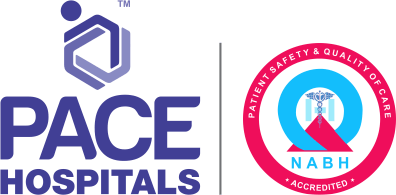
Pelvic Inflammatory Disease (PID) Symptoms, Causes, Risk Factors, Treatment
PID full form in medical - Pelvic inflammatory disease
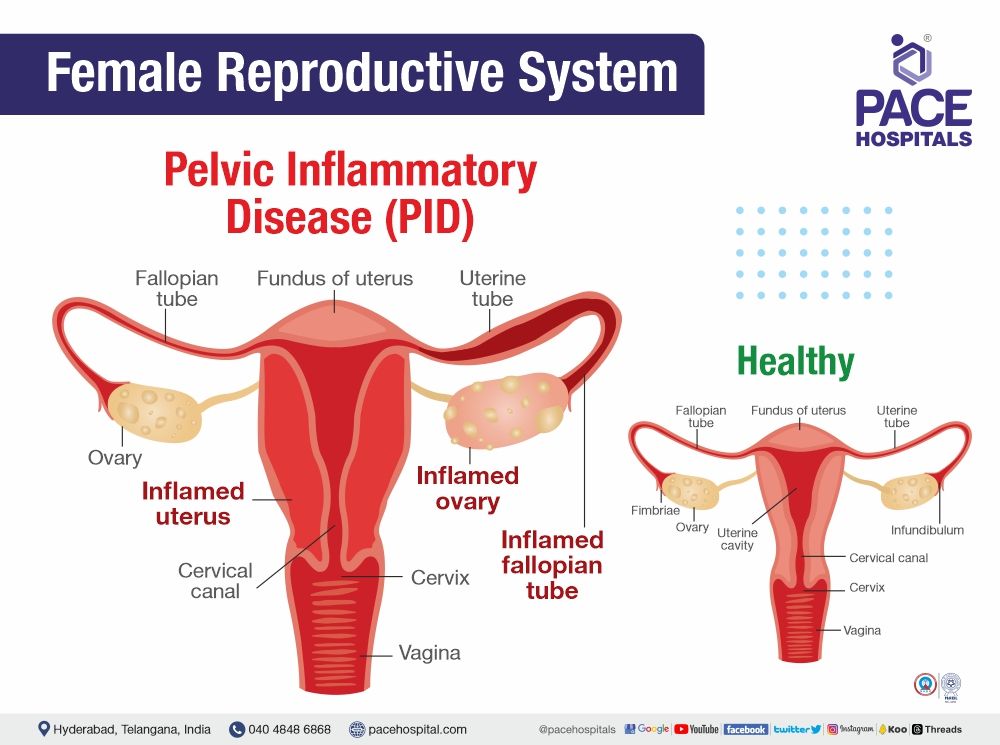
Pelvic inflammatory disease (PID) is characterised by inflammation of a woman's reproductive organs (uterus, fallopian tubes and ovaries), which is caused by infection. It is generally an ascending infection, spreading from the lower genital tract (vulva and vagina) to the upper genital tract (uterus, ovaries, and fallopian tubes).
This condition is commonly seen in women aged 15 to 25 years. Over the past decade, the incidence of PID has decreased due to more women getting tested regularly for bacteria. However often it is seen in both outpatient clinics and emergency department settings.
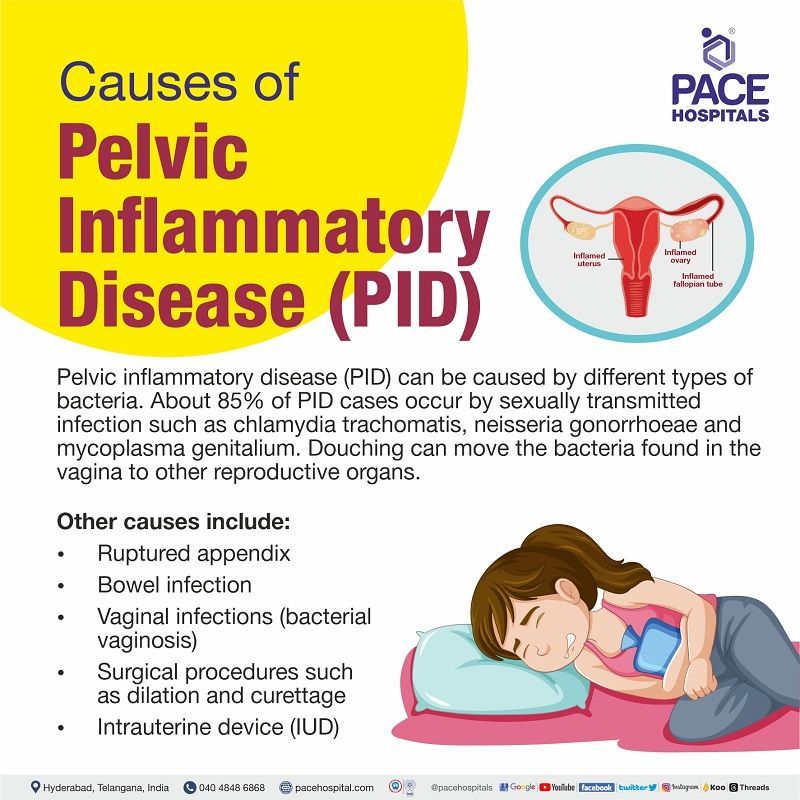
Pelvic inflammatory disease - PID causes
Pelvic inflammatory disease causes include different types of bacteria. However, PID is commonly caused by the bacteria from sexually transmitted infections (STIs) - Chlamydia trachomatis and Neisseria gonorrhoeae. Mycoplasma genitalium (another type of STI) is considered to be increasingly responsible for PID cases.
Other causes of PID (Pelvic inflammatory disease) include:
- Vaginal infections (bacterial vaginosis)
- Ruptured appendix
- Bowel infection (gastroenteritis)
- Some surgical procedures such as dilatation and curettage
- Surgical abortion or intrauterine device (IUD)
About 85% of PID cases occur by sexually transmitted bacteria that travel from the vagina to the cervix and up into the uterus, fallopian tubes and ovaries. A woman gets PID without having a sexually transmitted infection. In some cases, it may also be caused by the normal bacteria that found in the vagina. Sometimes, the bacterium moves up to the female reproductive organs because of douching (washing or cleaning the outside of the vagina using the water or a mixture of fluids to remove odour).
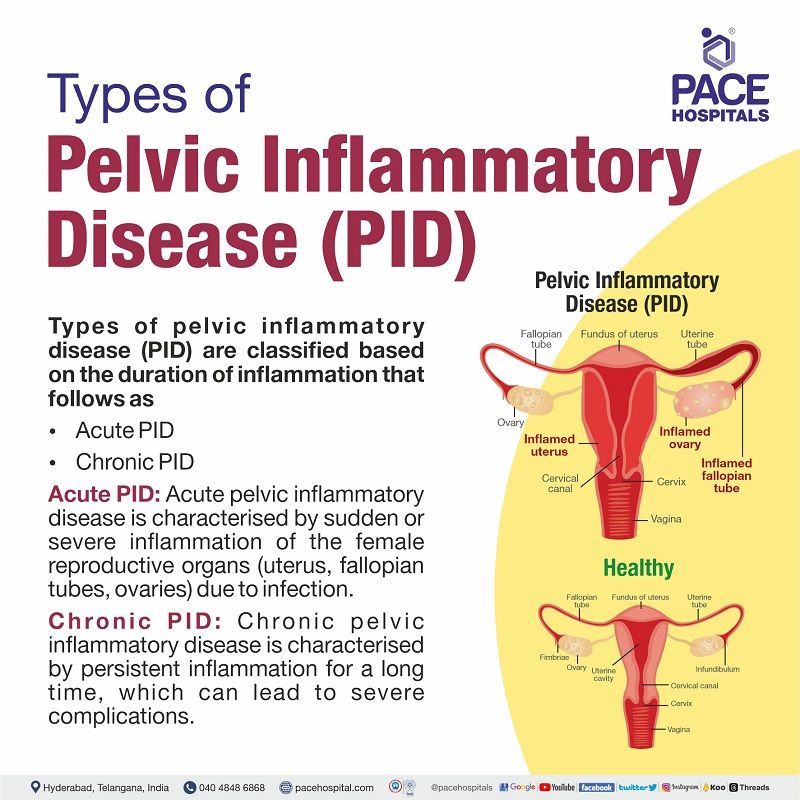
Types of PID - Pelvic inflammatory disease
Types of pelvic inflammatory disease (PID) are classified based on the duration of inflammation that follows as
- Acute PID (Pelvic inflammatory disease)
- Chronic PID (Pelvic inflammatory disease)
Acute PID: Acute pelvic inflammatory disease is characterised by sudden or severe inflammation of the female reproductive organs (uterus, fallopian tubes, ovaries) due to infection.
Chronic PID: Chronic pelvic inflammatory disease is characterised by persistent inflammation for a long time, which can lead to severe complications.
Pelvic inflammatory disease - PID symptoms
Most pelvic inflammatory disease symptoms (female) are mild and may include one or more of the following signs and symptoms of pelvic inflammatory disease:
- Lower abdominal or pelvic pain (common)
- Vaginal discharge (yellow, green or fishy odour).
- Abnormal vaginal bleeding
- Dyspareunia (painful sex)
- Increased temperature
- Painful urination
- Bleeding and spotting after sex
- Pain in the upper right abdomen (rare)
Regular reproductive health checkups are crucial for sexually active women since some individuals may not experience noticeable symptoms of pelvic inflammatory disease. However, PID symptoms might show extreme pain and fever if it is caused by a bacteria called gonorrhoea.
Pelvic inflammatory disease - PID in pregnancy
Pelvic inflammatory disease is rare in pregnancy but causes severe health consequences. Early identification is crucial in improving positive outcomes. Therefore, treatment should not be delayed if there is a high suspicion. Pelvic inflammatory disease can occur in the second trimester of pregnancy. History of sexually transmitted infections, structural abnormality in the pelvis, recent pelvic surgery and invitro fertilization can increase the risk of PID during pregnancy.
Effects of PID on pregnancy
Infection of reproductive organs leads to inflammation, which causes adhesions, scarring and partial or total obstruction (blockage) of fallopian tubes, resulting in infertility (difficulty conceiving), ectopic pregnancy (fertilized egg grows outside of the uterus), and chronic (long-term) pelvic pain.
PID - Pelvic inflammatory disease risk factors
The following are the PID risk factors that include:
- Having untreated sexually transmitted infections (STIs)
- History of pelvic inflammatory disease
- Sexually active women under the age of 25 (common in 15-24 aged females)
- Having multiple (more) sex partners or a partner with more than one sex partner.
- Douche: washing or cleaning the outside of the vagina using a mixture of fluids or water to remove odour (which pushes the bacteria into reproductive organs and hides the signs of PID).
- Tubal ligation (a surgical procedure where fallopian tubes are permanently clipped, blocked, or removed)
- Recently inserted intra-uterine device (IUD) (risk is high in the first few weeks after inserting the IUD).
Complications of PID - Pelvic inflammatory disease
Complications of pelvic inflammatory disease include three main conditions, as follows:
- Chronic pelvic pain
- Infertility
- Ectopic pregnancy
- Recurrent pelvic inflammatory disease
- Tubo-ovarian abscess (fallopian tubes and ovaries)
If left untreated (not treated), pelvic inflammatory disease can lead to above-mentioned complications.
Infections cause inflammatory damage to reproductive organs, which results in long-term (chronic) scarring and blockages (obstruction) in the fallopian tubes. Over time, changes in the fallopian tube can lead to difficulty conceiving due to the inability of a fertilised egg to travel into the uterus through the fallopian tube.
Chronic pelvic pain: The pain may be related to scarring, adhesions and inflammation from the infectious process (when germs enter the body, they increase in number and cause reactions). Recurrent PID is the strongest predictor of developing chronic pelvic pain.
Infertility: Infection causes severe damage to the fallopian tubes, which results in difficulty conceiving.
If chlamydia is an infectious cause of PID, it is more likely to develop infertility.
- One episode of PID can double the risk of tubal infertility.
- The infertility rate will increase with the number of infection episodes.
Ectopic pregnancy: Ectopic pregnancy usually occurs due to damage to fallopian tubes and may appear in 15-60% of women.
- One episode of PID increases the ectopic pregnancy risk (the development of the foetus outside the uterus) by sevenfold.
Recurrent pelvic inflammatory disease: Sometimes, the patient can experience repeated episodes of PID due to the uncleared initial infection. One episode of PID can damage the uterus or fallopian tubes, which makes it easier for bacteria to infect again in future, creating a high chance of getting this condition.
Abscesses: Sometimes, PID causes the development of abscesses, that are infected fluid collections commonly seen in the fallopian tubes and ovaries.
As per the research studies, 18% of females aged between 20-24 with pelvic inflammatory diseases (PID) had developed chronic pain gradually, and 16.8% had difficulty in getting pregnant followed by 8.5% had experience ectopic pregnancies. Three or more episodes of PID can increase the risk of fallopian tube blockage (obstruction) by 75%.
Pelvic inflammatory disease - PID diagnosis
Pelvic inflammatory disease (PID) diagnosis can be made by physical examination, medical history and other tests. First, a healthcare professional can diagnose PID after hearing the symptoms. Then, tests will be done to confirm the PID.
PID tests include:
- Pelvic examination: To examine the pelvic organs and check for abnormal vaginal discharge and tenderness.
- Cervical culture: To analyse the cervix for infections.
- Blood tests: To check for signs of infection
- Urine test: To check for signs of cancer, blood and other diseases. Urinalysis is conducted to detect urinary tract infections that may show (cause) symptoms, such as pelvic pain.
- Pelvic ultrasound: Imaging test that uses sound waves to create images of internal organs
- Endometrial biopsy: A healthcare professional takes or removes a tiny tissue sample from the lining of the uterus for further laboratory evaluation.
- Laparoscopy: A gynecologist inserts a small instrument through an incision in the abdomen and takes images of pelvic organs.
- Swab test: Taking the fluid samples from the vagina and cervix with a swab to find the bacteria in it.
- A pregnancy test: To rule out the ectopic pregnancy
- Nucleic acid amplification tests (NAAT): To check for C. trachomatis and N. gonorrhoeae.
- Culdocentesis: This technique examines the abdominal fluid in the space just behind the vagina.
Differential diagnosis for PID - Pelvic inflammatory disease
PID differential diagnosis include:
- Ectopic pregnancy
- Ovarian cyst rupture
- Ovarian torsion
- Endometriosis
- Cystitis
- Appendicitis
- Diverticulitis
- Traumatic injury
- Pyelonephritis
Pelvic inflammatory disease - PID treatment
Pelvic inflammatory disease treatment majorly involves the combination of antibiotics that can act against bacteria (usually, it has to be taken for two weeks). Most of the time, at least two antibiotics are given to reduce the infection.
If PID is untreated, it causes complications such as persistent pelvic pain due to scarring. If PID is diagnosed early, then it can be treatable. So, early identification and treatment play a significant role in minimising the risk of complications.
A gynaecologist may recommend going into the hospital to treat PID if the person is very sick or pregnant or symptoms are not going away even after taking the antibiotics or having an abscess in a fallopian tube or ovary.
The bacteria that cause PID can spread to another partner through sexual contact. Men can be asymptomatic carriers of bacteria causing PID. Treatment for partners is necessary to prevent the recurrence of infection.
Make sure to finish all medicines until the disease is cleared out completely. If symptoms persist even after the therapy(treatment) seek a medical help.
A hospital stay is needed if the patient has a pregnancy, increased oral temperature, no response to oral antimicrobial therapy, or tubo-ovarian abscess. Surgery may also be required depending on the patient's overall health condition.
Surgical management of Pelvic inflammatory disease (PID)
If the patient is not improving within 72 hours, a re-examination is performed with laparoscopic or surgical intervention, especially when the diagnosis is uncertain.
Surgical treatment may involve:
- Unilateral salpingo-oophorectomy: Surgical removal of one fallopian tube and ovary (located on the same side)
- Hysterectomy: Surgical removal of uterus
- Bilateral salpingo-oophorectomy: Surgical removal of both fallopian tubes and ovaries
Prevention of Pelvic inflammatory disease (PID)
Prevention of pelvic inflammatory disease includes the following:
- Practice safe sex: Use condoms to avoid getting infected by the partner. Practising it can effectively prevent sexually transmitted infections (STIs).
- Get tested: Both partners need to get tested for sexually transmitted infections (STIs). Discussing with a partner and encouraging them to get tested is crucial for the sexual health of both individuals. Regular reproductive health checkups help identify and make treating STIs at earlier stages easier.
- Be monogamous: Having sexual intercourse with one partner can decrease the chances (risk) of developing sexually transmitted infections.
- Limit the sexual partners: Having multiple partners can increase the risk of getting this condition, which shows the negative impacts on reproductive health.
- Seeking treatment: if there are any noticeable symptoms such as pelvic pain, vaginal discharge, and painful sex, medical help will be needed.
- Avoid douche: Douching can remove the normal bacteria found in the vagina that protects from infection and may raise the risk of PID by moving the bacteria to other areas such as the uterus, ovaries and fallopian tubes.
FAQs (frequently asked questions on PID - Pelvic Inflammatory Disease)
Can PID infect pelvic bones?
No, pelvic inflammatory disease cannot infect the pelvic bones directly, because PID mainly infects the reproductive organs of the woman, which spreads from the vagina or cervix to the upper organs, including the uterus and fallopian tubes. Even though it cannot infect the pelvic bones directly, if left untreated, it may lead to complications such as the collection of pus (abscess formation) or chronic inflammation that might affect the surrounding structures.
-
Is Pelvic inflammation disease permanent?
No, Pelvic inflammatory disease is not permanent. It can be cured if the condition is diagnosed and treated early. But if it is not treated(untreated), it causes complications such as pelvic pain, difficulty conceiving and ectopic pregnancy. However, most PID cases who completed their course of antibiotics have no long-term problems.
-
Is Pelvic inflammatory disease curable?
Yes, it is possible to cure this condition by diagnosing it early and receiving immediate treatment, which may include antibiotics.
Delayed treatment can raise the risk of PID complications. It is crucial to complete the prescribed medication when taking antibiotics, even if symptoms disappear before the infection is completely cured. It is essential to ensure that both partners get tested and treated for sexually transmitted diseases (STDs).
-
Does Pelvic inflammatory disease show on ultrasound?
Yes, Pelvic inflammatory disease (PID) may be visualised on an ultrasound. Ultrasound may help identify causative factors or rule out similar conditions, such as endometriosis. Ultrasound findings suggest PID include abscess (fluid collections), thickened fallopian tubes, or increased ovarian volumes in the pelvic area. Pelvic ultrasound is an imaging method that uses sound waves to produce (create) the inside pictures of pelvic area that examine the female bladder, uterus, cervix, ovaries and fallopian tubes.
-
How to diagnose Pelvic inflammatory disease (PID)?
To diagnose Pelvic inflammatory disease, a gynaecologist usually asks for the patient’s medical and medication history and does a physical and pelvic examination to check for signs of PID, such as unusual discharge from the vagina, tenderness or pain in the pelvic area.
Other tests may include:
- Blood tests
- Urine tests
- Swabs of the vagina and cervix
- Ultrasound
- Laparoscopy
-
How to treat Pelvic inflammatory disease (PID)?
A gynecologist will give antibiotics to treat Pelvic inflammatory disease. In most cases, at least the combination of two antibiotics (for two weeks) is used to act against the different types of bacteria.
It is essential to complete the entire course of antibiotics to cure the infection, even if the symptoms disappear fully.
-
How to cure Pelvic inflammatory disease?
In most cases, Pelvic inflammatory disease (PID) is cured by taking medications as the gynecologist prescribes.
