Eyelid Terminology and Measurements
Palpebral Fissure
The palpebral fissure refers to the normal exposed area between upper and lower eyelids.
The palpebral fissure vertical height (PFH) is measured between the margin of the lower eyelid to the margin of the upper eyelid.
The normal palpebral fissure height is 8-11 mm. This is a key measurement that you need when assessing for ptosis.
Margin-To-Reflex Distance
As you might expect, it is the distance from the eyelid margin to the corneal light reflex.
It is measured by having the patient fixate on a light, and measuring the distance from the margin of the eyelid to the corneal light reflex. There are two margin-to-reflex distances (MRD), corresponding to the measurement from the upper and lower eyelids:
MRD1: upper eyelid margin-to-light reflex; this is probably the single most important measurement when evaluating ptosis.
MRD2: lower eyelid margin-to-light reflex
MRD1 + MRD2 should equal the palpebral fissure height.
Levator Palpebrae Superioris Function (Excursion)
Levator. function test. The position of the upper eyelid margin is noted in downgaze by the 1 cm hash (A), and then in upgaze without activation of the frontalis muscle (B). In this patient with ptosis, the levator excursion is approximately 5 mm. Normal levator function is approximately 15 mm.
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.
The levator palpebrae superioris muscle is innervated by the superior division of CN III.
It is the greatest contributor to upper eyelid movement.
It provides 15 mm of eyelid elevation; this can typically be measured by having the patient look down, then as high as possible while holding the frontalis muscle down. Frontalis muscle contracture can open the eyelids an additional 2 mm.
The eyelid margin.
This diagram demonstrates the conceptual split between the anterior lamella (skin and orbicularis, right side) and posterior lamella (tarsus and conjunctiva, left side) of the eyelid. The gray line, which is the muscle of Riolan (the most superficial aspect of the orbicularis muscle), is also shown. Note that this is just anterior to the meibomian gland orifces, which come from the tarsus.
Image credit: plasticsurgerykey.com (available online), used for educational purposes.
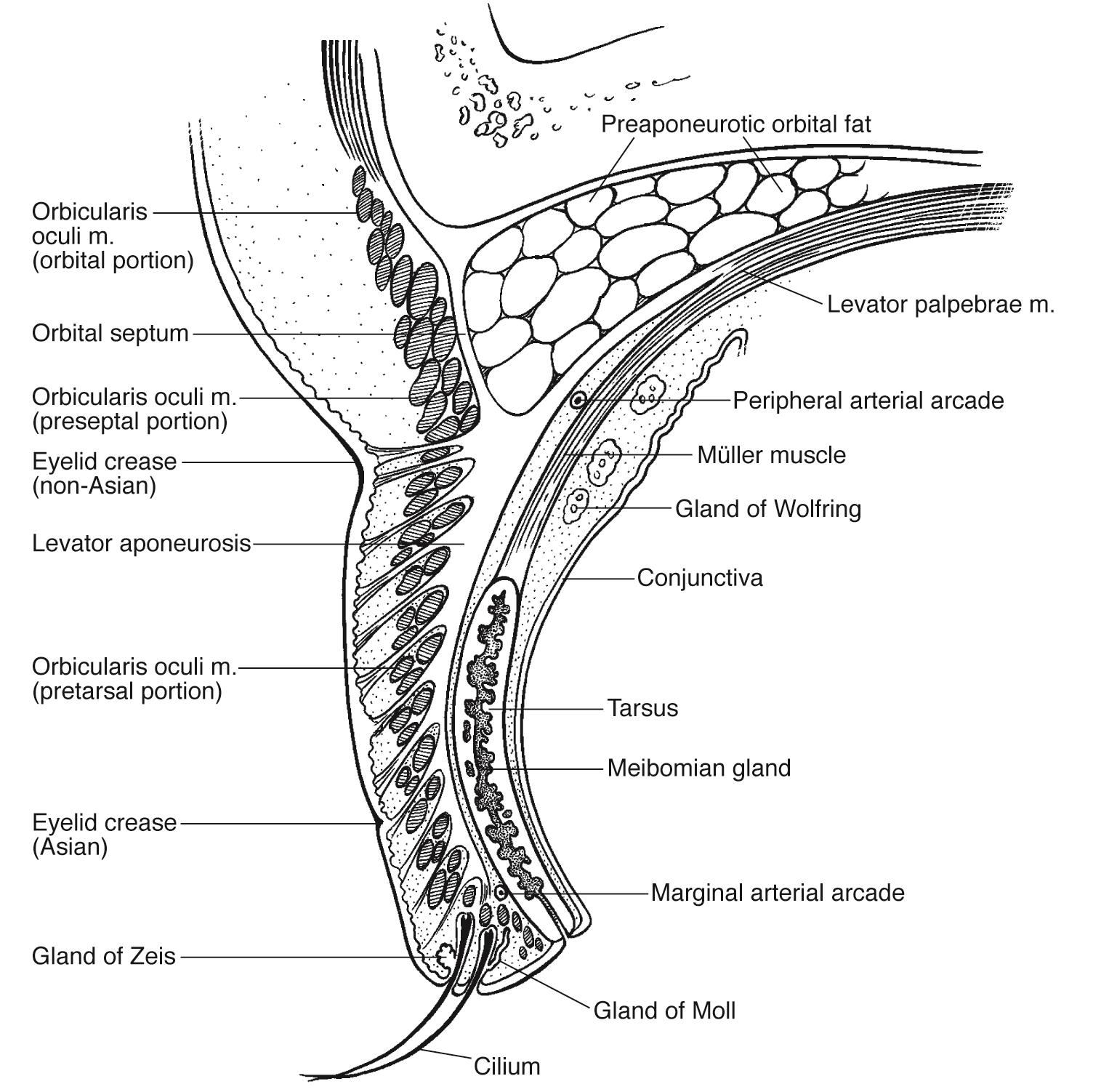
Organization of the Upper Eyelid
There are several ways to mentally organize the multiple layers of the upper eyelid. The Fundamentals BCSC book lists 9 structures, while the Oculoplastics BCSC book lists 7 structures; they are essentially the same lists so there’s no need to fret over which list to memorize.
I personally have found that thinking through the layers of the eyelid from anterior (external) to posterior (internal) makes the most sense to me. After all, if you are doing eyelid surgery, you are going to make an incision through various layers of the eyelid and it’s helpful to know what tissues you’re cutting through and in what order. The layers are:
Skin
Subcutaneous connective tissue (the Oculoplastics BCSC book lumps the skin and subcutaneous tissue into one layer, as clinically they are fairly indistinct)
Orbicularis oculi muscle
Orbital septum
Levator palpebrae superioris muscle (not present in the lower eyelid)
Müller muscle (inferior tarsal muscle in the lower eyelid)
Tarsus
Conjunctiva
The eyelid margin is another unique aspect of the eyelids, which is important to understand for surgical landmarks and various pathologies. This will be discussed in a separate section.
Anterior and Posterior Lamellae
Another method of thinking about eyelids (especially in surgery) is dividing the eyelid into anterior and posterior lamellae. In this framework, the orbital septum separates the anterior tissues from the posterior tissues. When considering certain treatments for conditions such as ectropion or entropion, this may potentially help understand why and how to repair the eyelid tissues.
Anterior Lamellae
Skin and connective tissues
Orbicularis oculi muscle
Posterior Lamellae
Tarsus
Conjunctiva
Cross-section of the upper eyelid.
Image credit: Illustration by Christine Gralapp. American Academy of Ophthalmology. Used with permission for educational purposes.
Eyelid Structures
Skin
The eyelid skin is the thinnest in the body.
The skin contains fine hairs, sebaceous glands, and sweat glands.
Eyelid Folds
In non-Asians, the levator palpebrae superioris muscle has some attachments to the upper border of the tarsus, which forms a superior eyelid fold.
In Asians, the levator palpebrae superioris muscle does not have these attachments, so the superior eyelid fold is minimal or absent.
Subcutaneous Connective Tissue
The significant eyelid swelling seen in conditions such as preseptal cellulitis (shown above) is caused by the accumulation of fluid in the loose connective tissue.
Eyelid creases (folds).
The levator palpebrae superioris (red) has firm attachments to anterior aspect of the tarsus, approximately 3 mm superior to the eyelid margin. At Whitnall ligament it splits into the levator aponeurosis (blue) and the superior tarsal (Müller) muscle (green), which inserts at the superior border of the tarsus.
In non-Asians, there are some attachments to the superior aspect of the tarsus, which forms a superior eyelid crease. In Asians, these attachments are not present, and so the superior eyelid crease is not present and the crease associated with the firm attachments 3 mm superior to the eyelid margin is more prominent.
Image credit: Modified from illustration by Christine Gralapp. American Academy of Ophthalmology. Used with permission for educational purposes.
Preseptal cellulitis.
The significant eyelid swelling is caused by accumulation of fluid in the subcutaneous connective tissue.
Image credit: Courtesy of Dr. Richard C. Allen, M.D., Ph.D., FACS. American Academy of Ophthalmology. Used with permission for educational purposes.
Orbicularis Oculi Muscle
The orbicularis muscle consists of the concentric bands of muscle surrounding the eyelid. It is innervated by the facial nerve (CN VII). It has multiple functions, including involuntary blinking, voluntarily and forcibly closing the eyelids, and tear drainage.
Orbicularis oculi muscle.
There are two main segments of the orbicularis oculi - orbital and palpebral. The medial palpebral (canthal) tendon and lateral palpebral (canthal) tendon are strongly attached to the orbicularis muscle.
Image credit: healthfixit.com (available online). Used for educational purposes.
Orbicularis oculi muscle.
The palpebral segment of the orbicularis oculi muscle can be further subdivided into the preseptal and pretarsal segments.
Image credit: Modified from Codner MA, Burke RM. Chapter 46: Blepharoplasty. In: Plastic Surgery. doctorlib.info. Available online. Used for educational purposes.
Organization
There are 2 sections of the orbicularis oculi muscle:
Orbital segment
Palpebral segment: further subdivided into the pretarsal and preseptal segments
Pretarsal segment
Preseptal segment
Orbital Segment of the Orbicularis Oculi Muscle
The orbital segment provides voluntary forced closure of the eyelids.
Pretarsal segment of the Orbicularis Oculi Muscle
The pretarsal segment is involved in tear drainage (“preTarsal helps with Tearing”)
The portion that attaches to the anterior and posterior lacrimal crest is called the Horner muscle.
The upper and lower eyelid segments fuse laterally to form the lateral canthal tendon.
Preseptal segment of the Orbicularis Oculi Muscle
The preseptal muscles form the lateral palpebral ligament (raphe), which inserts into Whitnall’s tubercle.
Riolan Muscle
The muscle of Riolan represents the most superficial portion of the orbicularis muscle.
It corresponds to the gray line of the eyelid margin, and may contribute to meibomian gland secretion, eyelash position, and blinking.
It arises from the palpebral segment of the orbicularis muscle.
Orbital Septum
The orbital septum is an extension of periosteum from the orbital roof (upper eyelid) and orbital floor (lower eyelid).
It serves as a barrier for preventing infections/blood/inflammation from spilling over between the anterior eyelid and the orbit.
Preseptal cellulitis refers to inflammation and infections that are anterior (superficial) to the orbital septum. These may be treated with oral or IV antibiotics first, and may not require additional hospital treatment or surgery.
Orbital celluiltis affects the tissues posterior to the orbital septum and may result in subperiosteal abscesses, cavernous sinus thrombosis, or systemic infection.
It separates the anterior lamellae of the eyelid from the posterior lamellae.
Levator Palpebrae Superioris Muscle
Levator palpebrae superioris and Whitnall ligament.
A) Diagram showing surrounding structures (right eye).
B) During ptosis surgery, the Whitnall ligament is seen as a horizontal white line in the fascia (black arrow). The preaponeurotic fat is superior to the ligament (blue arrow). Whitnall ligament divides the levator palpebrae superioris muscle into the levator aponeurosis anteriorly (white arrow), and Müller muscle posteriorly (not seen).
C) Eyelid structures and their position within the orbit (right eye).
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.
