2010 SAGES Final Program
2010 SAGES Final Program
2010 SAGES Final Program
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
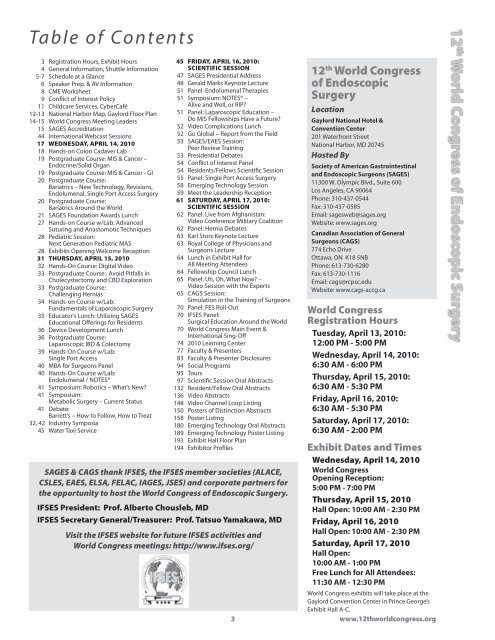
Table of Contents<br />
3 Registration Hours, Exhibit Hours<br />
4 General Information, Shuttle Information<br />
5-7 Schedule at a Glance<br />
6 Speaker Prep. & AV Information<br />
8 CME Worksheet<br />
9 Conflict of Interest Policy<br />
11 Childcare Services, CyberCafé<br />
12-13 National Harbor Map, Gaylord Floor Plan<br />
14-15 World Congress Meeting Leaders<br />
15 <strong>SAGES</strong> Accreditation<br />
44 International Webcast Sessions<br />
17 Wednesday, April 14, <strong>2010</strong><br />
18 Hands-on Colon Cadaver Lab<br />
19 Postgraduate Course: MIS & Cancer –<br />
Endocrine/Solid Organ<br />
19 Postgraduate Course: MIS & Cancer - GI<br />
20 Postgraduate Course:<br />
Bariatrics – New Technology, Revisions,<br />
Endolumenal, Single Port Access Surgery<br />
20 Postgraduate Course:<br />
Bariatrics Around the World<br />
21 <strong>SAGES</strong> Foundation Awards Lunch<br />
27 Hands-on Course w/Lab: Advanced<br />
Suturing and Anastomotic Techniques<br />
28 Pediatric Session:<br />
Next Generation Pediatric MAS<br />
28 Exhibits Opening Welcome Reception<br />
31 Thursday, April 15, <strong>2010</strong><br />
32 Hands-On Course: Digital Video<br />
33 Postgraduate Course: Avoid Pitfalls in<br />
Cholecystectomy and CBD Exploration<br />
33 Postgraduate Course:<br />
Challenging Hernias<br />
34 Hands-on Course w/Lab:<br />
Fundamentals of Laparoscopic Surgery<br />
35 Educator’s Lunch: Utilizing <strong>SAGES</strong><br />
Educational Offerings for Residents<br />
36 Device Development Lunch<br />
36 Postgraduate Course:<br />
Laparoscopic IBD & Colectomy<br />
39 Hands-On Course w/Lab:<br />
Single Port Access<br />
40 MBA for Surgeons Panel<br />
40 Hands-On Course w/Lab:<br />
Endolumenal / NOTES®<br />
41 Symposium: Robotics – What’s New?<br />
41 Symposium:<br />
Metabolic Surgery – Current Status<br />
41 Debate:<br />
Barrett’s – How to Follow, How to Treat<br />
32, 42 Industry Symposia<br />
45 Water Taxi Service<br />
45 Friday, April 16, <strong>2010</strong>:<br />
Scientific Session<br />
47 <strong>SAGES</strong> Presidential Address<br />
48 Gerald Marks Keynote Lecture<br />
51 Panel: Endolumenal Therapies<br />
51 Symposium: NOTES® –<br />
Alive and Well, or RIP?<br />
51 Panel: Laparoscopic Education –<br />
Do MIS Fellowships Have a Future?<br />
52 Video Complications Lunch<br />
52 Go Global – Report from the Field<br />
53 <strong>SAGES</strong>/EAES Session:<br />
Peer Review Training<br />
53 Presidential Debates<br />
54 Conflict of Interest Panel<br />
54 Residents/Fellows Scientific Session<br />
55 Panel: Single Port Access Surgery<br />
58 Emerging Technology Session<br />
59 Meet the Leadership Reception<br />
61 Saturday, April 17, <strong>2010</strong>:<br />
Scientific Session<br />
62 Panel: Live from Afghanistan:<br />
Video Conference Military Coalition<br />
62 Panel: Hernia Debates<br />
63 Karl Storz Keynote Lecture<br />
63 Royal College of Physicians and<br />
Surgeons Lecture<br />
64 Lunch in Exhibit Hall for<br />
All Meeting Attendees<br />
64 Fellowship Council Lunch<br />
65 Panel: Uh, Oh, What Now? –<br />
Video Session with the Experts<br />
65 CAGS Session:<br />
Simulation in the Training of Surgeons<br />
70 Panel: FES Roll-Out<br />
70 IFSES Panel:<br />
Surgical Education Around the World<br />
70 World Congress Main Event &<br />
International Sing-Off<br />
74 <strong>2010</strong> Learning Center<br />
77 Faculty & Presenters<br />
83 Faculty & Presenter Disclosures<br />
94 Social <strong>Program</strong>s<br />
95 Tours<br />
97 Scientific Session Oral Abstracts<br />
132 Resident/Fellow Oral Abstracts<br />
136 Video Abstracts<br />
148 Video Channel Loop Listing<br />
150 Posters of Distinction Abstracts<br />
158 Poster Listing<br />
180 Emerging Technology Oral Abstracts<br />
189 Emerging Technology Poster Listing<br />
193 Exhibit Hall Floor Plan<br />
194 Exhibitor Profiles<br />
<strong>SAGES</strong> & CAGS thank IFSES, the IFSES member societies (ALACE,<br />
CSLES, EAES, ELSA, FELAC, IAGES, JSES) and corporate partners for<br />
the opportunity to host the World Congress of Endoscopic Surgery.<br />
IFSES President: Prof. Alberto Chousleb, MD<br />
IFSES Secretary General/Treasurer: Prof. Tatsuo Yamakawa, MD<br />
Visit the IFSES website for future IFSES activities and<br />
World Congress meetings: http://www.ifses.org/<br />
12 th World Congress<br />
of Endoscopic<br />
Surgery<br />
Location<br />
Gaylord National Hotel &<br />
Convention Center<br />
201 Waterfront Street<br />
National Harbor, MD 20745<br />
Hosted By<br />
Society of American Gastrointestinal<br />
and Endoscopic Surgeons (<strong>SAGES</strong>)<br />
11300 W. Olympic Blvd., Suite 600<br />
Los Angeles, CA 90064<br />
Phone: 310-437-0544<br />
Fax: 310-437-0585<br />
Email: sagesweb@sages.org<br />
Website: www.sages.org<br />
Canadian Association of General<br />
Surgeons (CAGS)<br />
774 Echo Drive<br />
Ottawa, ON K18 5NB<br />
Phone: 613-730-6280<br />
Fax: 613-730-1116<br />
Email: cags@rcpsc.edu<br />
Website: www.cags-accg.ca<br />
World Congress<br />
Registration Hours<br />
Tuesday, April 13, <strong>2010</strong>:<br />
12:00 PM - 5:00 PM<br />
Wednesday, April 14, <strong>2010</strong>:<br />
6:30 AM - 6:00 PM<br />
Thursday, April 15, <strong>2010</strong>:<br />
6:30 AM - 5:30 PM<br />
Friday, April 16, <strong>2010</strong>:<br />
6:30 AM - 5:30 PM<br />
Saturday, April 17, <strong>2010</strong>:<br />
6:30 AM - 2:00 PM<br />
Exhibit Dates and Times<br />
Wednesday, April 14, <strong>2010</strong><br />
World Congress<br />
Opening Reception:<br />
5:00 PM - 7:00 PM<br />
Thursday, April 15, <strong>2010</strong><br />
Hall Open: 10:00 AM - 2:30 PM<br />
Friday, April 16, <strong>2010</strong><br />
Hall Open: 10:00 AM - 2:30 PM<br />
Saturday, April 17, <strong>2010</strong><br />
Hall Open:<br />
10:00 AM - 1:00 PM<br />
Free Lunch for All Attendees:<br />
11:30 AM - 12:30 PM<br />
World Congress exhibits will take place at the<br />
Gaylord Convention Center in Prince George’s<br />
Exhibit Hall A-C.<br />
3 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
General Information<br />
Leadership for the<br />
<strong>2010</strong> World Congress<br />
World Congress <strong>Program</strong> Chairs:<br />
Daniel M. Herron, M.D.<br />
(<strong>SAGES</strong> Co-Chair)<br />
Barry A. Salky, M.D. (<strong>SAGES</strong> Chair)<br />
Christopher M. Schlachta, M.D.<br />
(CAGS Chair)<br />
World Congress Presidents:<br />
Gerald M. Fried, M.D. (CAGS)<br />
David W. Rattner, M.D. (<strong>SAGES</strong>)<br />
<strong>SAGES</strong> President: C. Daniel Smith, M.D.<br />
CAGS President: Chris Jamieson, M.D.<br />
IFSES President: Alberto Chousleb, M.D.<br />
D.C. Shuttle Service From Gaylord National<br />
World Congress Corporate Supporters<br />
Diamond Donors<br />
COVIDIEN<br />
ETHICON ENDO-SURGERY, INC.<br />
<strong>SAGES</strong> EDUCATION AND RESEARCH FOUNDATION<br />
PLATINUM DONORS<br />
KARL STORZ ENDOSCOPY-AMERICA<br />
OLYMPUS<br />
GOLD DONORS<br />
ASCENT HEALTHCARE SOLUTIONS<br />
STRYKER ENDOSCOPY<br />
SILVER DONORS<br />
BOSTON SCIENTIFIC DAVOL INC., A BARD COMPANY GORE & ASSOCIATES<br />
BRONZE Donors<br />
SYNOVIS SURGICAL INNOVATIONS<br />
Visit the Transportation Desk (Lobby Level) or Call 301-839-5261<br />
Hours of Operation: 8:00am - 10:00pm (major credit cards accepted)<br />
Shuttle management will make every effort to maintain the<br />
schedule but may experience delays due to traffic conditions<br />
beyond our control especially during peak business hours.<br />
Subject to availability. Dates, times, and prices subject to change.<br />
Additional restrictions may apply.<br />
Roundabout Tour and Shuttle<br />
Visit more than a dozen stops in and around the region and jump on<br />
and off as you please! OnBoard Tours’ Roundabout is the best way to<br />
see the Capital Region – and at the best value! 3-Day Unlimited Passes<br />
Start at Just $35 Per Person!<br />
Sightseeing Tours and<br />
Roundabout Services<br />
Choose from the area’s most exciting tours, including “The DC It All<br />
Tour,” “DC the Lights” (the only downtown night tour), and more!<br />
Downtown D.C. Shuttle Service<br />
Featuring continuous service to:<br />
– Old Post Office (1100 Pennsylvania Avenue NW)<br />
– Union Station (H. Street and 2nd Street NE)<br />
Departing every hour, on the hour, from Gaylord National’s main<br />
entrance<br />
Seven days a week: 8:00 a.m. - 9:00 p.m.<br />
One-way tickets: $13<br />
Round-trip tickets: $20<br />
Unlimited, 3-Day Pass: $49<br />
King Street Metrorail Station and Old<br />
Town Alexandria Shuttle Service<br />
Enjoy Metrorail’s unparalleled accessibility to the area (including<br />
the museums and monuments of the National Mall) or the dining,<br />
shopping, and entertainment of Old Town’s historic waterfront<br />
community. Metrorail fare-cards may also be purchased at the<br />
Gaylord National Transportation Desk.<br />
One-way tickets are $5 per person, with continuous service to:<br />
– King Street Metrorail Station (Yellow and Blue lines)<br />
– Old Town Alexandria (King Street and Route 1)<br />
Departing every 30 minutes* from Gaylord National’s main entrance<br />
Sunday - Thursday: 6:30am - 9:00pm<br />
Friday - Saturday: 6:30am - 10:00pm<br />
Water Taxis to Old Town,<br />
Georgetown, and Mount Vernon<br />
Potomac Riverboat Company’s Water Taxis depart regularly<br />
from Gaylord National’s pier, offering exciting trips along the<br />
storied Potomac River to and from Old Town Alexandria, historic<br />
Georgetown, and George Washington’s Mount Vernon Estate and<br />
Gardens.<br />
Airport Shuttle Services<br />
Hourly shuttle service is available from Reagan National Airport<br />
(DCA). And SuperShuttle service, private sedans, and taxis are<br />
available to all major airports and most locations locally.<br />
12 th World Congress of Endoscopic Surgery 4
World Congress Schedule-at-a-Glance<br />
Wednesday, April 14, <strong>2010</strong><br />
Time Session Location<br />
7:00 AM - 11:30 AM Hands-on Colon Cadaver Lab **Offsite Lab<br />
7:30 AM - 12:00 PM MIS & Cancer Endocrine/Solid Organ Postgraduate Course Potomac Ballroom B<br />
1:00 PM - 5:00 PM MIS Gastrointestinal Cancer Postgraduate Course Potomac Ballroom B<br />
7:30 AM - 12:00 PM<br />
Bariatric Postgraduate Course: New Tech/Revisions/Endolumenal/<br />
Single Port Access Surgery<br />
Potomac Ballroom A<br />
1:00 PM - 5:00 PM Bariatric Postgraduate Course: Around the World Potomac Ballroom A<br />
12:00 PM - 1:00 PM <strong>SAGES</strong> Education and Research Foundation Awards Luncheon Maryland Ballroom C<br />
1:00 PM - 5:00 PM Hands-on Advanced Suturing and Anastomotic Techniques Lab Maryland Ballroom B-D<br />
1:00 PM - 5:00 PM<br />
Pediatrics Session: Next-Generation Pediatric MAS –<br />
A Move Toward “Scarless” Surgery<br />
Potomac Ballroom C<br />
5:00 PM - 7:00 PM World Congress Welcome Exhibit Opening Reception Prince George’s Exhibit Hall A-C<br />
Thursday, April 15, <strong>2010</strong><br />
Time Session Location<br />
6:00 AM - 7:15 AM<br />
7:30 AM - 11:30 AM<br />
Industry Satellite Symposia<br />
Covidien – “Advances in SILS Technology, Technique and Evidence”<br />
Postgraduate Surgeon in the Digital Age: Video Editing Course – Basic<br />
Video Editing with an Introduction to Advanced Techniques<br />
Potomac Ballroom D<br />
Chesapeake Conference Rooms D-E<br />
7:30 AM - 11:30 AM Avoid Pitfalls in Cholecystectomy and CBD Exploration Potomac Ballroom B<br />
7:30 AM - 11:30 AM Challenging Hernias Postgraduate Course Potomac Ballroom A<br />
7:30 AM - 12:00 PM Fundamentals of Laparoscopic Surgery Hands-on Course<br />
Lectures – Maryland Ballroom C<br />
Lab – Maryland Ballroom A<br />
9:30 AM - 11:30 AM SS01 Best of Videos 1 Potomac Ballroom C<br />
10:00 AM - 2:30 PM World Congress Exhibits, Posters & Learning Center Open Prince George’s Exhibit Hall A-C<br />
11:30 AM - 1:00 PM BREAK: Exhibits, Posters, Learning Center<br />
11:30 AM - 1:30 PM<br />
Educators Luncheon:<br />
Utilizing <strong>SAGES</strong> Educational Offerings for Residents<br />
Potomac Ballroom D<br />
11:30 AM - 1:30 PM Device Development Luncheon: From Funding to Freedom to Operate Maryland Ballroom C<br />
1:30 PM - 5:00 PM<br />
Laparoscopic IBD and Colectomy Postgraduate Course:<br />
The Status and Direction of Laparoscopic Colorectal Surgery<br />
in the Treatment of Inflammatory Bowel Disease<br />
Potomac Ballroom A<br />
1:30 PM - 5:00 PM Single Port Access Surgery Hands-On Course **Offsite lab<br />
1:30 PM - 5:00 PM<br />
MBA for Surgeons Panel:<br />
Asset Management and Protection for Surgeons<br />
Potomac Ballroom C<br />
1:30 PM - 5:00 PM Hands On Endolumenal/NOTES® Lab Maryland Ballroom B-D<br />
1:30 PM - 2:30 PM Robotics Symposium: What’s New? Potomac Ballroom B<br />
2:30 PM - 4:00 PM Metabolic Surgery Symposium: Current Status Potomac Ballroom B<br />
4:00 PM - 5:30 PM Barrett’s Debate: How to Follow, How to Treat? Potomac Ballroom B<br />
5:30 PM - 7:30 PM Industry Satellite Symposia (No Registration Required)<br />
Boston Scientific – “Intraluminal Stents and the Surgeon –<br />
Who, What, Where, When and Why?”<br />
Covidien – “Insights into the Future of Surgical Stapling: Integrated<br />
Materials, Tri-Staple Technology, Powered Staplers”<br />
Davol Inc., a BARD Company – “Advanced Endoscopic Techniques for<br />
Abdominal Wall Reconstruction”<br />
Ethicon Endo-Surgery, Inc. – “Minimally Invasive Surgery –<br />
Where is it Going?”<br />
Karl Storz Endoscopy – “The Great Debate: S-PORTAL (Single<br />
Portal Access) Surgery vs. Mini-Laparoscopy”<br />
Chesapeake D-E<br />
Potomac Ballroom D<br />
