Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Erem AS, Turashvili G. Pigmented lesions-vulva. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/vulvapigmented.html. Accessed May 1st, 2024.
Definition / general
- Vulvar lesions that appear pigmented either grossly or microscopically
Essential features
- Pigmented vulvar lesions are a poorly characterized group of entities with variable gross and histologic appearances
- Lesions containing melanin and those that appear pigmented but lack melanin microscopically
- Postinflammatory reactive and reparative changes, purpura, vascular lesions, debris filled comedones and normal genital skin variations may be included in this category (Dermatol Clin 2010;28:795)
ICD coding
- ICD-O
- 8720/0 - nevus, NOS
- 8761/0 - congenital melanocytic nevus, NOS
- 8720/0 - atypical melanocytic nevus of genital type
- 8727/0 - dysplastic nevus
- 8720/3 - malignant melanoma, NOS
- 8077/0 - low grade squamous intraepithelial lesion
- 8077/2 - high grade squamous intraepithelial lesion
- 8071/2 - differentiated vulvar intraepithelial neoplasia (VIN)
- 8085/3 - squamous cell carcinoma, HPV associated
- 8086/3 - squamous cell carcinoma, HPV independent
- 8070/3 - squamous cell carcinoma, NOS
- 8090/3 - basal cell carcinoma, NOS
- 8542/3 - Paget disease, extramammary
- C51.0 - labia majus / labia majora, NOS; Bartholin gland; skin of the labia majora
- C51.1 - labia minus / labia minora
- C51.2 - clitoris
- C51.8 - overlapping lesions of the vulva
- C51.9 - vulva, NOS
- ICD-10
- D22.9 - melanocytic nevi, unspecified
- N90.89 - vulvar lesion(s), nontraumatic
- N76 - inflammation of the vulva
- D28.0 - benign neoplasm of the vulva
- D39.0 - neoplasm of uncertain behavior of female genital organs
- N90.3 - intraepithelial neoplasia (VIN)
- D07 - carcinoma in situ of other and unspecified genital organs
- C51 - malignant neoplasm of the vulva
- ICD-11
- 2C70 - malignant neoplasm of the vulva
- 2C70.0 - basal cell carcinoma of the vulva
- 2C70.2 - squamous cell carcinoma of the vulva
- 2E67.1 - carcinoma in situ of the vulva
- 2E67.11 - vulvar Paget disease
- 2E67.12 - vulvar intraepithelial neoplasia, HPV independent
- 2E67.13 - high grade squamous intraepithelial lesions of the vulva
- EA83.00 - lichen simplex of the vulva
- EB60.0 - lichen sclerosus of the vulva
- ED61.11 - vulvar melanotic macule
- GA13.1 - low grade squamous intraepithelial lesions of the vulva
- XH5FT2 - vulvar intraepithelial neoplasia, grade III
Epidemiology
- Different types of vulvar pigmented lesions are found in 8 - 12% of females (Ann Pathol 2022;42:79)
- In reproductive aged women (median age: 40 - 44 years), 68% of vulvar pigmented lesions are lentigines (Dermatol Clin 2010;28:795, J Am Acad Dermatol 1990;22:104)
- In children with vulvar melanosis, multisystem genodermatoses should be considered (see Table 3)
- Prevalence of vulvar melanocytic nevi is 2.3% (J Am Acad Dermatol 1990;22:104)
- Vulvar nevus (nevus of special site; pigmented nevi, nevocellular nevi, common nevi)
- Premenopausal women (median age: 28 - 33 years) (J Am Acad Dermatol 2014;71:1241)
- Prevalence is 3.3% in girls younger than 18 years (Am Acad Dermatol 2014;70:429)
- Majority of nevi are acquired, while congenital nevi are uncommon
- Atypical melanocytic nevi of the genital type (also known as nevi with site related atypia)
- Generally occur in young women (median age: 17 - 26 years) (see Table 4) (J Cutan Pathol 2008;35:24, J Am Acad Dermatol 2014;71:1241, Dermatology 2011;222:157, Am J Surg Pathol 2008;32:51)
- Seborrheic keratoses mostly occur in Caucasian patients aged > 40 years but can be diagnosed in all age groups and races (Dermatol Clin 2010;28:795)
- Angiokeratoma of Fordyce (genital angiokeratoma)
- Usually occurs in young women and may be associated with pregnancy or vulvar varicosity (Arch Dermatol 1967;95:166)
- Pigmented condylomata acuminata (anogenital warts)
- More common in patients with darker skin tones in association with high risk human papillomavirus (HPV) types (Dermatol Ther 2010;23:449)
- Anogenital warts affect 1% of adults
- Pigmented vulvar intraepithelial neoplasia (previously known as Bowen disease or Bowenoid papulosis) (Dermatol Clin 2010;28:795, J Low Genit Tract Dis 2013;17:320)