The levator palpebrae superioris muscle travels from the posterior orbit (arising from the lesser wing of the sphenoid).
It is innervated by the superior division of CN III. There one common central subnuclei for the eyelids present in the CN III nucleus.
Lesions in the midbrain affecting the CN III nucleus on one side may result in an ipsilateral CN III palsy with bilateral ptosis.
In accordance with Hering’s law of equal innervation, unilateral ptosis may create the false impression of contralateral eyelid retraction; likewise, unilateral eyelid retraction may result in contralateral pseudoptosis.
The Whitnall ligament (a condensation of the superior rectus and levator palpebrae superioris muscles) affects the levator palpebrae superioris muscle in several ways:
At the Whitnall ligament, the levator palpebrae superioris muscle changes direction from horizontal to vertical.
At the Whitnall ligament, the levator palpebrae superioris muscle divides into the levator aponeurosis and the superior tarsal (Müller) muscle.
Superior Tarsal (Müller) Muscle
The superior tarsal muscle, also termed the Müller muscle, is a smooth muscle (nonstriated, as opposed to the striated/skeletal muscles of the orbicularis oculi, levator palpebrae superioris, and other extraocular muscles). It is innervated by the sympathetic nerves with cell bodies in the superior cervical ganglion. It provides a small amount of additional eyelid retraction.
Müller muscle originates from the posterior surface of the levator palpebrae superioris muscle at the level of the Whitnall ligament and inserts on the upper border of the tarsus. There are also attachments to the conjunctiva at the upper fornix.
There is a sympathetically-innervated muscle in the lower eyelid that functions as the analogue of the Müller muscle, the capsulopalpebral (inferior tarsal) muscle, which inserts on the lower border of the lower eyelid tarsus.
In Horner syndrome, loss of sympathetic tone results in ~2 mm of upper eyelid ptosis and also lower lid ptosis.
Horner syndrome.
Note that there is both upper eyelid ptosis (green arrow) and lower eyelid ptosis (red arrow). The right pupil is smaller than the left pupil (miosis), as a result of loss of the sympathetic tone to the right pupil.
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.
Tarsus
The tarsal plates of the eyelids are comprised of dense connective tissue.
They are attached to the periosteum horizontally via the medial and lateral canthal tendons.
The meibomian glands of the eyelid are holocrine sebaceous glands that lie within the tarsus. They produce oil which forms the oily layer of the tear film.
There are more meibomian orifices in the upper eyelid compared to the lower eyelid (30-40 vs. 20-30).
The upper tarsus is wider than the lower tarsus.
With age the medial and lateral canthal tendons stretch and become more lax, resulting in horizontal displacement of the tarsal plate. A lateral tarsal strip procedure sutures the lateral tarsus to the periosteum, restoring the horizontal tension on the tarsus.
Lateral tarsal strip procedure.
A. Lateral stretching of the eyelid demonstrates the potential of lower eyelid tightening.
B. Lateral tarsal strip procedure: anchoring of tarsal strip to periosteum inside the lateral orbital rim.
Image credit: Images in A courtesy of Bobby S. Korn, M.D., Ph.D. Illustration (B) by Christine Gralapp. American Academy of Ophthalmology. Used with permission for educational purposes.
Conjunctiva
The conjunctiva is a transparent vascularized membrane that covers the eyelids (palpebral conjunctiva) and globe (bulbar conjunctiva).
It is composed of nonkeratinizing squamous epithelium.
It contains goblet cells, which secrete mucin (forming the mucin layer of the tear film).
It contains accessory lacrimal glands of Wolfring and Krause, which secrete the basal aqueous layer of the tear film.
The glands of Wolfring are located along the upper border of the tarsus in the upper lid and the lower border of the tarsus in the lower lid (“nonmarginal tarsal borders”).
The glands of Krause are located in the fornices (“Krause in the crack”).
Eyelid Margin
The eyelid margin contain many important structures and are ordered in specific way, as are all the layers of the eyelid. Knowing the orientation and position of the margin structures is especially important with trauma, where restoration of the anatomy as best as possible is critical.
From anterior to posterior, the structures seen are:
Skin
Eyelashes (cilia)
Gray line
Meibomian gland orifices
Mucocutaneous junction
Palpebral conjunctiva
Eyelid margin anatomy.
