Written by: Ben Kiesel, MD (NUEM PGY-1) Edited by: David Kaltman, MD (NUEM PGY-4) Expert Commentary by: Kirsten Loftus, MD, MEd
Expert Commentary
Thank you for providing this succinct review of HSP. This is not a diagnosis you will encounter frequently, but it’s an important one not to miss because, as you point out, there are several key implications for outpatient monitoring and follow-up. Here are a few additional tips when it comes to the diagnosis and initial management of HSP:
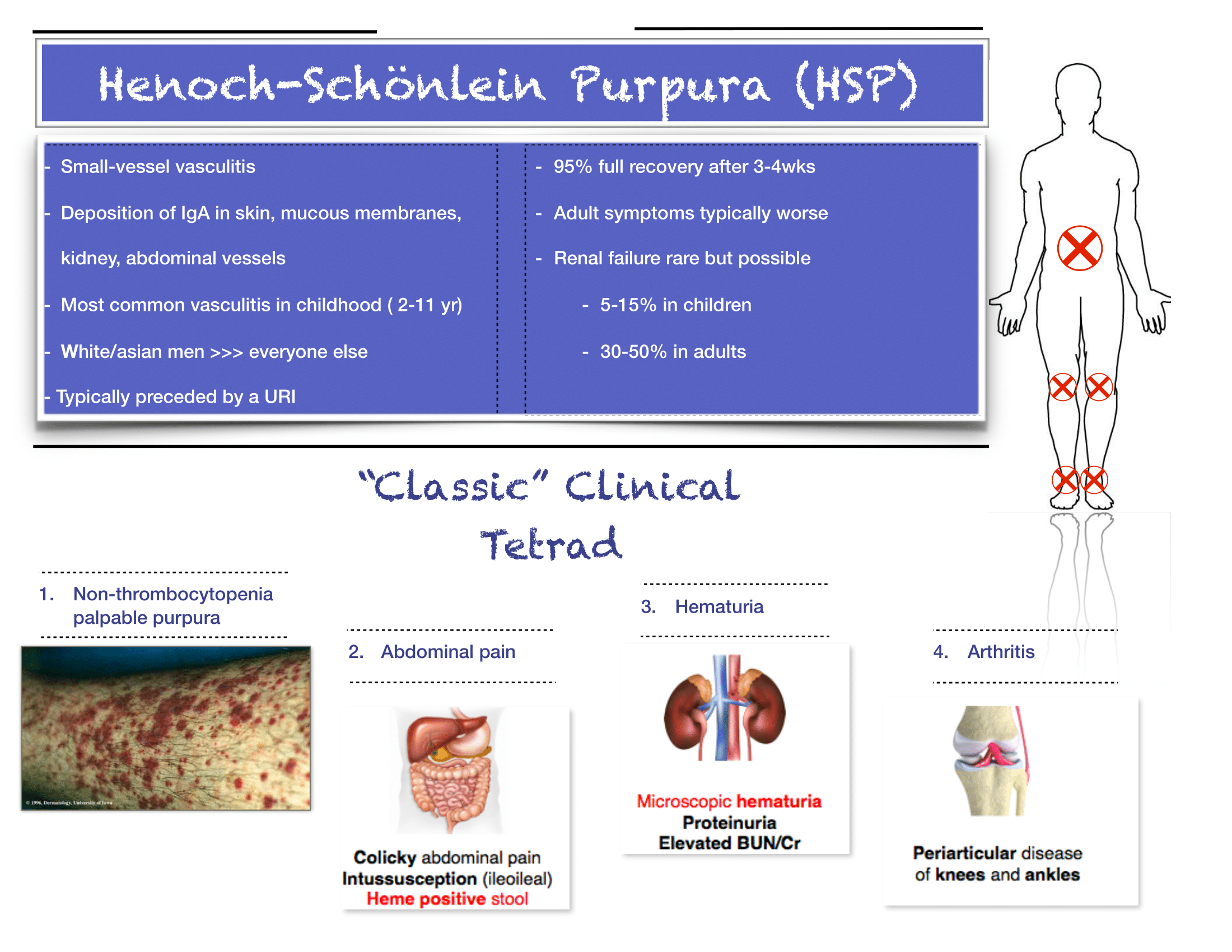
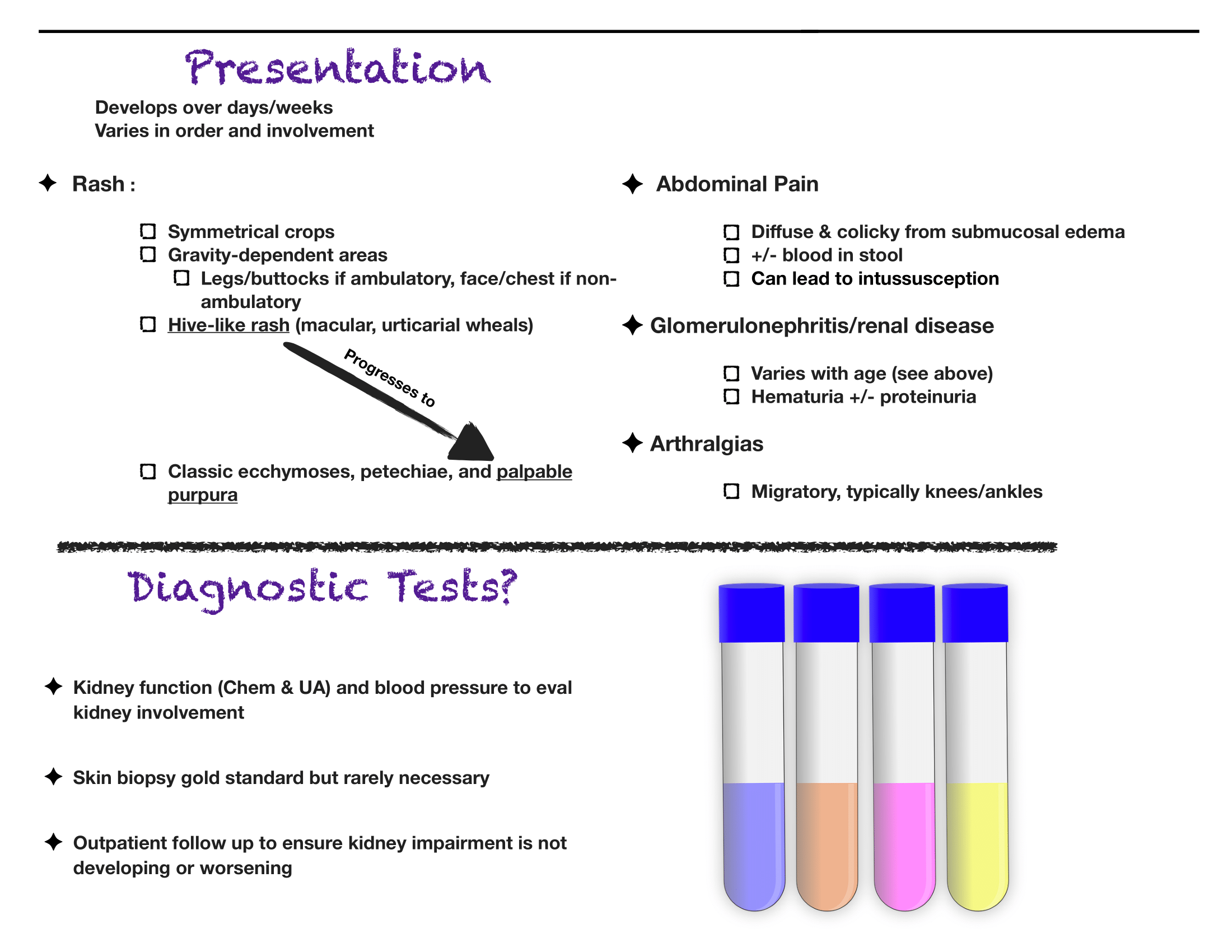
The diagnosis is truly a clinical one. If you have bilateral lower extremity petechiae/purpura plus belly pain, arthritis/arthralgia, or renal involvement, then you’ve made your diagnosis. Outside a urinalysis to evaluate for hematuria/proteinuria and checking a blood pressure to look for hypertension, there is limited utility for other diagnostic tests. Don’t forget to consult your favorite reference for normal pediatric blood pressure values to ensure you aren’t missing hypertension.
Renal disease is less common in kids compared to adults with HSP, but does happen. If you have hematuria/proteinuria or hypertension, go ahead and at least check a chemistry to look at BUN/Cr. Then talk with your favorite local pediatric nephrologist (if available) or PEM doc at your pediatric referral center to determine need for transfer versus close outpatient follow-up.
You appropriately point out that steroids are rarely indicated, and that hydration and NSAIDs will be your primary management. If you feel compelled to start steroids for severe abdominal pain (once you are sure it is not due to intussusception), you may need a longer (e.g. 4-8 week) taper, given the risk of rebound pain if tapered too quickly.
As always, set clear expectations with families and make sure they have good follow-up. I find that this can be a tough diagnosis to explain to parents, who are often quite scared about the rash. Spending some extra time talking with families once you’ve made the diagnosis can really go a long way. Warn parents that the rash is likely to persist for weeks and that the development of some additional petechiae/purpura is okay- you will prevent some unnecessary ED return visits this way. Strict return precautions for severe belly pain are key as HSP-associated intussuception is a very real complication. Every discharged patient should be seen by their PCP within about 1 week for a repeat UA and BP check- even if patients do not have evidence of renal disease at the time of diagnosis, it may develop later on, and close outpatient monitoring is critical.
Kirsten V. Loftus, MD, MEd
Attending Physician Emergency Medicine
Ann & Robert H. Lurie Children’s Hospital of Chicago
Instructor of Pediatrics (Emergency Medicine)
Northwestern University Feinberg School of Medicine
How to Cite This Post
[Peer-Reviewed, Web Publication] Kiesel, B, Kaltman, D. (2020, May 18). Henoch-Schonlein Purpura. [NUEM Blog. Expert Commentary by Loftus, K]. Retrieved from https://www.nuemblog.com/blog/hsp