Maryland Ballroom C<br />
Potomac Ballroom C<br />
Maryland Ballroom A<br />
12 th World Congress of Endoscopic Surgery<br />
5 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
World Congress Schedule-at-a-Glance<br />
Friday, April 16, <strong>2010</strong><br />
Time Session Location<br />
7:00 AM - 8:00 AM Posters of Distinction Potomac Ballroom C<br />
8:00 AM - 9:00 AM SS02 Plenary Session 1 Potomac Ballroom A-B<br />
9:00 AM - 9:30 AM<br />
9:30 AM - 10:00 AM<br />
<strong>SAGES</strong> Presidential Address: Everyone Knows Plan A: Its All About Plan B<br />
C. Daniel Smith, M.D.<br />
Gerald Marks Lecture: The Making of a Surgeon – Revisited<br />
Richard H. Bell, M.D.<br />
Potomac Ballroom A-B<br />
Potomac Ballroom A-B<br />
10:00 AM - 2:30 PM Exhibits, Posters, Learning Center Open Prince George’s Exhibit Hall A-C<br />
10:00 AM -11:00 AM<br />
Concurrent Sessions (accepted oral & video presentations)<br />
SS03 Solid Organ<br />
Maryland Ballroom B-D<br />
SS04 Basic Science<br />
Maryland Ballroom A<br />
10:00 AM - 11:00 AM Endolumenal Therapies Session Potomac Ballroom C<br />
10:00 AM - 11:00 AM NOTES® Symposium – Alive & Well or RIP? Potomac Ballroom A-B<br />
10:00 AM - 11:00 AM Laparoscopic Education Panel – Do MIS Fellowships Have a Future? Potomac Ballroom D<br />
11:00 AM - 12:30 PM Video Complications Luncheon: What Has Happened and What Do We Have to Do? Maryland Ballroom C<br />
12:30 PM - 1:30 PM Go Global Report from the Field Panel: Teaching Laparoscopic Surgery Abroad Maryland Ballroom A<br />
12:30 PM - 2:30 PM Peer Review Training Session Potomac Ballroom D<br />
12:30 PM - 2:30 PM <strong>SAGES</strong> Presidential Debates Potomac Ballroom A-B<br />
1:30 PM - 2:30 PM Conflict of Interest Panel Maryland Ballroom A<br />
2:30 PM - 5:30 PM Resident and Fellows Scientific Session Maryland Ballroom C<br />
2:30 PM - 4:00 PM Single Port Access Surgery Panel Potomac Ballroom A-B<br />
2:30 PM - 4:00 PM<br />
Concurrent Sessions<br />
SS05 Hepatobiliary/Pancreatic<br />
Maryland Ballroom B-D<br />
SS06 Hernia<br />
Potomac Ballroom D<br />
Concurrent Sessions<br />
SS07 Best of Video 2<br />
Maryland Ballroom B-D<br />
4:00 PM - 5:30 PM<br />
SS08 Education/Simulation<br />
Maryland Ballroom A<br />
SS09 NOTES®<br />
Potomac Ballroom D<br />
2:30 PM - 5:30 PM Emerging Technology Session Potomac Ballroom C<br />
6:00 PM - 7:00 PM Meet the Leadership Reception For Residents, Fellows & New Members Pose, 18-19th Floor<br />
IMPORTANT AV INFORMATION:<br />
You may now upload your presentation on line at any point during the meeting. Please load your<br />
presentation online (http://sages.presentationman.com/) or on the show computer in the Speaker<br />
Prep room no later than 2 hours before your presentation.<br />
Please Note: Even if you have submitted your presentation online you must visit the Speaker Prep<br />
room to check in, your session moderator may not allow you to present if you do not.<br />
Speaker Prep Hours:<br />
4/13/10: 7:00 am - 5:00 pm<br />
4/14/10: 5:30 am - 5:00 pm<br />
4/15/10: 6:00 am - 5:00 pm<br />
4/16/10: 5:30 am - 5:30 pm<br />
4/17/10: 5:30 am - 5:00 pm<br />
12 th World Congress of Endoscopic Surgery 6
World Congress Schedule-at-a-Glance<br />
Saturday, April 17, <strong>2010</strong><br />
Time Session Location<br />
7:00 AM - 8:30 AM Live From Afghanistan Session: Video Conference Military Coalition Potomac Ballroom A-B<br />
7:00 AM - 8:30 AM Hernia Debates Panel: What Has Happened and What Do We Have to Do? Potomac Ballroom C<br />
8:30 AM - 9:00 AM<br />
9:00 AM - 9:30 AM<br />
Karl Storz Lecture: New Trends in Endoscopy –<br />
What Technology and Techniques are in it for You?<br />
Christopher J. Gostout, M.D.<br />
The Royal College of Physicians and Surgeons of Canada Lecture<br />
VR Systems for Surgical Oncology<br />
Robert DiRaddo, Ph.D.<br />
Potomac Ballroom A-B<br />
Potomac Ballroom A-B<br />
9:30 AM - 11:00 AM SS10 Plenary Session 2 Potomac Ballroom A-B<br />
10:00 AM - 1:00 PM<br />
11:00 AM - 11:30 AM<br />
Last Chance to Visit Exhibits, Posters, Learning Center Open –<br />
Please note 1:00 PM Closing Time!<br />
<strong>SAGES</strong> Annual General Membership Business Meeting<br />
All <strong>SAGES</strong> Members Encouraged to Attend!<br />
11:00 AM - 1:00 PM BREAK: Exhibits, Posters & Learning Center Open<br />
11:30 AM - 12:30 PM FREE Lunch in Exhibit Hall for all World Congress Scientific Session Registrants!<br />
Prince George’s Exhibit Hall A-C<br />
Potomac Ballroom C<br />
11:30 AM - 1:00 PM Fellowship Council Luncheon: The Future of Fellowships: How Will They Be Funded Maryland Ballroom C<br />
1:00 PM - 3:00 PM “Uh Oh! What Now?” Video Panel Potomac Ballroom C<br />
1:00 PM - 3:00 PM CAGS Simulation in the Training of Surgeons Session Maryland Ballroom B-D<br />
1:00 PM - 3:00 PM FES Roll-Out Session Maryland Ballroom A<br />
1:00 PM - 5:00 PM Concurrent Sessions (accepted oral & video presentations)<br />
1:00 PM - 2:00 PM SS11 Robotics Maryland Ballroom B-D<br />
1:00 PM - 3:00 PM SS12 Bariatric Potomac Ballroom A-B<br />
2:00 PM - 3:00 PM SS13 Research Grant Presentations Maryland Ballroom B-D<br />
3:00 PM - 4:00 PM SS14 Complications/Ergonomics/Instruments Maryland Ballroom B-D<br />
3:00 PM - 5:00 PM SS15 Esophageal/Gastric Potomac Ballroom D<br />
3:00 PM - 5:00 PM SS16 Colorectal Potomac Ballroom C<br />
3:00 PM - 5:00 PM SS17 Best of Video 3 Potomac Ballroom A-B<br />
3:00 PM - 5:00 PM IFSES Surgical Education Around the World Panel Maryland Ballroom A<br />
7:30 PM - 11:00 PM<br />
World Congress Gala, Featuring Dinner & the International Sing-Off<br />
Shuttles begin departing at 7:15 PM at the Bus Pickup are of the Gaylord hotel ONLY. Go to<br />
the Group Bus Loading area, located at the Woodrow Wilson exit on the 2nd level, opposite<br />
of guest parking. Buses will circle all evening until the event ends.<br />
Newseum<br />
12 th World Congress of Endoscopic Surgery<br />
Interactive Sessions: Featuring Google Moderator!<br />
Back by popular demand, <strong>SAGES</strong> is increasing the number of interactive sessions available for the<br />
<strong>2010</strong> meeting. All Scientific Sessions occurring in the MAIN SESSION Room Friday & Saturday,<br />
April 16-17, <strong>2010</strong> will feature Google Moderator, enabling attendees to participate in the<br />
presentation as it occurs! The audience will help determine the direction of the discussion by rating<br />
the submitted comments and suggestions. Moderators will address the highest rated questions.<br />
The room will be equipped with WIFI connectivity. Please bring your laptop and/or iPhone/<br />
Android/Blackberry (newest generation or with Opera Mini).<br />
Evaluation & CME Credit Claim<br />
Visit the kiosks next to registration to complete<br />
your online evaluation and CME credit form on-site.<br />
Attendees may print CME certificates two weeks<br />
after the conclusion of the meeting.<br />
The programs and lectures presented at the <strong>2010</strong> World<br />
Congress Meeting are copyrighted products of the Society<br />
of American Gastrointestinal and Endoscopic Surgeons.<br />
Any reproduction or rebroadcasting without the express<br />
written consent of <strong>SAGES</strong> is strictly prohibited.<br />
7 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
CME Worksheet<br />
<strong>SAGES</strong> Accreditation<br />
Accreditation: The Society of American Gastrointestinal and Endoscopic Surgeons (<strong>SAGES</strong>) is accredited by the Accreditation Council for<br />
Continuing Medical Education (ACCME) to sponsor Continuing Medical Education for physicians. <strong>SAGES</strong> designates this Continuing Education<br />
activity for a maximum of 41.5 AMA PRA Category 1 Credit(s). Physicians should only claim credit commensurate with the extent of their<br />
participation in the activity.<br />
CME Worksheet for the 12th World Congress of Endoscopic Surgery: This is NOT your CME credit form. Please use the worksheet below to track the<br />
number of CME hours you attend for each activity. <strong>SAGES</strong> has instituted a new process for claiming CME credits and printing certificates. All attendees<br />
wishing to receive a CME certificate for activities attended at the <strong>2010</strong> <strong>SAGES</strong> Annual Meeting (12th World Congress of Endoscopic Surgery)<br />
must first complete an on-line meeting evaluation form. Attendees will be able to print and re-print their certificates throughout the year<br />
beginning two weeks after the conclusion of the meeting.<br />
• On-site: There will be on-site kiosks located near the registration area to complete the meeting evaluation and credit claim form. Two weeks after the<br />
conclusion of the meeting, an email will notify attendees that the certificates are available to print.<br />
• During or after the meeting: Attendees will also have access to the on-line meeting evaluation and credit claim form via a link on the World Congress<br />
website.<br />
Be sure to retain your Conference Badge as the ID number will be your online PIN number. An email will also be sent, reminding attendees of<br />
this service. Those wishing to obtain a simple certificate of attendance may do so at the Evaluation Kiosks.<br />
Wednesday<br />
Activity Hours I Attended Credits Available<br />
Bariatric New Tech/Revisions/Endolumenal/Single Port PG Course 4.25<br />
MIS & Cancer: Endocrine/Solid Organ Postgraduate Course 4.25<br />
HO Course: Colon Surgery 4.5<br />
Bariatrics Around the World Postgraduate Course 3.75<br />
MIS Gastrointestinal Cancer Postgraduate Course 3.75<br />
HO Course: Advanced Suturing and Anastomotic Techniques 4.0<br />
Pediatrics Session 4.0<br />
SUBTOTAL MAX – 8.5<br />
Thursday<br />
Activity Hours I Attended Credits Available<br />
Postgraduate Surgeon in the Digital Age: Video Editing Course 3.75<br />
Challenging Hernias Postgraduate Course 3.75<br />
HO Course: Fundamentals of Laparoscopic Surgery 4.25<br />
Avoid Pitfalls in Cholecystectomy and CBD Exploration 3.75<br />
Scientific Session 1 2.0<br />
Educators Luncheon: Utilizing <strong>SAGES</strong> Educational Offerings for Residents 2.0<br />
Device Development Luncheon: From Funding to Freedom to Operate 2.0<br />
HO Course: Endolumenal/NOTES 3.5<br />
HO Course: Single Port Access Surgery 3.5<br />
Lap IBD & Colectomy Postgraduate Course 3.25<br />
MBA for Surgeons Panel<br />
0-NO credit available<br />
Symposium: Robotics: What’s New? 1.0<br />
Symposium: Metabolic Surgery :Current Status 1.5<br />
Barrett’s Debate: How to Follow, How to Treat? 1.5<br />
SUBTOTAL MAX – 10<br />
Friday<br />
Activity Hours I Attended Credits Available<br />
Scientific Sessions (panels, debates, lectures and abstract presentations including plenary) 9.0<br />
Video Complications Luncheon: What has Happened and What We Have to Do 1.5<br />
Emerging Technology Session<br />
0-NO credit available<br />
SUBTOTAL MAX – 10.5<br />
Saturday<br />
Activity Hours I Attended Credits Available<br />
Learning Center (*although the Learning Center is open Thurs-Sat, only 3.0 credits are available) 3.0<br />
Scientific Sessions (panels, debates, lectures and abstract presentations including plenary) 8.0<br />
Fellowship Council Lunch 1.5<br />
SUBTOTAL MAX – 12.5<br />
12 th World Congress of Endoscopic Surgery 8
Conflict of Interest Policy<br />
Revised and approved by <strong>SAGES</strong> Executive Committee, March, <strong>2010</strong><br />
A. Identifying Conflicts of Interest<br />
<strong>SAGES</strong> has implemented a five-tiered approach towards identifying potential conflicts of interest.<br />
1. Members of committees involved in the planning of CME activities, including the Board of Governors, must provide a<br />
financial disclosure. These disclosures are sent to the committee in advance of each committee meeting. Attendees are<br />
reminded about the disclosure policy at each committee meeting, and any committee member with a conflict is asked to<br />
recuse him or herself from the discussion of any CME activities.<br />
2. Course Directors for CME activities must provide their financial disclosures along with their suggested course outline<br />
and faculty. This information is forwarded to the Conflict of Interest Task Force, who then determines whether or not a<br />
potential conflict exists and makes suggested edits.<br />
3. Invited faculty for CME activities must provide their financial disclosures upon invitation to serve as faculty.<br />
4. For abstract submissions for the scientific session, the presenting and senior authors must provide disclosures.<br />
Abstracts are peer reviewed in a blinded fashion by multiple reviewers and are selected for presentation based on<br />
scientific merit. All disclosures are provided to the <strong>Program</strong> Committee during the “Put-The-<strong>Program</strong>-Together”<br />
meeting at which abstracts are selected for presentation.<br />
5. All speakers at <strong>SAGES</strong> CME activities must display a list of financial disclosures on the first slide of their presentation.<br />
B. Managing Potential Conflicts of Interest<br />
<strong>SAGES</strong> has implemented several mechanisms to manage conflicts of interest prior to an educational activity.<br />
1. Self-management, such as the committee member recusing him or herself from discussion of CME activities.<br />
2. The <strong>SAGES</strong> Conflict of Interest Task force reviews all Course Director’s disclosures, proposed course outlines and<br />
faculty lists. The Conflict of Interest Task Force will make edits to the course outline or faculty list if necessary.<br />
3. The <strong>SAGES</strong> disclosure form requires faculty to provide management suggestions if there is a relationship with<br />
