Published online Aug 16, 2023. doi: 10.12998/wjcc.v11.i23.5573
Peer-review started: May 19, 2023
First decision: June 1, 2023
Revised: June 10, 2023
Accepted: July 21, 2023
Article in press: July 21, 2023
Published online: August 16, 2023
Recent reports have described cases of metachronous breast metastasis in patients with nasopharyngeal carcinoma. However, no similar cases of synchronous breast metastasis have been reported, and evidence that can be used to support the clinical diagnosis of stage IV nasopharyngeal carcinoma in patients with concu
We report the case of a 46-year-old woman who visited our hospital with a right breast mass as the first symptom. The first pathological biopsy report suggested triple-negative breast invasive carcinoma. Subsequent imaging revealed a nasopharyngeal mass. Further puncture biopsy of the nasopharyngeal mass, molecular pathological Epstein–Barr virus in situ hybridization, and immunohistochemistry confirmed the diagnosis of nasopharyngeal carcinoma with breast metastasis. The patient did not undergo a mastectomy and achieved complete remission after chemotherapy and radiotherapy. She continued to receive oral chemotherapy as maintenance therapy and experienced no recurrence or metastasis during the 6-month follow-up period.
This case report suggests that breast specialists should carefully rule out secondary breast cancers when diagnosing and treating breast masses. Furthermore, clinicians should aim to identify the pathological type of the tumor to obtain the most accurate diagnosis and prevent excessive diagnosis and treatment.
Core Tip: The most common sites of distant metastasis in patients with nasopharyngeal carcinoma (NPC) are the bones, lungs, liver, and distant lymph nodes; metastasis to the breast is rare. To date, only a few cases of NPC metastasis to the breast have been reported in the literature, and all occurred secondary to the diagnosis and treatment of NPC. Here, we present the clinical characteristics, treatment strategies, and follow-up information for a patient with newly diagnosed stage IV NPC who developed synchronous breast metastasis. Furthermore, we conducted a literature review to provide evidence for comprehensive management of this condition.
- Citation: Lei YY, Li DM. Nasopharyngeal carcinoma with synchronous breast metastasis: A case report. World J Clin Cases 2023; 11(23): 5573-5579
- URL: https://www.wjgnet.com/2307-8960/full/v11/i23/5573.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i23.5573
Nasopharyngeal carcinoma (NPC) is a type of head and neck cancer with a distinct geographical distribution, representing a significant public health problem in Eastern and Southeast Asia[1]. In 2013, there were approximately 42100 new cases of nasopharyngeal cancer and 21320 related deaths in China, accounting for 1.14% of all new cancer cases and 0.96% of all tumor-related deaths in that year[2]. Advancements in screening and treatment strategies have resulted in a gradual decline in the incidence and mortality of these diseases in recent decades[3,4]. However, approximately 30% of patients with NPC continue to experience a poor prognosis, mostly due to distant metastasis[5].
Distant metastasis is among the leading causes of death in patients with NPC, including both synchronous distant metastases identified at diagnosis and metachronous distant metastases identified after systematic therapy[5,6]. The most common sites of distant metastasis of NPC are the bone, lungs, liver, and distant lymph nodes, while metastasis to the breast is rare[7]. To date, only a few cases reports have described metastasis of NPC to the breast[8-10], all of which occurred secondary to the diagnosis and treatment of NPC.
In this report, we discuss a newly diagnosed case of stage IV NPC with synchronous breast metastasis in terms of clinical characteristics, treatment strategies, and follow-up. Furthermore, we summarize the findings from a review of the relevant literature to provide evidence that can aid in the comprehensive management of this condition.
A 46-year-old female patient visited Sun Yat-sen University Affiliated Cancer Hospital because of advanced NPC with synchronous breast metastasis.
On 28 September 2020, the patient visited the Guangdong Chinese Medicine Hospital Zhuhai Branch because of a breast mass.
