Abstract
Mucormycosis is a life-threatening opportunistic angioinvasive fungal infection. We aimed to describe the frequency, presentations, predictors, and in-hospital outcome of mucormycosis patients in the scope of CoronaVirusDisease-19 (COVID-19) during the third viral pandemic wave. This cross-sectional retrospective study included all patients who fulfilled the criteria of mucormycosis with concurrent confirmed covid19 infection admitted to Assuit University Hospital between March 2021 and July 2021. Overall, 433 patients with definite covid-19 infection, of which 33 (7.63%) participants were infected with mucormycosis. Mucormycosis was predominantly seen in males (21 vs. 12; p = 0.01). Diabetes mellitus (35% vs. 63.6%; p < 0.001), hypertension (2% vs.45.5%; p 0.04), and Smoking (26.5% vs. 54.5%; p < 0.001) were all significantly higher in mucormycosis patients. Inflammatory markers, especially E.S.R., were significantly higher in those with mucormycosis (p < 0.001). The dose of steroid intake was significantly higher among patients with mucormycosis (160 mg vs. 40 mg; p < 0.001). Except for only three patients alive by residual infection, 30 patients died. The majority (62%) of patients without mucormycosis were alive. Male sex; Steroid misuse; D.M.; Sustained inflammation; Severe infection were significant risk factors for mucormycosis by univariate analysis; however, D.M.; smoking and raised E.S.R. were predictors for attaining mucormycosis by multivariate analysis.
Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has been related to aggressive bacterial and fungal diseases1. Mucormycosis is a fungal infection caused by Mucorales fungi such as Rhizopus, Mucor, Rhizomucor, Cunninghamella, and Lichtheimia2. Phagocytes are the primary host defense against mucormycosis3.
Mucormycosis infection is characterized by extensive angio-invasion, culminating in arterial thrombosis and tissue destruction4. The clinical presentation of mucormycosis is variable because it spreads rapidly into the body systems; it affects the paranasal sinuses, then orbits, central nervous system, lungs, gastrointestinal system, kidneys, and skin. Manifestations of mucormycosis usually depend on: (a) the route of entry of fungal spores into the body, mainly by inhalation or ingestion or direct skin injection; (b) the comorbid diseases of the infected patients2.
Mucormycosis is more common in immunocompromised individuals. Diabetic ketoacidosis and steroids are the most common risk factors for mucormycosis infection. And complications such as ocular and brain involvement5. As corticosteroid treatment impairs macrophages' ability to prevent mucor fungi spores from germinating4. Moreover, high glucose due to diabetes, new-onset hyperglycemia or steroid-induced hyperglycemia is considered an ideal low oxygen environment (hypoxia).
There are many other risk factors for mucormycosis like increased ferritin, acidic medium (metabolic acidosis, diabetic ketoacidosis [DKA]) and prolonged hospitalization with or without mechanical ventilators. Also, mucormycosis can occur due to decreased phagocytic activity of white blood cells (WBC) resulting from immune suppression caused by coronavirus 19 related severe acute respiratory syndrome (SARS-CoV-2)6. Therefore, mucormycosis in those patients suffering or recovering from COVID-19 infection increased worldwide because COVID-19 infection provides a suitable environment for mucormycosis7.
Even with appropriate treatment, the rhino-orbital infection caused by the Mucorales fungus has a terrible prognosis, with up to 50% mortality8. Mucormycosis is treated by early diagnosis and controlling risk factors, then by proper surgical debridement and administration of the suitable antifungal medication. Liposomal amphotericin B (LAmB) is an efficient antifungal drug for treating mucormycosis with a minimum of 5 mg/kg. However, posaconazole and voconazole are recommended for severe refractory cases9.
Given that the current pandemic is still a significant public health concern worldwide, patients with COVID-19 should be mindful of mucormycosis, as the two illnesses can cause severe morbidity and mortality when combined. The study's objective was to describe the frequency, presentations, predictors, and in-hospital outcomes of mucormycosis patients in the context of COVID-19.
Materials and methods
Ethical statement and informed consent
We conducted a retrospective cross-sectional observational study at Assuit University Hospital's tertiary-care center. The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Assiut University College of Medicine (IRB.17300662), and the study protocol has been registered on clinical trials.gov (NCT05074043).
Informed consent was obtained from all subjects involved in the study. All patients provided informed consent after being informed that we could utilize their clinical and radiological data and face photos for research purposes and publication of identifying information/images in an online open-access publication.