a commercial entity. This information is forwarded to the Course Director, who is responsible for determining<br />
whether or not a conflict exists and if so, how to manage this conflict.<br />
4. If a conflict is determined, then a letter is sent to the faculty member, requiring them to adhere to the<br />
management technique or else recuse him or herself from the presentation.<br />
5. During the session, the Course Director observes the presentations and makes note of commercial bias.<br />
If any is perceived, this is immediately reported to the staff.<br />
6. All attendees of CME activities are requested to make note of perceived commercial bias in activity evaluations.<br />
The Conflict of Interest Task Force and/or the CME Committee will investigate substantive concerns.<br />
12 th World Congress of Endoscopic Surgery<br />
Commercial Bias<br />
The Society of American Gastrointestinal and Endoscopic Surgeons (<strong>SAGES</strong>) has an obligation to the medical profession and<br />
society as a whole to elucidate bias in order to protect the objectivity, scientific integrity and quality of its continuing medical<br />
education (CME) programs and to provide CME in an ethical and impartial manner. Bias is defined when a preference<br />
or predisposition exist toward a particular perspective or result that interferes with an individual’s ability to be impartial,<br />
unprejudiced or objective in order to further personal gain and disregard for data. Particular preferences may be favorable<br />
or unfavorable. When bias exists, impartial judgment and neutrality may be compromised. Bias may be minimized through<br />
a declaration of conflict of interest or commercial interests, an evaluation of peer-reviewed evidence-based medicine with<br />
an integration of clinical expertise and/or experience, and an assertion of published sources for evidence-based reporting.<br />
<strong>SAGES</strong> requires presenters at all educational events to specifically avoid introducing bias, commercial or otherwise, into their<br />
presentations.<br />
<strong>SAGES</strong> Mission Statement<br />
“Our mission is to provide leadership in surgery, particularly gastrointestinal and<br />
endoscopic surgery, to optimize patient care through education, research and innovation.”<br />
– <strong>SAGES</strong> has evolved over the last 25 years into a leading society for gastrointestinal surgery,<br />
endoscopy and minimal invasive technology.<br />
– Not only does <strong>SAGES</strong> provide leadership in clinical care, but it also helps surgeons optimize patient care by<br />
providing direction for cutting edge technology, basic and translational science, and educational opportunities.<br />
– <strong>SAGES</strong> represents leadership in the surgical world for gastrointestinal disease.<br />
– <strong>SAGES</strong> is the society to improve your clinical skills.<br />
9 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Notes<br />
12 th World Congress of Endoscopic Surgery 10
General Information (continued)<br />
Save the Date!<br />
CAGS Canadian Surgery Forum<br />
September 2 - 5, <strong>2010</strong>, Québec City Convention Centre, Canada<br />
<strong>SAGES</strong> Scientific Session & Postgraduate Course<br />
March 30 - April 2, 2011, San Antonio, Texas<br />
CAGS Canadian Surgery Forum<br />
September 15 - 18, 2011, London Convention Centre, Canada<br />
<strong>SAGES</strong> Scientific Session & Postgraduate Course<br />
March 7 - 10, 2012, San Diego, CA<br />
<strong>SAGES</strong> Scientific Session & Postgraduate Course<br />
April 17 - 20, 2013, Baltimore Convention Center, Baltimore, MD<br />
<strong>SAGES</strong> Scientific Session & Postgraduate Course<br />
April 2 - 5 , 2014, Salt Lake Convention Center, Salt Lake City, UT<br />
Childcare Services<br />
White House Nannies<br />
www.whitehousenannies.com<br />
(301) 652-8088 Temporary Division<br />
(800) 266-9024 Toll Free<br />
White House Nannies, Inc. is owned and managed by Barbara G. Kline. Mrs.<br />
Kline is a current member and former board member of the International Nanny<br />
Association (INA). The agency is also a member of the Association of Premier<br />
Nanny Agencies (APNA). White House Nannies. Inc. was awarded national<br />
recognition as APNA’s 2000 Agency of the Year. The hallmark of the agency is the<br />
thoughtful matching of Client and Caregiver needs to assure the best possible inhome<br />
childcare placements. With 25 years of experience, the agency has become<br />
the premier agency in the Washington area.<br />
Caregiver rates:<br />
Negotiated with Caregiver, generally $16-$20 per hour.<br />
Additional Agency Referral Rates:<br />
Hotel Child Care, booked in advance $65.00 per day per Caregiver<br />
Hotel Child Care, booked within 48hrs of need $75.00 per day per Caregiver<br />
A free Cyber Café is available for<br />
all World Congress attendees and<br />
exhibitors, located in the Registration<br />
area and open during normal<br />
registration hours. No message<br />
center is available this year.<br />
Please leave the following numbers<br />
with your offices and families, in<br />
case they cannot reach you on<br />
your cell phone:<br />
World Congress On-Site Office:<br />
Phone: (301) 965-5343<br />
Fax: (301) 965-5344<br />
A Gentle Reminder<br />
About Safety/Security:<br />
We have taken every precaution to assure the<br />
safety and security of our guests and their<br />
possessions. However, we urge you to be<br />
aware and take simple steps to guard your<br />
possessions.<br />
– Do not leave your purse or briefcase<br />
unattended.<br />
– Do not leave your laptop, phone or other<br />
electronic devices on the floor or out of your<br />
sight in a darkened room<br />
– Be aware of your surroundings, in the Gaylord<br />
Hotel, in and around the National Harbor area<br />
and in Washington, DC.<br />
Have a safe & secure meeting!<br />
12 th World Congress of Endoscopic Surgery<br />
11 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
National Harbor, MD Map<br />
12 th World Congress of Endoscopic Surgery 12
Gaylord National Floor Plans<br />
Maryland & Potomac Ballrooms<br />
Convention Center | Level 2<br />
6<br />
5<br />
4<br />
3<br />
2<br />
4<br />
F W hi B d<br />
B<br />
A<br />
D<br />
Maryland Ballroom<br />
C<br />
L K J<br />
I H G<br />
F E D<br />
C B A<br />
12 11 10<br />
Chesapeake Conference Rooms<br />
Escalators<br />
To Hotel<br />
Ballroom Level<br />
9 8 7<br />
6 5 4<br />
1 2 3<br />
B<br />
Potomac Ballroom<br />
World Congress Exhibits, Posters, Learning Center (see pg. 193)<br />
Stage<br />
A<br />
D<br />
C<br />
6<br />
5<br />
4<br />
3<br />
2<br />
1<br />
12 th World Congress of Endoscopic Surgery<br />
Chesapeake Conference Rooms:<br />
Potomac Ballrooms:<br />
Speaker Prep<br />
World Congress Office<br />
<strong>SAGES</strong> Foundation Lounge<br />
FLS Testing<br />
Thursday Digital Hands-On Course<br />
Industry Education<br />
Wednesday through Saturday Main and Concurrent Session Rooms<br />
Postgraduate Courses<br />
Scientific Sessions<br />
Keynote Lectures<br />
Panels, Symposia<br />
Lunches<br />
Industry Education<br />
Maryland<br />
GaylordNational.com<br />
Ballrooms:<br />
| 1-877-677-9352<br />
Wednesday<br />
|<br />
through<br />
201 Waterfront<br />
Saturday<br />
Street,<br />
Concurrent<br />
National Harbor,<br />
Session<br />
MD 20745<br />
Rooms<br />
Hands-On Courses<br />
(WASHINGTON D.C. AREA )<br />
Scientific Sessions<br />
Panels, Symposia<br />
Lunches<br />
Industry Education<br />
13 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Wo r l d C o n g r e s s 2 0 1 0 Le a d e r s<br />
<strong>Program</strong> Co-Chair (<strong>SAGES</strong>): <strong>Program</strong> Chair (<strong>SAGES</strong>): <strong>Program</strong> Chair (CAGS):<br />
Daniel Herron, M.D. Barry Salky, M.D. Christopher Schlachta, M.D.<br />
<strong>2010</strong> Course Chairs & Unit Coordinators<br />
Equipment Czar Chair: Kevin M. Reavis, M.D.<br />
Equipment Czar Co-Chair:<br />
Gretchen Purcell-Jackson, M.D.<br />
Poster Chair: Subhash U. Kini, M.D.<br />
Poster Co-Chair: Melina C. Vassiliou, M.D.<br />
Video Chair: Donald J. Selzer, M.D.<br />
Video Co-Chair: Leena Khaitan, M.D.<br />
Learning Center Chair: Allan E. Okrainec, M.D.<br />
Learning Center Co-Chair: Brian P. Jacob, M.D.<br />
Advanced Suturing and Anastomotic<br />
Techniques HO Course Chair:<br />
Kelvin D. Higa, M.D.<br />
Advanced Suturing and Anastomotic<br />
Techniques HO Course Co-Chair:<br />
Aureo L. De Pauala, M.D.<br />
Colon HO Course Chair:<br />
Mark H. Whiteford, M.D.<br />
Colon HO Course Co-Chair:<br />
Conor P. Delaney, M.D.<br />
Digital Video HO Course Chair:<br />
Dmitry Oleynikov, M.D.<br />
Digital Video HO Course Co-Chair:<br />
John R. Romanelli, M.D.<br />
Endolumenal/NOTES® HO Course Chair:<br />
Santiago Horgan, M.D.<br />
Endolumenal/NOTES® HO Course Co-Chair:<br />
Christopher C. Thompson, M.D.<br />
Single Port Access Surgery HO Course Chair:<br />
Paul G. Curcillo II, M.D.<br />
Single Port Access Surgery HO Course Co-<br />
Chair: Daniel J. Scott, M.D.<br />
Avoid Pitfalls in Cholecystectomy and<br />
CBD Exploration PG Course Chair:<br />
Michael B. Edye, M.D.<br />
Avoid Pitfalls in Cholecystectomy and<br />
CBD Exploration PG Course Co-Chair:<br />
Bertrand Millat, M.D.<br />
Bariatric Around the World PG Course Chair:<br />
Alfons Pomp, M.D.<br />
Bariatric Around the World PG<br />
Course Co-Chair: Manolo Cortez, M.D.<br />
Bariatric New Techniques PG Course Chair:<br />
Scott A. Shikora, M.D.<br />
Bariatric New Techniques PG Course Co-Chair:<br />
Raul J. Rosenthal, M.D.<br />
Challenging Hernias PG Course Chair:<br />
Kristi Lee Harold, M.D.<br />
Challenging Hernias PG Course Co-Chair:<br />
Shirin Towfigh, M.D.<br />
FLS PG Course Chair: E. Matthew Ritter, M.D.<br />
FLS PG Course Co-Chair: Gerald M. Fried, M.D.<br />
Lap IBD & Colectomy PG Course Chair:<br />
John H. Marks, M.D.<br />
Lap IBD & Colectomy PG Course Co-Chair:<br />
Eric Glenn Weiss, M.D.<br />
MIS & Cancer Endocrine/Solid Organ PG<br />
Course Chair: William Barry Inabnet III, M.D.<br />
MIS & Cancer Endocrine/Solid Organ PG<br />
Course Co-Chair: Miguel Herrera, M.D.<br />
MIS & Cancer GI PG Course Chair:<br />
Horacio J. Asbun, M.D.<br />
MIS & Cancer GI PG Course Co-Chair:<br />
Seigo Kitano, M.D.<br />
Pediatric Surgery Symposium Chair:<br />
Sanjeev Dutta, M.D.<br />
Pediatric Surgery Symposium Co-Chair:<br />
Jacob Langer, M.D.<br />
3-Hour MBA for Surgeons Chair:<br />
Demetrius E.M. Litwin, M.D.<br />
3-Hour MBA for Surgeons Co-Chair:<br />
Fredrick J. Brody, M.D.<br />
Device Development Luncheon Chair:<br />
Raymond P. Onders, M.D.<br />
Device Development Luncheon Co-Chair:<br />
Dennis L. Fowler, M.D.<br />
Education Luncheon Chair:<br />
L. Michael Brunt, M.D.<br />
Education Luncheon Co-Chair:<br />
Daniel J. Gagne, M.D.<br />
Fellowship Council Lunch Chair:<br />
Adrian E. Park, M.D.<br />
Fellowship Council Lunch Co-Chair:<br />
Bruce D. Schirmer, M.D.<br />
Video Complications Lunch Chair:<br />
Bipan Chand, M.D.<br />
Video Complications Lunch Co-Chair:<br />
Manabu Yamamoto, M.D.<br />
Emerging Technology Session Chair:<br />
Steven D. Schwaitzberg, M.D.<br />
Emerging Technology Session Co-Chair:<br />
Alex Gandsas, M.D.<br />
Resident’s Day Coordinators:<br />
Gregory F. Dakin, M.D. & Adheesh A. Sabnis, M.D.<br />
12 th World Congress of Endoscopic Surgery 14<br />
<strong>SAGES</strong> Panel/Session/Symposium/<br />
Debates Chairs/Co-Chairs:<br />
Barrett’s Debate Chair: John Hunter, M.D.<br />
Barrett’s Debate Co-Chair: Karl H. Fuchs, M.D.<br />
<strong>SAGES</strong> Presidential Debate Chair:<br />
Daniel J. Deziel, M.D.<br />
<strong>SAGES</strong> Presidential Debate Co-Chair:<br />
Nathaniel J. Soper, M.D.<br />
Hernia Debates Chair: Guy R. Voeller, M.D.<br />
Hernia Debates Co-Chair:<br />
Edward H. Phillips, M.D.<br />
Conflict of Interest Panel Chairs:<br />
Steve Eubanks, M.D. & Neely Panton, M.D.<br />
IFSES Panel Chair: Alberto Chousleb, M.D.<br />
IFSES Panel Co-Chair: Natan Zundel, M.D.<br />
Lap Education Panel Chair:<br />
Bruce D. Schirmer, M.D.<br />
Lap Education Panel Co-Chair:<br />
Joseph Mamazza, M.D.<br />
Global Panel Chair: Raul J. Rosenthal, M.D.<br />
Global Panel Co-Chair: Horacio J. Asbun, M.D.<br />
Single Port Access Surgery Panel Chair:<br />
Joel Leroy, M.D.<br />
Single Port Access Surgery Panel Co-Chair:<br />
Andrew A. Gumbs, M.D.<br />
“Uh Oh, What Now?” Video Panel Chair:<br />
David R. Urbach, M.D.<br />
“Uh Oh, What Now?” Video Panel Co-Chair:<br />
David Bryan Earle, M.D.<br />
Endolumenal Therapies Session Chair:<br />
Dean J. Mikami, M.D.<br />
Endolumenal Therapies Session Co-Chair:<br />
Simon Bergman, M.D.<br />
FES Roll-out Session Chair: Brian J. Dunkin, M.D.<br />
FES Roll-out Session Co-Chair:<br />
Jeffrey M. Marks, M.D.<br />
Live from Fellujah Session Chair:<br />
Steven P. Bowers, M.D.<br />
Live from Fellujah Session Co-Chair:<br />
Richard M. Satava, M.D.<br />
CAGS Simulation in the Training of Surgeons<br />
Session Chair: Liane S. Feldman, M.D.<br />
CAGS Simulation in the Training of Surgeons<br />
Session Co-Chair:<br />
Teodor P. Grantcharov, M.D.<br />
Peer Review Training Session Chair:<br />
Abe L. Fingerhut, M.D.<br />
Peer Review Training Session Co-Chair:<br />
Sir Alfred Cuschieri, M.D.<br />
Metabolic Surgery Symposium Chair:<br />
Philip R. Schauer, M.D.<br />
Metabolic Surgery Symposium Co-Chair:<br />
Francesco Rubino, M.D.<br />
NOTES® Symposium Chair:<br />
David W. Rattner, M.D.<br />
NOTES® Symposium Co-Chair: G. V. Rao, M.D.<br />
Robotics Symposium Chair:<br />
Mehran Anvari, M.D.<br />
Robotics Symposium Co-Chair:<br />
Jacques Marescaux, M.D.<br />
Conflict of Interest Panel Chair:<br />
Steve Eubanks, M.D.<br />
Conflict of Interest Panel Co-Chair:<br />
Neely Panton, M.D.