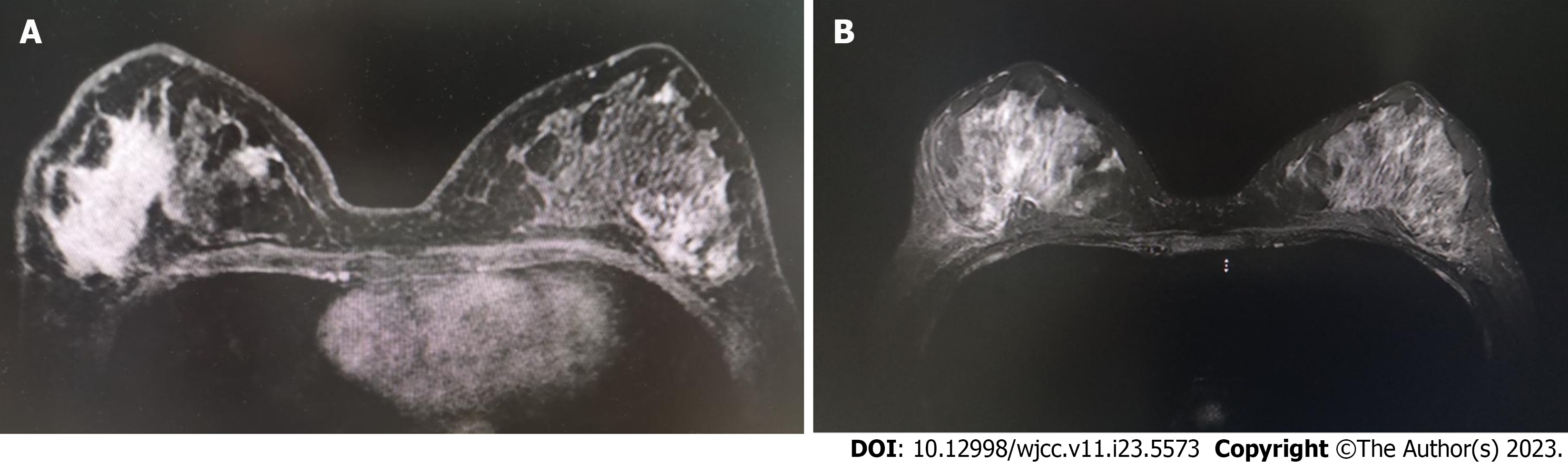
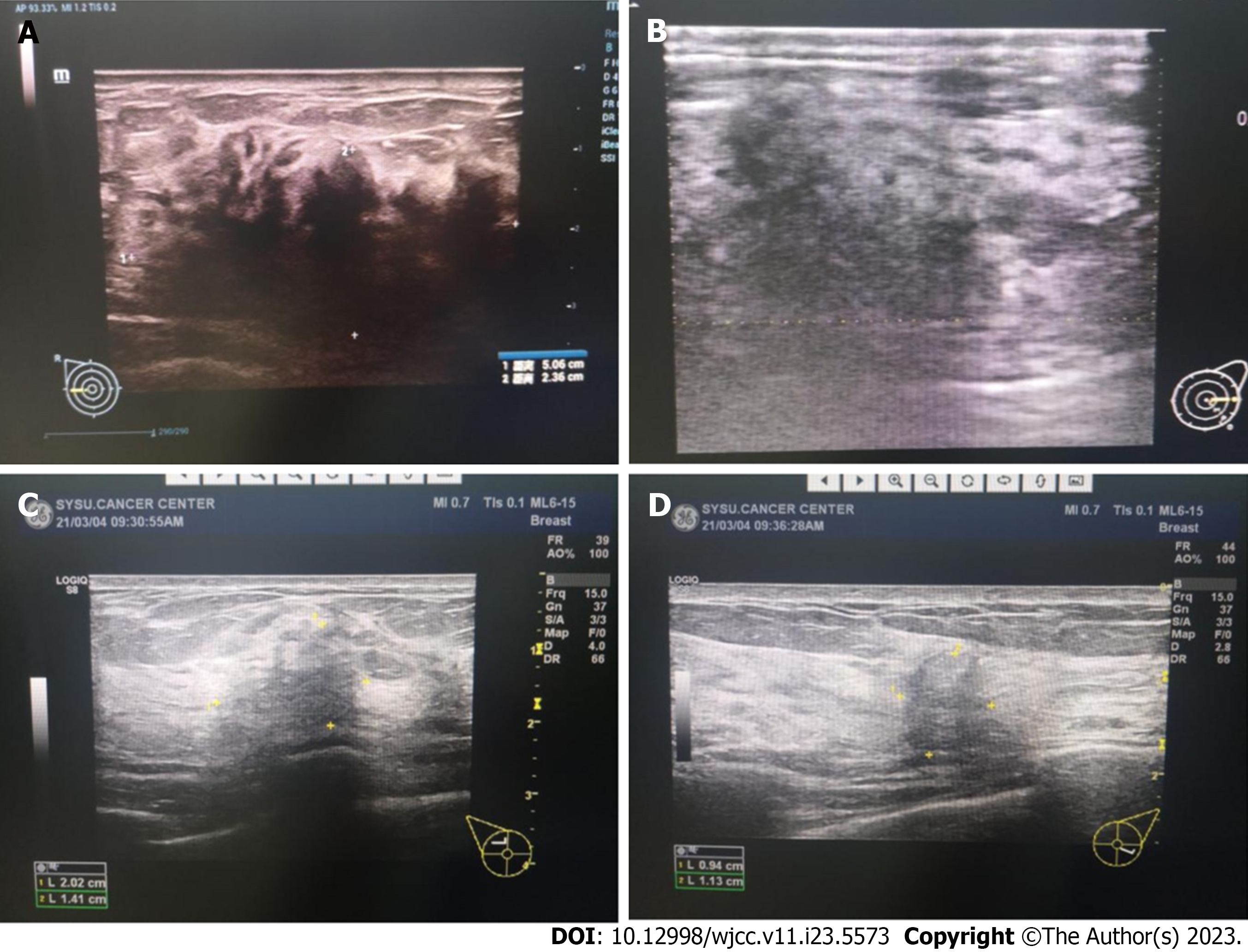
Breast ultrasonography revealed a solid mass (57 × 25 × 51 mm) in the right breast with a breast imaging reporting and data system score of 4C (suspicious of breast cancer)[11,12] and an enlarged and abnormal structure in the right axillary lymph node. A core needle biopsy (CNB) was performed for the right breast lesions (Figure 1) and right axillary lymph nodes. Subsequent pathological examination revealed that the tissue within the right breast mass was consistent with invasive breast carcinoma. Immunohistochemical results were as follows: ER (-), PR (-), HER-2 (-), Ki67 (approximately 60% +), CK (+), GATA3 (-), P63 (partial +), Calponin (deletion of myoepithelium), CD68 (-), E-cad (+), P120 (cell membrane +), and CK7 (-). Metastatic cancer was detected in the biopsy sample of the right axillary lymph node tissue. Immunohistochemical results were as follows: GATA3 (scattered/weak +) and S-100 (scattered +). Given these findings, right invasive breast cancer with right axillary lymph node metastasis was considered.
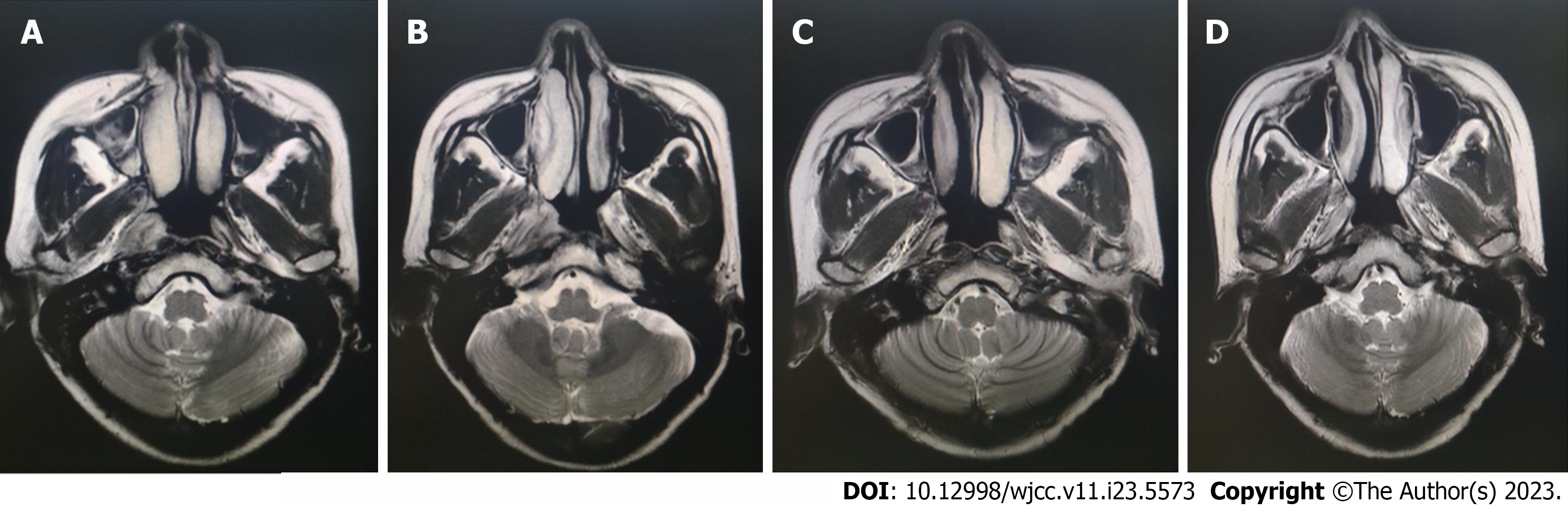
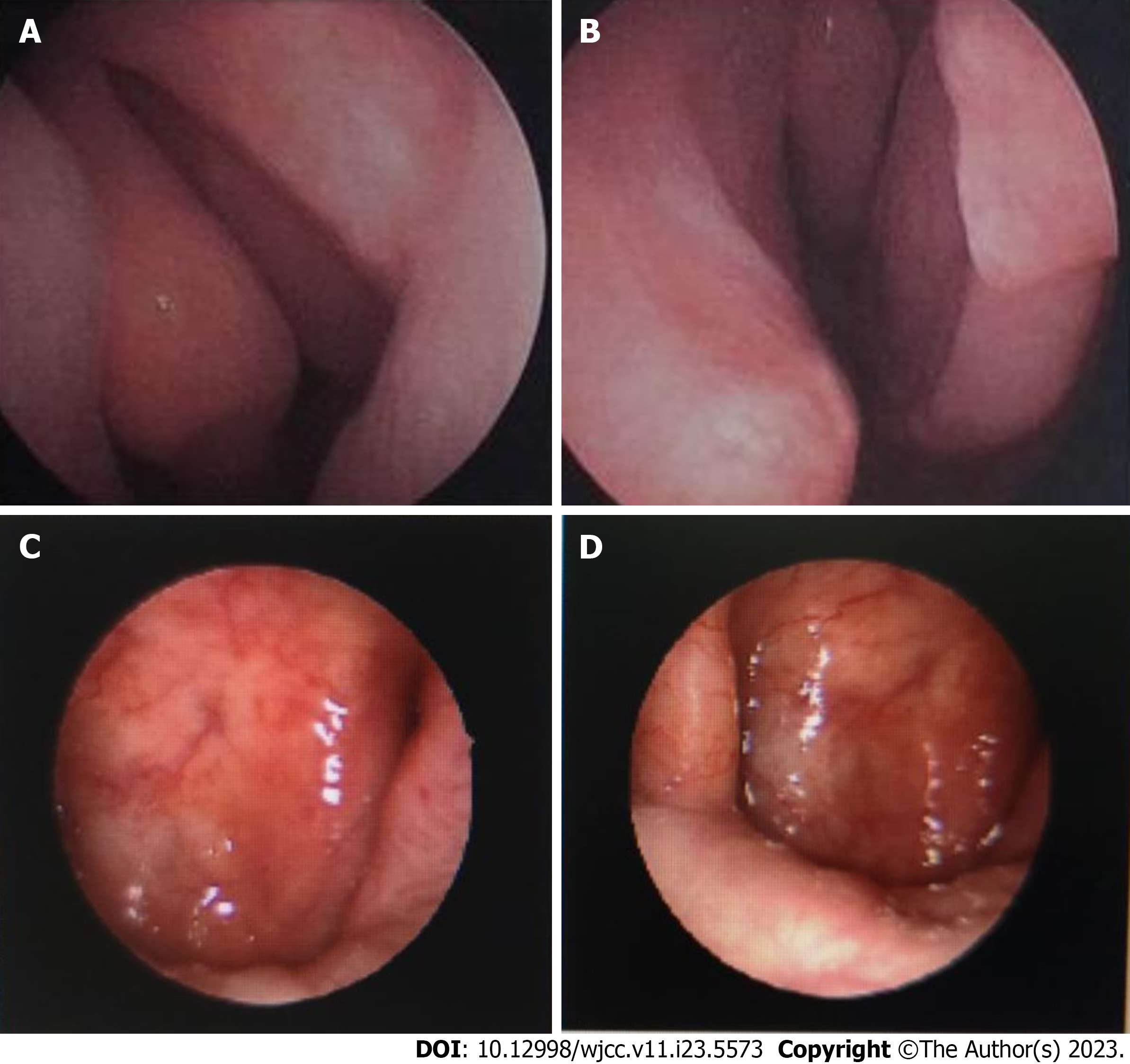
Since the breast tumor was accompanied by lymph node metastasis, a detailed general examination was subsequently performed. Subsequent magnetic resonance imaging (MRI) of the head revealed thickening of the nasopharyngeal lateral wall and a shallow pharyngeal recess on the right side (Figure 2). Breast MRI (Figure 1) and breast ultrasound (Figure 3) revealed suspicious bilateral masses. Based on the MRI results, nasopharyngeal endoscopy plus biopsy (Figure 4), in situ hybridization Epstein–Barr virus (EBV) examination of the breast tumor specimen obtained via CNB, and whole-body positron emission tomography/computerized tomography (PET-CT) were performed. Nasopharyngeal endoscopic biopsy of tissues obtained from the top of the right nasopharynx revealed undifferentiated non-keratinizing carcinoma (Figure 4) and a positive in situ hybridization result for EBV in some cells of the breast and lymph node tissue, while immunohistochemical examination for Ki67 indicated 80% positivity. Whole-body PET-CT revealed thickening of the right nasopharyngeal wall.
Based on these findings, stage IV NPC with bilateral breast and axillary metastases was the primary diagnosis. The investigators recommended chemotherapy and follow-up radiotherapy. However, the patient visited Guangzhou for further diagnosis and treatment after being discharged for personal reasons.
The patient had no history of infectious diseases, family history of breast cancer, or history of other malignancies.
Physical examination revealed that the patient’s right supraclavicular lymph node was swollen, with a hard mass (approximately 1.0 cm × 1.0 cm in size, clear boundaries, and poor activity). There was no palpable mass in the left breast or axillary area. Furthermore, there were no palpable masses in the neck lymph nodes, and general physical examination revealed no obvious abnormalities.
The breast mass, bilateral axillary lymph nodes, and right cervical lymph nodes were re-biopsied. The pathological findings were consistent with those of nasopharyngeal undifferentiated non-keratinizing cancer metastasis to the breast. In addition, in situ hybridization of EBV was positive in all examined tissues.
The breast mass, bilateral axillary lymph nodes, and right cervical lymph nodes were re-biopsied. The pathological findings were consistent with those of nasopharyngeal undifferentiated non-keratinizing cancer metastasis to the breast. In addition, in situ hybridization of EBV was positive in all examined tissues.
The patient received six cycles of paclitaxel plus carboplatin chemotherapy (albumin-paclitaxel, 200 mg, Day1 and Day7+; carboplatin, 40 mg, Day1-Day3) from 26 October 2020 to 10 February 2021. The chemotherapy dose was determined based on the patient’s skin area. Tomo-direct radiotherapy was initiated on 26 March 2021, with a planned radiotherapy dose of PGTVnx69 Gy/30 F and PGTVnd63 Gy/30 F in the neck and face areas, respectively. The planned number of radiotherapy sessions was 30. However, only 26 radiotherapy sessions were completed at the patient’s discretion.
After completing six cycles of chemotherapy and radiotherapy, the patient underwent CNB for both breast nodules. MRI (Figures 2C) and nasopharyngeal endoscopy (Figure 4C and D) performed after treatment revealed complete remission of the tumor in the nasopharynx. In addition, breast MRI (Figure 2C and D) and ultrasound (Figure 3C and D) performed after six cycles of chemotherapy revealed remission of the breast lesions. No cancer was found on pathological examination, and complete remission had been achieved. As the patient had advanced NPC, oral maintenance therapy was continued with capecitabine at 1000 mg bid. Each cycle included a two-week treatment, followed by a one week off treatment.
Follow-ups were scheduled every 3 mo. During the follow-up visit, in addition to the physical examination, ultrasound examinations of the breast and axillary areas, bilateral supraclavicle, uterus, and abdomen were performed. Furthermore, chest computed tomography and nasopharyngeal MRI scans were reviewed every 6 mo. A systemic examination in December 2021 revealed no recurrence or metastasis.
Malignant tumors rarely metastasize to the breast, with a reported incidence of merely 0.5%–2.0% worldwide[13-15]. These tumors include malignant lymphoma; malignant melanoma; and lung, gastric, prostate, and ovarian cancers[15-17]. In recent years, cases of NPC metastases to the breast have been occasionally reported[8-10,15,18,19]. However, these reports described cases of metachronous breast metastases that developed after the diagnosis and treatment of NPC. Given this rare incidence, no systematic clinical studies have been conducted to date.
In the present case, the patient had a breast mass as the first sign, and CNB examination revealed invasive breast carcinoma and axillary lymph node metastasis. Primary NPC was detected by MRI and PET-CT, and repeated biopsies with immunohistochemical and EBV tests confirmed that the breast tumors were secondary to the NPC, thereby avoiding overtreatment. In the present case, lymphatic metastasis and obstruction may have been caused by lymphatic reflux to the breast[20].
The present case differs from metachronous breast metastases reported previously[8-10]. Based on our experience, patients with locally advanced tumors should first undergo a systematic examination, including craniocerebral CT/MR, to ensure better understanding of the patient’s condition and prevent omissions. Second, it is essential to clarify the specific pathological type of breast cancer. When the pathological type is unclear or results suggest triple-negative breast cancer, attention should be paid to the possibility of secondary breast metastasis.
No studies have definitively indicated that patients with breast metastases from NPC can benefit from modified radical mastectomy for breast cancer. Therefore, in the present case, systemic treatment of the metastatic tumors and radical radiotherapy for the primary NPC were performed. Efficacy evaluation at the six-month follow-up revealed complete remission. However, the short follow-up time represents a limitation of the present report. While regular reviews and follow-ups are being undertaken to monitor changes in the patient’s condition, further evidence is required to determine the optimal management strategies for this condition.
This case report suggests that breast specialists should carefully rule out secondary breast cancer during diagnosis and treatment. Furthermore, for patients with malignant tumors, the pathological type of the tumor should be identified to obtain the most accurate diagnosis and prevent excessive diagnosis and treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Simmons DG, Australia; Stenina-Adognravi O, United States S-Editor: Lin C L-Editor: A P-Editor: Cai YX
| 1. | Chen YP, Chan ATC, Le QT, Blanchard P, Sun Y, Ma J. Nasopharyngeal carcinoma. Lancet. 2019;394:64-80. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1109] [Cited by in F6Publishing: 1455] [Article Influence: 291.0] [Reference Citation Analysis (0)] |
| 2. | Wei KR, Zheng RS, Zhang SW, Liang ZH, Li ZM, Chen WQ. Nasopharyngeal carcinoma incidence and mortality in China, 2013. Chin J Cancer. 2017;36:90. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 164] [Cited by in F6Publishing: 208] [Article Influence: 29.7] [Reference Citation Analysis (0)] |
