Published online May 28, 2022. doi: 10.3748/wjg.v28.i20.2243
Peer-review started: November 28, 2021
First decision: January 8, 2022
Revised: January 12, 2022
Accepted: April 21, 2022
Article in press: April 21, 2022
Published online: May 28, 2022
Intramural duodenal hematoma is a rare condition described for the first time in 1838. This condition is usually associated with blunt abdominal trauma in children. Other non-traumatic risk factors for spontaneous duodenal haematoma include several pancreatic diseases, coagulation disorders, malignancy, collagenosis, peptic ulcers, vasculitis and upper endoscopy procedures. In adults the most common risk factor reported is anticoagulation therapy. The clinical presentation may vary from mild abdominal pain to acute abdomen and intestinal obstruction or gastrointestinal bleeding.
The aim of this case summary is to show a case of intramural spontaneous hematoma with symptoms of intestinal obstruction that was properly drained endoscopically by an innovative system lumen-apposing metal stent Hot AXIOS™ stent (Boston Scientific Corp., Marlborough, MA, United States).
Endoscopic lumen-apposing metal stent Hot AXIOS™ stent is a safe and feasible treatment of duodenal intramural hematoma in our case.
Core Tip: The present case explored the feasibility, safety and efficacy of endoscopic ultrasound-guided drainage of spontaneous duodenal hematoma. The new lumen-apposing self-expandable metallic stent Hot AXIOS™ could be considered a valid alternative to conventional endoscopic incision of the hematoma by using a needle-knife, a biopsy forceps or surgical drainage and percutaneous drainage to relieve pain and a persistent duodenal ulcer.
- Citation: Valerii G, Ormando VM, Cellini C, Sacco L, Barbera C. Endoscopic management of intramural spontaneous duodenal hematoma: A case report. World J Gastroenterol 2022; 28(20): 2243-2247
- URL: https://www.wjgnet.com/1007-9327/full/v28/i20/2243.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i20.2243
Intramural duodenal hematoma (IDH) is a rare intestinal condition described for the first time at autopsy in 1838[1], and the first source in the PubMed database accessing the MEDLINE database (http://www.ncbi.nlm.nih.gov/pubmed/) dates from 1952[2].
This condition is usually associated with blunt abdominal trauma in children[3] and upper endoscopy procedures (duodenal biopsy or injection therapy for bleeding peptic ulcers) or various non-traumatic conditions in adults (> 70% of cases). These include several pancreatic diseases even if the association remains unclear, such as certain coagulation disorders (anticoagulant therapy, haemophilia, Von Willebrand disease, Henoch-Schönlein purpura), malignancy, collagenosis, peptic ulcers and vasculitis[4-7].
Clinical symptoms for IDH may vary from vague abdominal pain to acute abdomen, intestinal obstruction or gastrointestinal bleeding[3,8], and diagnosis is subsequently confirmed by magnetic resonance imaging or computed tomography (CT) and upper gastrointestinal endoscopy (UGIE).
Most IDH cases resolve spontaneously or with correction of abnormal coagulation. Percutaneous drainage or surgery may be needed in some refractory IDH cases, malignancy, perforation and intestinal tract obstruction.
Here we present the use of the innovative lumen apposing metal stent catheter (LAMS) Hot AXIOS™ (Boston Scientific Corp., Marlborough, MA, United States) in the case of spontaneous IDH with intestinal substenosis, which was non-responsive to conservative management, in a patient without risk factors. This innovative device, with a lumen apposing self-expandable metal stent fitted onto an electrocautery-enhanced tip catheter, is safe and feasible in gallbladder drainage, choledochoduodenostomy and drainage of pancreatic fluid collections. In recent years, Hot AXIOS™ has also been used for off-label indications including gastrojejunostomy, gastro-gastrostomy and drainage of postsurgical collections. Herein we report the use of Hot AXIOS™ in the rare digestive disorder spontaneous IDH.
A 51-year-old man was admitted to the hospital with abdominal pain, bloating and vomiting.
The clinical data suggested a diagnosis of intestinal obstruction.
The patient did not report comorbidities or recent abdominal trauma without relevant previous medical history and in particular without having taken anti-platelet medication.
He did not have relevant family history.
Physical examination on admission revealed slight tenderness over the epigastric region and right flank.
Initial biochemical analysis indicated neutrophilic leukocytosis (13.07 × 109/L) and an increased level of C-reactive protein without alterations of serum haemoglobin, D-dimer, platelet function and coagulation parameters.