Wo r l d C o n g r e s s 2 0 1 0 Le a d e r s<br />
World Congress<br />
<strong>Program</strong> Committee<br />
Chair: Steven D. Schwaitzberg, M.D.<br />
Horacio J. Asbun, M.D.<br />
Yves Bendavid, M.D.<br />
Simon Bergman, M.D.<br />
Daniel Birch, M.D.<br />
Steven P. Bowers, M.D.<br />
Fredrick J. Brody, M.D.<br />
Robin Boushey, M.D.<br />
L. Michael Brunt, M.D.<br />
James Ellsmere, M.D.<br />
Liane Feldman, M.D.<br />
Edward L. Felix, M.D.<br />
Denise W. Gee, M.D.<br />
Teodor Grantcharov, M.D.<br />
Carroll M. Harmon, M.D.<br />
Daniel M. Herron, M.D.<br />
Michael D. Holzman, M.D.<br />
Santiago Horgan, M.D.<br />
Gretchen Purcell Jackson, M.D.<br />
Timothy D. Kane, M.D.<br />
Namir Katkhouda, M.D.<br />
Dimitrios A. Linos, M.D.<br />
John H. Marks, M.D.<br />
Brent D. Matthews, M.D.<br />
Marian P. McDonald, M.D.<br />
Stephen S. McNatt, M.D.<br />
Adam Meneghetti, M.D.<br />
Michael S. Nussbaum, M.D.<br />
Dmitry Oleynikov, M.D.<br />
Allan Okrainec, M.D.<br />
Neely Panton, M.D.<br />
Edward H. Phillips, M.D.<br />
William S. Richardson, M.D.<br />
Raul J. Rosenthal, M.D.<br />
Barry A. Salky, M.D.<br />
Cliff Sample, M.D.<br />
Christopher M. Schlachta, M.D.<br />
Daniel J. Scott, M.D.<br />
Paul A. Severson, M.D.<br />
Neal E. Seymour, M.D.<br />
Carl J. Westcott, M.D.<br />
Manabu Yamamoto, M.D.<br />
Tonia M. Young-Fadok, M.D.<br />
Natan Zundel, M.D.<br />
FLS Testing Available!<br />
Wednesday, April 14 - Saturday, April 17, <strong>2010</strong><br />
Location: Chesapeake Conference Rooms 7-9<br />
All testing appointments must be made by April 9 –<br />
no onsite appointments available<br />
Contact FLS@sages.org for more details or to schedule your test.<br />
<strong>SAGES</strong> Accreditation<br />
The Society of American Gastrointestinal and Endoscopic Surgeons (<strong>SAGES</strong>) is accredited by<br />
the Accreditation Council for Continuing Medical Education (ACCME) to sponsor Continuing<br />
Medical Education for physicians.<br />
The Society of American Gastrointestinal and Endoscopic Surgeons (<strong>SAGES</strong>) designates this<br />
educational activity for a maximum of 41.5 hours AMA PRA Category 1 Credit(s). Physicians<br />
should only claim credit commensurate with the extent of their participation in the activity.<br />
New Process for Claiming CME Credit for<br />
Meeting Attendees!<br />
<strong>SAGES</strong> has instituted a new process for claiming CME credits and printing certificates. All<br />
attendees wishing to receive a CME certificate for activities attended at the <strong>2010</strong> <strong>SAGES</strong><br />
Annual Meeting (12 th World Congress of Endoscopic Surgery) must first complete an online<br />
meeting evaluation form. Attendees will be able to print and re-print their certificates<br />
throughout the year beginning two weeks after the conclusion of the meeting.<br />
• On-site: There will be on-site kiosks located near the registration area to complete the<br />
meeting evaluation and credit claim form. Two weeks after the conclusion of the meeting,<br />
an email will notify attendees that the certificates are available to print.<br />
• During or after the meeting: Attendees will also have access to the on-line<br />
meeting evaluation and credit claim form via a link on the World Congress website<br />
(www.12thworldcongress.org).<br />
Be sure to retain your Conference Badge as the ID number will be your online PIN<br />
number. An email will also be sent, reminding attendees of this service. Those<br />
wishing to obtain a simple certificate of attendance may do so at the Evaluation<br />
Kiosks.<br />
To fully comply with ACCME regulations,<br />
all World Congress attendees must have their badge<br />
scanned before entering any course or session room<br />
in order to receive CME credit for that event.<br />
12 th World Congress of Endoscopic Surgery<br />
15 www.12thworldcongress.org
Wednesday, April 14, <strong>2010</strong><br />
Time Session Location<br />
7:00 AM - 11:30 AM Hands-on Colon Cadaver Lab **Offsite Lab<br />
7:30 AM - 12:00 PM<br />
MIS & Cancer Endocrine/Solid Organ Postgraduate<br />
Course<br />
Potomac Ballroom B<br />
1:00 PM - 5:00 PM MIS Gastrointestinal Cancer Postgraduate Course Potomac Ballroom B<br />
7:30 AM - 12:00 PM<br />
Bariatric Postgraduate Course: New Tech/Revisions/<br />
Endolumenal/Single Port Access Surgery<br />
Potomac Ballroom A<br />
1:00 PM - 5:00 PM Bariatric Postgraduate Course: Around the World Potomac Ballroom A<br />
12:00 PM - 1:00 PM<br />
<strong>SAGES</strong> Education and Research Foundation Awards<br />
Luncheon<br />
1:00 PM - 5:00 PM<br />
Hands-on Advanced Suturing and Anastomotic<br />
Techniques Lab<br />
1:00 PM - 5:00 PM<br />
Pediatrics Session: Next-Generation Pediatric MAS –<br />
A Move Toward “Scarless” Surgery<br />
Maryland Ballroom C<br />
Maryland Ballroom B-D<br />
Potomac Ballroom C<br />
5:00 PM - 7:00 PM World Congress Welcome Exhibit Opening Reception Prince George’s Exhibit Hall A-C<br />
World Congress Goes Green!<br />
In an effort to support the environment, you will see less paper for the 12th Annual World Congress.<br />
The printed <strong>Final</strong> <strong>Program</strong> will include the regular schedule and course/panel outlines, as well as<br />
oral abstracts, Poster of Distinction abstracts and poster listing. However, electronic copies of all<br />
the abstracts, digital posters, and Postgraduate course syllabi will be available on thumb drive for<br />
all attendees. The “Electronic Meeting Guide” will be completely navigational and searchable. Print<br />
kiosks will also be available throughout the Convention Center.<br />
12 th World Congress of Endoscopic Surgery<br />
IMPORTANT AV INFORMATION:<br />
You may now upload your presentation on line at any point during the meeting. Please load your<br />
presentation online (http://sages.presentationman.com/) or on the show computer in the Speaker<br />
Prep room no later than 2 hours before your presentation.<br />
Please Note: Even if you have submitted your presentation online you must visit the Speaker Prep<br />
room to check in, your session moderator may not allow you to present if you do not.<br />
Speaker Prep Hours:<br />
4/13/10: 7:00 am - 5:00 pm<br />
4/14/10: 5:30 am - 5:00 pm<br />
4/15/10: 6:00 am - 5:00 pm<br />
4/16/10: 5:30 am - 5:30 pm<br />
4/17/10: 5:30 am - 5:00 pm<br />
17 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Wednesday, April 14, <strong>2010</strong><br />
7:00 AM - 11:30 AM *Separate Registration Fee<br />
Hands-on Colon Cadaver Lab<br />
Chair: Mark H. Whiteford, M.D.; Co-Chair: Conor P. Delaney, M.D.<br />
**Offsite Lab<br />
Location: Washington Institute of Surgical Endoscopy (WISE)<br />
The George Washington University Medical Center<br />
2300 I Street, NW, Ross Hall, Washington DC, 20037<br />
Shuttles for faculty and course registrants will depart at 6:15AM from the Gaylord National Hotel and Convention Center.<br />
Go to the Group Bus Loading area, located at the Woodrow Wilson exit on the 2 nd level, opposite of guest parking.<br />
This half-day practical cadaver lab course is designed for general and colorectal surgeons, fourth year or chief residents and MIS or colorectal<br />
fellows. All applicants should be familiar with advanced laparoscopic techniques and wish to expand their skills in laparoscopic colon and<br />
rectal surgery. Techniques for straight laparoscopic and single incision colectomies, bowel mobilization, vessel division, and anastomoses will<br />
be taught with an emphasis on oncologic principles. The course will emphasize common alternative approaches including lateral-to-medial,<br />
medial-to-lateral, and hand-assisted techniques, to facilitate resection of the entire intra-abdominal colon and the rectum. Lab stations will<br />
have a 1:3 faculty:participant ratio.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• Discuss multiple approaches to mobilization, resection and anastomosis of the right and left colon<br />
• List techniques, tips and tricks for total mesorectal dissection of the rectum<br />
• Understand the principles in laparoscopic colorectal surgery for both benign and malignant disease<br />
Schedule<br />
6:30 AM Shuttles Depart Gaylord Hotel<br />
7:00 AM Introduction Mark H. Whiteford, M.D. & Conor P. Delaney, M.D.<br />
7:10 AM Video: Single Incision Laparoscopic Right and Transverse Colectomy Mark Whiteford, M.D.<br />
7:30 AM Video: Laparoscopic Left Colectomy and Proctectomy Conor Delaney, M.D.<br />
7:50 AM Right Colectomy Techniques<br />
Transverse Colectomy Techniques<br />
left Colectomy Techniques<br />
rectal Dissection Techniques<br />
Lab Instructors<br />
11:10 AM Questions/Discussion All Faculty<br />
11:30 AM Shuttles Return to Gaylord Hotel<br />
Lab Instructors:<br />
Christopher Cunningham, M.D.<br />
Jonathan Efron, M.D.<br />
Matthew Kalady, M.D.<br />
Michael K. W. Li, M.D.<br />
John Park, M.D.<br />
Sonia Ramamoorthy, M.D.<br />
<strong>SAGES</strong> acknowledges educational grants in support of this World Congress course from:<br />
Applied Medical, Covidien, Ethicon Endo-Surgery, Inc., Olympus and Stryker Endoscopy<br />
<strong>SAGES</strong> acknowledges contributions in-kind in support of this World Congress course from:<br />
Applied Medical, Cambridge Endoscopy, Covidien, Ethicon Endo-Surgery, Inc., Ethicon Inc.,<br />
Karl Storz Endoscopy-America, Microline Surgical, Novare Surgical Systems, Olympus and Stryker Endoscopy<br />
To fully comply with ACCME regulations, all World Congress<br />
attendees must have their badge scanned before entering any<br />
course or session room in order to receive CME credit for that event.<br />
12 th World Congress of Endoscopic Surgery 18
Wednesday, April 14, <strong>2010</strong><br />
7:30 AM - 12:00 PM *included in Registration SuperPass (Option A) or Registration Option B<br />
MIS & Cancer Endocrine/Solid Organ Postgraduate Course<br />
Chair: William B. Inabnet III, M.D.; Co-Chair: Miguel Herrera, M.D.<br />
location: Potomac Ballroom B<br />
Description:<br />
The Endocrine/Solid Organ course will provide a comprehensive update on disorders of the thyroid, adrenal and pancreas. The course will<br />
combine didactic presentations with video-based education and panel discussions to emphasize established and novel minimally invasive<br />
techniques.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• Cite the changing paradigm in the work-up and management of thyroid malignancy<br />
• Describe current minimally invasive techniques for thyroid, adrenal and pancreas surgery<br />
• Differentiate benign from malignant adrenal pathology<br />
• Describe the appropriate work-up and treatment of islet cell tumors of the pancreas<br />
Schedule<br />
7:30 AM Introduction William B. Inabnet III, M.D. & Miguel Herrera, M.D.<br />
7:35 AM Thyroid Cancer Update Allan Siperstein, M.D.<br />
7:50 AM Video-Endoscopic and Robotic-Assisted Thyroidectomy W. Y. Chung, M.D.<br />
8:05 AM Minimally Invasive Thyroidectomy with Intra-Operative Nerve Monitoring Allan Dackiw, M.D.<br />
8:20 AM Video-Endoscopic and Thoracoscopic Parathyroidectomy James Lee, M.D.<br />
8:35 AM Discussion<br />
8:55 AM Adrenal Incidentaloma Steven Schwaitzberg, M.D.<br />
9:10 AM Pheochormocytoma Quan Yang Duh, M.D.<br />
9:25 AM Adrenal Malignancy and MIS Vivian Strong, M.D.<br />
9:40 AM Laparoscopic Transabdominal and Retroperitoneal Adrenalectomy Martin Walz, M.D.<br />
10:00 AM Discussion<br />
10:15 AM BREAK<br />
10:30 AM Functioning Islet Cell Tumors Juan-Pablo Pantoja, M.D.<br />
10:45 AM Pancreatic Incidentaloma Horacio Asbun, M.D.<br />
11:00 AM Gastric Bypass Induced Hyperinsulinemic Hypoglycemia Sayeed Ikramuddin, M.D.<br />
11:15 AM Laparoscopic Enucleation and Distal Pancreatic Resection Andrew Gumbs, M.D.<br />
11:30 AM Laparoscopic Resection of Hepatic Neuroendocrine Metastases Brice Gayet, M.D.<br />
11:45 AM Discussion<br />
1:00 PM - 5:00 PM *included in Registration SuperPass (Option A) or Registration Option B<br />
MIS Gastrointestinal Cancer Postgraduate Course<br />
Chair: Horacio J. Asbun, M.D.; Co-Chair: Seigo Kitano, M.D.<br />
location: Potomac Ballroom B<br />
Description:<br />
We will discuss on Indication, Procedures of MIS and Outcome etc. of minimally invasive surgery (MIS) for Gastrointestinal Cancer.<br />
Additionally, we will define the role of MIS for cancer treatment according to the clinical evidences. In this session, we will have a great<br />
opportunity that World leading surgeons discuss on minimally invasive surgery for gastrointestinal cancer.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• Choose appropriate Indication of MIS for Gastrointestinal Cancer<br />
• Assess what the safe techniques of MIS for Gastrointestinal Cancer<br />
• Deepen their knowledge on Clinical Evidence related to MIS for Gastrointestinal Cancer<br />
• Define the problems regarding MIS for Gastrointestinal Cancer and state the prospect for the future<br />
Schedule<br />
1:00 AM Introduction Horacio J. Asbun, M.D. & Seigo Kitano, M.D.<br />
1:05 PM Thoracoscopic Esophagectomy for Cancer Haruhiro Inoue, M.D.<br />
1:25 PM Laparoscopic TransHiatal Esophagectomy for Early Cancer Abeezar Sarela, M.D.<br />
1:45 PM Laparoscopic Gastrectomy for Early Cancer Han-Kwang Yang, M.D.<br />
2:05 PM Laparoscopic Gastrectomy for Advanced Cancer Vivian E.M. Strong, M.D.<br />
2:25 PM Discussion<br />
2:45 PM BREAK<br />
3:05 PM Clinical Evidences of Laparoscopic Surgery for Advanced Colorectal Cancer R. Larry Whelan, M.D.<br />
3:25 PM Laparoscopic Total Mesorectal Excision for Rectal Cancer Eric Rullier, M.D.<br />
3:45 PM Laparoscopic Procedures for Rectal Cancer After Radiochemotherapy Joel Leroy, M.D.<br />
4:05 PM Laparoscopic Approach for Obstructing Colorectal Cancer Nicolas Demartines, M.D.<br />
4:25 PM Current Status of Robotic Colorectal Surgery Richard M. Satava, M.D.<br />
4:45 PM Discussion<br />
<strong>SAGES</strong> acknowledges an educational grant in support of this World Congress course from Ethicon Endo-Surgery, Inc.<br />
19 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
Wednesday, April 14, <strong>2010</strong><br />
7:30 AM - 12:00 PM *Included in Registration SuperPass (Option A) or Registration Option B<br />
Bariatric Postgraduate Course:<br />
New Tech/Revisions/Endolumenal/Single Port Access Surgery<br />
Chair: Scott A. Shikora, M.D.; Co-Chair: Raul J. Rosenthal, M.D.<br />
location: Potomac Ballroom A<br />
This postgraduate course will review some of the latest and novel technologies being proposed or currently introduced into the field of<br />
bariatric surgery. These operative techniques and devices all claim to offer less invasive and lower risk options for patients who qualify<br />
for bariatric surgery. Some even offer new and innovative mechanisms of action. The faculty, all of whom have an experience with these<br />
procedures, will offer their opinions concerning their feasibility, cost-effectiveness, and clinical relevance.<br />
Objectives: At the conclusion of this session, participants will be able to:<br />
• Review the feasibilities and techniques for endolumenal bariatric procedures and in particular, gastric partitioning for weight loss<br />
• Become familiar with the techniques and applications of single port surgery and to understand the controversy surrounding its benefit<br />
• Understand the theoretical benefits and clinical results of neuromodulation<br />
• Become familiar with the current and possible future surgical options for revision of failed bariatric operations<br />
Schedule<br />
7:30 AM Introduction Scott A. Shikora, M.D. & Raul J. Rosenthal, M.D.<br />
7:35 AM Overview of Endolumenal Procedures – Do They Really Work? Jacques M. Himpens, M.D.<br />
7:55 AM Endolumenal Gastric Partitioning Roberto Fogel, M.D.<br />
8:15 AM Can a Gastric Bypass be Created Endoscopically? Alfonso Torquati, M.D.<br />
8:35 AM Single Port Bariatric Surgery – An Analysis of Feasibility and Benefit Julio Teixeira, M.D.<br />
8:55 AM Single Port is NOT Beneficial Raul J. Rosenthal, M.D.<br />
9:15 AM Update on Neuromodulation Scott A. Shikora, M.D.<br />
9:35 AM Discussion<br />
10:10 AM BREAK<br />
10:30 AM Banding a Failed Gastric Bypass (Fixed and Adjustable) Matthew Hutter, M.D.<br />
10:45 AM How to Rescue a Patient After a Failed Band Luigi Angrisani, M.D.<br />
11:00 AM Are there Any Options for a Failed Biliopancreatic Diversion With or Without Duodenal Switch? Michel Gagner, M.D.<br />
11:15 AM Endolumenal Pouch and Anastomosis Reduction: An Analysis Christopher Thompson, M.D.<br />
11:30 AM Discussion<br />
<strong>SAGES</strong> acknowledges educational grants in support of this World Congress course from Covidien, Gore & Associates and Stryker Endoscopy.<br />
1:00 PM - 5:00 PM *Included in Registration SuperPass (Option A) or Registration Option B<br />
Bariatric Postgraduate Course: Around the World<br />
Chair: Alfons Pomp M.D.; Co-Chair: Manolo Cortez, M.D.<br />
location: Potomac Ballroom A<br />
Description:<br />
During this half-day course international surgeons will provide expert commentary on how they choose the appropriate weight loss operation.<br />
Experienced clinicians will discuss their therapeutic strategy when patients who have been submitted to surgery fail to sustain weight loss.<br />
Surgeons will discuss the prevention and treatment of complications of bariatric surgery. An introduction to the mechanisms of “metabolic”<br />
surgery and a brief overview of emerging techniques, including single port access and endoluminal techniques will complete this synopsis<br />
Objectives: At the conclusion of this session, participants will be able to:<br />
• Differentiate and compare weight loss surgery options<br />
• Analyze and compose a strategy to deal with bariatric surgery failures<br />
• Recognize, assess and treat complications of weight loss surgery<br />
• Integrate and review the indications of metabolic surgery into a bariatric practice<br />
• Review and appraise the indications for new therapeutic weight loss surgery options<br />
Schedule<br />
1:00 PM Introduction Alfons Pomp, M.D. & Manolo Cortez, M.D.<br />
1:05 PM Gastric Banding is the Best Weight Loss Operation Amiki Szold, M.D.<br />
1:20 PM Why I No Longer Perform Gastric Banding Jacques Himpens, M.D.<br />
1:35 PM Discussion<br />
1:45 PM Gastric Bypass is the Best Operation for BMI > 50 Ninh Nguyen, M.D.<br />
2:00 PM Bilopancreatic Diversion is the Best Operation for BMI > 50 Simon Biron, M.D.<br />
2:15 PM Discussion<br />
2:25 PM What I Do When the Band Does Not Work John Dixon, M.D.<br />
2:40 PM What I Do When Gastric Bypass Does Not Work Michel Gagner, M.D.<br />
2:55 PM Discussion<br />
3:05 PM BREAK<br />
3:25 PM Complications of Gastric Banding (and What I DO with Them) Karl Miller, M.D.<br />
3:40 PM Complications of Gastric Sleeve Antonio Lacy, M.D.<br />
3:55 PM Complications of Gastric V Bypass Scott Shikora, M.D.<br />
4:10 PM Discussion<br />
4:20 PM Metabolic Surgery – What’s it All About Ricardo V. Cohen, M.D.<br />
4:35 PM Single Access and Endoluminal Bariatric Surgery Marc Bessler, M.D.<br />
4:50 PM Discussion<br />
<strong>SAGES</strong> acknowledges an educational grant in support of this World Congress course from Ethicon Endo-Surgery, Inc.<br />
12 th World Congress of Endoscopic Surgery 20
Wednesday, April 14, <strong>2010</strong><br />
12:00 PM - 1:00 PM Location: Maryland Ballroom C<br />
<strong>SAGES</strong> Education and Research Foundation Awards Luncheon<br />
The <strong>2010</strong> Awards Luncheon will recognize distinguished leaders for their work in minimally invasive surgery and raise funds that will keep<br />
patient safety and minimal access surgery in the forefront.<br />
Cost: $125 per ticket / $1,100 per table (10 seats) Please bring your ticket or name of company hosting you.<br />
<strong>SAGES</strong> Foundation thanks the following sponsors of this event:<br />
Applied Medical, Atrium Medical, Covidien, Gore & Associates, Karl Storz Endoscopy, Simbionix<br />
Host: Bruce Schirmer, MD, <strong>SAGES</strong> Foundation President<br />
To register on-site, visit the World Congress Registration desk by Wednesday at 10:00 AM. A portion of your contribution is tax-deductible to<br />
the extent permitted by law.<br />
<strong>SAGES</strong> does not offer CME credits for this lunch.<br />
<strong>2010</strong> <strong>SAGES</strong> Career Development Award & Research Grant Winners<br />
Presented by: Aurora Pryor, MD, Research Committee Chair & Representatives of Supporting Companies as follows.<br />
Career Development Award – TBA On-Site<br />
Research Grant Awards:<br />
<strong>SAGES</strong> thanks the <strong>SAGES</strong> Foundation for their support of this award.<br />
Name: Sarah Evans, MD<br />
Institution: Duke University<br />
Title: Gastric Bypass Surgery Alters the Secretion of the Anorexogenic<br />
Gut-Derived Hormones Glucagon-like Peptide-1 and Peptide YY<br />
Supported by Covidien<br />
Name: Toshitaka Hoppo, MD<br />
Institution: The Heart, Lung and Esophageal Surgery Institute<br />
Title: Prevention of Stricture Formation Following Subtotal Endoscopic<br />
Mucosal Sleeve Resection in the Swine Model<br />
Supported by Covidien<br />
Name: Kyle Perry, MD<br />
Institution: The Ohio State University<br />
Title: Identifying the Optimal Duration of Gastric Ischemic<br />
Conditioning to Improve Gastroesophageal Anastomotic<br />
Wound Healing<br />
Supported by Covidien<br />
Name: Corey Deeken, MD<br />
Institution: Washington University School of Medicine<br />
Title: Fixation of Biologic Mesh at the Hiatus with Fibrin or<br />
Polyethylene Glycol (PEG) Sealeant in a Porcine Model<br />
Supported by Ethicon Endo-Surgery<br />
Name: Karem Harth, MD<br />
Institution: University Hospitals Case Medical Center<br />
Title: Tension Free Ventral Hernia Repair: Is This the Wrong Operation?<br />
Supported by Ethicon Endo-Surgery<br />
Name: Brian Dunkin, MD<br />
Institution: The Methodist Hospital<br />
Title: A Pilot Study to Determine the Risk of Graft Contamination<br />
Following Transvaginal Extraction of the Kidney During<br />
Laparoscopic Living Donor Nephrectomy<br />
Supported by Karl Storz Endoscopy<br />
Name: Liane Feldman, MD<br />
Institution: McGill University Health Centre<br />
Title: Mastery Versus Standard Proficiency Laparoscopic Technical<br />
Skills Training: A Randomized Controlled Trial<br />
Supported by <strong>SAGES</strong> Foundation<br />
Name: Eric Hungness, MD<br />
Institution: Northwestern University Department of Surgery<br />
Title: Laparoscopic Common Bile Duct Exploration: Simulator<br />
Development<br />
Supported by <strong>SAGES</strong> Foundation<br />
Name: William Richards, MD<br />
Institution: University of South Alabama<br />
Title: Downregulation of G6PD Activity is a Mechanism of Action of<br />
Improvement of Type II Diabetes after Bariatric Surgery<br />
Supported by <strong>SAGES</strong> Foundation<br />
12 th World Congress of Endoscopic Surgery<br />
Honoring Gerald Marks on his 85th Birthday<br />
He started it all and is considered the father of <strong>SAGES</strong>. Gerry Marks was and is a man of vision, tenacity and audacity.<br />
He created the formula for <strong>SAGES</strong> success and lived by it. <strong>SAGES</strong> would have a strong founding leadership that would<br />
rotate so that no one personality would dominate the organization. The organization would cultivate young cutting<br />
edge surgeons and give them a seat at the table. The organization had the word “American” in its name but would<br />
begin and continue to be an international society. <strong>SAGES</strong> would lead in education and research and become a force<br />
to be reckoned with. He stepped back as president after a few years. He stayed on to serve in many other capacities<br />
including as an editor of <strong>SAGES</strong> Journal, our representative to the ACS Board of Governors and as a member of the<br />
<strong>SAGES</strong> Foundation board. He was instrumental in organizing the International Federation of Societies Endoscopic<br />
Surgeons and was its founding president. He is still a voice for visionary thought. He still has a warm smile, quick wit and dreams for better<br />
endoscopic surgery.<br />
Why are we telling you this? Gerry Marks is about to celebrate his 85th Birthday. Who could believe it!? Still sporting a bounce in his step, a<br />
gleam in his eye and looking like he stepped off the cover of GQ, Gerry is still the quintessential surgeon’s surgeon.<br />
To celebrate 85 years of surgical splendor, please honor Gerald Marks and his work for <strong>SAGES</strong> by making a contribution in his<br />
honor to the <strong>SAGES</strong> Education and Research Foundation. You may donate on line at www.sagesfoundation.org or stop by the<br />
Foundation Donor Lounge or <strong>SAGES</strong> membership booth to fill out your commemorative donation form.<br />
Gerry, we love you. Happy Birthday!<br />
21 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Wednesday, April 14, <strong>2010</strong><br />
<strong>2010</strong> <strong>SAGES</strong> Young Researcher Award Winner<br />
Presented by: Aurora Pryor, MD, Research Committee Chair & representative from Olympus<br />
Recipient: Vivian Strong, MD<br />
The Young Researcher Award is given to a <strong>SAGES</strong> Candidate or Active member in a residency program, fellowship or<br />
within 5 years of training, who has demonstrated an interest and ability in research.<br />
Vivian Stong, this year’s Young Researcher recipient, is Assistant Professor of Surgery, Weill Medical College of Cornell<br />
University, New York, NY and Assistant Attending Surgeon, Memorial Sloan-Kettering Cancer Center, New York, NY.<br />
Dr. Strong has a research profile that is both broad and deep. She began performing research projects while still in<br />
secondary school. During her residency she spent time completing productive basic science research related to<br />
oncology. Following her fellowship in minimally invasive surgery, she was recruited to join the faculty at Memorial Sloan-Kettering Cancer<br />
Center. There she has distinguished herself by bringing minimally invasive surgery to cancer patients who formerly rarely had that option,<br />
and then studying the effect of minimally invasive surgery in that setting. She has developed new technology for using a beta probe to<br />
identify tumor sites intraoperatively during either open or laparoscopic surgery using PET scanning technology (including a <strong>SAGES</strong> grant<br />
to study this). She has also focused on minimally invasive treatment of gastric cancer and has recently published a significant series of<br />
oncologically sound minimally invasive gastric resections. She has developed collaboration with Asian surgeons to further the development<br />
of better minimally invasive techniques for treating gastric cancer. Her research is a well-rounded body of work including basic science,<br />
education, and development and assessment of better clinical techniques for cancer patients.<br />
<strong>SAGES</strong> gratefully acknowledges Olympus for their support of the Young Researcher Award.<br />
<strong>2010</strong> <strong>SAGES</strong> Researcher in Training Award Winner<br />
Presented by: Aurora Pryor, MD, Research Committee Chair<br />
Recipient: Erica Moran, MD<br />
The Researcher in Training Award is new this year, given to a <strong>SAGES</strong> Candidate member in a residency program or<br />
fellowship, who shows great promise for a career in academic GI/endoscopic practice or potential for significant<br />
contributions to the advancement of minimally invasive or endoscopic surgery.<br />
Erica Moran is a General Surgery Resident (PGY4) that has been active in an interdisciplinary research laboratory from<br />
January 2008 until December 2009. During that time, she completed the Clinician Investigator Training <strong>Program</strong> at the<br />
Mayo Medical Foundation. She has conducted research projects in three different units of the Mayo Medical School. The<br />
research involves the randomized comparisons of laparoscopic and transluminal procedures as well as new applications<br />
of endoscopic tools. During her laboratory experience, she was instrumental in securing three extramural research grants as the primary<br />
investigator. She had participated in close to ten different experimental studies. In addition, she has presented the data that she collected at<br />
regional, national (including <strong>SAGES</strong>), and international meetings. Her outstanding work has been recognized at the Balfour Surgical Society<br />
meeting, where she was awarded the Resident Best Paper Award as well as the Minnesota Surgical Society Best Paper Presentation Award, for<br />
her excellent presentations.<br />
She has given six oral presentations, presented 16 posters and authored 6 original articles<br />
Her current research projects include: “Feasibility of translumenal endoscopic omental patch closure of perforated viscus”—Clinical Trial; as<br />
well as: “Feasibility of transvaginal cholecystectomy “—Clinical Trial.<br />
<strong>2010</strong> <strong>SAGES</strong> IRCAD Fellowship Award Winner<br />
Presented by: Lee Swanstrom, MD, Awards Committee Chair & representative from Karl Storz Endoscopy<br />
Recipient: Basil Yurcisin, MD<br />
The <strong>SAGES</strong> IRCAD Traveling Fellowship Award is available to a <strong>SAGES</strong> Candidate member who is enrolled in a Fellowship<br />
Council recognized program.<br />
Dr. Yurcisin first stepped onto the <strong>SAGES</strong> horizon when he worked in the <strong>SAGES</strong> Learning Center as a second year clinical<br />
