Anatomy and Physiology of the Thyroid Gland
1. Thyroid Anatomy
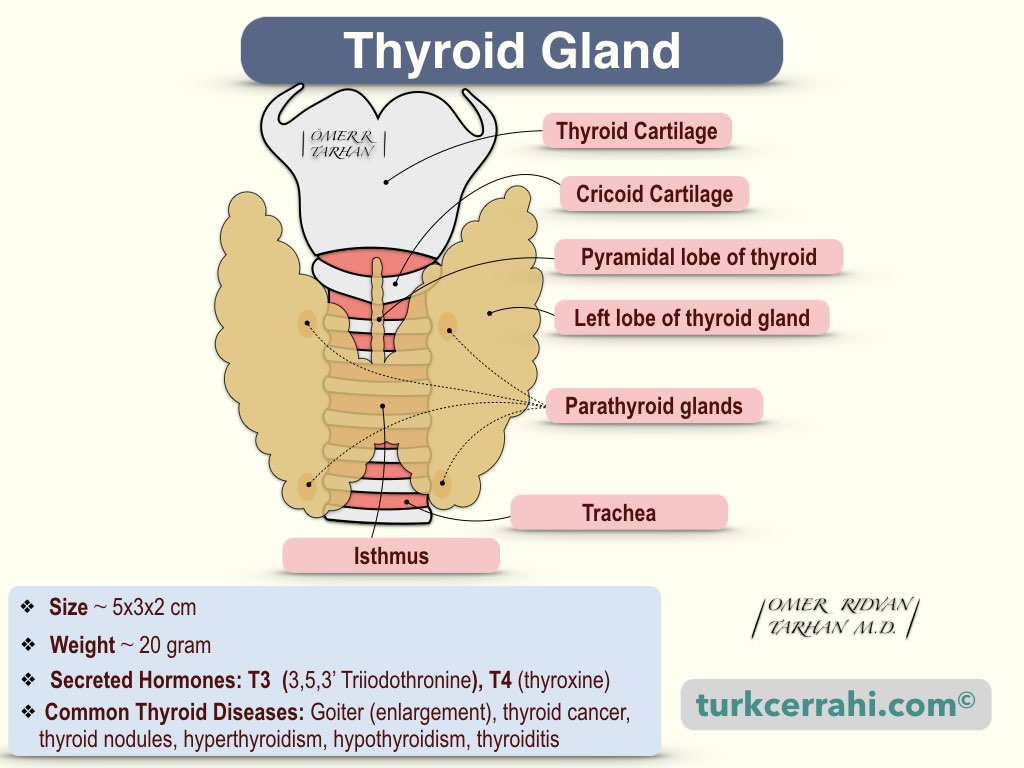
The thyroid, or thyroid gland, is an endocrine gland (it produces hormones) in the anterior part of the neck, consisting of two lobes connected by an isthmus. The thyroid gland is located under the laryngeal prominence (Adam's apple) in the front of the neck, between 2-4 tracheal rings. Each lobe is approximately 5x3x2 cm (height, width, and depth). Thyroid means shield-shaped in Latin (thyroides).
The pyramidal lobe, which extends upward from the isthmus, is found in 50% of people. The pyramidal lobe, a thin epithelial tube, a fibrous cord, or the thyroglossal duct may all extend to the foramen cecum at the base of the tongue. Because the thyroid gland develops near the base of the tongue, from the floor of the pharynx, and descends (along the thyroglossal duct). The thyroglossal duct disappears (typically) after birth. If the thyroglossal duct does not disappear completely, it may persist as a thyroglossal cyst or as a fistula extending into the foramen cecum (thyroglossal fistula).
Lingual thyroid is ectopic thyroid tissue that appears as a small nodule at the base of the tongue. Ectopic means located away from the normal position. The thyroid gland develops near the base of the tongue between the first and second pharyngeal pouches. A lingual thyroid is caused by developing thyroid tissue failing to migrate from the foramen cecum to its normal location in the neck.
Zuckerkandl's Tubercle is a pyramidal thyroid gland projection located posterior to the thyroid lobes and just lateral to the Berry's ligament. The significance of this projection is that the inferior laryngeal nerve passes just posteriorly or posteromedially to the tubercle of Zuckerkandl. As a result, the tubercle of Zuckerkandl serves as a landmark (or, for some, an arrow) for locating the inferior (recurrent) laryngeal nerve. The detection rate was 84% in cadaver studies and 69% in surgical studies (mean 76.5%).
The Zuckerkandl tubercle of the thyroid should not be confused with the Zuckerkandl organ, which may cause paraganglioma (Zuckerkandl body, aortic, or paraaortic body).
Capsules of the Thyroid Gland
Two capsules cover the thyroid gland: an inner true capsule and an outer false capsule.
True Capsule of Thyroid (Anatomical Capsule, Inner)
The anatomic capsule of the thyroid is a connective tissue structure that covers the thyroid gland, adheres to it, enters between the septa, and even forms the thyroid stroma.
False Capsule of Thyroid (Surgical Capsule, Outer)
Outside of the anatomical capsule, it is a looser connective tissue surrounding the thyroid. It is an extension of the deep cervical fascia.
Berry Ligament (Suspensory Ligament of Thyroid Gland)
The pseudocapsule (surgical or outer capsule) thickens and firmly connects the thyroid lobe (medially) to the cricoid cartilage. The reason why the thyroid gland moves with swallowing is the strong connection of this ligament to the trachea. The main significance of this ligament is that the inferior (recurrent) laryngeal nerve enters the larynx at a distance of 1-2 mm from the Berry ligament. Also, several thin (millimeter-sized) arteries enter the thyroid gland through the Berry ligament. These small arteries should be grasped and ligated with mosquito forceps. If the arteries are cut without ligation, they will bleed, and the cut artery tip will escape into the tissue. As a result, nerve injury occurs mostly at the end of a lobectomy or total thyroidectomy.
2. Arteries of the Thyroid
The thyroid gland has two pairs of arteries on the right and left.
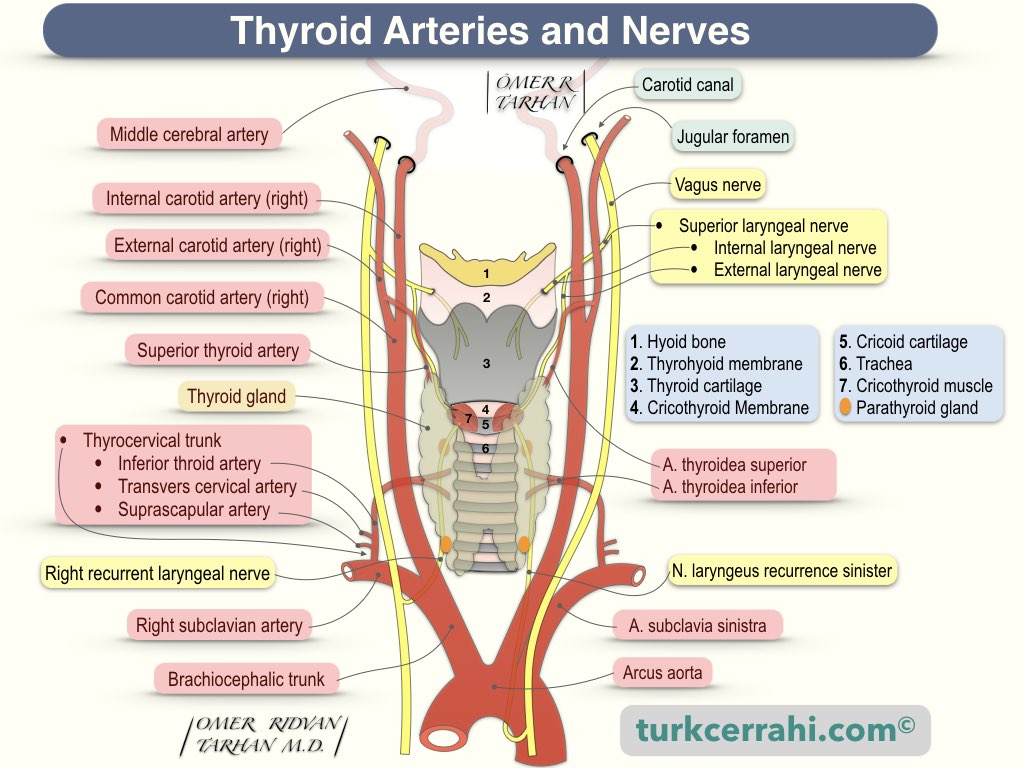
Superior Thyroid Artery
The Superior Thyroid Artery is the first branch of the external carotid artery. The superior thyroid artery originates near the carotid artery branching (same level, slightly above, slightly below). When the superior thyroid artery reaches the upper pole of the thyroid, it divides into two branches (the anterior and posterior glandular branches). The anterior branch continues from the upper part of the thyroid gland and merges with the other side (anastomoses). The posterior branch supplies the superior parathyroid gland with branches and connects with the inferior thyroid artery.
Inferior Thyroid Artery
The Inferior Thyroid Artery is the third branch of the thyrocervical trunk: 1. suprascapular artery; 2. transverse cervical artery; 3. inferior thyroid artery (terminal branch). The inferior thyroid artery divides into two or three branches in the posteromedial portion of the thyroid lobe. The inferior (recurrent) laryngeal nerve passes in front of, behind, or between branches of the inferior thyroid artery. During the surgical procedure, the recurrent laryngeal nerve is searched in this region. The lowest branch of the inferior thyroid artery supplies the inferior parathyroid gland.
Thyroid Ima Artery
The thyroid ima artery is an anatomical variant found in 3-10% of individuals. It is a single, unpaired artery. The thyroid IMA artery may originate from the brachiocephalic artery, aortic arch, or left common carotid artery. It runs in front of the trachea and enters the thyroid around the isthmus. Its importance is that it may bleed during the tracheostomy procedure.
3. Veins of the Thyroid
Three pairs of veins drain the thyroid gland: the superior, middle, and inferior thyroid veins.
- The Superior Thyroid Vein drains into the internal jugular vein
- The Middle Thyroid Vein drains into the internal jugular vein.
- The Inferior Thyroid Vein drains into the right and left brachiocephalic veins
4. Nerves of the Thyroid
Both the superior and inferior laryngeal nerves are branches of the vagus nerve.
The Vagus nerve is the 10th cranial nerve and originates from the spinal accessory nucleus (medulla oblongata) > jugular foramen > carotid sheath (neck; between the internal carotid artery and internal jugular vein) > chest > abdomen.
Superior Laryngeal Nerve
The superior laryngeal nerve is a branch of the vagus nerve. The cricothyroid muscles are innervated by the superior laryngeal nerve (external branch). All other intrinsic laryngeal muscles are innervated by the inferior (recurrent) laryngeal nerve.
The superior laryngeal nerve has two branches
- External Branch of Superior Laryngeal Nerve (=External Laryngeal Nerve): It is a motor nerve that innervates the cricothyroid muscle.
- Internal Branch of Superior Laryngeal Nerve (=Internal Laryngeal Nerve): It is a sensory nerve, it consists of sensory fibers from the laryngeal mucosa.
The superior laryngeal nerve descends on either side of the pharynx and, behind the internal carotid artery, divides into two branches. The internal laryngeal nerve enters the larynx through the thyrohyoid membrane and then distributes throughout the mucosa. The external laryngeal nerve distributes (innervates) the cricothyroid muscle.
The external branch raises pitch by tensing the vocal cords via the cricothyroid muscle. The rate of superior laryngeal nerve injury after thyroidectomies is about 4%.
When the external laryngeal nerve is injured unilaterally, the pitch of the voice decreases (problems with low voices, inability to shout), and explosive sounds (P and T sounds) are diminished.
When the external laryngeal nerve is injured bilaterally, the voice becomes fatigued and hoarse. Bilateral injuries can cause vocal cord separation, which can lead to aspiration, especially when consuming liquid foods.
Inferior (Recurrent) Laryngeal Nerve
The inferior laryngeal nerve is referred to as recurrent because it ascends after separating from the vagus, while the vagus descends.
Inferior (recurrent) laryngeal nerves innervate all intrinsic muscles of the larynx except the cricothyroid muscle. The cricothyroid muscle is innervated by the superior laryngeal nerve. The intrinsic muscles of the larynx produce sound. Therefore, injury to the recurrent laryngeal nerve causes paralysis or paresis (weakness) of the ipsilateral (ipsilateral) vocal cord.
The right inferior (recurrent) laryngeal nerve leaves the vagus at the level of the right subclavian artery > passes in front of the right subclavian artery > returns immediately below the artery, and then returns > ascends through the tracheoesophageal groove > enters the larynx under the inferior constrictor muscle (behind the cricothyroid junction).
The left inferior (recurrent) laryngeal nerve leaves the vagus at the level of the aortic arch > passes in front of the aortic arch > returns immediately below the arch, then behind it > ascends through the tracheoesophageal groove > enters the larynx under the inferior constrictor muscle (behind the cricothyroid junction). The left recurrent laryngeal nerve is longer than the right, as it returns under the aortic arch.
5. Parathyroid Glands
Four parathyroid glands (two pairs) are located behind the thyroid's lateral lobes. The parathyroid glands are located outside the thyroid gland, inside the thyroid capsule. They are yellowish (light) brown to tan in color, lentil size, and shape (flat and ovoid).
The superior (upper) parathyroid glands are embryologically derived from the fourth pharyngeal pouch and then descend. Their location is relatively constant, approximately 1 centimeter above the entrance of the inferior thyroid arteries to the thyroid gland (lower cricoid cartilage).
The inferior (lower) parathyroid glands are embryologically derived from the fourth pharyngeal pouch and then descend. The inferior parathyroid glands are more variable in their location, usually near the lower poles of the thyroid gland. Occasionally, parathyroid glands can descend into the upper mediastinum.
Parathyroid glands resemble adipose tissue in color and structure. Sometimes it cannot be determined whether the removed tissue is parathyroid gland tissue or fatty tissue. In such a case, the surgeon immersed the tissue in a normal saline solution. If the tissue can swim (not sink), it is adipose tissue; if the tissue can't swim (sink), it is the parathyroid gland, and the parathyroid gland is fragmented into small pieces with a scalpel and usually reimplanted into the sternocleidomastoid or brachioradialis muscle (lateral forearm).
The parathyroid glands secrete parathyroid hormone (PTH). Parathyroid hormone increases the blood's (serum's) calcium concentration. Inadvertent removal or damage of the parathyroid glands during thyroid surgery (predominantly thyroidectomy) causes hypoparathyroidism, and hypoparathyroidism causes hypocalcemia (low blood calcium concentration).
6. Thyroid Hormones
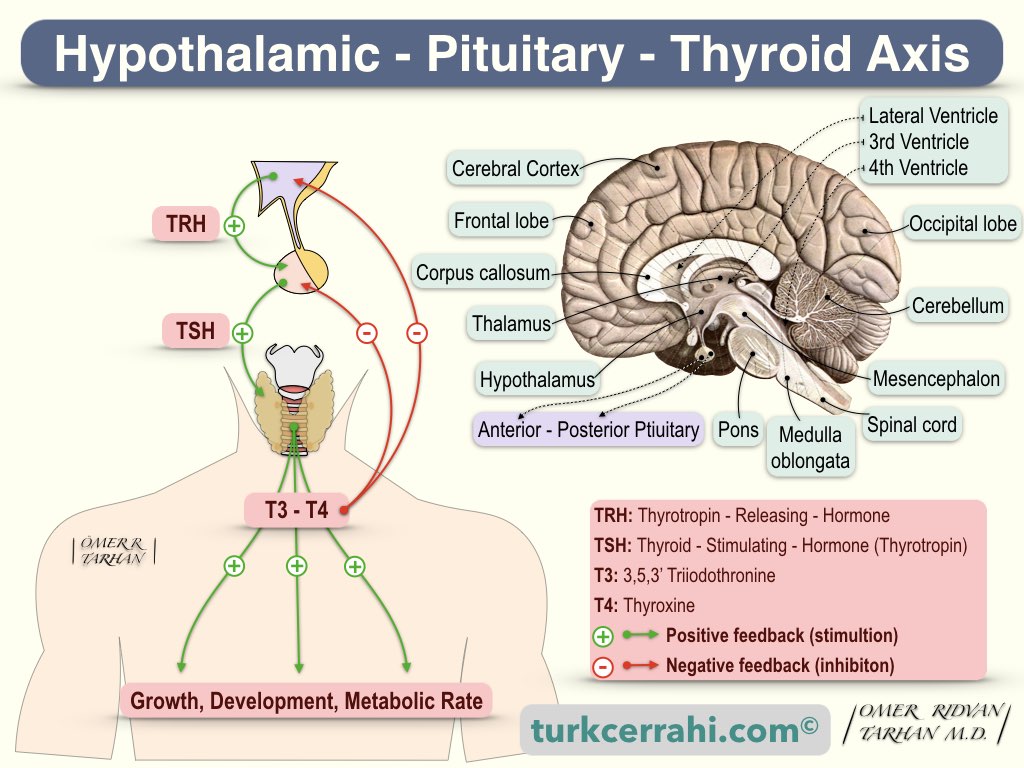
The function of the thyroid gland is to produce thyroid hormones. Thyroid hormones predominantly control the body's metabolism rate.
- Thyroid hormones increase the rate of metabolism, glycogenolysis, hepatic gluconeogenesis, intestinal glucose absorption, cholesterol synthesis, and degradation.
- Thyroid hormones affect the work of many organs. Thyroid hormones have positive inotropic and chronotropic effects on the heart, increase gastrointestinal motility, bone and protein turnover.
- Hyperthyroidism (too much of the thyroid hormones) causes diarrhea, and hypothyroidism ( low levels of the thyroid hormones) causes constipation.
- Thyroid hormones are necessary for children's growth and brain development (including the fetal period).
Thyroid hormones are iodized amino acids produced from tyrosine. T3 is 3,5,3'-triiodothyronine, and T4 is thyroxine (tetraiodothyronine). Thyroid hormones are synthesized and stored in the thyroid gland, bound to a protein called thyroglobulin. Thyroid hormones circulate in balance in the blood, both bound to thyroglobulin and free. However, only free thyroid hormones enter the cell and have biological effects.
Free thyroid hormones increase oxygen consumption, body temperature, heart rate, and metabolism (carbohydrate, fat, and protein metabolism are accelerated). The functioning of the thyroid gland, namely the secretion of thyroid hormone, is controlled by the TSH (thyroid-stimulating hormone) secreted from the anterior pituitary (adenohypophysis). TSH is controlled by TRH (Thyrotropin - Releasing Hormone), which is secreted from the hypothalamus. TRH stimulates the secretion of TSH, and TSH stimulates the secretion of T3 and T4. T3 and T4 inhibit the secretion of TSH and TRH. This control mechanism is called the “hypothalamic-pituitary-thyroid axis."
7. Anterior Pituitary (Adenohypophysis) Hormones
- FSH (Follicle Stimulating Hormone)
- LH (Luteinizing Hormone)
- Prolactin (prepares the breast for milk production during pregnancy and stimulates and maintains milk production (lactation) at the end of pregnancy)
- Growth Hormone
- ACTH (AdrenoCorticoTropic Hormone)
- TSH (Thyroid Stimulating Hormone).
8. Posterior Pituitary (Neurohypophysis) Hormones
- ADH (AntiDiuretic Hormone, Vasopressin)
- Oxytocin (Stimulates contractions of the uterus (induce labor) and ejection of milk)