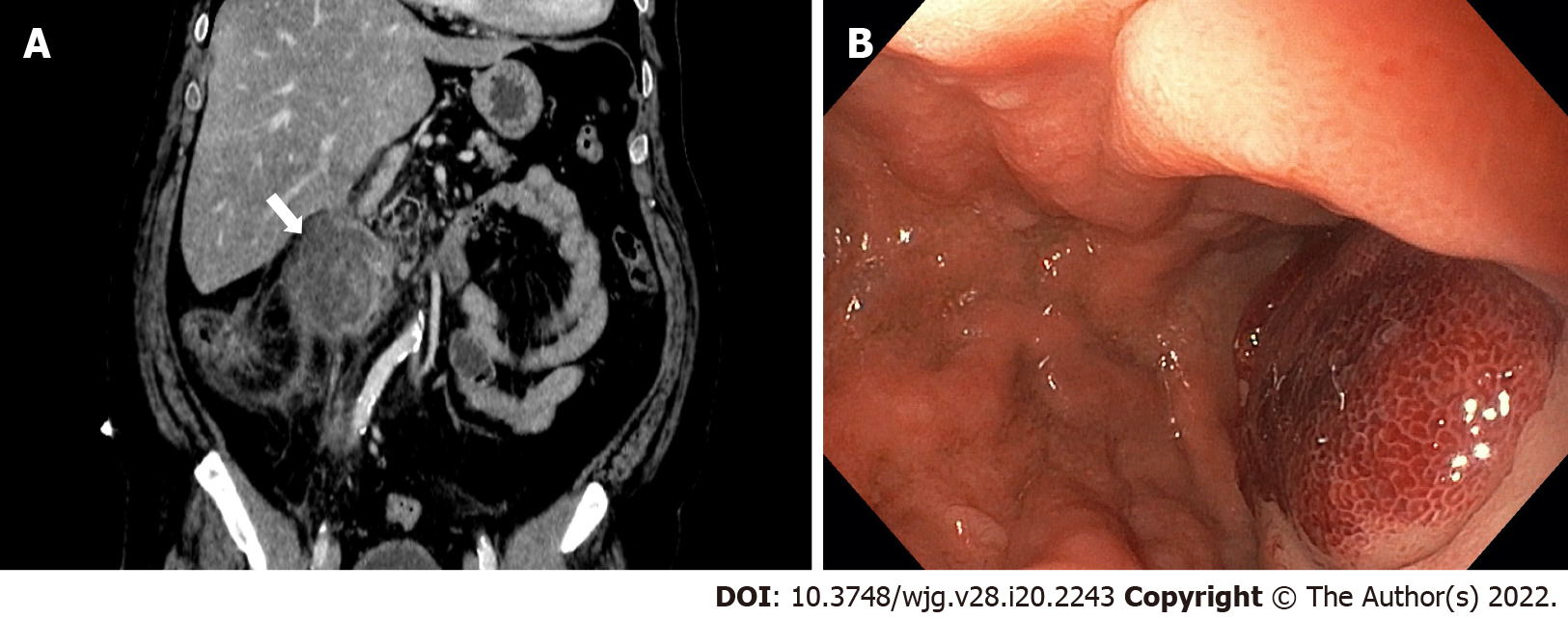
A contrast-enhanced abdominal CT scan revealed an IDH (Figure 1A). On admission UGIE and then endoscopic ultrasound (EUS) confirmed submucosal swelling of the second part of the duodenum that measured approximately 90 mm along the long axis with substenosis of the duodenal lumen (Figure 1B).
A conservative approach was attempted with clinical observation and empirical antibiotic therapy. The patient was discharged in good clinical condition after 8 d of intravenous antibiotic therapy.
Intramural spontaneous duodenal hematoma.
After 48 h the patient was readmitted to the hospital due to clinical relapse. Biochemical analysis indicated a significant increase of both leukocytosis and C-reactive protein, and the radiological evaluation confirmed the previous diagnosis. After 10 d a multidisciplinary evaluation was performed, and minimally invasive endoscopic treatment was proposed.
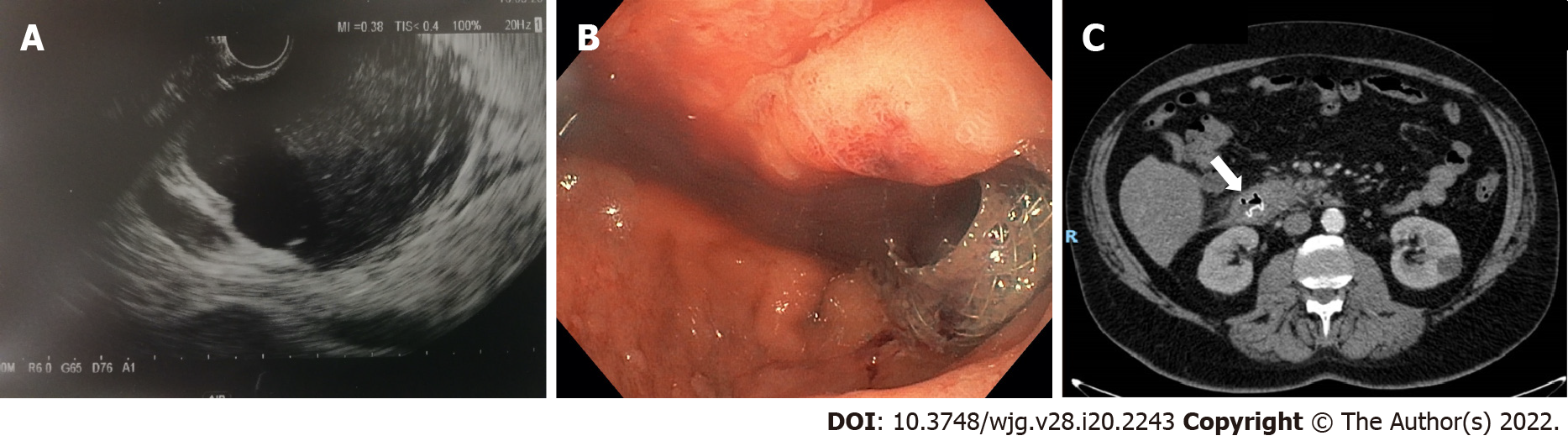
EUS-guided drainage was performed with the Hot AXIOS™ system. A direct LAMS 15 mm × 10 mm was inserted into the submucosa lumen with an electrocautery-enhanced tip catheter and released under complete EUS control after the second flange was deployed in the duodenal lumen (Figure 2A). UGIE control confirmed the correct LAMS placement, and hematinic material associated with slightly purulent drainage was observed (Figure 2B).
A control CT scan demonstrated the presence of LAMS and the complete drainage of the intramural collection (Figure 2C). The patient was discharged in good clinical condition after 7 d. After an additional 2 wk he repeated UGIE, which revealed a complete resolution of the duodenal bulging, and the LAMS was contextually removed with complete closure of the mucosal defect with a clip. At the 30-d follow-up the patient was completely asymptomatic.
IDH is a rare condition usually caused by trauma, anticoagulant therapy, rupture of a duodenal aneurysm or biopsy[4-7,9]. Rare cases of IDH have also been described as a consequence of acute pancreatitis[3] or after endoscopic retrograde cholangiopancreatography procedures[10].
CT and magnetic resonance imaging represent the most sensitive diagnostic exams for IDH. Radiological exams have a role both for diagnosis as well as follow-up of small bowel hematoma within 2 wk[11,12]. Once IDH is confirmed, conservative management with fasting and total parenteral nutrition should be given[13]. Traditionally, in the case of persistent IDH, surgical drainage[14,15] and percutaneous drainage were performed[16], both causing great trauma for the patient. The indications for surgical intervention are not well clarified, certainly in the case of occlusive symptoms over 7-10 d or where there is evidence of perforation with a generalized peritonitis[17].
To date there are few described cases of endoscopic drainage of duodenal hematoma. This consists of endoscopic incision of the hematoma using a needle-knife or a biopsy forceps in order to obtain rapid submucosal decompression[18,19] with improvement of abnormal laboratory findings and abdominal pain in up to 1 wk. The persistence of duodenal ulcer at the site of endoscopic incision has also been described with a complete resolution only after 1 mo[18].
In our case we had a patient with an unremarkable previous medical history, with no risk factors for IDH who presented with intestinal pseudo-obstruction symptoms and leukocytosis without evidence of pancreatitis. We first attempted a conservative approach according to the existing data, but after recurrence of symptoms an endoscopic approach was proposed.
The Hot AXIOS™ lumen-apposing stent is a novel double-flanged covered, self-expanding metal stent, safe and effective in gallbladder drainage, choledochoduodenostomy and drainage of pancreatic fluid collections. In the recent years, Hot AXIOS™ stents have also been used for off-label indications including gastrojejunostomy, gastro-gastrostomy and drainage of postsurgical collections.
Here we present the use of Hot AXIOS™ in a rare but possible digestive disorder with a rapid and complete resolution of this insidious clinical entity, as confirmed by CT scan and with only 7 d length of stay without abnormal laboratory findings and abdominal pain after the procedure.