resident. He is now in the second and clinical year of a two-year fellowship in Minimally Invasive and Bariatric Surgery at<br />
Duke University Medical Center. In his fellowship he has exposure to a wide range of minimally invasive surgical as well<br />
as some endoscopic procedures. He believes that the future of surgery lies within minimally invasive surgery. His work to<br />
date is extraordinary and there is no doubt he will benefit from his fellowship at IRCAD.<br />
Dr. Yurcisin did his residency training at the University of Pittsburgh Medical Center Mercy Hospital, Pittsburgh, PA. He earned his MD at<br />
Southern Illinois University School of Medicine, Springfield, IL.<br />
He has to date served as faculty for the 2006, 2007 and 2008 <strong>SAGES</strong> Learning Centers and was a recipient of the Resident Achievement Award<br />
- Society of Laparoendoscopic Surgeons, University of Pittsburgh Medical Center Mercy Hospital, June 2005 & 2007. He has already given 5<br />
presentations, written 7 peer reviewed papers and published one book chapter.<br />
<strong>SAGES</strong> gratefully acknowledges Karl Storz Endoscopy for their support of the IRCAD Fellowship Award.<br />
12 th World Congress of Endoscopic Surgery 22
12 th World Congress of Endoscopic Surgery<br />
Wednesday, April 14, <strong>2010</strong><br />
<strong>2010</strong> <strong>SAGES</strong> Excellence in Clinical Care Award Winner<br />
Presented by: Lee Swanstrom, MD, Awards Committee Chair<br />
Recipient: Paul Hansen, MD<br />
The Excellence in Clinical Care Award, new this year, is designated for a clinician who is recognized by the surgical/<br />
GI community for excellence in patient care and surgical practice, and has significant surgical/endoscopic skills, and<br />
contributions to the community and/or volunteerism.<br />
Paul Hansen is Clinical Associate Professor of Surgery, Oregon Health Sciences University and Director, Hepatobiliary<br />
<strong>Program</strong>, Providence Portland Medical Center. He also serves as <strong>Program</strong> Director, HPB postgraduate fellowship program,<br />
Providence Portland Medical Center. Dr. Hansen is Triple Fellowship trained and has been active in <strong>SAGES</strong> since he was<br />
a resident. He helped to pioneer minimally invasive approaches to liver and pancreatic cancers and has done original<br />
research on technology and approaches for liver tumor ablation (RFA).<br />
Paul Hansen was a leader in laparoscopic liver resections and has advanced research in Laparoscopic assisted liver chemotheratpy, including<br />
Laparoscopic chemotherapy pump placement, Laparoscopic assisted chemo-embolization. His work in robotic assisted laparoscopic<br />
Whipple procedure is well known.<br />
He was the driving force is the creation of a regional “center of excellence” for pancreatic and liver cancer and established one of the<br />
few postgraduate fellowships in hepatobiliary/pancreatic surgery. His educational efforts have included local MIS resident, nursing and<br />
community surgeon courses, national MIS courses as well as having developed and run an annual surgery day for local school children to<br />
come and tour operating rooms and practice laparoscopic surgery in his training lab.<br />
He annually volunteers for overseas medical missions: Pakistan, Guatemala, Vietnam, Cambodia, and elsewhere. He is an example of the fully<br />
realized surgeon: dedicated family man, brilliant clinician, productive researcher, constant teacher and selfless volunteer. He continues to<br />
push the frontiers of therapy in quest of better care of his patients. He is the paragon for clinical excellence.<br />
<strong>2010</strong> Jeffrey L. Ponsky Master Educator in Endoscopy Award – A <strong>SAGES</strong> Foundation Award<br />
Presented by: David Duppler, MD & Jeffrey Marks, MD<br />
Recipient: Carol Scott-Conner, MD<br />
Carol Scott-Conner, MD, PhD, MBA, has been selected to receive the Jeffrey L. Ponsky Master Educator in Endoscopy<br />
Award. The Ponsky Flexible Endoscopy Research Fund was established by the <strong>SAGES</strong> Foundation in 2007 as a tribute<br />
to Dr. Jeffrey Ponsky for his outstanding contributions to endoscopy and surgical education. The Master Educator<br />
award recognizes a distinguished <strong>SAGES</strong> leader who exemplifies Dr. Ponsky’s visionary leadership and his dedication to<br />
teaching of surgical endoscopy.<br />
Dr. Scott-Conner’s lifelong commitment to education and research, and her trailblazing achievements as a scholar and<br />
surgeon, embody the qualities that define compassionate greatness. As Chair of Surgery at University of Iowa College<br />
of Medicine from 1995 through 2004, she was only the second woman to lead a surgery department at an academic medical center. She<br />
currently serves as Professor of Surgery at the University of Iowa’s Roy J. and Lucille A. Carver College of Medicine.<br />
Carol Scott-Conner has enriched the world as a mentor and many of us have been impacted by her teachings and by volumes of seminal<br />
writings, including eight medical textbooks that have been translated into at least five languages.<br />
Since joining <strong>SAGES</strong> in 1984, she has served as Vice-President, a member of the <strong>SAGES</strong> Board of Governors, Chair of the Research Grants<br />
Committee, and has made an invaluable contribution as a key figure in the development and growth of the organization. She edited the first<br />
<strong>SAGES</strong> manual and two subsequent volumes, Herculean tasks, all. We are in her debt as our teacher.<br />
<strong>2010</strong> Gerald Marks Rectal Cancer Award – A <strong>SAGES</strong> Foundation Award<br />
Presented by: Gerald Marks, MD & Bruce Schirmer, MD<br />
Recipient: Bastiaan Klarenbeek, MD<br />
The Gerald Marks Rectal Cancer award is selected from each year’s submitted abstracts. This award is chosen from the<br />
hundreds of abstracts submitted by a special committee of reviewers and given to one individual each year in honor of<br />
Dr. Gerald Marks, <strong>SAGES</strong> first President and Founder.<br />
12 th World Congress of Endoscopic Surgery 24
Wednesday, April 14, <strong>2010</strong><br />
<strong>2010</strong> <strong>SAGES</strong> Distinguished Service Award Winner<br />
Presented by: Lee Swanstrom, MD, Awards Committee Chair<br />
Recipient: Nathaniel Soper, MD<br />
Nat Soper clearly did not have a mentor or parent who told him “don’t volunteer.” Or he did not get the message. Dr.<br />
Soper was President of <strong>SAGES</strong> from April 2000-2001. He served on the Board of Governors from 1993 to present and<br />
is currently <strong>SAGES</strong> representative to the American College of Surgeons Board of Governors. His work as one of the<br />
founding fathers of FLS and as its project chair for several years (including currently) has made him one of the major<br />
forces of surgical education in this country and the world. Along the way he has served on the Development, Continuing<br />
Education, <strong>Program</strong> and Publications Committees. He was the Poster Chairman of the 1993 and 1994 annual scientific<br />
sessions, Postgraduate Course Director of the 1998 meeting, and was the <strong>Program</strong> Chairman of the 1999 meeting. He is<br />
on the Editorial Board of eight journals, and his publications include more than 200 manuscripts and book chapters. He was among the first<br />
academic American surgeons to perform laparoscopic surgery and has been involved in its maturation and development over the ensuing<br />
years.<br />
He has distinguished himself by the service he has given to <strong>SAGES</strong> and the surgical community. He has done it with good humor (sometimes<br />
a challenge), great patience, common sense and refreshing humility.<br />
<strong>2010</strong> Berci Lifetime Achievement Award Winner<br />
Presented by: Lee Swanstrom, MD, Awards Committee Chair<br />
Recipient: Jacques Marescaux, MD<br />
If you don’t know who Jacques Marescaux is, you are simply not paying attention. Since his early presentations in the<br />
mid 1990’s related to laparoscopic surgery he has contributed an enormous amount to the surgical body of knowledge<br />
and shared that knowledge with literally thousands of surgeons. His world renowned training facility in Strasborg,<br />
IRCAD, has set the bar for training and the dissemination of clinical training in the world of minimal access surgery.<br />
IRCAD was founded in 1994 and has run courses covering a wide variety of subjects. These courses attract world class<br />
faculty to provide high content didactic teaching in addition to one of the finest animal laboratories ever established. Dr.<br />
Marescaux gave the Karl Storz Keynote Lecture in New Technology at the <strong>SAGES</strong> 2001 Meeting in St. Louis.<br />
There is no doubt that Dr. Marescaux is one of the world leaders in terms of innovation in minimally invasive surgery and surgical education.<br />
His vision and success in creating a world leading center for internet based surgical education is unmatched. The website that he created,<br />
WebSurg is the #1 source of information for people looking on the internet for educational content about minimally invasive surgery. Many<br />
such ventures have come and gone, but WebSurg has not only survived the shake out in a dot com industry, but became the world leader in<br />
this area. Every surgical resident knows about this website and most use it.<br />
12 th World Congress of Endoscopic Surgery<br />
World Congress Corporate Supporters<br />
Diamond Donors<br />
COVIDIEN<br />
ETHICON ENDO-SURGERY, INC.<br />
<strong>SAGES</strong> EDUCATION AND RESEARCH FOUNDATION<br />
PLATINUM DONORS<br />
KARL STORZ ENDOSCOPY-AMERICA<br />
OLYMPUS<br />
GOLD DONORS<br />
ASCENT HEALTHCARE SOLUTIONS<br />
STRYKER ENDOSCOPY<br />
SILVER DONORS<br />
BOSTON SCIENTIFIC DAVOL, INC., A BARD COMPANY GORE & ASSOCIATES<br />
BRONZE Donors<br />
SYNOVIS SURGICAL INNOVATIONS<br />
25 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Notes<br />
12 th World Congress of Endoscopic Surgery 26
Wednesday, April 14, <strong>2010</strong><br />
1:00 PM - 5:00 PM *Separate Registration Fee<br />
Hands-on Advanced Suturing and Anastomotic Techniques Lab<br />
Chair: Kelvin D. Higa, M.D.; Co-Chair: Aureo L. De Paula, M.D.<br />
location: Maryland Ballroom B-D<br />
Description:<br />
Laparoscopic suturing skills allow smooth transition from basic to advanced surgery. In this lab, world-recognized experts in advanced<br />
suturing and anastomotic techniques will provide direct, hands-on training to take your suturing skills to the next level. If you want to take<br />
your skills from advanced to expert, this is an opportunity you don’t want to miss.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• Become familiar with advanced suturing techniques: tissue approximation, knot tying, anastomoses.<br />
• Understand the advantages and disadvantages of intracorporal sutures.<br />
• Adopt the principles for continued efficiency and skill.<br />
• Apply these techniques to common surgical problems encountered<br />
Schedule<br />
1:00 PM Introduction – Overview of Tools and Suture Material Kelvin D. Higa, M.D. & Aureo L. De Paula, M.D.<br />
1:15 PM Principles of Efficient Laparoscopic Suturing Kelvin D. Higa, M.D.<br />
1:30 PM How to Tie a Knot Aureo L. De Paula, M.D.<br />
1:45 PM Specific Applications: Anastomoses, Internal Hernia Closure, Staple-Line Reinforcement Aureo L. De Paula, M.D.<br />
2:00 PM Lab Instructions Kelvin D. Higa, M.D. & Aureo L. DePaula, M.D.<br />
2:05 PM Hands-On Lab<br />
Lab Instructors:<br />
Jose Ribamar Azevedo, M.D.<br />
Daniel Birch, M.D.<br />
Elias Chousleb, M.D.<br />
Pradeep Chowbey, M.D.<br />
Edward Felix, M.D.<br />
Kazunori Kasama, M.D.<br />
Nilton Kawahara, M.D.<br />
Marina Kurian, M.D.<br />
Adam Meneghetti, M.D.<br />
Chinnasamy Palenivelu, M.D.<br />
Paresh Shah, M.D.<br />
Surendra Ugale, M.D.<br />
Tony Vine, M.D.<br />
12 th World Congress of Endoscopic Surgery<br />
<strong>SAGES</strong> acknowledges contributions in-kind in support of this World Congress course from:<br />
Covidien, Ethicon Endo-Surgery, Inc., Karl Storz Endoscopy-America, Olympus and Stryker Endoscopy.<br />
Evaluation & CME Credit Claim<br />
Visit the kiosks next to registration to complete<br />
your online evaluation and CME credit form on-site.<br />
Attendees may print CME certificates two weeks<br />
after the conclusion of the meeting.<br />
The programs and lectures presented at the <strong>2010</strong> World<br />
Congress Meeting are copyrighted products of the Society<br />
of American Gastrointestinal and Endoscopic Surgeons.<br />
Any reproduction or rebroadcasting without the express<br />
written consent of <strong>SAGES</strong> is strictly prohibited.<br />
Pencil us in for next year:<br />
CAGS Canadian Surgery Forum<br />
September 2 - 5, <strong>2010</strong>, Québec City Convention Centre, Canada<br />
<strong>SAGES</strong> Scientific Session & Postgraduate Course<br />
March 30 - April 2, 2011, San Antonio, Texas<br />
27 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Wednesday, April 14, <strong>2010</strong><br />
1:00 PM - 5:00 PM *Included in Registration SuperPass (Option A) or Registration Option B<br />
Pediatrics Session:<br />
Next-Generation Pediatric MAS – A Move Toward “Scarless” Surgery<br />
Chairs: Sanjeev Dutta, M.D. and Jacob Langer, M.D.<br />
location: Potomac Ballroom C<br />
Pediatric minimal access surgery (MAS) has grown to encompass virtually every pediatric surgical condition, including even complex<br />
neonatal anomalies. This has enabled faster recovery and less pain, with smaller scars. The next wave of innovation in pediatric MAS<br />
involves further minimizing incisions, transferring them to inconspicuous sites, or avoiding them altogether. Termed “stealth surgery” in the<br />
pediatric surgical community, the intent is to perform complex procedures without leaving evidence they occurred, and thereby address the<br />
psychological consequences that surgical scars can have on children.<br />
Objectives:<br />
At the conclusion of this session, participants will have a better understanding of current cutting edge minimal access procedures in<br />
pediatric surgery. They will be able to:<br />
• Describe the current experience, instruments, and operative techniques relevant to performing transaxillary subcutaneous endoscopic<br />
surgery including benign lesions of the neck and chest, as well as thyroid and parathyroid lesions.<br />
• Describe the current experience, instruments, and operative techniques relevant to pediatric single incision laparoscopic surgery<br />
including appendectomy, cholecystectomy, splenectomy, and neonatal procedures.<br />
