Primary Authors: Annalise Lang, Vi Dinh; Co-authors: Jessica Ahn, Jade Deschamps, Satchel Genobaga, Victor Lee, Reed Krause, Devin Tooma, Seth White. Oversight, Review, and Final Edits by Vi Dinh (POCUS 101 Editor).
Gynecologic and pelvic complaints are common in the clinical settings and can be a result of many causes such as fibroids, adnexal masses, pregnancy, ovarian cysts, ovarian torsion, pelvic inflammatory disease, etc.
Ultrasound is a first-line imaging study for several gynecologic pathologies, so point-of-care ultrasound (POCUS) is a perfect tool to quickly and easily narrow down your differential diagnosis. Other potential benefits of POCUS to your patients include shortening the time before gynecologic consultation (Alonso et al., 2020) and decreasing the length-of-stay of patients in the Emergency Department (Wilson et al., 2016).
We’ll walk you through the steps of how to perform gynecology/pelvic ultrasound using transabdominal and transvaginal approaches. Lastly, we will take a look at several of the main gynecologic pathologies.
By the end of this post, you will be able to use Gynecology/Pelvic Ultrasound to:
- Identify indications for pelvic ultrasound evaluation
- Perform a pelvic ultrasound exam using Transabdominal and Transvaginal techniques
- Evaluate patients for common gynecologic pathologies using ultrasound
- Identify emergent gynecologic cases requiring referral
This post will focus on covering point of care ultrasound (POCUS) pelvic applications of the non-pregnant patient. We cover Obstetric/OB Ultrasound in a different post which you can read HERE.
Table of Contents
Indications/Contraindications
Gynecology/Pelvic Ultrasound Indications
- Pelvic pain
- Dysmenorrhea/Amenorrhea
- Menorrhagia/Metrorrhagia
- Prepubertal/postmenopausal bleeding
- Signs/symptoms of pelvic infection
- Localization of intrauterine contraceptive device
- Screening for malignancy
Gynecology/Pelvic Ultrasound Contraindications
The following contraindications apply only to transvaginal ultrasound.
- Pediatric age
- Premature rupture of membranes
- Bleeding associated with known placenta previa
Transabdominal Pelvic Ultrasound Protocol
Transabdominal Pelvic Ultrasound can detect most larger abnormalities such as large fibroids, ovarian cysts, neoplasms, etc. However, its views may be limited by abdominal structures such as bowel gas.
In general for POCUS exams, it is usually good to start with the transabdominal ultrasound and then use the transvaginal approach if needed.
Patient Preparation
- Supine
- Full bladder (if possible)
Ultrasound Machine Preparation
- Transducer: Curvilinear Ultrasound Probe (Ideal Choice) or Phased Array Probe.
- Preset: Pelvic or Abdomen
- Machine Placement: Position the ultrasound machine on the right side of the patient with the screen facing you. With this configuration you can face both the patient and the ultrasound screen, scanning with your right hand and manipulating buttons on the machine with the left hand.

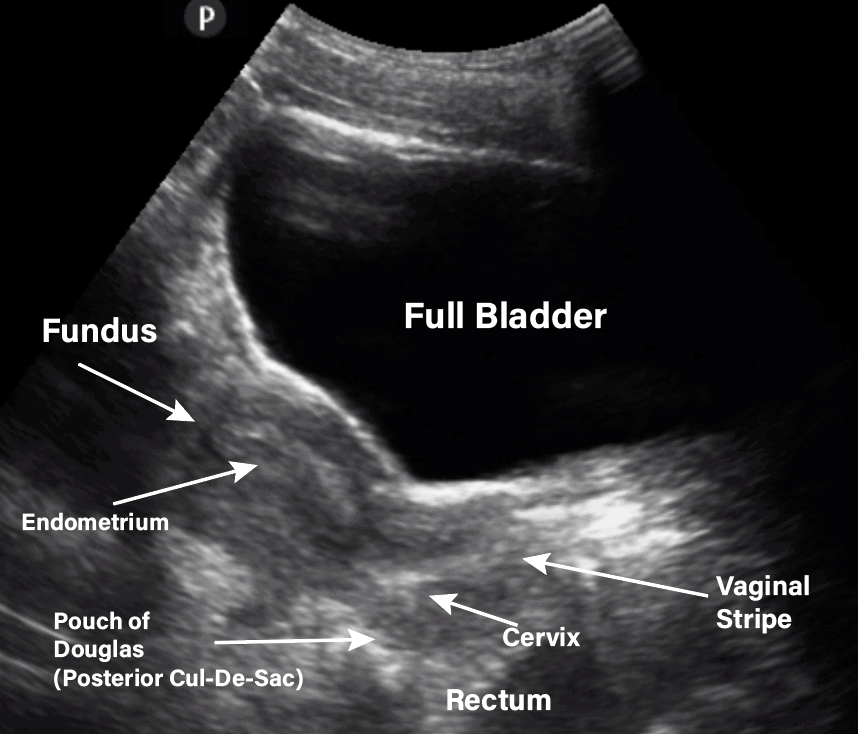
Step 1: Obtain Sagittal/Longitudinal View of Uterus
The sagittal view of the uterus is also known as the longitudinal view on ultrasound.
- Position the curvilinear probe with the probe indicator toward the patient’s head along the midline of the patient’s abdomen in the suprapubic area.
Identify the following structures:
- Bladder (use as acoustic window)
- Uterine fundus
- Uterine body
- Endometrial Stripe
- Cervix
- Vagina
- Posterior Cul-de-Sac (Pouch of Douglas)
- Rectum
- You may see Nabothian cysts (small, anechoic/hypoechoic circular structures on the cervix) on ultrasound. Nabothian cysts are usually considered benign findings and can occur in about 12% of the population (Fogel 1982).
Here is an pelvic ultrasound video we made showing you the sagittal/longitudinal view:
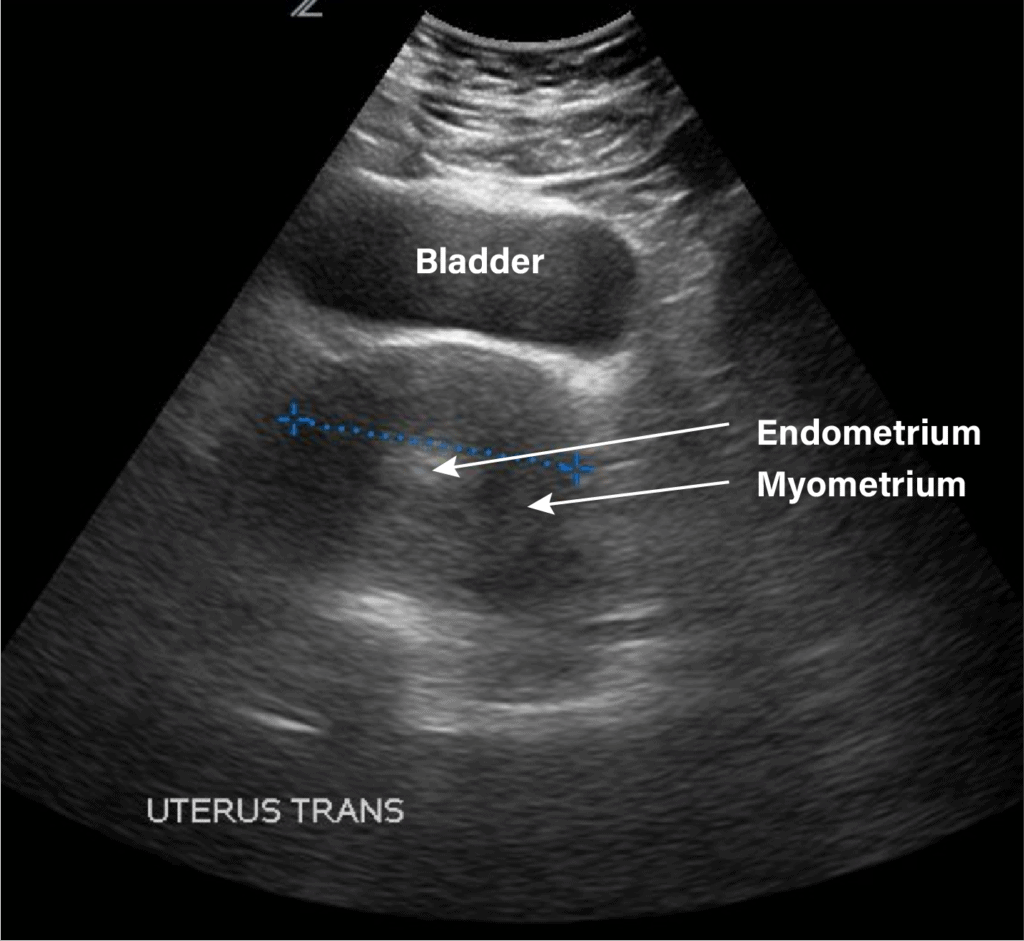
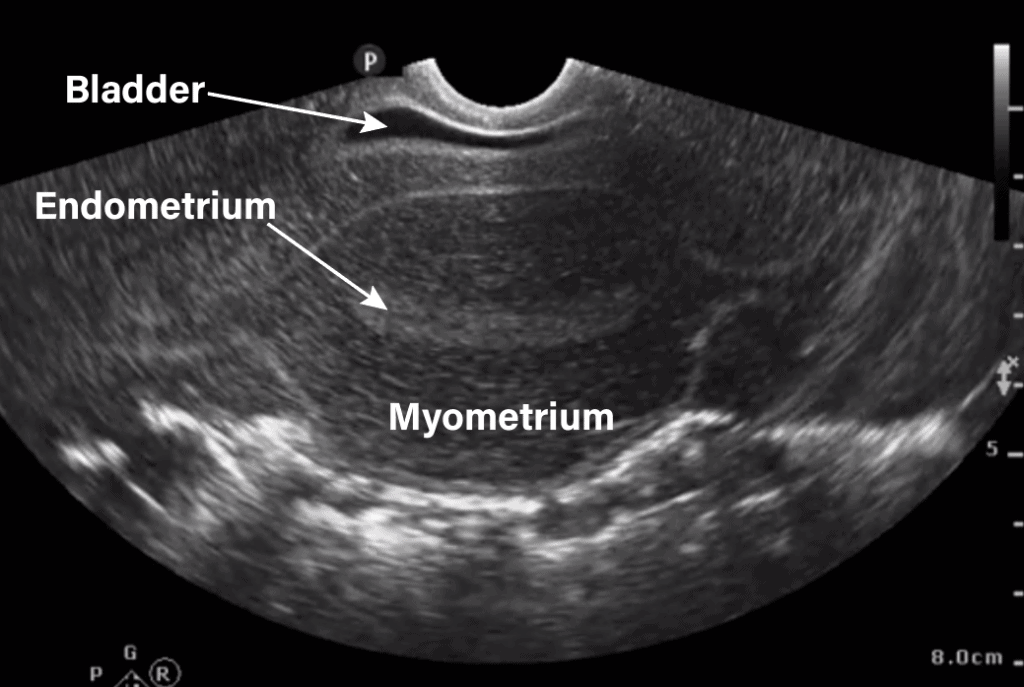
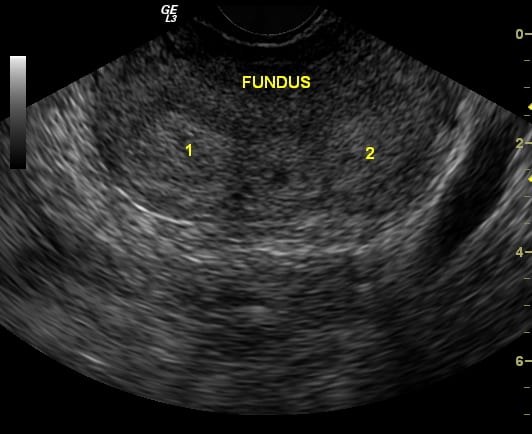
Step 2: Obtain Transverse View of Uterus
- Rotate the probe 90 degrees counterclockwise with the indicator towards the patient’s right.
- Obtain a good view of the fundus of the uterus as well as the endometrium and myometrium.
- Tilt/fan your probe through the entire uterus in the transverse view.
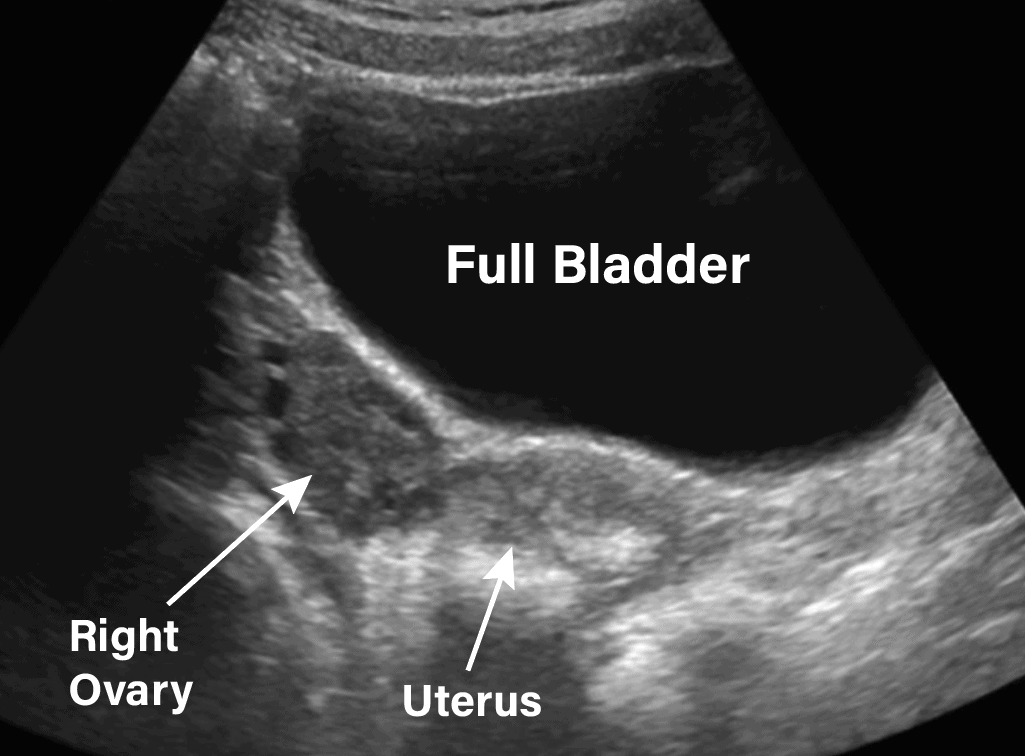
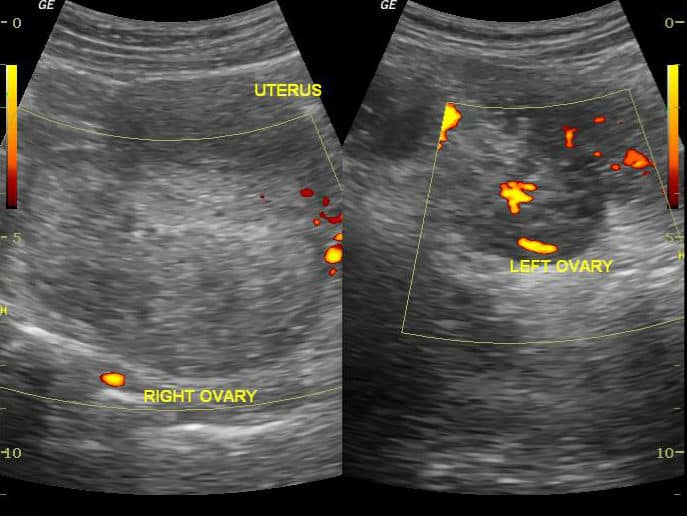
Step 3: Obtain View of Ovaries
The ovaries can be difficult to find because of the overlying bowel gas. Having a full bladder can help visualize the ovaries in a transabdominal view since the bladder can be used as an acoustic window. For the most part, transvaginal ultrasound should be used to evaluate the ovaries.
