Clinical Concepts in Pelvic Ultrasound
/Your patient is a well appearing, otherwise healthy 22 year old female who presents with lower abdominal pain x3 days. She is unsure of her LMP, but thinks she had some spotting about a month ago. Vital signs: Temp 99.3F, HR 92, BP 102/70, RR 20, 98% on RA. She has a benign, non-gravid abdomen. Urine pregnancy is positive. You fire off a quantitative hCG and don’t expect that result to come back for a while. What do you do next?
ACEP recommends (Level C recommendation) obtaining a diagnostic pelvic ultrasound regardless of the beta hCG level in a symptomatic pregnant patient, even though you may not definitively see an IUP. Other secondary findings on ultrasound, such as increased amounts of free fluid, can suggest the diagnosis of ectopic pregnancy. Pelvic ultrasounds can be acquired both trans-vaginally (TV) and trans-abdominally (TA). The threshold for detecting an IUP is 5-6 weeks by TV ultrasound and 6-7 weeks by TA ultrasound.
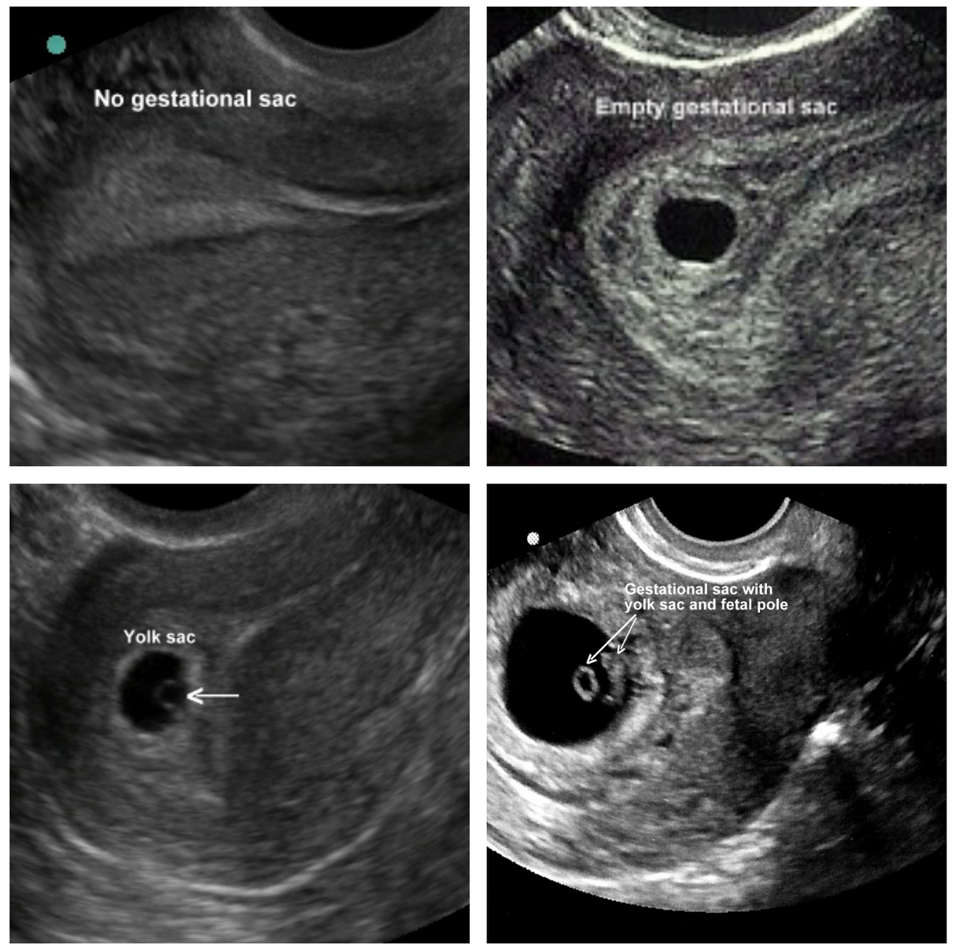
To diagnose an IUP, you must see a gestational sac with a yolk sac, +/- a fetal pole. The endometrial stripe must be continuous from the cervix to the gestational sac, and when you interrogate in the longitudinal and transverse planes, you must be able to appreciate myometrium surrounding the entire gestational sac at a minimum thickness of 5-8mm. To the right, you see a representative negative image (top left), an empty gestational sac (top right), and two positive IUPs (bottom).
The following are some examples of pelvic ultrasound findings. Watch the video and then click to read the discussion.
+ What is the Differential Diagnosis for this Finding?
This is an empty uterine sac. It can represent three things:
- Too early in pregnancy to see a yolk sac or fetal pole
- Missed abortion
- A gestational pseudosac, an endometrial reaction to hormones from an ectopic pregnancy
With the finding of a gestational pseudosac, your history, physical exam, and beta hCG will be useful adjuncts. Be sure to carefully look for secondary signs of ectopic pregnancy such as free fluid in the pelvis
+ How do you quantify free fluid on pelvic ultrasound?
This is a clear ectopic pregnancy, with a significant amount of free fluid in the pouch of Douglas. Understandably, we sometimes reflexively assume that any free fluid in the pelvis is pathologic. However, most women have at least some physiologic free fluid in the pelvis. When evaluating for clinically significant free fluid, the fluid is measured relative to the uterus.
- Fluid behind 1/3 of the total length of the uterus (generally the cervix/distal body) = mild free fluid, and is considered physiologic in the absence of other concerning factors
- Fluid behind 2/3 of the length of the uterus (cervix/body) = moderate free fluid
- Fluid behind 3/3 of the length of the uterus (cervix/body/fundus) = severe free fluid
With moderate or severe free fluid, it is recommended that the examiner add a RUQ FAST view to your exam to evaluate for more extensive bleeding. Additionally, free fluid may be easier to appreciate than clotted blood, which can sometimes mimic myometrium. In those cases, be sure to delineate your anatomy and be guided by your clinical suspicion. Ectopic pregnancies are only ~2% of total pregnancies, but amongst ED patients who present as symptomatic with a positive pregnancy test, 7.5% are diagnosed with an ectopic pregnancy.
+ Where is this pregnancy located?
This pregnancy is cervical. There are no fetal heart tones appreciated in this clip, which is concerning for a miscarriage in process, or less commonly a cervical ectopic with fetal demise. Only 2% of ectopic pregnancies are located in the cervix. Remember that your uterine anatomy is all relative to the angle of the bladder, and keep the orientation of the probe in mind as you interrogate the structures of the pelvis.
References
- Cadogan, Mike. Emergency Ultrasound. http://lifeinthefastlane.com/emergency-ultrasound/ Accessed 4/27/2016.
- Hahn SA, Lavonas EJ, Mace SE, Napoli AM, Fesmire FM. Critical issues in the initial evaluation and management of patients presenting to the emergency department in early pregnancy. Ann Emerg Med 2012;60:381-90. 55.
- Hwang JQ, Kimberly HH, Liteplo AS, Sajed D (2011). An Evidence-Based Approach to Emergency Ultrasound. Emergency Medicine Practice, 13(3)
- Lozeau AM, Potter B. Diagnosis and management of ectopic pregnancy. Am Fam Physician. 2005 Nov 1;72((9)):1707–14.
- Stovall TG, Kellerman AL, Ling FW, Buster JE. Emergency department diagnosis of ectopic pregnancy. Ann Emerg Med.1990;19(10):1098-1103.