• Describe current experience, instruments, and operative techniques relevant to endolumenal therapies in children including antireflux<br />
procedures and gastroduodenal lesions.<br />
• Describe future potential MAS therapies in children such as natural orifice translumenal endoscopic surgery (NOTES®).<br />
Schedule<br />
1:00 PM Introduction Sanjeev Dutta, M.D.<br />
1:05 PM Transaxillary Subcutaneous Endoscopic Surgery Moderator: Sanjeev Dutta, M.D.<br />
Transaxillary excision of Benign Neck and Truncal Lesions<br />
Sanjeev Dutta, M.D.<br />
1:20 PM Transaxillary Excision of the Thyroid and Parathyroids Thom Lobe, M.D.<br />
1:35 PM Discussion<br />
1:45 PM Single Incision Laparoscopic Surgery Moderator: Jacob Langer, MD<br />
Transumbilical Non-Laparoscopic Surgery in the Neonate<br />
Jacob Langer, M.D.<br />
2:00 PM Overview of Single Incision Surgery Tool Box and Technique Jeff Ponsky, M.D.<br />
2:15 PM Single Incision Surgery Splenectomy and Cholecystectomy Sanjeev Dutta, M.D.<br />
2:30 PM Neonatal Single Incision Surgery Carroll “Mac” Harmon, M.D.<br />
2:45 PM Discussion<br />
2:55 PM 10 min BREAK<br />
3:05 PM Endolumenal Surgery and NOTES® Moderator: Timothy Kane, M.D.<br />
3:10 PM Endolumenal to Translumenal: The Prospect of NOTES® in Children Lee Swanstrom, M.D.<br />
3:25 PM Endolumenal Therapy for GERD in Children –<br />
Early Experience with Transoral Incisionless Fundoplication<br />
Michael Thomson, M.D.<br />
3:35 PM GERD in Children – A Surgical Perspective Steven S. Rothenberg, M.D.<br />
3:40 PM Endolumenal Therapy for Pancreatic and Gastroduodenal Lesions Timothy Kane, M.D.<br />
3:55 PM Discussion<br />
Video Session<br />
Moderators: Panel<br />
4:05 PM Video – Thyroid Matias Bruzoni, M.D.<br />
4:15 PM Video – Gall bladder Single Incision Surgery Katherine Barsness, M.D.<br />
4:25 PM Video – Spleen-Single Incision Surgery Zachary Kastenberg, M.D.<br />
4:35 PM Video – Endoscopic-assisted Esophagectomy Jose Prince, M.D.<br />
4:45 PM Video – Single Incision Surgery Pyloromyotomy Erik Hansen, M.D.<br />
4:55 PM Closing Remarks Jacob Langer, M.D<br />
Please join us for the<br />
World Congress Welcome Exhibit Opening Reception<br />
5:00 PM - 7:00 PM<br />
World Congress exhibits will take place at the Gaylord Convention Center in<br />
the Prince George’s Exhibit Hall A-C. The Learning Center and Posters will NOT<br />
be open until Thursday.<br />
13 th World Congress of Endoscopic Surgery leaders will be introduced.<br />
12 th World Congress of Endoscopic Surgery 28
<strong>SAGES</strong><br />
2011<br />
Scientific Session &<br />
Postgraduate Course<br />
<strong>Program</strong> Chair:<br />
Brian Dunkin, MD<br />
March 30 - April 2, 2011<br />
San Antonio Convention Center<br />
San Antonio, TX<br />
www.sages.org<br />
Registration & program information will be available Fall, <strong>2010</strong>
Thursday, April 15, <strong>2010</strong><br />
Time Session Location<br />
6:00 AM - 7:15 AM<br />
7:30 AM - 11:30 AM<br />
Industry Satellite Symposia<br />
Covidien – “Advances in SILS Technology,<br />
Technique and Evidence”<br />
Postgraduate Surgeon in the Digital Age:<br />
Video Editing Course – Basic Video Editing<br />
with an Introduction to Advanced Techniques<br />
Potomac Ballroom D<br />
Chesapeake Conference Rooms D-E<br />
7:30 AM - 11:30 AM Avoid Pitfalls in Cholecystectomy and CBD Exploration Potomac Ballroom B<br />
7:30 AM - 11:30 AM Challenging Hernias Postgraduate Course Potomac Ballroom A<br />
7:30 AM - 12:00 PM Fundamentals of Laparoscopic Surgery Hands-on Course<br />
Lectures – Maryland Ballroom C<br />
Lab – Maryland Ballroom A<br />
9:30 AM - 11:30 AM SS01 Best of Videos 1 Potomac Ballroom C<br />
10:00 AM - 2:30 PM World Congress Exhibits, Posters & Learning Center Open Prince George’s Exhibit Hall A-C<br />
11:30 AM - 1:00 PM BREAK: Exhibits, Posters, Learning Center<br />
11:30 AM - 1:30 PM<br />
Educators Luncheon:<br />
Utilizing <strong>SAGES</strong> Educational Offerings for Residents<br />
Potomac Ballroom D<br />
11:30 AM - 1:30 PM<br />
Device Development Luncheon:<br />
From Funding to Freedom to Operate<br />
Maryland Ballroom C<br />
1:30 PM - 5:00 PM<br />
Laparoscopic IBD and Colectomy Postgraduate Course:<br />
The Status and Direction of Laparoscopic Colorectal Surgery in<br />
the Treatment of Inflammatory Bowel Disease<br />
Potomac Ballroom A<br />
1:30 PM - 5:00 PM Single Port Access Surgery Hands-On Course **Offsite lab<br />
1:30 PM - 5:00 PM<br />
MBA for Surgeons Panel:<br />
Asset Management and Protection for Surgeons<br />
Potomac Ballroom C<br />
1:30 PM - 5:00 PM Hands On Endolumenal/NOTES® Lab Maryland Ballroom B-D<br />
1:30 PM - 2:30 PM Robotics Symposium: What’s New? Potomac Ballroom B<br />
2:30 PM - 4:00 PM Metabolic Surgery Symposium: Current Status Potomac Ballroom B<br />
12 th World Congress of Endoscopic Surgery<br />
4:00 PM - 5:30 PM Barrett’s Debate: How to Follow, How to Treat? Potomac Ballroom B<br />
5:30 PM - 7:30 PM Industry Satellite Symposia (No Registration Required)<br />
Boston Scientific, Inc. – “Intraluminal Stents and the Surgeon –<br />
Who, What, Where, When and Why?”<br />
Covidien – “Insights into the Future of Surgical Stapling:<br />
Integrated Materials, Tri-Staple Technology,<br />
Powered Staplers”<br />
Davol Inc., a BARD Company – “Advanced Endoscopic<br />
Techniques for Abdominal<br />
Wall Reconstruction”<br />
Ethicon Endo-Surgery, Inc. – “Minimally Invasive Surgery –<br />
Where is it Going?”<br />
Karl Storz Endoscopy – “The Great Debate: S-PORTAL<br />
(Single Portal Access) Surgery vs.<br />
Mini-Laparoscopy”<br />
Chesapeake D-E<br />
Potomac Ballroom D<br />
Maryland Ballroom C<br />
Potomac Ballroom C<br />
Maryland Ballroom A<br />
<strong>2010</strong> Poster Session<br />
Posters will be on display, Thursday, Friday & Saturday.<br />
Poster presenters will be available for Q&A on Friday, from 11:15 AM - 12:15 PM<br />
<strong>SAGES</strong> acknowledges our Diamond and Platinum Level Donors for their support of the poster session:<br />
Diamond: Covidien, Ethicon Endo-Surgery, Inc. and <strong>SAGES</strong> Education and Research Foundation<br />
Platinum: Karl Storz Endoscopy, Olympus<br />
To fully comply with ACCME regulations, all World Congress attendees must have their badge scanned<br />
before entering any course or session room in order to receive CME credit for that event.<br />
31 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Thursday, April 15, <strong>2010</strong><br />
6:00 AM - 7:15 AM Free for any World Congress Attendee<br />
Industry Satellite Symposia These events are not planned nor accredited for CME by <strong>SAGES</strong>.<br />
Industry presentations will take place on Thursday morning, immediately prior to Congress sessions.<br />
Registration is FREE for any World Congress attendee.<br />
Covidien - “Advances in SILS Technology, Technique and Evidence”<br />
Location: Potomac Ballroom D<br />
Presenters: Jerry Stirman, MD<br />
Paul Enochs, MD<br />
Shawn Garber, MD, FACS<br />
This is a non-CME activity presented and supported by Covidien.<br />
7:30 AM - 11:30 AM *Separate registration fee<br />
Postgraduate Surgeon in the Digital Age: Video Editing Course<br />
Basic Video Editing with an Introduction to Advanced Techniques<br />
Chair: Dmitry Oleynikov, M.D.; Co-Chair: John Romanelli, M.D.<br />
location: Chesapeake Conference Rooms D-E<br />
This course is a hands-on (1 to a station) PC-based course and workshop using the latest video editing software. This course is designed<br />
to take users through the basic steps of digital video editing. The skills learned in this course will be applicable to digital video editing on<br />
most Widows-based computers and editing programs. Led in real time by an experienced surgeon facilitator, participants will import clips,<br />
edit them, create transitions and add voice-over sound tracks. Additional advanced techniques which are useful in medical videos will be<br />
reviewed. <strong>Final</strong> products will be transcoded for a variety of purposes. A CD with the course files is included for later practice. Once this course is<br />
completed, users should be able to have the skills necessary to create edited digital videos for medical meetings, education or personal use.<br />
Objectives:<br />
At the completion of this course the surgeon (or other participant) will be able to:<br />
• Demonstrate a working knowledge as to how the video signal used to perform laparoscopic surgical procedures is transferred to a variety<br />
of digital formats (e.g. – CD, DVD, digital tape) for the purposes of creating materials that could be used for:<br />
– Electronic medical records<br />
– Formal presentation at medical meeting<br />
– Patient education<br />
– Website presentation for patient or physician education<br />
– Archival needs<br />
• Manipulate the acquired digitized video material for the purposes above by methods utilizing the following skills in order to create<br />
effective medical educational materials:<br />
– Editing<br />
– Titling<br />
– Transitions<br />
– Annotation with audio<br />
– Addition of still photography<br />
– Selected special effects<br />
• Produce output of the acquired and manipulated digital material for specific needs in the medical educational arena including:<br />
– Videotape<br />
– CD-ROM<br />
– Web-based media files<br />
– DVD<br />
Schedule<br />
7:30 AM The Operation<br />
7:40 AM Image acquisition from different devices<br />
7:50 AM Getting video footage onto the computer<br />
8:15 AM Break<br />
8:30 AM Editing<br />
8:45 AM Editing Clips in the Timeline<br />
9:30 AM Transitions<br />
10:15 AM Outputting Your Project<br />
10:30 AM Internet Publishing and Podcasting<br />
11:30 AM Conclusion<br />
Faculty:<br />
Shanu Kothari, M.D.<br />
John Feng, M.D.<br />
Sergey Kantsevoy, M.D. Matthew Goede, M.D.<br />
Rhonda Prewitt, M.D.<br />
<strong>SAGES</strong> acknowledges an educational grant in support of this World Congress course from Stryker Endoscopy.<br />
12 th World Congress of Endoscopic Surgery 32
Thursday, April 15, <strong>2010</strong><br />
7:30 AM - 11:30 AM *included in Registration SuperPass (Option A) or Registration Option B<br />
Avoid Pitfalls in Cholecystectomy and CBD Exploration<br />
Chair: Michael B. Edye, M.D.; Co-Chair: Bertrand Millat, M.D.<br />
location: Potomac Ballroom B<br />
Description:<br />
The essence of surgery is to be aware of potential pitfalls in advance and to take steps that are known to avoid them. This session will build<br />
on a sound anatomic foundation for laparoscopic cholecystectomy and common duct exploration. Practical recommendations for safe<br />
techniques that work in straightforward and complicated settings, and a final syntehsis will provide a basis for best practice.<br />
Objectives: At the conclusion of this session, participants will be able to:<br />
• Describe common anatomic anomalies of the biliary tree that can complicate laparoscopic cholecystectomy and strategies to avoid these<br />
complications<br />
• Recognize how new surgical approaches to cholecystectomy can increase the risk of bile duct injury and devise methods to prevent these<br />
injuries in their subsequent practice<br />
• Approach complicated presentations of cholecystitis with great confidence<br />
• Review their current approach to common duct stones and recognize the benefits and difficulties of surgical versus endoscopic bile duct clearance<br />
Schedule<br />
7:30 AM Introduction Michael B. Edye, M.D. & Bertrand Millat, M.D.<br />
7:35 AM Anatomic Pitfalls of Cholecystectomy and CBD Exploration Brice Gayet, M.D.<br />
7:50 AM Lessons from a High Volume Laparoscopic Biliary Surgeon Surendra Ugale, M.D.<br />
8:05 AM Rationale for Cholangiography William Traverso, M.D.<br />
8:20 AM Operative Bile Duct Clearance vs. Preoperative ERCP:<br />
other Combined Approaches to Duct Clearance<br />
Augusto Tinoco, M.D.<br />
8:40 AM Pitfalls of T-Tubes and Other Biliary Drains, and the Place of Primary Duct Closure Ian Martin, M.D.<br />
9:00 AM Discussion<br />
9:20 AM Break<br />
9:40 AM Cholecystectomy in Chirrhotics: If, When and How? Luis Burbano, M.D.<br />
9:50 AM Acute Cholecystitis: Tricks to Success, When to Convert and When to Start Open Bertrand Millat, M.D.<br />
10:05 AM Single Port Cholecystectomy: Umbilical Anatomic Techniques and Devices Paul G. Curcillo, M.D.<br />
10:20 AM “SKIN” Cholecystectomy (Skinny Instrument i.e. 2-3 mm): The Forgotten Alternatives to NOTES® Michael B. Edye, M.D.<br />
10:35 AM Synthesis of Recommendations Michael B. Edye, M.D. & Bertrand Millat, M.D.<br />
10:50 AM Discussion<br />
7:30 AM - 11:30 AM *included in Registration SuperPass (Option A) or Registration Option B<br />
Challenging Hernias Postgraduate Course<br />
Chair: Kristi L. Harold M.D.; Co-Chair: Shirin Towfigh, M.D.<br />
location: Potomac Ballroom A<br />
Hernia repair remains one of the most common surgical procedures performed around the world. Despite many standardized techniques<br />
new procedures, instruments, and biomaterials continue to emerge to address the problem of challenging hernias. Surgeons attending<br />
<strong>SAGES</strong> will benefit from this half-day course which will utilize evidence- based medicine to cover a wide variety of topics surrounding<br />
challenging hernias and the modern approaches to their repair.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• Discuss uses and shortcomings for various types of synthetic and biological meshes<br />
• Recognize the role of bariatric operations in hernia patients<br />
• Distinguish patients who may benefit from a combined approach by general and plastic surgery for hernia repair<br />
• Formulate a tailored approach to patients with sports hernias<br />
Schedule<br />
7:30 AM Introduction Kristi L. Harold, M.D. & Shrin Towfigh, M.D.<br />
7:35 AM Parastomal Hernia Repair – Best Techniques Kristi Harold, M.D.<br />
7:50 AM Loss of Domain – Definition and Management Michael Rosen, M.D.<br />
8:05 AM Biological Meshes – Indications and Shortcomings Gina Adrales, M.D.<br />
8:20 AM Discussion<br />
8:30 AM What are we doing to predict and prevent hernias? B. Todd Heniford, M.D.<br />
8:45 AM Hernias in Difficult Locations: Flank, Supra-pubic, Sub-xyphoid Alfredo Carbonell, D.O.<br />
9:00 AM LVHR: Dealing with Complications Pradeep Chowbey, M.D.<br />
9:15 AM Discussion<br />
9:25 AM BREAK<br />
9:40 AM Biological Mesh for Paraesophageal Hernia Repair – Pros & Cons Steven P. Bowers, M.D.<br />
9:55 AM Is There a Role for Synthetic Mesh in an Infected Field? Shirin Towfigh, M.D.<br />
10:10 AM Options in the Management of Infected Abdominal Wall Mesh Brent Matthews, M.D.<br />
10:25 AM Discussion<br />
10:35 AM Ventral Hernia in the Morbidly Obese Patient – Timing of Repair /<br />
role of Weight Loss Surgery / Hernia During Weight Loss Surgery<br />