- With the probe still in the transverse position, rock the tail of the probe to the patient’s left to visualize the right ovary.
- You can visualize the left ovary using a similar technique (rock the tail of the probe to the patient’s right).
An ovary can be identified on ultrasound by the following characteristics:
- Lateral and/or posterior to the uterus
- Typically measures 2-3 cm in diameter
- Less echogenic than surrounding tissue
- Static (compared to surrounding bowel)
- Anechoic follicular structures
Transvaginal Pelvic Ultrasound Protocol
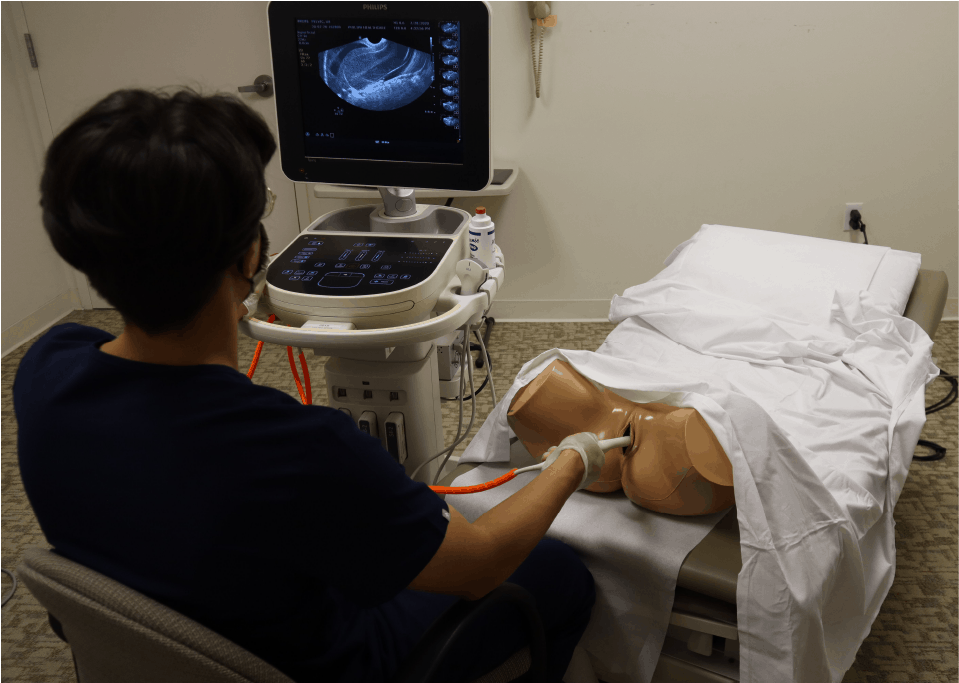
Transvaginal ultrasound gives the best resolution and visualization of the female pelvic structures. However, it is considered more invasive than the transabdominal approach.
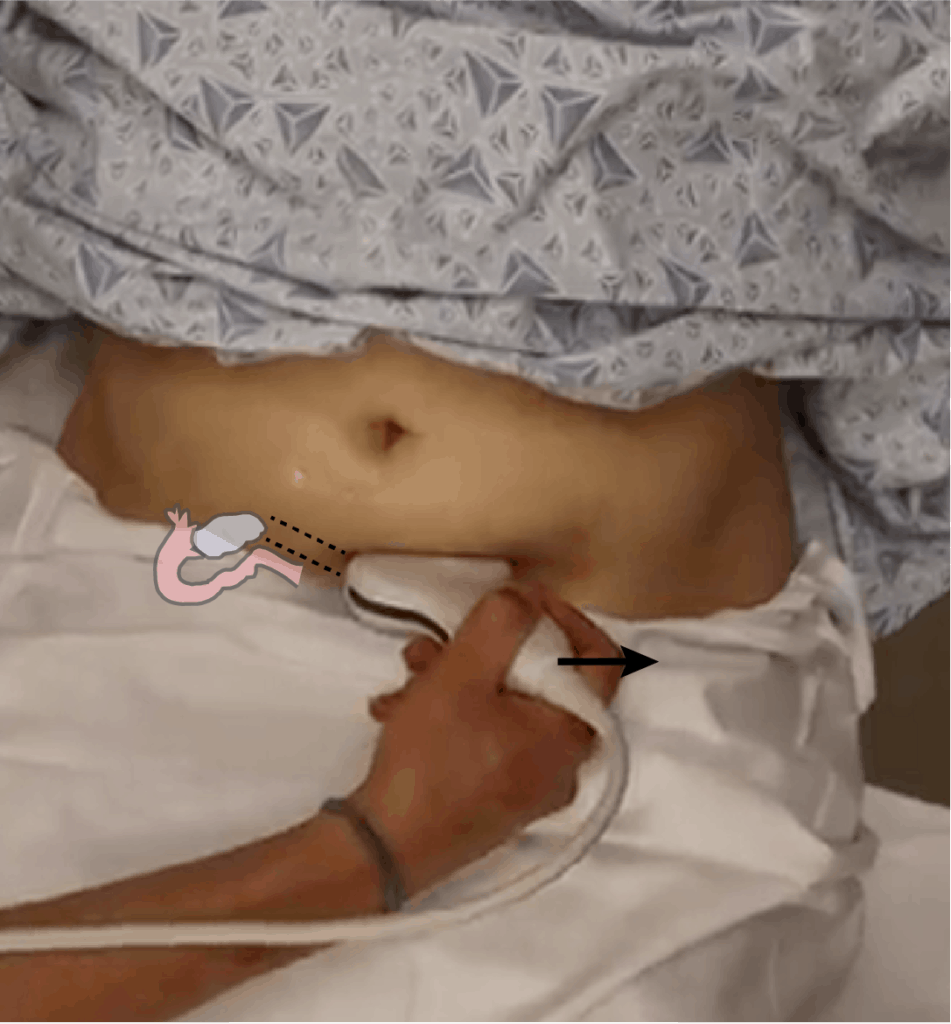
Patient Preparation
- Dorsal Lithotomy position. Make sure to have a drape/sheet and cover the patient properly. Position them similarly to how you would perform a normal pelvic exam.
- Empty bladder (if possible)
- Have a chaperone present in the room with you.
Ultrasound Machine Preparation
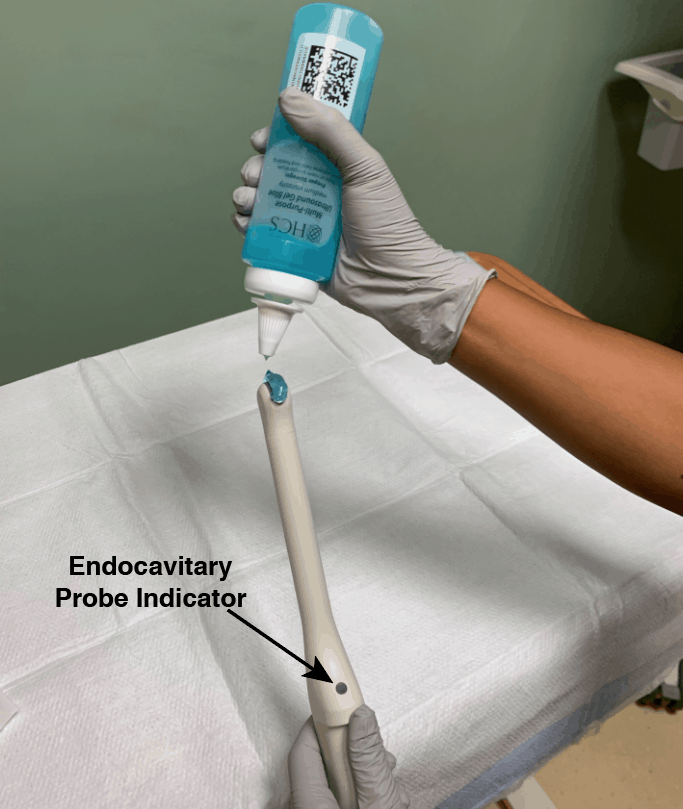
- Transducer: Transvaginal/Endocavitary probe.
- Preset: Gyn/Pelvic
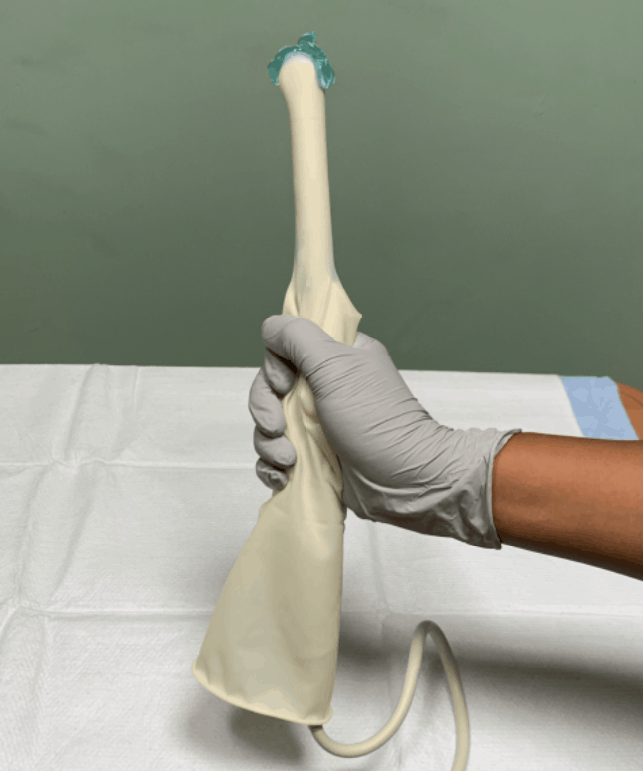
- Will also need a sterile condom (or sterile glove) and sterile gel.
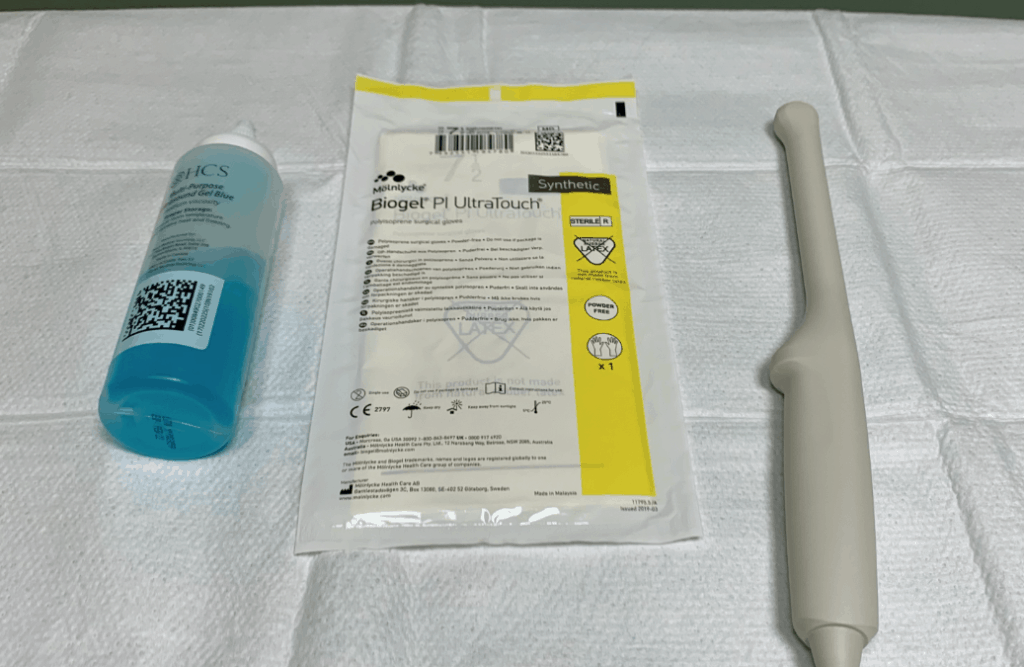
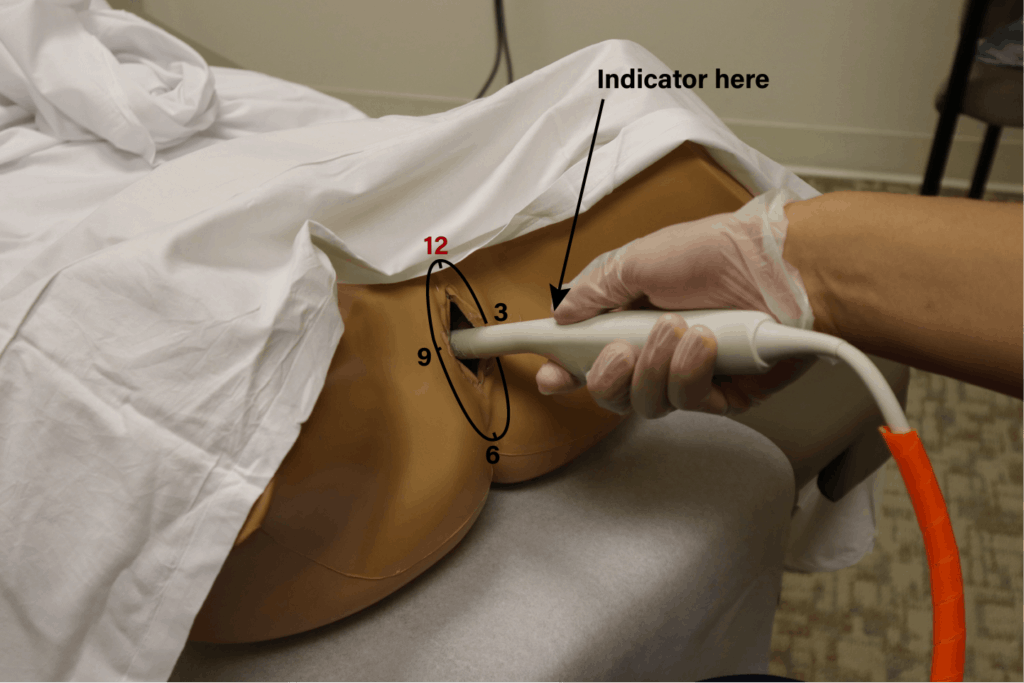
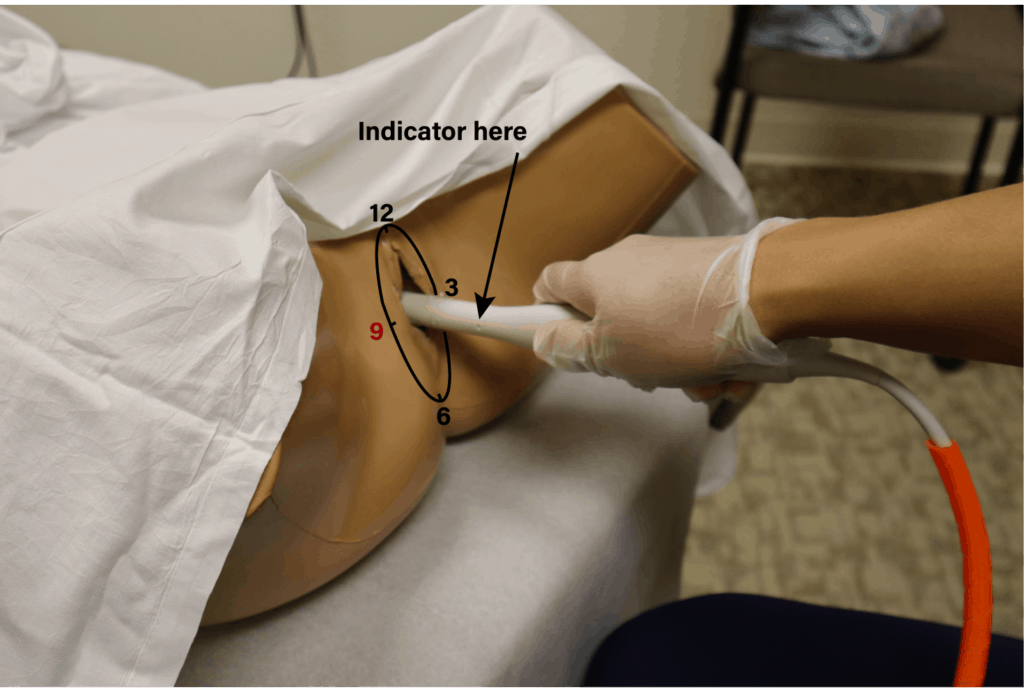
- The indicator is located at the 12 o’clock position of the probe.
- Place gel at the tip of the endocavitary probe.
- Apply sterile glove or sterile condom over the endocavitary probe
- Apply sterile gel to the tip of the covered endocavitary probe.
- Machine Positioning: Position the ultrasound machine on the right side of the patient with the screen facing you. With this configuration you can face both the patient and the ultrasound screen, scanning with your right hand and manipulating buttons on the machine with the other hand. Also position a chair at the foot of the bed to sit in while performing the scan.
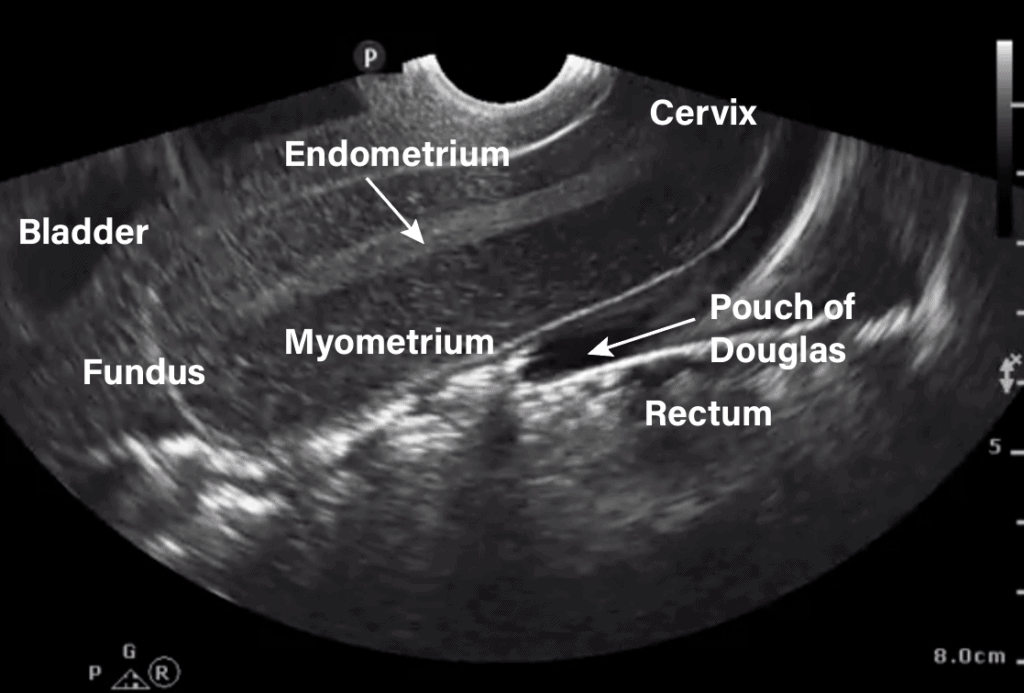
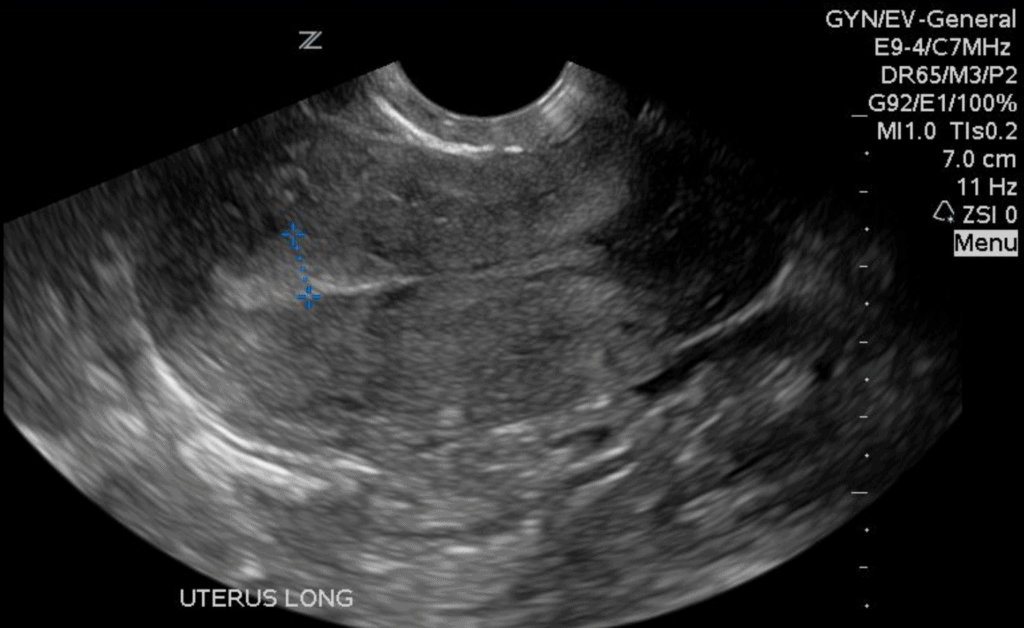
Step 1: Obtain Sagittal/Longitudinal View of Uterus
- Gently insert the probe into the patient’s vagina with the indicator at 12 o’clock (toward the ceiling).
POCUS 101 Tip: Aligning your thumb with the probe indicator helps you know the exact orientation of the probe despite any manipulation you do throughout the exam.
- Keep an eye on the ultrasound monitor as you insert the probe because the depth of insertion will vary depending on patient anatomy. The goal is to orient the hyperechoic endometrial stripe in the center of the image.
- Tilt/Fan your probe to medially and laterally to visualize the entire uterus in the sagittal/longitudinal view.
Identify the following structures:
- Bladder
- Uterine fundus
- Endometrium/Endometrial stripe
- Myometrium
- Cervix
- Pouch of Douglas (Posterior cul-de-sac)
- Rectum
Step 2: Obtain Transverse View of Uterus
- Rotate the probe 90 degrees counterclockwise (toward the patient’s right, or the 9 o’clock position) to obtain a good view of the bladder, myometrium, and endometrium of the uterus. Tilt/Fan superiorly and inferiorly to view then entire uterus in the transverse view.
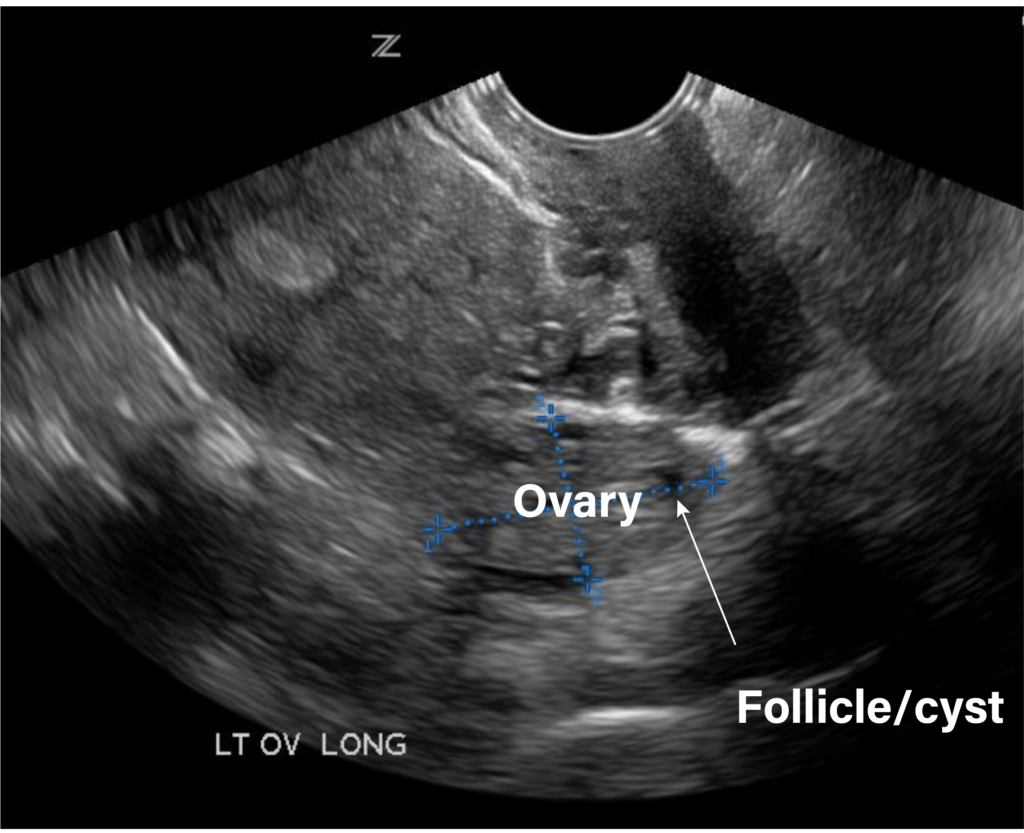
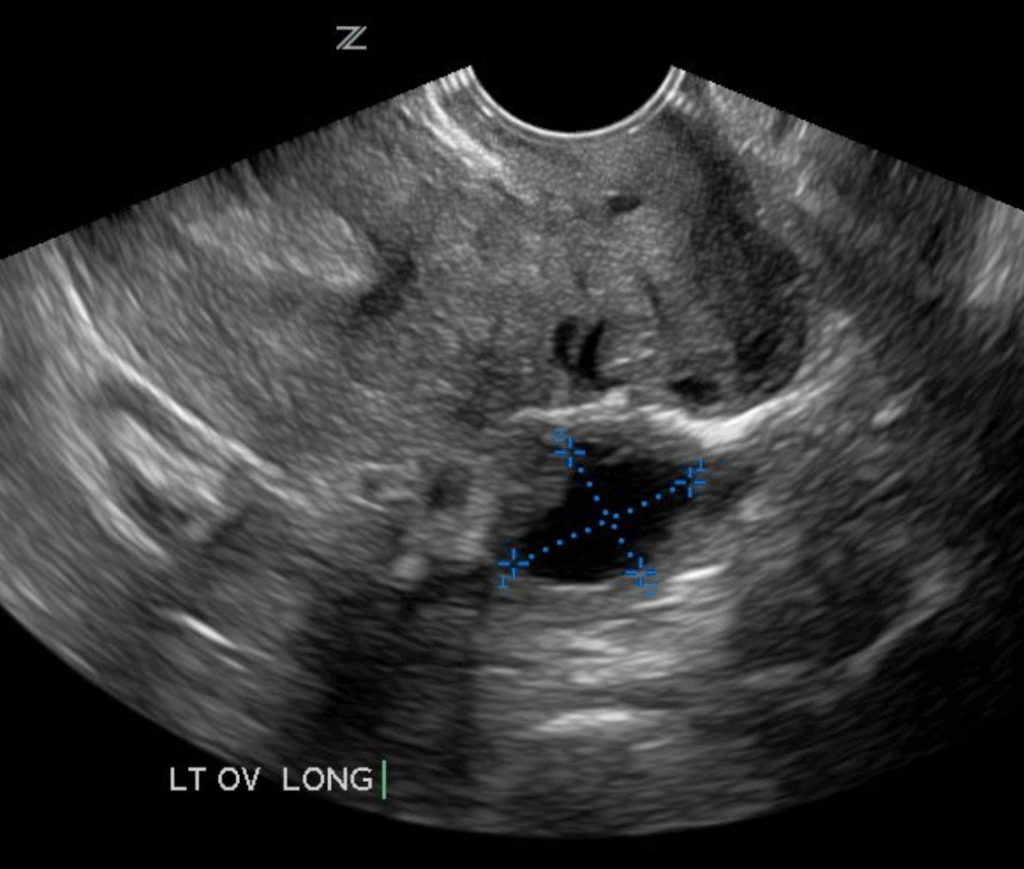
Step 3: Obtain View of Ovaries
In general, you can use either a sagittal or transverse view to identify the ovaries, which are usually located lateral and/or posterior to the uterus (Sohoni 2014).
POCUS 101 Tip: If you have trouble viewing the ovary, try directing the endocavitary probe more posteriorly.
An ovary can be identified on transvaginal ultrasound by the following characteristics:
- Posterior and lateral to uterus
- Typically measures 2-3 cm in diameter
- Less echogenic than surrounding tissue
- Static (compared to surrounding bowel)
- Anechoic follicular structures
Step 4: Disinfect Endocavitary Probe
When you complete your transvaginal ultrasound exam it is imperative that you disinfect the probe properly using your hospital approved process. You can read the American Institute of Ultrasound in Medicine (AIUM) policy for disinfection here.
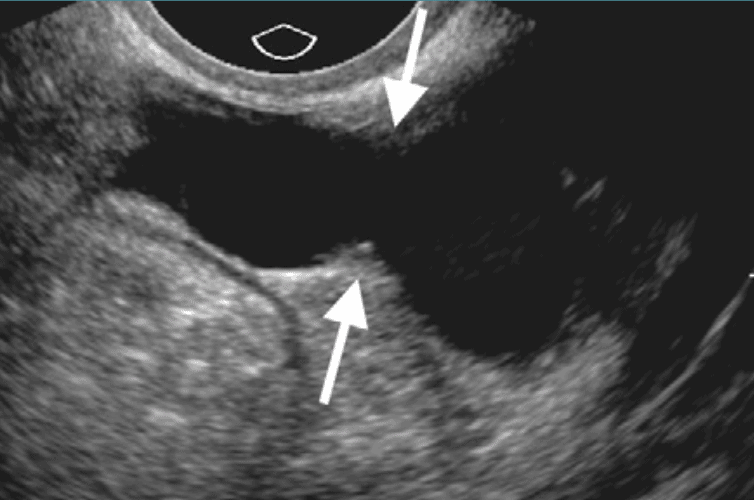
Free Fluid Evaluation with Pelvic Ultrasound
Free fluid is one of the most common findings during pelvic ultrasound. A variety of abdominal and pelvic conditions are associated with free fluid accumulation in the pelvis.
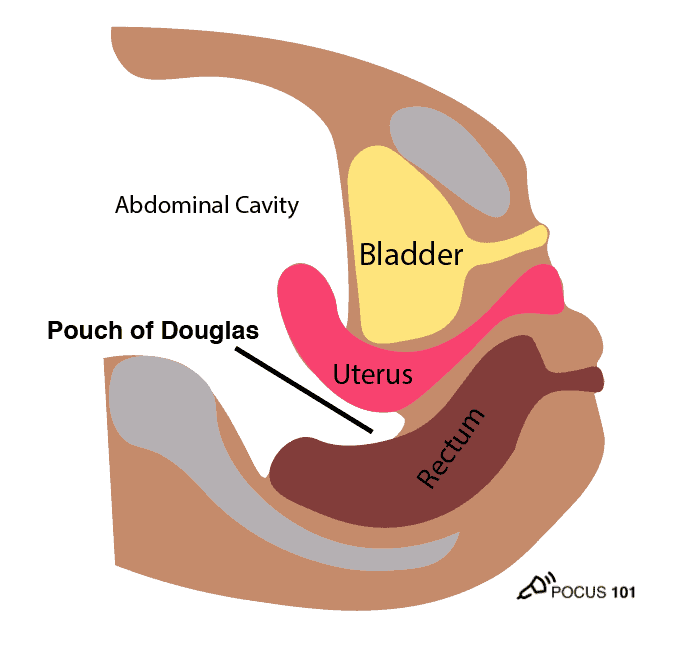
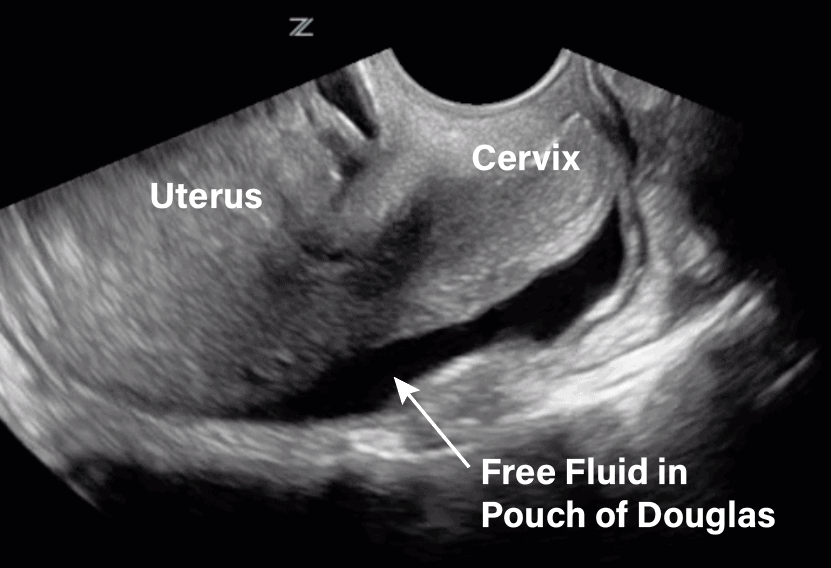
In females, free fluid from the abdominal cavity sinks into the pelvic cavity and settles in the Pouch of Douglas (also called the Posterior Cul-De-Sac and Rectouterine Pouch), located posterior to the uterus and anterior to the rectum. Anechoic fluid in this location can be detected by ultrasound imaging using either the transabdominal or transvaginal approaches.
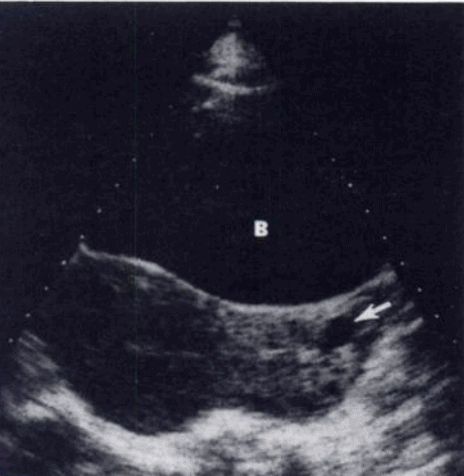
Normal Amount of Pelvic Free Fluid
Small amounts of free fluid in the pelvis (usually <10 mL but up to ~20 mL near ovulation) can be normal in females (Ritchie, 1986; Hall et al., 1979). This is especially true in patients following ovulation, after menopause, or during early pregnancy. Make sure to look for the free fluid in the Pouch of Douglas.
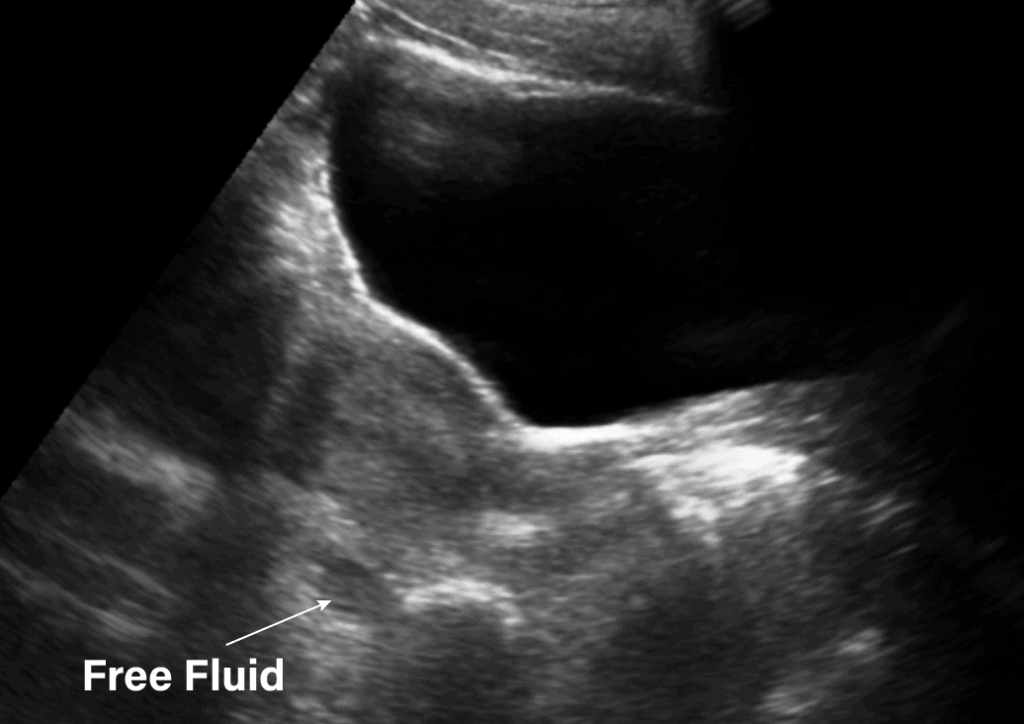
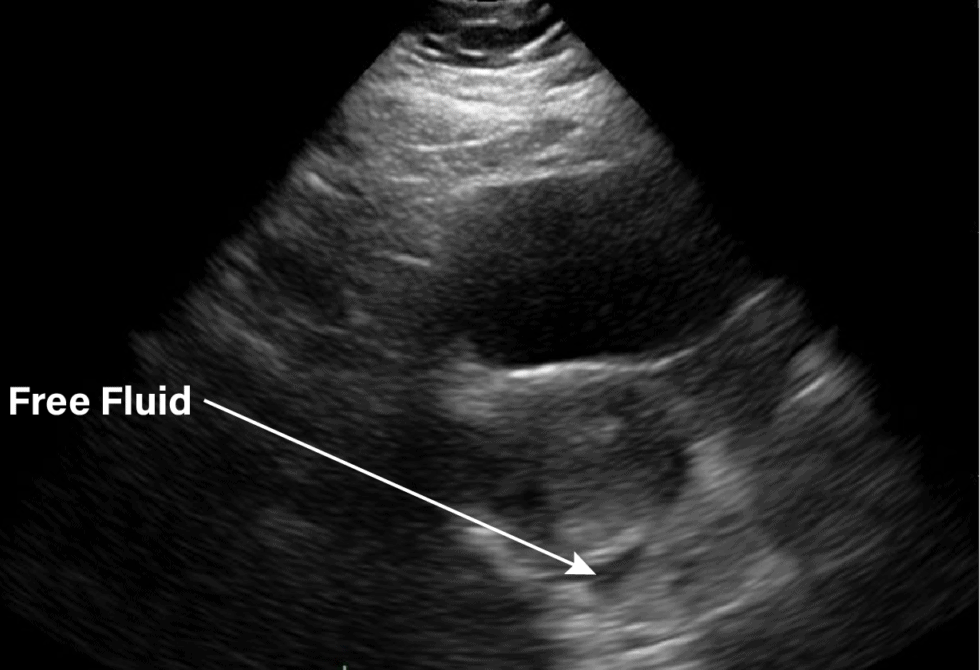
Here are some pelvic ultrasound images of normal amounts of free fluid in the pouch of Douglas.
Abnormal Pelvic Free Fluid
There are several pathologic conditions (both pelvic and non-pelvic) associated with an abnormal buildup of free fluid in the pelvis.
Here is a list of potential pelvic causes of abnormal amounts of free fluid in the Pouch of Douglas:
- Endometriosis
- Malignancy
- Leiomyoma
- Pelvic Inflammatory Disease
- Ectopic Pregnancy
When you do see a significant amount of free fluid in the Pouch of Douglas make sure to check the right upper quadrant (RUQ) in Morison’s Pouch and the left upper quadrant (LUQ) to evaluate for more free fluid. Remember, free fluid can also be due to non-pelvic causes such as liver cirrhosis (alcohol-related or viral), heart failure, renal failure, and trauma. Below are ultrasound images of abdominal free fluid in the left and right upper quadrants.
Uterine Ultrasound Pathology
Uterine abnormalities are a common cause of pelvic complaints that can be detected well using Point-of-Care Ultrasound. You may especially want to assess for uterine pathologies if uterine measurements are larger than the normals indicated in the chart below (Nalaboff 2001; Ozcan & DeCherney, 2019).
| Normal (nulliparous) | Normal (parous) | |
| Length (cm) | 6-8.5 | 8-10.5 |
| Depth (cm) | 2-4 | 4-6 |
| Width (cm) | 3-5 | 4-6 |
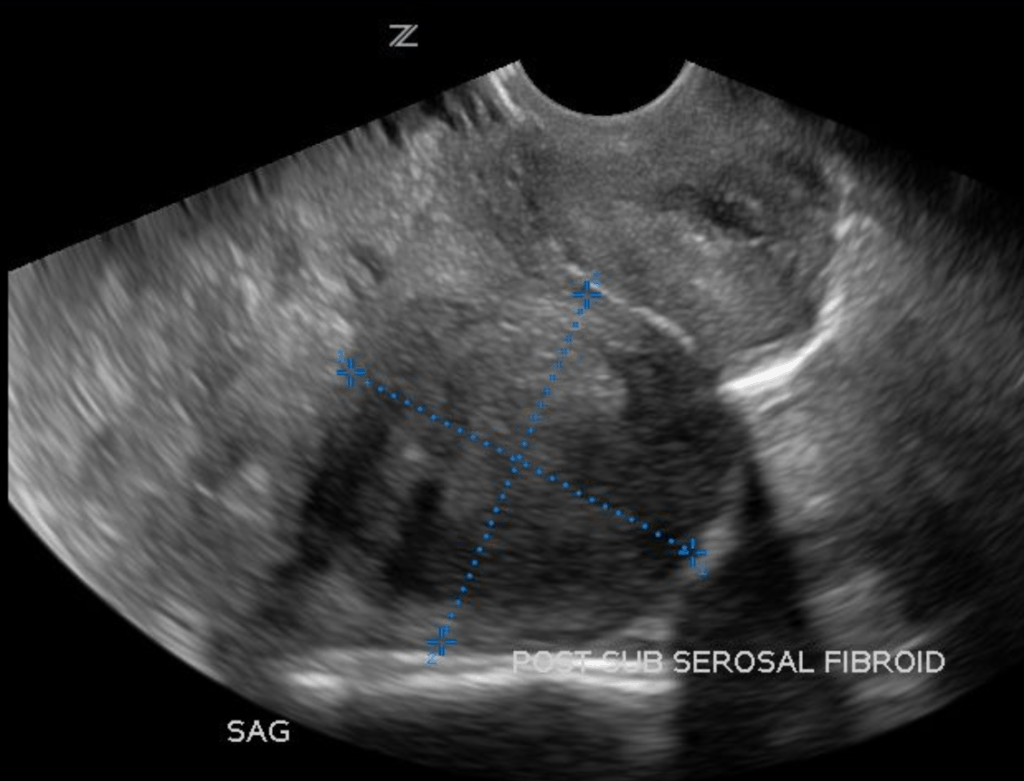
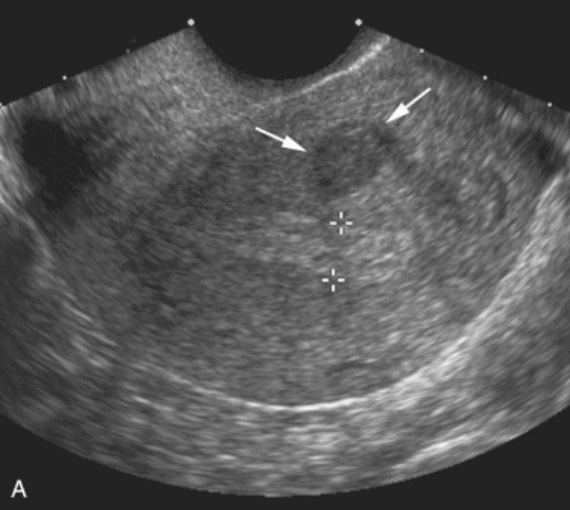
Fibroids (Leiomyomas)
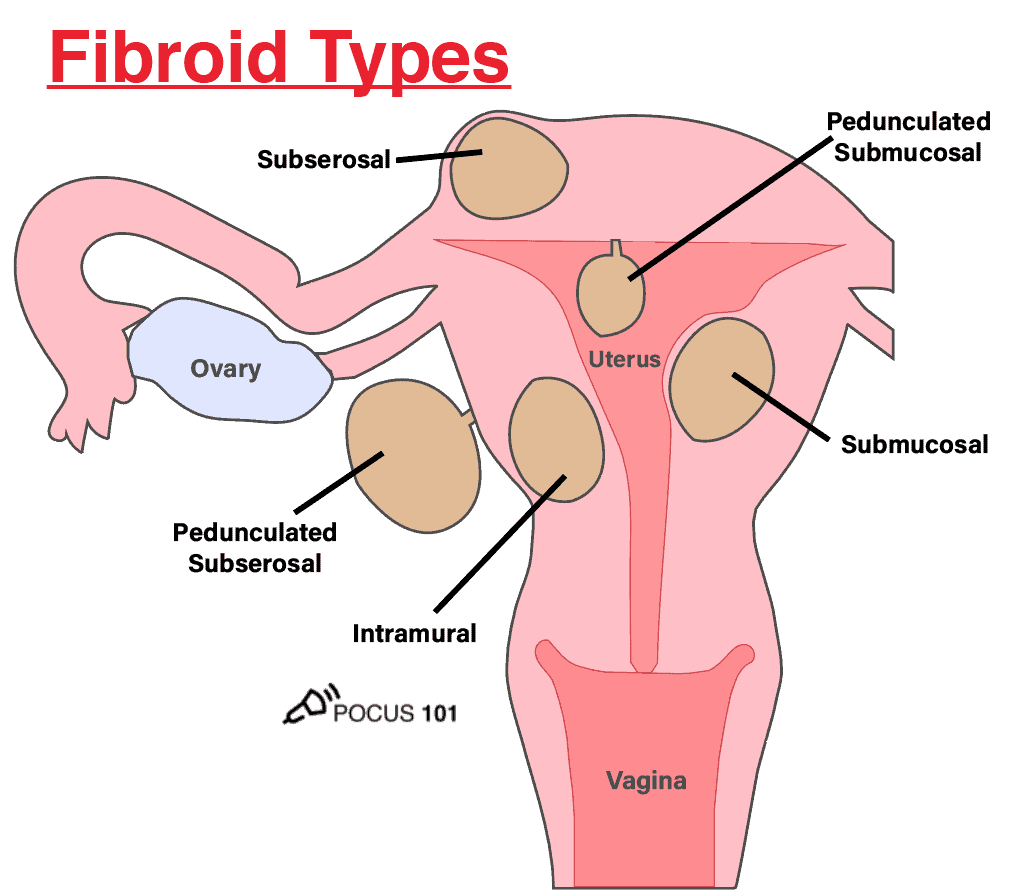
Fibroids are the most common type of benign uterine neoplasm. These estrogen-dependent tumors can arise in a variety of locations within the smooth muscle layer of the uterus and therefore produce a spectrum of symptoms depending on the size and location of the mass.
