIC). In fact, high d-dimer levels, low platelet count and prolonged PT are critical parameters of ISTH Criteria for DIC3. These findings corroborate the hypothesis that considers the COVID-19, in its most severe form, an endothelial disease7.
No differences in aPTT levels were found between the two groups, consistent with the results of a recently published metanalysis including 2277 patients51. In a study by Tang et al. from Wuhan, 71% of non-survivors from COVID-19 infection met the ISTH criteria for DIC compared to 0.4% of survivors. Elevated D-dimer values at admission and markedly increased over time were associated with a worse clinical outcome, likely reflecting coagulation activation from infection, cytokine storm and multiorgan failure52,53.
Lippi et al.54 showed in a brief letter reporting a pooled analysis of 4 studies that D-dimer is associated with the severity of COVID-19 disease. The mean difference of the four studies which reported continuous values (totaling 553 patients, 22% with severe disease) showed that D-dimer values are considerably higher in COVID-19 patients with severe disease than in those without (WMD: 2.97 mg/L; 95% CI 2.47–3.46 mg/L). Similarly, a recent metanalysis reported higher D-Dimer levels in patients with a more severe form of the disease (WMD 0.60, 0.49–0.71, I2 = 83.85%). Interestingly, this association seems to be independent from race and ethnicity55.
The obvious consideration is related to therapy with heparin to limit coagulopathy. However, to degrade pre‐existing fibrin in the lung it is essential to promote local fibrinolysis and a nebulizer form of tissue‐type plasminogen activator (tPA) to treat COVID‐19 has been recently proposed56.
Only one of the study included in our analysis investigated the effects of anticoagulation with low molecular weight heparin (LMWH) therapy on survival of Covid-19 patients, demonstrating that the use of anticoagulant therapy resulted in lower mortality in patients with severe coagulopathy with SIC score ≥ 4 (LMWH: 40.0% vs No-LMWH: 64.2%, P = 0.029) or D-dimer > sixfold of upper limit of normal (32.8% vs 52.4%, P = 0.017), but no overall benefit between heparin users and nonusers (30.3% vs 29.7%, P = 0.910)23. Moreover, a propensity-score matched retrospective study of 2785 COVID‐19 patients showed a significantly reduced cumulative incidence of in‐hospital death (HR 0.518 [0.308–0.872]) with the use of intermediate‐dose of anticoagulation compared to the only prophylactic‐dose and with the use of aspirin compared to no antiplatelet therapy (HR 0.522 [0.336–0.812])57.
Although coagulopathy recognizes multifactorial aetiology, our findings suggest that the worsening of coagulation parameters may indicate progressive severity of COVID-19 infection and may predict the need of more aggressive critical care and treatment. Thus, patients in the Intensive Care Unit (ICU) should have pharmacologic prophylaxis if there is not a contraindication and the benefit of heparin in COVID-19 patients in different stages of disease should be assessed. Clotting problems and antithrombotic therapy should be included in the daily COVID-19 management process, rather than just focusing on the infection. Furthermore, possible complications related to intravascular clotting should always be taken into account in the presence of worsening clinical conditions. Obviously, the risk of bleeding should always be considered in the individual patient when anticoagulant drugs are administered58.
Further studies are needed to define the role of coagulation indices in guiding the optimal timing to start antithrombotic drugs and the selection of patients in which this kind of therapies could have a greater prognostic impact.
Limitations
Our study has some limitations. First, in the absence of randomized clinical trials, our analysis reported only data from retrospective and observational studies. Second, since there is significant heterogeneity, we used a random-effects model for all analyses. Third, the definition of the endpoints is variable in the different studies. Thus, we performed a subgroup analysis (Severe/Non Severe, Non Survivors/Survivors) to overcome this issue. Moreover, we took for our analysis laboratory data on admission in hospital of COVID-19 patients and this could represents a bias. However, the purpose of our study was to identify reliable biomarkers of severity on admission, in order to investigate the association of these biomarkers with disease severity.
Conclusions
Results of the present meta-analysis demonstrate that Severe COVID-19 infection is associated with higher D-dimer values, lower platelet count and prolonged PT. This data suggests a possible role of disseminated intravascular coagulation in the pathogenesis of severe COVID-19 disease.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Zhu, N. et al. a novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382, 727–733 (2020).
Guan, W. et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. https://doi.org/10.1056/nejmoa2002032 (2020).
Giannis, D., Ziogas, I. A. & Gianni, P. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J. Clin. Virol. 127, 104362 (2020).
Taylor, F. Jr., Toh, C.-H., Hoots, K., Wada, H. & Levi, M. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb. Haemost. 86, 1327–1330 (2001).
Fauvel, C. et al. Pulmonary embolism in COVID-19 patients: A French multicentre cohort study. Eur. Heart J. 41, 3058–3068 (2020).
Zhang, L. et al. Deep vein thrombosis in hospitalized patients with COVID-19 in Wuhan, China. Circulation 142, 114–128 (2020).
Libby, P. & Lüscher, T. COVID-19 is, in the end, an endothelial disease. Eur. Heart J. 41, 3038–3044 (2020).
Favresse, J. et al. D-dimer: Preanalytical, analytical, postanalytical variables, and clinical applications. Crit. Rev. Clin. Lab. Sci. 55, 548–577 (2018).
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet 395, 497–506 (2020).
Zhou, F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. The Lancet 395, 1054–1062 (2020).
Xiang, G. et al. The effect of coagulation factors in 2019 novel coronavirus patients. Medicine 100, e24537 (2021).
Thachil, J. et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J. Thromb. Haemost. 18, 1023–1026 (2020).
Wan, X., Wang, W., Liu, J. & Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. https://doi.org/10.1186/1471-2288-14-135 (2014).
De Rosa, S., Polimeni, A., Petraco, R., Davies, J. E. & Indolfi, C. Diagnostic performance of the instantaneous wave-free ratio. Circ. Cardiovasc. Interv. https://doi.org/10.1161/CIRCINTERVENTIONS.116.004613 (2018).
Polimeni, A., De Rosa, S., Sabatino, J., Sorrentino, S. & Indolfi, C. Impact of intracoronary adenosine administration during primary PCI: A meta-analysis. Int. J. Cardiol. 203, 1032–1041 (2016).
Polimeni, A. et al. Clinical and procedural outcomes of 5-French versus 6-French sheaths in transradial coronary interventions. Medicine 94, e2170 (2015).
De Rosa, S., Polimeni, A., Sabatino, J. & Indolfi, C. Long-term outcomes of coronary artery bypass grafting versus stent-PCI for unprotected left main disease: A meta-analysis. BMC Cardiovasc. Disord. https://doi.org/10.1186/s12872-017-0664-5 (2017).
Chen, G. et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J. Clin. Investig. https://doi.org/10.1172/jci137244 (2020).
Chen, T. et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study. BMJ https://doi.org/10.1136/bmj.m1091 (2020).
Deng, Q. et al. Suspected myocardial injury in patients with COVID-19: Evidence from front-line clinical observation in Wuhan, China. Int. J. Cardiol. https://doi.org/10.1016/j.ijcard.2020.03.087 (2020).
Gao, Y. et al. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J. Med. Virol. https://doi.org/10.1002/jmv.25770 (2020).
Han, H. et al. Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. Clin. Chem. Lab. Med. 58, 1116 (2020).
Tang, N. et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J. Thromb. Haemost. https://doi.org/10.1111/jth.14817 (2020).
Wan, S. et al. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J. Med. Virol. https://doi.org/10.1002/jmv.25783 (2020).
Wang, D. et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA 323, 1061 (2020).
Wang, L. et al. Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up. J. Infect. https://doi.org/10.1016/j.jinf.2020.03.019 (2020).
Wu, J. et al. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19). J. Intern. Med. https://doi.org/10.1111/joim.13063 (2020).
Wu, C. et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med. https://doi.org/10.1001/jamainternmed.2020.0994 (2020).
Zhang, J. et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. https://doi.org/10.1111/all.14238 (2020).
Zheng, C. et al. Risk-adapted treatment strategy for COVID-19 patients. Int. J. Infect. Dis. 94, 74–77 (2020).
Zhou, Y., Zhang, Z., Tian, J. & Xiong, S. Risk factors associated with disease progression in a cohort of patients infected with the 2019 novel coronavirus. Ann. Palliat. Med.e 9, 428–436 (2020).
Cai, Q. et al. COVID-19 in a designated infectious diseases hospital outside Hubei Province, China. Allergy. https://doi.org/10.1101/2020.02.17.20024018 (2020).
Huang, H. et al. Prognostic factors for COVID-19 pneumonia progression to severe symptom based on the earlier clinical features: A retrospective analysis. Front. Med. https://doi.org/10.1101/2020.03.28.20045989 (2020).
Li, K. et al. Radiographic findings and other predictors in adults with Covid-19. MedRxiv 236, 1067. https://doi.org/10.1101/2020.03.23.20041673 (2020).
Li, Z. et al. Kidney dysfunctions of COVID-19 patients: A multi-centered, retrospective, observational study. SSRN Electron. J. https://doi.org/10.2139/ssrn.3556634 (2020).
Li, J. et al. Leukopenia predicts risk for death in critically ill patients with COVID-19 in Wuhan, China: A single-centered, retrospective study. SSRN Electron. J. https://doi.org/10.2139/ssrn.3555248 (2020).
Liu, J. et al. Exploring the law of development and prognostic factors of common and severe COVID-19: A retrospective case-control study in 122 patients with complete course of disease. SSRN Electron. J. https://doi.org/10.2139/ssrn.3555209 (2020).
Liu, J. et al. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients. EBioMedicine 55, 102763. https://doi.org/10.1101/2020.02.16.20023671 (2020).
Lu, H. et al. A descriptive study of the impact of diseases control and prevention on the epidemics dynamics and clinical features of SARS-CoV-2 outbreak in Shanghai, lessons learned for metropolis epidemics prevention. MedRxiv. https://doi.org/10.1101/2020.02.19.20025031 (2020).
Lu, Z. et al. Clinical characteristics and risk factors for fatal outcome in patients with 2019-coronavirus infected disease (COVID-19) in Wuhan, China. SSRN Electron. J. https://doi.org/10.2139/ssrn.3546069 (2020).
Luo, X. et al. Characteristics of patients with COVID-19 during epidemic ongoing outbreak in Wuhan, China. MedRxiv. https://doi.org/10.1101/2020.03.19.20033175 (2020).
Ma, K.-L. et al. COVID-19 myocarditis and severity factors: An adult cohort study. MedRxiv. https://doi.org/10.1101/2020.03.19.20034124 (2020).
Qian, G.-Q. et al. Epidemiologic and clinical characteristics of 91 hospitalized patients with COVID-19 in Zhejiang, China: A retrospective, multi-centre case series. Int. J. Med. https://doi.org/10.1101/2020.02.23.20026856 (2020).
Wang, K. et al. Clinical and laboratory predictors of in-hospital mortality in 305 patients with COVID-19: A cohort study in Wuhan, China. SSRN Electron. J. https://doi.org/10.2139/ssrn.3546115 (2020).
Xu, Y. et al. Clinical characteristics of SARS-CoV-2 pneumonia compared to controls in Chinese Han population. MedRxiv. https://doi.org/10.1101/2020.03.08.20031658 (2020).
Zeng, J.-H. et al. Clinical characteristics and cardiac injury description of 419 cases of COVID-19 in Shenzhen, China. SSRN Electron. J. https://doi.org/10.2139/ssrn.3556659 (2020).
Zhang, F. et al. Myocardial injury is associated with in-hospital mortality of confirmed or suspected COVID-19 in Wuhan, China: A single center retrospective cohort study. MedRxiv 395, 497. https://doi.org/10.1101/2020.03.21.20040121 (2020).
Zhang, G. et al. Clinical features and outcomes of 221 patients with COVID-19 in Wuhan, China. SSRN. https://doi.org/10.1101/2020.03.02.20030452 (2020).
Zheng, X. et al. Clinical features and risk factors for the severity of inpatients with COVID-19: A retrospective cohort study. SSRN Electron. J. https://doi.org/10.2139/ssrn.3562460 (2020).
Zhou, Y. et al. A new predictor of disease severity in patients with COVID-19 in Wuhan, China. MedRxiv. https://doi.org/10.1101/2020.03.24.20042119 (2020).
Zhang, A. et al. Meta-analysis of coagulation parameters associated with disease severity and poor prognosis of COVID-19. Int. J. Infect. Dis. 100, 441–448 (2020).
Tang, N., Li, D., Wang, X. & Sun, Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 18, 844–847 (2020).
Gungor, B. et al. Elevated D-dimer levels on admission are associated with severity and increased risk of mortality in COVID-19: A systematic review and meta-analysis. Am. J. Emerg. Med. 39, 173–179 (2021).
Lippi, G. & Favaloro, E. J. D-dimer is associated with severity of coronavirus disease 2019: A pooled analysis. Thromb. Haemost. https://doi.org/10.1055/s-0040-1709650 (2020).
Chaudhary, R. et al. Thrombo-inflammatory biomarkers in COVID-19: Systematic review and meta-analysis of 17,052 patients. Mayo Clin. Proc. Innov. Qual. Outcomes. https://doi.org/10.1016/j.mayocpiqo.2021.01.009 (2021).
Whyte, C. S., Morrow, G. B., Mitchell, J. L., Chowdary, P. & Mutch, N. J. Fibrinolytic abnormalities in acute respiratory distress syndrome (ARDS) and versatility of thrombolytic drugs to treat COVID-19. J. Thromb. Haemost. https://doi.org/10.1111/jth.14872 (2020).
Meizlish, M. L. et al. Intermediate-dose anticoagulation, aspirin, and in-hospital mortality in COVID-19: A propensity score-matched analysis. Am. J. Hematol. 96, 471–479 (2021).
Bikdeli, B. et al. COVID-19 and thrombotic or thromboembolic disease: Implications for prevention, antithrombotic therapy, and follow-up. J. Am. Coll. Cardiol. https://doi.org/10.1016/j.jacc.2020.04.031 (2020).
Author information
Authors and Affiliations
Contributions
A.P., C.S. and S.S. designed the study and acquired, analysed, and interpreted data. I.L., A.P. and A.M. did the literature search and study selection procedures. J.S., S.D.R. and C.I. drafted the manuscript, with critical revisions for important intellectual content from all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Polimeni, A., Leo, I., Spaccarotella, C. et al. Differences in coagulopathy indices in patients with severe versus non-severe COVID-19: a meta-analysis of 35 studies and 6427 patients. Sci Rep 11, 10464 (2021). https://doi.org/10.1038/s41598-021-89967-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-89967-x
This article is cited by
-
Coagulation biomarkers and coronavirus disease 2019 phenotyping: a prospective cohort study
Thrombosis Journal (2023)
-
Status of major hemostatic components in the setting of COVID-19: the effect on endothelium, platelets, coagulation factors, fibrinolytic system, and complement
Annals of Hematology (2023)
-
Endothelium dysfunction and thrombosis in COVID-19 with type 2 diabetes
Endocrine (2023)
-
Plasma biomarkers associated with survival and thrombosis in hospitalized COVID-19 patients
International Journal of Hematology (2022)
-
Current and novel biomarkers of thrombotic risk in COVID-19: a Consensus Statement from the International COVID-19 Thrombosis Biomarkers Colloquium
Nature Reviews Cardiology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.