SOFT 2004 Meeting Abstracts - Society of Forensic Toxicologists
SOFT 2004 Meeting Abstracts - Society of Forensic Toxicologists
SOFT 2004 Meeting Abstracts - Society of Forensic Toxicologists
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
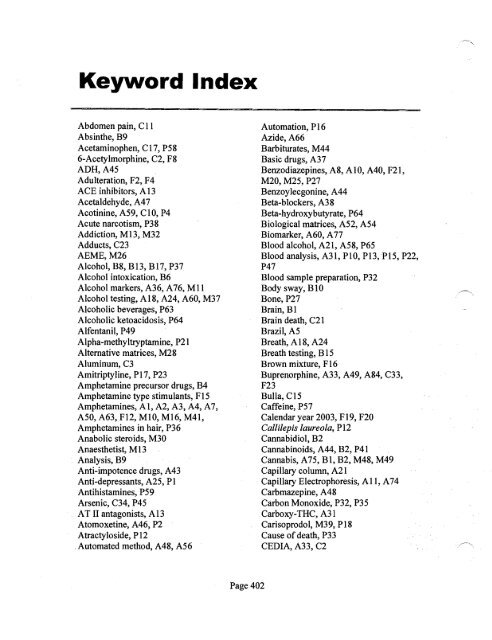
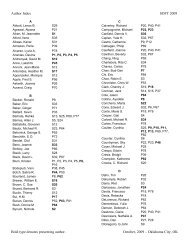
KeY'Nord Index <br />
Abdomen pain, C II<br />
Absinthe, B9<br />
Acetaminophen, C17, P58<br />
6-Acetylmorphine, C2, F8<br />
ADH,A45<br />
Adulteration, F2, F4<br />
ACE inhibitors, A 13<br />
Acetaldehyde, A47<br />
Acotinine, A59, ClO, P4<br />
Acute narcotism, P38<br />
Addiction, M13, M32<br />
Adducts, C23<br />
AEME,M26<br />
Alcohol, B8, B13, B17, P37<br />
Alcohol intoxication, B6<br />
Alcohol markers, A36, A 76, Mil<br />
Alcohol testing, A18, A24, A60, M37<br />
Alcoholic beverages, P63<br />
Alcoholic ketoacidosis, P64<br />
Alfentanil, P49<br />
Alpha-methy ltryptamine, P2l<br />
Alternative matrices, M28<br />
Aluminum, C3<br />
Amitriptyline, PI7, P23<br />
Amphetamine precursor drugs, B4<br />
Amphetamine type stimulants, F15<br />
Amphetamines, AI, A2, A3, A4, A7,<br />
A50, A63, F12, MIO, M16, M41,<br />
Amphetamines in hair, P36<br />
Anabolic steroids, M30<br />
Anaesthetist, M 13<br />
Analysis, B9<br />
Anti-impotence drugs, A43<br />
Anti-depressants, A25, PI<br />
Antihistamines, P59<br />
Arsenic, C34, P45<br />
. AT II antagonists, A 13<br />
Atomoxetine, A46, P2<br />
Atractyloside, PI2<br />
Automated method, A48, A56<br />
Automation, Pl6<br />
Azide, A66<br />
Barbiturates, M44<br />
Basic drugs, A37<br />
Benzodiazepines, A8, AIO, A40, F2l,<br />
M20, M25, P27<br />
Benzoylecgonine, A44<br />
Beta-blockers, A38<br />
Beta-hydroxybutyrate, P64<br />
Biological matrices, A52, A54<br />
Biomarker, A60, A 77<br />
Blood alcohol, A21, A58, P65<br />
Blood analysis, A31, PIO, P13,P15, P22,<br />
P47<br />
Blood sample preparation, P32<br />
Body sway, BI0<br />
Bone, P27<br />
Brain, Bl<br />
Brain death, C21<br />
Brazil, A5<br />
Breath, A 18, A24<br />
Breath testing, B 15<br />
Brown mixture, FI6<br />
Buprenorphine, A33, A49, A84, C33,<br />
F23<br />
Bulla, CI5<br />
Caffeine,P57<br />
Calendar year 2003, FI9, F20<br />
Callilepis laureola, PI2<br />
Cannabidiol, B2<br />
Cannabinoids, A44, B2, P41<br />
Cannabis, A 75, B 1, B2, M48, M49<br />
Capillary column, A21<br />
Capillary Electrophoresis, All, A 74<br />
Carbmazepine, A48<br />
Carbon Monoxide, P32, P35<br />
Carboxy-THC, A31<br />
Carisoprodol, M39, PI8<br />
Cause <strong>of</strong> death, P33<br />
CEDIA, A33, C2<br />
Page 402
Channelopathy, C34<br />
Chemical bums, C 15<br />
Chemical warfare agents, C23<br />
Children, C28<br />
Chloramphenicol, A39<br />
Chloramphenicol glucuronide, A39<br />
Chlorinated MDMA, F25<br />
Chlor<strong>of</strong>ormates, Al<br />
Chloropyrifos, C24<br />
Chromium, F2<br />
Chronic abuse, P49<br />
Chronic administration, C 1 0<br />
Citalopram, P3<br />
Clandestine, C28<br />
CLND,A69<br />
Clomipramine, P6<br />
Clozapine, M14<br />
Cluster analysis, P64<br />
Cocaine, A29, C31, Fl1, M26, M28,<br />
M51,P27,P29,P33<br />
Cocaethylene, M43<br />
Codeine, F16, M29<br />
Collection, C3<br />
Comparative analysis, A 17<br />
Consolidated workstation, A 19<br />
Contamination, A 75, M8<br />
Controlled cocaine administration, M51<br />
Conversion, A81<br />
Corticosteroids, A37<br />
Cotinine, M45<br />
Crack, M26<br />
Criminal poisoning, C 19<br />
Criteria, A6<br />
Cryogenic Grinding, M2<br />
Cytochrome P450, B4<br />
Cytotoxicity, M43<br />
Cyanide, P44<br />
Dark Agouti rats, B4<br />
Death, P25, P61<br />
Death investigation, P53<br />
Demethylation, A 16<br />
Depot, M49<br />
Derivatisation, An<br />
Designer drugs, Al<br />
Detection window, C32<br />
Detoxification programme, C 1<br />
Dextromethorphan, M39<br />
Diagnosis, C23<br />
2,4-dichlorophenol (2,4-DCP), C20<br />
2,4-dichlorophenoxyacetic acid (2,4-D),<br />
C20<br />
Dietary supplements, A43<br />
Diethylene Glycol, C26<br />
Differential display, C17<br />
2,5-dimethoxy-4-bromoamphetamine,<br />
C29<br />
2,4-Dinitrophenol, P62<br />
Direct and affordable analysis, A60<br />
Disinfectant, C 14<br />
Distribution, P 11<br />
Diuretics, C30<br />
DNA,A77<br />
DOB overdose, C29<br />
Doping, A65, M30<br />
DRE, M34<br />
Driving, B 12, B 13<br />
Dronabinol, B3<br />
Drug, P28, P37<br />
Drug analysis, A69<br />
Drug diversion, C27<br />
Drug-facilitated crime, M9<br />
Drug-facilitated sexual assault, B8, B 17,<br />
C5, C32, P23<br />
Drug identification, A 70<br />
Drugs <strong>of</strong> Abuse, AI9, A28, An, B7,<br />
B12, B13, Cl, Fl, M2, M15, M24, M33,<br />
M35,M37,M42,M46,M50,P31<br />
Drug testing, F13<br />
Drug Use History, M6<br />
Drunken driving, B 15<br />
Dual-column, A25<br />
DUI, A73, B3<br />
Ecstasy, AI2, AI7, P25, P43<br />
EIA, M34, A50<br />
ELISA, A57, A65, F23, M16, M24,<br />
M40<br />
Emblica <strong>of</strong>ficinalis, C 18<br />
EMIT II Plus immunoassay, A44<br />
Enantiomer, A63, P42<br />
Enantiomer separation, A4<br />
Enantioselective Separation, M 10<br />
Entomology, M44<br />
Page 403
Environmental toxicology, C4<br />
Enzyme immunoassay, A32, C 13<br />
Epidemiology, P28<br />
Ephedrine, A8I, P42<br />
Ephedrone, C7<br />
Epidemiology, C6<br />
Error, P65<br />
Estazolam, B5<br />
Ethanol, A27, A35, A45, A55, BIO, C25,<br />
MI8, P35, P47<br />
Ethanol metabolism, A36<br />
Ethyl-glucuronide, A35, A53, MIl<br />
Ethyl sulfate, A36, A76<br />
Exhaled breath, M45<br />
Exposure, M46<br />
External contamination, P45<br />
Extraction, A30<br />
FAS, A77<br />
Fatal Intoxication, C29, P8, Pl4<br />
Fatality, P46, P48, P52, P62<br />
Femoral, P65<br />
Fentanyl, P22, P48<br />
Fire, P35<br />
Flunitrazepam, A23, B8<br />
Food products, P63<br />
Forced ingestion, C31<br />
<strong>Forensic</strong>, A6, A52<br />
<strong>Forensic</strong> Laboratories, A5<br />
<strong>Forensic</strong> Toxicology, P36<br />
Formalin-induced, P39<br />
FOXY,C9<br />
Free-morphine, FlO<br />
Friction coefficient, B5<br />
Fungi, A75<br />
Furosemide, A 14<br />
GHB, A73, P46, P63<br />
GC-FID, A27, C24<br />
GC-HRMS, M41<br />
GC-MS, AI, AI5, A29, A30, A32, A4I,<br />
A47, A63, A70, An, A73, A80, A8I,<br />
B7, B9, CI5, C2I, C24, C30, FI7, F24,<br />
F25, F27, MI5, M2I, M23, M29, M45,<br />
PI, P57<br />
GC-MS/MS, A3I, A53, A56, C8, M35,<br />
P49<br />
GCIMS/SIM, CIO, M7<br />
Glucuronide metabolites, A84<br />
Goat, C12<br />
Go-pills, FI2<br />
Hair, M3, M4, M8, M9, M13, MI6,<br />
M28,M35,M41,P9,P49<br />
Hair analysis, M2, M5, M7, MIO, MIl,<br />
MI2,M20, M39,M40, P30<br />
Hallucinogens, P21<br />
Haulage drivers, F22<br />
Headspace GC, A2I, A58<br />
Headspace-SPME, A54<br />
Heroin, F8, FlO, P24<br />
Heroin maintenance program, MI2<br />
Heroin related death, P29<br />
HHS-certified laboratories,FI9, F20<br />
HPLC, AIO, AI7, A20, A62, C20, P5<br />
HPLC-MS, Pl2<br />
Human, BI1<br />
Hydrocodone, P20<br />
Hydroxychloroquine, P52<br />
Hydroxy radical, A55<br />
ICP-MS, C3<br />
IDA, A83<br />
Illicit drug, C7<br />
Illicit substances, F22<br />
1midacloprid, P 14<br />
ImmunoassaY,A3, F5, F24, PI8<br />
Immunoassay comparison to GC/MS, F6<br />
Immunoassay confirmation rates, F19,<br />
F20<br />
IMS, C5<br />
Inductively Coupled Plasma, A22<br />
Infant, P40<br />
Information, A9<br />
Information dependent acquisition, A68<br />
Inhalation, Cll<br />
Insecticide poisoning, P34<br />
Intect, F4<br />
Interaction, P29<br />
Internal standard, P32<br />
Internet, P44<br />
Interpretation, PI9, P59<br />
Intoxication, P7, P40, P44, P57<br />
Intoxilyzer 8000, A 18, A24<br />
In Utero Exposure, M47<br />
Iodine, F4<br />
Page 404
Ion chromatography, A66<br />
Ion-paired extraction, F3<br />
Ion trap, C8<br />
Ketamine, C32, M7, M40<br />
Labetalol, P8<br />
L-Ascorbyl-2-phosphate, A55<br />
LA-ICP-MS, M4<br />
Laser spray, A59<br />
Laxatives, C30<br />
LCIAPCIIMS, P9<br />
LC-MS, A42, A43, A79, FI8, P14, P50<br />
LC-ESI-MS, AlO, A25, A28, A51, A67,<br />
A83,M25,M27,M3l,M42<br />
LC-MS/APCI, A34, A38<br />
LC-MSIMS, A8, A13, A37, A39, A40,<br />
A49, A52, A76, A78, A83, F7, F2l, F26,<br />
M9,<br />
MI4, M20, P48<br />
LC-MSIMS library, A68<br />
Lead, BI6<br />
Legal and judicial issues, A9, M32<br />
Lethal dose, C26<br />
Levetiracetam, P 15<br />
LiquidlLiquid, FI7<br />
Liver, B16<br />
Liver fibrosis, C 18<br />
LOD,A6<br />
Lorazepam, A15, P53<br />
Low dose, P58<br />
LSD, A78<br />
Marijuana, Fil<br />
Mass detector, A22<br />
Mass spectrometry, A42, A59, A64, A69,<br />
C31<br />
Matrix, A7l<br />
MBTFA,AI6<br />
MDA,A4,A7<br />
MDMA, A3, A4, All, A20, Fll, M5,<br />
M36, P43<br />
Measurement uncertainty, F3<br />
Meconium, M47<br />
Medical pr<strong>of</strong>essional, F26<br />
Melanin, M3, M14<br />
Mellanby, B17<br />
Meprobamate, C6<br />
Mercury analysis, C 19<br />
Mercury poisoning, C 19<br />
Metabolic acidosis, C25<br />
Metabolism, C9, C33<br />
Metabolites, A29, C3l<br />
Metalloids, A22<br />
Metals analysis, C4<br />
Metaxalone, P7<br />
Methadone, C22, F17, Ml, P19, P20,<br />
P40,P60,P6l<br />
Methamphetamine, A4, B14, CIl, C28,<br />
M4l,M47,P39,P4l<br />
Methamphetamine chronic toxicity, P36<br />
Methcathinone, C7<br />
Method development, A42, A 79<br />
Method Validation, A57, FI5, M5<br />
5-Methoxy-alpha-methyltryptamine, P2I<br />
5-Methoxy-N,N-diisopropyltryptamine,<br />
C9<br />
Methylation, P39<br />
Methylhippuric acid, A5I<br />
Microdiffusion method, A66<br />
Microvascular Endothelium, M43<br />
Microwave-assisted Extraction, M 19<br />
Mirtazapine, P 13<br />
6-mono-acetyl Morphine, FlO<br />
Monoliths, A 7<br />
Morphine, F8, F13, F16, P24, P25<br />
Multicenter evaluation, A48<br />
Multiple Analyte Enzyme Immunoassay,<br />
FI<br />
Multi target screening, A68<br />
Multisite sampling, MI8<br />
Nail analysis, M30<br />
Nails, M26<br />
Naloxone, A83<br />
Napoleon, C34, P45<br />
Narcotics, C27<br />
NAS, C22<br />
Neonate, P54<br />
Nerve gas, C8<br />
Nicotine, C22, M22<br />
Nicotine metabolites, M22<br />
Nitrite, F2<br />
N,N-dimethylamphetamine, F18<br />
NNSL, F14<br />
Page 405
Non-controlled psychotropic substances,<br />
A61<br />
Non-negative, Fl4<br />
Non-regulated testing, F20<br />
11-nor-delta-9-carboxytetrahydrocannabinol,<br />
F5<br />
Norephedrine, P42<br />
Norketamine, C32<br />
Nornaloxone, A83<br />
Noscapine metabolites, F9<br />
On-Site testing, F6, M33, M36<br />
Opiates, A44, A64, C2, F7, M12, P30<br />
Opioids, A16, BI4<br />
Oral administration <strong>of</strong>THC, B2, M17,<br />
M23<br />
Oral Cannabinoids, M38<br />
Oral fluid, MI5, M22, M24, M27, M31,<br />
M33,M34,M36,M37,M48,M49,M50<br />
OraSure, M17<br />
Organophosphorous pesticides, A54<br />
Outcomes, C22<br />
Overdose, C6, PI, P8, P51, P55<br />
Oxcarbazepine, P9<br />
Oxycodone,A32,CI3,F24,P20,P26<br />
Oxymorphone, CI3<br />
P450, C33<br />
Paclitaxel, A 79<br />
Paint thinner abuser, A51<br />
Papaverine metabolites, F9<br />
Paramethoxyamphetamine, P41<br />
Pediatric, P52<br />
Perfonnance toxicology, B 11<br />
Pennethrin, P34<br />
Phannaceutical testing, C27<br />
Phannacogenomics, CI7, P60, P61<br />
Pharmacokinetics, A84<br />
Phenazepam, A80<br />
Phenethylamines, A61, A67<br />
Piperazine, A 7 4<br />
Plasma, A38, M23, M24<br />
PMA,A26<br />
Poisoning, C24, C26, P22<br />
Portugal, B 12<br />
Positive chemical ionization, A 15<br />
Positive rates, F26<br />
Postmortem, PII, P13, PI5, PI8, P24,<br />
P26,P31,P34,P37,P38,P47,P5I,P56,<br />
P58,P62<br />
Postmortem blood concentrations, P33,<br />
P59<br />
Postmortem diffusion, P4<br />
Postmortem ethanol, P50<br />
Postmortem fluids and tissues, PI9<br />
Postmortem redistribution, P3, P6, P 17<br />
Postmortem specimens, M 18, P2, P5<br />
Postmortem toxicology, P23, P46, P52,<br />
P53,P55<br />
Post-rotational nystagmus, B6<br />
Posturography, B5<br />
Pregnancy, M46<br />
Prenatal, C22<br />
Pr<strong>of</strong>iling, A26<br />
Pr<strong>of</strong>iling MDMA, AI2<br />
Propylene glycol, C25<br />
Protease, F5<br />
Psilocin, A34, FII<br />
Psychomotor performance, B 10<br />
Puffer fish, C 16<br />
Putrefaction, P4<br />
Pyrolysis products, A29<br />
Pyrosequencing, P60<br />
Quantitation, A45, A49, A71, A80<br />
Quetiapine, PII, P55, P56<br />
Rat, C18, P3<br />
Redistribution, P43<br />
Residue cytotoxicity ACTP, C12<br />
Retention time locking, A 70<br />
rhuEPO, A65<br />
RIA, A57<br />
Roadside survey, B 15<br />
Saliva, All, M21, M24, M42<br />
Salivette, M17<br />
SAMHSA, F14<br />
Sampling, A20<br />
San Francisco, P28<br />
Scatchard Analysis, M3<br />
Science and law, A9<br />
Screening, A28, A40, A62, F23<br />
Sebum, MI9<br />
Segmental Hair Analysis, M6, M32<br />
Self-injurious behavior, B14<br />
Page 406
Serotonin metabolites, PSO<br />
Sertraline, PS4<br />
Serum, B16<br />
Sexual assault, B7<br />
Sildenafil, PS<br />
S ilymarin, B 16<br />
Skelaxin, P7<br />
SNRI, A46<br />
Sodium chloride, A27<br />
Soils, C4<br />
Solid Phase Extraction, A14, A23, A41,<br />
AS3, A62, MI, Pl6<br />
Solid Phase Microextraction, A2, Ml<br />
Specimen validity testing, F2<br />
STA, A83<br />
Stability, A47, PIO<br />
Standard addition, A 71<br />
Statistical evaluation, P38<br />
Street heroin markers, F9<br />
Strychnine, A41<br />
Substance abuse, P30<br />
Substitution therapy, C 1<br />
Sulfonylurea, PIO<br />
Supercritical Fluid Extraction, M 19<br />
Surfactant, C 14<br />
Survey, AS<br />
Sweat, M29, MSI<br />
Sweat patch, M38<br />
Tetrodotoxin, C16<br />
THC, A30, AS6, M27, M31, M38, M48,<br />
M49<br />
THC metabolites, F27<br />
Therapeutic drug monitoring, A 19<br />
Tissue Distribution, P2<br />
Tissue Samples, P16<br />
Toxicity, C14, PS6, PS8<br />
Toxicokinetic, Cl2<br />
Toxicology, A9, A46, CS, M44, P26<br />
Trace analysis, M4<br />
Traffic safety, BI<br />
Tramadol, PI7, PSI<br />
Tricyclic antidepressants, P6<br />
Tryptamines, A6I, A67<br />
Turkey, BII<br />
Turnaround time, FI<br />
Underground water, C4<br />
Urinalysis, F6, FlS, F18<br />
Urinary sulfate metabolites, F3<br />
Urine, A23, A33, F7, F12, F21, F27<br />
Urine Drug Screen, M34<br />
Urine Drug Testing, MSO<br />
Vagina, C16<br />
Validation, A8, C21<br />
Vegetables analysis, C4<br />
Vigilance, F22<br />
Vitamin C, Bl6<br />
Vitreous fluid, P47<br />
Vitreous humor, P6S<br />
Washing, M8<br />
Whole blood, A14, A23, A34, ASO, A64,<br />
A78<br />
Withdrawal, PS4<br />
Workplace, F13<br />
Page 407
Presenting Author Index <br />
.<br />
· A' Zary, Edward<br />
F17<br />
I Chen Meng<br />
A47<br />
i Adamowicz Piotr<br />
C32 Cheng. W C<br />
Fl8<br />
I Akgur 5 A Bll · Chien Beckie F4<br />
AI-Ahmadi Tareq A72 Choo Robin E C22<br />
Anderson Dan P2 I Chung, Hee-5un MS I<br />
· Andrenyak, David M A1S • Chung, Heesun PS<br />
~r,MikeK A46 i Chung, H 5 P44 I<br />
Anne Lakshmi C13 ! Clarke Joe M1S<br />
Augsburger, Marc B13 • Clarkson Jayne E PS3 i<br />
Avella, Joseph P6 i Clelland Brandi L All<br />
Avila,S B12 I C<strong>of</strong>finq, Mary J A48 i<br />
• Aydin Handan C20 Colangelo C H C4<br />
Baker, Daniel D P20 Collison Ines B P63<br />
LBaker, Ginger PSl Cone Edward J M49<br />
! Balikova, Marie C29 Cooper, Gail Ml6<br />
Balikova, Marie P36 • Coopman, Vera P48<br />
• Barroso M A4l I Couper, Fiona J P40<br />
Battah A H PlO i Coyer Michael J Fl<br />
Beck Ol<strong>of</strong> A33 ! Croal Bernard P3l<br />
I<br />
• Behonick George 5 P22 • Cruickshank Yvonne M2<br />
Belhadj-Tahar H C7 : Darwin t William D Ml7<br />
Bellissima Brandi L AlO Davis Paul J A56 !<br />
• Bernhard, W P24 De Jesus Rosa E A70<br />
Beyer, J C30 • De MartiniS, Bruno 5 Ml8<br />
· Bishop, Sandra C A74 I Diaz-Vazquez liz M Ml9<br />
~m LeeM C3 ! Dresen, Sebastian A76<br />
Boettcher, Michael C2 I Druid Henrik P30<br />
!<br />
Bogusz, Maciej J A39 Drummer Olaf H PS8<br />
Boland Diane M P2l ! Duffort, G M20<br />
· Bosman I J P33 I Dumestre-Toulet, V P49<br />
I Braithwaite R A Pl3 I Edinboro Leslie E F7<br />
I Brewer William E A30 Elliott Simon P43<br />
I Burrows David L F5 · Fang, WenfCl~ A83<br />
! Burt, Martha J P55 FeeneYI Michael A58<br />
: Burton Fiona C B8 Feldman, Michael A3S<br />
I Bush, Donna M F19 Ferrara Santo D B10<br />
~I§!r, Jessie C<br />
C8<br />
C26<br />
~ii LA<br />
I Bynum Nichole D<br />
P17 Ferrari l A<br />
P3S<br />
CalieryL Patrick 5 P39 ~erald Robert l C25<br />
Cardona Patrick 5 A29 est, A RW P64<br />
! Cawley, Adam F3 Fortner Neil F8<br />
Caylor Curtis P47 Frison G A2<br />
: Cazenave, S.O.S. A7S Fritz, Kristina P23<br />
Cervenak Juraj P7 Fucci Nadia P38<br />
Chang, Yan C33 Fuller Dwain C A16<br />
Chasin, A M AS Gautam l<br />
Lata M3<br />
Page 409
Gelhaus, Stacy L<br />
A77 • Laloup, Marleen<br />
A50<br />
! Gergov Merja<br />
A49 Lambert Willy<br />
A79<br />
Gerostamoulos Jim P25 Larson Scott F27<br />
Giroud C B3 · Lebrun B A12<br />
Gordon Ann M C28 i Lechowicz, Wojciech A34<br />
•<br />
i Goulle, J P A22 i Lemos, N P P28 i<br />
• Hackett Jeffery A23 Leong, H S M7<br />
Hamzah Asimah F23 I Lewis Russell J P42<br />
• Harden Wat L M4 ! Lim, Mi-ae F1S<br />
Hayakawa, Hideyuki P4 Linden Rafael A62<br />
Hegstad, S F21<br />
!<br />
Liu, HSiu-Chuan F16<br />
Helander A A36 Liu, Ray H A63<br />
i Hieda Yoko C14 Lood Yvonne A1<br />
Hirata Yukari A66 Lyle Charles R M21<br />
Hodda A E P6S Maralikova Barbora A13<br />
Horak Erica All • Maresova Vera F2S I<br />
Huang, Wei A84 Margalho C A14<br />
Huestis Marilyn A M47 Marinetti Laureen J I PS4<br />
Humbert, L C31 Martinez, Maria A I C24<br />
Itoh, Shinobu ASS Martins, Liliane M10<br />
i Jannetto Paul J AS7 Marti-Ortiz, A A6<br />
• Jayashanker G CS Maurer, Hans H A38<br />
i Johansen Sys S A78 Mayer J P26<br />
Johnson, R D PSO • Mazarr-Proo, Susan P46<br />
Jordan S A19 McGrath Kelly K P27<br />
Juhascik Matthew B7 McIntyre lain M P62<br />
Jurado C Mll l\1cKaque Kathleen A40<br />
Kacinko Sherri L MS1 McMullin Matthew F26<br />
Kala Maria BS Meatherall Robert A64<br />
• Kaneko, Rina A59 Meenan Gerard A32<br />
! Karch Steven B C34 Merves, Michele L M4S<br />
Kardos Keith M48 Mireault Pascal AS2 .<br />
~ovsek Majda Z B6 Mobley, P L F12<br />
shik Romina A60 ! Monforte Joseph R F24<br />
Kerrigan Sarah PS7 Moody, David E F6<br />
Kiat Wenceslo Cll Morl, Tomohisa 814<br />
Kikura-Hanajiri R A61 Moringa Masatoshi AS1<br />
Kim Insook M22 Mozayani Ashraf S<br />
• Kim Jin Y M41 Muller 18 A20<br />
• Kinkennon Amy A31 \\1ura, P B1<br />
! Kintz P M13 Mussh<strong>of</strong>f F M12<br />
· Klys Malgorzata P9 Mykkanen, Sirpa A80<br />
i Koski A P37 Namera A A7<br />
Kraemer Thomas B4 Namiki, Mizuho C17<br />
Krist<strong>of</strong>fersen Lena A4S i Nebro Wesenyalsh M23<br />
Kronstrand, Robert M14 Nippert H P52<br />
!<br />
Kucmanic, John J A24 Noort D C23<br />
Kuqelberq, F C P3 • Nunes-Daniel F P18<br />
Kuntz, David J F2 O'Hanlon, L M1<br />
• Kupiec, Thomas M24 Ojanpera I1kka A69<br />
! Labat, L F22 Papa, Vincent M Fll<br />
Page 410
Parker Dawn R<br />
PS6<br />
Paterson Sue<br />
F9<br />
I Paul Buddha D<br />
A4<br />
~e MichelieR<br />
M44<br />
Pehourcq, Fabienne<br />
C6<br />
Peters, Frank T<br />
C21<br />
Petrova, V<br />
P41<br />
Pichini S<br />
M46<br />
Pirnay,S<br />
P45<br />
i Poklis l Alphonse<br />
C19<br />
Poklis Justin L<br />
P34<br />
· Polettini A P29<br />
: Portman M B1S<br />
i Pragst, Fritz<br />
B2<br />
Proenca P<br />
P14<br />
I Quintela, 0<br />
M2S<br />
i Ragoucy-Sengler, Catherine<br />
M26<br />
Raikos, Nikolaos<br />
A54<br />
: Rasanen, llpo A21<br />
Razatos Gerasimos<br />
A18<br />
Rivadulla, Manuel<br />
M27<br />
· Ropero-Miller Jeri D P19<br />
ISahu C R<br />
C12<br />
I Saisho, K<br />
A43<br />
· Samkova, H P32<br />
Sandberg, Michelle<br />
PS9<br />
Sasaki, Tania A<br />
A42<br />
Schaffer Michael<br />
M8<br />
Scheidweiler 1 Karl B<br />
M28<br />
• Schur B C<br />
P60<br />
Schwilke Eugene W<br />
M29<br />
I Scott Karen S<br />
M6<br />
Shalan M G<br />
B16<br />
· Simonsen K W A44<br />
! Sklerov, Jason H A2S<br />
• Smith AC<br />
B9<br />
• Snyder Ann<br />
MSO<br />
i Soper John W<br />
flO<br />
• Stankova, Marie<br />
P1<br />
Steenkamp, Paul A<br />
P12<br />
Steent<strong>of</strong>t, A<br />
A8<br />
Stimpfl T<br />
P16<br />
Stripp, Richard<br />
A6S<br />
Sutheimer Craig A<br />
• Swienton Anjali R<br />
Tacker, Danyel H<br />
Takaichi Kenichi<br />
Tasduqi SA<br />
Teixeira, H M<br />
Tsatsakis Aristidis<br />
Tsujino Yoshio<br />
Tyler Mark<br />
i Vallejo! Yli R<br />
I Valouch, Tara J<br />
! Van Bocxlaer, Jan F<br />
• Verstraete Alain<br />
Villain M<br />
i Vorce Shawn P<br />
· Vorisek V<br />
Wada Kentaro<br />
! WagnerL Michael A<br />
Wan Terence SM<br />
Wang, M<br />
• Waumans D<br />
Weinmann Wolfgang<br />
Westenbrink, William<br />
Wicks John<br />
• Wille, Sarah<br />
Wilson J M<br />
Wilson Lisa<br />
~<br />
Wolf Carl E<br />
Wonq, Raphael C<br />
i Wong L Steve<br />
i Woodall, Karen<br />
I Wtsadik Abraham T<br />
i Wu Anthon'i<br />
· Yang, Wonkyung<br />
Yashiki, Mikio<br />
• Yazzie Janice<br />
~nglCY<br />
~g, Michael S<br />
Zaney, M E<br />
Zuba, Dariusz<br />
Zweigenbaum, Jerry<br />
F20<br />
A9<br />
M43<br />
M30<br />
C18<br />
M31<br />
M32<br />
C1S<br />
617<br />
M33<br />
Pll<br />
A82<br />
A3<br />
M9<br />
A67 <br />
C1 <br />
C10 <br />
M34 <br />
A37 <br />
AS3 <br />
A26 <br />
A68 <br />
F13 <br />
M35 <br />
A81 <br />
C9 <br />
M36 <br />
C27 <br />
M37 <br />
P61 <br />
P8 <br />
M38 <br />
Fl4 <br />
M39 <br />
C16 <br />
A27 <br />
M40 <br />
M42 <br />
A73 <br />
A17 <br />
A28 <br />
Page 411
Scientific Session <br />
<strong>Abstracts</strong>: <br />
Analytical Methods <br />
Page 113
At<br />
DETERMINATION OF PHENETHYLAMINE· AND PIPERAZINE·DERIVED DESIGNER<br />
DRUGS IN URINE BY GAS CHROMATOGRAPHY-MASS SPECTROMETRY<br />
Yvonne Lood* and Arne Eklund, National Board <strong>of</strong> <strong>Forensic</strong> Medicine, Department <strong>of</strong><strong>Forensic</strong> Chemistry,<br />
University Hospital, SE-5S1 S5 Linkoping, Sweden<br />
New designer drugs have appeared on the illicit drug market during the last years. Many <strong>of</strong> these drugs are<br />
easily available on the Internet and there are several web sites that give a lot <strong>of</strong> information about these<br />
substances. <strong>Forensic</strong> laboratories are continuously in need <strong>of</strong> complementary addition <strong>of</strong> existing methods<br />
or developing new methods for these substances. Screening <strong>of</strong> urine samples for amphetamines in our<br />
laboratory is routinely done by enzyme immunoassay and those giving positiv results are confirmed by<br />
another analyze. The urine is analyzed by gas chromatography-mass spectrometry (GC-MS) in the selected<br />
ion monitoring mode (81M) after liquid-liquid extration with isooctane followed by derivatization with<br />
tritluoroaceticanhydride. This method is quantitative for amphetamine, methamphetamine, MDMA, MDA<br />
and qualitative for MDEA, MBDB, phentermine, phenylpropanolamine, ephedrine, pseUdoephedrine and<br />
phenmetrazine. If the result <strong>of</strong> this method is negative in spite <strong>of</strong> positive immunological testing or if the<br />
police or the pathologists have a request about other central stimulating designer drugs we use our method<br />
for phenetylamines and piperazines. It is a rapid and simple method because we use the sample extract<br />
from the former analysis and just reinject it on the GClMS using the SIM. Verification <strong>of</strong> a positive result<br />
is done by full scan analysis and searching in our own reference library. The method was developed for<br />
identification <strong>of</strong> the phenetylamines p-methoxyamphetamine (PMA), p-methoxymethamphetamine<br />
(PMMA), 4-methylthioamphetamine (4-MTA), 3,4,5-trimethoxyamphetamine (TMA), 2,5-dimethoxy-4<br />
methylamphetamine (DOM), 4-bromo-2,5-dimethoxyamphetamine (DOB), 4-chloro-2,5<br />
dimethoxyamphetamine (DOC), 4-ethyl-2,5-dimethoxyamphetamine (DOET), 4-bromo-2,5<br />
dimethoxyphenetylamine (2C-B), 4-iodo-2,5-dimethoxyphenetylamine (2C-I), 4-ethyl-2,5<br />
dimethoxyphenetylamine (2C-E), 3,4,5-trimethoxyphenetylamine (mescaline) and the piperazines N<br />
benzylpiperazine (A2), N-(3-tritluoromethylphenyl)piperazine (TFMPP), N-( 4-methoxyphenyl)piperazine<br />
(MeOPP) and N-(3-chlorophenyl)piperazine (CPP). The selection <strong>of</strong>substances included in the method was<br />
dependent on the seizures done by the police and the availability <strong>of</strong>the substances. Seven <strong>of</strong>the substances<br />
were kindly received from the National Laboratory <strong>of</strong><strong>Forensic</strong> Science, Linkoping, Sweden. Immunoassay<br />
screening methodology is <strong>of</strong> limited value in detecting designer drugs in urine because <strong>of</strong> low cross<br />
reactivity for most <strong>of</strong> these substances. When a case, with clearly symptoms <strong>of</strong> being under the influence <strong>of</strong><br />
central stimulant, needs to be investigated the described method is used even if the urine has been tested<br />
negative with immunological methods. In November 2003 one 17-year- and two IS-year-old males were<br />
found positive for 2C-E. They were caught by the police in the street showing symptoms that indicated<br />
ingestion <strong>of</strong> some narcotics. The urine samples were negative for screening but we analyzed further with<br />
the method for phenetylamines and piperazines and could by that identify 2C-E. The concentrations were<br />
2,1 IlglmL, O,S Ilg/mL and 0,06 IlglmL respectively. Until today we have in 54 cases identified and verified<br />
seven <strong>of</strong>these substances in urine samples, 2C-E, MeOPP, A2, DOC, PMA, PMMA and 4-MT A.<br />
Keywords: Designer drugs, Amphetamines, GC-MS<br />
Page 115
A2 <br />
DETERMINATION OF AMPHET AMINE-RELA TED DRUGS IN BIOFLUIDS BY GCIMS<br />
AFTER AQUEOUS-PHASE DERIV A TIZA TION WITH 2,2,2 TRICHLOROETHYL<br />
CHLOROFORMATE AND SOLID-PHASE MICRO EXTRACTION<br />
G. Frison"', L. Tedeschi, D. Favretto, S. Maietti, F. Castagna, A. Nalesso, S.D. Ferrara, <strong>Forensic</strong><br />
Toxicology and Antidoping, University Hospital <strong>of</strong> Pad ova, Via Falloppio 50,1-35121 Padova, Italy<br />
The potential <strong>of</strong> 2,2,2-trichloroethyl chlor<strong>of</strong>ormate derivatization for the GCIMS analysis <strong>of</strong> a large range<br />
<strong>of</strong> amphetamine-related drugs (ARDs) and ephedrines in plasma, urine and hair samples has recently been<br />
demonstrated.<br />
A new and simpler analytical approach has been developed for ARDs bioanalysis, based on aqueous-phase<br />
2,2,2 trichloroethyl chlor<strong>of</strong>ormate derivatization, subsequent direct solid-phase micro extraction (SPME) <strong>of</strong><br />
derivatives, and their GCIMS detection.<br />
Preliminary studies on amphetamine, MDMA, MBDB, TMA and DOB have been carried out to check<br />
feasibility <strong>of</strong> derivatization in aqueous conditions and to optimize reaction conditions. Comparative studies<br />
were undertaken to optimize SPME conditions: choice <strong>of</strong> SPME fiber, working pH, effects <strong>of</strong> salts,<br />
adsorption temperature, and adsorption and desorption times.<br />
Results demonstrate that: ARDs can be derivatized in aqueous phase with 2,2,2 trichloroethyl<br />
chlor<strong>of</strong>ormate; carbamate derivatives can be extracted by direct immersion SPME; a simple and fast<br />
analytical procedure can beappUed for sample preparation and GCIMS analysis (1.2 ml sample total<br />
volume, 5 III derivatizing agent, reaction time 5 min, use <strong>of</strong> a PDMS 100 SPME fiber, buffered working<br />
conditions at pH 9, absence <strong>of</strong> salts, SPME adsorption temperature 30°C and time 20 min).<br />
The procedure has been successfully applied to the analysis <strong>of</strong> blank, spiked and true positive plasma, urine<br />
(0.5 ml) and hair (50 mg) samples.<br />
Key words: Amphetamines, Chlor<strong>of</strong>ormates, SPME.<br />
Page 116
A3 <br />
COMPARISON OF THE SENSITIVITY AND SPECIFICITY OF SIX IMMUNOASSAYS FOR THE<br />
DETECTION OF AMPHETAMINES<br />
Alain Verstraete' and Fien Vander Heyden, Laboratory <strong>of</strong> Clinical Chemistry, Section Toxicology, Ghent University<br />
Hospital, De Pintelaan 185, B·9000 Gent<br />
Introduction: In drug <strong>of</strong> abuse screening, the ideal amphetamine immunoassay should detect amphetamine and the<br />
different illicit amphetamine analogues (e.g. MDMA, MDEA, MDA) without false positive results from anorectics,<br />
other stimulants or other drugs like ranitidine. We compared the sensitivity and specificity <strong>of</strong> 6 commercial urine<br />
amphetamine immunoassays for the analysis <strong>of</strong> the urine samples that were sent to our laboratory during a 2.5·month<br />
period.<br />
Methods: Two hundred twenty five urine samples that had been sent to our laboratory for screening or confirmation<br />
<strong>of</strong> amphetamines were analyzed for amphetamines with the FPIA amphetamine/methamphetamine II assay (on<br />
Abbott ADx and AxSYM instruments), EMIT (Emit II Plus Monoclonal AmphetaminelMetamphetamine Assay and<br />
the new EMIT II Plus Amphetamines Assay) and KIMS (standard protocol and MDMA protocol, KIMS and KIMS<br />
X respectively). All assays were calibrated and used semi·quantitatively. All samples that screened positive by any<br />
amphetamine screening method and 15% <strong>of</strong> the negative samples were confirmed by LC-MS/MS. Briefly, 10 ilL <strong>of</strong><br />
urine was mixed with 90 ilL <strong>of</strong> a mixture <strong>of</strong> deuterated internal standards and 20 ilL was injected in the LC-MSIMS.<br />
The assay LOQ is less than 15 ng/mL <strong>of</strong> amphetamine, methamphetamine, MDMA, MDEA, MDA, 4·MTA and<br />
PMA. A sample was considered positive for amphetamines if any <strong>of</strong> these substances was present at > 200 ng/mL.<br />
Results and discussion.·_Ninety·one (40%) <strong>of</strong> the samples were positive by LC-MS/MS. The number <strong>of</strong> positive<br />
samples, lowest, median and highest concentration (in ng/mL) are 74, 71, 2560 and 155000 for amphetamine, 1,33,<br />
33 and 33 for methamphetamine, 27, 46,5975 and 108000 for MDMA, 23, 15,516, 12400 for MDA and 4,27, 1530<br />
and 24800 for MDMA. MBDB, 4-MTA and PMA were not found.<br />
Some c haractenstlcs 0fthe d'ff< I erent assays are given İn tea h t ble:<br />
ADx AxSYM EMIT EMITN KIMS KIMSX<br />
Area under the ROC curve 0.999 0.988 0.977 0.984 0.975 0.972<br />
95% confidence interval 0.982<br />
1.000<br />
0.963·<br />
0.998<br />
0.948<br />
0.993<br />
0.958<br />
0.996<br />
0.944·<br />
0.991<br />
0.941<br />
0.990<br />
Optimal cut-<strong>of</strong>f (ng/mL) 350 677 565 271 404 493<br />
Sensitivity at the cut-<strong>of</strong>f (%) 98.9% 95.6% 96.6% 90.9% 94.4% 93.3% I<br />
Specificity at that cut-<strong>of</strong>f(%) 98.5% 97.8% 90.2% 100% 88.5% 89.3%<br />
# false negatives at that cut-<strong>of</strong>f 1 4 3 8 5 6<br />
# false positives at that cut-<strong>of</strong>f 2 3 13 0 15 14<br />
i # false negatives at 500 ng/mL 2 4 3 19 11 7<br />
, # false positives at 500 ng/mL 2 15 18 0 11 14<br />
Discussion and conclusion: The best results were seen with the Abbott ADx assay that is not available anymore in<br />
Europe. If the cut-<strong>of</strong>f is increased to 677 ng/mL, the AxSYM gives a low number <strong>of</strong> false positives and negatives.<br />
The new EMIT assay has excellent specificity, but misses more true positive samples: 2 samples containing<br />
amphetamine (225 and 253 ng/mL), 1 sample containing MDA (231 ng/mL), 4 samples containing MDMA (319<br />
2760 ng/mL and MDA (113-516 ng/mL) and one sample containing amphetamine and MDMA). For the older EMIT<br />
assays and both KIMS methods, there was more overlap between negative and positive samples, reSUlting in a high<br />
number <strong>of</strong> false positives. The optimal cut-<strong>of</strong>fs, calculated by analysis <strong>of</strong>the receiver operating characteristic curves,<br />
varied between 271 and 677 ng/mL. Use <strong>of</strong> 500 ng/mL cut-<strong>of</strong>f doesn't change much for the ADx and KIMS X<br />
assays, increases the number <strong>of</strong> false positives for AxSYM and EMIT, and increases the number <strong>of</strong> false negatives<br />
for the new EMIT method and the KIMS method.<br />
Keywords: Amphetamine, MDMA, Immunoassay<br />
Page 117
A4 <br />
(R)-(-)-a-METHOXY-a-(TRIFLUOROMETHy)PHENYLACETYL CHLORIDE (MTPA) AS AN<br />
USEFUL CHIRAL REAGENT FORENANTIOMERIC SEPARATION AND QUANTITATION OF<br />
AMPHETAMINE, METHAMPHETAMINE, MDA, MDMA, AND MDEA IN URINE SPECIMENS<br />
Buddha D. Paui', John Jemionek, David Lesser, Aaron Jacobs, and Douglas A. Searles, Division <strong>of</strong><br />
<strong>Forensic</strong> Toxicology, Office <strong>of</strong> the Armed Forces Medical Examiner, Armed Forces Institute <strong>of</strong> Pathology,<br />
Rockville, Maryland20850 and Navy Drug Screening Laboratory, San Diego, California 92134<br />
In drug testing, the presence <strong>of</strong> methamphetamine in urine is generally confirmed by a GC-MS method.<br />
Prior to confirmation, the basic drug is derivatized to a suitable pertluoroalkylamide for better<br />
chromatographic separation. Once methamphetamine is detected, a second GC-MS test is necessary to<br />
distinguish positive results from medical use <strong>of</strong> Vick's inhaler or selegiline (Deprenyl). R-( -)<br />
Methamphetamine is the urinary product from use <strong>of</strong> these medications. The second GC-MS test is to<br />
confirm the illicit use <strong>of</strong> (S)-(+)-methamphetamine. In the procedure, the two methamphetamine isomers<br />
are changed to the chromatographically separable diastereomers by a chiral derivatizing agent, (S)-(-)<br />
trifluoroacetylprolyl chloride (TPC). But the method has inherent limitations. Racemization <strong>of</strong> the reagent<br />
produces mixed diastereomers even from pure (S)-(+)-methamphetamine. Instead <strong>of</strong> using TPC, we utilized<br />
(RH-)-a-methoxy-a-(trifluoromethyl)phenylacetyl chloride (MTPA) to prepare the diastereomers <strong>of</strong><br />
methamphetamine amide. The reagent showed no recemization because it contained no a-proton next to the<br />
carbonyl function. The method was extended to resolve GC peaks <strong>of</strong> (R)-(-)- and (S)-(+)-isomers <strong>of</strong><br />
amphetamine, 3,4-methylenedioxyamphetamine (MDA), N-methyl-MDA (MDMA) and N-ethyl-MDA<br />
(MDEA). Three ions from the drug and two ions from the deuterated internal standard were monitored to<br />
characterize and quantitate the drugs. For MDEA, only one ion was used. The compounds in urine after<br />
acid-base separation and solvent extraction were derivatized by (R)-(-)-MTPA and tested by the GC-MS.<br />
The quantitation was linear over 25 to 5,000 nglmL for MDEA and 25 to 10,000 nglmL for all other drugs.<br />
Correlation coefficients were >0.996. Precision calculated as the coefficient <strong>of</strong> variation at the calibrator<br />
concentration <strong>of</strong> 500 nglmL was within ±ll% for all drugs. The method was applied to test forty-three<br />
urine specimens. In 95% <strong>of</strong> the methamphetamine-positive specimens, only the (S)-(+)-isomer was<br />
detected. In all MDMA-positive specimens, the concentrations <strong>of</strong> (RH-)-isomer were greater than that <strong>of</strong><br />
the (S)-(+)-isomer indicating longer retention <strong>of</strong> (R)-(-)-MDMA in the human body. In all specimens the<br />
total enantiomer concentrations (R + S) detected by the MTPA method compared well with that <strong>of</strong> a nonchiral<br />
method that used 4-carboethoxyhexafluorobutyryl chloride as derivatizing agent (I ~ 0.650, tail<br />
2.069, N=24, 95% confidence). But the MTPA method has some advantage. It alone can replace the two<br />
GC-MS methods needed to confirm the presence <strong>of</strong> (S)-(+)-isomers <strong>of</strong> amphetamine and<br />
methamphetamine.<br />
Keywords: Amphetamine!Methamphetamine, MDAlMDMA, Enantiomer separation<br />
Page 118
AS <br />
SURVEY ON FORENSIC TOXICOLOGICAL ANALYTICAL LABORATORIES IN BRAZIL<br />
E.F. Mendes, V.F. Barbosa, N.F.G. Pereira, and A.M. Chasin*, REBLAS/ANVISA I Brazil; <strong>Forensic</strong><br />
Toxicology Lab, Medical Legal Institute- SP and College <strong>of</strong>Phannacy Oswaldo Cruz, Sao Paulo- Brazil<br />
<strong>Forensic</strong> Toxicology in Brazil is carried out, principally, by public laboratories, except for Doping and<br />
Workplace Drug Testing that are done in private laboratories. Compared to other countries, there are neither<br />
established guidelines to orient these analyses nor a system <strong>of</strong> certification to orient Toxicological Analyses,<br />
in general, and specifically for forensic purposes.<br />
This paper had as objectives the following: to identify the laboratories that work with or have the potential to<br />
carry out tests pertaining to <strong>Forensic</strong> Toxicology and the respective assays, as required by the current public<br />
health legislation, as well as the methodologies used and the Quality Systems followed by this labs; to<br />
evaluate, beforehand, the technical capacity <strong>of</strong> these laboratories and what they must do in order to be<br />
qualified by the Brazilian Network <strong>of</strong> Laboratories in Public Health REBLAS/ANVISA (the Brazilian<br />
Agency for Health and Sanitary Safety Vigilance and Management).<br />
A survey was prepared <strong>of</strong> several assays carried out by the labs and were divided in three major groups:<br />
Group I - Analysis <strong>of</strong> Controlled Substances and Abusive Drugs in materials seized by the Police (in natura),<br />
with 120 assays; Group II - Presumptive Tests and Confinnation <strong>of</strong> Controlled Substances and Abusive<br />
Drugs in Biological Matrices in vivo, with 1000 assays; Group III Presumptive Tests and Confirmation <strong>of</strong><br />
Controlled Substances and Abusive Drugs in Biological Matrices post mortem, with 906 assays. Also<br />
included were a "Survey on Quality Systems" and a "Registration Card".<br />
The surveys were prepared with the aim <strong>of</strong> dividing substances up into categories and respective subcategories,<br />
with the most representative substance tests being included. The presumptive and the confinnation<br />
tests were included for all groups. Fifteen labpratories, representing all Brazilian geographic regions, took part<br />
in the research. The regions <strong>of</strong> South and Southeast Brazil were the most represented, each one with six<br />
participating laboratories, although the regions <strong>of</strong> North, Northeast and Middle-East Brazil also participated,<br />
with only one laboratory, however, presenting analyses <strong>of</strong> Group I. Of the 15 laboratories taking part in the<br />
research, only 9 <strong>of</strong> them answered to the Group I survey; 3 answered to both Group I and Group II; 2<br />
laboratories answered only to Group II and only 1 laboratory, located in Southeast Brazil, declared that they<br />
had completely carried out the Group III survey.<br />
Most <strong>of</strong> the laboratories taking part (80%) carried out the Group I assays- Analysis <strong>of</strong> Control led Substances<br />
and Abusive Drugs. Group II Presumptive Tests and Confirmation <strong>of</strong> Controlled Substances and Abusive<br />
. Drugs in Biological Matrices in vivo was carried out by 33% <strong>of</strong> the institutions and Group III - Presumptive<br />
Test and Confirmation <strong>of</strong> Controlled Substances and Abusive Drugs in Biological Matrices post mortem was<br />
carried out by only one laboratory (6.6% <strong>of</strong> the laboratories studied). It was concluded that 26% <strong>of</strong> the<br />
laboratories taking part in the research still do not follow any <strong>of</strong> the quality parameters. The infonnation from<br />
the Survey will serve as a basis for preparing policies, establishing and managing <strong>Forensic</strong> Toxicological<br />
Laboratories in Brazil.<br />
Keywords: Brazil, <strong>Forensic</strong> Laboratories, Survey<br />
Page 119
A6 <br />
APPLICABLE CRITERIA IN DETERMINING LIMITS OF DETECTION (LOD)<br />
A. Marti-Ortiz·, V.R. Hernandez, B. Mauricio, and N. Santiago<br />
University <strong>of</strong> Puerto Rico School <strong>of</strong> Pharmacy, Chemical <strong>Forensic</strong> Laboratories, San Juan, Puerto Rico<br />
00936<br />
The proposed HHS SAMHSA guidelines for the analysis <strong>of</strong> drugs <strong>of</strong> abuse will affect directly or indirectly<br />
a very large number <strong>of</strong> laboratories involved in workplace drug testing. The acceptance <strong>of</strong> the analysis <strong>of</strong><br />
alternative matrices and the varied instrumentation used poses regulatory and forensic challenges. The<br />
criteria that a laboratory employs to attest as to the presence <strong>of</strong> drug are <strong>of</strong> the utmost importance.<br />
Chromatographic and mass spectral behavior <strong>of</strong> chemical species at the instrumental limit <strong>of</strong> detection is<br />
subject to variability as the method is being challenged at its limit <strong>of</strong> performance. A number <strong>of</strong> recent<br />
publications have suggested a "relaxation" <strong>of</strong> the chromatographic parameters and propose stressing more<br />
the mass spectral behavior <strong>of</strong>chemical species this could be problematic for forensic defensibility.<br />
As the criteria used to determine the limit <strong>of</strong> detection will affect the limit <strong>of</strong> quantification and the lower<br />
limit <strong>of</strong> linearity <strong>of</strong> calibration curves and fundamentally the performance <strong>of</strong> the method it is <strong>of</strong> the utmost<br />
importance that a laboratory clearly and objectively define the criteria to apply. A comprehensive study<br />
using GCIMS was undertaken to revisit generally accepted chromatographic and mass spectral criteria at<br />
the limit <strong>of</strong> detection. Benzolyecgonine, ll-nor-~ 9 - tetrahydrocannabinol-9-carboxylic acid (THC) and<br />
amphetamines were used to assess the following contributors on limits <strong>of</strong> detection determinations:<br />
matrix background , chromatographic pr<strong>of</strong>iles, mass spectral ion variability and statistical acceptance<br />
criteria. For example, we observed with benzolyecgonine chromatographic variations <strong>of</strong> the individual ion<br />
fragments and ion ratios that would be acceptable or not for the determination <strong>of</strong> LOD depending on the<br />
laboratory criteria.<br />
Advances in analytical instrumentation and techniques are increasingly lowering the limits <strong>of</strong> detection.<br />
Acceptable criteria must comply with existing scientific principles and provide sound forensic evidence as<br />
to be useful in the detection <strong>of</strong> prohibited substances not only in workplace drug testing but also in<br />
laboratories where only the presence <strong>of</strong>the drug is required.<br />
Keywords: LOD, Criteria, <strong>Forensic</strong><br />
Page 120
A7 <br />
QUANTITATIVE DETERMINATION OF AMPHETAMINES AND METHYLENEDIOXY<br />
AMPHETAMINES IN URINE BY MONOLITHIC COLUMN AND HPLC-DAD<br />
A Namera*", M Nishida", M Yashiki", A Nakamoto b , Y Takei", Y Shintani", M FurunoC, H Minakuchid, K<br />
Nakanishi", K Kimura"<br />
a Department <strong>of</strong> Legal Medicine, Graduate School <strong>of</strong> Biomedical Sciences, Hiroshima University,<br />
Hiroshima, b Scientific Investigation Laboratory, Hiroshima Prefectural Police Headquarters, Hiroshima, C<br />
GL Sciences Inc., Tokyo, d Kyoto Monotech, Kyoto, e Department <strong>of</strong> Material Chemistry, Graduate School<br />
<strong>of</strong>Engineering, Kyoto University, Kyoto, JAPAN<br />
Aims: A monolithic silica was developed for a new material <strong>of</strong> a micro or capillary scale HPLC. The<br />
material consists <strong>of</strong> continuous porous silica having a double-pore structure (through-pore and meso-pore).<br />
In this study, we developed a simple extraction <strong>of</strong> amphetamines and methylenedioxyamphetamines from a<br />
small volume <strong>of</strong> urine by using a capillary column packed with a Cis-bonded monolithic silica.<br />
Methods: The mixture <strong>of</strong> sample urine (0.1 ml), buffer and an internal standard was introduced into the<br />
monolithic capillary column using a gas tight syringe. Analytes were adsorbed on. the column and<br />
endogenous interferences were washed with an acidified buffer. Analytes were then eluted with 20-micro-L<br />
<strong>of</strong> a mobile phase and direct injected into a HPLC.<br />
Results: The recoveries <strong>of</strong> amphetamines and methylenedioxyamphetamines from urine were over 90%.<br />
The calibration curves showed linearity in the range <strong>of</strong> 100 - 50,000 ng/g in urine. The coefficients <strong>of</strong><br />
variation <strong>of</strong> intraday and interday were below 10%.<br />
Conclusion: These results demonstrated that the C1s-bonded column was useful for the extraction <strong>of</strong><br />
amphetamines in urine. This column has a potential as a new tool for the extraction <strong>of</strong> chemicals in<br />
biological materials.<br />
Keywords: Amphetamines, Methylenedioxyamphetamines, Monoliths<br />
Page 121
AS <br />
QUANTITATIVE DETERMINATION OF DIAZEPAM AND NORDIAZEPAM IN WHOLE<br />
BLOOD BY<br />
LC-MS/MS<br />
A. Steent<strong>of</strong>t* and K. Wiese Simonsen, Department <strong>of</strong> <strong>Forensic</strong> Chemistry; University <strong>of</strong> Copenhagen;<br />
Denmark<br />
Aims: To present a full validated LC-MSIMS method for quantification <strong>of</strong> diazepam and nordiazepam in<br />
whole blood for routine use.<br />
Methods: Blood samples were extracted with ethyl acetate at pH 9. After evaporation <strong>of</strong> the organic<br />
solvent, the residue was dissolved in solvent. Spiked blood samples (0.0025-2.5 mg/kg diazepam and<br />
nordiazepam) were used for the calibration curve. The analysis was performed on a Quatro micro MSIMS<br />
(Waters) coupled to an HPLC (Agilent). The separation column was a Zorbax SB-C8. The solvent consist<br />
<strong>of</strong> formic acid: ammonium acetate buffer pH 5.0: methanol (0.16:400:400). The masses: mlz 140 for<br />
nordiazepam and mlz 154 for diazepam were used for quantification.<br />
Results: Detection limit was 0,001 mglkg and the quantification limit was 0.002 mg/kg for both<br />
compounds. The calibration curves were linear in the measuring interval. The linearity was evaluated with<br />
polynomial regression. Within day precisions for blood controls spiked at 0.05 mg/kg, 0.5 mglkg and 1.5<br />
mglkg (diazepam and nordiazepam) were
A9 <br />
. RESOURCE GUIDE FOR USERS OF SCIENCE AND TECHNOLOGY AND THE NATIONAL<br />
CLEARINGHOUSE FOR SCIENCE, TECHNOLOGY AND THE LAW<br />
Anjali R. Swienton*, Interim Deputy Director, Director <strong>of</strong> Outreach, National Clearinghouse for Science,<br />
Technology and the Law, Stetson University College <strong>of</strong> Law; SciLaw<strong>Forensic</strong>s, Ltd., 25 Wahlutwood Ct.,<br />
Germantown, MD; Carol Henderson, Director, National Clearinghouse for Science, Technology and the<br />
Law, Stetson University College <strong>of</strong> Law, 1401 61 51 Street South, Gulfport, FL<br />
New challenges for expert witnesses and the legal community have arisen due to recent developments in<br />
science and technology. New technologies and methodologies, as well as fields long considered<br />
established, such as latent print identification and tool marks are facing increased scrutiny. Given this<br />
explosion <strong>of</strong> scientific evidence litigation, scientists, law enforcement, laboratory personnel, judges and<br />
lawyers are overwhelmed by the amount <strong>of</strong> information required to educate them to meet these legal<br />
challenges. Until now, judges, lawyers, scientists and law enforcement personnel did not have one source<br />
that allowed them to navigate all the existing case law, journals, reports, proceedings and other resources<br />
necessary to conduct effective investigations and litigation. The Resource Guide for Users <strong>of</strong>Science and<br />
Technology was created to fill an information need specifically relating to legal issues implicated by the use<br />
<strong>of</strong> new technology in criminal and civil justice. Supported by a joint cooperative agreement between the<br />
NFSTC and NIJ (#2000-RC-CX-K001), the project developed a comprehensive searchable database from a<br />
variety <strong>of</strong> sources covering a wide range <strong>of</strong> topics. The database provides information on topics such as<br />
bloodstain pattern analysis, body scans/retinal scans, digital image enhancement, entomology, expert<br />
witness malpractice, fingerprints, questioned documents, smart cards, toxicology, trace evidence and tool<br />
marks. The Resource Guide covers existing court rulings, pending court cases, scientific and legal articles<br />
from applicable sources, relevant information from books, current and pending legislation, conference<br />
proceedings, university and continuing education courses, and pronouncements from pr<strong>of</strong>essional<br />
organizations. The NFSTCINIJ project produced a searchable CD. The information contained in the<br />
Resource Guide will be included in and expanded upon in the online resource being developed by the<br />
National Clearinghouse on Science, Technology and the Law at Stetson University College <strong>of</strong> Law. The<br />
Clearinghouse is supported by a grant from the National Institute <strong>of</strong> Justice (#2003-I1-CX-K024). In<br />
addition to the development <strong>of</strong> the online resource, the Clearinghouse Program is building partnerships<br />
with law schools, pr<strong>of</strong>essional associations and federal agencies, sponsoring a forensic science/science and<br />
technology seminar series, convening Community Acceptance Panels at the request <strong>of</strong> NIJ, developing<br />
training modules qn a variety <strong>of</strong> forensic disciplines with an emphasis on distance education, and building a<br />
reference collection <strong>of</strong> law, science and technology literature available through interlibrary loan to other<br />
institutions.<br />
Keywords: Science and law, Information, Toxicology<br />
Page 123
AIO <br />
IDENTIFICATION OF BENZODIAZEPINES USING HPLC-ESI-MS-MS<br />
Brandi L. Bellissima·, Diane M. Boland, and W. Lee Hearn<br />
Miami-Dade Medical Examiner Department, Toxicology Laboratory, 1851 NW 10 th Avenue, Miami,<br />
Florida 33136<br />
A confirmatory method for twenty-three commonly detected benzodiazepines in postmortem biological<br />
matrices has been developed using solid phase extraction (SPE) coupled with high performance liquid<br />
chromatography positive ion electro spray ionization tandem mass spectrometry (HPLC-ESI-MS-MS).<br />
Isolation and purification <strong>of</strong> the drugs was performed using mixed-mode SPE columns installed on a<br />
Zymark RapidTrace system. After addition <strong>of</strong> internal standard, samples were diluted with sodium<br />
phosphate buffer and extracted using UCT Clean Screen® SPE columns. The SPE columns were<br />
sequentially rinsed with 2% ammonium hydroxide (NH 40H) in ethyl acetate, methanol, de-ionized water,<br />
and phosphate buffer. Samples were loaded onto the column at a flow rate <strong>of</strong> 2.0mLlmin. The cartridges<br />
were then washed with de-ionized water, followed by a wash with 20% acetonitrile in de-ionized water,<br />
and dried under vacuum prior to elution with 2% NH 4 0H in ethyl acetate mixture. Residues were<br />
reconstituted with the HPLC mobile phase and injected onto a Restek reversed phase C8 HPLC column.<br />
The analytes were eluted at a flow rate <strong>of</strong> 3751ll/min with a solvent mixture composed <strong>of</strong> methanol:water<br />
containing 0.1% formic acid, and detected using an Advantage LCQTM ion trap mass spectrometer.<br />
Positive ion ESI-MS resulted in ion spectra for each <strong>of</strong> the benzodiazepines at their expected retention time<br />
on the LC column. Unique MS-MS spectra for each <strong>of</strong> the benzodiazepines were obtained and matched the<br />
direct infused data acquired with neat standards (See Table I). The limit <strong>of</strong> detection for each<br />
benzodiazepine was estimated from extracted samples with decreasing concentrations. This method<br />
provides a rapid, sensitive approach to isolate, purify and confirm a broad spectrum <strong>of</strong>benzodiazepines.<br />
Table 1 Benzodiazepine Spectral Data<br />
Benzodiazepine Molecular Product Benzodiazepine Parent Product<br />
Ion Ion Ion Ion<br />
IM+Hr (amu) [M+Hr (amu)<br />
(amu)<br />
-(amu)<br />
7 -aminoclonazepam 286 250,222 Estazolam 295 267,192<br />
7 -amin<strong>of</strong>lunitrazepam 284 264,256<br />
H!!<br />
304 276,290<br />
7 -aminonitrazepam 252 121,114 raze pam 388 315,288<br />
Alphahydroxymidazolam 342 203,324 321 303,275<br />
Alphahydroxytriazolam 259 331,279 Midazolam 326 291,244<br />
i Alphydroxyalprazolam 325 297,279 Nltrazepam 282 236,254<br />
: Alprazolam 309 281.274 Nordiazepam 271 243,208<br />
Bromazepam 316 288,261 Norflunitrazepam 300 254,243<br />
Chlordiazepoxide 300 283,241 Oxazepam 287 269,259<br />
Clonazepam 316 270,251 Temazepam 301 283,255<br />
Desalkylfurazepam 289 261,226 Triazolam 343 226,308<br />
I Diazepam 285 257,228<br />
Keywords: Benzodiazepines, HPLC, ESI-MS-MS<br />
Page 124
All<br />
DIRECT ANALYSIS OF MDMA AND METABOLITES IN SALIVA USING CAPILLARY<br />
ELECTROPHORESIS<br />
Brandi L. Clelland-' I, Stephen L. Morgan l , Demi Garvin2, William E. Brewer 3<br />
1 University <strong>of</strong> South Carolina, Department <strong>of</strong> Chemistry and Biochemistry, 631 Sumter St, Columbia, SC<br />
29208; 2Richland County Sheriffs Department, 5623 Two Notch Rd, Columbia, SC 29223; 3Clemson<br />
University Veterinary Diagnostic Center, 500 Clemson Rd, Columbia, SC 29223<br />
Ecstasy, or 3,4-methylenedioxymethamphetamine (MDMA), has gained popularity among young adults in<br />
the past few decades mainly for its euphoric and stimulating effects. Though this drug has a "street"<br />
reputation <strong>of</strong> being safe, case studies have shown its toxic effects. Drug testing in recent years has focused<br />
on. analysis <strong>of</strong> alternative biological specimens because <strong>of</strong> the invasiveness and ease <strong>of</strong> adulteration <strong>of</strong> the<br />
more commonly used blood and urine. Testing <strong>of</strong> saliva as an alternative biological matrix has advantages<br />
over conventional matrices: saliva sampling is noninvasive and the presence <strong>of</strong>MDMA in saliva correlates<br />
with individual being under the pharmacological effects <strong>of</strong> the drug. MDMA is a basic drug with an<br />
approximate pK.= 9.9. At two pH units below the pK., MDMA is fully charged and amenable for<br />
separation by capillary electrophoresis. Analysis <strong>of</strong> MDMA in saliva by CE also does not require<br />
derivatization or extraction; consequently minimal sample pretreatment is required.<br />
Capillary electrophoresis separates analytes by electrophoretic mobility, and allows a simplified rapid<br />
method for drug analysis. On-capillary detection in CE is generally performed by a diode array detector<br />
(DAD). Sample stacking is used to increase the sensitivity <strong>of</strong> the CE-DAD system. This paper demonstrates<br />
methods for the direct analysis <strong>of</strong> MDMA in saliva employing both CE-DAD as well as capillary<br />
electrophoresis/diode array/quadrupole time-<strong>of</strong>-flight mass spectrometry (CE/DAD/Q-T<strong>of</strong>-MS). The DAD<br />
and Q-T<strong>of</strong>-MS provide extremely sensitive on-line detection for CE as well as rapid component<br />
identification by UV-Vis or mass spectra. Limits <strong>of</strong> detection and reproducibility for the detection <strong>of</strong><br />
MDMA and its primary metabolites will be discussed.<br />
Key words: MDMA, Saliva, Capillary electrophoresis<br />
Page 125
A12 <br />
ANALYSIS OF XTC SEIZURES IN THE COUNTY OF TOURNAI (BELGIUM)<br />
B. Lebrun*, E. Noel; IPHB, Toxicology DepartlIjent, 55 boulevard Sainctelette 7000 Mons (Belgium)<br />
P. Ludinant; SJA de Tournai, 19 Dreve de Maire 7500 Tournai (Belgium)<br />
Introduction: By the early 1980s, ecstasy (XTC) was used as a recreational drug. Its consumption became<br />
particularly prominent in the United Kingdom, Spain, the Netherlands, Belgium and Germany. Recently, the<br />
dance culture is growing almost everywhere in Europe. Its usage was even described in less-festive events<br />
like athletic meetings. This led us to collaborate with the "Service Judiciaire d'Arrondissement" <strong>of</strong> Tournai<br />
for more than two years. In Belgium the presence <strong>of</strong> many "megadancing" is on the French - Belgian border.<br />
Relationship between cross-border consumption and cross-border traffic is not clear. Typological data<br />
(weight, logo, diameter, thickness, color ...) does not provide any information regarding synthetic procedures<br />
used by the laboratories nor it provides the location <strong>of</strong> the clandestine laboratories. In order to control the<br />
drug trafficking, it is important to know the synthetic procedures used by the laboratories and also the<br />
distribution networks. In this study we investigated the pr<strong>of</strong>iling <strong>of</strong> impurities in ecstasy and spatial analysis<br />
<strong>of</strong> seizures that could provide useful information to the legal authorities in controlling drug trafficking.<br />
Materials and methods: We analysed 2052 XTC pills received from 857 seizures realised in the County <strong>of</strong><br />
Tournai. Each pill was examined for its colour, diameter, thickness, logo, and weight. The pills were then<br />
analysed for chemical impurities. Five milligram <strong>of</strong> the pill were treated by 1 ml <strong>of</strong> dichloromethane, mixed<br />
for 15 seconds, and centrifuged. The supernatant were separated and evaporated to dryness under nitrogen.<br />
The sample was then dissolved in 250 IJ.I <strong>of</strong> methanol and analysed by GC-MS. Results were encoded in a<br />
database and the pr<strong>of</strong>iling was analysed. Similarities between seizures were recorded in a larger Europol<br />
database. Analytical data were also introduced into a geographical information system in order to identifY<br />
clusters <strong>of</strong> similar pr<strong>of</strong>iles.<br />
Results: The typological analysis showed that sometime logos were not used on the pills. In fact, we<br />
observed four logo-use patterns: I) period for less than a month, 2) for several months, 3) for a year or 4)<br />
with a cyclical appearance. The pattem depends not only on the consumer (bad pills identified very fast) but<br />
also on the trafficker (capacity <strong>of</strong> production, material available). These observations provide information<br />
about the behaviour <strong>of</strong> dealers, traffickers, and tablet makers. The chemical impurities indicated primarily<br />
two synthetic routes used by the clandestine laboratories: one with reductive ami nation and the other with<br />
Leukart's method. The information allowed us to identify pills from different geographic locations and<br />
helped us to monitor and control drug trafficking.<br />
Conclusion: Spatial, typological and chemical results enabled us to build a database. The information is<br />
helpful in identifYing clandestine laboratories. It also provides information on the synthetic route used and<br />
the technical means employed to make the pills. This database permits to unveil links between different legal<br />
cases.<br />
Keywords: XTC, Pr<strong>of</strong>iling MDMA<br />
Page 126
A13 <br />
SCREENING FOR ACE INHIBITORS AND AT-II-ANTAGONISTS IN URINE BY LC-MSIMS<br />
Barbora MaraIikova 1 ,2, Wolfgang Weinmann 1 , Claudia A. Muellerl,' <br />
lInstitute <strong>of</strong> <strong>Forensic</strong> Medicine, University Hospital, Albertstr. 9, D 79104 Freiburg (Germany) <br />
Phone: ++49 7612036878, Fax: ++49 761 2036858, Email: muel1erc@ukl.uni-freiburg.de <br />
2University <strong>of</strong> Par dub ice, FCHT, Department <strong>of</strong> Analytical Chemistry, nam. Cs.legii 565, 53210 <br />
Pardubice, Czech Republic <br />
For the detection <strong>of</strong> Angiotensin-Converting Enzyme inhibitors (ACE inhibitors: enalapril, Iisinopril, <br />
perindopril, captopril, ramipril, cilazapril as prodrug and active drug) and Angiotensin-II-Receptor <br />
Antagonists (candesartan, eprosartan, irbesartan, \osartan, telmisartan, valsartan) an LC-MS/MS target <br />
screening method has been developed to be used in clinical and forensic toxicological analysis. These drugs <br />
are widely used for lowering blood pressure besides betablockers, diuretics and calcium channel blockers <br />
which have been the aim <strong>of</strong> our previous work [I] - and their intake after prescription or even the non<br />
compliance <strong>of</strong> patients, not taking the drugs, could have severe effects on traffic safety. Furthermore, <br />
overdosage <strong>of</strong>these drugs can cause severe lowering <strong>of</strong> the blood pressure. <br />
For method development by LC-MSIMS ESI and APCI mass spectra <strong>of</strong> the compounds have been <br />
compared. ESI was found to be more suitable in terms <strong>of</strong> sensitivity for the ACE inhibitors, whereas the <br />
AT -II-Receptor Antagonists were detectable by both ionization modes. <br />
Linearity for quantitation was found for captopril, cilazapril, enalapril, Iisinopril, perindopril, ramipril and <br />
ramiprilat in the range <strong>of</strong> 10 to 500 nglmL with ESI after extraction from urine. LOD was below 10 ng/ml <br />
in urine. In patients' urine samples the ACE inhibitors were detectable in their active form (carboxylic <br />
form) by electrospray ionization after intake <strong>of</strong> therapeutic doses. However, the active form was not <br />
available as reference substance for all compounds and had to be generated by hydrolysis <strong>of</strong> the esters. The <br />
internal standard still remains a problem for quantitative analysis, since deuterated compounds are not <br />
available. For patients' urine and serum samples Benazepril was used as internal standard for quantitation, <br />
since it was not prescribed for these patients. <br />
Method development for the sartanes included liquid-liquid extraction (LLE). LC-ESI-MRM was found to <br />
be suitable for target screening for these drugs after spiking to urine; irbesartan was detected in a forensic <br />
case. <br />
Results <strong>of</strong> the method development and applications to patients' urine and also some serum samples are <br />
presented. <br />
[1] Mueller CA, Baranda AB, Weinmann W. Screening for l,4-dihydropyridine calcium channel blockers<br />
in plasma and serum by solid-phase extraction and LC-MS-MS. J Mass Spectrom (in Press, <strong>2004</strong>).<br />
Keywords: ACE inhibitors, AT II antagonists, LC-MS/MS<br />
Page 127
A14 <br />
DETERMINATION OF FUROSEMIDE IN WHOLE BLOOD USING SPE AND GCIEI-MS<br />
C. Margalho',!, E. Gallardo!, M. Barroso!, S. Avila!, E. Marques\ D. de Boer, D. N. Vieira!<br />
!Instituto Nacional de Medicina Legal - Portugal<br />
2Instituto Nacional do Desporto Laboratorio de Analises de Dopagem e Bioquimica - Portugal<br />
Introduction: Furosemide (4-chloro-N-furfuryl-5-sulfamoylanthranilic acid) is an anthranilic acid derivative<br />
with strong diuretic potential. It exerts its action on the luminal side <strong>of</strong>the thick ascending limb <strong>of</strong>the Henle's<br />
loop by inhibiting chloride transport or sodium chloride co-transport. This loop diuretic is employed for the<br />
treatment <strong>of</strong> renal diseases, congestive heart failure and hypertension. Although furosemide is included on the<br />
Iist <strong>of</strong> prohibited doping substances, indicated by the World Anti-Doping Agency (W ADA), it is widely used<br />
in sports, mainly in competitions classified by weight or to avoid detection <strong>of</strong>other drugs.<br />
The aim <strong>of</strong> this work was the development and validation <strong>of</strong> a methodology for application in forensic<br />
toxicology. A simple, rapid and validated gas chromatography-electron ionization-mass spectrometry (GeIEI<br />
MS) method is described to evaluate the use <strong>of</strong> whole blood in the quantitation <strong>of</strong> furosemide. A solid-phase<br />
extraction (SPE) technique was used to extract this compound from blood samples.<br />
Materials and Methods: Stock solutions <strong>of</strong> furosemide and ketopr<strong>of</strong>en (internal standard) were prepared in<br />
methanol, protected from light and stored in the freezer at 4°C until use. Extraction - To 1 ml <strong>of</strong> whole blood<br />
were successively added 50 /ll <strong>of</strong> internal standard solution (10 /lglml) followed by furosemide at different<br />
concentrations (0.10,0.25,0.50, 1.00,2.50 and 5.00 /lglml). The mixture was vortex-mixed, sonicated for 15<br />
min and centrifuged for 15 min at 3000 rpm. The sample was extracted using BondElut® -LRC Certify 300 mg<br />
SPE columns and the organic solvent evaporated to dryness in a vacuum rotary evaporator. Selective<br />
derivati=ation - The dry residue was dissolved with 25 /ll <strong>of</strong>tetramethylammonium hydroxide 0.2 M (TMAH)<br />
and injected directly into the chromatographic system. ChromatographiC conditions - Initial oven temperature<br />
was 160°C for 1 min, increased by 20°C/min to 270°C and held for 8.50 min. The temperatures <strong>of</strong> the injector<br />
and detector were set at 2500C and 280°C, respectively. The mass spectrometer was operated at 70 eV in the<br />
electron ionization (El) mode using selected ion monitoring (SIM). The ions were monitored at mI::, 81, 372<br />
and 96 for furosemide and 209, 205 and 268 for ketopr<strong>of</strong>en.<br />
Results: Calibration curves were measured daily, based in one-day assay protocol between 0.10 and 5.00<br />
/lglml, and correlation coefficients were above 0.9910. Control samples at low, middle and high<br />
concentrations <strong>of</strong> furosemide were measured in the same day. The calculated LOD and LOQ were 10.05 and<br />
45.44 nglml respectively. Intraday precision (coefficient <strong>of</strong> variation - CV) was inferior to 7.9 % for all<br />
concentration levels. For the interday precision, the calculated CV was inferior to 13.9 % for all control<br />
samples. The relative recovery calculated for the three levels <strong>of</strong> the control samples (0.30, 0.75 and 3.00<br />
/lglml) were respectively 104%, 89% and 91 %.<br />
Conclusion: A sensitive, specific and reliable procedure has been developed for the determination <strong>of</strong><br />
furosemide in whole blood samples. The experimental work was performed so that all validation parameters<br />
are considered simultaneously in one day <strong>of</strong> assay. We may conclude that the validated methodology is<br />
suitable for the application in forensic toxicology routine analysis.<br />
Keywords: Furosemide, Whole blood, Solid-phase extraction<br />
Page 128
A15 <br />
ANALYSIS FOR LORAZEPAM IN BLOOD AND URINE BY GAS CHROMATOGRAPHY <br />
MASS SPECTROMETRY - POSITIVE CHEMICAL IONIZATION<br />
David M. Andrenyak·. Center for Human Toxicology, University <strong>of</strong> Utah, Salt Lake City, Utah 84112,<br />
USA.<br />
Lorazepam is a benzodiazepine drug that is used to treat anxiety and seizures. It is also prescribed as a pre<br />
operative sedative. Because lorazepam is a powerful CNS depressant and can enhance the effect <strong>of</strong> other<br />
CNS depressants, effective procedures for the analysis <strong>of</strong> lorazepam in biological samples are essential.<br />
This study reports on the analysis for \orazepam by gas chromatography - mass spectrometry (GC-MS) in<br />
biological samples. Liquid - liquid extraction was performed on 1 mL sample volumes using clean,<br />
separate 16 x 100 mm silanized culture tubes with PTFE lined screw caps. Prior to extraction, the urine<br />
samples were hydrolyzed by adding 1 mL <strong>of</strong> 5000 units I mL ~-glucuronidase in 0.1 M sodium Acetate, pH<br />
5.0. The urine samples were incubated 3 hours at 40' C in an incubation oven. Following incubation,<br />
internal standard (100 ilL <strong>of</strong> 1 ng/!lL lorazepam-d 4 ) was added to the urine and unhydrolyzed blood<br />
samples. A 1 mL volume <strong>of</strong> saturated sodium borate buffer (pH 9) and 5 mL <strong>of</strong>toluene: dichloromethane<br />
(70:30) was added to each urine and blood sample. After mixing 20 minutes on a reciprocal shaker, the<br />
tubes were centrifuged at 2000 rpm for 10 minutes. The organic layer was collected into clean, separate 13<br />
x 100 mm culture tubes. The extracts were evaporated to dryness under a stream at air at 40' C using the<br />
Turboevap evaporator. The extracts were derivatized by adding 100 ilL <strong>of</strong> N,O-bis(trimethylsilyl)<br />
trifluoroacetamide +1% trimethylchlorosilane) to each tube. The extract tubes were heated at 70' C for 20<br />
minutes by using a dry block heater. After heating, the extracts were cooled to room temperature and<br />
transferred to clean, separate autosampler vials. The derivative reaction incorporated 2 trimethylsilyl<br />
(TMS) groups on the lorazepam molecule. The derivatized extracts were analyzed by GC-MS using an<br />
Agilent 5973 GC-MSD system. Chromatographic separation was achieved using an HP-1 MS 30 M x 0.25<br />
mm, 0.33 11m film capillary column (AgiJent) and UHP helium (1 mL/min) as the carrier gas. The column<br />
oven temperature program was 125' C, hold O. 2 minutes, 20· C/ minute to 300', hold 7.5 minutes.<br />
Splitless injection with injection port temperature at 250· C was used. The transfer line temperature was<br />
set at 300' C. Positive chemical ionization was utilized with ammonia as the reagent gas and an ion source<br />
temperature at 200' C. Selected ion monitoring was employed to analyze (mlz) 465 for 10razepam-diTMS<br />
and (m/z) 471 for lorazepam-d 4 -diTMS. The 10razepam-diTMS mass spectrum had a base peak at (m/z)<br />
465 and the 10razepam-~-diTMS mass spectrum had a base peak at (mlz) 469. Since 10razepam-diTMS<br />
had a significant (m/z) 469 ion fragment, the (m/z) 471 ion was used to monitor for the lorazepam-~diTMS.<br />
Calibration standards were prepared with blank bovine blood and ranged from 2.5 nglmL to 1000<br />
ngimL. In house controls were prepared with blank blood at 3.5 nglmL, 100 nglmL, 650 nglmL and with<br />
blank human urine at 100 ngimL. In the intra-assay accuracy evaluation, the lorazepam concentration was<br />
within 13% <strong>of</strong> target. In the intra-assay precision evaluation, the coefficients <strong>of</strong> variation were within 8%.<br />
This method was used to analyze blood and urine samples from a post mortem case.<br />
Keywords: Lorazepam , GC-MS, Positive Chemical Ionization<br />
Page 129
A16 <br />
MATRIX DEPENDENT O-DEMETHYLATION OF 3-METHOXY OPIOIDS DURING<br />
DERIVA TIZA TION<br />
Dwain C. Fuller* and Paul J. Orsulak. Department <strong>of</strong> Psychiatry, University <strong>of</strong>Texas Southwestern<br />
Medical Center at Dallas, Dallas, TX and VA North Texas Health Care System, Toxicology 113, 4500<br />
South Lancaster Road, Dallas, TX 75216<br />
Several in-vitro conversions <strong>of</strong> compounds to their metabolites during the extraction process have been<br />
observed by various investigators. Among these are the conversion <strong>of</strong> methamphetamine to amphetamine,<br />
methadone to EDDP, cocaine to benzoylecgonine, and ethanol to acetaldehyde. These authors have<br />
observed the O-demethylation <strong>of</strong> the 3-methoxy opioids, codeine, hydrocodone and oxycodone to their<br />
respective metabolites, morphine, hydromorphone and oxymorphone, during derivatization with N<br />
methylbistritluoroacetamide (MBTFA). The transformation was observed to be dependent on specimen<br />
matrix, incubation time and incubation temperature. It is important for the toxicologist to be aware <strong>of</strong> this<br />
phenomenon when developing analytical assays and interpreting results.<br />
Key words: Opioids, Demethylation, MBTF A<br />
Page 130
A17 <br />
HIGH.PERFORMANCE LIQUID CHROMATOGRAPHY AS AN ALTERNATIVE METHOD<br />
FOR COMPARATIVE ANALYSIS OF SEIZED DRUG SAMPLES<br />
2<br />
Bogumila Byrska\ Dariusz Zuba*\ Malgorzata Swisf, Andrzej Parczewski l •<br />
I Institute <strong>of</strong> <strong>Forensic</strong> Research, ul. Westerplatte 9,31-033 Cracow, Poland; 2 Faculty <strong>of</strong> Chemistry,<br />
Jagiellonian University, ul. Ingardena 3, 30-060 Cracow, Poland<br />
The comprehensive testing <strong>of</strong> seized drug samples performed in forensic laboratories allows identification<br />
and determination <strong>of</strong> the controlled psychoactive substances, identification <strong>of</strong> additives (e.g. caffeine or<br />
paracetamol) and diluents (e.g. palmitylic acid or glucose), as well as chemical impurities. The results <strong>of</strong><br />
analysis deliver information about synthesis methods applied by illegal producers. It is also possible to<br />
establish if the seizure drug samples originate from the same production batch or the same illegal<br />
laboratory and even to link the dealer with drug users. Hitherto, mainly gas chromatographic methods<br />
(GClFlO, GCIMS) are used for this purpose.<br />
The aim <strong>of</strong> the present study was to develop an analytical procedure that makes possible separation <strong>of</strong> the<br />
substances occurring in the seized ecstasy tablets by means <strong>of</strong> the high-performance liquid chromatography<br />
(HPLC). The studies have been carried out on the samples <strong>of</strong> 3,4-methylenedioxymethamphetamine<br />
(MDMA, ecstasy) prepared by different routes: reductive amination, Leuckart reaction and safrole<br />
bromonation. The reductive amination was performed using various reducing agents: sodium<br />
cyanoborohydride, aluminium amalgam and sodium borohydride. In order to estimate the repeatability,<br />
each synthesis route was repeated three times. HPLC analyses were carried out on LaChrom D·7000<br />
System (Merck-Hitachi) liquid chromatograph.<br />
The solid-phase extraction (SPE) was used as the sample preparation method. FIrst, 200 mg <strong>of</strong> ecstasy<br />
sample was dissolved in mixture <strong>of</strong> 1.5 ml <strong>of</strong> the ammonium buffer (pH 8.5) and 0.5 ml <strong>of</strong> 30 mg/l<br />
diphenylamine solution (internal standard). Than the suspension was vigorously shaken for 25 min at 2000<br />
rpm. The optimisation <strong>of</strong>SPE conditions was focused on selection <strong>of</strong> the appropriate column filling, which<br />
enables to bind the main compound and to thicken the impurities that are important in view <strong>of</strong> comparative<br />
analysis. Bakerbond spe Octadecyl (3 ml, 500 mg) turned out to be the most effective. SPE was<br />
performed as follows: 1.5 ml <strong>of</strong> sample was rinsed with 6.0 ml <strong>of</strong> water and 0.3 ml <strong>of</strong> methanol and the<br />
impurities were extracted with 0.8 ml <strong>of</strong> methanol. Than, 0.3 ml <strong>of</strong> collected fraction was diluted with the<br />
phosphoric acid solution up to pH <strong>of</strong> 6.<br />
Chromolith Performance RP-18 e (100 - 4.6 mm) monolithic column was used in HPLC analysis. Taking<br />
into account the variety <strong>of</strong> physicochemical properties <strong>of</strong> the impurities, the separation was done in<br />
gradient conditions. In order to optimise the resolution, the simplex method was applied. Four factors were<br />
taken into account which describe gradient conditions. After eight steps <strong>of</strong> optimisation the following<br />
conditions were selected: 0 min - 100% <strong>of</strong> phase A (water + 0.1 mIll phosphoric acid), 21.3 min - 59% <strong>of</strong><br />
phase A + 41 % <strong>of</strong> phase B (acetonitryle), 32.7 min 100% <strong>of</strong> phase B, 34 min 100% <strong>of</strong> phase A. The<br />
flow was 1.0 mUmin. Diode array detector (DAD) was used.<br />
The applied conditions <strong>of</strong> SPE extraction and HPLC analysis allow good separation <strong>of</strong> the characteristic<br />
impurities occurring in ecstasy samples. Because most <strong>of</strong> the impurities give similar UVIVIS spectra, it is<br />
impossible to identifY them using diode-array detector. It is highly probable that application <strong>of</strong> LCIMS<br />
system will solve this problem. The obtained HPLC chromatograms could be treated equivalently to FlO<br />
chromatograms where the impurities pattern is a subject to further chemometric analysis. The preliminary<br />
results show that the worked-out method allows to distinguish the samples prepared by different synthesis<br />
route as well as it could be useful in comparative analysis <strong>of</strong> seized drug samples.<br />
The study was supported by the grant <strong>of</strong> the State Committee for Scientific Research, Warsaw, Poland,<br />
number OT OOC 01024.<br />
Keywords: Comparative analysis, Ecstasy, HPLC<br />
Page 131
Al8<br />
EV ALUA nON OF A PORTABLE EVIDENTIAL BREA TH ALCOHOL ANALYZER<br />
Gerasimos Razatos*, Ruth Luthi, Sarah Kerrigan <br />
New Mexico Department <strong>of</strong> Health, Scientific Laboratory Division, Toxicology Bureau. PO Box 4700, <br />
Albuquerque, NM 87196-4700. <br />
The Scientific Laboratory Division <strong>of</strong> the Department <strong>of</strong> Health acts by mandate as the regulatory agency<br />
for the Implied Consent Program for the State <strong>of</strong>New Mexico. The Laboratory is responsible for all blood<br />
and breath alcohol testing activities for law enforcement statewide. The geographical size and the nature <strong>of</strong><br />
the state, characterized by a highly rural population, demands portable breath alcohol testing equipment.<br />
Moreover, future expansion and success <strong>of</strong> the breath testing program has focused on instrument portability<br />
and data management as critical issues amongst law enforcement agencies and the courts. Thus, the Implied<br />
Consent Section <strong>of</strong> the SLD evaluated the performance <strong>of</strong> the Intoxilyzer® 8000, a portable instrument,<br />
against the Intoxilyzer® 5000, a stationary instrument which is currently approved for use.<br />
Instrument performance was evaluated at various alcohol concentrations, ranging from 0.04 to 0.55 g/dL in<br />
blood or gl210L breath. Special attention was placed on instrument performance at the per se and<br />
aggravated DWI levels <strong>of</strong> 0.08 gldL and 0.16 gldL, respectively, due to their legal significance. Precision<br />
and accuracy were evaluated using in-house ethanol controls in a wet bath simulator. Coefficients <strong>of</strong><br />
variation using the Intoxilyzer® 8000 ranged from 0.30 - 1.3% (n=102), while CV ranges for the<br />
Intoxilyzer~ 5000 were 0.7 2.1 % (n=102). Calibration stability was assessed in addition to the<br />
distribution <strong>of</strong> data at concentrations between 0.04 and 0.55 g/210L. Accuracy was 100 102% for the<br />
Intoxilyzer® 5000 and 99-101 % using the Intoxilyzer® 8000. Linear regression analysis <strong>of</strong> more than 700<br />
comparative measurements revealed an R2 <strong>of</strong> 1.000 (y = I.005x 0.001), where the lntoxilyzer® 5000 and<br />
the Intoxilyzer® 8000 were plotted on the y and x-axis respectively. Instrument response to mouth alcohol<br />
and volatile interferences was also investigated. Potential interferences were evaluated alone or in<br />
combination with ethanol using a wet bath simulator at 34.0"C.<br />
The effects <strong>of</strong> extreme temperature and altitude were also examined using wet bath simulators and dry gas<br />
cali brant. Accuracy and precision were evaluated at high and low temperatures. High altitude performance<br />
was evaluated at 10,600 feet above sea level at a local ski resort. In addition to the scientific study, field<br />
evaluations were also conducted by law enforcement personnel. Based upon the results <strong>of</strong> the study, the<br />
Intoxilyzer® 8000 was approved as an evidential breath alcohol analyzer in the State <strong>of</strong> New Mexico.<br />
Keywords: Intoxilyzer 8000, Breath, Alcohol<br />
Page 132
A19 <br />
PERFORMANCE OF ASSAYS FOR THERAPEUTIC DRUG MONITORING AND URINE<br />
DRUGS-OF-ABUSE SCREENING ON A CONSOLIDATED WORKSTATION<br />
H. Luthet, I. Domke 2 , S. 10rdan·· J, M. Oellerich I, W. Stockmann 2<br />
IGeorg-August-Universitaet, Goettingen, Germany, 2Roche Diagnostics GmbH, Mannheim, Germany,<br />
JRoche Diagnotics Corp., Indianapolis, USA<br />
Introduction: The study objective was the assessment <strong>of</strong> performance <strong>of</strong> nine Therapeutic Drug Monitoring<br />
(TOM) assays and nine Drugs-<strong>of</strong>-Abuse assays (OAT) when processed in combination with simulated<br />
routine workload on Modular Analytics P (Roche Diagnostics).<br />
Methods: All TOM and OAT assays involve the kinetic interaction <strong>of</strong> microparticles in solution (KIMS)<br />
except one enzymatic method. The study design comprises imprecision in simulated routine runs. The<br />
experiment tests for potential systematic or random errors by comparing the imprecision <strong>of</strong> reference results<br />
(standard batch) with results from samples run in a pattern simulating routine sampling. The study was<br />
supported by a program for computer aided evaluation (CAEv).<br />
Results: Within-run CVs <strong>of</strong> the reference runs ranged from 2 to 5 % for the majority <strong>of</strong> TOM<br />
(Acetaminophen, Amikacin, Carbamazepine, Digitoxin, Gentamicin, Lidocaine, Phenobarbital, Phenytoin)<br />
and OAT assays (Barbiturates, Cannabinoids, Cocaine Metabolite, Methadone, Opiates, Phencyclidine,<br />
Propoxyphene). CVs up to 7 % were obtained for Digoxin, Amphetamines, and Benzodiazepines. Routine<br />
simulation resulted in slightly increased CVs <strong>of</strong> maximal 2 %. This is in agreement with experience from<br />
previous routine simulation studies.<br />
Conclusion: With these results we conclude that no relevant reagent interactions occur on Modular Anaiytics<br />
P when using it as a consolidated workstation for TOM, OAT, serum proteins and general chemistry assays.<br />
Keywords: Therapeutic Drug Monitoring, Drugs-<strong>of</strong>-Abuse-Screening, Consolidated Workstation<br />
Page 133
A20 <br />
VALIDA TION OF A HPLC METHOD FOR QUANTIT A TION OF MDMA IN TABLETS AND<br />
REPRESENTA TIVE DRUG SAMPLING<br />
LB. MUlier', B.B. Klinke; Department <strong>of</strong> <strong>Forensic</strong> Chemistry, Institute <strong>of</strong> <strong>Forensic</strong> Medicine, University <strong>of</strong><br />
Copenhagen, Frederik V's Vej 11, DK-2100 Copenhagen, Denmark<br />
A method for quantification <strong>of</strong> MDMA (ecstasy) in powder/tablets using HPLC-DAD will be described.<br />
The powder was extracted with HPLC solvent (KHzP0 4 -buffer, pH 3.2:Acetonitrile (9:1» in 5-10 minutes,<br />
and analyzed using HPLC-DAD. The column used was a Chromspher B5 column at 30 °C and 0,4 ml/min<br />
solvent flow. The identity was confirmed using UV-detection with a UV-curve fit <strong>of</strong>900 or more and peak<br />
purity <strong>of</strong> 990 or more. The specificity <strong>of</strong> the method has been examined for other phenyl amines, and<br />
showed that only PMMA co-elutes with MDMA. The robustness <strong>of</strong> the method was good, and minor<br />
changes in solvent composition and solvent flow was possible. The method uncertainty was found to be<br />
10%. The limit <strong>of</strong> detection was 0.001 mg/ml and the limit <strong>of</strong> quantification was 0.003 mg/mt.<br />
Representative sampling <strong>of</strong> the ecstasy tablets was applied prior to MDMA analysis. Visual inspection was<br />
done to establish if a seizure was heterogeneous or homogenous. Heterogeneous seizures were divided in<br />
populations <strong>of</strong> similar appearance and were treated separately in further analysis. The validated method <strong>of</strong><br />
MDMA analysis and sampling <strong>of</strong> tablets will be presented in the poster.<br />
Keywords: MDMA, HPLC-DAD, Sampling.<br />
Page 134
A21 <br />
ALCOHOL DETERMINATION BY HEAD SPACE DUAL COLUMN CAPILLARY GAS<br />
CHROMATOGRAPHY<br />
Jlpo Rasanen', Ilkka Ojanpera, Kaisa Kurkinen, Juhani Vartiovaara, Erkki Vuori<br />
Department <strong>of</strong> <strong>Forensic</strong> Medicine, PO Box 40, FIN-00014 University <strong>of</strong> Helsinki, FINLAND<br />
A head space dual column capillary gas chromatographic method was developed for the simultaneous<br />
determination <strong>of</strong> ethanol, methanol, acetone, isopropyl alcohol, ethyl methyl ketone and n-propanol in<br />
blood and urine. The method consisted <strong>of</strong> two identical instruments and conditions, but using different<br />
internal standards, I-propanol and 2-butanol.<br />
The gas chromatographs were 6890 Series GCs equipped with two flame ionisation detectors and<br />
ChemStation s<strong>of</strong>tware (Agilent Technologies, USA). The autosamplers were Combi Pal Head space<br />
samplers (CTC Analytics, Switzerland). The parallel capillary columns were a Rtx-BACI, 30m x 0.53mm,<br />
3 !lm film and a Rtx-BAC2, 30m x 0.53mm, 2 !lm film (Restek, USA). The columns were connected to<br />
single injector with a Graphpack Divider (Gerstel, Germany). The head space conditions were as follows:<br />
incubation temperature 60 °C, incubation time 5 min (agitation speed 500 rpm), syringe temperature 65 °C,<br />
injection volume 500 !ll. The GC conditions were as follows: split ratio I :20, column flow rate 10.7 mllmin<br />
(He), injection port temperature 200 °C, oven temperature 45°C (4 min), detector temperature 250°C, H2<br />
flow 40 ml/min, air flow 450 mllmin, make-up flow (N2) 45 mllmin. The total analysis time was 5 min 50<br />
s.<br />
A baseline separation was obtained for all six compounds on both columns. Thirty-eight compounds were<br />
tested for interference. Methyl acetate co-eluted with I-propanol on Rtx-BACI and with acetone on Rtx<br />
BAC2. No other compound was found to co-elute with an analyte on both columns. However, ten<br />
compounds co-eluted with an analyte on one column. The reporting limit was set to 0.2 mg/g for ethanol<br />
and 0.1 mglg for the other analytes. The method was accredited for the determination <strong>of</strong> ethanol in blood<br />
and urine according to the standard SFS-EN ISO/IEC 17025. The uncertainty <strong>of</strong> measurement was 4 % for<br />
both blood and urine samples.<br />
The present method takes advantage <strong>of</strong> the facility <strong>of</strong> the head space sampling by gas-tight syringe over<br />
loop or pneumatic systems. Two dual-column instruments with different internal standards comprise a<br />
reliable but still compact set up for forensic alcohol determination.<br />
Key words: Head space GC, Blood alcohol, Capillary column<br />
Page 135
A22<br />
METAL AND METALLOID MULTIELEMENTARY ICP-MS VALIDATION IN WHOLE<br />
BLOOD, PLASMA, URINE, AND HAIR. REFERENCE VALUES<br />
J.P. Goulle", L. Mahieu, J. Castermant, N. Neveu, L. Bonneau, G. Laine, D. Bouige, C. Lacroix<br />
Groupe Hospitalier du Havre, B.P. 24, F-76083 Le Havre, France<br />
Four multi-elementary metal and metalloid quantification methods using inductively coupled plasma mass<br />
spectrometry (ICP-MS) have been developed and validated in human whole blood, plasma, urine and hair<br />
using a single preparation procedure for each sample.<br />
The ICP-MS measurements were performed using a Thermo Elemental X7CCT series and PlasmaLab<br />
s<strong>of</strong>tware without a dynamic reaction cell. Twenty-four to thirty-two elements are simultaneously quantified<br />
in biological matrices: Li, Be, B, AI, Y, Cr, Mn, Co, Ni, Cu, Zn, Ga, Ge, As, Se, Rb, Sr, Mo, Pd, Ag, Cd,<br />
Sn, Sb, Te, Ba, W, Pt, Hg, TI, Pb, Bi, U. 0.4 ml whole blood, plasma and urine sample are acid diluted with<br />
purified water prepared extemporaneously, triton X100 and butanol. In and Rh are used as the internal<br />
standards. For the urine samples, the results were corrected after enzymatic creatinine determination. 25 mg<br />
hairs are acid mineralized after a decontamination procedure and diluted as previously described for the<br />
biological fluids. To be validated, each element has to force: linearity with a correlation coefficient higher<br />
than 0.99. The intra-assay and inter-assay imprecision measured as the CY should be below 5% and 10%<br />
respectively. Global performance was assessed by quality control program. Our laboratory is a registered<br />
participant <strong>of</strong> the Institut National de Sante Publique du Quebec (Sainte-Foy, Canada) inter-laboratory<br />
comparison program for whole blood, urine, and beard hair <strong>of</strong> non-occupationally exposed individuals<br />
spiked with selected elements.<br />
Multi-element metal and metalloid analysis has been validated for 24 elements in the whole blood, 27<br />
elements in the plasma, 29 elements in the urine and 32 elements in the hair, from 0 to 25, 250 or 1000<br />
ng/ml owing to the element. Quantification limits range from 0.002 ng/ml (U) to 4.4 ng/ml (B) for the<br />
whole blood, from 0.002 nglml (U) to 7.7 ng/ml (AI) for the plasma, from 0.001 nglml (U) to 2.2 ng/ml<br />
(Se) for the urine, and from 0.2 pglmg (Tl) to 0.5 nglmg (B) for the hair. Normal values have been<br />
determined in the whole blood, the plasma, the urine (n=100), and the hair (n=45) based on healthy<br />
volunteers, leading to approximately 10,000 analyses. AI results are presented and discussed. Some clinical<br />
toxicology and forensic toxicology applications are reported.<br />
ICP-MS has made significant advances in the field <strong>of</strong> clinical biology, particularly important in<br />
toxicological analysis. This is due the use <strong>of</strong> extremely effective equipment that permits better clinical and<br />
forensic toxicological analysis <strong>of</strong> metals and metalloids status <strong>of</strong> each individual.<br />
Keyswords: Inductively coupled plasma, Mass detector, Metalloids<br />
Page 136
A23 <br />
THE EXTRACTION AND ANALYSIS OF FLUNITRAZEPAM FROM WHOLKBLOODIURINE<br />
USING A NOVEL SOLID PHASE EXTRACTION PROCEDURE AND HIGH PERFORMANCE<br />
LIQUID CHROMATOGRAPHY-PHOTODIODE ARRA Y DETECTION<br />
Jeffery Hackett*, <strong>Forensic</strong> Toxicology Laboratory, Center for <strong>Forensic</strong> Sciences, Syracuse NY <br />
Jeanna M. Marraffa" Fellow in Clinical Toxicology, Poison Control Center, Syracuse NY <br />
Flunitrazepam, has been well recognized as a drug <strong>of</strong> concern within the forensic toxicology community <br />
for many years. Several methods have been published for the analysis and detection <strong>of</strong> the drug <br />
previously.I-3 The method described in this poster takes a novel yet simplified approach to the extraction! <br />
detection <strong>of</strong> flunitrazepam in bi<strong>of</strong>luids. Solid phase extraction followed by high performance liquid <br />
chromatography is employed without the need for a mass spectrometry unit for detection <strong>of</strong> low levels <strong>of</strong> <br />
the drug. Data is presented to exhibit the efficiency <strong>of</strong> the method in terms <strong>of</strong> limit <strong>of</strong> detection and <br />
quantitation_ <br />
Blood and urine were spiked with both the drug (flunitrazepam) and an internal standard (Prazepam) over a <br />
range <strong>of</strong> concentrations (O-IOng mL- 1 ). The samples were buffered with a small volume <strong>of</strong>O.IM acetic acid <br />
and applied to commercially available mixed mode (Cs/SCX) columns that had been previously <br />
conditioned. The columns were washed, dried and eluted twice, once using ethyl acetate (3 mL) and again <br />
using an elution solvent containing ethyl acetate/ acetonitrile! ammonia (3 mL). Both portions <strong>of</strong>the eluates <br />
were collected and combined. Evaporation was performed at room temperature. The residue was dissolved <br />
in 100 JlI <strong>of</strong>0.1 % aqueous trifluoroacetic acid. <br />
LC Conditions: <br />
Column:<br />
Mobile phase:<br />
Flow Rate:<br />
Column Temperature:<br />
Detection:<br />
Injection Volume:<br />
CIS, ISO x 2.lmm, 3.SJlm <br />
0.1 % Trifluoroacetic acidl Acetonitrile (67: 33) <br />
0.3 mL min-I <br />
. 40°C <br />
220, 2S0 nm <br />
SOJlL <br />
References: <br />
1. LeBeau M.A., Montgomery M_A., Wagner J.R., and Miller M.L., J <strong>Forensic</strong> Sci. 2000 <br />
Sep;4S(S): 1133-41. <br />
2. Ahrens B., Schwandt H.J., and Schutz H., Ar:neimitteiforschung. 2000 Dec;SO(12):10S7-62.<br />
3. Elian A.A., <strong>Forensic</strong> Sci Int. 1999 Apr 26;101(2):107-11.<br />
Keywords: Flunitrazepam, Solid-phase extraction, Blood and urine<br />
Page 137
A24 <br />
OHIO DEPARTMENT OF HEALTH EV ALVA TION OF THE INTOXILYZER 8000<br />
John J. Kucmanic*, Dean M. Ward, James E. Dykes, Ohio Department <strong>of</strong> Healthl Bureau <strong>of</strong> Alcohol and<br />
Drug Testing. 35 E. Chestnut Avenue, Columbus, Ohio 43215, USA<br />
Recently, a new Breath Alcohol testing instrument was evaluated by the Ohio Department <strong>of</strong> Health. The<br />
Intoxilyzer 8000 is a smaller shielded plastic body breath alcohol analyzer that utilizes a pulsed infra-red<br />
energy source.as well as makes use <strong>of</strong> a primary filter in the nine micron range to quantifY alcohol. The<br />
instrument is engineered with the latest generation <strong>of</strong> power converters. This technology significantly<br />
reduces the weight <strong>of</strong> the instrument so that it can easily be carried using the attached handle. Furthermore,<br />
the instrument can operate in a limited fashion with an optional battery pack or continuously with a 12<br />
VDC source such as a cigarette lighter plug. No electrical inverter is necessary to operate the device in<br />
mobile situations.<br />
We examined several properties <strong>of</strong>this unit. Specifically, we looked at the in-vitro performance <strong>of</strong>two like<br />
instruments. Nine solutions were prepared in eight liter carboys to contain a range <strong>of</strong> concentration <strong>of</strong><br />
ethanol and or acetone while purified water was used to evaluate a negative sample. The prepared solutions<br />
were analyzed by the Bureau on a Hewlett Packard 6890/7693 gas chromatograph using a dual capillary<br />
column headspace method. Standards were prepared from SRM 1828a and reagent grade acetone. All<br />
simulators used throughout the study were certified by the manufacturer prior to the evaluation.<br />
Furthermore, simulators were dried and replenished with a new bottle <strong>of</strong> solution after every twenty tests.<br />
As a consequence <strong>of</strong> rapid acetone depletion, acetone solutions were replaced after every ten tests. Transfer<br />
hoses which were connected to the calibration inlet during the evaluation were purged with dry air after<br />
every five tests. This procedure minimized the build up <strong>of</strong> excess condensate that would accumulate over<br />
the course <strong>of</strong>testing.<br />
Mean concentrations <strong>of</strong> ethanol reported and the % coefficient <strong>of</strong> variance did not deviate by more than 5%<br />
in both instruments. A regression analysis between the mean alcohol concentration <strong>of</strong> twenty tests and the<br />
target concentration indicated a correlation <strong>of</strong> greater than 0.999 for both instruments over the respective<br />
concentrations. Prepared solutions containing acetone at a clinically significant concentration with or<br />
without ethanol were detected as an interferent for both instruments. Our results correlated well with the<br />
NHTSA evaluation <strong>of</strong>the Intoxilyzer 8000 which examined ten replicates <strong>of</strong>tive ethanol concentrations <strong>of</strong><br />
0.020,0.040,0.080,0.160, and O.300g/21OL.<br />
In conclusion, the results from the in-vitro test performed on the Intoxilyzer 8000 instrument demonstrate<br />
that it is accurate, precise, and linear at the concentrations <strong>of</strong> ethanol tested. Furthermore, the results<br />
demonstrate that the unit is able to detect the presence <strong>of</strong> acetone vapors or a combination <strong>of</strong> acetone and<br />
ethanol vapors at the respective concentration for each volatile.<br />
Keywords: Intoxilyzer, Alcohol, Breath<br />
Page 138
A25<br />
A RAPID METHOD FOR MEASURING ANTI-DEPRESSANTS IN POSTMORTEM BLOOD<br />
USING DUAL COLUMN LIQUID CHROMATOGRAPHY MASS SPECTROMETRY<br />
Jason H. Sklerov' <br />
Office <strong>of</strong> the Armed Forces Medical Examiner, Division <strong>of</strong> <strong>Forensic</strong> Toxicology, Armed Forces Institute <strong>of</strong> <br />
Pathology, Rockville, MD, U.S.A. <br />
A dual column, liquid chromatography mass spectrometry method was developed for the analysis <strong>of</strong> eleven<br />
anti-depressants and metabolites in 200uL <strong>of</strong> postmortem blood. Sample preparation consisted <strong>of</strong> internal<br />
standard addition, protein precipitation, and micr<strong>of</strong>iltration. Filtrates were injected onto an extraction<br />
column (Oasis® HLB, 20 x 2.1mm, dp=25um) and washed with deionized water, 20% acetonitrile, at<br />
3mLlmin. The trapped analytes were backflushed through a 10-port switching valve onto an analytical<br />
column (Zorbax® SB-CI8, 30 x 2.1mm, dp=3.5um) using a gradient <strong>of</strong> acetonitrile (20-80%) and 0.1%<br />
formic acid at a flow rate <strong>of</strong> O.5mLlmin. The positive, pseudomolecular ions <strong>of</strong> imipramine, desipramine,<br />
amitriptyline, nortriptyline, fluoxetine, paroxetine, fluvoxamine, trimipramine, N-desmethyl-trimipramine,<br />
clomipramine, and N-desmethyl-clomipramine were monitored following electrospray ionization. Overall<br />
instrumental analysis time was 11 minutes per sample including extraction and detection. Sample<br />
carryover, assessed by area% <strong>of</strong> signals in blank injections, was < 1.4% by the use <strong>of</strong> both a needle wash<br />
phase and injector programming. Linear ranges varied within a 0.025-lmg/L range and the online<br />
extraction recovery was between 75-105%. Additional time savings could be gained by the direct injection<br />
<strong>of</strong> diluted plasma, however, due to the inconsistencies in sample collection and the potential for signal<br />
suppression, a protein precipitation step was adopted for this work.<br />
Keywords: Anti-depressants, Dual-column, LC/MS<br />
r--<br />
Page 139
A26 <br />
1-(4-METHOXYPHENYL)-1-PROPANAMINE AS CONTAMINANT IN 1-(4-METHOXY<br />
PHENYL)-2-PROPANAMINE (PMA) PREPARED VIA THE LEUCKART REDUCTIVE<br />
AMINA TION METHOD<br />
D Waumans', B Hermans, N Bruneel, J Tytgat<br />
Laboratory <strong>of</strong> Toxicology, K.U. Leuven, Eduard van Evenstraat 4, B-3000 Leuven, Belgium<br />
Introduction: 1-(4-Methoxyphenyl)-2-propanamine (4-methoxyamphetamine, PMA) is an amphetamine<br />
analogue (co-)responsible for a series <strong>of</strong> lethal drug accidents the last few years. It is <strong>of</strong>ten traded as<br />
MDMA (N-methyl-I-(3,4-methylenedioxyphenyl)-2-propanamine) and facilely prepared from anethole, the<br />
main component <strong>of</strong> (star) anise oil. From a forensic point <strong>of</strong> view, the pr<strong>of</strong>iling <strong>of</strong> synthesis impurities that<br />
can be attributed to a specific synthetic pathway is very important. The following presents 1-(4<br />
methoxyphenyl)-I-propanamine as a new PMA impurity. It is formed via the Leuckart reductive amination<br />
<strong>of</strong> 1-(4-methoxyphenyl)-I-propanone, an impurity arising from the peracid oxidation <strong>of</strong> anethole.<br />
Methods: Synthesis: The performic oxidation reaction <strong>of</strong> anethole, the pinacol-pinacolone rearrangement<br />
and Leuckart reductive ami nation were performed using standard reaction conditions. 1-(4<br />
methoxyphenyl)-I-propanone was prepared quantitatively via a solventless Friedel-Crafts acylation<br />
reaction <strong>of</strong> anisole with lithium perchlorate as catalyst. GCIMS analysis: Agilent 6890 Plus GC coupled to<br />
Agilent 5973N mass selective detector (EI, 36 - 400 amu, 70 eV). Column: Varian VF5-MS FactorFour<br />
capillary (30 m x 0.250 mm x 0.25 flm). Injection and oven programming: I flL injection (split I: 10); 50°C<br />
(hold I min), 5°C/min to 270°C (hold 15 min). Carrier gas: He (I mLlmin).<br />
Results: The peracid oxidation <strong>of</strong> anethole yields anethole glycol (and esters), which is converted to 1-(4<br />
methoxyphenyl)-2-propanone by refluxing in a methanol/sulfuric acid mixture. Also, we have<br />
demonstrated that 1-( 4-methoxypheny l)-I-propanone is formed as a contaminant during the peracid<br />
oxidation <strong>of</strong> anethole. Both substances can serve as substrate in the Leuckart reductive amination reaction,<br />
where 1-( 4-methoxyphenyl)-I-propanone will yield 1-(4-methoxyphenyl)-I-propanamine and 1-(4<br />
methoxyphenyl)-2-propanone will yield 1-(4-methoxyphenyl)-2-propanamine. When exammmg<br />
confiscated PMA preparations, 1-( 4-methoxyphenyl)-I-propanamine is found to be present next to PMA,<br />
hereby giving an indication for anethole's application as precursor.<br />
Conclusion: 1-(4-Methoxyphenyl)-I-propanamine is a new impurity formed during the Leuckart reductive<br />
amination reaction <strong>of</strong> 1-(4-methoxyphenyl)-I-propanone, a contaminant produced in the peracid oxidation<br />
reaction <strong>of</strong> anethole. Its formation is demonstrated by a simulated synthesis, and its applicability is proven<br />
by its presence in confiscated clandestine PMA samples. There are only few data available on the<br />
pharmacology and toxicity <strong>of</strong> this newly discovered impurity.<br />
Keywords: Pr<strong>of</strong>iling, PMA, 1-( 4-Methoxyphenyl)-I-propanamine<br />
Page 140
A27 <br />
EFFECT OF SODIUM CHLORIDE ON HEADSPACE BLOOD ALCOHOL ANALYSIS BY<br />
GC-FID<br />
Janice Yazzie*, Ruth Luthi, Sarah Kerrigan <br />
New Mexico Department <strong>of</strong>Health, Scientific Laboratory Division, Toxicology Bureau, PO Box 4700, <br />
Albuquerque, NM 87196-4700. <br />
Sodium chloride is frequently utilized as an additive for headspace alcohol analysis. The addition <strong>of</strong> salt to<br />
the mixture in the headspace vial increases the partial pressure <strong>of</strong> volatile compounds including alcohol and<br />
the internal standard. This is advantageous because the concentration <strong>of</strong> alcohol in the vapor phase is a<br />
function <strong>of</strong> both the temperature and the concentration <strong>of</strong>alcohol in the liquid phase.<br />
The effect <strong>of</strong> salt was investigated in a series <strong>of</strong> experiments in which sodium chloride was added to the<br />
internal standard solution containing n-propanol and t-butanol. Ethanol was quantitatively determined using<br />
an Agilent HP 6890 GC equipped with dual capillary columns and a flame ionization detector (FlO).<br />
In-house and external whole blood controls were used for comparison purposes. When no salt was added,<br />
CVs ranged from 1.3 to 4.0% for alcohol concentrations between 0.04 and 0.30 g/dL. By comparison, CVs<br />
using the salt solution ranged from 1.2 to 4.2%. Accuracy was 100-105% and 99-109%, when either salt or<br />
no salt was added, respectively. A comparison <strong>of</strong>quantitative values obtained by both methods showed that<br />
the results were not statistically different. A total <strong>of</strong> 80 antemortem and postmortem casework samples<br />
were included in the study. These ranged in concentration from 0 to 0.567 gldL ethanol. Linear regression<br />
analysis showed an R2 value <strong>of</strong>0.996 and a mean difference <strong>of</strong> 0.001 g/dL between methods.<br />
Keywords: Ethanol, Sodium chloride, GC-FID<br />
Page 141
A28 <br />
HIGH THROUGHPUT SCREENING OF DRUGS OF ABUSE BY LCIMS<br />
Jerry Zweigenbaum*; Agilent Technologies, Wilmington, DE, USA<br />
Kolbjorn Zahlsen, Trond Aamo; Department <strong>of</strong> Clinical Pharmacology, St. Olav Hospital, University<br />
Hospital <strong>of</strong>Trondheim, Trondheim, Norway<br />
Drugs <strong>of</strong> abuse are screened in blood and urine throughout the world by immunoassay. This technology<br />
has the advantages <strong>of</strong> high-throughput, inexpensive and generally applicable as a screening tool. However,<br />
there is a reasonable possibility for both false positive and false negative results. In addition, to be reliable<br />
the methodology must typically utilize a high concentration cut<strong>of</strong>f. In contrast, screening by a highly<br />
selective methodology as liquid chromatography/mass spectrometry (LCIMS) is less susceptible to false<br />
negatives and positives. Because <strong>of</strong> its sensitivity it has a much lower cut<strong>of</strong>f than immunoassay.<br />
One argument for immunoassay lies in its ability to detect classes <strong>of</strong>compounds and therefore would detect<br />
designer drugs not listed as a sought compound. LC/MS screening for specific drugs <strong>of</strong> abuse would miss<br />
this. However, all immunoassay positives must be confirmed, as there is no indication <strong>of</strong> what the<br />
substance is. This step would, like LCIMS, miss the non-listed substance.<br />
I f an immunoassay were to produce a positive screen for amphetamines, there would be no indication <strong>of</strong><br />
what the compound(s) was. However, LCIMS would provide the specific amphetamine and its<br />
concentration. A clinician reviewing these data in the screen can make assessment about dose and the<br />
possibility <strong>of</strong> confounding substances that may also be present. It is this additional data that makes the<br />
LC/MS screen both reasonable and desirable from a quality <strong>of</strong> results standpoint.<br />
We will present how the Department <strong>of</strong> Clinical Pharmacology performs high-throughput drugs-<strong>of</strong>-abuse<br />
screening using LCIMS. The operation <strong>of</strong> the instrumentation and maintenance procedures will be<br />
described showing how large numbers <strong>of</strong> samples are analyzed side-by-side for both drugs-<strong>of</strong>-abuse and<br />
therapeutic drug monitoring. Additionally, the quality control processes needed to assure all results are<br />
accurate will be discussed. These processes encompass the sample handling, preparation, analysis, and<br />
reporting <strong>of</strong>almost one million determinations (equivalent immunoassays) per year run on 24 instruments<br />
operating seven days a week.<br />
Keywords: Screening, Drugs-<strong>of</strong>-abuse, LC/MS<br />
Page 142
A29 <br />
SIMULTANEOUS DETERMINATION OF COCAINE, COCAETHYLENE, AND THEIR<br />
POSSIBLE PENTAFLUOROPROPYLA TED METABOLITES AND PYROLYSIS PRODUCTS BY<br />
GAS CHROMATOGRAPGY IMASS SPECTROMETRY<br />
Patrick S. Cardona', Arvind K. Chaturvedi, John W. Soper, and Dennis V. Canfield. Bioaeronautical<br />
Sciences Research Laboratory (AAM-610), Aerospace Medical Research Division, Civil Aerospace<br />
Medical Institute, Federal Aviation Administration, U. S. Department <strong>of</strong> Transportation, P. O. Box 25082,<br />
Oklahoma City, OK 73125-5066, USA<br />
Cocaine (COC) is abused by smoking, nasal insufflation, and intravenous injection, and it is also taken with<br />
ethanol. Therefore, it is important to determine concentrations <strong>of</strong>COC and its metabolites, ethanol analogs,<br />
and pyrolysis products for establishing the degree <strong>of</strong> toxicity, the possible ingestion <strong>of</strong> ethanol, and the<br />
possible route <strong>of</strong> administration. In this study, a sensitive and selective procedure is developed for the<br />
simultaneous analyses <strong>of</strong> COC, benzoylecgonine, norbenzoylecgonine, norcocaine, ecgonine, ecgonine<br />
methyl ester, m-hydroxybenzoylecgonine, anhydroecgonine methyl ester (AEME), anhydroecgonine<br />
(AECG), cocaethylene, norcocaethylene, and ecgonine ethyl ester in blood, urine, and muscle homogenate.<br />
In the analysis, available deuterated analogs <strong>of</strong> these analytes were used as internal standards. Proteins from<br />
blood and muscle homogenate were precipitated with cold acetonitrile. After the removal <strong>of</strong> acetonitrile by<br />
evaporation, the supernatants and urine were extracted by solid-phase chromatography. The eluted analytes<br />
were converted to hydrochloride salts and derivatized with pentafluoropropionic anhydride and 2,2,3,3,3<br />
pentafluoro-l-propanol. The derivatized products were analyzed on a gas chromatograph (GC)/mass<br />
spectrometer by selected ion monitoring.<br />
This method was successfully applied in analyzing 13 case specimens from aviation accident pilot fatalities<br />
and/or motor vehicle operators. AEME concentrations found in the 13 specimens were consistent with<br />
those produced solely by the GC inlet pyrolysis <strong>of</strong> COC controls, suggesting that COC was not abused in<br />
these cases by smoking. Although AEME remains a potential marker for establishing the abuse <strong>of</strong> COC by<br />
smoking, AECG was not a useful marker because <strong>of</strong> its low recovery and GC inlet production from COC<br />
metabolites.<br />
The developed procedure is unique because multiple analytes can be analyzed in urine, blood, and solid<br />
tissues by a single extraction with increased sensitivity through formation <strong>of</strong> hydrochloride salts and using<br />
a one-step derivatization.<br />
Keywords: Cocaine, Metabolites, Pyrolysis Products, Gas ChromatographylMass Spectrometry<br />
Page 143
A30 <br />
RAPID ANALYSIS OF THe AND METABOLITES IN WHOLE BLOOD<br />
William E. Brewer', \ Dwight Flammia 2 , Randall Edwards 2 , and Terri Wood 2 , IClemson Veterinary<br />
Diagnostic Center, P.O. Box 102406, Columbia, SC 29224, 2Common Wealth <strong>of</strong>Virginia, Dept. <strong>of</strong><br />
Criminal Justice Service, 700 N. Fifth St., Richmond, VA 23219<br />
Extraction <strong>of</strong> whole blood samples for tetrahydrocannabinol (THC) and metabolites may be timeconsuming,<br />
especially with liquid-liquid extraction methods. Recently, a novel solid-phase extraction (spe)<br />
method has been developed for extracting THC and metabolites from whole blood. This spe method uses a<br />
pipette tip that houses the solid-phase sorbent; the extraction method is referred to as disposable pipette<br />
extraction (DPX). For this application, a 5 mL DPX tip is utilized to provide the lower detection limits<br />
required for the analysis. For the DPX extraction, 1 mL blood was spiked with 10 ng <strong>of</strong> internal standard<br />
(drTHC and d)-COOH-THC). The blood was vortexed with 2 mL acetonitrile then centrifuged. The<br />
supernatant was transferred to a clean tube and 4 mL DI water was added. Approximately 3.5 mL <strong>of</strong> the<br />
solution and 5 mL <strong>of</strong> air (for mixing) were drawn into the DPX tip with a syringe attachment. After waiting<br />
45 seconds, the solution was dispensed to waste. The rest <strong>of</strong> the sample solution and 5 mL <strong>of</strong> air were<br />
drawn into the DPX tip, and after 45 seconds it was dispensed to waste. Subsequently, 300 uL hexane-ethyl<br />
acetate (50/50) and 5 mL <strong>of</strong> air was drawn into the DPX tip, and this solution was dispensed into a GC vial.<br />
Another elution with 300 uL <strong>of</strong> hexane-ethyl acetate was used and added to the GC vial. The solution was<br />
dried under nitrogen and heat (90°C). For the derivatization, 25 uL ethyl acetate was added to the dried vial,<br />
25 uL BSTF A was added, and the solution was capped under nitrogen and vortex mixed. The solution was<br />
derivatized at 90°C for 20 min. The GC vial was decapped and the solution was transferred to a GC vial<br />
insert. The insert was returned to the same GC vial, capped, and placed on the GC autosampler for sample<br />
injection (2 uL split/ess). The parameters for this analysis are crucial because <strong>of</strong> potential interfering peaks<br />
from sample matrix components. The GC/MS instrument (HP 6890 with HP 5973 MSD) was equipped<br />
with a 30 m GC column (RTX-5 ms, 0.25 mm ID, 0.2 urn film). The oven temperature program started at<br />
80°C for 1 min, then ramped at 40°C/min to 200 C, then ramped at 20°C/min to 240°C with the temperature<br />
held at 240°C for 5 min, then it was ramped at 20°C/min to 300°C and the temperature held for 8 min. The<br />
flow rate was set constant at 2 mLlmin. It was found that this higher flow caused separation <strong>of</strong> the 371 ion<br />
<strong>of</strong>THC from a prominent interfering ion. For the MS conditions, selected ion monitoring was used and the<br />
ions mlz 371,374,386,389,303, and 306 were scanned at 50 ms for THC and (int. std.), and mlz == 371,<br />
374,473,476,488, and 491 for COOH-THC (and int. std.). Using the above parameters, THC and COOH<br />
THC at levels <strong>of</strong> 1 ng/mL were detected using 3 ions. A semi-automated extraction device is demonstrated<br />
to perform 12 extractions simultaneously in just minutes (not including protein precipitation and<br />
derivatization). Results <strong>of</strong> extractions from actual case samples are presented, and direct comparisons with<br />
standard liquid-liquid procedures are presented. It is found that DPX <strong>of</strong>fers a much-improved method for<br />
the analysis <strong>of</strong> THC and metabolites from whole blood in terms <strong>of</strong> sensitivity, selectivity and speed <strong>of</strong><br />
analysis.<br />
Keywords: THC, GCJMS, Extraction<br />
Page 144
A31 <br />
ANALYSIS OF TETRAHYDROCANNABINOL (THC) AND CARBOXY·<br />
TETRAHYDROCANNABINOL (CTHC) IN WHOLE BLOOD<br />
Amy Kinkennon*, Tim Robert, David Black, Peter Stout<br />
Aegis Sciences Corporation, Nashville, TN, USA<br />
THC and CTHC were isolated from I mL <strong>of</strong> whole blood using SPEWare Cerex PolyChrom THC SPE<br />
cartridges (35 mg beds). Analytes were eluted, and then derivatized with PFPA. Samples were<br />
reconstituted in 50 ul <strong>of</strong> ethyl acetate, and 2 uL injected on an HP 5890 GC interfaced to a Finnigan TSQ<br />
7000 MSIMS.<br />
The MSIMS was used in the positive CI mode for THC, and negative CI mode for the CTHC, with methane<br />
as the reagent gas. The THC molecular ion at 461 mlz was selected in Ql, collided with Ar in Q2, and two<br />
daughter ions monitored in Q3. The CTHC did not generate a strong molecular ion (622 m/z), so a 602 m/z<br />
fragment was selected in Q L This fragment was collided with Ar in Q2, and two daughter ions monitored<br />
in Q3. D3·THC and D3-CTHC were used as internal standards, and appropriate ions were monitored for<br />
these compounds. Analysis time was -15 min per sample.<br />
The method was shown to have a linear range <strong>of</strong> I-50 nglml for THC and 5-50 ng/ml for CTHC. Precision<br />
and accuracy studies were conducted using known control materials manufactured in drug free blood with<br />
good accuracy and precision over the linear range. Interference studies indicated that neither ibupr<strong>of</strong>en<br />
(110 uglml), acetaminophen (110 ug/ml), salicylate (700 uglml), nor ethanol (63 uglml) affected the<br />
analysis. Forty authentic blood samples from previous casework were analyzed using this method. Twenty<br />
had screened positive, and had been confirmed by an outside laboratory. Nine had screened positive, were<br />
sent for confirmation, and were returned negative. Eleven had screened negative and had not been<br />
previously confirmed.<br />
Keywords: Blood analysis, Carboxy-THC, Tandem mass spectrometry<br />
Page 145
A32 <br />
OXYCODONE ABUSE CONCERN IN METHADONE MAINTENANCE PATIENTS<br />
Gerard Meenan', Karl Verebey, and Mohan Patel. Ammon Analytical Laboratory, Linden, NJ.<br />
Detection <strong>of</strong> oxycodone abuse is a significant problem for drug treatment facilities. A common<br />
misconception concerns the idea that oxycodone is a synthetic opiate and staff members believe that the<br />
urine screen for opiates detects oxycodone, also. For example, the amount <strong>of</strong> oxycodone that yields a<br />
positive opiates screen on the DRI Opiates Assay is greater than 16,000 ng/mL. The usual level in patients<br />
taking oxycodone is from 300 to 1,000 nglmL.<br />
Microgenics Corporation has developed a specific urine oxycodone homogeneous enzyme immunoassay.<br />
Evaluation <strong>of</strong> this DRI Oxycodone Assay was added to screening <strong>of</strong> methadone "intake" patients followed<br />
by GCIMS confirmation <strong>of</strong> tests positive for oxycodone. Microgenics has proposed either a 100 or 300<br />
nglmL cut<strong>of</strong>f level. The cut<strong>of</strong>f concentration used for this study was 100 nglmL. The oxycodone<br />
immunoassay was tested on a Hitachi 717 Analyzer. 224 drug treatment "intake" patients' urine samples<br />
were screened with the specific oxycodone immunoassay. Using a 100 nglmL cut<strong>of</strong>f level 45 urine<br />
samples screened positive for oxycodone yielding a positive rate <strong>of</strong> 20. I %. All presumptive positive<br />
samples were extracted through Biochemical Diagnostics GV~65 Detectabuse columns; derivatized by<br />
BSTFA with 1% TMCS; and analyzed by selective ion monitoring (SIM) on an Agilent Technologies<br />
5973 GCIMSD system. The GC/MS confirmation cut<strong>of</strong>f was 25 nglmL. 45 <strong>of</strong> the 45 samples confirmed<br />
positive for oxycodone demonstrating a 100% confirmation rate. The amount <strong>of</strong> oxycodone recovered in<br />
the urine samples by GCIMS ranged from 25 nglmL to 37,116 ng/mL.<br />
The DRI Oxycodone Assay identified 20.1 % <strong>of</strong> the subjects as positive for the synthetic opiate. The<br />
specificity <strong>of</strong> the assay was 100% as determined by GCIMS analysis. Thus, in this population 20.1 % <strong>of</strong><br />
the Methadone Maintenance "intake" patients were using oxycodone. With the FDA approval <strong>of</strong> a<br />
generic sustained release oxycodone, abuse is likely to increase. The DRI Oxycodone ErA will be very<br />
useful in differentiating oxycodone from other opiate abuse.<br />
Keywords: Oxycodone, Enzyme Immunoassay, GC/MS<br />
Page 146
A33 <br />
EVALUATION OF BUPRENORPHINE CEDIA ASSAY USING SAMPLES FROM PATIENTS IN<br />
SUBSTITUTION TREATMENT<br />
Michael Bottcher and Ol<strong>of</strong> Beck*. Arztpraxis f. Medizinische Mikrobiologie, Labordiagnostik & Hygiene,<br />
Dessau, Germany. Department <strong>of</strong> Medicine, Division <strong>of</strong> Clinical Pharmacology, Karolinska University<br />
Hospital, Stockholm, Sweden.<br />
Buprenorphine is used as an analgesic drug, and for detoxification and substitution therapy <strong>of</strong> opioid<br />
dependence. However, in combination with the increased medical use, buprenorphine also occurs on the<br />
black market as an illicit drug and fatalities due to poly-drug use has been reported. In addition, pausing<br />
from buprenorphine intake during opiate relapsing has been observed and can make compliance monitoring<br />
necessary. As a consequence there is a need for analytical service and toxicological monitoring <strong>of</strong> patients.<br />
However, there has been a lack <strong>of</strong> an immunoassay suitable for automated high-volume screening. The aim<br />
<strong>of</strong> this study was to evaluate the prototype buprenorphine CEDIA (Microgenics Inc.) by comparing it with<br />
existing ELISA (Diagnostix Ltd) and GC-MS methods. Urine samples were collected from patients in<br />
heroin substitution treatment with methadone, buprenorphine or dihydrocodeine. In total, 1552 samples<br />
were obtained from approximately 600 patients, consisting <strong>of</strong> 70% males and having an age range <strong>of</strong> IS-54<br />
y. The CEDIA test was performed on Hitachi 911 and 912 (Roche Diagnostics, IN) instruments with a<br />
semiquantitative test protocol (five calibrators in the range 0-7S IlglL, sample volume 10 ilL) supplied by<br />
Microgenics Inc. Samples with response >75 Ilg/L were diluted 10- or 100-fold with saline ..<br />
At the levels exceeding the 5 Ilg/L cut<strong>of</strong>f level, a variability lower than 10% was observed both within- and<br />
between-ctays. The correlation <strong>of</strong> CEDIA and ELISA was studied in 221 samples. There was a 96.S %<br />
agreement in qualitative results between the methods. In three samples (2.7 % <strong>of</strong> all positives) CEDIA<br />
produced a false positive response as the GC-MS confirmation was clearly negative. In one sample the<br />
CEDIA result was false negative as the sample contained 26 Ilg/L <strong>of</strong> buprenorphine according to GC-MS.<br />
The agreement between the CEDIA and GC-MS methods in quantifying buprenorphine was studied in the<br />
range from 0 to 6000 Ilg/L. The samples were obtained from 72 patients receiving buprenorphine doses<br />
between 0.5 - 25 mg/day. The slope was 1.09 with an intercept <strong>of</strong> -12 on the CEDlA axis. The median ratio<br />
between CEDIA and GC-MS was 0.96 (n=29S). By pooling data for all samples with a buprenorphine<br />
concentration >5 Ilg/L according to GC-MS or ELISA (n=400), the sensitivity for CEDIA <strong>of</strong> detecting<br />
positive samples at the cut<strong>of</strong>f level <strong>of</strong> 5 Ilg/L was calculated to be 99.5%. A total <strong>of</strong> 1011 samples from<br />
patients who were not receiving prescribed buprenorphine but received other heroin substitution treatments<br />
(mainly methadone) were used to estimate specificity. Thirty samples (3.0 %) were found to be positive by<br />
CEDIA at the cut<strong>of</strong>f level <strong>of</strong> 5 Ilg/L. One <strong>of</strong> these had detectable buprenorphine by GC-MS but at a low<br />
level (0.6 Ilg/L). Fourteen <strong>of</strong> the 30 samples were from patients prescribed dihydrocodeine and contained<br />
high amounts <strong>of</strong> this substance and metabolites. A further 20 samples from patients prescribed<br />
dihydrocodeine in daily doses <strong>of</strong> 14 -SO mg were therefore studied and all were positive in the CEDlA<br />
assay with responses ranging from 5 - 34 IlglL. The 15 false positive samples out <strong>of</strong> the 1011 (1.5%) all<br />
had a low response «10) and all expect for one were highly positive in the CEDI A test for opiates,<br />
indicating that a cross-reactivity with codeine can be suspected.<br />
In conclusion, the new CEDI A assay for buprenorphine is suitable for use in clinical routine testing at a<br />
cut<strong>of</strong>f limit at 5 Ilg/L.<br />
Key words: Buprenorphine, Urine, CEDI A<br />
Page 147
A34 <br />
RAPID DETERMINATION OF PSILOCIN IN WHOLE BLOOD BY LC-MS/APCI<br />
Wojciech Lechowicz', 1, Andrzej Parczewski l ,2, Ewa Chudzikiewiczl, lInstitute <strong>of</strong> <strong>Forensic</strong> Reasearch,<br />
Cracow, Poland, 2Jagiellonian University, Cracow, Poland<br />
Psilocin and psilocibin are naturally occurring mushroom alkaloids, with their structure being similar to<br />
serotonin. Hallucinogenic properties <strong>of</strong> these compounds make them desirable for drug addicts especially<br />
for those who experiment with so-called "altered state <strong>of</strong> consciousness". However, there are many species<br />
<strong>of</strong> mushrooms similar to psilocybe but not containing psilocibin or psilocin. Ingestion <strong>of</strong> unknown<br />
mushrooms may lead to serious intoxication. Rapid method analysis by means <strong>of</strong> liquid chromatographymass<br />
spectrometry with atmospheric pressure chemical ionization (LC-MS/APCI) for detection and<br />
quantification <strong>of</strong> psilocin in whole blood has been proposed. Optimization <strong>of</strong> ionization and fragmentation<br />
parameters was performed using flow injection analysis (FIA). Total ion current (TIC) was recorded.<br />
Optimization was conducted for most abundant ions <strong>of</strong> mlz 20S, 160, llS. Seven parameters were chosen<br />
for optimization: fragmentor voltage (60/120 V), capillary voltage (4000 V), vaporizer temperature<br />
(320°C), drying gas temperature (300°C), pressure (SO psig) and gas flow (7 Llmin) and corona current (4.5<br />
IlA); (in parentheses optimal value is given). Liquid-liquid extraction using a mixture <strong>of</strong> n-propyl<br />
chloride:dichloromethylene (2:1, v/v) after blood alkalization (pH 11) was applied. Psilocin-D IO was used<br />
as the internal standard. Separation was carried out using chromatographic column, prepared according to<br />
customer requirement: LiChroCART (SSx4 mm) filled with Superspher 60 RP-8e stationary phase. The<br />
stationary phase ensured appropriate retention: Psilocin - TR=2.42 min; Psilocin-D IO - TR=2.41 min. For<br />
quantification ramped SIM mode was applied. The pseudomolecular ions <strong>of</strong> mlz 20S, 21S were recorded at<br />
fragmentor voltage <strong>of</strong> 60 V and fragmentation ions <strong>of</strong> m/z 160, 170, lIS, 12S at l20V. The method was<br />
thoroughly validated. Intra- and inter-day precision (repeatability) for target concentration <strong>of</strong> 10 IlglL was<br />
9% and accuracy measured for the concentration range <strong>of</strong> 4-40 Ilg/L, expressed as a mean recovery, was<br />
102±lS%. Results <strong>of</strong> three mushroom intoxication cases have been studied. Only in one tested blood<br />
sample did the concentration <strong>of</strong> psilocin exceed S.2 Ilg/L, the level determined to be LOQ. The determined<br />
concentration was 8 Ilg/L <strong>of</strong> free psilocin and 12 IlglL <strong>of</strong> total psilocin. In case <strong>of</strong> two others person's<br />
concentration <strong>of</strong> free psilocin was above 1.7 Ilg/L (LOD) but lower than LOQ. Some important remarks<br />
concerning ion suppression caused by matrix, adsorption and solubility <strong>of</strong> psilocin have been shown to<br />
exert substantial influence on signal intensity.<br />
Keywords: Psilocin, Blood, LC-MS/APCI<br />
Page 148
A35 <br />
ETHYLGLUCRONIDE ANALYSIS IN URINE BY LIQUID CHROMATOGRAPHY WITH<br />
TANDEM MASS SPECTROMETRY<br />
Michael Feldman*' \ KC Van Home 2 , Zhichun Liu 2 , Patrick Bennete, David J. Kuntz!. lNorthwest<br />
Toxicology, a division <strong>of</strong>Lab One, Salt Lake City, UT 84124, USA and 2Tandem Labs, Salt Lake City, UT<br />
84124, USA<br />
~-D-ethylglucuronide (EtG) is a metabolite <strong>of</strong> ethanol which is formed by the conjugation <strong>of</strong> ethanol with<br />
activated glucuronic acid in the presence <strong>of</strong> membrane-bound mitochrondrial UDP glucuronyl transferase.<br />
EtG is produced at approximately 0.02-0.06% <strong>of</strong> an ingested dose. EtG is stable, water-soluble and can be<br />
detected in urine and can be detected for up to three days following ethanol consumption. Urine ethanol<br />
levels are normally detected only for several hours, thus making EtG a unique metabolite for monitoring<br />
abstinence <strong>of</strong> alcoholics in alcohol treatment programs.<br />
Urine samples for analysis are prepared by the direct addition <strong>of</strong> 100 IJ,L <strong>of</strong> urine with 400 IJ,L <strong>of</strong> internal<br />
standard (EtG-D5) in water into the liquid sample vial. No extraction is required. The HPLC used in the<br />
analysis is a Shimadzu SCL-IOA with a Phenomenex Luna 31J,m column with a mobile phase consisting <strong>of</strong><br />
methanol, water and formic acid with a flow rate <strong>of</strong> 400lJ,Llminute. The mass spectrometer is a Sciex API<br />
3000 using a Turbo Ion Spray Source in the negative ion mode. Quadrupole 1 was set to pass the 221 and<br />
226 ions for EtG and EtG-D5, respectively. Transition ions <strong>of</strong> 75 (quantitation) and 85 (qualifier) were<br />
monitored for each compound.<br />
The assay was linear between 40 nglmL to 10,000 ng/mL with a cut<strong>of</strong>f established at 100 ng/mL with a<br />
Limit <strong>of</strong> Detection and Limit <strong>of</strong> Quantitation <strong>of</strong> 40 ng/mL. Precision was determined with %CV <strong>of</strong> less<br />
than 1 % between the concentrations <strong>of</strong> 40-150 ngimL. The %CV between runs was determined to be less<br />
than 7%. Data from dosing studies, including incidental exposure, will be presented.<br />
Keywords: Ethylglucuronide, Ethanol<br />
Page 149
A36 <br />
MASS SPECTROMETRIC IDENTIFICATION OF ETHYL SULFATE IN HUMANS - A NEW<br />
ETHANOL METABOLITE AND A BIOMARKER OF ACUTE ALCOHOL INTAKE<br />
A. Helander- and O. Beck. <br />
Karolinska Institute & University Hospital, SE-171 76 Stockholm, Sweden. <br />
The traditional way to establish whether a person has recently consumed alcohol is by the analysis <strong>of</strong><br />
breath, blood or urine samples for the presence <strong>of</strong> ethanol. However, because ethanol is rapidly<br />
metabolized and eliminated from the body, a method to reveal recent drinking even after ethanol has been<br />
cleared would have considerable importance in clinical and forensic toxicology. A very small fraction<br />
«0.1%) <strong>of</strong> the ethanol consumed undergoes a phase II conjugation reaction catalyzed by UDPglucuronosyltransferase<br />
to produce ethyl glucuronide (EtG), which is excreted in urine. This non-oxidative<br />
trace metabolite has attracted interest mainly as a specific biochemical marker for recent consumption <strong>of</strong><br />
alcohol.<br />
Animal studies have indicated that ethanol may also undergo sulfate conjugation to produce ethyl sulfate<br />
(EtS). In the present study on humans, a direct electrospray LC-MS method was used to confirm ifEtS is<br />
formed following intake <strong>of</strong> alcohol and excreted in the urine. Urine samples were collected from healthy<br />
subjects at timed intervals after drinking a single ethanol dose. Urine samples were also selected at random<br />
from those sent to the laboratory for routine testing <strong>of</strong> recent alcohol consumption. Samples were stored at<br />
-20°C until analysis.<br />
LC-MS analysis <strong>of</strong> EtS was performed in the negative ion mode, with selected-ion monitoring at mlz 125<br />
for EtS (Mw 126.1 g/moJ) and mlz 226 for EtG-ds (used as internal standard). The identity <strong>of</strong> EtS was<br />
confirmed by the correct S isotope ratio in authentic specimen, as compared to EtS reference material. The<br />
EtS concentration <strong>of</strong> unknown samples was determined from the peak area ratio <strong>of</strong> EtS to EtG-ds, by<br />
reference to a calibration curve. The calibration curve was linear (r 2 =0.99, p
..~.<br />
A37 <br />
HIGH THROUGHPUT SCREENING OF CORTICOSTEROIDS AND BASIC DRUGS IN HORSE<br />
URINE BY LC-MS-MS<br />
Gary N. W. Leung, Evonne W. Chung, Emmie N. M. Ho, W. H. Kwok, David K. K. Leung, Francis P. W.<br />
Tang, Terence S.M. Wan*, and Nola H. Yu<br />
Racing Laboratory, The Hong Kong Jockey Club, Sha Tin Racecourse, Sha Tin, N.T., Hong Kong, China;<br />
terence.sm. wan@hkjc.org.hk<br />
Introduction: Gas chromatography - mass spectrometry (GC-MS) has long been accepted as a powerful<br />
technique for the screening and confirmation <strong>of</strong> the presence <strong>of</strong> prohibited substances in biological samples<br />
from human and animal athletes. Over the past decade, liquid chromatography - mass spectrometry (LC<br />
MS) has evolved into a mature technique and is gaining wide acceptance in many doping control<br />
laboratories. LC-MS or LC-MS' is particularly suited for the analyses <strong>of</strong> polar, non-volatile and heatlabile<br />
drugs that cannot be adequately handled by GC-MS. In addition, tedious derivatization steps can<br />
<strong>of</strong>ten be omitted. This paper describes two high throughput LC-MS-MS methods for the screening <strong>of</strong> two<br />
important classes <strong>of</strong> drugs in equine sports, namely the corticosteroids and the basic drugs, at low ppb<br />
levels in horse urine. The method utilized a high efficiency reversed phase LC column (3 cm L x 2.1 mm<br />
ID with 2.5 Jlm particles) to provide fast turnaround times as well as achieving significant reduction in the<br />
consumption <strong>of</strong> expensive HPLC solvents. The performance <strong>of</strong> these two methods on real samples was<br />
demonstrated by analysing drug administration and positive postrace urine samples.<br />
Method: Corticosteroids and basic drugs were extracted from enzyme-treated urine by solid-phase<br />
extraction using a Bond Elut CertifY® cartridge and analysed by LC-MS-MS in multiple reaction<br />
monitoring (MRM) mode using a Thermo Finnigan triple quadrupole TSQ Quantum mass spectrometer.<br />
Separation <strong>of</strong> the corticosteroids and basic drugs was achieved using a short reversed-phase CI8 column (3<br />
cm Lx 2.1 mm ID with 2.5 Jlm particles) on two different LC gradient solvent systems.<br />
Results: Using the methods developed in this study, the detection <strong>of</strong> 23 corticosteroids and 42 basic drugs<br />
could be achieved within a 2.5-min and a 3.5-min LC-MS-MS run respectively. The overall turnaround<br />
time for the corticosteroid screen was 5 minutes and that for the basic drug screen was 8 minutes, inclusive<br />
<strong>of</strong> post-run and equilibration times. The results on the analysis <strong>of</strong> drug administration and positive<br />
postrace urine samples also demonstrated that both methods were effective in detecting corticosteroids and<br />
basic drugs in horse urine at low ppb levels.<br />
Conclusion: Two high throughput LC-MS-MS methods with the use <strong>of</strong> a high efficiency LC column have<br />
been developed for the screening <strong>of</strong> corticosteroids and basic drugs at low ng/mL levels in equine urine.<br />
Validation data will also be presented. These methods can be used to control the abuse <strong>of</strong> these two classes<br />
<strong>of</strong> drugs in racehorses.<br />
Keywords: Corticosteroids, Basic drugs, High throughput LC-MS-MS<br />
Page 151
A38 <br />
SCREENING FOR, LIBRARY-ASSISTED IDENTIFICATION AND FULLY VALIDATED<br />
QUANTITATION OF TWENTY-TWO beta-BLOCKERS IN BLOOD PLASMA BY LIQUID<br />
CHROMATOGRAPHY-MASS SPECTROMETRY WITH ATMOSPHERIC CHEMICAL<br />
IONIZATION<br />
Hans H. Maurer*, Oliver Tenberken, Carsten Kratzsch, Annin A. Weber, and Frank T. Peters<br />
Department <strong>of</strong> Experimental and Clinical Toxicology, University <strong>of</strong> Saarland, D-66421 Homburg (Saar),<br />
Gennany, E-mail: hans.maurer@unikIinik-saarland.de<br />
Background: Overdose <strong>of</strong> beta-blockers may lead to life-threatening situations. Although there is no strong<br />
correlation between plasma concentration <strong>of</strong> beta-blockers and their pharmacological and toxic effects,<br />
suitable analytical procedures are necessary for toxicological screening, identification and quantification in<br />
clinical and forensic toxicology. Therefore, an assay was developed for such purposes in human blood<br />
plasma using LC-APCI-MS.<br />
Methods: After mixed-mode (Confirm HCX) solid-phase extraction <strong>of</strong> 0.5 mL <strong>of</strong> plasma, the beta-blockers<br />
were separated on a Superspher 60 RP Select B column (125 x 2 mm J.D., guard column: 10 x 2 mm I.D.)<br />
using fast gradient elution (ammonium formate buffer/acetonitrile). The compounds were screened for and<br />
identified using an LC-APCI-MSD (SL version) in the scan mode with fragmentor voltages <strong>of</strong> 100 and 200 V<br />
by mass chromatography with selected ions followed by library search <strong>of</strong> the underlying full APCI mass<br />
spectra with our new LC-MS reference library. The drugs were quantified in the SIM mode at 100 or 200 V<br />
using calibration curves. The assay was fully validated according to internationally accepted<br />
recommendations.<br />
Results: The assay allowed screening for, library-assisted identification (both in scan mode) and<br />
quantification (selected-ion mode) <strong>of</strong>the beta-blockers acebutolol, diacetolol, alprenolol, atenolol, betaxolol,<br />
bisoprolol, bupranolol, carazolol, carteolol, carvedilol, celiprolol, esmolol, labetalol, metoprolol, nadolol,<br />
nebivolol, oxprenolol, penbutolol, propranolol, sotalol, talinolol and timolol in blood plasma. The assay was<br />
found to be selective for all tested compounds. No interfering peaks were observed in the extracts <strong>of</strong> ten<br />
different blank plasma samples. Interferences with common drugs typically taken in combination were tested<br />
and could be excluded due to different retention time and/or mass spectra. The assay was linear from<br />
sub-therapeutic to overdose concentrations <strong>of</strong> all compounds. A weighted (lIx 2 ) least squares model was<br />
used for calculation <strong>of</strong> calibration curves. Low and high level recoveries ranged from 46.9% to 94.8% for all<br />
studied analytes. LODs were determined in the full scan mode and they were all lower or equal to the<br />
corresponding LOQs in the SIM mode. The LOQs corresponded to the lowest calibrator concentrations with<br />
a signal-to-noise ratio <strong>of</strong>at least 10. Within-day, between-day and total precision (combination <strong>of</strong>with in- and<br />
between-day effects) lay within the required limits <strong>of</strong>:::;15% RSD (::520% RSD at LOQ). Accuracy data also<br />
all lay within the acceptance interval <strong>of</strong> ±15% (±20% at the LOQ) <strong>of</strong> the nominal values. In processed<br />
samples, the analytes were stable for a period <strong>of</strong> more than 24 hours at room temperature. No instability <strong>of</strong><br />
analytes in spiked samples was observed over three freeze/thaw cycles or during storage at -20°C for a one<br />
month period. The procedure has proven to be applicable in the analysis <strong>of</strong>authentic plasma samples during<br />
routine work. The presented assay is the first fully validated procedure for the simultaneous detennination <strong>of</strong><br />
a large number <strong>of</strong>beta-blockers in plasma. In emergency toxicology, it should be applicable to confine to one<br />
point calibration because the y-intercepts <strong>of</strong> the calibration curves were either not significant (p < 0.05) or<br />
small compared to the response at high therapeutic concentrations.<br />
Conclusions: The LC-MS assay has proven to be appropriate for screening, identification and quantification<br />
<strong>of</strong> beta-blockers in plasma after intake <strong>of</strong>therapeutic as well as <strong>of</strong> toxic dosages. It was successfully applied<br />
to authentic plasma samples allowing confirmation <strong>of</strong>diagnosis <strong>of</strong>overdose situations as well as monitoring<br />
<strong>of</strong> patients' compliance.<br />
Keywords: liquid chromatography-mass spectrometry; beta-blockers; plasma<br />
Page 152
A39 <br />
RAPID DETERMINA nON OF CHLORAMPHENICOL AND ITS GLUCURONIDE IN FOOD<br />
PRODUCTS BY LIQUID CHROMATOGRAPHY- ELECTROSPRA Y NEGA nVE IONIZAnON<br />
TANDEM MASS SPECTROMETRY<br />
Madej J.Bogusz*, Huda Hassan, Eid Al-Enazi, Mohammed AI-Tufail<br />
King Faisal Specialist Hospital and Research Centre, P.O.Box 3354, 1211 Riyadh, Kingdom <strong>of</strong> Saudi<br />
Arabia<br />
Chloramphenicol (CAP) is subjected to monitoring in food products, with a mllllmum required<br />
performance level set at 0.3 ng/g. CAP was isolated from chicken meat and seafood by very simple solvent<br />
extraction procedure. For honey, a fast SPE procedure was applied. CAP-D5 was used as internal standard.<br />
HPLC separation was done on RP18 123 x 3mm column in acetonitrile-ammonium formate 10 mM, pH 3.0<br />
(40:60) at flow rate <strong>of</strong> 0.3 m/min. A TSQ Quantum instrument with ESI source has been used in negative<br />
ionization mode. A MRM procedure has been applied and following transitions were monitored: rn/z<br />
321>152 (quantifier), 321>194, 321>257 (qualifiers), 326>157 (IS). CAP peak was eluted at around 5 min;<br />
the total run time was 7 min. LOD was around 0.1 nglg meat or 0.05 nglg honey. For confirmation, ion<br />
intensity ratios were used. Matrix effects were studies using various approaches. The method allows<br />
analyzing up to 30 duplicate samples/day, including all calibration standards. Additionally, the method for<br />
determination <strong>of</strong> CAP glucuronide (CAP-G) was established. As a source <strong>of</strong>CAP-G urine specimens taken<br />
from rats which were given CAP were used. For the isolation <strong>of</strong> CAP and CAP-G a SPE procedure, used<br />
also for honey, was applied.<br />
Keywords: Chloramphenicol, Chloramphenicol glucuronide, LC-MS-MS<br />
Page 153
A40 <br />
BROAn..SPECTRUM BENZODIAZEPINE SCREENING BY LC-MSIMS<br />
Kathleen McKague* and Michael Whiteside<br />
Centre <strong>of</strong> <strong>Forensic</strong> Sciences, Toronto, Ontario, Canada<br />
Screening biological samples for benzodiazepines is <strong>of</strong>ten carried out using immunoassay (IA) techniques.<br />
However, due to the chemical diversity <strong>of</strong> this class <strong>of</strong> drugs, specific identification, confirmation and<br />
quantitation <strong>of</strong> the benzodiazepines present in forensic toxicology generally requires multiple analytical<br />
systems (LC, GC & GCIMS). Prior to validation <strong>of</strong> this work, confirmation <strong>of</strong> a putative positive result by<br />
IA in this laboratory necessitated the use <strong>of</strong> 11 separate analytical methods with the potential to consume<br />
19 mL <strong>of</strong> sample. This led us to develop a single analytical technique for the screening and identification<br />
<strong>of</strong> benzodiazepines. A solid phase extraction (SPE) method coupled with LC-MSIMS analysis, was<br />
developed to simultaneously detect 14 benzodiazepines and 9 benzodiazepine metabolites in 1 mL <strong>of</strong> blood<br />
or urine. The compounds and their respective limits <strong>of</strong> detection (LOD) in blood included in this assay are<br />
alprazolam (1.5 nglmL), a-hydroxyalprazolam (1.5 nglmL), bromazepam (1.5 nglmL), chlordiazepoxide (5<br />
nglmL), demoxepam (5 ng/mL), clobazam (3 nglmL), clonazepam (1.5 nglmL), 7-aminoclonazepam<br />
(3nglmL), diazepam (20 ng/mL), nordiazepam (5 ng/mL), flunitrazepam (1.5 ng/mL), 7<br />
amin<strong>of</strong>lunitrazepam (1.5 ng/mL), n-desmethylflunitrazepam (1.5 nglmL), flurazepam (1.5 ng/mL), n<br />
desalkylflurazepam (1.5 nglmL), lorazepam (3 ng/mL), midazolam (1.5 nglmL), nitrazepam (3 nglmL), 7<br />
aminonitrazepam (1.5 nglmL), oxazepam (3 ngfmL), temazepam (20 ng/mL), triazolam (1.5 nglmL) and a<br />
hydroxytriazolam (1.5 ngfmL).<br />
The extraction method utilizes Waters Oasis HLB extraction cartridges on a Zymark Rapidtrace SPE<br />
workstation. Samples are precipitated with acetonitrile and then diluted with pH 6 phosphate buffer prior<br />
to loading onto the extraction columns. After washing with water, phosphate buffer, and 5% methanol, the<br />
compounds are eluted with 95% methanol. The samples are subsequently derivatized with acetic<br />
anhydride. Analysis <strong>of</strong>the extracted samples is performed on a Thermo-Finnigan LC-MSIMS system. The<br />
HPLC is a ThermO-Finnigan Surveyor equipped with a Waters Symmetry® CIS (2.1 mm x 20 mm, 5 Ilm<br />
particle) guard column followed by an Agilent Zorbax SB-CIS (2.1 mm x 150 mm, 3.5 Ilm particle)<br />
analytical column. Separation is achieved isocratically using a 54:46 methanol:ammonium formate pH 3<br />
buffer at a flow rate <strong>of</strong> 225 ilL/min and a temperature <strong>of</strong> 35°C. The MSIMS system is a Thermo-Finnigan<br />
TSQ Quantum operated in APCI/SRM (atmospheric pressure chemical ionization/selected reaction<br />
monitoring) mode. With the exception <strong>of</strong> alprazolam, a-hydroxyalprazolam, fl unitrazepam , 7<br />
amin<strong>of</strong>lunitrazepam a-hydroxyalprazolam and lorazepam, the limit <strong>of</strong> detection for this method is<br />
significantly lower than any <strong>of</strong> the previously used target analyses utilized by our laboratory.<br />
From July 2003 to April <strong>2004</strong>, we have analyzed 382 case samples. 52% <strong>of</strong> these samples were positive<br />
for at least one benzodiazepine or benzodiazepine metabolite. The most commonly found benzodiazepines<br />
were clonazepam, diazepam, lorazepam, and temazepam. No case samples were positive for either<br />
flunitrazepam or its metabolites. Of the positive findings, 81 % were below the limit <strong>of</strong> detection for the<br />
original target analysis used in our laboratory. While the detection <strong>of</strong> low concentrations <strong>of</strong> these<br />
compounds is not usually an essential requirement in death investigations, they can be critical in drugfacilitated<br />
sexual assault investigations. In the latter instance, sexual assaults are <strong>of</strong>ten associated with the<br />
ingestion <strong>of</strong> low drug doses and a long time elapse between the assault and sample collection. These<br />
factors create an analytical challenge that requires sensitive and specific methodology. The benefits <strong>of</strong> this<br />
assay will be highlighted with case examples.<br />
Key Words: Benzodiazepines, LC-MSIMS, Screening<br />
Page 154
A41 <br />
DETERMINATION OF STRYCHNINE IN HUMAN BLOOD USING SOLID PHASE<br />
EXTRACTION AND GCIEI-MS<br />
M. Barroso'· I, E. Gallard0 2 , S. Avila l , C. Margalho l , E. Marques I ,M. Lopez-RivaduIla 2 , D.N. Vieira l<br />
INational Instutute <strong>of</strong> Legal Medicine, Delegation <strong>of</strong>Coimbra, Portugal<br />
2Institute <strong>of</strong> Legal Medicine, University <strong>of</strong> Santiago de Compostela, Spain<br />
Introduction: Strychnine is the main alkaloid in Strychnos nux vomica, an Indian tree. This plant was first<br />
introduced in Germany in the XVI century, as a poison to rats and other pests. Although widely used in the<br />
past, even with pharmaceutical purposes, its use is now limited in many countries. Strychnine is not<br />
commercialized in Portugal since 1974, but sometimes it is still associated with forensic intoxications,<br />
because small amounts may remain in storage, particularly in rural areas. The objective <strong>of</strong> this work was<br />
the development and validation <strong>of</strong> a simple and rapid method for the determination <strong>of</strong> strychnine in human<br />
blood, employing solid phase extraction (SPE) and GC/EI-MS.<br />
Materials and Methods: Oasis HLB (30 mg) extraction cartridges were obtained from Waters (Milford,<br />
MA, USA). Stock solutions <strong>of</strong> strychnine and papaverine (internal standard) were prepared in methanol,<br />
protected from light and stored at 4°C until use.<br />
The sample was submitted to the following procedure: to 500 J.1L <strong>of</strong> blood were added 2 mL <strong>of</strong> distilled<br />
water, and the mixture was centrifuged at 3000 rpm for 5 minutes. The supernatant was then applied to<br />
previously conditioned SPE columns. After elution <strong>of</strong> the sample the columns were washed with 1 mL <strong>of</strong><br />
5% methanolic solution, and then dried under full vacuum for 15 minutes. The elution was performed with<br />
1 mL <strong>of</strong> chlor<strong>of</strong>orm, which was afterwards evaporated to dryness under a gentle stream <strong>of</strong> nitrogen. The<br />
dry residue was reconstituted in 50 J.1L <strong>of</strong> methanol, and an aliquot <strong>of</strong> 1 J.1L was injected in the GC.<br />
The GC oven temperature program started at 150°C for 1 minute, then raised by 35 °C/min to 200°C, held<br />
for 1 minute and finally elevated by 40 °C/min to 270°C, where it was kept for 7 minutes.<br />
The injector port was set to 200 "C. The mass spectrometer temperature was 280 "C, and it was operated in<br />
the SIM (Selective Ion Monitoring) mode. The selected ions were 334, 120 and 162 for strychnine; and<br />
338, 324 and 308 for papaverine.<br />
Results: The calibration curve was established in spiked blood within a range <strong>of</strong> 0.10 to 2.50 J.1g/mL, and<br />
the correlation coefficient was 0.9994. The limits <strong>of</strong> detection and quantification were respectively 60.27<br />
and lOO nglmL. The precision (coefficient <strong>of</strong> variation), calculated at both low and high concentrations,<br />
was inferior to lO%. Accuracy was superior to 90% for all calibrators. Mean recovery for strychnine was<br />
90.66%. The method was applied to authentic samples obtained from the Laboratories <strong>of</strong> <strong>Forensic</strong><br />
Toxicology <strong>of</strong> the National Institute <strong>of</strong>Legal Medicine, Coimbra and Lisbon, Portugal.<br />
Conclusion: One may conclude that the proposed technique is analytically suitable for the extraction and<br />
determination <strong>of</strong> strychnine in blood, since it is linear within the studied range, and presents adequate<br />
precision and accuracy. Therefore, it can be applied in forensic cases where the compound is involved.<br />
Keywords: Strychnine, SPE, GClMS<br />
Page 155
A42 <br />
EXTENDING AND IMPROVING SCREENING AND TARGET ANALYSIS UTILIZING LC-MS<br />
Tania A. Sasaki'· I and Byron Curtis 2<br />
IApplied Biosystems, 850 Lincoln Centre Dr., Foster City, CA 94404; 20ffice <strong>of</strong> the Chief Medical<br />
Examiner, 901 Stonewall, Oklahoma City, OK 73117<br />
GC/MS has long been a powerful and useful technique for analysis <strong>of</strong> complex mixtures, as well as target<br />
analyses, because <strong>of</strong> its inherent specificity and sensitivity. However, the necessity for analytes to be labile<br />
limits the types <strong>of</strong> compounds that can be analyzed utilizing this technique and also requires some<br />
extensive sample preparation, such as derivatization, for successful analysis. However, over the past 15<br />
years, LCIMS has grown in popularity due to its applicability for analysis <strong>of</strong> polar molecules, which<br />
includes most drug and pharmaceutical compounds. LCIMS also has the capabilities to analyze higher<br />
molecular weight compounds that are not easily examined by GC/MS due to their high boiling points;<br />
derivatization is rarely, if ever, necessary. Furthermore, chromatographic analysis times are generally<br />
between 10-40 minutes for LC, which are much shorter than the averagetimes used for GC analysis. This<br />
paper examines the utility <strong>of</strong> LC/MS to reduce total analysis times <strong>of</strong> current protocols, as well as develop<br />
methods to analyze or screen for compounds that have no current methodology in the forensics field.<br />
Several types <strong>of</strong> compounds were studied for target analysis, both quantification and general screening,<br />
covering a range from warfarins to common pesticides to neurontin. Currently, these compounds have<br />
been analyzed by either GC/MS or immunoassay. However, the utility <strong>of</strong> these methods is limited by<br />
throughput and/or cost. By using LC coupled with a triple quadrupole mass spectrometer, screening <strong>of</strong><br />
over 50 compounds in a single analytical experiment can be accomplished with low ppb detection limits.<br />
Furthermore, the compounds can be analyzed with minimal sample preparation and short analysis times,<br />
improving the throughput and greatly reducing expense.<br />
Key words: Method development, Mass spectrometry, LCIMS<br />
Page 156
A43 <br />
SIMULTANEOUS DETERMINATION OF SILDENAFIL. VARDENAFIL AND TADALAFIL AS<br />
ADULTERANTS IN DIETARY SUPPLEMENTS BY LC-ESI-MS<br />
K. Saisho*, H. Kamakura, M. Kawamura, R. Kikura-Hanajiri, Y. Goda<br />
National Institute <strong>of</strong> Health Sciences, I-IS-I, Kamiyoga, Setagaya-ku, Tokyo 15S-S50I, Japan<br />
In recent years, there is a problem with illegally added prescription ingredients and/or their synthetic<br />
analogues (as active adulterants) in dietary supplements. Prolonged or excessive consumption <strong>of</strong> these<br />
products may cause possible serious health risks to some users. It has been reported that sildenafil (SDF),<br />
which is therapeutically used for penile erectile dysfunction, is one <strong>of</strong> the active adulterants in products<br />
advertising roborant nutrition. Moreover, its structurally similar anti-impotence drugs, vardenafil (VDF) and<br />
tadalafil (TDF), may be alternative adulterants <strong>of</strong> SDF. In this study, a simultaneous analytical procedure for<br />
three anti-impotence drugs, SDF, VDF and TDF (as adulterants in dietary supplements advertising roborant<br />
nutrition) was developed using LC-ESI-MS.<br />
These drugs were extracted with the solvent consisted <strong>of</strong> acetonitrile and distilled water containing I %<br />
formic acid (4: 1, v/v) under ultrasonication. The separation was achieved on an Inertsil ODS-3 column (2.1 x<br />
150 mm, 5 Om) at 40°C. The following gradient system was used with mobile phase A(5 mM ammonium<br />
formate buffer (pH 3.5) I acetonitrile (75:25, v/v» and mobile phase B (acetonitrile); B: 0 % (0-3 min), B<br />
linear from 0 to 30 % (3-13 min), B: 30 % (13-30 min). The flow rate was at 0.3 mLlmin. LC-MS with ESI<br />
interface in the positive ion mode was used. The linear regression <strong>of</strong>the peak area ratios versus concentration<br />
in standard solution was fitted over the concentration range <strong>of</strong> 10 - 10000 ng/mL (SDF), 5 5000 ng/mL<br />
(VDF) and 50 - 25000 ng/mL (mF). All calibration curves were obtained with correlation coefficients <strong>of</strong><br />
greater than 0.9990. The recoveries <strong>of</strong> SDF, VDF and mF spiked a functional food at O.Olmg/mg<br />
concentrations were 9S.8%, 100.2% and 99.S %, respectively.<br />
The developed method was applied to the determination <strong>of</strong> SDF, VDF and TDF in 91 dietary supplements<br />
obtained from the Japanese market. SDF was identified in seven samples and their contents were in the range<br />
<strong>of</strong>24.2 mg 120.9 mg /capsule or bottle. In addition to SDF, homosildenafil (a synthetic analogue <strong>of</strong>SDF)<br />
was also detected in one <strong>of</strong> the seven samples. TDF was detected in one sample and the content was 0.32<br />
mg/capsule, while VDF was not found in any sample. Moreover, a new synthetic analogue <strong>of</strong> SDF,<br />
hydroxyhomosildenafil, which has never been reported, was also identified in the sample.<br />
Keywords: Anti-impotence drugs, LC-MS, Dietary supplements<br />
Page 157
A44 <br />
SCREENING OF CANNABINOIDS, BENZOYLECGONINE AND OPIATES IN WHOLE BLOOD<br />
AND URINE USING EMIT II PLUS IMMUNOASSAY AND KONELAB 30<br />
K. Wiese Simonsen*, N. Christiansen, I. Breum MUller, Department <strong>of</strong> <strong>Forensic</strong> Chemistry; University <strong>of</strong><br />
Copenhagen; Denmark<br />
Aims: To present a full validated simple and automatic method for screening <strong>of</strong> cannabinoids,<br />
benzoylecgonine and opiates in whole blood and urine for routine use.<br />
Methods: Blood samples were extracted with acetone before analysis. Urine samples were automatically<br />
diluted 5 times. EMIT II Plus calibrator levell, 2,3 and 5 were used for calibration. The analysis was done<br />
with EMIT II PLUS reagents (cannabinoids, cocaine metabolite and opiate assays) on a Konelab 30<br />
instrument at 340 nm.<br />
Results: Cut <strong>of</strong>fs in blood and urine are respectively: cannabinoids: 0.0045 mglkg (blood) and 0.050 mg/kg<br />
(urine); benzoylecgonine: 0.015 mg/kg (blood) and 0.300 mglkg (urine); morphine: 0.020 mg/kg (blood)<br />
and 0.300 mg/kg (urine). Within day precisions for blood controls spiked at cut <strong>of</strong>f were 5-10%<br />
(cannabinoids), 10% (benzoylecgonine) and 5-10% (morphine) (n=10). Between day precisions were 6%<br />
(cannabinoids), 18% (benzoylecgonine) and 12% (morphine) (n=7). Sensitivity was 100% (cannabinoids),<br />
93% (benzoyJecgonine) and 97% (opiates). Specificity was 86% (cannabinoids), 99% (benzoylecgonine)<br />
and 95% (opiates).<br />
Conclusion: A validated method has been described. The method is precise, robust and useful for screening<br />
<strong>of</strong> cannabinoids, benzoylecgonine and opiates in whole blood and urine.<br />
Keywords: Cannabinoids, Benzoylecgonine and opiates, EMIT II Plus immunoassay<br />
Page 158
A45 <br />
FAST QUANTIFICATION OF ETHANOL IN WHOLE BLOOD SPECIMENS BY THE<br />
ENZYME ALCOHOL DEHYDROGENASE METHOD; OPTIMIZA TION BY<br />
EXPERIMENTAL DESIGN<br />
Lena Krist<strong>of</strong>fersen·· l , Bjorn Skuterud 1 , Bente R. Larssen 1 , Svetlana Skurtveit 2 , Anne Smith<br />
Kielland l<br />
lNorwegian Institute <strong>of</strong> Public Health, Division <strong>of</strong> <strong>Forensic</strong> Toxicology and Drug Abuse, P.O. Box<br />
4404 Nydalen, N-0403, Oslo, Norway; 2Norwegian Institute <strong>of</strong> Public Health, Division <strong>of</strong><br />
Epidemiology, P.O. Box 4404 Nydalen, N-0403, Oslo, Norway<br />
A sensitive, fast, simple and high throughput enzymatic method for the quantification <strong>of</strong> ethanol in<br />
whole blood (blood) on Hitachi 917 is presented. Alcohol dehydrogenase (ADH) oxidizes ethanol<br />
to acetaldehyde using the coenzyme nicotinamide adenine dinucleotide (NAD), which is<br />
concurrently reduced to form NADH. Method development was performed with the aid <strong>of</strong> factorial<br />
design, varying pH and concentrations <strong>of</strong>NAD+ and ADH. The linear range increased and reaction<br />
end point decreased with increasing NAD+ concentration and pH. The method was linear in the<br />
concentration range 0.0024-0.4220 g/d!. The limit <strong>of</strong> detection (LOD) and limit <strong>of</strong> quantification<br />
(LOQ) were 0.0007 g/dl and 0.0024 gldl, respectively. Relative standard deviations (RSD) for the<br />
repeatability and within laboratory reproducibility were in the ranges 0.7-5.7 % and 1.6-8.9 %,<br />
respectively. The correlation coefficient when compared to head space gas chromatography flame<br />
ionization detection (HS-GC-FID) methods was 0.9903. Analysis <strong>of</strong> authentic positive blood<br />
specimens gave results that were slightly lower than those <strong>of</strong> the reference method.<br />
Key words: Ethanol, ADH, Quantitation<br />
Page 159
A46 <br />
A RAPID METHOD FOR THE ANALYSIS OF ATOMOXETINE IN BLOOD USING GCIMS<br />
Mike K. Angier*, Russell 1. Lewis & Robert D. Johnson, Federal Aviation Administration, Civil Aerospace<br />
Medical Institute, Bioaeuronautical Sciences Research Laboratory, P.O. Box 25082, Oklahoma City,<br />
Oklahoma 73125<br />
Atomoxetine is a selective norepinephrine reuptake inhibitor (SNRI) prescribed for the treatment <strong>of</strong><br />
attention deficitJhyperactivity disorder (ADHD). It is the first non-stimulant drug approved by the FDA for<br />
the treatment <strong>of</strong> this disorder in both adults and children. Since its approval in November 2002, over two<br />
million prescriptions have been filled. It has been estimated that 3% <strong>of</strong> the U.S. adult population may have<br />
ADHD. A review <strong>of</strong> the current literature has identified no gas chromatographic/mass spectrometric<br />
(GCIMS) methods for the detection <strong>of</strong> atomoxetine in the forensic toxicology setting. Therefore, our<br />
laboratory developed a method for the identification and quantitation <strong>of</strong> atomoxetine in postmortem blood<br />
using GCIMS. This procedure incorporates a Varian Bond Elut® Certify solid phase extraction (SPE)<br />
followed by derivitization with pentafluoropropionic anhydride (pFPA). Derivitization <strong>of</strong> atomoxetine<br />
with PFPA, although not required for the GC/MS analysis <strong>of</strong> this compound, affords both superior linearity<br />
and sensitivity over the non-derivatized compound. The method described is highly selective and sensitive,<br />
having a limit <strong>of</strong> detection <strong>of</strong> 1 ng/mL for atomoxetine. Atomoxetine was found to have a linear dynamic<br />
range <strong>of</strong> 3 - 800 ng/mL on a calibration curve weighted by a factor <strong>of</strong> l/x. The SPE provided an efficient<br />
sample extraction yielding recoveries <strong>of</strong> 40 ± 3% and 51 ± 4% at 25 and 250 ng/mL (n=5 for each group).<br />
Furthermore, the developed procedure provided superb accuracy and precision. This procedure showed<br />
intra-day (within day) relative errors <strong>of</strong>::; 5% and relative standard deviations (RSD) within 2% for both the<br />
25 ng/mL and 250 ng/mL control groups (n=5 for each group). Using whole blood controls stored at 4°C<br />
the inter-day (between day) relative errors for the 25 ng/mL control group were 9%, 10% and 3% for days<br />
2,3 and 7, respectively (n:=:5). The relative errors for the 250 ng/mL control group were 6%, 3% and 4%<br />
for days 2, 3 and 7, respectively (n=5). The RSDs were all < 5% for both control groups over the 7-day<br />
period. Based on the day 7 results, it is clear that atomoxetine is stable in blood stored at 4°C for at least<br />
one week. The method developed proved to be rapid, reliable and sensitive for the identification and<br />
quantitation <strong>of</strong>atomoxetine in blood.<br />
Key Words: Atomoxetine, SNRI, <strong>Forensic</strong> Toxicology<br />
Page 160
A47 <br />
STABILITY OF PLASMA ACETALDEHYDE DETERMINED BY GAS CHROMATOGRAPHY<br />
POSITIVE ION CHEMICAL IONIZATION-MASS SPECTROMETRY<br />
Meng Chen"', David M. Andrenyak, David E. Moody and Rodger L. Foltz. Center for Human Toxicology,<br />
Department <strong>of</strong> Pharmacology and Toxicology, University <strong>of</strong> Utah, Salt Lake City, Utah 84112.<br />
Simultaneous abuse <strong>of</strong> drugs and alcohol is common. Acetaldehyde is a metabolite <strong>of</strong> ethanol that<br />
accumulates when ethanol is taken with disulfiram and in many individuals with genetic variants in alcohol<br />
dehydrogenase and lor aldehyde dehydrogenase. Analysis <strong>of</strong> acetaldehyde is considerable difficult due to<br />
the volatility and various factors, such as enzymatic and nonenzymatic oxidation. Most previously<br />
published methods require immediate on-site handling <strong>of</strong> specimens to allow analysis. A goal <strong>of</strong> this work<br />
was to develop a method where samples can be collected as plasma, stored and shipped for <strong>of</strong>f-site<br />
analysis. A novel method was developed for the determination <strong>of</strong> acetaldehyde in human plasma that<br />
utilizes a simple liquid-liquid extraction procedure and gas chromatography-positive ion chemical<br />
ionization-mass spectrometry (GC-PCI-MS). Using acetaldehyde-dt as internal standard, both acetaldehyde<br />
and acetaldehyde-d 4 were derivatized directly in plasma with 2, 4-dinitrophenylhydrazine in hexane solvent<br />
at room temperature. The derivatized- acetaldehyde and acetaldehyde-d 4 were extracted into hexane. After<br />
centrifugation, an aliquot <strong>of</strong> supernatant was transferred to an autosampler vial for analysis. A GC capillary<br />
column was used for the separation <strong>of</strong> the derivatives, which were subsequently ionized with ammonia<br />
reagent gas and analyzed by MS. The GC oven temperature was initially set at 120'C and increased to<br />
300'C at 20'C Iminute. Run time for each injection was 10 minutes. MS source and quadruple temperatures<br />
were set at 200 and 150 'C, respectively. The prominent ions at m/z 242 and 246 for acetaldehyde and<br />
acetaldehyde-dt. respectively, were analyzed by selected ion monitoring. The lower limit <strong>of</strong> quantification<br />
was 0.3 j.tg/mL in 0.5 mL <strong>of</strong> plasma and the linearity in 4 assays was ~=0.998, over a range from 0.3 to 20<br />
j.tglmL. When intra- and inter-assay precision and accuracy were evaluated at concentrations <strong>of</strong> 0.75, 8 and<br />
15 j.tglmL, mean measured concentrations did not deviate more than 14% from the target and coefficient <strong>of</strong><br />
variance did not exceed 4%. After derivatization, the extracts <strong>of</strong> acetaldehyde and acetaldehyde-dt were<br />
found to be stable for up to 117 hrs in autosampler vials at room temperature. This method is simple<br />
because <strong>of</strong>: no need for protein precipitation; single step in liquid-liquid solvent extraction; no<br />
concentration steps, such as drying supernatant and reconstitution. The method was used to study the<br />
stability <strong>of</strong> acetaldehyde in human plasma. In conclusion, this simple and reliable method appears to be<br />
useful in toxicology and other researches. The research is supported by NIDA Contract NO 1 DA-3-8829.<br />
Key Words: Acetaldehyde, GC-MS, Stability.<br />
Page 161
A48 <br />
MULTICENTER EV ALUA TION OF THE ROCHE ONLINE® TDM CARBAZEPINE ASSA Y FOR<br />
ROCHEIHITACHI ANALYZER SYSTEMS<br />
Mary Jane C<strong>of</strong>fing* I, Roger L. Bertholf, Martin Kroll 3 , Hilmar H. Luthe 4 , Alain Verstraete 5, Heike<br />
Sauter 6 , RaifRoeddiger 6<br />
IClinical Trials, Roche Diagnostics Cooperation, Indianapolis, IN, USA; 2University <strong>of</strong> Florida Health<br />
Science Center, Jacksonville, FL, USA; 3Dallas VA Medical Center, Dallas, TX, USA; 4Department<br />
Clinical Chemistry, Universitiit G6ttingen, Germany; 5Ghent University Hospital, Ghent, Belgium;<br />
6Clinical Trials, Roche Diagnostics GmbH, Mannheim, Germany<br />
Carbamazepine is an anticonvulsant and anti-manic drug, used in the treatment <strong>of</strong> trigeminal neuralgia,<br />
bipolar disorders, epilepsy, and a wide variety <strong>of</strong> seizure disorders. Monitoring carbamazepine<br />
concentrations is essential during therapy in order to ensure achievement <strong>of</strong> optimal therapeutic effect,<br />
while avoiding the impact <strong>of</strong> both subtherapeutic and toxic drug levels.<br />
The analytical performance <strong>of</strong> a new, Roche homogeneous microparticle immunoassay for Carbamazepine<br />
was evaluated at four sites two in Europe and two in the Unites States. Intra- and interassay imprecision,<br />
lower detection limit, control recovery, and linearity were assessed. Further, the assay method was compared<br />
to the CEDIA Carbamazepine assay on RochelHitachi 917 and MODULAR P analyzers, Abbott FPIA<br />
Carbamazepine assay on the Abbott AxSYM and TDx analyzers, and the Roche FP assay on INTEGRA 800.<br />
Serum vs. sodium heparin plasma comparison was also performed.<br />
OnLine Carbamazepine intra-assay imprecision showed 8Ds sO.14 J..lg/mL for concentrations up to 4<br />
J..lg/mL and CVs s3.4 for concentrations >4 J..lg/mL. Interassay imprecision showed SDs s0.15 J..lglmL for<br />
concentrations up to 4 J..lglmL and CVs s4.1 for concentrations >4 J..lglmL. Analytical sensitivity (lower<br />
detection limit) to 0.22 J.lglmL and linearity to the 20.0 J..lglmL were observed. Roche COBAS FP control<br />
materials recovered within range at all sites and competitor control materials recovered within<br />
manufacturers' ranges with one exception.<br />
PassinglBablok regression analysis was used to assess method comparison. All comparisons demonstrated<br />
c I ose agreement between competitive met h 0 d s as note d'mthetable b eow: I<br />
Methodoiogyllnstrument<br />
N Slope Intercept Correlation<br />
x<br />
y<br />
Coefficient<br />
Site 1 CEDIA MODP OnLine MOD P 168 1.055 -0.248 0.993<br />
8ite2 CEDIA 917-R OnLine 917-R 157 0.982 0.093 0.983<br />
Site 3 CEDIA MODP OnLine MODP 161 1.059 -0.642 0.972<br />
COBASFP OnLineMODP 161 1.121 -0.458 0.984<br />
INTEGRA 800<br />
Abbott AxSYM I OnLine MOD P 161 1.120 -0.426 0.975<br />
Site 4 CEDIA 917 OnLine 917 145 1.039 -0.409 0.988<br />
Abbott TDx OnLine 917 145 1.068 -0.111 0.986<br />
Comparison <strong>of</strong> serum vs. sodium heparin plasma produced this regression equation: y 1.l07x - 0.074,<br />
r=0.982 (n=47). The OnLine Carbamazepine TDM reagent met or exceeded analytical specifications and<br />
all clinically relevant performance criteria in this evaluation.<br />
Key Words: Carbamazepine, Automated Method, Multicenter Evaluation<br />
Page 162
A49 <br />
AN LC-MSIMS METHOD FOR THE QUANTIFICATION OF BUPRENORPHINE AND<br />
NORBUPRENORPHINE IN BLOOD AND URINE<br />
Merja Gergov*, Pirjo Tiainen and I1kka Ojanperli<br />
Department <strong>of</strong> <strong>Forensic</strong> Medicine, University <strong>of</strong>Helsinki, P.O. Box, 40, FIN-00014 University <strong>of</strong> Helsinki,<br />
Finland<br />
Background: The synthetic opioid buprenorphine has become common in the maintenance therapy <strong>of</strong><br />
opioid addicts in Finland since 1999. The increasing number <strong>of</strong> samples has required a simple and reliable<br />
analytical method suitable for routine use. LC-MS/MS provides high selectivity and sufficient sensitivity<br />
for the quantitation <strong>of</strong>buprenorphine and its metabolite norbuprenorphine in urine and blood.<br />
Methods: Urine samples were hydrolyzed with ~-glucuronidase enzyme. Sample work-up for blood and<br />
hydrolyzed urine involved liquid-liquid extraction with ethyl acetate at pH 7. The extracts were run by LC<br />
on a Genesis CIS reversed phase column using acetonitrile-ammonium acetate mobile phase at pH 3.2. The<br />
mass spectrometric analysis was performed with a triple quadrupole mass spectrometer equipped with a<br />
turbo ion spray interface in positive mode using multiple reaction monitoring (MRM). Sufficient<br />
sensitivity was achieved only by monitoring the surviving parent ions both for buprenorphine (mlz 468.0)<br />
and norbuprenorphine (mlz 414.2) at the collision energy <strong>of</strong> 20 eV. Quantification was performed using<br />
deuterated internal standards and four-point calibration.<br />
Results: Validation curves were prepared with four replicates at ten concentration levels. The linearity<br />
criterion was accuracy better than ± 20% at the calibration curve. The method exhibited good linearity<br />
from 1 to 200 /lg/l for urine (r2 ~ 0.996, quadratic regression) and from 0.2 to 100 !lg/l for blood (r ~<br />
0.998, linear regression through zero). The average intra-day precision <strong>of</strong> real autopsy samples was 3 %<br />
for both compounds in urine, and 7% for buprenorphine and II% for norbuprenorphine in blood. Criteria<br />
for the LOQ were: 1) precision better than ± 20%, 2) inaccuracy lower than ± 25% in urine and 20% in<br />
blood, and 3) signal-to-noise ~ 10. The LOQs for both compounds were I /lgll in urine and 0.2 /lg/l in<br />
blood. In the study <strong>of</strong> uncertainty <strong>of</strong> measurement, systematic errors were not observed. The expanded<br />
uncertainty <strong>of</strong> measurement (at the confidence level <strong>of</strong> 95%) contained only random errors being for both<br />
compounds 15% and 30% in urine and blood, respectively. A total <strong>of</strong> six pr<strong>of</strong>iciency testing samples<br />
(UKNEQAS 2003, Labquality <strong>2004</strong>) containing buprenorphine were analyzed with the established method,<br />
and the results were within II% <strong>of</strong> the consensus or average value.<br />
Discussion: The present method has been applied to blood and urine samples from more than 420 autopsy<br />
cases and 670 living patients. Interferences from sample matrix have been detected only very rarely even<br />
though the surviving parent ions are monitored to obtain adequate selectivity. Successful participation in<br />
international pr<strong>of</strong>iciency testing schemes proves the high reliability <strong>of</strong>the method.<br />
Keywords: Buprenorphine, Quantification, LC-MS/MS<br />
Page 163
A50 <br />
V ALIDA nON OF AN EIA-BASED SCREENING ASSAY FOR THE DETECTION OF<br />
AMPHETAMINE AND MDMAIMDA IN BLOOD AND ORAL FLUID<br />
Marleen Laloup·' I, Gaelle Tilman l ,2, Gert De Boeck!, Pierre Wallemacq2, Viviane Maes 3 and Nele Samyn l<br />
INational Institute <strong>of</strong> Crimina lis tics and Criminology (NICC), Section Toxicology, Brussels, Belgium;<br />
2Labo Clinical Chemistry and Toxicology, St. Luc University, Hospital-UCL, Brussels, Belgium<br />
3Department <strong>of</strong> Clinical Chemistry-Toxicology, Academic Hospital, Free University <strong>of</strong>Brussels, Belgium.<br />
The number <strong>of</strong> seizures and the use <strong>of</strong> amphetamine and 'ecstasy' (MDMA) have increased exponentially<br />
in Belgium since the late nineties. Therefore, screening for these substances in biological specimens has<br />
become an important part <strong>of</strong> routine analysis in forensic toxicology laboratories. The use <strong>of</strong> a reliable<br />
sensitive immunological assay for the screening <strong>of</strong> blood and oral fluid samples is less widespread than for<br />
the preliminary analysis <strong>of</strong> urine. Such an assay would save cost and labor time in comparison to a more<br />
specific analysis as gas chromatography-mass spectrometry (GC-MS).<br />
The objective <strong>of</strong> this study was to evaluate the suitability <strong>of</strong> the Cozart® AMP enzyme-linked<br />
immunoassays (EIA) for the screening <strong>of</strong> blood and plasma samples, collected with sodium fluoride and<br />
potassium oxalate as anticoagulant, and oral fluid samples, collected with the Intercept® device.<br />
Authentic blood samples (n "" 260) were assayed on the EIA plate, using an optimal 1 :5-fold dilution. True<br />
positive, true negative, false positive and false negative results were determined relative to our routine GC<br />
MS analysis. The EIA readily detects MDA but shows minimal crossreactivity with MDMA « 0.1%), so<br />
the interpretation <strong>of</strong> the GC-MS result <strong>of</strong> the MDMA-only samples was based on the combined<br />
MDAIMDMA concentrations. Samples consisted <strong>of</strong> 100 amphetamine-only positives, 100 MDMAIMDAonly<br />
positives, and 60 negatives, using the limit <strong>of</strong> quantitation as the cut-<strong>of</strong>f level for confirmation (10<br />
nglml). Using these results, receiver operating curves (ROC) were generated and optimal cut-<strong>of</strong>f values for<br />
the screening assay were calculated.<br />
For the amphetamine positive samples, the analysis showed an optimal cut-<strong>of</strong>f value at 66.5 nglml<br />
amphetamine equivalents with a sensitivity <strong>of</strong> 99.0 % and a specificity <strong>of</strong> 96.9 %. For MDMA/MDA<br />
positive samples, 97.0 % sensitivity and 96.9 % specificity were reached at the same cut-<strong>of</strong>f value <strong>of</strong> 66.5<br />
nglml amphetamine equivalents. The area under the ROC curve exceeded 0.97. When combining the<br />
results, the EIA assay is able to predict the presence <strong>of</strong> either amphetamine or MDMAIMDA in plasma<br />
samples with 98.0 % sensitivity and 96.9 % specificity at a cut-<strong>of</strong>f value <strong>of</strong> 66.5 nglml amphetamine<br />
equivalents.<br />
A similar analysis was conducted on 216 oral fluid specimens collected from a controlled double blind<br />
study. Subjects received placebo or a high (l00 mg) or low (75 mg) dose <strong>of</strong>MDMA. Plasma and oral fluid<br />
samples were collected at 1.5 and 5.5 hours after administration. Preliminary analysis <strong>of</strong> the oral fluid<br />
samples indicated a screening cut-<strong>of</strong>f <strong>of</strong> 51 ng/ml amphetamine equivalents with a sensitivity <strong>of</strong> 97.9 % and<br />
a specificity <strong>of</strong> 98.6 %, using the plasma data for confirmation. LC-MSIMS confirmation <strong>of</strong> the oral fluid<br />
samples is in progress.<br />
In conclusion, these data indicate that the Cozart® AMP EIA plates constitute a fast and accurate screening<br />
technique for the identification <strong>of</strong> amphetamine and MDA/MDMA positive blood samples and oral fluid<br />
specimens collected with Intercept®.<br />
Keywords: EIA, Amphetamine, Blood<br />
Page 164
AS1 <br />
SIMULTANEOUS ANALYSIS OF HIPPURIC ACID AND METHYLHIPPURIC ACIDS IN<br />
URINE FROM PAINT THINNER ABUSERS USING HIGH-PERFORMANCE LIQUID<br />
CHROMATOGRAPHY-ELECTROSPRAY IONIZATION MASS SPECTROMETRY<br />
Masatoshi Morinaga*, <strong>Forensic</strong> Science Laboratory Fukuoka Prefectural Police Headquarters, 7-7 Higashi<br />
Koen, Hakata-ku, Fukuoka-ken 812-8576, Japan<br />
A high-perfonnance liquid chromatography-electrospray ionization mass spectrometry (LC-ESI-MS) assay<br />
for the simultaneous analysis <strong>of</strong> hippuric acid and methylhippuric acids in urine is described. Urine samples<br />
were collected from abusers sniffing paint thinner including toluene and a small amount <strong>of</strong> xylenes. These<br />
samples were centrifuged at 3000 rpm for 10min, then diluted by distilled water 100 times and a 10ui<br />
aliquot <strong>of</strong> sample was injected into LCIMS. 1% acetic acid, methanol, THF (90:5:5, VN) was used as a<br />
mobile phase. The method described allows separation <strong>of</strong> hippuric acid and methylhippuric acid in less<br />
than 40 minutes using a stainless steel column packed with octadecyl dimethylsilyiI silica. The separation<br />
was possible for m-hippuric acid and p-methylhippuric acid. The detection limits <strong>of</strong> hippuric acid and<br />
methylhippuric acids were 0.5ug/ml (SIR mode), respectively. The calibration curves were linear in range<br />
<strong>of</strong> 1 to 1000ug/ml. Methylhippuric acids were detected from 36 cases <strong>of</strong> paint thinner abusers and were not<br />
detected in urines <strong>of</strong> 10 nonnal subjects.<br />
•<br />
Key words: Methylhippuric acids, LCIESI-MS, Paint thinner abuser<br />
Page 165
A52 <br />
LCIMSIMS AS A ROUTINE METHOD FOR ANALYSIS OF THERAPEUTIC AND ILLICIT<br />
DRUGS IN FORENSIC SCIENCE<br />
Pascal Mireault· and France Jobin <br />
Laboratoire de Sciences Judiciares et de Medecine Legale, 1701 Parthenais, Montreal, Quebec, Canada, <br />
H2K 3S7. <br />
Introduction: The aim <strong>of</strong> this presention was to evaluate the usefulness <strong>of</strong> Liquid Chromatography coupled<br />
with Tandem Mass Spectrometry (LC/MS/MS) in routine forensic toxicological casework. Presently, Gas<br />
Chromatography coupled with Mass Spectrometry (GCIMS) is the most common method used for<br />
confirmation <strong>of</strong> drugs and its metabolites. However, this technique has the disadvantage <strong>of</strong> requiring<br />
derivatization, because some substances and metabolites are polars and thermolabiles. This drawback can<br />
be overcomed by using LCIMS/MS. LC/MS interface does not involve heat and <strong>of</strong>fer gentle ionization <strong>of</strong><br />
polar and thermolabile compounds. This technique has been used for routine determination <strong>of</strong> several<br />
groups <strong>of</strong> drugs: opiate, cocaine and its metabolites, amphetamine and other psychoactive phenethylamines,<br />
benzodiazepines derivatives, ~9-THC and its metabolites and cardiac g\ycosides.<br />
Experimental: The basic urine or blood were extraction using a solid phase extraction (SPE).<br />
Chromatographic separation was acheived using a Symmetry (Waters) C-1S or C-S column. Mobile phase<br />
conditions used a ratio <strong>of</strong> MeOH and buffer at a flow rate <strong>of</strong> 1 mLimin. A TSQ-7000 API2 triple<br />
quadrupole instrument equipped with a APC} ionization source was used in positive or negative mode.<br />
Results: LC/MSIMS became a very powerful and flexible method for dedicated analyses <strong>of</strong> substances <strong>of</strong><br />
forensic interest. It has been show that the use <strong>of</strong> fast LCIMSIMS provide excellent specificity and high<br />
sensitivity. Spiked urine and blood samples <strong>of</strong> opiate, cocaine and its metabolites, amphetamine and other<br />
psychoactive phenethylamines, benzodiazepines derivatives, ~9-THC and its metabolites and cardiac<br />
gJycosides were analyzed in selected reaction monitoring (SRM) mode to evaluate limit <strong>of</strong> detection<br />
(LaD), limit <strong>of</strong> quantification, linearity and accuracy. LaD obtained range from 0.05 to 2 ng/mL for target<br />
coumpounds in matrices. The specificity <strong>of</strong> the method was evaluated with numerous antemortems and<br />
post-mortem matrices show no significant interferences at the expected retention time <strong>of</strong>target compounds.<br />
This technique improve the analysis <strong>of</strong> polars and thermolabile compounds and decrease analysis time.<br />
Key Words: LC/MSIMS, Biological Matrices, <strong>Forensic</strong><br />
Page 166
AS3 <br />
DETERMINATION OF ETHYL GLUCURONIDE IN URINE BY GAS CHROMATOGRAPHY<br />
TANDEM MASS SPECTROMETRY<br />
M Wang* <br />
Department <strong>of</strong> Biochemistry, Queensland Medical Laboratory, Brisbane, Queensland, Australia <br />
Ethyl glucuronide (EtG) is a metabolite <strong>of</strong> ethanol, formed by enzymatic conjugation <strong>of</strong> ethanol with<br />
glucuronic acid, and is regarded as a useful bio-marker <strong>of</strong> recent alcohol consumption. EtG can be detected<br />
in blood, urine, tissues and hair for an extended time period due to its specific properties <strong>of</strong> non-volatility,<br />
water-solubility and general stability in comparison to ethanol. A gas chromatography-tandem mass<br />
spectrometry (GC-MSIMS) method was therefore developed for the routine determination <strong>of</strong> EtG in urine.<br />
Initial extraction involves 3 ml <strong>of</strong> urine specimen being spiked with 45 ul <strong>of</strong> EtG-D5 (200 uglml) as<br />
internal standard and was adjusted to pH 6.0. Following extraction using a Strata NH2 SPE column with<br />
methanol and water, the extract was evaporated and derivatized with BSTFA (in 1% TMCS and pyridine)<br />
at 80°C for 30 minutes. After evaporation, the residue was reconstituted in 100 III <strong>of</strong> acetonitrile. EtG was<br />
assayed on a Varian Saturn 2000 ion trap GC·MS!MS. The standard curve was linear between 1000 and<br />
10,000 Ilglml with curve correlation coefficients exceeding 0.99. The recovery <strong>of</strong> EtG from solid phase<br />
extraction was approximately 99% at 1000 Ilg/L and 102 % at 8,000 Ilg/L. Measurement <strong>of</strong> EtG in urine<br />
makes it possible to monitor ethanol consumption using a direct metabolite. This GC-MSIMS method<br />
provides a rapid, simple and specific determination <strong>of</strong> ethyl glucuronide.<br />
Key words: Ethyl glucuronide, Gas Chromatography -Tandem Mass Spectrometry, Solid Phase Extraction<br />
Page 167
A54 <br />
SOLID PHASE MICROEXTRACTION GAS CHROMATOGRAPHIC ANALYSIS OF<br />
ORGANOPHOSPHORUS PESTICIDES IN BIOLOGICAL SAMPLES<br />
Nikolaos Raikos*·a, lfigeneia Grigoratou b , Georgios Theodoridis b , Heleni Tsoukali a ,<br />
Dimitrios Psaroulis'<br />
aLaboratory <strong>of</strong> Toxicology and <strong>Forensic</strong> Medicine, Medical School; bLaboratory <strong>of</strong>Analytical Chemistry,<br />
Department <strong>of</strong> Chemistry, Aristotle University, 541 24, Thessaloniki, Greece<br />
A headspace solid phase microextraction (HS-SPME) method in combination with GC-NPD was<br />
developed for the determination <strong>of</strong> a mixture <strong>of</strong> organophosphorus pesticides (malathion, parathion,<br />
methyl parathion and diazinon) in biological samples. Fenithothrion was selected as the internal standard.<br />
A 85 !-lm polyacrylate (PA) SPME fiber was selected for sampling. Various extraction parameters were<br />
studied and optimized: salt addition, desorption time, extraction time, extraction temperature. Best<br />
conditions found were: 0.8 g NaCI added in 3 ml aqueous sample, 20 min sampling at 70 ec, 3 min<br />
desorption at 230°C, The HS-SPME method in combination with GC-NPD provided satisfactory detection<br />
sensitivity and liner dynamic range. The method was applied in the determination <strong>of</strong> the pesticides in<br />
various biological specimens: human whole blood, plasma, liver, kidney and cerebrospinal fluid. The<br />
inherent selectivity provided by the NPD detector together with the efficient sample clean-up <strong>of</strong> the HS<br />
SPME resulted in clear chromatograms with no interferences. Extraction recovery varied significantly from<br />
specimen to specimen. Linear response data for these OPPs was obtained with correlation coefficients<br />
ranging between 0.9866 and 0.9999. High GC signals were observed for diazinon, as a result low limits <strong>of</strong><br />
detection were observed. Limits <strong>of</strong> detection (LODs) were in the range <strong>of</strong> 2-10 nglg for diazinon. In<br />
contrast the signals obtained for methyl parathion and malathion were significantly lower, thus higher<br />
limits <strong>of</strong> detection were observed. Estimated LODs ranged from 35 to 55 ng/g for methyl parathion. The<br />
proposed methodology renders an efficient, cost effective and simple and sample preparation process for<br />
the determination <strong>of</strong> OPPs. Most important, the technique overcomes limitations and obstacles <strong>of</strong><br />
conventional methods such as the use <strong>of</strong> expensive and toxic organic solvents and the application <strong>of</strong> tedious<br />
and cumbersome procedures.<br />
Keywords: Organophosphorus pesticides, HS-SPME, Biological samples<br />
Page 168
ASS <br />
EFFECTS OF ASCORBATE DERJV A TIVE ON SERUM HYDROXY RADICALS IN<br />
ETHANOL-TREATED RATS<br />
Shinobu Itoh" ',Tomohisa Mori', Akiko Tamagawa 2 , Nobuhiko Miwi, Toshiko Sawaguchi I<br />
lDepartment <strong>of</strong> Legal Medicine, Tokyo Women's Medical University, 8-1 Kawada-cho, Shinjuku-ku,<br />
Tokyo 162-8666, Japan; 2Department <strong>of</strong> eel! Biochemistry, Hiroshima Prefectural University School <strong>of</strong><br />
BioSciences, Shobara, Hiroshima 727-0023, Japan<br />
Objective: It is well known that acute and/or chronic ethanol (EtOH) increases toxicity in human and<br />
animals, which might be mediated through oxidative stress. The present study was designed to investigate<br />
the effects <strong>of</strong> EtOH on serum hydroxy radicals (HR), Furthermore, radical scavenge effect <strong>of</strong><br />
L-ascorbyl-2-phosphate Na (APS) was also examined.<br />
Materials and Methods: In order to investigate the oxidative stress caused by EtOH in blood, I mllkg b.w,<br />
<strong>of</strong> 95% EtOH was administered orally to male Wistar rats under pentbarbital anesthesia, and blood<br />
sampling from heart were done 5, 10, 15, 20, 30 and 60 min after administration <strong>of</strong> EtOH, The signal<br />
intensity <strong>of</strong> serum hydroxy radicals (HR) was measured using the ESR LJElectron Spin ResonanceD-Spin<br />
Trap method based on the DMPO 5,5-dimethl-l-pyrroline-N-oxideD-Fenton reaction. ESR apparatus type<br />
JES-FR30 and recorded in a Krebs-Henselelt buffer containing 100 mM DMPO. APS or saline was then<br />
administered to EtOH-treated rats, and the signal intensity <strong>of</strong> serum HR was measured in the same manner<br />
in an attempt to determine their suppressive effects on EtOH-induced oxidative stress.<br />
Result: EtOH significantly increased the signal intensity <strong>of</strong> serum HR about twice as compared with saline<br />
(P
A56 <br />
AUTOMATED SOLID PHASE EXTRACTION PROCEDURE FOR THE SIMULTANEOUS<br />
ANALYSIS OF DELTA-9-TETRAHYDROCANNABINOL (THC), ll-HYDROXY-DELTA-9<br />
TETRAHYDROCANNABINOL (11-0H-THC), AND Il-NOR-DELTA-9-TETRAHYDRO<br />
CANNABINOL-9-CARBOXYLIC ACID (THCC) IN BLOOD, PLASMA, AND ORAL FLUID BY<br />
GCIMSIMS<br />
Paul J. Davis*' \ Nadine Koenigl, Joann Sell I and Dean F. Fritch2, lHealth Network Laboratories, 2024<br />
Lehigh Street, Allentown, PA, 20raSure Technologies, Inc., 150 Webster Street, Bethlehem, PA<br />
A forensic automated procedure for the quantitative determination <strong>of</strong> THC, II-OH-THC, and THCC in<br />
whole blood, plasma, and oral fluid by GCIMS/MS is presented. Samples are treated with acetonitrile,<br />
acidified with dilute acid, and all three analytes are simultaneously extracted by solid phase extraction<br />
using the Caliper Life Sciences Zymark RapidTrace® Solid Phase Extraction Workstation with Varian<br />
SPEC® C-IS SPE cartridges. The RapidTrace® conditioned the SPE cartridges with methanol, added the<br />
sample, washed the cartridges with water/methanol, dried the cartridges with nitrogen, and then eluted the<br />
three cannabinoids with hexane/ethyl acetate. The final extracts were evaporated, derivatized with BSTFA<br />
with 1% TMCS, and analyzed by GCIMSIMS using the Varian 1200 Quadrupole GCIMSIMS System.<br />
Quantitation was accomplished using THC-d3 and THCC-d3 as internal standards. Two product ions were<br />
chosen for each analyte with one product ion serving as the qualifier ion. Retention time had to be within<br />
I% and the ion ratio <strong>of</strong> the qualifier product ion within 20% for identification <strong>of</strong> the analytes. The limit <strong>of</strong><br />
quantitation (LOQ) for THC and II-OH-THC is I ng/mL while the LOQ for THCC is 5 ng/mL. The limit<br />
<strong>of</strong> detection (LOD) for THC and II-OH-THC is 0.5 ng/mL, and 2.5 ng/mL for THCC. Both THC and 11<br />
OH-THC are linear to at least 40 ng/mL While THCC is linear to at least 200 ng/mL. The recovery <strong>of</strong> all<br />
three analytes was approximately 50% for all three specimen types tested. At the LOQ for all three<br />
analytes, between-run precision resulted in a relative standard deviation <strong>of</strong>less then 12%.<br />
Key words: THC, Automated, GCIMS/MS<br />
Page 170
A57 <br />
ELISA FOR THE SCREENING OF OPIA TES, BENZODIAZEPINES, CANNABINOIDS,<br />
METHAMPHETAMINE, AND COCAINE METABOLITE IN POSTMORTEM FORENSIC<br />
WHOLE BLOOD<br />
Paul J. Jannetto', 1,2, Elvan Laleli-Sahin,,2, Susan Gock', Steven H. Wong"2, and Jeffrey Jentzen l , 2<br />
'Milwaukee County Medical Examiner's Office; 2Department <strong>of</strong> Pathology, Medical College <strong>of</strong> Wisconsin<br />
In both forensic and clinical toxicology, enzyme-linked immunosorbent assay (ELISA) based screening<br />
methods are becoming increasingly popular and replacing radioimmunoassay (RIA) methods for numerous<br />
reasons including: cost, automation, ease <strong>of</strong> use, and disposal issues. Currently, the Milwaukee County<br />
Medical Examiner's Office uses the Immunalysis RIA kits to screen whole blood specimens for common<br />
classes <strong>of</strong> drugs such as opiates, benzodiazepines, cannabinoids, methamphetamine, and cocaine<br />
metabolite. In this study, the assay performance <strong>of</strong> the RIA kits was compared to the ELISA kits from the<br />
same manufacturer using fifty-one forensic samples. To further validate the ELISA-based assays, the intraand<br />
interday precision, cross-reactivity, and dose-response curves were analyzed for opiates,<br />
benzodiazepines, cannabinoids, methamphetamine and cocaine metabolite to determine if the ELISA kits<br />
were an acceptable alternative to the RIA kits.<br />
Of the fifty-one samples screened by both RIA and ELISA for opiates, benzodiazepines, cannabinoids<br />
(THC), methamphetamine and cocaine metabolite, there were a total <strong>of</strong> five discordant results (3 THC, and<br />
2 methamphetamine). Gas chromatography-mass spectrometry analysis indicated five unconfirmed positive<br />
results (false-positives) by RIA (3 cases for THC and 2 cases for methamphetamine). On the other hand,<br />
the ELISA kits had a 100% positive and negative predictive value for all five assays. The intraday<br />
coefficient <strong>of</strong>variation (CVs; n == 10) near the immunoassay cut<strong>of</strong>f concentration (60 ng/mL) was 4.0-7.7%<br />
for all five assays, while the interday CVs (n 5) at the immunoassay cut<strong>of</strong>f concentration (50 ng/mL) was<br />
8.4-10.7%.<br />
Overall, a comparative assessment <strong>of</strong> common drug screening assays by RIA and ELISA from the same<br />
manufacturer indicated some differences in analytical performance. The ELISA based screening kits<br />
<strong>of</strong>fered acceptable precision, superior specificity/sensitivity and was an economical alternative to the RIA<br />
kits. The ELISA-based assays are particularly attractive for forensic specimens for several reasons<br />
including: the ability to use a variety <strong>of</strong>sample matrices (e.g. whole blood), small sample volumes reducing<br />
interferences from some forensic matrices, a long shelf life, and the ability to incorporate automation and<br />
increase throughput. Based on these criteria, the Milwaukee County Medical Examiner's Office has<br />
adopted the ELISA-based assays to screen forensic samples for drugs <strong>of</strong> abuse. All presumptive positive<br />
immunoassay results are then confirmed by GCIMS.<br />
Key words: ELISA, RIA, Method validation<br />
Page 171
AS8 <br />
THE DETERMINATION OF FORENSIC BLOOD ALCOHOLS WITH AN INERT AUTOMATED<br />
HEADSPACE SAMPLER<br />
Roger L. Firor, Chin-Kai Meng, Cinthia Cai, Michael Feeney'<br />
Agilent Technologies, Wilmington, Delaware, USA<br />
Blood alcohol analysis is a widely used high-throughput application in forensic laboratories. The use <strong>of</strong><br />
static headspace sampling has many well know advantages for determination <strong>of</strong>volatiles in a variety <strong>of</strong>less<br />
than ideal matrices. Blood or other biological fluids are certainly not the cleanest <strong>of</strong> matrices and therefore<br />
are well suited for headspace sampling. In terms <strong>of</strong> GC analysis, reduced inlet and column maintenance,<br />
better quantitation, and increased throughput are some <strong>of</strong> the advantages <strong>of</strong> automated headspace. Dual<br />
column systems <strong>of</strong>fer an advantage in that the elution order <strong>of</strong> ethanol and some other common metabolites<br />
differ on the DB-ALCl and DB-BAC2 stationary phases. This provides added confirmation and a potential<br />
reduction in possible inferences or coelutions with ethanol.<br />
A new automated headspace sampler with 70-sample tray and inert flow path is introduced for the<br />
determination <strong>of</strong> forensic blood alcohols. The headspace sampler employs a completely inert flow path,<br />
uniform heated zones, and unique vent line purging capability. When taken together, these important<br />
attributes lead to a reduction in carryover and improved repeatability. Standard mixtures in water were used<br />
to demonstrate the analyses. Two headspace-based solutions, based on 0.53mm 10 and 0.32mm ID<br />
columns, are detailed. Isothermal analyses with cycle times below 5 min are easily achieved with sufficient<br />
resolution to avoid common interferences. Total system control from the GC Chern Station is possible with<br />
21 CFR Part 11 compliant s<strong>of</strong>tware specific for headspace sampling.<br />
Key words: Blood Alcohols, Headspace, Gas chromatography<br />
Page 172
A59 <br />
DETERMINATION OF ACONITINE ALKALOIDS BY HPLCITOF-MS: COMPARISON OF<br />
ELECTRO-SPRAY AND LASER-SPRAY IONIZATIONS<br />
Rina Kaneko·'], Satoshi Hattori], Shiho Furuta l , Yukari Hirata l , Kanako Watanabe 2 , Hiroshi Seno\ Makoto<br />
Hamajima l , Akira Ishiil; IDepartment <strong>of</strong> Legal Medicine, Fujita Health University School <strong>of</strong> Medicine,<br />
Japan, 2Department <strong>of</strong> Legal Medicine, Hamamatsu University School <strong>of</strong> Medicine, Japan, 3Department <strong>of</strong><br />
Legal Medicine, Aichi Medical University, Japan<br />
Background: Aconitum species (Ranunculaceae) are widely distributed in Northern Asia and North America.<br />
Their roots are popularly used in herbal medicines in China and Japan; however, their diesterditerpene-type<br />
alkaloids are extremely toxic. For example, the LD50 values <strong>of</strong>aconitine in mice are 1.8 mg/kg (orally) and<br />
0.12 mg/kg (intravenously); the estimated minimal lethal dose in man is about 2 mg. Accidental poisoning<br />
cases by aconite usually happen in Japan. Also, it is sometimes used in suicidal and homicidal cases,<br />
because <strong>of</strong> its high toxicity. It is thus important to determine aconitine alkaloids in body fluids with high<br />
sensitivity. We have succeeded in determining aconitine and its related compounds by HPLC/time-<strong>of</strong>-flight<br />
(TOF)-mass spectrometry (MS). Also, we have tried to detect aconitine alkaloids by laser-spray ionization<br />
and compared its sensitivity with that by conventional electro-spray ionization.<br />
Methods: Aconitine alkaloids (aconitine, mesaconitine, hypaconitine, and jesaconitine) and<br />
methyllycaconitine (internal standard; IS) spiked in plasma samples were purified using a BondElut Certify<br />
HF column. Extracted and dried aconitine alkaloids are reconstituted with 50/lL <strong>of</strong> mobile phase, which<br />
consists <strong>of</strong>70 % <strong>of</strong>20mM ammonium acetate (solvent A) and 30 % <strong>of</strong> acetonitrile (solvent B). HPLC was<br />
employed in the isocratic mode (A:B 70:30) at flow rate <strong>of</strong> 0.2mLlmin. MS was performed on a JEOL<br />
(Tokyo, Japan) AccuTOF HPLC-TOF mass spectrometer; the ionization used was electro-spray ionization<br />
(ESI) in positive ion mode. The MS conditions were as follows: spray voltage; 2.2kV, orifice voltage; 75V<br />
(for quantitation) or 135V (for identification), nebulizing gas (nitrogen); lOLimin. For the laser-spray<br />
ionization, a 10 W infrared laser was used.<br />
Results: All aconitine alka:Ioids and IS are completely separated on chromatogram. In human plasma samples,<br />
the calibration curves gave good linearity in the range <strong>of</strong> 5 and 300 ng/mL in all the compounds; their<br />
detection limits were about 0.3 to 1 ng/mL. Their limits for identification were about 0.7 to 2 ng/mL. The<br />
intraday CV values were less than 21 % for 200 ng/mL. In the laser-spray ionization, the ion current<br />
intensity was about 5 times higher compared to that by electron-spray ionization.<br />
Conclusion: The calibration curves gave good linearity in the range <strong>of</strong> 5 and 300 ng/mL; aconitine alkaloids<br />
can be sufficiently detectable at toxic concentrations. Thus this method is useful for quantitation and<br />
identification <strong>of</strong> aconitine alkaloids. Laser spray ionization could be also applied to identify trace amounts<br />
<strong>of</strong> aconitine alkaloids.<br />
Keywords: Aconitine, Mass spectrometry, Laser spray<br />
Page 173
A60 <br />
THE DETERMINATION OF ETHYL GLUCURONIDE IN URINE USING REVERSED-PHASE<br />
HPLC AND PULSED ELECTROCHEMICAL DETECTION<br />
Romina Kaushik*, Barry Levine and William R. LaCourse<br />
University <strong>of</strong>Maryland, Baltimore, Maryland, USA<br />
There is a need for a method to distinguish between ethanol levels detected in biological matrices due to<br />
alcohol consumption versus ethanol production after death as a result <strong>of</strong> decomposition. Ethyl glucuronide<br />
(EtG) is a non-volatile, water-soluble, direct metabolite <strong>of</strong> ethanol that can serve as a biological marker <strong>of</strong><br />
alcohol consumption. This metabolite can be a marker <strong>of</strong> acute alcohol consumption even at low levels<br />
unlike traditional biomarkers. It is an intermediate marker <strong>of</strong> alcohol consumption, bridging the gap<br />
between long-term (COT, MCV & GGT) and very short-term (ethanol & HTOL) biomarkers. EtG is a<br />
highly sensitive and specific alcohol consumption marker that can be detected for up to 80 hours after<br />
complete alcohol elimination from the body. This has very important clinical and forensic applications.<br />
Clinical applications for this biological marker would include monitoring patients in treatment for alcohol<br />
abuse. This marker could improve therapy outcome and quality <strong>of</strong> life in patients by preventing relapse<br />
episodes. Furthermore monitoring would increase safety in the workplace and prevent traffic accidents.<br />
Finally, fetal alcohol syndrome could be avoided by detecting and monitoring EtG in the mother which<br />
would reduce costs by making therapy more effective. In addition, the metabolite exhibits very high storage<br />
stability which is important as forensic samples are <strong>of</strong>ten stored for extended periods <strong>of</strong> time. Sometimes<br />
samples are not analyzed until the case goes to court which could take months or years. In previous studies<br />
there have been various methods used to detect EtG. These include gas chromatography (GC) coupled with<br />
mass spectrometry (MS), and liquid chromatography (LC) coupled with MS. GC/MS is available at almost<br />
all forensic facilities at a moderate cost. However, GC·MS detection <strong>of</strong> this metabolite requires prior<br />
derivatization. LC/MS is advantageous because it doesn't require derivatization nonetheless it is an<br />
expensive technique. For widespread use <strong>of</strong> EtG as a marker, simpler and less expensive methods are<br />
necessary.<br />
The current study involved developing a method for the detection <strong>of</strong> EtG in postmortem urine samples<br />
using reversed-phase liquid chromatography with pulsed electrochemical detection. Methyl glucuronide<br />
served as the internal standard. The mobile phase consisted <strong>of</strong> 1% acetic acid/water and acetonitrile (98:2),<br />
with a 600mM sodium hydroxide post-column system attached to enable pulsed electrochemical detection<br />
(PED). This amperometric detection technique applies alternated positive and negative potential pulses at a<br />
noble metal electrode. The analyte is oxidized followed by oxidative and reductive cleaning steps. The<br />
analyte concentration is determined by measuring the electric current resulting from the molecule gaining<br />
or losing electrons. In order to separate EtG from the biological matrix a solid-phase extraction (SPE) was<br />
used using aminopropyl columns. EtG was found to have a retention time <strong>of</strong> 5.3 minutes with LOQ and<br />
LOD values <strong>of</strong> 0.4 and 0.1 uglmL respectively. The extraction recovery following SPE was approximately<br />
50%. This method is specific, reproducible and sensitive. Reversed-phase chromatography enabled a<br />
simple separation <strong>of</strong> the analyte without requiring the ion-pairing reagents typically associated with ion<br />
chromatography. PED is a direct (no derivatization) and affordable detection method. This method is a<br />
potential tool to clinical and forensic toxicologists for determining alcohol consumption in live and<br />
deceased individuals.<br />
Keywords: Alcohol, Biomarker, Direct and affordable analysis<br />
Page 174
A61 <br />
SIMULTANEOUS ANALYSIS FOR PSYCHOTROPIC TRYPTAMINES AND<br />
PHENETHYLAMINES USING GC-MS AND LC-ESI-MS<br />
R. Kikura-Hanajiri*, M. Hayashi, K. Saisho, Y. Goda<br />
National Institute <strong>of</strong> Health Sciences, 1-18-1, Kamiyoga, Setagaya-ku, Tokyo 158-8501, Japan<br />
Many analogs <strong>of</strong>try pta mines and phenethylamines are hallucinogenic substances that exist naturally in some<br />
plants, fungi and animals, but can also be produced synthetically. Some <strong>of</strong> these drugs are strictly controlled<br />
by the Narcotics and Psychotrophics Control Law in Japan but many non-controlled analogs have been<br />
widely distributed as easily available psychotropic substances, especially via the Internet.<br />
To investigate the trend <strong>of</strong> these non-controlled drugs <strong>of</strong> abuse, simultaneous analytical methods were<br />
developed using GC-MS and LC-ESI-MS for 9 tryptamines/carbolines (AMT, 5-MeO-AMT, 5-MeO-DMT,<br />
5-MeO-DIPT, 4-0H-DIPT, 4-acetoxy-DIPT, bufotenine, harmine and harmaline), 5 phenethylamines (2C-I,<br />
2C-T-2, 2C-T-4 and 2C-T-7, including MBDB) <strong>of</strong> typically non-controlled substances in Japan, and,<br />
additionally, 4lega\ly controlled tryptamines and phenethylamines originally found in fungi or plants (DMT,<br />
Psylocin, Psylocybin and mescaline). Moreover, the proposed methods were applied to analyses <strong>of</strong> these<br />
drugs in 99 products (purchased at video shops or via the Internet over the past 2 years in Japan), which<br />
advertised psychotrophic/psychoactive effects.<br />
The samples (powder, tablets or liquid) were extracted with methanol under ultrasonication. After<br />
centrifugation, the extracts were filtered thorough a 0.45-0m membrane filter prior to the injection. GC-MS<br />
analysis was performed within 30 minutes using a DB-5MS capillary column (0.25 mm i.d. x 30 m, 0.25 Om<br />
film thickness). Regarding the LC-ESI-MS analysis, the separation <strong>of</strong> the target drugs was optimized on an<br />
ODS column (Atlantis dC18, 2.1 x 150 mm, 5 Om) in an acetonitrile-IOmM ammonium formate buffer (pH<br />
3.0) by a linear gradient program and a quantitative analysis was carried out by the monitoring <strong>of</strong> each<br />
[M+Ht in the positive ion mode <strong>of</strong>ESI-MS.<br />
As a result <strong>of</strong>the analyses using GC-MS and LC-ESI-MS, 5-MeO-DIPT (the synthetic substance known by<br />
the street name "Foxy") was found in 7 out <strong>of</strong>the 99 products except the products sold as "chemical reagents",<br />
and AMT, 5-MeO-DMT and harmine were also found in some <strong>of</strong> the 99 products. These analytical methods<br />
will be useful for the investigation <strong>of</strong> the distribution <strong>of</strong> the non-controlled psychotropic tryptamines and<br />
phenethylamines in the market.<br />
Keywords; Tryptamines, Phenethylamines, Non-controlled psychotropic substances<br />
Page 175
A62 <br />
A FULLY AUTOMATED METHOD FOR THE SCREENING OF BASIS DRUGS IN WHOLE<br />
BLOOD THROUGH ON LINE SPE-HPLC-DAD<br />
Rafael Linden* <br />
Instituto Geral de Pericias, Porto Alegre, RS, Brazil; Centro Universitario Feevale, Novo Hamburgo, RS, <br />
Brazil <br />
One <strong>of</strong> the major tasks in forensic toxicology laboratories, especially those with high workloads, is to<br />
provide adequate drug screening analysis in a limited amount <strong>of</strong> time. The purpose <strong>of</strong> this work was to<br />
develop a screening method, with reasonable discrimination capabilities, that could work unattended, using<br />
an aumomated device for solid phase extraction (SPE) coupled to a HPLC-DAD. Postmortem blood<br />
samples, (free <strong>of</strong> drugs) were spiked with cocaine, benzoylecgonine, lignocaine, diazepam, nordazepam,<br />
fluoxetine and sertraJine, until final concentrations <strong>of</strong> 500 nglmL were achieved. The whole blood samples<br />
were sonicated, than diluted from 3.5 to 7 mL with carbonate buffer (pH 9.3). The diluted samples were<br />
centrifuged and the supemadant was used for SPE. The extraction was performed in an Aspec® system,<br />
using Speed® C18 200mg cartridges, with the following steps: conditioning with 2 mL <strong>of</strong> methanol and 2<br />
mL <strong>of</strong> carbonate buffer pH 9.3, loading <strong>of</strong> 6.5 mL <strong>of</strong> diluted samples, washing with 2 mL <strong>of</strong> 9: 1 carbonate<br />
buffer:acetonitrile and eluting with 1 mL <strong>of</strong> 9: I acetonitrile:phosphate buffer pH 2.3. The solvents flows<br />
and air pushes were optimized. The eluate was injected on line in the HPLC, using a 100 ilL loop. For the<br />
hplc analysis, a C8 column, 25cm x 4.6 mm, was used in isocratic mode, with a mobile phase composed <strong>of</strong><br />
phosphate buffer and acetonitrile (63:37). The identification <strong>of</strong> the drugs was made based on their relative<br />
retention times to imipramine (I.S.) and on a spectral library. Recoveries above 80% were obtained for all<br />
drugs tested, with extracts sufficiently clean for hplc-dad identification. The method is now being<br />
expanded to a bigger number <strong>of</strong> drugs, including a acidic fraction.<br />
Key words: Solid phase extraction, Drug screening, HPLC-DAD<br />
Page 176
A63<br />
SOLID-PHASE MICROEXTRACTION BASED APPROACH FOR ENANTIOMERIC ANALYSIS<br />
OF AMPHETAMINES<br />
3<br />
Sheng-Meng Wang J ,2 and Ray H. LiU 2 . ,4 •• , ICentral Police University, Taoyuan, Taiwan. 2Toxicology and<br />
Accident Research Laboratory, FAA Civil Aerospace Medical Institute, Oklahoma City, OK, U.S.A.<br />
3Department <strong>of</strong> Medical Technology, Fooyin University, Kaohsiung Hsien, Taiwan. 4Department <strong>of</strong> Justice<br />
Sciences, University <strong>of</strong>Alabama at Birmingham, Birmingham,AL, U.S.A.<br />
As a solventless approach and with recent advances in the fiber manufacturing technology, solid-phase<br />
micro extraction (SPME) is now widely studied for its effectiveness for the pretreatment <strong>of</strong>various categories<br />
<strong>of</strong> samples. This study explores a novel SPME approach for enantiomeric analysis <strong>of</strong> amphetamines, in<br />
which absorption and derivatization are accomplished in one step. Specifically,<br />
(S)-(-)-N-(Trifluoroacetyl)-prolyl chloride was adapted as the chiral derivatizing reagent and added directly<br />
into the sample matrix. Analytical parameters, such as temperature, absorption/desorption duration, and the<br />
amount <strong>of</strong> derivatizing reagent, were studied to determine their effects on the yields <strong>of</strong> analytes on the fiber.<br />
The derivatization products resulting from this study show excellent desorption characteristics on the<br />
polydimethylsiloxane-coated fiber adapted for this study. For example, a one-time 5-min desorption leaves<br />
no detectable carry-over. Optimal operational parameters (absorption: 70°C for 10 minutes; injection: 250°C<br />
for 5 minutes) cause minimal negative impact on the fiber, allowing repeated used <strong>of</strong> the fiber for more than<br />
30 times. This method was evaluated and proved to be effective in (a) quantitative determination <strong>of</strong> the<br />
enantiomeric pairs <strong>of</strong> amphetamine and methamphetamine, in terms <strong>of</strong> repeatability, linearity, and limits <strong>of</strong><br />
detection and quantitation; and (b) generating case-specimen data comparable to those derived from a<br />
conventional liquid-liquid extraction approach (Table I).<br />
/~,<br />
Table 1. Comparison <strong>of</strong> enantiomeric composition data resulting from two methods (one-step solventJess<br />
SPME vs. conventional two-step liquid-liquid extraction/derivatization)<br />
SPME (concentration in ~/mL) Li~id-liquiifconcentration in ng/mL) .<br />
Sample d-Methamp. : I-Methamp. -Amp. : I-Amp. d-Met amp .. 1- ethamp. d-Amp. .<br />
I-Amp.<br />
1 12,169 1,280 2,477 72 ]0,638 1,564 2,702 63<br />
2 1,821 219 1,010 42 1,427 146 976 32<br />
3 7,436 593 1,329 36 7,768 429 1,318 37<br />
4 13,845 1,960 2,581 94 11,753 1,233 2,545 67<br />
5 3,766 340 2,675 93 3,310 252 2,763 72<br />
6 10,745 1,254 3,324 92 9,931 1,315 2,973 79<br />
7 3,090 704 1,466 78 2,564 591 1,381 79<br />
8 2,482 5,863 580 403 2,010 6,317 482 538<br />
9 5,398 486 1,971 50 4,680 435 1,928 43<br />
10 6,667 608 2,376 84 5,649 543 2,230 66<br />
11 6,761 947 2,220 78 5,632 449 2,100 73<br />
12 8,600 972 1,308 90 6,276 950 1,276 58<br />
Keywords: Amphetamines, Enantiomer, GC-MS<br />
Page 177<br />
1
A64 <br />
GC-MS QUANTlTATlON OF CODEINE, MORPHINE, 6-ACETYLMORPHINE,<br />
HYDROCODONE, HYDROMORPHONE, OXYCODONE, AND OXYMORPHONE IN BLOOD<br />
Robert Meatherall' <br />
Department <strong>of</strong>Biochemistry, S1. Boniface General Hospital, 409 Tache Avenue, Winnipeg, Manitoba, <br />
Canada, R2H 2A6. <br />
A method is described for the simultaneous analysis <strong>of</strong> seven opiates - codeine, morphine, 6<br />
acetylmorphine, hydrocodone, hydromorphone, oxycodone and oxymorphone in blood samples by gas<br />
chromatography - mass spectrometry. One milliliter <strong>of</strong> blood is combined with an internal standard<br />
mixture containing 200 nanograms <strong>of</strong> each <strong>of</strong> the seven deuterated opiates. Two milliliters <strong>of</strong> acetonitrile<br />
are added to precipitate the proteins and cellular material. After centrifugation, the clear supernatant is<br />
removed and the acetonitrile is evaporated. The remaining aqueous portion is adjusted to pH 9 with<br />
sodium bicarbonate buffer from which the drugs are extracted into chlor<strong>of</strong>orm / trifluoroethanol (10: 1).<br />
The organic extractant is transferred and dried under nitrogen. The residue is reconstituted in dilute<br />
hydrochloric acid and washed consecutively with hexane, then chlor<strong>of</strong>orm. The purified aqueous portion is<br />
adjusted to pH 9 with bicarbonate buffer and the drugs are again extracted into chlor<strong>of</strong>orm /<br />
trifluoroethanol (10:1). The organic portion is removed from the aqueous fraction and dried under<br />
nitrogen. The residue is consecutively derivatized with methoxyamine, then propionic anhydride using<br />
pyridine as a catalyst. The ketone groups on hydrocodone, hydromorphone, oxycodone and oxymorphone<br />
are converted to methoximes. Hydroxyl groups present at the C-3 and C-6 positions <strong>of</strong> codeine, morphine,<br />
6-acetylmorphine, hydromorphone and oxymorphone are converted to their respective propionyl esters.<br />
After a post derivatization purification step, the extracts are analyzed by full scan gas chromatography <br />
mass spectrometry using electron impact ionization.<br />
The method is linear to at least 2000 ng/mL. Day-to-day precision (N 15) at 500 nglmL and 75 nglmL<br />
were less than 10% for all 7 targeted opiates. Extraction efficiencies at these two concentrations ranged<br />
from 50% to 68%. For each opiate, the limit <strong>of</strong> quantitatlon was 10 nglmL, while the limit <strong>of</strong> detection was<br />
2 ngimL.<br />
Keywords: Opiates, Blood, Mass Spectrometry<br />
Page 178
A65 <br />
A STUDY OF CROSS-REACTIVITY OF SELECTED ANIMAL PROTEINS ON AN ENZYME<br />
LINKED IMMUNOASSAY FOR RECOMBINANT HUMAN ERYTHROPOIETIN<br />
Richard Stripp' and Lillian Guia<br />
John Jay College <strong>of</strong> Criminal Justice, The City University <strong>of</strong>New York, New York, NY, USA<br />
The FDA approved recombinant human erythropoietin, otherwise known as rhuEPO, for human use in<br />
1991. Recombinant human erythropoietin was created for patients with anemia to boost red blood cell<br />
production, termed erythropoiesis. Alleged abuse due to availability during clinical trials has been reported<br />
as early as 1987 in human athletes. Administration <strong>of</strong> rhuEPO to a healthy patient is similar to blood<br />
doping or training at high altitudes. It increases the level <strong>of</strong> circulating erythrocytes, increasing the oxygen<br />
carrying capacity <strong>of</strong> the blood to reduce fatigue in the athlete competing in endurance sports. This abuse,<br />
not limited to human athletes, has been reported in horseracing as well. The unique characteristic <strong>of</strong><br />
administration <strong>of</strong>rhuEPO to the equine athlete results in an immune reaction to the drug. This results in an<br />
autoimmune reaction to the horse's intrinsic erythropoietin, causing severe anemia and in some cases death.<br />
These reactions create antibodies detectable in an enzyme-linked immunoassay (ELISA). Questions have<br />
been proposed as to the specificity <strong>of</strong> this assay to react only to the anti- rhuEPO, and not to other intrinsic<br />
proteins in equine serum. In order to ensure the assay is detecting only the horse's antibody to rhuEPO, we<br />
have tested the assay against various immunoglobulins and sera from equine and other sources. Reactions<br />
from all <strong>of</strong> the 19G's and sera tested and potential cross reactivity between the ELISA rhuEPO plate and<br />
serum proteins in animals are presented.<br />
Keywords: rhuEPO, Blood doping, ELISA<br />
Page 179
A66 <br />
DETERMINATION OF SODIUM AZIDE IN BODY FLUIDS AND BEVERAGES BY ION<br />
CHROMATOGRAPHY<br />
Yukari Hirata', \ Saori Ishida l , Hitoshi Tsuchihashi 2 , Makoto Hamajima l , Kanako Watanabe 3 , Hiroshi<br />
Seno 4 , Rina Kaneko I,Akira Ishii!, IDepartment <strong>of</strong> LegaJ Medicine, Fujita Health University School <strong>of</strong><br />
Medicine, Japan, 2<strong>Forensic</strong> Science Laboratory, Osaka Prefectural Police Headquarters, Japan, 3Department<br />
<strong>of</strong>Legal Medicine, Hamamatsu University School <strong>of</strong> Medicine, Japan, 4Department <strong>of</strong> Legal Medicine,<br />
Aichi Medical University, Japan<br />
Background: Sodium azide, which is widely used as a bactericide in protein samples in clinical or research<br />
laboratories, is highly toxic. Actually, its oral LD50 value is estimated to be 45 mg/kg, which is only 5<br />
times greater than that potassium cyanide. In 1998, several mass poisoning cases with sodium azide<br />
occurred in Japan. It was then regulated as a poison by the Poisonous and Deleterious Substances Control<br />
Law. It is thus important to determine azide in body fluids and beverages with high sensitivity. We have<br />
succeeded in determining azide in different materials by ion chromatography.<br />
Methods: Azide ion in various samples was extracted using a Conway microdiffusion cell. Hydrazoic acid<br />
was vaporized from 1 mL sample (plasma or beverages) by adding 1 mL <strong>of</strong> 5% sulfuric acid in the outer<br />
groove, and absorbed in 250 ~L <strong>of</strong> 0.1 M NaOH solution in the central round basin. After the cell was<br />
incubated at 37°C for 30 min, a 20-j..tL aliquot <strong>of</strong> 0.1 M NaOH was injected to an ion chromatography<br />
system equipped with a suppressor and a conductivity detector (Dionex DX 500 system). The guard and<br />
separation columns used were a Dionex AG15 (50 x 2 mm Ld.) and an AS 15 (250 x 2 mm Ld.) column.<br />
The mobile phase was 38 mM NaOH and the flow rate was set at 0.4 mLimin.<br />
Results: The retention time <strong>of</strong> azide ion was about 10 min. In human plasma samples, the calibration curve<br />
gave good linearity in the range <strong>of</strong> 50 ng/mL and 10 ~g/mL; its detection limit was about 30 ng/mL. The<br />
intraday and interday CV values for 5 ~g/mL plasma were 2.8 and 8.8 %, respectively. We have tried<br />
several internal standards, but the use <strong>of</strong> an internal standard did not improve the reproducibility in<br />
quantitation <strong>of</strong> azide. Also, similar experiments were performed in different beverage samples spiked with<br />
sodium azide. It gave good linearity in the range <strong>of</strong> 50 ng/mL and 5 llg/mL; its detection limit was about<br />
10 ng/mL.<br />
Conclusion: Combination <strong>of</strong> the microdiffusion method and a semi-microcolumn has enabled the detection<br />
<strong>of</strong> azide with 3 to 4 times higher sensitivity compared to the methods previously reported. Thus, the<br />
present method can be applicable for clinical and forensic toxicology, because <strong>of</strong> its simplicity and<br />
sensitivity .<br />
Keywords: Azide, Ion chromatography, Microdiffusion method<br />
Page 180
A67 <br />
A GENERAL SCREENING AND CONFIRMATION APPROACH TO THE ANALYSIS OF<br />
DESIGNER TRYPTAMINES AND PHENETHYLAMINES IN BLOOD AND URINE USING<br />
GCIEI-MS AND HPLCIELECTROSPRA Y -MS<br />
Shawn P. Vorce*, Jason H. Sklerov, Office <strong>of</strong>the Armed Forces Medical Examiner, Division <strong>of</strong> <strong>Forensic</strong><br />
Toxicology, Armed Forces Institute <strong>of</strong>Pathology, 1413 Research Boulevard, Building 102, Rockville,<br />
Maryland 20850-3125<br />
Recent additions <strong>of</strong> designer tryptamines and phenethylamines to the Drug Enforcement Administration's<br />
list <strong>of</strong> controlled substances necessitate analytical procedures for their detection and quantitation. As<br />
specific immunoassays are not currently available and cross-reactivities with existing assays are unknown,<br />
a screening method based on gas chromatography mass spectrometry was developed. The method was<br />
capable <strong>of</strong> measuring the pentafluoropropionic derivative <strong>of</strong> a-methyltryptamine (AMT), N,Ndimethyltryptamine<br />
(DMT), 4-bromo-2, 5-dimethoxy-~-phenethylamine (2CB), N, N-dipropyltryptamine<br />
(DPT), 2,5-dimethyl-4-N-propylthio-~-phenethylamine (2C-T-7), and 5-methoxy-N, N<br />
diisopropyltryptamine (5-Me-DiPT). Separation was optimized to allow tentative identification <strong>of</strong><br />
metabolites, which display common electron impact ionization fragmentation patterns. The screening<br />
method gave limits <strong>of</strong> detection between 5-10 ng/mL and demonstrated linearity between 50-1000 nglmL.<br />
The method was successfully applied to blood and urine samples in suspected AMT intoxications.<br />
Confirmation <strong>of</strong> 5-Me-DiPT in one <strong>of</strong> the subjects' urine was achieved using liquid chromatography/mass<br />
spectrometry (LCIMS). Quantitation by selected ion monitoring (SIM) yielded a urinary concentration <strong>of</strong><br />
229 nglmL. The method was linear from 25 - 1500 ng/mL with a correlation coefficient <strong>of</strong> 0.995. The<br />
limit <strong>of</strong> detection was 5 nglmL in urine on the LCIMS. Two additional peaks were observed and presumed<br />
to be metabolic products reported previously as 5-methoxy-N-isopropyltryptamine and 5-methoxy-N, N<br />
diisopropyltryptamine-N' -oxide.<br />
Keywords: Tryptamine, Phenethylamines, HPLClES-MS<br />
Page 181
A68 <br />
MULTI TARGET SCREENING (MTS) FOR 300 DRUGS USING A LINEAR ION TRAP MASS<br />
SPECTROMETER AND LIBRARY SEARCHING<br />
Wolfgang Weinmann', I, Claudia A. MUller l , Barbora Maralikova I, Andre Schreiber 2 , Merja Gergov 3 ,<br />
[Institute <strong>of</strong> <strong>Forensic</strong> Medicine, University Hospital, AlbertstraBe 9, D 79104 Freiburg (Germany), Phone:<br />
++497612036828, Fax: ++49 7612036858, Email: Weinmann@ukl.uni-freiburg.de, 2Applied<br />
Biosystems; Frankfurter StraBe 129B; 64293 Darmstadt (Germany), 3University <strong>of</strong> Helsinki; Department <strong>of</strong><br />
<strong>Forensic</strong> Medicine; P.P, Box 40; 00014 Helsinki (Finland)<br />
A Multi Target Screening (MTS) procedure for drugs in blood and urine for toxicological analysis has been<br />
developed for the rapid detection and identification <strong>of</strong> tranquilizers (benzodiazepines), hypnotics, drugs <strong>of</strong><br />
abuse (opiates, cocaine, amphetamines, cannabinoids), antidepressants, neuroleptics, and cardiac drugs<br />
using LC/MSIMS with a linear ion trap-based tandem-mass spectrometer. In comparison to common<br />
GC/MS or LC/MSIMS methods used for target analysis, the combination <strong>of</strong> Multiple Reaction Monitoring<br />
(MRM) and Enhanced Product Ion (EPI) scan in an Information Dependent Acquisition (IDA) experiment<br />
with library searching <strong>of</strong>fers both sensitive target analyte detection and subsequent identification by a mass<br />
spectrometric database in a single LC/MS/MS run. Liquid-Liquid Extraction or Solid Phase Extraction has<br />
been used for sample clean up. Reversed-phase gradient LC with run-time <strong>of</strong> 30 minutes and MS/MS<br />
analysis have been performed in MRM using a Q TRApTM LC/MSIMS system with a TurboIonSpray®<br />
source. Similar to previous work <strong>of</strong>Gergov et at. [1] and in contrast to a method presented by Marquet et<br />
at. [2] , who used scan-mode for the survey scan - in the presented method 300 MRM-transitions have<br />
been monitored with short dwell times <strong>of</strong> 5 milliseconds each as survey scan <strong>of</strong> the IDA experiment. In<br />
case <strong>of</strong> a positive detection <strong>of</strong> an MRM transition, an EPI scan <strong>of</strong> the precursor ion was triggered as<br />
dependent scan, yielding product ion mass spectra at three pre-selected collision energies with the high<br />
sensitivity <strong>of</strong> the linear ion trap. Obtained EPI spectra were then searched against a newly created product<br />
ion spectral library, Fit, Reverse fit and Purity fit values are given as results in a library search hit list. A<br />
ready-to-use acquisition method and mass spectral library with Enhanced Product Ion spectra <strong>of</strong> 300<br />
compounds is presented. The developed method was successfully applied to samples <strong>of</strong> forensic cases,<br />
Dynamic exclusion <strong>of</strong> detected MRM transitions was used to detect co-eluting compounds. This was<br />
especially important for intoxication cases, where concentrations are usually 10 to more than 100 times<br />
higher than normal therapeutic concentrations. Examples <strong>of</strong> library searching with identification based on<br />
fit and purity fit values are given for amitriptyline (at CE <strong>of</strong> 35eV) and dibenzepine (CE <strong>of</strong> 50eV) and<br />
others. Purity fit values above 0.9 were obtained for all cases. The results were confirmed by established<br />
chromatographic screening methods, The developed method showed high sensitivity and selectivity. A<br />
further advantage <strong>of</strong> this method in contrast to the published method <strong>of</strong> Gergov at al. [1] is that the sample<br />
has to be injected only once, so less time is needed for the analysis. Conclusions: The developed method is<br />
useful for the rapid detection and identification <strong>of</strong> 300 pre-selected target compounds in blood extracts <strong>of</strong><br />
forensic and clinical cases using ESI or APCI. After introduction <strong>of</strong> retention time windows ("periods")<br />
with each containing up to 300 compounds the number <strong>of</strong> target analytes can even be increased to more<br />
than 1000 compounds per analysis.<br />
l. Gergov M, Ojanpera I, Vuori E. Simultaneous screening for 238 drugs in blood by liquid<br />
chromatography-ion spray tandem mass spectrometry with multiple-reaction monitoring. J<br />
Chromatogr B 2003,795, 41 - 53.<br />
2. Marquet P, Saint-Marcoux F, Gamble TN, Leblanc J C. Comparison <strong>of</strong> a preliminary procedure<br />
for the general unknown screening <strong>of</strong> drug and toxic compounds using a quadrupole linear iontrap<br />
mass spectrometer with a liquid chromatography - mass spectrometry reference technique. J<br />
Chromatogr B 2003,798,9 18<br />
Keywords: Multi target screening, LC-MS/MS library, Information dependent acquisition<br />
Page 182
A69 <br />
FORENSIC DRUG ANALYSIS WITHOUT PRIMARY REFERENCE STANDARDS<br />
Ilkka Ojanpera*, Suvi Laks, Anna Pelander, and Erkki Vuori<br />
Department <strong>of</strong> <strong>Forensic</strong> Medicine, P.O. Box 40, FlN-00014 University <strong>of</strong> Helsinki, Finland<br />
Previously, primary reference standards have been considered essential for substance identification and a<br />
prerequisite for quantitative analysis. However, standards for designer drugs, metabolites or rare substances<br />
cannot be obtained in a reasonable period <strong>of</strong> time to allow a prompt forensic investigation. This paper<br />
reports a new approach in forensic sciences to characterize drugs without the immediate need <strong>of</strong> primary<br />
reference standards.<br />
By liquid chromatography - time-<strong>of</strong>-flight mass spectrometry (LC-TOFMS) or Fourier transform mass<br />
spectrometry (LC-FTMS), it is possible to measure exact molecular masses on a routine basis. Especially<br />
benchtop LC-TOFMS instruments, being more cost-effective, are suitable for high-throughput work.<br />
Modern LC-TOFMS gives a high mass accuracy (approximately 5 ppm) and a moderately high mass<br />
resolution (5000-10000 FWHM). A target library consisting <strong>of</strong> exact monoisotopic masses for thousands <strong>of</strong><br />
drugs and metabolites can be created in-house to determine the elemental formulas <strong>of</strong> sample components.<br />
This kind <strong>of</strong> mass list is easily updated by typing recent data from the literature. Even complex biological<br />
samples can be analysed without complete chromatographic separation <strong>of</strong> the components.<br />
Chemiluminescence nitrogen detector (CLND) possesses an equimolar response to nitrogen, and<br />
consequently it provides a universal means for quantification <strong>of</strong> nitrogen containing compounds using a<br />
single secondary standard. As approximately 90% <strong>of</strong> drugs contain nitrogen, CLND is an attractive tool in<br />
forensic sciences. However, the technique has not been used in this area thus far.<br />
In this paper, various critical aspects <strong>of</strong> LC-TOFMS analysis are discussed. These include internal mass<br />
scale calibration, dynamic range, sensitivity, library search options, isotope pattern analysis, and utilization<br />
<strong>of</strong> urine metabolic patterns. CLND analysis is discussed in terms <strong>of</strong> sensitivity, linearity, equimolarity, and<br />
general performance. The merits <strong>of</strong> LC-TOFMS identification and CLND quantification are demonstrated<br />
in instances, where the availability <strong>of</strong> standards is a problem, such as in the analysis <strong>of</strong> street drugs and in<br />
the determination <strong>of</strong> a plasma parent drug/metabolite ratio.<br />
Keywords: Mass spectrometry, CLND, Drug analysis<br />
Page 183
A70 <br />
FAST SCREENING AND IDENTIFICATION OF DRUGS USING RETENTION TIME<br />
LOCKINGIRESUL TS SCREENER BY GC-MS<br />
Rosa E. De Jesus·, Robert A. Middleberg; National Medical Services, Willow Grove, PA 19090<br />
A major challenge for all forensic toxicology laboratories is to isolate, detect, identify and quantify the<br />
wide array <strong>of</strong> toxicants or drugs that may be present in a case where the cause <strong>of</strong> death is unknown. It is a<br />
challenge to screen, in a single analysis, hundreds <strong>of</strong> the most common toxicants that could be present.<br />
However, the use <strong>of</strong> a retention time locking process with GCIMS analysis affords this opportunity. This<br />
very powerful tool allows for the automated, rapid screening and identification <strong>of</strong> mUltiple analytes in just<br />
one injection. This tool combines the two key characteristics for the positive identification <strong>of</strong> a compound:<br />
retention time and mass spectra. After maintenance <strong>of</strong> the chromatographic system (Le. cutting or<br />
changing the column), the retention times <strong>of</strong> the analytes can drift, which makes the positive identification<br />
<strong>of</strong> analytes more time-consuming. Furthermore, although two or more instruments may be running under<br />
the same conditions, the retention times <strong>of</strong> those analytes may not be the same. However, when using<br />
retention time locking, the inlet pressure is adjusted and the methods are locked to that pressure, resulting<br />
in consistent retention times <strong>of</strong> all compounds from run to run. With the use <strong>of</strong> this technique the event<br />
times <strong>of</strong> the method will stay the same, allowing the comparison <strong>of</strong> real time data with previously acquired<br />
data. Also the chromatograms can be superimposed, leading to easy observation and comparison <strong>of</strong><br />
patterns. Retention time locking is used then in conjunction with a results screener, where a database is<br />
created for the locked methods. Results screener contains information <strong>of</strong> the target and qualifier ions <strong>of</strong>the<br />
analytes <strong>of</strong> interest, with their relative intensities, at their expected retention times. Therefore, every<br />
injection is made using a locked method containing a previously created database, and the system scans for<br />
the ions produced associated with an analyte in a window at its expected retention time. This allows for<br />
rapid identification <strong>of</strong> all compounds, including coeluting analytes. This detection and identification <strong>of</strong> the<br />
compounds in the sample, based on retention time and mass spectra, is achieved automatically in justa few<br />
seconds. The information obtained is then reviewed by the analyst and summarized in a customized report.<br />
Having no limits in the number <strong>of</strong> compounds that can be included in the database, retention time locking /<br />
results screener is a very powerful automated tool for the fast screening and identification <strong>of</strong> compounds in<br />
a sample. The use <strong>of</strong> this tool will be demonstrated as it is utilized for the routine analysis <strong>of</strong> toxicology<br />
samples.<br />
Keywords: Retention time locking; GC-MS drug screening; Drug identification<br />
Page 184
A71 <br />
USE OF STANDARD ADDITION/STANDARD DILUTION FOR QUANTITATION OF<br />
TOXICANTS IN UNUSUAL MATRICES<br />
Erica Horak', Robert Middleberg, National Medical Services, Willow Grove, PA 19090<br />
At the core <strong>of</strong> forensic toxicology is the desire to quantitate toxicants from a vast array <strong>of</strong> biological<br />
matrices. Often a forensic case involves unusual matrices, including decomposed or embalmed tissues,<br />
which present complexity to the sample preparation and analysis. Analyte recovery can be variable in these<br />
types <strong>of</strong> samples; therefore, alternate approaches to quantitation must be considered. One approach taken is<br />
to construct a matrix matched calibration curve. However, blank matrix is <strong>of</strong>ten not readily available, and<br />
particularly by the very nature <strong>of</strong> embalmed or decomposed tissues, a true matrix match does not exist.<br />
Furthermore, recoveries from the blank matrix and actual case samples may still differ. The standard<br />
addition/standard dilution (SASD) technique, on the other hand, accounts for variable percent recovery,<br />
matrix effects, and loss <strong>of</strong> sample, while the sample itself serves as its own quality control. The SASD<br />
technique can take any <strong>of</strong> several approaches. The simplest approach involves establishing a relationship<br />
between the responses <strong>of</strong> the analyte in the native sample (blank) with the response <strong>of</strong> the native sample<br />
with a known analyte concentration added (spike), without consideration <strong>of</strong> an internal standard in the<br />
event one is not available. A second approach includes the use <strong>of</strong> an internal standard, ideally an isotopic<br />
analog <strong>of</strong> the analyte, and establishing the relationship between the response ratios <strong>of</strong> both the blank and<br />
the spike (at one or more concentrations). In a third approach, the native sample is divided into four<br />
aliquots. One aliquot is left untreated and the others are either spiked with various analyte amounts or<br />
diluted. Each sample is then assayed through the analytical method. A plot <strong>of</strong> the response ratio data<br />
versus the amount <strong>of</strong> analyte added yields a line such that the extrapolated negative x-intercept is the<br />
concentration <strong>of</strong> the analyte in the native sample. In a final approach, three measurements can be made:<br />
that <strong>of</strong> the blank, the blank spiked at one or more analyte concentration, and the blank diluted by some<br />
factor. The use <strong>of</strong> a derived formula relates the relative responses, and spiked addition and dilution<br />
amounts, to the concentration <strong>of</strong> analyte in the native sample. In this presentation, the method <strong>of</strong> standard<br />
addition/standard dilution as an ideal approach to quantitation <strong>of</strong> drugs in complex and unusual matrix<br />
types will be demonstrated from actual forensic case data. Advantages and disadvantages <strong>of</strong> the technique<br />
will also be discussed.<br />
Keywords: Standard addition; Matrix; Quantitation<br />
Page 185
A72 <br />
COMPARISON OF CHEMICAL DERIVATIVES FOR SYSTEMATIC TOXICOLOGICAL<br />
ANALYSIS OF AUTOPSY BLOOD USING GAS CHROMATOGRAPHY MASS<br />
SPECTROMETRY<br />
Tareq AL-Ahmadi', R.A. Anderson <br />
<strong>Forensic</strong> Medicine and Science, University <strong>of</strong> Glasgow, Glasgow G12 8QQ, UK. <br />
Aims: Different derivatisation techniques have been developed for drug analysis in whole blood using GC<br />
MS. The method was validated for six drugs <strong>of</strong> abuse and their metabolites.<br />
Method: A mixed standard stock solution was prepared to give a final concentration <strong>of</strong> I Ilg/ml for each<br />
analyte and this was used to spike whole blood. Solid phase extraction (SPE) was carried out using the<br />
polymeric phase Phenomenex Strat-X (60 mg/3ml cartridges containing 331lm particles). Blank blood<br />
(lml) was mixed with internal standard solution and different concentrations <strong>of</strong> mixed standard stock<br />
solution, and phosphate buffer (pH 6, 3.5ml). This was centrifuged for to minutes and transferred to SPE<br />
columns. The extracts, in methanol, were evaporated to dryness and derivatised using three different<br />
methods: (a) acylation·esterification with PFPAI PFP-OH (2:1 vlv, 150 Ill); (b) acylation-methylation with<br />
PFPAI trimethylsilyldiazomethane (TMS) (5:1 v/v, 120 Ill); (c) silylation with MTBSTFA containing 1%<br />
TBDMSCI (30 Ill). Reaction vials were heated with a microwave oven for one minute. After<br />
derivatisation, vials for methods (a) and (b) were cooled to room temperature and evaporated to dryness<br />
under a stream <strong>of</strong> nitrogen. The derivatised extracts were reconstituted in 50111 <strong>of</strong> ethyl acetate prior to<br />
analysis by GC-MS. Extracts derivatised by method (c) were analysed directly. A Thermo-Finnigan Trace<br />
GC·MS instrument was used in selected ion monitoring (S1M) mode except method (c) which used full<br />
scan mode. The GC was equipped with an HP5 column (30m x 0.32 mm x 0.25Ilm) from J&W scientific<br />
and split/splitless injection port at 280°C. The oven temperature was at tOO°C for 2 min, programmed at<br />
12°C/min to 300°C. Ions monitored for quantitative analysis were as follows:<br />
Derivative Amp MA MOR BZE THC<br />
THC<br />
COOH<br />
PFPAIPFP·OH 118 204 414 82 417 459<br />
PFPAITMS 118 204 414 82 417 489<br />
MTBSTFA 158 172 341 282 371 515<br />
The method was subsequently applied to 35 forensic autopsy case samples.<br />
Results: Recoveries for all drugs <strong>of</strong> interest were found to be over 70%. Limits <strong>of</strong> detection (LOD) were<br />
calculated as 3 times the standard error <strong>of</strong> the regression line plus the intercept. LOD's in blood ranged<br />
from 0.4 ng/ml to 3.7 ng/ml with PFPA/PFP-OH, O.3ng/ml to 1.4ng/ml with PFPA/TMS and with<br />
MTBSTFA were from 1.9 ng/mJ to 7.3 ng/mt. Limits <strong>of</strong> quantification (LOQ) were calculated as to times<br />
the standard error. They were ::::::12.4 ng /ml with PFPAIPFP·OH, ::::::4.7 ng/ml with PFPAlTMS and ::::::19.8<br />
ng/ml with MTBSTF A <strong>of</strong> blood. The case samples analysed were found to contain various drugs <strong>of</strong> abuse<br />
and prescription drugs. The different derivatisation techniques gave varying results; however acylation·<br />
methylation gave the best sensitivity and chromatography.<br />
Conclusion: A validated, sensitive and specific method for the extraction and quantification <strong>of</strong> drugs abuse<br />
in blood is presented. An alternative derivatisation method (acylation-methylation) is proposed which<br />
gives better sensitivity and improved chromatography for detection and quantification <strong>of</strong> drugs <strong>of</strong> abuse<br />
compared to silylation or acylation alone.<br />
Keywords: Drugs <strong>of</strong> abuse, Derivatisation, GC-MS<br />
Page 186
A73 <br />
PREVALENCE OF GHB IN SUSPECTED DUI CASES IN MIAMI-DADE COUNTY, FLORIDA<br />
M. Elizabeth Zaney*, WiIJiam D. Gennaro, Gaudelio Saavedra, Bernard W. Steele, H. Chip Walls<br />
University <strong>of</strong> Miami School.<strong>of</strong> Medicine - <strong>Forensic</strong> Toxicology Laboratory<br />
According to numerous police and poison control center reports, GHBis a commonly abused substance in<br />
Miami-Dade County. Therefore, we wanted to study the prevalence <strong>of</strong> GHB in urine and blood samples<br />
submitted from suspected Driving Under the Influence (DUI) cases to the University <strong>of</strong> Miami, <strong>Forensic</strong><br />
Toxicology Laboratory.<br />
Ninety-one consecutive urine samples received from September-December 2003 (whether positive or<br />
negative for other drugs) were tested for GHB. In addition, a further 114 urine samples, and 74 blood<br />
samples which tested negative for alcohol were tested for GHB and other drugs. Urine samples were<br />
received and stored at 4 'c in containers without preservatives; blood samples were received and stored at<br />
4'C in gray top vacutainertubes with sodium fluoride as a preservative.<br />
A method taken from the Journal <strong>of</strong> Chromatography B, 792 (2003) 83-87 (Marion Villain, Vincent<br />
Cirimeie, Bertrand Ludes, Pascal Kint=*) was modified utilizing rapid protein precipitation and Iiquidliquid<br />
extraction using 40 microL <strong>of</strong> sample, 40 microL <strong>of</strong> deuterated internal standard, 90 microL <strong>of</strong> cold<br />
acetonitrile and high speed centrifugation. The supernatant was then carefully evaporated to dryness and<br />
the residue reconstituted with 70 microL <strong>of</strong> BSTF A + 1 % TMCS and heating at 70'C for 25 minutes to<br />
derivatize. Samples were analyzed by GCIMS with a Hewlett Packard Series 5890 GC coupled to an HP<br />
Series MSD run in SIM mode. A 5-point calibration curve ranging from 10 mgfL to 200 mg/L was used to<br />
determine the amount <strong>of</strong>GHB present in the specimen.<br />
Of the total 205 urine specimens tested, 5 tested positive for GHB (2.4% positive) with a concentration<br />
range <strong>of</strong>237 mg/L 2147 mg/L (mean 789 mgfL, median = 484 mgfL). The above 205 samples were<br />
made up <strong>of</strong>91 consecutive urines <strong>of</strong> which only 1 was positive for GHB (1.1% positive), and 114 samples<br />
selected by case history, <strong>of</strong> which 4 were positive for GHB (3.5% positive). 2 blood samples from the 74<br />
tested were positive for GHB (2.7% positive) with concentrations <strong>of</strong> 147 mgfL and 235 mg/L. A summary<br />
<strong>of</strong>the positive findings can be seen in the Table.<br />
Our findings would suggest that either GHB is not as prevalent as it is thought, or that users are so impaired<br />
that they don't attempt to drive a vehicle until metabolism and/or excretion have resulted in below<br />
detection limit samples, which may account for our low positivity rates. Of interest to note is the<br />
concurrent use <strong>of</strong>GHB and Methamphetamine.<br />
Case one Urine<br />
Case two Urine<br />
Case three Urine<br />
Case four Urine<br />
Case five Urine<br />
(These belong to the<br />
same defendant)<br />
Case five Blood<br />
Case six Blood<br />
GHB: 2147 mgfL<br />
Other drue:s present: Ibupr<strong>of</strong>en<br />
GHB: 609 mg/L<br />
Other dru2:s present: Amphetamine, Methamphetamine, Naoroxen<br />
GHB: 469 mg/L<br />
Other dru2:s Dresent: Amphetamine, Methamphetamine<br />
GHB: 237 mg/L<br />
Other drugs present: Amphetamine, Methamphetamine, MDMA, PPA,<br />
Pseudoephedrine, Dextromethorphan, Ecgonine methyl ester, Oxazepam,<br />
Alprazolam, Hydroxy-Alprazo!am<br />
GHB: 484 mg/L<br />
Other drugs present: Amphetamine, Methamphetamine<br />
GHB: 147 mg/L<br />
Other dru2:s Dresent: Acetone 0.003 g/IOOmL, presumptive positive Amp. class<br />
GHB: 235 mg/L<br />
Other dru2s present: Methamphetamine<br />
Keywords: GHB, GC/MS, DUI<br />
Page 187
A74 <br />
SEPARATION OF AMPHETATIME AND PIPERAZINE DESIGNER DRUGS BY CAPILLARY<br />
ELECTROPHORESIS<br />
Sandra C. Bishop" J, Bruce R. McCord], Samuel R. Gratz 2 , Jill R. Loelige~, Mark R. Witkowski 2<br />
IOhio University, Department <strong>of</strong> Chemistry and Biochemistry, Athens, OH, USA; 2U.S. Food and Drug<br />
Administration, <strong>Forensic</strong> Chemistry Center, Cincinnati, OH, USA<br />
The recent emergence <strong>of</strong> a new class <strong>of</strong> piperazine-type compounds has brought about the need· for laboratory<br />
screening methods for both seized drugs and toxicological samples. These piperazine compounds, which include 1<br />
benzylpiperazine (BZP) and 1-(3-trifluoromethylphenyl)piperazine (TFMPP), exhibit comparable physiological<br />
effects and can be substituted for the classic amphetamine-type drugs. We have optimized a chiral capillary<br />
electrophoresis (CE) separation that detects a set <strong>of</strong> 6 piperazine and 4 chiral amphetamine compounds in less than<br />
23 minutes using a 200 mM phosphate buffer at pH 2.8 with 20 mM hydroxypropyl-f3-cyclodextrin (HPf3CD). A<br />
liquid-liquid back extraction and a solid phase extraction (SPE) were developed for urine samples. The SPE used an<br />
altered version <strong>of</strong>the Varian Bond Elut Certify Amphetamines in Urine procedure. In addition to the above standard<br />
compounds, a series <strong>of</strong> "clandestine" BZP diHCl samples were also analyzed to assess the ruggedness <strong>of</strong> the<br />
method. One <strong>of</strong>the Internet synthetic methods yielded 1,4-dibenzylpiperazine, an unscheduled analog <strong>of</strong> I-BZP. All<br />
peak ratios were verified by LC-MS. The novel CE separation was tailored to simultaneously detect piperzine<br />
compounds in addition to amphetamine-like drugs. Since the reported effects <strong>of</strong> these two classes <strong>of</strong> drugs are<br />
strikingly similar, this method will greatly benefit laboratory analysis where the abused or seized substance is in<br />
question. Distinct migration time and UV -spectral data were obtained for all compounds <strong>of</strong> interest.<br />
Keywords: Piperazine, Amphetamine, CapiHary electrophoresis<br />
Page 188
A7S <br />
IDENTIFICATION AND ISOLATION OF FILAMENTOUS FUNGI IN SAMPLES OF<br />
CANNABIS SATIVA L.<br />
S.O.S. Cazenave', C. Darini, M.M.R.S. Soares<br />
Laboratorio de Toxicologia Forense de Campinas, Rua Barao de Parnaiba 322, 1. andar, Centro 13100-000<br />
Campinas, Sao Paulo (Brasil)<br />
Cannabis sativa L. (Marijuana) is considered an illegal drug being widely used mostly by young adults.<br />
The plant dried after harvesting and stored under favorable environment to grow fungi which is spread in<br />
nature. Since literature lacks studies related to filamentous fungi present in Cannabis sativa L... The<br />
objective <strong>of</strong> this study was to isolate and identify filamentous fungi in samples <strong>of</strong> Cannabis sativa L...<br />
retained in Campinas area and analyzed in The Laboratory <strong>of</strong> <strong>Forensic</strong> Toxicology. Sixty samples were<br />
used divided as follows: 30 samples with evident contamination and 30 without any traces <strong>of</strong><br />
contamination. First, 5 grams <strong>of</strong> sample were macerated in 50 ml <strong>of</strong> sterile distillated water to isolate the<br />
fungi. Next, samples were filtered and placed in sterile tubes. Volume transferred to sterile Petri dish was<br />
Iml with 15 ml <strong>of</strong> Sabouraud Dextrose Agar, subsequent homogenizing and after solidification it was<br />
incubated in room temperature for five days. If colony growth was found identification was carried out<br />
with macro and microscopy analysis. Most common species <strong>of</strong> fungi found were as follows: Aspergillus.<br />
Fusarium, Penicillium and Scapular/apsis. For this reason, Cannabis sativa L. represents a source <strong>of</strong> fungi<br />
contamination as fungi were found even in samples that were not visibly contaminated. These<br />
mycotoxigenic fungi might cause allergy in hypersensitive individuals, diseases in immune suppressed<br />
patients, or intoxication through ingestion <strong>of</strong> contaminated samples, therefore presenting a potential risk for<br />
users and toxicologists as well.<br />
Keywords: Fungi, Cannabis sativa, Contamination.<br />
Page 189
A76 <br />
LC-MSIMS IDENTIFICATION OF ETHYL SULFATE - ANOTHER DIRECT MARKER FOR<br />
RECENT ETHANOL INTAKE<br />
Sebastian Dresen*·I, Wolfgang Weinmann\ Friedrich M. Wurse <br />
IInstitute <strong>of</strong> <strong>Forensic</strong> Medicine, University Hospital Freiburg, Alberstr. 9, D 79104 Freiburg, Germany, <br />
Email: Weinmann@ukl.lIni-freibllrg.de; <br />
2Psychiatric University Hospital, Wilhelm Klein Str. 27, CH 4025 Basel, Switzerland, Email: <br />
friedrich. wurst@pukbasel.ch <br />
Besides ethyl glucuronide (EtG), fatty acid ethyl esters (FAEE) and others, one more direct ethanol<br />
metabolite - ethyl sulfate (EtS) - has been detected by LC-MSIMS in human urine samples. The structural <br />
characterization has been performed by LC-MS/MS using electrospray ionization with precursor-ion scan <br />
and product-ion scan techniques. After the synthesis <strong>of</strong> a deuterated analogue, the urinary excretion pr<strong>of</strong>ile <br />
has been investigated in samples obtained from volunteers up to 44 hours after drinking known amounts <strong>of</strong> <br />
alcohol ( 9 and 18 g, respectively). Ethyl sulfate was detectable up to 24 hours in urine, Le., 16 to 22 hours <br />
longer than ethanol could be detected with a headspace GCIFID method in urine. In summary, the urinary <br />
excretion pr<strong>of</strong>ile <strong>of</strong> EtSwas similar to that <strong>of</strong> ethyl glucuronide, which is characterized by longer <br />
detectability than ethanol in urine samples and therefore is a marker for ethanol consumption covering the <br />
time range <strong>of</strong> up to approximately three days after severe ethanol abuse. The results <strong>of</strong> structural <br />
characterization, way <strong>of</strong> synthesis <strong>of</strong> the deuterated analogue, method validation data including analyte <br />
stability in urine and stock solution are presented. EtS can be used for pro<strong>of</strong> <strong>of</strong> ethanol intake besides EtG. <br />
The presented method fulfills· forensic-toxicological guidelines for compound identification by <br />
chromatographic separation, use <strong>of</strong> deuterated internal standard, quantitation and identification with <br />
precursor and two product ions being monitored as target and qualifier ions. <br />
Key words: Ethyl sulfate, Direct ethanol marker, LC-MSIMS <br />
Page 190
A77 <br />
DETERMINING THE USE OF N1-ETHYL· GUANINE AS A BIOMARKER· FOR FATAL<br />
ALCOHOL SYNDROME<br />
Stacy L. Gelhaus', William R. LaCourse, Janine Cook, Katherine Squibb<br />
Department <strong>of</strong>Chemistry and Biochemistry, University <strong>of</strong> Maryland, Baltimore County, Baltimore,<br />
Maryland, USA<br />
Background: Fetal alcohol syndrome (FAS) and fetal alcohol spectrum disorders (FASD) represent the<br />
largest categories <strong>of</strong> preventable mental retardation syndromes and birth defects. It is theorized that<br />
ethanol's toxicity is in part mediated by damage to DNA. In DNA, ethanol's primary metabolite,<br />
acetaldehyde forms an N2-ethylguanine DNA adduct. The duration <strong>of</strong> this adduct, its affect on DNA<br />
replication, and its repair mechanism are currently unknown. A case study is presented to assess N 2 _<br />
ethylguanine as a potential alcohol biomarker with possible clinical utility in predicting the risk <strong>of</strong><br />
FASIFASD in infants born to alcohol-using women.<br />
Methods: The case subject was a 20 year old who reported binge drinking on hard alcohol for the first 5<br />
weeks <strong>of</strong> her pregnancy. The separation and quantification <strong>of</strong> N 2 -ethylguanine from unadducted<br />
nucleosides was performed by an in-house protocol. DNA was purified from whole blood using a<br />
commercial genomic DNA purification kit. The isolated DNA was completely hydrolyzed into monomer<br />
bases using established digestion procedures to liberate purine bases; recovery <strong>of</strong> the purine bases was<br />
>96%. The N 2 -ethylguanine DNA adduct was isolated and quantified by reversed phase HPLC with<br />
isocratic elution and UV/fluorescence detection. Bases were identified by retention time and by standard<br />
spiking. Base quantitation was by calibration curves <strong>of</strong>standard peak height signals.<br />
Results: The identification <strong>of</strong> N 2 -ethylguanine by HPLC was confirmed through standard spiking and<br />
LCIMS. HPLC precision for the N2-ethylguanine was 0.2% for peak area or 3.9% for peak height.<br />
Standard curve linearity was to 15 ~mol (r = 0.9999). Preliminary analytical sensitivity was 29 nmol<br />
(HPLC/uV detection), 2.9 nmol (HPLClfluorescence detection), and 20 fmol (LC/MS). No interference<br />
was found from free bases. The subject's N 2 -ethylguanine concentration determined by LCIMS at 20 weeks<br />
gestation was 11.7 pmol/mg DNA, which declined to 8.3 pmol/mg DNA by 30 weeks. Her adduct levels<br />
are higher than a comparison nonpregnant social drinker whose N 2 -ethylguanine concentration was 6.9<br />
pmol/mg. Reproducibility <strong>of</strong> these initial subject results is pending. The subject's fullterm daughter was in<br />
the 75th percentile for weight, 17th percentile for length and 10th percentile for head circumference, an<br />
indicator <strong>of</strong>FAS.<br />
Conclusions: Initial studies indicate the acceptability <strong>of</strong> this method for the separation and detection <strong>of</strong><br />
purines, including the N 2 -ethylguanine. Additional subject data is needed to confirm the adduct's clinical<br />
utility.<br />
Public Health implications: Clinical validation <strong>of</strong>N2-ethylguanine as a biomarker for alcohol damage will<br />
fortify the established panel <strong>of</strong> alcohol biomarkers, aiding in the identification <strong>of</strong> pregnancies at risk for<br />
FASIFASD and elucidation <strong>of</strong>the mechanisms <strong>of</strong> alcohol pathology.<br />
Keywords: DNA, Biomarker, FAS<br />
Page 191
A78 <br />
LCIMSIMS DETERMINATION OF LSD, ISO-LSD, AND THE MAIN METABOLITE 2-0XO-3<br />
HYDROXY-LSD IN WHOLE BLOOD AND URINE<br />
Sys Stybe Johansen* and Jytle Lundsby Jensen <br />
Department <strong>of</strong> <strong>Forensic</strong> Chemistry, Institute <strong>of</strong> <strong>Forensic</strong> Medicine, University <strong>of</strong> Copenhagen, <br />
Frederik V's vej 11, DK-2100 Copenhagen OE, Denmark. Phone +45-35326241. Fax: +45-35326085. E<br />
mail: SSJ@forensic.ku.dk <br />
Aim: To develop simple LC/MSIMS applications that identify, confirm and quantify rare potent drugs in<br />
forensic cases. An application with the very potent hallucinogenic drug LSD is shown.<br />
Method: A liquid chromatography mass spectrometric (LCIMSIMS) method has been developed for the<br />
determination <strong>of</strong> LSD in whole blood and urine. Furthermore, determination <strong>of</strong> the common LSD impurity<br />
iso-LSD (inactive) and the main metabolite 2-oxo-3-hydroxy-LSD were included. The procedure involved<br />
a simple liquid-liquid extraction <strong>of</strong> I g sample containing the analyte and LSD-D3 (internal standard) with<br />
butyl acetate at pH 9.8. After centrifugation, the organic fraction was removed and evaporated to dryness at<br />
40°C and reconstituted in 100 III mobile phase. A gradient LC system (HP 1100 system, Agilent tech.) with<br />
a Zorbax SB CI8 (30 x 2.lmm, 3.5 Ilm) was used to separate the analytes within 10 min. Identification,<br />
confirmation and quantification were done by positive electrospray ionisation with a triple quadrupole mass<br />
spectrometer (Quattro micro, Waters) operating in multiple reaction monitoring (MRM) mode. For each<br />
analyte two MRM's were set up, one for quantification and one as qualifier using one precursor ion and<br />
two product ions per analyte. The ratio between the responses <strong>of</strong> the two MRM's was used for<br />
identification purposes along with the retention time.<br />
Results: The curves <strong>of</strong> extracted whole blood standards were linear over a working range <strong>of</strong> 0.01 to 5.0<br />
Ilg/kg for LSD and iso-LSD <strong>of</strong> both transitions. The limit <strong>of</strong> quantification (LOQ) <strong>of</strong> LSD and iso-LSD was<br />
O.ot Ilglkg in whole blood, while LOQ <strong>of</strong> 2-oxo-3-hydroxy-LSD was 0.5 Ilglkg. The repeatability<br />
expressed by relative standard deviation (RSD) was better than 10% and the relative accuracy was between<br />
92-99% for LSD and 89-108% for iso-LSD, respectively. The ratio was determined for each analyte and a<br />
RSD <strong>of</strong> max. 10% was confirmed.<br />
The method was applied for a case investigation involving a 26-year-old man who admitted to have been<br />
abusing LSD. Blood concentrations <strong>of</strong> LSD and iso-LSD were determined to 0.27 Ilglkg and 0.44 Ilglkg. 2<br />
oxo-3-hydroxy-LSD was detected in the urine sample and confirmed the abuse <strong>of</strong> LSD. The case illustrated<br />
the importance <strong>of</strong> analyte separation before MRM detection <strong>of</strong> a sample. The chromatographic separation<br />
<strong>of</strong> LSD and iso-LSD were <strong>of</strong> importance because the diastereoisomers have identical fragmentation paths<br />
leading to fragments <strong>of</strong>equal m/z ratio.<br />
Conclusion: The method was proved to be suitable for forensic cases being simple, reproducible and<br />
selective. However, it was observed that monitoring typical fragments <strong>of</strong> LSD without chromatographic<br />
separation is inadequate. After the development <strong>of</strong> this LCIMSIMS method, the initial screening by RIA<br />
(radioimmunoassay) for LSD was cancelled because it was too time-consuming and expensive considering<br />
the low number <strong>of</strong> investigations/cases per year.<br />
Keywords: LSD, Whole blood, LC/MS/MS<br />
Page 192
A79 <br />
LC-MSIMS METHOD DEVELOPMENT FOR A PACLITAXEL ASSAY<br />
W. Lambert"' I, K. Mortier!, A. Verstraete 2 , and C. Van Peteghem 1 , I Laboratorium voor Toxicoiogie, Ghent<br />
University, Hareibekestraat 72, B-9000 Gent, Belgium, 2Afdeling Klinische Bioiogie, Ghent University<br />
Hospital, De Pintelaan 185, B-9000 Gent, Belgium<br />
The development <strong>of</strong> a method with liquid chromatography coupled to mass spectrometry (LC-MS) for the<br />
determination <strong>of</strong> the anticancer drug paclitaxel in plasma is described. The goal <strong>of</strong> the method is to produce<br />
accurate and reproducible data, in a sensitive assay. Therefore, factors that influence reproducibility are<br />
investigated. The method consisted <strong>of</strong> a basic Iiquidlliquid extraction <strong>of</strong> plasma with methyl-t-butyl ether.<br />
Subsequently, samples were analyzed using a standard narrow bore reversed phase column. MRM<br />
transitions <strong>of</strong> pac lit axel and the internal standard (cephalomannine) were monitored. Special attention was<br />
given to two typical electrospray phenomena: adduct formation and matrix effect. First <strong>of</strong> all, adduct<br />
formation was investigated. In the absence <strong>of</strong>additives like formic acid or ammonium acetate in the mobile<br />
phase, reproducibility <strong>of</strong> the LC-MS method was decreased, when samples <strong>of</strong> varying alkali metatcontent<br />
were analyzed. Already at a low concentration <strong>of</strong> additive in the mobile phase reproducibility increased to<br />
an acceptable level. Therefore, a small amount <strong>of</strong> additive was incorporated in the mobile phase. Different<br />
mobile phase additives were tested for optimum sensitivity and reproducibility. Secondly, matrix effect was<br />
examined, especially the influence <strong>of</strong> the vehicle used in the commercial formulation <strong>of</strong> paclitaxel (Taxo\):<br />
Cremophor EL. Ion suppression by formulation vehicles has been reported for e.g. polyethyleneglycol400.<br />
In view <strong>of</strong> the application <strong>of</strong> this method in a pharmacokinetic study with Taxol, investigation <strong>of</strong> the effect<br />
<strong>of</strong>Cremophor EL on the ionization was incorporated in the method development. When an isocratic LC run<br />
was used, ion suppression was noticed mainly as a result <strong>of</strong> carry-over to subsequent runs. Changing the<br />
mobile phase to a higher percentage <strong>of</strong> organic phase and incorporating a gradient step (column wash)<br />
resolved the matter. The strategy to evaluate and eliminate adduct formation as well as matrix effects can<br />
also be applied to LC-MS determinations <strong>of</strong> other compounds and in fact should become an essential part<br />
<strong>of</strong>a validation protocol.<br />
Keywords: Paclitaxel, Method development, LC-MS<br />
Page 193
A80 <br />
QUANTITATION OF PHENAZEPAM IN BLOOD BY GC-MS IN POSITIVE DRUG-DRIVING<br />
CASES IN FINLAND<br />
Sirpa Mykkanen*' I, Teemu Gunnar!, Kari Ariniemi 1 , Pirjo Lillsunde 1 , Raissa Krasnova 2<br />
lNational Public Health Institute, Laboratory <strong>of</strong> Substance Abuse, Helsinki, Finland<br />
2Bureau <strong>of</strong> <strong>Forensic</strong> Medicine <strong>of</strong> Moscow Region, Department <strong>of</strong> <strong>Forensic</strong> Chemistry, Moscow, Russia<br />
Phenazepam (1-bromo-5-( ortho-chloropheny 1)-2,3-dihydro-l H-l ,4-benzodiazepin-2-one) is white or white<br />
with cream-coloured crystal powder that is insoluble in water and slightly soluble in ethanoL After a single<br />
oral dose <strong>of</strong> 2 mg, the peak plasma concentrations <strong>of</strong> 8-15 ng/ml can be attained in 3-4 hours. Effective<br />
therapeutic concentration for persons with neurosis is in the range <strong>of</strong> 30-10 ng/ml. Phenazepam is<br />
comparable with lorazepam in respect <strong>of</strong> the dose and therapeutic action.<br />
Phenazepam is not medically used in Finland. However it is misused. Therefore, a reliable and rapid<br />
method for phenazepam analysis is necessary in Finland. In the present method the phenazepam was<br />
analyzed together with diazepam, midazolam, alprazolam, nordiazepam, oxazepam, temazepam,<br />
chlordiazepoxide, nitrazepam, bromazepam and lorazepam and their metabolites.<br />
The GC-MS procedure contained liquid-liquid extraction and derivatization by N-methyl-N-(Ierlbutyldimethylsilyl)trifluoroacetamide<br />
(MTBSTFA). Analysis was performed in selected ion monitoring<br />
(SIM) mode. The developed method was validated and the reliability <strong>of</strong> the developed method was tested<br />
on the basis <strong>of</strong> linearity, accuracy and precision. Phenazepam has been found among drivers suspected for<br />
driving under influence. Year 2003 there were 20 positive phenazepam cases and the concentrations found<br />
from Finnish drivers varied from 18 ng/ml to 400 nglml.<br />
Keywords: Phenazepam, GC-MS, Quantitation<br />
Page 194
A81 <br />
PHENMETRAZINE OR EPHEDRINE FOOLED BY LIBRARY SEARCH<br />
Sarah M. Wille*, Carlos H. Van Peteghem, Willy E. Lambert<br />
Laboratory <strong>of</strong> Toxicology, Ghent University, Harelbekestraat 72, B-9000 Gent, Belgium<br />
Phenmetrazine, a central nervous system stimulant, currently abused as an anorectic agent, was positively<br />
identified by library search after injecting a methanolic extract <strong>of</strong> an ephedrine containing powder using<br />
different GC-MS configurations. Phenmetrazine is a controlled substance as described in the UN<br />
Convention <strong>of</strong> Psychotropic Substances 1971, while ephedrine is used in over-the-counter medications as a<br />
vasoconstrictor. However, very recently, the Food and Drug Administration issued a final rule prohibiting<br />
the sale <strong>of</strong> dietary supplements containing ephedrine alkaloids because such supplements present a health<br />
risk.<br />
GC-MS analysis <strong>of</strong> a methanolic extract <strong>of</strong> the herbal product containing ephedrine resulted in a peak with<br />
a nearly identical retention time as ephedrine but identified as phenmetrazine after a library search. It is<br />
known that formaldehyde contamination in solvents such as methanol can result in conversion <strong>of</strong><br />
ephedrine-like compounds. Ephedrine reacts with formaldehyde to form 3, 4-dimethyl-5-phenyl-1, 3<br />
oxazolidine with a similar molecular weight as phenmetrazine (1). The fragmentation pattern is also<br />
similar because both chemical structures differ only in the position <strong>of</strong> one carbon unit. Thus, library<br />
searches alone can lead to erroneous conclusions. Experiments using a HP 7683 cold on-column- HP<br />
6890GC-HP 5973 MSD configuration and a split injector in combination with a 3400 Varian GC-Finnigan<br />
Magnum ion-trap MSD demonstrated that high injection temperatures influence the conversion speed. This<br />
was evidenced by injection <strong>of</strong> a freshly made ephedrine standard in methanol using injector temperatures<br />
from 60 up to 300°C.<br />
Attention should be paid to the possibility <strong>of</strong> chemical and/or thermal conversion <strong>of</strong> analytes in a sample<br />
and/or in the GC-injector, as this can lead to interpretation difficulties and erroneous identification <strong>of</strong><br />
analytes in a toxicological screening. As demonstrated by this case, ephedrine-containing samples are <strong>of</strong><br />
particular interest in view <strong>of</strong> the judicial implications.<br />
(I) Lewis RJ et aI., J. Foresic ScL, 45,898-901 (2000).<br />
Keywords: GC-MS, Ephedrine, Conversion.<br />
Page 195
A82 <br />
AN IDA MEDIATED LC-MSIMS SCREENING PROCEDURE WITH SEMI-QUANTITATIVE<br />
POTENTIAL<br />
Tineke N. Decaestecker l , Pierre E. Wallemacq2, Carlos H. Van Peteghem 3 , and Jan F. Van Bocxlaer" I<br />
1Laboratory <strong>of</strong> Medical Biochemistry and Clinical Analysis, Ghent University, Harelbekestraat 72, B-9000<br />
Ghent, Belgium, 2Laboratory <strong>of</strong> Toxicology and Special Chemistry, Clinical Hospital St.-Luc, Hippocrate<br />
Avenue, B-1200 Brussels, Belgium, lLaboratory <strong>of</strong> Toxicology, Ghent University, Harelbekestraat 72, B<br />
9000 Ghent, Belgium<br />
Systematic toxicological analysis (STA) in forensic toxicology comprises general unknown screening<br />
(GUS) procedures, whether or not restricted to well-defined subgroups, as well as specific confirmation and<br />
quantitation <strong>of</strong> individual compounds. Even though in some forensic cases, the substance involved is<br />
known or strongly suspected, the possibility that other toxic compounds may have contributed to the<br />
observed biological effect cannot be excluded. Efficient and extensive screening strategies are therefore<br />
indispensable. This study evaluated an IDA-mediated LC-MSIMS screening methodology, qualitatively as<br />
well as quantitatively, and shows its scope and limitations in a forensic setting. After all, an LC-MS<br />
screening strategy could on the one hand reduce the <strong>of</strong>f-line sample preparation mandatory in GC-MS,<br />
because relatively non-volatile compounds can be analyzed as such, and on the other hand increase the<br />
range <strong>of</strong> compounds amenable to MS. IDA is an artificial intelligence based product-ion scan mode<br />
providing automatic "on-the-fly" MS to MS/MS switching. This laboratory introduced in a preliminary<br />
communication, as first, the concept <strong>of</strong>IDA-based LC-MSIMS screening using a Q-TOFI. By performing<br />
information dependent scanning at two different fragmentation energies, two collision-induced dissociation<br />
(CID) spectra for each <strong>of</strong> the detected compounds are generated. As the MSIMS spectra derive from a<br />
single precursor ion, a very selective and very specific method was devised. Additionally, advance<br />
knowledge about the xenobiotics that could be responsible for a certain intoxication is not necessary.<br />
Limitation <strong>of</strong> the MSIMS acquisition time to an acceptable minimum resulted in an almost instant switch<br />
back to the MS mode. As such, this approach provided MS chromatograms that still could be <strong>of</strong> use for<br />
semi-quantitative purposes. Since former studies revealed that the IDA intensity threshold, unequivocally<br />
related to the background noise, seemed to be a critical parameter, the solid phase extraction procedure, the<br />
liquid chromatographic conditions and the mass spectrometric parameters all were optimized in advantage<br />
to IDA Optimization <strong>of</strong> the SPE procedure was performed by means <strong>of</strong> experimental design. Whole blood<br />
was preferred as biological matrix because <strong>of</strong> its relevant toxicological characteristics, although this did not<br />
facilitate the analysis since the drug concentration in whole blood are relatively low compared to urine<br />
samples. The influence <strong>of</strong> two different threshold values, Le. 100eV and 400eV, on the qualitative and<br />
quantitative results was examined. Finally, the screening procedure we developed was benchmarked on the<br />
one hand qualitatively against the results obtained from traditional GUS approaches in a number <strong>of</strong> routine<br />
toxicological laboratories (37 samples). To that end, immunochemical techniques (EMIT, RIA), HPLC<br />
DAD, GC-MS and GC-NPD techniques were applied to screen the whole blood samples. On the other hand<br />
the IDA-mediated screening strategy was compared semi-quantitatively against established LC-MSIMS<br />
methods (7 samples). From a qualitative point <strong>of</strong> view the procedure performed exceptionally well: when<br />
applying a threshold <strong>of</strong> 100eV, mostly all <strong>of</strong> the drugs detected by the conventional techniques were<br />
identified, as well as additional drugs that were not previously reported. The procedure proved well-suited<br />
for an initial semi-quantitative assessment, as is customary in e.g. forensic toxicology before accurate<br />
intoxication levels are determined using targeted analytical analysis.<br />
[l] Decaestecker et aI. Rapid Commun. Mass Spectrom. 2000, 14, 1787-1792.<br />
Keywords: LC-MSIMS, STA, IDA<br />
Page 196
A83 <br />
DETERMINA TION OF NALOXONE AND NORNALOXONE IN HUMAN PLASMA BY HIGH<br />
PERFORMANCE LIQUID CHROMATOGRAPHY - ELECTROSPRAY IONIZATION <br />
TANDEM MASS SPECTROMETRY<br />
Wenfang B. Fang' and David E. Moody, Center for Human Toxicology, Department <strong>of</strong> Pharmacology and<br />
Toxicology, University <strong>of</strong>Utah, Salt Lake City, UT 84112<br />
Naloxone is a jl-opioid antagonist that has been used clinically for over forty years mainly for the treatment<br />
<strong>of</strong> opioid overdose and to reverse narcotic-induced depression following surgery. A more recent<br />
application is the use <strong>of</strong> naloxone in a combination tablet containing buprenorphine at a fixed ratio <strong>of</strong> 4: I<br />
(buprenorphine: naloxone) for the treatment <strong>of</strong> opioid dependence. The purpose <strong>of</strong> the addition <strong>of</strong><br />
naloxone to buprenorphine tablet is to prevent diversion <strong>of</strong>buprenorphine for illicit Lv. use. ~ecause <strong>of</strong>the<br />
low doses <strong>of</strong> naloxone used in maintenance therapy, sensitive analytical methods are required. This has<br />
traditionally proven difficult for 6-keto nor-opiates such as nornaloxone. A highly sensitive method was<br />
developed to measure naloxone and its metabolite nornaloxone in human plasma to gain further knowledge<br />
about their metabolism and pharmacokinetics. drNaltrexone and d 3 -oxymorphone were used as internal<br />
standards for naloxone and nornaloxone. Preliminary experiments demonstrated that solid-phase extraction<br />
improved the recovery <strong>of</strong>norna lox one to 30% compared to 10% using liquid-liquid extraction. Solid-phase<br />
extraction was applied for sample preparation using C18 extraction columns and 0.01 M ammonium<br />
carbonate buffer (pH = 9). High performance liquid chromatography interfaced by electrospray ionization<br />
to a tandem mass spectrometric detector (HPLC-ESI-MSIMS) was used for quantitation. A XTerra MS<br />
CI8 3.5 Jlm 2.1x 50 mm column (Waters Corporation, Milford, MA) was used for separation. The mass<br />
spectrometer was a Finnigan model TSQ7000 Thermo Quest triple-stage quadrupole. Quadrupole 1 was<br />
set to pass only ions at m/z 328, 288, 345 and 305 that correspond to the MH+ ions <strong>of</strong> naloxone,<br />
nornaloxone and their internal standard d 3 -naltrexone and d 3 -oxymorphone. The MH+ ions were caused to<br />
undergo collision induced dissociation in quadrupole 2 that produced product ions at mlz 310, 270,327 and<br />
287 respectively, which were then monitored selectively by quadrupole 3. The calibration range was from<br />
0.075 to 20 ng/mL for naloxone and 1 to 20 ng/ml for nornaloxone with the calibration curve constructed as<br />
quadratic with llX weighting. The lower limit <strong>of</strong> quantitation (LLOQ) was determined at 0.075 ng/ml for<br />
naloxone and 1 ng/ml for nornaloxone. Specificity for naloxone and nornaloxone was determined from<br />
analysis <strong>of</strong> blank plasma fortified with internal standard only (3 replicates) and with LLOQ concentration<br />
(1 replicate) in six different lots <strong>of</strong> plasma. The primary evaluation was to compare the mean peak area<br />
ratio <strong>of</strong> any signal at the retention time <strong>of</strong> naloxone and nornaloxone to its internal standard for each lot<br />
with the mean peak area ratio <strong>of</strong> the six LLOQ samples. Mean ratios relative to mean LLOQ ranged from<br />
2.68 to 7.72 with a mean <strong>of</strong> 5.35% for naloxone and from 8.03 to 25.5 with a mean <strong>of</strong> 16.5% for<br />
nornaloxone. Intra-run accuracy <strong>of</strong> the LLOQ was within 5.1 % <strong>of</strong> target with intra-run precision within<br />
13.5% for naloxone and within 12% <strong>of</strong> target and with intra-ran precision within 7.4% for nornaloxone.<br />
(Supported by NIDA grant ROIDAIOIOO)<br />
Keywords: Naloxone, Nornaloxone, HPLC-ESI-MS/MS<br />
Page 197
A84 <br />
SIMULTANEOUS DETERMINATION OF BUPRENORPHINE. NORBUPRENORPHINE.<br />
BUPRENORPHINE-3-GLUCURONIDE AND NORBUPRENORPHINE-3-GLUCURONIDE IN<br />
HUMAN PLASMA AND URINE BY LIQUID CHROMATOGRAPHY ELECTROSPRA Y<br />
IONIZA TION TANDEM MASS SPECTROMETRY: APPLICATION TO HUMAN<br />
PHARMACOKINETICS<br />
Wei Huang" \ Elinore F.McCance-Katr and David E. Moodyl, lCenter for Human Toxicology,<br />
Department <strong>of</strong> Pharmacology and Toxicology, University <strong>of</strong> Utah, Salt Lake City, UT 84112 and 2Division<br />
<strong>of</strong> Addiction Psychiatry, Virginia Commonwealth University, Richmond, VA 23298<br />
Our previously described method for buprenorphine (BUP), norbuprenorphine (NBUP), buprenorphine-3<br />
glucuronide (BUPG) and norbuprenorphine-3-glucuronide (NBUPG) (<strong>SOFT</strong> 2003) has undergone a slight<br />
modification prior to full validation and use in a pharmacokinetics study. The monitored ions for NBUP<br />
and its internal standard d 3 -NBUP were changed from 101 (product ion) to 414 (parent ion) and 101 to 417,<br />
respectively. This provided stronger signals and a resultant lower limit <strong>of</strong> quantitation (LLOQ) <strong>of</strong> 0.1<br />
nglmL for NBUP.<br />
A full validation using human plasma with a cross-validation to human urine was conducted. The LLOQ<br />
was 0.1 ng/mL for all analytes in human plasma. For the urine samples, the LLOQ was 0.5 nglmL for<br />
BUP, BUPG and NBUPG and 2.5 ng/mL for NBUP due to interference in some urine samples. The intraassay<br />
precision, as coefficient <strong>of</strong> variation (%CV), at 0.1, 0.25, 25 and 40 ng/mL in plasma did not exceed<br />
17.5% at the LLOQ or 12.5% at all other concentrations for all analytes; in urine, the %CV did not exceed<br />
17.4% at the LLOQ or 13.3% at all other concentrations for all analytes. The intra-assay accuracy, as %<br />
deviation from target, in plasma did not exceed 12.3% at all concentrations for the four compounds; in<br />
urine the % deviation did not exceed 14% at all concentrations. The interassay precision and accuracy was<br />
determined at 0.25,25 and 40 ng/mL; %CV did not exceed 7.0% and the % deviation did not exceed 5.6%<br />
for the four analytes. The method has now been used to determine the pharmacokinetics <strong>of</strong> the four<br />
analytes in plasma and urine collected from five patients who had been maintained on a daily sublingual<br />
does <strong>of</strong> 16 mg buprenorphine for at least 21 days. Plasma was prepared from blood collected for 13 time<br />
points from just prior to 24 hours after the daily dose and urine collected for the same 24-hour period. The<br />
results were as follows:<br />
Pharmacokinetic parameter BUP NBUP BUPG NBUPG<br />
Plasma<br />
Cmax (ng)(mL)"1 4.47::1: 0.54 6.36::1: 1.84 7.19::1:3.27 21.5::1: 4.2<br />
Tmax(h) 0.85::1: 0.42 1.00::1: 0.47 0.80::1: 0041 1.80::1: 0.27<br />
AUC (ng)(mL)"I(h) 32.1::1: 3.8 87.6::1: 24.6 25.5::1: 7.9 316::1:172<br />
24-hour Urine<br />
Concentration (ng)(mLr l 0.94::1: 0.67 112::1: 58 94.9::1: 27.0 463::1: 153<br />
Amount (% daily dose) 0.014::1: 0.011 1.89::1: 1.10 1.01::1: 0.42 5.43 ::1:2.46<br />
Renal Clearance (mL)(min)"1 1.09::1: 0.83 48.7 ::1:23.9 148::1: 43 59.1::1: 6.8<br />
The current method has been shown to be accurate and precise with sufficient sensitivity to monitor all four<br />
analytes in human plasma and urine samples. The pharmacokinetic data, for the first time, show the<br />
magnitude <strong>of</strong> involvement <strong>of</strong>NBUPG in the clearance <strong>of</strong> buprenorphine.<br />
Supported by NIDA grants ROI DA 10100, ROI DA 13004, and K02 DA 00478<br />
Key words: Buprenorphine, Glucuronide metabolites, Pharmacokinetics<br />
Page 198
Scientific Session <br />
<strong>Abstracts</strong>: <br />
Behavioral <br />
Toxicology <br />
Page 199
Bl<br />
COMPARISON OF BLOOD AND BRAIN CANNABINOIDS CONCENTRA nONS IN 11 HUMAN<br />
CASES. CONSEQUENCES ON TRAFFIC SAFETY.<br />
Mura p.l', Raul S.B. 2 ,Dumestre V. 3 , Brunet B.l,4, Cavagna v.2, Hauet T.l.4, Kintz p: I Laboratoire de<br />
Toxicologie, University Hospital, Poitiers, France 2<strong>Forensic</strong> Toxicology Institute, Strasbourg, France<br />
3Toxgen laboratory, Bordeaux, France 4, INSERM ERM 324, University Hospital, Poitiers, France<br />
It is known that cannabis effects on cognitive and psychomotor tasks are proportional to the delta 9<br />
tetrahydrocannabinol (THC) amount consumed but that such impairments are not directly related to THC<br />
concentrations in blood. Some studies have also indicated that impairing effects could still be present while<br />
THC blood concentrations had dropped to a few ng/ml, but this assessment has never been confirmed by<br />
biological data. However, in a number <strong>of</strong> circumstances such as traffic safety or homicides, forensic<br />
toxicologists have frequently been asked to answer this question: according to the blood cannabinoids<br />
concentrations, was the subject under influence <strong>of</strong> cannabis In order to document this important question,<br />
we compared cannabinoids concentrations in blood and brain human samples.<br />
Blood and corresponding brain corresponding samples were provided from legal autopsies performed to<br />
determine the cause <strong>of</strong> death. In 11 cases, cannabinoids were found in blood: these 11 cases were<br />
consequently included in this study. All samples were stored at -20°C until analysis. THC, 11-hydroxy<br />
THC (II-OH-THC) and 11 nor-9-carboxy-THC (THC-COOH) were investigated by a gas chromatography<br />
mass spectrometric procedure derived from the method <strong>of</strong> Kemp et aL (1). Brain samples were initially<br />
grinded in pH 7.4 Tris buffer. In 10 cases, the precise location <strong>of</strong> brain sampling was not known. The<br />
results, expressed in ng/g, are indicated in the following table:<br />
I<br />
I Case number 1 2 3 4 5 I 6 7 8 9 10<br />
ITHC Blood 0.5 0.6 1.8 2.3 3.0 ! 4.4 11.5
B2 <br />
PROSPECTIVE STUDY ABOUT THE EFFECT OF CANNABIDIOL (CBD) ON THE<br />
PHARMACOKINETICS OF A 9 -TETRAHYDROCANNABINOL (THC) AFTER ORAL<br />
APPLICATION OF 10 MG THC AND 5.4 MG CBD IN CANNABIS EXTRACT<br />
Thomas Nadulskil, Fritz Pragst*\ Andreas Michael Stadelmann 2 , Patrik Roser 2 , Tom Schefte~, Martin<br />
Schnelle 3 , and E.-M. Fronk 3 : lInstitute <strong>of</strong> LegaJ Medicine and 20epartment <strong>of</strong> Psychiatry <strong>of</strong>the University<br />
Hospital Charite, Berlin, Germany; 31nstitute for Clinical Research, Berlin, Germany<br />
Besides the psychoactive delta 9-tetrahydrocannabinol (THC), varying amounts <strong>of</strong> cannabidiol (CBO) are<br />
contained in hashish and marihuana. Furthermore, cannabis-based medicine extracts and clinical grade<br />
cannabis contain high quantities <strong>of</strong> CBO, which frequently equal the percentage <strong>of</strong> THC. CBO is known<br />
from literature to modify the effects <strong>of</strong> THC and to have anti-anxiety effects and anti-psychotic benefits<br />
and to inhibit the P450 mediated conversion <strong>of</strong>THC to II-OH-THC. Therefore, in the present prospective<br />
and double blind study with 24 volunteers the concentration vs. time curves <strong>of</strong> THC and its main<br />
metabolites II-hydroxy-delta9-tetrahydrocannabinol (II-OH-THC) and II-nor-9-carboxy-delta9<br />
tetrahydrocannabinol (THC-COOH) as well as <strong>of</strong> CBO were measured after oral administration <strong>of</strong> 10 mg<br />
THC alone or in cannabis extract containing 5.4 mg CBO. Additionally, in 12 volunteers the effect <strong>of</strong> food<br />
on the concentration vs. time curves was tested. The analytical method was based on automatic solid phase<br />
extraction with CIS columns, derivatization with N,O-bistrimethylsilyltrifluoroacetamide (BSTFA) and<br />
electron impact ionization gas chromatography-mass spectrometry (GC-EIIMS) with deuterated standards.<br />
The limits <strong>of</strong> detection were between 0.15 and 0.29 ng/mL For the statistical evaluation, the course <strong>of</strong> the<br />
concentration vs. time curves and the areas under the curves (AUC) were compared and the metabolites as<br />
well as metabolite/drug ratios were included.<br />
The maximum plasma concentrations after intake <strong>of</strong> the cannabis extract ranged between 1.2 and 10.3<br />
nglml (mean 4.05 ng/ml) for THC, 1.8 andl2.3 nglml (mean 4.9 ng/ml) for II-OH-THC, 19 and 71 nglml<br />
(mean 35 nglml) for THC-COOH and 0.2 and 2.6 nglml (mean 0.95 ng/mg) for CBO. The peak<br />
concentrations (mean values) <strong>of</strong> THC, II-OH-THC, THC-COOH and CBO were observed 56, 82, 115 and<br />
60 min respectively after intake. As a mean slightly higher AUC for THC and slightly lower AUC for<br />
THC-COOH were measured after application <strong>of</strong> THC + CBO when compared with THC alone but the<br />
difference between both kinds <strong>of</strong> intake was not statistically significant. Therefore, an effect <strong>of</strong> CBO on the<br />
pharmakokinetics <strong>of</strong>THC at the studied concentrations could not be proved.<br />
The data were also compared with the results obtained by Huestis et aL in smoking experiments [1]. Caused<br />
by the strong first-pass metabolism, the concentrations <strong>of</strong> the metabolites were increased during the first<br />
three hours after oral drug intake as compared to smoking. Therefore, the concentration ratio THC<br />
COOH/THC is discussed as a criterion for distinguishing between oral and inhalative cannabis<br />
consumption. As a result, the differentiation between both ways <strong>of</strong> drug use based on this ratio is not<br />
possible in a practical case, since the exact time <strong>of</strong> drug intake before sampling is not known, since<br />
THC-COOH may be present in excess from previous consumption, and because <strong>of</strong> the large variation <strong>of</strong> the<br />
ratios within both groups. However, it is shown that the cannabis influence factor CIF introduced by<br />
Oaldrup et aL for interpretation <strong>of</strong> driving impairment by the drug [2] can also be used after oral intake.<br />
[1] M.A. Huestis, J.E. Henningfield, E.J. Cone. Blood cannabinoids. I. Absorption <strong>of</strong> THC and formation<br />
<strong>of</strong> ll-OH-THC and THCCOOH during and after smoking marijuana. J. Anal. ToxicoL 16:276-282.<br />
(1992).<br />
[2] T. Oaldrup, I. Meininger. Begutachtung der Fahrtlichtigkeit unter Cannabis im StrafVerfahren. In: G.<br />
Berghaus, H. P. KrUger (Eds.): Cannabis im StraBenverkehr. Gustav Fischer Verlag, Stuttgart 1998, pp.<br />
181-204.<br />
Keywords: Cannabinoids, Cannabidiol, Oral intake<br />
Page 201
B3 <br />
EFFECTS AND BLOOD CONCENTRATIONS OF THC, H-OH-THC AND THCCOOH<br />
FOLLOWING ORAL ADMINISTRATION OF 20 MG DRONABINOL OR OF A CANNABIS<br />
DECOCTION CONTAINING 20 OR60 MG DELTA9-THC<br />
A. MenetreyI, C. Giroud I *, M. Augsburgerl, L. Rothuizen 2 , M. Pin t, M. Appenzeller 2 , T. Buclin2, P.<br />
ManginI ILaboratoire de toxicologie et chimie forensiques, Institut Universitaire de Medecine Legale,<br />
Lausanne, 2Division specialisee de phannacoIogie et toxicologie cliniques, CHUV, Lausanne, Switzerland<br />
Smoking and oral ingestion are the most popular methods <strong>of</strong> Cannabis recreational use. Oral therapeutic<br />
administration, such as with Marinol® (synthetic THC (dronabinoJ) in sesame oil) was introduced in the US<br />
to alleviate anorexia in HIV/AIDS patients and to ease nausea in cancer chemotherapy. THC is also<br />
contained in hemp foods. In Switzerland, there is currently a great concern about the danger <strong>of</strong> driving<br />
under the influence <strong>of</strong> Cannabis. Epidemiological studies have indeed shown that Cannabis alone or with<br />
alcohol constitute the most frequent group <strong>of</strong> drugs detected in drivers involved in car accidents or in<br />
driving under the influence <strong>of</strong> drugs. The main objective <strong>of</strong> our study was to assess the effects <strong>of</strong> an acute<br />
oral intake <strong>of</strong> a medium to high dose <strong>of</strong>THC on driving capability. A hemp crude preparation containing<br />
1.5 % delta9-THC and 4.4 % delta9-THC-A was pre-treated at 140°C for 30 min to obtain a powder with<br />
4.9 % delta9-THC. From this powder containing 20 or 60 mg <strong>of</strong> delta9-THC, hemp milk decoctions were<br />
prepared with a yield <strong>of</strong> about 80%. A double-blind, ethical committee approved study was carried out with<br />
eight 20-30 years-old healthy male volunteers who were occasional Cannabis smokers. In 4 successive<br />
sessions, volunteers were administered a placebo, a decoction made with 20 or 60 mg delta9-THC or 20 mg<br />
dronabinol capsules in a randomised order. Blood samples were taken before administration and 1,2.5,4,<br />
5.5, 7, 10 and 24 hours following ingestion. In the same time-period, clinical examination and<br />
psychological tests were performed with a driving simulator. Blood levels <strong>of</strong> cannabinoids were determined<br />
by NCI GC-MS according to a method adapted from Huang et ae with limits <strong>of</strong> quantification <strong>of</strong> 0.3<br />
ng/mL forTHC, 0.8 ng/mL for II-OH-THC, and 0.1 ng/mL for THCCOOH.<br />
Because <strong>of</strong> anxiety events, which resolved spontaneously, two volunteers were withdrawn from the study<br />
after ingestion <strong>of</strong> the medium dose. Mean maximal concentrations [ng/mL] for THC, II-OH-THC and<br />
THCCOOH as well as the times [hours] to the maximum blood levels are listed below:<br />
Preparation <br />
dronabinol <br />
20 mg ~9-THC <br />
milk decoction <br />
16.5 mg ~9_THC <br />
milk decoction <br />
45.7 mg ~9-THC <br />
Parameter THC II-OH-THC THCCOOH<br />
I<br />
Tmax 1<br />
4 5.5<br />
Cmax 2.8 3.9<br />
27.8<br />
Tmax<br />
I<br />
I<br />
4<br />
Cmax 3.8<br />
4.7 27.8<br />
Tmax<br />
I<br />
2.5 2.5<br />
1<br />
Cmax I 8.4 12.8 66.2<br />
I<br />
The individual results show there was a considerable inter-subject variability. Mean maximum<br />
concentrations <strong>of</strong> 11-0H-THC exceeded the corresponding levels <strong>of</strong> THC. A 2 to 3 fold increase in<br />
cannabinoid concentrations was achieved following ingestion <strong>of</strong> the strongest decoction. Almost similar<br />
levels were measured after intake <strong>of</strong> the same dose <strong>of</strong> THC, regardless <strong>of</strong> the type <strong>of</strong> preparation (synthetic<br />
THC or crude plant extract). Obvious effects were observed with the tracking test showing a 50 % mean<br />
highest performance decrease after drinking the milk decoction containing 45.7 mg THC. Although a<br />
relatively high dose <strong>of</strong> THC was taken and significant psychoactive effects and performance reduction<br />
were noticed, THC and THCCOOH concentrations were much lower than those which are generally<br />
measured after marijuana smoking. In conclusion, this study shows that oral intake <strong>of</strong> delta9-THC may<br />
decrease human performance and exemplify the risks <strong>of</strong>driving under the influence <strong>of</strong> Cannabis.<br />
Key words: dronabinol, cannabis, driving under the influence <strong>of</strong> drugs<br />
3Huang W et aL J. Anal. Toxicol. 25: 531-537,2001<br />
Page 202
B4 <br />
REASONS FOR OVERESTIMATION OF THE ROLE OF CYP2D6 IN HUMAN METABOLISM<br />
OF AMPHETAMINE PRECURSOR DRUGS USING THE DARK AGOUTI RAT MODEL<br />
Thomas Kraemer', Denis Theobald and Hans H. Maurer: University Hospital, Homburg, Germany<br />
Background: Female Dark Agouti rats (fDA) have been proposed as a model <strong>of</strong> the human CYP2D6 poor<br />
metabolizer phenotype (PM) allowing a preliminary screening for CYP2D6 substrates. This rat model has<br />
successfully been used by the author's working group to investigate the role <strong>of</strong> CYP2D6 in human<br />
metabolism <strong>of</strong> the new designer drug TFMPP (1-(3-trifluoromethylphenyl)piperazine). However, the<br />
crucial role <strong>of</strong> CYP2D6 in N-dealkylation <strong>of</strong> amphetamine precursors (e.g. fenproporex) to amphetamine<br />
predicted by this rat model could not be confirmed using recombinant human CYPs and human liver<br />
microsomes (HLM). Four different CYP is<strong>of</strong>orms, namely CYPIA2, CYP2B6, CYP2D6 and CYP3A4,<br />
were involved in this metabolic step with CYP2D6 obviously not being <strong>of</strong> major importance. Using the<br />
data on intrinsic clearance for the particular is<strong>of</strong>orms the percentage <strong>of</strong> contribution <strong>of</strong> each is<strong>of</strong>orm to the<br />
entire microsomal clearance in vitro was calculated for fenproporex. The highest contribution was found<br />
for CYP2B6 (65 % for R(-) and 72 % for the S(+)-enantiomer) and the lowest values were found for<br />
CYP2D6 (7 % and 4 % for R(-) and S(+)-enantiomers, respectively). The aim <strong>of</strong> this study was to elucidate<br />
the reasons for the failure <strong>of</strong>the rat model. As a characteristic test reaction for CYP2B6 activity (CYP<br />
is<strong>of</strong>orm with the highest contribution), bupropion side chain hydroxylation was chosen.<br />
Methods: Data for calculation <strong>of</strong> intrinsic clearances for fenproporex N-dealkylation were taken from<br />
previous studies with recombinant CYPs. Bupropion hydrochloride (R,S-2-(tert-butylamino)-3'<br />
chloropropiophenone; amfebutamone; BU) was administered to Wistar (model <strong>of</strong> the human CYP2D6<br />
extensive metabolizer phenotype) and Dark Agouti rats for toxicological diagnostic reasons according to<br />
the corresponding German law. Urine was collected separately from the feces and analyzed directly after<br />
sampling. After enzymatic cleavage <strong>of</strong> conjugates and centrifugation, bupropion and hydroxy-bupropion<br />
were separated and quantified using an Agilent Technologies (AT, Waldbronn, Germany) AT 1100 series<br />
atmospheric pressure chemical ionisation (APCl) electrospray LC-MSD, SL version and an LC-MSD<br />
ChemStation using the A.OS.03 s<strong>of</strong>tware. Gradient elution was achieved on a Merck LiChroCART®<br />
column (125 x 2 mm LD.) with Superspher®60 RP Select B as stationary phase and a LiChroCART®1O-2<br />
Superspher®60 RP Select B guard column. The mobile phase consisted <strong>of</strong> ammonium formate (5 mM,<br />
adjusted to pH 3 with formic acid) (eluent A) and acetonitrile (eluent B). Human urine samples from<br />
volunteers after ingestion <strong>of</strong> BU were analyzed in the same way.<br />
Results and Discussion: BU and its metabolites could easily be separated using the applied LC-MS<br />
conditions. Characteristic fragments in the APCI-mass spectra allowed easy discrimination <strong>of</strong> the sidechain<br />
hydroxy from the ring hydroxy metabolites. Bupropion side chain hydroxylation was chosen as<br />
specific test reaction for CYP2B activity. Indeed, the side chain hydroxy bupropion (HO-BU) was the<br />
major BU metabolite in human urine samples, whereas it was almost completely absent in urine <strong>of</strong> the two<br />
rat strains. CYP2B6 seems to playa major role in human metabolism <strong>of</strong> amphetamine precursors. BU side<br />
chain hydroxylation, a characteristic test reaction for this is<strong>of</strong>orm, hardly occurs in either rat strain. As a<br />
consequence, it could be possible, that for lack <strong>of</strong> a corresponding CYP2B is<strong>of</strong>orm, CYP2D is<strong>of</strong>orms take<br />
over such metabolic reactions in rats leading to an overestimation <strong>of</strong> the role <strong>of</strong> CYP2D for human<br />
metabolism. In addition, it should also be kept in mind, that the lower extent <strong>of</strong> ring hydroxylation <strong>of</strong><br />
amphetamine precursors under in vitro conditions may also contribute to the differences found between<br />
animal in vivo models and human in vitro test systems.<br />
Keywords: Dark Agouti rats; cytochrome P450; amphetamine precursor drugs<br />
,~,--,,-<br />
Page 203
B5 <br />
CORRELATION OF SALIVA AND BLOOD ESTAZOLAM CONCENTRATIONS WITH<br />
BALANCE CHANGES IN SUBJECTS AFTER ADMINISTRATION OF THE DRUG AND/OR<br />
ALCOHOL<br />
Maria Kalal> Piotr Adamowicz l , Ewa Chudzikiewicz l , Wojciech Lechowicz l , Ewa Pufal 2 , Wojciech<br />
Piekoszewski l , Karol Sliwka 2 : IInstitute <strong>of</strong> <strong>Forensic</strong> Research in Krakow; 2Department <strong>of</strong> <strong>Forensic</strong><br />
Medicine <strong>of</strong>the Medical Academy in Bydgoszcz<br />
In 1992-1999, at the Institute <strong>of</strong> <strong>Forensic</strong> Research in Krakow, blood samples taken from 83 drivers<br />
involved in road incidents tested positive for morphine. Benzodiazepines (BZD) were found in 60% <strong>of</strong> the<br />
cases. In 2002-2003, the number <strong>of</strong> drivers under the influence <strong>of</strong> drugs involved in accidents was 166.<br />
There was a high prevalence (65%) <strong>of</strong>THC and amphetamines detected. 17% <strong>of</strong> the population were under<br />
the influence <strong>of</strong> morphine and other medications, and 23% tested positive for BZD. In 2002, 278 drivers<br />
were questioned about driving a car after intake <strong>of</strong> a medicinal drug. 134 respondents reported driving a<br />
car while taking a medicinal drug; 41% <strong>of</strong> them used BZD. Although the approach to the presence <strong>of</strong><br />
morphine, THC, cocaine and amphetamines in the blood <strong>of</strong> drivers should without doubt be one <strong>of</strong> "zerotolerance",<br />
the situation concerning the legal limit for BZD is not so clear. .<br />
On the basis <strong>of</strong> the results both <strong>of</strong> surveys and laboratory examinations, it can be stated that the BZD's<br />
most <strong>of</strong>ten used in Poland are diazepam and estazolam. Therefore, estazolam was chosen as a model<br />
substance for analysis <strong>of</strong> balance changes in persons influenced by the drug. The balance disturbance that<br />
occurs at the legal limit (0.5 giL) <strong>of</strong>alcohol in blood was used as a reference point.<br />
Concentrations <strong>of</strong> estazolam in blood and saliva samples were determined by the LC-MS/APCI method<br />
after LLE. Blood and saliva samples were taken from 25 healthy volunteers who received a single oral<br />
dose <strong>of</strong> 1 mg <strong>of</strong> estazolam. The samples were collected every hour, for four hours. Half an hour before the<br />
last sampling, volunteers received a dose <strong>of</strong> ethanol that led to a blood concentration <strong>of</strong> about 0.5g/1. On<br />
the next day, the same volunteers received alcohol alone at the same dose, and a blood and saliva sample<br />
was taken 0.5 h later.<br />
The LC-MS/APCI method had the following validation parameters [ng/mLl: LOD - 0.33 and 0.63, LOQ <br />
1.09 and 1.05, LOL - up to 200 and 20 for blood and saliva respectively.<br />
The dose <strong>of</strong> estazolam produced average blood concentrations <strong>of</strong> 21, 24, 24 and 29 ng/mL, and saliva <strong>of</strong><br />
2.8, 1.9, 1.9 and 2.2 ng/mL at the respective sampling points. The correlation coefficient between blood<br />
and saliva concentrations was 0.50.<br />
For estimation <strong>of</strong> balance changes in persons influenced by estazolam, alcohol, and estazolam with alcohol,<br />
posturography was used. Using the Langevin equation, the diffusion matrix and the friction coefficient<br />
were calculated. For each <strong>of</strong> the tested persons, 8 stabilograms were obtained, two (with open and closed<br />
eyes) for each <strong>of</strong> the four studied situations:· control (before estazolam or alcohol administration); after<br />
intake <strong>of</strong> alcohol alone; 2 h after intake <strong>of</strong> estazolam alone; as well as after intake <strong>of</strong> ethanol together with<br />
estazolam.<br />
It was shown that the values <strong>of</strong> the friction coefficient decreased when persons kept their eyes closed,<br />
1<br />
from: 9.45 to 7.25 5. , 9.45 to 6.95 5. 1 and 9.83 to 6.77 5. 1 after administration <strong>of</strong> estazolam, alcohol, and<br />
alcohol with estazolam respectively. These changes showed a trend when under the influence <strong>of</strong> estazolam<br />
(P=0.078) and ethanol (P=0.057), but were statistically significant for estazolam with ethanol (P=0.036) as<br />
compared to the placebo condition. The values <strong>of</strong> the friction coefficient after administration <strong>of</strong> alcohol<br />
and estazolam did not differ statistically (P=0.677).<br />
The results show that the friction coefficient can be used as an indicator that allows us to assess if a person<br />
is under the influence <strong>of</strong> a medicine that disturbs hislher balance.<br />
Keywords: Estazolam, Friction Coefficient, Posturography.<br />
Page 204
B6 <br />
EVALUATION OF THE POST-ROTATIONAL NYSTAGMUS TEST (PRN) IN DETERMINING<br />
ALCOHOL INTOXICATION<br />
Majda Zorec Karlovsek*, Joze Balazic: *University <strong>of</strong> Ljubljana, Institute for <strong>Forensic</strong> Medicine,<br />
Ljubljana, Slovenia<br />
Aims: With a blood alcohol concentration (BAC) legal limit <strong>of</strong>0.5 glkg (since 1965), Slovenia's road traffic<br />
legislation has increasingly oriented the work <strong>of</strong> forensic toxicologists towards quality assurance <strong>of</strong><br />
alcoholometric analyses <strong>of</strong> BAC and breath alcohol concentration (BrAC). The introduction <strong>of</strong> a<br />
Standardised Field Sobriety Test (SFST) for identifying suspected DUl <strong>of</strong>fenders raised our interest to<br />
evaluate the post-rotational nystagmus test or Tashen test, a part <strong>of</strong> the physician's examination for<br />
detecting alcohol intoxication. Post-rotational nystagmus is induced by suddenly stopping the rapid rotation<br />
<strong>of</strong> the body; large slow movements <strong>of</strong> the eyeballs occur in the opposite direction to the direction <strong>of</strong><br />
rotation.<br />
Performing the test: The person is turned with open eyes in a tight circle 5 times around his axis (while<br />
sitting on a swivel chair). Time is measured after the chair stops and the person fixes his gaze on an object<br />
(e.g., a pencil or finger), which the physician holds at a distance <strong>of</strong> approximately 30 cm from his eyes.<br />
Materials and methods: The study included the results <strong>of</strong> 1,006 PRN tests performed during medical<br />
examinations for DUl cases at the Institute for <strong>Forensic</strong> Medicine in Ljubljana in the years 1998-2002.<br />
Cases with a combination <strong>of</strong> alcohol and drugs were excluded. The evaluation <strong>of</strong> PRN test results with<br />
BAC as a reference was based on classification into the following categories and characteristics: true<br />
positives (TP), true negatives (TN), false positives (FP), false negatives (FN), sensitivity, specificity,<br />
positive predictive values (PPV), negative predictive values (NPV) and accuracy.<br />
Results: Measured interval values <strong>of</strong> post-rotational nystagmus time ranged from 1 to 45 s, mean value 14,<br />
median 13; BAC values were between 0.0 and 3.16 glkg, mean 1.12 g/kg, median 1.14 g/kg. The values <strong>of</strong><br />
post-rotation nystagmus time and BAC show a positive correlation, which is statistically significant (r =<br />
0.54,p < 0.01). For the regression line, the following formula was obtained: PRN = 6.0 x BAC + 7.2.<br />
Raising the threshold values for post-rotational nystagmus time (from 6 to 16 s) shows an increase in<br />
sensitivity accompanied by a decrease in specificity. The optimal cut-<strong>of</strong>f value <strong>of</strong> 10 s for post-rotational<br />
nystagmus time was chosen with the help <strong>of</strong> a Receiver Operating Characteristic curve (ROC curve) for<br />
BAC limit 0.5 g/kg (TP=584, FP=43, FN=229, TN=150, sensitivity=0.718, specificity=0.777, PPV= 0.931,<br />
NPV= 0.396, accuracy=0.730).<br />
Conclusions: According to the area under the ROC curve, the post-rotational nystagmus test is a fair test for<br />
predicting alcohol intoxication over 0.5 g/kg. However, as a part <strong>of</strong> the physician's examination it can<br />
contribute to the description <strong>of</strong>the clinical state.<br />
Key words: post-rotational nystagmus, alcohol intoxication<br />
Page 205
B7 <br />
DETECTION OF COMMONLY ABUSED DRUGS IN URINE OF SEXUAL ASSAULT<br />
COMPLAINANTS<br />
Matthew Juhascik 1 *, R.E. Gaensslen\ Christine M. Moore 2 , Paul J. Goldstein', Alice Lindner 4 , Pam<br />
Greene 4 , Diana Faugn0 5 , Linda Ledral, Barbara Haner 7 , Adam Negrusz 1 : lDepartment <strong>of</strong><br />
Biopharmaceutical Sciences, University <strong>of</strong> Illinois at Chicago, Chicago, IL, 2United States Drug Testing<br />
Laboratories, Inc., Des Plaines, IL, 'Epidemiology and Biostatistics, University <strong>of</strong>IlIinois at Chicago,<br />
Chicago, IL, 4Scott & White Memorial Hospital, Temple, TX 5Palomar Pomerado Medical Center,<br />
Escondido, CA, 6SARC, Hennepin County Medical Center, Minneapolis, MN, 7Providence Everett Medical<br />
Center, Everett, W A.<br />
There are approximately 100,000 reported cases <strong>of</strong> sexual assault in the U.S. every year. It is estimated<br />
(Bureau <strong>of</strong> Justice Statistics) that there are more than 300,000 sexual assaults every year, three times the<br />
number actually reported. Recently, the use <strong>of</strong> "date-rape" drugs to incapacitate someone has received<br />
considerable coverage in the media. However, before toxicologists can examine what "date-rape" drugs<br />
are present in a sexual assault complainant, it is important to know what drugs <strong>of</strong> abuse are also commonly<br />
found. This project is designed to estimate which drugs <strong>of</strong> abuse are found in sexual assault complainants<br />
through a random sample from four reasonably representative US jurisdictions. Sites include locations in<br />
Washington, Texas, California, and Minnesota.<br />
Sexual assault complainants are asked when presenting to the hospital ifthey would like to take part in this<br />
study. Ifthey agree, consent forms are filled out and the complainant provides a urine sample following a<br />
protocol approved by the UIC IRB. The sample is then sent to our laboratory for proper handling and<br />
storage. At the end <strong>of</strong> the subject recruitment phase <strong>of</strong>the study, 31 sexual assault complainants had been<br />
recruited at the Texas location, 56 from the California site, 15 from Washington, and 43 in Minnesota, for a<br />
total <strong>of</strong> 145. The racial distribution <strong>of</strong>the sample is: 70.3% White, 8.3% Black, 13.1% Latino, and 8.3%<br />
other/unknown. The ages <strong>of</strong>the complainants range from 18 to 56 with the highest number in the 21-25<br />
age cohort.<br />
Urine samples collected from all <strong>of</strong> the complainants are screened by immunoassay for the following drugs<br />
<strong>of</strong>abuse (values in parentheses are corresponding cut-<strong>of</strong>f values): ethanol (40 mg/dL), amphetamines (250<br />
ng/mL), opiates (50 ng/mL), PCP (10 ng/mL), cannabinoids (10 ng/mL), methadone (100 ng/mL),<br />
barbiturates (100 ng/mL), and benzodiazepines (100 ng/mL). Because drug-facilitated sexual assault<br />
victims may have only been given a single dose, low cut-<strong>of</strong>f values for the EMIT screen were used to<br />
achieve maximum sensitivity. All presumptive positive samples are confirmed by GC-MS following<br />
extraction and derivatization if appropriate. To date, 125 specimens have been analyzed. Confirmed<br />
positives include 13.6% for cocaine, 28% for marijuana, 2.4% for benzodiazepines, 6.4% for opiates, and<br />
7.2% for amphetamines. These preliminary results suggest that complainants <strong>of</strong> sexual assault have more<br />
drugs in their system than the normal population.<br />
In order to determine if sexual assault complainants are more or less likely to abuse drugs, our results will<br />
be compared to general population drug use data from NIDA' s Monitoring the Future and the National<br />
Household Survey on Drug Abuse conducted by SAMHSA. The confirmed positives will also be<br />
examined by race, age, and geographic location to determine ifany trends are apparent.<br />
Key Words: Sexual assault, drugs <strong>of</strong>abuse, GC-MS.<br />
Page 206
B8 <br />
TOXICOLOGICAL FINDINGS IN CASES OF ALLEGED DRUG FACILITATED SEXUAL<br />
ASSAULT IN THE UNITED KINGDOM<br />
Michael Scott-Ham BSc and Fiona C. Burton PhD*: The <strong>Forensic</strong> Science Service, London Laboratory,<br />
109 Lambeth Road, London, SEI 7LP, UK.<br />
The <strong>Forensic</strong> Science Service (FSS) is the major provider <strong>of</strong> forensic services in the UK. It has several<br />
laboratories throughout the country with two providing forensic toxicology services. These two<br />
laboratories annually deal with approximately 500 cases <strong>of</strong> alleged drug facilitated sexual assault (DFSA)<br />
submitted from various UK police forces.<br />
This study outlines the results from 1014 cases <strong>of</strong> claimed drug facilitated sexual assault analysed at the<br />
<strong>Forensic</strong> Science Service, London Laboratory between January 2000 and December 2002. As and where<br />
appropriate, either a whole blood sample or a urine sample from the complainant was initially analysed for<br />
alcohol and common drugs <strong>of</strong> abuse. The test for alcohol was by gas chromatography and for common<br />
drugs <strong>of</strong> abuse by immunoassay with positive results being confirmed by gas chromatography-mass<br />
spectroscopy (GC-MS). Common drugs <strong>of</strong> abuse tested for include cannabis, amphetamine, Ecstasy,<br />
cocaine, opiate drugs, methadone, barbiturates and the benzodiazepine drugs diazepam and temazepam. All<br />
urine samples (or blood sample if urine not collected) were further tested for potentially stupefYing drugs<br />
and their metabolites by either positive or negative ion GC-MS (as applicable). These tests have been<br />
shown to have the low limits <strong>of</strong> detection required to detect the drugs <strong>of</strong> concern. Potentially stupefYing<br />
drugs included a range <strong>of</strong> other benzodiazepine drugs (including flunitrazepam) and related drugs such as<br />
zopiclone, gammahydroxybutyrate (GHB) and a range <strong>of</strong> chemically basic pharmaceutical drugs such as<br />
ketamine and other medicinal drugs with sedative properties. The urine samples were also tested for<br />
trichlorinated compounds (e.g. chloral hydrate) by a colour test.<br />
The results are interpreted with respect to the numbers <strong>of</strong> each drug detected. An attempt has been made to<br />
distinguish between voluntary use and involuntary ingestion by using information provided by the<br />
investigating police <strong>of</strong>ficer (with follow-up discussion where necessary). Furthermore, in those cases<br />
where alcohol was detected, the most likely blood alcohol level at the time <strong>of</strong> the alleged incident has been<br />
calculated.<br />
Alcohol (either alone or with an illicit or medicinal drug) was detected in 46% <strong>of</strong> all cases and in 81 % <strong>of</strong><br />
the cases in which the samples were taken within 12 hours <strong>of</strong> the alleged incident. Of the cases where<br />
alcohol was detected, 60% had a high back-calculated figure. For the purposes <strong>of</strong>this paper high is defined<br />
as greater than 150 milligrams per 100 millilitres (%). Illicit drugs were detected in 34% <strong>of</strong> the 1014 cases<br />
with cannabis being the most commonly detected drug followed by cocaine, benzodiazepine drugs, opiate<br />
drugs, Ecstasy, amphetamine and methadone. A number <strong>of</strong> samples contained more than one illicit drug.<br />
In 2% <strong>of</strong> cases, a potentially stupefying drug was detected which had not been admitted and therefore could<br />
be a genuine DFSA case. GHB was detected in some <strong>of</strong> these cases but neither flunitrazepam nor its<br />
metabolites was detected. Although sedative drugs were detected in many more cases, complainants<br />
admitted prescribed use <strong>of</strong> these medications. A wide range <strong>of</strong> non-sedative pharmaceutical drugs were<br />
also detected. The types and numbers <strong>of</strong> all these drugs will be presented (together with examples <strong>of</strong><br />
typical limits <strong>of</strong> detection).<br />
The results <strong>of</strong> these studies are in agreement with other studies published in this area. However, this is the<br />
first study to our knowledge which has attempted to identifY the 'genuine' cases and which discusses in<br />
detail the significance <strong>of</strong> the alcohol levels found in cases <strong>of</strong> this type.<br />
Keywords: DFSA, flunitrazepam, alcohol<br />
Page 207
B9 <br />
ABSINTHE ANALYSIS: A STUDY OF TOXIC COMPONENTS OF THE NOTORIOUS<br />
BEVERAGE<br />
Smith AC 1 *, Vena J, Wu AH, McLane G; Departments <strong>of</strong>Pathology and Laboratory Medicine and Medical<br />
Toxicology, Hartford HospitallUniverity <strong>of</strong> Connecticut, and Absolute Standards, Inc.<br />
Introduction: Popular in the 1800's, absinthe is liquor made from the extract <strong>of</strong> the wormwood plant<br />
(Artemesia absinthium). The extract had a green hue, which led the drink to be known as the "green fairy".<br />
Historically color was enhanced with additives such as antimony and copper, which may have influenced<br />
toxic effects. The drink was popular among artists and writers because its inherent hallucinogenic<br />
properties known as the absinthe effect. The absinthe effect was known to stimulate creativity and sexual<br />
desire. Popularity and excess led to a public health problem, and it was banned in the early 1900's in many<br />
countries. There has been a recent resurgence as this ban has been lifted in Europe under new regulations ..<br />
In countries were absinthe is still banned, orders can be placed over the internet. The major active<br />
ingredients are bicyclic terpenes, o.-thujone and /3-thujone, which .are found as diastereoisomers in nature.<br />
Thujone is a neurotoxic and porphyrogenic compound. The more potent form is o.-thujone, which is<br />
believed to block the y-aminobutyric (GABA) gated chloride channel. The fractional content <strong>of</strong> a. and /3<br />
thujone is dependent upon plant source. CUrrent European guidelines limit thujone content to 10 ppm in<br />
alcoholic beverages. Analysis was conducted on 5 separate samples to determine thujone and other terpene<br />
content, as well as analysis <strong>of</strong> heavy metal and ethanol content.<br />
Materials and Methods: Five different commercially available absinthe bottles produced in France and<br />
Germany were analyzed, each claiming to have an infusion <strong>of</strong> wormwood plant. Extraction was performed<br />
using chlor<strong>of</strong>orm as the organic solvent. GCIMS analysis was performed on the extracts using total ion<br />
chromatography and selected ion monitoring. A 10 ppm 0.- thujone standard was used to quantifY results<br />
(Fluka >96%). Samples were treated with nitric acid, and assayed using ICPIMS to determine the metal<br />
content. Ethanol content was assayed on a Roche Integra chemistry analyzer using the alcohol<br />
dehydrogenase<br />
Results:<br />
0.- thujone (ppm)<br />
~- thujone (ppm)<br />
Total thujone (ppm)<br />
EtOH (label) v/v<br />
EtOH (measured) v/v<br />
Copper (ppb)<br />
Antimony (ppb)<br />
sample 1 sample 2 sample 3 sample 4 sample 5<br />
4.0 1.5 3.4 1.3 0.2<br />
2.1 1.2 3.2 0.0<br />
6.1 12.7 6.6 ]If 0.2<br />
55% !55% 60% 45% 55%<br />
53% 55% 56% 46% 53%<br />
15.3 71.3 25.8 19.5 19.6<br />
0 0 6.8 0 0<br />
A number <strong>of</strong> other related compounds appeared in the samples, which in addition to thujone, are extracts<br />
from plant sources used to make absinthe. These were identified with a library spectra match (> 90%).<br />
Compounds include camphor, menthol, fenchone, methone, and anisaldehyde.<br />
Conclusion: Modern absinthe does conform to current guidelines in regards to thujone content by our<br />
analysis. However, much variation was seen between each manufacturer. One sample did have high levels<br />
<strong>of</strong> antimony, and all had copper in varied concentration. The clinical toxicity <strong>of</strong> absinthe with high terpene<br />
and metal content in the presence <strong>of</strong> ethanol intoxication needs further research. Although absinthe is still<br />
<strong>of</strong>ficially banned in the U.S., this product is available on the Internet and popularity is rising. In July 2003,<br />
an article appeared in Maxim magazine describing this recent trend and Internet popularity in the U.S. The<br />
history <strong>of</strong> absinthe has shown it to be a public health concern. The high alcohol content combined with the<br />
effects <strong>of</strong> thujone may increase the risk <strong>of</strong> critical intoxication with consumption <strong>of</strong> modern absinthe.<br />
Keywords: Absinthe, Analysis, GC/MS<br />
Page 208
BIO<br />
LOW BLOOD ALCOHOL LEVELS, ATTENTIVE FUNCTIONS AND BODY SWA Y<br />
Raffaele Giorgetti, Santo Davide Ferrara*, Massimo Montisci, Rossella Snenghi, Silvano Zancaner, Mirella Libero: Centre <strong>of</strong><br />
Behavioural and <strong>Forensic</strong> Toxicology, University <strong>of</strong> Pad ova, Italy<br />
This double-blind study aimed at examining the effects <strong>of</strong> low blood alcohol levels (BAC) with placebo control and random<br />
cross-over distribution. Psychomotor performance and body sway were studied in 16 healthy volunteers after intake <strong>of</strong> low<br />
doses <strong>of</strong> ethyl alcohol (0.5 glkg). Neurosensory and psychomotor functions were assessed by a Divided Attention Test (DAT)<br />
together with Short-Term Memory and Response Competition Tests (RCT). Changes in body sway were recorded by a<br />
stabilometer. Tests were administered at 30, 60, 120 and 180 minutes after alcohol intake. Tests were repeated with a wash-out<br />
period <strong>of</strong>one week. BAC was monitored by breathalyser and analysis <strong>of</strong> blood levels.<br />
Statistical analysis showed that., as regards the RCT, the number <strong>of</strong> errors did not increase in a statistically significant way (p =<br />
0.9071) in any <strong>of</strong> the experimental phases after alcohol intake (Table I). Only the time effect (learning effect) reached<br />
statistical significance.<br />
TABLE I- Response Competition Test<br />
Treatment Time Treatment x Time<br />
F T p-value F I p-value F I p-value<br />
Errors 0.001 1 0.9071 10.61 I
Bll<br />
HUMAN PERFORMANCE FORENSIC TOXICOLOGY IN TURKEY<br />
S. A. Akgur*l, P. Ozturk l , S. Cengiz 2 , A. Yemiscigil l <br />
lEge University Faculty <strong>of</strong> Medicine, Department <strong>of</strong> <strong>Forensic</strong> Medicine, Bornova, Izmir, Turkey. <br />
2Institute <strong>of</strong> Legal Medicine and <strong>Forensic</strong> Science, Istanbul, Turkey. <br />
Human performance toxicology, also referred to as behavioral toxicology, is a branch <strong>of</strong> forensic<br />
toxicology concerned with the relationship between the presence <strong>of</strong> a drug and associated behavioral<br />
changes. <strong>Forensic</strong> toxicologists have become interested in human performance toxicology because it is a<br />
natural extension <strong>of</strong> their interest in the medicolegal implications <strong>of</strong> drug use, misuse, and abuse. This<br />
branch needs new educational and analytical approaches and developments in our country. The aim <strong>of</strong> this<br />
study is to describe the present status, progress and applications <strong>of</strong> human performance toxicology in<br />
Turkey.<br />
<strong>Forensic</strong> Toxicology in Turkey is carried out in the <strong>Forensic</strong> Medicine Council <strong>of</strong> the Ministry <strong>of</strong> Justice<br />
and <strong>Forensic</strong> Medicine Departments and <strong>Forensic</strong> Medicine Institutes <strong>of</strong> Universities. <strong>Forensic</strong> Toxicology<br />
is practiced almost exclusively as a result <strong>of</strong> investigation <strong>of</strong> fatalities. As a result, postmortem forensic<br />
toxicology is the main topic in the <strong>Forensic</strong> Medicine Council.<br />
In most countries <strong>Forensic</strong> Toxicology has progressed with the advances in analytical chemistry but the<br />
same progress has not been achieved yet in forensic chemistry in countrywide <strong>of</strong> Turkey except Istanbul<br />
Ankara and izmir. <strong>Forensic</strong> Medicine Departments that provide education in forensic medicine are also<br />
attempting to develop the fields <strong>of</strong> forensic sciences. There are several forensic toxicology education<br />
programs in universities and institutes, including Ege University.<br />
Ege University, in cooperation with the Police Department, is applying on-site (saliva) drug tests in traffic<br />
cases. The positive results will be· confirmed by Enzyme Multiplied Immunoassay (EMIT) and Gas<br />
Chromatography! Mass Spectrometry (GCIMS). Most countries have legislation covering driving under<br />
the influence <strong>of</strong> drugs (DUID). Most have an impairment approach but not an analytical approach. Several<br />
European Union (EU) member states have recently introduced or are preparing 'per se' laws on DUID.<br />
Driving under the influence <strong>of</strong> drugs is prohibited by traffic legislation in our country also, but<br />
unfortunately the analytical procedure is not yet effectively used. The Police Criminology Laboratories do<br />
not analyze biological specimens for drugs. In routine applications, the impairment approach is only related<br />
with driving under the influence <strong>of</strong> alcohol.<br />
At present, the breath alcohol tests performed by police are routinely applied to motor vehicle operators<br />
driving under the influence <strong>of</strong> alcohol. The allowed ethanol limit for driving under the Turkish Road<br />
Traffic Act is O.5gfL. In alcohol testing, the first suspicion <strong>of</strong> the police <strong>of</strong>ficer is followed by an on-site<br />
breath analyzer test and under certain conditions it is followed by the blood test for alcohol in Council <strong>of</strong><br />
<strong>Forensic</strong> Medicine cases. Blood Alcohol Determination is performed by Conway- micro diffusion,<br />
immunoassay techniques and gas chromatography. Recently, the <strong>Forensic</strong> Medicine Chemical Analysis<br />
Specialty Office has made an effort for analytical toxicological research projects to include GC, GCIMS,<br />
High Performance Liquid Chromatography (HPLC) and Head Space Gas Chromatography (HS-GC).<br />
More collaborative projects on educational and laboratory practices will help us to achieve improvements<br />
in <strong>Forensic</strong> Toxicology in Turkey.<br />
Keywords: Human, Performance Toxicology, Turkey<br />
Page 210
B12 <br />
DRUGS OF ABUSE IN PORTUGAL; A STATISTICAL REVIEW<br />
S Avila l "" A Castanheira, M Barroso, C Margalho, E Gallardo, S Santos, E Marques, D N Vieira:<br />
National Institute <strong>of</strong> Legal Medicine-Delegation <strong>of</strong> Coimbra Portugal<br />
Introduction: Drug abuse and its eventual association to fatal intoxications, or other violent deaths, is<br />
responsible for a great number <strong>of</strong> requests for drug testing at the Portuguese National Institute <strong>of</strong> Legal<br />
Medicine. With approval <strong>of</strong> recent legislation in 1998, which establishes procedures for conducting drug<br />
screening requested by driving enforcement authorities, it has been possible to develop a new approach to<br />
the evaluation <strong>of</strong> drug consumption linked to driving in situations which did not result in fatal accidents.<br />
Objectives: The authors present a retrospective study involving cases from 2003, from the centre <strong>of</strong><br />
Portugal. Drug testing in post mortem blood was performed in all cases requested by the pathologist, as<br />
well as in those cases <strong>of</strong> individuals aged less than 50 years old, when the autopsy was inconclusive. The<br />
authors also evaluated the incidence <strong>of</strong> drugs <strong>of</strong>abuse in deaths related to driving accidents, and discuss the<br />
actions <strong>of</strong> the pathologist, as well as <strong>of</strong> the law forces, in these situations, regarding the request <strong>of</strong> the drug<br />
screening.<br />
Methods: The samples tested were always whole blood. After screening by enzyme-linked immunoassay<br />
(EIA by Coda, Bio-Rad), the positive samples were submitted to a procedure involving solid phase<br />
extraction followed by confirmation and quantification analysis using a HP 6890 gas chromatographer<br />
equipped with a HP 5973 mass selective detector (GCIMS) using electron-impact ionization. Cut-<strong>of</strong>f values<br />
for the most common drugs are established by law: 100, 150,80 and 1000 ng/mL for opiates, cocaine and<br />
metabolites, cannabinoids and amphetamines, respectively. The limits <strong>of</strong> quantification (LOQ) are less than<br />
these cut-<strong>of</strong>f values for all drugs analysed.<br />
Results: The authors present the overall results <strong>of</strong>testing for drugs <strong>of</strong> abuse in post mortem samples, with a<br />
description <strong>of</strong> the circumstances <strong>of</strong> driving accidents. 261 analyses for drug testing in post mortem blood<br />
were performed and 18 were positive (6.9%). 61 (23.4%) <strong>of</strong> the cases were due to driving accidents and<br />
only I <strong>of</strong> these was positive for drugs <strong>of</strong> abuse. Law enforcement authorities requested 163 analyses for<br />
drug testing. There were 10 (6.1%) positive results. In 6 <strong>of</strong> these positive cases, the information was<br />
sufficient to establish links to driving accidents.<br />
Conclusion: Since the law that regulates drug screening in driving cases is very recent, it is still difficult to<br />
make reliable conclusions about the influence <strong>of</strong> these substances on driving, and on the incidence <strong>of</strong><br />
accidents. On the other hand, law enforcement authorities do not consistently request drug testing, because<br />
the law is not clear enough in this respect. The pathologists also use variable criteria to request testing,<br />
therefore, screening tests for drugs <strong>of</strong> abuse have only been performed on a small percentage <strong>of</strong> the total<br />
fatal accidents.<br />
Key words: Drugs <strong>of</strong> abuse, Driving, Portugal<br />
Page 211
B13 <br />
CONCENTRATION OF DRUGS IN BLOOD OF SUSPECTED IMPAIRED DRIVERS<br />
Marc Augsburger*\ Nicolas Donze 2 , Annick Menetreyl, Clarisse Brossard l , Frank Sporkert\ Christian<br />
Giroud l and Patrice Mangini : I Institut Universitaire de Medecine Legale, Lausanne, Switzerland; 2<br />
Consilia, Sion, Switzerland<br />
Blood has been undoubtedly considered to be the only suitable specimen for the evaluation <strong>of</strong> driving<br />
impairment due to drug consumption. In order to gain more information about the type and the<br />
concentrations <strong>of</strong> drugs used by drivers arrested for driving under the influence <strong>of</strong> drugs (DUID), we<br />
analyzed 440 blood samples. All <strong>of</strong>ficial DUID cases submitted by the Justice Department during a period<br />
ranging from 2002 to 2003 concerning living individuals were considered. This study included 400 men<br />
(91%) and 40 women (9%). The average age <strong>of</strong> the drivers was 28±1O years (minimum 16 and maximum<br />
81). One or more psychoactive drugs were found in 89% <strong>of</strong> blood samples. For the majority <strong>of</strong> cases (51%<br />
from 440), mixtures (from 2 to 6) <strong>of</strong> psychoactive drugs were detected in blood. The most commonly<br />
detected drugs in blood are cannabinoids (54%), ethanol (42%), cocaine (12%), benzodiazepines (11%),<br />
amphetamines (8%), opiates (8%) and methadone (6%). Among these 440 cases, THCCOOH was found in<br />
54% {mean 35 nglml (1 to 215 ng/ml)), ~9-THC in 49% {mean 5 ng/ml (I to 35 ng/ml)), ethanol in 42%<br />
{mean 1,28 g/kg (0.14 to 2.95 g/kg)), benzoylecgonine in 12% {mean 515 ng/ml (29 to 2430 ng/ml)), free<br />
morphine in 8% {mean 19 nglml (1 to 111 nglml)), methadone in 6% (mean 165 ng/ml (27 to 850 nglml)),<br />
MDMA in 6% {mean 388 nglml (1O to 2480 ng/ml)), free codeine in 5% {mean 5 ng/ml (I to 13 ng/ml)),<br />
cocaine in 5% {mean 109 ng/ml (15 to 560 ng/ml)), midazolam in 5% {mean 56 ng/ml (20 to 250 nglml)),<br />
nordiazepam in 4% {mean 492 ng/ml (30 to 1560 ng/ml)), amphetamine in 4% {mean 63 nglml (10 to 183<br />
nglml)), diazepam in 2% {mean 279 nglml (80 to 630 nglml)) and oxazepam in 2% {mean 614 nglml (165<br />
to 3830 ng/ml)). Other drugs, such as lorazepam, zolpidem, mirtazapine, methaqualone were found in less<br />
than 1 % <strong>of</strong> the cases. Propositions for a new zero-tolerance law will suggest that the presence <strong>of</strong> scheduled<br />
drugs like amphetamine (2:20 ng/ml), methamphetamine (2:20 nglml), MDMA (2:50 nglml), MDE (2:50<br />
ng/ml), cocaine (2:20 nglml), free morphine (2:20 nglml) and ~9-THC (2:2 ng/ml) is sufficient for<br />
prosecution, regardless whether the capacity <strong>of</strong> driving <strong>of</strong> the person was impaired. If we apply these<br />
conditions to these cases, 60% <strong>of</strong>the drivers tested in this study would be prosecuted.<br />
Keywords: drugs, alcohol, driving<br />
Page 212
B14 <br />
EFFECTS OF OPIOIDS ON METHAMPHETAMINE-INDUCED STEREOTYPICAL<br />
SELF-INJURIOUS BEHAVIOR IN MICE<br />
Tomohisa Mori"', Shinobu Itoh, Toshiko Sawaguchi : Department <strong>of</strong> Legal Medicine, Tokyo Women's<br />
Medical University, Tokyo, Japan<br />
Psychostimulants as well as other abused drugs, such as morphine and heroin, induce several behavioral<br />
effects in rodents, which is believed to be mediated by the activation <strong>of</strong> the dopaminergic system.<br />
Furthermore, relatively high doses <strong>of</strong> psycho stimulants induce stereotypical self-injurious behavior (SIB) in<br />
rodents. The combination <strong>of</strong>psycho stimulants and opioids is quite common and is reportedly used to produce<br />
a more intensely pleasurable "rush". Therefore, some investigators have sought to characterize the<br />
interactions <strong>of</strong> these psychostimulants and opioids. However, the effects <strong>of</strong> opioids on dopamine-related<br />
behavior, especially psychostimulant-induced SIB, remain to be fully elucidated. The present study was<br />
designed to investigate the effects <strong>of</strong> j.l.-, 0- and K-opioid receptor agonists (morphine (5.0 - 20 mg/kg, s.c.),<br />
SNC80 (1.25 - 5.0 mg/kg, s.c.) and U50,488H (1.0 - 10 mg/kg, Lp.), respectively) and buprenorphine (0.125<br />
- 2.0 mg/kg, s.c.) on methamphetamine-induced SIB. After the administration <strong>of</strong> methamphetamine, SIB,<br />
especially skin-picking behavior or self-biting around the chest, was measured for 3 min at 15 min intervals.<br />
A score <strong>of</strong> 0 was given for inactivity <strong>of</strong> SIB-like behavior, 1 for very mild SIB (less than 1 min), 2 for at least<br />
1 min <strong>of</strong> SIB, 3 for continuous SIB through 3 min. Methamphetamine (20 mg/kg) induced SIB in 6 out <strong>of</strong>7<br />
ddY mice, while· in the combination test, the opioid receptor agonists significantly attenuated<br />
methamphetamine-induced SIB. The relative potency <strong>of</strong> these opioids in attenuating<br />
methamphetamine-induced SIB was morphine> buprenorphine > U50,488H » SNC80. These results<br />
suggest that the stimulation <strong>of</strong> j.l.- and K- (particularly j.l.-) opioid receptors exerts an inhibitory effect on<br />
stereotyped high-dose methamphetamine-induced SIB in mice.<br />
Keywords: Self-injurious behavior; Methamphetamine; Opioid<br />
Page 213
B15 <br />
LONG-TERM ROADSIDE SURVEYS FOR DRUNKEN DRIVING IN FINLAND<br />
M Portman l .., A Penttila\ K Kuoppasalmil, P Lunetta 2 ,P Nevala 3 : lNational Public Health Institute<br />
Helsinki 2Department <strong>of</strong>foren sic Medicine, University <strong>of</strong> He\sinki 3The Mobi\e Police, Helsinki '<br />
Numerous reports have shown that the rate <strong>of</strong> drunken driving declined worldwide in the 1980s.<br />
Nevertheless, drunken driving is still a considerable factor in fatal motor vehicle accidents. In 2002, 415<br />
persons were killed in road traffic accidents in Finland (population 5.2 millions). In these accidents the<br />
number <strong>of</strong>fatalities involving drunken drivers was 91 (21.9%), whereas 12 persons (2.9 %) were killed in<br />
accidents involving other intoxicants than alcohol. Annual roadside surveys have been carried out since<br />
1978 in the province <strong>of</strong>Uusimaa in southern Finland to determine the incidence <strong>of</strong>drivers who had been<br />
drinking. The statutory limit <strong>of</strong> blood alcohol concentration for drunken driving in Finland is 0.5 0/00<br />
(glkg). The police can make a demand for a driver's breath sample to be tested for the presence <strong>of</strong> alcohol<br />
even in the absence <strong>of</strong>obvious signs <strong>of</strong>drunken driving. Annually a total <strong>of</strong>about 30000 drivers have been<br />
breath tested. The surveys have been carried out using the same protocol and, therefore, the results obtained<br />
from year to year are comparable. The surveys take place on three Tuesdays and three Saturdays during<br />
both spring and autumn. These days are chosen to represent one weekday and one day <strong>of</strong> the weekend.<br />
Every survey consists <strong>of</strong>4-5 roadblocks, each lasting 30-40 minutes. The roadside survey team includes<br />
one chief inspector, 8-14 police <strong>of</strong>ficers, one physician and a few assistants. The driver <strong>of</strong> every motor<br />
vehicle is breath tested with an Alcometer PST-MIR (Lion Laboratories Ltd., Cardiff, U.K.) or an<br />
Alcosensor IIIR (lntoximeters Inc., Saint Louis, Missouri, U.S.) screening device. The incidence <strong>of</strong><br />
drunken drivers has been 0.2 % since the beginning <strong>of</strong>the 1990s. The percentage <strong>of</strong> drivers with an alcohol<br />
concentration below the statutory limit has been 0.4 % during the 1990s and since 2000 a rising trend has<br />
been observed. In 2003 the frequency was 1.01 %. A possible explanation for the observed rise is that the<br />
attitude, especially <strong>of</strong> young drivers, has changed, resulting in an increase in the number <strong>of</strong> cases involving<br />
low blood alcohol concentrations. More and more young drivers recognize that while dining in restaurants<br />
or attending parties they can consume one to two beers or ciders while their blood alcohol concentration<br />
can remain safely below the statutory limit <strong>of</strong>0.5 0/00. The coming years will show whether the recent<br />
significant increase in Finland <strong>of</strong> drivers with low alcohol content is a permanent trend or not. The taxes <strong>of</strong><br />
alcohol beverages were substantially lowered in March this year, which may well contribute to<br />
maintaining, or accelerating this trend.<br />
Keywords: drunken driving, roadside survey, breath testing<br />
Page 214
B16 <br />
AMELIORATION OF LEAD TOXICITY WITH VITAMIN C AND SILYMARIN SUPPLEMENTS<br />
Shalan, M.G.*l; Mostafa, M.S.2; Hassouna, M.M; Hassab EI-Nabi, S.E. J , EI-Refaie, A.4: lBiological and<br />
Geological Sciences Dept., AI-Arish Faculty <strong>of</strong> Education, Suez Canal University, Egypt. 2Clinical<br />
Pathology Dept., National Liver Institute, Menoufiya University, Egypt. 3Zo010gy Dept., Faculty <strong>of</strong><br />
Science, Menoufiya University, Egypt. 4Pathology Dept., National Liver Institute, Minoufiya University,<br />
Egypt.<br />
The aim <strong>of</strong>the present study was to investigate the impact <strong>of</strong> the combined administration <strong>of</strong>vitamin C and<br />
silymarin on lead toxicity. Male albino rats were subdivided into 3 groups; the first was a control group, the<br />
second received lead acetate in the diet as 500 mg/Kg diet daily, the third received the same lead acetate<br />
dose and supplemented with vitamin C (I mg/IOO g body weight) and silymarin (I mg/lOO g body weight)<br />
by gastric tube 3 times per week. Blood samples were taken after 2,4 and 6 weeks <strong>of</strong>treatment. Significant<br />
lead-induced elevations in serum AL T, AST, GGT and ALP activities were observed after different periods<br />
<strong>of</strong> treatment. However serum LDLc was decreased. The intensities <strong>of</strong> RNA and apoptotic fragments <strong>of</strong><br />
DNA were measured as optical density by the Gel-pro program. Lead acetate decreased the intensity <strong>of</strong><br />
DNA at 6 weeks and induced apoptotic DNA fragments reversibly with time. After two weeks <strong>of</strong> lead<br />
administration dilation and congestion <strong>of</strong> terminal hepatic veins and portal vein branches were observed.<br />
Lead also induced hepatocyte proliferation without any localized distribution among zones 1,2,3. Portal<br />
inflammatory infiltrate with disruption <strong>of</strong> the limiting plates (interface hepatitis), steatosis, apoptosis and<br />
mild fibrosis were detected especially by sixth week <strong>of</strong> lead administration. Combined treatment <strong>of</strong> leadexposed<br />
animals with vitamin C and silymarin showed marked improvement <strong>of</strong>the biochemical, molecular<br />
and histopathological findings. These experimental results strongly indicate the protectiVe effect <strong>of</strong>vitamin<br />
C and silymarin against toxic effects <strong>of</strong> lead on liver tissue.<br />
Keywords: Lead, vitamin C, silymarin, liver, serum<br />
Page 215
B17 <br />
DFSA-REPORTED INCIDENTS IN THE UK AND THE MELLANBY EFFECT<br />
Mark Tyler* : Culham Science Centre, Abingdon, United Kingdom<br />
A study <strong>of</strong> 41 cases <strong>of</strong> drug-facilitated sexual assault (DFSA) in 2003 from 2 separate areas <strong>of</strong> the United<br />
Kingdom has shown some interesting trends. The vast majority (38) <strong>of</strong> complainants were female, 28 were<br />
under 30 years <strong>of</strong> age, and 30 <strong>of</strong> the alleged incidents occurred between 21:00 hours and 03:00 hours.<br />
Perhaps more significantly, 35 <strong>of</strong> the cases were alcohol-related. Apart from drugs <strong>of</strong> abuse (mainly<br />
cannabis) found in 16 cases, none <strong>of</strong>the so-called DFSA drugs (Rohypnol, GHB, sedatives) were detected.<br />
These findings echo previously published data (EISohly et aI, 1999) indicating that alcohol is the common<br />
denominator in these cases.<br />
The intensity <strong>of</strong> the CNS effects <strong>of</strong> alcohol are proportional to the blood alcohol concentration (BAC), as<br />
described by Dubowski in 1997, but as noted by Mellanby in 1919, the effects are far more pronounced as<br />
the BAC is rising as compared to when the BAC is falling. In addition, as the rate <strong>of</strong>alcohol ingestion rises,<br />
the greater the degree <strong>of</strong> intoxication (Moskowitz et al 1977).<br />
The number <strong>of</strong> reported "DFSA" cases in the UK has risen dramatically over the past 5 to 10 years. During<br />
a similar period, the UK has seen a steep increase in the availability and popularity <strong>of</strong> 'alcopop' drinks<br />
(bottles <strong>of</strong> brightly coloured drinks typically containing vodka and lemonade or other fruit flavours,<br />
designed to appeal to younger drinkers), plus a wider variety and choice <strong>of</strong> strong beers, and larger<br />
measures <strong>of</strong> wine and spirits in public houses. There is now government concern and a rising awareness <strong>of</strong><br />
"binge-drinking" amongst young people in the UK. All <strong>of</strong> these factors may just be coincidence, but it<br />
would appear that changing drinking habits and greater CNS intoxication associated with a rapid BAC rise,<br />
might be responsible for the majority <strong>of</strong>these DFSA allegations.<br />
Key words: DFSA, alcohol, Mellanby<br />
Page 216
·Scientific Session <br />
<strong>Abstracts</strong>: <br />
Clinical and <br />
Environmental. <br />
Toxicology <br />
Page 217
Cl<br />
THE VOLUNTARY DETOXIFICATION PROGRAMME - A SURVEY OF THE EFFICIENCY<br />
V.Vorisekl' ,J.Cizek 2 , V.Palicka l<br />
I Institute <strong>of</strong>Clinical Biochemistry and Diagnostics, University Hospital and Medical Faculty <strong>of</strong> Charles<br />
University, Hradec Kralove; 2Detoxification Centre, Department <strong>of</strong> Psychiatry, University Hospital, Hradec<br />
Kralove, Czech Republic<br />
Aims: The object <strong>of</strong> this survey was to evaluate the effectiveness <strong>of</strong> our detoxification strategy for future<br />
planning and corrections on the basis <strong>of</strong> the analytical results. Methadone and buprenorphine programme<br />
applied to opiate and amphetamine abusers in the detoxification centre for north-east area <strong>of</strong> the Czech<br />
Republic ( Hradec Kralove county) is based on the voluntary and liberal principle. However a common<br />
problem related to this approach is a relapse to drug abuse. Detection <strong>of</strong> the key analytes<br />
(methylamphetamine, amphetamine,MDMA, MDA, 6-MAM, morphine, codeine, acetylcodeine and<br />
cannabinoids, especially ll-nor-delta-9-tetrahydrocannabinolic acid) in urine specimens is the decisive<br />
cause <strong>of</strong> definitive or temporary discharge from the treatment according to the individual status <strong>of</strong> patient<br />
and all case consequencies.<br />
Methods: A total <strong>of</strong> 3464 urine specimens randomly collected from 85 patients admitted to programme ( 70<br />
males, 15 females, aged 19 to 43) over an 8-year (1996-2003 ) period were screened for illicit drug use,<br />
especially for opiates and amphetamines. The screening analyses were carried out by immunochemical<br />
methods (EMIT II) and full-automatic HPLC-UV procedure ( REMEDi HS Drug Pr<strong>of</strong>iling System ). The<br />
confirmations were performed by GC-MS (Magnum MAT Finnigan). A total <strong>of</strong> 25600 tests were done.<br />
Extraction procedures before GC-MS acquisition were carried out by solid phase extraction devices with<br />
reagents containing ethyl acetate, acetone, methylene chloride, 0.01 M acetic acid, methanol and<br />
ammonium hydroxide. Bond Elute CertifY II columns were used for the extraction <strong>of</strong> amphetamines and<br />
opiates after enzymatic hydrolysis with p- glucuronidase at 60°C for 3 hours. Positive samples for cannabis<br />
afterdeconjugation with lIN potassium hydroxide were extracted on SPEC CI8 AR columns.<br />
Amphetamines and opiates were detected simultaneously in one analysis in the form <strong>of</strong><br />
pentafluoropropionyl derivatives (PFPA reagent).Cannabinoids were derivatized with BSTFA + TMCS<br />
(99+1) mixture. Samples for evidence <strong>of</strong> psilocine abuse were extracted on SPEC MPI mixed disc and<br />
derivatized with acetic anhydride in pyridine in the ratio <strong>of</strong> 3:1 (LOD IOng/mL). The chromatographic·<br />
separations were achieved on a DB5ms fused-silica capillary column (30m x 0.25mm x 0,25J.lm film<br />
thickness) using helium as carrier gas at lml/min flow rate.<br />
Results: It was found that the commonest illicit drug detected in this programme was cannabis ( 20%)<br />
followed by opiates (9.9 % ) and amphetamines (9 %). Other classes <strong>of</strong> illicit drugs (cocaine, LSD and<br />
psilocine) were not detected.<br />
Conclusions: Specimens tested positive for opiates and amphetamines showed decreasing tendency during<br />
the whole period <strong>of</strong> the detoxification programme but specimens tested positive for cannabinoids were<br />
stable over time. It seems to be problem concerning the number <strong>of</strong> positives because positive results for<br />
cannabis caused temporary discharge from treatment. In addition to this problem we have to admit that GC<br />
MS such as Magnum does not able to <strong>of</strong>fer sufficient analytical sensitivity for LSD analysis. A cut-<strong>of</strong>f<br />
value <strong>of</strong> LSD immunochemical assay is 1 ng/ml but LOD for our GC-MS procedure was 25 ng/ml after<br />
silylation with BSTFA + TMCS, 99 + 1). However, methylamphetamine and heroin users mostly prevailed.<br />
Therefore LSD did not belong to main drugs <strong>of</strong> abuse in this controlled group <strong>of</strong> abusers. Positive results<br />
for LSD above a cut-<strong>of</strong>f value were not obtained. Nevertheless in spite <strong>of</strong> these facts the analytical data<br />
derived from this survey give relative satisfaction and demonstrate the high level <strong>of</strong> effectiveness <strong>of</strong> this<br />
manner <strong>of</strong> drugs <strong>of</strong> abuse therapy.<br />
Keywords: drugs <strong>of</strong> abuse, substitution therapy, detoxification programme<br />
Page 218
C2 <br />
PARADOXICAL RESULTS FROM SCREENING FOR URINARY 6-AM AND OPIATES WITH<br />
DIFFERENT IMMUNOASSA YS IN A HEROIN SUBSTITUTION TREATMENT POPULATION<br />
Ol<strong>of</strong>Beck and Michael Boettcher*<br />
Department <strong>of</strong> Medicine, Division <strong>of</strong> Clinical Phannacology, Karolinska University Hospital, Stockholm,<br />
Sweden. * Arztpraxis rur Medizinische Mikrobiologie, Labordiagnostik und Hygiene, Dessau, Gennany<br />
Identification <strong>of</strong> 6-Acetylmorphine (6-AM) in urine samples is regarded as an unequivocal pro<strong>of</strong> <strong>of</strong> recent<br />
heroin abuse. Due to its short elimination half-life <strong>of</strong> about 30min, 6-AM normally cannot be detected for a<br />
longer period than 24 hours after heroin consumption. In addition, it is generally assumed that the<br />
metabolite morphine and its glucuronidated fonns can be detected much longer. Therefore, the presence <strong>of</strong><br />
6-AM in urine samples at detectable levels is only expected together with high total morphine<br />
concentrations.<br />
Since the availability <strong>of</strong> the 6-AM CEDIA (Microgenics) we started to test opiate-CEDIA (Microgenics)<br />
positive samples with the 6-AM assay before GCIMS analysis for 6-AM is conducted. This is done<br />
semiquantitatively on a Hitachi 911 with calibrators at 0, 5, 10 and 20nglmL applying a cut<strong>of</strong>f at 5nglmL.<br />
Quantitative results within the measuring range <strong>of</strong> the 6-AM CEDIA mostly correlate well with the data <strong>of</strong><br />
GCIMS but are discrepant when increased amounts <strong>of</strong> free morphine are present in the sample. This crossreactivity<br />
<strong>of</strong> free morphine (~0.06%) can even lead to false positive results especially for samples from<br />
patients substituted with morphine.<br />
As we always screen urine samples from dihydocodeine substituted patients with the 6-AM CEDIA instead<br />
<strong>of</strong> opiate-CEDIA we wanted to learn if there are any other cross-reactive drugs increasing the 6-AM<br />
CEDIA result or can lead to false positives. We therefore run the 6-AM test together with the opiate<br />
CEDIA and opiate-DRI (Microgenics) on every urine sample from substituted patients on 49 consecutive<br />
workdays (3696 samples). No false positive results were found with the 6-AM assay. However, in 29<br />
(0.8%) samples from 23 different patients (9 females, 14 males) paradoxical results were observed with<br />
positive 6-AM CEDIA results (>5ng/mL) and negative (cut<strong>of</strong>f 100nglmL) or low positive results<br />
«400ng/mL) in the opiate tests. The DRI and CEDIA opiate immunoassays gave similar results.<br />
Interestingly all the samples analysed were confinned to be 6-AM positive with only small or undetectable<br />
amounts <strong>of</strong> free morphine. There were only two discrepant samples where the concentration <strong>of</strong> 6-AM<br />
found with GCIMS (9.3ng/mL, 2.5ng/rnL) was significantly lower than expected from the 6-AM CEDIA<br />
assay (both samples >20ng/mL). An additional cross-reactive substance or perhaps cross-reacting 6-AM-3<br />
glucuronide may be assumed. Ongoing investigations with LC-MS-MS will look for 6-AM-3-glucuronide<br />
and morphine-3- and morphine-6-glucuronide in all 29 samples.<br />
Conclusion: Positive screening results for urinary 6-AM as a pro<strong>of</strong> for very recent heroin abuse should be<br />
looked at very carefully and always in the context <strong>of</strong>total morphine concentration.<br />
Keywords: 6-AM, opiates, CEDIA<br />
Page 219
C2 <br />
..~<br />
no.<br />
substitute, dose<br />
[mg/day]<br />
creatinine<br />
[mg/dL]<br />
6-AMCEDIA<br />
>5 ng/mL<br />
Opiates-CEDIA<br />
[ng/ml)<br />
Opiates-DRI<br />
[ng/ml]<br />
"tree" 6-MAM GC/MS<br />
[ng/ml]<br />
free Morphine GC/MSI<br />
Ing/ml] .<br />
1 M14 66 16.0 41 42 18.5 1.5<br />
2 M4 91 >20 197 148 30.0 7.9<br />
3 M6 15 >20 85 54 20.7 20 212 212 9.3 37.0<br />
5 M13 14 >20 81 60 25.0 14.0<br />
6 M8 14 >20 125 119 35.3 41.5<br />
7 M17 52 >20 80 69 58.6 3.1<br />
8 M7 0 >20 217 203 n.t. n.t<br />
9 M5 106 >20 114 77 19.7 20 354 308 45.9 20 115 107 n.f. n.f.<br />
26 M16 14 >20 72 49 n.f. n.f.<br />
27 M3.5 33 >20 80 55 nJ. n.t.<br />
28 M4 74 >20 169 151 n.t. n.f.<br />
29 P2 132 >20 113 75 n.f. n.t.<br />
M = Methadone<br />
P = Polamidone<br />
B = Buprenorphine<br />
n.t. = not yet 'finished<br />
Page 220
C3 <br />
ALUMINUM TESTING IN TRACE-METAL FREE CONTAINERS<br />
Lee M. Blum*, Ela Bakowska, Gulo Gigolashvili<br />
National Medical Services, Inc., Willow Grove, PA<br />
The testing <strong>of</strong> biological samples for elemental analyses can be quit challenging. Specimen collection is a<br />
critical aspect <strong>of</strong> these tests. Proper specimen collection procedures are necessary in ascertaining an analytical<br />
result that is truly reflective <strong>of</strong> the amount <strong>of</strong> determinant in the specimen. Contamination <strong>of</strong> the specimen is a<br />
considerable problem especially in the analysis <strong>of</strong> trace metals. The results <strong>of</strong> analysis <strong>of</strong> blood and urine<br />
specimens can be misleading if proper precautions are not taken to minimize sample contamination. Because <strong>of</strong><br />
the prevalence <strong>of</strong> aluminum in our environment, the collection <strong>of</strong> specimens without precautions can lead to<br />
misinterpretation. Contamination may come from the patients themselves, the procedures and devices used in<br />
the specimen collection, and/or the laboratory performing the test (including particles and dusts in the air or<br />
reagents used in the analysis). Specimen collection tubes are a known source <strong>of</strong> contamination. The source <strong>of</strong><br />
the contamination may be from the glass, the stopper, and/or the specimen preservative in the tube. Aluminum<br />
testing in biological samples is important for assessing occupational/environmental exposures and for clinical<br />
monitoring <strong>of</strong> renal dialysis patients, among others. The accumulation <strong>of</strong> aluminum in the body can increase the<br />
risk <strong>of</strong> neurotoxicity ("dialysis encephalopathy"), bone disease and renal failure. This study examined the<br />
effectiveness <strong>of</strong> specially manufactured trace-metal free specimen collection tubes in the determination <strong>of</strong><br />
aluminum. Specimens were collected consecutively in trace-metal free tubes containing no preservative<br />
(serum), and trace-metal free tubes containing either heparin (plasma) or EDTA (plasma) as preservatives. The<br />
aluminum concentrations were determined under identical conditions by inductively coupled plasma/mass<br />
spectrometry (ICPIMS) with a reporting limit 0{5 mcg/L.<br />
A summary <strong>of</strong> the serum and plasma aluminum findings (mcg/L) is listed below:<br />
I<br />
Serum Aluminum I Heparinized Plasma EDTA Plasma<br />
I<br />
i Patient<br />
Aluminum<br />
Aluminum<br />
I A 8 6 II<br />
B 11 13 11<br />
C 5 7 57<br />
D 8 7 6<br />
I E 7 13 110<br />
F 8 19
C4 <br />
THE ENVIRONMENTAL IMPACT OF LEAD, CHROMIUM, ZINC AND CADMIUM PRESENT<br />
IN RUBBISH DUMP<br />
C.H. Colangelo*I,2,3 ,L.A. Ferrari 1,3 ,J.C. Chaumeil l , C.A. Seminario Correal, S. Georgeri l<br />
1. Laboratorio de Toxicologfa y Quimica Legal * Direcci6n General de Asesorias Periciales - Suprema<br />
Corte de Justicia de la Provincia de Buenos.Aires Calle 41 e/119 y 120 La Plata (1900) - Buenos<br />
Aires Republica Argentina .,2. University <strong>of</strong> La Pampa - Argentina, 3. University <strong>of</strong> Moron Argentina<br />
Lead, Chromiun, Zinc and Cadmiun concentrations in differents environmental matrixes (soils, drinking<br />
underground waters, surfaces waters and edibles fresh vegetables such as celery and lettuce) collected at<br />
selected areas near a rubbish dump located at Buenos Aires Province in Argentina were analyzed.<br />
The above mentioned samples were conditioned for their analysis by atomic absorption spectrophotometry.<br />
Soils and vegetables samples were first treated by microwave digestion with nitric acid, and then metal<br />
concentrations were determinated by aspiration in flame <strong>of</strong> air* acetylene technique.<br />
Water samples were analyzed by using a graphite oven.<br />
The following table shows the metal concentrations obtained for the different samples:<br />
Samples<br />
Lead Chromium Zinc Cadmium I<br />
ppb 1>pb ppb<br />
i<br />
..I!Pb<br />
Underground water 1 (e) 140 70 23
C5 <br />
DETECTION OF NITRAZEPAM USING ION MOBILITY SPECTROMETRY<br />
G. Jayashanker*, N.V.R.Kiran, A.K.Srivastava, M.Afzal, R.K.Jain,P.Samikannu, S.Sudhakar, R.K.Sarin.<br />
Central <strong>Forensic</strong> science laboratory, MHA, Govt. Of India, Ramanthapur, Hyderabad-India 500013.<br />
Ion Mobility Spectrophotometer (IMS) has been used as a rapid sensitive and selective technique for the<br />
detection <strong>of</strong> Nitrazepam in body fluids. Nitrazepam an tranquillizer is <strong>of</strong>ten misused/abused in criminal<br />
activities like theft, robbery, rape etc. The detection <strong>of</strong> specific compound in body fluid determines the drug<br />
administered in such cases. The standard routine procedures are time consuming. In this study IMS was<br />
used as rapid technique to detect Nitrazepam. The IMS utilizes the fact that a mixture <strong>of</strong> different ions may<br />
be separated into individual components as they travels at different velocities [mobilities] under the<br />
influence <strong>of</strong>an electric field, through a tube containing the drift gas.<br />
The case <strong>of</strong> a lady being sexually assaulted and found unconscious was brought to the hospital by police for<br />
treatment. The clinical symptoms <strong>of</strong> being drugged could be observed and the stomach wash collected and<br />
sent to the forensic lab for testing. The routine drug screening was followed and simultaneously a portion<br />
<strong>of</strong> the sample was subjected to IMS screening. The ion mobility <strong>of</strong> standard Benzodiazepines like<br />
Diazepam, Flurazepam, Nitrazepam were carried and the drift time and Ko value was noted.<br />
SINo Sample Drift time Ko<br />
1. Calibration 9.044 1.86<br />
2. Diazepam 13.79 1.213<br />
3. Flurazepam 16.44 1.023<br />
4. Nitrazepam 16.55 1.016<br />
5. Sample 16.55 1.016<br />
I<br />
I<br />
I<br />
I<br />
The exhibit was analysedand the drift time and Ko value could be matched with Nitrazepam. The standard<br />
screening procedure <strong>of</strong> Acidic and basic fraction analysis by GC-MS also confirmed the Nitrazepam. The<br />
standard solution <strong>of</strong> diazepam was studied for the limit <strong>of</strong> detection with 50 ng solution. The selectivity <strong>of</strong><br />
the method for the drug identification can be only compared with the standard samples ion motilities<br />
analysed sequentially with samples as the drift times <strong>of</strong>different compounds may overlap on the same. The<br />
IMS technique could detect the Nitrazepam even in the gastric lavage directly put on the sample holder <strong>of</strong><br />
IMS. The interference from the direct analysis had no shift in the peaks. The IMS was found to save time,<br />
simple and easy technique to detect drugs <strong>of</strong> abuse. The procedure can be used to screen for the presence<br />
<strong>of</strong> Benzodiazepine group <strong>of</strong> drugs in routine analysis and is an additional analytical corroboration in the<br />
analysis <strong>of</strong>drugs.<br />
Key words: IMS, Toxicology, Drug-facilitated sexual assault<br />
Page 223
C6 <br />
MEPROBAMATE OVERDOSE: A ONE-YEAR EVALUA TION OF REPORTS<br />
Fabienne Pehourcq <br />
Laboratoire de Pharmacologie, Universite Victor SegaJen, 33076 Bordeaux, France. <br />
Meprobamate is a mild sedative-hypnotic drug used in therapy since the 1955s. An overdose with this drug,<br />
even taken alone, may cause severe or even fatal respiratory depression, hypotension, shock, and heart<br />
failure. This drug is widely known in France, particularly for use in suicide attempts.<br />
One hundred and fifty-three cases <strong>of</strong> meprobamate intoxication were admitted to the emergency room <strong>of</strong><br />
our hospital during one year. In these patients, the plasma concentrations <strong>of</strong> meprobamate measured by gas<br />
chromatography after liquid-liquid extractions were above the therapeutic level <strong>of</strong> 15 mgIL. Ninety-seven<br />
intoxicated patients (63%) were female. The age <strong>of</strong> the patients studied was 14-75 years (mean ± SD, 42.2<br />
± 12.7). The mean age for females (43.7 ± 13.1) was significantly greater than that for males (39.6 ± 11.6)<br />
(p< 0.05). Most (58%) <strong>of</strong> the patients arrived in the emergency room during the time period 6:00 PM to<br />
6:00 AM. Among these 153 hospitalized patients, meprobamate was detected 95 times at concentrations<br />
above the toxic level <strong>of</strong> 50 mgIL. Thirty-two patients (21 %) presented with concentrations in the range <strong>of</strong><br />
100-200 mgIL; Six cases <strong>of</strong> overdose were described with meprobamate levels greater than 200 mgfL; and<br />
among them, three voluntary intoxications were fatal (1.96%). One third <strong>of</strong> the cases turned out to be<br />
combined intoxications, 82% <strong>of</strong> the patients also took benzodiazepines. Most poisonings took place in the<br />
first quarter <strong>of</strong>the year.<br />
In comparison with older studies, the pattern <strong>of</strong> meprobamate poisoning does not appear to have change in<br />
France over the last 25. years. An overdose with this drug, even when taken alone, produces intoxication<br />
that is <strong>of</strong>ten serious and sometimes fatal. The questionable efficacy <strong>of</strong> meprobamate as a selective antianxiety<br />
agent and its potential for life-threatening intoxication are important drawbacks to the clinical use<br />
<strong>of</strong>this drug.<br />
Keywords: meprobamate, overdose, epidemiology<br />
Page 224
C7 <br />
METHCATHINONE: A NEW POSTINDUSTRIAL DRUG<br />
H.Belhadj-Tahar 1 ' ,N.Sadeg 2<br />
1. Groupe Sante Recherche Toulouse, 35 rue Bernard de Ventadour, 31300 Toulouse, France.<br />
2. Laboratoire Claude Bernard, Centre Hospitaiier Rene Dubois, 95303 Pantoise, France.<br />
Methcathinone is an illicit drug also known as ephedrone, which is a methyl derivative <strong>of</strong> cathinone, a<br />
stimulant found in the « khat» plant, Catha edulis, and which can be easily manufactured by oxidation<br />
from pseudoephedrine. Target consumers <strong>of</strong> this drug seem to be well-educated people aware <strong>of</strong> the risks<br />
and precautionary measures 1 • Therefore, it is difficult to diagnose and to cure properly and it becomes even<br />
more complicated as there are misleading symptoms related to intoxication by cathinone derivatives <strong>of</strong><br />
synthetic or natural (derived from the khat) origin. Thus far, reports <strong>of</strong> methcathinone intoxication<br />
documented and based on reliable analyses are rare since it is not systematically detected. This paper<br />
describes a case <strong>of</strong> reiterated coma due to an overdose <strong>of</strong> pure methcathinone dissolved in alcohol and<br />
mixed with bromazepam.<br />
Case report: At 10 pm, a 29-year-old woman was admitted in emergency department from Paris suburbs<br />
for a coma <strong>of</strong> toxic origin. Medical history showed that it is the second episode occurring under similar<br />
circumstances and at one month interval. In both cases, the patient took Lexomil® dissolved in alcohol.<br />
Besides, the family indicated that the patient presented signs <strong>of</strong> depression, incoherent behavior. She is an<br />
amphetamine-like drug consumer. Clinical examination revealed a Glasgow coma score 9 and symmetrical<br />
reactive pupils with mydriasis. The patient presented a polypnoea. Her blood pressure was 93/53mmHg.<br />
The rest <strong>of</strong>the examination was unremarkable.<br />
Biological check-up: the ionogram and the blood gas analyses were normal, the blood alcohol level was<br />
1.67 gIL. Urinalysis revealed benzodiazepines, pH 5.4, along with a high concentration <strong>of</strong> amphetamines<br />
dosed by FPIA (Axsym, Abbott - USA) and identified by HPLC (Remedi, Biorad USA) as follows:<br />
methcathinone (17.24 mglL), ephedrine (11.60 mglL) and methylephedrine (1 LIO mglL). Serum analysis<br />
by HPLC revealed concentrations <strong>of</strong> bromazepan (8.89 mglL), methcathinone (0.50 mgIL) and<br />
methylephedrine (0.19 mgIL). The patient was kept in quiet room: the hemodynamic and neurological<br />
functions evolved quite favourably in the next hours.<br />
Discussion: This case illustrates a coma mainly due to a combined bromazepam and methcathinone<br />
intentional intoxication. This coma is not only ascribable to bromazepam and ethanol. Indeed, on one hand,<br />
the blood alcohol level at 1.67 gil, the absence <strong>of</strong> anionic and basic deficit related to an acetate outbreak<br />
eliminates the hypothesis <strong>of</strong> ethylic coma and, on the other hand, the paradoxical presence <strong>of</strong> polypnoea<br />
instead <strong>of</strong> respiratory distress eliminates the hypothesis <strong>of</strong> a coma due to benzodiazepine overdose.<br />
Therefore, we can affirm that cathinone altered typical clinical symptoms <strong>of</strong> bromazepamlalcohol<br />
intoxication, namely hypotension and respiratory distress. Methylephedrine detection at infratoxic doses<br />
could be a chemical precursor resulting from the alkylation <strong>of</strong> primary amine for monomethylamine<br />
(pseudoephedrine) and dimethylamine (methyl ephedrine) synthesis (Belhadj-Tahar H. et al. Therapie,<br />
2003,59: 265-271). It seems to be chemical tag <strong>of</strong> a fraudulent origin.<br />
Conclusion: This case describes an example <strong>of</strong> a new addictive behaviour <strong>of</strong> "well educated" people<br />
involving the intake <strong>of</strong> methcathinone, a postindustrial psychostimulant intentionally combined with anticonvulsant<br />
benzodiazepine.<br />
Keywords: methcathinone, ephedrone, illicit drug<br />
Page 225
C8 <br />
. ANALYSIS OF METHYLPHOSPHONIC ACID AND ISOPROPYLMETHYLPHOSPHONIC<br />
ACID, A METABOLITE OF SARIN NERVE GAS, BY TANDEM GC MASS SPECTROMETRY<br />
AND POSITIVE CHEMICAL IONIZATION<br />
Eric Phillips, Jessie Crockett Butler*, Trisa Robarge, and Meredith Conoley. Thermo Electron, 2215 Grand<br />
Ave Pkwy, Austin, TX 78728-3812<br />
The two primary metabolites <strong>of</strong> the nerve agent sarin are methylphosphonic acid (MPA) and<br />
isopropylmethylphosphonic acid (IPMPA). They are analyzed by GCMS after derivatization with BSTFA.<br />
In positive chemical ionization mode using isobutane, the MH+ ion <strong>of</strong>the derivatized compound is isolated<br />
and then fragmented into product ions for structural elucidation. Blank samples <strong>of</strong> urine, cleaned up by<br />
solid phase extraction, were spiked with commercially available MPA and IPMPA. The linearity and<br />
detection limits <strong>of</strong> the method were determined in urine using IPMPAd7 as an internal standard. Multiple<br />
scan events were set up to perform sequential Full Scan and MSIMS; The linear fit for MPA-TMS was R2=<br />
1.000 (Full Scan) and 0.9982 (MSIMS/MS) and for IPMPA-TMS, R2 = 0.9990 (Full Scan) and 0.9978<br />
(MS/MS) with a precision <strong>of</strong>5.1% RSD for the internal standard (IPMPA-d7-TMS). The precision for the<br />
internal standard for 60 replicate injections <strong>of</strong> spiked urine was 9.5 %RSD. The instrument <strong>of</strong> analysis was<br />
the external source quadrupole ion trap with a temperature programmable injector. Mass Frontier s<strong>of</strong>tware<br />
was used to predict the MS/MS product ions for assistance in the selection <strong>of</strong> a precursor ion <strong>of</strong> the<br />
derivatized target compounds.<br />
Keywords: Ion trap, MSIMS, nerve gas<br />
Page 226
C9 <br />
A PROPOSED SCHEME FOR FOXY METABOLISM<br />
JM Wilson*\ F McGeorge l , R Meatherale. <br />
l.Dept <strong>of</strong> Clinical Pathology and Emergency Medicine, William Beaumont Hospital, Royal Oak, MI USA. <br />
2. St. Boniface General Hospital, Winnipeg, Manitoba CAN.<br />
We report an emergency room admission following an ingestion <strong>of</strong> 5-Methoxy-N,N-diisopropyItryptamine,<br />
5-MeO-DIPT or FOXY. The subject was a 23 year old Caucasian male presenting 3 hours post ingestion<br />
<strong>of</strong> a capsule provided by an acquaintance and initially described as "acid". This ingestion was preceded by<br />
intake <strong>of</strong> 4 beers. Approximately thirty minutes before presentation the subject experienced four episodes<br />
<strong>of</strong> vomiting followed by tactile hallucinations and paranoia, primarily related to a suspicion <strong>of</strong> being<br />
poisoned. He denied auditory and visual hallucinations or other neurological symptoms. Vital signs<br />
revealed a temperature <strong>of</strong> 31 "C, pulse 16 bpm, respirations 18 per min and blood pressure <strong>of</strong> 135170 mm<br />
Hg. Pupils were midpoint and reactive with normal neurological, motor, reflex, cardiovascular and<br />
gastrointestinal function. Blood and urine chemistry and hematology results were not revealing. Urine<br />
toxicology screening reported presence <strong>of</strong> 5-MeO-DIPT and suspected metabolites. The subject received<br />
activated charcoal, intravenous fluids, three additional hours <strong>of</strong> supportive care with resolution <strong>of</strong> his initial<br />
condition and was discharged without complaints or subsequent readmission.<br />
Urine toxicology testing involved initial screening by ToxiLab® (Varian Inc, Lake Forest CA) followed by<br />
confirmation by electron impact GC/MS. Toxi-A revealed three spots at RF 2.4, 4.6,6.1 (S 1 all blanch, S2<br />
4.6 tan, others faded, S3 all UV absorption, S4 all brown). Extraction for confirmation was preceded by<br />
combination <strong>of</strong> 2 mL <strong>of</strong> urine, 0.5 mL <strong>of</strong> 1 N sodium hydroxide, 500 ng <strong>of</strong> internal standard (SKF-525-A)<br />
and 5 mL <strong>of</strong> dichloromethane. Mixing, separation <strong>of</strong> the organic layer, evaporation under an air stream at<br />
45 "C in a water bath was followed by reconstitution with 25 ilL <strong>of</strong> ethy I acetate. One ilL <strong>of</strong> the extract<br />
was injected for GCIMS analysis on a Hewlett Packard 5912A Mass Selective Detector equipped with a 30<br />
m, 0.25 mm id DB-5® (Agilent Technologies, Wilmington DE) capillary gc column with a 0.25 Ilm film<br />
thickness using splitless injection. Oven temperature was initially 120 "C for 3 min, raised to 225°C at 10<br />
"C per min and held for 5 min, followed by a second temperature increase to 300 "C at 15°C per min and a<br />
3 min hold.<br />
Electron impact GCIMS data revealed four chromatographic peaks (RT 15.86, 18.76, 20.13, 21.07) with<br />
molecular ions <strong>of</strong> 232, 274, 260, and 290 m/z, respectively. These have been tentatively identified, in<br />
chromatographic order, as 5-MeO-NIPT, the N-desalkyl metabolite, 5-MeO-DIPT, the parent substance, 5<br />
OH-DIPT, the O-desmethyl metabolite, and 5-MeO-DIPT N-oxide, the ring oxidation product <strong>of</strong> the parent<br />
substance. Identifications were based on comparative spectra with literature sources and, in the case <strong>of</strong> 5<br />
OH-DIPT, corroborative CIIMS with 5 % ammonia in methane, and ethylation with ethyl iodidelTMAH.<br />
Assuming that peak heights reflect urine concentrations, the relative magnitude <strong>of</strong> parent substance and<br />
metabolites were 5-MeO-DIPT>5-0H-DIPT>5-MeO-DIPT N-oxide>5-MeO-NIPT. Detection and<br />
identification <strong>of</strong> these metabolites permits the characterization <strong>of</strong> FOXY metabolism as three parallel<br />
oxidative pathways involving each <strong>of</strong>the molecule's non-carbon sites.<br />
Key words: 5-Methoxy-N,N-diisopropyltryptamine, metabolism, FOXY<br />
Page 227
CIO <br />
EFFECTS OF CHRONIC ACONITINE ADMINISTRATION ON ITS CONCENTRATION IN LIVER,<br />
KIDNEY, HEART, AND BLOOD OF MICE<br />
Kentaro Wada*, Makoto Nihira, Hideyuki Hayakawa, Yukari Tomita, Makiko Hayashida" Youkichi Ohno.<br />
Department <strong>of</strong>Legal Medicine, Graduate School <strong>of</strong> Medicine, Nippon Medical School, Tokyo, JAPAN<br />
Aims: Aconitum alkaloids are well known for their acute and high toxicity, for example, in the causation <strong>of</strong> severe<br />
arrhythmias leading to death. Aconitine, one <strong>of</strong>the major Aconitum alkaloids, is a highly toxic compound from the Aconilum<br />
species. The use <strong>of</strong>Aconitum alkaloids has been known since ancient times, over 2000 years in Asia as a homicidal agent,<br />
sometimes as poison for arrowheads. Even today, aconites are sometimes used as homicidal or suicidal agents. Until today,<br />
several cases <strong>of</strong> murder have been reported using single-dose <strong>of</strong>a large amount <strong>of</strong>Aconitum alkaloids in Japan. In 1995, a<br />
man murdered was subjected to autopsy in which Aconitum alkaloids were administered repeatedly over a period <strong>of</strong>months,<br />
in Saitama Prefecture, Japan. Although there are various studies reported on the single-dose effect <strong>of</strong>aconitine, no reports are<br />
available on the long-term effects <strong>of</strong> aconitine, probably due to its high toxicity. Therefore this study was conducted to<br />
investigate the influence <strong>of</strong>chronic administration <strong>of</strong>aconitine in experimental animal models.<br />
Methods: A total volume <strong>of</strong> 1.0 mg/kg/day was administered to the experimental animal models. The lethal dose 50%<br />
(LD50) <strong>of</strong> aconitine for mice is 1.8 mg/kg (orally, single dose) and 0.308 mg/kg (intraperitoneally, single dose). The male<br />
ICR (Institute <strong>of</strong>Cancer Research) mice were divided into 2 study groups: "acute group" (day 0: 0, 15,30,60,90, 120 min,<br />
1440 min = 24 hours) and "chronic group" (days 1,3,7,1O,15,19,and 22), according to the time when the animals were<br />
sacrificed. The experiments were conducted according to the guidelines <strong>of</strong> the Ethical Committee on Animal<br />
Experimentation <strong>of</strong> Nippon Medical School (Tokyo, Japan). We determined the concentration <strong>of</strong> aconitine and its<br />
metabolites (benzoylaconine and aconine) in organs and blood with gas chromatography/selected ion monitoring (GC/SIM).<br />
In addition, we concurrently recorded the electrocardiogram (ECG).<br />
Results: Fifteen min after administration on day 0, the early aconitine administered group (acute group) revealed peak organs<br />
and blood concentration levels <strong>of</strong> aconitine with gradual decrease, thereafter. The concentration <strong>of</strong> aconitine in organs and<br />
blood (from day 0 to day 22; 90 min after the last administration <strong>of</strong> aconitine) gradually decreased according to repeated<br />
administration, whereas benzoylaconine and aconine increased. ECGrevealed various types <strong>of</strong> arrhythmias (for example,<br />
ventricular fibrillation, ventricular tachycardia, torsade de pointes, atrioventricular block, and bundle branch block).<br />
However, the frequency <strong>of</strong>arrhythmias remarkably decreased with time and repeated administration <strong>of</strong> aconitine.<br />
Conclusions: In this study, 2 facts were revealed. First, the frequencies <strong>of</strong>fatal arrhythmias remarkably decreased to day 22.<br />
Secondly, the organs and blood concentration <strong>of</strong> aconitine (90 min after the last administration <strong>of</strong> aconitine) gradually<br />
decreased and its metabolites (benzoylaconine and aconine) increased until day 22. These 2 facts have raised the possibility<br />
that the activity <strong>of</strong> drug metabolism increased due to long-term administration <strong>of</strong> aconitine. In the case <strong>of</strong> long-term<br />
administration <strong>of</strong> aconitine, it is very important to determine not only the concentration <strong>of</strong>aconitine but also its metabolites<br />
(benzoylaconine and aconine) in the organs and blood from the viewpoint <strong>of</strong>forensic toxicology.<br />
Keywords: aconitine; chronic administration; GC/SIM<br />
Page 228
ell<br />
ABDOMINAL COMPLICATION OF INHALED METHAMPHETAMINE<br />
Wenceslo Kiat* and Irma Makalinao<br />
National Poison Control and Information Service, University <strong>of</strong> the Philippines-Philippine General<br />
Hospital Ward 14-A, Taft Avenue Manila, Philippines 1000<br />
Methamphetamine toxicity continues to be the leading cause <strong>of</strong> referral to the poison center. Despite the<br />
abundance <strong>of</strong> information regarding its cardiovascular and central nervous system toxicity; abdominal<br />
complications related to inhaled methamphetamine are not commonly encountered and anticipated. We<br />
report a case <strong>of</strong> a 33 year old female, a known methamphetamine abuser for the last five years who<br />
consulted the emergency room for acute onset <strong>of</strong> severe abdominal pain and dysuria noted a day prior to<br />
consult Gynecologic problem was ruled out. Abdominal ultrasound showed bile sludge in the gallbladder.<br />
She underwent emergency exploratory laparotomy under general anesthesia. However, intraoperative<br />
findings were normaL The initial urine methamphetamine level done on the fifth day after the last used<br />
showed 2157 ng/ml. This report suggests that methamphetamine toxicity could present as "acute abdomen"<br />
and should be anticipated by emergency room physicians.<br />
Key words: Inhalation, Methamphetamine, Abdomen pain<br />
Page 229
el2<br />
TOXICOKINETICS, RECOVERY, RESIDUES AND CYTOTOXICITY OF ACTP-ESTER IN<br />
THE GOAT<br />
C.R. Sahu*" Biplab Bagchi <br />
Department <strong>of</strong>Zoology, Kalyani University, Kalyani, West Bengal, India <br />
ACTP- Ester (Triclopyr butyl) marketed by Dow Elanco, USA is a selective herbicide used widely in<br />
agricultural field. In order to study the toxicokinetic, total recovery and cytotoxicity study <strong>of</strong> ACTP- Ester<br />
and its two potential metabolites - triclopyr acid (M]) and 3,5,6- trichloro-2 pyridinol (M2), the compound<br />
ACTP- Ester was administered orally 396 mglkg body wt. to Black Bengal Goats (Capra capra). The<br />
control groups were however treated with the same amount <strong>of</strong> carboxymethyl cellulose (CMC).<br />
Blood samples were collected before (0 hr) and after 0.25,0.50,0.75, 1,2,3,4,6,8,12,36,48,60,72,84,96,<br />
120, 144 and 168hr post administration (Pd) and were prepared for HPLC analysis following standard<br />
protocols. Toxicokinetic parameters <strong>of</strong> ACTP Ester were determined from computerized interactive curve<br />
fitting programme <strong>of</strong> respective blood level time pr<strong>of</strong>ile and data were analyzed as per the standard formula<br />
using various disposition kinetic parameters. Gross lesions for different tissues like liver, kidney, lung,<br />
brain etc were recorded for ACTP-Ester induced cytotoxicity in goats sacrificed on 4,5,6 and 7-day pd. An<br />
adequate blood level <strong>of</strong> ACTP-' Ester was detected as 4.94 ± 0.43 at 0.25 hr (pd). The concentration (C B<br />
max 25.15 ± 2.62 j.lg Iml was recorded at 6 hr followed by a slow decline and minimum (C B min 3.52 ±<br />
0.23 j.lg Iml) was detected at 60 hr pd. Kinetic behaviour <strong>of</strong> ACTP- Ester in goats followed a "two<br />
compartmental open model kinetics". The blood level for M] and M2 was 6.52 ± 0.89 and 2.61 ± 0.13<br />
. j.lg/ml respectively. The lower absorption rate constant suggested slow absorption <strong>of</strong> ACTPEster from<br />
GJ.tract. The CI H value, which is equivalent to CI B value suggested that major route <strong>of</strong> elimination <strong>of</strong><br />
ACTP-Ester be directed through liver. Very poor CI g value suggested that urine is the minor route <strong>of</strong><br />
excretion <strong>of</strong> the compound. The concentration <strong>of</strong> both metabolites appears zigzag fashion, which might be<br />
due to variable quantity as well as rate <strong>of</strong> metabolism in every unit <strong>of</strong> time.<br />
The recovery percentage <strong>of</strong> ACTP-Ester from faeces, G.I.tract content, urine and tissues were respectively<br />
65.38, 63.34, 66.10 and 66.24 in goats sacrificed on 4, 5, 6 and 7-day pd. Liver and lung showed gross<br />
malformations than other tissues due to the treatment.<br />
Keywords: Toxicokinetic, residue cytotoxicity ACTP, goat<br />
Page 230
C13 <br />
A HOMOGENEOUS ENZYME IMMUNOASSAY FOR THE DETECTION OF<br />
OXYCODONE AND OXYMORPHONE IN URINE<br />
Lakshmi Anne* Ming-che Wang, Vani Bodepudi, Scott Casseday, Manolito Datuin and Daryush<br />
Mirlohi; Microgenics Corporation, 46360 Fremont Boulevard, Fremont, CA.<br />
Oxycodone is an opioid analgesic derived from thebaine. It is structurally similar to codeine with a higher<br />
abuse potential than morphine. Oxycodone is prescribed for the treatment <strong>of</strong> moderate to severe pain,<br />
chronic pain or terminal cancer pain and is available as OxyContin® or in combination with acetaminophen<br />
or aspirin. Oxycodone is metabolized to oxymorphone, an active metabolite that has the same analgesic<br />
potency as oxycodone. Other metabolites <strong>of</strong> oxycodone include noroxycodone and noroxymorphone, which<br />
are inactive. The majority <strong>of</strong> oxycodone is excreted in urine within 24 hours as free oxycodone, conjugated<br />
oxycodone and oxymorphone. Increased use <strong>of</strong> oxycodone has resulted in an increase in oxycodone abuse<br />
and abuse-related deaths. None <strong>of</strong> the currently available opiate immunoassays has the sensitivity to detect<br />
oxycodone or oxymorphone at therapeutic or abuse levels. The objective <strong>of</strong> this study is to develop a<br />
homogeneous immunoassay for the specific detection <strong>of</strong> oxycodone and oxymorphone at therapeutic as<br />
well as abuse levels in urine.<br />
Microgenics DRI® Oxycodone Assay is a dual cut<strong>of</strong>f assay using 100 nglmL and 300 ng/mL oxycodone as<br />
cut<strong>of</strong>f calibrators. The assay uses a highly specific monoclonal antibody that can detect both oxycodone<br />
and oxymorphone. The assay is based on competition between drug labeled with glucose-6-phosphate<br />
dehydrogenase (G6PDH) and free drug from urine sample for a fixed amount <strong>of</strong> antibody binding sites. In<br />
the absence <strong>of</strong> free drug from the sample, the specific antibody binds the enzyme labeled drug causing a<br />
decrease in enzyme activity. This phenomenon creates a direct relationship between the drug concentration<br />
in urine and enzyme activity. The enzyme activity is determined spectrophotometrically at 340 nm by<br />
measuring its ability to convert NAD to NADH.<br />
The reagents and calibrators are liquid ready-to-use. The dynamic range <strong>of</strong> the assay is 0 to 1000 ng/mL.<br />
The performance <strong>of</strong>the assay was evaluated on the Hitachi 717 analyzer. The within-run and total precision<br />
(CV) for the cut<strong>of</strong>f calibrators and ± 25% controls is
C14 <br />
COMPARATIVE STUDY ON TOXIC MANIFESTATIONS INDUCED BY INGESTION OR INJECTION OF COMMONLY<br />
USED DISINFECTANTS AND SURFACTANTS<br />
Yoko Hieda*l, Yuying Xue', Koji Takayama', Yoshio Tsujin0 2 , Junko Fujihara l , Haruo Takeshita l - 'Department <strong>of</strong> Legal Medicine, Shimane<br />
University School <strong>of</strong> Medicine, Shimane, Japan, "Department <strong>of</strong> Dermatology, Shimane University School <strong>of</strong> Medicine, Shimane, Japan<br />
Background and aim: Accidental or intentional ingestion or injection <strong>of</strong> household products sometimes occur due to their easy accessibilities,<br />
but the toxic manifestations have not been well characterized when they are internally administered since these products are not developed for<br />
medicines. We previously evaluated the toxic and kinetic properties <strong>of</strong> Osvan® (benzalkonium chloride) that is widely used as a cationic<br />
surfactant and disinfectant, in which we showed that (I) different toxicological progression and manifestation appeared in administration via<br />
femoral artery (FA) among intravascular administrations even though the blood concentration pr<strong>of</strong>iles were similar, and (2) the degree <strong>of</strong><br />
toxicity correlated with the peak blood concentrations in orally dosed (PO) rats (Toxicol Lett 148: J13-123, <strong>2004</strong>). The aim <strong>of</strong>this study was to<br />
evaluate whether or not the difference in toxic manifestations among routes <strong>of</strong> administration observed in Osvan® were specific only to cationic<br />
surfactant, any kinds <strong>of</strong> surfactants, or any kinds <strong>of</strong> disinfectants.<br />
Materials and Methods: The test drugs involved Osvan® (cationic surfactant and disinfectant), Hyamine® (cationic surfactant and disinfectant),<br />
Tego® (zwitterionic surfactant and disinfectant), linear alkylbenzene sulfonate C I" (LAS,,) (anionic surfactant), VOlpo®20 (nonionic surfactant),<br />
Maskin® (non-surfactant and disinfectant), Ethanol (non-surfactant and disinfectant) and saline (control). Fifty-five male Sprague-Dawley rats<br />
'were administered one <strong>of</strong>the test drugs orally, intravenously via jugular vein (JV) or intraarterially via FA. Two to four different doses <strong>of</strong> drug<br />
were examined for each drug, and varied between 3 to 150 mglkg for a intravascular dose based on individual LD 5Q and 250 or 1250 mglkg for<br />
a oral dose except for ethanol. The dose <strong>of</strong>ethanol was set up at 0.3-1.5 glkg and 1.5-1.5 glkg for a intravascular and oral dose, respectively. The<br />
condition<strong>of</strong>rat was observed for 24 h after a dose and then the rat was sacrificed. The cardiac blood and tissue samples were collected for assay<br />
and histoIogical examination. The rats that died before 24 h were autopsied immediately after death to collect samples.<br />
Results and discussion: Toxic manifestations were different among the routes <strong>of</strong> administrations within the same test drugs except for Volpo"'20<br />
and saline. The toxic peak appeared soon after the dose following JV administration, while toxic effects developed with the lapse <strong>of</strong> time<br />
following higher doses <strong>of</strong>FA and ,PO administrations, though the degree <strong>of</strong>effects or time-course symptoms varied among drugs. Necrotic-like<br />
symptom developed around the injecting side <strong>of</strong> leg following FA administration in cationic or twitterionic surfactants and Maskin®, while it'<br />
appeared on opposite side <strong>of</strong>leg inLAS 12. The FA-dosed rats had higher blood myoglobin concentrations compared to JV- or PO-dosed. rats and<br />
they hardly urinated after a dose, suggesting that kidney was highly affected in FA administration. In PO administration, all high dose <strong>of</strong><br />
surfactants except for Volpo"'20 died at 5-20 h after a dose, while all non-surfactant disinfectants survived for I day at the same dose, suggesting<br />
that ionic surfactants have greater toxicities in PO administration. Severe damage <strong>of</strong> internal membrane <strong>of</strong> alimentary tract observed in ionic<br />
surfactants indicated that the ionic surfactant is critical chemical property to induce toxic effects in PO administration. The overall toxic degree<br />
based on the dose-size, except ethanol, could be ranked as strong as cationic surfactant =Maskin > zwitterionic surfactant =anionic surfactant<br />
> nonionic surfactant. These results suggested that (l) generally ranked stronger disinfectants have higher toxicities when they are<br />
intravascularly administered, (2) toxic manifestations are different between JV and FA administrations but with having similar trend in any kind<br />
<strong>of</strong> disinfectants and surfactants, and (3) ionic surfactants have stronger toxicities compared to nonionic surfactant or non-surfactant when they<br />
are orally administered.<br />
Keywords: surfactant, disinfectant, toxicity<br />
Page 232
CIS <br />
RAPID DETERMINATION OF CAUSATIVE AGENT USING DETACHED ROOF OF BULLA IN CHEMICAL BURNS OR<br />
DERMAL EXPOSURE<br />
Yoshio Tsujino' J , Yoko Hieda l , Haruo Takeshita 2 , Eishin Morita' - JDepartment <strong>of</strong> Dermatology, Shimane University School <strong>of</strong><br />
Medicine, Shimane, Japan, 2Department <strong>of</strong> Legal Medicine, Shimane University School <strong>of</strong> Medicine, Shimane, Japan<br />
Background and aim: Liquid specimens such as blood or urine are commonly used in forensic examinations, while skin samples are<br />
rarely used. Recently we have been studying the percutaneous absorption <strong>of</strong> chemicals and have shown that skin analysis is useful in<br />
identil'ying dermal exposure to petroleum products. Only small amounts <strong>of</strong> skin «0.03 g) are required for analysis since lipophilic<br />
chemicals, such as aliphatic hydrocarbons used to identil'y the petroleum product, remain in the skin (<strong>Forensic</strong> Sci Int 133, 141-145,<br />
2003). However, most living patients do not agree to have a skin biopsy for chemical analysis. We. present a case <strong>of</strong>a patient who was<br />
exposed dermally to some solvents where we determined the causative agent without skin biopsy.<br />
A case: A 73-year-old woman was first aware <strong>of</strong> slight redness with soreness on her anterior right thigh one evening. When she took <strong>of</strong>f<br />
her trousers 3 h later, the redness had spread over her rigbt thigh up to her abdomen with some erosion. When she visited our hospital<br />
next morning, extensive erythema with bulla and erosion appeared over 10% <strong>of</strong> her body.. These first- and second-degree bums were<br />
thought to be caused by exposure to some unidentified organic solvents.<br />
Examination: The lesions were first washed thoroughly with saline. To examine the lesions pathologically, and tojdentil'y the causative<br />
agent, a skin biopsy was recommended but not agreed upon with the patient. For an alternative specimen, small pieces <strong>of</strong> detached ro<strong>of</strong><br />
<strong>of</strong>bulla. which are usually taken <strong>of</strong>f, were collected for analYSis during topical treatment with a steroid ointment. For rapid examination<br />
to estimate the causative agent, a part <strong>of</strong> the collected bulla (0,01 g) was put into small amount <strong>of</strong>n-pentane in a glass tube, sonicated in<br />
an ultrasonic bath for I min, and then I iii oin-pentane was analyzed using a GC-MS system (HP5890)in a scan mode (mlz 30-400)<br />
. equipped with a capillary column (HP-5, 0.25 mm i.d. x 30 m, 0.25 lim thickness), The column temperature was set at 50°C for I min,<br />
then increased I O°C/min up to 280°C and held for 10 min. The temperature <strong>of</strong>injection port and ion source was set at 270°C and 280·C.<br />
respectively.<br />
Results: In the rapid analysis, typical kerosene components (aliphatic hydrocarbons with carbon number 9-16 and some aromatic<br />
hydrocarbons) were detected based on the retention times, mass spectra and pattern <strong>of</strong> the peaks. The causative agent was determined<br />
kerosene. Detailed analysis performed later using the remained collected ro<strong>of</strong> <strong>of</strong> bulla and blood sample (0.5 ml) utilizing liquid-liquid<br />
extraction confirmed kerosene components in the both samples. No other chemicals causing inflammatory response were detected.<br />
DisclISsion: The.patient may have had been exposed to kerosene while filling a kerosene stove at home about 5 h before first becoming<br />
aware <strong>of</strong> her skin irritation. Subepidermal bulla, <strong>of</strong>ten observed in second-degree bums is a phenomenon separating epidermis from<br />
dermis, indicating that the detached ro<strong>of</strong> <strong>of</strong> bulla in this case was composed mostly <strong>of</strong> epidermis. We recently reported that lipophilic<br />
chemicals tend to be trapped in lipophilic stratum corneum in epidermis (Int J Legal Med 118,41-46,<strong>2004</strong>). This suggests that a skin<br />
biopsy, which removes skin to the subcutaneous fat depth. and causes significant patients pain, is not necessary when petroleum products<br />
are involved. Analysis <strong>of</strong>only 0.0 I g <strong>of</strong> detached ro<strong>of</strong> <strong>of</strong> bulla with simple sample preparation is a useful diagnostic method for dermal<br />
exposure to petroleum products both in clinical and forensic fields,<br />
Key words: chemical burns, bulla, GC-MS<br />
Page 233
C16 <br />
A CASE OF TETRODOTOXIN POISONING CAUSED BY INSERTION OF A PUFFER FISH INTO<br />
THE VAGINA<br />
Mikio Yashikil*,Akira Namera l , Kengo Nishioka 2 , Manami Nishida l , Kojiro Kimura l<br />
lDepartment <strong>of</strong> Legal Medicine, Graduate School <strong>of</strong> Biomedical Sciences, Hiroshima University and<br />
2Department <strong>of</strong>Anesthesia, Chuden Hospital, Hiroshima, Japan.<br />
We report an unusual case <strong>of</strong> sudden heart and pulmonary failure in a 33 year-old young woman due to<br />
insertion <strong>of</strong>a puffer fish into the vagina. While traveling on a boat, the woman felt unwell while having sex<br />
with a man who had inserted a puffer fish into her vagina. Upon arriving at port, she became unconscious and<br />
then went into cardio-pulmonary arrest. She was immediately transported to a hospital where she received<br />
cardio-pulmonary resuscitation. Following an intravenous injection <strong>of</strong>2 mg <strong>of</strong>epinephrine, her heart rate and<br />
blood circulation recovered. Few days later, she began spontaneous breathing, however, her level <strong>of</strong><br />
consciousness continued at a low stage (JSC 200). She remained in a vegetable state for two months.<br />
Following her transfer to another hospital, she died <strong>of</strong> sequential pneumonia two months later. A serum<br />
specimen collected upon admission and a urine specimen collected two days post-admission were found to<br />
contain 58 nglg and 65 nglmL <strong>of</strong> tetrodotoxin (TTX). TTX in serum and urine was hydrolyzed. to<br />
2-amino-6-hydroxymethyl-8-hydroquinazoline (C 9 -bas)e by NaOH. C 9 -base was purified by CI8"SPE<br />
cartridge and analyzed by GC/MS after TMS derivatization. It is known that some species <strong>of</strong> puffer fish<br />
release TTX from the skin. In this case, a toxic concentration <strong>of</strong>TTX was rapidly absorbed by the victim's<br />
vaginal membrane, distributed throughout her body causing her cardio-pulmonary arrest and eventual death ..<br />
Key words: puffer fish, tetrodotoxin, vagina<br />
Page 234
C17 <br />
CHANGES OF GENE EXPRESSION BEFORE AND AFTER ACETAMINOPHEN INJECTION<br />
DETECTED BY DIFFERENTIAL DISPLAY<br />
2<br />
Mizuho Namiki I, Tomohisa Mori 2 , Shinobu It0 , Toshiko Sawaguche<br />
I Dept.<strong>of</strong> Emergency Medicine,Tokyo Women's Medical University,Tokyo,Japan<br />
2Dept.<strong>of</strong>Legal Medicine,Tokyo Women's Medical University,Tokyo,Japan<br />
Objectives; Acetaminophen is a familiar antipyretic analgesic. While the mechanism by which<br />
acetaminophen causes chemical damage has been fully explained, the molecular biological dynamics that<br />
takes place in the damaged liver has not been elucidated. The current study was conducted to advance the<br />
molecular biological understanding in the dynamics <strong>of</strong> the gene expression during the subsequent hepatic<br />
damage by acetaminophen.<br />
Materials and Method: I)Preparation <strong>of</strong> mice with acetaminophen-induced hepatic damage. Following<br />
fasting for 24 hours, 250 mglkg body weight <strong>of</strong> an acetaminophen solution was administered via a<br />
peritoneal route to mice to serve as a model for a drug-induced hepatic disorder, while the same amount <strong>of</strong><br />
a physiological saline was also given via the peritoneal injection to the control animals. Both groups fasted<br />
for an additional 24 hours thereafter. Under chlor<strong>of</strong>orm anesthesia, laparotomies were performed.<br />
Following blood specimen collection from the heart, the liver was excised. 2) Serum AL T and AST<br />
determinations were measured by using an autoanalyzer (Hitachi-7450). 3) The excised livers were frozen<br />
with liquid nitrogen and pulverized, from which RNA was collected by using Trizol. The product was then<br />
treated with DNAse and processed with phenol chlor<strong>of</strong>orm for cDNA synthesis. The DNA was amplified<br />
by using a primer from the Fluorescence Differential Display Kit (Takara). 4) The second PCR and<br />
acrylamide gel electrophoresis were conducted by employing the fluorescence differential display method.<br />
After a band pattern was visualized by a molecular imager FX, the bands with eminent differences were cut<br />
out, from which the amplified products were recovered for cloning. 5) The homology was confirmed<br />
between each base sequence that had been obtained from the Web site NCBI BRAST and the known mouse<br />
cDNA.<br />
Results: The model for a drug-induced hepatic disorder displayed numerous small white blotches, which<br />
were visible with the naked eye, around the hepatic portal system; and the results <strong>of</strong> blood chemical<br />
analyses indicated AST and AL T levels that were significantly higher (P
C18 <br />
EMBLICA OFFICINALIS (FRUIT) INHIBITION OF LIVER FIBROSIS INDUCED BY CARBON <br />
TETRACHLORIDE AND THIOACETAMIDE <br />
SA Tasduq, P. Kaiser, H.S. Maheshwari,R.K. Johri. <br />
Phannacology Division, Regional Research Laboratory, Jammu and Kashmir, India. <br />
The study was carried out to investigate the antifibrotic effects <strong>of</strong> hydro-ethanolic extract <strong>of</strong> a reputed <br />
Indian medicinal plant Emblica <strong>of</strong>ficinalis fruit on liver fibrosis induced by carbon tetrachloride (CCI 4 ) and <br />
thioacetamide in rats. Liver fibrosis was assessed by measuring levels <strong>of</strong> hydroxy proline, lipid <br />
peroxidation (LPO) based on malondialdehyde (MDA) production, microsomal drug metabolizing enzyme <br />
CYP450 2EI measured as aniline hydroxylation, along with the antioxidant enzyme systems as catalase <br />
(CAT), Glutathione peroxidase (GSH-Px), Glutathione (GSH). Liver Na+ K+ ATPase and y-glutathione <br />
transpeptidase (y-gt) were studied to assess the cell membrane disintegration together with serum enzyme <br />
activities (AST, AL T, ALP, Bilirubin). In both models <strong>of</strong> chemically induced liver fibrosis, the levels <strong>of</strong> <br />
hydroxyproline, LPO, CYP450 2EI, Na+ K+ ATPase, y-gt along with serum enzumes remained significantly <br />
increased with suppression <strong>of</strong> anti-oxidant defence enzymes. Treatment with a hydro-ethanolic extract <strong>of</strong> <br />
Emblica <strong>of</strong>ficinalis significantly reduced the levels <strong>of</strong> hydorxyporline, MDA, , Na + K+ ATPase, y-gt and <br />
serum enzymes. The anti-oxidant defence enzymes were restored to normal values as well. Thus this study <br />
finds Emblica <strong>of</strong>ficinalis as a useful alternative source <strong>of</strong>treatment in chronic liver fibrosis. <br />
Keywords: Liver fibrosis, Emblica oificinalis, rat <br />
Page 236
C19 <br />
A CASE OF SURREPTITIOUS NON-FATAL MERCURY POISONING<br />
Alphonse Poklis*. Department <strong>of</strong> Pathology, Medical College <strong>of</strong>Virginia Campus at Virginia<br />
Commonwealth University, Richmond, VA 23298-0165<br />
A case <strong>of</strong> non-fatal mercury poisoning disclosed suspicion <strong>of</strong> criminal poisoning and resultant toxicology<br />
testing is presented. A 46 yr-old, white male Fire Chief with episodes <strong>of</strong> chest pain and diaphoresis,<br />
presented in the emergency department with a one month history <strong>of</strong> fatigue, generalized weakness,<br />
headaches, "inability to focus at work" and "hardly able to walk up stairs", but denies shortness <strong>of</strong> breath.<br />
He had a prior history <strong>of</strong> episodes <strong>of</strong> chest pain and diaphoresis. Physical examination and chest X-rays<br />
were unremarkable, serum chemistries and enzymes including CPK and LDH, and thyroid were normal. He<br />
displayed an EKG on normal rhythm. His hospital course was uneventful and he was discharged after four<br />
days. Five weeks later, the chief once again presented in the emergency department with a four day history<br />
<strong>of</strong>: "chills and shakes", a fever <strong>of</strong> 102 0 F, back pain, headaches, increasing fatigue and muscular weakness,<br />
tingling in his fingers and toes and a palpable tender left axilla lymph node. Once again the physical<br />
examination was unremarkable and laboratory test normal with the exception <strong>of</strong> a serum creatinine <strong>of</strong> 1.5<br />
mg/dL and a urine protein <strong>of</strong> 60 mg. His hospital course was uneventful and he was discharged after three<br />
days. Three weeks after discharge while eating at work a lunch provided by his assistant-chief, the chief<br />
began vomiting violently. Suspicion <strong>of</strong> poisoning was raised by the comments <strong>of</strong> co-workers. Therefore,<br />
c<strong>of</strong>fee prepared the next morning for the chief by his assistant was saved and given to the police. Initial<br />
screening <strong>of</strong> the c<strong>of</strong>fee for toxic metals by the Reinsch Test resulted in a classic "silver mirror" indicating<br />
the presence <strong>of</strong> mercury. The c<strong>of</strong>fee and a 24 hour urine specimen obtained from the chief were then<br />
analyzed in a "cold vapor" Mercury Analyzer System (Perkin Elmer Corp.). The urine contained 20ug <strong>of</strong><br />
mercury/gm <strong>of</strong> creatinine. While executing a search warrant at the assistant-chiefs home, the police found<br />
over 128 reagent chemicals and explosives, including several mercury compounds. The assistant admitted<br />
adding mercurous nitrate periodically to the chiefs c<strong>of</strong>fee, to sandwiches the day the chief was violently<br />
vomiting, and to doughnuts the day <strong>of</strong> the chiefs first emergency room admission. The motive for the<br />
poisoning was that the assistant had been passed over for promotion. Three years prior to the presented<br />
case, a former chief working with the assistant, was retired with "complete disability" due to a<br />
neuromuscular disease <strong>of</strong> unknown etiology characterized by slow mental functioning, peripheral<br />
neuropathy and chronic nephritis! This case exemplifies the difficultly <strong>of</strong> diagnosing the rather diffuse and<br />
non-specific signs and symptoms <strong>of</strong> surreptitious chronic mercury poisoning.<br />
Keywords: Mercury poisoning, criminal poisoning, mercury analysis<br />
Page 237
C20 <br />
INVESTIGATION OF THE ACCUMULATION OF 2,4-D1CHLOROPHENOXYACETIC ACID<br />
(2,4-D) IN RAT KIDNEYS<br />
Handan Aydm* : University Istanbul, Faculty <strong>of</strong> Veterinary Medicine, Department <strong>of</strong> Pharmacology and<br />
Toxicology, 34310 Avcllar, Istanbul, Turkey<br />
A study was conducted to assess the accumulation in the kidneys <strong>of</strong> 2,4-dichlorophenoxyacetic acid (2,4<br />
D), the most widely used herbicide in the world, and its metabolite 2,4-dichlorophenol (2,4-DCP). 2,4-D is<br />
eliminated in humans and animals mainly through renal excretion. Male and female Sprague-Dawley rats<br />
were treated with 2,4-D that was introduced in their drinking water for 30 days. Group A (control group)<br />
was fed a normal diet, while Group B was treated with 50 ppm, and Group C 100 ppm 2,4-D. In addition,<br />
2,4-D was given daily as an oral dose, combined with their drinking water, consisting <strong>of</strong> 25 ppm in Group<br />
D and 50 ppm in Group E. Levels <strong>of</strong>2,4-D and its metabolite 2,4-DCP in the kidneys were measured using<br />
an HPLC method. It was observed that, though the administered doses <strong>of</strong> 2,4-D did not produce<br />
significant toxic effects, its metabolite in particular was present at high levels in the kidneys.<br />
Keywords: 2,4-dichlorophenoxyacetic acid (2,4-D); 2,4-dichlorophenol (2,4-DCP); HPLC<br />
Page 238
e21<br />
RAPID, SIMPLE AND V ALIDA TED GC-MS ASSAY FOR DETERMINATION OF DRUGS<br />
RELEVANT IN DIACNOSIS OF BRAIN DEATH IN HUMAN BLOOD PLASMA<br />
Frank T. Peters', Julia Jung, Thomas Kraemer and Hans H. Maurer<br />
Department <strong>of</strong>Experimental and Clinical Toxicology, University <strong>of</strong> Saarland, D-66421 Homburg (Saar),<br />
Germany, frank.peters@uniklinik-saarland.de<br />
Background: Before declaring the brain death <strong>of</strong> a patient (e.g. prior to explantation <strong>of</strong> organs), a ~umber<br />
<strong>of</strong> requirements have to be fulfilled. One <strong>of</strong> them is the exclusion <strong>of</strong> effective plasma concentratIOns <strong>of</strong><br />
drugs which might mimic brain death, especially <strong>of</strong>those typically administered in intensive Cl"e medicine.<br />
Recommendations for toxicological analysis in the context <strong>of</strong> the diagnosis <strong>of</strong> brain death have recently<br />
been published (Hall bach et a\., T1AFT Bulletin 34, <strong>2004</strong>, 14-16), which include a minimum consensus on<br />
the relevant analytes (thiopental, pentobarbital, methohexital, phenobarbital, diazepam, nordiazepam, and<br />
midazolam). The proposed limits <strong>of</strong> quantification correspond to one half <strong>of</strong> their lowest therapeutic<br />
concentrations. Therefore, the aim <strong>of</strong> the presented study was to develop and validate a rapid and simple<br />
assay for determination <strong>of</strong>the above mentioned drugs in human plasma samples.<br />
Methods: After addition <strong>of</strong> 50 J.1l <strong>of</strong> internal standard solution (4.0 mg/l pentobarbital-ds, 2.0 mg/l<br />
methohexital-ds, 40.0 mg/l phenobarbital-ds, 0.8 mg/l diazepam-ds, and 0.8 mg/l nordiazepam-ds in butyl<br />
acetate) and 50 J.11 <strong>of</strong> butyl acetate to 200 III <strong>of</strong> plasma, the samples were extracted for 2 min on a rotary<br />
shaker. After phase separation by centrifugation (1 min, 10000 g), 2 III <strong>of</strong> the organic phase (upper) were<br />
injected into the GC-MS system (Agilent, GC-MSD 5973). The analytes were separated within 10 min by<br />
gas chromatography (HP-l column, 12 m x 0.2 mm LD.) and detected by mass spectrometry. The mass<br />
spectrometer was operated in the full scan mode for identification and in the selected ion mode (S1M) for<br />
quantification (target ions ml= 156, 161, 172,247,252,204,209,256,261,242,247,310). Validation was<br />
performed according to a minimum consensus on method validation in this context currently developed by<br />
the Clinical Toxicology Committee <strong>of</strong> the GTFCh. This included evaluation <strong>of</strong> selectivity, calibration<br />
model, precision and accuracy. Furthermore, the results for accuracy and precision obtained with six-point<br />
and one-point calibration were systematically compared. Finally, the applicability <strong>of</strong> the described assay<br />
was tested by analysis <strong>of</strong>real samples from brain death cases.<br />
Results: The analytes were fully separated and sensitively detected. No interfering peaks were detected in<br />
blank plasma samples from ten different sources. The assay was linear from 0.25 to 10 mg/I for<br />
pentobarbital and thiopental, from 0.125 to 10 mg/l for methohexital, from 2.5 to 50 mg/I for phenobarbital,<br />
from 0.05 to 2.5 mg/I for diazepam and nordiazepam, and from 0.01 to 0.5 for midazolam. Using six-point<br />
calibration, accuracy data (in terms <strong>of</strong> bias) ranged from -17.9% to 23.7%. Within-day and intermediate<br />
precision data (expressed as CV) ranged from 1.4% to 6.4% and from 2.6% to 7.0%, respectively. Using<br />
one-point calibration with a calibrator close to the center _<strong>of</strong> the. linearity range, accuracy data (in terms <strong>of</strong><br />
bias) ranged from -11.6% to 29.7%. Within-day and intermediate precision data ranged from 1.3% to 6.2%<br />
and from 2.6% to 9.6%, respectively. Recoveries ranged from 85% to 109%. The acceptance criterion<br />
defined by the Clinical Toxicology Committee <strong>of</strong> the GTFCh (99% confidence interval <strong>of</strong> measured mean<br />
within ±50% <strong>of</strong>target value) was easily fulfilled for all analytes, even with one-point calibration. The assay<br />
was successfully applied to analysis <strong>of</strong>real brain death cases.<br />
Conclusion: The described assay allows rapid, fast and reliable determination <strong>of</strong> analytes relevant in the<br />
diagnosis <strong>of</strong> brain death. Systematic studies showed that the assay can be performed with one-point<br />
calibration. This is an important advantage, because it keeps the workload low for the usually single cases<br />
and because results are needed quickly in this context.<br />
Keywords: brain death, GC-MS, validation<br />
Page 239
e22<br />
NEONATAL ABSTINENCE SYNDROME IN METHADONE-EXPOSED INFANTS IS ALTERED<br />
BY LEVEL OF TOBACCO EXPOSURE<br />
Robin E. Choo*·, Marilyn A. Huestis·, Jennifer R. Schroeder·, Hendree E. Jones b , <br />
·IRP, NIDA, NIH, Baltimore, MD, bDept. Psychiatry and Behaviora\ Sciences, lHU School <strong>of</strong> Medi.cine <br />
Baltimore, MD 21224, US<br />
'<br />
In utero exposure to tobacco has been associated with lower birth weight infants, pre-term births, smaller<br />
head circumference, intrauterine growth retardation and increased fetal morbidity; however, few studies<br />
have examined the neurobehavioral effects <strong>of</strong> prenatal tobacco exposure. This report describes the effect <strong>of</strong><br />
prenatal tobacco exposure on neonatal abstinence syndrome (NAS) for infants born to methadone (mean<br />
dose 77.0 mg/day ± 19.4, range 40-110) maintained mothers. Twenty-nine pregnant women and their<br />
infants participated in this IRB approved study. Smoking histories were obtained by maternal self-report at<br />
enrollment into the study and at delivery. Sixteen women, light smokers (LS), reported cigarette<br />
consumption <strong>of</strong> 10 or less cigarettes/day (mean 8.4 ± 2.3) and thirteen women, heavy smokers (HS),<br />
reported smoking 20 or more cigarettes/day (mean<br />
21.5 ± 5.5). The onset, peak and duration <strong>of</strong> NAS<br />
were examined. Infants born to mothers in the HS group had significantly higher (p=0.014) NAS peak<br />
scores <strong>of</strong> 9.8 ± 4.8 as compared to 5.6 ± 3.8 as seen in the LS group. There was a significant difference<br />
(p=0.016) in time to peak between the HS group (113.8 ± 90.0 h) and the LS group (37.8 ± 33.8 h). The<br />
duration <strong>of</strong>NAS showed a trend towards statistical significance (p=0.054) between the HS (mean 9.5 ± 7.3<br />
days) and LS (mean 5.1 ± 4.6 days) grolJps. These data showed that infants born to mothers in the HS<br />
group had a 57% higher NAS peak score, took 33% longer to peak and had a 54% increase in NAS<br />
duration as compared to the LS group. These results demonstrate the need for future studies to examine the<br />
role <strong>of</strong> tobacco exposure as a variable in the examination <strong>of</strong> opioid associated NAS.<br />
Keywords: Prenatal, Methadone, Nicotine, NAS, Outcomes<br />
Page 240
C23 <br />
BIOMONITORING OF EXPOSURE TO CHEMICAL WARFARE AGENTS<br />
D. Noort*, MJ. van der Schans and H.P. Benschop<br />
Division <strong>of</strong> Chemical & Biological Protection, TNO Prins Maurits Laboratory, P.O. Box 45, 2280 AA<br />
Rijswijk,The Netherlands<br />
Methods to analyze chemical warfare agents (CWA) and their decomposition products in environmental<br />
samples were developed over the last decades. On the other hand, methods for such analyses in biological<br />
samples have only recently become available. Retrospective detection <strong>of</strong> exposure to CW A can be useful<br />
for various applications. With regard to the "Homeland Defense" program, it can be envisaged that rapid<br />
diagnostic methods can play a pivotal role in case <strong>of</strong> a terrorist attack with CWA. In the same context,<br />
confirmation <strong>of</strong> non-exposure <strong>of</strong> worried citizens is <strong>of</strong> utmost importance. Also, such methods can be used<br />
for forensic analyses in case <strong>of</strong> suspected terrorist activities ("chemical fingerprints"). It is self-evident that<br />
these methods will also be highly valuable from a military point <strong>of</strong> view, e.g., to establish firmly to which<br />
chemicals casualties have been exposed to, which is a starting point for adequate medical treatment, or for<br />
health surveillance <strong>of</strong> workers in destruction facilities <strong>of</strong> chemical warfare agents. This presentation will<br />
focus on a number <strong>of</strong> specific methods currently available for verification <strong>of</strong> exposure to the most common<br />
CWA, i.e., nerve agents and mustard agents.<br />
There are basically four methods to diagnose an exposure to a nerve agent:<br />
1. cholinesterase inhibition measurements<br />
2. analysis <strong>of</strong>hydrolysis products, e.g., alkyl methylphosphonic acids<br />
3. analysis <strong>of</strong> generated phosph<strong>of</strong>luoridates after treatment <strong>of</strong> blood with fluoride ions ("fluoride<br />
reactivation")<br />
4. mass spectrometric analysis <strong>of</strong> phosphylated peptides after enzymatic digestion <strong>of</strong> modified<br />
cholinesterase.<br />
For mustards, there are three distinct methods to assess an exposure:<br />
1. mass spectrometric analysis <strong>of</strong> low molecular urinary metabolites<br />
2. analysis <strong>of</strong> DNA adducts by means <strong>of</strong> mass spectrometric or immunochemical methods.<br />
3. mass spectrometric analysis <strong>of</strong> protein adducts, e.g., to hemoglobin and albumin.<br />
This presentation will focus on methods that are based on the analysis <strong>of</strong>long-Iived protein adducts, i.e., on<br />
methods 3 and 4 for nerve agents and on method 3 for mustards. Advantageously, protein adducts are stable<br />
and therefore detectable weeks or even months after the exposure, in contrast to DNA adducts and urinary<br />
metabolites which are excreted much more rapidly. The developed technology will be described briefly and<br />
examples <strong>of</strong> real exposure incidents will be presented.<br />
Acknowledgements: This presentation covers work that was funded by the US Army Medical Research and<br />
Materiel Command, by the Bundesministerium der Verteidigung, InSan I 3, Germany, and by the<br />
Directorate <strong>of</strong> Military Medical Service <strong>of</strong>the Ministry <strong>of</strong>Defense, The Netherlands.<br />
Keywords: chemical warfare agents, adducts, diagnosis<br />
Page 241
C24 <br />
ATTEMPTED SUICIDE BY INGESTION OF CHLORPYRIFOS: IDENTIFICATION IN SERUM<br />
AND GASTRIC CONTENT BY GC-FID/GC-MS<br />
Maria A. Martinez l , Salome Ballesteros 2 , Carolina Sanchez de la Torre l , Antonio Sanchiz\ Elena<br />
Almarza 1 , and Alejandro Garcia-Aguilera}<br />
IChemistry Department, National Institute <strong>of</strong> Toxicology and <strong>Forensic</strong> Sciences, Ministry <strong>of</strong> Justice, CI<br />
Luis Cabrera 9, 28002 Madrid, Spain. 2Spanish Poison Control Center, National Institute <strong>of</strong> Toxicology<br />
and <strong>Forensic</strong> Sciences, Madrid, Spain 3Emergency Service, Hospital Rafael Mendez, 30800 Lorca, Murcia,<br />
Spain<br />
The case history, toxicological findings, and poisoning characteristics <strong>of</strong> an attempted suicide by ingestion<br />
<strong>of</strong> a chlorpyrifos formulation are reported along with a description <strong>of</strong> the validated analytical method.<br />
Chlorpyrifos, an organophosphate pesticide introduced by Dow Chemical Company in 1965 as a<br />
broadspectrum insecticide, is the active ingredient in many commercial insecticide formulations available<br />
in Spain. Organophosphate insecticides inhibit cholinesterase activities which causes accumulation <strong>of</strong><br />
acetylcholine at synapse, and as a result an overstimulation <strong>of</strong> neurotransmission occurs. The mortality rate<br />
<strong>of</strong> suicide poisoning is usually high and therefore early diagnosis and appropriate treatment is <strong>of</strong>ten life<br />
saving. Other compounds can be present in organophosphate formulations and are responsible for part <strong>of</strong><br />
the toxicity <strong>of</strong> these commercialized products. In fact, aromatic hydrocarbons, such as toluene and/or<br />
xylenes, and other additives could increase the risk <strong>of</strong> toxicity after ingestion <strong>of</strong> pesticide formulations.<br />
Numerous cases <strong>of</strong> acute nonfatal and fatal poisoning because <strong>of</strong> the inhalation or ingestion <strong>of</strong> chlorpyrifos<br />
have been reported in the literature. However, there is a lack <strong>of</strong> chlorpyrifos poisoning cases published<br />
where analytical findings were included.<br />
A I5-year-old female teenager went to the emergency room after the ingestion <strong>of</strong> a product from a bottle<br />
marked with a label "Poison". On admission she was obtunded, with normal vital signs and a strong smell<br />
<strong>of</strong> solvent. Therapeutic measures included the application <strong>of</strong> decontamination procedures, oxygen and<br />
gastric protectors. She had a good outcome with mild CNS depression and bradycardia. Two hours after<br />
ingestion biological samples were collected in the emergency room and sent for analysis to our laboratory<br />
with instructions to investigate the presence <strong>of</strong> solvents. The serum and gastric content contained 5.3 and<br />
9.4 j.lg/mL <strong>of</strong> unmetabolized chlorpyrifos, 4.6 and 6.9 j.lg/mL <strong>of</strong> toluene, and 2.5 and 7.9 Jlg/mL <strong>of</strong> butyl<br />
acetate, respectively. The toxics were isolated after liquid-liquid extraction <strong>of</strong> 3 mL <strong>of</strong>sample with 1 mL <strong>of</strong><br />
diethyl ether using n-octyl-benzene as internal standard. The simultaneous determination <strong>of</strong> chlorpyrifos,<br />
toluene, and butyl acetate were performed using the combination <strong>of</strong> gas chromatography with flame<br />
ionization detector (GC-FID) for screening analysis, and gas chromatography-mass spectrometry (GC-MS)<br />
for confirmation <strong>of</strong> the obtained results. Both gas chromatographs were equipped with methylsilicone<br />
capillary columns. The previous GC-FID screening analysis was used for quantitation <strong>of</strong> toluene and butyl<br />
acetate, and GC-MS SIM mode was used for quantitation <strong>of</strong> chlorpyrifos, using serum calibration curves in<br />
the range <strong>of</strong> 0.l-5 j.lg/mL. Limits <strong>of</strong> detection were 25, 36 and, 23 ng/mL for chlorpyrifos, toluene, and<br />
butyl acetate, respectively. Absolute recoveries were more than 90 %, intra-assay precisions less than 5 %,<br />
and linearity up to 5.0 Jlg/mL for all the analytes.<br />
The method provides an excellent and rapid tool for use in cases <strong>of</strong> unknown poisonings allowing the<br />
simultaneous determination <strong>of</strong> a wide variety <strong>of</strong> pesticides and additives, including petroleum distillates, in<br />
the performance <strong>of</strong> systematic toxicological analysis in forensic and clinical laboratories.<br />
Keywords: Chlorpyrifos, Poisoning, GC-FID, GC-MS<br />
Page 242 1
C25 <br />
PROPYLENE GLYCOL IN EXTREMELY HIGH ION GAP LACTIC ACIDOSIS<br />
Robert L. Fitzgerald* and David A. Herold<br />
V A Healthcare System San Diego and University <strong>of</strong> California-San Diego, San Diego, CA.<br />
A 31-year-old male presented to the ED disoriented in acute distress. His admission laboratory data were<br />
remarkable for the degree <strong>of</strong> acidosis present. An arterial blood gas measurement showed his pH to be 6.85<br />
(reference range 7.35 to 7.45) with a pC02 <strong>of</strong> 14 mm Hg (reference 35 to 45) and a lactic acid <strong>of</strong> 30<br />
mmollL (reference range 0.7 to 2.1). Additional labs included an ethanol <strong>of</strong>217 mg/dL, and a measured<br />
osmolality <strong>of</strong> 376 mOsmikg (270 - 310). Taking the effect <strong>of</strong> ethanol into account, the patient had an<br />
unexplained osmol gap <strong>of</strong> 65 mOsmikg. In addition to the unexplained osmol gap the patient had an anion<br />
gap <strong>of</strong> 50 mEq/L (reference range 10 to 20), the L-Iactate <strong>of</strong> 30 explained this gap. Based on the<br />
unexplained osmol gap, the acidosis, and a high anion gap, stat methanol and ethylene glycol were ordered.<br />
Negative finding for methanol and ethylene glycol prompted a search for other causes <strong>of</strong> hyperosmolality.<br />
Discussion <strong>of</strong> the case with the toxicology laboratory revealed the presence <strong>of</strong> a large peak on the gas<br />
chromatographic tracing from a volatiles screen that was not reported initially. This peak represented 40<br />
mgldL <strong>of</strong> propylene glycol. Either ethanol or propylene glycol can result in a high anion gap lactate<br />
acidosis. The pr<strong>of</strong>ound acidosis and extremely high L-Iactate was a result <strong>of</strong> the patient drinking for 5 days.<br />
While the osmol gap could not be completely explained, the high anion gap could be explained by L-Iactate<br />
and the implied D-Iactate resulting from the propylene glycol metabolism.<br />
Based on the laboratory data, the patient was treated with intravenous bicarbonate and IV fluid replacement<br />
in an attempt to correct the acidosis. Despite 4 ampules <strong>of</strong> bicarbonate, the patients arterial blood gas pH<br />
did not increase significantly nor was there a significant increase in urinary output. Due to the impending<br />
renal failure and acidosis, the patient was hemodialyzed. Four hours <strong>of</strong> hemodialysis corrected his<br />
acidlbase imbalance. Unfortunately, after hemodialysis, the patient developed acute respiratory distress<br />
syndrome and required ventilation assistance. The patient also became septic and was treated with<br />
antibiotics. After a twelve day hospital stay which included intermittent hemodialysis for renal failure, the<br />
patient recovered and was discharged in apparent good health.<br />
This presentation will review the common causes <strong>of</strong> hyperosmolality in clinical toxicology and the<br />
diagnostic pathway for identifying various intoxicants that cause high anion gap metabolic acidosis. The<br />
importance <strong>of</strong> communicating directly with the laboratory to help identity unusual causes <strong>of</strong> combined<br />
osmol/anion gap metabolic acidosis will be emphasized.<br />
Key words: propylene glycol, metabolic acidosis, ethanol<br />
Page 243
C26 <br />
CORRELATION BETWEEN METABOLIC ACIDOSIS AND CLINICAL PARAMETERS IN<br />
DIETHYLENE GLYCOL (DEG) POISONING VICTIMS<br />
L.A.Ferrari*! ,L. Giannuzzi 2<br />
ILaboratory <strong>of</strong> Toxicology and Legal Chemistry, Buenos Aires Court <strong>of</strong> Justice. 41 y 119, (1900) La Plata,<br />
Argentina. laferrari@unimoron.edu.ar<br />
2Catedra de Toxicologla y Qulmica Legal. Facultad de Ciencias Exactas. Universidad Nacional de La Plata,<br />
47 y 115 (1900). Argentina.leda@biol.unlp.edu.ar<br />
This work analyzes fifteen victims <strong>of</strong> a massive intoxication that took place in Argentina in 1992 as a result<br />
<strong>of</strong> the intake <strong>of</strong> pro polis syrup: a popular medicinal agent used in the 90s for upper respiratory system<br />
infections. Diethylene glycol (DEG) was found as the responsible agent which caused metabolic acidosis,<br />
anuria, renal failure and death in the 15 studied victims.<br />
DEG poisoning cases were classified into three groups according to the survival time <strong>of</strong> the victims,<br />
namely: 1) those who survived up to 3 days; 2) those who survived from 3 to 5 days; and 3) those who<br />
survived from 5 to 21 days.<br />
A methanolic fraction extracted in a Soxhlet system with subsequent concentration and purification was<br />
obtained from viscera and blood. Gas Chromatography and FlO detector (GClFlO) methodology was<br />
performed. On the other hand, samples <strong>of</strong> the propolis syrup from each <strong>of</strong> the victims was studied through<br />
NMR and quantified by GClFlO, using ethylene glycol as internal standard. Finally, each clinical history<br />
from victims were studied in detail: anionic Gap (AG), Excess base (EB) and pH.<br />
Patients belonging to group 1 showed the highest AG values and the lowest (EB) values as well as the<br />
major severity in their clinical manifestations. Correlation between pH and EB was ~ =0.68, 0.99 and 0.55<br />
for groups 1,2 and 3 respectively. In 3 out <strong>of</strong> 15 fatal cases studied, DEG could be isolated from viscera<br />
and blood. The concentration ratio (DEG)viscer.l (DEG)blood ranged 1.45 - 1.55 with a coefficient correlation<br />
<strong>of</strong> ~ = 0.96. In the other victims, DEG could not be detected. This could be due to the long survival period<br />
<strong>of</strong> the deceased victims from the syrup ingestion to death, and to the fact that putrefYing mechanisms could<br />
be operating.<br />
Results showed that the syrup samples contained DEG in a 24% to 65.0% (p/v) range. A proper correlation<br />
between the amount <strong>of</strong>DEG ingested and the anionic Gap (r2=0.63-0.78) could be observed in the victims<br />
studied, according to theoretic amount <strong>of</strong> syrup ingestion (5 -20 ml). So, the lethal dose for humans in this<br />
episode was found to vary from 0.019 to O.l74mg DEGlKg corporal weight. These results could contribute<br />
to the understanding <strong>of</strong> DEG toxicity parameters On the other hand, they could provide data concerning<br />
lethal dose in humans.<br />
Keywords: Diethylene Glycol, poisoning, lethal dose<br />
Page 244
C27 <br />
PHARMACEUTICAL IDENTIFICATION AND QUALITY CONTROL TESTING AT A MAJOR<br />
MEDICAL CENTER<br />
Carl E. Wolf* and Alphonse Poklis. Department <strong>of</strong> Pathology, Medical College <strong>of</strong> Virginia Campus at<br />
Virginia Commonwealth University, Richmond, VA 23298-0165.<br />
Clinical Toxicology laboratories are <strong>of</strong>ten presented with the problem <strong>of</strong> identifying the contents <strong>of</strong><br />
pharmaceutical products. These preparations come into question in a variety <strong>of</strong> situations: the preparation is<br />
found outside <strong>of</strong> it's "controlled" environment, the inappropriate or wholly unexpected response <strong>of</strong> a<br />
patient to the administration <strong>of</strong> the preparation, or suspicions <strong>of</strong> drug diversion or abuse by a health care<br />
provider. Medical institutions generally address the issue <strong>of</strong> drug abuse by health care workers through preemployment<br />
urine drug testing, random drug testing, and/or "for cause" drug testing after an incident has<br />
occurred. However, such programs seldom, if ever address issues <strong>of</strong> pharmaceutical compounding or<br />
tampering.<br />
We have developed a simple HPLC method to routinely identify and quantitate pharmaceutical<br />
preparations for over 15 different drugs, including opiates, synthetic opiates, local anesthetics, and<br />
midazolam. The method uses a Beckman ODS column (4.6 x 250 mm), and an isocratic mobile phase<br />
consisting <strong>of</strong> acetonitrile: perchloric acid: water (33:0.134:67) for drug separation. Drugs are detected and<br />
quantitated using a UV detector at either 206 or 280 nm. In the past 6 years, we have analyzed thousands <strong>of</strong><br />
pharmaceutical products for content and concentration. Most <strong>of</strong> these products were analyzed for<br />
concentration, to verify proper compounding by our hospital pharmacy or local pharmacies.<br />
Several cases will be presented <strong>of</strong> typical findings from products that have not been tampered with, as well<br />
as, instances <strong>of</strong> mistaken compounding and drug. diversion. Cases include: preparations from patient<br />
controlled anesthesia, IV bag solutions, rescue squad drug boxes, and improper compounding <strong>of</strong> pediatric<br />
preparations for c1onidine, and hydromorphone.<br />
Keywords: Drug Diversion, Pharmaceutical Testing, Narcotics<br />
Page 245
C28 <br />
METHAMPHETAMINE DETECTION IN URINE OF CHILDREN CO-EXISTING WITH<br />
CLANDESTINE METHAMPHETAMINE MANUFACTURING<br />
Ann Marie Gordon*, Barry K. Logan, PhD <br />
Washington State Toxicology Laboratory, <strong>Forensic</strong> Laboratory Services Bureau, Washington State Patrol, <br />
2203 Airport Way South, Seattle, WA 98134. <br />
In 2000, the Washington State legislature enacted the "Drug Endangered Children's Law" to protect<br />
children found at clandestine methamphetamine manufacturing sites. The law mandates that children<br />
found at these sites be placed in protective custody and allows for a mandatory two-year enhancement on<br />
any "Unlawful Manufacturing <strong>of</strong> a Controlled Substance" conviction when children are present at the<br />
clandestine lab site. In March 2002, the legislature passed a follow-up bill mandating that any person<br />
allowing hislher child to be present at a methamphetamine lab, be charged with a felony child<br />
endangerment charge, regardless <strong>of</strong> whether they were charged with the manufacture <strong>of</strong> methamphetamine.<br />
The Washington State Toxicology Laboratory is tasked with providing forensic toxicological services for<br />
the coroners and medical examiners and all police agencies within the 39 counties <strong>of</strong> the state. We began<br />
receiving samples (typically urine) as part <strong>of</strong>the Drug Endangered Child program in 2000, without advance<br />
notice and without a suitable protocol for appropriate testing. Over the past two years, we have coordinated<br />
with two police agencies to develop a suitable sample collection and testing protocol.<br />
The Washington State Toxicology Laboratory received 26 samples, from February 2002 through February<br />
<strong>2004</strong>, collected from children for investigation <strong>of</strong> drug endangerment; 5 diapers, 1 serum and 20 urine<br />
samples were submitted to the laboratory for analysis. The ages <strong>of</strong>the children ranged from 4 months to 16<br />
years <strong>of</strong> age, mean and media age <strong>of</strong>7 years, half <strong>of</strong> the subjects were female and 23 <strong>of</strong> the 26 cases (88%)<br />
were positive for methamphetamine.<br />
In most <strong>of</strong> the cases (20 <strong>of</strong> the 23 positives), the concentrations <strong>of</strong> methamphetamine and amphetamine in<br />
the samples were relatively low, between 0.02 mg/L to 0.2 mgIL methamphetamine. In these cases, it is<br />
reasonable to state that the children ingested methamphetamine but may not have exhibited any associated<br />
effects. Of the remaining three cases, two exhibited signs <strong>of</strong> methamphetamine intoxication at the time <strong>of</strong><br />
their encounter with the police and were treated in the hospital for their symptoms. The first, a 6-monthold<br />
male, had a serum methamphetamine concentration <strong>of</strong> 0.12 mg/L and the second child, a 2-year-old<br />
male, had urine concentrations <strong>of</strong> 13.59 mgIL methamphetamine and 0.9 mg/L amphetamine. The third<br />
case with high drug concentrations was a 16-year-old male with urine methamphetamine <strong>of</strong> 0.05 mgIL and<br />
amphetamine <strong>of</strong> 18.5 mgIL.<br />
Children living in a methamphetamine-manufacturing environment are endangered by many associated<br />
factors, the toxicity <strong>of</strong> the associated chemicals used in the manufacture, inherent fire danger, neglect and<br />
are at a higher risk for sexual abuse. The presence <strong>of</strong> methamphetamine is an indicator that the children<br />
have been in unsafe environment and this data can be used to support a case <strong>of</strong> child endangerment. Child<br />
endangerment charges have been filed in at least 12 <strong>of</strong> the cases; in one case the defendant was convicted<br />
<strong>of</strong> illicit methamphetamine manufacture and he received a sentence enhancement for the child<br />
endangerment charge.<br />
Key Words: Methamphetamine, Children, Clandestine<br />
Page 246
C29 <br />
AN EVENT ASSOCIATED WITH FATAL 2,5-DIMETHOXY-4-BROMOAMPHETAMINE<br />
OVERDOSE<br />
Marie Balikova* <br />
Institute <strong>of</strong> <strong>Forensic</strong> Medicine and Toxicology, 1 st Medical Faculty, Charles University in Prague, <br />
121 08 Prague 2, Czech Republic, (mbali@lfl.cuni.cz)<br />
2,5-dimethoxy-4-bromoamphetamine (DOB) is a strongly acting hallucinogen with effective dose estimate<br />
for an 80 kg man being 2 mg (I). In the event reported here, two men were provided a capsule with white<br />
powder containing an unknown substance in order to test its effects as a new LSD like hallucinogen. They<br />
shared the content <strong>of</strong> a capsule and consumed it orally followed with strong rapid hallucinations and<br />
vomiting, unconsciousness and coma lasting several days. After unknown time elapsed since the<br />
application, they were admitted to the hospital in coma state without response to analgesic irritation. The<br />
man AX 28 years (113 kg) survived. The man BX 29 years (65 kg) experienced convulsions, metabolic<br />
acidosis (pH 6.6) and died after six days. Immediately after the admission to the hospital, gastric content,<br />
blood and urine specimens were sampled and sent for toxicological examination. Alcohol in blood samples<br />
was not found. Cedia urine screening indicated the presence <strong>of</strong> THCOOH in both cases, cocaine and<br />
metabolites in AX urine, and no signal corresponding to amphetamines presence was detected. Finally,<br />
GC-MS method for unknown drugs discovered the presence <strong>of</strong> DOB in gastric content and urine samples<br />
<strong>of</strong> both persons. GC-MS targeted analysis for acetylated DOB confirmed its presence in blood <strong>of</strong> both<br />
persons and quantitative analysis provided the concentration values in serum 13nglml (AX - survived)<br />
and 19 nglml (BX - deceased). This report both on nonfatal and fatal DOB overdose cases is based on clear<br />
toxicological evidence, moreover it is completed with antemortem DOB blood serum levels and probably<br />
it is the first sign <strong>of</strong>DOB occurence in the Czech Republic.<br />
Reference: (1) A. Shulgin, A. Shulgin: PiHKAL: A Chemical Love Story. Transform Press, Berkeley CA,<br />
1998<br />
Keywords: 2,5-dimethoxy-4-bromoamphetamine, DOB overdose, fatal intoxication<br />
Page 247
C30 <br />
SIMULTANEOUS DETECTION OF STIMULANT LAXATIVES AND DIURETICS IN HUMAN<br />
URINE USING GC-MS AFTER ENZYMATIC CLEAVAGE OF CONJUGATES AND<br />
EXTRACTIVE METHYLATION<br />
J. Beyer', A. BierI, F.T. Peters and H.H. Maurer<br />
Department <strong>of</strong> Experimental and Clinical Toxicology, University <strong>of</strong> Saarland<br />
0-66421 Homburg (Saar), Germany,jochen.beyer@uniklinik-saarland.de<br />
Background: Laxatives and diuretics are widely abused for various reasons. Surreptitious abuse <strong>of</strong> both is<br />
<strong>of</strong>ten associated with eating disorders or Milnchhausen syndrome. Concerning laxatives, there is also<br />
habitual abuse because <strong>of</strong> chronic constipation, whereas diuretics are also abused in doping. Such abuse<br />
may lead to serious disorders like chronic diarrhea, hypokalemia, dehydration, and disturbance <strong>of</strong> acid-base<br />
balance. Because <strong>of</strong> the heterogeneity <strong>of</strong> these side effects and their similarity to symptoms <strong>of</strong><br />
gastrointestinal or renal disorders, a toxicological screening for laxatives and diuretics should be part <strong>of</strong> the<br />
differential diagnosis <strong>of</strong> such syndromes. This may also help to avoid extensive and expensive diagnostic<br />
work.<br />
Methods: After accelerated enzymatic cleavage <strong>of</strong> conjugates (glucuronidase/arylsulfatase, EC no.<br />
3.2.1.3113.1.6.1, 100000 Fishman units per mL, 50 cC, 90 min), the drugs and their metabolites were<br />
isolated from 2 mL <strong>of</strong> urine by extractive methylation. For details <strong>of</strong> extractive methylation see Maurer HH<br />
et aI., JAT 25,2001,237. The extract was reconstituted in 50 I-lL ethyl acetate and 2 J..lL were injected into<br />
the GC-MS (Agilent GC-MSD 5972). Analytes were separated on an HP 1 column (12 m x 0.2 mm 1.0.)<br />
and detected by mass-spectrometry in the EI full scan mode. They were screened by using reconstructed<br />
mass chromatography using selective ions and identified by visual and computerized comparison <strong>of</strong> the<br />
peak underlying mass spectra with the corresponding reference mass spectra (PMW _tox4).<br />
Results: The assay allowed the detection <strong>of</strong> the diphenylmethane laxatives phenOlphthalein, bisacodyl and<br />
picosulfate (the latter two via their common metabolites bisacodyI diphenol, methoxy bisacodyl diphenol<br />
and dimethoxy bisacodyldiphenol) as well as <strong>of</strong> anthraquinone laxatives contained in plants like senna,<br />
cascara, rhubarb, frangula and aloe via their common metabolite rhein. Furthermore, the diuretics<br />
acetazolamide, bemetizide, bendr<strong>of</strong>lumethiazide, bumetanide, butizide, canrenoic acid (also main<br />
metabolite <strong>of</strong> spironolactone), carzenide, chlorothiazide, chlortalidone, c1opamide, cyclopenthiazide,<br />
cyclothiazide, dicl<strong>of</strong>enamide, etacrynic acid, etozolin, furosemide, hydrochlorothiazide, indapamide,<br />
mefruside, metolazone, piretanide, poly thiazide, tienilic acid and xipamide could be detected as well as the<br />
uricosurics benzbomarone, probenecide and sulfinpyrazone, which are relevant in doping control. Cleavage<br />
<strong>of</strong> conjugates was a prerequisite for sensitive detection <strong>of</strong> the laxatives and/or their metabolites, because<br />
these analytes are excreted mainly as conjugates. For analysis <strong>of</strong> diuretics, enzymatic hydrolysis is not<br />
necessary, because they are mainly excreted unchanged. The limits <strong>of</strong> detection (LOD, SIN 3) <strong>of</strong>the tested<br />
drugs and their metabolites lay in the range <strong>of</strong> I to 500 nglmL, 90% within 5 to 100 nglmL. Recoveries<br />
were determined for a limited number <strong>of</strong> analytes (bisacodyl diphenol, butizide, furosemide,<br />
hydrochlorothiazide, phenolphthalein, piretanide, probenecide, rhein, sulfinpyrazone, and tienilic acid)<br />
representing the different groups <strong>of</strong> the structurally heterogeneous analytes and ranged from 33 to 99 with<br />
coefficients <strong>of</strong> variation from 4.2 to 21.1 % (determined at 5 x LOD). Applicability studies showed that at<br />
least the given drugs and/or their metabolites were detectable over periods <strong>of</strong> 24 to 72 hours after<br />
administration <strong>of</strong> the lowest therapeutic dose (picosulfate, 5 mg; furosemide, 40 mg; hydrochlorothiazide,<br />
15 mg; spironolactone, 25 mg; or senna plant extract containing 7 mg <strong>of</strong>sen nos ide B) to one young healthy<br />
volunteer each (after informed consent). Furthermore, the extractive methylation (without the enzymatic<br />
cleavage) has proved to be suitable for simultaneous detection <strong>of</strong> other acidic drugs (Maurer HH, J.<br />
Chromatogr. B 733, 1999, 3).<br />
Conclusion: The presented GC-MS procedure allowed simultaneous identification and differentiation <strong>of</strong><br />
stimulant laxatives, diuretics and/or their metabolites in urine. This procedure should be applicable for<br />
diagnosis or differential diagnosis <strong>of</strong> an abuse <strong>of</strong>the described drugs or for doping control.<br />
Keywords: Diuretics, Laxatives, GC-MS<br />
Page 248
C31 <br />
DETECTION OF NEW MINOR METABOLITES BY LC/MS AND CHARACTERIZATION BY<br />
LCIMS/MS AFTER COMPELLED INGESTION OF COCAINE<br />
L. Humbert l , R. EljaoudLI, F. Orisel 2 , T. Kargar-OriseI 2 , D. Mathieu 3 , M. Lhermitte i<br />
I Laboratoire de Biochimie & Biologie Moleculaire, H6pital Calmette, 59037 Lille Cedex France.<br />
2 Waters Corporation, European Headquarters & Waters S.A.S., Rue Jacques Monod, 78280 Ouyancourt<br />
France. 3 Urgence respiratoire et reanimation medicale, H6pital Calmette, 59037 Lille Cedex France.<br />
A well-known cocaine addict presented spontaneously to the emergency service <strong>of</strong> the Lille Hospital<br />
(France) and reported that he was forced to ingest a large quantity <strong>of</strong> a white powder. Surprisingly, the<br />
patient did not present any intoxication symptoms but was placed under medical observation. Immunoassay<br />
screening <strong>of</strong> a blood sample did not reveal the presence <strong>of</strong> any drugs and immunoassays performed on<br />
urine led to positive results for cocaine only. LCIMS was used to confirm the immunoassay results and the<br />
anticipated metabolites <strong>of</strong> cocaine were found. In addition, many other minor metabolites were detected<br />
and characterized by LCIMSIMS.<br />
Materials and methods: The urine sample was extracted at alkaline pH using a chlor<strong>of</strong>orm/isopropyl<br />
alcohol mixture (9: 1) and evaporated to dryness. 100 ,.d <strong>of</strong> mobile phase was added to the extract and 20 J.l.1<br />
injected onto the LCIMS system. Chromatographic separation was performed using a Waters Alliance<br />
HPLC equipped with a Waters Xterra MS C18 column (ISO x 2.1, 3.5 J.l.m). Mass detection was achieved<br />
using a Waters ZQ mass spectrometer operated in the electrospray mode in both positive and negative ion<br />
polarities. Multi-functional full scan acquisitions were performed at different cone voltages. Well-known<br />
urinary metabolites <strong>of</strong> cocaine were identified through their fragmentation patterns and an additional<br />
LCIMSIMS analysis was performed to elucidate the structure <strong>of</strong> other analytes previously detected in MS<br />
mode that could correspond to new non-documented metabolites. Exhaustive LC/MSIMS study (neutral<br />
loss, parent and daughters, MRM) was performed using a Quattro Premier (Waters) operated in<br />
electrospray combined to modified chromatographic conditions leading to greater retention for the polar<br />
compounds and subsequent better separation efficiency.<br />
Results: The LC/MS analysis <strong>of</strong> the gastric content revealed the presence <strong>of</strong> cocaine. Subsequent LCIMS<br />
analysis <strong>of</strong> the urine samples led to the detection <strong>of</strong> many minors metabolites The oral ingestion was<br />
confirmed by the positive identification <strong>of</strong> characteristic metabolites such as m- and p<br />
hydroxybenzoylecgonine and norbenzoylecgonine l which has also been found metabolised as N<br />
hydroxynorbenzoylecgonine. It was possible to change the selectivity <strong>of</strong>the chromatographic separation by<br />
using a Xterra column at basic pH (10 mM ammonium bicarbonate) allowing the separation <strong>of</strong> several new<br />
polar metabolites which usually coelute when analysed in acidic conditions.<br />
Conclusion: Thanks to the spontaneous presentation <strong>of</strong> the patient, the delay between urine sample<br />
collection and cocaine oral absorption was very short thus allowing the detection <strong>of</strong> many minor<br />
metabolites <strong>of</strong> cocaine not usually found because <strong>of</strong> their very low concentrations. Combining the<br />
sensitivity and the selectivity <strong>of</strong> tandem mass spectrometry with enhanced chromatographic separation, the<br />
expected major metabolites were unambiguously identified and many other new metabolites were detected<br />
and assigned to compounds such as N-hydroxynorbenzoylecgonine, methoxyecgonine and norecgonine<br />
methyl ester.<br />
References: 1. Klette KL, Poch OK, Czarny R, Lau CO. Simultaneous OC-MS analysis <strong>of</strong> m- et p<br />
hydroxybenzoylecgonine and norbenzoylecgonine: a secondary method to corroborate cocaine ingestion<br />
using nonhydrolytic metabolites. J. Anal toxicol. 2000 Oct ;24(7) : 482-8.<br />
Keywords: Forced ingestion, cocaine, metabolite, mass spectrometry<br />
Page 249
C32<br />
URINARY EXCRETION RATES OF KETAMINE AND NORKETAMINE FOLLOWING<br />
THERAPEUTIC KETAMINE ADMINISTRATION: METHOD AND DETECTION WINDOW<br />
CONSIDERATION.<br />
Piotr Adamowicz·, Maria Kala<br />
Institute <strong>of</strong><strong>Forensic</strong> Research, ul. Westerplatte 9, 31-033 Krakow, Poland<br />
Ketamine is widely used in veterinary medicine. Its medical application in humans is limited to children because<br />
in adults it induces severe psychedelic episodes. In recent years, ketarnine has been (ab)used by teenagers as a<br />
recreational and club drug because <strong>of</strong> its hallucinogenic or stimulant effects. Ketarnine is also (mis)used as a 'daterape'<br />
drug - to induce amnesia in unsuspecting victims. In a typical scenario, ketarnine is surreptitiously added by<br />
the perpetrator to the alcoholic beverage <strong>of</strong>an unsuspecting person, who is subsequently sexually assaulted while<br />
under the influence <strong>of</strong>this substance. Many victims do not report the incident until several days after the event.<br />
This situation creates a demand for sensitive analytical methods to reveal the presence <strong>of</strong> the drug and/or<br />
metabolites in biological specimens collected from the victim. The second very important parameter in drug<br />
testing for forensic purposes is the detection window - how long after drug administration a person tests positive<br />
for the drug or metabol ite.<br />
Sensitive gas chromatography-mass spectrometry negative chemical ionization (NCI-GC-MS) and liquid<br />
chromatography-mass spectrometry atmospheric pressure chemical ionization (APCI-LC-MS) methods for the<br />
simultaneous quantification <strong>of</strong> ketarnine and its major metabolite - norketamine in urine were developed and<br />
validated. These methods were used to study the elimination <strong>of</strong>ketamine and norketamine in urine collected from<br />
six hospitalized children (age 4-13 years) who had received a single intravenous dose <strong>of</strong>ketarnine as an anesthetic<br />
for short surgical procedures. The doses ranged from 0.75 to 1.59 mglkg. Individual urine samples were collected<br />
every day or once every two days for 4-16 days.,~<br />
Target analytes were isolated from urine samples after enzymatic hydrolysis (with B-glucuronidaze) followed by<br />
solid phase extraction (HCX column). Ketamine-D 4 and norketamine-D 4 were used as internal standards. For<br />
NCI-GC-MS procedure, extracts were derivatized with HFBA. The monitored negative ions for ketamine<br />
derivative were (mlz) 226 and 357, for norketarnine, 383 and 399, and for norketamine-D 4 , 387 and 403. APCI<br />
LC-MS analyses were carried out without analytes derivatization. Pseudomolecular ions <strong>of</strong> (mlz) 224 and 228<br />
(for norketarnine-Do and -D 4 ), 238 and 242 (for ketamine-Doand -D4) were monitored.<br />
The NCI-GC-MS assay had an LOQ <strong>of</strong> 20 nglmL for ketamine and <strong>of</strong> 50 pg/mL for norketamine, and<br />
displayed LOL across a concentration range <strong>of</strong> 20-1000 nglmL and 50-I 500 pg/mL for parent drug and<br />
metabolite respectively. LOQ and LOL for the APCI-LC-MS method were 2 nglml and 2-2000 ng/mL for<br />
both compounds. For the NCI-GC-MS, mean inter-day precision for ketamine and norketamine ranged<br />
from 21.4-30.4% and 16.8-23.6%, respectively. For the APCI-LC-MS, mean inter-day precision for both<br />
compounds were between 1.6-3.7%.<br />
Using NCI-GC-MS, ketamine was detected in urine <strong>of</strong> four persons up to 1 day and in one up to 2 days<br />
after drug administration. Its concentrations ranged from 58 to 1181 ngimL. Norketamine (measured in<br />
concentrations <strong>of</strong> 1.18 !J.glmL-50 pglmL) was detected up to 14 days (average 7 days). Using the APCI<br />
LC-MS method, ketamine was detected in two persons up to 2 days, in one up to 4 days, in one up to 11<br />
days and in one only up to one day at concentrations <strong>of</strong> 2-813 ngimL. Norketamine (at concentrations <strong>of</strong><br />
1276-2 nglmL) was detected up to 3, 4, 5 and 6 days after drug administration. In one person, ketamine<br />
was not detected through the entire 16-day period using both methods.<br />
Detection window <strong>of</strong> the analytes is highly dependent on the method used for determination and<br />
interindividual variability.<br />
Keywords: ketamine, norketamine, detection window, drug facilitated sexual assault<br />
Page 250
C33 <br />
NOVEL ASPECTS OF IN VITRO METABOLISM OF BUPRENORPHINE<br />
Van Chang* and David E. Moody<br />
Center for Human Toxicology, University <strong>of</strong> Utah, Salt Lake City, UT<br />
Buprenorphine is mainly metabolized by cytochrome P450 (P450) 3A4 mediated N-dealkylation to<br />
norbuprenorphine; both buprenorphine and norbuprenorphine conjugate with glucuronic acid. Previously,<br />
tentative 6-0-desmethyl norbuprenorphine in free and conjugated form and some unknown polar<br />
metabolites were observed in rats; while no other metabolites were observed in human. We find higher<br />
buprenorphine elimination compared to norbuprenorphine formation in human liver microsomes (HLM),<br />
which supports the hypothesis that other metabolic pathways might exist. In the current study, the phase I<br />
and phase II metabolism <strong>of</strong> buprenorphine was investigated in HLM and eDNA-expressed P450s.<br />
Metabolites were screened by LC-MS/MS, coupled with precursor-ion scan, product-ion scan and neutralloss<br />
scan.<br />
The incubation for phase I metabolism was performed in a mixture <strong>of</strong> 0.1 M phosphate buffer (pH 7.4, 1.0<br />
mM EDTA and 5.0 mM MgCh); the NADPH generating system (10 mM glucose-6-phosphate, 1.2 mM<br />
NADP, and 1.2 units gluscose-6-phosphate); and 0.5 mglml microsomal protein. The reaction was initiated<br />
by the addition <strong>of</strong>NADPH generating system in a 37°C shaking water bath and continued for 30 min. The<br />
incubations <strong>of</strong>buprenorphine in cDNA- expressed P450s were performed as described above except that 25<br />
pmol eDNA-expressed P450s was used and the incubation time was 20 min. The incubation for phase II<br />
metabolism was conducted in the presence <strong>of</strong> 25 Ilg/ml alamethicin and 2 mM UDPglucuronosyltransferases.<br />
LC-MSIMS utilized a Finnigan TSQ 7000 equipped with a triple-quadrupole<br />
mass spectrometer and an electrospray ionization source.<br />
During phase I metabolism <strong>of</strong> buprenorphine, 5 metabolites (M 1-M5) in addition to norbuprenorphine were<br />
identified. MI and M2 are hydroxylations <strong>of</strong> buprenorphine at the tert-butyl group and ring moiety,<br />
respectively. M3-M5 are secondary hydroxylation metabolites <strong>of</strong>norbuprenorphine. The hydroxyl groups<br />
are on the tert-butyl group (M3) and ring moiety (M4 and M5), respectively. The metabolism <strong>of</strong><br />
buprenorphine in eDNA-expressed P450s showed that P450 3A5 had highest catalytic activity in Ml<br />
formation, with the involvement <strong>of</strong> 2C8 and 3A7, but their activity is only 5.9% and 3.3% <strong>of</strong> 3A5,<br />
respectively; P450 3A4 has the highest catalytic activity in M3 formation, with contributions <strong>of</strong> 3A7, 3A5<br />
and IA2 to a lesser extent, approximately 12.5%, 2.7% and 2.4% <strong>of</strong> 3A4, respectively. No detectable<br />
signal was observed for M2, M4 and M5 by selected reaction monitoring on LC-MSIMS. M3 is the major<br />
metabolite <strong>of</strong> norbuprenorphine in HLM, which is mediated mainly by P450 3A4, with the contribution <strong>of</strong><br />
3A5 and 3A 7 no more than 6% <strong>of</strong> 3A4. Norbuprenorphine metabolism suggested that secondary<br />
metabolite M3 <strong>of</strong> buprenorphine was formed through norbuprenorphine. The primary study on phase II<br />
metabolism <strong>of</strong> buprenorphine showed the presence <strong>of</strong> conjugated hydroxyl buprenorphine and hydroxyl<br />
norbuprenorphine, the structural identification will be processed in details in the future work.<br />
Keywords: Buprenorphine, Metabolism, P450<br />
Page 251
C34 <br />
CHANNELING THE EMPEROR; WHAT REALLY KILLED NAPOLEON<br />
Francesco Mari l , Elisabetta BertolI, Vittorio Finnechi 2 " Steven B. Karch*3.<br />
IUniversity <strong>of</strong>Florence, Italy, 2University <strong>of</strong>Foggia, Italy, Office <strong>of</strong>the Medical Examiner, City & County<br />
<strong>of</strong>San Francisco, CA<br />
Those with an opinion about the cause <strong>of</strong> Napoleon's death rely largely on the results <strong>of</strong> hair testing. Over<br />
30 different samples, <strong>of</strong> reasonable provenance, have been analyzed. Some samples were obtained during<br />
Napoleon's first exile in Elba, years before he arrived on Saint Helena. Others were obtained at autopsy. All<br />
studies have revealed elevated concentrations <strong>of</strong> arsenic and, in the most recent study, elevated<br />
concentrations <strong>of</strong> antimony as well. These observations, coupled with written accounts <strong>of</strong> the symptoms<br />
and signs exhibited by the Emperor, have led to near universal agreement that arsenic poisoning was the<br />
cause <strong>of</strong> death. For proponents <strong>of</strong> this view, the only question remaining is whether poisoning was<br />
accidental or intentional. Evidence for intentional poisoning comes from the Emperor's own hand. He wrote<br />
in his will, "I die before my time, murdered by the British oligarchy and its hired assassin." Others maintain<br />
that exposure was environmental. Many sources <strong>of</strong> environmental contamination have been proposed, but<br />
there is compelling evidence that Napoleon was poisoned by his own wallpaper; it was painted with<br />
"Scheele's green" pigment, a mixture <strong>of</strong> copper arsenides. It has been known for more than 100 years that<br />
certain molds, some likely to have been present in Napoleon's wall coverings, can volatilize arsenical salts.<br />
Other explanations are possible. Those favoring the poisoning theory tend to minimize the facts that<br />
Napoleon had a rather thorough autopsy. He had requested one because he believed that he, like his father,<br />
might have stomach cancer, and that his children were at risk. The autopsy was performed by one <strong>of</strong><br />
Napoleon's personal physicians, a Corsican named Francesco Antommarchi. Five English physicians were<br />
present, but since Antommarchi was the only one actually trained in anatomic pathology, he performed the<br />
dissection. Though some physicians later expressed divergent opinions about the cause <strong>of</strong> death, none<br />
disputed his anatomic findings: an ulcerated, regionally invasive, carcinoma <strong>of</strong> the greater curvature,<br />
metastasizing into the regional lymph nodes. Since high levels <strong>of</strong> arsenic were clearly present at death and,<br />
according to the latest studies, present for many years, the question to be answered is whether Napoleon<br />
died "<strong>of</strong>" arsenic poisoning, or "with" arsenic poisoning. Recent developments in the treatment <strong>of</strong><br />
promyelocytic leukemia (APL) may provide the answer. Treatment with arsenic trioxide is complicated by<br />
the occurrence <strong>of</strong> QT prolongation, torsades des pointes, and sudden death. Tissue culture studies have<br />
shown that at clinically relevant concentrations, arsenic blocks both I Kr and I ks channels and, at the same<br />
time, also activates kATP channels. The effects cancel each other out, and normal cardiac repolarization is<br />
maintained. The unpredictability <strong>of</strong>QT interval prolongation, and the occurrence <strong>of</strong> ventricular arrhythmias<br />
during arsenic therapy in APL patients, is the result <strong>of</strong> competing effects, blocking and activating multiple<br />
repolarizing potassium currents. The balancing <strong>of</strong>these forces is clearly a delicate matter, one that could be<br />
disrupted by any number <strong>of</strong> extrinsic or intrinsic physiologic forces. Napoleon was given a huge dose <strong>of</strong><br />
tartar emetic (potassium antimony tartrate) the night before he died. Antimony binds to potassium channels.<br />
It appears that the immediate cause <strong>of</strong> death was neither gastric carcinoma, nor chronic arsenic poisoning,<br />
but medical misadventure. Had Napoleon not been given the tartar emetic, arsenical effects on cardiac<br />
conduction would have remained balanced; he would have lived to die a natural death, probably from<br />
gastric carcinoma.<br />
Key Words: Arsenic, Napoleon, Channelopathy<br />
Page 252
Scientific Session <br />
<strong>Abstracts</strong>: . <br />
<strong>Forensic</strong> Urine <br />
Drug Testing & <br />
Adulteration <br />
Page 253
Fl<br />
COMPARISON OF SIMULATANEOUS CAMP AND BMBP MULTIPLE ANALYTE ENZYME<br />
IMMUNOASSA Y REAGENTS WITH ABBOTT AND SYV A EMIT SINGLE ANALYTE<br />
IMMUNOASSA Y REAGENT<br />
Michael 1. Coyer*, Jill Mahoney and Dana Robosky, Clinical Laboratories, Inc, A LabCorp Company,<br />
901 Keystone Industrial Park, Throop, PA 18512.<br />
The development <strong>of</strong> drugs <strong>of</strong> abuse testing (DOA) has seen significant changes since the principals<br />
competitive binding <strong>of</strong> Yalow and Solomon were adapted to DOA screening. The changes in the governing<br />
regulations, the instrumentation and testing requirements has led to more emphasis being placed on turn<br />
around times and cost <strong>of</strong> the test to the client. The many advances in antibody production have enhanced<br />
the selectivity and specificity <strong>of</strong> screening tools much to the advantage <strong>of</strong>the laboratory and the client.<br />
This investigator has begun the evaluation <strong>of</strong> a Multiple Analyte Enzyme Immunoassay (MAEl) products:<br />
specifically, 1.) Cocaine-Amphetamine-Morphine-Phencyclidine (CAMP) and 2.) Barbiturate-Methadone<br />
Benzodiazepine-Propoxyphene (BMBP) recently approved by the FDA for use in the U.S. The design <strong>of</strong><br />
the dual reagent system CAMP and BMBP takes into account the values that are associated with the widely<br />
accepted NIDN SAMHSA screening cut-<strong>of</strong>fs. The reagents are designed to test the four (4) drugs in each<br />
group in a single sampling. The resulting response <strong>of</strong> the instrumentation will be relative to a previously<br />
determined cut-<strong>of</strong>f value. Any result being above the threshold for a positive will be subjected to individual<br />
analyte analysis. The samples giving no response will be considered negative and no further testing would<br />
be performed. The reagent design is based on certain statistical data, specifically, > 90% <strong>of</strong> all urine drug<br />
screens are negative. The design <strong>of</strong> the reagent system will enhance the turnaround time and costs<br />
associated with testing operations while still holding the same high quality standards required <strong>of</strong>the testing<br />
facilities.<br />
This report will focus on the comparison <strong>of</strong> the MAEI reagents with previously tested samples. The<br />
discussions will include comparisons <strong>of</strong>the MAEl with several reagent systems including, but not limited<br />
to, Abbott (FPIA), and SYVA EMIT. The correlations <strong>of</strong> these analysis and discussion <strong>of</strong> the reagent<br />
system will be presented. The preliminary testing has been completed and will be furthered after the<br />
submission <strong>of</strong> this abstract to include statistics, cross reactivity and overall effectiveness in the testing for<br />
drugs <strong>of</strong>abuse.<br />
Keywords: Multiple Analyte Enzyme Immunoassay, drugs <strong>of</strong>abuse, turnaround time<br />
Page 254
F2<br />
URINE ADUL TERA TION TRENDS FROM 2001-2003 <br />
David J. Kuntz*, Chuck Jones, Kris Botelho, and Michael Feldman. Northwest Toxicology, a division <strong>of</strong> <br />
LabOne Inc., Salt Lake City, UT 84124, <br />
The use <strong>of</strong> urine adulterant products to defeat a urine drug test has become an increasingly important issue<br />
for the federal and private drug testing programs. Initially, adulteration products were common household<br />
chemicals. In approximately 1990, the first <strong>of</strong> designed adulterants appeared as Urine Luck containing<br />
glutaraldehyde. Nitrite quickly followed once the detection <strong>of</strong> glutaraldehyde was established. Since that<br />
time a number <strong>of</strong> products have evolved with chromium VI, iodine, iodate, and fluoride as the primary<br />
purchased adulterants. And another disturbing trend in the increase in the number <strong>of</strong> substituted and<br />
invalid specimens reported by the laboratory. These specimens indicate the increased use <strong>of</strong> excessive<br />
hydration to lower urine levels <strong>of</strong> drugs <strong>of</strong> abuse or in the case <strong>of</strong> invalid specimens, the use <strong>of</strong> an<br />
unidentified adulterant.<br />
~.,<br />
The analysis <strong>of</strong> adulteration trends includes only specimens tested by Northwest Toxicology during the<br />
period <strong>of</strong>2001-2003. The total number <strong>of</strong>specimens during each year was approximately 600,000 samples<br />
per year. Each specimen tested by the laboratory receives an analysis for creatinine (specific gravity if<br />
creatinine is less than 20 mg/dL), pH, and adulterants. During 2001-2002, the adulterant test was an<br />
analysis for nitrite and chromium. In 2003, the nitrite and chromium tests were replaced by a general<br />
oxidant test. The analysis <strong>of</strong> the data for the three year period reveals several significant trends in specimen<br />
validity testing (SVT). The number <strong>of</strong> specimens reported as substituted or invalid has more than doubled<br />
from 2001 to 2003 while chromiumVI positive specimens have been reduced by 75%. Nitrite positive<br />
specimens have been reduced by 20% with unexpected increases in bleach and abnormal pH specimens.<br />
Iodine and iodate analysis began in 2002 and has quickly become the number one detected adulterant by<br />
the laboratory. Fluoride is frequently encountered when iodate is also present.<br />
2001 2002 2003 <br />
Substituted 136 192 248 <br />
Unsuitllnv 202 248 442 <br />
Nitrites 98 88 77 <br />
Chromium 241 102 58 <br />
Bleach 5 30 20 <br />
Soap 1 3 ] <br />
pH 48 72 97 <br />
Iodinellodate NA 30 105 <br />
Fluoride NA NA 9 <br />
Glutaraldehyde 0 0 1 <br />
0.12% 0.13% 0.16%<br />
The number <strong>of</strong> adulterated specimens clearly indicates that the routine testing for a single adulterant, such<br />
as nitrite, will not detect the majority <strong>of</strong>adulterated samples and that a comprehensive SVT program must<br />
be developed for the identification <strong>of</strong>these specimens.<br />
Keywords: Specimen validity testing, adulteration, nitrite, chromium<br />
Page 255
F3 <br />
ANALYSIS OF URINARY STEROID SULFATE METABOLITES USING ION-PAIRED<br />
EXTRACTION<br />
'12<br />
Ad am Cawley " Rymantas Kazlauskas<br />
l , Graham Trout l , Adrian George 2<br />
1. Australian Sports Drug Testing Laboratory, National Measurement Institute, Sydney, Australia, 2.<br />
School <strong>of</strong>Chemistry, University <strong>of</strong> Sydney, Sydney, Australia<br />
Urinary steroid metabolites may be excreted in their unchanged (free) form, and/or more likely, as<br />
glucuronide or sulfate conjugates. Routinely, doping control laboratories accredited by the International<br />
Olympic Committee (JOC) and the World Anti-Doping Agency (WADA) screen urine samples collected<br />
from athletes for the presence <strong>of</strong> free and glucuronide conjugated steroids by Gas Chromatography-Mass<br />
Spectrometry (GC-MS) following enzymatic hydrolysis and solid phase extraction. There is a clear need,<br />
however, for laboratories to analyse a number <strong>of</strong> steroids excreted primarily as their sulfate conjugates in<br />
order to further metabolic research and develop confirmation methods that are more specific to particular<br />
steroid administrations. Published methods utilising a range <strong>of</strong> chemical hydrolysis techniques to cleave the<br />
sulfate moiety from steroid metabolites and make them amenable to GC-MS analysis have been<br />
problematic to implement due to urinary matrix effects. To circumvent this problem, ion-pairing extraction<br />
with (-)-N,N-dimethylephedrinium bromide under basic conditions was optimised to obtain a purified<br />
sulfate fraction. Cleavage <strong>of</strong> the sulfate moiety was efficiently achieved by chemical hydrolysis under mild<br />
conditions using methanolic-HCI derived from trimethylchlorosilane (TMCS). The free steroids were<br />
extracted into hexane at pH 9.8 before reaction with N-methyl-N-(trimethylsilyl)trifluoroacetamide<br />
(MSTFA) to form TMS enol ether derivatives that were subsequently analysed by GC-MS. This method<br />
provided linear recoveries (R 2 2:0.9993, 100 to 5000 ng/mL) <strong>of</strong> greater than 90% for androsterone (5aandrostane-3a-oI-17-one)<br />
extracted as the sulfate conjugate. The potential <strong>of</strong> direct urinary sulfate<br />
metabolite analysis using Liquid Chromatography-Mass Spectrometry (LC-MS) is also discussed as a<br />
means to alleviate the need for chemical hydrolysis. While these methods are directed at steroid detection<br />
for IOCfW ADA laboratories they may be applied in a broader toxicological sense for the analysis <strong>of</strong><br />
sulfated metabolites <strong>of</strong> other drugs <strong>of</strong> abuse. Novel analysis methods such as these may also allow more<br />
detailed metabolic studies to be carried out to determine new markers <strong>of</strong> specific drug abuse, thus<br />
demonstrating their potential as a valuable confirmation technique. Incorporated into the GC-MS method<br />
validation was an evaluation <strong>of</strong> a reasonable estimate <strong>of</strong> measurement uncertainty that is presented as an<br />
example to emphasise the importance <strong>of</strong>ISO 17025 compliance for forensic toxicology laboratories.<br />
Keywords: urinary sulfate metabolites, ion-paired extraction, measurement uncertainty<br />
Page 256
F5 <br />
PAPAIN, A NOVEL URINE ADULTERANT<br />
David L. Burrows l ', M.S.; Andrea Nicolaides\B.S.; David A. Johnson 2 , Ph.D.; Michelle M. Duffourc\<br />
Ph.D.; Kenneth E. Ferslew i , Ph.D., Section <strong>of</strong> Toxicologyl, Dept. <strong>of</strong> Phannacology',3; Dept. <strong>of</strong><br />
Biochemistry and Molecular Biology2, James H. Quillen College <strong>of</strong> Medicine, East Tennessee State<br />
University, Johnson City, TN. 37614<br />
The estimated number <strong>of</strong> employees in the United States screened annually for illicit drugs is<br />
approximately 20 million, with marijuana being the most frequently abused drug. Urine adulterants<br />
provide an opportunity for illicit drug users to obtain a false negative result on commonly used primary<br />
drug screening methods such as the Fluorescence Polarized Immunoassay (FPIA) technique. Typical<br />
chemical adulterants such as nitrites are easily detected or render the urine specimen invalid as defined in<br />
the proposed SAMHSA guidelines for specimen validity testing based on creatinine, specific gravity and<br />
pH.<br />
Papain is a cysteine protease with intrinsic ester hydrolysis capability and several residues that serve as<br />
hydrophilic and hydrophobic binding sites that can act as a potential urine adulterant. These mechanisms<br />
would exists in a. novel class <strong>of</strong> urine adulterants and urine adulteration with hydrolytic enzymes can be<br />
attained with a relatively smaller quantity as compared to their typical chemical counterparts. The primary<br />
metabolite <strong>of</strong> the psychoactive chemical in marijuana, Il-norcarboxy-delta-9-tetrahydrocannibinol<br />
(I INC), was assayed by FPIA in concentrations ranging from 25 to 500 ng/mL, at pH values ranging from<br />
4.5 to 8, over the course <strong>of</strong>3 days with papain concentrations ranging from 0 to 10 mg/mL. FPIA analysis<br />
<strong>of</strong> other frequently abused drugs: amphetamines, barbiturates, benzodiazepines, cocaine, opiates, and<br />
phencyclidine, along with gas chromatography I mass spectrometry (GCIMS) <strong>of</strong> IINC and high<br />
perfonnance liquid chromatography I ultraviolet (HPLC/uV) <strong>of</strong> nordiazepam was perfonned in order to<br />
determine if the mechanism <strong>of</strong> urine adulteration by papain was analyte specific. Control and adulterated<br />
urine specimens (n=30) were assayed for creatinine, specific gravity, osmolarity and pH to detennine if<br />
papain rendered the specimens invalid based on the proposed SAMHSA guidelines. There was a direct<br />
pH, temperature, and time dependent correlate between the increase in papain concentration and the<br />
decrease in IINC concentration from the untreated control groups (p
---.,.<br />
F4<br />
IODINE CONTAINING ADULTERANT -<br />
DETECTION BY INTECT® 8<br />
ITS EFFECT ON RAPID DRUG SCREEN AND<br />
Beckie Chien*, Jan Sook, Raphael C. Wong, Branan Medical Corporation, Irvine, CA, USA<br />
Aims:New generation <strong>of</strong> commercial adulterants have included iodine as the main ingredient at sample<br />
concentration <strong>of</strong> about 1 mg per ml. The objective <strong>of</strong> this study was to evaluate iodine's effect on a certain<br />
rapid drug screen and its detection by an onsite adulterant dipstick, Intect®8.<br />
Method: The adulteration effect <strong>of</strong> iodine was studied by adding iodine to a urine sample containing three<br />
times the SAMHSA cut-<strong>of</strong>f concentrations <strong>of</strong> five drugs including benzoyl ecgonine (COC), morphine<br />
(OPI), amphetamine (AMP), THC and PCP. The final concentration <strong>of</strong> iodine in the sample was 1 mg/mt.<br />
The adulterated sample was then tested by an onsite rapid drug screen Monitect® PCll over one hour<br />
period. The same sample was also tested with the new Intect 8 onsite adulteration test strip that contains g<br />
test pads including creatinine (CR), nitrite (NI), glutaraldehye CGL), pH, specific gravity (SG), bleach (BL),<br />
pyridinium chlorochromate (PCC) and iodine (I) to evaluate the adulterant's detection over time.<br />
Results: Negative (-) result in the drug screen indicates adulterant was able to modify the positive drug test<br />
result to negative result whereas (+1-) indicates a possible adulteration effect for that specific drug; normal<br />
(N) result in the Intect 8 pad suggests no effect <strong>of</strong> iodine on the specific test pad while abnormal (A)<br />
indicates detection <strong>of</strong>the adulterant by the specific pad.<br />
! Time (min.) COC OPI I AMP I THC PCP<br />
Drug 5 Invalid results due to no control line<br />
i<br />
Screen 10 +<br />
+ + I -<br />
+<br />
Result 30 + + L + I - +<br />
60 + +1 I + I - +<br />
Time I· CR I Nl GL I ~H SG BL PCC L I<br />
I<br />
5 I N I N N N N A A I A<br />
Intect 8<br />
Result<br />
10 N : N N N N A A I<br />
I<br />
A<br />
30 N j N N N N A A I A<br />
60 I N 1 N N N N N N I N<br />
I<br />
Urine spiked with PCC or BL did not cause an abnormal result with the Iodine pad.<br />
Conclusion: Iodine containing adulterant is shown to mask the presence <strong>of</strong>THC. It also has some effect on<br />
opiate. This adulterant is detectable by an onsite adulteration test device Intect®g in a 30-minute window.<br />
Keywords: Adulteration, Intect, iodine<br />
Page 257
F6 <br />
A COMPARATIVE EVALUATION OF THE INSTANT-VIEW 5 PANEL TEST CARD WITH<br />
ONTRAK TESTCUP PRO 5: COMPARISON TO GCIMS AND INSTRUMENT SCREENING<br />
WITH ONLINE REAGENTS<br />
David E. Moody'*, Wenfang B. Fangl, David M. Andrenyak ' , Kim S. Monti l , and Chuck Jones 2. <br />
ICenter for Human Toxicology, University <strong>of</strong> Utah, Salt Lake City, UT 84112, 2 Northwest Toxicology, <br />
Salt Lake City, UT 84124 <br />
We have compared the ability <strong>of</strong> two on-site testing devices, Instant-View Test Card (Alfa Scientific<br />
Designs, Inc., Poway, CA) (I) and OnTrak TesTcup (Roche Diagnostics Corp., Indianapolis, IN) (T) to<br />
discriminate negative from positive urine samples for the following five drug groups: cannabinoids,<br />
cocaine metabolite, opiates, amphetamines and benzodiazepines. Samples for a precision study were<br />
prepared for each device separately due to cut<strong>of</strong>f and primary antigen differences. A drug-free urine pool<br />
was fortified in a random fashion to contain the primary antigen at seven concentrations (0, 2S, SO, 75, 12S,<br />
ISO and 17S% <strong>of</strong> cut<strong>of</strong>f). These stocks were than submitted for GCIMS confirmation and then 10 aJiquots<br />
from each where prepared and assigned random numbers <strong>of</strong> I-70 for each test device. All drug groups,<br />
except for cannabinoids were within 10% <strong>of</strong> target and target concentrations were used for the evaluation.<br />
Cannabinoids deviated more than IS% from target. The GCIMS-determined concentrations were used for<br />
cannabinoids; this resulted in samples at 0,62, 80, 102, 136, 158 and 170% <strong>of</strong> cut<strong>of</strong>f. Two individuals<br />
tested each sample. None <strong>of</strong> the °or 2S% (0 or 62% for cannabinoids) cut<strong>of</strong>fs tested positive with any<br />
device. The results for the rest <strong>of</strong> the samples can be summarized as follows where for each device we first<br />
list the % <strong>of</strong> below cut<strong>of</strong>f samples testing positive and the % <strong>of</strong> above cut<strong>of</strong>f samples testing negative:<br />
cannabinoids (1-3.3, 47.5; T-O, 40); benzoylecgonine (1-2S, 8.3; T-16.4, 0); morphine (I-2.5; 21.7; T -10,0);<br />
amphetamines (1-0, 60; T-22.S, 0) and benzodiazepines (I-8.8, \S; T-O, 21.7). Similar data were collected<br />
for an automated immunoassay using Online reagents; the only imprecise result was for cannabinoids at<br />
102% <strong>of</strong> cut<strong>of</strong>f where IS% <strong>of</strong> the samples tested negative. Samples submitted to NWT were used for the<br />
clinical study. Seventy-five samples that recently screened negative were rescreened for the five drug<br />
groups and the fifty with the lowest absorbance readings were selected as negative samples. Positive<br />
samples were selected from actual positives that had reached their disposal date. They were rescreened for<br />
all five drug groups. Those with results> the 75% control in the screening batch were then submitted to<br />
GCIMS confirmation for the particular drug group. Sufficient samples were screened and confirmed to get<br />
at least 45 samples above the device specific cut<strong>of</strong>f; with many samples near cut<strong>of</strong>f and some just below<br />
cut<strong>of</strong>f. As each on-site device will test for all five drug groups simultaneously, this provided::::: ISO<br />
additional samples that were presumptively negative per drug group. Samples were assigned random<br />
numbers, and two individuals tested each sample. Providing results as the percent <strong>of</strong> device positives when<br />
the GC/MS results (sum <strong>of</strong> analytes in many case) are
F7 <br />
Direct Analysis <strong>of</strong> Opiates in Urine by Liquid ChromatographylMass Spectrometry!<br />
Mass Spectrometry<br />
Leslie E. Edinboro, MS, PhD, *,1,2 Ronald C. Backer, PhD. 3 & Alphonse Poklis, PhD.l<br />
1. Department <strong>of</strong> Pathology, School <strong>of</strong> Medicine, 2. Department <strong>of</strong> Pharmaceutics, School <strong>of</strong> Pharmacy,<br />
Virginia Commonwealth University, Richmond, Virginia, 3. AmeriTox Laboratory, Midland, Texas.<br />
A method for the direct analysis <strong>of</strong> ten opiate compounds in urine was developed using Liquid<br />
ChromatographylMass SpectrometrylMass Spectrometry (LCIMSIMS). Opiates included were: morphine-<br />
3-f3-glucuronide, morphine-6~~-glucuronide, morphine, oxymorphone, hydromorphone, norcodeine,<br />
codeine, oxycodone, 6-monoacetylmorphine (6MAM) and hydrocodone. Deuterated internal standards<br />
used were morphine-d 3 and 6MAM-~. Urine samples were prepared by addition <strong>of</strong> the internal standard<br />
solution, centrifugation to remove large particles and direct injection into the LCIMSIMS. Gradient reverse<br />
phase separation was accomplished on a phenyl column using acetonitrile and water modified with formic<br />
acid and ammonium formate. An electrospray ionization (ESI) interface was used to introduce the LC<br />
eluent into the MS. Multiple Reaction Monitoring (MRM) was utilized for detection in the MSIMS mode<br />
based upon pre-established precursor: product mJz transitions. Separation and detection <strong>of</strong> all compounds<br />
was accomplished within six minutes. Selectivity and possible ion suppression were evaluated using 10<br />
different blank urines. Linearity was established for all opiates except 6MAM from 50 nglmL to 10,000<br />
nglmL; 6MAM from 0.25 ng/mL to 50 ngimL. Correlation coefficients (r) for all opiates was > 0.99. Interrun<br />
precision (%CV) ranged from 1.1 % to 16.7%. Intra-run precision ranged from 1.3% to 16.3%.<br />
Accuracy (% Bias) ranged from -7.3% to 13.6% and -8.5% to 11.8 for inter and intra-run respectively. 89<br />
urine samples previously analyzed by GCIMS were re-analyzed by the LCIMSIMS method. The qualitative<br />
results found an 88% agreement for negative samples between the two methods and 94% for positive<br />
samples. The LCIMSIMS method identified 19 samples with additional opiates in the positive samples.<br />
Ten samples were oxymorphone positive that the GCIMS method was not setup to detect. Of these, 90%<br />
were associated with GCIMS positiYe oxycodone samples, which metabolically are justified. Additionally<br />
three samples were· hydromorphone positive for GCIMS hydrocodone positive samples, which also is<br />
likely. The remaining positive samples were oxymorphone, oxycodone, hydrocodone and hydromorphone.<br />
Quantitatively it was difficult to compare the two methods as the GCIMS method utilized a glucuronidase<br />
step that was not included in the LCIMSIMS method. Therefore only the morphine results could be<br />
compared if the LCIMSLMS results for the glucuronide metabolites were summed on a molar basis with the<br />
morphine. The R2 was 0.78. The difference between the methods is probably due to the efficiency <strong>of</strong> the<br />
GCIMS glucuronidase procedure. Overall the direct injection LCIMSIMS method performed well and<br />
permitted the rapid analysis « 6,0 minutes) <strong>of</strong> urine samples without extensive sample preparation for<br />
several opiates simultaneously. Additionally the method provided a lower limit <strong>of</strong> quantitation for 6MAM<br />
than previously reported utilizing direct injection techniques. The method could be further improved with<br />
the addition <strong>of</strong> compound specific deuterated internal standards and other glucuronide metabolites, i:e.,<br />
hydromorphone.<br />
Keywords: Opiates, LCIMS/MS, Urine<br />
Page 260
F8 <br />
UNUSUAL DRUG TEST RESULTS FROM KNOWN HEROIN USERS<br />
Neil Fortner*l , Doug Crook l , Dr. Robert Turk 2 , Andrew Waszyn 3<br />
iPharmChem Inc., Haltom City, TX, USA, 2Center for Toxicology Services, Inc, Humble, TX, USA<br />
,3United States Probation, Western District <strong>of</strong>Pennsylvania<br />
The use <strong>of</strong> total morphine levels in urine has traditionally been one approach to predicting the use <strong>of</strong><br />
heroin. Recently we have encountered several situations that would suggest this practice should be revisited.<br />
Five individuals that were either on supervised release or on parole were tested for illicit drugs as a<br />
condition <strong>of</strong> their release. These individuals were comprised <strong>of</strong> two black males, one black female, one<br />
white male and one white female. The ages <strong>of</strong> these individuals ranged from 29 to 70 years, with an<br />
average age <strong>of</strong> 51 years. All individuals were experienced with heroin (either use or possession). Based on<br />
their history <strong>of</strong> drug use, these individuals were subject to periodic urine drug testing. These samples were<br />
screened for illicit drugs, including opiates, using reagents manufactured by Diagnostic Reagents, Inc. The<br />
screening cut<strong>of</strong>f level for opiates was 300 ng/ml. All samples screened negative for opiates. Due to their<br />
past experience with heroin, a special test for 6-AM was requested on each sample. All samples were<br />
positive for 6-AM with the concentrations ranging from 10 to 144 nglml. To investigate this apparent false<br />
negative immunoassay screen, all samples were analyzed for the presence <strong>of</strong> codeine, total morphine and<br />
heroin. All samples were negative for both codeine and heroin. All total morphine levels were less than 300<br />
nglml, which substantiated the negative immunoassay results. Total morphine levels ranged from 18 to 245<br />
nglmL These results suggest that the traditional approach for predicting heroin use based on total morphine<br />
levels need to be looked at more closely, as current practice may in fact underestimate instances <strong>of</strong> heroin<br />
use.<br />
Keywords: heroin, 6-acetylmorphine, morphine<br />
Page 261
F9 <br />
ESTIMA TE OF DETECTION PERIOD IN URINE FOR MARKERS OF STREET HEROIN<br />
Sue Paterson*, Rosa Cordero, Simon Burlinson<br />
Toxicology Unit, Imperial College London, St Dunstan's Road, London W6 8RP, UK<br />
Nick Lintzeris<br />
National Addiction Centre, 4 Windsor Walk, London SE5, UK<br />
There is growing international interest in prescribed pharmaceutical heroin as treatment for individuals who<br />
are unable to stop injecting opiate drugs. The rationale for this treatment is one <strong>of</strong> "harm minimisation". In<br />
a previous paper (1) co-workers reported on the GC-MS analysis <strong>of</strong> over 1000 urine samples from patients<br />
attending a substance misuse service during which metabolites <strong>of</strong> various contaminants <strong>of</strong> street heroin<br />
were detected. They concluded that the detection <strong>of</strong> papaverine and noscapine metabolites was likely to<br />
provide a reasonably sensitive and highly specific means <strong>of</strong> identifying the illicit use <strong>of</strong> heroin in patients<br />
prescribed diamorphine. We believe that these markers <strong>of</strong>fer the best means <strong>of</strong> determining the use <strong>of</strong> street<br />
heroin in these patients. The aim <strong>of</strong> this study was to estimate the detection period for identifying markers<br />
in the urine <strong>of</strong> street heroin users. Over 50 urine samples were collected from patients who admitted to the<br />
use <strong>of</strong> street heroin within the previous 72 hours. The researcher interviewed each subject regarding all<br />
episodes <strong>of</strong> drug use within the preceding 72 hours, including details <strong>of</strong> amount used, route <strong>of</strong><br />
administration and time <strong>of</strong> use. The time the urine was passed was also noted. These samples were analysed<br />
by the method currently in use for the routine analysis <strong>of</strong> urine samples from patients attending drug<br />
treatment centres, that is mixed-mode solid-phase extraction (SPE) followed by GC-MS (2). Urine samples<br />
were subjected to enzymatic hydrolysis followed by SPE using Bakerbond narc-2 columns. The eluent was<br />
selectively derivatised with N-methyl-bis-tritluoroacetamide and N-methyl-N-trimethylsilyltrifluoroacetamide<br />
+ 1% trimethylchlorosilane. Analysis was performed using a GC-MS system operating in full<br />
scan mode. The study samples were analysed for the commonly abused drugs plus a range <strong>of</strong> other drugs<br />
including antidepressants and certain anti psychotics that are prescribed to these patients. In addition, the<br />
metabolites <strong>of</strong> papaverine, hydroxy and dihydroxypapaverine, and the metabolites <strong>of</strong> noscapine, meconine<br />
and hydroxymeconine, were looked for in each sample. Other contaminants <strong>of</strong> street heroin including<br />
papaverine, noscapine, thebaine, and acetylcodeine were also monitored. Using this assay the limit <strong>of</strong><br />
detection for morphine was 0.05 ugimL. The limit <strong>of</strong> detection for hydroxy and dihydroxypapaverine could<br />
not be determined as pure standards were not commercially available. A characteristic peak pattern in the<br />
chromatogram was found to be indicative <strong>of</strong> the presence <strong>of</strong> the papaverine metabolites, which were then<br />
matched by retention time and spectra obtained from the elucidation <strong>of</strong> these metabolite derivatives as<br />
reported previously (1). Initial analysis <strong>of</strong> the data shows that hydroxy and dihydroxpapaverine were<br />
detected in urine for approximately the same period as morphine. This data supports the findings <strong>of</strong><br />
McLachlan-Troup et al that hydroxy and dihydroxypapaverine can be used to determine if patients<br />
prescribed injectable diamorphine are "topping-up" with street heroin. Papaverine, noscapine, thebaine and<br />
acetyl codeine were not detected in any <strong>of</strong> the study samples.<br />
l. N, McLachlan-Troup, G.W. Taylor, B.c. Trathen. Diamorphine treatment for opiate dependence:<br />
putative markers <strong>of</strong> concomitant heroin misuse. Addiction Biology, 2001; 6: 223-231<br />
2. S Paterson, R Cordero, S McCulloch, P Houldsworth. Analysis <strong>of</strong> urine for drugs <strong>of</strong> abuse using mixedmode<br />
solid-phase extraction and gas chromatography/mass spectrometry. Ann. Ojefin. Biochem. 2000; 37:<br />
690-700.<br />
Keywords: Street heroin markers, papaverine metabolites, noscapine metabolites<br />
Page 262
FlO<br />
EFFECTIVENESS OF FREE AND TOTAL MORPHINE CONCENTRATION AS CRITERIA FOR<br />
SELECTING URINE SPECIMENS FOR TESTING 6-ACETYLMORPHINE<br />
3 4<br />
Sheng-Meng Wan~I.2, John W. Soper',2, Dennis Canfield 2 , and Ray H. Liu 2 . • , ICentral Police University,<br />
Taoyuan, Taiwan. Toxicology and Accident Research Laboratory, FAA Civil Aerospace Medical Institute,<br />
Oklahoma City, OK, U.S.A. 3Department <strong>of</strong> Medical Technology, Fooyin University, Kaohsiung Hsien,<br />
Taiwan. 4Department <strong>of</strong> Justice Sciences, University <strong>of</strong> Alabama at Birmingham, Birmingham, AL,<br />
U.S.A. *Presenting Author<br />
The U.S. Department <strong>of</strong> Health and Human Services' workplace urine drug testing program has adopted a<br />
2000 ng/mL total morphine concentration as the criterion for testing 6-acetylmorphine (6-AM). We were<br />
interested in evaluating whether such a criteria can be applied to specimens collected from workers in<br />
Taiwan, a genetically different group than the typical US worker. Two hundred and thirteen workplace<br />
specimens, testing positive for opiates by immunoassay (cut<strong>of</strong>f 300 ng/mL), were analyzed for 6-AM, and<br />
for free and total morphine, by GC-MS methods. Recovery efficiencies <strong>of</strong> extraction and hydrolysis<br />
protocols (for total morphine determination) were evaluated and used to derive analyte concentrations in<br />
test specimens. In reference to an earlier report by Paul et al [1], data hereby obtained were used to<br />
determine whether free or total morphine concentration is more effective in predicting the presence <strong>of</strong> 6<br />
AM in 2 different concentration ranges: >10 ng/mL and 5-10 ng/mL. As shown in Table 1,4 specimens<br />
were found to contain from 5-10 ng/mL <strong>of</strong> 6-AM, while 55 specimens were ~10 ng/mL. This total <strong>of</strong> 59<br />
specimens showed the presence <strong>of</strong> 6-AM at >5ng/ml, regardless <strong>of</strong> whether total morphine (2000 ng/mL)<br />
or free morphine (50,100, or 200 ng/mL) concentration was used as the cut<strong>of</strong>f for selecting specimens for<br />
6-AM determination.<br />
Table 1. Effectiveness <strong>of</strong> free and total morphine in predicting the presence <strong>of</strong> 6-AM<br />
,"~,<br />
Analyte concn No. <strong>of</strong> No. <strong>of</strong> specimen with 6-AM concn (ng/mL)<br />
(ng/mL) specimen >10 5.0-10 1.0-4.9 Negative"<br />
Total morphine<br />
~300 213 55 (25.8%)t 4 14 140<br />
~2000 162 55 (34.0%) 4 12 91<br />
~4000 142 55 (38.7%) 3 9 75<br />
Free morphine<br />
~50 181 55 (30.4%) 4 12 110<br />
~100 168 55 (32.7%) 4 12 97<br />
~200 154 55 (35.7%) 4 11 84<br />
" Limit <strong>of</strong> detection: 1 ng/mL.<br />
t Numbers inside parentheses are the percentages <strong>of</strong>the morphine positive (using the cut<strong>of</strong>f listed in the<br />
first column in respective rows) specimens that were found to contain ~1 0 ng/mL 6-AM.<br />
Data resulting from this study indicate comparable effectiveness in using either 2000 ng/mL total morphine<br />
or 100 ng/mL free morphine as the criterion for selecting specimens to further test for the presence <strong>of</strong> 6<br />
AM at the 10 or 5 ng/mL level. The free morphine option is less costly, avoids uncertainty associated with<br />
the hydrolysis process, and may produce more nearly accurate results. This study provides an addition to<br />
the free morphine-related database and adds further confidence to the use <strong>of</strong> free morphine data, which is<br />
not readily available.<br />
References:<br />
1. B.D. Paul, E.T. Shimomura, and M.L. Smith. A practical approach to determine cut<strong>of</strong>f concentrations<br />
for opiate testing with simultaneous detection <strong>of</strong> codeine, morphine, and 6-acetylmorphine in urine.<br />
C/in. Chern. 45: 510-519 (1999).<br />
Keywords: Heroin, free-Morphine, 6-mono-acetyl Morphine<br />
Page 263<br />
1
Fll<br />
REVIEW OF AN UNUSUAL MULTI-DRUG POSITIVE USAF MEMBER CASE<br />
Vincent M.Papa l *, Sarah Ozmene, Timothy Cox 2 , Terence FarreU 2 , Aaron Jacobs 3<br />
I Air Force Drug Testing Laboratory Brooks City-Base, Texas 78235; 2 1 FW/JA LangeJy AFB, Virginia<br />
23655; 3 Division <strong>of</strong> <strong>Forensic</strong> Toxicology, Armed Forces Institute <strong>of</strong> Pathology, Division <strong>of</strong> <strong>Forensic</strong><br />
Toxicology, Rockville, MD 20850<br />
The Air Force Drug Testing Laboratory (AFDTL) tests approximately 400,000 military specimens/year for<br />
THC, cocaine, amphetamines, PCP, opiates, barbiturates and LSD. Only 88-90 member specimens are<br />
positive for multiple drugs. A case report on specimens positive for mUltiple drugs may have a complex<br />
interpretation. The member underwent on consent urinalysis on late Friday evening/Saturday morning. The<br />
week preceding this positive result, the individual member had an occupational accident where the cleaner<br />
" Googone " was sprayed into his eyes. He was prescribed Tylox for pain resulting from ocular damage.<br />
On the night preceding the drug test, a call was made to 911 after his girlfriend found him unresponsive.<br />
EMTs noted dilated pupils and that he was not cooperative. He was transported exhibiting combative and<br />
belligerent behavior to a local hospital. At the hospital, the member responded to questions but had lapses<br />
in memory. A drug and alcohol screen was performed at the hospital. The alcohol screen was negative but<br />
the drug screen was positive for cocaine and THC as benzoylecognine and I I-nor carboxy THC. A consent<br />
urinalysis was obtained and analyzed at the Armed Forces Institute <strong>of</strong> Pathology (AFIP). Analysis for THC,<br />
cocaine, amphetamines, PCP, opiates and barbiturates were performed by Axsym screen and GCMS<br />
confirmation. Medical history indicated that he had ingested psilocin mushrooms so an analysis for<br />
psilocyn was accomplished using a gas chromatography (GC) screen and GCMS confirmation. The<br />
following drugs were detected and quantified:<br />
1) Benzoylecognine 3148 ng/ml<br />
2)MDMA<br />
5947 ng/ml<br />
3) Psilocin 6450 ng/ml<br />
4) 11- nor carboxy THC 135 ng/ml<br />
The defense asserted that the individual was not capable <strong>of</strong> giving consent due to the number <strong>of</strong> drugs<br />
detected and the fact that he was taking Tylox and drinking heaVily. There were 15 pills missing. His<br />
girlfriend reported that he was dinking beer and mixed drinks. Additional analysis at AFIP revealed the<br />
presence <strong>of</strong> 165 ng/ml urinary oxycodone. Psychiatric analysis was performed for competency to consent.<br />
At trial, the military judge ruled the member mentally capable. Investigation revealed that the member the<br />
evening <strong>of</strong> the hospital admission consumed 4-5 caps <strong>of</strong> psilocyn mushrooms, one MDMA tablet and<br />
smoked a marijuana blunt laced with cocaine. In this case, psilocyn results were approximately 6X higher<br />
than the levels reported by Sticht et.aI.(I). Furthermore, there are reports <strong>of</strong> smoking marijuana blunts that<br />
have elevated THC percentages. Aggressive and belligerent behavior exhibited in the above report is<br />
consistent with synergistic effects <strong>of</strong> multiple drug consumptions <strong>of</strong>hallucinogens and stimulants.<br />
l.G.Sticht, H.Kaferstein" Detection <strong>of</strong>psilocin in body fluids, <strong>Forensic</strong> Science International 113 (2000)<br />
403-407.<br />
Keywords: psilocin, marijuana, cocaine, mdma<br />
Page 264
F12 <br />
TITLE: AMPHETAMINE CONCENTRATIONS IN URINE AFTER THE USE OF DEXEDRINE<br />
"GO-PILLS": COMPARISON OF SINGLE AND DOUBLE DOSES OF D-AMPHETAMINE.<br />
P.L. Mobley*, S.H. Constable, R.D. Vanderbeek, T.A. Frazier, C.S. Ramsey, D. Wheeler<br />
Presenting Author: Philip L. Mobley, Ph.D. Business Address: Air Force Drug Testing Laboratory,<br />
AFIOH/SDT, 2730 Louis Bauer Drive, Brooks AFB, TX 78235<br />
The Air Force, under the close supervision <strong>of</strong> flight surgeons, approves the use <strong>of</strong> amphetamine for both<br />
active duty and reserve Air Force aviators to counter performance problems during long military missions<br />
associated with fatigue and sleep deprivation. These pilots may also be subjected to urine drug tests, which<br />
include testing for amphetamines by DoD. Studies were conducted to determine the window <strong>of</strong> detection<br />
for amphetamine after the administration <strong>of</strong> Dexedrine ("Go-Pills") at two approved doses. Volunteers<br />
(22-58 years, mean=38.7 years) were administered a single IOmg dose <strong>of</strong> d-amphetamine (N=31), or two<br />
10mg doses four hours apart (N=31). A urine specimen was collected from each subject just prior to drug<br />
administration and collected ad libitum thereafter for several days. Urine was screened using the KIMS<br />
immunoassay. GCIMS was performed on specimens from each subject until the amphetamine<br />
concentration fell consistently below 350ng/ml in the screen test. Based on GC/MS analysis, peak urine<br />
concentrations <strong>of</strong> amphetamine ranged from 602 ng/ml to 12,191 ng/ml with a mean <strong>of</strong> 3345 ng/ml in the<br />
single-dose study, and from 1,339 ng/mJ to 15,359 ng/ml with a mean <strong>of</strong> 6076 ng/ml in the two-dose study.<br />
The time at which the highest (peak) concentration was observed ranged from 2.6 to 29.6 hours with a<br />
mean <strong>of</strong> 12.3 hours (sd=6.3) in the single dose study, and from 4.0 to 26.5 hours with a mean <strong>of</strong> 13.8 hours<br />
(sd=6.7) in the two-dose study. The time to the last identified positive (>500 ng/ml) in each subject ranged<br />
from 2.6 to 46.7 hours with a mean <strong>of</strong> 31.3 hours (sd=9.7) in the single-dose study, and from 29.1 to 71.5<br />
hours with a mean <strong>of</strong> 44.8 hours (sd=9.3) in the two-dose study. The excretion rate half-life <strong>of</strong><br />
amphetamine in the urine was approximately 12 to 13 hours in both test groups. These studies indicate that<br />
most pilots should be below the DoD cut<strong>of</strong>f <strong>of</strong> 500 ng/mJ within 48 hours after a single 10 mg dose, and<br />
within 72 hours after the 2xlO mg dose.<br />
Key Words: Amphetamine, Urine, Go-Pills<br />
Page 265
F13 <br />
WORKPLACE URINE OPIATE TESTING: A CASE OF SCIENTIFIC INJUSTICE IN THE U.K.<br />
William Westenbrink*, <strong>Forensic</strong> Alliance Limited, Abingdon, Oxon, U.K.<br />
A successful pr<strong>of</strong>essional accepts a supervisory nursing position, provisionally, pending a negative urine<br />
drug test. She advises that she may have taken paracetamol within two weeks prior to the testing.<br />
Unexpectedly, the subject's urine, Sample A, is found to contain a 'total' morphine concentration <strong>of</strong> 403<br />
ngimL. The employer, based on this 'positive' test, refuses her the position, and the company's medical<br />
review <strong>of</strong>ficer will hear no explanation whatsoever. Five months later the certificate with the test result <strong>of</strong><br />
Sample A and the second urine sample, Sample B, are released to the donor. Independent analyses indicate<br />
'free' morphine <strong>of</strong> 27 nglmL, 'total' <strong>of</strong> 687 ng/mL and the presence <strong>of</strong> thebaine in this second sample. No<br />
codeine is detected. The total morphine values exceed the U.K. morphine limit <strong>of</strong> 300 ng/mL, yet both<br />
sample results are below the U.S. and U.S. Military limits <strong>of</strong> 2,000 ng/mL and 4,000 ng/mL respectively.<br />
As will be discussed, selected requirements within the U.K. Guidelines for Legally Determined Workplace<br />
Drug Testing were not followed. Violations include: the lack <strong>of</strong>temperature measurements, witnessing the<br />
original sealing <strong>of</strong> the samples followed by the samples being subsequently unsealed, repackaged, and<br />
resealed with the original seals, no hand washing between various samples being handled, no disclosure <strong>of</strong><br />
original results, no timed release <strong>of</strong> Sample B, nor the availability <strong>of</strong> declaring a 'dietary source' on the<br />
disclosure forms, amongst others. No interpretations were carried out with consultation between the<br />
medical review <strong>of</strong>ficer with the original toxicologist and the general medical practitioner <strong>of</strong> the donor,<br />
concerning the 'positive' result, as required. In fact, the donor was originally verbally told that 'codeine'<br />
was present in her urine via telephone.<br />
The source <strong>of</strong> morphine was the consumption <strong>of</strong> 'Warburton's Seeded Batch Bread' containing<br />
approximately 0.5 grams <strong>of</strong> poppy seeds per slice. The donor had eaten this bread during the four days<br />
prior to the drug testing date and on many other previous occasions. Having provided the employer with<br />
this information, the company refuses to overturn its original decisions: that the donor was positive for<br />
morphine without reasonable excuse nor place her in the position for which she had been successful,<br />
despite having dismissed the original medical review <strong>of</strong>ficer. The donor remains unable to secure suitable<br />
pr<strong>of</strong>essional employment in her field because on all subsequent employment applications she must indicate<br />
that she has been refused employment as a result <strong>of</strong> a positive urine drug test. Each time such violations<br />
occur in drug testing at the workplace programs, insurmountable injustices are placed on the victims, as this<br />
cases demonstrates.<br />
Keywords: workplace, drug-testing, morphine<br />
Page 266
F14 <br />
AUTOMATED APPROACH TO NON-NEGATIVE SPECIMEN LIST (NNSL) PRODUCTION<br />
AND APPLICATION FOR SAMHSA-CERTIFIED LABORATORIES.<br />
William N. Bennett and Anthony Wu* - ACL Laboratories, West Allis, WI.<br />
SAMHSA-certified laboratories are required to produce a Non-Negative Specimen List (NNSL) for the<br />
National Laboratory Certification Program (NLCP) on a semi-annual basis. This list must be submitted to<br />
the NLCP staff Research Triangle Institute (RTI) on a specifically formatted Excel spreadsheet. From the<br />
list, NLCP staff select those specimens whose documentation are to be reviewed by inspectors at the next<br />
scheduled on-site inspection. For ease <strong>of</strong> review, as mandated by the inspection guidelines, these<br />
documents must be organized in a manner that reflects the selected NNSL. To decrease the time needed to<br />
compile this information, we have designed an approach to automate this organization process. Our<br />
application <strong>of</strong> this approach uses SQL and Turbo Pascal computer languages and the spreadsheet Excel,<br />
with Commercial Lab as the Laboratory Information Management System (LIMS). First, SQL queries are<br />
run which produce text files from resident databases on the LIMS. Second, the text files are moved to a PC<br />
and imported into pre-formatted Excel worksheets, which are then forwarded to RTI. Third, the files are<br />
refined using a Turbo Pascal program and imported into Excel calendar worksheets. Calendar entries<br />
include: Access number, Batch number, CCF number and the Non-negative test for which the sample was<br />
targeted. The listings on the calendar (placed on boxes containing the sample documentation), in<br />
conjunction with the selected NNSL, organize the specimen documentation for easy retrieval and review<br />
by the inspectors. Inspectors to our laboratory have praised this organizational scheme. As pre-inspection<br />
guidelines become increasingly time consuming, this approach may be useful for other SAMSHA-certified<br />
laboratories.<br />
Keywords: NNSL, SAMHSA, Non-negative<br />
Page 267
F15 <br />
METHOD VALIDATION FOR THE ANALYSIS OF AMPHETAMINE, METHAMPHETAMINE,<br />
MDAAND MDMA IN URINE<br />
Mee-lung Park, Sang-Kit Choi, Eun-Mi Kim, Mi-Ae Lim*, Myungyoon PyOI), Hee-Sun Chung<br />
Division <strong>of</strong>Narcotic Analysis, National Institute <strong>of</strong> Scientific Investigation, Seoul, Korea<br />
I)The school <strong>of</strong> Pharmacy, Sookmyung Women's University, Seoul, Korea<br />
The purpose <strong>of</strong> this study is to provide the standard method for the. assay <strong>of</strong> stimulants in urine, especially<br />
ATS (amphetamine type stimulants; amphetamine (AM), methamphetamine (MA),<br />
methylenedioxyamphetamine (MDA) and methylenedioxymethamphetamine (MDMA». We performed<br />
method validation for these drugs in urine according to EURACHEM Guide (A laboratory guide to method<br />
validation).<br />
Analytical method for AM, MA, MDA and MDMA in urine was as follows. For the analysis <strong>of</strong><br />
amphetamines in urine. immunoassay (fluorescence polarization immunoassay, TDxFLx) was used for<br />
screening test and confirmation test was performed with GC/MS. After the analysis by immunoassay, the<br />
positive specimens were alkalized with 6 M-NaOH and the analytes were extracted with ethyl acetate. After<br />
centrifugation <strong>of</strong> specimens, the supernatants were evaporated to dryness under the nitrogen stream at 450<br />
with vacuum. The residues were derivatized with pentafluoropropionic anhydride (PFPA). They were<br />
analyzed by gas chromatography/mass spectrometry (GC/MS). Ds-deuterated amphetamines were used as<br />
internal standards. To validate this method, selectivity, linearity <strong>of</strong> calibration, within- and between-run<br />
reproducibility (precision), accuracy, limit <strong>of</strong>detection and quantification were studied.<br />
As a result, the calibration curves were ranged from 100 to 8,000 ng/ml with the correlation coefficients <strong>of</strong><br />
greater than 0.9. Within- and between-run precisions were measured in three different concentrations (250<br />
ng/ml, 500 ng/ml, 1,000 ng/ml). Coefficients <strong>of</strong>variance (CV %) <strong>of</strong> their precisions were under 10 % at all<br />
concentrations. Those accuracies (% bias) were also under 10 %. The limit <strong>of</strong>detection (LOD) and limit <strong>of</strong><br />
quantification (LOQ) for all analytes studied were 20 ng and 100 ng, respectively. The selectivity <strong>of</strong><br />
amphetamines in urine was observed by spiking high concentrations <strong>of</strong> those, which have similar chemical<br />
structures such as ephedrine, pseudoephedrine and norephedrine into low QC urine samples (500 ng).<br />
Those chemicals did not show any inferences in the analysis <strong>of</strong>ATS in urine by this method.<br />
It was concluded that validation data by Eurachem guide was proved to be adequate for the analysis <strong>of</strong><br />
amphetamine, methamphetamine, MDA and MDMA in urine Samples ..<br />
Keywords; method validation, ATS (amphetamine type stimulants), urinalysis<br />
Page 268
F16 <br />
URINARY EXCRETION OF MORPHINE AND CODEINE FOLLOWING THE<br />
ADMINISTRA TION OF SINGLE- AND MULTIPLE-DOSE OF BROWN MIXTURE<br />
Dong-Liang Lin,I,2, Hsiu-Chuan LiU*,1,2, Hsiu-O H02, Chung-Yi Wang l and Ray H, Liu 1 ,3,4, IInstitute <strong>of</strong><br />
<strong>Forensic</strong> Medicine, Ministry <strong>of</strong>Justice, Taipei, Taiwan. 2Taipei Medical University, Taipei, Taiwan. 3Fooyin<br />
University, Kaohsiung Hsien, Taiwan. 4Graduate Program in <strong>Forensic</strong> Science, University <strong>of</strong> Alabama at<br />
Birmingham, Birmingham, Alabama<br />
Parallel to the "poppy-seed defense" strategy commonly reported in the United States, donors <strong>of</strong> urine<br />
samples tested positive for opiates in Taiwan <strong>of</strong>ten claimed the consumption <strong>of</strong> Brown Mixture (BM) as the<br />
source <strong>of</strong> the observed morphine and codeine. Since BM contains opium powder (10-10.5% morphine),<br />
opium tincture (0.9-1.1% morphine), or camphorated opium tincture (0,045-0.055% morphine) and is a<br />
popular remedy, while heroin use is considered a serious criminal act, the claim <strong>of</strong> BM use has to be<br />
adequately addressed.<br />
In this study, BM from 7 different manufacturers (5 tablets and 2 solutions) and urine samples from patient<br />
and alleged heroin users were analyzed for their morphine and codeine contents. The analytical procedure<br />
included hydrolysis, trimethylsilylation, and monitoring <strong>of</strong> the following ions designated for<br />
TMS-derivatized codeine, morphine, and nalorphine (internal standard): mh 371,356,343; 429, 414, 401;<br />
455,440,414, respectively. The first ion listed for each compound was used for quantitation using a six-point<br />
calibration protoco I (50-2000 ng/mL).<br />
The contents <strong>of</strong> morphine and codeine and their ratios ([M]/[C]) in: (a) BM tablets (n =5), and BM solution<br />
(n = 2) available in Taiwan and (b) urine specimens collected from alleged heroin users and patients (n 7)<br />
ingesting 1-6 tablets (or 5-20 mL solution) -- one-time single dose or three times per day for two days -- are<br />
summarized in Table I. The contents <strong>of</strong> morphine and codeine in the tablets are very consistent, but vary<br />
considerably in the 2 BM solution. Morphine concentrations found in urine specimens collected from<br />
patients ingesting BM tablets or solution, are always 5.0) for patients ingesting BM<br />
tablets and alleged heroin users. It appears that (a) BM ingestion (tablet or solution) is unlikely to result in<br />
morphine concentration >4000 ng/mL; and (b) [M]/[C] ratio may not be an effective parameter for the<br />
differentiation <strong>of</strong>BM tablet ingestion and heroin use.<br />
Table 1. Morphine and codeine contents in Brown Mixture tablet, Brown Mixture solution, and urine<br />
specimens collected from alleged heroin users and patients ingesting Brown Mixture<br />
Brown Mixture<br />
Urine specimen o collected users <strong>of</strong><br />
[M]/[C] Tablet Solution Tablet Solution Heroin h<br />
N 25 10 56 68 90<br />
Range 8.46-9.18 2.56-2.93 4.88-14.8 1.31-9.09 3.15-40.8<br />
Mean 8.77 2.74 7.76 2.62 8.52<br />
Std dev. 0.19 0.15 1.92 0.87 4.03<br />
°Only specimens with morphine concentration higher than 300 nglmL are included.<br />
b Alleged heroin users.<br />
Key words: Brown mixture, morphine, codeine<br />
Page 269
F17 <br />
A MODIFIED METHOD FOR THE LIQUID-LIQUID EXTRACTION AND GCIMS ANALYSIS<br />
OF METHADONE FROM HUMAN URINE IN A CAP-FUDT CERTIFIED DRUG TESTING<br />
LABORATORY<br />
Jeffrey Lavelle, Brian Brunelli, Edward A'Zary*, and Judy Keller. Quest Diagnostics Incorporated,<br />
3175 Presidential Drive, Atlanta, Georgia 30340<br />
In order to produce forensically accurate and reproducible results in a competitive, cost-effective, and time<br />
conserving manner, we took an existing method (1,2) for the extraction <strong>of</strong> methadone from urine and made<br />
several significant modifications. The internal standard was changed from phenyltoloxamine to methadoned9.<br />
The extraction method was changed from a solid phaselback extraction to a liquid/liquid extraction.<br />
Four organic solvents were tested: <br />
Solvent A comprised <strong>of</strong>(35:15:40: 1 0) toluene:ethyl acetate:hexane:methanol. <br />
Solvent B comprised <strong>of</strong>(25:25:50) toluene:ethyl acetate:hexane. <br />
Solvent C comprised <strong>of</strong>(10:90) toluene:hexane. <br />
Solvent D comprised <strong>of</strong> (5:95) isoamyl alcohol:hexane. <br />
All solvents were evaluated in a liquid-liquid extraction procedure for quantitation ion areas 72 m/z and}8<br />
mlz with calibrators spiked at 80 nglmL,. 200 ng/mL, and 2000 nglmL. Area recovery studies showed tnat<br />
solvent B was the most desirable <strong>of</strong> the four extraction solvents. Solvent A was eliminated because it had<br />
the second lowest correlation coefficient (r2 ==0.999985), and because it contained methanol, which could<br />
cause emulsions to form. Solvent C was eliminated because it had the lowest recovery <strong>of</strong> internal standard<br />
and the largest variation in internal standard recovery. Finally, solvent D was eliminated because it had the<br />
lowest correlation coefficient (r=0.999929) and the second largest variation in internal standard recovery.<br />
Linearity studies with our previous extraction method produced an LOD (Limit <strong>of</strong> Detection) <strong>of</strong> 50ng/mL,<br />
LOQ (Limit <strong>of</strong> Quantitation) <strong>of</strong> lOOng/mL and an ULOL (Upper Limit <strong>of</strong> Linearity) <strong>of</strong>2,OOOnglmL. The<br />
new extraction method allowed this laboratory to expand our ULOL from 2,000ng/mL to 10,OOOnglmL<br />
allowing for an accurate quantitation <strong>of</strong> high concentrated samples on a first time run without prior dilution.<br />
This method modification reduced the rescheduled rate from 27% to 9%.<br />
1. Clean Screen Basic Drug Procedure, Worldwide Monitoring<br />
2. Taylor, RS,Greutink, C. and Jain, NC "Identification <strong>of</strong> Underivatized Basic Drugs in Urine by Capillary<br />
Column Gas Chromatography". Journal <strong>of</strong>Analytical Toxicology, 10:205-208 (1986).<br />
Keywords: Methadone, LiquidILiquid, GCIMS<br />
Page 270
FI8 <br />
A RAPID LCIMS METHOD FOR THE DETERMINATION OF<br />
METHAMPHETAMINEIDIMETHYLAMPHETAMINE AND THEIR METABOLITES IN URINE <br />
A STUDY OFTHE CURRENT SITUATION IN HONG KONG<br />
WC Cheng*, Vincent KK MOK, <strong>Forensic</strong> Science Division, Government Laboratory, Homantin<br />
Government Offices, Hong Kong Special Administrative Region, People's Republic <strong>of</strong> China<br />
Methamphetamine (MA) abuse, both in high purity "Ice" form or in tablets, continues to be one the popular<br />
drugs <strong>of</strong> abuse found in Hong Kong. Recently, some <strong>of</strong> drug seizures in crystalline or tablets received by our<br />
laboratory were found to contain N,N-dimethylamphetamine (DMA), a MA analog. The crystalline samples<br />
with DMA found were either in its pure form or mixed with MA. For tablets containing DMA, they were<br />
physically similar to those Ecstasy tablets, and the compositions were complex and usually mixed with MA,<br />
MDMA, ketamine and/or other drugs. As it is difficult to distinguish physically between DMA and MA,<br />
DMA can be mistakenly sold as MA.<br />
lt has been reported that DMA, N,N-dimethylamphetamine N-oxide (DMANO), MA, and amphetamine (A)<br />
were excreted in human urine after administration <strong>of</strong> DMA. As DMANO, one <strong>of</strong> the main and specific<br />
metabolite <strong>of</strong>DMA, is thermally labile; the use <strong>of</strong> LCIMS would allow the simultaneous detection <strong>of</strong>all four<br />
analytes without derivatization possible. In order to have a clear picture <strong>of</strong> the current state <strong>of</strong> MAIDMA<br />
abuse in Hong Kong, a rapid and sensitive LCIMS method has been successfully developed for the<br />
urinalysis <strong>of</strong> suspected drug abusers under the drug use surveillance program. LC/MS analysis was<br />
performed on a Finnigan Surveyor LC connected to a Finnigan LCQ Advantage ion trap mass spectrometer.<br />
Using solid phase extraction <strong>of</strong> urine with Alltech CI8 columns followed by LCIMS analysis fitted with an<br />
Alltech Rocket Platinum EPS C-18 column and using a mobile phase (O.OIM ammonium formate (pH=3):<br />
acetonitrile =77:23) at a flow rate <strong>of</strong> 0.2 ml/min, the simultaneous identification and quantitation <strong>of</strong> MA,<br />
DMA and their metabolites could be achieved within 5 min. Based on the urinalysis results, an overview <strong>of</strong><br />
current MAIDMA abuse will be described.<br />
Keywords: N,N-dimethylamphetamine, LCIMS, urinalysis<br />
Page 271
F19 <br />
CONFIRMATION RATES OF INITIAL DRUG ASSAYS IN A GROUP OF HHS-CERTIFIED<br />
LABORATORIES, JANUARY 01 THROUGH DECEMBER 31, 2003<br />
I: FEDERALLY REGULATED SPECIMENS<br />
Donna M. Bush '*, Michael R. Baylor 2, John Irving2, John M. Mitchelf, Craig A. Sutheime~: lDivision <strong>of</strong><br />
Workplace Programs, CSAP, SAMHSA, Rockville, MD, USA; 2RTI International, Research Triangle Park,<br />
NC, USA<br />
As the U.S. Department <strong>of</strong>Health and Human Services (HHS) moved to expand the analytical methods, the<br />
approaches to drug detection, and the biological matrices allowed as specimens in the workplace drug<br />
testing program for Federal employees, an in-depth analysis <strong>of</strong>current practices was initiated. Of particular<br />
interest was the specificity and cross-reactivity <strong>of</strong> the immunoassays currently found in HHS-certified<br />
laboratories. The specificity <strong>of</strong> the immunoassays associated with urine drug testing has long been a<br />
subject <strong>of</strong> discussion among forensic toxicologists. While it has been known that some drug class<br />
immunoassays have very high rates for the confirmation <strong>of</strong> presumptive positives, it is also recognized that<br />
other drug class immunoassays produce a significant number <strong>of</strong> presumptive positives that fail to confirm<br />
when subjected to confirmatory testing by GCIMS. These observations led to an examination <strong>of</strong> the<br />
immunoassays currently in use with the goal <strong>of</strong> documenting the possible differences in specificities and<br />
cross-reactivities <strong>of</strong> the technologies .<br />
. The study included data from 11 HHS-certified laboratories encompassing nearly 4 million specimens<br />
tested under Federal mandate during 2003. These specimens represented between 55 to 60% <strong>of</strong>all federally<br />
regulated specimens tested in accordance with the Mandatory Guidelines for Federal Workplace Drug<br />
Testing Programs (59 Fed. Reg. 29908-29931, June 9, 1994 and 63 Fed. Reg. 63483-63484, November 13,<br />
1998) during 2003. The data were obtained from laboratories that used CEDIA, EIA and KIMS<br />
technologies as a primary initial test. Some laboratories conducted additional screening <strong>of</strong> presumptive<br />
positives with FPIA as a second initial test. Summaries <strong>of</strong> specimen testing and confirmation rates are<br />
presented in the tables below. The confirmation rates are expressed as percent <strong>of</strong>the presumptive positives<br />
confirmed by GCIMS for each drug class. The mean, lowest and highest laboratory confirmation rate for<br />
each drug class are also provided.<br />
I Amphetamines BZE Opiates PCP THC-COOH<br />
I Specimens Tested 3,939,614 3,946,445 3,937,611 3,937,611 3,946,445<br />
i Presumptive Positives 21,577 23,570 21,586 1,772 54,578<br />
I Confirmed Positives 11,715 22,920 6,550 1,229 48,458<br />
IInitial Test Assay<br />
• Confirmation Rates<br />
Amphetamines<br />
{lstl2 nd Test)<br />
BZE Opiates PCP THC-COOH.<br />
: Mean Rate 51.9%/82.8% 98.1% 30.2% 69.7% 91.0%<br />
I Lowest Rate 37.40/0/81.3% 91.1% 17.3% 51.6% 73.0%<br />
I Highest Rate 77.8%/84.3% 99.9% 55.9% 91.0% 98.8%<br />
This study evaluated the presumptive positive rates and the confirmation rates for primary initial tests by<br />
immunoassay method as well as paired immunoassay methods (primary initial test plus second initial test).<br />
The results were examined with consideration <strong>of</strong> assay cross-reactivity and specificity. As expected, some<br />
assays and technologies appear to better identify specimens containing analytes <strong>of</strong> interest at or above the<br />
administrative cut<strong>of</strong>fs required by the Mandatory Guidelines for Federal Workplace Drug Testing<br />
Programs. While the study assesses current capabilities <strong>of</strong>existing technologies from a large population <strong>of</strong><br />
"real" federally regulated workplace specimens, it also provides information that may be useful in<br />
formulating future guidelines by which newer technologies and approaches may be evaluated.<br />
Keywords: HHS-certified laboratories, Immunoassay confirmation rates, calendar year 2003<br />
Page 272
F20 <br />
CONFIRMATION RATES OF INITIAL DRUG ASSAYS IN A GROUP OF HHS-CERTIFIED<br />
LABORATORIES, JANUARY 01 THROUGH DECEMBER 31, 2003<br />
II: NON-REGULATED SPECIMENS<br />
Craig A. Sutheimer l *, Michael R. Baylor I, John Irvingl, John M. Mitchell\ Donna M. Bush 2 : IRTI<br />
International, Research Triangle Park, NC, USA; 2DWP, SAMHSA, Rockville, MD, USA<br />
The specificity <strong>of</strong> immunoassays associated with urine drug testing has long been a subject <strong>of</strong> discussion among<br />
forensic toxicologists. While it has been known that some drug class immunoassays have very high rates for the<br />
confirmation <strong>of</strong> presumptive positives, it is also recognized that other drug class immunoassays produce a<br />
significant number <strong>of</strong> presumptive positives that fail to confirm when subjected to confirmatory testing by<br />
GCJMS. These observations are further confounded as initial and confirmatory drug test cut<strong>of</strong>f concentrations<br />
change and as the number <strong>of</strong> drug analytes in confirmatory panels are broadened. These observations led to an<br />
examination <strong>of</strong> the immunoassays currently in use at drug testing laboratories. The goal <strong>of</strong> this study was to<br />
document the possible differences in specificities and cross-reactivities <strong>of</strong> the technologies with multiple cut<strong>of</strong>fs<br />
in both the initial and confirmation testing procedures in addition to possible variability in the analytes defined in<br />
the confirmatory panels.<br />
The study included data from 10 laboratories certified by the U. S. Department <strong>of</strong> Health and Human Services<br />
(HHS) encompassing over 10 million specimens tested during 2003. These specimens were not subject to the<br />
criteria <strong>of</strong> the Mandatory Guidelines for Federal Workplace Drug Testing Programs. The data was obtained from<br />
laboratories that used CEDI A, EIA and KIMS technologies as a primary initial test, with varying initial and<br />
confirmatory test cut<strong>of</strong>fs. Some laboratories conducted additional screening <strong>of</strong> presumptive positives with a<br />
second initial test. Summaries <strong>of</strong> specimen testing and confirmation rates are presented in the tables below. The<br />
confirmation rates are expressed as percent <strong>of</strong> the presumptive positives confirmed by GC/MS for each drug<br />
class. The lowest and highest confirmation rate for each "initial/confirmatory testing cut<strong>of</strong>f pair" identified is<br />
provided.<br />
Amohetamines BZE<br />
Specimens Tested 10 142,363 10,136424<br />
Presumptive Positives 101,653 97,891<br />
Confirmed Positives I 57,283<br />
96,283<br />
Opiates PCP<br />
10,117,626 10 006,492<br />
103,081 5,838<br />
36,821 3,389<br />
I<br />
THC-COOH<br />
10,188,976 i<br />
347,905 I<br />
326,039 1<br />
T Barbs I Benzos Methadone MQL Propoxyphene<br />
. Specimens Tested T 4,585,890 I 4,271,398 3,943430 2,504,097 3,852,794<br />
Presumptive Positives I 15,281 47,639 10,305 56 28,188<br />
Confirmed Positives T 13,729 L 28,260 9,248 4 26,045<br />
I Initial Test Assay<br />
: Confirmation Rates<br />
Amphetamines BZE Opiates PCP I THC-COOH<br />
i Lowest Rate 3.4% 80.5% 25.0% 59.0% I 60.8%<br />
I Highest Rate 97.2% 99.3% 71.8% 96.4% l 100.0%<br />
I<br />
Initial Test Assay Barbs Benzos Methadone MQL ! Propoxyphene<br />
I Confirmation Rates<br />
-<br />
i Lowest Rate 76.1% 45.9% 69.8% NA 22.7%<br />
I<br />
I Highest Rate i 100.0% 83.7% 100.0% 8.3% 100.0~<br />
This study evaluated the presumptive positive rates and the confirmation rates for primary initial tests by<br />
immunoassay method. The results w~re examined with consideration <strong>of</strong> assay cross-reactivity and specificity.<br />
As expected, some assays and technologies appear to better identifY specimens containing analytes <strong>of</strong> interest<br />
above the defined cut<strong>of</strong>fs. While the study assesses current capabilities <strong>of</strong> existing technologies from a large<br />
population <strong>of</strong> "real" specimens, it also provides information that may be useful in formulating future guidelines<br />
by which newer technologies, additional drug classes and additional analytes may be evaluated.<br />
Keywords: non-Regulated testing, HHS-certified laboratories, Immunoassay confirmation rates, Calendar Year<br />
2003<br />
Page 273
F21 <br />
DETERMINA TION OF BENZODIAZEPINES IN HUMAN URINE USING SOLID-PHASE<br />
EXTRACTION AND HIGH PERFORMANCE LIQUID CHROMATOGRAPHY<br />
ELECTROSPRA Y IONISATION TANDEM MASS SPECTROMETRY<br />
S Hegstad*, E L 0iestad, U Johansen and A S Christophersen<br />
Division <strong>of</strong> <strong>Forensic</strong> Toxicology and Drug abuse, Norwegian Institute <strong>of</strong> Public Health, P.O. Box 4404<br />
Nydalen, NO-0403 Oslo.<br />
Aims: A liquid chromatography-tandem mass spectrometry (LCIMSIMS) method has been developed and<br />
validated for the determination <strong>of</strong> benzodiazepines registered in Norway and/or their metabolites in human<br />
urine. These compounds are frequently associated with misuse. The following compounds are included: 7<br />
aminonitrazepam, 7-aminoc)onazepam, 7-amin<strong>of</strong>lunitrazepam, alprazol am, alphahydroxyalprazolam,<br />
oxazepam, 3-0H-diazepam and N-desmethyldiazepam. The method was evaluated by analysing urine<br />
specimens from prison inmates, suspected <strong>of</strong> drug abuse.<br />
Methods: Urine samples (0.5 ml) were hydrolysed with l3-glucuronidase (from Patella vulgata) at 60°C for<br />
2 hours before solid-phase extraction with a polymer-based mixed-mode column (Oasis MCX).<br />
Chromatographic separation <strong>of</strong> extracts was achieved using a Waters Symmetry CI8 (2.IXlOO mm, 3.5<br />
/-1m) column with a flow rate at 0.3 mllmin with gradient elution. The analyses were performed on a Waters<br />
Alliance 2695 system in combination with a Waters Quattro Ultima Pt tandem-quadropole mass<br />
spectrometer equipped with a Z-spray electrospray interface. Positive ionization was performed in the<br />
MRM (multiple reaction monitoring) mode. Two transitions were monitored for the analytes, and one for<br />
the internal standards. Deuterated analogues were used as internal standard for all analytes except for 7<br />
aminonitrazepam and alphahydroxyalprazolam, which were quantified using 7-aminoclonazepam-d4 and<br />
alprazolam-d5, respectively.<br />
Results: The concentration range was 0.1-8.0 /-1M for 7-aminonitrazepam, 7-aminoclonazepam, 7<br />
amin<strong>of</strong>lunitrazepam, alprazolam, alphahydroxyalprazolam and 0.5-40 /-1M for the other compounds. The<br />
average recovery <strong>of</strong> the analytes ranged from 56-83 %. The between-day relative standard derivation <strong>of</strong> the<br />
method ranged from 3 -12 %. The limits <strong>of</strong>quantification were found to be between 0.002 and 0.01 /-1M.<br />
Conclusion: The LC/MSIMS method proved to be robust and specific for the determination <strong>of</strong><br />
benzodiazepines in urine. The method developed <strong>of</strong>fers significant efficiency advantages in our routine<br />
laboratory replacing two chromatographic methods, which involved time-consuming derivatisation<br />
techniques. (HPLC-fluorescence, GC-MS). In addition, inclusion <strong>of</strong> new benzodiazepines is more<br />
convenient due to high specificity and flexibility <strong>of</strong>the new method.<br />
Keywords: Benzodiazepines, urine, LC/MS/MS<br />
Page 274
F22 <br />
USE OF COMPOUNDS ALTERING VIGILANCE PERFORMANCE: PRELIMINARY RESULTS<br />
OF PREVALENCE IN HAULAGE DRIVERS IN THE NORD-PAS-DE-CALAIS REGION<br />
(FRANCE)<br />
L. Labatl, B. Dehon\ M. Lhermitte l ' and regional group <strong>of</strong> «Toxicomanie et Travail »2<br />
I Laboratoire de Biochimie et Biologie Moleculaire - H6pital Calmette - Avenue du Pr Leclercq - 59037<br />
Lille cedex - France; 2 Institut de Sante au Travail du Nord de la France A venue Oscar Lambret - 59037<br />
Lille cedex - France.<br />
Introduction: In 1995, a French study showed that the number <strong>of</strong> users <strong>of</strong> compounds that could alter<br />
vigilance performance was significantly more important in a population <strong>of</strong> workers in security posts than in<br />
the general working population (1). Moreover, even if the number <strong>of</strong> road accidents involving haulage<br />
drivers has decreased since 1985, their severity is greater. A multicentric study was initiated by a local<br />
group «Toxicomanie et Travail }) on haulage drivers from different cities in the Nord-Pas-de-Calais region<br />
(France). The objectives <strong>of</strong> this study are the standardisation <strong>of</strong> occupational medicine practices in order to<br />
define a harmonized policy for prevention and screening, to validate analytical screening methods, as well<br />
as the course <strong>of</strong> action in the case <strong>of</strong> positive detection.<br />
Methods: 1000 haulage drivers were included in the study. Occupation was the only criterion <strong>of</strong> selection.<br />
Urine samples were collected anonymously. Information collected included: haulage area, age, gender,<br />
nature <strong>of</strong> appointment with occupational practitioners and day <strong>of</strong> the sampling. A urine screen (test<br />
TriageS, BMD) was performed for methadone (cut <strong>of</strong>f 300 ng/mL), benzodiazepines (300 ng/mL),<br />
cocaine (300 ng/mL), amphetamine derivatives (1000 ng/mL), opioides (300 ng/mL) and cannabis (50<br />
ng/mL). Buprenorphine detection was achieved with Elisa method (Microgenics). All positive results were<br />
confirmed by GC-MS or HPLC-MS. Alcohol levels were determined by an enzymatic method (Dade<br />
Behring).<br />
Results: Up to February <strong>2004</strong>, 707 samples were collected. 99% are men and participants were on average<br />
36.4 +/- 9.9 years old. Results expressed as percentage <strong>of</strong> positives were: opioides (4.SI%), cannabis<br />
(9.05%), cocaine (0.14%), amphetamine derivatives (0%), buprenorphine (1.98%), methadone (0.56%),<br />
benzodiazepines (0.42%), alcohol (5.51%). The 34 positive cases for opioides were distributed as follows:<br />
6-MAM 0; morphine 10; codeine 11 ; pholcodine 20. THC-COOH was the only compound identified in<br />
urine samples from individuals tested positive for cannabis.<br />
Conclusion: Only legal opioid drugs were identified. They correspond to antitussive medications that are<br />
broadly prescribed during the winter period (time <strong>of</strong> the urine collection). The lack <strong>of</strong> sensitivity and<br />
specificity <strong>of</strong> the immunologic test could explain the low percentage observed for benzodiazepine positive<br />
cases. Our results are in good agreement with the results <strong>of</strong>the previously mentioned study <strong>of</strong> Haguenoer et<br />
aI., (1995) in the North <strong>of</strong> France, for the use <strong>of</strong> cannabis and alcohol by workers in security posts. In<br />
contrast, the number <strong>of</strong> positive cases for amphetamine derivatives, opioides and benzodiazepines was less.<br />
Other molecules were not investigated in the previous study <strong>of</strong> Haguenoer et at.. Considering these<br />
preliminary results, it would be <strong>of</strong> great interest to extend the screening to other psychoactive molecules by<br />
using a more efficient screening method such as HPLC-DAD.<br />
References: 1. Haguenoer lM. et coil. Prevalence des conduites toxicophiIes en milieu pr<strong>of</strong>essionnel : une<br />
etude dans la region du Nord Pas de Calais. Bulletin du Conseil departemental du Nord, Ordre des<br />
Medecins, 1997; SO : 11-15.<br />
Keywords: vigilance, haulage drivers, illicit substances<br />
Page 275
F22 <br />
USE OF COMPOUNDS ALTERING VIGILANCE PERFORMANCE: PRELIMINARY RESULTS<br />
OF PREVALENCE IN HAULAGE DRIVERS IN THE NORD-PAS-DE-CALAIS REGION<br />
(FRANCE)<br />
L. Labat l , B. Dehon l , M. Lhermitte l • and regional group <strong>of</strong> ({ Toxicomanie et Travail »2<br />
1 Laboratoire de Biochimie et Biologie Moleculaire - Hopital Calmette - Avenue du Pr Leclercq - 59037<br />
Lille cedex - France; 2 Institut de Sante au Travail du Nord de la France A venue Oscar Lambret - 59037<br />
Lille cedex - France.<br />
Introduction: In 1995, a French study showed that the number <strong>of</strong> users <strong>of</strong> compounds that could alter<br />
vigilance performance was significantly more important in a population <strong>of</strong> workers in security posts than in<br />
the general working population (1). Moreover, even if the number <strong>of</strong> road accidents involving haulage<br />
drivers has decreased since 1985, their severity is greater. A multicentric study was initiated by a local<br />
group « Toxicomanie et Travail» on haulage drivers from different cities in the Nord-Pas-de-Calais region<br />
(France). The objectives <strong>of</strong> this study are the standardisation <strong>of</strong> occupational medicine practices in order to<br />
define a harmonized policy for prevention and screening, to validate analytical screening methods, as well<br />
as the course <strong>of</strong> action in the case <strong>of</strong> positive detection.<br />
Methods: 1000 haulage drivers were included in the study. Occupation was the only criterion <strong>of</strong> selection.<br />
Urine samples were collected anonymously. Information collected included: haulage area, age, gender,<br />
nature <strong>of</strong> appointment with occupational practitioners and day <strong>of</strong> the sampling. A urine screen (test<br />
Triage8, BMD) was performed for methadone (cut <strong>of</strong>f = 300 nglmL), benzodiazepines (300 nglmL),<br />
cocaine (300 ng/mL), amphetamine derivatives (1000 ng/mL), opioides (300 ng/mL) and cannabis (50<br />
ng/mL). Buprenorphine detection was achieved with Elisa method (Microgenics). All positive results were<br />
confirmed by GC-MS or HPLC-MS. Alcohol levels were determined by an enzymatic method (Dade<br />
Behring).<br />
Results: Up to February <strong>2004</strong>, 707 samples were collected. 99% are men and participants were on average<br />
36.4 +/- 9.9 years old. Results expressed as percentage <strong>of</strong> positives were: opioides (4.81%), cannabis<br />
(9.05%), cocaine (0.14%), amphetamine derivatives (0%), buprenorphine (1.98%), methadone (0.56%),<br />
benzodiazepines (0,42%), alcohol (5.51 %). The 34 positive cases for opioides were distributed as follows:<br />
6-MAM 0 ; morphine 10 ; codeine II ; pholcodine 20. THC-COOH was the only compound identified in<br />
urine samples from individuals tested positive for cannabis.<br />
Conclusion: Only legal opioid drugs were identified. They correspond to antitussive medications that are<br />
broadly prescribed during the winter period (time <strong>of</strong> the urine collection). The lack <strong>of</strong> sensitivity and<br />
specificity <strong>of</strong> the immunologic test could explain the low percentage observed for benzodiazepine positive<br />
cases. Our results are in good agreement with the results <strong>of</strong>the previously mentioned study <strong>of</strong> Haguenoer et<br />
a!., (1995) in the North <strong>of</strong> France, for the use <strong>of</strong> cannabis and alcohol by workers in security posts. In<br />
contrast, the number <strong>of</strong> positive cases for amphetamine derivatives, opioides and benzodiazepines was less.<br />
Other molecules were not investigated in the previous study <strong>of</strong> Haguenoer et al.. Considering these<br />
preliminary results, it would be <strong>of</strong> great interest to extend the screening to other psychoactive molecules by<br />
using a more efficient screening method such as HPLC-DAD.<br />
References: ·1. Haguenoer 1.M. et colI. Prevalence des conduites toxicophiles en milieu pr<strong>of</strong>essionnel : une<br />
etude dans la region du Nord Pas de Calais. Bulletin du Conseil departemental du Nord, Ordre des<br />
Medecins, 1997; 80: 11-15.<br />
Keywords: vigilance, haulage drivers, illicit substances<br />
Page 276
F23 <br />
SCREENING OF BUPRENORPHINE IN URINE OF SUSPECTED ABUSERS BY ELISA<br />
Asimah Hamzah*, P.C. Peh, C.M. Lim, C.P.Lui, PhD, Narcotics II Laboratory, Centre for <strong>Forensic</strong><br />
Science, Health Sciences Authority, 11 Outram Road, Singapore 169078<br />
Introduction: Buprenorphine is a synthetic thebaine derivative that has both analgesic and opioid antagonist<br />
properties. As an analgesic, it is 25 to 40 times more potent than morphine, and has a slower onset <strong>of</strong> pain<br />
relief and longer duration <strong>of</strong> action. Hence it is used for the treatment <strong>of</strong> chronic pain, and in treatment <strong>of</strong><br />
heroin addiction as an alternative to methadone. In human, buprenorphine is metabolised primarily by N<br />
dealkylation to norbuprenorphine. Both the metabolite and the parent drug undergo extensive conjugation<br />
to glucuronides that are excreted in urine. It is known that buprenorphine has been abused by heroin addict;<br />
therefore there is a need for the laboratory to develop a screening method for the suspected abusers.<br />
Aim: The purpose <strong>of</strong> this study is to evaluate the use <strong>of</strong> an Enzyme Linked Immunosorbent Assay (ELISA)<br />
test kit in the screening <strong>of</strong> buprenorphine in urine to detect suspected abusers.<br />
Method: The ELISA test kits were purchased from Neogen Corp. USA. The assay principle is based on the<br />
competitive binding between the free drugs in the urine and the drug enzyme conjugates for antibodies,<br />
which are coated onto the 96-well microplate. After incubating the urine and drug enzyme conjugate in the<br />
wells for 45 min at room temperature, the wells were washed with buffer, and K·blue substrate was added<br />
to each well. After a further 30 min <strong>of</strong> incubation, Red Stop solution was added to each well to stop the<br />
reaction. Multiskan Ascent Microplate Photometer was used to measure the absorbance at wavelength <strong>of</strong><br />
650 nm. The color intensity <strong>of</strong> each well is inversely proportional to the concentration <strong>of</strong> the drug in the<br />
urine. Confirmatory test, using Gas chromatography-mass spectrometry (GC·MS) was also carried out on<br />
all the urine specimens to compare with the screening results.<br />
Results: The linearity <strong>of</strong> the ELISA kit was found to be up to about 5 ng/ml <strong>of</strong> buprenorphine. The<br />
coefficients <strong>of</strong> variation (CVs) <strong>of</strong> the within-day and between-day variations for buprenorphine ranged<br />
from 2.0% to 6.7% and 8.3% to 19.1% respectively. Norbuprenorphine was found to cross react to certain<br />
extend. No cross-reactivity was found with other common drugs <strong>of</strong> abuse such as morphine, codeine,<br />
hydrocodone, hydromorphone, Il-nor-L'1 9 -THC-9-carboxylic acid, cocaine, benzoylecgonine, amphetamine,<br />
methampethamine, N,a-Dimethyl-3,4-(methylenedioxy)phenethylamine (MDMA), a-Methyl-3,4<br />
(methylenedioxy)phenethylamine (MDA), N-Ethyl-a,methyl·3,4-(methylenedioxy)phenethYlamine<br />
(MDEA), ketamine and norketamine. Out <strong>of</strong> the 3 urine specimens that were collected from suspected<br />
abusers, 17 were found to be screened positive, using the cut-<strong>of</strong>f at 1 ng/ml. The linearity range <strong>of</strong><br />
buprenorphine was found to be up to 50 ng/ml. The LOQ was found to be 0.25 nglml. The results from the<br />
confirmatory test are also discussed.<br />
Conclusions: The use <strong>of</strong> ELISA test kit was found to be a simple, rapid, specific and effective method for<br />
the screening <strong>of</strong> buprenorphine in urine. It helps to minimize the cost <strong>of</strong> the GC-MS test in a mass<br />
screening exercise.<br />
Keywords: ELISA, Screening, Buprenorphine<br />
Page 277
F24 <br />
A COMPARISON OF THE MICROGENICS DRI® OPIATE AND MICROGENICS DRI®<br />
OXYCODONE IMMUNOASSA YS WITH GAS CHROMATOGRAPHY IMASS SPECTROMETRY<br />
FOR THE DETECTION OF OPIATES AND OXYCODONE IN URINE<br />
Joseph R. Monforte, Ph.D., DABFT *, Ronald Backer, Ph.D., DABFT and Alphonse PokJis, Ph.D.,<br />
DABFT<br />
Oxycodone is a semi-synthetic opioid prescribed for pain management <strong>of</strong> moderate to severe pain. It is<br />
considered to have a high abuse potential and is prescribed as oxycodone HCl in preparations such as<br />
Oxycontin® (a controlled- release preparation), Percodan® (with aspirin) and Percocet® (with<br />
acetaminophen). Oxymorphone and noroxycodone are metabolites <strong>of</strong> oxycodone. Oxymorphone is a<br />
potent analgesic while noroxycodone is relatively inactive.<br />
Various immunoassays are available for the detection <strong>of</strong> opiates in urine. These assays generally have<br />
lower sensitivities to oxycodone and oxymorphone. Consequently, oxycodone may not be detected<br />
employing available opiate assays, even when taken under abused conditions. The Microgenics DRI®<br />
Oxycodone Assay uses specific antibodies that can detect oxycodone and oxymorphone without significant<br />
cross-reactivity from other opiates. The assay employs either a 100ng/mL or a 300ng/mL cut<strong>of</strong>f.<br />
Seventy specimens received from pain management patients were tested for opiates with the Microgenics<br />
DRI® Opiate and Microgenics DRI® Oxycodone Immunoassays, and gas chromatography/mass<br />
spectrometry. Immunoassay reagents were employed as directed by the manufacturers. The cut<strong>of</strong>f for the<br />
Microgenics DRI® Opiate Assay was 300 ng/mL, and the cut<strong>of</strong>f for the Microgenics DRI® Oxycodone<br />
Assay was<br />
100 ng/mL. The GC/MS SIM procedure employed hydrolysis <strong>of</strong> the specimen, treating the urine with<br />
hydroxylamine, a solid phase column extraction, and formation <strong>of</strong> the BSTF A derivative. The method'<br />
detects oxycodone, oxymorphone, hydrocodone, morphine and codeine. The limit <strong>of</strong> detection and limit <strong>of</strong><br />
quantitation is 20 ng/mL for each opiate.<br />
Of the seventy specimens tested by the Microgenics DRI® Opiate Assay, fifty-three (53) specimens tested<br />
positive and seventeen specimens tested negative. All seventeen negative specimens were confirmed<br />
negative for the opiates included in the GC/MS SIM procedure and all seventeen specimens tested negative<br />
for oxycodone using theMicrogenics DRI® Oxycodone Assay. An opiate was detected by GCIMS in all <strong>of</strong><br />
the specimens testing positive by the Microgenics DRI® Opiate Assay with four exceptions.<br />
Of the seventy specimens tested by the Microgenics DRI® Oxycodone Assay, twenty-four specimens tested<br />
positive for oxycodone. All twenty-four specimens tested positive for oxycodone by GCIMS, and twentytwo<br />
<strong>of</strong> the specimens also contained oxymorphone. One specimen, which did not contain a reportable<br />
oxymorphone concentration, also contained morphine (4,679 ng/mL). One specimen tested one point<br />
below the Microgenics DRI® Oxycodone cut<strong>of</strong>f and contained morphine (18, 522 ng/mL) but no reportable<br />
oxycodone. All forty-six specimens, which tested negative for oxycodone with the Microgenics DR1®<br />
Oxycodone Assay, also tested negative for oxycodone and oxymorphone by GC/MS.<br />
The results obtained with this limited number <strong>of</strong> specimens indicates that the Microgenics DRI®<br />
Oxycodone Assay is highly specific for oxycodone and, consequently, has the potential to be very effective<br />
in discriminating oxycodone from other opiates which may be present in a urine specimen.<br />
Keywords: Oxycodone, Immunoassay, Gas ChromatographylMass Spectrometry<br />
Page 278
F25 <br />
IDENTIFICATION OF CHLORINATED 3,4-METHYLENEDIOXYMETHAMPHETAMINE<br />
IN ILLICIT DRUG ABUSER URINE<br />
4<br />
Vera Maresova 1 ', Jan Hamplt, Zdenek Chundela 2 , Frantisek Zrcek 3 , Miroslav Pohgek , Jiff Chadt' <br />
'Institute <strong>of</strong> <strong>Forensic</strong> Medicine and Toxicology, 1 st Medical Faculty and Hospital, Charles University <strong>of</strong> <br />
Prague; 2 Department <strong>of</strong> Doping Control, General Faculty Hospital, Prague, 3 Institute <strong>of</strong> Criminalistics, <br />
Prague, 4 J. Heyrovsky Institute <strong>of</strong> Physical Chemistry, Prague, Czech Republic <br />
Aim: The aim <strong>of</strong> this study was to identify 3,4-methylenedioxymethamphetamine (MDMA, Ecstasy) and<br />
chlorinated 3,4-methylenedioxymethamphetamine (CI-MDMA) using combined thin layer chromatography<br />
(TLC) and gas chromatography-mass spectrometry (GC-MS). The compound was identified jointly with MDMA<br />
in illicit drug abuser urine. The urine specimen has yielded positive EMIT immunoassay screenings for<br />
cannabinoides, amphetamines and cocaine. GC-MS confirmation <strong>of</strong> amphetamines has revealed the presence <strong>of</strong><br />
amphetamine, methamphetamine, ephedrine, norephedrine, 3,4-methylenedioxymethamphetamine and 3,4<br />
methylenedioxyamphetamine (MDA).<br />
Methods: Thin layer chromatography: In the basic extract a routine analysis <strong>of</strong> urine by TLC for amphetamines<br />
using fractional diethylether liquid/liquid extraction identified ephedrine, the major component MDMA and an<br />
unknown compound. In the TLC system our unknown compound behaved differently than the MDMA. The TLC<br />
plate with silica stationary phase was used (Merck), eluent ethylacetate ethanol ammonia (36:2:2). Gas<br />
chromatography-mass spectrometry: The unknown compound isolated by TLC technique was analysed by<br />
positive chemical ionization (PCI). The base peak mlz 228 (MH+) exhibited a characteristic A+2 isotopic cluster<br />
indicating the presence <strong>of</strong> a monochloro-substituted compound. The molecular ion <strong>of</strong> CI-MDMA was found at<br />
227 mlz. The MS spectrum <strong>of</strong> the unknown compound in electron ionization (EI) exhibited characteristic A+2<br />
chlorine isotopic cluster typical for ion at mlz 169 (mlz 135-1+35) and for molecular ion at mlz 227 (mlz 193<br />
1+35). To confirm CI-MDMA structure, the unknown compound isolated by TLC technique was acetylated,<br />
trifluoroacetylated, silylated, heptafluorobutyrylated and analyzed by GC-MS. The EI-MS spectra <strong>of</strong>MDMA and<br />
CI-MDMA after derivatization exhibited structural similarities. The EI-MS spectrum <strong>of</strong> MDMA contained ions<br />
193, 177, 135, 77, 58 [I]. The EI-MS spectra <strong>of</strong> derivatized CI-MDMA exhibited characteristic A +2 isotopic<br />
cluster for ion at mlz 169 (mlz 135 -I +35) for all used derivatization methods mentioned above. Another<br />
isotopic A + 2 cluster was created in all molecular ions <strong>of</strong> each derivatized chlorinated MDMA: acetylated CI<br />
MDMA had molecular ion at mlz 269 (mlz 227 - I + 43), silylated CI-MDMA had molecular ion at mlz 299 (mlz<br />
227 - I +73), trifluoroacetylated CI-MDMA had molecular ion at mlz 323 (mlz 227 I + 97),<br />
heptafluorobutyrylated CI-MDMA had molecular ion at mlz 423 (mlz 227 - I + 197). Next joint cluster at mlz 196<br />
(162 - I + 35) occurred in acetylated, trifluoroacetylated and heptafluorobutyrylated derivates with the exception<br />
<strong>of</strong> silylated derivates. GC-MS analysis were performed using Hewlett Packard 5890 Gas Chromatograph with<br />
5890 autosampler coupled to a Hewlett Packard 5972 MS detector and Finnigan MAT Magnum. CI-GC-MS<br />
Finnigan MAT Magnum conditions were as follows: ionization gas methanol vapour, ionization energy <strong>of</strong><br />
electrons 70 eV, specific conditions for ion trap CIIMCI parameters: CI maximum ionization time 1500 IlSec, CI<br />
maximum reaction time 100 msec, CI ionizatin storage level 82 dacs, CI reaction storage level 164 dacs, reagent<br />
ion ejection level 85 amu, MCI ionization time 100 Ilsec, reagent ion ejection adjust 100 %, reagent reaction time<br />
54001lsec.<br />
Conclusion: A chlorinated MDMA was identified after derivatization <strong>of</strong> unknown compound isolated by TLC<br />
technique. With using literature source [2] and interpretation our mass spectra <strong>of</strong> heptafluorobutyrylated CI<br />
MDMA we can declare that unknown compound should be 6-CI-MDMA. 6-CI-MDMA is listed in New<br />
synthetic drugs reported in Europe and the USA since the mid-1990s in joint action <strong>of</strong> The European Monitoring<br />
Centre for Drugs and Drug Addiction (EMCDDA)[3].<br />
Acknowledgment: The work has been supported by the project <strong>of</strong>MSMNo. 111100005.<br />
l. H. H. Maurer, A. Weber, K. Pfleger: Mass Spectra and GC data <strong>of</strong> Drugs, Poisons, Pesticides, Pollutants<br />
and their metabolites, 1-4, VCH Verlagsgesellschaft, Weinheim, Germany, 1992<br />
2. R.l Lewis, D. Reed, A. G. Service, A. M. Langford: J. <strong>Forensic</strong>. Sci. 2000; 45(5): 1119-1125<br />
3. L. A. King, A. J. Poortman van der-Meer: Sci. & Just. 2001, 41(3): 200-202<br />
Keywords: chlorinated MDMA, GC-MS analysis<br />
Page 279
F26 <br />
TESTING MEDICAL PROFESSIONALS FOR AN EXPANDED MENU OF DRUGS-<br />
PRELIMINARY SUMMARY OF POSITIVE FINDINGS<br />
Matthew McMullin* and Anthony Costantino. National Medical Services, Willow Grove, PA, USA.<br />
A<br />
Testing medical pr<strong>of</strong>essional for drugs <strong>of</strong> abuse presents a challenge because <strong>of</strong> their access to drugs <strong>of</strong><br />
choice that are not included in the scope <strong>of</strong> most drug testing menus. To assist substance abuse recovery<br />
programs, designed to allow medical pr<strong>of</strong>essionals to continue to practice in their field <strong>of</strong> expertise, we<br />
developed an expanded menu <strong>of</strong> analytes that includes many <strong>of</strong> the known abuse drugs encountered in the<br />
medical pr<strong>of</strong>essional population. The positive results data was summarized in three drug groups: Group I<br />
includes those analytes contained in a SAMHSA regulated test menu; Group 2 includes additional opiates<br />
and amphetamine like compounds not covered in the SAMHSA scope, benzodiazepines, propoxyphene,<br />
barbiturates, and methadone; Group 3 includes (cut-<strong>of</strong>f concentration in nglmL) nor-alfentanil (0.5),<br />
butorphanol (20), nor-fentanyl (0.5), ketamine (100), MDMA (200), nor-meperidine (200), nalbuphine (8),<br />
nor-sufentanil (0.5) and tramadol (500). Group 1 and 2 analytes were screened by EMIT while group 3<br />
analytes are screened by LCIMSIMS. All screens were confirmed by either GCIMS or an alternate<br />
LCIMSIMS procedure. The confirmation menus were extensive with low concentration cut-<strong>of</strong>fs. Ethanol<br />
and ethyl glucuronide were not included in this study.<br />
A total <strong>of</strong> 5,817 samples from medical pr<strong>of</strong>essionals were tested for group I and 2 drugs. The number <strong>of</strong><br />
positive drugs findings for the SAMHSA drugs include in group I was 100, with amphetamine at 56 and<br />
opiates at 34 representing most <strong>of</strong> the positive findings. With the group 2 drugs there were an additional<br />
386 positive drug findings with 193 benzodiazepines findings and the expanded opiates panel (excluding<br />
morphine and codeine) accounting for 134 <strong>of</strong> the positive findings. A total <strong>of</strong> 4,043 samples were tested<br />
for group 3 analytes, and there were 186 positive drug findings. Tramadol, meperidine, and nalbuphine<br />
were the most frequently reported positive findings in the group 3 drugs, accounted for 120, 30 and 14,<br />
respectively.<br />
Drug Groupings<br />
Positive Drug Findings!<br />
Drug Group<br />
Cumulative Positive<br />
Drug Findings<br />
(Group 1) SAMHSA Drugs 100 <strong>of</strong> 5817 samples 100<br />
(Group 2) expanded EMIT panels 386 <strong>of</strong> 5817 samples 486<br />
i<br />
. (Group 3) LCMSMS panel<br />
i<br />
207 <strong>of</strong>4043 samples 693<br />
These preliminary finding support the use <strong>of</strong> expanded testing menus when testing medical pr<strong>of</strong>essionals<br />
who are in drug recovery programs. Caution must be used when interpreting these findings since some<br />
positive findings were listed as prescribed medications.<br />
Keywords: medical pr<strong>of</strong>essional, positive-rate, LCIMSIMS.<br />
Page 280
F27 <br />
LINEAR RELATIONSHIPS OF 6.-9-TETRAHYDROCANNABINOL METABOLITES IN URINE<br />
Scott Larson· and James D. Hutchison, Jr. <br />
Montana State Crime Laboratory, University <strong>of</strong> Montana, Montana, USA <br />
Many studies have focused on the metabolic patterns <strong>of</strong> marijuana and the relationship these compounds<br />
may have to possible time <strong>of</strong> cannabis exposure, based on their concentrations in urine samples. The<br />
objective <strong>of</strong> this study was to investigate the linear relationships <strong>of</strong> a group <strong>of</strong> 6,9-tetrahydrocannabinol<br />
metabolites in random urine samples (n=95). In this study, gas chromatography-mass spectrometry (using<br />
S1M pr<strong>of</strong>iles) was used to monitor and quantify I1-nor-6. 9 -carboxy-9-tetrahydrocannabinol (THCCOOH),<br />
Il-Hydroxy-6. 9 -tetrahydrocannabinol (ll-OH-THC), 6,9-tetrahydrocannabinol (THC), cannabinol (CBN),<br />
and cannabidiol (CBD). Deuterated THCCOOH-d J and 1 I-OH-THC-d J were used as internal controls. The<br />
random urine samples were collected and submitted to the Montana State Crime Lab from adult probation<br />
& parole, Pre-release centers, and Youth Court cases. Since these are random urine samples, there was no<br />
way to definitely determine time <strong>of</strong> marijuana use. The results <strong>of</strong> this study indicate significant linear<br />
relationships between some <strong>of</strong> the metabolites <strong>of</strong> THC, and also the ability to detect CBN and CBD in<br />
random urine samples. The data presented will provide a collection <strong>of</strong>THCCOOH concentrations in urine<br />
with respective comparisons to the other metabolites studied.<br />
Keywords: 6.-9-Tetrahydrocannabinol metabolites, Urine, GCIMS<br />
Page 281
Scientific Session <br />
<strong>Abstracts</strong>: <br />
Alternative <br />
Matrices <br />
Page 283
Ml<br />
COMPARISON STUDY OF SPE AND HS-SPME IN THE DETERMINATION OF METHADONE<br />
AND ITS METABOLITES EDDP AND EMDP IN HUMAN HAIR USING GC-MS<br />
L O'Hanlon l *, J S Oliveri, and K S Scott 2<br />
IPorensic Medicine and Science, University <strong>of</strong> Glasgow, Glasgow, UK<br />
2Department <strong>of</strong><strong>Forensic</strong> Science and Chemistry, Anglia Polytechnic University, Cambridge, UK<br />
The objective <strong>of</strong> this research was to develop and optimize a robust head-space solid phase microextraction for the<br />
extraction <strong>of</strong> methadone and its metabolites from hair and to compare this method to a pre-existing solid phase<br />
extraction method. Methadone (6-dimethylamino-4,4-diphenyl-3-heptanone hydrochloride) is a synthetic opioid<br />
agonist with characteristics similar to those <strong>of</strong> morphine, including actions on the central nervous system and organs<br />
composed <strong>of</strong>smooth muscle. Although structurally it has no resemblance to morphine, its analgesic and spasmolytic<br />
properties have allowed it to be used as a substitute for heroin in opiate addiction programmes.<br />
Aliquots <strong>of</strong> blank hair (IOmg) were spiked with methadone and EDDP at two different concentrations and incubated<br />
in sodium hydroxide solution 1 M (Iml) with anhydrous sodium chloride. This was carried out in 4 ml amber screwtop<br />
vials with a PTPE/siIicone septum. The vial was preheated for 20 min under agitation. The needle probe holding<br />
the IOOJ,lm polydimethylsiloxane (PDMS) fibre was then pushed through the septum and the fibre was immersed in<br />
the specimen for 20 min at a temperature <strong>of</strong> 75°C while agitated. The fibre was then transferred to the GC inlet. The<br />
injection port (operated in splitlsplitless mode) was set to 225°C and the purge time to 3 min. The column<br />
temperature was initially held at 80°C for 2 min, then increased to 280°C at lOOC/min and held for 5 min.<br />
This SPME method was compared to the following SPE method. Aliquots <strong>of</strong> spiked hair (lOmg) were incubated in<br />
methanol for ISh at 37'C. This methanol was then removed and the sample was sonicated with more methanol. The<br />
methanolic fractions were combined and evaporated under nitrogen and reconstituted in distilled water and<br />
phosphate buffer, pH 6. The samples were homogenised and applied to preconditioned Clean Screen columns.<br />
These were selectively washed with various solvent and aqueous mixtures; Methadone and EDDP were extracted<br />
using dichloromethane/isopropanol/concentrated ammonia (78:20:2). These fractions were then evaporated to<br />
dryness under nitrogen and reconstituted in 25 J,ll <strong>of</strong> ethyl acetate. They were then analysed using the same GC-MS<br />
chromatographic conditions. Relative recoveries <strong>of</strong> methadone and EDDP from hair were determined by comparing<br />
the peak heights obtained from spiked hair with unextracted standards and both were determined to be above 5%.<br />
The HS-SPME method proved to be fast and efficient and also has the advantages <strong>of</strong> being solvent free and<br />
producing cleaner extracts.<br />
This paper presents a comprehensive, comparative study <strong>of</strong> both SPE and HS-SPME <strong>of</strong> methadone and EDDP from<br />
human hair and will report on the advantages and disadvantages <strong>of</strong> both methods.<br />
Keywords: Methadone, Solid Phase Extraction, Solid Phase Microextraction<br />
Page 284
M2 <br />
DRUG ANALYSIS IN HAIR: COMPARISON OF CRYOGENIC GRINDING AND CUTTING<br />
FOR SAMPLE PREPARATION.<br />
Yvonne Cruickshank i *, Fiona M. Wylie 2 and Robert A. Anderson 2 .: i<strong>Forensic</strong> Science Unit, University <strong>of</strong><br />
Strathclyde, Glasgow Gl lXW, United Kingdom' ; 2<strong>Forensic</strong> Medicine and Science, University <strong>of</strong><br />
Glasgow, Glasgow G12 8QQ, United Kingdom.<br />
Sample preparation is potentially the most important step in an analytical procedure. The forensic<br />
toxicology laboratory at Glasgow University has established methods for the extraction <strong>of</strong> drugs from<br />
keratinous matrices by cryogenic grinding (nail) and by cutting with scissors (hair) (1,2). To date, only one<br />
report has compared drug extracts obtained from cut and ground hair. Eser et al. found that both the<br />
qualitative and quantitative results from ground hair were better than from cut hair (3). In this report, two<br />
methods <strong>of</strong> sample preparation for the analysis <strong>of</strong> drugs <strong>of</strong> abuse in hair are compared, namely cutting and<br />
cryogenic grinding <strong>of</strong> hair. The drugs analysed were morphine, 6-monoacetylmorphine, codeine,<br />
dihydrocodeine, methadone, EDDP, diazepam, cocaine and ecgonine methyl ester.<br />
Samples <strong>of</strong> hair from 20 drug-related deaths were used for the evaluation. These were collected at autopsy<br />
by plucking from the occipital region <strong>of</strong> the scalp and the root balls were removed prior to analysis. Drugfree<br />
hair was obtained from laboratory personnel for use as a control and for preparation <strong>of</strong> standards. Each<br />
sample was washed with SDS (0.1 % w/v), DI water and dichloromethane before being dried at room<br />
temperature overnight. Each sample was weighed and separated into two portions <strong>of</strong> equal size that were<br />
subsequently minced with scissors or ground, respectively. Mincing was carried out in screw-cap tubes<br />
with long-blade scissors for 1 minute. Grinding was carried out in liquid nitrogen using a Glen Creston<br />
Model 6750 freezer mill equipped with micro-inserts. The optimum grinding cycle was established as 2 x<br />
2 min by SEM examination <strong>of</strong> the powders obtained following various grinding periods. The ground hair<br />
was recovered from the grinding tube and reweighed.<br />
Hair standards were prepared by adding solutions containing known amounts <strong>of</strong> drugs to drug-free hair and<br />
allowing it to dry. After addition <strong>of</strong> deuterated internal standards, hair standards and the case hair samples<br />
(up to 20 mg) from both series were suspended in methanol (1 ml), sonicated (15 min) and left for 12 hours<br />
at 45°C. The methanol was removed from the samples to clean vials and evaporated under a flow <strong>of</strong><br />
nitrogen at room temperature. The mixture was redissolved in 4 ml phosphate buffer for SPE with Bond<br />
Elut Certify LRC cartridges. Extracts were derivatised at 70°C for 20 min using 50 Jll BSTFA containing<br />
1 % TMCS and analysed by GC-MS using a Thermo-Finnigan Trace instrument fitted with a 30 m x 0.25<br />
mm x 0.25 Jlm HP-l column.<br />
The cryogenic grinding device worked effectively and produced small hair particles (19-57 Jl). However<br />
specimen losses (up to 50%) during the procedure were significant. The grinding method was time<br />
consuming and, coupled with the use <strong>of</strong> liquid nitrogen, made grinding a less cost-effective procedure.<br />
Comparison <strong>of</strong> the extracts from cut and ground hair by GC-MS indicated that grinding resulted in more<br />
matrix interferences and also that ground hair was more likely to produce a false negative result. For<br />
example in the case <strong>of</strong> methadone five samples were identified as containing methadone using cut hair but<br />
only one <strong>of</strong> these samples was identified as containing methadone using ground hair. However, ground<br />
hair gave higher recoveries <strong>of</strong> drugs than cut hair, after correction for sample losses, in many cases up to<br />
twice the amount <strong>of</strong> drug was extracted from ground hair.<br />
The results confirmed the findings <strong>of</strong> Eser et al. that the ground hair was best in terms <strong>of</strong> quantitative<br />
analysis but the findings in terms <strong>of</strong> the qualitative analysis showed clearly that cut hair is the best<br />
preparation technique. Further work will indicate if grinding will permit the use <strong>of</strong> a shorter extraction<br />
period than cut hair.<br />
Keywords: Hair Analysis, Cryogenic Grinding, Drugs <strong>of</strong> Abuse<br />
(1 ) K. Takaichi, N. P. Lemos, R. Anderson, Analysis <strong>of</strong> Opiates in Nail Clippings from Chronic Heroin<br />
Abusers, Presented at the 39 th Annual TIAFT <strong>Meeting</strong>, Prague, 2001.<br />
(2) F.M Wylie, Personal Communication.<br />
(3) H.P. Eser, L. Potsch, G. Skopp and M.R. Moeller, Influence <strong>of</strong> sample preparation on analytical<br />
results: drug analysis (GC/MS) on hair powder using various extraction techniques. For. Sci. Int.,<br />
84,271-279 (1997).<br />
Page 285
M3 <br />
AMPHETAMINE BINDING TO SYNTHETIC MELANIN AND SCATCHARD ANALYSIS OF BINDING<br />
DATA<br />
Lata Gautam*, Karen S Scott, and Michael Cole: Department <strong>of</strong> <strong>Forensic</strong> Science and Chemistry, APU, Cambridge,<br />
United Kingdom, CBI IPT<br />
The determination <strong>of</strong> drug use and drug history has historically been carried out through the analysis <strong>of</strong> biological<br />
fluids (blood and urine). In the past decade, hair analysis has been exceedingly used in order to determine recent past<br />
drug use as well as long-term drug histories through the use <strong>of</strong> segmental analysis. In order to fully understand the<br />
implications <strong>of</strong> a positive hair test result, it is important to understand how the drugs are incorporated into hair and how<br />
they bind. Keratin, melanin and lipids are possible drug binding sites in hair. Keratin and melanin have many polar<br />
groups which serve as attachment points for the drugs. Previous research into drug-hair binding has shown that<br />
different amounts <strong>of</strong> drug bind in hair <strong>of</strong> different colours. There are no structural differences in hair <strong>of</strong> different<br />
colours other than in the type and content <strong>of</strong> melanin present. For this reason, this investigation focuses on<br />
amphetamine binding to synthetic melanin in order to help to explore the possible binding mechanisms.<br />
The binding study was carried out at room temperature in the presence <strong>of</strong> light and oxygen using 0.1 M phosphate<br />
buffer at pH 7.4. Both compounds were found to be stable under these conditions. Amphetamine-d-sulphate and<br />
melanin, synthesized by the oxidation <strong>of</strong> tyrosine, were purchased from Sigma Chemical Company. As melanin is only<br />
sparingly soluble in buffer, it was solubilised in dimethyl sulphoxide (DMSO) prior to dilution with buffer. An indirect<br />
spectroscopic method was used by measuring the decrease in absorbance <strong>of</strong> amphetamine as the concentration <strong>of</strong><br />
melanin was increased. Aliquots <strong>of</strong> amphetamine were titrated against the melanin solution. Samples were incubated<br />
for 45 minutes with constant shaking. Background correction was done at each step using the same amount <strong>of</strong> melanin<br />
as present in the sample for matrix matching. The interaction was monitored using a Genesys 6v, UVNis<br />
spectrophotometer in scanning mode from 250-264 nm focussing on changes in the amphetamine spectral fingerprint at<br />
257.2 nm. Positive controls were prepared using the same amount <strong>of</strong> amphetamine as in the sample with the addition <strong>of</strong><br />
buffer instead <strong>of</strong> melanin at each step. Buffer was used for the background correction to run positive controls.<br />
To determine the classes <strong>of</strong> binding sites, association/dissociation constants and the binding capacity <strong>of</strong> melanin, the<br />
data were analysed by Scatchards' method (Scatchard et al., 1949). As the molecular weight and the structure <strong>of</strong><br />
melanin is still not clear, the number <strong>of</strong> binding sites can not be calculated directly as an integer. Instead, the ratio <strong>of</strong><br />
the number <strong>of</strong> pmoles <strong>of</strong> drug bound and the dry weight <strong>of</strong> melanin in pg is considered. This study has proved that<br />
amphetamine binds to synthetic melanin in-vitro. Data analysis from the Scatchard method has yielded a curvilinear<br />
plot with upward concavity. The curvilinear plot indicates multiple binding sites and the upward concavity indicates<br />
negative co-operativity.<br />
Scatchard Analysis <strong>of</strong> Melanin Binding <br />
Capacity for Amphetamine <br />
0.60,.......-----------------------, <br />
•<br />
0.10<br />
•<br />
•<br />
• •• • • •<br />
0.00<br />
0.20 0.25 0.30 0.35 0.40 0.45 0.50 0.55 0.60 !<br />
Reference: Scatchard G., (1949) The attractions <strong>of</strong> proteins for small molecules and ions, Annals 0/ the New York<br />
Academy o/Science. 51:660-672<br />
Keywords: Hair, Melanin, Scatchard Analysis<br />
Page 286
M4 <br />
ANALYSIS OF TRACE METAL CONTENT IN HUMAN HAIR USING LASER ABLATION<br />
INDUCTIVELY COUPLED PLASMA MASS SPECTROSCOPY (LA-ICP-MS)<br />
Wat L. Harden I * and Robyn Hannigan 2 ; IArkansas State University, Dept. <strong>of</strong> Biology, P.O. Box 419, State<br />
University, Arkansas 72467, 2Arkansas State University, Dept. <strong>of</strong> Environmental Sciences, P.O. Box 419,<br />
State University, Arkansas 72467<br />
Measuring the trace element content in human hair is traditionally done by acid digestion and analysis by<br />
atomic absorption or Inductively Coupled Plasma Mass Spectrometry (ICP-MS). Acid digestion <strong>of</strong><br />
samples can introduce contamination, which then lowers the accuracy <strong>of</strong>the analytical method. In addition<br />
to the contamination issues, acid digestion under trace metal clean conditions can be labor intensive and<br />
costly. Laser ablation (LA) is a sample introduction technique that, when combined with the ICP-MS, has<br />
the potential to provide accurate metal concentration data.<br />
Here we present method development data comparing traditional acid digestion liquid-based ICP-MS to<br />
LA-ICP-MS on two certified hair standards (International Atomic Energy Agency Reference Material<br />
Human Hair IAEA-085 and The People's Republic <strong>of</strong> China Reference Material Human Hair GBW 07601)<br />
and laboratory internal standard (USGS basalt standard BCR-2). The two sample preparation techniques<br />
that were compared were acid-digestion and solid sampling via laser ablation. Internal standards were used<br />
to calibrate both liquid and solid analysis techniques to monitor instrument drift (liquid - 115 In; solid-total<br />
Si in ppm). The concentrations <strong>of</strong> Fe, Zn, Ca, Cu, Mg and Mn <strong>of</strong> each sample were compared, using the<br />
known concentrations from each hair standard.<br />
Following the analysis <strong>of</strong> the BCR-2 standards and samples, we found that LA-ICP-MS analysis is<br />
reproducible only within an error <strong>of</strong> 20%. This could be due to matrix interferences (organic v.s. silicate)<br />
which were not corrected for in this preliminary study. Overall laser ablation is an excellent tool for trace<br />
metal analysis providing accurate element ratio data (eg; CulCa) but not concentrations at this time. Future<br />
studies will focus on the development <strong>of</strong> a matrix matched solid standard mitigating matrix interferences.<br />
Keywords: Trace Analysis, LA-ICP-MS, Hair<br />
Page 287
M5 <br />
METHOD VALIDATION AND DETERMINATION OF MDMAAND MDA IN HAIR<br />
Hee-Sun Chung l *, Eun-Young Hanl, Won-Kyung Yang l , Jae-Sin Lee l , Yong-Hoon Park I, Eun-Mi Kiml,<br />
Mi-Ae Lim l and Youngchan Y002 : lNational Institute <strong>of</strong> Scientific Investigation, Seoul; 2Korea, School <strong>of</strong><br />
Pharmacy, Chungbuk Nat. University, Chungbuk, Korea<br />
Recently, MDMA and MDA have been used as a recreational drug among young people in Korea. MDMA<br />
is a substitute for methamphetamine (MA), and has recently received much attention from media and law<br />
enforcement as a novel and popular psychoactive agent. As a result <strong>of</strong> the recent interest in designer drug,<br />
the abuse <strong>of</strong> MDMA and MDA has increased and there were cases in which both MA and MDMA were<br />
detected in hair samples. Therefore it was necessary for us to establish the detection method <strong>of</strong>MDMA and<br />
MDA in hair samples. The method validation and uncertainty measurement were also studied and<br />
described. The prevalence <strong>of</strong> MDMA was surveyed in hair specimens submitted for drug testing by this<br />
method.<br />
MDMA, MDA, MDMA-ds, and MDA-ds were purchased from Radian International LLC (Austin, TX,<br />
USA). Hair samples were collected from 791 subjects who were suspected MDMA and MDA users. After<br />
washing, the hair was cut into small pieces <strong>of</strong> less than 1 mm and incubated. SPME extraction was applied<br />
and extracts were derivatized by trifluoroacetic anhydride (TF A). Gas chromatograph-mass spectrometry<br />
(GCIMS) analysis was performed under selective ion monitoring (SIM) conditions for the identification<br />
and quantitation <strong>of</strong>MDMA and MDA.<br />
Limit <strong>of</strong> detection (LOD) and limit <strong>of</strong> quantitation (LOQ) <strong>of</strong> MDA and MDMA were 0.125 ng/mg,<br />
0.25ng/mg respectively. The linear calibration curve ranged from 0.25 to 10 ng/mg with the coefficient<br />
determination <strong>of</strong> R2 >0.99 . Within- and between run precisions were measured in three concentrations<br />
(low 0.8 ng/mg, med 4 ng/mg, high 8 ng/mg). The specificity in blank hair and dyed artificial hair was<br />
studied.. The high concentration <strong>of</strong> ephedrine, norephedrine, pseudoephedrine, nicotine, caffeine,<br />
methoxyphenamine, phenterminein in low QC hair samples (0.8ng/mg) didn't show any interference in this<br />
method. To value the confidence <strong>of</strong> the method, uncertainty was performed at the cut-<strong>of</strong>f level 5 ng/mg<br />
hair samples. The measurement in uncertainty <strong>of</strong> MDMA was ±0.22 -0.30 (95% confidence interval, k=2).<br />
Among 791 hair samples studied, 44 hair samples were positive for MDMA or MDA (5.6 %). The<br />
concentration <strong>of</strong> MDA was low in the hairs where both MDMA and MDA were detected indicating MDA<br />
was the metabolite <strong>of</strong> MDMA, while in 4 specimens the level <strong>of</strong> MDA was very high with no MDMA<br />
indicating MDA was administered. However in urine samples from same 44 subjects showed 35 were<br />
negative for MDMA or MDA, while 9 were positive for MDMA. The hair analysis <strong>of</strong>MDMA showed that<br />
a hair sample is a good specimen for the confirmation <strong>of</strong> long abuse <strong>of</strong> MDMA and MDA in comparison<br />
with urine.<br />
Keywords: MDMA, Hair Analysis, Method Validation<br />
Page 288
M6 <br />
MONITORING DRUG USE THROUGH SEGMENTAL HAIR ANALYSIS. A THREE YEAR<br />
CASE STUDY.<br />
Karen S. Scott*, Kerri-Ann Hoy: Department <strong>of</strong> <strong>Forensic</strong> Science and Chemistry, AngJia Polytechnic<br />
University, Cambridge<br />
Segmental analysis <strong>of</strong> hair for the determination <strong>of</strong> past drug use is an area which receives mixed views<br />
within the field <strong>of</strong> <strong>Forensic</strong> Toxicology. The aim <strong>of</strong> this study was to ascertain if an accurate pattern <strong>of</strong><br />
drug use can be predicted by the segmental analysis <strong>of</strong>a length <strong>of</strong> hair. The hair sample (33cm length) was<br />
obtained from a 47 year old male with a known history <strong>of</strong> use <strong>of</strong> three types <strong>of</strong> medication. Atenolol<br />
(IOOmg) was taken as required; diazepam (3x 5mg) was taken as required and dihydrocodeine (3 x 30 mg)<br />
was taken daily. All three drugs had been prescribed over a period <strong>of</strong>9 years following a serious injury.<br />
The hair was cut into eleven 3 cm sections each representing an approximate period <strong>of</strong> three months<br />
(assuming a hair growth rate <strong>of</strong> I cm/month). The segments were prepared for extraction by washing and<br />
cutting. Blank hair was obtained from a subject known not to have used any <strong>of</strong> the drugs under<br />
investigation and similarly prepared. Triplicate aliquots (20 mg) <strong>of</strong> the hair were subjected to overnight<br />
acidified methanolic digestion along with standards and blanks. Following digestion the samples were<br />
filtered, evaporated to dryness, derivatised using BSTF A 1% TMCS and analysed by GCIMS in the SIM<br />
mode.<br />
Analysis <strong>of</strong> atenolol in the hair segments showed a variable pattern <strong>of</strong> use. No accurate record <strong>of</strong> atenolol<br />
use was obtained other than an increased use for short periods <strong>of</strong> time 9 and 18 months prior to sampling.<br />
The highest concentration <strong>of</strong> atenolol in the hair segments was obtained in segment three (corresponding to<br />
6-9 months hair growth). A slight increase in the levels measured in segment six (corresponding to 15-18<br />
months) was also observed.<br />
The analysis <strong>of</strong> diazepam in hair showed an overall increase <strong>of</strong> drug in hair from the proximal end to the<br />
distal end. It is known that the subject decreased the frequency <strong>of</strong> diazepam use in the 18 months prior to<br />
sampling which is consistent with the decreased concentrations in these hair sections. However there is a<br />
threefold increase in the amount <strong>of</strong> diazepam detected between segment six (15-18 months) and segment II<br />
(30-33 months). No drug use history <strong>of</strong> diazepam is available for this period.<br />
Finally, the analysis <strong>of</strong>dihydrocodeine for which the full drug history was known (90 mg/day for 9 years)<br />
yielded extremely interesting results. If no environmental issues (e.g. UV exposure, washing) affect the<br />
amount <strong>of</strong> drug in hair then we would expect the levels in the proximal and distal segments to give the<br />
same concentration. However a decrease <strong>of</strong> approximately 90% in the level <strong>of</strong> dihydrocodeine detected<br />
was observed (r2 0.77).<br />
This study demonstrates that hair analysis can be used to detect drugs which were taken several years ago.<br />
More work is required to determine the exact relevance <strong>of</strong> history evaluation through segmental analysis<br />
but the results for dihydrocodeine indicate that this is not a futile exercise. The importance <strong>of</strong> obtaining a<br />
full drug use history from subjects participating in studies <strong>of</strong> this type is highlighted in the analysis <strong>of</strong> both<br />
atenolol and diazepam where gaps in the history meant that a full interpretation <strong>of</strong> the results could not be<br />
carried out.<br />
Keywords: Segmental Analysis, Drug Use History<br />
Page 289
M7 <br />
EVALUATION OF KETAMINE ABUSE USING HAIR ANALYSIS: CONCENTRATION<br />
TRENDS IN A SINGAPORE POPVLA TION<br />
H.S. Leong', N.L. Tan, C.P. Lui, and T.K. Lee: Narcotics II Laboratory, Centre for <strong>Forensic</strong> Science,<br />
Health Sciences Authority, 11 Outram Road, Singapore 169078.<br />
Ketamine has been used as an anaesthetic since its discovery in 1961. Today, the drug is used primarily in<br />
veterinary medicine, and in some short-term surgical procedures in humans. Ketamine also produces posthypnotic<br />
emergence reactions such as prolonged hallucination and delirium, which has led to its abuse.<br />
Due to the increasing abuse <strong>of</strong> ketamine in Singapore, ketamine, norketamine and its dehydro derivatives<br />
were listed as Class B Controlled Drugs under the Misuse <strong>of</strong> Drugs Act (CAP.185) in September 1999. As<br />
a drug <strong>of</strong> abuse, ketamine can be administered orally, snorted, or injected. In Singapore, the most common<br />
mode <strong>of</strong> administration is through snorting. The majority <strong>of</strong> the ketamine abusers consist <strong>of</strong> teens and<br />
young working adults.<br />
The laboratory has been analyzing ketamine in urine <strong>of</strong> suspected abusers since September 1999. In the<br />
period <strong>of</strong> January 2000 to April <strong>2004</strong>, there were a total <strong>of</strong> 17,133 urine samples submitted for ketamine<br />
analysis, out <strong>of</strong> which 26.6 % were tested positive for ketamine during the period <strong>of</strong> January 2000 to April<br />
2001. The number <strong>of</strong> positive samples increased significantly to 51.2 % during the period <strong>of</strong> May 2003 to<br />
April <strong>2004</strong>. Recently, the enforcement agency <strong>of</strong> Singapore has indicated interest in the detection <strong>of</strong><br />
ketamine in hair. This is because many <strong>of</strong> the abusers have claimed that their drinks were spiked with<br />
ketamine to avoid prosecution. The detection <strong>of</strong> ketamine in hair would determine whether they were<br />
habitual users or it was an one-<strong>of</strong>f consumption.<br />
This paper presents a method for the detection <strong>of</strong> ketamine in hair. Hair samples (25 mg) were washed,<br />
pulverized and digested in hydrochloric acid (O.5M) overnight at 45°C. The samples were extracted by an<br />
automated solid-phase extraction procedure and the extracts were subsequently analyzed using gas<br />
chromatography/mass spectrometry (GCIMS) in selected ion monitoring mode (SIM). Good linearity up to<br />
120 ng/mg was obtained for both ketamine and norketamine (r 0.9987 and r2 0.9985, respectively).<br />
Limit <strong>of</strong> detection (LOD) was found to be at 0.4 ng/mg for both drugs while the limit <strong>of</strong>quantitation (LOQ)<br />
was found to be 0.6 and 0.8 ng/mg for ketamine and norketamine, respectively. Other parameters- such as<br />
intra- and inter-day variation were also determined.<br />
About 9 I hair segments from suspected ketamine abusers were analyzed. In most <strong>of</strong> the hair segments,<br />
ketamine was found to bethe predominant analyte (norketamine to ketamine ratio < 1). This is in contrast<br />
to urine where the metabolite norketamine is usually found to be the predominant analyte. The range <strong>of</strong><br />
ketamine detected in hair was found to be from 0.6 ng/mg to 489.0 ng/mg (Mean = 49.0 ng/mg) whereas<br />
the range <strong>of</strong> norketamine detected was from 0.8 ng/mg to 196.3 ng/mg (Mean = 12.1 ng/mg). At<br />
concentrations higher than 120 ng/mg, about 5 mg <strong>of</strong> hair is sufficient for the re-analysis <strong>of</strong> the sample.<br />
Based upon the· voluntary confession <strong>of</strong> the ketamine abusers, a correlation between the amount <strong>of</strong><br />
ketamine detected and the frequency <strong>of</strong> abuse was observed. For abusers who snort the drug occasionally<br />
(once a week), the concentration <strong>of</strong>ketamine detected in hair was in the range <strong>of</strong> 1.1 ng/mg to 42.7 ng/mg<br />
(Mean 9.9 ng/mg). For those who abuse the drug more frequently (twice or thrice a week), the<br />
concentration <strong>of</strong> ketamine detected was in the range <strong>of</strong> 13.5 ng/mg to 111.l ng/mg (Mean 37.4 ng/mg).<br />
For those who abuse the drug daily, the concentration <strong>of</strong> ketamine detected was above 45.1 ng/mg (Mean =<br />
121.3 ng/mg). Based on the results <strong>of</strong> the analysis, three types <strong>of</strong> trends for ketamine abuse were observed:<br />
Low (1.0 - 10.0 ng/mg), medium (11.0 50.0 ng/mg), and high (>50.0 ng/mg). Segmental analysis <strong>of</strong> the<br />
hair samples <strong>of</strong> the abusers was also performed and its significance is discussed in relation to the history <strong>of</strong><br />
drug use.<br />
In conclusion, ketamine in hair can be determined by using acid digestion and subsequent GCIMS analysis.<br />
Based on the amount <strong>of</strong> ketamine found in hair, certain patterns <strong>of</strong> consumption among ketamine abusers<br />
can be demonstrated.<br />
Keywords: Ketamine, hair analysis, GC/MS/SIM<br />
Page 290
M8 <br />
THE REQUIREMENT FOR EFFECTIVE WASH PROCEDURES FOR HAIR TESTING, AND<br />
THE APPLICATION OF A WASH METHOD TO SAMPLES SOAKED IN COCAINE<br />
SOLUTIONS OF 1 TO 50 UG/ML<br />
Michael Schaffer*, Virginia Hill, Thomas Cairns: Psychemedics Corporation, 5832 Uplander Way, Culver<br />
City, C:A<br />
It has been proposed that issues <strong>of</strong> external contamination <strong>of</strong> hair can be resolved by relying on the<br />
presence <strong>of</strong> metabolites. However, even if some metabolites such as cocaethylene are sufficiently<br />
definitive to indicate certainty <strong>of</strong> use, others such as benzoylecgonine also occur as contaminants. In<br />
addition, for phencyclidine only the parent is determined. Therefore effective washing procedures are<br />
important in order to rule out contamination as the source <strong>of</strong> the parent and or metabolite. The protection<br />
provided by cut<strong>of</strong>fs is also dependent on effective washing procedures to remove surface contamination;<br />
such contamination can range from very little to at least as much as 20 times the amount in the hair. In<br />
testing head hair samples from 75 drug rehabilitation subjects with cocaine-positive urines, cocaine<br />
contamination ranged from 0.7 to 8009 ngllO mg hair; the amounts in the washes ranged from 4% to over<br />
2000% <strong>of</strong> the drug content <strong>of</strong> the hair. The wash procedure used for these samples was as follows. First,<br />
dry isopropanol (2 mL) was added t6 about 12 mg <strong>of</strong> hair in 12 x 75 mm tubes; the tubes were shaken<br />
vigorously at 37"C for 15 minutes, after which the isopropanol was removed to a separate tube and saved<br />
for later analysis. Then 2 mL <strong>of</strong> 0.0 1 M phosphate buffer/O.O 1 % BS:A, pH 6, was added to the hair samples<br />
in the tubes and the tubes shaken vigorously for 30 minutes at 37"C, after which the buffer was removed<br />
and saved to a another tube for later analysis.· This 30-minute wash was repeated twice more, followed by<br />
two 6O-minute washes using the same conditions. :After the final (Sib) phosphate buffer wash and removal<br />
<strong>of</strong> the buffer, the hair sample was enzymatically digested for confirmation by LCIMSIMS. The washes are<br />
routinely analyzed by RIA. The wash criterion is computed by multiplying by 5 the amount <strong>of</strong> drug per mg<br />
hair in the last wash and subtracting the result from the amount <strong>of</strong> drug per mg hair in the hair digest. The<br />
Wash Criterion is actually an overestimate <strong>of</strong> the amount <strong>of</strong> drug that would be removed by 5 additional 1<br />
hour washes. If the result after the subtraction is less than the cut<strong>of</strong>f for the parent drug, the result is<br />
considered negative in indicating drug use. The parent-drug cut<strong>of</strong>f value for cocaine was 5 ng 110 mg hair (<br />
500 pg/mg).<br />
The effectiveness <strong>of</strong> the wash procedure was challenged by contaminating negative hair (including blonde,<br />
auburn, brown and black samples) by soaking for one hour in 1000, 10,000, and 50,000 nglmL cocaine.<br />
These amounts far exceed any likely real-life contamination scenarios. :After drying, the samples were<br />
washed by the procedures described and digested for confirmation by LC/MSIMS The uptake <strong>of</strong> the<br />
cocaine was approximately linear with increasing concentrations <strong>of</strong> cocaine in the soaking solutions, and<br />
the amounts <strong>of</strong> cocaine in the hair and washes were correspondingly increased. Total cocaine measured in<br />
the wash and hair ranged from 20.6 to 66.5 ng cocainellO mg hair for those samples soaked in 1000 nglm;<br />
from 185.6 to 590.7 for those samples soaked in 10,000 ng/m; and 885.6 to 1916.7 for those soaked in<br />
50,000 ng/mL. By application <strong>of</strong> the wash criterion, all samples were clearly identified as contaminated.<br />
The values for hair digests after application <strong>of</strong> the wash criterion were -0.04 to 1.45 ng/IO mg hair for<br />
samples soaked in 1000 ng/mL; -18.28 to 2.83 for those soaked at 10,000 nglml; and -258.0 to -42.9 for<br />
those soaked at 50,000 ngllO mg hair. Thus the wash procedure and criterion were effective even for<br />
extreme conditions <strong>of</strong> contamination by soaking.<br />
Keywords: Hair, Contamination, Washing<br />
Page 291
M9 <br />
SCREENING OF BENZODIAZEPINES AND HYPNOTICS IN HAIR BY LC-MSIMS:<br />
APPLICATION TO FOUR DRUG-FACILITATED CRIMES<br />
M. VilIain 1 *, M. Cheze 2 , B. Ludes 1 , P. Kintz!; 1 Institut de Medecine Legale, II rue Humann, 67000<br />
Strasbourg, France and 2 ToxLab, 7 rue Jacques Cartier, 75018 Paris, France<br />
The use <strong>of</strong> a drug to modifY a person's behavior is not a recent phenomenon, but reports dealing with drugfacilitated<br />
crimes (sexual assaults, robbery ... ) are constantly increasing. Among drugs involved in such<br />
cases, benzodiazepines (flunitrazepam, bromazepam, ... ) and hypnotics (zopiclone, zolpidem) are largely<br />
concerned.<br />
In most cases and due to a long delay between the event and the claim to the police, blood and even urine<br />
samples are <strong>of</strong> little value. This is the reason why this laboratory developed a original approach based on<br />
hair testing. In practice, hairs <strong>of</strong> the victim are collected about one month after the alleged <strong>of</strong>fense,<br />
segmented and analyzed by LC-MSIMS. In positive cases, the drug is supposed to be found only in the<br />
segment corresponding to the period <strong>of</strong>the event.<br />
The Hair strand is twice decontaminated using methylene chloride and then segmented (3 segments <strong>of</strong> 2<br />
cm). Each segment is cut into small pieces «lmm). About 20 mg are overnight incubated in phosphate<br />
buffer at pH 8.4, in the presence <strong>of</strong> 1 ng <strong>of</strong> diazepam-ds used as internal standard (IS). After a liquid-liquid<br />
extraction with a mixture <strong>of</strong> methylene chlorideldiethyl ether (80/20) and evaporation to dryness, the<br />
residue is reconstituted in 50 J.1L <strong>of</strong> acetonitrile/water (50/50).<br />
Chromatography is achieved using a XTerra MS CI8 column (100 x 2.1 mm, 3.5J.1m) eluted with a<br />
gradient <strong>of</strong> acetonitrile and formate buffer delivered at a flow rate <strong>of</strong> 0.2 mLlmin.<br />
A Quattro Micro triple-quadrupole mass spectrometer is used for analyses. Ionization is achieved using<br />
electrospray in the positive ionization mode (ES+). For each compound, detection is related to two<br />
daughter ions.<br />
To demonstrate the applicability <strong>of</strong>this method, 4 expertises are describe as follows:<br />
1. A-21 year old girl was <strong>of</strong>fered a c<strong>of</strong>fee that made her unconscious. The victim's hair, collected 15<br />
days after the alleged <strong>of</strong>fense, was tested by LC-MSIMS and the first 2 cm segment was positive<br />
at a concentration <strong>of</strong>4.4 pg/mg whereas the 2 other segments were zolpidem free.<br />
2. A 16-year old girl claimed to have been raped during an afternoon, while sedated. Hair was<br />
sampled 9 weeks after the alleged <strong>of</strong>fense and the first 3 cm segment was positive for zopiclone at<br />
a concentration <strong>of</strong> 4.2 pg/mg, the second (3 to 5 cm) at 1.0 pg/mg, whereas the last segment (5 to<br />
7 cm) was zopiclone free.<br />
3. A 39-year old woman felt sleepy for 24 hours after having drunk a c<strong>of</strong>fee. Hair was collected I<br />
month after the event and the proximal 2 cm-Iong segment was positive for bromazepam at 10.3<br />
pg/mg and the other segments (2-4 and 4-6 cm) remained negative.<br />
4. A woman was confined illegally for 12 days, repetitively raped and forced to sign .cheques, while<br />
being under the influence <strong>of</strong> an hypnotic. Hair was positive for 7-amin<strong>of</strong>lunitrazepam in the<br />
proximal segment (0 to 3 cm) at 31.7 pg/mg, in the second segment (3 to 6 cm) at 2.0 pg/mg and<br />
was negative in the distal one (6 to 9 cm).<br />
In drug-facilitated crimes, hair is a very useful alternative specimen, and the concentrations measured, in<br />
the pg/mg range, require tandem mass spectrometry.<br />
Keywords: Hair, LC-MS/MS, drug-facilitated crime<br />
Page 292
MIO <br />
QUANTIFICATION OF AMPHETAMINE AND METHAMPHETAMINE ENANTIOMERS IN<br />
HAIR SPECIMENS BY GC-MSINCI<br />
Liliane Martins!, Michel Yegles 1 , Heesun Chung 2 , Robert Wennig l *: I Laboratoire National de Sante,<br />
Toxicologie, CRP-Sante, Universite du Luxembourg and 2 National Institute <strong>of</strong> Scientific Investigation,<br />
Seoul, Korea<br />
Introduction: Enantioselective separation <strong>of</strong> amphetamines is <strong>of</strong> great importance in clinical and forensic<br />
toxicology, as the S-(+)-enantiomers <strong>of</strong> methamphetamine (MA) and amphetamine (AM) are known to be<br />
considerably more stimulant than the R-(-) isomers. The determination <strong>of</strong> their respective enatiomeric<br />
ratios allows the distinction between legal intake and illicit MA and/or AM consumption.<br />
A method describing the chiral separation <strong>of</strong> AM and MA after derivatisation with S-(-)<br />
heptafluorobutyrylprolyl chloride (S-HFBPCI) and quantification by gas chromatography coupled to mass<br />
spectrometry operating in the negative-ion chemical ionization mode (GC-MSINCI), has already been<br />
applied to serum, urine and oral fluid. In the present study the previous method was modified to be suitable<br />
for abusers' hair analysis.<br />
Material and methods: Hair specimens were obtained from I I Korean suspected MA abusers. After<br />
digestion with 1 M sodium hydroxide at 100°C during 30 min, followed by solid phase extraction using<br />
Cleanscreen ZDAU and derivisation with S-HFBPCI, the enantiomers were quantified by GC-MSINCI<br />
using deuterated internal standards were operated. Extraction yields varied between 88.5 and 100 %, LODs<br />
were 10.6 and 2.2 pglmg hair for MA and AM respectively.<br />
Results: Concentration ranges <strong>of</strong> 25.2 to lOlA ng/mg hair for MA and 0.69 to 4.54 nglmg hair for AM<br />
were observed. For 2 specimens, only the S-(+)-enantiomer was detected, for 8 specimens the RlS ratio was<br />
< I (0.17 - 0.59 for MA and 0.12 - 0.3 I for AM), whereas for one specimen a RlS ratio <strong>of</strong> 10.1 and 1.2 was<br />
determined for MA and AM respectively.<br />
Conclusions: Similar to serum, urine and saliva, our results point out the predominance <strong>of</strong> the S-(+)<br />
enantiomer in hair. In one case the R-(-)-MA concentration was higher than the S-(+)-enantiomer. This<br />
may be due to the consumption <strong>of</strong> prescription drugs either containing R-(-)-MA or biotransformed to R-(<br />
)-MA. The present study shows that hair analysis <strong>of</strong> amphetamines' enantiomers may be helpful to avoid<br />
misinterpretation in the discrimination between prescription drug use and illegal drug consumption.<br />
Keywords: Hair analysis, Enantioselective Separation, Amphetamines<br />
Page 293
Mll<br />
DIAGNOSIS OF CHRONIC ALCOHOL CONSUMPTION. HAIR ANALYSIS FOR ETHYL<br />
GLUCURONIDE<br />
C. Jurado·, T. Soriano, M.P. Gimenez, M. Menendez :Instituto Nacional de Toxicologfa. P.O. Box 863.<br />
41080 Sevilla. Spain<br />
Alcohol abuse is one <strong>of</strong>the most serious social problems throughout the world. Ethyl-glucuronide is minor<br />
metabolite <strong>of</strong> ethanol and has proved to be a good alcohol marker. In addition, hair analysis has<br />
demonstrated its usefulness in establishing chronic consumption <strong>of</strong> drugs <strong>of</strong> abuse. The objective <strong>of</strong> the<br />
present study is to develop and validate a sensitive, precise and specific analytical method for the<br />
determination <strong>of</strong> ethyl-glucuronide in hair samples.<br />
During method development the efficacy <strong>of</strong> extraction <strong>of</strong> EtG from hair was compared in four extraction<br />
methods: a) methanol; b) methanol:water (1:1); c) water; and d) water:trifluoroacetic acid (9:1). Water was<br />
found to be the best extracting solvent, since it provided the highest recoveries, with cleaner extracts. The<br />
final method is as follows: about 100 mg <strong>of</strong> hair are sequential\y washed with water and acetone. The<br />
decontaminated sample is finely cut with scissors, then the deuterated internal standard (EtG-d 5 ) and 2 mL<br />
<strong>of</strong> water are added. After sonication for two hours, the sample is maintained at room temperature overnight<br />
Derivatization is performed with PFPA. Derivatives are injected into a GCIMS system in the electronic<br />
impact mode. The method shows linearity over the range <strong>of</strong> concentrations from 0.050 ng/mg to 5 ng/mg.<br />
Detection and quantification limits are 0.025 ng/mg and 0.050 ng/mg, respectively. Mean recoveries for the<br />
three studied concentrations (low, medium and high) are higher than 87%. The coefficients <strong>of</strong> variation in<br />
intra- and inter-assay precision are always lower than 7%. The method is being routinely applied in our lab<br />
for the diagnosis <strong>of</strong> chronic alcohol consumption. Some examples will be shown. All <strong>of</strong> them derived from<br />
divorce proceedings where chronic alcohol consumption was required by the Court. EtG concentrations<br />
ranged from 0.05 to 0.75 ng/mg <strong>of</strong> hair.<br />
Keywords: Ethyl-glucuronide, Alcohol Markers, Hair Analysis<br />
Page 294
.~.<br />
M12 <br />
OPIATE CONCENTRATIONS IN HAIR FROM SUBJECTS IN A CONTROLLED HEROIN<br />
MAINTENANCE PROGRAM AND FROM OPIATE-ASSOCIATED FATALITIES<br />
Mussh<strong>of</strong>fF*, Lachenmeier K., Wollersen H., Madea B.: Institut <strong>of</strong>LegaJ Medicine, Bonn, Germany<br />
Introduction: The objective <strong>of</strong> this study was the determination <strong>of</strong> the concentration <strong>of</strong> opiates (heroin =<br />
HER, mono acetyl morphine MAM, morphine = MOR, codeine COD, acetyl codeine AC) in hair,<br />
and in particular an investigation <strong>of</strong> dose-concentration relationships as well as the possibility <strong>of</strong> using AC<br />
as a marker for consumption <strong>of</strong> illicit heroin in contrast to pharmaceutical heroin.<br />
Methodology: After the controlled Lv. administration <strong>of</strong> pharmaceutical heroin-HCI (l0-1000 mg/d), the<br />
concentrations <strong>of</strong> opiates in head hair were determined (n = 46), using a validated GC-MS method with<br />
LOD's between 0.02 and 0.04 ng/mg. In addition, a collective <strong>of</strong> opiate-associated fatalities was examined<br />
(n 24).<br />
Results: The concentrations obtained in the proximal segment (1 cm) <strong>of</strong> the patients were between 0.04<br />
and 0.21 ng/mg for HER, for MAM betv.een 0.05 and 5.64 ng/mg and for MOR between 0.03 and 8.37<br />
ng/mg. There was no statistically significant difference in the concentrations in comparison to the opiate<br />
fatalities (HER 1.55-5.20 ng/mg, MAM 0.04-30.01 ng/mg, MOR 0.03-11.87 ng/mg in the proximal<br />
segments). After controlled heroin administration, a correlation between the dose and the total opiate<br />
concentration in the hair was found (r=0.66). When considering a single analyte, the coefficient <strong>of</strong><br />
correlation increased when plasma half-life increases (r=OA2, r=0.58 and r=O.69 for HER, MAM and<br />
MOR). COD and AC were detected in 13.0 % and 10.9 % <strong>of</strong> the samples <strong>of</strong> the heroin program, as well as<br />
in 33.3 % and 16.7 % in opiate-associated fatalities, respectively.<br />
Discussion: The results confirm the first observations <strong>of</strong> Kintz et aI., who found only limited doseconcentration<br />
relationships after HER abuse in hair. The correlation is influenced by the plasma half-lifes<br />
<strong>of</strong> analytes. The lack <strong>of</strong> differences between obtained opiate concentrations in the hair <strong>of</strong> participants in a<br />
controlled heroin maintenance program and <strong>of</strong> opiate-associated fatalities does not support the hypothesis<br />
that a lack <strong>of</strong> tolerance can be regarded as a potential cause <strong>of</strong> death. In addition, the absence <strong>of</strong> AC also in<br />
the majority <strong>of</strong>the deaths questions its suitability as a characteristic marker <strong>of</strong> a preceding consumption <strong>of</strong><br />
illicit heroin.<br />
Keywords: Hair analysis, opiates, heroin maintenance program<br />
Page 295
M13 <br />
EVIDENCE OF ADDICTION BY ANAESTHETISTS AS DOCUMENTED BY HAIR ANALYSIS<br />
P. Kintz*, M. Villain, B. Ludes: Institut de Mectecine Legale, 11 rue Humann, F-67000 Strasbourg, France<br />
Chemical dependency is a disease that can affect all pr<strong>of</strong>essions. Among the health care pr<strong>of</strong>essionals,<br />
anesthesiologists represent a specific group. Numerous factors have been proposed to explain the high<br />
incidence <strong>of</strong> drug abuse among anesthesiologists. These include: easy access to potent drugs, particularly<br />
narcotics, highly addictive potential <strong>of</strong> agents with which they are in contact, and easy diversion <strong>of</strong> these<br />
agents since only small doses will initially provide an effect desired by the abuser. Opioids are the drugs <strong>of</strong><br />
choice for anesthesiologists, and among them fentanyl and sufentanil are the most commonly used.<br />
Alcohol, mostly in older anesthesiologists, prop<strong>of</strong>ol, ketamine, thiopental and midazolam are also abused.<br />
In fact, all but quaternary ammonium drugs can be observed. Symptoms <strong>of</strong>addiction in the hospital include<br />
: unusual changes in behavior, desire to work alone, refuse <strong>of</strong> lunch relief or breaks, volunteer for extra<br />
cases, call, come in early and leave late, frequent restroom breaks, weight loss and pale skin, malpractice,<br />
behind on charts, etc. Toxicological investigations are difficult, as the drugs <strong>of</strong> interest are difficult to test<br />
for. In most cases, half-lives <strong>of</strong> the compounds are short, and the circulating concentrations weak. It is<br />
therefore necessary to develop GCIMS/MS or LC/MS procedures to satisfY the criteria <strong>of</strong> identification and<br />
quantitation. In most cases, blood and/or urine analyses are not useful to document impairment, as these<br />
specimens are collected at inadequate moments. Hair analysis appears therefore as the unique choice to<br />
evidence chronic exposure. Depending the length <strong>of</strong> the hair shaft, it is possible to establish an historical<br />
record, associated to the pattern <strong>of</strong> drug use, considering a growth rate <strong>of</strong> about 1 crn/month.<br />
After decontamination with dichloromethane, drugs are extracted from the hair after incubation in pH 8,4<br />
phosphate buffer either by Iiquidlliquid extraction or headspace technology. Opiates, fentanyl derivatives,<br />
benzodiazepines and prop<strong>of</strong>ol are analyzed by GCIMS, GCIMS/MS, LCIMS/MS and headspace GCIMS,<br />
respectively.<br />
The following cases will be reviewed:<br />
Case 1: 50-year old anaesthetist, positive for fentanyl (644 pglmg)<br />
Case 2: 42-year old anaesthetist, positive for fentanyl (101 pg/mg) and sufentanil (2 pglmg)<br />
Case 3: 40-year old anaesthetist, positive for codeine (210 pglmg), alfentanil (30 pg/mg) and<br />
midazolam (160 pglmg)<br />
Case 4: 44-year old nurse, found dead, positive for midazolam (760 pglmg) and prop<strong>of</strong>ol (1390<br />
pglmg)<br />
In these cases, the combination <strong>of</strong> an alternative specimen (hair) and hyphenated analytical techniques<br />
(tandem mass spectrometry) appears as a pre-requisite.<br />
Keywords: Addiction, Anaesthetist, Hair<br />
Page 296
M14 <br />
CLOZAPINE DOSE-HAIR CONCENTRATION RELATIONSHIPS: EVALUATION OF<br />
INPA TlENT AND OUTPA TlENT DATA<br />
Robert Kronstrand*, Ingrid Nystrom, Markus Roman, and Martin Josefsson: National Board <strong>of</strong> <strong>Forensic</strong><br />
Medicine, Dep. <strong>Forensic</strong> Chemistry, Linkoping, Sweden<br />
The aim <strong>of</strong> this work was to test the hypothesis that the concentration <strong>of</strong> clozapine in hair is dependent on<br />
the dose administered. The hypothesis was tested both in an inpatient (N=22) and an outpatient (N=41)<br />
population, with and without correction for hair pigmentation.<br />
Samples were taken from the head and stored dark at room temperature until analyzed. Five cm <strong>of</strong> each hair<br />
sample was analyzed. Briefly, the hair was cut into small pieces and weighed into a 10 mt screw-capped<br />
tube. To approximately 25 mg <strong>of</strong> hair were added 0.5 mL <strong>of</strong> mobile phase (10:10:80 mixture <strong>of</strong><br />
acetonitrile:methanol:20mM formate buffer pH 3.0) and 25 /-ll <strong>of</strong> internal standard (2.0 Ilg/ml <strong>of</strong> d3<br />
mianserine) and the sample was incubated in a water bath (with orbital shaking) at 37 °C during 18 hours.<br />
A 150-/-ll aliquot was transferred to an autosampler vial and 10 /-ll were injected into the chromatographic<br />
system.<br />
The LC-MS-MS analysis was performed on a Perkin Elmer Series 200 chromatography system consisting<br />
<strong>of</strong> a Series 200 pump, Series 200 auto sampler, and a SCIEX API 2000 MS-MS instrument equipped with<br />
an electrospray interface (Turbo Ion Spray). We used a 50x2.l mm Zorbax SB-Cyano analytical column<br />
with 3-fJ.m particle size. For clozapine, two transitions, 327.11270.0 and 327.1/192.2, were monitored and<br />
for d3-mianserine 268.31208.2 was monitored. All samples were also analyzed for melanin using<br />
spectrophotometry (Iambda=550 nm) as previously described (Kronstrand et al. Clinical Chemistry 1999,<br />
45:9, pp 1485). The daily doses ranged from 125 to 800 mgs.<br />
The hair melanin concentrations ranged from 5 to 49 /-lg/mg and the clozapine concentrations ranged<br />
between 1.1 to 37 nglmg. In the outpatient population a coefficient <strong>of</strong> determination <strong>of</strong> r=0.14 was achieved<br />
when correlating the dose with the hair c10zapine concentration, as compared to 0.36 for the inpatient<br />
population. When melanin was taken into account the coefficients were increased to 0.36 (out) and 0.62<br />
(in), respectively. The results indicated that melanin influenced the incorporation <strong>of</strong> c10zapine into hair and<br />
that the outpatients might have been less compliant than the inpatients, and thus obscuring the results. In<br />
summary, it seems that the more controlled the dosing is, and the more factors that influence incorporation<br />
are taken into consideration, the better the relationship between dose and hair concentration. Our<br />
hypothesis was only confirmed under the certain circumstances <strong>of</strong> controlled dosing and melanin correction<br />
(see figure), otherwise no correlation could be found between the dose and the hair c10zapine concentration.<br />
Inpatient Dose vs CLZlMEL<br />
1,6<br />
1,2 •<br />
r=O,62<br />
01<br />
• • • <br />
• •<br />
~ 0,8<br />
c<br />
0,4<br />
0,0 I <br />
100 300 500 700 900 <br />
mg/day<br />
Page 297
M15 <br />
DRUG DETECTION IN ORAL FLUID: IDENTIFICATION OF POLY DRUG USE BY EIA AND GC<br />
MS<br />
Joe Clarke 2 *, Lolita Tsanaclisl , and John Wicks! : !Tricho-Tech Limited, The Cardiff Medicentre, Heath Park,<br />
Cardiff, CF14 4UJ, United Kingdom.; 2Altrix Healthcare Pic, Birchwood Science Park, Warrington, WA3 7BP,<br />
United Kingdom.<br />
The analysis <strong>of</strong> drugs <strong>of</strong> abuse in oral fluid is becoming more widely used and accepted across a number <strong>of</strong><br />
testing disciplines, particularly because <strong>of</strong> its simplicity to collect in relation to urine. Commonly abused and<br />
prescribed drugs are known to be detectable in oral fluid. The objective <strong>of</strong> this study was to assess the prevalence<br />
<strong>of</strong> a number <strong>of</strong> drugs in oral fluid with specimens collected from known and unknown drug users. The cut-<strong>of</strong>f<br />
levels for oral fluid are much lower then those for urine. Certain analytical methods that are used with urine<br />
samples, including immunoassay and GC-MS, are not necessarily applicable for screening oral fluid specimens.<br />
This study provides a compilation <strong>of</strong> data for the confirmation by GC-MSIEI, GC-MS/CI or GC-MS/MS <strong>of</strong> oral<br />
fluid for a wide range <strong>of</strong> analytes. Oral fluid specimens (N=8911) were collected with prior consent from various<br />
establishments in the U.K including private companies, rehabilitation clinics, and criminal justice services using<br />
the Intercept® DOA collection device (OraSure Technologies, USA) according to manufacturer's instructions.<br />
Specimens were initially screened for a combination <strong>of</strong> Opiates, Cocaine metabolites, Cannabinoids,<br />
Amphetamines, Benzodiazepines and Methadone using separate OraSure Technologies Inc. micro-plate enzyme<br />
immunoassays and Buprenorphine (Diagnostix Ltd, Canada), according to manufacturer's instructions.<br />
For the confirmation analysis by Gas Chromatography-Mass Spectrometry (GC-MS), the samples were cleaned<br />
using Oasis® MCX Cartridges and derivatised with TFA or BSTFA (Sigma, Poole, UK). The derivatised<br />
extracts were injected onto either gas-chromatograph HP5973 for GC-MSIEI and GC-MS/CI (Agilent, Berkshire,<br />
UK) or Varian Inc. Saturn for GC-MS/MS (Walton-on-Thames, UK) equipped with capillary column 15mxO.25<br />
mm Varian, Factor Four. The dynamic range was from 2 to 2000 ng/mL. Three ions for the drugs and two ions<br />
for the internal standards were monitored. The confirmation rate for each drug group, relative to applied cut-<strong>of</strong>f<br />
levels, is presented in Table I.<br />
.r--"<br />
Table 1. Total oral fluid sampl es teste db)y GC.MSt)oreachdrug ~oup and con fiIrmatlon rates.<br />
GCMS<br />
Confirmation Rate<br />
Drug Group N N %<br />
Amphetamines 337 305 (91%)<br />
Benzodiazepines 1027 823 (80%)<br />
Buprenorphine 175 104 (59%)<br />
Cannabis 632 316 (50%)<br />
Cocaine 1358 1026 (76%)<br />
1<br />
Methadone 1536 11437 (94%)<br />
Omates 116460 15189 (80%t I<br />
Percentiles: 50% (Median), 95% and maximum levels for all analytes in each drug group were calculated and<br />
will be presented. Detailed results for the Cocaine group <strong>of</strong> analytes are shown in Table 2.<br />
Table 2. Results showing Percentiles: 50% (Median), 95% and maximum levels in ng/mL for Cocaine group.<br />
Median 95% Maximum N<br />
AEME 62.0 1409.1 3458.9 75<br />
BenzoyJecgonine 49.1 566.0 5240.2 865<br />
Cocaethylene 12.3 101.4 136.7 33<br />
Cocaine 3004 2135.6 29613.4 843<br />
Oral fluid testing <strong>of</strong>fers a convenient, reliable and consistent method to determine the presence <strong>of</strong> poly-drug use<br />
and can identifY the presence <strong>of</strong> specific drug metabolites by the GC-MS methods established.<br />
Keywords: Drugs <strong>of</strong> Abuse, Oral Fluid, GC·MS<br />
Page 298
M16 <br />
VALIDA TION OF THE COZAR~<br />
AMPHETAMINES IN HAIR<br />
MICROPLATE ELISA FOR THE DETECTION OF<br />
Gail Cooper* and Chris Hand: Cozart Bioscience Ltd, Abingdon, Oxfordshire, OXI4 4RU<br />
The purpose <strong>of</strong> this study was to determine the performance characteristics <strong>of</strong> the Cozart® Amphetamine<br />
Microplate ELISA assay for the detection <strong>of</strong> amphetamines in hair samples. Hair samples (N=50) were<br />
collected from volunteers with a history <strong>of</strong> drug use and from drug related deaths. The hair samples were<br />
sonicated in methanol and then extracted overnight at 60°C. The methanol extract was evaporated to<br />
dryness and reconstituted in ELISA negative calibrator. 251lL <strong>of</strong> calibrator (0, 50, 100,200,300,500 and<br />
1000pg/mg), control and sample were assayed in duplicate according to manufacturers instructions for the<br />
Cozart@ Amphetamine ELISA - <strong>Forensic</strong> Application Kit.<br />
For GC-MS analysis, deuterated internal standards (amphetamine-d5, methamphetamine-d5, MDA-d5,<br />
MDMA-d5, MDEA-d6 and MBDB-d5) mixture, p-glucuronidase and O.lM, pH 6.0 phosphate buffer were<br />
added to approximately 20 mg <strong>of</strong> sample, or spiked blank hair and sonicated for I hour. Isolation <strong>of</strong><br />
amphetamine, methamphetamine, MDA, MDMA, MDEA and MBDB was achieved through simple solidphase<br />
extraction using Bond Elut certifY cartridges.<br />
The true positives (N=20), true negatives (N=30), false positives (N=O) and false negatives (N=O) for<br />
different cut-<strong>of</strong>fs with the ELISA were determined by comparison <strong>of</strong> the ELISA response (normalised to<br />
weight <strong>of</strong> hair extracted) to the GC-MS results as the reference method. Hair concentrations ranged from O.<br />
- 10.1 ng/mg (amphetamine), 0 - 0.8 ng/mg (MDA) and 0 17.4 ng/mg (MDMA).<br />
.r-~.<br />
The optimum cut-<strong>of</strong>f for the Cozart® Amphetamine Microplate ELISA was determined to be 500pg<br />
amphetamine equivalents/mg hair using a 20 mg hair sample with an overall precision <strong>of</strong> 100% vs GC-MS.<br />
Keywords: Amphetamines, Hair, ELISA<br />
Page 299
M17 <br />
CANNABINOID ANALYSIS OF ORAL FLUIDS COLLECTED FROM CLINICAL SUBJECTS<br />
FOLLOWING ORAL TETRAHYDROCANNABINOL (THC) ADMINISTRATION (HEMP OIL<br />
AND DRONABINOL)<br />
William D. Darwin l *, Richard A. Gustafson 2 , Jason Sklerov 3 , Dean Fritch 4 , Aaron Jacobs\ Kristen Blum 4 ,<br />
Sam Niedbala 4 , Eric T. Moolchan l , and Marilyn A. Huestis' : IChemistry and Drug Metabolism Section,<br />
IRP, NIDA, NIH, 5500 Nathan Shock Drive, Baltimore, MD 21224; 2Jacksonville Naval Air Station,<br />
Jacksonville, FL 32212; 3Armed Forces Institute <strong>of</strong> Pathology, Research Blvd., Rockville, MD 20850;<br />
40raSure Technologies, Inc., 150 Webster Street, Bethlehem, PA 18015<br />
Therapeutic usefulness <strong>of</strong> oral cannabinoids is being investigated to address analgesia, AIDS-wasting<br />
disease, counteracting spasticity <strong>of</strong> motor diseases, and emesis following chemotherapy. In addition,<br />
cannabis is among the most abused psychoactive substances. Following cannabis use, physiological and<br />
behavioral changes occur necessitating testing to detect impairment. In recent years, food products (hemp<br />
oil) derived from cannabis have been introduced into the U.S. Analysis <strong>of</strong> hemp oils reveals that THC is<br />
present in a wide concentration range. If these products produce positive drug test for urine and alternate<br />
matrices, screening programs to identify cannabis use may be affected. A clinical study to investigate the<br />
pharmacokinetics and pharmacodynamics <strong>of</strong> oral THC was performed. The randomized, double blind,<br />
placebo-controlled within-subject, inpatient study compared the effects <strong>of</strong> hemp oil in liquid and capsule<br />
form to dronabinol (synthetic THC) doses consistent with therapy for appetite-stimulation. Hemp oil<br />
dosing followed manufacturer's recommendations. Five dosing conditions (0.0, 0.39, 0.47, 7.5, and 14.8<br />
mg/day) <strong>of</strong> oil/capsules were administered three times daily with meals for five consecutive days. One<br />
objective was to determine if hemp oil could produce positive cannabinoid alternative matrices tests. Two<br />
devices were used to collect oral fluids, OraSure (OraSure Technologies) and Salivette (Sarstedt) from 90<br />
min after the first dose to 1 day after the last dose. Salivette samples were analyzed by LCIMS.<br />
LiquidlIiquid extractions isolated THCCOOH from ll-OH-THC and THC. Extraction efficiencies were<br />
280%. An LCIMSD (Agilent) with an Eclipse C18 column and electrospray interface with data acquired in<br />
the NCI mode was used for analysis. SIM ions monitored were: THCCOOH, mlz 343.2; d3-THCCOOH,<br />
mlz 346.2; 11-0H-THC, mlz 329.2; d3-11-0H-THC, mlz 332.2; THC, m/z 313.2; and d3-THC m/z 316.2.<br />
Limits <strong>of</strong> quantitation (LOQ) were 1.0, 0.5, and 0.5 ng/mL and limits <strong>of</strong> detection (LOD) 0.5, 0.2, and 0.2<br />
ngimL for THCCOOH, ll-OH-THC, and THC, respectively. 511 Salivettes from 7 subjects were<br />
analyzed. OraSure oral fluid specimens were analyzed according to manufacturer's specifications with<br />
Cannabinoids InterceptTM MICRO-PLATE Enzyme Immunoassay (OraSure Technologies) with a 12<br />
ngimL cut<strong>of</strong>f and confirmed by GC/MS/MS. After SPE, extracts were derivatized with HFPA/PFIP.<br />
Extraction efficiency was 50%. THC was analyzed on a Saturn Ion Trap Quadrupole (Varian) equipped<br />
with a 5% phenyl-methyl column. Ions monitored were: THC, mlz 492 and d3-THC, mlz 495 (parent<br />
ions); THC, m/z 238 and d3-THC, m/z 238 (product ions). LODILOQ for THC were 0.75 ngimL. 497<br />
OraSures from 8 subjects were analyzed. All Salivette and OraSure oral fluid specimens were negative at<br />
the specified cut<strong>of</strong>fs. In contrast, several authors reported cannabinoid positive results for Salivette and<br />
OraSure oral fluid samples after smoked THC (Samyn, J <strong>Forensic</strong> Sci, 2002, 47: 1380; Niedbala, JAT,<br />
2001,75:289). In addition, Niedbala found positive tests for OraSure oral fluid samples collected after oral<br />
THC (20-25 mg THC-laced brownie), but concentrations were low ('5.7 ngimL). THC is well absorbed, but<br />
has low bioavailability «20%) via the oral route. There is evidence that deposition <strong>of</strong>THC into oral fluid<br />
is via direct sequestering into oral mucosa during drug use with minimal contribution from blood to oral<br />
fluid (Hawks, The Cannabinoids, Academic Press, 1983, 8). Characterization <strong>of</strong> rates <strong>of</strong> absorption and<br />
elimination <strong>of</strong> orally administered THC with different vehicles (flax oil, sesame seed oil, cookies/brownies,<br />
and emulsions) and with direct administration and encapsulation have shown variable absorption <strong>of</strong>THC.<br />
Little data have been published about oral fluid drug levels after oral THC administration; questions remain<br />
including the degree <strong>of</strong> absorption inherent to the collection devices and THC contamination <strong>of</strong> the oral<br />
cavity immediately following hemp oil/capsule administration. The fact that all oral fluid specimens<br />
collected were negative with two different devices for THC-containing hemp oils and capsules suggests<br />
little contamination <strong>of</strong> the oral fluid following ingestion <strong>of</strong> dronabinol or hemp oils by the time the first<br />
specimen was collected, at least by 90 minutes after dosing.<br />
Keywords: OraSure, Salivette, Oral Administration <strong>of</strong>THC<br />
/--.'~<br />
Page 300
MI8 <br />
COMPARISON OF ALCOHOL CONCENTRATIONS IN POSTMORTEM BODY FLUIDS<br />
Bruno Spinosa De Martinis*, Adriano Braga, Henrique Turin Moreira, Carolina Melo Candido de Paula<br />
and Carmen Cinira Santos Martin: Department <strong>of</strong> Pathology, Center <strong>of</strong> Legal Medicine, Faculty <strong>of</strong><br />
Medicine <strong>of</strong> Ribeir1io Preto, University <strong>of</strong>S1io Paulo. Rua Tenente Camo Roxo 2418, Ribeirao Preto, Sao<br />
Paulo, 14051-140, Brazil<br />
The determination <strong>of</strong> postmortem ethanol is probably one <strong>of</strong> the most important and frequently requested<br />
analyses in forensic toxicology. Because <strong>of</strong> its hydrophilic characteristics, ethanol distributes with body<br />
water and studies have demonstrated the existence <strong>of</strong> substantial site dependence. Factors such as quality<br />
and sampling site; trauma to the body; length <strong>of</strong> time between death and sampling; presence <strong>of</strong><br />
microorganisms in the body; diffusion <strong>of</strong> alcoholic beverages present in the stomach into the pericardial<br />
fluid; diffusion <strong>of</strong> ethanol in aspirated vomitus into cardiac blood; blood contamination and unavailability<br />
<strong>of</strong> blood samples must be considered to interpret the postmortem blood ethanol concentration. Due those<br />
factors, there is an enormous effort to find alternative sampling sites and correlations between blood<br />
alcohol concentration and other biological fluids to establish different procedures for specimens to sample<br />
for alcohol analysis.<br />
In addition, considering the medicolegal purposes, the implications <strong>of</strong> postmortem alcohol concentrations<br />
are extremely important, especially when they are found to be above the legal level for intoxication at one<br />
specimen and below that level at another.<br />
The use <strong>of</strong> vitreous humor as an alternative specimen for ethanol analysis in postmortem cases has<br />
increased, because it is stable, readily available, easily sampled and less susceptible to bacterial<br />
contamination.<br />
In this work it was determinated the ethanol concentrations in biologic fluids, collected during the autopsy<br />
examination from 103 cadavers victims <strong>of</strong> different cause <strong>of</strong> death, to establish a correlation between the<br />
concentrations <strong>of</strong> ethanol in vitreous humor with urine and blood specimens, sampled from femoral,<br />
subclavian and heart.<br />
Determinations <strong>of</strong> ethanol in the specimens were performed using capillary gas chromatographylflame<br />
ionization detector and headspace techniques.<br />
Statistical analysis <strong>of</strong>the results indicated that there were no significant differences among urine and blood<br />
samples, collected in different sites, with vitreous humor.<br />
Comparing the vitreous humor ethanol concentration with respect to Pearson's correlation test, it was found<br />
0.97 for femoral blood and urine, 0.96 for heart blood, 0.94 for subclavian blood. These results demonstrate<br />
that all the fluids tested with vitreous humor were significantly correlated with "p" (associated probability<br />
for the used correlation tests) being always lower than 0,05. It indicates that vitreous humor can be use as<br />
an alternative sample for urine and blood.<br />
Keywords: Postmortem Specimens, Multisite Sampling, Ethanol.<br />
Page 301
M19 <br />
METHOD DEVELOPMENT OF MICROWAVE-ASSISTED EXTRACTION AND<br />
SUPERCRITICAL FLUID EXTRACTION OF SOME PERSISTENT ORGANIC POLLUTANTS<br />
IN HUMAN SEBUM<br />
Diaz-Vazquez, Liz M.*; Garcia, Oscar; Madero, Mayraliz; Velazquez, Zorangelys; and Rosario, Osvaldo,<br />
Department <strong>of</strong> Chemistry, University <strong>of</strong>Puerto Rico, Rio Piedras Campus, P.O. Box 23346, San Juan, P.R.,<br />
00931-3346<br />
Sebum has been used to monitor use <strong>of</strong> controlled drugs as well as exposure to dioxins. Based on this, it is<br />
logical to extrapolate its use to also monitor exposure to other environmental pollutants. Methodology is<br />
being pursued which will allow the analysis <strong>of</strong> persistent organic pollutants (POPs) through sebum testing.<br />
Statistical Analysis methods based on Minitab® s<strong>of</strong>tware were applied to optimize microwave-assisted<br />
extraction (MAE) and supercritical fluid extraction (SFE) conditions for the analysis <strong>of</strong> some standards<br />
representative <strong>of</strong> POPs. For practical purpose a model matrix <strong>of</strong> synthetic sebum spiked with the following<br />
standards: 1,4- benzodioxan, 1,2,4, 5- tetrachlorobenzene, aldrin, dursban and pyrene was used for the<br />
optimization <strong>of</strong> the extraction techniques. A stock solution <strong>of</strong> the model matrix was prepared as follow:<br />
synthetic sebum was dissolved in dichloromethane and the standards <strong>of</strong> interest were spiked into the<br />
solution. An aliquot 31lL <strong>of</strong> the spiked sebum solution was taken, deposited on the sebutape® and the<br />
solvent allowed to evaporate. The final concentration <strong>of</strong> the standards, if a 100 % recovery was obtained,<br />
was 3 ppm. The Recoveries <strong>of</strong> analytes were followed using GC-MS. All compounds were successfully<br />
extracted from sebum with recoveries ranging from 69 for 1,4 -benzodioxan to 91 % for dursban under the<br />
optimum MAE conditions: 5 mL acetonitrile, 70°C extraction temperature, and 10 min microwave heating.<br />
The average recoveries in SFE ranging from 84 for 1,4-benzodioxan to 95 % for pyrene under the<br />
following conditions: 30 min <strong>of</strong> extraction at 40°C, under CO 2 at 4000psi modified with 20% (v/v)<br />
methanol. The addition <strong>of</strong> a small volume (10-20 %) <strong>of</strong> methanol to the extraction cell enhanced the<br />
recoveries <strong>of</strong> representative persistent organic pollutants. A comparison <strong>of</strong> MAE, SFE was also conducted.<br />
The results indicated that ~ 69 % average recoveries were obtained by both optimized techniques. Good<br />
precision with RSD less than 10% was attained for most <strong>of</strong> the standards with both techniques. Although<br />
with SFE higher percents <strong>of</strong> recoveries were obtained, it also is more efficient extracting the components <strong>of</strong><br />
the sebum like saturated hydrocarbons and fatty acids than MAE. In addition to further optimizing our SFE<br />
approach, both MAE and SFE are now being compared with ultrasonic extraction commonly used for the<br />
extraction <strong>of</strong> biological matrices. Solid phase extraction, with different stationary phases, was used to<br />
remove sebum components from the extract. Also SPME was tested to improve the detection limits. Real<br />
samples <strong>of</strong> human sebum are being analyzed from an area impacted by the emission from an incinerator <strong>of</strong><br />
biomedical wastes. The compounds found in these persons will be compared to compounds found in air<br />
samples from the same region. This will show if specific air pollutants are being incorporated by this<br />
population. Once completed and validated this noninvasive approach will provide a powerful method for<br />
monitoring exogenous compounds in human.<br />
Keywords: Microwave-Assisted Extraction, Supercritical Fluid Extraction, Sebum<br />
Page 302
M20 <br />
DRUG-FACILITATED CRIMES - INTEREST OF TANDEM MASS SPECTROMETRY AND<br />
HAIR ANALYSIS - STATISTICS OF DRUGS IMPLICATED DURING A YEAR OF WORK AT<br />
TOXLAB<br />
Duffort G.*, Cheze M., Pepin G. <br />
TOXLAB Laboratory, 7 rue Jacques Cartier -75018 Paris - FRANCE <br />
AIMS: Drug-facilitated crimes cases are <strong>of</strong>ten difficult to resolve, from an analytical point <strong>of</strong> view, since<br />
the drugs administered, largely benzodiazepines or hypnotics, are generally given as one therapeutic dose,<br />
and most <strong>of</strong>ten have a short half-life elimination. In France, for these kind <strong>of</strong> aggression cases, the police<br />
directs the victim towards a hospital or, in big cities, to an emergency forensic service <strong>of</strong>fice. Ifnecessary,<br />
after the clinical exam, blood and sometimes urine samples are taken. Using HPLCIDAD and/or GCIMS,<br />
immunochemical as well as toxicological screenings are performed on these samples. The immunochemical<br />
techniques constantly produce negative results. HPLCIDAD and GCIMS do not permit most basic<br />
molecules used in drug-facilitated crimes to appear because the aggression reports, and then the samples,<br />
are <strong>of</strong>ten late and thus substances are undetectable with those techniques. This is why we have developed<br />
an HPLC-MSIMS method for the benzodiazepines and hypnotics determination in biological fluids and<br />
hair. By that way, we can reach the detection limits <strong>of</strong> the nglmL order in biological fluids and <strong>of</strong> the<br />
pglmg order in hair. Human hair is sampled by us, about one month after the exposure. The sequential hair<br />
analysis by LC-MSIMS allows to affirm that the identified molecules in blood and/or in urine were in fact<br />
from an isolated single dose and not from a medical treatment, so it brings evidence for drug-facilitated<br />
crimes.<br />
METHODS: The detection <strong>of</strong> main benzodiazepines in biological fluids were performed by LC-MS/MS<br />
after an extraction <strong>of</strong> I mL with Toxitube A ® (Varian). Hair was segmented, decontaminated, cut, then 20<br />
mg were extracted with deuterated standard, whether one night incubation in ImL Soerensen buffer (PH<br />
7.6), or whether, for aminometabolites, at 95° for 15 minutes in NaOH O,IN. A liquid-liquid extraction was<br />
performed with dichloromethane/ether (80/20). The organic phase was filtered before being evaporated.<br />
The dry extract was reconstituted by 60JlL <strong>of</strong> ACNlMeOH (50/50) and injected into the LC-MS/MS<br />
(ThermoElectron). The liquid chromatography was carried out on an Uptisphere ODB C18 51-! 150 x 2mm<br />
column (Interchim) with a gradient <strong>of</strong> acetonitrile and formate 2mM pH3 buffer. The run was 15 minutes<br />
long. The mass tandem TSQ Quantum detection allowed the simultaneous determination <strong>of</strong> 27<br />
benzodiazepines in SRM mode with two runs.<br />
RESULTS: The detection limits reached by these techniques, are in the order or inferior to 0.5 nglmL in<br />
urine and about 1 pglmg in hair for the 27 benzodiazepines studied. We present two cases <strong>of</strong> drug-facilitated<br />
crimes in which cIonazepam and flunitrazepam were found in blood and urine samples. In these two cases,<br />
a single dose <strong>of</strong> these molecules appeared on the specific segment <strong>of</strong> hair corresponding to the period <strong>of</strong> the<br />
<strong>of</strong>fense. From June 2003 to May <strong>2004</strong> we treated 90 cases <strong>of</strong> presumed drug-facilitated crimes, for which<br />
we had urine and/or hair samples. In 35.5% <strong>of</strong>these cases, the benzodiazepines or hypnotics were detected.<br />
Among these, a single dose, taken without someone's knowledge, appeared in 65.5%. In the 90 cases,<br />
35.5% <strong>of</strong> the victims were vulnerable following an alcohol and/or illegal drugs consumption; in 22.2% the<br />
investigation showed that it was not a drug-facilitated crimes and 6.7% were not able to be solved.<br />
CONCLUSIONS: This technique produces an analytical response that is essential to police and justice<br />
authorities. It brings out criminal acts and produces the scientific pro<strong>of</strong> <strong>of</strong> drug-facilitated crimes with<br />
benzodiazepines and hypnotics as shown by our statistics and the two specific cases cited.<br />
Keywords: Benzodiazepines, LC/MS/MS, Hair Analysis<br />
Page 303
M21 <br />
IMPROVED GCMS ANALYSIS OF THC IN SALIVA<br />
Charles R. Lyle, Matthew P. Clabaugh, F. Roark Galloway*: Shimadzu Scientific Instruments, Columbia,<br />
MD; Nadina Giorgi: Redwood Toxicology Laboratory, Santa Rosa, CA<br />
One <strong>of</strong>the most challenging GCMS applications is the determination <strong>of</strong>THC in saliva. Detection for THC<br />
at low ppb [nglml] levels is required due to several factors including; I) rapid elimination <strong>of</strong>THC in saliva<br />
from time <strong>of</strong> exposure, 2) low amount <strong>of</strong> drug for 'active' dose and 3) small sample volume available at<br />
time <strong>of</strong> collection. This application demonstrates an example <strong>of</strong> how the Shimadzu GCMS QP-2010 can<br />
provide the instrument performance necessary to complete this challenging analysis. Samples were<br />
collected using the Quantisal saliva collection kit. Extractions are performed by extraction with<br />
hexane:ethyl acetate [9:1] with 3 % acetic acid. Derivatization is completed using 50 uL BSTFA to form<br />
the trimethylsilane derivative. 1.0 uL <strong>of</strong> sample extract is injected for analysis. Using the standard SPL<br />
2010 split/splitless injection port on the GC-2010 as a high pressure injector, the method was performed<br />
with a splitless injection using a Restek 3.4mm. id. SIL TEK liner. With high-pressure injection <strong>of</strong> 175 kPa,<br />
fast temperature ramping <strong>of</strong>35 C/min and high column flow rate, the peaks eluted from the column into the<br />
mass spectrometer ion source in less than 3.00 minutes. These results were obtained using a 15m X<br />
0.25mm X .25 urn phase DB-IMS column. Calibration from 1.0 25 ppb THC produced a linearity<br />
coefficient <strong>of</strong> 0.9999 by internal standard calculation using THC-D3 at 12.5 ppb. Preliminary LOQ is<br />
determined to be 0.25 ppb. Precision at 3.0 ppb THC is 5.97%.<br />
1.0 ppb THC [TMS] Standard Calibration, 1.0 - 25 ppb THC<br />
AnaR.tliu<br />
2.<br />
,.<br />
y2 = 0.99986<br />
Keywords: THC, Saliva, GCMS<br />
Page 304
M22 <br />
SIMULTANEOUS ASSAY FOR NICOTINE AND ITS METABOLITES IN ORAL FLUID BY SPE<br />
AND GCIMS/EI.<br />
Insook Kim*, William D. Darwin, and Marilyn A. Huestis: Chemistry and Drug Metabolism Section, IRP,<br />
NIDA, NIH, 5500 Nathan Shock Drive, Baltimore, MD 21224<br />
Nicotine, the major alkaloid in tobacco, is rapidly and extensively metabolized in humans, but its<br />
metabolism varies among individuals. Nicotine is primarily metabolized by cytochrome P450 (CYP2A6) to<br />
cotinine, which is subsequently hydroxylated to trans-3'-hydroxycotinine. This method was designed to<br />
simultaneous quantifY nicotine, cotinine, norcotinine, and trans-3'-hydroxycotinine in human oral fluid, a<br />
noninvasive biological matrix. An aliquot (0.5 mL) <strong>of</strong> each oral fluid sample, quality control (QC) sample,<br />
or calibration standard was mixed with 2 mL <strong>of</strong> 2M sodium acetate buffer (pH 5.5). Deuterated internal<br />
standards (d)-nicotine, d)-cotinine, and d)- trans-3'-hydroxycotinine) were added to each sample. Solid<br />
phase extraction (SPE) columns (200 mg Clean Screen® ZSDAU020, United Chemical Technologies,<br />
Bristol, PA) were preconditioned with elution solvent, methanol, water, and buffer. Each sample was<br />
loaded onto the SPE column and washed with water, 0.2 N HCI, and methanol. Analytes were eluted with<br />
methylene chloride: 2-propanol: ammonium hydroxide (80:20:2 v/v/v), and 100 J.lL <strong>of</strong> 1% hydrochloric<br />
acid in methanol (v/v) was added prior to evaporation. Extracts were evaporated to dryness under a stream<br />
<strong>of</strong> nitrogen at 40°C using a Zymark Turbovap LV Evaporator. Extracted residues were reconstituted in<br />
acetonitrile, derivatized with BSTF A (with 1 % TMCS), and analyzed by GCIMSIEI in the selected ion<br />
monitoring (SIM) mode. GCIMS analysis was performed using an HP6890 gas chromatograph interfaced<br />
with HP5973 mass-selective detector, equipped with HP-5MS column (30m x 0.25mm Ld.; 0.25J.1m-fiIm<br />
thickness) with helium gas at 1.0 mLlmin. The instrument was operated in the splitless mode. The initial<br />
column temperature <strong>of</strong> 70°C was held for 1 min, followed by increases to 190°C at 30°C/min, to 230°C at<br />
5°C/min, to 290°C at 25°C/min. The ions for each analyte were monitored in the following elution order<br />
(quantitative ions are indicated in parenthesis) for the derivatized analytes: d)-nicotine, mlz (87), 165;<br />
nicotine, m/z (84), 162; d)-cotinine, mlz (101), 179; cotinine, m/z (98), 176; norcotinine, m/z (234), 219;<br />
d 3<br />
-trans-3'-hydroxycotinine, mlz (252), 147; and trans-3'-hydroxycotinine, mlz (249), 144. The base peak<br />
and molecular ions <strong>of</strong> each analyte and internal standards were evaluated by SIM analysis. However, the EI<br />
spectra <strong>of</strong> these drugs do not possess many fragments that can be used as confirming ions. The mid-mass<br />
range ions for these drugs contain non-specific interferences probably from co-extracted endogenous<br />
material. For this reason, only two ions, the base peak and the molecular ion, were monitored in this assay.<br />
Eight point calibration curves for nicotine, cotinine, norcotinine, and trans-3'-hydroxycotinine were linear<br />
across a concentration range <strong>of</strong> 2.5 to 500 ng for all compounds/0.5 mL <strong>of</strong> blank oral fluid. Correlation<br />
coefficients <strong>of</strong> the calibration curves were >0.99. The limits <strong>of</strong> determination and quantitation are 2.5<br />
ng/0.5 mL (50 pg on column) for all analytes. Recovery was 90 - Il5% for nicotine, 76 - Il7% for<br />
cotinine, 88 -101% for norcotinine, and 66 -77% for trans-3'-hydroxycotinine at 8, 80, and 400 ng/O.5 mL<br />
(low, mid, and high, respectively), QC sample concentrations. Intra-assay precision (% CV) and accuracy<br />
(percent difference between mean and target concentrations) ranged from 1.6 5.7 and 1.6 - 17.8%,<br />
respectively, at low, mid, and high QC sample concentrations for all analytes. Inter-assay precision and<br />
accuracy for low, mid, and high QC sample concentrations ranged from 4.4 - 8.8 and 0.2 - 12.6%,<br />
respectively, for all analytes. Suitable precision and accuracy were achieved for the simultaneous<br />
determination <strong>of</strong> nicotine and three metabolites in the oral fluid <strong>of</strong> smokers. This assay is applicable to<br />
pharmacokinetic studies <strong>of</strong> nicotine and its metabolites in oral fluid and provides a biomarker for<br />
identification <strong>of</strong> smoking, which could be helpful in smoking cessation programs.<br />
Keywords: Nicotine, Nicotine Metabolites, Oral Fluid<br />
Page 305
M23 <br />
~9-TETRAHYDROCANNABINOL (THC), 11-HYDROXy-~9-TETRAHYDROCANNABlNOL (11<br />
OH-THC) AND 11-NOR-9-CARBOXy-~9-TETRAHYDROCANNABINOL (THCCOOH) IN<br />
HUMAN PLASMA FOLLOWING ORAL ADMINISTRATION OF HEMP OIL.<br />
Wesenyalsh Nebro'*, Allan Barnes', Richard A. Gustafson 2 , Eric T. Moolchan l and Marilyn A. Huestis l : '<br />
Chemistry and Drug Metabolism Section, IRP, NIDA, NIH, 5500 Nathan Shock Drive, Baltimore, MD<br />
21224; 2 Jacksonville Naval Air Station, Jacksonville, FL 32212<br />
Usefulness <strong>of</strong> therapeutic oral cannabinoids is being investigated for several medicinal applications.<br />
Cannabis is among the most abused psychoactive substances causing behavioral and physiological changes<br />
that necessitate testing to detect impairment. In recent years, hemp oil products derived from cannabis<br />
have been introduced into the U.S. Analysis <strong>of</strong> hemp oils reveals that THC is present in a range <strong>of</strong><br />
concentrations. A clinical study to investigate the pharmacokinetics and pharmacodynamics <strong>of</strong> oral THC<br />
was performed. The randomized, double blind, placebo-controlled within-subject, inpatient study<br />
compared the effects <strong>of</strong> hemp oil in liquid and capsule form to dronabinol (synthetic THC) doses consistent<br />
with therapy for appetite-stimulation. The NIDA IRB approved this study and each participant provided<br />
informed consent. One aspect <strong>of</strong> this study was to determine the detection times and levels <strong>of</strong>THC, 11-0H<br />
THC and THCCOOH in plasma following oral THC administration. Hemp oil dosing followed<br />
manufacturer's recommendations. Five healthy volunteers with a history <strong>of</strong> marijuana abuse ingested<br />
commercially available hemp oils/capsules <strong>of</strong> differing THC concentrations. Five dosing conditions (0.0,<br />
0.39,0.47,7.5, and 14.8 mg/day) <strong>of</strong> oil/capsules were administered three times daily with meals for five<br />
consecutive days followed by a ten-day washout period before the next dosing session began. Plasma<br />
samples were collected prior to and following each <strong>of</strong> the five dosing conditions throughout the study and<br />
were frozen at -20°C until analysis. Plasma was extracted by SPE (200 mg Clean Screen® ZSDAU020,<br />
United Chemical Technologies). The extracts were derivatized with BSTFA (l%TMCS), separated and<br />
quantified on a GCIMS(Agilent) operated in the positive chemical ionization mode with SIM monitoring.<br />
The following table lists the mean minimum and maximum concentrations (ng/mL) for all plasmas<br />
collected from 30 minutes before the first dose to 2 days after the last dose for each session for five<br />
subjects:<br />
THC ll-OH-THC THCCOOH<br />
Session Dose Amount Min Max Min Max Min Max<br />
~gh Potency Hemp Oil 14.8 mg/day 0.0 6.5 0.0 5.6 0.0 15.2<br />
Dronabinol Capsules 7.5 mg/day 0.0 3.6 0.0 2.6 0.0 24.4<br />
~emp Oil Capsules 0.47 mg/day 0.0 0.0 0.0 0.0 0.0 2.5<br />
Low Potency Hemp Oil 0.39 mg/day 0.0 1.2 0.0 3.8 0.0 3.1<br />
Placebo__ ~_ c.JJ.0 mg/day 0.0 ~~ 0.0 0.0 0.0 0.0<br />
~-<br />
Drug levels <strong>of</strong> plasmas varied within the same dose between subjects. In general, the THC, 11-0H-THC,<br />
and THCCOOH levels were low and erratic across the collection timeline after all doses. The peak<br />
concentrations and time to peak concentrations varied, sometimes considerably, between subjects. In<br />
general, the maximum concentrations <strong>of</strong> 1I-0H-THC were seen in the liquid hemp oil sessions. The<br />
sessions in which capsules were administered had lower concentrations, less than the low dose <strong>of</strong> hemp oil<br />
administered, or zero concentrations. Plasma THC and 11-0H-THC were negative for all participants and<br />
for all doses by 16 hours after the last THC dose. Plasma THCCOOH persisted for a longer period <strong>of</strong>time<br />
following the two highest doses <strong>of</strong> 7.5 mg/day dronabinol and 14.8 mg/day THC in hemp oil. Ohlsson et<br />
al. (Clin. Pharmacol. Ther., 1980, 28:409) reported that orally administered (20 mg cookie) THC yielded<br />
low and irregular plasma concentrations compared to intravenous and inhaled THC. Bioavailability <strong>of</strong><br />
orally administered THC is low. This may be due to poor absorption, degradation by stomach acid, or<br />
biotransformation to metabolites via first pass through the liver.<br />
Keywords: Oral Administration <strong>of</strong>THC, Plasma, GCIMS.<br />
Page 306
M24 <br />
A MICROTITER PLATE ELISA PLATFORM FOR SCREENING ABUSE DRUGS IN ORAL FLUID<br />
Thomas Kupiec*, Lacinda DeCicco, Susan Bernard, Nicole Vu' Analytical Research Laboratories, Oklahoma<br />
City, OK.<br />
The purpose <strong>of</strong> this study was to evaluate the suitability <strong>of</strong> microtiter plate ELISA assays (Neogen Corp) for<br />
screening <strong>of</strong> abuse drugs in oral fluid (OF), and the efficiency <strong>of</strong> drug recovery from a oral sampling device,<br />
Sarstedt Salivette®. The following drugs were tested at the proposed cut<strong>of</strong>f levels for the respective compound<br />
according to the Federal Workplace Drug Testing Program draft guidelines: cocaine, morphine, 6<br />
monoacetylmorphine (6-MAM), d-amphetamine, d-methamphetamine, and methylenedioxymethamphetamine<br />
(MDMA) and methylenedioxyamphetamine (MDA). Twenty, non-smoking, drug-free donors by testimony spit<br />
approximately 25 mL OF into a clean cup and the sample was then poured away from the froth and centrifuged.<br />
All OF samples were confirmed negative by GCIMS for all <strong>of</strong> the tested analytes. The samples were then pooled<br />
to create a blank OF matrix pool used in all assays. The OF pool portions were spiked with the above analytes at<br />
the proposed cut<strong>of</strong>f levels for the respective compound. Next, spiked or blank OF was collected from a cup<br />
using an oral sampling device. The collector pad was held with tweezers and immersed in the cups <strong>of</strong> OF and<br />
then processed according to the manufacturer's protocol. OF samples <strong>of</strong> 20~L were analyzed alongside a<br />
standard curve by ELISA to determine the dilution factor needed to bring the %BlBo <strong>of</strong> each drug in OF at the<br />
standard proposed industry cut<strong>of</strong>f levels into the optimal range for the ELISA. The calibration curve was<br />
established by plotting log concentration VS logit transformation <strong>of</strong> the absorbance ratio for each calibrator and<br />
the blank sample (%BlB o ). The concentrations <strong>of</strong> the analyte in the test samples were then determined from the<br />
calibration curve based on their absorbance ratios, BlB n . The percentage <strong>of</strong> drug recovery from the oral<br />
sampling device was calculated by comparing the concentration <strong>of</strong> the processed sample using the device to the<br />
non-processed sample concentration. The amount <strong>of</strong> drug detected by the ELISA when no collection device was<br />
utilized was determined by Observed/Experimental x 100. The intra-assay precision was evaluated based on the<br />
mean absorbance ratio BlBo <strong>of</strong> the 16 replicate analyses <strong>of</strong> blank samples that were used in LOD determination.<br />
These results are summarized in Table I. The results indicated that this ELISA platform is suitable for the<br />
analysis <strong>of</strong> the following drugs in OF: cocaine, morphine, 6-MAM, d-amphetamine, d-methamphetamine, and<br />
MDMA.<br />
Table 1<br />
I<br />
!<br />
I<br />
Drug<br />
i Dilution <strong>of</strong><br />
. OF<br />
I<br />
Drug Conc.<br />
.<br />
inOF<br />
(ng/mL)<br />
I<br />
i<br />
1<br />
Amount Recovered<br />
<strong>of</strong> OF<br />
(ng/mL)<br />
No Collector<br />
Collector<br />
Intra-assay<br />
Precision <strong>of</strong><br />
BlBo<br />
!<br />
i Cocaine I: 50<br />
Amphetamine I: 5 i<br />
5<br />
20<br />
25<br />
50<br />
i<br />
4.76±0.15<br />
24.01±1.90<br />
! 17.86±2.56<br />
!<br />
40.86±3.85<br />
2.07±0.32<br />
14.96±2.47<br />
13.84±0.55<br />
36.55±1.94<br />
3.863<br />
3.863<br />
I<br />
I MDA<br />
No dil.<br />
I Methamphetamine 1: 5<br />
MDMA I: 5<br />
Morphine I: 50<br />
I<br />
i 6-MAM I: 5<br />
I<br />
I<br />
I<br />
I<br />
I<br />
50<br />
100<br />
25<br />
50<br />
25<br />
50<br />
20<br />
40<br />
2<br />
4<br />
10.42±2.58<br />
23.58±23.52<br />
36.37±2.56<br />
56.32±3.20<br />
30.26±6.45<br />
50.07±5.78<br />
I9.62±5.71<br />
42.36±0.96<br />
3.13±0.77<br />
5.67±0.72<br />
56.24±8.96<br />
63.19±16.74<br />
36.30±IO.l8<br />
58.42±2.12<br />
10.581<br />
2.755<br />
22.53±7.5<br />
44.08±6.64 I<br />
8.316<br />
15.18±4.43<br />
32.79±7.43<br />
2.43±0.19<br />
5.56±L25<br />
I<br />
I<br />
I 3.798 i<br />
I<br />
i<br />
4.564<br />
!<br />
I<br />
Keywords: ELISA, Oral Fluid, Drugs <strong>of</strong> Abuse<br />
Page 307
M25 <br />
,---<br />
LIQUID CHROMATOGRAPHY -ELECTROSPRA Y IONIZATION MASS SPECTROMETRY<br />
FOR THE DETERMINAnON OF SELECTED BENZODIAZEPINES<br />
O.Quintela*, A. Cruz, A. de Castro M. Concheiro and M.L6pez-Rivadulla. <br />
<strong>Forensic</strong> Toxicology Service. Institute <strong>of</strong> Legal Medicine. University <strong>of</strong> Santiago de Compostela. SPAIN <br />
A simple, rapid, and sensitive method based on the use <strong>of</strong> liquid chromatography-eJectrospray ionizationmass<br />
spectrometry (LC-ESI-MS), which allows the simultaneous determination <strong>of</strong> nine Benzodiazepines<br />
(Midazolam, Bromazepam, Tetrazepam, Alprazolam, Lorazepam, Triazolam, Diazepam, Flunitrazepam<br />
and Lormetazepam) was developed. The method was applied to plasma and saliva samples. The collection<br />
<strong>of</strong> saliva samples were done with the Salivette®device. Lorazepam-d4, Diazepam-d5, and Alprazolam-d5<br />
were used as internal standards.<br />
The separation <strong>of</strong> the nine benzodiazepines was performed by using acetonitrile/O.l% formic acid in<br />
gradient mode as a mobile phase, on a XTerra RP18 5 J.lm (l50x 2.1mm I.D.) reverse phase column. The<br />
liquid-liquid extraction procedure <strong>of</strong> the compounds and their respective internal standards was carried out<br />
with diethyl ether. The quantification study was done by operating in selected ion monitoring (SIM) mode,<br />
and two mlz ratios for each compound were chosen. The method was validated for both biological samples.<br />
LOD LOQ Selected<br />
Plasma Saliva Plasma Saliva mlz ratios 8<br />
Midazolam 0.5 0.1 0.2 326.1<br />
291.3<br />
Bromazepam 0.2 5 0.5 318.0<br />
290.0<br />
Tetrazepam 0.5 0.1 0.2 289.2<br />
261.3<br />
Alprazolam 0.5 0.2 0.5 309.1<br />
281.2<br />
Lorazepam 0.5 0.2 0.5 321.0<br />
303.1<br />
Triazolam 0.5 0.1 2 0.2 343.1<br />
308.1<br />
Flunitrazepam 0.5 0.1 0.2 314.2<br />
268.2<br />
Diazepam 0.5 0.1 0.2 285.3<br />
257.2<br />
Lormetazepam 0.5 0.1 0.2 335.0<br />
289.0<br />
Lorazepam-d 4<br />
Alprazolam-ds<br />
Diazepam-ds<br />
N.D. b<br />
N.D. b<br />
N.D. b<br />
N.D. b<br />
N.D.b<br />
N.D. b<br />
N.D. b<br />
N.D.b<br />
N.D.b<br />
325.1<br />
N.D. b<br />
N.D. b 290.3<br />
N.D. b 314.2<br />
"Quantifying ions are in bold characters<br />
~.D.==Not Detected<br />
In addition, a preliminary pharmacokinetic study for two <strong>of</strong> the nine Benzodiazepines (Midazolam and<br />
Lormetazepam) was carried out in order to check the possible saliva and plasma levels correlations.<br />
Keywords: Benzodiazepines, Plasma and Saliva, LC-ESI-MS<br />
Page 308
M26 <br />
DETECTION OF SMOKED COCAINE MARKER (ANHYDROECGONINE METHYLESTER) IN<br />
NAILS.<br />
Catherine Ragoucy-Sengler l * and Pascal Kintz 2 : lLaboratoire de Biochimie, Centre Hospitalier<br />
Universitaire BP 465 97110 Abymes, Guadeloupe (FWI) and 21nstitut de Medecine Legale, 11 rue Human<br />
67085 Strasbourg France<br />
Objective: The chronic intoxication by smoked cocaine or crack results in psychic disturbances that may<br />
lead to asocial and aggressive behavior. For medical, legal and epidemiologic purpose it is interesting to be<br />
able to detect this drug-addiction. The detection <strong>of</strong> anhydroecgonine methy ester (AEME) marker <strong>of</strong><br />
coca'ine pyrolysis in hair is significant <strong>of</strong>chronic consumption. The collection <strong>of</strong>hair is not always possible<br />
among Afro-Americans, and that <strong>of</strong> the nails can represent an interesting alternative to search AEME.<br />
Materials and methods: Two samples <strong>of</strong> 50 mg <strong>of</strong> nails collected with informed consent from two subjects<br />
consuming smoked cocaine were analyzed by gas chromatography coupled to mass spectrometry detection.<br />
The AEME was searched in these samples.<br />
Prior to analysis, the samples were washed with hot water then by 5 baths <strong>of</strong> dichloromethane in order to<br />
eliminate any possibility <strong>of</strong> contamination by the contact with the product or the smoke before being<br />
analyzed. The analysis was carried out in mode SIM on a Gaz Chromatograph (6890) coupled to a mass<br />
selective detector (5973) Agilent Technologies, (Palo Alto, CA) (1). AEME was quantitated by comparing<br />
ratios <strong>of</strong> peak areas with those <strong>of</strong>deuterated cocaine.<br />
Results: The analysis <strong>of</strong> the nails samples <strong>of</strong> both subjects (1 and 2) leads to detection <strong>of</strong> cocaine, its<br />
metabolites and the AEME. The analysis <strong>of</strong> dichloromethane baths were negative from the 3 me bath.<br />
ng/mg COC BE EME CE AEME<br />
Subject 1 28.7 7.3 6.3
M27 <br />
DETERMINA TION OF THC IN ORAL FLUID SAMPLES USING LC-MS<br />
Manuel Rivadulla*, Oscar Quintela, Marta Concheiro, Ana Rios, and Angelines Cruz.: <strong>Forensic</strong><br />
Toxicology Service, Institute <strong>of</strong> Legal Medicine, University <strong>of</strong> Santiago de Compostela, Galicia, Spain,<br />
15782<br />
Analysis <strong>of</strong> THC and its metabolites in biological samples is <strong>of</strong> great relevance for forensic purposes. In the<br />
case <strong>of</strong> oral fluid the analysis should determine THC, whereas in urine, it detects the inactive metabolite<br />
THC-COOH. Most laboratories analyze THC in such samples using GC-MS methods, but these<br />
procedures are time-consuming and involve unavoidable previous extraction and derivatization. In this<br />
paper we report a validation method in which the THC is isolated from oral fluid by a simple liquid-liquid<br />
extraction with hexane. The separation and quantitation was done on a positive ion electrospray (BSI<br />
positive) high performance liquid chromatography-mass spectrometry (LC-MS) in the selected ion<br />
monitoring (SIR) mode. Calibration curves for ,1.9-THC were performed in oral fluid, achieving linearity<br />
between 2 nglmL and 100 ng/mL. The procedure was validated in terms de linearity (coefficient <strong>of</strong><br />
correlation: 0,9956±0,0035), repeatability (5.33-10.02 %, n=6), reproducibility (2.58-14.7 %, n=6). The<br />
limit <strong>of</strong> quantification (LOQ) was defined as the lowest concentration <strong>of</strong> analyte that could be measured<br />
reproducibly and accurately (CV < 20% and bias> 80%), which was 2 ngimL. The LOD was estimated on<br />
the criteria <strong>of</strong> the lowest concentration <strong>of</strong> an analyte that the bioanalytical procedure can reliably<br />
differenciate from the backgroud noise, which was 1 ng/mL. The mean recovery was 86.62%. The method<br />
requires only 200 ilL <strong>of</strong> oral fluid, and has been used to analyze oral fluid samples collected from drivers,<br />
by spitting, salivette and intercept@ modes.<br />
Keywords: LC-MS, Oral Fluid, THC<br />
Page 310
M28 <br />
DOSE-RELATED DISTRIBUTION OF CODEINE, COCAINE AND METABOLITES INTO<br />
HUMAN HAIR FOLLOWING CONTROLLED ORAL CODEINE AND SUBCUTANEOUS<br />
COCAINE ADMINISTRATION<br />
Karl B. Scheidweiler l *, Edward J. Cone 2 , Eric T. Moolchan l and Marilyn A. Huestis l : 1 National Institute<br />
on Drug Abuse, 5500 Nathan Shock Drive, Baltimore, MD: 2 ConeChem Research, LLC, Severna Park,<br />
MD<br />
Ten volunteers with histories <strong>of</strong> cocaine and opiate use consented to reside on a secure clinical research<br />
ward at the Intramural Research Program, National Institutes on Drug Abuse, National Institutes <strong>of</strong> Health<br />
to participate in a ten-week controlled cocaine and opiate administration study. This Intramural Research<br />
Board approved study was designed to investigate excretion <strong>of</strong> opiates, cocaine and metabolites into hair<br />
following multiple subcutaneous (s.c.) cocaine hydrochloride and oral (p.o.) codeine sulfate doses. The<br />
first three weeks <strong>of</strong> the study comprised the drug washout phase. During the low dose drug administration<br />
week (week 4) 75 mg/ 70 kg cocaine, s.c. and 60 mg/ 70 kg codeine, p.o. doses were administered on<br />
alternating days for a total <strong>of</strong> three doses for each drug. The high dose drug administration week began on<br />
week 8 during which, subjects received three doses <strong>of</strong> 150 mg/ 70 kg cocaine, s.c. and 120 mgi 70 kg<br />
codeine, p.o. on alternating days. An electric razor was used to collect hair at the end <strong>of</strong> each week during<br />
the study. Drugs were extracted from pulverized hair via methanolic sonication and extracts were analyzed<br />
for cocaine, norcocaine, benzoyl ecgonine (BE), ecgonine methyl ester (EME), cocaethylene (CE), codeine,<br />
norcodeine, morphine and 6-acetylmorphine (6-AM) via liquid chromatography-atmospheric pressure<br />
chemical ionization tandem mass spectrometry. Limits <strong>of</strong> quantitation (LOQ) for cocaine and metabolites<br />
were 17 pg/mg, except for EME (50 pg/mg). Opiate LOQs were 83 pg/mg, except for norcodeine (240<br />
pgimg).<br />
Maximum cocaine and metabolite concentrations (Cmax) were generally measured in hair samples<br />
collected two weeks after drug dosing (range: one to three weeks). Average cocaine and metabolite<br />
Cmax's (::I: standard error <strong>of</strong> the mean) measured in hair reflecting the low dose cocaine week<br />
administrations were 2,997 ::I: 619, 314 ::I: 51, 187 ::I: 27, 84 ::I: 21 pg/mg <strong>of</strong> cocaine, BE, EME and<br />
norcocaine, respectively. Mean cocaine and metabolite Cmax's measured reflecting the high dose cocaine<br />
week administrations were 6,419::1: 1,698,708::1: 163,425::1: 65, 218::1: 46 pg/mg <strong>of</strong> cocaine, BE, EME, and<br />
norcocaine, respectively. Norcocaine did not exceed the LOQ after the low cocaine dosing in one <strong>of</strong>ten<br />
individuals. In all other cases, cocaine and metabolites exceeded the LOQ after low and high cocaine<br />
dosings. Comparison <strong>of</strong> cocaine and metabolite hair Cmax's that occurred after low and high dose cocaine<br />
weeks revealed significant dose-relationships and were significantly different from hair concentrations at<br />
the conclusion <strong>of</strong>the washout phase as evaluated using Wilcoxon signed rank test (p
M29 <br />
CODEINE AND METABOLITE DISPOSITION IN HUMAN SWEAT FOLLOWING<br />
CONTROLLED ORAL CODEINE ADMINISTRATION<br />
Eugene W. Schwilke 1 *, Sherri L. Kacinkol, Allan J. Barnesl, Jonathan M. Oyler2, Edward 1. Cone 3 , Eric T.<br />
Moolchan l , and Marilyn A. Huestis l : IChemistry and Drug Metabolism Section, Intramural Research<br />
Program, NIDA, NIH, Baltimore, MD, 2Department <strong>of</strong> the Army, US Army Research, Development and<br />
Engineering Command, Aberdeen Proving Ground, MD, 3ConeChem Research, LLC., Severna Park, MD<br />
Analysis <strong>of</strong> codeine is included in drug treatment, military, criminal justice and workplace programs<br />
because <strong>of</strong> its abuse potential and performance impairing effects. Interest in monitoring drug exposure with<br />
human sweat, as an alternative biological specimen is increasing, as sweat collections are convenient, less<br />
invasive and difficult to adulterate. Our objective for this study was to determine the excretion pr<strong>of</strong>ile <strong>of</strong><br />
codeine and metabolites into human sweat using the PharmChek Sweat Patch. Volunteers with a history<br />
<strong>of</strong> opiate use (n=9) provided informed consent to participate in this IRB-approved study and resided on the<br />
closed clinical research ward for 12 weeks. Low (60mg/70kg) and high (l20mg/70kg) doses <strong>of</strong> codeine<br />
sulphate were administered three times a week, four weeks apart. Codeine, norcodeine, morphine,<br />
normorphine, and 6-monoacetylmorphine were isolated by SPE and GCIEI-MS. The limit <strong>of</strong> quantitation<br />
(LOQ) for codeine and morphine were 2.5 ng/patch, and 5 ng/patch for metabolites.<br />
We present data from patches representing four categories <strong>of</strong> sweat collection. First, weekly sweat patches<br />
were collected from the time <strong>of</strong> entry onto the secure ward until the time <strong>of</strong> first codeine administration,<br />
reflecting excretion <strong>of</strong> previously self-administered opiates. No patch was positive for 6-acetylmorphine,<br />
codeine, morphine or metabolites at the methods' LOQs.<br />
Second, weekly sweat patches also were applied prior to and removed 7 days after dosing for 5 <strong>of</strong> 9 and 3<br />
<strong>of</strong> 6 participants for the low and high doses, respectively. 80% <strong>of</strong> the low and 100% <strong>of</strong> the high dose<br />
weekly patches were positive for codeine, but negative for metabolites. The mean codeine concentration for<br />
these patches was 65 ng/patch (median 27, SD 92, range 16-225) for the low dose and 82 ng/patch (median<br />
84, SD 15, range 67-96) for the high dose.<br />
Third, other sweat patches were worn for between 1 to 15 hours during the first 48 hours after dosing. Of<br />
139 patches worn during the first 48 hours following the first codeine administration, only 11 (8%)<br />
contained codeine levels greater than our LOQ. Codeine was the only analyte detected and could be found<br />
as early as 1 hour after dosing. A total <strong>of</strong>7 patches (8%) were positive for codeine following the low dose,<br />
and 4 patches (8%) following the high dose. The mean codeine concentration (data from 3 <strong>of</strong>9 subjects) in<br />
sweat was 43 ng/patch (median 28, SD 50, range 5 - 153) for the low dose and 12 ng/patch (median 11.0,<br />
SD 9.0, range 3-24, data from 3 <strong>of</strong> 6 subjects) for the high dose. Codeine was detected in sweat patches for<br />
up to 26 h after administration; patches applied after 26 hours and worn for up to 15 hours were below the<br />
LOQ.<br />
Fourth, weekly patches also were applied to 4 <strong>of</strong> 9 participants two weeks after the last codeine dose. All<br />
<strong>of</strong> the patches also were negative for codeine and metabolites.<br />
Sweat has recently been proposed by the Substance Abuse and Mental Health Services Administration<br />
(SAMHSA) for federally-mandated workplace drug testing. A confirmation cut<strong>of</strong>f <strong>of</strong> 25 ng/patch has been<br />
proposed for patches worn 7 to 14 days. Two patches for one subject and I patch for another collected<br />
within the first 48 hours following dosing, would be positive using these criteria. In comparison, 6 <strong>of</strong> 8<br />
patches worn for 7 days during the dosing period would be positive under the new SAMHSA guidelines.<br />
Sweat provides an adequate matrix for detection <strong>of</strong> opioid use. There was large intra- and inter-subject<br />
variability. No correlation <strong>of</strong> codeine concentration with dose was found for the doses investigated.<br />
Patches worn for 1 week were more likely to contain codeine above the LOQ than patches worn for 1 to 15<br />
hours.<br />
Keywords: Sweat, Codeine, GCMS<br />
Page 312
M30 <br />
DOPING STEROID ANALYSIS IN NAIL CLIPPINGS<br />
Kenichi Takaichi l ., R.A. Anderson I and D. Thieme 2 : IDepartment <strong>of</strong> <strong>Forensic</strong> Medicine and Science, University <strong>of</strong><br />
Glasgow, Glasgow G 12 8QQ, United Kingdom and 21nstitute <strong>of</strong> Doping Analysis/Sports Biochemistry, Dresdner Strasse<br />
12, D-01731 Kreischa, Germany.<br />
Extraction <strong>of</strong>analytes from fingernail is difficult due to its hard keratin composition. Our group has shown the feasibility<br />
<strong>of</strong> drug analysis in nail using a cryogenic grinding technique, including cannabinoids and opioids (I). In particular,<br />
cryogenic grinding has been shown to allow the extraction and analysis <strong>of</strong> intact esters such as diamorphine by avoiding<br />
the alternative alkaline hydrolysis step. To date, few papers have reported the detection <strong>of</strong>steroids in nail (2). By contrast,<br />
several papers have reported the detection and analysis <strong>of</strong> anabolic steroids in hair.<br />
In the present study, cryogenic grinding was used to prepare nail clippings from doping abusers for extraction <strong>of</strong><br />
endogenous and anabolic steroids to show that both can be detected, as in hair. This method was compared to blood<br />
(plasma) and urine samples that had been analysed at the same time.<br />
Fingernail clippings from users <strong>of</strong> anabolic steroids (including testosterone esters, stanozolol and methenolone acetate)<br />
were obtained from the Institute <strong>of</strong> Doping Analysis/Sports Biochemistry, Kreischa. Blank nail samples were obtained<br />
from volunteers. The nail samples were first decontaminated by washing with 0.1% sodium dodecyl sulfate, water (x 3)<br />
and methanol (x 3). After drying, the samples were pulverised for 4 min in a liquid-nitrogen cryogenic miII (SPEX<br />
CertiPrep 6750 Freezer Mill). The powdered nail was then extracted with methanOl/ethyl acetate (7:3 v/v, 7 mL).<br />
Deuterated anabolic steroids (5a-estran-3B-oI-17-one-d 3 , testosterone-d 3 , and stanozolol-d 3 ) and medroxyprogesterone<br />
were used as internal standards.<br />
The extracts were converted to TMSi derivatives with MSTFAlNH 4 112-mercaptoethanol and analyzed by GC-MS in the<br />
EI + full scan and SIM modes, on a Finnigan Trace instrument equipped with an HP-5 column (30 m x 0.32 mm i.d.; film<br />
thickness 0.25 J.lm) with temperature programming from 180°C to 240 °C at 3 °C/min, 240°C to 300 °C at 5 °C/min, and<br />
final temperature held for 10 min.<br />
In this initial study endogenous steroids (androsterone (And), etiocholanolone (Etio), dehydroepiandrosterone (DHEA),<br />
epiandrosterone (epi-And), epitestosterone (epi-Test) and testosterone (Test» were identified and quantified in the nail<br />
samples from both steroid users and non-users.<br />
No. And Etio DHEA epi-And epi-Test Test<br />
Suspect # I (Nail) 4.1 0.0 5.6 3.3 3.0 4.3<br />
Suspect #2(Nail) 4.7 0.0 3.0 1.9 1.5 3.9<br />
Suspect #3(Nail) 9.6 0.0 25.3 14.3 11.0 10.6<br />
Suspect #4(Nail) 12.8 0.0 12.0 6.2 10.9 25.0<br />
Suspect #5(Nail) 1.7 0.0 1.8 0.8 0.6 0.6<br />
Healthy # 1 (Nail) 1.5 0.0 1.4 0.7 0.6 6.5<br />
Healthy #2(Nail) 8.4 0.0 4.5 1.7 2.6 l.l<br />
Healthy #1(Plasma) 30322.9 54222.5 11218.3 Trace 222.2 3583.8<br />
Healthy #2(Plasma) 9923.3 2966.7 100.6 Trace 200.2 196.0<br />
Healthy # I (Urine) 351.6 392.5 11.2 Trace 9.0 11.0<br />
Healthy #2(Urine) 926.8 868.7 115.8 Trace 7.4 13.6<br />
* Suspect #3<br />
Test 292 pg/mL in urine,<br />
Test-enanthate, decanoate<br />
in hair were 20 and 18<br />
pg/rng, respectively.<br />
* Suspect #4<br />
Test 30 pglrnL in urine,<br />
Test-enanthate,<br />
phenyl-propionate,<br />
decanoate, and isocaproate<br />
in hair were 25, 425, 220,<br />
and 340 pg/rng,<br />
respectively.<br />
In general, endogenous steroid concentrations in nail were low, in the pgjmg range. Also, elevated concentrations <strong>of</strong><br />
testosterone in nail were positively associated with high concentrations in plasma and urine. However, although the<br />
analytical results provided evidence for the presence <strong>of</strong> anabolic steroids in the samples from steroid users, including<br />
testosterone and testosterone esters at low concentrations, it has not yet been possible to confirm this due to interference<br />
from other endogenous substances. Nail remains a potential, but still to be confirmed, alternative biological specimen to<br />
hair for the detection <strong>of</strong>past exposure to doping steroids.<br />
References:<br />
(1) K. Takaichi, N.P. Lemos, R.A. Anderson, Analysis <strong>of</strong> Opiates in Nail Clippings from Chronic Heroin Abusers,<br />
presented at the 39 th Annual TIAFT <strong>Meeting</strong>, Prague, 200 I.<br />
(2) M.H. Choi, Y.S. Yoo, B.C. Chung, Measurement <strong>of</strong> testosterone and pregnenolone in nails using GC-MS.,<br />
J. Chromatogr., B 754, 495·501 (2001).<br />
Keywords: Nail Analysis, Doping, Anabolic Steroids<br />
Page 313
M31 <br />
DETERMINATION OF A'.TETRAHYDROCANNABINOL (THC) IN ORAL FLUID USING<br />
SOLID PHASE EXTRACTION AND HIGH-PERFORMANCE LIQUID CHROMATOGRAPHY<br />
AND ELECTROSPRA Y IONIZATION MASS SPECTROMETRY<br />
H.M. Teixeira *, P. Proenyal, A. Castanheira l , M. L6pez-Rivadulla 2 , F. Corte-Reali, E.P. Marques l , D.N.<br />
'<br />
Vieira l : I National Institute <strong>of</strong> Legal Medicine, Coimbra, Portugal and 2 Legal Medicine Institute, Santiago<br />
de Compostela, Spain<br />
Aim: High-performance liquid chromatography with electro spray ionization mass spectrometry was used to<br />
determine /19-tetrahydrocannabinol (t/-THe) in oral fluid.<br />
Methods: Oral fluid samples were extracted using Bond Elut LRC-CertiiY solid-phase extraction columns<br />
(lOcc, 300mg), elution performed with n-hexane/ethyl acetate. The separation and quantitation was done on<br />
a positive ion electro spray (ESl positive) high performance liquid chromatography-mass spectrometry (LC<br />
MS) in the single ion recording (SIR) mode. Quantitation was achieved by the addition <strong>of</strong> the deuterated<br />
analogue as internal standard. The compounds were detected by single ion monitoring <strong>of</strong>mlz 315 and mlz<br />
318 for the protonated molecules [THC+H+J and [d 3 -THC+H+J, respectively. In the chromatographic<br />
separation, a X-Terra MS CIS column (2.1x50mm, 3.5j.1m) was used and the mobile phase was<br />
composed <strong>of</strong> acetonitrile and ammonia 0.05%, at a OJ mLimin flow rate.<br />
Results: No interferences were detected in 10 blank oral fluid samples <strong>of</strong> different origin. The precision and<br />
accuracy were tested on spiked oral fluid samples at three different concentrations (2, 25 and 100nglmL).<br />
The mean recovery was 79%, coefficients <strong>of</strong> variations were between 2.9-6.9% and the limits <strong>of</strong> detection<br />
(LOD) and quantitation (LOQ) were 1.0 nglmL and 2.0 ng/mL, respectively. Calibration curves for /e/.<br />
THC were performed in methanol solutions and in oral fluid samples using seven different concentrations,<br />
achieving linearity between 2 nglmL and 100 ng/mL. This validated method is currently being applied to<br />
real cases where oral fluid specimens are collected with the Salivette® and also by spitting from marijuana<br />
smokers attending the world's largest music event in recent years, "Rock in Rio - Lisboa".<br />
Conclusions: The method is sensitive, accurate and reproducible and may be utilized in ongoing controlled<br />
cannabinoid administration studies and in roadside studies and thus, important for the fields <strong>of</strong> forensic<br />
toxicology.<br />
Keywords: /1'-THC, Oral Fluid, LC-MS<br />
Page 314
M32 <br />
LEGAL ISSUES OF ADDICTION AND HAIR TESTING FOR DRUGS OF ABUSE<br />
Aristidis Tsatsakis*, Manolis Savvopoulos, Joanna Dialyna, Manolis Tzatzarakis, and Eleftherios Pallis<br />
Center <strong>of</strong> Toxicology Science and Research, Department <strong>of</strong>Medicine, University <strong>of</strong> Crete, Greece.<br />
Aim: The purpose <strong>of</strong>this paper is to present legal issues <strong>of</strong> addiction and hair testing results regarding to the<br />
service <strong>of</strong> Law in Greece.<br />
Methods Legal Part: Details (such as the process, the decision and the competence <strong>of</strong> the Court, the<br />
police record, the indictment, the expert reports, the defendant's individuality, the crimes and the penal<br />
confrontal and many others) from legal cases related to addiction and its judicial verification were collected<br />
and analysed.<br />
Methods - Laboratory Part: Laboratory data <strong>of</strong> cases concerning the laboratory evaluation <strong>of</strong> addiction in<br />
drug users and also occasionally the legal course <strong>of</strong> cases with addict defendants are presented. In four<br />
representative cases segmental hair analysis proved that as long as the individuals were imprisoned findings<br />
with drug substances corresponding to that period were lesser or practically absent comparably with<br />
samples corresponding to the time out <strong>of</strong> prison, which proved increased drug abuse.<br />
Results: Hair analysis provides information on chronic exposure rather than acute poisoning. Its detection<br />
window varies from some days to months or even years and the length <strong>of</strong> the hair is the only limit. The<br />
procedure that the Law lays in many cases is insufficient and in most cases unable to be abided by. Details<br />
about the addicted person's pr<strong>of</strong>ile are presented. Our study presents that the segmental hair analysis<br />
method is a subject <strong>of</strong> growing interest for drugs <strong>of</strong> abuse because it provides information on chronic<br />
exposure to the drug and the drug history pr<strong>of</strong>ile <strong>of</strong>each subject<br />
Conclusions: Although hair testing for drugs <strong>of</strong> abuse is not specially referred by any law, Greek Courts<br />
accept the method for the final conclusion about the defendant's claim <strong>of</strong> addiction. Segmental hair<br />
analysis may be the only tool to prove this claim, not only when the medical examiner is not able to decide<br />
about defendant's addiction and it's severity but also in cases where the time period <strong>of</strong> drug abuse is to be<br />
defined.<br />
Keywords: Addiction, Legal and Judicial Issues, Segmental Hair Testing.<br />
Page 315
M33 <br />
ENHANCED SENSITIVITY FOR DRUGS OF ABUSE IN ORAL FLUID USING THE<br />
INNOVATIVE NEW ORALSTAT TEST SYSTEM FOR ON-SITE TESTING.<br />
Yli Remo Vallejo*, Martin Gould, Matthew Lomonico, and John Donovan: American Bio Medica<br />
Corporation, 603 Heron Drive, Unit #3, Logan Township, New Jersey 08085<br />
The New OralStat is an innovative test system for the rapid on-site detection <strong>of</strong>drugs <strong>of</strong> abuse in oral fluid<br />
that dramatically improves the limits <strong>of</strong> detection. This test system consists <strong>of</strong> an untreated collector<br />
sponge with a built-in sample adequacy feature, an integrated test device containing separate receptacles for<br />
a sample buffer, gold conjugates, and immunochromatographic test strips. The device allows the lateral<br />
flow process to be separated into discrete stages by enabling the dilution <strong>of</strong> the oral fluid sample with<br />
buffer, the preincubation <strong>of</strong> the sample with the antibody-coated gold reagents, then allowing the sample<br />
mixture to chromatograph on the lateral flow test strips. The use <strong>of</strong> a buffer minimizes the problems<br />
associated with viscous saliva. The. preincubation <strong>of</strong> the sample with the antibody-coated gold reagent<br />
greatly improves sensitivity. The device can accommodate any combination <strong>of</strong>6 drug assays.<br />
The folfowing performance was observed in a study involving spiked oral fluid from 3 non-users:<br />
Drug<br />
Sensitivity (nglmU<br />
THC (parent compound) 25<br />
PCP 5<br />
Amphetamine 25<br />
Methamphetamine 25<br />
Opiates 20<br />
Cocaine (Benzoy I Ecgonine) 12<br />
Benzodiazapines 25<br />
Methadone 25<br />
The NewOralStat test system can detect PCP, Opiates, Amphetamine, Methamphetamine, and Cocaine<br />
metabolite at lower levels than the SAMHSA proposed cut<strong>of</strong>fs ..THC detectability at 25 ng/mL, though<br />
still above the SAMHSA cut<strong>of</strong>f <strong>of</strong> 4 ng/mL, is a major improvement over current POCTs, improving the<br />
detection <strong>of</strong> recent marijuana use by many hours. The results <strong>of</strong> a current study with samples from drug<br />
users will be presented.<br />
The New OralStat test system is visually read and requires no instrumentation to attain these levels <strong>of</strong><br />
sensitivity. It is however expected that the use <strong>of</strong> a reflectance reader along with agitation during the<br />
preincubation period will further improve these limits <strong>of</strong> detection. Initial results show that by applying<br />
such measures the THC cut<strong>of</strong>f <strong>of</strong> 4 ng/mL can be achieved.<br />
Keywords: Oral Fluid, Drugs <strong>of</strong>Abuse, On-Site Testing<br />
Page 316
M34 <br />
COMPARISON OF ORAL FLUID WITH URINE TESTING IN DRE CERTIFICATIONS<br />
Michael A. Wagner!*, Colleen Scarneo l , Emily Rice l , Kris Valas l , Susan Lefebvre l and Christina Werner2<br />
IOepartment <strong>of</strong> Safety, State Police <strong>Forensic</strong> Toxicology Group 33, Hazen Dr., Concord, NH 03301, and<br />
20raSure Technologies, 150 Webster Street, Bethlehem, PA 18015<br />
Determination <strong>of</strong> impairment by drugs in OWl cases or in the work place <strong>of</strong>ten requires the analysis <strong>of</strong> biological<br />
specimens. The most common matrices tested are blood, urine and saliva. Each <strong>of</strong> these matrices has inherent<br />
advantages and disadvantages. For example, urine has advantages <strong>of</strong> providing a historical perspective to drug<br />
use yet does not supply impairment interpretation. Saliva has the potential for supplying interpretation with<br />
respect to blood concentration and impairment with similar detection widows to blood. This abstract reviewed<br />
61 ORE cases, July 8 1h 2002 until June 30 1h 2003, involving roadside stops for OWl and ORE certifications<br />
events. Twenty-six <strong>of</strong> the 61 cases involved ORE certification events such as; concerts, and evaluation nights<br />
arranged by various police departments were the subject <strong>of</strong> this initial study. During the certification events the<br />
laboratory personnel was able to attend and assist law enforcement with the collection <strong>of</strong> oral fluids and urine<br />
samples. Oral fluids were collected using the Intercept Collection device from OraSure Technologies Inc. The<br />
process entailed having the subject place an oral collection pad (attached to a handle) between the lower cheek<br />
and gum, rubbing back and forth until moist. Most subjects just sucked on the pad until the sampling time<br />
interval was completed (2 minutes). The pad was placed in the sampling tube containing 800 uls <strong>of</strong> OraSure<br />
buffer solution. The specimens were collected typically upon completion <strong>of</strong> the ORE evaluation. Matched urine<br />
and oral fluids specimens were collected. The oral fluids were tested in the on Intercept® Micro-Plate EIA,<br />
while the urines used the on Micro-Plate EIA serum kits optimized for urine analysis. Both analyses were<br />
performed on a PersonalLABTM automated analyzer. All subjects were screened for seven classes <strong>of</strong> drugs:<br />
Benzodiazepines, Cocaine, Cannabinoids, Opiates, Methamphetamines, Amphetamines, Barbiturates, PCP, and<br />
Methadone.<br />
Summarized in Table I are the correlated analytical results between urine and oral fluid testing as they relate to<br />
ORE interpretation. The positive rates with respect to the various drug categories appears to be the highest for<br />
Cocaines and Cannabinoids, 87% and 94% respectively, while Barbiturates had the highest percentage <strong>of</strong> oral<br />
fluid positive results 75% versus 25% for urine. ORE percent corroboration varied between 25% for Stimulants,<br />
36% for Depressants, 47% for Cannabinoids, and 100% for Narcotic Analgesics. These results seem to parallel<br />
with the subject's admission rate. Certainly one issue confounding the ORE corroboration was the percentage <strong>of</strong><br />
positive polydrug cases. 57% <strong>of</strong> the cases had two or more drug categories test positive, 27% screened positive<br />
for three or more drugs, 15% <strong>of</strong> the cases screened positive for four or more drugs, and 8% <strong>of</strong> the cases screened<br />
positive for five or more drugs.<br />
The ease <strong>of</strong> administration for oral fluid testing in ORE evaluations may provide additional information with<br />
respect to impairment interpretation. This initial study demonstrated that Cocaine and Cannabinoids appeared to<br />
have a better correlation with urine as compared to other drug classes, while Barbiturates had the highest<br />
specificity for oral fluids.<br />
Table I<br />
! Drug Urine Oral No. Tests Urine OF ORE Subject<br />
Categories NH-ForenTox NH-Foren Tox "'+" "+" Opinions Admission<br />
Cut<strong>of</strong>f ng/mL Cut<strong>of</strong>fng/mL<br />
Benzodiaz 100 1.0 11 11 2 3 2<br />
cac 100 5.0 16 13 14 4 4<br />
THC 20 1.0 17 16 12 8 IO i<br />
Opiates 200 10 8 8 4 8 5<br />
Methamph 300 40 4 4 1 1 2<br />
Barbiturate 200 20 3 1 3 2 2<br />
Methadone 300 5.0 3 3 1 3 3<br />
PCP 25 1.0 ND - - - -<br />
Amphet 300 100 NO - - - -<br />
Key Words: DRE, Oral Fluids, Urine Drug Screen, ErA<br />
Page 317
M35 <br />
DRUG DETECTION IN HAIR: ASSESSMENT OF LEVELS FROM LARGE VOLUME SCREENING AND<br />
CONFIRMATION TESTING<br />
John Wicks*, John Sullivan and Lolita Tsanaclis: Tricho-Tech Limited, The Cardiff Medicentre, Heath Park, Cardiff,<br />
CFI4 4UJ, United Kingdom.<br />
In recent years understanding <strong>of</strong> the benefits <strong>of</strong> the use <strong>of</strong> hair in drug testing has increased, particularly its advantages<br />
over urine, and more recently, oral fluid. The key benefit is the long time window <strong>of</strong> detection. This understanding<br />
together with reliable techniques has contributed to the dramatic increase in the use <strong>of</strong> hair samples in the detection <strong>of</strong><br />
drug use. Amongst the wide variety <strong>of</strong> sectors that currently use hair for the detection <strong>of</strong> drugs, the largest are clinics,<br />
family law firms, the police and various organisations for workplace testing. The main purpose is to verifY drug use or<br />
monitor drug abstinence. Very <strong>of</strong>ten when the analysis is performed and the results issued, the most common question<br />
that is raised is: what do the levels detected tell me about how much drugs were used by the person being tested<br />
Because it is difficult to establish an accurate estimation <strong>of</strong> the amount <strong>of</strong> dose taken in relation to levels <strong>of</strong> drug in<br />
hair, the levels <strong>of</strong> drugs detected in hair are best used as a guide to changes in use in the individual when sectional<br />
analysis is performed or two different periods are compared in the same individual.<br />
Nonetheless, it can be very useful, as a guide when writing reports or communicating with clients, to compare results<br />
obtained from a hair test from an individual's hair sample with results obtained in other samples from a large group <strong>of</strong><br />
people. Hair samples (N=12,218) from various sources were received by Tricho-Tech for screening for drugs over a<br />
two-year period and analysed using the same method. All samples were washed, extracted then screened using coatedplate<br />
ELISA test for each drug group (Immunalysis Corporation, Pomona, CA, USA) and processed by an automated<br />
analyser Triturus (Grifols, Cambridge, UK) at a cut-<strong>of</strong>f <strong>of</strong> 0.5 ng/mg (Table I). Samples above the cut-<strong>of</strong>f were<br />
submitted for confirmation analysis by Gas Chromatography-Mass Spectrometry (GC-MS or GC-MS/CI) using<br />
HP5973 (Agilent, Berkshire, UK) or Varian Inc. Saturn for GC-MS/MS (Walton-on-Thames, UK). The dynamic range<br />
was from 2 to 160 ng/mL. Three ions for the drugs and two ions for the internal standards were monitored.<br />
Tabl e I H' air samples analyse dbJy ELISA and GCMS WI·th confiIrmatlOn rates or eac hdruJg group.<br />
I iScreened GCMS Confirmation Rate<br />
i<br />
i Group .N<br />
N % N %<br />
Amphetamines 7355 4128 (56%) 1839 (45%)<br />
Benzodiazepines 5804 1879 (32%)<br />
Buprenorphine 786<br />
1415 (75%)<br />
113 (14%) 63 (56%)<br />
Cocaine 8919 3150 (35%) 2490 (79%)<br />
Methadone 6127 .1893 (31%)<br />
1666 (88%)<br />
Opiates 8970 4164<br />
1<br />
J46%) 2901 -.i70o/~<br />
Percentiles 25%, 50% (Median), 75%, 95% and maximum levels for all analytes in each drug group were calculated<br />
and will be presented. Results for Cocaine Group are shown in Table 2.<br />
Percentiles and maximum levels in n m <strong>of</strong> hair for Cocaine rou<br />
25% 50% 75% 95% Maximum N<br />
0.3 0.8 1.6 5.5 34.8 305<br />
i""WY',,,,,,i",<br />
Cocaethylene 0.3 0.5 1.2 4.1 9.4 339<br />
0.4 1.1 3.6 16.5 163.7 1988<br />
Cocaine 0.9 2.9 11.9 59.5 814.2 2483<br />
Using Cocaine as an example <strong>of</strong> drug levels by sector, median levels were: Clinical=6.9 ng/mg; Police=5.0 ng/mg;<br />
Medico-Legal=2.5 ng/mg and Employment =0.4 ng/mg. A consistent pattern was seen for the other drug groups.<br />
The results show a wide range <strong>of</strong> levels for all analytes, frequency and distribution. Thus, this assessment <strong>of</strong> levels<br />
provides an important comparative aid for interpreting results <strong>of</strong> detected drugs in samples <strong>of</strong> hair.<br />
Keywords: Drugs, Hair, GC-MS/MS<br />
Page 318
M36<br />
EV ALUA TION OF A RAPID ORAL FLUID POINT OF CARE TEST FOR MDMA<br />
Lisa Wilson*, Gail Cooper, Chris Hand and Ahmed lehanli: Cozart Bioscience Ltd., 45 Milton Park,<br />
Abingdon, Oxfordshire, United Kingdom OX144RU<br />
Recreational use <strong>of</strong> 3,4-methylenedioxymethamphetamine (MDMA) either alone or in combination with<br />
other drugs such as alcohol and cannabis has become increasingly popular among young people throughout<br />
the UK, Europe and the US. The Cozart® RapiScan oral fluid drug test system has been use successfully for<br />
monitoring compliance within treatment centres, criminal justice settings and more recently at the roadside.<br />
The aim <strong>of</strong> this study was to evaluate the Cozart® RapiScan test cartridge developed for the detection <strong>of</strong><br />
MDMA and methamphetamine in oral fluid. Fifty oral fluid samples were obtained from drug addicts<br />
attending drug dependency units and were screened initially using the Cozart® microplate ELISA for<br />
amphetamines. All samples were then screened using the Cozart® RapiScan test cartridge for MDMA<br />
followed by confirmation by gas chromatography-mass spectrometry (GC-MS).<br />
A total <strong>of</strong>23 samples screened positive and were confirmed for MDMA either alone or in combination with<br />
amphetamine. A further 15 samples were confirmed negative for all amphetamines by GC-MS and 14 <strong>of</strong><br />
these samples also screened negative using the Cozart® RapiScan. The false positive sample was<br />
investigated further and was found to contain an extremely high concentration <strong>of</strong> pseudoephedrine. The<br />
remaining 12 samples were confirmed positive for amphetamine only. Six samples screened negative and<br />
the other six screened positive due to the extremely high concentrations <strong>of</strong> amphetamine in these samples.<br />
No samples tested in this study contained methamphetamine.<br />
The Cozart® RapiScan Drug Test System for the detection <strong>of</strong> MDMA correctly identified 100% <strong>of</strong> MDMA<br />
~. positive samples ranging from 53nglmL to concentrations in excess <strong>of</strong> lS0ng/mL. False positive results<br />
were only observed when samples contained extremely high concentrations <strong>of</strong> amphetamine or<br />
pseudoephedrine, which is consistent with the cross reactivity pr<strong>of</strong>ile <strong>of</strong> the drug test.<br />
Keywords: MDMA, Oral fluid, Onsite Test<br />
Page 319
M37 <br />
ALCOHOL TESTING BY AN ONSITE ONE-STEP ORAL FLUID ALCOHOL AND DRUG<br />
COMBINATION TEST DEVICE ORATECTPLUSTM<br />
Raphael C Wong·, Jan Sook, Richard Zoltek: Branan Medical Corporation, 10015 Muirlands Road, Suite<br />
F" Irving, CA 926l8, USA<br />
Aims: The objective <strong>of</strong> this study is to compare the alcohol detection <strong>of</strong>OratectPlus, an onsite oral fluid<br />
alcohol and drug combination test device with Alco-screenTM a saliva alcohol test.<br />
Methods and Results: Oratect is a one-step rapid drug screen that integrates oral fluid collection, drug<br />
testing and confirmation sampling in one single device. OratectPlus is a new generation <strong>of</strong> Oratect that<br />
includes alcohol testing with drug testing and provides faster collection and test times. The new device<br />
consists a cap and a plastic housing containing a collection pad that is connected to an alcohol test pad on<br />
one side and two lateral flow immunoassay test strips that test for 6 abused drugs on another side. To run<br />
the test, the collection pad end <strong>of</strong>the device is inserted into the donor's mouth for one to two minute till red<br />
color fluid starts to appear on both lateral flow test strips. The color on the alcohol test pad is noted<br />
immediately. Negative alcohol level does not change the original tan color pad. Presence <strong>of</strong> bluish gray<br />
color on this pad indicates alcohol level at or exceeding 0.02% blood alcohol concentration. Drug test<br />
results are available from the two lateral flow strips after 3 minutes with the absence <strong>of</strong> red lines indicating<br />
positive results. In a field trial, forty individuals without drinking any alcohol were all tested negative with<br />
the OratectPlus and Alco-screen. Another forty individuals allowed to consume beer and then tested for<br />
alcohol within 20 minutes were all found to test positive for both OratectPlus and Aleo-screen. Nonalcoholic<br />
drinks including sodas, tea and c<strong>of</strong>fee were found not to interfere with the test result.<br />
Conclusion: OratectPlus is shown to be a viable onsite device for testing alcohol use.<br />
Keywords: Alcohol Testing, Oral Fluid, Drugs <strong>of</strong> Abuse<br />
Page 320
M38 <br />
Ll9-TETRAHYDROCANNABINOL (THC) IN SWEAT PRIOR TO AND FOLLOWING<br />
CONTROLLED ORAL ADMINISTRATION OF HEMP OIL AND MARINOLTM TO CANNABIS<br />
USERS<br />
Abraham T. Wtsadik 1 *, Karl Scheidweilerl,Takeshi Saito), Richard A. Gustafson 2 , Eric T. Moolchan 1 and<br />
Marilyn A. Huestis l : IChemistry and Drug Metabolism, IRP, NInA, NIH, 5500 Nathan Shock Drive,<br />
Baltimore, MD 21224, 2Jacksonville Naval Air Station, Adams Avenue, Jacksonville, FL 32212<br />
3Department <strong>of</strong> <strong>Forensic</strong> Medicine, Tokai University School <strong>of</strong> Medicine Bohseidai, Isehara, Kanagawa<br />
259-1193 Japan<br />
Six healthy individuals with a history <strong>of</strong> cannabis use resided on the secure clinical research unit <strong>of</strong> the<br />
Intramural Research Program, National Institute on Drug Abuse, National Institutes <strong>of</strong> Health for the 10 to<br />
12 week study. Participants provided informed consent for this Institutional Review Board-approved oral<br />
cannabinoid administration protocol. This was a randomized, double blind, double dummy, placebocontrolled<br />
within-subject study. Sweat was collected throughout the study with PharmCheck sweat<br />
patches worn for 24 hours or 7 days. The initial washout phase <strong>of</strong> this study lasted from admission until<br />
subjects' urine cannabinoid concentrations were below 10 ng/mL by fluorescence polarization<br />
immunoassay. Sweat patches worn during the initial washout phase enabled investigation <strong>of</strong> excretion <strong>of</strong><br />
THC resulting from previously self- administered cannabis. The dosing phase <strong>of</strong> the study followed the<br />
initial washout phase, during which the participants were dosed three times a day for five consecutive days<br />
followed by a ten-day washout period before the next dosing session. All subjects ingested commercially<br />
available hemp seed oil <strong>of</strong> differing THC concentrations: 0, 0.39, 0.47 (contained within capsules), and<br />
14.8 mg THC/day. In addition, 7.5 mg/day dronabinol or Marinol, was administered as a positive control.<br />
PharmChek sweat patches collected throughout the study were frozen at _20DC until analysis. Patches<br />
were extracted in methanol: 0.2M sodium acetate buffer, pH 5.0, 3:1 v/v, followed by solid phase<br />
extraction using Clean Screen, ZSTHC020, (United Chemical Technologies, Bristol, PAl. Dried extracts<br />
were derivatized with trifluoroacetic acid (TFAA) and analyzed using gas chromatography negative<br />
chemical ionization mass spectrometry (GC-NCI-MS) for THC. Daily and weekly sweat patches collected<br />
during the initial washout period were analyzed along with weekly patches collected during and following<br />
dosing. None <strong>of</strong> the patches worn during or following dosing tested positive for THC with a cut<strong>of</strong>f <strong>of</strong> 0.4<br />
ng/patch. Patches worn during the first week <strong>of</strong> residence on the research unit, reflecting drug excretion<br />
from previously self-administered cannabis tested positive for THC in two individuals. The concentrations<br />
<strong>of</strong> THC were 0.51 and 0.82 ng THC/patch for patches worn for the first seven days on the research unit.<br />
These participants self-reported cannabis smoking an average <strong>of</strong> 3.0 and 4.5 days per week and claimed to<br />
have last used cannabis one to two days prior to study enrollment. However, these usage histories did not<br />
differ significantly from those reported by the other four subjects and whose sweat patches tested negative<br />
for THC. In conclusion, this study demonstrates that oral administration <strong>of</strong>THC at, as high a dose as 14.8<br />
mg/day for 5 consecutive days did not produce positive sweat tests for cannabinoids with a 0.4 ng<br />
THC/patch cut<strong>of</strong>f in patches worn for seven days. The cannabinoid confirmation cut<strong>of</strong>f for THC in sweat<br />
as proposed by the Substance Abuse Mental Health Services Administration is 1 ng THC/patch. It is<br />
important to note that the bioavailability <strong>of</strong> oral THC has been estimated to be 6 to 20% and plasma THC<br />
concentrations did not exceed 6.5 ng/mL following any <strong>of</strong> the dosing regimens during this study. These<br />
data indicate that previously administered THC in daily cannabis smokers did not produce positive<br />
cannabinoid sweat tests when patches were applied at the beginning <strong>of</strong> abstinence and worn for 7 days if a<br />
1.0 ng THC/patch cut<strong>of</strong>f is used. In addition, no sweat patches were positive at this cut<strong>of</strong>f when up to 14.8<br />
mg THC/day for 5 consecutive days was ingested by cannabis users. Ingestion <strong>of</strong> commercially available<br />
hemp oil products and Marinol up to 7.5 mg/day did not produce positive sweat cannabinoid tests.<br />
Keywords: /':,.9-Tetrahydrocannabinol, Oral Cannabinoids, Sweat Patch<br />
Page 321
M39 <br />
QUANTITATIVE ANALYSIS OF DEXTROMETHORPHAN, CARISOPRODOL AND THEIR<br />
METABOLITES IN HAIR BY GC-MS<br />
Wonkyung Yang l *, Eunyoung Han l , Yonghoon Park l ,Miae Lim', Myungyun Py02 and Heesun Chung I :<br />
INational Institute <strong>of</strong> Scientific Investigation, Seoul; 2Korea, School <strong>of</strong> Pharmacy, Sookmyung Women's<br />
University, Seoul, Korea<br />
Dextromethorphan, which is used as an antitussive agent, and carisoprodol, which is used as a muscle<br />
relaxant, have been widely abused among young people in Korea. Even though these are known to be very<br />
safe drugs for therapeutic use, people abused them for their hallucinogenic properties. Due to the serious<br />
abuse liability potential <strong>of</strong> these drugs, our government recently decided to control them as psychotropic<br />
agents. It was necessary for us to establish a detection method for dextromethorphan and carisoprodol and<br />
their metabolites in hair to demonstrate the abuse <strong>of</strong> these drugs. A method was established to<br />
simultaneous quantify dextromethorphan, dextrorphan, 3-methoxymorphinan, carisoprodol and<br />
meprobamate in hair samples. Analytes were extracted from fine cuttings <strong>of</strong> hair in 1 % HCI in methanol for<br />
16 hours. After evaporation under N2, residues were separated on a HP - 5MS column using a 16 min<br />
program and identified by mass spectrometry in the SIM mode (EI-GC-MS).This method was validated for<br />
the recovery, linearity <strong>of</strong> calibration, within-and between-day precision, accuracy, limit <strong>of</strong> detection and<br />
quantification. Calibration curves exhibited correlation coefficients > 0.99. Within and between-run<br />
precision was calculated at 8, 80 and 400 nglmg <strong>of</strong> drug or metabolite in hair with coefficients <strong>of</strong> variation<br />
less than 14 %, except for meprobamate (17%). Accuracy at the same concentrations was 14% <strong>of</strong>target for<br />
all analytes except meprobamate (18%). Recoveries at 10 and 100 ng <strong>of</strong> drug or metabolite in hair were 88<br />
to 117 %. With this method, we performed quantitative analysis <strong>of</strong> dextromethorphan and carisoprodol in<br />
abuser's hair. The concentrations <strong>of</strong> dextromethorphan, dextrorphan and 3-methoxymorphinan ranged from<br />
1.4 - 225.0, 1.3 - 44.7, and 0 - 42.7 nglmg in hair from 31 donors studied, respectively. The level <strong>of</strong><br />
carisoprodol and meprobamate were 2.3 - 52.9 and 11.3 - 365.1 ng/mg respectively in 11 hair samples. We<br />
present a validated, sensitive and specific GC-MS method to simultaneously quantify dextromethorphan,<br />
carisoprodol and metabolites in hair.<br />
Keywords: Dextromethorphan, Carisoprodol, Hair Analysis<br />
Page 322
M40 <br />
EV ALUA TION OF THE IDS ONE-STEP ELISA KIT FOR THE SCREENING OF KETAMINE IN<br />
HAIR<br />
C.Y. Yong*, H.S. Leong, and C.P. Lui: Narcotics II Laboratory, Centre for <strong>Forensic</strong> Science, Health<br />
Sciences Authority, 11 Outram Road, Singapore 16907S.<br />
An evaluation study was conducted with the commercially available ketamine microtiter plate enzymelinked<br />
immunoassay (ELISA) <strong>of</strong>International Diagnostic System (IDS), USA, in the screening <strong>of</strong>ketamine<br />
in hair. The assay principle is based on the competitive binding between the ketamine-enzyme conjugate<br />
and the free ketamine extracted from the hair for a limited number <strong>of</strong> antibody-binding sites. Aliquots <strong>of</strong>20<br />
III <strong>of</strong> the sample or calibrator was added to the antibody-coated microwell followed by 100 III <strong>of</strong> diluted<br />
enzyme conjugate. After an incubation period <strong>of</strong> 30 min at room temperature, any unbound material was<br />
removed with washing. An enzyme substrate was then added and further incubated for 15 min for the<br />
colour development. An acid stop solution was added to stop the reaction. The absorbance is measured at<br />
450 nm with 650 nm as the reference filter. The absorbance obtained is inversely proportional to the<br />
amount <strong>of</strong>ketamine present in the sample.<br />
During the sample preparation, the hair specimens were washed and decontaminated before being<br />
pulverized in a Retch ball mill. About 25 mg <strong>of</strong> the pulverized hair was digested overnight at 45°C in 1 ml<br />
<strong>of</strong> 0.5 M hydrochloric acid. The samples were allowed to cool before the addition <strong>of</strong> 1 ml <strong>of</strong> 0.5 M sodium<br />
hydroxide and 1 ml <strong>of</strong> phosphate buffer solution (pHS). 20 fll <strong>of</strong> the clear supernatant were used for the<br />
immunoassay.<br />
The objective <strong>of</strong> this study is to determine if a commercially available ELISA system was sufficiently<br />
sensitive for the routine screening <strong>of</strong>ketamine in hair. We evaluate the immunoassay performance in terms<br />
<strong>of</strong> precision, accuracy, efficiency, sensitivity and specificity. The limit <strong>of</strong> detection (LOD) <strong>of</strong> the kit was<br />
found to be 0.6 ng/mg. The linearity range for ketamine was found to be up to 4.3 ng/mg using spiked hair<br />
samples. The intra-day % CV (within-day precision) for ketamine at concentrations <strong>of</strong> 0.6, O.S and 1 ng/mg<br />
was found to be from 3.73 % to 6.12 %. Interference study was evaluated by measuring the extent <strong>of</strong> cross<br />
reactivity <strong>of</strong> various cOmmon drugs <strong>of</strong> abuse such as opiates, 11-nor-b. 9 -THC-9-carboxylic acid,<br />
amphetamines and their ring analogues, cocaine and its metabolites, benzodiazepines, buprenorphine and<br />
its metabolites, LSD and its metabolites with ketamine. All the drugs above do not interfere with the<br />
detection <strong>of</strong> ketamine using ELISA. Only a low cross-reactivity was observed for low concentrations <strong>of</strong><br />
norketamine.<br />
A total <strong>of</strong> 62 hair segments from suspected ketamine abusers were screened using the ELISA test kit. These<br />
hair specimens were obtained from suspected ketamine abusers. The effciency, sensitivity and specificity <strong>of</strong><br />
the immunoassay were evaluated in comparison with gas chromatography/ mass spectrometry (GCIMS)<br />
using these hair specimens. Confirmatory cut-<strong>of</strong>f for ketamine was 0.6 ng/mg. True positives, true<br />
negatives, false positives, and false negatives were determined using immunoassay cut-<strong>of</strong>f at 0.8 ng/mg and<br />
1.0 ng/mg. An optimum immunoassay cut-<strong>of</strong>f concentration <strong>of</strong> 1.0 ng/mg was determined for the kit. At<br />
this cut-<strong>of</strong>f, a total <strong>of</strong> 55 hair samples were screened positive and 7 screened negative. Comparing with<br />
GCIMS results, 2 false negatives and no false positives were determined. The immunoassay exhibited an<br />
efficiency <strong>of</strong> 96.7 %, a sensitivity <strong>of</strong>96.4 % and a specificity <strong>of</strong> 100 %.<br />
The results collected support that the IDS One-StepTM ELISA test kit provides a suitable preliminary<br />
screening procedure for the detection <strong>of</strong> ketamine in hair specimens. It <strong>of</strong>fers a rapid, sensitive, and<br />
effective method to determine the presence <strong>of</strong>ketamine in hair in suspected ketamine abusers.<br />
Keywords: ELISA, Ketamine, Hair Analysis<br />
Page 323
M41<br />
GAS CHROMATOGRAPHY:'HIGH-RESOLUTION MASS SPECTROMETRIC METHOD FOR<br />
DETERMINING METHAMPHETAMINE AND ITS MAJOR METABOLITE AMPHETAMINE<br />
IN HUMAN HAIR<br />
Jin Young Kim* and Moon Kyo In, Drug Analysis Laboratory, <strong>Forensic</strong> Science Division, Supreme Public<br />
Prosecutors' Office, Seoul 137-730, Korea<br />
Objective: The purpose <strong>of</strong> this study is I) to effectively eliminate the biological background or interference<br />
by cosmetic treatment and 2) to develop a suitable confirmatory procedure for analyzing methamphetamine<br />
(MA) and amphetamine (AMP) in human hair using a gas chromatography high-resolution mass<br />
spectrometric (GC-HRMS) technique.<br />
Nature <strong>of</strong>the study: GC-HRMS method development for detecting MA and its metabolite AMP containing<br />
an extremely low concentration in human hair, and eliminating co-eluted compounds in cosmetically<br />
treated hair samples.<br />
Material and methods: We measured the total length <strong>of</strong> hair samples, and noted special features such as<br />
coloring, bleaching, etc. Before we analyzed hair samples, we 1) washed them twice with 10 mL water and<br />
10 mL acetone, 2) then dried them under a fume hood, 3) finely cut the hair with scissors into small<br />
fragments below 1 mm, and 4) weighed each hair sample. We then transferred thirty milligrams <strong>of</strong> hair to a<br />
Teflon-faced, rubber-lined screw-cap test tube (16 x 100 mm). To extract analytes from the specimens, we<br />
added 2 mL <strong>of</strong> methanol-5 M hydrochloric acid (20:1, vlv) containing 100 ng <strong>of</strong> AMP-ds and MA-ds as<br />
internal standards into test tubes. Then, we directly extracted the hair samples under ultrasonication for lh<br />
and left them to stand at room temperature overnight. The hair was filtered <strong>of</strong>f and filtrate was evaporated<br />
under a nitrogen stream in a TurboVap LV evaporator (Zymark Corp., USA). We dissolved the dried<br />
sample in 50 ilL <strong>of</strong> trifluoroacetic anhydride (TFAA) and 50 ilL <strong>of</strong> ethyl acetate and placed it in a dry /~,<br />
heating block for the derivatization at 70°C for 30 min. The mixture was allowed to cool to room<br />
temperature. The residue was reconstituted with 40 ilL volume <strong>of</strong> ethyl acetate. We injected an aliquot (1<br />
ilL) <strong>of</strong> the sample solution into GC-MS.<br />
Results: With the HRMS method the limits <strong>of</strong> detection (LOD) were 9 pglmg for MA and 21 pg/mg for<br />
AMP using a 30 mg hair sample, and the SIM responses were linear with coefficients <strong>of</strong> correlation<br />
ranging from 0.9998 to 0.9999. The recoveries were found to be 91.1-92.3%. By using HRMS (resolution<br />
<strong>of</strong> 5000), we improved the detection sensitivity due to eliminating the biological background. The LODs<br />
for MA and AMP were 2.4-4.4 times lower than low-resolution mass spectrometry (LRMS). We applied<br />
the described method to hair samples from suspected MA abusers. In nineteen <strong>of</strong> the thirty hair samples<br />
not detected by the LRMS SIM technique, we confirmed AMP using an accurate HRMS SIM measurement<br />
<strong>of</strong> diagnostic ions. In cases where there is a low concentration <strong>of</strong> AMP in the hair, high resolution SIM is<br />
useful to eliminate chemical background, which is present in single-quadrupole LRMS due to solvent<br />
and/or matrix ionization. The HRMS technique makes the detection <strong>of</strong> rather low concentrations <strong>of</strong> drugs<br />
in hair samples possible. In this experiment, the hair samples analyzed using GC-HRMS are not specially<br />
prepared and are the same as those analyzed by GC-LRMS.<br />
Conclusion: The proposed GC-HRMS method shows a high sensitivity and specificity. This method can<br />
also be used as a suitable analytical tool for identirying AMP as major metabolite <strong>of</strong> MA in human hair,<br />
where identirying metabolites at a low amount in hair samples is requested, and especially in cosmetically<br />
treated hair.<br />
Keywords: Hair, GC-HRMS, Methamphetamine, Amphetamine<br />
Page 324
M42 <br />
A MIXED MODE SOLID-PHASE EXTRACTION METHOD FOR THE LC/MS<br />
DETERMINATION OF DRUGS OF ABUSE IN PRESERVED SALIVA<br />
Kevin M. Jenkins, Michael S. Young*: Waters Corporation, 34 Maple Street, Milford, MA<br />
Saliva is a less invasive alternative to urine or blood in forensics analysis for drugs <strong>of</strong> abuse. Because drug<br />
residues are typically less concentrated in saliva than in other biological fluids such as blood or urine,<br />
quantification limits for saliva samples must be considerably lower than for urine, in the low nglmL range.<br />
Compared with GCIMS, LCIMS is a simpler analytical approach requiring no derivatization. However, the<br />
saliva collection fluid contains ingredients (stabilizers and preservatives) that present some interference<br />
problems for LCIMS. A mixed-mode (cation-exchange) SPE cartridge, Oasis MCX, provided effective<br />
cleanup suitable for LCIMS determination <strong>of</strong> basic drugs <strong>of</strong> abuse in preserved saliva. The drugs studied<br />
were cocaine, codeine, morphine, amphetamine, methamphetamine, ecstasy (MDMA) and phencyclidine<br />
(PCP). MDMA-d5 was used as an internal standard. Calibration was accomplished in the range from 5 to<br />
250 ng/mL. Correlation coefficients (r2) for all constituents were better than 0.998. Reproducibility for all<br />
constituents was better than 10 % (RSD) for 6 replicate samples fortified at the 10 nglmL and 50 nglmL<br />
levels. Recovery was better than 85 % for all constituents.<br />
Keywords: Saliva, LCIMS, Drugs <strong>of</strong> Abuse<br />
Page 325
M43 <br />
COCAETHYLENE: A POTENTIALLY LETHAL TOXICANT<br />
Danyel H. Tacker* and Anthony O. Okorodudu: Department <strong>of</strong> Pathology, University <strong>of</strong> Texas Medical<br />
Branch, Galveston, TX, USA<br />
Introduction: Cocaethylene (CE) is an active metabolite <strong>of</strong> cocaine and ethanol, produced by the liver in a<br />
majority <strong>of</strong> cocaine abusers who concomitantly abuse ethanol. Though the mechanism <strong>of</strong> death associated<br />
with cocaine overdose has historically been relative to vasospasm and cardiac/cerebral infarct and failure,<br />
we propose a role for CE as a toxicant to the vascular endothelium. We investigated the effects <strong>of</strong>CE on<br />
microvascular endothelium to further characterize mechanisms <strong>of</strong> vasculotoxicity and associated tissue<br />
ischemia.<br />
Methods: An in vitro model <strong>of</strong> microvascular endothelial CE exposure (ImM) was used. Cytotoxicity<br />
assays included viability and LDH release analysis. Morphological (silver stain) and electricallresistance<br />
analysis was used to determine the effect <strong>of</strong> CE on monolayer permeability. Analysis <strong>of</strong> variance for n :: 3<br />
was significant when p
M44 <br />
FORENSIC ENTOMOTOXICOLOGY: A STUDY IN THE DEPOSITION OF BARBITURATES<br />
INTO THE LARVAE OF THE BLACK BLOW FLY, PHORMIA REGINA<br />
Michelle R. Peace, M.F.S.* and Alphonse Poklis, Ph.D., Department <strong>of</strong> Pathology and the <strong>Forensic</strong> Science<br />
Program, Virginia Commonwealth University, Richmond VA 23284<br />
Due to events in severe decomposition, either no s<strong>of</strong>t tissue remains on which to perform a toxicological<br />
analysis or putrefactive fluids complicate and interfere with the analysis <strong>of</strong> the s<strong>of</strong>t tissues. The purpose <strong>of</strong><br />
this experiment was to study the trends in the deposition <strong>of</strong> barbiturates into the larvae <strong>of</strong> the black blow<br />
fly, Phormia regina, in order to better understand the value <strong>of</strong> entomological evidence as toxicological<br />
specimens. Drug deposition was analyzed by linear regression to find a correlation between whole larvae<br />
drug concentration and food source drug concentration. P. regina larvae were raised at 21°C on pork<br />
homogenized with three concentrations <strong>of</strong> barbital (200, 400, 800mglkg), phenobarbital (20, 40, 80mglkg),<br />
pentobarbital (20, 40, 80mglkg), and thiopental (15.5, 31, 62mglkg). The middle dosage <strong>of</strong> each drug<br />
reflected the LDso <strong>of</strong> the drug in rabbits. At the end <strong>of</strong> the feeding stage, the larvae were harvested,<br />
washed, and frozen. Ten larvae were subsequently homogenized, diluted in 2 ml water, and subjected to a<br />
liquid-liquid extraction. The extracted drugs were derivatized with MethElute and analyzed by GCiMS. In<br />
the concentration ranges investigated, the concentrations <strong>of</strong> barbital, phenobarbital, pentobarbital, and<br />
thiopental found in the larvae strongly correlated with the concentration <strong>of</strong> the drug in the food source (R 2<br />
= 0.9976, 0.9914, 0.8938, and 0.9095, respectively). Larvae feeding on pork homogenized with 800mglkg<br />
<strong>of</strong> barbital accumulated 1.8 times more drug than those feeding on 200mgikg. Larvae which fed on the<br />
high concentrations <strong>of</strong> phenobarbital, pentobarbital, and thiopental accumulated, respectively, 3.1, 5.4, and<br />
68.5 times more drug than those that fed on the low concentrations <strong>of</strong> drugs. This data indicated that as the<br />
Iipophilicity <strong>of</strong> the drug increased, the larvae accumulated significantly more drug.<br />
Keywords: Entomology, Toxicology, Barbiturates<br />
Page 327
M45 <br />
DETECTION OF COTININE IN EXHALED BREATH BY GAS CHROMATOGRAPHY-MASS<br />
SPECTROMETRY: A PRELIMINARY STUDY<br />
3<br />
Michele L. Merves J *, Chris W. Chronister l , Bruce A. Goldberger l • , Richard J. Melker and Mark S. Gold 3 • 4 :<br />
University <strong>of</strong> Florida College <strong>of</strong> Medicine, IDepartment <strong>of</strong> Pathology, Immunology and Laboratory Medicine;<br />
2Department <strong>of</strong> Anesthesiology; JDepartment <strong>of</strong> Psychiatry, Division <strong>of</strong> Addiction Medicine; 4Departrnents <strong>of</strong><br />
Neuroscience, Community Health and Family Medicine; 'Gainesville, FL; 4800 S.W. 35 th Street, Gainesville,<br />
FL 32608.<br />
Exhaled breath analysis is a very useful diagnostic tool in the fields <strong>of</strong> medicine and forensic science. Exhaled<br />
breath is routinely used to detect markers <strong>of</strong> disease, as well as correlate ethanol concentrations with effects on<br />
human performance and behavior (DUI). Compared to other biological specimens, the collection <strong>of</strong> exhaled<br />
breath is simple and non-invasive, with minimal exposure to infectious material. Because exhaled breath is a<br />
physiological waste product, the quantity available exceeds those <strong>of</strong> other biological matrices such as blood and<br />
urine. In addition, little sample preparation is required. Finally, exhaled breath accounts for all routes <strong>of</strong> drug<br />
exposure including oral ingestion, injection, inhalation, and dermal absorption.<br />
This is a preliminary study to determine if cotinine, an oxidative metabolite <strong>of</strong> nicotine, is detectable in exhaled<br />
breath <strong>of</strong> humans. Cotinine was chosen as a metabolic marker <strong>of</strong> nicotine use because <strong>of</strong> its long half-life<br />
compared to nicotine. Exhaled breath specimens were collected onto commercially-available XAD-4 traps<br />
(Supelco) and analyzed by gas chromatography-mass spectrometry (GC-MS). The resin, XAD-4, is a polymeric<br />
adsorbent available as beads within a small glass tube (70 mm x 6 mm). Upon collection <strong>of</strong> the exhaled breath,<br />
the resin was removed, fortified with drcotinine (Cerilliant Corporation), and sonicated in methanol for 30<br />
minutes. The organic layer was separated from the resin and dried under a gentle stream <strong>of</strong> nitrogen at 40°C. The<br />
residue was reconstituted in phosphate buffer (PH 6). The cotinine was isolated from the buffer utilizing<br />
CleanScreen® solid-phase· extraction (SPE) cartridges (ZSDAU020) manufactured by United Chemical<br />
Technologies, Inc. Following elution from the SPE cartridges using a solution <strong>of</strong>methylene chloride, isopropanol,<br />
and ammonium hydroxide, the extracts were dried under a gentle stream <strong>of</strong> nitrogen at 40°C and reconstituted in<br />
methanol. The extracts were subjected to GC-MS analysis using an Agilent Technologies 6890N series gas<br />
chromatograph equipped with a Agilent Technologies 5973 network mass spectrometer operated in electron<br />
ionization and selected ion monitoring (SIM) modes. Helium was used as the carrier gas at a constant flow rate <strong>of</strong><br />
1.0 mLimin. Automated injections (2-3 ).iL) were made onto a capillary GC column. The ions (mlz) monitored<br />
for cotinine were 98.1, 175.1 and 176.1, and the ions (mlz) monitored for d 3 -cotinine were lOLl and 179.1.<br />
Initial studies have demonstrated cotinine in the exhaled breath <strong>of</strong> cigarette smokers, while cotinine was not<br />
detected in control (non-smokers) exhaled breath. These data will serve as a model for detection <strong>of</strong> other<br />
compounds (drugs and their metabolites) present in exhaled breath which may be beneficial for many other<br />
medical, forensic, and toxicological applications.<br />
Keywords: Cotinine, Exhaled Breath, GC-MS<br />
Page 328
M46 <br />
"THE MECONIUM PROJECT": AN ITALIAN-SPANISH JOINT STUDY TO ASSESS<br />
EXPOSURE TO ILLICIT DRUGS DURING PREGNANCY AND BIRTH OUTCOMES<br />
S. Pichini*, P. Zuccaro, E. Marchei, M. Pellegrini, J Murillo, C. Puig, O. Vail, R. Pacifici, 6 Garcia-Algar:<br />
Istituto Superiore di Sanita, Rome Italy, V. Le Regina Elena 299, Rome, RM 00161, Italy<br />
Servicio de Pediatria, Hospital del Mar, Barcelona, Spain<br />
The accurate assessment <strong>of</strong> fetal exposure to drugs <strong>of</strong> abuse through the objective measure <strong>of</strong> biomarkers<br />
could provide the basis for appropriate treatment and follow-up <strong>of</strong> new-borns, which can present symptoms<br />
<strong>of</strong> drug withdrawal. Furthermore, information regarding the real prevalence <strong>of</strong> drugs <strong>of</strong> abuse use during<br />
pregnancy could also be disclosed.<br />
For the first time in Europe the "Meconium Project" aimed to estimate the prevalence <strong>of</strong> drug use by<br />
pregnant women and the effects <strong>of</strong> exposure to illicit drugs during pregnancy on the mother, fetus, and<br />
infant.<br />
Between September 2002 and February <strong>2004</strong>, among the mother-infant dyads from the Hospital del Mar,<br />
the fourth biggest hospital <strong>of</strong> the city, 1439 dyads met eligibility criteria and 1151 (79%) <strong>of</strong> those eligible<br />
agreed to participate in the study. Exposure was defined as an admission <strong>of</strong> use <strong>of</strong> cocaine, opiates or<br />
amphetamines by structured interview or the presence <strong>of</strong> drugs and their metabolites in 24 and 48 h<br />
meconium as determined by use <strong>of</strong> liquid chromatography-mass spectroscopy assay. Nonexposure was<br />
defined as a negative drug use history by interview and a negative analytical result. When exposure could<br />
not be confirmed, such as when meconium was not obtained or was inadequate for confirmatory analysis,<br />
the mother-infant dyad was excluded (n =288).<br />
Preliminary results on the analyzed 497 mother-infant dyads showed that structured interview disclosed a<br />
0.8, 1.8 and 2.2% mothers exposed to opiates, cocaine and both drugs while only one mother declared<br />
ecstasy consumption. Meconium analysis showed that prevalence <strong>of</strong> opiates, cocaine and combined drugs<br />
exposure was 9.1,3.8 and 10.7%, respectively and confirmed the case <strong>of</strong> ecstasy use. Arecoline, the main<br />
Areca nut alkaloid, was found in meconium specimens from 4 out <strong>of</strong> 10 Asiatic newborns, whose mothers<br />
declared areca nut consumption during pregnancy.<br />
A similar percentage <strong>of</strong> drug-exposed mothers were found between Spanish, American and African women<br />
(11.5,9.9 and 8.6%, respectively), while only a 6.3% Asiatic women resulted drug consumers. Exposure<br />
status caused a significant low birth weight in newborns from mothers exposed to cocaine (mean and S.D.=<br />
2848 ± 315 g in newborns from cocaine mothers vs 3262 ±504 g in newborns from non-exposed mothers).<br />
Other somatometric differences included crown-heel height.<br />
Of the 4 newborns exposed to arecoline, one showed a low birth weight, low intrauterine growth,<br />
hyporefiexia, hypotonia and a second presented a withdrawal neonatal syndrome by Finnegan test.<br />
In conclusion, these preliminary findings indicate a prevalence <strong>of</strong> opiates, cocaine and amphetamines<br />
consumption during pregnancy in this mixed mediterranean and non-european population lower that that<br />
reported in the North-american pregnant women. The higher sensitivity <strong>of</strong> meconium analysis, already<br />
demonstrated, in comparison to maternal interview, was confirmed making this test ideal for screening<br />
maternal and fetal exposure to conventional and non-conventional drugs <strong>of</strong> abuse during pregnancy.<br />
Keywords: Drugs <strong>of</strong>Abuse, Exposure, Pregnancy<br />
Page 329
M47 <br />
METHAMPHETAMINE AND AMPHETAMINE CONCENTRATIONS IN MECONIUM OF<br />
NEONATES OF WOMEN ENROLLED IN THE IDEAL STUDY OF IN UTERO<br />
METHAMPHETAMINE EXPOSURE<br />
2<br />
Zirong Zhao!, Jing Liu , Linda L. LaGasse 2 , Chris Derauf, Penny Gran!, Rizwan Shah 2 Amelia Arria"<br />
William Haning 2 , Lynne M. Smith 2 , Barry Lester" and Marilyn A. Huestis l *: I Che~istry and Dru~<br />
Metabolism, IRP, NIDA, NIH, Baltimore, MD 21224; .2 IDEAL Community Research Network<br />
Background: Tobacco, cannabis and methamphetamine (MA) use by pregnant women can negatively impact<br />
child development. The Infant Development, Environment, and Lifestyle (IDEAL) study is a multi-center,<br />
longitudinal investigation <strong>of</strong> the effects <strong>of</strong> prenatal methamphetamine exposure. Meconium, a useful matrix for<br />
identifYing in utero drug exposure, was employed to identify gestational drug use. Little published data are<br />
available on MA detection in meconium.<br />
Objective: To characterize the detection and quantification ~f MA, tobacco and cannabis in meconium compared<br />
to self-report.<br />
Method: Mothers who used tobacco, cannabis or alcohol during pregnancy were included in both MA-exposed<br />
and control groups. Meconium samples were analyzed by EMIT (USDTL) for cannabinoids, cocaine, opiates,<br />
amphetamines with cut<strong>of</strong>f concentrations <strong>of</strong> 40, 75, 150 and 500 nglg, respectively. Positive samples were<br />
confirmed by GC/MS with cut<strong>of</strong>fs <strong>of</strong> 2 nglg for II-nor-L'l.9-carboxy-THC and 5 nglg for cocaine,<br />
benzoylecgonine (BE), m-OH-BE, and cocaethylene, morphine, codeine, hydrocodone, hydromorphone, and<br />
MA, amphetamine (AMP), and MDMA. Tobacco use was identified with an ELISA cotinine screen<br />
(International Diagnostics Systems Corp., cut<strong>of</strong>f to nglg).<br />
Results: Of the 13,808 mothers screened, 1631 were consented and 176 enrolled. MA exposed mothers (n=84)<br />
were identified by self-report <strong>of</strong> gestational MA use and/or GCIMS confirmation <strong>of</strong> MA, AMP, and/or MDMA<br />
in infant meconium. Comparison participants (n=92) were matched by race, birth weight, maternal education<br />
and type <strong>of</strong> insurance, denied amphetamines use and had negative meconium results. Among the 1631 mothers,<br />
self-reported use rates were 5.2% (amphetamines), 25% (tobacco) and 5.9% (cannabis). Positive meconium<br />
screening rates were 3.6% for any amphetamine, 20% cotinine and 11.2% cannabis. For specimens that screened<br />
positive, 40.7% <strong>of</strong> amphetamines and 20.2% <strong>of</strong> cannabis specimens were confirmed. EMIT sensitivity and<br />
specificity were checked by reanalyzing 35 specimens from babies <strong>of</strong> women who reported MA use but had a<br />
negative screen and 35 specimens from the control group that also tested negative. All controls' meconium<br />
specimens were negative by GClMS (5-nglg), while 4 <strong>of</strong>35 specimens from self-reporters that screened negative<br />
were found positive by GCIMS, albeit at low concentrations (MA 8 52 and AMP 5 - 26 nglg meconium).<br />
Users reported administering MA by the fonowing routes: 48% smoked; 9% injected, II % sniffed, 6% ingested<br />
and 26% used multiple routes <strong>of</strong> administration. On average, 68% <strong>of</strong> the meconium from neonates whose<br />
mothers reported 3 nl trimester use had detectable MA, while detection rates were :::;10% for self-reported use<br />
during the 1 st and/or 2nd trimesters. Mean±SD, median and range <strong>of</strong>MA concentrations were 3674 ± 3406, 2623,<br />
479 to 13,431 nglg meconium and AMP 569 ± 543, 403, 30 to 2000 nglg meconium in infants whose mothers<br />
reported 3 nl trimester use. However, the highest MA (19,376 and 16,976 nglg) and AMP (2765 ng/g)<br />
concentrations were found in <strong>of</strong>fspring born to women who reported MA use only in the 1 st or 1 5t and 2 nd<br />
trimesters, raising questions about the self-report. The log transformed meconium MA concentrations<br />
significantly correlated with the frequency <strong>of</strong>MA use in the 3 nl trimester (r=0.645, P=O.004), although variability<br />
prevents prediction <strong>of</strong> frequency <strong>of</strong> use for an individual mother. AMP was always detected in MA positive<br />
meconium. In 55% <strong>of</strong> the GCMS positive samples, the ratios <strong>of</strong> amphetamine to MA were 0.1 to 0.2; 14% were<br />
less than 0.1 and 18% were 0.2 to 0.3.<br />
Limitations: Data are preliminary as the IDEAL study continues to recruit; larger samples in the future may<br />
strengthen or refute interim observations.<br />
Conclusions: Meconium analysis for MA is a useful adjunct to self-report for identification <strong>of</strong> MA exposure;<br />
however, the [reatest sensitivity was achieved with specimens collected from <strong>of</strong>fspring <strong>of</strong> women who reported<br />
use in the 3 r trimester. Further research is needed to determine if there are additional MA metabolites in<br />
meconium that could improve the identification <strong>of</strong> MA-exposed infants.<br />
Keywords; Methamphetamine, Meconium, In Utero Exposure<br />
Page 330
M48 <br />
PASSIVE CANNABIS SMOKE EXPOSURE AND ORAL FLUID TESTING<br />
1* I I I 1<br />
Keith Kardos ,Sam Niedbala, Sal Salamone, Dean Fritch, Matth Bronsgeest and Edward J. Cone 2 ; I<br />
OraSure Technologies, Bethlehem, PA, and 2 ConeChem Research, LLC, Severna Park, MD<br />
Illicit cannabis use continues to be highly prevalent in the United States. Oral fluid testing for /19<br />
tetrahydrocannabinol (THe) provides a convenient means <strong>of</strong> detection <strong>of</strong> recent usage. In this study, the<br />
risk <strong>of</strong> positive oral fluid tests from passive cannabis smoke exposure was investigated by housing four<br />
cannabis-free volunteers in a small, unventilated and sealed room with an approximate volume <strong>of</strong> 36 m 3 •<br />
Five active cannabis smokers also were present in the room and each smoked a single cannabis cigarette<br />
which contained an average <strong>of</strong> 1.75% THC. Cannabis smoking occurred over the first 20 minutes <strong>of</strong> the<br />
study session. All subjects remained in the room for approximately 4 hrs and provided oral fluid and urine<br />
specimens at designated times. Oral fluid specimens were collected with the Intercept DOA Oral Specimen<br />
Collection Device before the start <strong>of</strong> the session and periodically throughout the session. Three urine<br />
specimens were collected (0, 20 and 245 min), In addition, three air samples were collected (first 5 min<br />
during smoking, for 20 min immediately following smoking, and at 65-100 min after start <strong>of</strong> session) for<br />
measurement <strong>of</strong> THC concentrations in air. All oral fluid specimens were screened by enzyme<br />
immunoassay (EIA) for cannabinoids (cut<strong>of</strong>f concentration == 3 ng/mL) and tested by GC-MS-MS for THC<br />
(LOQILOD = 0.25 ng/mL). All urine specimens were screened by EIA for cannabinoids (cut<strong>of</strong>f<br />
concentration =50 nglmL) and tested by GC-MS-MS for THCCOOH (LOQ/LOD 1 nglmL). Air samples<br />
were measured for THC by GC-MS (LOD = I ng/L). A total <strong>of</strong> eight oral fluid specimens (collected 20 to<br />
50 min following initiation <strong>of</strong> smoking) from the four passive subjects screened and confirmed positive for<br />
THC at concentrations ranging from 3.6-26.4 ng/mL. Two additional specimens from one passive subject,<br />
colIected at 50 and 65 min, screened negative but contained THC in concentrations <strong>of</strong> 4.2 and 1.1 ng/mL,<br />
respectively. All subsequent specimens for passive participants tested negative by EIA and GC-MS-MS for<br />
the remainder <strong>of</strong> the 4 hr session. All urine specimens collected during the session from the passive<br />
participants screened and confirmed negative at LOQ/LOD by GC-MS-MS with the exception <strong>of</strong> one<br />
subject whose specimen collected at the end <strong>of</strong>the session contained 3.4 ng/mL <strong>of</strong>THCCOOH by GC-MS<br />
MS. In contrast, oral fluid specimens collected from the five cannabis smokers generally screened and<br />
confirmed positive for THC throughout the session at concentrations substantially higher than observed for<br />
passive subjects. Urine specimens from cannabis smokers also screened and confirmed positive at<br />
conventional cut<strong>of</strong>f concentrations. Based on the limited air sample measurements, it was estimated that<br />
passive subjects inhaled a total <strong>of</strong> approximately 0.05 mg <strong>of</strong> THC during the exposure session. A biphasic<br />
pattern <strong>of</strong> decline for THC was observed in oral fluid specimens collected from cannabis smokers, whereas<br />
a linear decline was seen for passive subjects suggesting that initial oral fluid contamination is cleared<br />
rapidly and is followed by THC sequestration in the oral mucosa. It is concluded that the risk <strong>of</strong> positive<br />
oral fluid tests from passive cannabis smoke inhalation is limited to a period <strong>of</strong> approximately one hour<br />
following exposure.<br />
Keywords; Cannabis, THC, Passive, Oral Fluid<br />
Page 331
M49<br />
DISPOSITION OF NJ-TETRAHYDROCANNABINOL IN ORAL FLUID AND PLASMA AFTER<br />
CONTROLLED ADMINISTRATION OF SMOKED CANNABIS<br />
Edward J. Cone 1 * and Marilyn A. Huestis 2 : I ConeChem Research, LLC, Severna Park, MD; 2 National<br />
Institute on Drug Abuse, 5500 Nathan Shock Drive, Baltimore, MD'<br />
Understanding the relationship <strong>of</strong> A9-tetrahydrocannabinol (THC) concentrations in oral fluid and plasma<br />
is important in interpretation <strong>of</strong> oral fluid test results. Current evidence suggests that THC is deposited in<br />
the oral cavity during cannabis smoking. This "depot" represents the primal)' or sole source <strong>of</strong> THC found<br />
when oral fluid is collected and analyzed. In this research, oral fluid and plasma specimens were collected<br />
from six subjects following smoking <strong>of</strong> cannabis cigarettes containing 1.75% and 3.55% THC. There was<br />
at least one week between each cannabis administration. Plasma specimens were analyzed by GC-MS and<br />
paired oral fluid specimens were analyzed by radioimmunoassay (RIA). In addition, one individual's oral<br />
fluid specimens were also analyzed by GCIMS. These data are unique in that they represent simultaneous<br />
or near simultaneous collection <strong>of</strong> oral fluid and plasma specimens in subjects following controlled<br />
cannabis dosing. The first oral fluid specimen, collected from one subject at 0.2 hr following initiation <strong>of</strong><br />
smoking, contained a THC concentration <strong>of</strong> 5800 ng/mL (GC-MS). By 0.33 hr, the THC concentration in<br />
oral fluid had fallen to 81 nglmL. From approximately 0.3 hr through 4.0 hr, the mean (± SD) THC ratio <strong>of</strong><br />
oral fluid to plasma THC concentrations was LI8 (0.62) with a range <strong>of</strong> 0.5 to 2.2. Within 12 hr, both oral<br />
fluid and plasma THC concentrations generally declined below 1 nglmL. RIA analyses <strong>of</strong> oral fluid<br />
specimens for six subjects demonstrated the same pattern <strong>of</strong> initial high levels <strong>of</strong> contamination<br />
immediately after smoking, followed by rapid clearing, and a slower decline over 12 hr. Mean THC oral<br />
fluid concentrations by RIA at 0.2 hr were 864 nglmL and 4167 nglmL compared to plasma concentrations<br />
<strong>of</strong> 52 ng/mL and 230 ng/mL at 0.27 hr following the low and high dose cannabis cigarettes, respectively.<br />
The similarity in oral fluid and plasma THC concentrations following the dissipation <strong>of</strong> the initial<br />
"contamination" indicates the likelihood <strong>of</strong> a physiological link between these specimens. Recent studies<br />
have shown that sublingual or transmucosal administration <strong>of</strong> pure THC results in direct absorption <strong>of</strong>'~'<br />
intact THC into the bloodstream, thereby bypassing the gastrointestinal tract. The current study<br />
demonstrates that THC is deposited in the oral cavity and remains for up to 24 hr following cannabis<br />
smoking. The decline in THC oral fluid concentration over this time suggests that there may be absorption<br />
<strong>of</strong> THC into blood as previously shown with pure THC. Passive cannabis exposure studies appear to<br />
indicate that positive oral fluid tests for THC can occur shortly after cannabis smoke exposure, but results<br />
were negative within one hour. Consequently, when vel)' recent passive exposure to cannabis smoke can<br />
be ruled out, it is concluded that a positive oral fluid test provides credible evidence <strong>of</strong> active cannabis use.<br />
Keywords: Cannabis, THC, Oral Fluid, Depot<br />
Page 332
M50 <br />
DETECTION OF DRUGS OF ABUSE USING ORAL FLUID WITHIN A PAROLE SETTING<br />
Ann Snyder'*, Tiffany Miller\ Eileen Sevem 2 , Chris CiottiZ, Dean Fritch 2 , Sal Salamone 2 , Keith Kardos 2 ,<br />
R. Sam Niedbala 2 :: 'Cuyahoga County Court <strong>of</strong> Common Pleas Laboratory, 1276 West Third St,<br />
Cleveland, OH 44113; 2 OraSure Technologies, 150 Webster St, Bethlehem PA 18015.<br />
A study was conducted using rapid on-site and lab based oral fluid tests as well as urine for drugs <strong>of</strong> abuse<br />
detection in a probation facility that requires routine testing <strong>of</strong> participants. Individuals in this facility are<br />
required to routinely visit with a probation <strong>of</strong>ficer. As part <strong>of</strong> their visit a urine specimen is collected, any<br />
presence <strong>of</strong> drug is punishable and grounds for revocation <strong>of</strong> probation. This study was organized to<br />
compare new technologies for on-site and lab-based oral fluid tests comparing them to routine urinalysis.<br />
On-site oral fluids were determined using the UPlink Test System. UPlink is based on instrumented<br />
analysis <strong>of</strong> lateral flow chromatography using Up-Converting Phosphors. Lab-based oral fluids were<br />
determined using the Intercept System. The Intercept oral fluid collection device gathers an average <strong>of</strong><br />
OAmL <strong>of</strong> oral fluids, which is express-sent to a laboratory. After isolation <strong>of</strong> the sample, Intercept<br />
specimens are screened using microplate assays followed by GCMSMS confirmation <strong>of</strong> positive samples.<br />
Urine analysis was performed using Microgenics Inc. reagents on a Hitachi 917. A total <strong>of</strong>217 specimens<br />
were tested in oral fluids. A total <strong>of</strong> 207 specimens were tested with urine due to problems with subjects<br />
unable to provide a specimen. Positive samples were found in all fluids for all major classes <strong>of</strong> drugs<br />
including cocaine, THC, opiates, PCP and amphetamines. True Positives and True Negatives were judged<br />
based upon manufacturers recommendations for oral fluids and Substance Abuse and Mental Health<br />
Services Administration Federal workplace drug testing guidelines for urine, with the exception <strong>of</strong> opiates,<br />
which use a 300 nglmL cut<strong>of</strong>f. Overall, the % agreement when comparing on-site UPlink and lab-based<br />
Intercept results to GCMSMS was 98.7% and 99.6% respectively. Overall % agreement between urine<br />
screening results and GCMS was 99.8%. These results demonstrated the analytical performance <strong>of</strong> either<br />
oral fluid test system was comparable to lab-based urine testing. However, collection <strong>of</strong> oral fluid negated<br />
the requirements for special facilities allowing probation <strong>of</strong>ficers to directly observe collections.<br />
Keywords: Oral Fluid, Urine Drug Testing, Drugs <strong>of</strong>Abuse<br />
Page 333
MSl<br />
DISPOSITION OF COCAINE AND METABOLITES IN HUMAN SWEAT FOLLOWING<br />
CONTROLLED COCAINE ADMINISTRATION<br />
Sherri L. Kacinkol*, Allan J. Barnes l , Eugene W. Schwilke 1 , Jonathan M. Oyler 2 , Edward J. Cone\ Eric T.<br />
Moolchan\ and Marilyn A. Huestis l : IChemistry and Drug Metabolism Section, Intramural Research<br />
Program, NIDA, NIH, 5500 Nathan Shock Drive, Baltimore, MD 21224; 2Department <strong>of</strong> the Army, US<br />
Army Research, Development and Engineering Command, 5183 Blackhawk Road, Aberdeen Proving<br />
Ground, MD 21010 ; 3ConeChem Research, LLC. 441 Fairtree Drive, Serverrna Park, MD 21146<br />
The analysis <strong>of</strong> sweat for drugs <strong>of</strong> abuse <strong>of</strong>fers a convenient, non-invasive technique for monitoring drug<br />
exposure. Sweat can be collected using the Pharmchek® Sweat Patch; an absorbent cellulose pad with<br />
adhesive backing that is worn on the body. The comparison <strong>of</strong> sweat test results to urinalysis indicates that<br />
sweat may be an acceptable matrix for drugs <strong>of</strong> abuse screening for drug treatment, criminal justice, and<br />
employment screening purposes.<br />
Healthy volunteers (n=8), with a history <strong>of</strong> cocaine (COC) use, provided informed consent to participate in<br />
this IRB approved research study and resided on the closed ward throughout the 12-week study. After an<br />
initial three-week washout period, volunteers received 3 low dose (15 mg/10 kg) subcutaneous injections <strong>of</strong><br />
cocaine HCI on every other day and, three weeks later, 3 high doses (150 mgl10 kg).<br />
Pharmchek® Sweat Patches collected for up to 48 hours following the first low (n=82) and high (n=18)<br />
doses were isolated for cocaine and eleven metabolites by solid phase extraction and analyzed by GCIEI<br />
MS. LOD and LOQ were 2.5 ng/patch for COC, ecgonine methyl ester (EME), benzoylecgonine (BE) and<br />
meta- and para-hydroxycocaine (m- poOH-COC)o<br />
COC was the primary analyte detected in patches worn for 1-15 hours after the first low (26 <strong>of</strong> 82, 32%<br />
positive patches) and high (36 <strong>of</strong>18, 46% positive patches) doses. COC Cmax ranged from 6-64 ng/patch<br />
and 5-315 ng/patch following low and high doses, respectively. Not only was there large variability in<br />
Cmax, but there also was wide variability for the time <strong>of</strong> Cmax. Several patches (2 <strong>of</strong> 21 for low dose and<br />
6 <strong>of</strong> 26 for high dose) worn for four or less hours were positive for COC 24-48 hours after administration.<br />
Half <strong>of</strong> the participants had positive COC results for both low and high dose sweat patches applied 32<br />
hours after dose and worn for 15 hours, demonstrating improved detection in patches worn for extended<br />
periods.<br />
EME was detected in sweat patches collected from 3 participants after low dose (1% positive patches) and<br />
4 participants after the high dose (13% positive patches) and was detected only in patches collected for the<br />
first 24 hours after dosing. Maximum EME concentrations ranged from 8-41 ng/patch and 5-51 ng/patch<br />
for the low and high dose, respectively. BE was detected in 6% <strong>of</strong> the low and 8% <strong>of</strong> the high dose patches.<br />
with concentration ranges <strong>of</strong> 5-13 ng/patch after low dose and 6-12 ng/patch after high dose. One<br />
participant had a positive m-OH-COC patch (3 ng/patch) after high dose administration. In addition, m<br />
and p-OH-COC were detected concurrently in the 2-4 hour (3 ng/patch m-OH-COC, 6 ng/patch p-OH<br />
COC) and 8-23 hour (3 ng/patch m-OH-COC and 5 ng/patch p-OH-COC) patches collected from one<br />
participant after the high dose.<br />
COC, BE and EME can be detected within 2 hours <strong>of</strong> drug administration but there is wide intra- and intersubject<br />
variability in the amount detected and the time at which Cmax is reached. During the 24 hours after<br />
exposure COC can be detected in patches worn for short periods (1-2 hours) but after 24 hours the patch<br />
must be worn for longer periods to detect COCo EME was detected more <strong>of</strong>ten and at higher<br />
concentrations than BE; both were detected only within the first 24 hours after exposure.<br />
Sweat testing for COC and BE has been proposed by the Substance Abuse and Mental Health Services<br />
Administration for federally-mandated workplace drug testing with patches worn for 1-14 days. In this<br />
study patches were only worn for 15 hours. It should be noted, however, that EME was detected more<br />
frequently and at higher concentrations than BE.<br />
Keywords: Cocaine, Sweat, Controlled Cocaine Administration<br />
Page 334
Scientific Session <br />
<strong>Abstracts</strong>: <br />
Postmortem <br />
Toxicology <br />
Page 335
PI <br />
NEW GENERATIONS OF ANTIDEPRESANTS IN FATAL INTOXICATIONS<br />
Marie Stankova*, Petr Kurka, 1. DvoraCek<br />
Institute <strong>of</strong> <strong>Forensic</strong> Medicine, University Hospital, Ostrava, Czech Republic<br />
New generations <strong>of</strong> antidepresants are widely used for treatment <strong>of</strong> various types <strong>of</strong> depressive and other<br />
disorders. These drugs have a relatively low toxicity, and fatalitiesexclusively from these newer drugs are<br />
uncommon.<br />
The authors describe six cases <strong>of</strong> fatal intoxications with a combination <strong>of</strong> some newer antidepresant with<br />
other drugs. Although these newer antidepresants are relatively safe, in combination with other drugs<br />
(especially with psychoactive drugs) they can cause death.<br />
There drugs were isolated from biological specimes using either a diethyl ether extraction for qualitative<br />
analysis or by solid phase extraction for quantitative analysis.<br />
Detection <strong>of</strong> drugs in biological specimes (urine, gastric contents, liver, kidney) was performed by thin<br />
layer chromatography/colour reactions (TLC/CR) and confirmed by gas chromatography/mass<br />
spectrometry method (GC/MS). Concentrations <strong>of</strong> drugs in postmortem bloods (subclavian artery blood)<br />
were determined using GC/MS method.<br />
'<br />
The results are presented in the table:<br />
case gender/age antidepressant blood lev. other drugs blood lev.<br />
1. F/41 citaloprarn 0.80 Promethazine 10.20<br />
2. F/47 moclobemide 18.20 7.44<br />
3. M/50 mianserin 1.33 0.51<br />
Dosulepin 2.76<br />
4. M/38 moclobemide 32.00 Promethazine 19.00<br />
Alcohol<br />
5. M/51 citalopram 1.24 Levomepromazine<br />
ketamine<br />
6. M/37 citaloprarn 2.39 Morphine<br />
blood (subclavian artery) level: mg/I - drugs, g/kg - alcohol<br />
NQ - no quantification<br />
Keywords: new antidepresants, overdose, GCMS<br />
Page 336
P2 <br />
IT'S ONLY JUST BEGUN A POSTMORTEM TISSUE DISTRIBUTION OF STRATTERA® OR<br />
A TOMOXETINE IN TWO FATALITIES<br />
Dan Anderson"', Kristina Fritz, Michelle Sandberg, Jamie Lintemoot, Sara Kegler, and Joseph J. Muto<br />
Los Angeles County Dept. a/Coroner, 1104 N. Mission Road, Los Angeles, CA 90033<br />
Stratterl~ or Atomoxetine is a selective norephinephrine reuptake inhibitor approved by the Food and Drug<br />
Administration in December 2002. It is considered the first non-stimulant treatment <strong>of</strong> attention deficit<br />
hyperactivity (ADHD) in both children and adults. Atomoxetine is prescribed in lO, 18,25,40, and 60-mg<br />
dose capsules. Since Strattera® has entered the market, the Los Angeles County Dept. <strong>of</strong> Coroner<br />
Toxicology Laboratory has only encountered two cases where atomoxetine was detected. Presented are the<br />
case histories, cause and manner <strong>of</strong> death, the postmortem tissue distribution <strong>of</strong> atomoxetine, all designed<br />
to aid the forensic toxicologist with the interpretation <strong>of</strong> their own casework.<br />
The analysis <strong>of</strong> atomoxetine from postmortem specimens consisted <strong>of</strong> a basic, Iiquid/liquid (nbutylchloride)<br />
extraction procedure with screening and quantitation by GC/NPD. Linearity was achieved<br />
from 0.05 to 5.0 mgIL with the limit <strong>of</strong> quantitation at 0.05 mgIL. Confirmation <strong>of</strong> atomoxetine was<br />
determined using a GCIMS by comparison with an analytical standard.<br />
The tissue distribution <strong>of</strong> atomoxetine was as follows:<br />
...<br />
Atomoxetine ._._,.-->-' (mg/L r:-:-- or mg/kg) _.,...__.__._-- ---,<br />
Chest Blood Femoral Blood Vitreous Liver Gastric Bile Urine<br />
I Case No. 1 0.08 0.04 -- - -- -- 0.16<br />
I Case No.2 1.3 0.23 0.34 4.2 1.2 or 0.17 mg total 1.5 0.62<br />
It's the author's belief that these are one <strong>of</strong> the first cases <strong>of</strong> atomoxetine being detected and reported from<br />
postmortem specimens.<br />
Keywords: Atomoxetine; Tissue Distribution, Postmortem<br />
Page 337
P3 <br />
POSTMORTEM REDISTRIBUTION OF THE ENANTIOMERS OF CITALOPRAM AND ITS<br />
METABOLITES IN A RAT MODEL<br />
Kugelberg FC i ', Kingback M i , Carlsson B i , Druid H2<br />
iDepartment <strong>of</strong> Clinical Pharmacology, Linkoping University, SE-581 85 Linkoping, Sweden<br />
2Department <strong>of</strong> <strong>Forensic</strong> Medicine, Karolinska Institutet, SE-171 77 Stockholm, Sweden<br />
Enantioselective drug analysis is used to study the variation in the disposition <strong>of</strong> the enantiomers <strong>of</strong><br />
racemic drugs. This type <strong>of</strong> analysis may give additional information in interpreting forensic toxicological<br />
results, provided that the postmortem redistribution is <strong>of</strong> the same magnitude for the enantiomers. One<br />
example <strong>of</strong> a racemic drug is the widely used antidepressant citalopram (CIT) that belongs to the selective<br />
serotonin reuptake inhibitors (SSRIs). Different therapeutic properties have been shown for the CIT<br />
enantiomers, and the S-(+)-enantiomer is responsible for the clinically relevant effects. Recent data indicate<br />
that the R-(-)-enantiomer instead counteracts the SSRI effect that is produced by the S-(+)-enantiomer. The<br />
major CIT metabolites, demethylcitalopram (DCIT) and didemethylcitalopram (DDCIT), are less potent<br />
than the parent compound with regard to SSRI properties. In recent years, several reports on CIT<br />
concentrations in human postmortem cases have become available. However, only limited data are<br />
available describing postmortem concentrations <strong>of</strong> the separate enantiomers <strong>of</strong> CIT and metabolites. There<br />
is a general awareness that the concentration <strong>of</strong> a drug in an autopsy blood sample may not necessarily<br />
reflect the in vivo concentration just before death, and this difference is explained by postmortem drug<br />
redistribution. Thus, in order to accurlltely interpret the postmortem concentrations <strong>of</strong> CIT a general<br />
understanding <strong>of</strong> the changes in the enantiomer concentrations after death is required. Hence, the aim <strong>of</strong> the<br />
present study was to investigate if postmortem redistribution <strong>of</strong> the enantiomers <strong>of</strong> CIT, DCIT .and DDCIT<br />
occurs in an experimental rat model after three different dosing procedures with racemic CIT. Two rat<br />
groups underwent chronic administration (20 mglkg daily) using subcutaneously (s.c.) implanted osmotic<br />
pumps. After 10 days, one <strong>of</strong> these groups received an acute-on-chronic drug challenge by a single s.c.<br />
injection <strong>of</strong> 100 mg/kg. The third group received the single 100 mg/kg dose only. Heart blood and brain<br />
samples were collected antemortem and 1,3 or 24 h postmortem after storage in room temperature. In an<br />
additional experiment, we examined the role <strong>of</strong> the lungs as a reservoir <strong>of</strong> postmortem drug release and if<br />
the early-phase postmortem redistribution was different in room temperature (21°C) as compared with a<br />
cold environment (4°C). The samples were analyzed with an enantioselective HPLC method with<br />
fluorescence detection. Increased postmortem blood drug and metabolite concentrations compared to<br />
corresponding antemortem concentrations were observed in all groups (p
P4 <br />
INFLUENCE OF PUTREFACTION AND WATERY CIRCUMSTANCES ON THE<br />
CONCENTRATIONS OF ACONITINE IN TISSUES<br />
Hideyuki Hayakawa 1 *, Makoto Nihira zl , Makiko Hayashida 2l , Morihisa Sagil), Toshiji Mukai l ) and<br />
Youkichi Ohn0 2 ; 1) Department <strong>of</strong>LegaJ Medicine, St. Marianna University School <strong>of</strong> Medicine<br />
2) Department <strong>of</strong>LegaJ Medicine, Nippon Medical School<br />
Aconitium plants (Ranunculaceae) are showy herbaceous flowering perennials that are widely distributed in the mountainous or<br />
cooler parts <strong>of</strong> northern temperate zones. They contain highly toxic Aconitum alkaloids such as aconitine, mesaconitine,<br />
hypaconitine and jesaconitine in the root, leaf and stem. Because <strong>of</strong> their high toxicity, Aconitum alkaloids have been used in<br />
suicides and homicides. In such cases, quantitative analysis <strong>of</strong>Aconitum alkalo ids in the body fluids and tissues is necessary to<br />
determine the cause <strong>of</strong> death. For correct diagnosis <strong>of</strong> poisoning in cases where only putrefied material is available, it is<br />
necessary to investigate the influence <strong>of</strong> putrefaction on the concentrations <strong>of</strong>Aconitum alkaloids in body tissues. Moreover, we<br />
sometimes encounter cases <strong>of</strong> putrefied cadavers floating in the water, where toxicological analysis is necessary. Although the<br />
rate <strong>of</strong> non-enzymatic hydrolysis <strong>of</strong> aconitine dissolved in phosphate buffer has been studied, no reports are available on<br />
postmortem changes <strong>of</strong> Aconitum alkaloids in putrefied tissue. Therefore, we performed animal experiments to determine the<br />
influence <strong>of</strong> putrefaction over a 4-weekperiod on the concentrations <strong>of</strong> Aconitum alkaloids .in body tissues after oral<br />
administration <strong>of</strong> aconitine; one group <strong>of</strong> animals has been kept in the water for putrefaction, as a model <strong>of</strong> putrefied humans<br />
found in the water. ICR mice were divided into a whole-body storage group and an excised-organ storage group. Aconitine was<br />
administered orally at a dose <strong>of</strong> 4 mglkg body weight to the mice, which were sacrificed within 35 min; for the whole-body<br />
storage group, each cadaver <strong>of</strong>the animals was placed in a bottle containing 750 ml water, followed by incubation at 20 or 35 "C<br />
for 1, 3, 7, 14 and 28 days. For the excised-organ storage group, the liver and brain were separately incubated without any water<br />
at 20 'C for the same intervals. The concentrations <strong>of</strong> aconitine and its hydrolysis products were measured by gas<br />
chromatography-mass spectrometry in the selected ion monitoring mode. In the whole-body storage group, the concentration<br />
<strong>of</strong> aconitine markedly increased in the liver and brain, showing postmortem diffusion <strong>of</strong> aconitine from the stomach.<br />
Concentrations <strong>of</strong> benz oyla conine and aconine also increased in the liver; but when expressed as ratios <strong>of</strong> the amounts <strong>of</strong> these<br />
substances to the total amounts <strong>of</strong> alkaloids, the ratios <strong>of</strong> aconitine gradually decreased, while those <strong>of</strong> its hydrolysis products<br />
increased. In the excised-organ storage group, no increase <strong>of</strong>aconitine concentration was observed; while benzoylaconine in the<br />
liver increased significantly on days 3 and 7. Only small amounts <strong>of</strong> aconitine were detected in the bottle water. The above<br />
results show that aconitine changes through hydrolysis and postmortem diffusion. But aconitine can be detected in the liver even<br />
on day 28. Our results <strong>of</strong> the whole-body storage group suggest that the postmortem diffusion <strong>of</strong> aconitine from the stomach to<br />
the brain via tissues and body fluids may occur in watery circumstances. Caution should be taken against the postmortem<br />
diffusion <strong>of</strong> aconitine for victims found in the water.<br />
Keywords: Aconitine, Putrefilction, Postmortem diffusion<br />
Page 339
PS <br />
POSTMORTEM DETERMINATION OF SILDENAFIL IN BLOOD<br />
Hwakyung Choi, SangHee Woo, Juseon Lee, Yooshin Park, Myungyun Pyo, Heesun Chung*<br />
National Institute <strong>of</strong> Scientific Investigation, Seoul, Korea<br />
School <strong>of</strong>Pharmacy, Sookmyung Women's. University, Seoul, Korea<br />
Sildenafil is sold as a remedy for an oral therapy for erectile dysfunction by the name <strong>of</strong> ViagraTM. It is an<br />
. inhibitor <strong>of</strong> cGMP phosphodiesterase and has a potential for cardiac risk during sexual activity in patients<br />
with preexisting cardiovascular disease. Therefore, patients who have cardiovascular problems should not<br />
use sildenafil citrate.<br />
There have been 10 sildenafil related deaths in Korea. All were males in their late thirties to sixties. To<br />
investigate the cause <strong>of</strong> death, the gastric contents and blood underwent toxicological screening. To Iml<br />
blood 50[J <strong>of</strong> 100/0 tadanafil (lnt.std) were added. Blood samples were purified by solid phase<br />
extraction using a Bond Elut-Certify .column (Varian®). Blood was loaded into a cartridge that was prewashed/conditioned<br />
with methanol and O.IMphosphate buffer. The elution was performed with ethyl<br />
acetate:ammonia (98:2). After the solid phase extraction <strong>of</strong> blood, sildenafil was analyzed with high<br />
performance liquid chromatography with photodiode array detector (HPLCIPDA). The mobile phase<br />
consisted <strong>of</strong> 0.05M triethylamine-phosphate (pH 3.0), methanol and acetonitrile (580:250: 170,v/v).<br />
Postmortem bloods were analyzed at a flow rate <strong>of</strong> 1.0mllmin with a detection wavelength <strong>of</strong> 290nm.<br />
Standard curve <strong>of</strong> spiked sildenafil into blank blood was linear with a correlation coefficient <strong>of</strong> 0.998. The<br />
limit <strong>of</strong> detection and the limit <strong>of</strong> quantification for sildenafil were 0.02 llg/mL and O.IIlg/mL, respectively.<br />
The relative recovery was 99.4%.<br />
The concentration range <strong>of</strong> sildenafil <strong>of</strong> postmortem blood was 0.00-0.70 Ilg/mL.(mean 0.166±0.067) in all<br />
ten cases. In case 6, the blood concentration <strong>of</strong> sildenafil was below the limit <strong>of</strong> quantification (0.1 Ilg/mL),<br />
however, sildenafil was confirmed in the gastric contents. In case I, 2 and 5, the victims had a medical<br />
history <strong>of</strong> cardiac disease.<br />
Key words: Sildenafil; postmortem blood concentration, HPLC/PDA<br />
Page 340
P6 <br />
TWO CASES INVOLVING CLOMIPRAMINE INTOXICATION<br />
Joseph Avella*, Michael Lehrer, Michael Katz and Edward Minden. <br />
Suffolk County Office <strong>of</strong> the Medical Examiner, Toxicology Laboratory, Hauppauge NY. <br />
Clomipramine and its active metabolite norclomipramine were identified and quantitated in multiple tissues <br />
recovered from two postmortem cases using liquid chromatography/mass spectrometry (LCIMS). The <br />
LCIMS method afforded the consistent chromatography needed to accurately determine both the parent <br />
drug and the more polar metabolite while simultaneously providing the specificity associated with mass <br />
spectral data. <br />
In the first case a 23-year-old female with a history <strong>of</strong> depression presented to her attending pulmonologist <br />
with a respiratory tract infection. She was diagnosed with pneumonia upon admission to the hospital. The <br />
patient was placed on antibiotics and oxygen and appeared stable. Within twelve hours the patient became <br />
confused and anxious. She began to have difficulty breathing and subsequently coded and expired despite <br />
resuscitative efforts. An autopsy was conducted and tissues were submitted for toxicological analysis. <br />
Clomipramine and norclomipramine was detected in the following concentrations: Heart blood; 1.39 mg/L <br />
and 2.64 mg/L, Brain; 8.02 mg/kg and 26.74 mg/kg, Liver; 14.25 mg/kg and 41.12 mg/kg, Urine; 0.48 <br />
mg/L and 1.15 mg/L and Gastric Contents 3.99 mg/total and 0.61 mg/total. <br />
~\<br />
Case #2 was a 56-year-old female with a history <strong>of</strong> depression who had previously attempted suicide with <br />
prescription painkillers. The evening prior to her death, the decedent had no complaints and retired for the <br />
night. The following morning she was found dead in her bed. Autopsy revealed evidence <strong>of</strong> medication <br />
around her mouth and in her gastric contents. No significant natural disease was present and toxicology <br />
was requested to assess the possibility <strong>of</strong> an overdose. In this case clomipramine and norclomipramine was <br />
detected in the following .amounts: Femoral blood; 0.70 mg/L and 0.66 mg/L, Pulmonary artery blood; 1.00 <br />
mg/L and 1.11 mg/L Brain; 4.86 mg/kg and 7.43 mg/kg, Liver; 11.68 mg/kg and 20.76 mg/kg, Gastric <br />
21.20 mg/total and 1.34 mg/total and Small Intestinal contents; not detected and 0.10 mg/total. The other<br />
significant finding was the presence <strong>of</strong>hydro cod one in femoral blood at a concentration <strong>of</strong>0.13 mg/L.<br />
In both cases the determination <strong>of</strong> clomipramine and metabolite in the brain samples was considered<br />
especially useful for assessing toxicity. The author's found the brain to be helpful for several reasons.<br />
First, although the blood results were potentially toxic, the liver results were not conclusively indicative <strong>of</strong><br />
an overdose. Patients that have undergone long-term tricyclics antidepressant (TCA) therapy can sequester<br />
substantial amounts <strong>of</strong> parent drug and metabolite in liver, a particular concern because the TCA's may<br />
exhibit postmortem redistribution. In some cases <strong>of</strong> TCA overdose the liver results are unmistakable (i.e.<br />
clomipramine concentrations exceeding 200 mg/kg after acute poisoning). In the cases detailed in this<br />
report the liver results were considered insufficient to confidently establish fatal toxicity. Blood specimens<br />
(especially central) were viewed critically while interpreting results due to the concern <strong>of</strong> possible<br />
postmortem changes. The use <strong>of</strong> brain was advantageous because concentration changes are unlikely to<br />
occur in brain tissue due to postmortem redistribution. In these cases the analysis <strong>of</strong> brain provided further<br />
insight with respect to toxicity by establishing the concentrations <strong>of</strong> clomipramine and norclomipramine at<br />
the site <strong>of</strong> action without complications arising from postmortem redistribution.<br />
This communication supplements the database on clomipramine and norclomipramine by providing<br />
quantitative determinations <strong>of</strong> both parent drug and metabolite in multiple tissues. A literature search<br />
revealed a paucity <strong>of</strong> data on clomipramine and norclomipramine levels in general and an absence <strong>of</strong><br />
documented brain levels. When conducting these postmortem investigations, the inclusion <strong>of</strong> brain<br />
determinations provided valuable information in assessing the magnitude <strong>of</strong> toxicity in these cases<br />
involving clomipramine and its active metabolite norclomipramine.<br />
Keywords: clomipramine, postmortem redistribution, tricyclic antidepressants<br />
Page 341
P7 <br />
A COMBINED DRUG INTOXICATION INVOLVING METAXALONE (SKELAXIN®)<br />
Juraj Cervenak*, Sarah M. Colvin, and Fiona J. Couper <br />
Office <strong>of</strong> the Chief Medical Examiner, 1910 Massachusetts Ave SE, Bldg 27, Washington, D.C. 20003. <br />
We present a case <strong>of</strong> a 24-year old female who was found dead on her bedroom floor, in a secure<br />
apartment. She had a history <strong>of</strong> anxiety and had been prescribed antidepressants for several years. A scene<br />
investigation revealed empty beer cans and numerous prescription and over-the-counter medications.<br />
Prescribed medications included Lexapro® (citalopram), Skelaxin® (metaxalone), Ritalin®<br />
(methylphenidate), and Restoril® (temazepam). An autopsy was performed and the findings were<br />
unremarkable. Specimens were submitted for a full toxicological analysis, including an alcohol analysis by<br />
headspace gas chromatography with flame ionization detection; a screen for drugs <strong>of</strong> abuse and several<br />
prescription drug classes using an enzyme-linked immunosorbent assay technique (ELISA); and a screen<br />
for basic compounds using gas chromatography-mass spectrometry (GC-MS). Positive findings were<br />
confirmed and quantitated using GC-MS. The following drug concentrations were measured in postmortem<br />
blood: metaxalone 38 mg/L, citalopram 0.49 mglL, diphenhydramine 0.10 mgIL and ethanol 0.02 g/100<br />
mL. Methylphenidate and temazepam were not detected. Further investigation revealed the following<br />
prescription history for the decedent prior to her death:<br />
# Prescribed # Remainin<br />
100 tablets 66 tablets<br />
180 o<br />
60 o<br />
30 5<br />
Metaxalone is a centrally acting muscle relaxant prescribed for the relief <strong>of</strong> pain associated with acute,<br />
musculoskeletal conditions. The recommended dose for adults is 2 x 400 mg tablets, three to four times a<br />
day. The circumstances and drug results in this case were similar to those reported in the only other<br />
metaxalone-related fatality cited in the literature: a 29-year old female with a history <strong>of</strong> depression had<br />
postmortem blood metaxalone and citalopramconcentrations <strong>of</strong> 39 mglL and 0.77 mgIL, respectively. In<br />
the present study, the cause <strong>of</strong> death was determined to be due to "combined effects <strong>of</strong> metaxaione,<br />
citaiopram, diphenhydramine and ethan<strong>of</strong>', and the manner <strong>of</strong> death was "undeterminec!'. A discussion <strong>of</strong><br />
the case circumstances, the toxicology findings and the pharmacology <strong>of</strong> metaxalone will be presented.<br />
Keywords: Metaxalone, Skelaxin, Intoxication<br />
Page 342
P8 <br />
A CASE OF FATAL OVERDOSE WITH LABETALOL<br />
Karen Woodall"', Centre <strong>of</strong> <strong>Forensic</strong> Sciences, Toxicology Section, 25 Grosvenor Street, Toronto, Ontario,<br />
Canada<br />
Labetalol (Normodyne®, Trandate®) is an alpha and beta-adrenergic and beta-adrenergic receptor<br />
antagonist used in the treatment <strong>of</strong> hypertension. A typical dose <strong>of</strong>labetalol ranges from 200 400 mg/day<br />
however some individuals may require up to 2100 mg/day. Symptoms <strong>of</strong> labetalol overdose are excessive<br />
hypotension and bradycardia. There is very limited information available regarding labetalol concentrations<br />
and toxicity and no reports where the cause <strong>of</strong> death has been attributed solely to a labetalol overdose. This<br />
study describes a case where the cause <strong>of</strong>death was attributed to an acute overdose <strong>of</strong> labetalol.<br />
A 79-year-old female was admitted to hospital for high blood pressure and chest pain. She was stabilized<br />
and after remaining in hospital for 7 days was being prepared for discharge. At this time she was observed<br />
to have swallowed numerous tablets by another patient. She subsequently became hypotensive and<br />
bradycardic, and resuscitation attempts were unsuccessful. A blood sample taken during the attempted<br />
resuscitation was tested at the hospital and the drug screen showed that labetalol was significantly higher<br />
than the therapeutic range. Empty prescription bottles <strong>of</strong> labetalol, lorazepam and furosemide (medications<br />
she brought with her to the hospital) were found at the scene, however the actual number <strong>of</strong> tablets taken is<br />
not known. There were no other significant findings in the hospital drug screen except for the elevated<br />
labetalol concentration.<br />
A postmortem was conducted and toxicology testing was performed on a heart blood sample. Labetalol was<br />
measured by high-pressure liquid chromatography (HPLC) and the detected concentration was 15 mg/L.<br />
Lorazepam was measured by mass spectrometry (MS) and was detected at a concentration <strong>of</strong> 73 ng/mL. In<br />
addition to specific testing for labetalol and lorazepam, a general basic drug screen using gas<br />
chromatography and mass spectrometry (GC and GCIMS) was performed and traces <strong>of</strong> sertraline and<br />
metoprolol were detected. This laboratory does not have a method for the analysis <strong>of</strong> furosemide.<br />
Therapeutic concentrations <strong>of</strong> labetalol in serum have been shown to range from 0.02 - 0.25 mg/L, and<br />
levels over 0.5 mg/L are considered to be toxic. In one case report, a woman who suffered renal failure<br />
following an acute ingestion <strong>of</strong> labetalol (16g) had a serum concentration <strong>of</strong> 29 mg/mL. The concentration<br />
<strong>of</strong> labetalol in this case is approximately 60 times higher than the therapeutic levels. The autopsy showed<br />
signs <strong>of</strong> chronic hypertension but no gross or microscopic cause <strong>of</strong> death. In the absence <strong>of</strong> other<br />
significant drug findings the cause <strong>of</strong>death was reported as acute labetalol intoxication.<br />
Key words: labetalol, fatality, overdose<br />
Page 343
P9 <br />
DETERMINATION OF OXCARBAZEPINE AND ITS METABOLITES IN POSTMORTEM<br />
SPECIMENS INCLUDING HAIR BY MEANS OF LIQUID CHROMATOGRAPHY WITH MASS<br />
DETECTION (HPLC/APCIIMS) IN AN EPILEPTIC PATIENT AFTER A FATAL DRUG<br />
POISONING<br />
Malgorzata Klys* and Sebastian Rojek<br />
Grzegorzecka str 16, Krakow, Malopolskie, 31-531, Poland<br />
One use <strong>of</strong>hair analysis in forensic toxicology is the documentation <strong>of</strong> prior drug administration. This is<br />
illustrated in a suicidal death <strong>of</strong> a 58-year-old epileptic patient who was treated with oxcarbazepine and<br />
probably with levomepromazine.<br />
The toxicological analysis carried out by HPLC/APCIIMS included also the hair (6cm length) besides <strong>of</strong><br />
postmortem blood and liver samples. The method was validated for oxcarbazepine (OXCBZ) and its two<br />
metabolites, 10-hydroxycarbazepine (CBZ-100H) and trans-diol-carbazepine (CBZ-diOH) in various<br />
biological matrices.<br />
Thetoxicological findings are as follows:<br />
Hair<br />
Autopsy<br />
Segment (2 Segment (2<br />
Segment (cm)<br />
cm)<br />
cm)<br />
I<br />
II<br />
III<br />
Blood Liver<br />
Concentration (I!Wg)<br />
Oxcarbazepine 3.9 10.4 13.0 0.79 n.d.<br />
18.4<br />
53.9<br />
105.9 13.96 15,28<br />
i CBZ-100H<br />
4.7*<br />
5.1 *<br />
8.1 * 17.6* -<br />
.0.5<br />
1.2<br />
3.0 0.23 n.d<br />
CBZ-diOH<br />
0.12*<br />
0.12* 0.23* 0.29*<br />
-<br />
Levomepromazine - - - 1.96 30,25<br />
*Relatlve concentration metabolite / prekursor<br />
n.d. - not detected<br />
The analysis <strong>of</strong> the postmortem blood indicated oxcarbazepine and its two main metabolites were present at<br />
therapeutic concentrations; levomepromazine was detected at a fatal concentration. In three 2-cm segments<br />
<strong>of</strong>hair,.oxcarbazepine and its two metabolites were detected; however, levomepromazine was not detected<br />
in this . specimen. A complex chemical-toxicological investigation confirmed the information that the<br />
decedent. was an epileptic patient and was treated with oxcarbazepine for at least 6 months before death. In<br />
addition, he took a toxic dose <strong>of</strong> levomepromazine in order to commit suicide. The analysis revealed<br />
differences between the' concentration levels <strong>of</strong> oxcarbazepine and its active metabolite CBZ-IOORin<br />
postmortem specimens and hair, suggesting different mechanisms <strong>of</strong> penetration <strong>of</strong> certain metabolites and<br />
their precursors into these materials.<br />
Keywords: oxcarbazepine, hair, LClAPCIIMS<br />
Page 344
PIO <br />
STABILITY OF SULFONYLUREAS IN STORED POSTMORTEM BLOOD SPECIMENS AND<br />
WATER STANDARDS<br />
A.H. Battah, M.D, Ph.D*, <strong>Forensic</strong> Medicine and Toxicology Division, Faculty <strong>of</strong> Medicine, University <strong>of</strong><br />
Jordan, Amman 11942, Jordan.<br />
K.A. Hadidi, Ph.D, Toxicology Laboratory, <strong>Forensic</strong> Medicine and Toxicology Division, Faculty <strong>of</strong><br />
Medicine, University <strong>of</strong> Jordan, Amman 11942, Jordan.<br />
Stability <strong>of</strong> three commonly prescribed sulfonylureas (gJipizide, chlopropamide and glibenclamide) in<br />
postmortem blood and water stored at -20,4, and 25°C were evaluated over a I-year period. The drugs<br />
were analyzed simultaneous by utilizing solid phase extraction techniques and were identified and<br />
quantified by high performance liquid chromatography. The data showed that, significant loss <strong>of</strong><br />
g/ibenclamide (GB) was noticed at second and third week <strong>of</strong> storage at 25 and 4°C respectively. The<br />
decrease was gradual but no clear pattern could be established. At the end <strong>of</strong> the I-year storage period at<br />
either 4 or 25°C, the level <strong>of</strong> GB was about 37% and 46% <strong>of</strong> its initial value in aqueous solution and<br />
postmortem blood samples respectively. There was no significant loss <strong>of</strong> both glipizide and chlopropamide<br />
in all stored samples over the first 6-month period. After that time a significant decrease in their levels<br />
were noticed, and at the end <strong>of</strong> the I-year <strong>of</strong> storage concentrations ranged from 67.5 to 84.1 % <strong>of</strong> their<br />
initial values. Storage at -20°C showed the least loss <strong>of</strong> drug concentration. Authentic samples <strong>of</strong> these<br />
drugs showed similar results. This study supports the importance <strong>of</strong> paying careful attention to using<br />
prepared aqueous drug standards even when stored in cold conditions. In order to obtain reliable results <strong>of</strong><br />
drug analysis and drug stability in biological samples, such studies should be considered after prolonged<br />
sample storage time. The best storage temperature to keep aqueous standards and blood samples for the<br />
investigated drugs with sufficient stability was found to be at -20°C.<br />
Keywords: Stability, Sulfonylurea, Blood.<br />
Page 345
PH <br />
DISTRIBUTION OF QUETIAPINE IN NINE POSTMORTEM CASES<br />
Tara J. Valouch, B.S.'", Dwight Flammia, Ph.D., James K. Kuhlman, Ph.D., Virginia Division <strong>of</strong> <strong>Forensic</strong><br />
Science<br />
Quetiapine (Seroquel ®) is an antipsychotic drug approved by US FDA in September 1997 for the<br />
treatment <strong>of</strong> schizophrenia. It is classified as a dibenzothiazepine and structurally related to clozapine. The<br />
molecular formula is C21H2sN30zS with a molecular weight <strong>of</strong> 383.6. It is believed to exert its<br />
pharmacological effect through antagonism <strong>of</strong> sertonergic (5HT2) and dopaminergic (D2) receptors in the<br />
brain. Quetiapine is extensively metabolized, but the pharmacological effect is primarily attributed to<br />
parent drug. It is rapidly absorbed after oral administration, reaching peak plasma concentrations in 1.5 h.<br />
The elimination half life is 6 h. Peak serum quetiapine concentrations range from 0.17 - 0.37 mgIL<br />
following a single oral 75 mg dose to 0.19 0.63 mg/L following a 450 mg dose.<br />
Nine postmortem quetiapine cases identified by the Virginia Division <strong>of</strong> <strong>Forensic</strong> Science toxicology<br />
laboratories during 2003 are presented. Quetiapine was identified by full scan electron impact gas<br />
chromatography-mass spectrometry (GCMS) following a basic drug extraction from blood. Quantitation<br />
was performed using a basic solid-phase extraction followed by the addition <strong>of</strong> BSTF A and selected ion<br />
monitoring GCMS. The following mean tissue concentrations and ranges were determined: heart blood<br />
18.9 mgIL (0.53 - 76 mgIL, n = 4), peripheral blood 11.5 mg/L (0.46 - 37 mg/L, n = 6), urine 16.4 mg/L<br />
(1.9 - 37 mg/L, n 6), liver 123 mg/Kg (7.2 510 mg/Kg, n = 9), and gastric 48.2 gIL (15-130 gIL, n = 4).<br />
Medical examiners certified the cause <strong>of</strong> death in eight <strong>of</strong> the nine cases as combined drug toxicity. In one<br />
case the cause <strong>of</strong> death was quetiapine toxicity and the manner <strong>of</strong> death was suicide. The quetiapine<br />
concentrations in this case were 15 mglL in antemortem blood, 18 mgIL in peripheral postmortem blood,<br />
and 89 mglKg in liver. Only one case contained both heart and peripheral blood (7.0mgIL and 3.4 mg/L<br />
respectively). The heart/peripheral blood ratio was 2.0 suggesting postmortem redistribution.<br />
Keywords: quetiapine, postmortem, distribution<br />
Page 346
P12 <br />
DETERMINATION OF ATRACTYLOSIDE IN CALLILEPIS LAUREOLA USING SOLID-PHASE<br />
EXTRACTION AND LIQUID CHROMATOGRAPHY - ATMOSPHERIC PRESSURE<br />
IONISATION MASS SPECTROMETRY<br />
Paul A. Steenkamp"', Nial M. Harding', Fanie R. van Heerden b .•, Ben-Erik van Wyk C<br />
"<strong>Forensic</strong> Chemistry Laboratory, Department <strong>of</strong>Health, P.O. Box 1080, Johannesburg 2000, South Africa;<br />
bDepartment <strong>of</strong> Chemistry and Biochemistry, Rand Afrikaans University, P.O. Box 524, Auckland Park<br />
2006, South Africa; CDepartment <strong>of</strong> Botany, Rand Afrikaans University, P.O. Box 524, Auckland Park<br />
2006, South Africa<br />
A selective analytical method based on high-performance liquid chromatography, combined with<br />
atmospheric pressure ionisation mass spectrometry, was developed for the detection <strong>of</strong> atractyloside. The<br />
tuberous root <strong>of</strong> the plant Callilepis laureola is used in traditional medicine by the Zulu and Xhosa people<br />
<strong>of</strong> South Africa and it is well known by the Zulu name impila, which means 'health'. However, C. laureola<br />
has also been implicated in the death <strong>of</strong> numerous patients who used medication prepared from impila in<br />
which atractyloside, the dipotassium salt <strong>of</strong> a sulfonated kaurene glycoside, was identified as the toxic<br />
principle. This compound, together with carboxyatractyloside, was also identified as the toxic principle <strong>of</strong><br />
Atractylis gummifera L. (Asteraceae), a plant linked to human fatalities in Mediterranean countries since<br />
ancient times.<br />
The analysis was performed on an Xterra Phenyl column utilising a gradient elution pr<strong>of</strong>ile and a mobile<br />
phase consisting <strong>of</strong> 10 mM aqueous ammonium acetate buffer-MeOH-acetonitriIe. The developed method<br />
showed a good linearity for the calibration curve spanning the 10 ng/mL to 1 j.ig/mL (r2 = 0.997) range.<br />
The limit <strong>of</strong> detection and limit <strong>of</strong> quantitation were determined and found to be 100 pglmL and 10 ng/mL,<br />
respectively. The method was successfully applied to the analysis <strong>of</strong> C. laureola tuber, herbal medicine<br />
mixtures and viscera samples (stomach, stomach contents, liver, kidney, blood, urine, bile) for the presence<br />
<strong>of</strong> atractyloside.<br />
Keywords: Atractyloside, CallUepis laureola, HPLC-MS<br />
* Corresponding author. Tel: +27-11-725-2279; fax: +27-11-725-4731. E-mail address: fcIjhb@icon.co.za<br />
Page 347
P13<br />
MIRTAZAPINE-RELATED DEATHS<br />
R A Braithwaite* and S P Elliott<br />
Regional Laboratory for Toxicology, City Hospital, Birmingham. UK<br />
Mirtazapine is a novel antidepressant drug which has a pharmacological action on both noradrenergic and<br />
serotonergic systems. The drug has been on the US and European markets for about 10 years, but<br />
relatively few deaths associated with mirtazapine have been reported in the literature. Post-mortem blood<br />
mirtazapine concentrations <strong>of</strong> up to 0.3 mglL have been reported in cases where the drug is not implicated<br />
in the cause <strong>of</strong> death. There is also evidence to show that the drug undergoes post-mortem redistribution,<br />
which can make interpretation <strong>of</strong>findings more difficult.<br />
Relatively few deaths reported in UK have noted the presence <strong>of</strong> mirtazapine. However, in the last few<br />
years (2001-2003) the Laboratory has investigated a total <strong>of</strong> 8 cases (5 male, 3 female) aged between 17<br />
and 77 years where mirtazapine has been found to be present in significant concentrations, but generally in<br />
association with other drugs. Post-mortem blood mirtazapine and its desmethyl metabolite<br />
(normirtazapine) have been measured using liquid chromatography with U.V-diode array detection. In<br />
addition, extensive screening <strong>of</strong> blood and other fluids was undertaken to determine the presence <strong>of</strong> other<br />
drugs and alcohol.<br />
Details <strong>of</strong> the 8 cases investigated are shown in the Table below. In 7 <strong>of</strong> the 8 cases blood was taken from<br />
a peripheral site at post-mortem. Post-mortem blood mirtazapine concentrations ranged between 1.0 - 404<br />
mglL (mean 2.1 mglL) The ratio <strong>of</strong> mirtazapine to normirtazapine concentrations ranged between 1.9 and<br />
20.<br />
Age Sex Site oj Mirta:: Normirta= MirtiN ormirta:: Other drugs present and<br />
Collect (mgIL) (mgIL) Ratio (concentrations mglL)<br />
/~...<br />
75 M Femoral 2.2 OJ 7J Temazepam, (2.2), venlafaxine<br />
(3.6). Found dead at home<br />
46 M Femoral 2.0 20 Temazepam (Ll) ethanol<br />
(214 mg/dL). Found dead at home<br />
60 M Unknown 1.6 0.8 2.0 No other drugs detected. Found<br />
dead in river<br />
56 M Femoral 1.0 OJ 3.3 Diazepam (1.5), Sildenafil (trace),<br />
alcohol (72 mg/dL). Found dead at<br />
home<br />
77 M Femoral 2.1 1.1 1.9 Zopic1one (1.6). Found dead in bed<br />
51 F Femoral 2.5 004 6.7 Zopiclone (1.7), Lorazepam (004),<br />
chlorpromazine (trace), alcohol<br />
(54 mgldL). Found dead in bath<br />
21 F Common 1.3 0.3 5.0 Dextropropoxyphene (2.4),<br />
Iliac<br />
Paracetamol (124), Venlafaxine<br />
(1.4) Zopidem (trace). Found dead<br />
at home<br />
17 F Femoral 4.4 0.7 6.1 Diltiazem (4.2), paracetamol (70),<br />
Zopic1one (trace). Found dead at<br />
home with suicide note<br />
In conclusion, mirtazapine appears to be more commonly seen in recent post-mortem cases, probably due<br />
to prescribing trends. In all but one <strong>of</strong> the cases, other drugs or alcohol were present. However,<br />
mirtazapine overdosage appeared to be a significant factor in at least half <strong>of</strong> the deaths reported and were<br />
associated with a parent blood mirtazapine concentration >2.0 mgIL and a ratio <strong>of</strong> mirtazapine to<br />
normirtazapine >2.<br />
Keywords: blood, mirtazapine, postmortem<br />
Page 348
.~.<br />
P14 <br />
TWO FATAL INTOXICATION CASES WITH IMIDACLOPRID: LC~MS ANALYSIS<br />
P.Proen~a*, H.M. Teixeira, F. Castanheira, P. Monsanto, J.Pinheiro, S. Santos, E.P. Marques, D.N. Vieira<br />
National Institute <strong>of</strong> Legal Medicine, Coimbra, PORTUGAL .<br />
Aim: Imidacloprid [1~(6-chloro-3pyridylmethyl)-N-nitroimidazolidin~2-ylideneamine] is a new and potent<br />
nitro methylene insecticide with high insecticidal activity at very low application rates. It is the first highly<br />
effective insecticide for which the mode <strong>of</strong> action has been found to deviate from the almost complete and<br />
irreversible blocking <strong>of</strong> the postsynaptic nicotinergic acetylcholine receptors. The authors present two fatal<br />
cases due to this pesticide, in two males, 33 and 66 years old.<br />
Methods: An LC~MS with electrospray method is described for measuring imidacloprid and its metabolite<br />
in postmortem samples. In the chromatographic separation, a reverse-phase column CIS (2.1xI50mm,<br />
3.5Jlm) was used and the mobile phase composed with acetonitrile and 0.1 % formic acid (15:85), at a 0.25<br />
mllmin flow rate. The samples were prepared by a liquid-liquid extraction procedure with dichloromethane.<br />
Results: Calibration curves for imidacloprid were performed in acetonitrile in blood and urine, achieving<br />
linearity between 0.2Jlg/ml and 15Jlg/ml. The mean recovery was 86%, coefficient <strong>of</strong> variation was ±5.9%<br />
and the detection limit 2.0ng/ml. Quantitative results were obtained for all postmortem matrices available<br />
<strong>of</strong> the two fatal cases: blood, urine, stomach contents, liver and kidney. The concentrations found ranged<br />
between 0.29Jlglml (urine) and 350Jlg/mi (stomach contents). Postmortem blood concentrations found were<br />
12.5Jlglml and 2.05Jlg/mL<br />
Conclusions: The authors developed a sensible and validated method to detect and quantify imidacloprid in<br />
postmortem samples and emphasize the lack or even absence <strong>of</strong> literature with fatal cases related to this<br />
insecticide.<br />
Keywords: Imidacloprid, fatal intoxication, LC-MS<br />
Page 349
PIS <br />
LEVELS OF LEVETIRACETAM IN POSTMORTEM BLOOD<br />
Ashraf Mozayani* and Terry J. Danielson. Harris County Medical Examiner, 1885 Old Spanish Trail,<br />
Houston, Texas, 77054<br />
Levetiracetam (LEV) is a recently introduced anticonvulsant agent and little information is available to<br />
assist in the interpretation <strong>of</strong> levels seen in post-mortem cases. Our objective is to report our observations<br />
from three Medical Examiner cases in which LEV was detected.<br />
LEV is said to have "ideal" pharmacokinetic characteristics for clinical application. It is well absorbed after<br />
oral administration and is distributed approximately into body water. It is not appreciably bound to plasma<br />
protein and its apparent plasma elimination half-life is near to 6 hours.<br />
LEV was extracted from acidified blood into dichloromethane and was assayed by gas chromatography I<br />
mass spectrometry using hexobarbital as internal standard. The retention factor, relative to hexobarbital,<br />
was 0.79 on a HP-5 column (initial temp, 50 ·C; time 1, 1 min; ramp 1,50 ·C Imin to 100 ·C; ramp 2, 20<br />
·C/min to 285 "C). The electron impact mass spectrum contained an intense ion at mlz 126, minor ions at<br />
mlz 170 (m*), 98 and 69.<br />
Case summaries and levels <strong>of</strong> LEV in postmortem blood are reported in Table 1. The data suggest that<br />
postmortem levels <strong>of</strong> LEV near 60 mgIL may be within the normal therapeutic range, and might be<br />
encountered, without toxicological consequence. A lower level, near 10 mgIL as seen in case number 3,<br />
may be sub-therapeutic.<br />
Table 1: Levels <strong>of</strong> Levetiracetam (LEV) in postmortem blood, Case 1, femoral. Cases 2 and 3, source not<br />
indicated<br />
Case # Age Sex LEV Other drugs<br />
Cause <strong>of</strong>Death<br />
Manner<br />
(mg/L) (mg/L blood)<br />
1 22 M 60 None detected Idiopathic epilepsy, Natural<br />
cerebral sclerosis<br />
2 58 M 61 Hydrocodone, 0.25 Hypertensive<br />
Natural<br />
Metoprolol, 1.4<br />
Amitriptyline, 0.38<br />
Nortriptyline, 0.57<br />
Paroxetine, 0.33<br />
cardiovascular disease<br />
Post -cerebral vascular<br />
infarct seizure disorder<br />
I<br />
Trazadone, 0.93<br />
Phenobarbital, < 10<br />
3 35 M 11 None detected Drowning,<br />
Accident<br />
Seizure due to remote<br />
leptomeningitis<br />
Keywords: Levetiracetam, blood, postmortem<br />
Page 350
P16 <br />
OPTIMIZING AN AUTOMATED SOLID-PHASE EXTRACTION PROCEDURE FOR<br />
POSTMORTEM TISSUE SAMPLES<br />
T. Stimpf1*, Department <strong>of</strong> <strong>Forensic</strong> Medicine, Medical University <strong>of</strong> Vienna, Sensengasse 2, A-1090<br />
Vienna, Austria<br />
Quality assurance regulations in forensic laboratories, efforts to reduce systematic errors, costs, time spent per case as<br />
well as efforts to improve technician-safety all lead to the consideration <strong>of</strong>automated procedures for sample extraction.<br />
In contrast to liquid-liquid extraction, solid-phase extraction (SPE) can be more easily automated by incorporating<br />
robotics improving the sample quality in respect to the analyte yield and increasing consistency and laboratory<br />
productivity .<br />
Today, automated SPE procedures are widely used for the extraction <strong>of</strong> body fluids such as urine, serum, plasma and<br />
whole blood. In postmortem forensic toxicology, however, these specimens are not always available and, with regard to<br />
the investigation <strong>of</strong> the cause <strong>of</strong> death, human tissue samples - especially brain - can be highly important.<br />
Drummer and Gerostamoulos pointed out that"... there is little evidence that extraction efficiencies <strong>of</strong>drugs from solid<br />
tissues are likely to be much worse than with fluid specimens ifsuitable precautions are taken. These include a suitably<br />
fluid homogenate prepared from the solid tissue with sufficient water or buffer" [I].<br />
In an automated SPE procedure published by our working group, a crude extract from postmortem tissue samples could<br />
be achieved, avoiding protein precipitation and the resulting loss <strong>of</strong>analytes by adsorption or occlusion.<br />
In respect to the problem that tissue homogenates <strong>of</strong>ten do not easily pass through tightly-packed cartridges, it could be<br />
shown that - after homogenization and dilution with large volumes <strong>of</strong> buffer solution - the resulting colloidal solution<br />
could be directly applied to the polymeric sorbent [2].<br />
For routine solid-phase extraction <strong>of</strong> tissue samples, several adaptations <strong>of</strong> the automated system ASPECTMXL,<br />
operated under 735-sampler s<strong>of</strong>tware V 5.1 for Win NT 4.0 (Gilson Inc., Middleton, WI, USA), were necessary.<br />
• A large volume <strong>of</strong>sample had to be applied in order to dilute the sample and dissolve protein bonds.<br />
• The upper frit <strong>of</strong>the extraction cartridge had to be removed to minimize the risk <strong>of</strong>clogging.<br />
• A 5mL stainless steel sample loop for HPLC (Supeico, Bellefonte, PA, USA) was installed on the ASPEC<br />
XL to avoid adsorption <strong>of</strong> analytes to synthetic plastic materials (transfer tubing).<br />
• Special cleaning routines with 2N NaOH and 2N RN0 3 were used to remove any precipitated proteins. from<br />
the system.<br />
• The sample was applied very slowly to make use <strong>of</strong> "micellar chromatography", thus avoiding the adsorption<br />
<strong>of</strong>macromolecular interferences with larger than pore-sized diameters to the polymeric sorbent.<br />
• A pressure sensor was installed to compensate for inconsistent flow rates during loading, washing and<br />
eluting.<br />
When postmortem samples <strong>of</strong> tissue have to be extracted by automated SPE, monitoring <strong>of</strong> the overall system pressure<br />
is essential. Pressure control allows for high-pressure release if clogging <strong>of</strong> the cartridge occurs, avoiding<br />
contamination <strong>of</strong> the working area with the infectious sample; the aborted sample is then replaced to the sample tube.<br />
1. O.H. Drummer, J. Gerostamoulos, Postmortem drug analysis: analytical and toxicological aspects. Therap.<br />
Drug Monit. 24 (2002) 199-209.<br />
2. T. Stimpfl, J. Jurenitsch, W. Vycudilik, General unknown screening in postmortem tissue and blood samples:<br />
a semi-automatic solid-phase extraction using polystyrene resins followed by liquid-liquid extraction. J.<br />
Anal. Toxieo!. 25 (2001) 125-129.<br />
Keywords: automation, solid-phase extraction (SPE), tissue samples<br />
Page 351
P17 <br />
POSTMORTEM DISTRIBUTION OF TRAMADOL, AMITRIPTYLINE AND THEIR<br />
METABOLITES IN A SUICIDAL OVERDOSE<br />
Nichole D. Bynum*, Justin L. Poklis, Maryanne Gaffney-Kraft and Jeri D. Ropero-Miller. Office <strong>of</strong> the<br />
Chief Medical Examiner, Chapel Hill, NC 27599 U.S.A.<br />
A case report involving a 34 year old white male who was found dead at home by a roommate is presented. The<br />
decedent's history included a suicide attempt and pain as result <strong>of</strong> a motor vehicle accident occurring 5 months<br />
earlier. At the time <strong>of</strong> death, he was being treated with tramadol/acetaminophen, metaxalone, oxycodone and<br />
amitriptyline. The descendant's mother stated that he had been taking increasing amounts <strong>of</strong> pain medication in<br />
order to sleep at night.<br />
Further investigation <strong>of</strong> this case was based on the fact that seven tissues were available for a fatal multi-drug<br />
ingestion concerning several analytes <strong>of</strong> interest, one <strong>of</strong> them being tramadol, which has limited information<br />
concerning tissue and metabolite concentrations. Toxicology tests yielded acetaminophen, oxycodone and<br />
cyclobenzaprine aortic blood concentrations <strong>of</strong> 140, 0.42, and 0.97 mg/L, respectively. Metaxalone and<br />
ibupr<strong>of</strong>en were detected at below therapeutic concentrations. The following matrices were analyzed for tramadol,<br />
n-desmethyltramadol, o-desmethyltramadol, amitriptyline and nortriptyline: aortic and iliac blood, urine, liver,<br />
vitreous humor, bile, brain, heart, kidney, lung, muscle and spleen. Analytes were quantitated by electron impact<br />
gas chromatography/mass spectrometry (GeIMS).<br />
The following table contains the postmortem analyte concentrations obtained for each tissue analyzed in this<br />
study.<br />
Matrix Tramadol N-Desmethyl O-DesmethyI Amitriptyline Nortriptyline<br />
Tramadol Tramadol<br />
Blood (aorta) mgIL 31.0 BQL* 0.901 5.79<br />
1.49<br />
Blood (iliac) mglL 6.21 0.20<br />
0.68 2.33 0.88<br />
Liver (mg/kg) 14.0 BQL 2.47 82.3<br />
29.1<br />
Urine (mg/L) 55.3 1.45 8.27 27.1<br />
6.63<br />
Vitreous Humor (mglL) 3.32 BQL<br />
0.25 0.25 BQL<br />
Bile (mgIL) 2.95 BQL 0.45<br />
41.4<br />
4.59<br />
Brain (mglkg) 4.62 BQL<br />
0.73 24.3<br />
9.29<br />
Heart (mg/kg) 4.95 BQL 1.08 17.4<br />
8.98<br />
Kidney (mglkg) 9.61 BQL 2.54<br />
25.8 8.40<br />
Lung (mg/kg) 87.0 BQL 1.15<br />
134<br />
22.2<br />
Muscle (mglkg) 22.0 BQL BQL<br />
22.6 2.47<br />
Spleen (mglkg) 29.1 BQL<br />
2.61 28.8 16.9<br />
, ~l,!L' Below quanbtat",n IIm.t 01 11.1; mglL (mSlkgJ.<br />
For all analytes, the parent-to-metabolite ratios support an acute toxicity with the parent concentrations being 5<br />
10 times greater than its major metabolite. For amitriptyline and nortriptyline, the order <strong>of</strong> highest to lowest<br />
concentrations detected are lung, liver, bile, urine and other solid tissues (spleen, kidney, brain, muscle and<br />
heart), central and peripheral blood, and finally vitreous humor. On the other hand, tramadol and its metabolites<br />
demonstrate a similar concentration trend with the exception <strong>of</strong> central blood and liver. It has been suggested that<br />
tramadol does not sequester into liver tissues or demonstrate postmortem redistribution from .drug-rich tissues.<br />
This case does not support or refute these observations since gastric contents were not collected and we cannot<br />
confirm the possibility <strong>of</strong> diffusion from the gastrointestinal tract to the central blood or timing <strong>of</strong> the ingestion<br />
<strong>of</strong> these drugs with respect to one another. There were no significant findings at autopsy; however, toxicology<br />
results supported a cause and manner <strong>of</strong> death resulting from suicidal mixed tramadol and amitriptyline toxicity.<br />
This case reports the tissue and fluid distribution <strong>of</strong> tramadol, amitriptyline, and their metabolites in an acutely<br />
fatal ingestion in an effort to document concentrations <strong>of</strong> these analytes in 12 matrices with respect to one<br />
another to assist toxicologists in difficult interpretations.<br />
Keywords: postmortem distribution, tramadol, amitriptyline<br />
Page 352
P18 <br />
SCREENING BY ELISA FOR CARISOPRODOL IN POST-MORTEM BLOOD<br />
F. Nunes-Daniel and D. Boehme<br />
Ventura County Sheriff <strong>Forensic</strong> Sciences Laboratory; 800 S. Victoria Ave; Ventura, CA 93009<br />
Carisoprodol is an unscheduled substance widely prescribed in the USA to promote skeletal muscle<br />
relaxation. The use <strong>of</strong> carisoprodol is associated with CNS depression, which can lead to impairment in<br />
driving and other psychomotor activities. Therefore, it is very important to have a reliable method to test<br />
post-mortem blood sample for carisoprodol. Using Immunalysis Direct Elisa Kit and the PersonnalLABTM<br />
as the analyzer we developed an application to screen carisoprodol in post-mortem blood. We tested a<br />
variety <strong>of</strong> samples using different sample volumes and cut<strong>of</strong>fs. Using 25uL as the sample volume and<br />
500nglmL as the cut<strong>of</strong>f, thirty-two samples were analyzed by ELISA v. GCfMS and GCfNPD. Ten were<br />
positive by both the immunoassay and the chromatographic methods. One sample screened between the<br />
negative control and the cut<strong>of</strong>f calibrator, and was found to contain 4.78 mglmL <strong>of</strong> carisoprodol. The<br />
concentrations <strong>of</strong> carisoprodol in samples that screened positive ranged from 0.12 mgIL to 45.2 mgIL.<br />
These samples also contained meprobamate, ranging in concentration from 2.26 mg/L to 20.2 mgIL. None<br />
<strong>of</strong> the ELISA-negative samples contained carisoprodol at greater than 500 ngimL. The twenty-one samples<br />
that were negative by both the ELISA and by the chromatographic methods contained a broad range <strong>of</strong><br />
other drugs, including cocaine, benzoylecgonine, codeine, morphine, hydrocodone, methadone,<br />
amitriptyline, nortriptyline, diazepam, nordiazepam, temazepam, alprazolam, acetaminophen, bupropion<br />
and its metabolites, norchlorcyclizine, nicotine, cotinine, caffeine, olanzapine, fluoxetine, norfluoxetine,<br />
norpropoxyphene, doxylamine, tripolidine, and metoclopramide. A precision study was conducted by<br />
analyzing 10 replicates each <strong>of</strong> the negative calibrator, a 250 ng/mL control, the 500 ng/mL calibrator, and<br />
a positive control containing 1000 nglmL carisoprodol. The OD's were tracked and the results were as<br />
follows: negative calibrator: 1.386 ±..0.051 (CV= 3.7%); 250 ng/mL control: 0.510 ± 0.015 (CV= 2.9%);<br />
500 nglmL calibrator: 0.440 ± 0.024 (CV= 5.4%); and 1000 ng/mL control: 0.410 ± 0.014 (CV= 3.4%).<br />
Keywords: Carisoprodol; immunoassay; postmortem blood<br />
Page 353
P19 <br />
EVALUA TION OF DEBATED QUESTIONS: DO POSTMORTEM METHADONE<br />
CONCENTRATIONS OF AL TERNA TIVE SPECIMENS HAVE INTERPRETIVE VALUE<br />
Jeri D. Ropero-MiIler* and Ruth E. Winecker. Office <strong>of</strong> the Chief Medical Examiner, Chapel Hill, NC<br />
27599 U.S.A.<br />
Deaths due to methadone ingestion are escalating in many geographical locations nationwide. Often these deaths<br />
are the result <strong>of</strong> naIve users ingesting methadone either recreationally or as prescribed, however, their systems do<br />
not tolerate the dose taken. With the increased use <strong>of</strong> methadone, either as a recreational drug or to treat chronic<br />
pain, the population dying from methadone toxicity has radically changed over the last decade. Many factors<br />
contribute to the difficulty <strong>of</strong> interpreting methadone's role in a death. Some postmortem laboratories do not<br />
practice analyzing alternative matrices to interpret methadone's contribution to a death. In fact, limited<br />
publications discuss whether postmortem redistribution occurs and if so to what degree. Furthermore, some<br />
postmortem laboratories have traditionally ignored methadone liver concentrations based on the belief that their<br />
interpretative values are minimal. Moreover, overlapping therapeutic and toxic ranges make it difficult to<br />
interpret methadone's contribution to a death without having additional history, pathological findings (e.g.<br />
bronchopneumonia or peri mortem aspiration), and/or dosing regime. Given these observations, the Office <strong>of</strong> the<br />
Chief Medical Examiner (NC-DCME) retrospectively reviewed all deaths in the State <strong>of</strong> North Carolina between<br />
200 I and 2002 in which methadone was detected during toxicological analysis. This presentation evaluates 223<br />
death investigations in which methadone was detected in several postmortem tissues and fluids to ascertain<br />
whether or not data from alternative specimens are more useful than originally thought.<br />
After careful review <strong>of</strong> the history, pathology and toxicology findings, it was determined that 180 (80%) cases<br />
could be evaluated given the data obtained. Exclusion criterion included cases in which the prescription status<br />
was unknown or multiple drugs were detected in toxic concentrations. To assist in interpretation, these cases<br />
were divided into several groups based on their drug use pattern and the assigned cause <strong>of</strong> death. These groups<br />
are as follows: 1) methadone-related death in a methadone-prescribed!tolerant individual 2) methadone-related<br />
death in a methadone-not prescribed or -recently prescribed! non-tolerant individual 3) methadone unrelated to<br />
death or indirectly contributed to death (i.e. controls). The following table presents data from representative<br />
observations <strong>of</strong> this study:<br />
Group<br />
Central Peripheral Central! Liver Liverl Presence <strong>of</strong> Presence <strong>of</strong><br />
Blood Blood Peripheral (mglkg) Central Broncho<br />
(mglL) (mglL)<br />
aspiration<br />
Ratio Ratio pneumonia <br />
mean <br />
(n= 46) median 0.68 0.36 1.5 2.6 4.7 10 (21%) 3 (6.5%) <br />
range 0.1-9.9 0.07-1.9 OAI-2.3 0.44-17 0.72-19 <br />
2 mean OA9 0.34 1.8 2.5 7.5 <br />
(n= 105) median 0.38 0.35 1.2 2.2 6.3 42 (40%) 14 (13%)<br />
range 0.05-2.5 0.047-0.82 OA7-7.3 0.36-9.3 1.4-25<br />
mean<br />
(n= 29) median 0.25 2.2 1.7 4 (13%) 2 (6.8%)<br />
range 0.03-0.72 1.2-3.8 0.19-27<br />
This investigation supports that postmortem redistribution <strong>of</strong> methadone can occur and may be significant in<br />
some cases. Liver concentrations when compared to central blood do not readily distinguish a methadone<br />
overdose from a methadone-unrelated death, especially if the dosing regime is unknown. Bronchopneumonia and<br />
perimortem aspiration, although they can support methadone ingestion, do not always occur (13-40% and 6-13%,<br />
respectively). These data suggest that while collection and analysis <strong>of</strong> blood from a peripheral source, in addition<br />
to review and consideration <strong>of</strong> pathological findings and drug use history, can improve the interpretation <strong>of</strong><br />
toxicological data in methadone-related deaths, liver concentrations may have less interpretive value.<br />
Keywords: Methadone, Interpretation, Postmortem Fluids and Tissues<br />
Page 354
P20 <br />
A COMPARISON OF METHADONE, HYDROCODONE, AND OXYCODONE ASSOCIATED<br />
MORTALITY IN CUYAHOGA COUNTY, OHIO: 1998 - 2003<br />
Daniel D. Baker IV*, and Amanda J. Jenkins, The Office <strong>of</strong>the Cuyahoga County Coroner<br />
11001 Cedar Ave., Cleveland, OH 44106, U.S.A.<br />
Significant increases in methadone related deaths have been recently documented across the United States.<br />
Historically, the substantial rise in oxycodone associated mortality is well documented as opposed to<br />
hydrocodone, where a paucity <strong>of</strong> literature remains. In response to these reports, the authors investigated<br />
cases over a six-year period in which postmortem toxicological analyses revealed the presence <strong>of</strong><br />
methadone, hydrocodone, and oxycodone in any matrix type. The study was designed to detennine<br />
whether methadone associated mortality in Cuyahoga County reflected national trends and more<br />
specifically, to distinguish methadone trends from other commonly used opioid analgesics.<br />
All records <strong>of</strong> decedents that were found to be positive for methadone, hydrocodone, and oxycodone from<br />
1998-2003 were reviewed. Demographic information including age, sex, race, and location <strong>of</strong> residence<br />
was collected. The cause and manner <strong>of</strong> death was compiled and the cases were divided into drug<br />
overdoses and those cases where a positive result was detennined to be an incidental finding. Overdoses as<br />
a result <strong>of</strong> only methadone, hydrocodone, and oxycodone were separated from poly drug overdoses. The<br />
data was calculated for each type <strong>of</strong> drug based on quantitative heart blood drug concentrations for<br />
comparison.<br />
Review <strong>of</strong>21,460 deaths in Cuyahoga County, from 1998-2003, revealed that a total <strong>of</strong> 55 decedents were<br />
positive for methadone and <strong>of</strong> these, 29% were ruled overdoses. 202 cases were found to be positive for<br />
hydrocodone in which, 28% were due to a lethal dose. Oxycodone was discovered in 190 decedents <strong>of</strong><br />
which, 29% were caused by an overdose. Mortality caused by methadone, hydrocodone, and oxycodone<br />
increased 400%,183%, and 366% respectively from 1998 to 2003.<br />
Demographic data revealed 286 males and 161 females were positive for the studied opioids. 351 opioid<br />
positive decedents were white, as opposed to 96 black. Decedent ages ranged from 2 to 101 years.<br />
Caucasian males between the ages <strong>of</strong> 34 and 51 (mean 42.5 ±2SD) were the demographic group<br />
predominantly positive for each <strong>of</strong> the three opioids. Decedents in which methadone was detected were<br />
shown to live within Cleveland city limits vs. the suburbs 3:1, as opposed to hydrocodone and oxycodone<br />
positive decedents who principally resided in the suburbs.<br />
Heart blood methadone overdose concentrations ranged from 0.11-1.31 mg/L (mean=0.67 mgIL, n=19) <br />
Similarly, heart blood methadone incidental finding concentrations ranged from 0.08-4.26 mgIL <br />
(mean=0.76 mgIL, n=35). Lethal. hydrocodone heart blood concentrations ranged from 0.01-1.66 mgIL <br />
(mean=0.29 mg/L, n=54). Incidental hydrocodone findings ranged from 0.01-2.56 mgIL (mean=0.11 mgIL, <br />
n=112). Oxycodone overdose concentrations ranged from 0.01-36.54 mg/L (mean=1.80 mg/L, n=48). <br />
Oxycodone positive concentrations that were detennined to be incidental findings ranged from <br />
0.01-1.78 mg/L (mean=0.31 mg/L, n=81). <br />
During the study period, an increase was observed in the number <strong>of</strong> positive cases for all three opioid<br />
analgesics. In conflict with recent national data however, although the number <strong>of</strong> methadone positive cases<br />
increased from 4 cases in 1998 to 18 cases in 2003, this did not result in a substantial increase in methadone<br />
overdoses, 1 death in 1998 to 4 deaths in 2003. No methadone level <strong>of</strong> lethal toxicity was discemable by<br />
comparing decedents whose death was caused by methadone intoxication as opposed to, an incidental<br />
finding. In contrast, the mean lethal hydrocodone and oxycodone blood concentrations were definable, at<br />
two and five times greater than non-overdose mean blood concentrations, respectively. Methadone,<br />
hydrocodone, and oxycodone overdoses equally comprised 28-29% <strong>of</strong> cases in which these drugs were<br />
detected.<br />
Keywords: Methadone, Oxycodone, Hydrocodone<br />
Page 355
P21 <br />
"STUDENT ON ALPHA-METHYLTRYPTAMINE DISCOVERS mE SECRET OF THE<br />
UNIVERSE.•• AND DIES"<br />
Diane M. Boland*, Wilmo Andollo, George W. Hime, and William L. Hearn, Dade County Medical<br />
Examiner, Number One on Bob Hope Rd, Miami, FL, 33136<br />
Alpha-methyltryptamine (AMT) is a synthetic indole analog <strong>of</strong> amphetamine initially investigated as a<br />
monoamine oxidase inhibitor. In the 1960s, the Soviet Union marketed AMT as an antidepressant under<br />
the name <strong>of</strong>lndopan. During the same period, the Upjohn Company studied the alpha-ethylated analog for<br />
use as a commercial antidepressant known as Monase, but found it to be <strong>of</strong> little medicinal value.<br />
Although clinical use <strong>of</strong> AMT is obsolete today, recreational use has gained popularity due to its intense<br />
hallucinogenic properties lasting up to 16 hours. To illustrate recreational use <strong>of</strong> AMT in the 1960s,<br />
Alexander Shulgin in his book Tihkal, references the author Ken Kesey and his experiences with AMT and<br />
other hallucinogenic drugs.<br />
Today, AMT is recognized as a powerful psychedelic drug among high school and college-aged men and<br />
women who may have experienced the effects <strong>of</strong> other hallucinogenic amphetamines. Its popularity is<br />
partly due to the legality and availability <strong>of</strong> AMT for purchase via the Internet prior to April 2003.<br />
Emergency designation <strong>of</strong> AMT as a Schedule 1 controlled substance by the Drug Enforcement<br />
Administration occurred shortly after the Miami-Dade Medical Examiner reported the death <strong>of</strong> a 22 yearold<br />
college student who ingested a large amount <strong>of</strong> AMT. Prior to death, the deceased advised his<br />
roommate that he was ''taking hallucinating drugs" and as a result had "discovered the secret <strong>of</strong> the<br />
universe". The roommate reported that the deceased was shaking and sweating pr<strong>of</strong>usely. Approximately<br />
12 hours later, the roommate discovered the deceased lying in bed unresponsive. An empty Igram vial <strong>of</strong><br />
AMT was recovered from the scene and sent to the Toxicology Laboratory. An autopsy by the Medical<br />
Examiner did not reveal any significant gross findings <strong>of</strong> any organs, and no evidence <strong>of</strong>traumatic injury.<br />
Initial screening <strong>of</strong> urine by enzyme-multiplied immunoassay technique was positive for amphetamines,<br />
and the basic drug blood screen detected a small peak later identified by mass spectrometry as AMT. For<br />
quantitation, AMT was isolated using solid phase extraction, derivatized with pentafluoropropionic<br />
anhydride, and analyzed using gas chromatography/mass spectrometry. Ions monitored for AMT included<br />
mlz 276, 303, and 466. Quantitative analysis was based upon mJz 276 for AMT and mJz 306 for the<br />
internal standard 5-methoxy-alpha-methyltryptamine. A linear calibration curve from 50 to 500ng/mL was<br />
used to calculate· the concentration <strong>of</strong> AMT in the samples and controls. Blood, tissue, and gastric<br />
specimens were diluted to bring the observed concentration within the limits <strong>of</strong> the standard curve. Matrix<br />
matched controls were extracted and analyzed with each run. Postmortem blood revealed 2.0mg/L, gastric<br />
contents 9.6mg total, liver 24.7mgikg, and brain 7.8mgikg.<br />
Keywords: Alpha-methyltryptamine, 5-Methoxy-alpha-methyltryptamine, hallucinogens<br />
Page 356
!~.<br />
P22 <br />
TILL DEATH DO US PART: FENTANYL POISONING IN A HUSBAND AND WIFE<br />
George S. Behonick, Ph.D:, Tara Valouch, B.S., Virginia Division <strong>of</strong> <strong>Forensic</strong> Science Western<br />
Laboratory and Susan E. Venuti, M.D., Assistant Chief Medical Examiner, Western District Office <strong>of</strong> The<br />
Chief Medical Examiner and Assistant Clinical Pr<strong>of</strong>essor, Department <strong>of</strong> Legal Medicine at Virginia<br />
Commonwealth University, 6600 Northside High School Road, Roanoke, V A 24019<br />
One treatment modality for chronic pain is the application <strong>of</strong> fentanyl transdermal patches (Duragesic®).<br />
However, the transdermal therapeutic system, designed for the rate-controlled delivery <strong>of</strong> drug, is<br />
increasingly favored by members <strong>of</strong> the opioid-misusing/abusing population. Deliberate misuse or abuse<br />
may include cutaneous application <strong>of</strong> mUltiple patches, transmucosal absorption (buccal cavity), inhalation<br />
<strong>of</strong> volatilized fentanyl and intravenous injection <strong>of</strong> contents extracted from trans dermal patches. The selfdelivery<br />
<strong>of</strong> drug also occurs by simultaneously combining different routes <strong>of</strong> administration. Herein we<br />
describe a case report <strong>of</strong> two fatal fentanyl poisonings which occurred in a married couple within a five<br />
hour time interval. We discuss the available medical histories <strong>of</strong> the two decedents (including prescribed<br />
medications) together with first responder witness reports and significant findings from both autopsies and<br />
the postmortem toxicological analyses in each case. Physical evidence included a 75 jlg/h fentanyl<br />
transdermal patch retrieved from the oral cavity or airway <strong>of</strong> the female decedent during resuscitative<br />
efforts at the scene and a "disrupted" (e.g., cut) 75 jlg/h fentanyl transdermal patch recovered in the<br />
personal effects <strong>of</strong> the male decedent at autopsy. The postmortem blood fentanyl concentrations measured<br />
in the 45-year-old white female decedent and the 52-year-old white male decedent were 0.050 mg/L and<br />
0.030 mg/L, respectively. Fentanyl was extracted from blood using solid phase extraction and quantitated<br />
by 81M GCMS using a previously published procedure.<br />
Key Words: fentanyl, poisoning, blood<br />
Page 357
P23 <br />
CASE REPORT: THE USE OF AMITRIPTYLINE IN DRUG FACILITATED SEXUAL ASSAULT<br />
Kristina Fritz* <br />
Los Angeles County Department <strong>of</strong> Coroner, 1104 N. Mission Road, Los Angeles, CA 90033 <br />
Amitriptyline is a tricyclic antidepressant with sedative effects that has been available in the United States<br />
since the early 1960's. It is administered in 10-150 mg tablets or as a 10 mgIL injectable solution. While<br />
amitriptyline is commonly encountered by the Los Angeles County Department <strong>of</strong> Coroner Toxicology<br />
Laboratory, the circumstances <strong>of</strong> its use in four Southern California homicides is unique.<br />
Four murders occurred between April 2000 and April 2001. The victims, two females and two males, were<br />
initially invited for consensual sex. They were then drugged, sexually abused, bound with ligatures, and<br />
ultimately killed. This report reviews four cases <strong>of</strong> drug-facilitated sexual assault using amitriptyline. The<br />
presence <strong>of</strong> amitriptyline in high concentrations coupled with unique criminalistics evidence aided in the<br />
linking <strong>of</strong> this series <strong>of</strong> homicides across county jurisdictions.<br />
The analysis <strong>of</strong> amitriptyline from postmortem. specimens consisted <strong>of</strong> a basic, liquid/liquid (nbutylchloride)<br />
extraction procedure with screening and quantitation by GC/NPD. Linearity was achieved<br />
from 0.10 to 5.0 mg/L with the limit <strong>of</strong> quantitation at 0.10 mgIL. Confirmation <strong>of</strong> amitriptyline was<br />
determined using a GCIMS by comparison with an analytical standard.<br />
The following amitriptyline concentrations are reported.<br />
~..,__,__,.._. ,~.._..,_..__~!!tr_~~,~~~..._..._,__ -,_.._......._._...<br />
Central Hood Peri(Deral Hood liver Gastric Brain<br />
Case # 1 - - 86 19rrg 62<br />
Case #2 - - 76 - 83<br />
Case #3 O.IX> 0.11 1
P24 <br />
"THE DOSE MAKES THE POISON", DISCUSSION OF THREE CASES OF LETHAL HEROIN<br />
INTOXICA TIONS<br />
W Bemhard*, B Aebi, M Gasser, St. Bolliger, Institute <strong>of</strong> Legal Medicine, Bern, Switzerland,<br />
W. Vycudilik, Institute <strong>of</strong>Legal Medicine, Vienna, Austria<br />
Introduction: The lethal dose <strong>of</strong> heroin differs widely. Tolerance plays a key role. To the persons in the<br />
<strong>of</strong>ficial Swiss heroin program, the drug is <strong>of</strong>ten prescribed in high dose. In spite <strong>of</strong> the medical<br />
surveillance, lethal poisoning is not an uncommon finding.<br />
Results: Case A) A 35 y.o. male administered himself (intravenously) under medical observation in 30 min.<br />
400 mg chemically pure heroin and ingested 500 mg Morphine-retard. He then went back home. Two days<br />
later he was found death in his flat. Toxicological findings: heart blood: free morphine 1605 nglmL, M-3-G<br />
686 ng/mL, M-6-G 390 ng/mL. Interpretation: the deceased did not swallow the Morphine-retard capsules.<br />
He smuggled them out <strong>of</strong> the injection place, the so-called "Fixerstilbli" and injected them instead. Cause<br />
<strong>of</strong> death: heroin and morphine intoxication. Manner <strong>of</strong> death: suicide or accident. Case B) A 39 y.o. male<br />
came by himself to a hospital with stomach pain. During the medical treatment he received O.2mg <strong>of</strong><br />
fentanyl and 5mg diazepam by the medical staff. During his stay he snorted two times a powder which was<br />
believed by the nurses to be cocaine. Four hours after the start <strong>of</strong> the medical treatment he died.<br />
Toxicological findings: serum (peripheral) sample taken at the hospitalization: free morphine 267 nglmL,<br />
Codeine 32 nglmL. Serum from heart blood collected at the autopsy: free morphine 726 nglmL, codeine<br />
120 ng/mL. Findings: The patient snorted, instead <strong>of</strong> cocaine, "street heroin". Cause <strong>of</strong> death: heroin<br />
poisoning. Manner <strong>of</strong> death: suicide or accident. Case C) A 28 y.o. female was found dead in her flat. An<br />
injection mark was found in her right antecubital fossa. Toxicological findings: heart blood: free morphine<br />
140 nglmL, total morphine 693 ng/mL. Results <strong>of</strong> police investigation: a stranger injected approx. 400 mg<br />
<strong>of</strong> street heroin (purity approx 15%) intravenously on this female on her request. Cause <strong>of</strong> death: heroin<br />
poisoning. Manner <strong>of</strong> death: killing on request.<br />
Conclusions: High doses <strong>of</strong> heroin and morphine are needed to satisfy the patients in the <strong>of</strong>ficial heroin<br />
program, and are typically tolerated by them. However, in spite <strong>of</strong> medical surveillance lethal overdoses are<br />
observed. Quite low heroin doses may be lethal for opiate-naive subjects.<br />
Keywords: heroin, morphine, postmortem<br />
Page 359
P25 <br />
ECSTACY MANUFACTURE: A CASE FOR QUALITY CONTROL<br />
Jim Gerostamoulos*, Matthew Lynch, and Olaf H. Drummer.<br />
Victorian Institute <strong>of</strong> <strong>Forensic</strong> Medicine, Department <strong>of</strong> <strong>Forensic</strong> Medicine, Monash University, 57-83<br />
Kavanagh St., South bank, Victoria 3006, AUSTRALIA<br />
This case report involves the death <strong>of</strong>a 25 year old male who was found deceased in his boarding room some<br />
2!t2 days after last being seen alive. The decedent's body was located face down on his bed. There were no<br />
signs <strong>of</strong> drug use and no medication/illicit drugs were discovered at the scene by attending police.<br />
A full autopsy was performed on the deceased to determine the cause <strong>of</strong> death. Macroscopic findings<br />
indicated putrefactive changes with extensive autolysis <strong>of</strong> internal organs in keeping with early stages <strong>of</strong><br />
decomposition. There was marked pUlmonary oedema and bilateral hydronephrosis. There were no other<br />
significant pathological findings. Specimens submitted for toxicological analysis revealed a free morphine<br />
concentration (cavity blood)-60 mgIL; 4.2 mg/kg (liver); total morphine 76 mgIL (urine); and 190 mg <strong>of</strong><br />
morphine in stomach contents. No 6-acetyl morphine was detected in blood or urine, and no other drugs or<br />
alcohol were detected. The cause <strong>of</strong> death was given as morphine toxicity.<br />
Additional information provided by the family indicated a family history <strong>of</strong> sleep apnoea. Tablets, located in<br />
the decedent's bedroom and which according to the girlfriend belonged to the deceased, were submitted to<br />
the laboratory for analysis some weeks after the death. The 3 tablets (green, scored with the markings CK on<br />
either side) and initially purchased presumably as ecstacy, were identified as containing 100 mg <strong>of</strong> morphine<br />
with trace amounts <strong>of</strong> methamphetamine. The decedent had consumed at least two <strong>of</strong> these tablets or more<br />
resulting in his death. This case illustrates the danger <strong>of</strong> experimenting with illicit drugs and serves as a<br />
reminder that information germane to medicolegal death investigation can come from a variety <strong>of</strong> sources.<br />
The Coroner found that the death was an accidental overdose.<br />
Keywords: ecstacy, morphine, death.<br />
Page 360
P26 <br />
A RETROSPECTIVE STUDY OFOXYCODONE DEATHS IN ONTARIO 1999-2003<br />
lCentre <strong>of</strong> <strong>Forensic</strong> Sciences, 25 Grosvenor St, Toronto, Ontario, M7A 208. 2Northem Regional <strong>Forensic</strong><br />
Laboratory, Centre <strong>of</strong> <strong>Forensic</strong> Sciences, 70 Foster Dr, Sault Ste. Marie, Ontario, P6A 6V3. 30ffice <strong>of</strong> the<br />
Chief Coroner, 26 Grenville St, Toronto, Ontario, M7A 2G9.<br />
This report presents the results <strong>of</strong> a retrospective study aimed at determining the role <strong>of</strong> oxycodone in<br />
deaths investigated by the Office <strong>of</strong> the Chief Coroner in Ontario, Canada, between 1999 and 2003. The<br />
objectives <strong>of</strong> the study were 1) to assess changes over this period in the prevalence <strong>of</strong> oxycodone in deaths<br />
investigated by the coroners, and 2) to assess the extent to which these deaths were oxycodone-induced or<br />
oxycodone-related. The cases included in this study were death investigations in which specimens obtained<br />
from a medico-legal autopsy, were submitted to the Centre <strong>of</strong> <strong>Forensic</strong> Sciences for a toxicological<br />
examination. In all but three cases, examinations consisted <strong>of</strong> analysis for alcohols, a general drug<br />
screening procedure that detects a range <strong>of</strong> therapeutic agents and illicit substances that exhibit central<br />
nervous system toxicity and are encountered in postmortem toxicology, and targeted analyses for the<br />
quantitation and confirmation <strong>of</strong> screen findings. Cases were included in this study only when a blood<br />
oxycodone finding was available. In the majority <strong>of</strong> cases, analysis was performed on heart blood, and in<br />
others, on samples identified as femoral or peripheral venous, or from an unspecified source. Quantitation<br />
<strong>of</strong> total oxycodone in whole blood was carried out using a liquidlliquid basic extraction, followed by a gas<br />
chromatographic analysis using a nitrogen/phosphorous detector and capillary fused silica columns.<br />
A total <strong>of</strong> 291 cases met the inclusion criteria for this study, representing 194 males and 97 females.<br />
Oxycodone-positive cases submitted to this laboratory in 1999 numbered 22 and increased steadily each<br />
year to reach 101 in 2003. The increase in annual submissions was markedly disproportionate to the<br />
overall increase in submissions. Although no attempt was made in this phase <strong>of</strong> the study to determine<br />
whether the detected oxycodone was due to the ingestion <strong>of</strong> Oxycontin® or any other oxycodonecontaining<br />
formulation, it is noteworthy that the increase in the prevalence <strong>of</strong> oxycodone findings in death<br />
investigations coincides with the introduction <strong>of</strong> Oxycontin® to the Canadian market in about 1996. In<br />
order to assess the involvement <strong>of</strong> oxycodone in these deaths, the coroner's conclusion regarding the cause<br />
<strong>of</strong> death was recorded. In 39 cases over this five-year period, death was attributed to natural causes or<br />
trauma, but not related to the presence <strong>of</strong> oxycodone. Blood oxycodone concentrations ranged from less<br />
than 0.01 to 0.9 mg/L.<br />
In the remaining cases (n == 252), death was determined by the coroner to be drug-induced or drug-related.<br />
Based on the reported postmortem blood toxicology findings, cases were divided into four categories: 1)<br />
oxycodone alone (2%); 2) oxycodone and other drugs in therapeutic concentrations, with ethanol present at<br />
or below 50 mg/IOO mL (20%); 3) oxycodone and other drugs in potentially toxic concentrations, with<br />
ethanol in excess <strong>of</strong> 50 mg/l00 mL (59%); and 4) oxycodone and other drugs in potentially fatal<br />
concentrations (19%). The blood oxycodone concentration ranges for each group were 0.1 to 0.92 mg/L,<br />
0.1 to 5.5 mg/L, less than 0.01 to 9.8 mglL, and 0.03 to 4.4 mg/L, respectively.<br />
The observed overlap in blood oxycodone concentrations across these groups underscores the importance<br />
<strong>of</strong> other factors such as polydrug use, drug formulation, and the experience <strong>of</strong> the user in assessing the<br />
contribution <strong>of</strong>oxycodone to the death.<br />
Keywords: oxycodone, postmortem, toxicology<br />
Page 361
P27 <br />
ANALYSIS OF POSTMORTEM BONEIBONE MARROW SPECIMENS FOR DRUGS OF<br />
IMPORTANCE IN FORENSIC TOXICOLOGY<br />
Kelly K. McGrath* and Amanda 1. Jenkins, Ph.D, The Office <strong>of</strong> the Cuyahoga County Coroner, 11001<br />
Cedar Avenue, Cleveland, OH 44106, U.S.A.<br />
To date, there is a paucity <strong>of</strong> literature published on the determination <strong>of</strong> drugs in bone and bone marrow.<br />
This type <strong>of</strong> research is important forensically because the extraction <strong>of</strong> bone specimens may be useful<br />
when traditional postmortem samples are not available for toxicological analysis. Postmortem bone<br />
samples, taken from the iliac crest in adults and vertebrae in infants, were extracted and analyzed for the<br />
presence <strong>of</strong> benzodiazepines and cocaine and metabolites. The purpose <strong>of</strong> this study was to correlate the<br />
concentration <strong>of</strong> drugs found in postmortem blood with the concentrations in boneibone marrow samples.<br />
The specimens were thoroughly cleaned by removing all traces <strong>of</strong> skeletal muscle and tissue and then<br />
rinsing with deionized water until the wash ran clear. Two grams <strong>of</strong> each bonelbone marrow sample was<br />
cut into slivers and soaked in 4 milliliters <strong>of</strong> methanol for sixteen hours (± 0.5 hours). Cocaine and<br />
metabolites were extracted from the methanol by liquid/liquid extraction followed by solid phase extraction<br />
(SPE), derivatization with MSTFA,· and analysis by GCIMS in single ion monitoring (SIM) mode.<br />
Benzodiazepines (BDP) were isolated from the methanol extract by liquid/liquid extraction and analyzed<br />
by GC/ECD.<br />
The concentration <strong>of</strong> drugs found in the bonelbone marrow samples was compared to postmortem blood<br />
toxicology results. Three <strong>of</strong> seven cases analyzed for cocaine and metabolites were positive. In one case,<br />
cocaine was quantitated at 120 nglg bone, cocaethylene 80 nglg bone, and ecgonine methyl ester (EME)<br />
was qualitatively positive. The heart blood results in this case were benzoylecgonine (BE) 332 ng/ml,<br />
cocaine 144nglml, cocaethylene 32 nglml, and EME qualitatively positive. In another case, BE was<br />
quantitated at 666 nglg bone and in the heart blood BE was 522 nglml. The third case had 48 nglg bone<br />
cocaethylene and EME was qualitatively positive. The heart blood in this case contained 211 ng/ml BE, 29<br />
nglml cocaine, and EME was qualitatively positive. The remaining four cases were negative for cocaine<br />
and metabolites in the boneibone marrow and the blood concentrations for BE and cocaine ranged from<br />
123 nglrnl-394 nglml and 24 ng/ml-29 nglml respectively. These positive cases demonstrate that cocaine<br />
and metabolites can be detected in bone, but the presence <strong>of</strong> specific analytes may differ from those present<br />
in the blood and the concentration <strong>of</strong> the analytes in boneibone marrow may be higher or lower than that in<br />
the blood. Therefore, these results should be interpreted cautiously.<br />
Six cases were examined for the presence <strong>of</strong>BDP. Ofthese six cases, four were positive for diazepam with <br />
values ranging from 0.60 ug/g bone-2.4 ug/g bone, four were positive for desmethyldiazepam (DMD) with <br />
. values ranging from 0.32 uglg bone-l.6 uglg bone, and one case was unsuitable for analysis. In the cases <br />
where diazepam was positive in the bonelbone marrow, the heart blood concentrations ranged from 0.13 <br />
mg/L-0.39 mg/L. DMD in the heart blood ranged from 0.10 mg/L-0.67 mg/L. In every case where <br />
diazepam and/orDMD were present in the heart blood, both were also recovered in the boneibone marrow. <br />
These results demonstrate that· bonelbone marrow specimens may be utilized as an alternative matrix for<br />
postmortem toxicological analysis where traditional matrices are not available. The preliminary data on<br />
cocaine and metabolites and BDP failed to show a linear correlation between boneibone marrow and blood<br />
drug concentrations. It appears that the likelihood <strong>of</strong> detecting a drug in boneibone marrow specimens<br />
depends on the type <strong>of</strong> drug being analyzed. Future investigation <strong>of</strong> other drug classes such as opiates,<br />
basic, and acidic/neutral drugs may provide additional information for the elucidation <strong>of</strong> correlation data<br />
between bonelbone marrow and blood specimens.<br />
KEYWORDS: Bone, Cocaine, Benzodiazepine<br />
Page 362
P28 <br />
DRUG RELATED DEATHS IN THE CITY AND COUNTY SAN FRANCISCO<br />
NP Lemos*, PhD, SB Karch, MD, E Lin, MS, G Nazareno, MD, V Azar, MD, A Hart, MD and BG<br />
Stephens, MD<br />
Aims: The timely detection <strong>of</strong> drug-related health problems and emerging drug trends depend, at least in<br />
part, on information provided by coroners and medical examiners. To assist in this process we reviewed all<br />
drug-related deaths occurring in our jurisdiction during 2002.<br />
Design: Retrospective analysis <strong>of</strong> all death investigations carried out by the San Francisco Office <strong>of</strong> the<br />
Chief Medical Examiner (SFOCME), from January 1, 2002 until December 31, 2002, where postmortem<br />
toxicology revealed the presence <strong>of</strong> psychoactive or abused drugs, and complete autopsy performed.<br />
Methods: If available, urine is first screened with EMIT testing and results confirmed by GCIMS or<br />
LCIMS. In the absence <strong>of</strong> urine, GCIMS is used to screen blood, liver, CSF or other biological specimens<br />
directly.<br />
Findings: The SFOCME serves a population <strong>of</strong> approximately 750,000, and this number has been stable for<br />
several decades. In 2002, 1463 cases came under the jurisdiction <strong>of</strong> our <strong>of</strong>fice, and drugs were detected in<br />
257 <strong>of</strong> these cases. Cocaine or benzoylecgonine was found in the blood and/or urine <strong>of</strong> 153 (59%) cases.<br />
Morphine and/or codeine were detected in the blood or urine <strong>of</strong> 119 (46%), and methamphetamine was<br />
present in 19% (48/257). Poly-drug abuse was common among the cases which came under our<br />
jurisdiction. Morphine was present in nearly a third (72/257, 28%), <strong>of</strong> the cocaine users. The occurrence<br />
rate for other drugs was much lower; methadone was present in 33 cases, oxycodone in 23, fentanyl in 7,<br />
hydrocodone in 6, MDMA in 5, and PCP in 2 cases.<br />
Conclusions: The number <strong>of</strong> methamphetamine-related deaths continues to be remarkably stable within our<br />
jurisdiction and is, in fact, lower than in 1994, when 52 deaths were recorded (J <strong>Forensic</strong> Sci. 1999 Mar;<br />
44(2):359-68). The rate for methadone related deaths also appears to be stable, while the number <strong>of</strong><br />
oxycodone-related deaths appears to be increasing, suggesting that allocating additional resources to treat<br />
methadone diversion may be unnecessary in our jurisdiction. On the other hand, the increasing number in<br />
fentanyl-related deaths suggests that diversion <strong>of</strong> Duragesic® patches in our jurisdiction is an increasing<br />
problem worthy <strong>of</strong> further investigation.<br />
Keywords: Drug, Epidemiology, San Francisco<br />
Page 363
P29 <br />
THE ROLE OF COCAINE IN HEROIN RELATED DEATHS. HYPOTHESIS ON THE HEROIN<br />
COCAINE INTERACTION<br />
A. Polettini*, V. Poloni, A. Groppi, C. Stramesi, C. Vignali, L. Politi, M. Montagna<br />
Department <strong>of</strong> Legal Medicine & Public Health, University <strong>of</strong> PaVia, Via Forlanini 12, 27100 PAVIA,<br />
Italy<br />
In recent years, drugs-<strong>of</strong>-abuse related deaths involving cocaine observed at the Department <strong>of</strong> Legal<br />
Medicine & Public Health <strong>of</strong> Pavia have shown an increase, probably reflecting the rising trend in cocaine<br />
use in Western Europe: "pure" cocaine deaths have increased from 6 cases in 1979-1991 (1.5% <strong>of</strong> drug-<strong>of</strong>abuse<br />