- HPV associated high grade squamous intraepithelial lesion (linked to high risk HPV types, most commonly 16, 18, 31)
- Risk factors: smoking, multiple sex partners, immunosuppression
- Younger women
- Typically multifocal, hyperpigmented flat topped papules or plaques with distinct margins
- HPV independent, differentiated vulvar intraepithelial neoplasia
- Older women
- Arises in a background of lichen sclerosus
- HPV associated high grade squamous intraepithelial lesion (linked to high risk HPV types, most commonly 16, 18, 31)
- Pigmented basal cell carcinoma
- Accounts for 5% of primary vulvar cancers (Dermatol Clin 2010;28:795)
- Prevalence of genital basal cell carcinoma ranges from 0.5 to 1.7% and affects older women (J Cutan Pathol 2018 Jun 19 [Epub ahead of print], Int J Gynecol Pathol 2022;41:86)
Sites
- Vulvar pigmented lesions generally show predilection for labia majora, labia minora and clitoris, less commonly mons pubis and perineum (Arch Pathol Lab Med 2011;135:317)
- Vulvar melanosis
- Most common in mucosal surfaces followed by hair bearing skin of external genitalia (Dermatol Clin 2010;28:795)
- Vulvar nevus
- Most commonly located on labia majora, labia minora or clitoral hood
- Atypical melanocytic nevi of the genital type
- Labia majora (most common)
- More frequent on mucosal areas in children younger than 10 years (Hum Pathol 1998;29:S1, Am J Surg Pathol 2008;32:51)
- In adults, equal distribution between mucosal and hair bearing surfaces (Am J Surg Pathol 2008;32:51)
- Angiokeratoma of Fordyce
- Labia majora
Etiology
- Physiologic hyperpigmentation
- Dark skin > light skin complexion
- Hormonal variation
- Postinflammatory hyperpigmentation (Dermatol Clin 2010;28:795)
- Most commonly occurs in areas of previous injury or dermatosis
- Associated with known inflammatory conditions
- Lichen sclerosus
- Lichen planus
- Erythema multiforme
- Fixed drug eruptions
- Trauma and dermatologic treatments
- Acanthosis nigricans
- Strong association with insulin resistance (diabetes mellitus, obesity, hyperandrogenism) (Am J Clin Dermatol 2004;5:199)
- Malignancy (adenocarcinoma most common) related acanthosis nigricans
- Production of hormones and peptides by malignancy have been implicated
- Secretion of transforming growth factor alpha (TGFα) in large quantities is associated with increased keratinocyte proliferation (J Gastroenterol 1997;32:71)
- Medication: nicotinic acid, glucocorticoids, oral contraceptives and diethylstilbestrol, protease inhibitors in human immunodeficiency virus infected patients (Clin Infect Dis 2002;34:716)
- Seborrheic keratosis
- Proliferation of keratinocytes of unknown cause (Dermatol Clin 2010;28:795)
- Subset of genital seborrheic keratosis may be related to low risk HPV, though this is controversial (Hum Pathol 2003;34:559, APMIS 2012;120:477, J Low Genit Tract Dis 2014;18:190)
- Genital / vulvar melanosis / lentiginosis
- Largely unknown
- Variation in hormonal levels may play a role (onset of melanosis after oral contraceptive use and the immediate postpartum period) (J Am Acad Dermatol 2014;71:1241)
- Vulvar nevus
- May relate to hormonal milieu (J Low Genit Tract Dis 2013;17:320)
- Atypical melanocytic nevi of the genital type
- Largely unknown but associated with anatomic milk line (Am J Surg Pathol 2008;32:51)
- Angiokeratoma of Fordyce
- Associated with pregnancy or vulvar varicosity (Arch Dermatol 1967;95:166)
- Speculated pathogenesis is localized hypertension (Arch Dermatol 2005;141:1325)
- Pigmented condylomata acuminata
- HPV infection (90% accounted for HPV 6 and 11)
- Pigmented basal cell carcinoma
- Sun exposure, ultraviolet (UV) specific p53 mutations in sun exposed areas
- Previous radiation
- Limited studies in Chinese population proposed p53 overexpression independent to UV specific pathway (J Cutan Pathol 2018 Jun 19 [Epub ahead of print])
Diagrams / tables
Table 1: Features distinguishing vulvar nevi, melanosis and melanoma (adapted from J Am Acad Dermatol 2014;71:1241)
| Reassuring features suggestive of a benign process | Concerning features for possible malignancy | |
| Clinical |
|
|
| Dermoscopy |
|
|
| Reflectance confocal microscopy |
|
|
Table 2: Clinical morphology for pigmented vulvar lesions (adapted from Dermatol Ther 2010;23:449)
| Papules and macules | Patches and plaques |