Study participants
In this retrospective cross-sectional study, the clinical-record analysis included all patients who fulfilled the criteria of mucormycosis with concurrent confirmed covid19 infection who were admitted to Assuit University Hospital between March 2021 and July 2021 during the third pandemic wave to describe the frequency; presentations; predictors; the in-hospital outcome proved cases of mucormycosis infection in the context of COVID-19 diseases. With the cooperation of internists, intensivists, neurologists, otolaryngologists; ophthalmologists; and pathologists who help in confirmation of mucormycosis diagnosis by Clinical, radiological, and histopathological assessment.COVID-19 infection in the patients' records was evidence of a positive reverse transcription-polymerase chain reaction (RT-PCR) test for SARS-CoV-2. The fulfilled criteria for diagnosis of mucormycosis were based on the global guideline for diagnosing and managing mucormycosis published by the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium10. Non-confirmed COVD-19 patients by polymerase chain reaction (PCR) or suspected fungal infection were excluded from the study.
Assessment parameters
Clinical and demographics
Clinical records included patient demographics, clinical data, including age, weight, gender, body mass index (B.M.I.), and COVID-19 severity, as defined by World Health Organization (WHO) guidelines: mild, moderate, and severe was recorded11. Also, clinical records includedMucormycosissympyoms and signs, corticosteroids use, dose and duration, and other treatment modalities (antibiotics, antifungal drugs and any adjunct surgery performed for mucormycosis). In-hospital outcomes and comorbidities like the presence or absence of diabetes and its duration are also covered in the recorded data. Other comorbidities, i.e., hypertension (Cardiac, renal disease, chronic hepatic diseases. Cardiac diseases according to WHO classification12. Renal disease, whether acute kidney injury (A.K.I.)13, which is defined as any of the following: increase in serum creatinine ≥ 0.3 mg/dl within 48 h or increased serum creatinine to ≥ 1.5 times baseline within 7 days or urine volume < 0.5 ml/kg/h for 6 h) or chronic kidney disease (CKD) (Kidney damage for ≥ 3 months, as defined by structural or functional abnormalities of the kidney)14.
Laboratory; radiological and histopathological assessment
Laboratory
d-dimer, blood glucose, C-reactive protein, ferritin, creatinine; Liver function; C.B.C., electrolyte. COVID-19 was diagnosed using real-time polymerase chain reaction (RT-PCR) assays from nasopharyngeal or oro-pharyngeal swabs and C.T. chest scan (HRCT). Mucormycosis was confirmed through specific histological characteristics in biopsy specimens based on the global guideline for the diagnosis and management of mucormycosis10.
Radiology
For patients, a computerized tomography (C.T.) scan of the orbit, paranasal sinuses, and lung were done as the initial imaging examination to determine the clinical and histological types of mucormycosis, Gadolinium-enhanced magnetic resonance imaging (M.R.I.) of the orbits, brain and paranasal sinuses was also conducted for individuals with symptoms that included M.R.V.
Histopathology
Nasal mucosal tissue biopsies were obtained from the E.N.T. Department, Assiut University Hospital. Biopsies were immediately fixed in 10% formalin solution and processed by automated tissue processing till paraffin embedding, and then biopsies were serially cut into 5 µm thick sections on a glass slide. The slide was stained with hematoxylin and eosin (H&E) for microscopic evaluation using an Olympus CX41 microscope. If H&E stained sections suspected fungal bodies, other sections were prepared and stained with GomoriMethenamine Silver (G.M.S.) stain to confirm and detect the precise morphology of the fungal bodies.
Surgical procedures
Multiple sessions of transnasal endoscopic debridement of necrotic tissue from the sinonasal tract extended to the orbit and skull base in affected patients.
Outcomes
The primary endpoint of our study was to detect the predictors of mucormycosis in COVID-19 patients. Secondary endpoints included the frequency and in-hospital mortality of C.A.M.
Sample size
Our study was retrospectively enrolled all COVID 19 patients in a specific period to estimate the frequency of C.A.M. (Covid associated mucormycosis).
Statistical analysis
Data was collected and analyzed using SPSS (Statistical Package for the Social Science, version 20, I.B.M., and Armonk, New York). The Shapiro test was used to determine compliance of the data to normal distribution. Quantitative data with normal distribution were expressed as mean ± standard deviation (S.D.) and compared with the Student t-test. Quantitative data with abnormal distribution expressed as median (minimum–maximum) and compared by the Mann–Whitney test was used.
Nominal data were given as a number (n) and percentage (%). Chi2 test was implemented on such data. Predictors of mucormycosis among patients with COVID-19 infection were determined by logistic regression analysis. The confidence level was kept at 95%, and hence, the P-value was considered significant if < 0.05.
Institutional Review Board statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Assiut University College of Medicine (IRB.17300662) and the study protocol have been registered in Clinicaltrials.gov (NCT050740043).
Informed consent statement
Informed consent was obtained from all subjects involved in the study. All patients provided informed consent after being informed that we could utilize their clinical and radiological data and face photos for research purposes and publication of identifying information/images in an online open-access publication.
Results
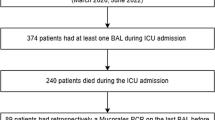
The current study enrolled 433 patients with confirmed COVID-19 infection; 33 (7.6%) patients were infected with mucormycosis based on histopathology results (Fig. 1A,B). So, the enrolled patients were subdivided based on the development of mucormycosis into; patients who were infected with mucormycosis, known as the study group (n = 33), and those who didn't infect with mucormycosis known as the control group (n = 400) (Fig. 2).
Histopathology of nasal mucormycosis. (A) A photomicrograph of a section of nasal mucormycosis that shows obvious necrosis of nasal mucosal glands and mononuclear inflammatory infiltrate (H&E stain, ×200). (B) GomoriMethenamine Silver fungal stained section of the same case in this figure highlights branched, thick fungal bodies were invading the nasal mucosal tissue (G.M.S. stain, ×200).
Baseline data of enrolled patients
Baseline line data showed that both groups had a significant difference as regard sex distribution with male predominance among patients with mucormycosis (21 (63.6%) vs. 175 (43.8%); p = 0.02). Also, patients with mucormycosis had significantly higher frequency of smoking (18 (54.5%) vs. 106 (26.5%); p < 0.001), hypertension (15 (45.5%) vs. 116 (29%); p = 0.04) and diabetes mellitus (21 (63.6%) vs. 140 (35%)). Other data are summarized in Table 1.
Clinical, laboratory and radiological data among enrolled patients
Patients with mucormycosis had significantly higher random blood sugar and lower leucocytes and hemoglobin level. Also, the erythrocyte sedimentation rate was significantly higher among those patients with mucormycosis (54.5% vs. 12%; p < 0.001). Based on chest radiology, all patients with mucormycosis had ground-glass opacity (G.G.O.). Patients with mucormycosis had a more severe disease where 48.5% and 30.3% of the severe and life-threatening disease, meanwhile 50% of those without mucormycosis had moderate disease severity.
Both groups had insignificant differences as regard SOFA score (p = 0.47).
The SOFA (Sequential Organ Failure Assessment) score can determine the level of organ dysfunction and mortality risk in I.C.U. (Intensive Care Unit) patients. based on six scores, one for each respiratory, cardiovascular, hepatic, coagulation, renal and neurological system, each scored from 0 to 4 with an increasing score reflecting worsening organ dysfunction15. Other data are summarized in Table 2.
Therapy among enrolled patients
There were significant differences between both groups regarding the use of cephalosporin, Teicoplanin, and Carbapenems, where the use of those agents was significantly higher among patients without mucormycosis. The dose of steroid intake was significantly higher among patients with mucormycosis (160 (160–200) vs. 40 (40–200) (mg); p < 0.001) Table 3.
Antifungal treatment (Amphotericin B) was given to only ten mucormycosis patients; seven patients died before the completion of their doses, and three were improved with residual infection for further surgical intervention and antifungal treatment.
Presentation among patients with mucormycosis
Except for one patient presented by rhino orbital affection.; the remaining patients presented by rhino-orbital—cerebral type. The majority of patients presented with headache and nerve palsy (mostly ocular nerves; 3rd, 4th, 6th, 5th) (81.81%); periorbital swelling and proptosis in 78.78%, which consecutively leads to diminution and loss of vision in 75.75%; hemiparesis was the least recorded neurological presentation in 9.09% (Table 4).
Predictors of mucormycosis among patients with COVID-19 infection
Based on the current study, the predictors for the development of mucormycosis among patients with COVID-19 diabetes mellitus with an odd's ratio (OR) was 13.99 (95% confidence interval (CI) = 1.96–29.79), and current smoking with OR was 3.49 (95% CI = 3.13–6.33) as well as raised E.S.R. with OR was 2.69 (95% CI = 1.71–4.03) (Table 5).
Outcome among enrolled patients
Except for only three patients alive by residual infection (one patient completely cured after antifungal and surgical debridement; 2nd 3rd by ptosis and ophthalmoplegia on treatment with diminution of vision); all other patients with mucormycosis (30 patients) were deteriorated and died. In contrast, the majority (63%) of patients without mucormycosis improved and were alive (Table 6).
Specific case scenarios of the enrolled patients (Figs. 3 and 4)
Case (1) Female patient;35y old; housewife from; Egypt; diabetic, presented by Fever; cough; respiratory failure diagnosed as severe COVID-19 by PCR; C.T. chest; admitted to I.C.U. for 1 month; received high doses of steroids injection (both methylprednisolone; dexamethasone) for 1 month then oral prednisolone for 1 month(60-40-30 mg); presented to neurology clinic by rt.3rd nerve palsy. Brain M.R.I. M.R.V. (Magnetic Resonance Venography) and C.T.; M.R.I. sinus were done with evidence of opacities on the rt side. E.N.T. surgical intervention was done with biopsy from maxillary and ethmoid sinuses mucosa showed invasive granulomatous fungal sinusitis mucormycosis. After surgical debridement and antifungal treatment, partial improvement then, she developed progressive ptosis and ophthalmoplegia, which need another surgical intervention and till now, she is still under repeated debridement and antifungal with progressive ophthalmoplegia and diminution of vision (Fig. 3).
Case (2) Male patient 62 y old; from Assiut; Egypt; heavy smoker; uncontrolled D.M., CKD grade 4 (estimated G.F.R. = 13.9 ml/min/1.73 m2); presented by bilateral rhino-facial mucormycosis and bilateral 1st;3rd,4th and 6th C.N. palsy. Diagnosed COVID-19 (by C.T. chest and PCR) during preparation for E.N.T. (Ear, Nose, and Throat) intervention. Brain M.R.I. M.R.A. C.T. sinuses with biopsy and histopathology were done to confirm the diagnosis of rhino orbital cerebral black fungus complicated by right cavernous sinus thrombosis and complete internal carotid artery occlusion. The patient showed rapid deterioration with sepsis and multi-organ failure and died (Fig. 4).
Discussion
The COVID-19 pandemic has been related to aggressive bacterial and fungal infections.The current analysis comprised 433 cases, including 33 cases of COVID-19 associated Mucormycosis (C.A.M.) (8.25%) reported between March 2021 and July 2021 during the third pandemic wave providing an updated summary of this rare clinical entity. This percentage matched with the most published articles in this context; Rawson et al. found that 8% of corona virus-positive or recovered participants had secondary fungal or bacterial infections during hospitalization, despite frequent administration of broad-spectrum antibiotics and steroids16. There was male predominance with a history of diabetes, hypertension, smoking, and glucocorticoid medication for COVID-19 control. C.A.M. patients had a high mortality rate, although adjunct surgery for mucormycosis and antifungal treatment had been given for C.A.M. cases as recorded in clinical data for better clinical results.
Old age men, smokers, diabetics, hypertensive patients, and cardiac patients have a higher risk of developing mucormycosis, which could be attributed to a change in their innate immunity, and catching a more severe and persistent COVID-19 infection and using steroids concurrently. Most of our mucormycosis patients had severe COVID-19 illness, and they all had bilateral lung affection.
Aside from the catastrophic pulmonary consequences of smoking, it is also a powerful predictor of black fungus since it can be a significant underlying cause of fungi's oral proliferation17.
Mucormycosis is associated with diabetes mellitus, a substantial risk factor18. The majority of the patients had diabetes mellitus (63.6%). According to existing evidence, people lacking phagocytes or a reduced phagocytic activity may be more prone to mucormycosis19. Neutrophils are required to stop fungal spores from spreading. In a normal host, Mucorales are also eliminated by mononuclear and polymorphonuclear phagocytes, which create reactive oxygen species and cationic peptides called defensins3. Hyperglycemia causes phagocyte malfunction, poor chemotaxis, and inefficient intracellular killing by oxidative and non-oxidative processes, as shown in patients with uncontrolled diabetes mellitus20.
Smoking is a powerful predictor of black fungus since it can operate as a crucial underlying factor in the oral proliferation of fungi, as reported by Ali et al.17, in addition to serious pulmonary problems.
Like the ones found in COVID-19 patients, excess cytokines can aggravate insulin resistance21. Insulin resistance is induced by interleukin-6 (IL-6), affecting insulin receptor and substrate-1 phosphorylation, common in COVID-19 patients22. One-third of those with mild COVID-19 had elevated IL-6 levels, which may contribute to dysglycemia in these patients23. Finally, COVID-19 treatments such as glucocorticoids, lopinavir-ritonavir, and remdesivir can lower glycemic control and raise mucormycosis21.
In addition to uncontrolled hyperglycemia, free unbound iron in the serum plays a role in the development of mucormycosis. As a result of acidosis and proton-mediated displacement of ferric iron from transferring, diabetic ketoacidosis, a key risk factor for mucormycosis, is linked to higher serum-free iron levels24.
COVID-19 is also a hyper-ferritinemic disorder. Serum ferritin levels that are too high result in the rise of intracellular iron, promoting hepatocyte apoptosis by creating reactive oxygen species. Cytokines, particularly IL-6, boost ferritin production while limiting iron export, trapping more iron inside the cell and exacerbating the situation25. Ferritin is released into the bloodstream after tissue damage; circulating ferritin loses some of its inner iron content, resulting in high free iron26. The development of ketoacidosis is another putative relationship between COVID-19 and mucormycosis. Even in the absence of diabetes mellitus, people with COVID-19 have developed ketonemia and ketoacidosis27. Acidosis reduces phagocytic function, which predisposes to mucormycosis and boosts free iron levels20.
The use of glucocorticoids is a known risk factor for developing mucormycosis19. Glucocorticoids produce immunosuppression, hyperglycemia, and lymphopenia, all of which predispose to the development of mucormycosis. The common usage of glucocorticoids in COVID-19 patients has contributed to an increase in C.A.M. cases28,29,30. Viral-induced lymphopenia and endothelities are two more variables that predispose COVID-19 patients to the development of C.A.M. Mucorales adherence and penetration to the endothelium may be aided by widespread endothelial damage reported in COVID-19 patients. Early phases in the pathophysiology of mucormycosis include endothelial adhesion and penetration30. Indeed to previous causes, early use of steroids in our patients had moderate to severe COVID-19 infection as a risk factor for catching mucormycosis.
As regards the severity of covid 19 as a predictor of M.A.C. as shown in a study by Riadetal., who found that the clinical symptoms and severity were reported in only 44.5% of the patients. Of those patients with available information, 40.8% were severe, 26.5% moderate, 18.4% mild, and 14.3% critical cases31, which correlate with our study.
The spread of fungal spores via water used in oxygen humidifiers is another indirect link between the concurrent rise in COVID-19 and mucormycosis. Indeed, hospital water can serve as a breeding ground for fungi like Mucorales32.
Furthermore, long-term usage of broad-spectrum antibiotics (carbapenems; averozolids) was a significant univariate risk factor. This is in line with the findings of 210-patient research on black fungus, which indicated that antibiotics were used to treat 100 percent of COVID-19 patients who were later diagnosed with mucormycosis. Antibiotics (Azithromycin, Doxycycline, and Carbapenems) enhance fungal infections in COVID patients in India.
In univariate analysis, high steroid doses were linked to black fungus infection, but this was not the case in multivariate analysis, which could be attributable to the early and prolonged use of steroids in all COVID 19 patients. According to the Randomized Evaluation of COVID-19 Therapy ('RECOVERY') Collaborative Group of the National Institute of Health, steroids should only be used in patients on a ventilator or require supplementary oxygen, not in milder cases33.
Furthermore, some of our participants could not afford treatment or had to discontinue using liposomal amphotericin due to financial difficulties. Participants who had combined medical and surgical care had a much better outcome, consistent with earlier research34. Surgical debridement of necrosed tissue likely allows antifungal medicines to penetrate more effectively, improving results. Those with rhino-orbital mucormycosis had the highest surgical rate. Unfortunately, even in the case of rhino-orbital illness, drastic surgery was not always possible. Patients with intracranial extension had a much higher mortality rate, with the majority being inoperable. Despite receiving proper antifungal treatment, death was significant among inoperable subjects, indicating the need for earlier detection and better therapeutic options.
