Chapter 2
Chapter 2
Chapter 2
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Chapter</strong> 2<br />
URETHRITIS IN MALES<br />
ETIOLOGY<br />
Urethritis is the most frequent STD syndrome seen in men. Customarily, clinicians categorize<br />
urethritis into gonococcal and nongonococcal etiologies. The relative frequency of nongonococcal<br />
urethritis (NGU) and gonococcal urethritis varies by population studied, but overall, more cases of<br />
NGU than gonococcal urethritis are now being seen in the United States. Up to one-fourth of heterosexual<br />
men with gonorrhea also have simultaneous Chlamydia trachomatis (CT) infections.<br />
C. trachomatis causes 20 to 40% of cases of NGU, and some studies indicate that Mycoplasma<br />
genitalium and Ureaplasma urealyticum may cause an additional 10 to 20%. The remaining cases<br />
probably result from sexually transmitted pathogens, but their precise etiology remains unclear. Occasionally,<br />
urethritis results from infection with Trichomonas vaginalis, adenovirus or herpes simplex<br />
virus. Most patients with urethritis due to genital herpes infection will have obvious herpetic penile<br />
lesions, and many with urethritis due to T. vaginalis will have sex partners with trichomonal vaginitis.<br />
INCUBATlON PERIOD<br />
Gonorrhea usually develops 2 to 6<br />
days after exposure to Neisseria gonorrhoeae<br />
(GC), whereas NGU generally<br />
develops between 1 and 5 weeks<br />
after infection, with a peak around 2<br />
weeks.<br />
CLINICAL<br />
MANIFESTATIONS<br />
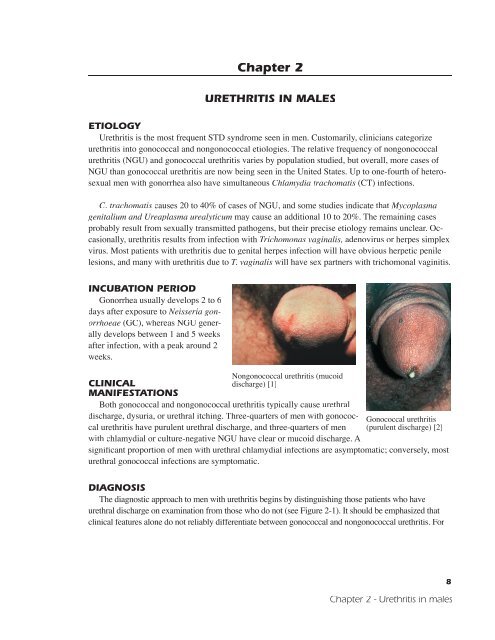
Nongonococcal urethritis (mucoid<br />
discharge) [1]<br />
Both gonococcal and nongonococcal urethritis typically cause urethral<br />
discharge, dysuria, or urethral itching. Three-quarters of men with gonococcal<br />
urethritis have purulent urethral discharge, and three-quarters of men<br />
with chlamydial or culture-negative NGU have clear or mucoid discharge. A<br />
Gonococcal urethritis<br />
(purulent discharge) [2]<br />
significant proportion of men with urethral chlamydial infections are asymptomatic; conversely, most<br />
urethral gonococcal infections are symptomatic.<br />
DIAGNOSIS<br />
The diagnostic approach to men with urethritis begins by distinguishing those patients who have<br />
urethral discharge on examination from those who do not (see Figure 2-1). It should be emphasized that<br />
clinical features alone do not reliably differentiate between gonococcal and nongonococcal urethritis. For<br />
8<br />
<strong>Chapter</strong> 2 - Urethritis in males
this reason, diagnosis and<br />
treatment should be based<br />
on the results of a urethral<br />
Gram stain and appropriate<br />
cultures or tests.<br />
Document<br />
Urethritis<br />
by the presence of at least<br />
two of the following three<br />
features:<br />
1. Symptoms: history<br />
of urethral<br />
discharge and/or<br />
dysuria<br />
2. Examination: presence<br />
of purulent,<br />
mucopurulent, or<br />
mucoid urethral<br />
discharge<br />
3. Laboratory: (any<br />
one of following is<br />
sufficient)<br />
Intacellular Gram-negative diplococci<br />
(GNDC) in urethral Gram stain [3]<br />
Lesion of disseminated gonococcal<br />
infection [5]<br />
• urethral Gram-stained smear showing ≥5 PMNs/1000X field in areas of maximal cellular<br />
concentration<br />
• urinalysis showing ≥10 PMNs/400X field in centrifuged sediment<br />
• positive urine leukocyte esterase test<br />
Patients with symptoms of urethritis, but without a visible discharge on exam or laboratory evidence<br />
of urethritis, should be reexamined within 7 days when they have not urinated for 4 to 8 hours.<br />
If only one diagnostic criterion is met on reexamination, obtain the first 5 to 10 ml of voided urine,<br />
centrifuge, and examine the sediment microscopically: ≥10 PMNs/400X field confirms urethritis.<br />
A urethral Gram-stained smear showing ≥5 PMNs/l000X field is suggestive of urethritis, even in<br />
the absence of other criteria.<br />
Exclude Gonorrhea<br />
1. Gram-stained smear of urethral exudate<br />
• negative for intracellular Gram-negative diplococci (IGND)<br />
2. Confirmed by negative culture for N. gonorrhoeae (GC)<br />
Urethral Gram stain with >5 PMNs<br />
per high power field (nongonococcal<br />
urethritis) [4]<br />
Normal urethral cells on Gram stain [6]<br />
Test for Chlamydia<br />
Obtain urethral specimen for C. trachomatis (CT) antigen-detection or DNA test, culture, or NAAT<br />
(LCR, PCR).<br />
9<br />
<strong>Chapter</strong> 2 - Urethritis in males
Sexually active man with history of urethral<br />
discharge or dysuria or sexual contact with<br />
an infected partner<br />
Abnormal urethral discharge on examination<br />
Yes<br />
No<br />
Gram-stained smear of<br />
urethral exudate or<br />
endourethral smear<br />
Gram-stained<br />
endourethral smear*<br />
No GND; ≥5 PMNs<br />
/ 1000X field<br />
Extracellular GND<br />
or intracellular GND<br />
with atypical<br />
morphology<br />
PMNs with<br />
intracellular GND<br />
No GND;
TREATMENT<br />
For a more detailed discussion of these regimens and other treatment considerations, please refer<br />
to the CDC<br />
STD Treatment Guidelines<br />
at http://www.cdc.gov/std/treatment/.<br />
Gonococcal Urethritis<br />
Uncomplicated anogenital gonorrhea<br />
Any of the following:<br />
• Cefixime 400 mg PO (single dose)<br />
• Ciprofloxacin 500 mg PO (single dose)<br />
• Ofloxacin 400 mg PO (single dose)<br />
• Levofloxacin 250 mg PO (single dose)<br />
• Ceftriaxone 125 mg IM (single dose) and doxycycline 100 mg bid for 7 days<br />
Note: 1) Doxycycline is also provided with any of the above treatments for empirical treatment<br />
of possible coexisting C. trachomatis infection. Alternatively, azithromycin 1 gm PO<br />
single dose can be used instead of doxycycline for treatment of possible co-existing<br />
chlamydial infection.<br />
2) Avoid flouroquinones if gonococcal infection was acquired in Hawaii or southeast Asia, due<br />
to higher rates of quinolone resistance in GC or if treating MSM infected with gonorrhea.<br />
3) Cefixime is currently not available in pill form, but is expected to be back on the market<br />
sometime in late 2004. In the interim, Cefpodoxime 400 mg PO (single dose) is being recommended<br />
and is under formal study. The liquid formulation of Cefixime is still available<br />
though not feasible or available in most clinics.<br />
Nongonococcal Urethritis<br />
Recommended regimens<br />
Either of the following:<br />
• Azithromycin 1 g orally in a single dose,<br />
• Doxycycline 100 mg orally twice a day for 7 days<br />
Alternative regimens<br />
Any of the following:<br />
• Erythromycin base 500 mg orally four times a day for 7 days,<br />
• Erythromycin ethylsuccinate 800 mg orally four times a day for 7 days,<br />
• Ofloxacin 300 mg twice a day for 7 days or Levofloxacin 500 mg once daily for 7 days<br />
Immediate treatment failure<br />
(persistent urethritis while on therapy or recrudescence immediately after completion of treatment)<br />
1. Confirm urethritis by examination and laboratory.<br />
2. Obtain urethral wet prep and culture for trichomonas.<br />
3. Pending results of trichomonas culture:<br />
• Treat with erythromycin if doxycycline was used initially<br />
- Erythromycin stearate or base 500 mg qid for 7 days<br />
4. Treat with metronidazole 2 gm PO single dose (microscopy of first-void urine or urethral<br />
swabs shows trichomonads or if trichomonas culture is positive, or empirically if culture is<br />
unavailable)<br />
• Treat with doxycycline if erythromycin was used initially<br />
- Doxycycline 100 mg bid for 7 days<br />
11<br />
<strong>Chapter</strong> 2 - Urethritis in males
Recurrence of urethritis<br />
(within 6 weeks, following apparent resolution)<br />
1. Evaluate to confirm the diagnosis of urethritis.<br />
2. Confirm that the treatment was followed and whether or not the patient had sexual activity<br />
before he or his partner were fully treated. If the patient has been noncompliant or has been<br />
exposed to an untreated partner, retreat with the original regimen.<br />
3. Retreat with Metronidazole 2 g orally in a single dose, plus Erythromycin base 500 mg orally four<br />
times a day for 7 days, or Erythromycin ethylsuccinate 800 mg orally four times a day for 7 days.<br />
FOLLOW-UP<br />
Initial or isolated episode<br />
Patients with gonococcal urethritis<br />
A test-of-cure is recommended only for patients with a known resistant strain of GC or for<br />
those with persistent symptoms.<br />
Men with NGU<br />
Request a return after 7 to l4 days only if symptoms persist or recur.<br />
Persistent or recurrent NGU<br />
Request that patients return prn for persistent or recurrent symptoms.<br />
Consider referral to a urologist or other specialist.<br />
Confirmed cases<br />
of gonorrhea and chlamydia should be reported to the state/local health department (see Appendix<br />
B).<br />
MANAGEMENT OF SEX PARTNERS<br />
All contacts within the previous 4 weeks,<br />
and any other contacts suggested by the epidemiologic history:<br />
1. Perform routine STD examination.<br />
2. Regular partners and source contacts<br />
• of gonorrhea:<br />
Treat with cefixime 400 mg PO (or other single dose regimen listed above) and provide<br />
doxycycline for possible coexisting C. trachomatis infection.<br />
• of chlamydia urethritis or CT-NGU:<br />
Treat with doxycycline, ofloxacin or azithromycin.<br />
When practical, use the same regimen used for the patient, unless contraindicated because<br />
of pregnancy or drug intolerance.<br />
3. Casual contacts:<br />
Individualize treatment, depending on the clinical examination, epidemiologic setting (for<br />
example, suspected source vs. spread contact), and results of gonorrhea and chlamydia tests.<br />
Do not dispense antibiotics or prescriptions for contacts who are not examined, except in special<br />
circumstances.<br />
Contacts of men with recurrent NGU<br />
The need and value of treatment are unknown. Individualize the approach on the basis of available<br />
clinical, epidemiological, and microbiological data.<br />
12<br />
<strong>Chapter</strong> 2 - Urethritis in males
SEQUELAE<br />
With the advent of antibiotics, complications as a result of gonococcal urethritis, such as locally<br />
invasive infection, urethral strictures, or disseminated gonococcal infection are now rare. NGU is<br />
generally a self-limited disease and, even without therapy, clinical consequences are minimal. Epididymitis<br />
can develop in up to 2% of cases, and conjunctivitis<br />
occasionally occurs. Reiterʼs syndrome may result from untreated<br />
chlamydial urethritis in genetically predisposed individuals. The<br />
psychological impact of persistent urethritis or frequent recurrences<br />
can be great.<br />
LABORATORY SCREENING FOR URETHRITIS IN<br />
ASYMPTOMATIC MEN<br />
A urethral Gram stain and cultures for chlamydia and gonorrhea<br />
should be obtained from heterosexual men who are seen in<br />
high-risk settings such as an STD clinic and who have no history<br />
of urethral symptoms or signs and no history of contact with an<br />
infected partner. An example of columnar epithelial cells obtained<br />
from an endourethral swab from an asymptomatic man is shown to<br />
the right; the presence of columnar epithelial cells indicates that the<br />
swab specimen has been obtained adequately to test for C. trachomatis.<br />
Some of these men will have asymptomatic gonorrhea or<br />
NGU as evidenced by persistent urethral leukocytosis, pyuria (as<br />
measured by urine microscopy or LE test), and/or a positive test<br />
for chlamydia or gonorrhea.<br />
Lesion of disseminated gonococcal<br />
infection [5]<br />
Normal urethral cells on Gram<br />
stain [6]<br />
13<br />
<strong>Chapter</strong> 2 - Urethritis in males



![الاختناق Asphyxia.ppt [Compatibility Mode]](https://img.yumpu.com/22145682/1/190x146/-asphyxiappt-compatibility-mode.jpg?quality=85)