| 3. | Xu HF, Chen Q, Liu Y, Liu SZ, Guo LW, Zheng LY, Kang RH, Zhang SK. Incidence and mortality of nasopharyngeal carcinoma in Henan Province in 2016. Zhongguo Aizheng Fangzhi Zazhi. 2021;13:262-266. [DOI] [Cited in This Article: ] |
| 4. | Carioli G, Negri E, Kawakita D, Garavello W, La Vecchia C, Malvezzi M. Global trends in nasopharyngeal cancer mortality since 1970 and predictions for 2020: Focus on low-risk areas. Int J Cancer. 2017;140:2256-2264. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 5. | Li AC, Xiao WW, Shen GZ, Wang L, Xu AA, Cao YQ, Huang SM, Lin CG, Han F, Deng XW, Zhao C. Distant metastasis risk and patterns of nasopharyngeal carcinoma in the era of IMRT: long-term results and benefits of chemotherapy. Oncotarget. 2015;6:24511-24521. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 6. | Liao W, Tian M, Chen N. Characteristic And Novel Therapeutic Strategies Of Nasopharyngeal Carcinoma With Synchronous Metastasis. Cancer Manag Res. 2019;11:8431-8442. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Ahmad A, Stefani S. Distant metastases of nasopharyngeal carcinoma: a study of 256 male patients. J Surg Oncol. 1986;33:194-197. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 139] [Cited by in F6Publishing: 145] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Zhao JH, Pan Y, Gao B, Li YK, Wang M. Bilateral breast metastasis from nasopharyngeal carcinoma. Breast J. 2020;26:1045-1046. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Albasri AM. Nasopharyngeal carcinoma metastasis to the breast. Saudi Med J. 2020;41:1130-1134. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Sham JS, Choy D. Breast metastasis from nasopharyngeal carcinoma. Eur J Surg Oncol. 1991;17:91-93. [PubMed] [Cited in This Article: ] |
| 11. | Liberman L, Menell JH. Breast imaging reporting and data system (BI-RADS). Radiol Clin North Am. 2002;40:409-430. [DOI] [Cited in This Article: ] [Cited by in Crossref: 207] [Cited by in F6Publishing: 192] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 12. | Magny SJ, Shikhman R, Keppke AL. Breast Imaging Reporting and Data System. Treasure Island (FL): StatPearls Publishing. 2023. [PubMed] [Cited in This Article: ] |
| 13. | Vergier B, Trojani M, de Mascarel I, Coindre JM, Le Treut A. Metastases to the breast: differential diagnosis from primary breast carcinoma. J Surg Oncol. 1991;48:112-116. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 138] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 14. | Bitencourt AGV, Gama RRM, Graziano L, Negrão EMS, Sabino SMPS, Watanabe AHU, Guatelli CS, Souza JA, Mauad EC, Marques EF. Breast metastases from extramammary malignancies: multimodality imaging aspects. Br J Radiol. 2017;90:20170197. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 15. | Klingen TA, Klaasen H, Aas H, Chen Y, Akslen LA. Secondary breast cancer: a 5-year population-based study with review of the literature. APMIS. 2009;117:762-767. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Jones GE, Strauss DC, Forshaw MJ, Deere H, Mahedeva U, Mason RC. Breast cancer metastasis to the stomach may mimic primary gastric cancer: report of two cases and review of literature. World J Surg Oncol. 2007;5:75. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 17. | Yuan JL, Jiang K. Ovarian cancer breast metastasis: A case report. Dalian Yike Daxue Xuebao. 2019;41:472-475. [Cited in This Article: ] |
| 18. | Pai T, Nair N, Pantvaidya G, Deodhar K, Shet T. Metastatic nasopharyngeal carcinoma presenting as an isolated breast mass: A diagnostic pitfall and a review of literature. Indian J Pathol Microbiol. 2017;60:119-121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 19. | Driss M, Abid L, Mrad K, Dhouib R, Charfi L, Bouzaein A, Ben Romdhane K. Breast metastases from undifferentiated nasopharyngeal carcinoma. Pathologica. 2007;99:428-430. [PubMed] [Cited in This Article: ] |
| 20. | Pavlista D, Eliska O. Analysis of direct oil contrast lymphography of upper limb lymphatics traversing the axilla -- a lesson from the past -- contribution to the concept of axillary reverse mapping. Eur J Surg Oncol. 2012;38:390-394. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |