VT (Ventricular Tachycardia)
Diagnostic criteria: (boldfaced with * indicates an important feature)- * Rate: > 100
- Rhythm: regular
- * P waves: not easily identified (but they could be present)
- * PR interval: if P waves are present, they are not associated with QRS
- * QRS: wide (> 3 little squares)
Electrophysiology
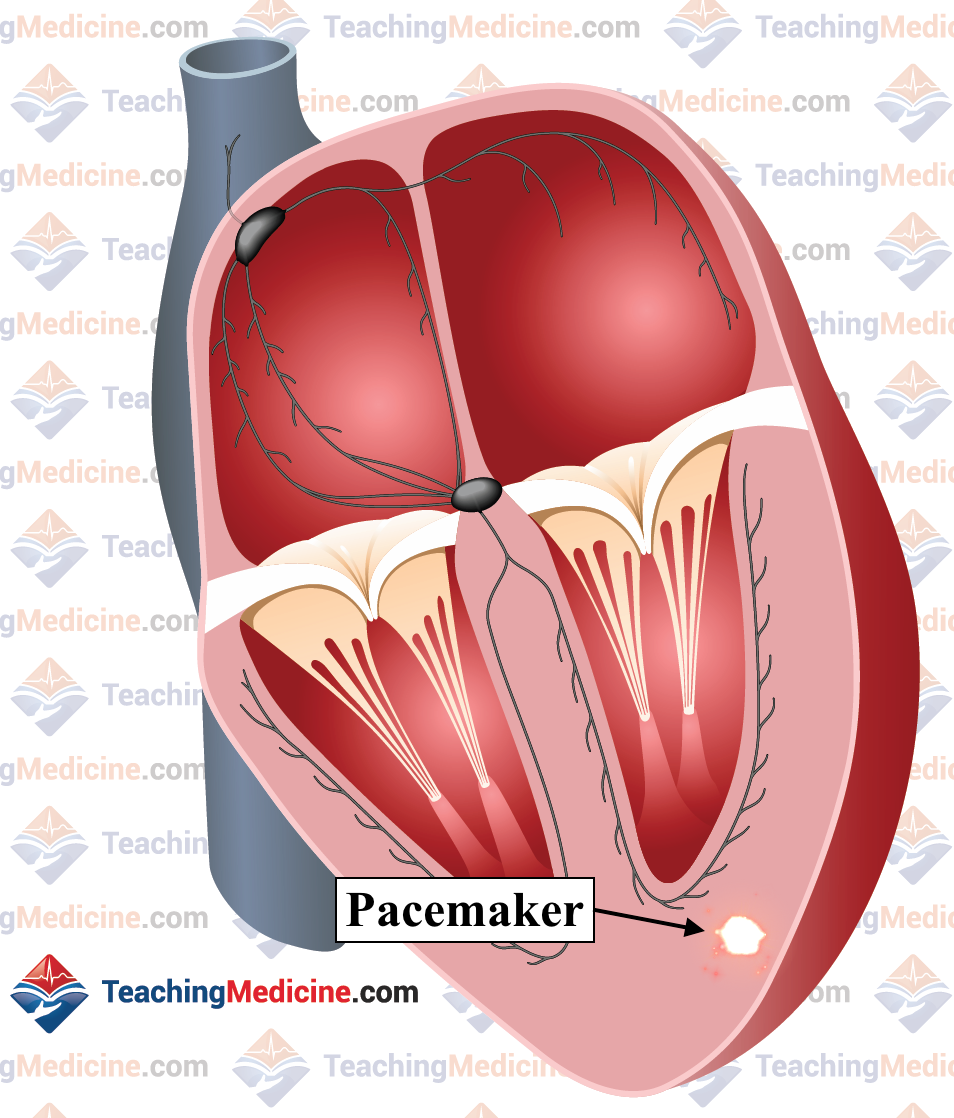
Ventricular tachycardia is caused by an abnormal pacemaker that is located inside the ventricle. Normally, the SA node is the pacemaker, but in pathological states, a pacemaker can arise in the ventricles due to a re-entry circuit or other mechanism. These pacemakers are typically very fast.
Sometimes, the SA node is still firing even when the ectopic pacemaker (ectopic means any location outside the SA node) is firing very fast. Therefore, you can sometimes see P waves superimposed in between the QRS complexes.
The QRS complex can be very wide and very abnormal. The T wave can also be very abnormal and it can sometimes be difficult to tell where the QRS ends and where the T wave begins.
VT can be categorized as monomorphic (all the QRS's are the same size and shape and all come from the same pacemaker) or polymorphic (QRS's are different size and shape and come from different pacemakers in the ventricle).
There are many "variants", causes, and sub-types of VT that will not be discussed here. They will be discussed in more advanced modules.
Clinical Significance:
Ventricular tachycardia should be considered a medical emergency. It is always pathological and has a very high probability to be pulseless or deteriorate into ventricular fibrillation (one form of cardiac arrest).
Stroke volume, cardiac output, and blood pressure are usually very low with ventricular tachycardia. This is due to 3 main reasons (and there are more):
- the heart rate is very fast so diastolic time (filling time for the ventricle) is very short. Therefore, the ventricle is often underfilled.
- depolarization of the ventricle occurs outside of the normal conducting fibers. Therefore, activation of the myocardium is abnormally slow, so contraction is abnormal and stroke volume is reduced.
- further, the wave of depolarization travels across the ventricle in an abnormal pattern, therefore activating the ventricle in a suboptimal pattern compared to when the ventricle is activated using the normal conducting fibers. This results is reduced efficiency of contraction and a smaller stroke volume.
As a result of the many reasons why stroke volume and cardiac output are reduced in VT, many patients with VT will not have a pulse. Patients who do not have a pulse are considered to be in cardiac arrest and require CPR.
VT needs to be treated as soon as possible. Treatment for VT is well described in ACLS (Advanced Cardiac Life Support), a course for treating cardiac arrests. Treatment involves drugs, cardioversion or defibrillation, and if pulseless, CPR.
Some patients with VT receive a surgically implanted AICD (automatic implantable cardioverter-defibrillator). These devices are similar to pacemakers, but have the ability to detect VT (or ventricular fibrillation) and deliver a very strong shock. If a patient is awake when one of these shocks is administered, it is very painful. However, it could save their life by terminating a lethal rhythm.
Some patients with VT can also be treated with ablation, which is an invasive treatment to "burn" abnormal electrical circuits inside the heart with the hope that they are eradicated and no longer generate VT.
Causes of Ventricular Tachycardia include:
- myocardial ischemia or infarction
- dilated cardiomyopathy
- myocarditis
- many others
Examples:
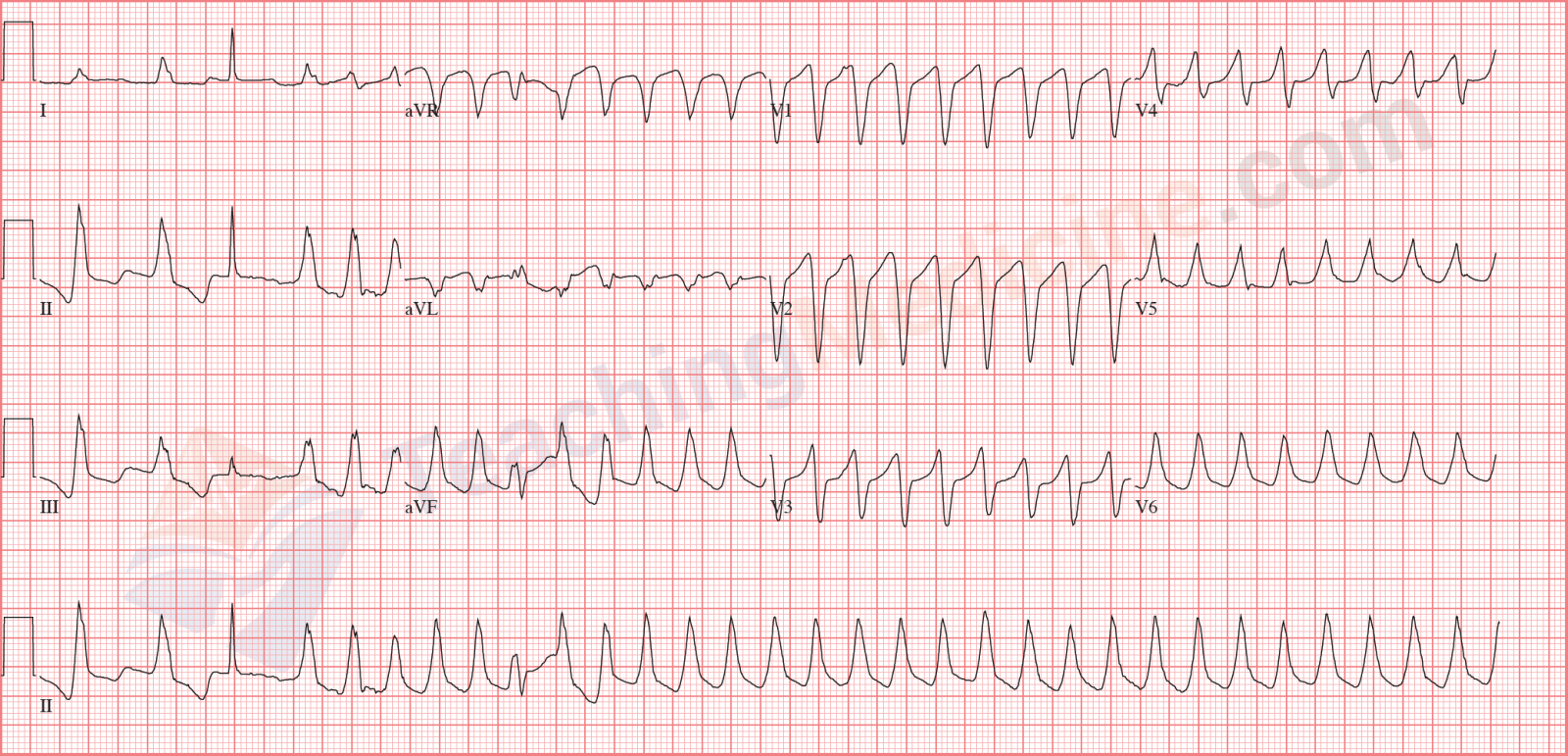
Monomorphic VT:
Monomorphic VT. Difficult to tell where the QRS ends and the ST or T wave starts:
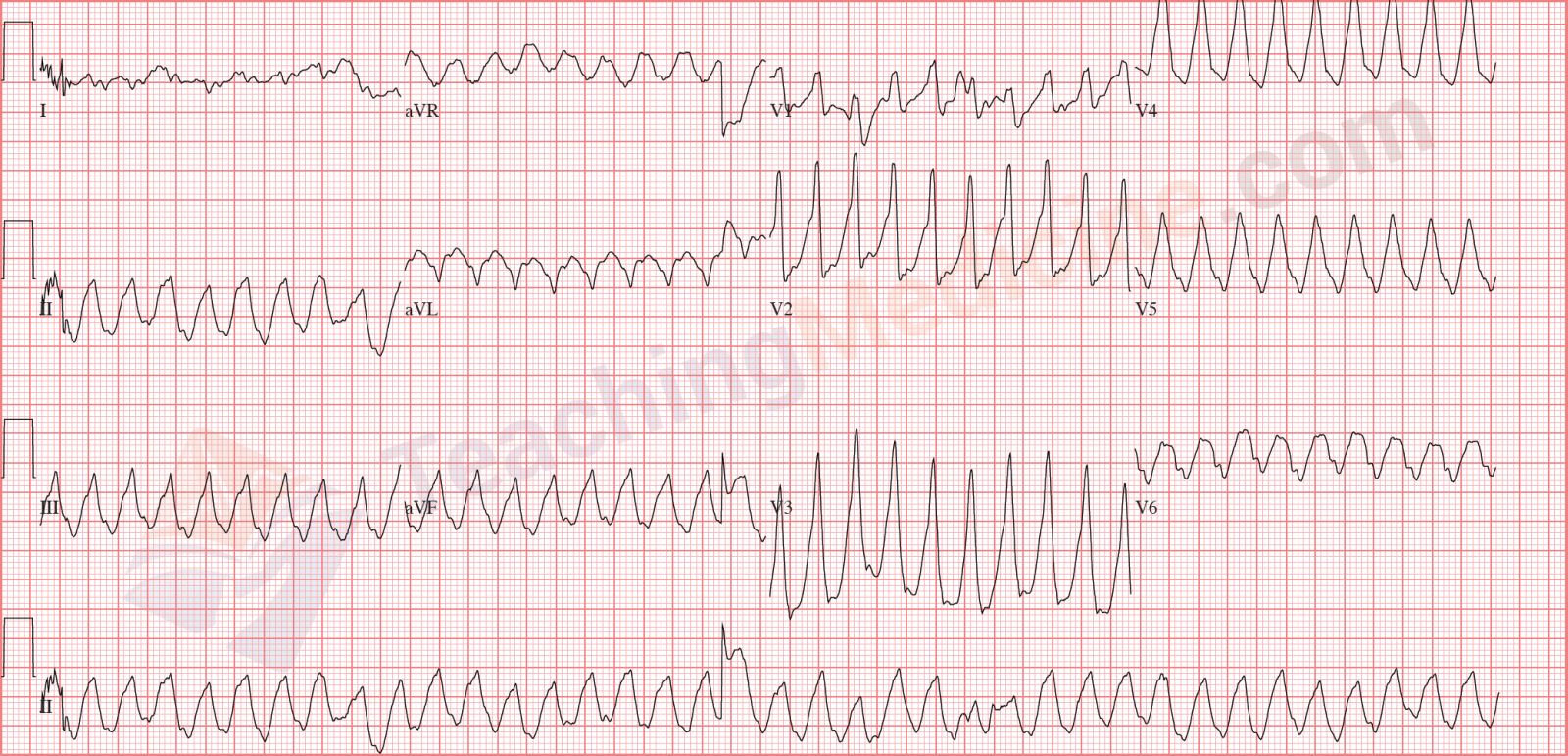
QRS's are different size and shape, so this is polymorphic VT:
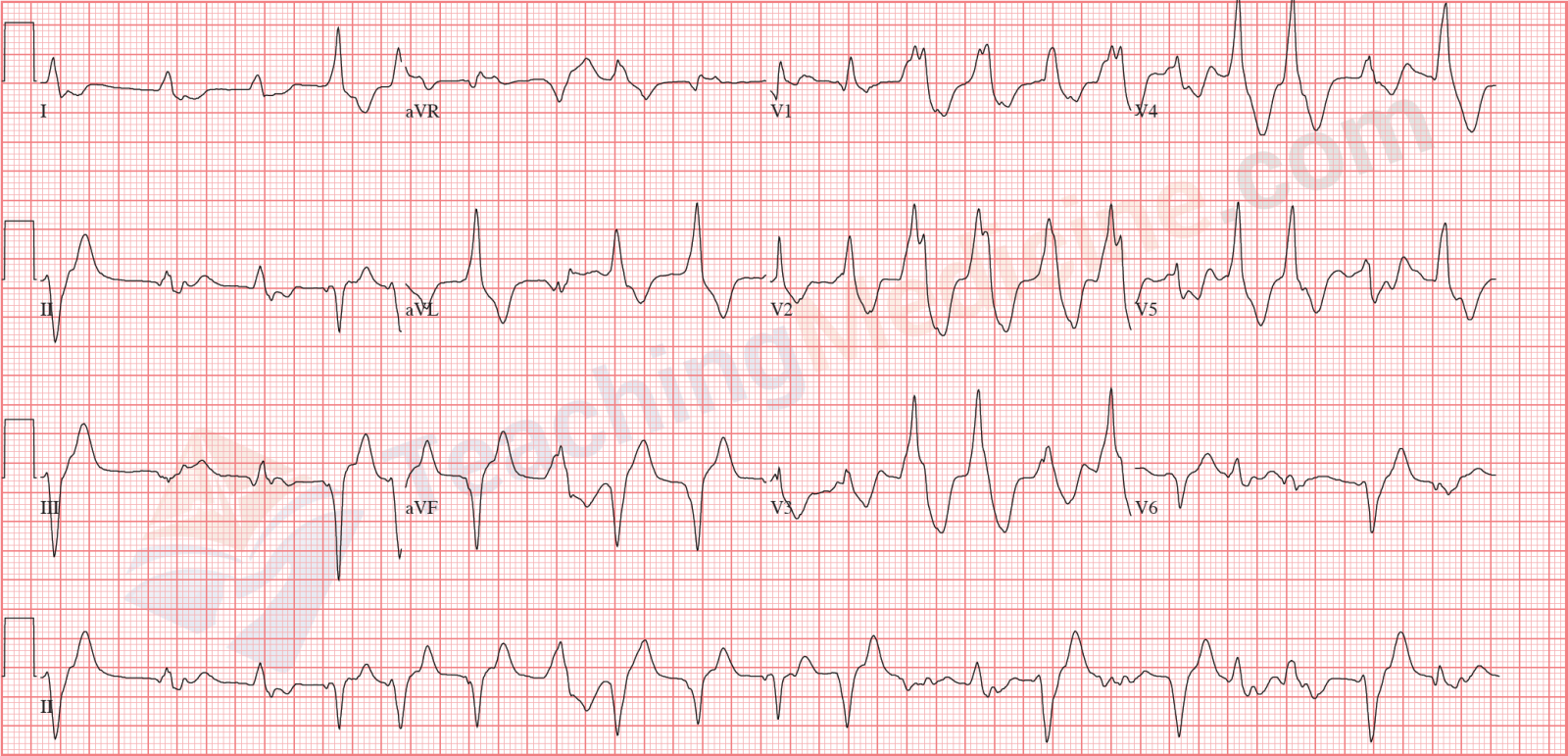
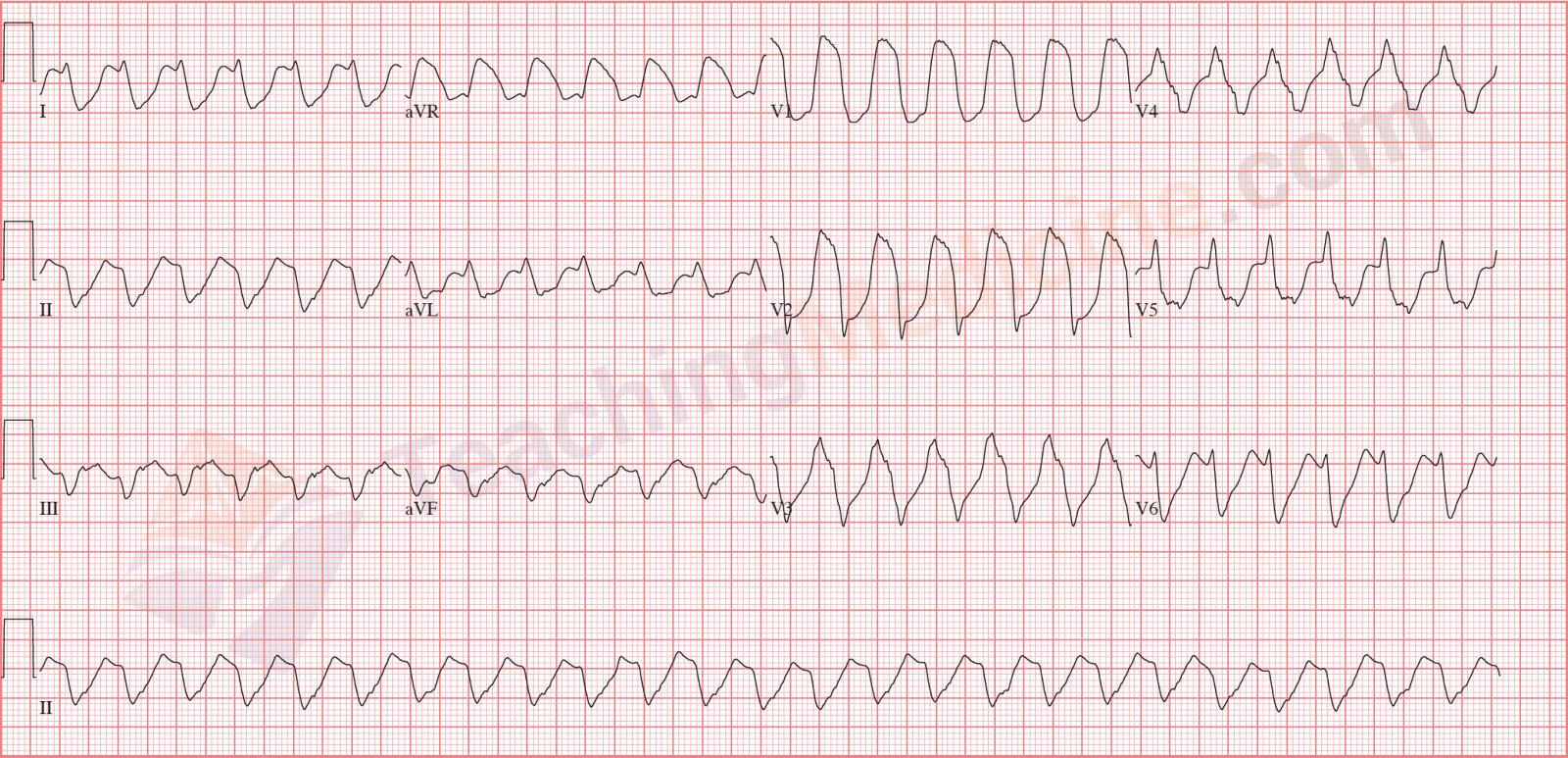
At the beginning of this ECG, you can see a narrow QRS (the 3rd heart beat). This is a QRS that is generated by the SA node that is still firing. This is called a capture beat. Sometimes, a QRS is a combination of a capture beat and a ventricular beat (the 9th QRS might be one of these). These are called fusion beats.