deaths) to 13 in 1992-2002 (3,2%), and in the same periods heroin related deaths (HRDs) involving<br />
cocaine amounted to 8 (1.9%) and 22 (5.4%), respectively. In the attempt to investigate the role <strong>of</strong> cocaine<br />
in HRDs, acute narcotism cases testing positive for cocaine and/or metabolites in blood (>10 ngtml,<br />
COC+) were examined. Only cases occurred from 1997 to 2001 were considered as in this period all data<br />
were obtained using the same analytical procedures (free morphine and total morphine by DPC Coat-A<br />
Count radioimmunoassay before and after enzymatic hydrolysis, cocaine and metabolites in blood by SPE,<br />
TMS derivatization and GC-MS). The median, minimum and maximum concentration <strong>of</strong> free morphine<br />
(FM) and total morphine in blood (TM), urine (UM) and bile (BM) in the COC+ group (n=9) were<br />
compared with those calculated in the group <strong>of</strong> "pure" HRDs (no other drugs detected in blood, COCo,<br />
n=30). Differences among the two groups were statistically evaluated using the two-tailed Mann-Whitney<br />
U Test. Statistical analysis was also carried out including in both groups cases testing positive (>2 mgtdL)<br />
for blood alcohol (COC+, n=19; COCo, n=76). The median TM was found to be lower in the COC+ group<br />
(0.32 mg/l vs. 0.90 mg/l, P=0.0214) and also the median FM (0.08 mgtl vs. 0.28 mg/l, P=O.l064). The<br />
FMITM ratio was similar in the two groups (0.33 and 0.35) and also UM (21.0 mg/J and 18.0 mg/J),<br />
whereas BM was higher (90.0 mgtl vs. 49.0 mgtl, P=0.0268). Similar results were obtained by repeating<br />
statistical analyses after including in the two groups cases with positive blood alcohol concentration<br />
(BAC). This picture is very different from what was previously observed for the heroin-ethanol interaction<br />
in HRD cases CA. Polettini et al., J. Anal. Toxico!., 23, 570, 1999), and updated with more recent data: in<br />
the high-ethanol (HE, BAC >100 mg/dl) group TM was lower than in the low-ethanol (LE, BAC:5100<br />
mgtdl) group (0.59 mg/l vs. 0.90 mgtl, P=0.0180), the FMlTM ratio was higher (0.66 vs. 0.43, P=0.0038),<br />
FM was equal, UM was lower (0.21 mgtl vs. 26.5 mg/J, P=O.OOOl), and so BM (10.0 mgtl vs. 26.5 mg/l,<br />
P"-'0.0156). Indeed, the observed lower TM in the COC+ and in the HE groups support the hypothesis <strong>of</strong>an<br />
interaction <strong>of</strong> both cocaine and ethanol with heroin in the occurrence <strong>of</strong> death. Ethanol results suggest that<br />
a pharmacokinetic interaction is prevalent (inhibition <strong>of</strong> heroin metabolism, as suggested by the increased<br />
FM/TM ratio, resulting in reduced urinary and biliary excretion). In the case <strong>of</strong> cocaine, a<br />
pharmacodynamic interaction seems to prevail, as the FMITM ratio remains unchanged and UM and BM<br />
are not lower in the COC+ group. This hypothesis could not be confirmed owing to the paucity <strong>of</strong> data and<br />
the many uncontrolled variables involved.<br />
Keywords: heroin related death, cocaine, interaction<br />
Page 364
P30 <br />
DRUG EXPOSURE PATTERN IN HAIR AND FEMORAL BLOOD IN DECEASED DRUG<br />
ADDICTS<br />
Henrik Druid!', Joakim Strandberg!, Ingrid Nystrom 2 , Kanar Alkassl, Fredrik Kugelberg 3 and Robert<br />
Kronstrand 2<br />
IDepartment <strong>of</strong> <strong>Forensic</strong> Medicine, Karolinska Institutet, SE-171 77 Stockholm, Sweden; 2Department <strong>of</strong><br />
<strong>Forensic</strong> Chemistry, National Board <strong>of</strong> <strong>Forensic</strong> Medicine, SE-581 85 Linkoping, Sweden; 3Departrnent <strong>of</strong><br />
Clinical Pharmacology, University <strong>of</strong>Linkoping, SE-581 85 Linkoping, Sweden<br />
Blood drug levels <strong>of</strong> illicit drugs are <strong>of</strong>ten not particularly high in postmortem overdose cases. This is true<br />
for amphetamine and cocaine as well as for opiates. Thus, the postmortem investigations do not support the<br />
use <strong>of</strong> the word "overdose", since the dose taken in these cases is probably not much larger than is usually<br />
taken by chronic addicts. One explanation for this outcome may be reduced drug tolerance following a<br />
period <strong>of</strong> abstinence, but - although some epidemiological reports suggest a recent interruption in drug use<br />
in some cases -there are no firm data to confirm this hypothesis. It is difficult to estimate the degree <strong>of</strong> drug<br />
tolerance in deceased subjects, but hair analysis <strong>of</strong> illicit drugs may at least provide a map <strong>of</strong> the past and<br />
recent drug use pattern. In the present study, segmental hair analysis was applied on hair samples collected<br />
from 40 deceased, supposedly drug addicts, including both cases <strong>of</strong> probable drug overdoses, and cases<br />
with other causes <strong>of</strong> death. Portions <strong>of</strong> the hair samples were analyzed with an LC-MS-MS screening<br />
method, which covers amphetamine and -derivatives, cocaine and metabolites, morphine, 6<br />
monoacetylmorphine (6-MAM), codeine, diazepam, flunitrazepam, nicotine and cotinine. Positive findings,<br />
except nicotine and cotinine, were confirmed with GC-MS verification methods. For these analyses, the<br />
hair was carefully aligned and cut in short segments (the first three segments 5 mm each, and additional<br />
segments 10 mm long). The verification methods also included washing steps, and analysis <strong>of</strong> washings<br />
was carried out to control for external contamination. Femoral blood, urine and vitreous humor were also<br />
collected at the postmortem examinations for the routine toxicological drug screen. Twelve <strong>of</strong> the cases<br />
were classified as heroin overdoses by the responsible forensic pathologist. In Table 1 the number <strong>of</strong><br />
detections <strong>of</strong> seven different drugs/metabolites in hair and blood (results for benzodiazepines not shown) in<br />
these 12 cases are displayed. In most cases, a marked change in abuse pattern was evident. Hence, a<br />
gradual decrease in morphine and/or 6-MAM levels was observed in 6 <strong>of</strong> 12 cases. It was also found that<br />
the drug use at time <strong>of</strong> death, as reflected by the drugs detected in femoral blood, more <strong>of</strong>ten than not<br />
differed from the drug use pattern seen in hair. Amphetamine, cocaine, benzoylecgonineand 6-MAM were<br />
more <strong>of</strong>ten detected in hair than in blood. The opposite was true for codeine and morphine. In four cases,<br />
fentanyl was found in femoral blood in concentrations that suggest that this drug most likely was the main<br />
or a contributory factor for the demise. The results from the segmental hair analyses showed that the final<br />
heroin dose in four cases obviously had been preceded by a period <strong>of</strong> lowered drug use, or abstinence,<br />
whereas in other cases, a continuous drug use before death was disclosed. Thus, reduced tolerance may be<br />
<strong>of</strong> importance in certain cases, but in the majority <strong>of</strong> the cases, other factors seem to be more important.<br />
Interestingly, in at least four <strong>of</strong> these twelve "overdose" cases, there was evidence <strong>of</strong> a delayed death,<br />
leading to a drop in blood morphine levels. This observation underscores the importance <strong>of</strong> considering<br />
autopsy findings and circumstantial information when interpreting postmortem toxicological data - the<br />
finding <strong>of</strong> low morphine levels, and/or lack <strong>of</strong> 6-MAM does not exclude an acute opiate intoxication. It is<br />
concluded from the present study that hair analysis can assist in the toxicological evaluation <strong>of</strong> postmortem<br />
cases, and that segmental analysis can improve the interpretation further.<br />
Table 1. Number <strong>of</strong> detections <strong>of</strong> different drugs <strong>of</strong> abuse in hair and blood from 12 deceased heroin<br />
addicts classified as overdoses.<br />
L Codeine Morphine 6-MAM Amphetamine Cocaine Benzoylecgonine Fentanyl<br />
I Hair 5 5 9 5 2 2 n.a.<br />
I Blood 7 12 3 3 0 1 4<br />
Key words: Hair analysis, opiates, substance abuse<br />
Page 365
P31 <br />
TRENDS IN THE DETECTION OF DRUGS OF ABUSE IN POSTMORTEM SAMPLES<br />
Bernard Croal"', Stephen Duncan, Daniel Docherty and Patricia Rooke, Department <strong>of</strong> Clinical<br />
Biochemistry, Aberdeen Royal Infirmary, Aberdeen, Aberdeenshire, AB25 2ZD, UK<br />
Introduction: Drug misuse is a major social and economic problem facing the Grampian and Highland<br />
regions <strong>of</strong> Northern Scotland. The Oil and Fishing industries have brought wealth and reduced<br />
unemployment in these regions. Consequently, drug dealers have targeted these areas as a potential market<br />
for the selling <strong>of</strong> drugs. As a result, there has been a dramatic increase over the last decade in the number<br />
<strong>of</strong> samples screened for drugs-<strong>of</strong>-abuse in Grampian. Unfortunately, the rise in drug misuse has also seen<br />
an increase in the number <strong>of</strong> drug related deaths in Grampian and Highland over this time. Fatalities from<br />
suspicious causes are frequently associated with illegal drug misuse. We have assessed the trends <strong>of</strong> the<br />
presence <strong>of</strong> commonly abused illicit drugs in post-mortem specimens from individuals who died under<br />
suspicious and accidental circumstances in Grampian and Highland from 1994 to 2000.<br />
Methods: Post-mortem data was obtained from an archival laboratory database <strong>of</strong> forensic cases for<br />
accidental or suspicious death over the period 1994 to 2000. Drug trends were assessed in cases in which<br />
at least one drug was detected. The drugs chosen for this investigation included Amphetamine, 3,4<br />
Methylenedioxyamphetamine (MDA), 3,4-Methylenedioxymethamphetamine (MDMA; Ecstasy),<br />
Cannabinoids, Benzoylecgonine, Cocaine, Codeine, Diazepam, Dihydrocodeine, Methadone, Morphine and<br />
6-Monoacetylmorphine, since they represented the most commonly abused drugs found in Grampian and<br />
Highland. Drug detection was assessed from post-mortem blood and urine specimens collected into plain<br />
tubes and extracted by liquid-liquid or solid-phase extraction using either GC-MS or HPLC for detection.<br />
Results: A total <strong>of</strong> 2993 forensic cases were referred for analysis over the six year period. There was no<br />
evidence that the number <strong>of</strong>cases was increasing (mean =458 cases per year, regression coefficient:: 9.57,<br />
p 0.51). From these cases, 641 positive drug screens were obtained from a total <strong>of</strong> 330 individuals. A<br />
rising trend (regression coefficient; significance level) from 1994 to 1999 was observed for the presence <strong>of</strong><br />
Cannabinoids (6.29; 0.002), Codeine (5.77; 0.006), Diazepam (6.89; 0.002), Dihydrocodeine (3.26; 0.002)<br />
and Morphine (7.43; 0.004). Overall, a rising trend was observed for the presence <strong>of</strong> at least one drug<br />
(regression coefficient 13.89; p :: 0.001), with the finding <strong>of</strong> more than one drug being present also<br />
increasing.<br />
Conclusions: From 1994 to 2000 the number <strong>of</strong> positive drug tests in post-mortem specimens from this<br />
source are increasing on average by 37 cases per year. Ofthese, the number <strong>of</strong> patients with more than one<br />
positive drug is also increasing. This would fit in with the view that drug abuse is increasing within society,<br />
as is multiple drug use. Overall this study provides evidence that drugs <strong>of</strong> abuse are increasingly implicated<br />
or associated with death from suspicious causes. This evidence <strong>of</strong>the increasing involvement <strong>of</strong> drug abuse<br />
in fatalities arising from suspicious and accidental causes will strengthen the demand for increasing<br />
specialised toxicological analysis by the Procurator Fiscal, which will have pr<strong>of</strong>ound economic and<br />
resource implications upon laboratories both in Grampian and nationally.<br />
Page 366
.. ~..<br />
P32 <br />
METHOD FOR CARBON MONOXIDE DETERMINATION IN BLOOD USING GAS <br />
CHROMATOGRAPHY WITH METHANE AS AN INTERNAL STANDARD <br />
H.Samkova*, J.Pivnicka, M.Spackova <br />
Institute <strong>of</strong> <strong>Forensic</strong> Medicine <strong>of</strong> St. Anne's University Hospital Brno, Czech Republic. <br />
A gas chromatographic procedure for determination <strong>of</strong> carboxy haemoglobin in blood with a thermal <br />
conductivity detector is commonly used. Processing <strong>of</strong> blood samples for the measurement <strong>of</strong> liberated <br />
carbon monoxide and obtaining reproducible results, especially in cases <strong>of</strong> postmortem blood samples, is <br />
performed using a method with methane as an internal standard. An apparatus for postmortem blood <br />
sample preparation for CO liberation and subsequent GC determination is presented together with a <br />
description <strong>of</strong>the method that includes schematic drawings. A core part <strong>of</strong>the device is a simple reaction <br />
tube partly filled with saturated NaCI solution. Blood, diluted 1: 1 with distilled water, is added into the <br />
tube. Then the tube is closed and deaerated through a rubber septum. Through the same septum, a <br />
ferricyanide reagent and a gas mixture <strong>of</strong> H2 and CH 4 (10:1) are added. The addition <strong>of</strong> reagents and gas <br />
phase is performed in a system <strong>of</strong> communicating vessels. Methane serves as an internal standard. The <br />
reaction mixture is shaken and an aliquot part <strong>of</strong> the gas phase is injected into the gas chromatograph <br />
(chromatographic column packed with molecular sieve 5A, isothermal conditions 80'C , TCD, carrier gas: <br />
hydrogen). A blood sample saturated with carbon monoxide up to 100% is processed in the same way. <br />
Total concentration <strong>of</strong> bonded CO in the sample is calculated from peak areas <strong>of</strong> analysed sample and 100 <br />
% saturated one. <br />
Aco<br />
ACH4<br />
%CO = ( **--*--.- )samPle X ( ---.---.- )100% X 100 %<br />
ACH4<br />
Aco<br />
The calibration curve was obtained on the basis <strong>of</strong> measurements <strong>of</strong> intermixture fully saturated blood<br />
sample and negative one in required ratios.<br />
The method was validated with following parameters:<br />
COHb calibration in the range <strong>of</strong> 0 - 100% <br />
Y= 0,0031x + 0,0045 <br />
R2=0,9973 <br />
LOD 0,44 % COHb <br />
LOQ = 1,47 % COHb <br />
The method is applicable even in cases <strong>of</strong> decomposed blood. Replicate injection <strong>of</strong> the homogenous gas<br />
phase into the gas chromatograph may be performed. The precision <strong>of</strong> the determination expressed as<br />
coefficient <strong>of</strong>variation deteriorates in cases <strong>of</strong>lower concentration <strong>of</strong>COHb.<br />
Keywords: blood sample preparation, carbon monoxide, internal standard<br />
Page 367
P33<br />
POSTMORTEM CASES RELATED TO COCAINE IN THE NETHERLANDS<br />
Ll. Bosman*, M. Verschraagen, KJ. Lusth<strong>of</strong><br />
Netherlands <strong>Forensic</strong> Institute<br />
Cocaine is a popular drug and is <strong>of</strong>ten encountered in postmortem toxicology cases. In this study, we<br />
present cocaine-'related deaths in the Netherlands from October 2002 to October 2003. In this period, the<br />
presence <strong>of</strong> cocaine, benzoylecgonine and methylecgonine was demonstrated in 45 cases in which cocaine· .<br />
concentrations were 0.02 mg/I or higher. Of these 45 cases, 34 were male. The 45 deaths were divided into<br />
the following categories:<br />
I. anatomical cause <strong>of</strong> death; cocaine present with or without ethanol and other drugs (ACD, n=17)<br />
2. toxicological cause <strong>of</strong> death, cocaine as most likely cause (TCD, n=12)<br />
3. toxicological cause <strong>of</strong> death, cocaine and other drugs present, other drug(s) as most likely cause or<br />
combination (TCD+, n=6)<br />
4. no clear cause <strong>of</strong> death, cocaine present with or without ethanol and other drugs (NCD, n=8)<br />
In 12 <strong>of</strong>these 45 cases, cocaine-overdose (TCD) was the most probable cause <strong>of</strong> death. In these 12 cases, <br />
mean concentrations (± standard deviation) <strong>of</strong> cocaine, benzoylecgonine and methylecgonine in femoral <br />
blood were 8.0 (±4.9) mg/I, 9.4 (±4.0) mg/I and 7.0 (±3.9) mg/I, respectively. In eleven <strong>of</strong> these cases, <br />
packages were found in the stomach. The other case was most probably a fatal case <strong>of</strong> cocaine delirium <br />
with a cocaine concentration in femoral blood <strong>of</strong> 0.23 mg/I, a benzoyJecgonine concentration <strong>of</strong> 7.0 mg/! <br />
and a methylecgonine concentration <strong>of</strong> 1.64 mg/1. <br />
The mean concentrations <strong>of</strong> cocaine and metabolites in femoral blood in the TCD+ category were much<br />
lower compared to the TCDcategory: the concentrations <strong>of</strong> cocaine, benzoylecgonine and methylecgonine<br />
. in these cases were 0.54 mg/I, 1.99 mg/l and 1.21 mg/I, respectively. In these cases <strong>of</strong> TCD+, combinations<br />
with ethanol, amphetamines, benzodiazepines, methadone, morphine and GHB were found.<br />
Compared to the TCD and TCD+ category, the mean concentrations <strong>of</strong> cocaine and metabolites in femoral<br />
blood in the categories ACD and NCD were much lower: the mean concentrations were 0.10 mg/I and 0.18<br />
mg/I for cocaine, 1.11 mg/I and 1.91 mg/I for benzoylecgonine and 0.25mg/l and 0.45 mg/I for<br />
methylecgonine , respectively. In the cases <strong>of</strong> anatomical cause <strong>of</strong> death (A CD), there were two cases in<br />
which cocaine was the only drug present. In the other 15 cases <strong>of</strong> ACD, combinations <strong>of</strong> cocaine with<br />
ethanol and other drugs (amphetamines, benzodiazepines, methadone and morphine) were found. Out <strong>of</strong> 8<br />
cases where no clear cause <strong>of</strong> death (NCD) was found, 7 cases had combinations <strong>of</strong> cocaine and ethanol or<br />
other drugs (benzodiazepines, methadone and morphine). There were no striking differences between the·<br />
categories TCD+; ACD and NCD in combinations <strong>of</strong> drugs found together with cocaine.<br />
In two <strong>of</strong> the total 45 cases, the cause <strong>of</strong> death could be anatomical as well as toxicological. One <strong>of</strong> these <br />
cases was a woman with packages in the stomach and one package in the trachea (mechanical obstruction): <br />
the concentrations <strong>of</strong> cocaine, benzoylecgonine and methylecgonine in femoral blood were 3 mg/I, 4.3 mg/I <br />
and4.7 mg/I respectively. The other case was a shooting; a cocaine concentration in femoral blood <strong>of</strong> 1.9 <br />
mg/I was found. <br />
Keywords: postmortem blood concentrations, cause <strong>of</strong> death, cocaine<br />
Page 368
P34<br />
DETERMINA TION OF PERMETHRIN, ETHYLBENZENE, XYLENE AND THEIR METABOLITES IN<br />
AN ACUTE INGESTION OF INSECTICIDE<br />
Justin L. Poklis* I, Jeri D. Ropero-Miller l , Diana Garside l , William KeIly2 and Ruth E. Winecker l . IOffice<br />
<strong>of</strong> the Chief Medical Examiner, 100l Brinkhous-Bullitt Building, Chapel Hill, NC 27599 U.S.A. 2Coastal<br />
Pathology Associates, PO Box 317 Western Boulevard, Jacksonville, NC 28546 U.S.A.<br />
The case history and toxicological findings <strong>of</strong> an acute ingestion <strong>of</strong> the insecticide permethrin in a 7 year<br />
old female found in bed with vomit and blood on her face are presented. Permethrin and its carriers,<br />
ethylbenzene and xylene, are all components found in the commercial product, Atroban. The concentration<br />
<strong>of</strong> permethrin was measured in the liver, aortic blood and gastric content using gas chromatography-mass<br />
spectrometry (GCIMS). Concentrations <strong>of</strong> ethylbenzene and xylene were measured in the same biological<br />
samples by headspace-gas chromatography. Blood and liver concentrations <strong>of</strong> permethrin, ethyl benzene<br />
and xylene were detected at concentrations below the lowest curve calibrator. Therefore, permethrin and<br />
ethylbenzene were reported as < 1.0 mgIL(kg), and xylene as
P35 <br />
CARBON MONOXIDE AND ETHANOL IN FIVE VICTIMS OF A FIRE FATALITY<br />
Ferrari,L.A.* ,Arado M.G. , Nardo,C.A., .Mirson,D Krbavcic,I & Garrote, LV. <br />
Laboratory <strong>of</strong> Toxicology & Legal Chemistry, Supreme Court <strong>of</strong> Justice Province, Buemos Aires, <br />
Argentina. Depart. Toxicology, University <strong>of</strong> Mor6n, Argentina <br />
Several reports have been published about carbon monoxide and ethanol in fire fatalities, but possible<br />
physiological interaction between these toxic agents is still under discussion. We report a tragic mattress<br />
fire that occurred in a small room at a prison where five young men under the influence <strong>of</strong> alcohol died.<br />
Blood specimens were obtained from heart <strong>of</strong> victims and tested for ethanol by headspace gas<br />
chromatography ( HS-GClFlO). Shimadzu GC-14, CR 4A with FlO detector, stainless steel column<br />
packed with 0.3% carbowax 1500 graphapac 60/80 and tert butanol internal standard were used. Percent<br />
<strong>of</strong> carboxihemoglobin (%COHb) was determined by microdifussion methods. Additionaly, micro<br />
quantitative determination <strong>of</strong> cyanide was determined according to the method proposed by Gelttler and<br />
Goldbaum. Comprehensive testing for drugs <strong>of</strong> abuse, psychotopic drugs and other therapeutic drugs was<br />
performed by HPTLC. The %COHb and ethanol (giL) in the five victims were: 60% and 0.54; 35 % and<br />
3.99; 55% and 0.39; 45% and 0.70, 50% and 0.81 respectively. No other components with toxic relevance<br />
were found. According to this study we concluded that there was no evidence for an ethanol protective<br />
effect against carbon monoxide poisoning.<br />
Keywords: carbon monoxide, ethanol, fire<br />
Page 370
P36 <br />
METHAMPHETAMINE IN HAIR AND INTERPRETATION OF FORENSIC FINDINGS IN A<br />
FATAL CASE<br />
Katei'ina Benmkova, Vilma Habrdova, Marie Balikova" Pl'emysl Strejc<br />
Institute <strong>of</strong> <strong>Forensic</strong> Medicine and Toxicology, 1st Medical Faculty, Charles University in Prague, 121 08<br />
Prague 2, Czech Republic, (mba\i@lfl.cunLcz)<br />
Hair analyses for drugs are considered to be a significant tool for distinguishing between recent and long<br />
term drug abuse in forensic and clinical toxicology. Chronic consumption <strong>of</strong> drugs can gradually induce<br />
certain harmful effects on the human organism and it can exacerbate some pre-existing diseases. Neither<br />
analyses for drugs in blood or urine in isolation can yield sufficient information about the history <strong>of</strong> a<br />
person and their results can not be correlated directly with the toxic effects displayed. The chronic abuse <strong>of</strong><br />
methamphetamine is known to be connected with cardiovascular diseases. During or after autopsy certain<br />
types <strong>of</strong> morphologic alterations are found in the hearts <strong>of</strong> stimulant addicts. The rapid increase <strong>of</strong><br />
blood pressure after a methamphetamine intravenous dose can be risky for addicts with arteriosclerosis.<br />
However, the anamnestic data about a deceased person may not always be available to explain the<br />
pathological findings and to clasify the cause <strong>of</strong> death correctly.<br />
The aim <strong>of</strong> this presentation is to demonstrate the usefulness <strong>of</strong> hair analyses for drugs in the context <strong>of</strong><br />
explaining the development <strong>of</strong> pathological cardiovascular alterations found after the autopsy <strong>of</strong> a case<br />
where methamphetamine consumption was involved. In this case (31 year old man) only methamhetamine<br />
and metabolites were detected with traces <strong>of</strong> ephedrine which is the precursor in illicit synthesis <strong>of</strong>Pervitin.<br />
The femoral blood level <strong>of</strong> methamphetamine was 1500 nglml. It was documented by a witness that the<br />
man died within one hour after an intravenous injection <strong>of</strong> the drug. The cause <strong>of</strong> death was<br />
established as cerebral edema due to cerebellar bleeding shortly after an intravenous<br />
dose <strong>of</strong> methamphetamine. Findings <strong>of</strong> methamphetamine in the first three 2 cm hair segments<br />
numbered from the roots were nearly equal (132 nglmg), in the fourth 2 cm segment it was approximately<br />
a half <strong>of</strong> previous values. In the remaining, distal 7 cm hair segment sample the value <strong>of</strong> methamphetamine<br />
was comparable to the first one. These results provide clear evidence that the man had been a chronic<br />
methamphetamine abuser for about more than a . year and this information can help to explain the<br />
pathology, the consequence <strong>of</strong> which could be the bleeding into the cerebellum after the last single<br />
methamphetamine dose.<br />
Keywords: forensic toxicology, amphetamines in hair, methamphetamine chronic toxicity<br />
Page 371
P37 <br />
QUANTITA TIVE APPROACH TO DRUG ALCOHOL INTERACTION BASED ON<br />
POSTMORTEM DATA<br />
A Koski*, I Ojanpera, E Vuor, Department <strong>of</strong> <strong>Forensic</strong> Medicine, University <strong>of</strong> Helsinki, FINLAND<br />
Our objective was to investigate the drug-alcohol interaction in terms <strong>of</strong> postmortem concentrations <strong>of</strong> both<br />
drugs and alcohol in fatal poisonings. As our target analytes, we chose the three drugs most commonly<br />
causing fatal single-drug poisonings in Finland: the tricyclic antidepressant amitriptyline, the opioid<br />
analgesic propoxyphene and the phenothiazine antipsychotic promazine. The effect <strong>of</strong> benzodiazepines<br />
(BDZs) on drug and alcohol concentrations was also evaluated in the study.<br />
The laboratory database was searched for fatal poisonings caused by A) amitriptyline, propoxyphene or<br />
promazine alone, B) one <strong>of</strong> these drugs with alcohol present, or C) alcohol (ethanol) with one <strong>of</strong> these<br />
drugs detected. In order to increase sample size, cases with therapeutic or subtherapeutic concentrations <strong>of</strong><br />
some <strong>of</strong> the most frequently occurring BDZs were also included, but separate statistical treatments were<br />
performed to evaluate their effect. The drug and alcohol concentrations included in the study had been<br />
measured in femoral venous blood. The final data set consisted <strong>of</strong> 116 amitriptyline cases, <strong>of</strong> which 60<br />
(S2%) BDZ positive, 120 propoxyphene cases, <strong>of</strong> which 43 (36%) BDZ positive, and 96 promazine cases,<br />
<strong>of</strong> which 42 (44%) were BDZ positive.<br />
The blood drug concentrations found in the unmixed amitriptyline poisonings were compared with those<br />
detected in the amitriptyline-alcohol cases, and likewise for propoxyphene and promazine. The blood<br />
alcohol concentrations found in the drug-alcohol poisonings were in turn compared with those in a<br />
previously compiled reference group consisting <strong>of</strong> fatal alcohol poisonings caused by alcohol alone<br />
(n=61S).<br />
The median drug concentrations in unmixed drug poisonings (BDZ+) and drug-alcohol poisonings (BDZ+)<br />
were 3.S (2.1) mg!l and 1.9 (0.7S) mg!1 for amitriptyline, 8.2 (4.9) mg/l and 6.1 (2.7) mg/I for<br />
propoxyphene, and 6.3 (7.6) mg/l and 6.7 (S.I) mg/l for promazine. Regarding the effect <strong>of</strong> BDZs, the<br />
difference between the median drug concentrations was statistically significant in amitriptyline poisonings<br />
with and without BDZs (p
P38 <br />
TREND OF ACUTE NARCOTISM DURING THE LAST TEN YEARS<br />
Nadia Fucci"', Nadia De Giovanni, Fabio De Giorgio, Marcello Chiarotti<br />
Istituto di Medicina Legale e delle Assicurazioni, Universita Cattolica del Sacro Cuore, L.go F. Vito,1 <br />
00168 Roma (Italy)<br />
Since 1993 the Laboratory <strong>of</strong> <strong>Forensic</strong> Toxicology at the Catholic University <strong>of</strong> Rome has evaluated the<br />
trends <strong>of</strong> deaths from narcotism ..We have already studied previous periods and our data were compared<br />
with D.C.S.A. (Dipartimento Centrale Servizi Antidroga - Central Antidrug Department) and GTF (Gruppo<br />
Tossicologi Forensi - Italian <strong>Forensic</strong> Toxicologist Association) informations. In this paper we present a<br />
statistical analysis <strong>of</strong> the lethal intoxications in the period 2000-2003 and compare to two prior periods<br />
(period A 1993-1996; period B 1997-1999).<br />
Annually cruel deaths observed by the Legal Medicine Institute <strong>of</strong> Catholic University range between 300<br />
to 400. About 18-22% <strong>of</strong> these cases are submitted for toxicologic analyses; less than 10% <strong>of</strong> total deaths<br />
could be referred to lethal intoxications.<br />
Analysis <strong>of</strong> data showed interesting observations relative to the last ten years:<br />
• A decreasing in overdose cases<br />
• Morphine alone is stiil the main drug accounting for death<br />
• An increase in methadone-related-deaths<br />
• A slight reduction in cases <strong>of</strong> acute cocaine intoxications<br />
A separate study on morphine and ethanol related deaths was performed; this study showed that the<br />
presence <strong>of</strong> ethanol higher than 0.5 gil was more significant when morphine concentrations ranged<br />
between 20 and 250 ng/m!.<br />
Our study suggests the usefulness <strong>of</strong> periodic review <strong>of</strong> mortality phenomena related to drug intoxications.<br />
Keywords: acute narcotism, statistical evaluation, postmortem<br />
Page 373
P39 <br />
FORMALIN-INDUCED METHAMPHETAMINE DECOMPOSITION IN HUMAN LIVER<br />
l<br />
Diaa M. Shakleya , James C. Kraner 2 , James A. Kaplan 2 , and Patrick S. Callery*l,! Dept. <strong>of</strong> Basic<br />
Pharmaceutical Sciences, West Virginia University, Morgantown, WV 26506 and 20ffice <strong>of</strong>Chief Medical<br />
Examiner, Charleston, WV, 25302.<br />
Methamphetamine is methylated in the presence <strong>of</strong> aqueous formalin mixtures within hours at room<br />
temperature. The product, N,N-dimethylamphetamine, is also found in human liver exposed to<br />
methamphetamine followed by incubation with formalin. In the present study, we determined if liver<br />
samples from confirmed methamphetamine abuse subjects would produce N,N-dimethylamphetamine upon<br />
formalin fixation. Human liver samples were obtained from four deaths that were investigated by the West<br />
Virginia Office <strong>of</strong> the Chief Medical Examiner. Full toxicological analysis was conducted on samples<br />
from the decedents and methamphetamine was among the positive findings in each case. The method used<br />
to expose the tissue to formaldehyde involved treating a small piece <strong>of</strong> liver (100-200 mg) from each case<br />
with formalin solution (20% v/v) for 24 hrs at room temperature. The formalin treated tissues were<br />
homogenized and the resulting suspension was sonicated for 5 min and then centrifuged. Supernatant<br />
aJiquots (l0 f.l.1) were added to 500 f.l.1 <strong>of</strong> 0.1 % formic acid in acetonitrile for mass spectrometric analysis on<br />
a Finnigan LCQ DECA ion trap mass spectrometer with an electrospray ionization source. Positive ion<br />
spectra recorded in MS, MS2 and MS 3 modes were used to confirm the presence <strong>of</strong> N,Ndimethylamphetamine<br />
in the mixture, as well as the absence <strong>of</strong> methamphetamine. Liver tissue not treated<br />
with formalin did not contain a detectable level <strong>of</strong> N,N-dimethylamphetamine. The results suggest that<br />
embalmed tissues may give false negative findings for methamphetamine. Detection <strong>of</strong> N,Ndimethyl<br />
amphetamine in embalmed liver is a potential surrogate indicator <strong>of</strong> methamphetamine ingestion.<br />
This project was supported by Award 2001-RC-CX-K003 through the National Institute <strong>of</strong> Justice, Office<br />
<strong>of</strong> Justice Programs. The opinions, findings, and conclusions or recommendations expressed in this<br />
publication are those <strong>of</strong>the authors and do not necessarily reflect the views <strong>of</strong> the Department <strong>of</strong>Justice.<br />
Key words: Formalin-induced, Methamphetamine, Methylation<br />
,,-",<br />
Page 374
P40<br />
FATAL METHADONE INTOXICATION IN AN INFANT<br />
Fiona J. Couper*, Kiran Chopra and Marie Lydie Y. Pierre~Louis. <br />
Office <strong>of</strong> the Chief Medical Examiner, 1910 Massachusetts Ave SE, Bldg 27, Washington, D.C. 20003. <br />
We present the case history and toxicological findings <strong>of</strong> an infant fatality involving methadone. A lO~<br />
month old infant was found unresponsive in a crib by her mother. The infant was taken to hospital;<br />
however, she was cold and stiff on arrival and was pronounced dead. Few details regarding the case history<br />
were known at the time, and the autopsy findings were unremarkable. Specimens were submitted for a full<br />
toxicological analysis, including an alcohol analysis by headspace gas chromatography with flame<br />
ionization detection; a screen for drugs <strong>of</strong> abuse and several prescription drug classes using an enzyme~<br />
linked immunosorbent assay technique (ELISA); and a screen for basic compounds using gas<br />
chromatography~mass spectrometry (GC-MS). Positive findings were confirmed and quantitated using GC<br />
MS. Methadone was detected in subclavian blood at a concentration <strong>of</strong> 0.67 mglL. This unexpected result<br />
initiated a police investigation, and it was revealed that the mother had fed methadone to her infant in the<br />
baby's formula for several months to stop the infant from crying. The mother was on a methadone<br />
maintenance program and was given take-home doses <strong>of</strong> liquid methadone. On the day <strong>of</strong> the infant's<br />
death, the mother admitted to administering twice the amount <strong>of</strong> methadone she normally gave her child.<br />
The cause <strong>of</strong> death was determined to be "methadone intoxication", and the manner <strong>of</strong> death was<br />
"homicide". A discussion <strong>of</strong> the case circumstances, the toxicology findings and methadone<br />
pharmacokinetics will be presented.<br />
Keywords: Methadone, Infant, Intoxication<br />
Page 375
P41 <br />
SURVEY OF ABUSED DRUGS IN PERIOD 1986-2003 IN WEST BOHEMIA (MIDDLE EUROPE)<br />
V. Petrov;i*, D. Petr, M. Balvin<br />
Institute <strong>of</strong> <strong>Forensic</strong> Medicine, University Hospital in Pilsen, Czech Republic<br />
West Bohemia's area is about 11 000 km 2 and has a population <strong>of</strong>850 000 people. The center <strong>of</strong> the region<br />
is Pilsen. After the fall <strong>of</strong> Communistic regime in 1989, the number and spectrum <strong>of</strong> drug abuse cases has<br />
been gradually increasing. Before 1989, abuse <strong>of</strong> volatile substances (like toluene) and opiates (especially<br />
codeine) was prevalent. After 1989, the production and abuse <strong>of</strong> methamphetamine (pervitin) has<br />
significantly increased. The amphetamine derivatives are the most frequent abused drugs in this region as<br />
well as in the whole country. The number <strong>of</strong> cases has increased seven fold in the last decade to a total <strong>of</strong><br />
620 cases .. Most <strong>of</strong> deaths connected with drug abuse and overdosage are caused by methamphetamine.<br />
Occurrence <strong>of</strong> opiates (mostly heroin) and cocaine is less common - <strong>of</strong>ten in Asiatic communities (202<br />
cases <strong>of</strong> opiates and 12 <strong>of</strong> cocaine). In the last two years, occurrence <strong>of</strong> cannabinoids has also increased;<br />
reports have doubled from 2001 to 2003 to a 388 cases. The overall increase in drug abuse has also caused<br />
an increase in drugged drivers. From statistics it follows that the most dangerous drug in traffic are<br />
cannabinoids. Four fatal road accidents caused by drivers under the influence <strong>of</strong> THC were reported in the<br />
year 2003 (three drivers and three other road users died). There was one fatal road accident caused by<br />
methamphetamine (the driver and his front passenger died) in 2003).The first and so far unique case <strong>of</strong><br />
lethal paramethoxyamphetamine (PMA) intoxication in the Czech Republic was recorded in our laboratory<br />
in 200 I. It was a 21 year old man who had a blood PMA concentration <strong>of</strong> 1.3 mg/I. Included in these cases<br />
are two veterinary surgeons (39 and 41 years) who died in connection with ketamine abuse. The first one<br />
had been abusing this substance for a long time and shot himself. The other one committed suicide with<br />
combined ketamine, succinylcholine and alcohol intoxication.<br />
Keywords: paramethoxyamphetamine, methamphetamine, cannabinoids<br />
Page 376
P42 <br />
ENANTIOMERIC ANALYSIS OF EPHEDRINES AND NOREPHEDRINES<br />
2<br />
Sheng-Meng Wang l • 2 , Russell J. Lewis' 2 , Dennis Canfield 2 , and Ray H. LiU .J. 4 , 'Central Police University,<br />
Taoyuan, Taiwan. 2Toxicology and Accident Research Laboratory, FAA Civil Aerospace Medical Institute,<br />
Oklahoma City, OK, U.S.A. JDepartment <strong>of</strong> medical technology, Fooyin University, Kaohsiung Hsieh,<br />
Taiwan. 4Department <strong>of</strong>Justice Sciences, University <strong>of</strong>Alabama at Birmingham, Birmingham, AL, U.S.A.<br />
Concerned with variations in abuse potential and control status among various isomers <strong>of</strong> ephedrines and<br />
norephedrines, this study was conducted to develop an effective method for the simultaneous analysis <strong>of</strong><br />
nine structurally related ephedrine-type compounds. Select cold medications were then analyzed to<br />
characterize the enantiomeric compositions <strong>of</strong> ephedrine, norephedrine (phenylpropanolamine or PPA),<br />
pseudoephedrine, norpseudoephedrine (cathine), and cathinone.<br />
Among various approaches investigated, a 60-m HP-5MS (0.25 mm!D, 0.25 !!m film thickness) was found<br />
to successfully resolve the following compounds <strong>of</strong> interest that were derivatized with (-)-a-methoxy-a.<br />
trifloromethy lpheny lacetic acid (MTPA): (+ )-cathine, (+ )-cathinone, (-)-cathinone, (+)-ephedrine, (-)<br />
ephedrine, (+)-PPA, (-)-PPA, (+)-pseudoephedrine, (-}-pseudoephedrine. A (-}-cathine standard was not<br />
available, but should also be resolvable using this analytical procedure. The injector temperature was set at<br />
250°C and the oven pr<strong>of</strong>ile was 160-220°C at 5°C/min, hold 1 min, 220-250°C at 25°C/min. This method<br />
was applied to the analysis <strong>of</strong> various over-the-counter cold medications and the results derived from three<br />
samples are shown in Table 1. These compounds were isolated from the cold medications utilizing a<br />
simple liquid/liquid extraction with ethyl acetate. This method has proven to be an efficient procedure for<br />
the separation and identification <strong>of</strong>various enantiomeric ephedrine and norephedrine-type compounds.<br />
Table 1. Enantiomeric composition (JlglmL) <strong>of</strong> various ephedrines and norephedrines found in various cold<br />
remedies<br />
(+)-Cathinone<br />
PPA thinone PPA Cathine (+)-Ephedrine<br />
(+) H-Ca<br />
(-) (+)-<br />
SamJ;!le<br />
H-Ephedrine<br />
(-)-PseudoeJ;!hedrine<br />
(+)-PseudoeJ;!hedrine<br />
2 1.84 0.565<br />
16 0.549 0.414 48.1<br />
19 1.35 1.19 26.8 2130 340<br />
References<br />
1. Liu J-T, Liu RH: Enantiomeric Composition <strong>of</strong> Abused Amine Drugs--Chromatographic Methods <strong>of</strong><br />
Analysis and Data Interpretation Matrices; J Biochem Biophys Methods 54:115-146; 2002.<br />
2. Iwanicki RM, Maier K, Zlotnick JA, Liu RH, Kuo T-L, Tagliaro F: Separation <strong>of</strong> Enantiomeric<br />
Ephedrine and Pseudoephedrine-High Pressure Liquid Chromatography and Capillary Electrophoresis;<br />
J <strong>Forensic</strong> Sci 44:470--474; 1999.<br />
Key Words: Ephedrine, Norephedrine, Enantiomer<br />
Page 377
P43 <br />
"ECSTASY" IN THE A.M. AND P.M. <br />
MDMA CONCENTRATIONS IN FATALITIES FOLLOWING HOSPITAL ADMISSION<br />
Simon Elliott*, Regional Laboratory for Toxicology, City Hospital, Birmingham, U.K.<br />
Over the last 15 years numerous deaths involving "Ecstasy" (MDMA) have been reported and described in<br />
the literature. With most cases, either ante-mortem (AM) or post-mortem (PM) concentration data are<br />
available. Due to the wide range <strong>of</strong> results and potential idiosyncratic nature <strong>of</strong> MDMA toxicity,<br />
interpretation <strong>of</strong> either data set is difficult. The possible influence <strong>of</strong>post-mortem redistribution may also<br />
be a factor, however it has been suggested that most amphetamine analogues are less influenced by this<br />
phenomenon than some other drugs. The aim <strong>of</strong> this study was to evaluate the concentrations <strong>of</strong> MDMA<br />
found in 5 fatalities admitted to hospital where both ante-mortem and post-mortem blood samples were<br />
available. Concentration ratios between PM and AM samples were also calculated to compare case data<br />
and evaluate redistribution.<br />
Case 1: 31 year old male admitted to hospital following suspected injection <strong>of</strong> crushed amphetamine and<br />
"Ecstasy" tablets. He developed malignant hyperpyrexia and later died. An AM serum MDMA<br />
concentration <strong>of</strong> 1.22 mgIL was measured (45 minutes prior to death) with a corresponding PM (brachial)<br />
blood concentration <strong>of</strong>2.37 mg/L. This produced a PM:AM concentration ratio <strong>of</strong> 1.9. Amphetamine and<br />
ethanol were also detected.<br />
Case 2: 30 year old male recovered from a river after a night out drinking. He was admitted to hospital but<br />
later died. 6 AM samples were analysed (between 9-20 hours prior to death). An AM plasma MDMA<br />
concentration <strong>of</strong> 0.31 mg/L was measured (9 hours before death) with a PM (trunk) blood concentration <strong>of</strong><br />
0.47 mg/L (PM:AM ratio 1.5) and PM, (arm) concentration <strong>of</strong> 0.52 mgIL (PM:AM ratio 1.7).<br />
Chlordiazepoxide and ethanol were also detected.<br />
Case 3: 26 year old male found collapsed in the street after having taken several "Ecstasy" tablets. He was<br />
admitted to hospital but later died after suffering hyperpyrexia. An AM blood MDMA concentration <strong>of</strong><br />
2.04 mg/L was measured (1 hour prior to death) with a corresponding PM (femoral) blood concentration <strong>of</strong><br />
2.25 mgIL) and PM Ougular) blood concentration <strong>of</strong> 2.99 mg/L. These produced PM:AM concentration<br />
ratios <strong>of</strong> l.l and 1.5, respectively. A trace <strong>of</strong> par aceta mol was also detected but no ethanol.<br />
Case 4: 22 year old female admitted to hospital with hyperthermia following ingestion <strong>of</strong> approximately 12<br />
"Ecstasy" tablets. An AM serum MDMA concentration <strong>of</strong> 4.33 mg/L was measured (1 day prior to death)<br />
with corresponding PM blood concentrations <strong>of</strong>7.25 mgIL (left femoral), 6.19 mgIL (right femoral), 28.39<br />
mgIL (heart) and 11.93 mgIL (vitreous humor). These produced PM:AM concentration ratios <strong>of</strong> 1.7, 1.4,<br />
6.6 and 2.8, respectively. Cocaine metabolite and ethanol were also detected.<br />
Case 5: 63 year old male found collapsed at home having allegedly ingested 4 "Ecstasy" tablets. He was<br />
taken to hospital but later died following a cardiac arrest. 3 AM samples were analysed (between 0-2 days<br />
prior to death). An AM serum MDMA concentration <strong>of</strong> 0.44 mg/L was measured (day <strong>of</strong> death) with a<br />
corresponding PM (femoral) blood concentration <strong>of</strong> 1.14 mg/L (PM:AM ratio 2.6). Cannabinoids, cocaine<br />
metabolite and ethanol were also detected.<br />
Overall, the PM blood cOncentrations were higher compared to the AM concentrations in all 5 cases<br />
(PM:AM ratio l.l to 2.0 in 4 cases). In one case, there also appeared to be a significant difference in the<br />
PM blood concentrations between anatomical sites (heart and femoral). Consequently, the data suggest that<br />
post-mortem blood MDMA concentrations may not accurately relate to the concentration either at the time<br />
<strong>of</strong>, or prior to death and calculations based on this assumption (e.g; dosage) should not be made.<br />
Keywords: Ecstasy, MDMA, redistribution.<br />
Page 378
P44 <br />
FATAL CASES DUE TO CYANIDE INTOXICATION THROUGH A LOCAL SUICIDE<br />
FOSTERING WEBSITE<br />
SK Lee l , JY Yang l , KW Kiml, SY Lee!, YS Park l , HS Chung*l, YC Y002; INational Institute <strong>of</strong> Scientific<br />
Investigation, Seoul, KOREA; 2College <strong>of</strong>Phannacy, Chungbuk National University, KOREA<br />
With the rapid development <strong>of</strong> the infonnation technology industry, new opportunities for committing<br />
suicide have appeared and become a social problem. With internet availability at most schools, companies<br />
and homes, committing suicide using the information from internet websites has been increasing. An<br />
individual opens a local suicide-fostering website that provides the infonnation for suicide, selling poisons,<br />
recruiting members who want to commit suicide and promoting them to kill themselves together. The<br />
poisons mainly introduced on the suicide websites are cyanide salt and pesticides. Two cases related to<br />
cyanide salt were reported here. One man and two women in case 1 and three men and two women in case<br />
2 were found dead in a motel on two separate occasions. Experimental grade potassium cyanide was also<br />
discovered in both cases. Identification and quantification <strong>of</strong> cyanide ion were performed by microdiffusion<br />
method after blood and gastric contents were collected at autopsy. Postmortem blood concentrations <strong>of</strong><br />
cyanide ion ranged from 53.8 to 208 flglml in case 1 and from 5.4 to 194 flg/ml in case 2. The cyanide ion<br />
concentrations in case 2 were all over 100 flg/ml except one <strong>of</strong> the victims, where the blood concentration<br />
was 5.4 flglml. Based upon the history, autopsy and toxicology findings, (1) the victims were in their teens<br />
and 20s who use the internet, (2) experimental grade KCN was used in these cases while industrial grade<br />
NaCN was used in most <strong>of</strong> the previous cases, and (3) the postmortem blood concentrations in these cases<br />
were generally much higher than previous cases in Korea (0.4-74 flg/ml) and those reported in other<br />
countries (1.1-53 flg/ml). The government should strengthen education for human dignity as well as poison<br />
control in order to protect youth prone to suicide seduction.<br />
Keywords: Cyanide, Intoxication, Internet<br />
Page 379
P45 <br />
ARSENIC IN NAPOLEON'S HAIR: IS EXTERNAL CONTAMINATION A POSSIBLE SOURCE<br />
I. Ricordel l , S. Pirnay*\ A. Marechal l , P. Chevallier, G. Meyer 3 , N. Milani, 1. Plesse l <br />
I Laboratoire de toxicologie de la Prefecture de Police, 75012 Paris, France " 2 LURE 918980rsay France' <br />
3 ' "<br />
INSTN-CEA, 91190 GifNvette, France<br />
Since the end <strong>of</strong> the 20 th century, forensic toxicology experts have extensively studied the precise cause <strong>of</strong><br />
Napoleon's death. Several toxicological studies have shown that there were significant concentrations <strong>of</strong><br />
arsenic in Napoleon's hair, leading to the suspicion that he was poisoned with arsenic. In our work, we<br />
confirmed the presence <strong>of</strong> arsenic in the hair; however, the heterogeneity <strong>of</strong> the results between laboratories<br />
and high level <strong>of</strong> arsenic found in Napoleon's hair encouraged us to question the interpretation <strong>of</strong> these<br />
results. In a previous study by non-destructive X-ray fluorescence analysis, we could determine the<br />
presence <strong>of</strong> arsenic at high concentration in Napoleon's system. Another complicating factor was that there<br />
were no clinical symptoms <strong>of</strong> arsenic intoxication as reported by witnesses at that time. In this context, our<br />
objective was to determine if an arsenic external contamination <strong>of</strong> Napoleon Bonaparte's hair may be a<br />
plausible cause (only or associated with other factors) to explain arsenic rates <strong>of</strong> Emperor hair.<br />
From aqueous solutions <strong>of</strong> arsenic, our protocol was to establish the quantity <strong>of</strong> arsenic capable <strong>of</strong><br />
penetrating the hair (cut extremity protected). For this purpose, we chose varied parameters: 1) the<br />
composition <strong>of</strong> the aqueous solutions (5 different solutions), the time <strong>of</strong> contact with the hair (from 24 h to<br />
I month), the color <strong>of</strong> the hair (blonde, brown, and black) and the ethnic origin <strong>of</strong> the hair. Arsenic<br />
concentrations were determined on the hair, before and after four washes (five minutes successively with<br />
water, acetone, water and water sonicate), and on the liquids <strong>of</strong> washing by atomic absorption spectrometry<br />
in a pyrolytic oven with Zeemann correction (GTA 110 Zeemann, Varian®).<br />
Major results show that: (a) Trivalent arsenic can penetrate and remain in the hair, (b) Washing the hair<br />
induces the decrease <strong>of</strong> the arsenic rate, but a significant quantity <strong>of</strong> arsenic is still firmly fixed after<br />
different treatments. (c) The time <strong>of</strong> immersion <strong>of</strong> the hair in a trivalent arsenic solution, does not change<br />
the quantity <strong>of</strong> arsenic fixed on the capillary between 24 hours and 1 month, whatever its ethnic origin. (d)<br />
The additives, likely used to prepare the disulfides bonds <strong>of</strong> the keratin for facilitating arsenic penetration,<br />
do not significantly modifY the qualitative and quantitative arsenic binding, whatever the additive and the<br />
ethnic origin <strong>of</strong>the hair.<br />
In conclusion, our study confirms that arsenic can penetrate the hair through an external source as other<br />
reports. Arsenic may remain at least partly fixed at high and toxic levels into the hair, even after full<br />
washes. Although arsenic intoxication <strong>of</strong> Napoleon cannot be excluded, our data suggests that external<br />
contamination from arsenic may provide an alternate explanation for the pres.ence <strong>of</strong> arsenic in the hair.<br />
Keywords: Arsenic, Napoleon, external contamination.<br />
Page 380
P46 <br />
FATAL GHB INTOXICATION FOLLOWING RECREATIONAL USE<br />
Susan Mazarr-Proo, B.U.S.* and Sarah Kerrigan, Ph.D. <br />
New Mexico Department <strong>of</strong> Health, Scientific Laboratory Division, Toxicology Bureau. PO Box 4700, <br />
Albuquerque, NM 87196-4700. <br />
Gamma-hydroxybutyrate (GHB) is encountered in biological specimens both as an endogenous<br />
neuromodulator, and as a recreational drug. Illicit GHB is currently classified as a schedule I drug in the<br />
United States due its abuse among recreational drug users. Therapeutically the drug is used for the<br />
treatment <strong>of</strong> cataplexy. Illicit doses are typically 2-4 g and the onset <strong>of</strong> action is rapid, occurring 15-30<br />
minutes following oral ingestion. Dose dependent effects include drowsiness, euphoria, dizziness,<br />
vomiting, respiratory depression, coma and death.<br />
GHB was isolated from biological samples using a simple liquid-liquid extraction. Trimethylsilyl<br />
derivatives were analyzed using gas chromatography mass spectrometry using positive chemical ionization<br />
(GCIMSIPCI). Deuterated internal standard and selective ion monitoring is used throughout. Samples were<br />
analyzed using an HP 5973 MSD equipped with a 30m DB-5 capillary column.<br />
We report a GHB fatality involving a 35 year-old male who was "partying" with friends. Subjects at the<br />
party ingested unknown quantities <strong>of</strong> wine and GHB. A female companion at the party reported seeing the<br />
male alive earlier in day before she passed out. She awoke to find the individual decedent cold and stiff.<br />
Postmortem specimens were submitted to our laboratory for comprehensive toxicology testing. No alcohol<br />
or common drugs <strong>of</strong> abuse were detected in the femoral blood. A targeted analysis revealed GHB in urine,<br />
brain, vitreous fluid, femoral blood, heart blood and liver at concentrations <strong>of</strong> 1665 mg/L, 102 mg/kg, 48<br />
mg/L, 461 mg/L, 276 mg/L and 52.2 mg/kg respectively. Concentrations <strong>of</strong> the drug in urine and vitreous<br />
fluid are extremely important in death investigations due to significant postmortem production <strong>of</strong> GHB in<br />
blood specimens. The cause <strong>of</strong> death was attributed to GHB intoxication and the manner <strong>of</strong> death was<br />
accidental.<br />
Keywords: GHB, postmortem toxicology, fatality<br />
Page 381
P47 <br />
INTERPRETATION OF POSTMORTEM ALCOHOL CONCENTRATIONS: A CASE STUDY<br />
Curtis Caylor, B.S.,* Ruth Luthi, B.S. and Sarah Kerrigan, Ph.D. <br />
New Mexico Department <strong>of</strong> Health, Scientific Laboratory Division, Toxicology Bureau, PO Box 4700, <br />
Albuquerque, NM 87196-4700. <br />
Our laboratory performs drug and alcohol testing on approximately 2800 medical examiner cases each<br />
year. The preferred specimen for alcohol analysis was blood, and until recently, additional specimens were<br />
not routinely tested unless the submitting agency requested additional analyses. A new policy required that<br />
all positive blood alcohol measurements in postmortem cases were confirmed using an alternative<br />
specimen. Although this resulted in a 43% increase in alcohol casework, these analyses provided important<br />
interpretive information and also identified a number <strong>of</strong> unusual results that would not have been otherwise<br />
identified.<br />
Postmortem blood and vitreous alcohol concentrations were determined in a total <strong>of</strong> 295 alcohol-positive<br />
cases. The vitreous alcohol concentration (V AC) exceeded the blood alcohol concentration (BAC) in 209<br />
cases (71%). Blood alcohol concentrations exceeded vitreous concentrations in 81 cases (27%) and the<br />
concentrations were equivalent in 5 cases (5%). Samples that were negative in both specimens were<br />
excluded, as were cases where the confirmatory test was performed using a specimen other than vitreous<br />
fluid (e.g. urine, liver, blood from an alternative source). In casework where the VAC>BAC, linear<br />
regression analysis indicated an R2 value <strong>of</strong> 0.958 (n=295) and a V AC approximately 18% higher than the<br />
BAC. The VACIBAC ratio was more variable at lower BACs «0.1 glIOOmL). Although VACIBAC ratios<br />
were more consistent at concentrations <strong>of</strong>0.1 gllOOmL and above, the overall ratio ranged from 1.01-2.20.<br />
Ofthe 81 cases where the BAC>VAC, a total <strong>of</strong>24 cases indicated no vitreous alcohol. The range <strong>of</strong>blood<br />
alcohol concentrations among these cases was widely variable (0.01 to 0.30 glIOOmL). All analyses were<br />
conducted using dual column gas chromatography with flame ionization detection (GC-FID) with a<br />
reporting limit <strong>of</strong>0.0 1 g/l00mL for postmortem samples.<br />
A series <strong>of</strong> case studies are used to demonstrate postmortem interpretive issues and the benefits associated<br />
with multiple specimen analysis. Cases include in-situ contamination <strong>of</strong> specimens due to trauma,<br />
postmortem production <strong>of</strong> ethanol, death during the absorptive phase among others. Actual case studies<br />
involving other volatile organic compounds are also discussed including isopropanol and acetone from<br />
endogenous and exogenous sources. These cases studies highlight the importance <strong>of</strong> analyzing multiple<br />
specimens in postmortem casework.<br />
Keywords: ethanol, postmortem, blood, vitreous fluid<br />
Page 382
P48 <br />
DETERMINATlON OF FENTANYL IN POSTMORTEM BLOOD SAMPLES BY LIQUID<br />
CHROMA TOGRAPHY TANDEM MASS SPECTROMETRY<br />
Vera Coopman l ', Dirk. Van Varenbergh 2 , Karen Pien 2 and Jan Cordonnier l <br />
lDepartment <strong>of</strong> Analytical Toxicology, Chemiphar N.V., Lieven Bauwensstraat 4, Bruges, Belgium. <br />
2Department <strong>of</strong> <strong>Forensic</strong> Medicine, Free Brussels University, Brussels, Belgium. <br />
Fentanyl is a potent synthetic narcotic analgesic administrated in the form <strong>of</strong> a transdermal patch for the<br />
management <strong>of</strong> chronic pain. The authors present a liquid-liquid extraction procedure and a liquid<br />
chromatography-tandem mass spectrometry method (LC-MS-MS) for the quantitation <strong>of</strong> fentanyl in<br />
postmortem blood samples .. The method was applied in a case <strong>of</strong> acute intoxication due to excessive<br />
administrated Durogesic® transdermal patch.<br />
To a 1.0 mL aliquot <strong>of</strong> blood sample, 50 flL <strong>of</strong> internal standard solution fentanyl-ds (1 flgJmL) and 1 mL<br />
1M K 2 C0 3 was added. Extraction was performed with 7 mL <strong>of</strong> a mixture <strong>of</strong> n-hexane:ethylacetate (7:3,<br />
VN). After vortex mixing and centrifugation, the upper organic layer was evaporated and reconstituted in<br />
1.0 mL <strong>of</strong> initial mobile phase. The LC-MS-MS analysis were performed using an Alliance® 2695 system<br />
and a Quatro Micro mass spectrometer (Waters Milford, USA). Chromatography was achieved using a<br />
Xterra® MS C18 column 2.1 mm x 100 mm with a 3.5 flm particle size (Waters Milford, USA). A gradient<br />
elution was used with 0.15% formic acid and 0.15% formic acid in acetonitrile. The chromatographic<br />
duration was 30 minutes. The flow rate was 0.20 mLimin and the column oven temperature was set at<br />
35°C. A 20 flL aliquot <strong>of</strong> the sample was injected. Multiple reaction monitoring (MRM) with positive ion<br />
dectection (ES+) was used for selective detection <strong>of</strong> fentanyl and fentanyl-ds. The precursor ion and two<br />
fragment ions were selected as quantifier and qualifier, for fentanyl mlz 336.8 and fragments at m/z 187.95<br />
and 104.4, for fentanyl-ds mlz 341.9 and fragments at m/z 188.0 and 104.5. Calibration was performed by<br />
addition <strong>of</strong> standard solutions to fentanyl-free blood prior to extraction. Precision, accuracy and recovery<br />
experiments were carried out. The liquid-liquid extraction procedure in combination with LC-MS-MS<br />
proved to be a good alternative compared with the more labor-intensive solid-phase extractions previously<br />
described.<br />
The analytical procedure was applied in a forensic case: a 78-year-old woman was found death in bed,<br />
lying on het back. The external examination revealed 10 Durogesic® transdermal patches (fentanyl 100<br />
flglh) on the abdomen. An autopsy was carried out 2 days later. Multiple samples were taken for<br />
toxicological examination. The following fentanyl concentrations were found; 28.6 flglL (right) and 28.2<br />
fJg/L (left) in subclavian blood, 21.3 fJglL (right) and 20.9 fJg/L (left) in femoral blood, 37.6 fJglL (right)<br />
and 33.9 flg/L (left) in ventricular blood. The comprehensive systematic toxicological analysis did not<br />
reveal the presence <strong>of</strong> an other substance which contributed to the death <strong>of</strong> the woman. We concluded that<br />
death was caused by intoxication with fentanyl. The manner was presumed to be suicide.<br />
Keywords: fentanyl, LC-MS-MS, fatality<br />
.~.<br />
Page 383
P49 <br />
ALFENTANIL FATAL INJECTION: A CASE REPORT<br />
V.Dumestre-Toulet* I, M. Villain 2, P. Kintz 2<br />
ILaboratoire TOXGEN - Bordeaux; 2Institut de Medecine Legale - ChemTox - Strasbourg<br />
Introduction: We report a case <strong>of</strong> fatal intoxication with alfentanil (RAPIFEN,ALFENT A ampoules <strong>of</strong><br />
1 and 5 mg), an intravenous narcotic analgesic, chemically related to fentanyl and characterized by a very<br />
rapid onset and short duration <strong>of</strong> action. Alfentanil is used as an adjunct for surgical anaesthesia under<br />
assisted ventilation in medical units.<br />
Case-report: A 46-year-old anaesthetist male nurse was found dead in the toilets <strong>of</strong> an hospital. A syringe<br />
was found near the body. He was suspected <strong>of</strong> narcotic theft and abuse because a lot <strong>of</strong> ampoules were<br />
missing since several months in the unit. Autopsy findings revealed injection marks on the left ann, an<br />
oedematous and inflammatory aspect <strong>of</strong> various organs and a bilateral pulmonary oedema. Biological<br />
samples (blood, urine and hair) were collected and sent to the laboratory for forensic toxicological analysis.<br />
Methods: Screening analyses were performed by immunoassay, gas chromatography/mass spectrometry<br />
(GC/MS) and liquid chromatography/diode array detection (LCIDAD) using standardized methods <strong>of</strong> our<br />
laboratory. GC/flame ionisation detector with headspace injection (HS) was used to detennine blood<br />
alcohol concentration. Alfentanil and fentanyl were screened with GCIMS and quantification was<br />
performed with GC/MS/MS after liquid-liquid extraction with chlor<strong>of</strong>onn/2-propanol/heptane (33:17:50,<br />
v/v/v) and phosphate buffer (Iml, pH 9.5). Fentanyl d S was used as internal standard.<br />
Results: Alfentanil was identified in blood and urine at 45.1 and 2.7 nglml, respectively. Blood alcohol<br />
concentration was measured at 1.32 gil. Hair analysis revealed chronic use <strong>of</strong> alfentanil (2 pglmg) and<br />
fentanyl (8 pg/mg). No other drugs were detected.<br />
Adult surgical patients who received a bolus dose <strong>of</strong> 8 to 50 jlg/kg alfentanil by intravenous infusion<br />
developed plasma concentrations <strong>of</strong> 200 to 1000 nglml. Alfentanil is capable <strong>of</strong> producing severe<br />
respiratory depression with hypotension and coma during surgical operations even with assisted ventilation<br />
and plasmatic concentrations above 100 - 200 ng/ml (1). Whereas fentanyl is reported as a commonly<br />
abused substance by healthcare pr<strong>of</strong>essionals (2), alfentanil misuse and abuse seems exceptional (3).<br />
Conclusion: Although the measured concentrations are therapeutic, alfentanil injection without assisted<br />
ventilation may be the cause <strong>of</strong> the death. Hair analysis demonstrated chronic abuse <strong>of</strong> alfentanil and<br />
fentanyl by the anesthetist nurse.<br />
References:<br />
(1) Mahla ME, White SE, Moneta MD. Delayed respiratory depression after alfentanil. Anesthesiology<br />
1988 ; 69: 527-534<br />
(2) Villain M, Cirimele V, Ludes B, Kintz P. Toxicomanie d'un anesthesiste au fentanyl: la preuve<br />
fonnelle par analyse des cheveux en utilisant la CPG/SM/SM. Ann. Toxicol. Anal. 2001; 13 (1): 49<br />
53,<br />
(3) Kintz P, Villain M, Cirimele V, Ludes B. Conduites addictives en milieu hospitalier : particularites<br />
d'un service d'anesthesie. Ann. Toxicol. Anal. 2002; 14(1): 83- 89<br />
Keywords: alfentanil, chronic abuse, hair, GC/MSIMS.<br />
Page 384
P50 <br />
THE DETERMINATION OF ETHANOL ORIGIN IN FATAL AVIATION ACCIDENT VICTIMS:<br />
A MULTI-CASE STUDY<br />
Johnson, R.D.*!, Lewis, RJ. 1 , and Blank, C.L <br />
'Civil Aerospace Medical Institute, AAM-61O, CAM I Building, RM 205, 6500 S. Macarthur Blvd, <br />
Oklahoma City, OK 73169-6901 USA; 2The University <strong>of</strong> Oklahoma, Department <strong>of</strong> Chemistry and <br />
Biochemistry; 620 Parrington Oval, Rm 208, 1';/orman, OK 73019 <br />
Specimens from aviation accident victims are submitted to the FAA's Civil Aerospace Medical Institute<br />
(CAMI) for toxicological analysis. During toxicological evaluations, ethanol analysis is performed on each<br />
such case. Care must be taken when interpreting a positive ethanol result due to the potential for<br />
postmortem ethanol formation. Historically, ethanol distribution in various tissues and fluids from the same<br />
case and/or the presence <strong>of</strong> other volatile organic compounds (VOCs) at abnormal concentrations in these<br />
fluids and tissues has been employed as an indicator <strong>of</strong> postmortem microbial ethanol formation. However,<br />
these methods are not always reliable. The consumption <strong>of</strong> ethanol has been shown to alter the<br />
concentration <strong>of</strong> two major serotonin metabolites, 5-hydroxytryptophol (5-HTOL) and 5-hydroxyindole-3<br />
acetic acid (5-HIAA). While the 5-HTOLl5-HIAA ratio is normally low, previous studies have<br />
demonstrated that the urinary 5-HTOLl5-HIAA ratio is significantly elevated following ethanol ingestion.<br />
The S-HTOLl5-HIAA ratio is not affected by the microbial formation <strong>of</strong> ethanol, by consumption <strong>of</strong><br />
serotonin~rich foods or by the use <strong>of</strong> SSRl's.<br />
Recently, our laboratory has developed a single analytical approach to determine concentrations <strong>of</strong> both 5<br />
HTOL and 5-HIAA that has provided a convenient, rapid and reliable solution to this problem. This novel<br />
methodology eliminates the need for two separate and unrelated analytical techniques, GCIMS and LCIEC,<br />
for the determination <strong>of</strong> these metabolites. The simultaneous determination <strong>of</strong> 5-HTOL and 5-HIAA in<br />
forensic urine specimens was achieved using a liquid/liquid extraction technique in conjunction with<br />
LCIMS. The ion trap MS used allowed us to perform MSIMS/MS on both 5-HTOL and 5-HIAA, and<br />
afforded limits <strong>of</strong> quantitation below 1 ng/mL for each compound. After development <strong>of</strong> this method, the<br />
previously established, antemortem, 15 pmol/nmol 5-HTOLl5-HIAA ratio cut<strong>of</strong>f was investigated and<br />
subsequently validated for use with forensic specimens.<br />
Utilizing this newly validated method, we examined the 5-HTOLIS-HIAA ratio in urine specimens<br />
obtained from six separate fatal aviation accidents where ethanol was present, but its source was unclear. In<br />
one <strong>of</strong> these cases antemortem consumption <strong>of</strong> ethanol was indicated, even though microbial production<br />
was initially considered. After examining the 5-HTOLl5-HIAA ratio from the other five cases investigated<br />
we determined that recent ethanol consumption had not occurred. The ethanol present in these cases was<br />
due to microbial formation, and not consumption. This presentation will discuss, in depth, the difficulties in<br />
determining the source <strong>of</strong> ethanol in these six cases and the application <strong>of</strong> this novel methodology in<br />
elucidating its origin.<br />
Keywords: Postmortem Ethanol, LC/MS, Serotonin metabolites<br />
Page 385
PSt<br />
UNUSUAL TRAMADOL CONCENTRATIONS IN AN ACCIDENTAL DEATH INVOLVING<br />
POLY DRUG USE<br />
Ginger Baker, M.S., * Janice Yazzie, B.S., and Sarah Kerrigan, Ph.D. <br />
New Mexico Department <strong>of</strong> Health, Scientific Laboratory Division, Toxicology Bureau, PO Box 4700, <br />
Albuquerque, NM 87196·4700 <br />
Tramadol is a synthetic opioid-receptor agonist that is used clinically as an analgesic in daily doses <strong>of</strong> 100<br />
to 400 mg. Therapeutic concentrations in blood are reported in the range 0.1 to 0.8 mg/L. Overdoses <strong>of</strong> 500<br />
mg and higher may cause agitation, hypertension, tachycardia and seizures whereas doses greater than 800<br />
mg may result in coma and respiratory depression. We report a case involving unusually high postmortem<br />
tramadol (Ultram) concentrations in a 35 year-old male with a past medical history <strong>of</strong> bipolar illness,<br />
anxiety, depression and substance abuse.<br />
Tramadol concentrations were determined using solid phase extraction (Polychrom Clin II) and gas<br />
chromatography/mass spectrometry (GCIMS) using full scan analysis with mepivicaine as the internal<br />
standard. An R2 value in the linear range (0.2 4.0 mglL) was 1.000 for tramadol. The Intraassay CV<br />
was 6.4 % using laboratory fortified independent spikes.<br />
Initial toxicology findings <strong>of</strong> illicit drugs in femoral blood identified cocaine and benzoylecogonine at<br />
concentrations <strong>of</strong> 0.04 mg/L and 0.91 mg/L, respectively. Therapeutic prescription medications found in<br />
femoral blood included paroxetine, trazadone, tramadoland the active metabolite, O·desmethyltramadol.<br />
Quantitative analysis <strong>of</strong>tramadol revealed extraordinarily high concentrations <strong>of</strong> the parent drug. Tramadol<br />
concentrations in femoral blood, heart blood and vitreous fluid were 74 mg/L, 83 mg/L and 18 mg/L,<br />
respectively. O-desmethyltramadol concentrations in femoral blood, heart blood and vitreous fluid were 4<br />
mg/L,5mg/L and Img/L, respectively. Issues that need to be considered when interpreting toxicological<br />
findings associated with multiple drug use will be discussed.<br />
Keywords: tramadol, overdose, postmortem<br />
Page 386
P52 <br />
PEDIATRIC FATALITY DUE TO HYDROXYCHLOROQUINE INGESTION<br />
H. Nipper*, P. Studts, R. Baltaro, Creighton University Medical Center, Omaha, NE, 68131<br />
A 7 year-old African-American female was found at home unresponsive and cold approximately 4 hr after<br />
being given acetaminophen and sent to bed to rest after complaining <strong>of</strong> stomach ache and headache.<br />
At autopsy, findings were unremarkable for clues as to cause <strong>of</strong> death. Heart blood and vitreous humor<br />
were sent to Creighton University Medical Center for forensic testing. Initially, serum and vitreous humor<br />
electrolytes, hemoglobin electrophoresis were ordered, but all results were within expected limits. The<br />
acetaminophen level was 57.6 ~g/mL.<br />
Further testing was performed using gas chromatography with FIDINPD on an alkaline extract <strong>of</strong> blood.<br />
The presence <strong>of</strong> an unfamiliar peak was noted and the Douglas County (Nebraska) Coroner was alerted to<br />
return to the home with investigators to perform a full inventory <strong>of</strong> pharmaceuticals. The inventory<br />
included numerous arthritis medications including one identified as "hydroxychlor." The parents<br />
determined with investigators present that eleven 200 mg tablets (2.2g total drug) were unaccounted for<br />
from the bottle that they thought was stored safely.<br />
Simultaneously the laboratory was identifYing the unknown GC peak as hydroxychoroquine using GCIMS<br />
with a dosage form from the hospital pharmacy as a standard.<br />
Quantitation <strong>of</strong> the blood level <strong>of</strong> hydroxy chloroquine performed at National Medical Services revealed 70<br />
IJ.g1mL. (NMS therapeutic range: 0.1-1.0 IJ.g1mL) The cause <strong>of</strong> death was subsequently ruled to be acute<br />
overdose <strong>of</strong> hydroxy chloroquine. The manner <strong>of</strong> death was ruled to be accidental.<br />
According to the PDR (1) "Children are especially sensitive to the 4-aminoquinoline compounds. A<br />
number <strong>of</strong> fatalities have been reported following the accidental ingestion <strong>of</strong> chloroquine, sometimes from<br />
relatively small doses (0.75-1.0 g in one three-year-old child). Parents should be strongly warned to keep<br />
these drugs out <strong>of</strong> reach <strong>of</strong> children." Early symptoms <strong>of</strong> overdose are headache and drowsiness, and may<br />
occur within 30 minutes <strong>of</strong> ingestion. These symptoms may be followed by cardiovascular collapse, and<br />
"sudden and early respiratory and cardiac arrest". (1)<br />
1. Physicians Desk Reference (PDR), 58 th ed., (<strong>2004</strong>) p. 3031, Thomson PDR, Montvale, NJ 07645.<br />
Keywords: Pediatric, Postmortem toxicology, Hydroxychloroquine, Fatality<br />
Page 387
P53 <br />
LORAZEPAM AND DEATH INVESTIGATION<br />
Jayne E. Clarkson'·, Ann Marie Gordon', Barry K. Logan' <br />
IWashington State Toxicology Laboratory, <strong>Forensic</strong> Laboratory Services Bureau, Washington State Patrol, <br />
2203 Airport Way South, Seattle, WA 98134. <br />
The objective <strong>of</strong> this study was to evaluate the role <strong>of</strong> lorazepam (Ativan®), a benzodiazepine frequently<br />
used to manage anxiety and to sedate, in death investigations. Lorazepam has been detected with<br />
increasing frequency in death investigation cases in Washington State. A review <strong>of</strong> the literature revealed<br />
there is currently limited data on the significance <strong>of</strong> lorazepam in death investigation cases.<br />
We reviewed death investigation cases which were positive for lorazepam at the Washington State<br />
Toxicology Laboratory between January 1998 and December 2003. The mean drug concentration found in<br />
the blood <strong>of</strong> these decedents (n=112) was 0.15 mg/L (S.D. 0.39, median <strong>of</strong> 0.03 mg/L). Concentrations<br />
ranged from
P54 <br />
SERTRALINE WITHDRAWAL IN A NEWBORN - COULD THIS BE A FACTOR IN THE CAUSE OF<br />
DEATH<br />
Laureen J. Marinetti* and Russell L.Uptegrove. <br />
Montgomery County Coroner's Office (MCCO), 361 West Third Street, Dayton, OH 45402 <br />
A 4·day-old infant was found not breathing by her mother at about 6am. The infant was wrapped in a blanket <br />
and lying on her back on a large sectional couch near her sleeping father. The mother confirmed that the infant's <br />
face and head were several inches from her husband and were not obstructed in any way. The infant was <br />
transported to the emergency room where a heart rhythm was established and she was placed on a ventilator. <br />
The infant was later found to be brain dead and was removed from the ventilator. She was pronounced dead <br />
approximately 12 hours after the mother had first found her. <br />
The mother received regular pre-natal care and was diagnosed with gestational diabetes. As a result she had bi<br />
weekly testing for the last several weeks <strong>of</strong> her pregnancy. In addition she also experienced sleeplessness and <br />
had been prescribed sertraline, which she took as prescribed. The birth was induced and was an uneventful <br />
delivery reSUlting in a 71b, 60z infant. The infant was fed formula (similac) and was not breast-fed at any time. <br />
The infant was released from the hospital 2 days after she was born. Approximately 24 hours after birth the <br />
infant became irritable, screaming and crying after every feeding. The last two nights prior to her death she was <br />
awake all night in this highly irritable state. <br />
Significant findings at the time <strong>of</strong> autopsy included epicardial hemorrhage on the anterior surface <strong>of</strong> the heart, <br />
(consistent with cardiopulmonary resuscitative efforts), and pulmonary and liver congestion. <br />
The toxicology laboratory at MCCO received the following specimens; hospital blood (3 mL), heart blood (16 <br />
mL), cerebral spinal fluid (CSF), gastric, liver, vitreous fluid, bile and head hair. Analysis <strong>of</strong> the heart blood <br />
revealed the presence <strong>of</strong> 16 nglmL sertraline and 113 nglmL norsertraline, the hospital blood revealed 71 ng/mL <br />
norsertraline and analysis <strong>of</strong> the liver revealed 230 nglg sertraline and 4000 ng/g norsertraline. Sertraline was <br />
detected in the hospital blood but the small amount <strong>of</strong> specimen received precluded its accurate measurement. <br />
Sertraline and norsertraline quantitation was accomplished using high performance liquid chromatography <br />
(HPLC) with a CI8 column and ultra violet detection with confirmation by gas chromatography/mass <br />
spectrometry (GC/MS). <br />
A review <strong>of</strong> the literature reveals neonatal complications when selective serotonin re-uptake inhibitors (SSRl's) <br />
are used by the mother near term. Paroxetine, sertraline, fluvoxamine and fluoxetine have been associated with <br />
withdrawal symptoms in the neonate. The withdrawal symptoms are diverse but most commonly include; <br />
respiratory distress, hypoglycemia, jaundice (Costei et al. 2003) and irritability, constant crying, shivering, <br />
increased tonus, eating and sleeping difficulties and convulsions, (Nordeng et at. 2001). The symptoms usually <br />
occur after 2 days and last for an average <strong>of</strong> 10 days to one month (Salvia-Roiges et aL 2003). While the SSRI's <br />
have not been associated with teratogenic risks, it is clear that the potential for withdrawal exists - especially if <br />
the mother does not breast-feed the infant. Hendrick et at. 2003 determined cord blood concentrations <strong>of</strong> <br />
sertraline and norsertraline in II newborn babies whose mothers were prescribed the drug. The ranges were as <br />
follows, sertraline; less than I up to 14 nglmL and norsertraline; less than I up to 72 nglmL. None <strong>of</strong> these babies <br />
experienced withdrawal symptoms but it is unknown ifthey were breast-fed. <br />
Based on the clinical history <strong>of</strong> the infant's feeding and sleeping difficulties, irritability and crying, and the fact <br />
that the infant was being fed formula instead <strong>of</strong> being breast fed, it is possible that the infant was undergoing <br />
withdrawal from sertraline which it was exposed to in utero. A search <strong>of</strong> the medical literature revealed no <br />
reported cases <strong>of</strong> an infant's death due to exposure to or withdrawal from sertraline but some infants exposed to <br />
SSRI's in utero required treatment for the withdrawal symptoms. The cause and manner <strong>of</strong> death was listed as <br />
undetermined. In conclusion not enough information is known to conclude that SSRl's are safe to administer to <br />
a pregnant woman, especially in the third trimester. <br />
Key Words: Sertraline, Neonate, Withdrawal <br />
Page 389
P55 <br />
QUETIAPINE CONCENTRATIONS IN INTENTIONAL AND ACCIDENTAL DRUG<br />
INGESTIONS<br />
Martha J. Burt* and Diane M. Boland<br />
Miami-Dade County Medical Examiner Department<br />
Quetiapine (Seroquel) was introduced in 1993 as a neuroleptic agent in the treatment <strong>of</strong> psychosis. It has<br />
high affinity for serotoninergic receptor sites and less affinity for dopaminergic, adrenergic and histamine<br />
receptors. Since introduction, very few cases have been reported on the potential mortality <strong>of</strong> quetiapine<br />
overdose, alone or in combination with other drugs. We present our case series <strong>of</strong> single drug and mixed<br />
drug quetiapine overdoses from the Miami-Dade County Medical Examiner Department. The case records<br />
from the years 1998 to 2003 inclusive were searched for those cases where quetiapine was detected and<br />
quantitated in postmortem blood, gastric contents, or liver. A total <strong>of</strong> 17 cases were identified; three were<br />
excluded because no quetiapine was detected during the quantitation process, and one was excluded<br />
because a complete autopsy was not performed. Thus, 13 cases are reported in this series. The ages ranged<br />
from 28 to 55 years, with a mean age <strong>of</strong> 44 years. These cases were grouped into four categories: those<br />
where the quetiapine was the sole cause <strong>of</strong> death (Q only), those where quetiapine was related to the cause<br />
<strong>of</strong> death (QR), those where the quetiapine was unrelated to the cause <strong>of</strong> death (QUR) and those where it<br />
was unclear if quetiapine played any role in the cause <strong>of</strong> death (UNK). Two deaths were a result <strong>of</strong> solely<br />
quetiapine ingestions (Q only cases). One was a 35 year old white male with central blood, gastric and<br />
liver concentrations <strong>of</strong> 25 mgIL, 8370 mg total, and 36 mg/kg, respectively. The other was a 48 year old<br />
white female with blood, gastric and liver concentrations <strong>of</strong> 9.5 mgIL, 954 mg total, and 34 mg/kg,<br />
respectively. Two deaths in our series resulted from polydrug ingestions, where more than one agent,<br />
including quetiapine could have resulted in death (QR group). The blood quetiapine concentrations were<br />
15.6 mgIL and 13.6 mgIL, and both had significant concentrations <strong>of</strong> at least one benzodiazepine, in<br />
addition to other agents. Four cases fell into the unknown group (UNK), where it was unclear ifquetiapine<br />
contributed to the cause <strong>of</strong> death. In these cases, the mean quetiapine concentration was 1.86 mgIL, with a<br />
range <strong>of</strong> 0.34 - 2.8 mgIL. All four had other drugs detected, such as benzodiazepines, alcohol and/or<br />
cocaine. The last group, those where quetiapine clearly played no role in the cause <strong>of</strong> death, consisted <strong>of</strong> 5<br />
cases, with a mean quetiapine concentration <strong>of</strong> 0.88 mg/L and a range <strong>of</strong> 0.27 - 1.6 mg/L. This report<br />
provides evidence that quetiapine alone can result in death, and may significantly contribute to mortality in<br />
poly drug ingestions. Also, this data may assist medical examiners and toxicologists in separating lethal<br />
from non-lethal quetiapine concentrations in a variety <strong>of</strong> circumstances.<br />
Keywords: Quetiapine, postmortem toxicology, overdose<br />
Page 390
P56<br />
POSTMORTEM QUETIAPINE: THERAPEUTIC OR TOXIC CONCENTRATIONS<br />
Dawn R. Parker* and lain M. McIntyre. San Diego County Medical Examiner's Office, 5555 Overland<br />
Avenue, Bldg. # 14, San Diego, CA 92123.<br />
Currently, very little literature data are available on postmortem blood concentrations <strong>of</strong> quetiapine. A<br />
study was performed to establish relative guidelines for the delineation <strong>of</strong> therapeutic and potentially toxic<br />
concentrations. This study was conducted in medical examiner cases in which quetiapine was detected<br />
with routine screening methods.<br />
Quetiapine Fumarate (SEROQUEL®) is a dibenzothiazepine derivative (2-(2-(4-dibenzo [bj)<br />
[1 ,4]thiazepin-ll-yl-l-piperazinyl)ethoxy ]-ethanol fumarate) used in the treatment <strong>of</strong> psychosis. Fourteen<br />
fatalities in which quetiapine was detected were selected for investigation.<br />
Following liquid-liquid basic extraction, high performance liquid chromatography was used to analyze<br />
blood (peripheral and central), vitreous humor, and liver. The cases were organized into two groups: "nondrug<br />
related" fatalities and "drug related" fatalities.<br />
A total <strong>of</strong> eight "non-drug related" fatality cases were examined. Peripheral blood concentrations ranged<br />
from: 0.26 to 0.76 mg/L (mean +1- standard deviation 0.38 +1- 0.17 mg/L); central blood concentrations:<br />
0.23 to 0.73 mg/L (0.46 +1- 0.21 mg/L); vitreous humor concentrations: 0.08 to 0.32 mg/L (0.16 +/- 0.08<br />
mg/L); and liver concentrations:
PS7 <br />
CAFFEINE INTOXICA nON: MORE THAN JUST CREAM AND SUGAR<br />
Sarah Kerrigan* and Tania Lindsey. <br />
New Mexico Department <strong>of</strong> Health, Scientific Laboratory Division, Toxicology Bureau. PO Box 4700, <br />
Albuquerque, NM 87196-4700, <br />
Caffeine is a mild central nervous stimulant that occurs naturally in c<strong>of</strong>fee beans, cocoa beans and tea<br />
leaves. In large doses, it can be pr<strong>of</strong>oundly toxic, resulting in arrhythmia, tachycardia, vomiting,<br />
convulsions, coma and death, The average cup <strong>of</strong> c<strong>of</strong>fee or tea in the United States is reported to contain<br />
between 40 and 100 mg caffeine, Over-the-counter supplements that are used to combat fatigue typically<br />
contain 100 mg caffeine per tablet and doses <strong>of</strong> 32-200 mg are included in a variety <strong>of</strong> prescription drug<br />
mixtures.<br />
Caffeine was quantitatively determined in five cups <strong>of</strong> c<strong>of</strong>fee purchased from local retail outlets. The total<br />
amount <strong>of</strong> caffeine per 160z (473mL) cup ranged from 211-342 mg, Fatal caffeine overdoses in adults are<br />
relatively rare and require the ingestion <strong>of</strong> a large quantity <strong>of</strong> the drug, typically in excess <strong>of</strong> 5g, Over a<br />
period <strong>of</strong> approximately 12 months our <strong>of</strong>fice reported two cases <strong>of</strong> fatal caffeine intoxication. The first<br />
fatality may have occurred due to misidentification <strong>of</strong> the drug, and the second occurred after misuse <strong>of</strong> a<br />
dietary supplement.<br />
Case #1 involved a 39 year-old female with a past history if intravenous drug use. She was found<br />
unresponsive outside a restaurant. A syringe was found near the body. Blood samples were negative for<br />
ethanol and common drugs <strong>of</strong> abuse. Comprehensive toxicology analysis using gas chromatography mass<br />
spectrometry (GC/MS) revealed a caffeine concentration <strong>of</strong> 192 mgIL in femoral blood. The cause <strong>of</strong> death<br />
was ruled as caffeine intoxication and the manner was accidental.<br />
Case #2 involved a 29 year-old male with a history <strong>of</strong> obesity and diabetes who was admitted to the<br />
hospital with vomiting and seizures. Resuscitation efforts were unsuccessful. The family reported that he<br />
had taken a dietary supplement the day before. Toxicology results indicated a caffeine concentration <strong>of</strong> 567<br />
mglL in the femoral blood. The cause <strong>of</strong> death was ruled as caffeine intoxication and the manner was<br />
accidental.<br />
Keywords: Caffeine, Intoxication, GCMS<br />
Page 392
P58 <br />
LOW DOSE ACETAMINOPHEN DEATHS<br />
Olaf H. Drummer*, Victorian Institute <strong>of</strong> <strong>Forensic</strong> Medicine, Department <strong>of</strong> <strong>Forensic</strong> Medicine, Monash<br />
University, 57-83 Kavanagh St, Southbank 3006 AUSTRALIA, e-mail olaflal,yifin.org<br />
Acetaminophen (paracetamol) is a commonly used over the counter analgesic. It is well known that use <strong>of</strong><br />
excessive doses can lead to the development <strong>of</strong> liver toxicity. This is mediated through the formation <strong>of</strong>the<br />
toxic metabolite N-acetyl benzoquinone imine. In adults single doses required to initiate liver necrosis is<br />
believed to start from 6 to 10 grams, which is about 12 to 20 500-mg tablets. Typically blood<br />
concentrations are well over 200 mgIL. This presentation describes acetaminophen toxicity in three women<br />
following doses within therapeutic guidelines.<br />
Case 1. The deceased was a 28 year old female <strong>of</strong> age with a history <strong>of</strong> an eating disorder, depression and<br />
alcoholism. While in hospital for an unrelated condition she became drowsy, weak, ataxic, and had slurred<br />
speech. She died some hours later. She had received about ten tablets over the previous 3-4 days. Her<br />
maximum acetaminophen concentration was 38 mgIL.<br />
Case 2. The deceased was a 21-year-old healthy woman. She developed a laceration after falling on glass.<br />
Three days later she presented to hospital with severe headache associated with vomiting and mild<br />
photophobia. A few days later she was weak, was vomiting and had a high heart rate. She was diagnosed<br />
with hepatic encephalopathy and her acetaminophen concentration was 46 mglL. She had taken about 10<br />
acetaminophen tablets over a few days. Other causes <strong>of</strong> liver necrosis were excluded by exhaustive<br />
toxicology, serology and virology testing.<br />
Case 3. This 45-year old woman had undergone surgery for an obstructed bowel. A few days later she was<br />
confused and agitated. This worsened until her death on day six. The day previously she had been<br />
diagnosed with liver failure. Her maximum acetaminophen concentration was 46 mgIL. She had been<br />
given one gram acetaminophen two to three times daily for several days prior to her death.<br />
All cases showed typical liver necrosis at post-mortem and had clinical changes consistent with<br />
acetaminophen toxicity. None <strong>of</strong> the cases had circumstances suggesting recent abuse <strong>of</strong> acetaminophen.<br />
The low acetaminophen concentration and absence <strong>of</strong> other causes <strong>of</strong> liver necrosis suggests that some<br />
persons may be sensitive to this drug, perhaps because <strong>of</strong> low glutathione concentrations due to diet or<br />
genetic factors and/or were genetically predisposed to the development <strong>of</strong> the toxic metabolite. A full<br />
account <strong>of</strong>the toxicology and post-mortem findings will be presented.<br />
Keywords: acetaminophen, low-dose, toxicity, post-mortem<br />
Page 393
P59 <br />
INTERPRETING ANTIHISTAMINE LEVELS IN POST~MORTEM BLOOD; ESTABLISHING<br />
INCIDENTAL AND CONTRIBUTORY RANGES FOR EVALUATION PURPOSES<br />
Michelle Sandberg *, Dan Anderson, and Kristina Fritz<br />
Los Angeles County Department <strong>of</strong>Coroner, Los Angeles, CA<br />
Over the last ten years, the Food and Drug Administration has approved numerous prescription<br />
antihistamines safe for over~the~counter (OTC) distribution. Antihistamines are a broad class <strong>of</strong> drugs,<br />
frequently taken to <strong>of</strong>fer symptomatic relief from colds, sinus congestion, allergies, and are also a class <strong>of</strong><br />
drugs frequently abused.<br />
In forensic toxicology, post~mortem (PM) redistribution <strong>of</strong> drugs complicates the interpretation <strong>of</strong> results.<br />
Many <strong>of</strong> the reference materials available are for clinical interpretation, and extrapolating PM levels for<br />
comparison to clinical values is not ideal. The substantial volume <strong>of</strong> casework at the Los Angeles County<br />
Department <strong>of</strong> Coroner (LACDOC) Laboratory provided us the ability to establish applicable PM blood<br />
level ranges for interpretation <strong>of</strong>the first generation antihistamines by a query <strong>of</strong> the LACDOC toxicology<br />
database over a three-year period. First generation antihistamines are easily detected using a basic liquidliquid<br />
extraction with an acidic back extraction. Diphenhydramine, chlorpheniramine, doxylamine,<br />
promethazine, and hydroxyzine are commonly detected at the LACDOC by GCINPD.<br />
A brief summary <strong>of</strong>the query results and interpretation are as follows:<br />
Categories<br />
Published<br />
Clinical<br />
Therapeutic <br />
Drug Levels <br />
Post Mortem Central Blood Levels, mgIL<br />
Diphenhydramine Doxylamine Promethazine Hydroxyzine Chlorpheniramine<br />
(471 cases) (87 cases) (136 cases) (44 cases) (126 cases)<br />
-0.11 -0.10 -0.08 -0.02<br />
- 0.14<br />
Determined<br />
om 0.70 0.01- 0.70 0.01- 0.30 0.01 0.50 om 0.30<br />
"Incidental"<br />
81% (383) 84% (73) 74% (101) 73% (32) 96% (I21)<br />
Drug Levels<br />
0.31 - 0.0.90 0.51-1.1<br />
Determined<br />
16% (21) 18% (8)<br />
"contributory" >0.70 > 0.70<br />
>0.30<br />
and<br />
and<br />
. to the cause <strong>of</strong> 17% (80) 15% (1) 4%(5)<br />
>0.90 >1.1<br />
death<br />
10%(14) 9%(4) <br />
Determined as <br />
the > 19 > l32 <br />
"sole cause 2%(8) 1%(1) -- -- --<br />
<strong>of</strong> death" <br />
The query results were categorized as follows:<br />
• Incidental - Levels that represent over 70% <strong>of</strong> the quantitated cases for a particular drug, and<br />
correspond to therapeutic dosing<br />
• Contributory - Levels that were greater than therapeutic and could not be ruled out as a<br />
contributing cause <strong>of</strong>death<br />
• Sole Cause <strong>of</strong>Death - Due to the drug alone, not influenced by any other drug<br />
This study determined PM therapeutic central blood levels for five, first-generation antihistamines and<br />
central blood values that indicated the drug was a contributing factor in the cause <strong>of</strong> death. The Los<br />
Angeles County Coroner Laboratory continues to evaluate the cases where levels are greater than the<br />
"contributing" category and may have been the sole cause <strong>of</strong>death, ifother weren't drugs present.<br />
Keywords: Antihistamines, Interpretation, Post-mortem blood levels<br />
Page 394
P60 <br />
PHARMACOGENOMICS AS MOLECULAR AUTOPSY: GENOTYPING P450 2D6, 2C9 AND<br />
2Cl9 USING PYROSEQUENCING FOR METHADONE CASES<br />
B. Charles Schur 2, Elvan Laleli-Sahin 1.2, Steven H. Wong 1.2, Susan B. Gock 1.2, Paul J. Jannetto I, Jeffrey<br />
M. Jentzen 1.2 <br />
IMilwauke County Medical Examiners Office; 2Department Of Pathology, Medical College Of Wi, <br />
Milwaukee, Wi, U.S.A. <br />
Pharmacogenomics, the study <strong>of</strong> the impact <strong>of</strong> heritable traits on pharmacology and toxicology, has the<br />
potential to explain the relationship between drug administration, drug metabolism and adverse drug<br />
reactions. Genetically, single nucleotide polymorph isms (SNP's) are single base-pair changes in the DNA<br />
sequence <strong>of</strong> a gene. Base deletions or substitutions may result in a change in the amino acid sequence <strong>of</strong><br />
the polypeptide. These heritable mutations have the ability to change the structure and specificity <strong>of</strong> the<br />
enzyme to the extent that it may not metabolize the drug in question. Depending on the variant alleles<br />
present, an individuals' metabolic rate may be phenotypically described as poor (PM), intermediate (1M),<br />
extensive (EM, normal), or ultra-extensive (rapid). PM's have a high risk <strong>of</strong> adverse effects which can<br />
potentially be fatal, while 1M's have a metabolic rate between PM's and EM's.<br />
In <strong>Forensic</strong> Pathologyrroxicology, molecular techniques can determine the genotype <strong>of</strong> a decedent and<br />
may aide in the determination <strong>of</strong> the cause and manner <strong>of</strong> drug related deaths. Methadone, for example, is<br />
metabolized in the liver by cytochrome P450 (CYP) lA2, 3A4. 2D6 and, to a certain extent, 2C9 and 2CJ9<br />
enzymes. All <strong>of</strong> the genes encoding these enzymes are polymorphic. In this study we establish the<br />
technical feasibility <strong>of</strong> genotyping for known mutations in CYP2D6 (*3, *4, *5, *6, *7 and *8) as well as<br />
CYP2C9 (*2, *3) and CYP2C19 (*2, *3, *4) using Pyrosequencing.<br />
Twelve frozen, archived, blood samples from the Milwaukee County Medical Examiners Office<br />
(MCMEO), were selected as part <strong>of</strong> a multi-center retrospective analysis <strong>of</strong> cases from June 2002 to<br />
December 2002, which was approved by Medical College <strong>of</strong> Wisconsin IRE. These cases listed<br />
methadone as a contributing factor in the cause <strong>of</strong> death. After DNA extraction, PCR was performed and<br />
amplified product was then interrogated for the presence <strong>of</strong> specific SNP's using a Pyrosequencing<br />
PSQ96MA. Briefly, a sequencing primer is hybridized to a single stranded PCR product, and incubated<br />
with enzymes, DNA polymerase, ATP sulfurylase, luciferase, apyrase, adenosine 5' phosphosulfate (APS)<br />
and luciferin. A deoxynucleotide triphosphate (dNTP) is added to the reaction. If incorporated, a release<br />
<strong>of</strong> pyrophosphate occurs that is equimolar to the number <strong>of</strong> incorporated nucleotides. ATP sulfurylase<br />
quantitatively converts PPi to ATP in the presence <strong>of</strong> adenosine 5' phosphosulfate. This ATP converts<br />
luciferin to oxiuciferin and generates visible light detectable by a CCD camera and evident by a peak in<br />
the Pyrogram M. Each light signal is proportional to the number <strong>of</strong> nucleotides incorporated. Apyrase<br />
degrades the unincorporated dNTP's and excess A TP prior to the addition <strong>of</strong> another dNTP. S<strong>of</strong>tware<br />
correlates each Pyrogram to a reference sequence and genotype determinations are made. This platform<br />
has been previously validated for clinical samples, with results showing ] 00% concordance with other<br />
platforms including conventional PCR with RFLP analysis, direct sequencing using an ABI 3100, and<br />
rapid-cycle PCR with fluorescent melting curve analysis using a Roche LightCycier.<br />
Genotyping results for CYP2D6 indicated 8 cases (66.6%) <strong>of</strong> EM's, 3 cases (25%) <strong>of</strong> 1M's and ] case<br />
(8.3%) <strong>of</strong> a PM. For CYP2C19 SNP's, 8 samples (66.7%) were found to be EM's and 4 samples (33.3%)<br />
were found to be 1M's. No mutations (0%) were detected for CYP2C9 in any sample. These percentages<br />
are comparable to the expected prevalence ranges found in the general population. In this preliminary<br />
study, we demonstrate the feasibility <strong>of</strong> genotyping forensic samples for multiple SNP's associated with<br />
methadone metabolism. These protocols will be used in a large (n > 2000) multi-centers methadone study.<br />
Keywords: Pharmacogenomics, Methadone, Pyrosequencing<br />
Page 395
P61 <br />
A MULTI-CENTER STUDY OF PHARMACOGENOMICS AS AN ADJUNCT OF MOLECULAR<br />
AUTOPSY FOR METHADONE DEATH CERTIFICATION - PRELIMINARY FINDINGS OF<br />
DATA ACQUISITION AND MULTIPLEX GENOTYPING CYP 450 2D6, 2C9 AND 2C19 BY<br />
PYROSEQUENCING<br />
Steve Wong*, Susan Gock, and Jeffrey Jentzen, Milwaukee Medical Examiner Office, 933 Highland Ave.,<br />
Milwaukee, WI 53226 and the <strong>Forensic</strong> Pathologyrroxicology Pharmacogenomics Methadone Study<br />
Group (FPTPMSG<br />
Methadone is used in the treatment <strong>of</strong> heroin addiction and as an analgesic for pain management. Recently,<br />
there has been an increased incidence <strong>of</strong> methadone intoxication due to abuse and diversion. One <strong>of</strong> the<br />
contributing factors to drug therapy and toxicity is genetic variation. With the Human Genome Project near<br />
completion, genomic medicine based on genetic pr<strong>of</strong>iles has been proposed for personalized medicine for<br />
drug treatment and other therapeutic approaches. As an extension <strong>of</strong> genomics medicine in forensic<br />
science, a previous study examined the potential contribution <strong>of</strong> genetic variations in methadone death (J<br />
For Sci. 2003;48:1406-15). The allelic frequency <strong>of</strong> wild-type, defined for that study as non- CYP 2D6 *3,<br />
*4 and *5, was 71.4%, lower than that <strong>of</strong> living controls 82.7%. Due to the limited number <strong>of</strong> cases (n<br />
=21), the study was not adequately powered with sufficient cases to reach statistical significance. Studies<br />
for oxycodone and antidepressants also yielded a similar lower prevalence. Further, there is increasing<br />
understanding <strong>of</strong> methadone metabolism, readily characterized as mUlti-pathways with mUlti-enzymes<br />
(CYP 3A4, 2C9, 2C19, and 2D6). Some <strong>of</strong> the genes encoding these enzymes are polymorphic. Hence, a<br />
multi-center study was designed to enroll an adequate number <strong>of</strong> methadone cases to evaluate the potential<br />
contribution <strong>of</strong> genetic variation to methadone/related deaths Pharmacogenomics as an aspect <strong>of</strong><br />
Molecular Autopsy. The study was initiated with several planning sessions to consider all the key covariables<br />
and risk factors. In the fall <strong>of</strong> 2003, the following medical examiner/coroner <strong>of</strong>fices and personnel<br />
formed the <strong>Forensic</strong> Pathologyrroxicology Pharmacogenomics Methadone Study Group (FPTPMSG):<br />
Milwaukee - Wong, Jentzen, Gock, Jannetto, Schur, Sahin, Frolov, Rogalska. Cleveland/Cuyahoga<br />
Jenkins, Balraj, DetroitlWayne Hepler, Isenschmid, Schmidt, MiamilDade - Hearn, Uhlin-Hansen, New<br />
Hampshire - Wagner, Andrew, New Mexico - Kerrigan, North Carolina - Winecker, Ropera-MiIler, San<br />
Diego - McIntyre, San Francisco - Karch, Lemos, British Columbia/Canada- Langman, Washington, DC<br />
Couper, and Washington Logan, Gordon. In addition, drug-drug interaction interpretations will be<br />
performed by Moody (Univ. Utah) and secondary case reviews by Jortani (Univ. Louisville). The study<br />
period is 2002 and 2003, with some <strong>of</strong>fices providing samples before and after for trending studies. The<br />
Medical College <strong>of</strong> Wisconsin (MCW) approved an " Umbrella IRB", with subsequent endorsement by the<br />
participating <strong>of</strong>fices. Inclusion criteria are: cases certified with methadone toxicity, methadone related and<br />
methadone present. For the latter cases, each <strong>of</strong>fice would seek informed consent by decedent's family.<br />
Whole blood samples were mailed to the MeW Pharmacogenomics Lab for multiplex genotyping for CYP<br />
2D6 *3, *4, *5, *6, *7, *8., 2C9 *2 and *3., and 2C19*2,*3 and *4 by pyrosequencing (Clin Chern.<br />
2003;49:A] 2). By using a combination <strong>of</strong> Micros<strong>of</strong>t ACCESS and Excel database programs, case history<br />
and toxicology results were entered, followed by statistical analysis <strong>of</strong> transformed Excel data. At this<br />
preliminary stage, the study demonstrated the feasibility <strong>of</strong> coordinated planning and initial data entry and<br />
transfer to the MCW via Internet by 5 centers. The projected total caseload for FPTPMSG is more than<br />
1900. For a limited number <strong>of</strong> samples (n=22), the following variants were identified in 14 samples: 1<br />
homozygous for CYP 2D6*4, and the number for heterozygous variants 2 for 2D6*4 and 2C19*2., 1 for<br />
2D6*31*4., 2 for 2C9*2, 1 for 2C9*3, 4 for 2C19*2, Ifor 2D6*3, and 2 for 2D6*5. These preliminary<br />
results indicate that the multi-center study is proceeding on schedule, albeit with the expected degree <strong>of</strong><br />
logistic and technical difficulty.<br />
Key words: methadone, pharmacogenomics, death<br />
Page 396
P62 <br />
2,4-DINITROPHENOL (DNP): AN UNUSUAL FATALITY<br />
lain M. Mclntyre*, Ray D. Gary, James L. Sherrard, Dawn R. Parker, Julio Estrada and<br />
Robert E. Whitmore<br />
San Diego County Medical Examiners Office, 5555 Overland Ave., Bldg. 14, San Diego, CA 92123<br />
The decedent was a single 28-year-old male college student who resided with a roommate. His roommate<br />
found the decedent, with a fever, in a tub <strong>of</strong> ice. The roommate transported him to a local fire department,<br />
from where he was then transported to a local hospital. The decedent was conscious upon admission, but<br />
was soon pronounced dead despite resuscitative efforts. The decedent's roommate informed hospital staff<br />
that the decedent had been taking bodybuilding supplements. Bottles <strong>of</strong> medications and other materials<br />
found at the scene were brought to the Medical Examiner's Office. These included steroids, ephedrine,<br />
thyroid hormones, a yellow powder and a syringe.<br />
Autopsy showed a young muscular jaundiced Caucasian male with left ventricular hypertrophy <strong>of</strong> 1.6 cm,<br />
multiorgan congestion, and severe pulmonary edema. The liver was <strong>of</strong> a s<strong>of</strong>t mottled purple and brown<br />
appearance. There was 150 mL <strong>of</strong> blood in the stomach, signs <strong>of</strong> hemorrhagic gastritis, and evidence <strong>of</strong><br />
CPR (fractured sternum and anterior rib fractures). Autopsy also showed severe cerebral edema with uncal<br />
herniation and other evidence <strong>of</strong> medical therapy. Microscopically, the liver showed severe sinusoidal<br />
congestion and subtle centrilobular hepatocyte necrosis. No other significant macroscopic or microscopic<br />
findings were noted.<br />
Routine toxicological screens (alcohols, drugs <strong>of</strong> abuse, basic drugs, acidic drugs) were conducted on the<br />
antemortem specimens obtained from the admission. The only therapeutic drugs detected were<br />
diphenhydramine (0.13 mgIL) and lidocaine «0.05 mg/L). Specific analyses for steroids (postmortem<br />
urine) and ephedrine (antemortem blood) were negative. Analysis <strong>of</strong> the yellow powder by gas<br />
chromatography/mass spectrometry identified the powder as 2,4-dinitrophenol (DNP). Subsequent analysis<br />
<strong>of</strong> the postmortem urine (Toxi-Lab, confirmed by gas chromatography/mass spectrometry), then detected<br />
the presence <strong>of</strong> DNP. The acid drug screen (HPLe) also detected an unknown compound in the<br />
antemortem blood that was later identified as DNP. DNP was then quantitated by HPLC in the antemortem<br />
blood and in the following postmortem specimens: blood (peripheral), serum (peripheral), liver, urine, bile<br />
and gastric contents.<br />
DNP is primarily used commercially in the production <strong>of</strong> dyes, wood preservatives, photographic<br />
developers, explosives and pesticides. In the 1930's DNP was used extensively as a diet pill. DNP<br />
effectively increases the basal metabolic rate by inhibiting the synthesis <strong>of</strong> A TP in the mitochondria. This<br />
action also results in increased sweating, breathing rate, heart rate, weight loss and a marked increase in<br />
body temperature. In 1938 the U.S. Food and Drug Administration banned the use <strong>of</strong> DNP due to its<br />
harmful effects, which included cataracts, liver damage, and in some cases death.<br />
This is the first report <strong>of</strong> a fatality associated solely with DNP that describes the detection <strong>of</strong>the compound<br />
in antemortem blood and postmortem tissue concentration distribution.<br />
Keywords: 2,4-Dinitrophenol, postmortem, fatality<br />
Page 397
P63 <br />
GHB CONCENTRATIONS IN A V ARlETY OF ALCOHOLIC AND NONALCOHOLIC<br />
BEVERAGES AND LIQUID FOOD PRODUCTS<br />
Ines B. Collison"', Kristin Houg, Debra Eck, Robin Kott. <strong>Forensic</strong> Science Services, Orange County<br />
Sheriff/Coroner Department, 320 North Flower St. Santa Ana CA 92703<br />
Casework indicated the presence <strong>of</strong> small amounts <strong>of</strong> GHB in samples <strong>of</strong> Cabemet Sauvignon and Steel<br />
Reserve beer, which according to previous reports could be expected, at least in wine. Due to these results a<br />
variety <strong>of</strong> samples <strong>of</strong> different alcoholic, nonalcoholic beverages, and fermented liquid food products were<br />
analyzed for the presence <strong>of</strong> GHB following the method previously described by Couper and Logan* using<br />
smaller volumes <strong>of</strong> sample (100-200 mcL). The limit <strong>of</strong> detection was 0.25 mgIL. A total <strong>of</strong> 108 samples<br />
were tested in duplicate.<br />
A number <strong>of</strong> the samples analyzed were positive for GHB although at very low concentrations. In general,<br />
the concentration <strong>of</strong>GHB was higher in red wines (2.00-23.00mglL; n=l1) than in white wines (0.65-9.53<br />
mglL; n=l3). Of all the different kinds <strong>of</strong> vinegar tested (n=5) only white vinegar was negative for GHB<br />
while rice wine, red wine, balsamic and apple cider vinegar were positive (0.83-11.25 mgIL). The GHB<br />
concentration in beer «025-2.10 mgIL; n=29) was lower than it was in wine. For the different kinds and<br />
brands <strong>of</strong> beer tested, there appears to be a correlation between the GHB concentration and the ethanol<br />
content rather than with the type <strong>of</strong> beer analyzed. Although the sample size was small (n=3), the home<br />
brewed beers which typically have a higher alcoholic content also had the higher GHB concentration (1.71<br />
2.1 0 mg/L). The GHB concentration was either not detected or < 0.50 mgIL in the distilled alcohol samples<br />
tested (n=23). The GHB concentration in the liqueurs tested varied from not detected to 4.20 mgIL (n=II).<br />
A variety <strong>of</strong> other non distilled alcoholic drinks, such as sherry, vermouth, and champagne, showed<br />
intermediate concentrations <strong>of</strong> GHB (1.88-6.68 mglL; n=5). Neither <strong>of</strong> the two malt beverages contained<br />
GHB above our cut<strong>of</strong>f. GHB was detected in grape juice (n=2) but not in apple juice. GHB was in noni<br />
juice (Morinda citrifolia, (0.73 mglL)·, but not in the tea from the noni leaves. NoGHB was detected in the<br />
teriyaki sauce tested (n=I). Thethree different kinds <strong>of</strong> soy sauce tested were positive for GHB (2.79-18.10<br />
mglL).<br />
We conclude that although some <strong>of</strong> these products contain GHB,. a minimum <strong>of</strong> 210 L <strong>of</strong> these liquids<br />
would need to be consumed in order to ingest a 5 g dose <strong>of</strong> GHB.<br />
Couper and Logan *(2000) JAnalTox 24: 1-7<br />
Key Words: GHB, alcoholic beverages, food products.<br />
Page 398
P64 <br />
THE USE OF CLUSTER ANALYSIS TO ESTABLISH A REFERENCE RANGE FOR BETA<br />
HYDROXYBUTYRATE CONCENTRATIONS IN POSTMORTEM BLOOD AND ITS<br />
APPLICATION TO THE INVESTIGATION OF SUDDEN UNEXPECTED DEATH IN PROBLEM<br />
DRINKERS<br />
A Robert W Forrest* & Daniel Cooper. <strong>Forensic</strong> Pathology Unit, University <strong>of</strong> Sheffield, Medico-legal<br />
Centre, Watery Street, Sheffield S3 7ES, UK<br />
Alcoholic ketoacidosis is a relatively common cause <strong>of</strong> death in problem drinkers. (l) It should be<br />
considered in every case <strong>of</strong> sudden unexpected death in a problem drinker, particularly if hepatic steatosis<br />
(a fatty liver) is present and "routine" toxicology screening is unrevealing. An important clue may be a<br />
trace <strong>of</strong> acetone apparent on the ethanol assay chromatogram in association with a low or zero alcohol<br />
concentration. If the toxicologist or pathologist have any degree <strong>of</strong> suspicion that the death might be<br />
associated with alcoholic ketoacidosis, then beta-hydroxybutyrate should be measured in post mortem<br />
blood.<br />
Whilst the diagnosis <strong>of</strong> alcoholic ketoacidosis is straightforward when the beta-hydroxy butyrate<br />
concentration is grossly elevated in post mortem blood, the interpretation <strong>of</strong> the borderline result may be<br />
difficult. In life, clinical laboratories typically quote the upper limit <strong>of</strong> normal for the fasting plasma betahydroxybutyrate<br />
concentration as from 300 to 600 micromoles per litre. Unfortunately, whilst in principle it<br />
should be a simple matter to establish a reference range for the beta-hydroxy butyrate concentration in postmortem<br />
blood, in practice, for those working in England and Wales, this is fraught with difficulty. Most<br />
post-mortem examinations are non-consensual, carried out under the direction <strong>of</strong> the coroner. In the<br />
analysis <strong>of</strong> samples collected during such post-mortems, it is only permitted to carry out analyses directed<br />
at establishing who the deceased was and where and when he came to his death without the specific<br />
permission <strong>of</strong> the coroner and the relatives <strong>of</strong> the deceased. Whilst a "black letter" interpretation <strong>of</strong> the<br />
present law is arguably more liberal, those who have retained specimens obtained at a coroner's postmortem<br />
for research or teaching have been subject to considerable public criticism in the UK. (2). The<br />
practicalities <strong>of</strong> obtaining permission from the relatives <strong>of</strong> the deceased who is about to be subject to a<br />
coronial post mortem examination are daunting. If legislation currently before the UK Parliament becomes<br />
law in its present form, then the researcher who analyses a post mortem blood sample without permission<br />
will be liable to prosecution with a possible penalty <strong>of</strong> up to 3 years in prison on conviction. (3)<br />
Consequently it is necessary to make the best possible use <strong>of</strong> the data obtained when investigating any<br />
particular case to inform the interpretation <strong>of</strong> future cases. One approach that we have found useful is to use<br />
cluster analysis <strong>of</strong> all <strong>of</strong> the data we have obtained in the investigation <strong>of</strong> possible cases <strong>of</strong>alcoholic ketosis<br />
to delineate normal, equivocal and elevated beta-hydroxybutyrate concentrations in post-mortem blood. We<br />
further believe that the technique may be <strong>of</strong> more general application in the analysis <strong>of</strong> post-mortem<br />
toxicology data. To illustrate the technique we present the analysis <strong>of</strong> our data in relation to the<br />
investigation <strong>of</strong> alcoholic ketoacidosis and, more briefly, possible overdoses <strong>of</strong> diphenhydramine and<br />
tramadol.<br />
References:<br />
I. Pounder DJ, Stevenson RJ, Taylor KK. Alcoholic ketoacidosis at autopsy. Journal <strong>of</strong> <strong>Forensic</strong><br />
Sciences 1998;43(4):812-6.<br />
2. Metters J. Isaacs Report. London; 2003. http://www.publications.doh.gov.uklcmolisaacsreport/<br />
3. Human Tissue Bill.<br />
2003/4.http://www.publications.parliament.uklpalcm200304/cmbills/049!<strong>2004</strong>049.htm<br />
Keywords: alcoholic ketoacidosis, beta-hydroxy butyrate, cluster analysis<br />
Page 399
P65<br />
POSTMORTEM BLOOD ALCOHOL RELIABILITY: FEMORAL SAMPLING<br />
A.E. Hodda*, <strong>Forensic</strong> Toxicology, DALIICPMR, Lidcombe, Australia<br />
P. Ellis, Dept. <strong>Forensic</strong> Medicine, ICPMR, Westrnead, Australia<br />
The analysis <strong>of</strong> blood for alcohol is one <strong>of</strong> the more fundamental analysis undertaken by a forensic <br />
toxicology laboratory. The sources <strong>of</strong> error in the laboratory are well documented and international <br />
standards <strong>of</strong> laboratory practice (AS/ISO 17025) have been developed to safeguard the analytical <br />
processes, for any analysis. Discrepancies in the alcohol levels in post mortem specimens from a recent <br />
. vehicle accident death resulted in a detailed review <strong>of</strong> all aspects <strong>of</strong> the post mortem process. In this case <br />
two femoral blood samples gave alcohol levels <strong>of</strong> 0.3 IOg/IOOmL but a vitreous humor sample had no <br />
detectable alcohol.<br />
A number <strong>of</strong> papers have been published on the importance <strong>of</strong> the source <strong>of</strong> blood samples used in<br />
quantitative alcohol and drug analysis. Errors due to contamination, dilution and "post mortem<br />
redistribution" are cited. The conclusion is that peripheral samples should be used and best source is the<br />
femoral vessels. The recommended procedure for post mortem femoral blood sampling is reviewed. The<br />
sampling point is normally within the pelvic girdle and it is clear that poor adherence to correct procedures<br />
can result in adventitious contamination or a non-representative blood sample. Traumatic deaths present the<br />
greatest risk <strong>of</strong> contamination. The Laboratory receives approximately 3000 toxicology cases per year and<br />
a review <strong>of</strong> 2 years showed the median volume <strong>of</strong> preserved blood submitted from coronial cases was<br />
20mL.<br />
Mathematical modelling demonstrated that 200j.IL (4 drops) <strong>of</strong> an alcoholic spirit in the pelvic cavity could<br />
result in blood alcohol levels <strong>of</strong> 0.300g/l OOmL, if allowed to contaminate a 20mL blood sample. Several<br />
tables are presented <strong>of</strong> various collected blood volumes and potential contamination factors.<br />
The reliability and predictability <strong>of</strong> comparing blood and vitreous humor alcohol .levels was also tested. A<br />
set <strong>of</strong>33 blood alcohol levels greater than 0.200g/100mL were compared to their respective vitreous humor<br />
alcohol levels. The regression equation was y=1.2734x-O.0451, the R2 was 0.9488. This result was similar<br />
to other reports and demonstrated the value <strong>of</strong> this comparison as well as the improbable results for the<br />
reviewed case.<br />
The review did not categorically identify the source <strong>of</strong> error in this case but the work has highlighted the<br />
ease <strong>of</strong> introducing significant errors in blood alcohol analysis. It has also supported the strong correlation<br />
between blood alcohol and vitreous humor. This observation makes this specimen particularly useful in<br />
contentious toxicology cases and should be taken in matters involving severe trauma. The growing<br />
convention in forensic toxicology is to use femoral blood samples for quantitative analysis, is endorsed but<br />
correct sampling procedures must be followed by pathologists.<br />
Keywords: Blood alcohol, error, femoral, vitreous humor.<br />
Page 400