Image credit: Illustration by Christine Gralapp. American Academy of Ophthalmology. Used with permission for educational purposes.
Special Structures Of the Eyelid Margin
Puncta
The puncta of the canaliculus is present at the medial aspect of each eyelid margin.
The upper (superior) punctum is more medially located than the lower (inferior) punctum.
Gray Line (Intermarginal sulcus)
The gray line of the eyelid margin represents the most superficial portion of the palpebral (pretarsal) orbicularis oculi muscle, the muscle of Riolan.
Eyelashes (Cilia)
Eyelashes arise from the anterior eyelid margin just anterior to the tarsal plate.
Glands of Zeis are modified sebaceous glands associated with the cilia (“Zei-baceous” glands)
Glands of Moll are apocrine sweat glands in the skin.
Vascular Supply of the Eyelids
Arterial Supply
The eyelids are supplied by both the external carotid artery and internal carotid artery systems.
Eyelid vascular anatomy, left eye.
The eyelids are supplied by a robust and complex system of vessels that arise from both the external and internal carotid artery systems.
Image credit: plasticsurgerykey.com (available online).
External Carotid Artery System
The facial artery from the ECA (facial system) becomes the angular artery lateral to the nose and supplies the medial eyelid.
The angular artery is an important surgical landmark in dacryocystorhinostomy (DCR).
The temporal artery from the ECA supplies the lateral eyelid.
Internal Carotid Artery System
The circulation from the internal carotid artery (orbital system) arises from branches of the ophthalmic artery, namely the supraorbital and lacrimal arteries.
Arterial Arcades
Marginal arterial arcade: located 2-3 mm from the eyelid margin, it lies just above the ciliary follicles, either within the tarsus or between the tarsal plate and orbicularis oculi muscle.
Peripheral arterial arcade: located within the Müller/inferior tarsal muscles, at the border of the tarsus and those muscles.
Venous Drainage
Superficial (Pretarsal) System
These veins drain from preseptal tissues into the internal and external jugular veins.
The angular vein supplies the medial eyelid.
The superficial temporal vein supplies the lateral eyelid.
Deep (Posttarsal) System
These veins drain into the cavernous sinus.
Some notable veins include the orbital veins and deep branches of the anterior facial vein and pterygoid plexus.
Lymphatic Drainage of the Eyelids
Medial Drainage
The lymphatic vessels that serve the medial eyelids drain into the submandibular lymph nodes (Medial eyelids = subMandibular nodes).
Lateral Drainage
The lymphatic vessels that serve the lateral eyelids drain into the preauricular lymph nodes (lateral eyelids go to the ear).
Accessory Eyelid Structures
Accessory eyelid structures. The caruncle is the small fleshy, ovoid structure medial to the plica semilunaris. The plica semilunaris is a crescent-shaped fold of conjunctiva rich in goblet cells and is analogous to the nictitating membrane of other animals.
Image credit: Carter HV, Gray H (1918). Anatomy of the Human Body. Bartleby.com: Gray’s Anatomy, Plate 1205.
Caruncle
The caruncle is modified skin.
Histologically it is covered by nonkeratinized, stratified squamous epithelium and contains sebaceous glands and hair.
Plica Semilunaris
The plica semilunaris is a fold of the conjunctiva on the medial aspect of the globe.
Histologically, it resembles bulbar conjunctiva but the stroma contains fat and some nonstriated muscle. The epithelium is rich with goblet cells.
Of note (but probably not of testing consequence), it is a vestigial structure analogous to the nictitating membrane (third eyelid) of other animals.
References
Basic and Clinical Science Course, Section 2. Fundamentals and Principles of Ophthalmology. San Francisco: American Academy of Ophthalmology, 2018-2019:18-27.
Basic and Clinical Science Course, Section 7. Orbit, Eyelids, and Lacrimal System. San Francisco: American Academy of Ophthalmology, 2018-2019:145-154.
Tong J, Patel BC. Anatomy, Head and Neck, Eye Orbicularis Oculi Muscle. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available online from the National Library of Medicine.