Euglobin Lysis Time
Euglobin Lysis Time
Euglobin Lysis Time
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
TEST<br />
Euglobulin <strong>Lysis</strong> <strong>Time</strong><br />
METHOD<br />
TEST EVALUATION<br />
Don Jacobs, M.D.<br />
Venous blood is collected in a plasticized tube containing sodium citrate<br />
(approximately 1 part citrate/9 parts plasma). Platelet poor plasma is obtained by<br />
centrifugation at 4C. The plasma is diluted with distilled H2O (1:10) and acidified<br />
by the addition of acetic acid or CO2 to a pH of 5.9. This step causes precipitation<br />
of the euglobulins: plasminogen activators, plasminogen, plasmin, fibrinogen,<br />
factor V, and factor VIE. The inhibitors of fibrinolysis (anti-activators and antiplasmins)<br />
remain in the supernatant and are discarded. The euglobulin pellet is<br />
resuspended in buffer solution. Thrombin or calcium is added to the euglobulin<br />
suspension to form a clot. The specimen is incubated in a 37° water bath and<br />
observed every fifteen minutes until clot lysis is complete. Normal values are<br />
between 3 and 20 hrs. <strong>Lysis</strong> times less than 1 hour are indicative of severe<br />
fibrinolysis. The significance of an elevated lysis time has not been fully evaluated.<br />
The spontaneous fibrinolytic activity of plasma may be mathematically expressed as<br />
1000/ECL time (min).<br />
The significance of an elevated lysis time has not been fully evaluated.<br />
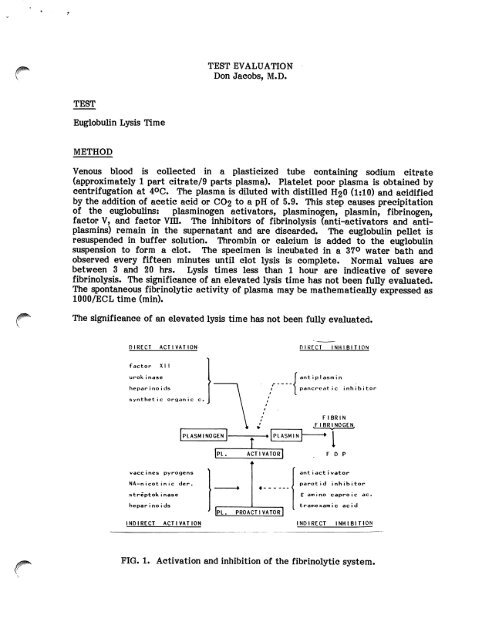
DIRECT ACTIVATION<br />
f a c t o r X I I<br />
urokinase<br />
hepar i no i ds<br />
s y n t h e t i c o r g a n i c c .<br />
v a c c i n e s p y r o g e n s<br />
N A - n i c o t i n i c d e r .<br />
s t r e p t o k i n a s e<br />
hepar i no i ds<br />
INDIRECT ACTIVATION<br />
PLASMINOGEN<br />
PL.<br />
» r<br />
ACTIVATOR<br />
*<br />
PLASMIN<br />
4 <<br />
Ipl. proactivatorI '<br />
DIRECT INHIBITION<br />
ant i pI asm i n<br />
p a n c r e a t i c i n h i b i t o r<br />
FIBRIN<br />
.FIBRINOGEN,<br />
-I<br />
F D P<br />
ant i act i vator<br />
parotid inhibitor<br />
£ a m i n o c a p r o i c a c .<br />
t r a m e x a m i c a c i d<br />
INDIRECT INHIBITION<br />
FIG. 1. Activation and inhibition of the fibrinolytic system.
INTRODUCTION<br />
Page 2<br />
The fibrinolytic system is a critical regulator of fibrin deposition and thrombosis.<br />
The components of the system are diagrammed above. Plasminogen, probably<br />
synthesized in the liver, is a circulating inactive proenzyme which is found in<br />
concentrations of 10-15 mg/dl. Plasminogen is converted into the active serine<br />
protease plasmin by a variety of plasminogen activators. These activators are<br />
widely distributed in a variety of tissues (tissue activator), plasma (activated<br />
Hageman factor/Kallikrein system) and urine (Urokinase). In addition to endogenous<br />
activators, a variety of bacterial products and pyrogens interact with the<br />
fibrinolytic system. The plasminogen activator of greatest physiologic importance<br />
is the tissue activator synthesized in venous endothelium and the vasa vasorum of<br />
muscular arteries. The release mechanism of the vascular-derived activator is<br />
poorly understood. To counterbalance the powerful proteolytic effects of plasmin,<br />
there are numerous fibrinolytic inhibitors which are normally present in<br />
approximately 30-fold excess concentration. These circulating anti-plasmins and<br />
anti-activators include alpha-1-antitrypsin, alpha-2-macroglobulin, antithrombin m,<br />
Cl-inhibitor, and alpha-2-anti-plasmin.<br />
The spontaneous fibrinolytic activity of blood may be measured by simply observing<br />
the time for clot lysis of whole blood collected in a glass tube (Whole Blood Clot<br />
<strong>Lysis</strong> <strong>Time</strong>). Due to the presence of natural inhibitors of fibrinolysis, clot lysis will<br />
occur only in cases of profoundly elevated fibrinolysis. In the Dilute Plasma Clot<br />
<strong>Lysis</strong> Test, dilution of the plasma results in differential depression of the inhibitors<br />
/#^ and allows lysis to occur in normal subjects or cases of slightly elevated fibrinolysis.<br />
^ The lysis time will generally be 18-24 hours. The ECL test is based on the<br />
concentration and precipitation of the fibrinolytic factors in the "euglobulin'1<br />
fraction with removal of the fibrinolytic inhibitors in the supernatant. Thus with<br />
most inhibitors removed, lysis time will be shortened. The ECL test is felt to<br />
reflect the spontaneous fibrinolytic activity of plasma and most closely corresponds<br />
to the level of plasminogen activators.<br />
TECHNICAL PROBLEMS<br />
Fibrinolytic activity is increased when plasma comes in contact with glass, probably<br />
due to the activation of the Hageman factor /Kallikrein system which is capable of<br />
generating plasmin. Thus, glass contact must be minimized. Venous occlusion is<br />
known to cause release of plasminogen activators from venous endothelium and<br />
particular attention to blood drawing technique is necessary. The method of<br />
precipitation of the euglobulin fraction is critical and the ECL times will change<br />
significantly with slight variations in pH and plasma dilution. Most (62%) of the<br />
fibrinogen is precipitated with the euglobulins, but this will vary if pH is not<br />
controlled. Some anti-plasmin activity, probably Cl-inactivator, will co-precipitate<br />
with the euglobulins even if pH and ionic strength of the plasma dilution are<br />
carefully standardized. A recent modification of the ECL test utilizes the addition<br />
of sodium flufenamate to the euglobulin fraction to neutralize any remaining Clinactivator<br />
(not done in the UCSF lab). Precipitation of euglobulins in the presence<br />
of dextran sulfate polymer will markedly increase the recovery of plasminogen<br />
activator and pro-plasminogen activator. Heparin and EACA (epsilon-amino-caproic<br />
acid) remain in the supernatant. Most authors strongly advise against storage of the
Page 3<br />
plasma prior to test performance. Storage at 20°C or 36°C will markedly decrease<br />
fibrinolytic activity. However, storage at -20°C may not affect outcome. For<br />
reproducible results, the test should probably be run within two hours of blood<br />
collection. The type of anticoagulant used will affect results. Citrate is<br />
recommended. EDTA will increase fibrinolysis whereas heparin will reduce it.<br />
Variations in the ECL time will occur with alterations in the fibrinogen level since<br />
the patient's fibrin clot is the substrate in the assay. Care should be taken to avoid<br />
undue handling of the tubes during performance of the ECL test. The endpoint<br />
(complete clot dissolution) is usually easy to read, although difficulties may occur in<br />
lipemic sera.<br />
CLINICAL APPLICATIONS<br />
The ECL test and related assays have been used to investigate a variety of factors<br />
which influence spontaneous fibrinolysis. Epinephrine, stress, and exercise will<br />
markedly increase fibrinolytic activity either by neuronally mediated release of<br />
plasminogen activator or through their effects on vascular permeability. ACTH and<br />
corticosteroids potentiate the effects of epinephrine in stimulating activator<br />
release. Numerous drugs, including procainamide, nicotinic acid, sulfonylureas,<br />
phenformin, reserpine, pitressin, androsterone and DDAVP will increase fibrinolytic<br />
activity. Some of these may find therapeutic application as antithrombotic agents.<br />
Various surgical procedures produce a biphasic response in fibrinolysis. Many<br />
neurologic procedures, including ventriculography and pneumoencephalography, have<br />
been shown to markedly increase spontaneous fibrinolysis and on occasion provoke<br />
severe bleeding. Post-operatively, fibrinolysis usually decreases, reaching a nadir on<br />
postoperative days 1 and 2. Studies have indicated that large rapid falls in<br />
fibrinolytic activity as measured by the ECL test are associated with increased<br />
incidence of post-operative deep venous thrombosis. In approximately 95% of<br />
normal subjects, venous occlusion stimulates fibrinolysis in blood collected from the<br />
occluded vein. This potentiation of fibrinolysis with occlusion is more marked in<br />
arm than in leg veins. Subjects with idiopathic deep venous thrombosis frequently<br />
show no such enhancement of fibrinolysis upon venous occlusion. Release of<br />
plasminogen activators from venous endothelium of occluded vessels may be<br />
physiologically important in controlling thrombosis in situations of stasis.<br />
Fibrinolysis has also been reported to be reduced in individuals with multiple risk<br />
factors for myocardial infarction and in patients with peripheral atherosclerotic<br />
disease, vasculitis, and Raynaud's phenomenon.<br />
Thrombolytic agents such as Urokinase and Streptokinase markedly accelerate<br />
fibrinolysis through direct and indirect mechanisms (see chart). The ECL test was<br />
formerly used to monitor patients receiving thrombolytic therapy for acute<br />
myocardial infarction. Currently, however, only PT, PTT, TT, platelets and<br />
fibrinogen are commonly monitored during intracoronary streptokinase infusion.<br />
The ECL test has been used to monitor patients receiving urokinase therapy for the<br />
treatment of DVT.<br />
The ECL test has been used in the investigation of primary fibrinogenolysis<br />
(hyperplasminemia). Various tissues, including prostate, uterus, and colon appear to<br />
be exceptionally rich in plasminogen activator substances. Surgical manipulation of<br />
these organs may give rise to a consumptive coagulopathy based on widespread
Page 4<br />
intravascular activation of fibrinolysis. Plasmin has a wide range of substrates,<br />
including factors V and VIII, and will interfere with coagulation by multiple<br />
mechanisms. Production of abnormal quantities of plasminogen activator has also<br />
been described in certain tumors and acute leukemias. In primary fibrinogenolysis,<br />
there will be a marked increase in the spontaneous fibrinolytic activity of plasma.<br />
Increased fibrinolytic activity may also be seen, although usually to a lesser extent,<br />
in DIC.<br />
There are no studies providing detailed comparisons of coagulation and fibrinolytic<br />
parameters in primary fibrinogenolysis versus DIC. The utility of the ECL test in<br />
making this distinction is uncertain. In clinical practice, DIC should be ruled out on<br />
clinical and laboratory grounds before primary defects in fibrinogenolysis are<br />
suspected. There is little agreement on the specific clinical indications for<br />
employing the ECL test in general patient management. At present, the test<br />
appears useful mainly as an investigative and research tool. Additionally, the<br />
variety of factors sited above which affect fibrinolysis detract from the specificity<br />
and diagnostic utility of the ECL test.<br />
FURTHER DEVELOPMENTS<br />
In the ECL test, the patient's own fibrin clot serves as the substrate for fibrinolysis.<br />
Different substrates may also be used, including casein (caseinolysis) and synthesis<br />
esters (esterolysis). The most important modification of the ECL time is the Fibrin<br />
^ Plate assay in which a sample of plasma or euglobulin fraction is placed directly on<br />
the surface of a petrie dish containing human or bovine fibrin. At approximately 20<br />
hours, the zone size of fibrinolysis is measured. There is a relatively good<br />
correlation between assays of fibrinolysis as measured in the fibrin plate and the<br />
ECL test. The fibrin plate assay has a more precise and easily quantifiable endpoint<br />
and demands less technician intervention. However, it is not suitable for stat<br />
determinations. A recent modification of the ECL test used the addition of radiolabelled<br />
fibrinogen to the euglobulin fraction. The rate of radioactivity release is<br />
proportional to the fibrinolytic activity of the test plasma. This technique is very<br />
precise and has been used to investigate fibrinolytic activity in families with mild<br />
bleeding tendencies. For many research and clinical purposes, the ECL test has<br />
been supplanted by recently developed assays based on a chromogenic substrate (S-<br />
2251) which is a specific substrate for plasmin and plasminogen activated<br />
streptokinase. Using the chromogenic substrate technique, plasminogen activator,<br />
plasminogen, plasmin, and anti-plasmins may be easily and readily quantified.<br />
REFERENCES<br />
1. Allen RA. Blood sampling techniques for fibrinolytic studies. Thromb Res<br />
23:1-2.<br />
2. Von Kaulla KN, von Kaulla E. "Remarks on the Euglobulin <strong>Lysis</strong> <strong>Time</strong>." In:<br />
JF Davidson (ed.), Progress in Chemical Fibrinolysis and Thrombolysis, Vol 1.<br />
Raven Press: New York, 1975.
fifik^<br />
Page 5<br />
3. Griffiths NJ, et al. Plasma fibrinolytic inhibitors post operation. Surg<br />
Gynecol Obst 144:673-676, 1977.<br />
4. Knight MTN, et al. Fibrinolytic response to surgery. Lancet 2:370-373, 1977.<br />
5. Gader AMA. The potentiating effect of corticosteroids on the fibrinolytic<br />
system in response to I.V. infusion of adrenalin in man. Haemostasis 17:353-<br />
356, 1982.<br />
6. Heimburger N. "Plasminogen Assay: a review and evaluation of various<br />
methods." In: JF Davidson (ed.), Progress in Chemical Fibrinolysis and<br />
Thrombolysis, Vol 1. Raven Press: New York, 1975.<br />
7. Prentice CRM. Basis of antifibrinolytic therapy. J Clin Pathol (Suppl.) 33<br />
(suppl 14) pp. 35-40.<br />
8. Horvath AE. The 125I-Fibrinogen Euglobulin Clot <strong>Lysis</strong> Test. Am J Clin<br />
Pathol 70(2):271-274, 1978.<br />
9. Latallo ZS, et al. Assessment of plasma fibrinolytic system with use of<br />
chromogenic substrate. Haemostasis 7:138-145, 1978.<br />
10. Blix S. Studies on the fibrinolytic system in the euglobulin fraction of human<br />
plasma. Scand J Clin Lab Invest 13(suppl 58), 1961.<br />
11. Arneson H, et al. "A comparison between the ECL time and the fibrin plate<br />
method for the estimation of fibrinolytic activity after venous stasis." In: JF<br />
Davidson (ed.), Progress in Fibrinolysis, Vol 5. Churchill Livingstone:<br />
Edinburgh, 1981.<br />
12. Nilsson IM, et al. "Physiology of Fibrinolysis." In: DL Kline, KNN Reddy<br />
(eds.), Fibrinolysis, CRC Press: Boca Raton, Florida, 1980.<br />
13. Theiss W, et al. Systemic fibrinolytic activity and inhibitor levels during<br />
treatment of deep venous thrombosis with urokinase and streptokinase.<br />
Thrombosis and Haemostasis 5(3):664-668, 1983.<br />
14. Kluft C. Studies on the fibrinolytic system in human plasma: quantitative<br />
determination of plasminogen activator and pro-activator. Thrombosis and<br />
Haemostasis 41:365-383, 1979.<br />
15. Von Kaulla KN, Schultz RL. Methods for evaluation of human fibrinolysis.<br />
Am J Clin Pathol 29:104-112, 1958.