| Pigmented nevi (nevocellular nevi) | Physiologic hyperpigmentation |
| Dysplastic nevi | Postinflammatory hyperpigmentation |
| Malignant melanoma | Vulvar melanosis (vulvar lentiginosis) |
| Anogenital warts | Acanthosis nigricans |
| Vulvar intraepithelial neoplasia | |
| Seborrheic keratosis | |
| Basal cell carcinoma | |
| Angiokeratoma |
Table 3: Genodermatosis syndromes with vulvar melanosis (adapted from J Am Acad Dermatol 2014;71:1241)
| Genodermatosis | Areas affected | Key features | Genetic mutation |
| Peutz-Jeghers syndrome | Oral, perianal and genital area, lips, nostrils, hands, feet | Hamartomatous polyps in the gastrointestinal tract (GIT), breast, ovarian, pancreatic and GIT cancers | STK11 |
| Carney complex | Oral and genital area, lips, eyelids, conjunctiva | Blue nevus, psammomatous melanotic schwannoma, myxomas (usually cardiac), endocrine neoplasms | PRKAR1A |
| Multiple lentigines syndrome (LEOPARD syndrome) | Face, neck, trunk, genital area | Delayed growth, sensorineural deafness, ECG abnormalities, ocular hypertelorism, pulmonic stenosis, abnormal genitalia | PTPN11, RAF1, BRAF |
| Bannayan-Riley-Ruvalcaba syndrome | Face, genital area | Macrocephaly, intellectual and motor deficiencies, joint hyperextensibility, pectus excavatum, scoliosis, intestinal hamartomatous polyposis, lipomas, hemangiomas | PTEN |
| Dowling-Degos syndrome | Axillae, neck, flexural folds, inguinal and genital area | Follicular papules, comedone-like lesions, perioral scar, reticulated hyperpigmentation, hypopigmented or erythematous macules | KRT5 |
Table 4: Clinical and histologic differences between atypical genital nevus and vulvar melanoma
(adapted from Hoang: Melanocytic Lesions - A Case Based Approach, 1st Edition, 2014)
| Proposed diagnosis | Atypical genital nevus of special anatomic site | Vulvar melanoma |
| Age | Premenopausal, young adult | Postmenopausal |
| Size | < 1 cm | > 1 cm |
| Delineation | Well circumscribed | Infiltrative |
| Symmetry | Present | Absent |
| Lateral extension of junctional component | Focal | Present |
| Lentiginous junctional component | Focal | Present |
| Junctional nests | Dyscohesive | Confluent |
| Retraction artefact | Present | Absent |
| Ulceration | Absent or due to trauma | Often present |
| Pagetoid upward spread | Focal, central, inconspicuous | Prominent |
| Cytologic atypia | Superficial, mild - moderate | Deep, moderate to severe |
| Dermal mitosis | Rare and superficial | Conspicuous, atypical, deep |
| Dermal maturation | Present | Absent |
| Melanin pigmentation | Coarse, uniform | Fine, irregular |
| Dermal fibrosis | Broad zone of superficial coarse dermal fibrosis | Regression type |
Clinical features
- During obstetrics / gynecologic visit
- Women rarely examine their vulva closely; consequently, duration and change are of minimum relevance (Dermatol Clin 2010;28:795)
- Consider endocrine disorders (e.g., congenital adrenal hyperplasia, Addison disease and Cushing disease) (Dermatol Clin 2010;28:795)
- Decision to biopsy is based on atypical appearance of pigmented lesion (Dermatol Clin 2010;28:795)
- Pigmented lesions on genital skin appear more atypical than on extragenital skin (Dermatol Clin 2010;28:795)
- Punch or excisional biopsy is preferred over shave biopsy (Dermatol Clin 2010;28:795)
- Physiologic hyperpigmentation (Dermatol Clin 2010;28:795)
- Most common in patients with dark complexion
- May vary with different hormonal stages (e.g., puberty, menopause, pregnancy, contraception use)
- Distribution
- Macular, symmetric, nonscaly or change in texture; usually darker at the posterior introitus, labia minora and perianal skin
- Proximal medial thighs may show uniform hyperpigmentation with fading into the color of nonmodified mucous membranes
- Postinflammatory hyperpigmentation
- May occur in all skin types
- Most notable in patients with dark skin complexion
- Most commonly in areas of previous injury or dermatosis
- Distribution
- Usually less symmetric than physiologic hyperpigmentation
- Macules and patches with different shades of brown
- Macular, symmetric, nonscaly or change in texture; usually darker at the posterior introitus, labia minora and perianal skin
- Proximal medial thighs may show uniform hyperpigmentation with fading into the color of nonmodified mucous membrane
- Acanthosis nigricans
- Velvety, leathery, wrinkly texture with a darker appearance versus unaffected sites of the body
- Skin tags within skin folds are common
- Spares mucous and modified mucous membranes (MMB)
- Seborrheic keratosis
- Typically single, keratotic, flat topped, sharply demarcated, brown lesions with a stuck on appearance, showing keratotic and follicular plugging; uniform color and shape
- Because of irritation, moisture and hair in genital area, the lesions may appear less keratotic due to loss of their coloration and uniformity (Dermatol Clin 2010;28:795)
- May have slightly verrucous surface
- Absence of seborrheic keratosis on other body parts coupled with a younger age and Ki67 immunohistochemical stain extending into the superficial part of the lesion would favor condyloma
- Detection of low risk HPV test would confirm diagnosis
- Unlikely to occur in the vulva if other skin sites appear unaffected (Dermatol Clin 2010;28:795)
- Clinically seborrheic keratosis may mimic nevi, pigmented condylomata acuminata and vulvar intraepithelial neoplasia and less often dysplastic nevi or melanoma (Dermatol Clin 2010;28:795)
- Only seborrheic keratosis that appear atypical, clinically and on dermoscopy, should be biopsied
- Genital / vulvar melanosis / lentiginosis
- Incidental finding on inspection
- Single or multiple asymptomatic, asymmetric, macules or patches with variation of size and color ranging from tan to black within the lesion, irregular and poorly demarcated borders (Dermatol Clin 2010;28:795, J Low Genit Tract Dis 2013;17:320)
- Concerning features: papular component, erosions, reported pruritis or pain
- Can be associated with a postinflammatory hyperpigmentation, such as in patient with lichen sclerosus and lichen planus (Dermatol Clin 2010;28:795)
- Biopsy is recommended to definitely exclude the presence of melanoma or pigmented vulvar intraepithelial neoplasia (Dermatol Clin 2010;28:795)
- Vulvar nevus
- Nevi can be flat (junctional) or domed (compound or intradermal)
- Common nevi range from tan to dark brown in color; bluish color is indicative of pigment in the dermis (Dermatol Clin 2010;28:795)
- Generally symmetrical, with sharp and regular border and even color throughout the lesion
- Common acquired nevi are usually < 0.6 cm, dysplastic are usually > 0.6 cm
- Atypical lesions should be biopsied to rule out dysplastic nevi versus melanoma
- Atypical melanocytic nevi of the genital type (Hum Pathol 1998;29:S1, Am J Surg Pathol 2008;32:51)
- Compared to nevi of special site, they may have alarming clinical features, darker pigmentation, irregular border and large size
- Angiokeratoma of Fordyce
- Typically multiple, small, shiny red to purple; some can appear very dark blue to black
- Early lesions are soft and blanchable; later lesions may become darker and keratotic
- Pigmented condylomata acuminata
- Usually multiple with variety of morphology (papillomatous, verrucous, fleshy papules and flat topped) (Dermatol Ther 2010;23:449)
- In patients with dark complexion, pigmented warts can be flat topped, lobular or papular; only the filiform variant is less likely to be hyperpigmented (Dermatol Ther 2010;23:449)
- Flat topped, brown, anogenital warts in individuals of light skin should be biopsied with concern of vulvar intraepithelial neoplasia (Dermatol Clin 2010;28:795)
- Clinically, anogenital warts may be indistinguishable with seborrheic keratosis
- Pigmented vulvar intraepithelial neoplasia
- HPV associated high grade squamous intraepithelial lesion
- Typically multifocal, hyperpigmented, flat topped papules or plaques with distinct margins
- Biopsies should be avoided if lesions were recently treated (e.g., podophyllin); treatment effect may be interpreted as vulvar intraepithelial neoplasia histologically
- HPV independent differentiated vulvar intraepithelial neoplasia
- Unifocal, often erythematous, well demarcated patches and plaques, with occasional hyperpigmentation
- Clinical differentials include nevi, seborrheic keratosis and anogenital warts
- Keratotic scale may be lacking on mucous and modified mucous membranes
- Clinical differentials include psoriasis, lichen simplex chronicus and tinea
- May be associated with lichen sclerosus or lichen planus
- HPV associated high grade squamous intraepithelial lesion
- Pigmented basal cell carcinoma
- Usually pink and flat or nodular with flesh colored, pearly appearing, translucent sheen but may be irregularly pigmented (brown-black)
- Can appear as nodules, polyps, ulcers or flat areas of hyperpigmentation and hypopigmentation
- Basal cell nevus syndrome may affect perineum
- Regular anogenital examinations are recommended
- See Table 2
Diagnosis
- Dermoscopy for nonmodified mucous membranes is useful (Dermatol Ther 2010;23:449)
- Pigmented condylomata acuminata are characterized by exophytic papillary structures with variation in pigment that includes jet black color, red dots and whitish halo (keratinization)
- Histologic diagnosis is confirmatory for other vulvar pigmented lesions (Dermatol Clin 2010;28:795, JAMA Dermatol 2020;156:1185)
- See Table 1
Laboratory
- Additional laboratory workup may be considered if syndromic association is suspected
Prognostic factors
- Vulvar nevus
- Atypical nevi formed along the milk line have no increased risk for malignant transformation (Dermatol Ther 2010;23:449)
- Risk for vulvar melanoma arising from vulvar nevi remains unclear
- Out of 219 Swedish patients, 98% of de novo melanomas occur on mucosal surfaces or the hairy - mucosal junction (Acta Oncol 2004;43:421, Cancer 1999;86:1273)
- 35% of these cases involve pre-existing nevi at the melanoma sites on the hair bearing skin
- Dysplastic nevi indicate increased risk for melanoma (Dermatol Ther 2010;23:449)
- Atypical melanocytic nevi of the genital type
- Thought to have a benign clinical course (Hum Pathol 1998;29:S1, Am J Surg Pathol 2008;32:51)
- Pigmented vulvar intraepithelial neoplasia
- Risk of progression to invasive vulvar carcinoma can be as high as 87.5% in women with untreated disease
- HPV independent differentiated vulvar intraepithelial neoplasia may coexist with lichen sclerosus
- Multifocal warty / basaloid HPV associated vulvar intraepithelial neoplasia may regress spontaneously in young women (Eur J Obstet Gynecol Reprod Biol 2008;137:97)
- Pigmented basal cell carcinoma
- Metastasis is very rare (< 1% of all basal cell carcinomas) (Arch Dermatol 2003;139:643)
- 10% recurrence rate for vulvar basal cell carcinomas (Arch Dermatol 2003;139:643)
- Basal cell carcinomas can be locally disfiguring and destructive, unless treated with excision and radiation
Case reports
- 18, 57 and 68 year old women with vulvar pigmented cystic lesions (Int J Gynecol Pathol 2022;41:93)
- 20 year old woman with irregular, darkly pigmented, vulvar lesion (J Cutan Pathol 2022;49:172)
- 24 year old woman with vulvar pigmented epithelioid melanocytoma (PEM) (Am J Dermatopathol 2020;42:544)
- 27 year old pregnant woman with massive vulvar Kaposi sarcoma (Int Med Case Rep J 2016;9:227)
- 33 year old woman with HIV and syphilis coinfection and genital Kaposi sarcoma (BMC Infect Dis 2019;19:1095)
- 34 year old woman with a hyperpigmented vulvar nodule (Am J Dermatopathol 2020;42:46)
- 39 year old woman with dark brown vulvar discoloration (Acta Dermatovenerol Croat 2022;30:261)
- 50 year old woman with vulvar mucosal PEM (Dermatol Pract Concept 2020;10:e2020070)
- 80 and 92 year old women with hypopigmented and heavily pigmented vulvar nodules (Ceska Gynekol 2021;86:325)
- 86 year old White woman with hyperpigmentation on upper vulva (Medicina (Kaunas) 2023;59:206)
Treatment
- Vulvar nevus
- Atypical lesions should be biopsied to rule out dysplastic nevi and melanoma
- Simple excision is usually sufficient
- Angiokeratoma of Fordyce (Dermatol Ther 2010;23:449)
- Therapy is usually not needed
- If irritated or for cosmetic purposes, the individual lesions can be lightly hyfrecated or removed by shave
- Multiple lesions can be treated with cryotherapy, electrocautery, radiofrequency and ablative laser
- Depending on the exact location, simple excision may be preferred for some lesions
- Pigmented condylomata acuminata (Dermatol Ther 2010;23:449)
- Cryotherapy, laser, shave / snip excision
- Chemodestruction with podofilox, trichloroacetic / bichloroacetic acid
- Alternatively, immunotherapy with imiquimod can be used
- Pigmented vulvar intraepithelial neoplasia:
- Surgical excision (wide local excision), cryotherapy, laser, vaporization, shave / snip excision (Obstet Gynecol 2016;128:e178)
- For larger lesions, imiquimod is commonly used
- Less often, 5 fluorouracil (5FU) cream may be considered
- Topical 5 aminolevulinic, acid based, photodynamic therapy is a new modality
Clinical images
Contributed by José Alberto Fonseca Moutinho, M.D.
Images hosted on other servers:
Microscopic (histologic) description
- Physiologic hyperpigmentation
- Number of melanocytes and keratinocytes in the basal layer is usually higher compared with adjacent normal epithelium
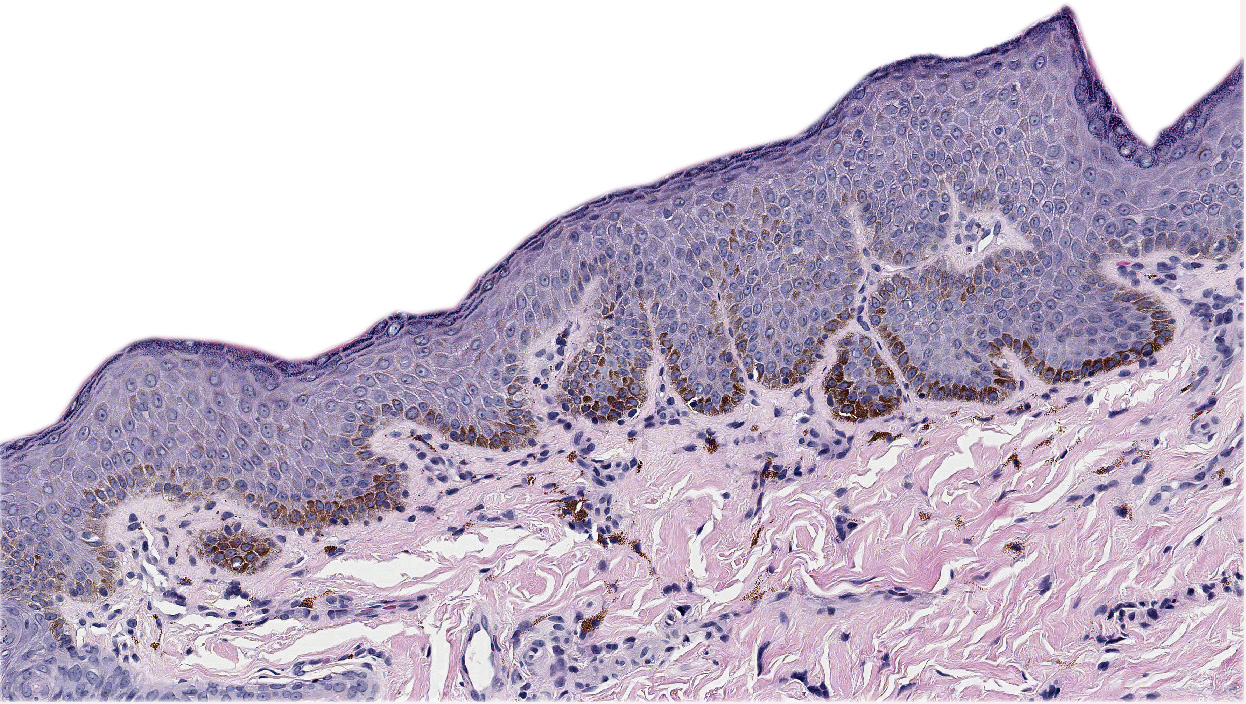
- Genital / vulvar melanosis / lentiginosis
- Basilar hyperpigmentation with mild melanocytic hyperplasia at the dermoepidermal junction arranged as solitary units more commonly than in nests, epithelial hyperplasia and stromal melanophages without cytologic atypia (Dermatol Clin 2010;28:795, J Low Genit Tract Dis 2013;17:320)
- Postinflammatory hyperpigmentation
- Basement membrane damage with pigment incontinence followed by melanin release into the superficial dermis (Dermatol Clin 2010;28:795, J Low Genit Tract Dis 2013;17:320)
- Acanthosis nigricans
- Mild hyperkeratosis, acanthosis and papillomatosis
- Can alternate with atrophic areas
- Occasional keratin filled cysts
- Nonspecific perivascular chronic inflammatory infiltrate may be present in superficial dermis
- Seborrheic keratosis
- Hyperkeratosis, acanthosis or pseudohorned cysts
- Occasional dendritic melanocytes in epidermis
- Vulvar nevus
- Pigmented nevi (nevocellular nevi) of the special site
- Proliferation of nonpigmented and pigmented melanocytes with no to mild cytologic atypia
- Involving the dermal epidermal junction in junctional nevus
- Involving the dermal epidermal junction and dermis in compound nevus
- Involving the dermis in intradermal nevus
- Typically, symmetrical silhouette with very minor irregularity or asymmetry
- Zonation (also known as maturation)
- Decrease in size of nests
- Decrease of individual melanocytes from the large epithelioid (type A melanocytes) appearance superficially to small epithelioid lymphocyte-like (type B) and fusiform schwannian (neural, type C) at the deep part of the lesion
- If melanin is present, it tends to be most prominent in epidermal and superficial dermal melanocytes with loss of pigmentation in the deeper part of the lesion
- Lack of mitoses
- No evidence of regression
- Proliferation of nonpigmented and pigmented melanocytes with no to mild cytologic atypia
- Dysplastic nevi diagnosis has undergone multiple revisions and the new World Health Organization (WHO) classification is still pending final diagnostic criteria
- Practically considered an entity that entails a deviation from stereotypical junctional nevi comprising architectural disorder and cytologic atypia (WHO 5th edition)
- Histologic features supporting dysplastic nevus
- Presence of junctional shoulders - basilar proliferation of atypical melanocytes that must extend beyond the dermal component
- Superficial nests are usually very similar and may show focal bridging or coalescence of the nests
- Elongation and bridging of the rete ridges with nests
- Melanocytes may scatter suprabasally (confined to the lower epidermal layer)
- Lamellar and concentric fibroplasia
- Patchy lymphocytic infiltrate
- Cytologic atypia is based on nuclear size comparing with neighboring basal keratinocytes, presence of nucleoli, chromatin hyperchromasia and clumping
- Pigmented nevi (nevocellular nevi) of the special site
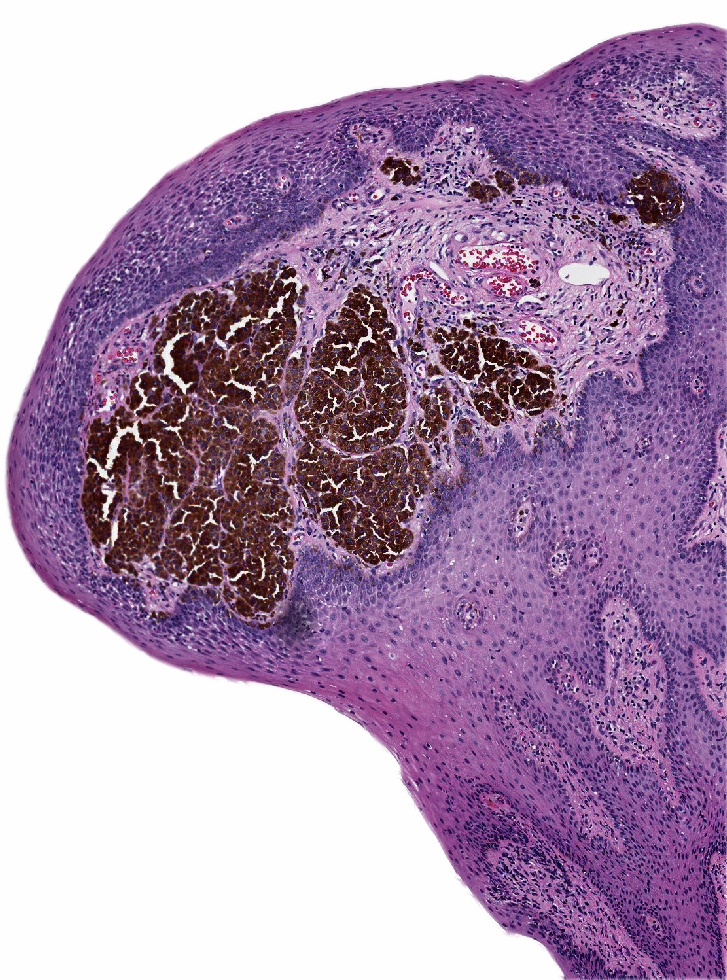
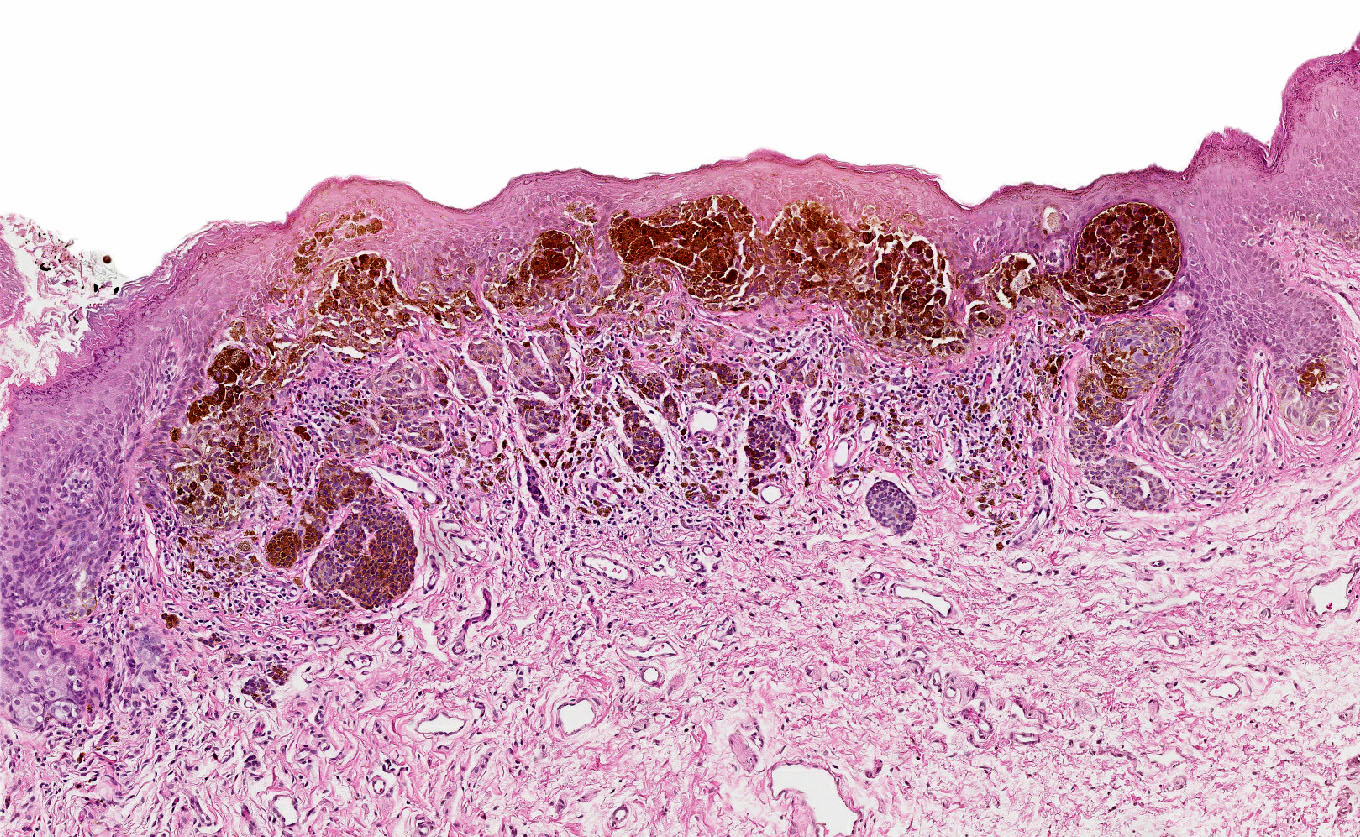
- Atypical melanocytic nevi of the genital type
- Symmetrical lesion with sharp demarcation and dermal maturation (J Cutan Pathol 2008;35:24)
- 3 histological patterns described by Clark (Hum Pathol 1998;29:S1)
- Nested: oval, typically large nests, perpendicular or parallel to dermoepidermal junction
- Dyshesive nests: nearly contiguous forming a band that separates the epidermis from the mature dermal melanocytes
- Crowded: closely apposed, ill defined nests and single cells obscuring the dermal epidermal junction
- Usually mild to moderate uniform cytologic atypia (J Cutan Pathol 2008;35:24)
- Single cell growth with focal pagetoid spread may be present but is usually located in the center of lesion (J Cutan Pathol 2008;35:24)
- Adnexal spread may be present (Hum Pathol 1998;29:S1)
- Dense eosinophilic fibrosis in the superficial dermis (Hum Pathol 1998;29:S1, J Cutan Pathol 2008;35:24)
- Intradermal component with maturation is often present (J Cutan Pathol 2008;35:24)
- Nevi within lichen sclerosus can appear more atypical
- For best diagnosis, lichen sclerosus should be controlled before excision of the nevus (J Am Acad Dermatol 2004;50:690, Arch Dermatol 2002;138:77)
- See Table 4
- Angiokeratoma of Fordyce (J Cutan Med Surg 2020;24:188)
- Dilated capillaries in superficial dermis only with overlaying acanthosis and hyperkeratosis
- Vessels may appear to herniate into epidermis (J Cutan Med Surg 2020;24:188)
- Lack of dilated vasculature in deep dermal and subcutaneous component
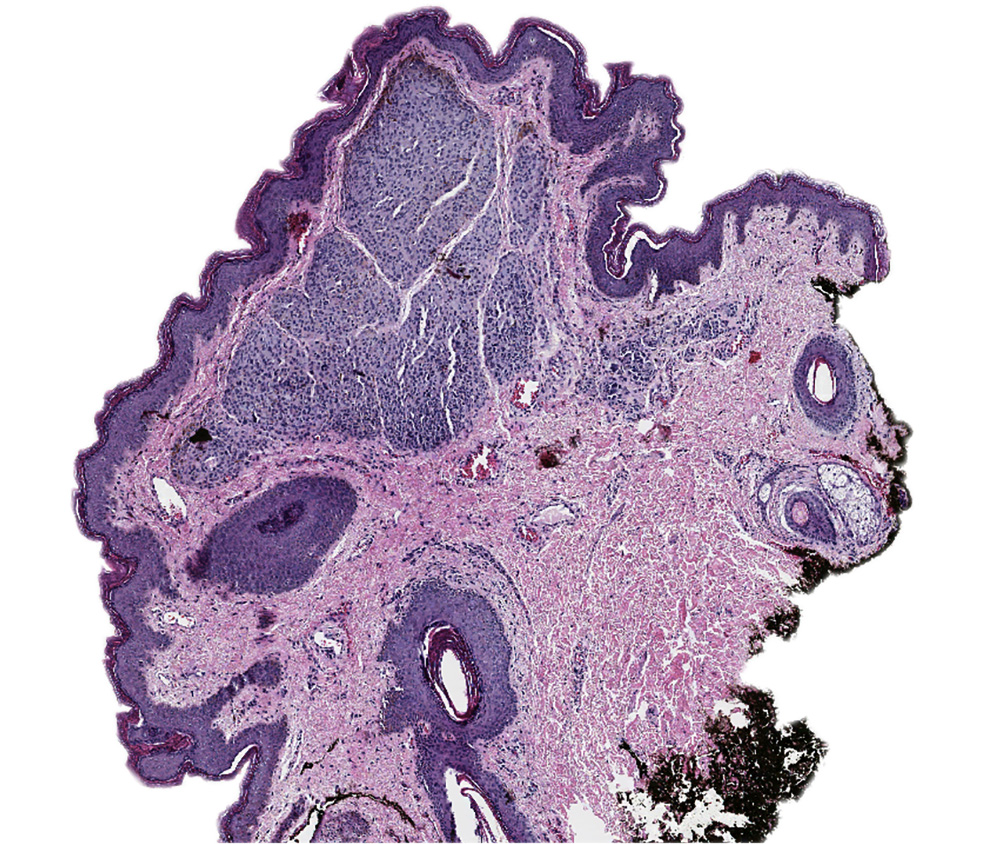
- Pigmented condylomata acuminata
- HPV related histologic changes
- Exophytic growth with marked acanthosis and trabecular or solid pattern
- Superficial koilocytes are characteristic
- Coarse keratohyalin granules may be seen
- Condylomas treated with podophyllin demonstrate marked epidermal pallor and increased mitosis as well as necrosis of keratinocytes in the lower half of epidermis
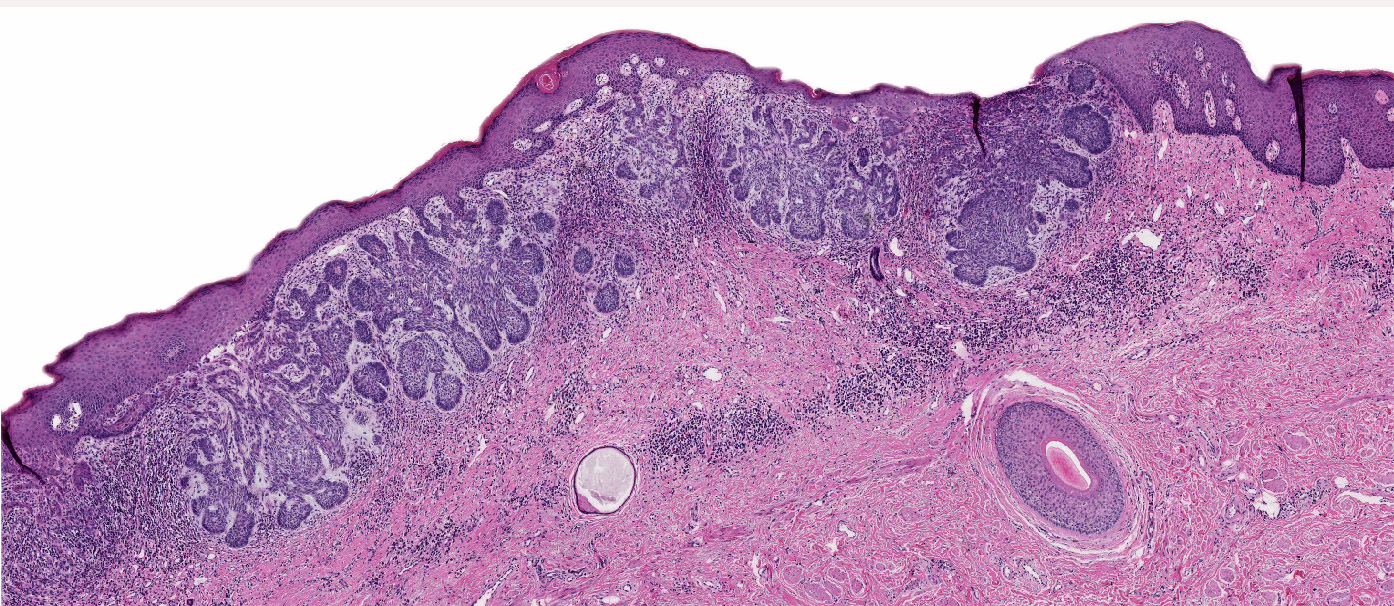
- Pigmented vulvar intraepithelial neoplasia
- Both types show hyperkeratosis with parakeratosis
- HPV associated high grade squamous intraepithelial lesion
- Parakeratosis with koilocytosis and full thickness epithelial involvement
- Enlarged hyperchromatic nuclei
- Easily identifiable mitoses
- Apoptotic bodies may be present
- HPV independent differentiated vulvar intraepithelial neoplasia
- Parakeratosis with acanthosis
- Elongation and anastomosis of rete ridges
- Enlarged hypereosinophilic keratinocytes with prominent intercellular bridges
- Basal layer with prominent cytologic atypia
- Pigmented basal cell carcinoma
- Islands or nests of basaloid cells with peripheral palisading
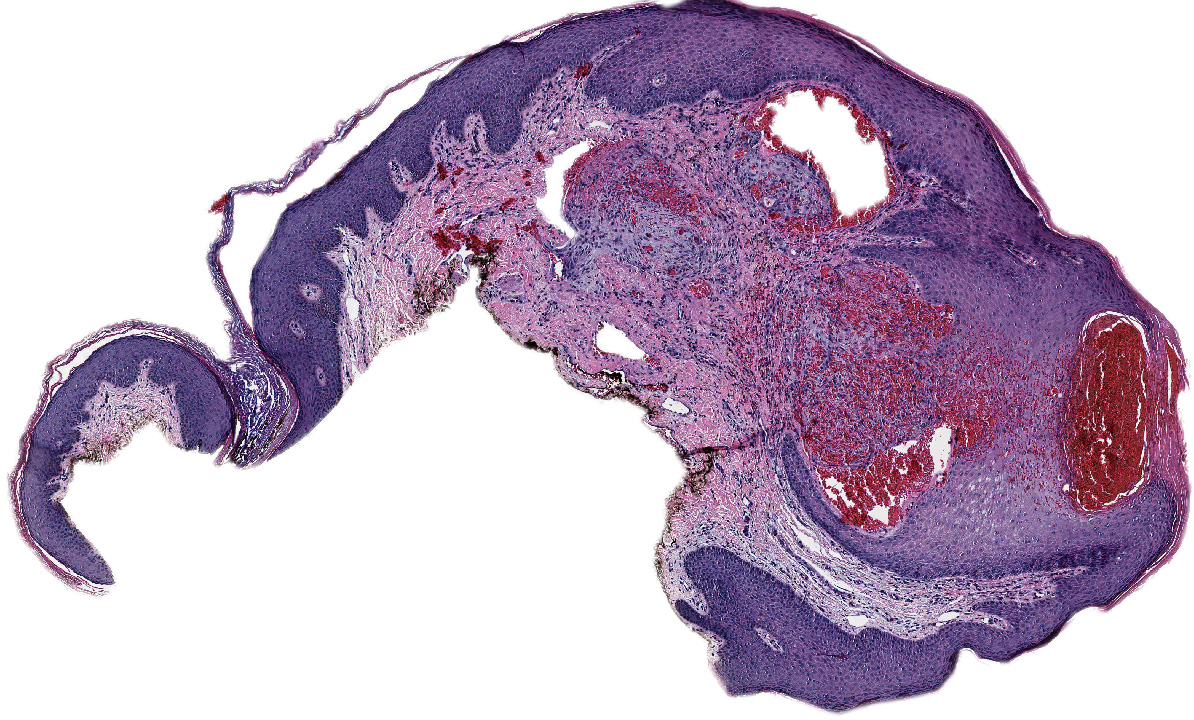
Microscopic (histologic) images
Positive stains
- HPV associated vulvar intraepithelial neoplasia: diffuse, block-like p16 expression as opposed to patchy expression in pigmented condylomata acuminata; wild type p53 expression (Adv Anat Pathol 2006;13:8)
- HPV independent differentiated vulvar intraepithelial neoplasia: aberrant p53 expression, negative or focal to patchy p16 expression (Int J Gynecol Pathol 2008;27:591)
- Basal cell carcinoma: BCL2 and BerEP4 expression in tumor cells (Mod Pathol 2013;26:1382, Clin Cancer Res 2015;21:1289, Arch Dermatol 2003;139:643)
- Melanocytic markers (Arch Med Res 2020;51:827)
- MelanA / MART1 may help highlighting fused nests in nevi
- HMB45 (Semin Diagn Pathol 2022;39:239)
- In common junctional and compound nevi, expressed in melanocytes at dermal epidermal junction
- Highlights maturation (zonation) pattern (diminished or loss of expression from top to bottom)
- Highly variable in Spitz and congenital nevi
- SOX10 highlights junctional melanocytes to help differentiate melanoma in situ from benign counterparts
- Ki67 rate should be low in the dermal component of genital nevi
Negative stains
- HMB45 is commonly negative in intradermal and compound nevi
- PRAME (preferentially expressed antigen in melanoma) is typically lost in nevi (J Cutan Pathol 2020;47:1123)
Videos
Angiokeratoma by Filip Sokol
Angiokeratoma by Pathology mini tutorials
Atypical nevi and nevi of special sites by Dr. Phillip McKee
Sample pathology report
- Vulva, labium majus, biopsy:
- Angiokeratoma
- Vulva, biopsy:
- Melanocytic macule
- Vulva, left, biopsy:
- Intradermal nevus
- Vulva, labium minus, biopsy:
- Blue nevus
- Vulva, labia minora, biopsy:
- Atypical melanocytic nevus of the genital type, compound pattern
Differential diagnosis
- Melanoma:
- Atypical melanocytes in epidermis as single cells or forming nests with pagetoid spread
- Dermal component shows no maturation with cells forming sheets, nests, cords, single cells and rarely fascicles
- S100, SOX10 and NGFR (nerve growth factor receptor) are the most sensitive markers in visualization of invasive growth
- PRAME shows diffuse staining
- Pigmented epithelioid melanocytoma (PEM) of vulva:
- PEM family consists of multiple, usually slow growing, distinct histologic melanocytic entities with potential to metastasize but with a better prognosis than melanoma (WHO 5th edition)
- Infiltrative deep dermal tumor that may involve subcutis
- Hypercellular tumor with cells ranging from medium sized epithelioid cells to large epithelioid cells and spindled cells
- Low mitotic activity
- PRKAR1A loss in 67% of PEMs (Am J Surg Pathol 2017;41:1333, Am J Surg Pathol 2019;43:480)
- Kaposi sarcoma:
- Associated with HIV / AIDS
- Increased number of anastomosing vascular channels in reticular dermis
- Promontory sign is rarely present: protrusion of native vessels into the lumen of dilated vascular neoplastic channels
- Infiltrative spindle cells with eccrine gland destruction
- Hemorrhage, extravasated erythrocytes and plasma cells are commonly present
- Nuclear HHV8 / LANA1 is positive in all cases of Kaposi sarcoma
- Pigmented fibroadenoma:
- Well circumscribed
- Uniformly paucicellular stroma surrounding epithelial component
- Focal intraluminal polypoid projections and cystic changes may be seen
- Pancytokeratin AE1 / AE3, CK7, estrogen and progesterone receptors (epithelial component)
- Purpura:
- Dilated superficial capillaries with extravasation of blood into the dermis
- Chronic forms may show hemosiderin laden macrophages and pigment incontinence in adjacent superficial dermis
Additional references
- Am J Surg Pathol 1995;19:792, Dermatol Surg 2004;30:1118, J Cutan Pathol 2005;32:40, J Cutan Pathol 2008;35:889, Ackerman: Pathology of Malignant Melanoma, 1st Edition, 1981, McKee: Pathology of the Skin - With Clinical Correlations, 3rd Edition, 2005, WHO Classification of Tumours Editorial Board: Skin Tumours, 5th Edition, 2023
Board review style question #1
A 19 year old patient presented with a 1.2 cm dark brown to black papule with irregular borders on the left labia minora. Histologic examination showed nearly contiguous large oval nests with striking atypia, nearly obscuring the dermal epidermal junction. What would be the most concerning feature?
- Adnexal spread
- Dense fibrosis in papillary dermis
- Lack of a mature dermal component
- Pagetoid spread to granular layer in the center of the lesion
Board review style answer #1
C. Lack of a mature dermal component. Atypical melanocytic nevus of genital type is usually a symmetric, well delineated lesion that can be associated with a common dermal component. Answers B and D are incorrect because atypical melanocytic nevus is characterized by dense fibrosis in the papillary dermis and focal pagetoid spread to the granular layer is usually present in the center of the lesion. Answer A is incorrect because adnexal spread and mature dermal component are also common features of atypical melanocytic nevus of genital type. Hence, the lack of maturation is the most concerning feature in this patient.
Comment Here
Reference: Pigmented lesions-vulva
Comment Here
Reference: Pigmented lesions-vulva
Board review style question #2
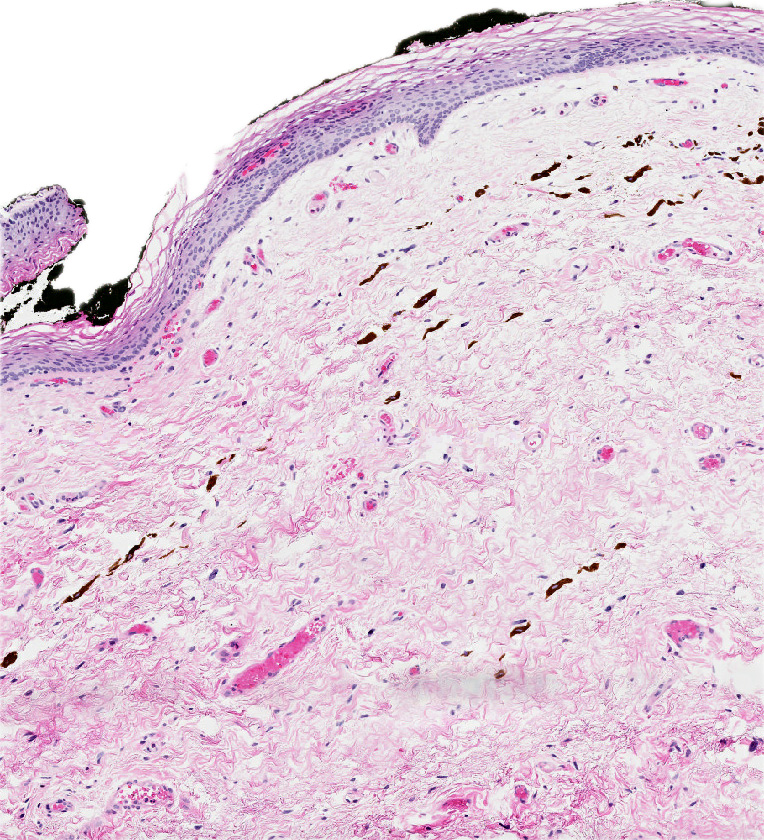
A 65 year old woman presented with a dark brown macule with irregular borders measuring 0.7 cm in the largest dimension, located at the mucosal junction of right labia majora (left image). Shave biopsy is shown (right image). Which of the following is true for this patient's condition?
- HPV test will help to diagnose the lesion
- p63 will highlight neoplastic cells
- PRAME will highlight an in situ component
- SOX10 may demonstrate slight increase in density of the isolated melanocytes at the dermal - epidermal junction
Board review style answer #2
D. SOX10 may demonstrate a slight increase in density of isolated melanocytes at the dermal epidermal junction. Melanocytic macules with hyperpigmentation in basal keratinocytes may show a slight increase in melanocytes at the dermal - epidermal junction, with no confluence. Hence, SOX10 may demonstrate a slight increase in density of isolated melanocytes at the dermal - epidermal junction. Answer C is incorrect because PRAME is typically positive in melanoma. Answer B is incorrect because p63 is positive in squamous epithelial cells. Answer A is incorrect because pigmented HPV associated lesions demonstrate koilocytic changes, hyperplastic squamous epithelium and a lack of basal layer maturation.
Comment Here
Reference: Pigmented lesions-vulva
Comment Here
Reference: Pigmented lesions-vulva