PID can be cured by following steps:
- Taking the antibiotics course without skipping
- Rest is needed for severe infection.
- Eating healthy food and staying hydrated.
- Avoiding douche (washing or cleaning the outside of the vagina using water or a mixture of fluids to remove odour).
- Avoiding multiple sexual partners
- Keeping regular (follow-up) appointments to ensure the treatment works, even if the symptoms are absent.
-
Is Pelvic inflammation disease serious?
Yes, PID can be serious if not diagnosed and treated early. If untreated, it causes long-term complications such as pelvic pain, infertility (difficulty conceiving) and ectopic pregnancy (fertilized egg grows outside of the uterus). So, Early diagnosis and treatment are important to lowering the risk of long-term complications.
-
Can Pelvic inflammatory diseases be found in a urine test?
It is not possible to diagnose Pelvic inflammatory disease through urine tests alone. Urinalysis is conducted to detect urinary tract infections that may show (cause) symptoms, such as pelvic pain. It is also used to determine the presence of bacteria such as Neisseria gonorrhoeae and Chlamydia trachomatis, common causes of sexually transmitted infections (STIs). However, it is essential to note that a positive urinalysis does not necessarily indicate(signify) the presence of PID.
-
How to prevent Pelvic inflammatory disease (PID)?
Get regular checkups for STIs: Regular reproductive health checkups can identify and make it easy to treat at earlier stages.
- Practice safe sex: Use condoms to prevent infection.
- Limit the sexual partners: Having multiple partners can increase the risk PID.
- Seeking treatment: if there are any noticeable symptoms such as pelvic pain, vaginal discharge, and painful sex.
- Avoiding douches
- Discussing infection with a partner and encouraging them to get tested is essential.
-
How to test yourself for PID?
No, it is impossible to self-diagnose Pelvic inflammatory disease as it requires medical assistance to evaluate symptoms and diagnose through a physical examination, pelvic examination, laboratory tests and imaging tests to confirm it. A gynaecologist examination is needed to diagnose this condition.
-
What is the best treatment for PID?
The primary treatment for PID involves a combination of antibiotics. Early identification and management of the symptoms is key in effectively addressing Pelvic inflammatory disease (PID). If diagnosed early, antibiotics can be used to treat it easily and effectively. However, if PID is untreated (not treated), it can lead to serious complications.
-
Can PID be cured?
Yes, it can be cured by early diagnosis and treatment (including antibiotics). Late (delayed) treatment can increase the risk of PID complications. When taking antibiotics, it's essential to finish the course prescribed by a healthcare professional, as even though the symptoms may disappear, there are chances of lingering infection. It is crucial to ensure both partners get tested and treated for sexually transmitted diseases (STDs).
-
How long does PID last after treatment?
An infected woman may feel better two to three days after starting the treatment. Complete recovery occurs in most cases if it is diagnosed early and treated with antibiotics as prescribed by healthcare professionals. Most women can expect to feel better within two to three days and fully recover within 10 to 14 days.
However, if it is not treated (untreated), it could spread to other parts and form fluid collections (abscesses) in fallopian tubes or ovaries.
-
Can laparoscopy detect pelvic infection?
Yes, Pelvic inflammatory disease can be identified (diagnosed) rapidly and precisely through laparoscopy. It helps detect ectopic pregnancy, which is a complication of Pelvic inflammatory disease. A laparoscope examines the reproductive organs, which helps detect infections.
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.

Our Locations
Subscribe to our newsletter and stay updated with the latest health information.
By clicking on subscribe now, you accept to receive communications from PACE Hospitals on email, SMS and Whatsapp.
Subscribe to PACE Hospitals News
Thank you for subscribing. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
-

Payment in advance for treatment (Pay in Indian Rupees)
For Bank Transfer:-
Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545
Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc)
Call us at 04048486868
ADDRESS
PACE Hospitals
Hitech City : Beside Avasa Hotel, Pillar No. 18, Hyderabad - 500081
Madinaguda: Mythri Nagar, Beside South India Shopping, Madinaguda, Hyderabad - 500050
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals as such.