In our experience Hot AXIOS™ is a safe and effective endoscopic procedure for the treatment of IDH, reserved for patients who are not responsive to conservative management. However, it should be performed by expert endoscopists trained in EUS and radiological procedures. To reduce the rate of postoperative complications and improve clinical outcome a previous careful clinical evaluation focusing on coagulopathies is mandatory.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kumar R, India; Tanpowpong P, Thailand S-Editor: Yan JP L-Editor: Filipodia P-Editor: Yan JP
| 1. | McLauchlan J. False aneurysmaltumouroccupyingnearly the whole of the duodenum. Lancet. 1838;2243-2247. [DOI] [Cited in This Article: ] |
| 2. | Dey DL. Acute duodenal obstruction due to an intramural haematoma. Med J Aust. 1952;1:708. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Kumar R, Athwal PSS, Kumar M, Devi K, Kahlon S. Spontaneous Intramural Duodenal Hematoma: A Rare Complication of Pancreatitis. Cureus. 2020;12:e8491. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Chang CM, Huang HH, How CK. Acute pancreatitis with an intramural duodenal hematoma. Intern Med. 2015;54:755-757. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Eichele DD, Ross M, Tang P, Hutchins GF, Mailliard M. Spontaneous intramural duodenal hematoma in type 2B von Willebrand disease. World J Gastroenterol. 2013;19:7205-7208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 12] [Cited by in F6Publishing: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Frostick SP, Collin J, Daar AS, Kettlewell M, Nolan DJ. Non-traumatic intramural haematoma: an unusual cause of duodenal obstruction. Br J Surg. 1984;71:313-314. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Tseng CY, Fan JS, Yang SC, Huang HH, Chen JD, Yen DH, Huang CI. Anticoagulant-induced intramural intestinal hemorrhage. Am J Emerg Med. 2010;28:937-940. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Kang EA, Han SJ, Chun J, Lee HJ, Chung H, Im JP, Kim SG, Kim JS, Yoon H, Shin CM, Park YS, Kim N, Lee DH, Jung HC. Clinical features and outcomes in spontaneous intramural small bowel hematoma: Cohort study and literature review. Intest Res. 2019;17:135-143. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Iuchtman M, Steiner T, Faierman T, Breitgand A, Bartal G. Post-traumatic intramural duodenal hematoma in children. Isr Med Assoc J. 2006;8:95-97. [PubMed] [Cited in This Article: ] |
| 10. | Pan YM, Wang TT, Wu J, Hu B. Endoscopic drainage for duodenal hematoma following endoscopic retrograde cholangiopancreatography: a case report. World J Gastroenterol. 2013;19:2118-2121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 9] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Abbas MA, Collins JM, Olden KW, Kelly KA. Spontaneous intramural small-bowel hematoma: clinical presentation and long-term outcome. Arch Surg. 2002;137:306-310. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 51] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Zhou H, Ma X, Sheng M, Lai C, Fu J. Evolution of intramural duodenal hematomas on magnetic resonance imaging. Pediatr Radiol. 2018;48:1593-1599. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Eurboonyanun C, Somsap K, Ruangwannasak S, Sripanaskul A. Spontaneous Intramural Duodenal Hematoma: Pancreatitis, Obstructive Jaundice, and Upper Intestinal Obstruction. Case Rep Surg. 2016;2016:5321081. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Banieghbal B, Vermaak C, Beale P. Laparoscopic drainage of a post-traumatic intramural duodenal hematoma in a child. J Laparoendosc Adv Surg Tech A. 2008;18:469-472. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Chirkov RN, Abakumov MM, Blokhin VN. [Diagnostics and surgical treatment of traumatic intramural duodenal haematomes]. Khirurgiia (Mosk). 2008;33-36. [PubMed] [Cited in This Article: ] |
| 16. | Kwon CI, Choi KH, Ko EH, Lee JH, Song YJ, Ko KH, Hong SP, Park PW. [A case of duodenal intramural hematoma treated by percutaneous external drainage]. Korean J Gastroenterol. 2007;49:45-49. [PubMed] [Cited in This Article: ] |
| 17. | Jewett TC Jr, Caldarola V, Karp MP, Allen JE, Cooney DR. Intramural hematoma of the duodenum. Arch Surg. 1988;123:54-58. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 70] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Kwon CI, Ko KH, Kim HY, Hong SP, Hwang SG, Park PW, Rim KS. Bowel obstruction caused by an intramural duodenal hematoma: a case report of endoscopic incision and drainage. J Korean Med Sci. 2009;24:179-183. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Lee JY, Chung JS, Kim TH. Successful endoscopic decompression for intramural duodenal hematoma with gastric outlet obstruction complicating acute pancreatitis. Clin Endosc. 2012;45:202-204. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |