Postscript
Prev
1 / 0 Next
Prev
1 / 0 Next
Description
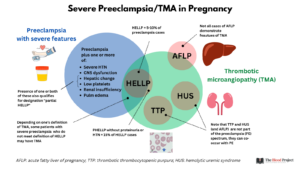
- HELLP is the acronym for hemolysis, elevated liver enzymes, and low platelet count syndrome.
- HELLP is a serious life-threatening form of pre-eclampsia in pregnancy (occurring mostly in second and third trimesters) characterized by:
- Hemolysis
- Elevated liver enzymes
- Low platelet count
- Though currently regarded as a severe form of preeclampsia, the relationship between the two disorders remains controversial. Notably, up to 15-20% of patients with HELLP do not have antecedent hypertension or proteinuria.
- HELLP is a type of thrombotic microangiopathy (TMA)
- It is the most common cause of a TMA in the late second/third trimesters
- It is important to distinguish between HELLP and thrombotic thrombocytopenia purpura (TTP) and hemolytic uremic syndrome (HUS) as their treatment differs greatly with urgent delivery indicated only for the former.
- HELLP is associated with substantial risk for the mother and her fetus:
- Increased risk of severe complications for both mother and offspring.
- Maternal mortality rate reported to be as high as 24%.
- Perinatal mortality rate reported to be up to 37%.
- A woman with a history of HELLP pregnancy is at high risk for recurrence of HELLP in subsequent pregnancies.
Definitions
- Preeclampsia is defined by presence of both:
- Hypertension
- systolic blood pressure ≥ 140 mm Hg and/or diastolic blood pressure ≥ 90 mm Hg on 2 occasions ≥ 4 hours apart after 20 weeks gestation in a patient with previously normal blood pressure or
- Systolic blood pressure ≥ 160 mm Hg and/or diastolic blood pressure ≥ 110 mm Hg
- Proteinuria requiring any of:
- ≥ 300 mg per 24 hour urine collection
- Protein/creatinine ratio ≥ 0.3
- Dipstick reading of 2+ (should only be used if other quantitative methods are not available)
- Hypertension
- If no proteinuria, diagnosis of preeclampsia requires new-onset hypertension with new onset of ≥ 1 severe features:
- Thrombocytopenia (platelet count < 100 x 109/L)
- Impaired liver function (elevated serum liver transaminases to twice normal concentration)
- Renal insufficiency (serum creatinine > 1.1 mg/dL or doubling of serum creatinine in patient without other renal disease)
- Pulmonary edema
- New-onset headache unresponsive to medication and not accounted for by other diagnoses
- Visual disturbances
- HELLP is a variant of severe preeclampsia typically diagnosed using the following the criteria:
- Lactate dehydrogenase (LDH) ≥ 600 units/L
- Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) > twice the upper limit of normal
- Platelet count < 100 x 109/L
History
- First described by Weinstein in 1982 as an additional criterion for preeclampsia with severe features.
Types
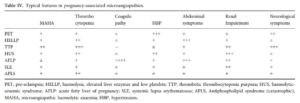
- Thrombotic microangiopathies (TMA) in pregnancy include:
- HELLP – the most common pregnancy-related TMA
- Thrombotic thrombocytopenic purpura (TTP)
- Hemolytic uremic syndrome
- Acute fatty liver disease of pregnancy – may have some features of TMA.
- Catastrophic antiphospholipid syndrome (CAPS)
- Complete HELLP syndrome:
- Requires presence of all 3 components:
- Hemolysis (H)
- Elevated liver enzymes (EL)
- Low platelets (LP)
- Requires presence of all 3 components:
- Partial or incomplete HELLP syndrome:
- Defined by the presence of one or two features of HELLP, but not the complete form.
- Includes presence of 1 or 2 components (H or EL or LP).
Epidemiology
- HELLP may occur:
- Antepartum – 70% of cases:
- Peak frequency between 27 and 37 weeks gestation (68% of cases).
- 10% of cases occur prior to 27 weeks gestation (onset before 23 weeks is very rare).
- 20% of cases occur after 37 weeks gestation.
- Postpartum – 30% of cases:
- Usually within 48 h, but may occur up to 7 days postpartum.
- Typically occurs in women who had proteinuria and hypertension in pregnancy (about 90% of cases).
- Prognosis is worse compared with antepartum HELLP, with higher risk of renal failure and pulmonary edema.
- Antepartum – 70% of cases:
- Reported to occur in:
- 0.5 to 0.9% of all pregnancies
- 10%-20% of pregnancies with severe preeclampsia
- Risk factors associated with complete or partial HELLP syndrome are similar to those associated with preeclampsia with the exception that nulliparity is not a risk factor for HELLP.
Pathophysiology
- The pathogenesis of preeclampsia and HELLP is incompletely understood, but it is believed to include abnormal placental angiogenesis secondary to an imbalance between angiogenic (placental growth factor) and antiangiogenic (soluble Flt1) factors.
- There is no evidence for a role of:
- Acquired or hereditary severe (< 10%) deficiency in ADAMTS13 activity
- Hereditary complement dysregulation
- Hemolysis due to microangiopathic hemolytic anemia, caused by high-velocity passage through small vessels involved with intima damage, endothelial dysfunction and fibrin deposition.
- Thrombocytopenia due to increased platelet consumption.
- Hepatic transaminitis:
- Due to liver injury; histopathologic findings in the liver include:
- Intravascular fibrin deposits that presumably lead to hepatic sinusoidal obstruction.
- Intrahepatic vascular congestion
- Increased intrahepatic pressure with ensuing:
- Hepatic necrosis
- Intraparenchymal
- Subcapsular hemorrhage
- Capsular rupture
- Serum AST (and LDH) are nonspecific markers that can be associated with severe hemolysis, acute hepatocellular injury, or both.
- Due to liver injury; histopathologic findings in the liver include:
Clinical presentation
- The clinical presentation of HELLP syndrome is highly variable.
- Symptoms include:
- General malaise
- Right upper quadrant or epigastric pain:
- Most common symptom (up to 90% of patients)
- Typically colicky
- Nausea and vomiting
- Headache (30–60% of cases)
- Visual disturbances (20% of cases)
- Altered consciousness
- Viral syndrome-like symptoms
- The symptoms often occur rapidly and progressively worsen.
- Hypertension and proteinuria present in about 85% of cases.
- Bleeding from thrombocytopenia is an unusual presentation.
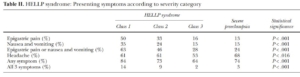
Am. J. Obstet. Gynecol. 1999, 180, 1373–1384
Diagnosis
- No single diagnostic finding; diagnosis of HELLP syndrome relies on simple clinical and laboratory parameters.
- Suspect diagnosis in pregnant women with:
- Signs of preeclampsia (hypertension and proteinuria) or eclampsia.
- The presence of schistocytes and elevated LDH, which supports the diagnosis of a microangiopathic hemolytic anemia and is concerning for a thrombotic microangiopathy (TMA).
- Confirm diagnosis using diagnostic criteria for HELLP syndrome:
- Complete HELLP:
- American College of Obstetricians and Gynecologists:
- LDH ≥ 600 IU/L
- AST and ALT elevated more than twice the upper limit of normal
- Platelet count < 100 x 109/L
- Tennessee Classification System for complete HELLP syndrome – widely used for diagnosis:
- Platelets ≤ 100 x 109/L
- AST ≥ 70 units/L
- LDH (or bilirubin) (with hemolysis as evidenced on abnormal peripheral smear) levels of 600 IU/L (≥0.2 mg/dL) or more.
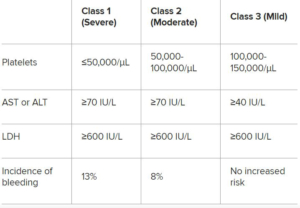
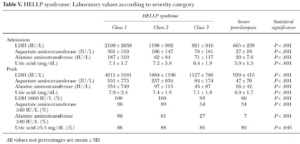
- Mississippi Triple-Class System – underlines the severity of the disorder according to the nadir of the platelet count:
- HELLP class 1 (severe)
- Platelets ≤ 50 x 109/L
- AST or ALT ≥ 70 units/L
- LDH ≥ 600 units/L
- HELLP class 2 (moderate)
- Platelets 50-100 x 109/L
- AST or ALT ≥ 70 units/L
- LDH ≥ 600 units/L
- HELLP class 3 (mild)
- Platelets 100-150 x 109/L
- AST or ALT ≥ 40 units/L
- LDH ≥ 600 units/L
- HELLP class 1 (severe)
- American College of Obstetricians and Gynecologists:
- Complete HELLP:
From Medscape
-
-
Partial HELLP syndrome is characterized by severe preeclampsia plus one of the following:
-
ELLP: Elevated liver enzyme levels, thrombocytopenia, no hemolysis
-
EL: Mildly elevated liver enzyme levels, no thrombocytopenia, no hemolysis
-
LP: Thrombocytopenia, no hemolysis, normal liver enzyme levels
-
HEL: Hemolysis, liver dysfunction, no thrombocytopenia
-
-
- Labs:
- Complete blood count:
- Anemia
- Thrombocytopenia
- Elevated reticulocytes
- Hemolytic markers in serum:
- Elevated:
- LDH
- Indirect bilirubin
- AST
- Decreased haptoglobin
- Specific marker of hemolysis.
- 25 mg/dL provides the best cutoff between hemolytic and non-hemolytic disorders.
- Elevated:
- Hemolytic markers in plasma:
- Plasma hemoglobinemia (10% of cases)
- Liver function tests, including elevated:
- AST
- ALT
- Glutathione S-transferase-A1 (GST-A1; assay not widely available)
- Peripheral smear:
- Presence of fragmented (schizocytes)
- Polychromatophilia
- Soluble fms-like tyrosine kinase-1/placental growth factor (sFlt1/PlGF) ratio
- Ratios > 85 before 34 weeks of gestation and > 110 after 34 weeks, are strongly suggestive of preeclampsia or HELLP syndrome, whereas ratios below 38 suggest an alternative diagnosis.
- Further prospective studies are needed to determine their widespread clinical utility.
- Urine:
- Proteinuria (85% of cases)
- Hemoglobinuria (10% of cases)
- Depending on clinical context, other tests may be ordered to rule out mimics of HELLP including:
- ADAMTS13 levels (low in TTP)
- Complement tests (abnormal in HUS)
- Tests for autoimmunity, for example:
- Lupus anticoagulant
- ANA
- Complete blood count:
Am. J. Obstet. Gynecol. 1999, 180, 1373–1384
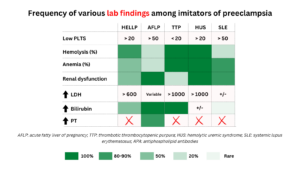
Differential diagnosis
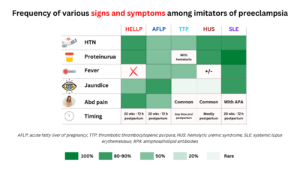
- Thrombocytopenia with macroangiopathic hemolytic anemia during pregnancy:
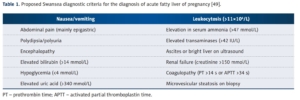
- Acute fatty liver of pregnancy (AFLD):
- Typically occurs in the third trimester between the 30th and 38th gestational weeks.
- Pathophysiology:
- Associated with microvesicular fatty infiltration of hepatocytes.
- May result from mitochondrial fatty acid beta-oxidation dysfunction, including deficiency of long-chain 3-hydroxyacyl-coenzyme A dehydrogenase (LCHAD).
- Patients may present with with a 1 to 2 week history of:
- Malaise
- Anorexia
- Nausea and vomiting
- Mild epigastric or right upper abdominal pain (reported in 50%-80% of cases)
- Headache
- Jaundice
- Symptoms associated with hepatic encephalopathy in advanced disease including:
- Mental status changes
- Asterixis (flapping tremor)
- Mood and behavior change
- Hypertension and proteinuria may be present.
- Labs reveal acute liver failure.
- Risk factors include multigravidas, preeclampsia, multiple gestation, and male fetus.
- Proposed diagnostic criteria (Swansea) for acute fatty liver of pregnancy includes ≥ 6 of the following in the absence of alternative diagnosis:
- Vomiting
- Abdominal pain
- Polyuria/polydipsia
- Encephalopathy
- Hypoglycemia (< 4 mmol/L [< 72 mg/dL])
- Leukocytosis (> 11 × 109 /L)
- Ascites or bright liver on ultrasound
- Elevated serum:
- Bilirubin (> 14 mcmol/L)
- Urate (> 340 mcmol/L)
- transaminases (alanine transaminase [ALT], aspartate aminotransferase [AST] > 42 units/L)
- Ammonia (> 47 mcmol/L)
- Renal impairment (creatinine > 150 mcmol/L)
- Coagulopathy (prothrombin time > 14 seconds or activated partial thromboplastin time > 34 seconds)
- Microvascular steatosis on liver biopsy
- May be complicated by:
- DIC
- Gastrointestinal bleeding
- Acute renal failure
- Pancreatitis
- Compared with HELLP:
- Both present late in pregnancy and can have similar features.
- Presence of hypoglycemia and prolonged prothrombin time may indicate acute fatty liver of pregnancy rather than HELLP syndrome.
- Acute fatty liver of pregnancy (AFLD):
Med Sci Monit, 2018; 24: 4080-4090
-
- Thrombotic thrombocytopenia purpura (TTP):
- Pregnancy is a clear trigger for TTP.
- Tends to occur most frequently during the second and third trimesters.
- Pregnancy-associated TTP accounts for 10% to 30% of all adult cases of TTP.
- Pathophysiology:
- Results from a severe congenital (disproportionately higher representation in pregnancy vs non-pregnancy compared with acquired form) or acquired deficiency in ADAMTS13, the specific metalloproteinase that cleaves ultralarge (UL) multimers of von Willebrand factor (VWF),
- Thrombosis occurs in the placenta in untreated TTP pregnancies and results in fetal growth restriction, intrauterine fetal death and preeclampsia.
- Characterized by:
- Neurological dysfunction including:
- Headache
- Visual disturbances
- Confusion
- Aphasia
- Transient paresis
- Weakness
- Seizures
- Fever
- Abdominal pain
- Bleeding
- Neurological dysfunction including:
- Features that should prompt consideration of TTP as the cause of TMA in a pregnant woman include:
- Presentation prior to 20 weeks
- Severe neurologic symptoms
- Cardiac injury
- Treatment is with plasma exchange, typically started based on high suspicion of the diagnosis while the ADAMTS13 levels are pending.
- Continued risk of relapse during subsequent pregnancies.
- Hemolytic uremic syndrome (HUS):
- Pregnancy is a clear trigger for HUS, specifically complement-mediated HUS (formerly known as atypical HUS).
- Pregnancy-associated HUS represents 16% of all atypical HUS (aHUS) cases occurring in women aged 18 to 45 years.
- Usually presents in the post-partum period with signs and symptoms of renal failure.
- Associated with inherited genetic mutations in complement or autoantibodies that result in overactivation of the complement pathway.
- Only form of thrombotic microangiopathy (TMA) to occur most frequently (three-fourths of cases) in the postpartum period (up to 3 months after delivery).
- TMA starting in the postpartum of an uneventful pregnancy is very suggestive of complement-mediated aHUS (though pregnancy-associated HUS may occur during any trimester).
- aHUS is a diagnosis of exclusion.
- Systemic lupus erythematosus (SLE) flare:
- May affect multiple organ systems including:
- Kidneys
- Lungs
- Heart
- Liver
- Brain
- The clinical and laboratory findings in women with lupus nephritis are similar to those with severe preeclampsia
- May affect multiple organ systems including:
- Thrombotic thrombocytopenia purpura (TTP):
British Journal of Haematology, 2012, 158, 323–335
- Both preeclampsia and HELLP syndrome have also been reported to occur concurrently or as a result of TTP or HUS.
Complications and prognosis
- Maternal complications include:
- Spontaneous rupture of a subcapsular liver hematoma (1% to < 2% of cases):
- Most often occurs in the right liver lobe.
- Typically present with:
- Sudden-onset severe pain in the epigastric and right upper abdominal quadrant radiating to the back
- Right shoulder pain
- Anemia
- Hypotension
- Morality 18%-86%
- Cerebral infarction and intracerebral hemorrhage
- Disseminated intravascular coagulation (DIC)
- 38% of cases in one series
- Most often related to placental abruption
- Abruptio placentae, which increases the risk of:
- DIC
- Pulmonary edema
- Renal failure
- Maternal mortality 1.1-25%
- Spontaneous rupture of a subcapsular liver hematoma (1% to < 2% of cases):
- Neonatal complications:
- Neonatal thrombocytopenia occurs in between 15% and 38% of cases
- Perinatal mortality rate related to the HELLP syndrome is between 7.4% and 34%:
- 34% before 32 weeks of gestation
- 8% after the 32nd gestational week
- Leading causes of neonatal death:
- Prematurity
- Placental insufficiency
- Intrauterine growth restriction (IUGR)
- Abruptio placentae
- The outcome of complete HELLP syndrome is worse that that of partial HELLP 1
- After a previous HELLP syndrome, the recurrence rate is 18% for preeclampsia and 7% for HELLP syndrome.
- Prevention of this recurrence is based on low-dose aspirin (75-150 mg per day) once a day in the evening, started before 16 weeks of gestation.
Treatment
- Management of patients presenting before delivery:
- Treat hypertensive crisis with antihypertensive such as IV labetalol.
- Patients with severe right upper quadrant/epigastric pain may have hepatic bleeding or hepatic swelling. Treat accordingly.
- Patients with disseminated intravascular coagulation (DIC), pulmonary edema, or acute kidney injury should be stabilized and delivered.
- Delivery is the mainstay of treatment:
- Prompt delivery is indicated after maternal stabilization for any of the following:
- Hepatic bleeding, DIC, pulmonary edema, or acute kidney injury
- Pregnancies ≥34 weeks of gestation
- Pregnancies that have not reached a stage of fetal maturity that ensures a reasonable chance of extrauterine survival.
- Fetal demise.
- Placental abruption
- Otherwise delivery may be delayed until a course of antenatal corticosteroids to promote fetal pulmonary maturity (for example, betamethasone) has been administered and completed (48 h after first injection) in those whose gestational age is above the lower limit of viability and <34 weeks of gestation.
- Conservative management for more than 48 hours (expectant management) is investigational.
- ACOG practice bulletin summary:
- Delivery is recommended when gestational hypertension or preeclampsia with severe features is diagnosed at or beyond 34 0/7 weeks of gestation, after maternal stabilization or with labor or prelabor rupture of membranes.
- Delivery should not be delayed for the administration of steroids in the late preterm period.
- Most women (about 80%) with HELLP syndrome have delivery by caesarean section.
- Prompt delivery is indicated after maternal stabilization for any of the following:
- Other supportive treatment includes:
- RBC transfusion, for example if the hemoglobin is <7 g/dL.
- Platelet transfusion at time of delivery if the platelet count is less than 20,000 cells/microL.
- Therapeutic plasma exchange has no benefit in patients with HELLP.
- Management of patients presenting before delivery:
- All of the signs and symptoms of HELLP, including subcapsular hematoma and liver rupture, can initially appear in the postpartum period.
- Treatment is similar to that of HELLP diagnosed before birth, except fetal status no longer needs to be considered.
Prev
1 / 0 Next
