Barrett's esophagus – Symptoms, Causes, Types and Complications
barrett's esophagus definition
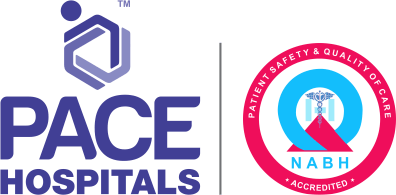
Barrett's oesophagus is a condition in which the normal stratified squamous epithelium (pink lining or mucosal lining) of the oesophagus (food/swallowing pipe that connects mouth and stomach) is damaged by acid reflux and thickens and reddens, as detected on endoscopic examination and pathologically confirmed by the presence of intestinal metaplasia columnar epithelium (the presence of thick cells similar to those present in intestine).
It is also considered a pre-malignant condition, where its prevalence was estimated to be 1.5% in the general population and as high as 15% in those with gastroesophageal reflux disease (GERD). It is an asymptomatic condition where the patient might feel the signs related to GERD, such as heartburn and acid regurgitation. It is diagnosed by
upper endoscopy; however, regular check-ups with thorough imaging and extensive biopsies of the oesophagus to screen for precancerous cells (dysplasia) are crucial as Barrett's oesophagus raises the chance of developing oesophageal cancer.
Barrett’s esophagus symptoms
Barrett's oesophagus is asymptomatic, but it can manifest symptoms of long-term GERD, such as heartburn and acid regurgitation. Along with this, the symptoms might also include:
- Difficulty in swallowing food
- Difficult to sleep due to heartburn
- Chest pain
- Constant sore throat
- Unintentional weight loss
- Blood in stool
- Vomiting
Barrett’s esophagus causes
The cause of Barrett's oesophagus is unknown. Most cases of Barrett's oesophagus are due to long-term gastroesophageal reflux. In some cases, patients might not have any reflux symptoms at all; hence, it is termed “silent reflux”.
Complications of barrett's esophagus
Barrett's oesophagus complication includes oesophageal cancer (rare). However, the probability of having oesophageal cancer is statistically minimal (one in every 860 Barrett’s esophagus patients). In some patients, Barrett's oesophagus might be associated with complications such as stricture, ulcer, and dysplasia.
Barrett's esophagus pathology
GERD is a condition, where the acid and bile from the stomach come back up through the lower oesophageal sphincter (LES), a critically important valve, present between the oesophagus and the stomach that prevents the reflux of gastric contents back into the oesophagus. The lining of the stomach is made of mucinous columnar epithelium, which can handle the acidic environment needed for digestion, whereas the lining of the oesophagus, on the other hand, is made of squamous epithelium.
The LES may eventually fail, allowing stomach acids to reach the lower part of the oesophagus. The acidic irritant causes the squamous epithelium (oesophageal lining) to become red and swollen. When oesophageal lining exposed to gastric acids for a long time, there is persistent inflammation (due to release of inflammatory cytokines such as interleukin-8, interleukin-6) and a columnar metaplasia reaction occurs, commonly known as Barrett’s oesophageal metaplasia. Eventually, goblet cells develop, which is a sign of an intestinal-type phenotype.
Barrett's esophagus screening
Barrett's oesophagus screening indicated when a patient has two or more risk factors for Barrett's oesophagus, including being
male, and over the age of 50, and having frequent (happening weekly or more) GERD symptoms such as chest pain, nausea, bloating, gas and belching, food intolerance, difficulty swallowing, regurgitation of food or sour liquid, sensation of a lump in your throat; the
gastroenterologist
may recommend screening for Barrett's oesophagus.
Barrett's esophagus risk factors
Barrett's oesophagus risk factors are complicated and need to be considered by gastroenterology professionals especially in identifying GERD patients who could obtain maximum benefit from an early investigation of Barrett's oesophagus. The following risk factors increase the likelihood of Barrett's oesophagus:
- Older age: Although the elderly is at risk for developing Barrett's oesophagus, it most commonly affects those over 50.
- Male sex: Males have a significantly higher prevalence of Barrett's oesophagus than females.
- Smoking: Cigarette smoking makes reflux disease worse. This is probably because, smoking causes acid reflux and may also lower the pressure of the lower oesophageal sphincter for a long time.
- Obesity: Body fat around the abdomen further increases the risk. According to the findings, while obesity may not have a direct effect on Barrett’s oesophagus, it is likely to be due to its association with GERD.
- White race or Caucasian: Evidenced by the studies conducted. Barrett's oesophagus was shown to be more common in white people than in any other racial or ethnic group.
- Family history of Barrett’s oesophagus or oesophageal cancer: Evidence from studies suggests that a risk of developing Barrett's oesophagus is inherited.
- Prolong heartburn symptoms: Long-term heartburn (more than 10 years) can cause severe damage to the oesophageal lining, resulting in Barrett's oesophagus.
- Presence of GERD: More than any other known cause, Barrett's oesophagus has been linked to gastroesophageal reflux disease (GERD).
Barrett's esophagus prevention
Barrett's oesophagus can be prevented by addressing the underlying cause; heartburn or GERD symptoms. In addition to this:
- Avoid smoking and chewing tobacco
- Avoid drinking alcohol
- Maintain a healthy body weight
- Avoid food that trigger GERD symptoms
- Sleeping with your head slightly elevated
- Diet with fruits and vegetables rich in vitamins
Barrett’s esophagus diagnosis
Barrett’s oesophagus diagnosis includes a biopsy and upper gastrointestinal (UGI) endoscopy. While investigating the root of a patient's GERD symptoms, gastroenterologist may make the diagnosis of Barrett's oesophagus.
Barrett’s esophagus treatment
Depending on the patient's health status and severity of dysplasia, the gastroenterologist will discuss the best course of treatment, which includes:
- Endoscopic ablative therapies
- Photodynamic therapy
- Radiofrequency ablation therapy
- Cryotherapy
- Endoscopic mucosal resection
- Surgery
- Esophagectomy
- Fundoplication (prophylactic)
- GERD medications
Frequently asked questions:
What are the types of Barrett's esophagus?
Barrett's oesophagus is classified into three types based on the presence of dysplasia
- No dysplasia: The absence of precancerous changes in the cell, despite the presence of Barrett's oesophagus.
- Low-grade dysplasia: Presence of precancerous cells exhibiting precancerous changes along with Barrett's oesophagus.
- High-grade dysplasia: This is the final stage before cells transform into oesophageal cancer, and it is characterised by several cellular alterations.
Can Barrett’s esophagus heal itself?
No, Barrett’s oesophagus is incurable. However, the disease, is treatable with acid-reducing medication and a surgical procedure. Acid -reducing medications such as proton pump inhibitors, antacids, histamine blockers, and prokinetic agents.
Surgical procedures such as esophagectomy and fundoplication (as a prophylactic measure).
- An esophagectomy is a technique in which the oesophagus (the tube connecting the mouth and stomach) is surgically removed and reconstructed using stomach tissue.
- Fundoplication is a surgical procedure that involves folding and sewing the fundus (upper part of the stomach) over the lower oesophageal sphincter (muscular valve at the bottom of the oesophagus). Due to the reoccurrence nature of Barrett's oesophagus, continuous monitoring is required.
What is the best treatment for Barrett’s esophagus?
The choice of treatment is purely based on the patient’s condition. However, cryoablation can be considered the best one, where the gastroenterologist uses extremely low temperatures to intentionally damage the Barrett's oesophagus cells in order to promote their regeneration into healthy tissue.
Does barium swallow show Barrett’s esophagus?
No, a barium swallow cannot be used to reliably diagnose Barrett's oesophagus. In this procedure, barium (a chalky white material) combined with water, coats the lining of the upper gastrointestinal tract (UGT) when swallowed by a patient. When a physician uses an X-ray machine, the film will show up white because barium lined in UGT absorbs the X-rays. In order to diagnose Barrett's oesophagus, specialised intestinal metaplasia (SIM) must be present in the oesophageal tissue, which can only be determined with a biopsy and not by a barium swallow procedure.
How often should you be checked if you have Barrett's esophagus?
The severity of the dysplasia will determine how often the patient needs to get checked.
- It is acceptable to re-evaluate patients with Barrett's once every two years if they do not have dysplasia.
- Low-grade dysplasia patients may benefit from having endoscopies performed every three to six months, with additional follow-up at intervals ranging from six months to one year.
- Due to the higher risk of malignancy, patients with high-grade dysplasia may need to have their oesophagus surgically removed (esophagectomy).
Can omeprazole (PPI) cure Barrett's esophagus?
Drug therapy for Bartlett's oesophagus often consists of proton pump inhibitors (PPIs). These medications are used to treat gastroesophageal reflux disease, where it reduces acid production in the stomach. Therefore, less damage to the oesophagus caused, as stomach acid is reduced.
What age does Barrett's esophagus develop?
Barrett's oesophagus can also develop in youngsters; however, it is extremely rare in individuals who are younger than five years old. Barrett's oesophagus is diagnosed at an average age of 55 years. People in their middle years and those in their older age are most likely to be affected by the condition.
What is alcian blue stain Barrett’s esophagus?
The presence of metaplastic columnar epithelium, as observed on endoscopy and confirmed histologically, is required for a diagnosis of Barrett's oesophagus. The epithelium of the patient's oesophagus must be columnar endoscopically and metaplastic histologically, as evidenced by the presence of goblet cells. The acidic mucin in goblet cells is stained by alcian blue at a pH of 2.5.
What is treatment for Barrett’s esophagus with dysplasia?
The treatment for Barrett’s oesophagus depends on the severity of the dysplasia.
- For low-grade dysplasia, the gastroenterologist might suggest for endoscopic ablative therapies such as photodynamic therapy, radiofrequency ablation and cryotherapy and endoscopic mucosal resection.
- For patients with high-grade dysplasia, the gastroenterologist might suggest for Esophagectomy surgery.
Can Barrett's esophagus reverse naturally?
No, Barrett's oesophagus cannot be cured naturally, as it is a precancerous condition. Although a few natural remedies, might subside the symptoms, they cannot reverse the condition.
What is Barrett’s esophagus misdiagnosis?
The presence of columnar epithelium in the distal part of the oesophagus is generally related to Barrett's oesophagus. In rare cases of gastric heterotopia, where columnar epithelium can be seen in the distal part of the oesophagus, this leads to a misdiagnosis of Barrett’s oesophagus.
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.

Our Locations
Subscribe to our newsletter and stay updated with the latest health information.
By clicking on subscribe now, you accept to receive communications from PACE Hospitals on email, SMS and Whatsapp.
Subscribe to PACE Hospitals News
Thank you for subscribing. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
-

Payment in advance for treatment (Pay in Indian Rupees)
For Bank Transfer:-
Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545
Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc)
Call us at 04048486868
ADDRESS
PACE Hospitals
Hitech City : Beside Avasa Hotel, Pillar No. 18, Hyderabad - 500081
Madinaguda: Mythri Nagar, Beside South India Shopping, Madinaguda, Hyderabad - 500050
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals as such.