Our research discovered various obstacles in controlling mucormycosis, including a delay in seeking medical help, a lack of expertise among clinicians, and financial constraints. In fact, despite being easily detectable by diagnostic sample, mucormycosis was detected after an extended period, which may explain the high fatality rate seen. Roden et al. investigated zygomycosis data in the English-language literature and assessed 929 eligible cases, finding that 96 percent of patients with disseminated illness died35.
In mucormycosis patients, the COVID-19 pandemic has spread. Over 6 months, retrospective observational research from an Egyptian tertiary care hospital discovered 12 rhino-orbito-cerebral mucormycosis (ROCM) (March 25, 2020, to September 25, 2020). During the same 6-month period in the preceding 3 years, the number of cases discovered was much higher than in the previous 3 years (1 case in 2017, 2 in 2018, and 1 in 2019)36.
Similarly, a prospective single-center observational study in India found 23 cases of invasive mucormycosis of the paranasal sinuses from August to December 202037. This contrasts with a 2015 study conducted by two prominent medical institutes in Mumbai, India, which included only 20 cases over 3 years38. Song et al. published a study in April 2020 that looked into the link between Covid-19 and invasive fungal sinusitis, concluding that a large number of patients who have been exposed to or recovered from Covid-19 are at an increased risk of developing invasive fungal diseases and offering a treatment protocol for such cases39. Except for one patient who presented early with rhino orbital infection, most of our patients presented with rhino orbital cerebral mucormycosis, requiring late surgical intervention and costly antifungal treatment. This resulted in an inferior outcome, as more than 90% of the mucor patients studied died from multi-organ failure and septicemia. This explains why mucor patients showed higher inflammatory markers (E.S.R., D-dimer, C.R.P., A.K.I., and acute liver injury) and decreased platelets and lymphopenia.
Finally, we must reevaluate the logic and value of delivering steroids to COVID-19 patients regularly to avoid the rising number of iatrogenic deaths associated with steroid usage in people infected with SARS-CoV-240.
Limitation
In this cross-sectional retrospective analysis, first, clinical records revealed that the death rate is higher than in other studies due to late presentation and the legacy of expensive therapy. Secondly, more cohort multicenter larger studies are required to better assess the incidence and prevalence of C.A.M.
Conclusions
Mucormycosis is a rare, severe and relatively fatal infection with neurological disabilities for survivors. It increased with COVID-19 due to immunity modulation and comorbidities, i.e., D.M., CKD, smoking. The main predisposing factor was uncontrolled diabetes mellitus, which was exacerbated by the use of glucocorticoids during the treatment of COVID-19. As a result, careful usage of this drug is required during the pandemic. Unfortunately, mucormycosis patients have a significant mortality rate even through adjunct surgery.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Kubin, C. J. et al. Open Forum Infectious Diseases. ofab201 (Oxford University Press US).
Skiada, A., Pavleas, I. & Drogari-Apiranthitou, M. Epidemiology and diagnosis of mucormycosis: An update. J. Fungi 6, 265 (2020).
Waldorf, A. R. Pulmonary defense mechanisms against opportunistic fungal pathogens. Immunol. Ser. 47, 243–271 (1989).
Bouchara, J. et al. Attachment of spores of the human pathogenic fungus Rhizopus oryzae to extracellular matrix components. Eur. J. Cell Biol. 70, 76–83 (1996).
Prakash, H. & Chakrabarti, A. Global epidemiology of mucormycosis. J. Fungi 5, 26 (2019).
Singh, A. K., Singh, R., Joshi, S. R. & Misra, A. Mucormycosis in COVID-19: A systematic review of cases reported worldwide and in India. Diabetes Metab. Syndr. Clin. Res. Rev. 15, 102146 (2021).
Hussain, S. et al. COVID-19-associated mucormycosis (CAM): An updated evidence mapping. Int. J. Environ. Res. Public Health 18, 10340 (2021).
Werthman-Ehrenreich, A. Mucormycosis with orbital compartment syndrome in a patient with COVID-19. Am. J. Emerg. Med. 42, 264.e265-264.e268 (2021).
Riley, T. T., Muzny, C. A., Swiatlo, E. & Legendre, D. P. Breaking the mold: A review of mucormycosis and current pharmacological treatment options. Ann. Pharmacother. 50, 747–757 (2016).
Cornely, O. A. et al. Global guideline for the diagnosis and management of mucormycosis: An initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect. Dis. 19, e405–e421 (2019).
Organization, W. H. Clinical Management of COVID-19: Interim Guidance, 27 May 2020 (World Health Organization, 2020).
Hertzer, N. R. et al. Coronary artery disease in peripheral vascular patients. A classification of 1000 coronary angiograms and results of surgical management. Ann. Surg. 199, 223 (1984).
Kellum, J. A. et al. Kidney disease: Improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. Suppl. 2, 1–138 (2012).
Levin, A. et al. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 3, 1–150 (2013).
Vincent, J. L. et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: Results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit. Care Med. 26, 1793–1800. https://doi.org/10.1097/00003246-199811000-00016 (1998).
Rawson, T. M. et al. Bacterial and fungal coinfection in individuals with coronavirus: A rapid review to support COVID-19 antimicrobial prescribing. Clin. Infect. Dis. 71, 2459–2468. https://doi.org/10.1093/cid/ciaa530 (2020).
Hameed, A. R. et al. Study of the relationship between cigarette smoking and fungi isolated from the oral cavity. Adv. Res. J. Med. Clin. Sci. 6, 92–95 (2020).
Prakash, H. et al. A prospective multicenter study on mucormycosis in India: Epidemiology, diagnosis, and treatment. Med. Mycol. 57, 395–402. https://doi.org/10.1093/mmy/myy060 (2019).
Ibrahim, A. S., Spellberg, B., Walsh, T. J. & Kontoyiannis, D. P. Pathogenesis of mucormycosis. Clin. Infect. Dis. 54(Suppl 1), S16-22. https://doi.org/10.1093/cid/cir865 (2012).
Chinn, R. Y. & Diamond, R. D. Generation of chemotactic factors by Rhizopus oryzae in the presence and absence of serum: Relationship to hyphal damage mediated by human neutrophils and effects of hyperglycemia and ketoacidosis. Infect. Immun. 38, 1123–1129. https://doi.org/10.1128/iai.38.3.1123-1129.1982 (1982).
Pal, R. & Bhadada, S. K. COVID-19 and diabetes mellitus: An unholy interaction of two pandemics. Diabetes Metab. Syndr. 14, 513–517. https://doi.org/10.1016/j.dsx.2020.04.049 (2020).
Rehman, K. et al. Role of interleukin-6 in development of insulin resistance and type 2 diabetes mellitus. Crit. Rev. Eukaryot. Gene Expr. 27, 229–236. https://doi.org/10.1615/CritRevEukaryotGeneExpr.2017019712 (2017).
Costela-Ruiz, V. J., Illescas-Montes, R., Puerta-Puerta, J. M., Ruiz, C. & Melguizo-Rodríguez, L. SARS-CoV-2 infection: The role of cytokines in COVID-19 disease. Cytokine Growth Factor Rev. 54, 62–75. https://doi.org/10.1016/j.cytogfr.2020.06.001 (2020).
Ibrahim, A. S., Spellberg, B. & Edwards, J. Jr. Iron acquisition: A novel perspective on mucormycosis pathogenesis and treatment. Curr. Opin. Infect. Dis. 21, 620–625. https://doi.org/10.1097/QCO.0b013e3283165fd1 (2008).
Perricone, C. et al. COVID-19 as part of the hyperferritinemic syndromes: The role of iron depletion therapy. Immunol. Res. 68, 213–224. https://doi.org/10.1007/s12026-020-09145-5 (2020).
Habib, H. M., Ibrahim, S., Zaim, A. & Ibrahim, W. H. The role of iron in the pathogenesis of COVID-19 and possible treatment with lactoferrin and other iron chelators. Biomed. Pharmacother. 136, 111228. https://doi.org/10.1016/j.biopha.2021.111228 (2021).
Li, J. et al. COVID-19 infection may cause ketosis and ketoacidosis. Diabetes Obes. Metab. 22, 1935–1941. https://doi.org/10.1111/dom.14057 (2020).
Garg, D. et al. Coronavirus disease (Covid-19) associated mucormycosis (CAM): Case report and systematic review of literature. Mycopathologia 186, 289–298. https://doi.org/10.1007/s11046-021-00528-2 (2021).
Moorthy, A. et al. SARS-CoV-2, uncontrolled diabetes and corticosteroids—an unholy trinity in invasive fungal infections of the maxillofacial region? A retrospective, multi-centric analysis. J. Maxillofac. Oral Surg. 20, 1–8. https://doi.org/10.1007/s12663-021-01532-1 (2021).
John, T. M., Jacob, C. N. & Kontoyiannis, D. P. When uncontrolled diabetes mellitus and severe COVID-19 converge: The perfect storm for mucormycosis. J. Fungi 7, 298. https://doi.org/10.3390/jof7040298 (2021).
Riad, A. et al. COVID-19-associated mucormycosis (CAM): Case-series and global analysis of mortality risk factors. J. Fungi 7, 837. https://doi.org/10.3390/jof7100837 (2021).
Rammaert, B. et al. Healthcare-associated mucormycosis. Clin. Infect. Dis. 54(Suppl 1), S44-54. https://doi.org/10.1093/cid/cir867 (2012).
Horby, P. et al. Dexamethasone in hospitalized patients with covid-19. N. Engl. J. Med. 384, 693–704. https://doi.org/10.1056/NEJMoa2021436 (2021).
Skiada, A. et al. Challenges in the diagnosis and treatment of mucormycosis. Med. Mycol. 56, 93–101. https://doi.org/10.1093/mmy/myx101 (2018).
Roden, M. M. et al. Epidemiology and outcome of zygomycosis: A review of 929 reported cases. Clin. Infect. Dis. 41, 634–653. https://doi.org/10.1086/432579 (2005).
Fouad, Y. A. et al. Spike in rhino-orbital-cerebral mucormycosis cases presenting to a tertiary care center during the COVID-19 pandemic. Front. Med. 8, 716 (2021).
Burggraf, O. R. Analytical and numerical studies of the structure of steady separated flows. J. Fluid Mech. 24, 113–151 (1966).
Sarin, S. et al. Asian-Pacific clinical practice guidelines on the management of hepatitis B: A 2015 update. Hepatol. Int. 10, 1–98 (2016).
Song, G., Liang, G. & Liu, W. Fungal co-infections associated with global COVID-19 pandemic: A clinical and diagnostic perspective from China. Mycopathologia 185, 599–606. https://doi.org/10.1007/s11046-020-00462-9 (2020).
Rodriguez-Morales, A. J. et al. Vol. 8, 1–5 (SAGE Publications, 2021).
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization S.F.Y., M.M.A., A.A.T., M.M.A., M.O.A.G., A.A., G.M.S., I.G., S.M.K..; methodology, S.F.Y., M.M.A., A.A.T., M.M.A., M.O.A.G., A.M. A., G.M.S., I. g., S.M.K., H.F.H. and A.M.A., N.M.A. software, S.F.Y.; validation, S.F.Y., M.M.A., A.A.T., M.M.A., M.O.A.G., A.A., G.M.S., I.G., S.M. K.; formal analysis, S.F.Y., M.M.A., A.A.T., M.M. A., M.O.A.G., A.A., G.M.S., I.G., S.M.K..; investigation, F.Y., M.M.A., A.A.T., M.M.A., M.O.A.G., A. A., G.M.S., I.G., S.M.K.; resources, S.F.Y.; data curation, A.M.A.; writing—original draft preparation, S.F.Y., M.M.A., A.A.T., M.M. A., M.O.A.G., A.A., G.M.S., I.G., S.M.K., H.F.H. and A.M.A.; writing—review and editing, S.F.Y., M.M.A., A.A.T., M.M.A., M.O.A.G., A.M.A., G.M.S., I.G., S.M.K..; G.E.B., N.M.A. visualization, S.F.Y.; supervision, S.M.K..; project administration, S.F.Y.; funding acquisition, S.F.Y. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Farghly Youssif, S., Abdelrady, M.M., Thabet, A.A. et al. COVID-19 associated mucormycosis in Assiut University Hospitals: a multidisciplinary dilemma. Sci Rep 12, 10494 (2022). https://doi.org/10.1038/s41598-022-13443-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-13443-3
This article is cited by
-
COVID-19 associated Mucormycosis among ICU patients: risk factors, control, and challenges
AMB Express (2023)
-
Fungal infection profile in critically ill COVID-19 patients: a prospective study at a large teaching hospital in a middle-income country
BMC Infectious Diseases (2023)
-
Mucormycosis and Its Upsurge During COVID-19 Epidemic: An Updated Review
Current Microbiology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.