Most patients with fibroids are asymptomatic but may experience abnormal uterine bleeding or infertility. Association of fibroids with severe pain or uterine bleeding warrants referral to gynecology.
The different types of fibroids you may encounter on pelvic ultrasound are illustrated below:
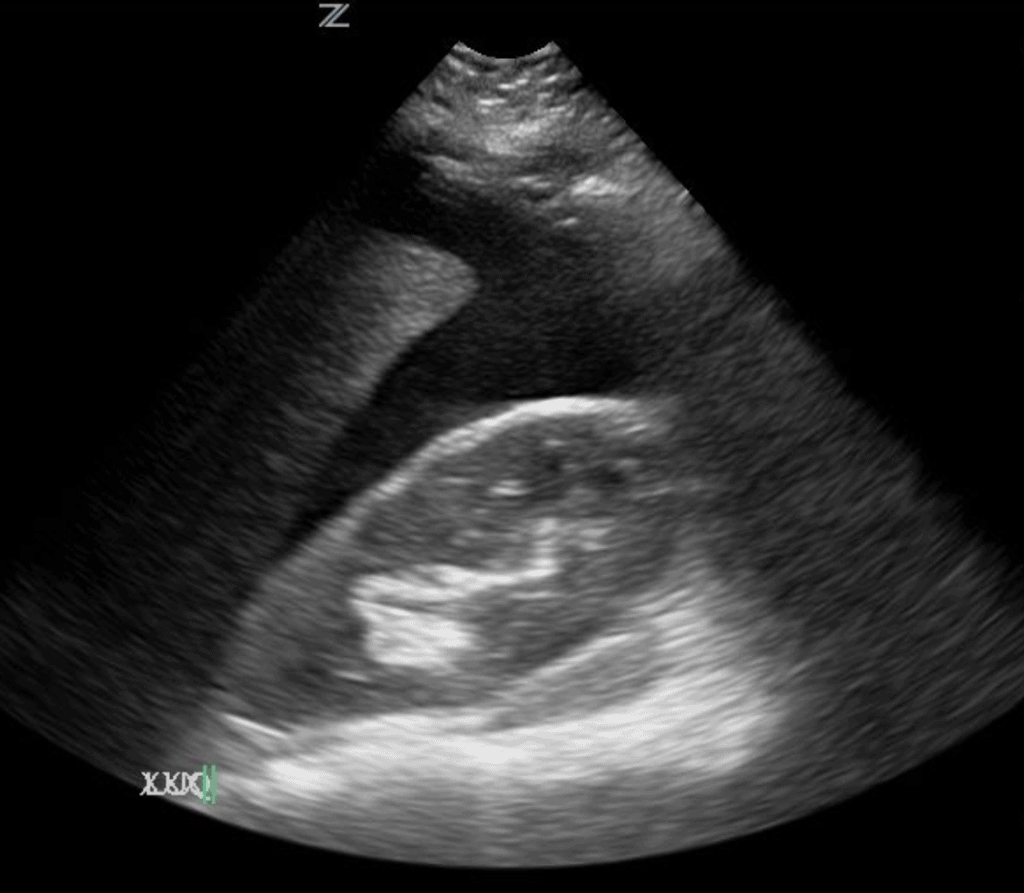
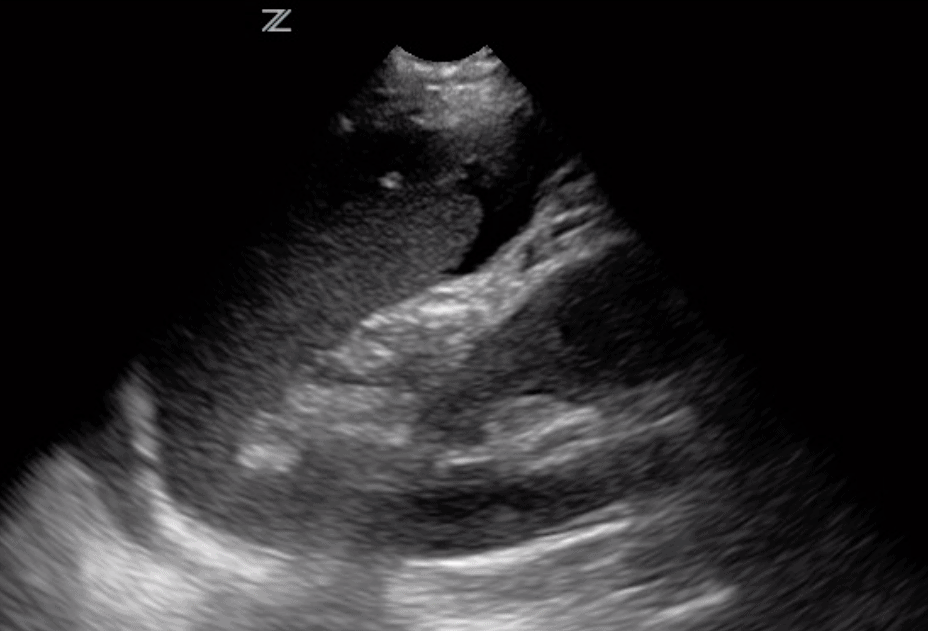
Ultrasound findings of Fibroids (Leiomyomas)
On ultrasound imaging, the presence of fibroids can usually be detected by heterogeneous enlargement of the uterus due to the presence of well-demarcated, hypoechoic masses within the myometrium. However, Fibroids may also appear isoechoic or hyperechoic.
Remember to examine all parts of the uterus because fibroids can extend beyond the normal contours of the uterus and may be found outside the myometrium alone.
Submucosal Fibroids
Submucosal fibroids are the most common subclass of fibroids and are located just beneath the endometrium. They may also be attached to the uterus by a small piece of tissue called a pedicle, in which case they are classified as pedunculated submucosal fibroids. Patients with submucosal fibroids may present with infertility and uterine bleeding as these tumors grow into the uterine cavity.
Subserosal Fibroids
Subserosal fibroids grow off the surface of the uterus and can extend to impinge on surrounding pelvic structures. Pedunculated subserosal fibroids are also possible.
Intramural Fibroids
Intramural fibroids are another common subclass of leiomyomas but are rarely symptomatic because they grow entirely within the myometrium of the uterus.
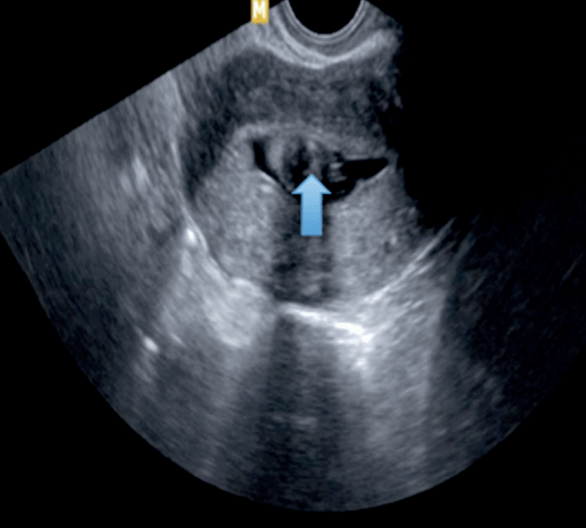
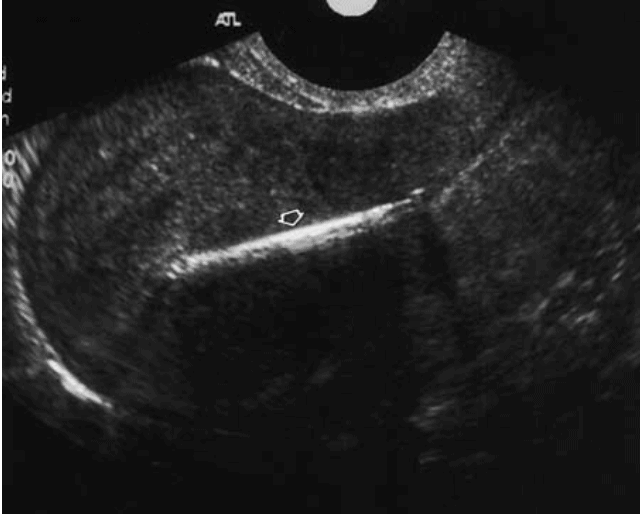
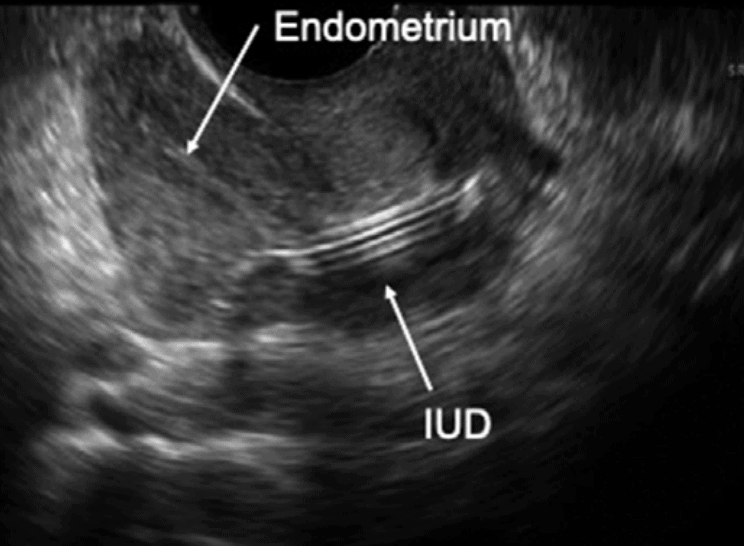
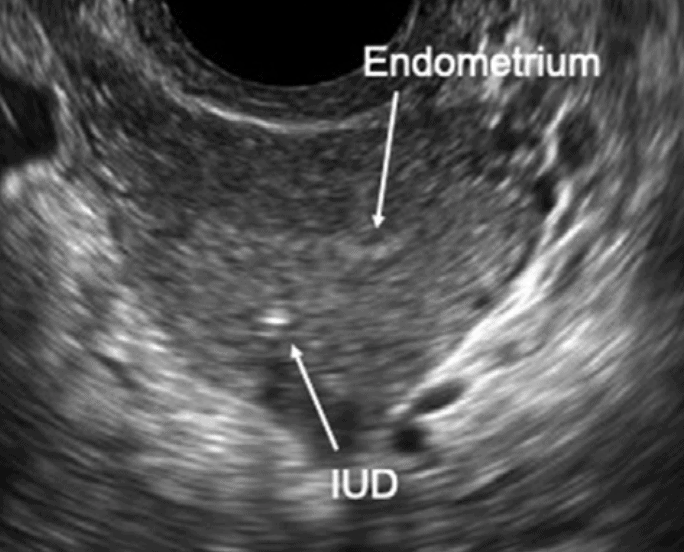
Intrauterine Device (IUD) Malplacement
An Intrauterine Device (IUD) is a birth control device identifiable on ultrasound as a hyperechoic structure exhibiting posterior shadowing and located within the uterine/endometrial cavity. Ultrasound can be used to confirm the proper placement of an Intrauterine Device (IUD) as well as to detect complications such as perforation, expulsion, or migration of the contraceptive device after insertion.
Endometrial Abnormalities
Measurement of the endometrium can be used to help assess for pathologies such as hyperplasia or neoplasm that may expedite referral to gynecology for further evaluation or biopsy. The table below outlines the normal values for endometrial thickness which generally decreases after menopause (Nalaboff et al., 2001; Ozcan & DeCherney, 2019). (Values may be slightly elevated in postmenopausal patients undergoing hormone replacement or tamoxifen therapy.)
| Normal Endometrial Measurement | |
| Premenopausal | <15 mm |
| Postmenopausal | <5 mm |
Endometrial Hyperplasia and Neoplasm
Endometrial hyperplasia is characterized by a high endometrial gland-to-stroma ratio. Hyperplasia is concerning because it can develop into endometrial neoplasm. Ultrasound assessment of the endometrium can enhance the detection of hyperplasia that may need referral to gynecology for definitive diagnostic biopsy to rule out neoplasm.
Presentation:
- Postmenopausal uterine bleeding
- History of high estrogen states like obesity, pregnancy, estrogen-secreting tumors, polycystic ovarian syndrome, etc.
- Enlarging pelvic mass (neoplasm, especially if rapidly growing in postmenopausal women)
- Pelvic pain
Assess for endometrial hyperplasia on pelvic ultrasound by measuring the endometrial lining.
Concern for endometrial hyperplasia and neoplasm may be raised by the following ultrasound findings:
- Diffuse thickening of the endometrium (Nalaboff et al., 2001):
> 15 mm in premenopausal women
> 5 mm in postmenopausal women - Focal thickening or heterogenous echogenicity of the endometrium (abnormal even if below threshold levels).
- Obscured endometrium-myometrium border in the case of neoplasm (Lobo et al., 2016).
Endometriosis
Endometriosis is defined as the presence of endometrial tissue (stroma or glands) outside the uterus. While several theories on the pathogenesis of endometriosis exist, most expand on Sampson’s theory which attributes endometriosis to retrograde transplantation of menstrual tissue (Nap et al., 2004; Sampson, 1927).
These ectopic lesions may infiltrate several areas of the pelvis including the ovaries, pouch of Douglas, bladder, and rectum. Given the various locations, sizes, and appearance of endometriosis on ultrasound, this pathology is not easily visualized by ultrasound and usually requires laparoscopic diagnosis.
Endometritis
Endometritis is acute or chronic infection of the endometrium due to a handful of causes including pelvic inflammatory disease, retained products of conception after miscarriage or delivery, and IUD placement.
Presentation:
- Fever
- Abnormal uterine bleeding
- Pelvic pain
- Infertility
While ultrasound imaging can be normal in early stages of infection, the following findings can be visualized as the infection progresses.
- Thickened endometrium
- Free fluid in the pelvis
- Increased vascularity (visualize with Doppler)
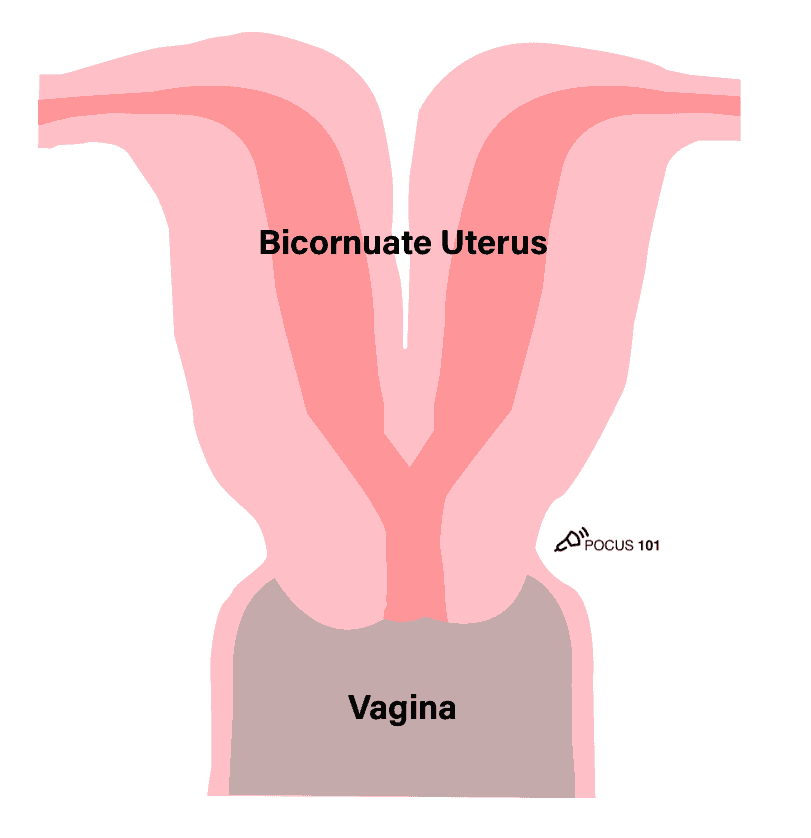
Bicornuate Uterus
Congenital uterine abnormalities such as a Bicornuate Uterus may be seen on pelvic ultrasound as a uterus with two conjoined cavities. The biggest risks of having a Bicornuate Uterus are preterm labor and cervical insufficiency.
Ovarian/Adnexal Pathology
Ovarian Cysts
Ovarian cysts are generally benign and show up on ultrasound in a variety of ways depending on their subtype. A few of the most common types are described below.
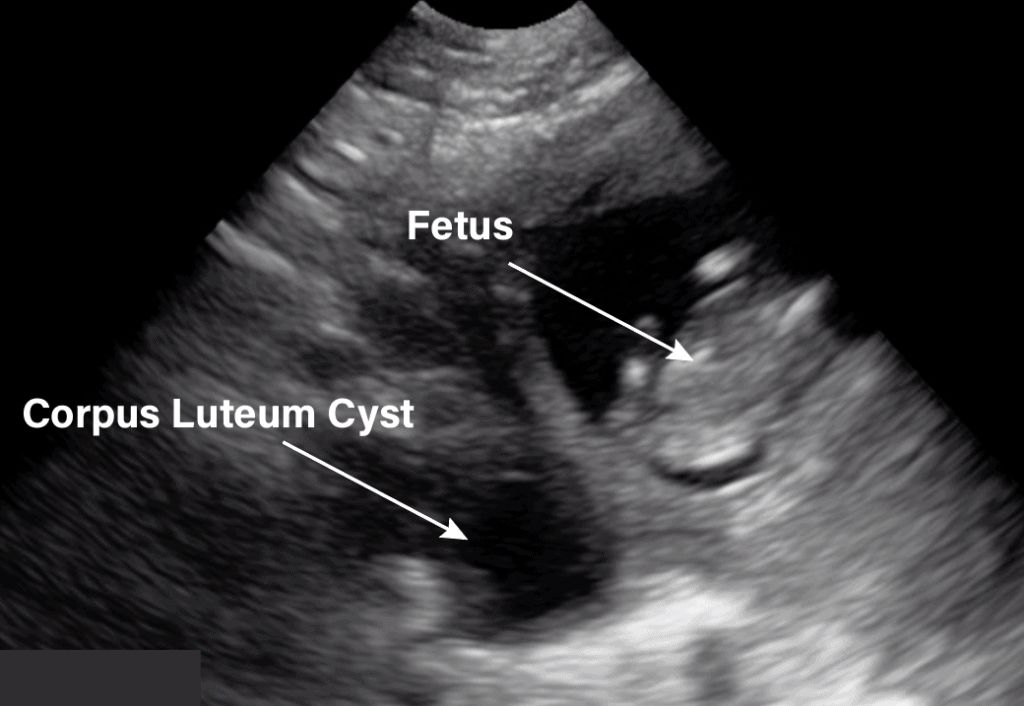
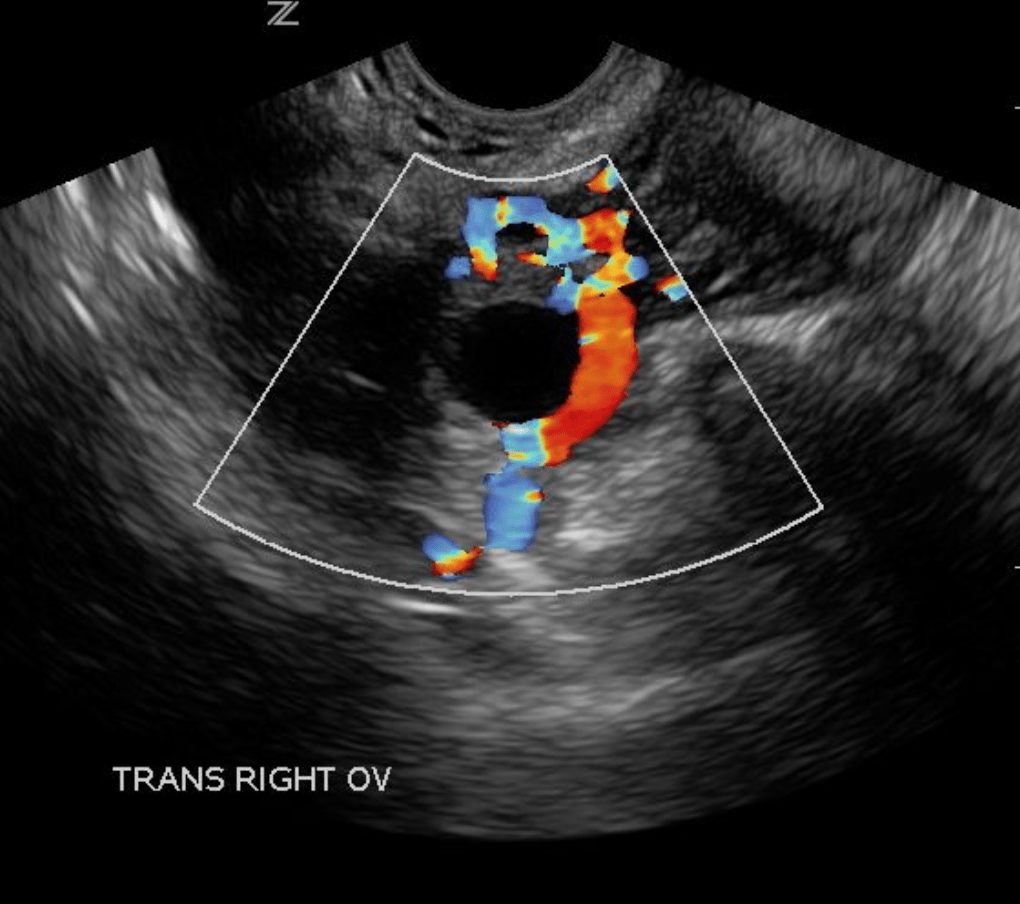
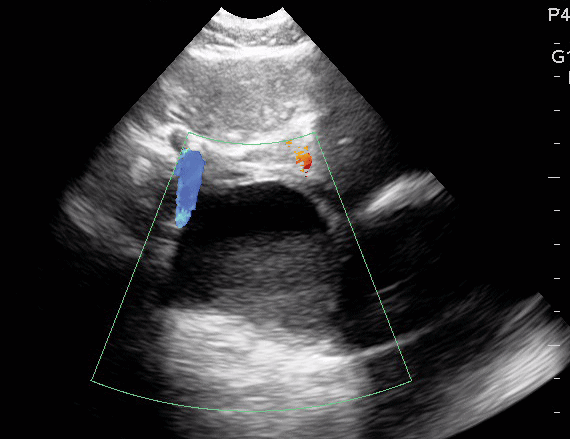
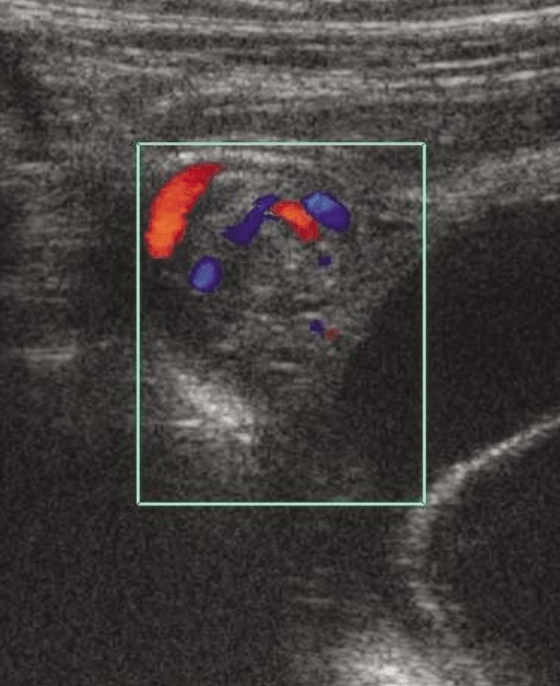
Corpus Luteum Cysts
Corpus Luteum Cysts are a normal part of the menstrual cycle and can enlarge further during pregnancy. These cysts are not usually associated with any significant symptoms unless they become hemorrhagic.
Ultrasound findings of Corpus Luteum Cysts:
- Fluid-filled mass with thick, crenulated (shallowly scalloped, notched) wall
- Internal echoes present
- No internal vascularization
- Possible extensive vascularization of corpus luteum wall on color Doppler – “Ring of Fire Sign” (this sign can also be seen in ectopic pregnancy)
- Usually < 3 cm
Simple Ovarian Cysts
Simple cysts are fluid-filled sacs in the ovary thought to be caused by hormonal imbalances. The majority of simple cysts are benign but should be followed consistently to monitor for changes.
Presentation:
- Often asymptomatic
- Possible bloating
- Possible pelvic/low back pain
Ultrasound findings of Simple Ovarian Cysts:
- Smooth/thin-walled pockets containing anechoic fluid
- Lacking internal vascularization
- Lacking septa
- Exhibiting posterior acoustic enhancement (increased echogenicity posterior to the cyst)
- Should be <5cm for premenopausal and <3cm for postmenopausal patients (if larger than followup may be warranted) – (Andreotti 2019)
Ruptured/Hemorrhagic Cysts
Hemorrhagic cysts are usually seen in premenopausal women and are typically the result of bleeding into an ovarian cyst, follicle, or corpus luteum cyst.
Presentation:
- Acute pelvic, flank, or abdominal pain
- Pelvic mass
- Possibly asymptomatic
Ultrasound findings of Hemorrhagic Cysts:
- Internal echoes with lacy/cobweb appearance (due to fibrin strands)
- Clot with irregular borders and no Doppler flow*
- Lack of internal vascularization
- Thin wall
- Posterior acoustic enhancement
*These characteristics can help differentiate between a hemorrhagic cyst and malignant nodule, which typically has internal vascular flow and clots with more rounded edges.
Hemorrhage cysts generally resolve spontaneously within 8 weeks. Postmenopausal women with cysts > 5 cm should be re-evaluated about 8 weeks after exam to ensure decreased cyst size.
The major complication associated with hemorrhagic cysts is rupture into the peritoneum resulting in symptoms similar to ectopic pregnancy (pain/tenderness on the affected side, nausea/vomiting, etc.).
Dermoid Cysts
Dermoid cysts (also called mature cystic teratomas) are the most common type of benign ovarian neoplasm. They are composed of at least 2 of the 3 fetal tissue layers (endoderm, mesoderm, ectoderm) and can therefore contain a variety of tissue types including thyroid tissue, cartilage, hair, skin, and bone.
Presentation:
- Typically asymptomatic (often found incidentally or when associated with ovarian torsion)
- Possible symptoms related to pressure on surrounding organs
Ultrasound Findings of Dermoid Cysts:
Due to the variety of tissue types that make up dermoid cysts, they can have several unique appearances on ultrasound imaging. The presence of two or more of the following findings is suggestive of dermoid cysts:
- Diffuse echogenicity with posterior acoustic enhancement (increased echogenicity posterior to the cyst) – sebaceous tissue and hair; calcified bone or teeth
- Echogenic mesh of lines and dots (“dot-dash sign”) due to the presence of hair.
- Floating echoic fat globules
- Fluid-fluid level – liquids of differing viscosities
Complications of dermoid cysts include conversion into a malignant tumor, ovarian torsion, hyperthyroidism (if ectopic germ cell tissue is of thyroid gland origin), and cystic rupture.
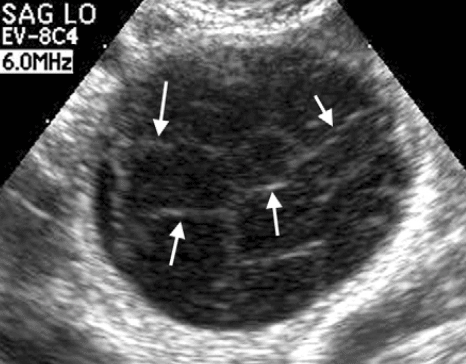
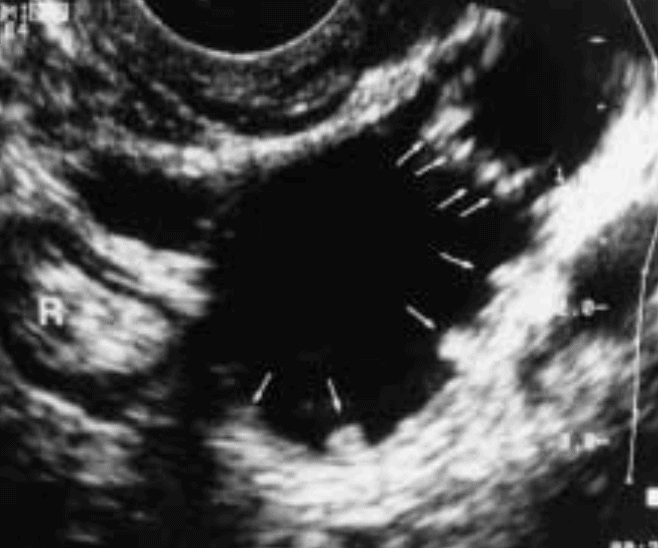
Polycystic Ovary Syndrome (PCOS)
Polycystic Ovary Syndrome (PCOS) is characterized by at least 2 out of 3 of the following criteria (Rotterdam 2004):
- Hyperandrogenism (Hirsutism, Infertility, Acne, Biochemical Tests)
- Ovulatory Dysfunction (Oligomenorrhea, Amenorrhea, or Anovulation)
- Polycystic Ovary Morphology (PCOM) on Ultrasound
- One or two ovaries that is >10 mL (volume = 0.5 × length × height × width)
- And/or: Large number of follicles (>12) measuring 2-9 mm in either ovary.
The title, polycystic ovary syndrome, is a bit of a misnomer because a polycystic ovary does not contain several cysts (>3 cm) but rather many follicles (< 3cm).
Editor’s Note: Within 8 years of menarche, the presence of many follicles within the ovary is generally considered a normal finding and ultrasound should not be used to diagnose PCOS (Dewailly, 2011; Lujan, 2013; Teede, 2019).
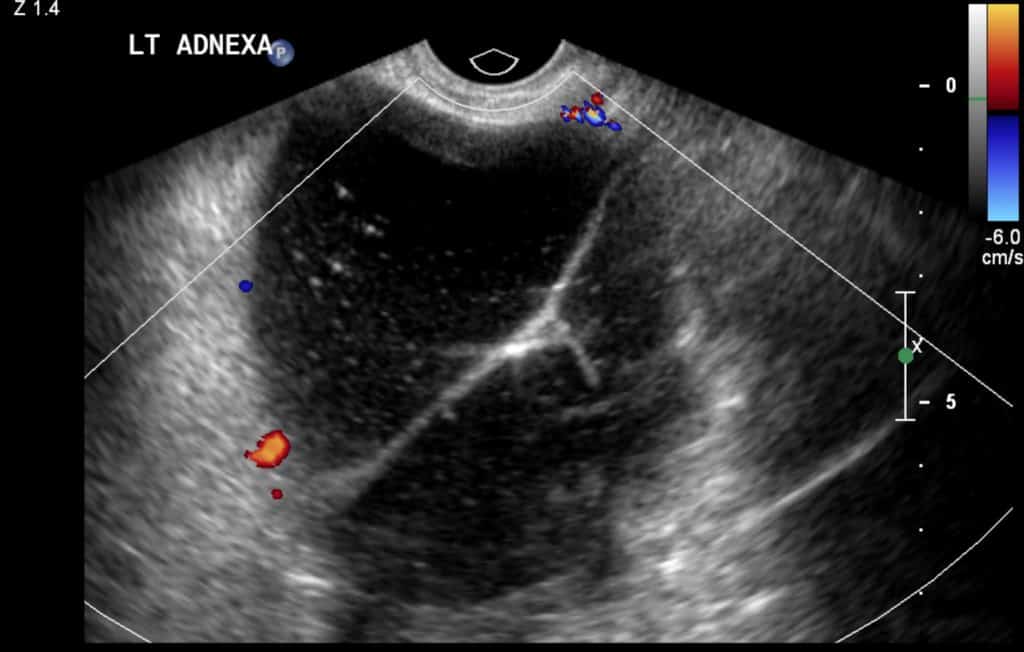
Ovarian Torsion
Ovarian Torsion is a gynecologic emergency in which the ovary has twisted on its ligaments and blood supply. Rotation of the ovary leads to compression of arteries, veins, and lymphatics causing congestion, ovarian edema, and potentially infarction if untreated.
Presentation:
- Acute pelvic or lower abdominal pain
- Tenderness upon palpation with the transvaginal transducer
- Nausea/vomiting
- Leukocytosis
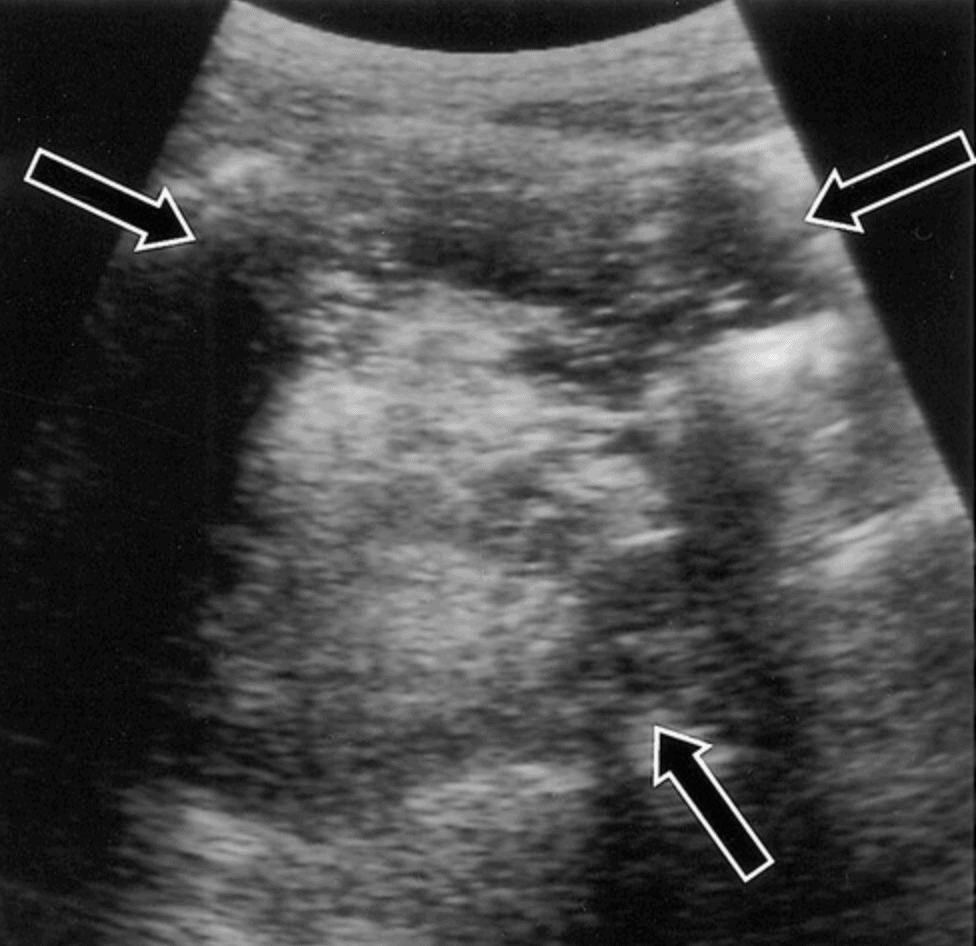
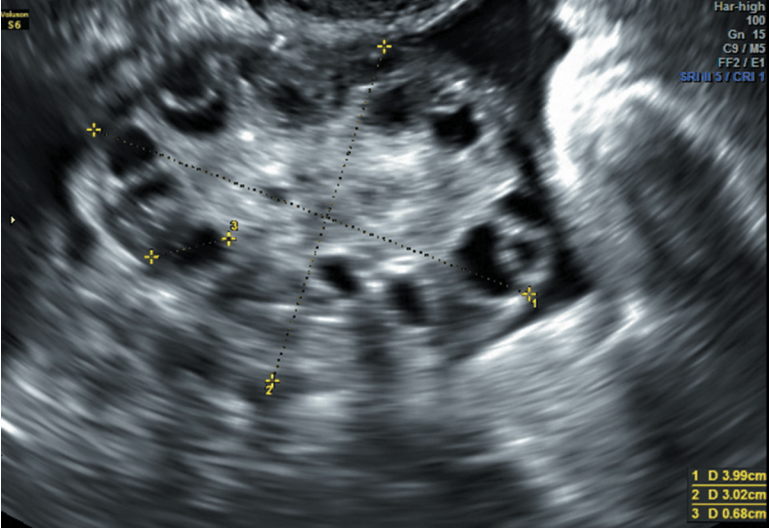
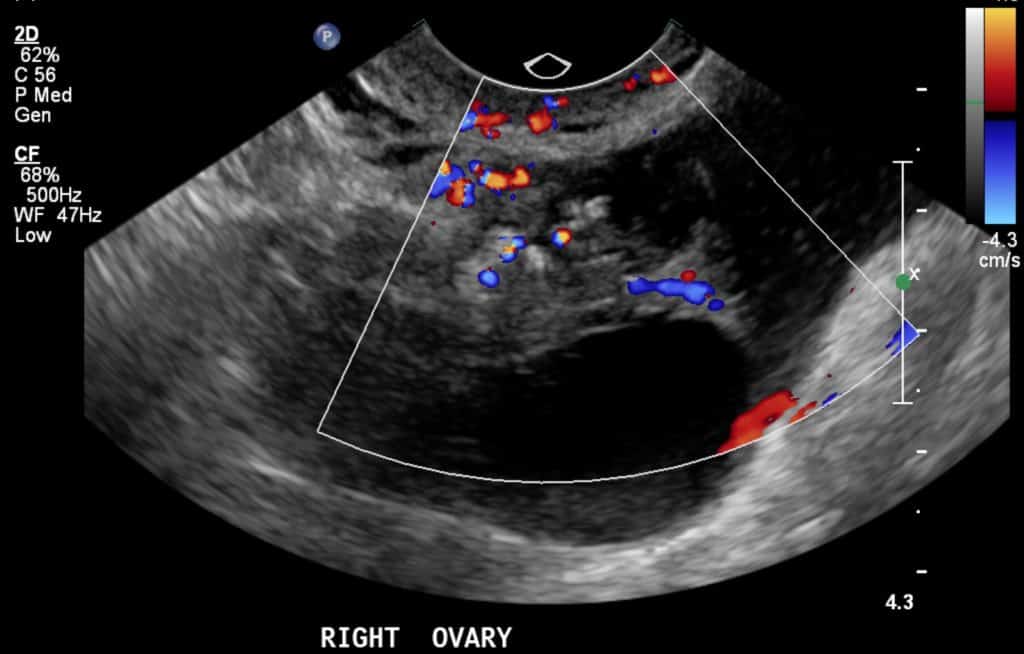
Ultrasound Findings of Ovarian Torsion:
- Decreased power and/or color Doppler flow of veins and arteries*
- Unilaterally enlarged/edematous ovary (>4 cm)
- Possible midline position of ovary
- String-of-Pearls sign – several peripheral follicles due to central lymphatic congestion
- Whirlpool sign – wrapping of vessels around central axis of the pedicle shown with Doppler flow
- Free pelvic fluid
- Ovarian mass
*The sensitivity and specificity for ultrasound diagnosis of ovarian torsion are 72.1% and 99.6%, respectively (Rostamzadeh 2014). Because sonography is not 100% sensitive, Color Doppler ultrasound findings may be normal (blood flow maintained) despite the presence of ovarian torsion. This is due to the dual blood supply of the ovaries from both the ovarian and uterine arteries.
Therefore ovarian torsion is considered a clinical diagnosis and emergent gynecology consult should still be obtained if you have a high clinical suspicion despite a normal-appearing ultrasound.
Hydrosalpinx
Hydrosalpinx is the abnormal accumulation of fluid in the fallopian tubes causing tubal swelling. Common underlying causes of hydrosalpinx include Pelvic Inflammatory Disease, Endometriosis, tubal obstructions/ligations, adhesions, and complications of hysterectomy.
Presentation:
- Chronic pelvic pain
- Infertility
- Possibly asymptomatic
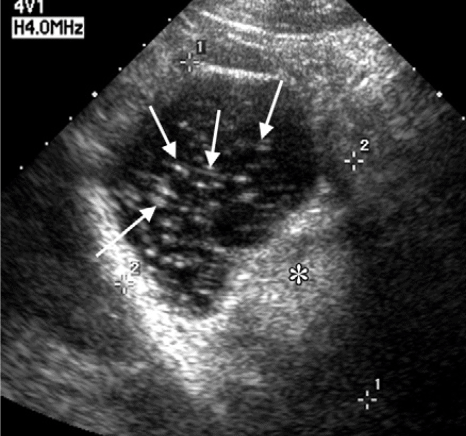
Ultrasound Findings of Hydrosalpinx:
While fallopian tubes are not normally visible on ultrasound, the dilated uterine tubes of hydrosalpinx can be visualized by the following characteristics on ultrasound imaging:
- Tubular shaped cystic mass discontinuous with the ipsilateral ovary
- Waist sign – indentations on both sides of the tubular mass
- Thin wall
- Beads-on-a-String sign – cross-sectional view with incomplete septations associated with chronic pelvic inflammation
- Cogwheel sign – cross-sectional view with thickened longitudinal folds of the uterine tubes associated with acute pelvic inflammation
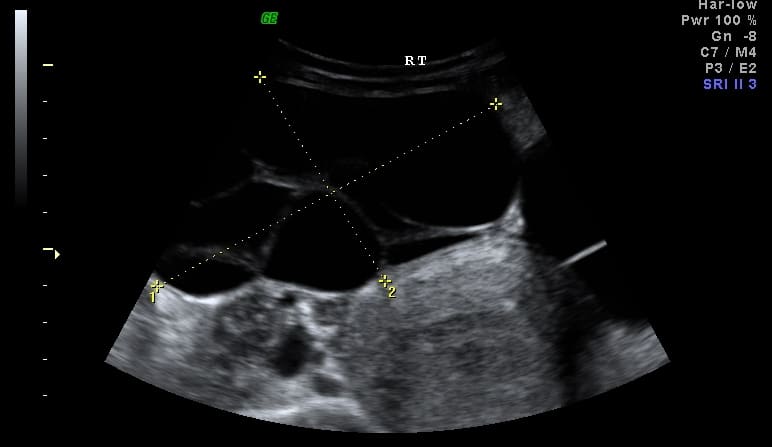
Tubo-ovarian Abscess
A tubo-ovarian abscess is a pus-filled mass originating in the uterine tube and often extending to involve the ovary. It is a late complication of pelvic inflammatory disease.
The abscess represents a retrograde spread of pelvic or abdominal infection/inflammation and requires prompt identification and treatment to prevent abscess rupture leading to septic shock.
Patient presentation may include the following:
- Acute onset pelvic/lower abdominal pain
- Cervical motion tenderness
- Palpable pelvic mass
- Fever
- High inflammatory markers
- Leukocytosis
- Vaginal discharge
- Previous history of STI or PID
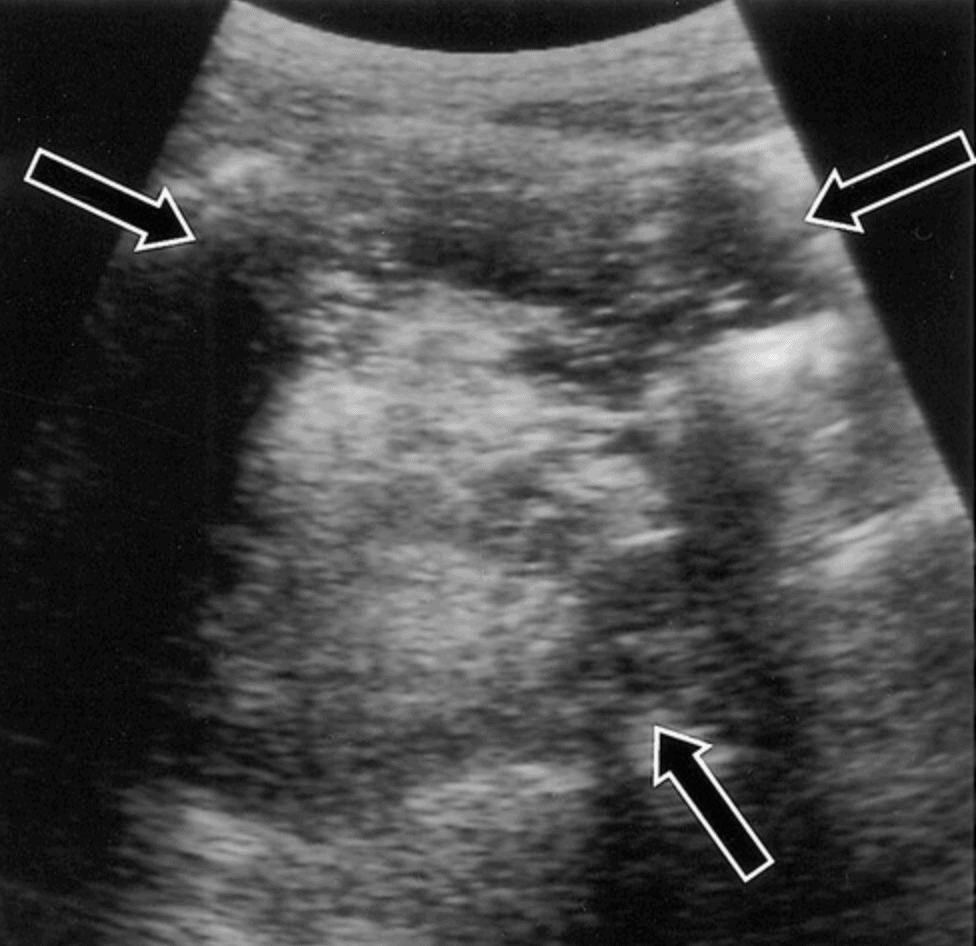
Ultrasound Findings of Tubo-ovarian Abscess:
Diagnosis by ultrasound imaging may be difficult due to the varied appearances of tubo-ovarian abscesses. However, some frequently seen ultrasound findings include:
- Adnexal mass: septated, irregular/thick walls, variable internal echogenicity, possible solid areas
- Ovary with ill-defined borders (mass obscures both ovary and fallopian tubes)
- Hydrosalpinx
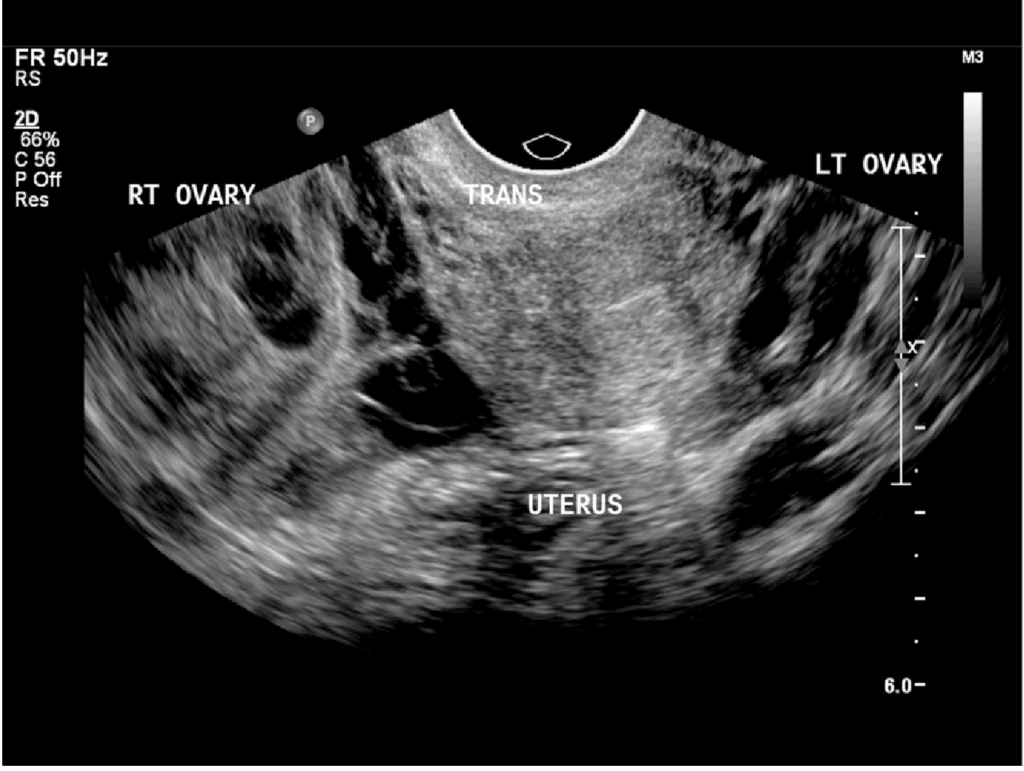
Pelvic Inflammatory Disease (PID)
Pelvic Inflammatory Disease (PID) is the result of an ascending spread of infection within the pelvis due to a causative organism (most commonly polymicrobial but also due to Chlamydia trachomatis or Neisseria gonorrhoeae infection). The condition is characterized by periovarian inflammation and is most common in women of reproductive age.
Presentation:
- Cervical motion tenderness
- Pelvic pain
- Vaginal discharge
- Fever
- Uterine/adnexal tenderness
- Leukocytosis
- Elevated inflammatory markers
Ultrasound findings of Pelvic Inflammatory Disease (PID):
Though PID is clinically diagnosed, ultrasound imaging is the first-line radiologic evaluation method of choice for PID and may be used to appreciate the following:
- Adnexal mass with heterogenous echogenicity (often bilateral)
- Pelvic free fluid (*hyperlink)
- Hydrosalpinx (waist sign, beads-on-a-string sign, (cogwheel sign) (*hyperlink)
- Multicystic ovaries (*hyperlink)
- Tubo-ovarian abscesses (end-stage) (*hyperlink)
Ovarian Neoplasms
Point-of-care ultrasound can be helpful in the differentiation of the three primary types of ovarian neoplasms: mucinous cystadenoma, serous cystadenoma, and cystadenocarcinoma.
Mucinous Cystadenoma
These types of tumors are the most common type of benign ovarian neoplasm. Patients may appear “gravid” if the mass has grown extensively into the abdomen.
On ultrasound, you can expect to see a cystic mass filled with mucinous material (several small, low-level internal echoes).
Serous Cystadenoma
These tumors are a less common type of benign ovarian neoplasm.
Ultrasound findings include a cystic mass with:
- Several thin septations that undulate with transducer palpation.
- Few/no internal echoes
Serous Cystadenocarcinoma
These tumors are malignant and appear on ultrasound as cystic masses with:
- Thick septa
- Mural nodularity
- Solid tissue with internal vascularization
- Another clue pointing toward malignancy is the presence of ascites, which is generally absent in benign conditions
References
- Sohoni, A., Bosley, J., Miss, J. (2014). Bedside Ultrasonography for Obstetric and Gynecologic Emergencies Critical Care Clinics 30(2), 207-226.
- Sarmiento J, Stewart K, Aguila J, Bagherpour A, Kupesic Plavsic S. Pelvic Ultrasound Simulation Training Models and Case Scenarios. Donald School J Ultrasound Obstet Gynecol 2014;8(1):22-30.
- Alonso, J., Ruffino, G., Hurdidge, E. (2019). Abdominal Pain in a Young Female Adolescent: Point-of-Care Ultrasound Added Value. Pediatric emergency care
- Atri, M. (2003). Ectopic Pregnancy Versus Corpus Luteum Cyst Revisited Journal of Ultrasound in Medicine 22(11), 1181-1184.
- Brown, D., Dudiak, K., Laing, F. (2010). Adnexal Masses: US Characterization and Reporting Radiology 254(2), 342-354.
- Evans, A., Szlachetka, K., Thornburg, L. (2019). Ultrasound Assessment of the Intrauterine Device. Obstetrics and gynecology clinics of North America 46(4), 661-681.
- Fogel, Slasky, B. (1982). Sonography of Nabothian cysts American Journal of Roentgenology 138(5), 927-930. https://dx.doi.org/10.2214/ajr.138.5.927
- Hall, D., Hann, L., Ferrucci, J., Black, E., Braitman, B., Crowley, W., Nikrui, N., Kelley, J. (1979). Sonographic Morphology of the Normal Menstrual Cycle Radiology 133(1), 185-188. https://dx.doi.org/10.1148/133.1.185
- Jantarasaengaram, S., Siricharoenthai, S., Vairojanavong, K. (2003). Cystic ovarian teratoma with intracystic fat balls: Picture of the Month Ultrasound in Obstetrics and Gynecology 22(1), 102-103. https://dx.doi.org/10.1002/uog.181
- Kyei-Mensah, A., Zaidi, J., Campbell, S. (1996). Ultrasound diagnosis of polycystic ovary syndrome Baillière’s Clinical Endocrinology and Metabolism 10(2), 249-262. https://dx.doi.org/10.1016/s0950-351x(96)80099-1
- Lobo, R. A., Gershenson, D. M., Lentz, G. M., & Valea, F. A. (2016). Comprehensive Gynecology E-Book. Elsevier Health Sciences.
- Nalaboff, K., Pellerito, J., Ben-Levi, E. (2001). Imaging the Endometrium: Disease and Normal Variants RadioGraphics 21(6), 1409-1424.
- Nap, A., Groothuis, P., Demir, A., Evers, J., Dunselman, G. (2004). Pathogenesis of endometriosis Best Practice & Research Clinical Obstetrics & Gynaecology 18(2), 233-244.
- Norton, M. E. (2016). Callen’s Ultrasonography in Obstetrics and Gynecology E-Book. Elsevier Health Sciences.
- Outwater, E., Siegelman, E., Hunt, J. (2001). Ovarian Teratomas: Tumor Types and Imaging Characteristics RadioGraphics 21(2), 475-490.
- Patel, M., Acord, D., Young, S. (2006). Likelihood Ratio of Sonographic Findings in Discriminating Hydrosalpinx from Other Adnexal Masses American Journal of Roentgenology 186(4), 1033-1038. https://dx.doi.org/10.2214/ajr.05.0091
- Poland, D., Bachanek, M., Abdalla, N., Cendrowski, K., Sawicki, W. (2015). Value of ultrasonography in the diagnosis of polycystic ovary syndrome – literature review. Journal of ultrasonography 15(63), 410-22.
- Rotterdam Group. (2004). Revised 2003 consensus on diagnostic criteria and long‐term health risks related to polycystic ovary syndrome (PCOS) Human Reproduction 19(1), 41-47.
- Sampson, J. A. (1927). Peritoneal endometriosis due to the menstrual dissemination of endometrial tissue into the peritoneal cavity. American Journal of Obstetrics & Gynecology, 14(4), 422-469.
- Senaldi, L., Gopi, R., Milla, S., Shah, B. (2015). Is ultrasound useful in the diagnosis of adolescents with polycystic ovary syndrome? Journal of Pediatric Endocrinology and Metabolism 28(5-6), 605-612. https://dx.doi.org/10.1515/jpem-2014-0307
- Timor-Tritsch, I., Lerner, J., Monteagudo, A., Murphy, K., Heller, D. (1998). Transvaginal sonographic markers of tubal inflammatory disease: Markers of tubal inflammatory disease Ultrasound in Obstetrics and Gynecology 12(1), 56-66. https://dx.doi.org/10.1046/j.1469-0705.1998.12010056.x
- Vijayaraghavan, S. (2004). Sonographic Whirlpool Sign in Ovarian Torsion Journal of Ultrasound in Medicine 23(12), 1643-1649.
- Rostamzadeh, A., Mirfendereski, S., Rezaie, M., Rezaei, S. (2014). Diagnostic efficacy of sonography for diagnosis of ovarian torsion. Pakistan journal of medical sciences 30(2), 413-6.
- Wilson, S., Connolly, K., Lahham, S., Subeh, M., Fischetti, C., Chiem, A., Aspen, A., Anderson, C., Fox, J. (2016). Point-of-care ultrasound versus radiology department pelvic ultrasound on emergency department length of stay World Journal of Emergency Medicine 7(3), 178.
- Woźniak, A., Woźniak, S. (2017). Ultrasonography of uterine leiomyomas Menopausal Review 16(4), 113-117.
- Case courtesy of Dr Prasanta Kumar Nayak, Radiopaedia.org. From the case rID: 24808
- Case courtesy of Dr Maulik S Patel, Radiopaedia.org. From the case rID: 30458
- Case courtesy of RMH Core Conditions, Radiopaedia.org. From the case rID: 26157
- Case courtesy of Dr Alexandra Stanislavsky, Radiopaedia.org. From the case rID: 78976
- Case courtesy of Dr Alexandra Stanislavsky, Radiopaedia.org. From the case rID: 78844
- Case courtesy of Dr Praveen Jha, Radiopaedia.org. From the case rID: 16979





[…] Gyn-Pelvic Ultrasound Tutorial […]