Yuri Novitsky, M.D.<br />
10:50 AM Chronic Pain Following Inguinal Hernia Repair TBA<br />
11:05 AM Best Approach to Recurrent Inguinal Hernia Abe Fingerhut, M.D.<br />
11:20 AM Discussion<br />
<strong>SAGES</strong> acknowledges educational grants in support of this World Congress course from: Covidien and Gore & Associates.<br />
33 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
Thursday, April 15, <strong>2010</strong><br />
7:30 AM - 12:00 PM *Separate Registration Fee<br />
Fundamentals of Laparoscopic Surgery Hands-on Course<br />
Chair: Gerald M. Fried, M.D.; Co-Chair: E. Matthew Ritter, M.D.<br />
location: Lectures – Maryland Ballroom C<br />
lab – Maryland Ballroom A<br />
The course will be based on the Fundamentals of Laparoscopic Surgery (FLS) <strong>Program</strong>, a collaborative effort between Society of American<br />
Gastrointestinal and Endoscopic Surgeons and the American College of Surgeons. This introductory course will begin with an overview<br />
of the history, science, and development of the FLS <strong>Program</strong>. It will continue with various chapters from the FLS curriculum, such as<br />
physiology, intraoperative considerations, basic laparoscopic procedures, and procedural complications. Part of the course will also cover<br />
the psychomotor and technical skills required in basic laparoscopic surgery. The course syllabus will outline the contents of the FLS online<br />
didactic curriculum.<br />
All course participants will receive online access to the FLS didactic curriculum and will be expected to review the materials prior to the<br />
course. The hands-on component will utilize a ratio of 3:1 participants to FLS trainer boxes and faculty for mentored skills practice.<br />
After completing the course, participants will be able to schedule an appointment to take the FLS exam (written and practical). The test fee<br />
is included in the course registration, although the test is optional. There will be testing appointments available starting directly after the<br />
course and throughout the <strong>SAGES</strong> meeting. Participants may also opt to take the FLS exam at an upcoming ACS Clinical Congress or <strong>SAGES</strong><br />
Annual Meeting or one of over 40 FLS Test Centers.<br />
Objectives:<br />
At the conclusion of this session participants will be able to:<br />
• Discuss the important preoperative considerations when faced with a patient requiring laparoscopic surgery.<br />
• List the key intraoperative considerations during laparoscopic operations.<br />
• Discuss the important concepts in postoperative care of patients undergoing laparoscopic surgery.<br />
Schedule<br />
7:30 AM Introduction and Rationale for FLS Lee L. Swanstrom, M.D.<br />
7:45 AM Preoperative Considerations Ashley Vernon, M.D.<br />
8:05 AM Intraoperative Considerations E. Matthew Ritter, M.D.<br />
8:25 AM Basic Laparoscopic Procedures Shawn T. Tsuda, M.D.<br />
8:45 AM Postoperative Considerations Melina C. Vassiliou, M.D.<br />
9:05 AM Technical Skills: Development of FLS Curriculum,<br />
Validation of Metrics, and Relationship to Operative Performance<br />
Gerald M. Fried, M.D.<br />
9:30 AM Implementing FLS: The Experience in the U.S. Department of Defense E. Matthew Ritter, M.D.<br />
9:50 AM Implementing FLS: The Experience of the Royal Australasian College of Surgeons Gerald M. Fried, M.D.<br />
10:10 AM FLS: FAQs – Who, When, Where, and How? Nathaniel J. Soper, M.D.<br />
10:25 AM BREAK<br />
10:40 AM Hands-On Workshop Lee L. Swanstrom, M.D.<br />
Ashley Vernon, M.D.<br />
E. Matthew Ritter, M.D.<br />
Shawn T. Tsuda, M.D.<br />
Jonathan Pearl, M.D.<br />
Gerald M. Fried, M.D.<br />
Nathaniel J. Soper, M.D.<br />
Melina C. Vassiliou, M.D.<br />
Allan E. Okrainec, M.D.<br />
<strong>SAGES</strong> acknowledges educational grants in support of this World Congress course from Covidien, Ethicon Endo-Surgery, Inc. and Stryker Endoscopy.<br />
<strong>SAGES</strong> acknowledges contributions in-kind in support of this World Congress course from: Covidien and Karl Storz Endoscopy-America.<br />
World Congress Goes Green!<br />
In an effort to support the environment, you will see less paper for the 12th Annual World Congress.<br />
The printed <strong>Final</strong> <strong>Program</strong> will include the regular schedule and course/panel outlines, as well as<br />
oral abstracts, Poster of Distinction abstracts and poster listing. However, electronic copies of all<br />
the abstracts, digital posters, and Postgraduate course syllabi will be available on thumb drive for<br />
all attendees. The “Electronic Meeting Guide” will be completely navigational and searchable. Print<br />
kiosks will also be available throughout the Convention Center.<br />
12 th World Congress of Endoscopic Surgery 34
Thursday, April 15, <strong>2010</strong><br />
9:30 AM - 11:30 AM *included in Registration SuperPass (Option A) or Registration Option B)<br />
SS01 Best of Videos 1<br />
Moderators: Donald Selzer, MD and Fredrick Brody, Md<br />
location: Potomac Ballroom C<br />
V001 IMPROVING FUNCTIONAL ESOPHAGEAL SURGERY WITH A “SMART” BOUGIE: ENDOFLIP® Silvana Perretta, MD, Bernard<br />
Dallemagne, MD, Barry Macmahon, MD, Jacopo D’Agostino, MD, Hurng-Sheng Wu, MD, Jacques Marescaux, MD, IRCAD, University Hospital<br />
of Strasbourg, France - Show Chwan Memorial Hospital, Changhua, Taiwan<br />
V002 REPAIR OF A HIATAL DEFECT USING A ROTATIONAL FALCIFORM FLAP Erica Sutton, MD, Adrian Park, MD, University of Maryland<br />
School of Medicine<br />
V003 LAPAROSCOPIC CHOLECYSTECTOMY USING INTRAOPERATIVE FLUORESCENT CHOLANGIOGRAPHY Takeaki Ishizawa, MD PhD,<br />
Nobuhiro Harada, MD, Arata Muraoka, MD, Masayoshi Ijichi, MD PhD, Koji Kusaka, MD PhD, Masayuki Shibasaki, MD PhD, Yasutsugu Bandai,<br />
MD PhD, Norihiro Kokudo, MD PhD, Department of Surgery, Central Hospital of Social Health Insurance<br />
V004 LAPAROSCOPIC D2 LYMPH NODE DISSECTION WITH TOTAL GASTRECTOMY AND HUNT LAWRENC JEJUNAL POUCH<br />
RECONSTRUCTION FOR CARCINOMA STOMACH C Palanivelu, MCh FACS FRCS, P Senthilnathan, MS DNB FRCS, S Rajapandian, MSFRCS, V<br />
Vaithiswaran, MS MRCS, R Sathiyamurthy, MS, P Praveen Raj, MS, GEM Hospital<br />
V005 TRANSCERVICAL VIDEOSCOPIC ESOPHAGEAL DISSECTION IN MINIMALLY INVASIVE ESOPHAGECTOMY Michael Parker, MD, Jason<br />
M Pfluke, MD, Kyle K Shaddix, MD, Leslie A Dowling, BS, Timothy A Woodward, MD, Horacio J Asbun, MD, C D Smith, MD, Steven P Bowers,<br />
MD, Mayo Clinic Florida, Jacksonville, FL, USA<br />
V006 NOTES-ASSISTED TRASVAGINAL SPLENECTOMY: THE NEXT STEP FOR THE MINIMAL INVASIVE APPROACH TO THE SPLEEN EM<br />
Targarona, MD, C Gomez- Oliva, MD, R Rovira, MD, JC Pernas, MD, C Balague, MD, C Guarner-Argente, MD, S Sainz, MD, M Trias, MD, Service<br />
of Surgery, Digestive Pathology, Gynecology and Radiology. Hospital de Sant Pau, UAB, Barcelona, Spain.<br />
V007 TOTAL ENDOSCOPIC GASTRIC BAND REMOVAL Kari Thompson, MD, Brian Wong, MD, Tom Savides, MD, Garth R Jacobsen, MD, Bryan<br />
Sandler, MD, Mark A Talamini, MD, Santiago Horgan, MD, University of California, San Diego, San Diego, California, USA<br />
V008 LAPROSCOPIC COMPLETION RADICAL CHOLECYSTECTOMY Shailesh Puntambekar, MS, Seema Puntambekar, MD, Geetanjali<br />
Agarwal, MS, Neeraj Rayate, MS, Galaxy-Care Laparoscopy Institute<br />
V009 THORACOSCOPIC ESOPHAGECTOMY IN DORSOLATERAL POSITION : AN INNOVATIVE APPROACH - THE PAWAR TECHNIQUE Suraj<br />
B Pawar, MS FICS FAIS FMAS, Prashant Mullerpatan, MS FRCS, Reshma S Pawar, MBBS DGO, Kolhapur Cancer Centre, India<br />
V010 SINGLE-INCISION LAPAROSCOPIC PROCTOCOLECTOMY WITH ILEAL J-POUCH-ANAL ANASTOMOSIS Alexandre Bouchard, MD,<br />
Jesse Lackey, SA, Tonia Young-Fadok, MD MS, Mayo Clinic - Arizona<br />
10:00 AM - 2:30 PM<br />
World Congress Exhibits, Posters & Learning Center Open<br />
11:30 AM - 1:00 PM<br />
BREAK: Exhibits, Posters, Learning Center<br />
11:30 AM - 1:30 PM **Separate Registration Fee: $55<br />
Educators Luncheon:<br />
Utilizing <strong>SAGES</strong> Educational Offerings for Residents<br />
Chair: L. Michael Brunt, M.D.; Co-Chair: Daniel Gagné, M.D.<br />
location: Potomac Ballroom D<br />
This session examines the broad array of materials that are available to complement education and skills training in minimally invasive<br />
surgery and flexible endoscopy. Topics to be covered include the Web Surg model of video education, <strong>SAGES</strong> video offerings and their<br />
integration into the SCORE national curriculum, and <strong>SAGES</strong> Fundamentals of Laparoscopic Surgery (FLS) and Fundamentals of Endoscopic<br />
Surgery (FES) programs. Practical methods by which these materials can be incorporated into resident and fellow education will be reviewed.<br />
Objectives:<br />
At the conclusion of this activity, the participant will be able to:<br />
• Describe <strong>SAGES</strong> educational resources available to complement resident and fellow training in minimally invasive surgery<br />
• Utilize effective strategies for incorporating FLS into residency training<br />
• Identify new methods for skills development and assessment in flexible endoscopy<br />
Schedule<br />
11:30 AM Introduction L. Michael Brunt, M.D.<br />
11:35 AM The Web Surg Model of Video Education Didier Mutter, M.D.<br />
11:50 AM From Top 14 to the SCORE Curriculum: Daniel Gagné, M.D. and<br />
Integrating <strong>SAGES</strong> Videos into Resident Education<br />
L. Michael Brunt, M.D.<br />
12:10 PM Strategies for Effective Integration of FLS into Your Skills <strong>Program</strong> Liane S. Feldman M.D.<br />
12:30PM FES: The Next Evolution in Endoscopic Skills Training Jeffrey Marks, M.D.<br />
12:45 PM Discussion<br />
<strong>SAGES</strong> acknowledges our Diamond Level Donors for their support of this session:<br />
Covidien, Ethicon Endo-Surgery, Inc. and <strong>SAGES</strong> Education and Research Foundation.<br />
12 th World Congress of Endoscopic Surgery<br />
35 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Thursday, April 15, <strong>2010</strong><br />
11:30 AM - 1:30 PM **Separate Registration Fee: $55<br />
Device Development Luncheon:<br />
From Funding to Freedom to Operate<br />
Chair: Raymond P. Onders, M.D.; Co-Chair: Dennis L. Fowler, M.D.<br />
location: Maryland Ballroom C<br />
The process from initial “idea or device” to help patient, to funding that idea, to working with the FDA to make sure that idea is safe and finally<br />
developing a company to manufacture and provide that idea to patients may seem daunting, but this session’s speakers will help make that<br />
journey easier with their wealth of experience.<br />
Objectives: At the conclusion of this session, participants will be able to:<br />
• Describe funding opportunities from the NIH and other sources<br />
• Understand the role of a university technology transfer office<br />
• Understand the role of the FDA in regulating devices<br />
• Appreciate the process of founding and funding enterprises for commercializing devices<br />
Schedule<br />
11:30 AM Introduction – The Story of the Diaphragm – Why Surgeons Innovate Raymond P. Onders, M.D.<br />
11:40 AM Funding – The NIH Can Help with Device Development Dennis Fowler, M.D.<br />
12:00 PM Technology Transfer – Friend or Foe to the Surgeon Innovator or to Industry Donna See, M.D.<br />
12:20 PM The Role of the FDA: From Patient Safety, 510(k), and from IDE to PMA –<br />
Why Designing a Trial and Endpoints are Important<br />
Markham C. Luke, M.D., Ph.D.<br />
12:40 PM Business Development – The Device Works – Now What? Baiju R. Shah<br />
1:00 PM Discussion<br />
<strong>SAGES</strong> acknowledges educational grants in support of this World Congress course from: Covidien and Ethicon Endo-Surgery, Inc.<br />
1:30 PM - 5:00 PM *included in Registration SuperPass (Option A) or Registration Option B)<br />
Laparoscopic IBD and Colectomy Postgraduate Course:<br />
The Status and Direction of Laparoscopic Colorectal Surgery<br />
in the Treatment of Inflammatory Bowel Disease<br />
Chair: John H. Marks M.D.; Co-Chair: Eric G. Weiss, M.D.<br />
location: Potomac Ballroom A<br />
This course will inform the practicing surgeon and trainee alike on the current status and the role of laparoscopic colorectal surgery in the<br />
treatment of inflammatory bowel disease. In a video intensive manner, controversies and technical “pearls” will be illustrated in the treatment<br />
of inflammatory bowel disease. The techniques and rationale for new minimally invasive colorectal surgical approaches as well as the<br />
implications of medical therapy on surgical approaches will be described.<br />
Objectives: At the conclusion of this session, participants will be able to:<br />
• Define the role of laparoscopic colorectal surgery in the treatment of inflammatory bowel disease<br />
• Restate laparoscopic approaches to ileal pouch-anal anastomosis for adult and pediatric patients<br />
• Indicate the impact of immunotherapy on the surgical treatment of inflammatory bowel disease<br />
• Describe the benefits of laparoscopic treatment of Crohn’s Disease<br />
Schedule<br />
1:30 PM Introduction John H. J Marks, M.D. & Eric G. Weiss, M.D.<br />
1:35 PM Presentation and Differentiation: Ulcerative Colitis & Crohn’s Disease John Monson, M.D.<br />
1:45 PM Medical management, Cancer Risk Surveillance, and<br />
indications for Surgery for ulcerative Colitis and Crohn’s Disease<br />
Conor Delaney, M.D.<br />
1:59 PM Laparoscopic Ileal Pouch-Anal Anastomosis: How to Do It Tonia Young-Fadok, M.D.<br />
2:13 PM Laparoscopic Pouches: Problem Area, Role of the Hand, Addressing Inadequate Length John H. Marks, M.D.<br />
2:27 PM Laparoscopic Pouches in the Pediatric Patient: When and How Keith E. Georgeson, M.D.<br />
2:41 PM Role of Single Port Proctocolectomy and Pouch: Fad? Trend? How I Do It Dan Geisler, M.D.<br />
2:55 PM Discussion<br />
3:15 PM BREAK<br />
3:30 PM Crohn’s Disease: Special Challenges of Surgery: Impact on Surgery of Immuno-Modulation –<br />
When Should Patients Stop? Port Placement and Planning Future Surgery. Strategy of Approach Toyooki Sonoda, M.D.<br />
3:44 PM Laparoscopy for Crohn’s Colitis – Total Abdominal Colectomy vs. Segmental Resection Kirk Ludwig, M.D.<br />
3:58 PM Lapaproscopic Approach to Crohn’s Disease:<br />
how I Approach Fistulous Disease, Abscess, and Strictures<br />
Petachia Reissman, M.D.<br />
4:12 PM Hand Assisted Approaches in Crohn’s Disease: When and Why Eric G. Weiss, M.D.<br />
4:26 PM Impact of Laparoscopy on Outcome for Crohn’s Disease Andre D’hoore, M.D.<br />
4:40 PM Discussion<br />
12 th World Congress of Endoscopic Surgery 36
Notes<br />
12 th World Congress of Endoscopic Surgery<br />
37 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Notes<br />
Hotel Video Loop<br />
Attention Guests at the Gaylord Hotel: The World Congress <strong>Program</strong> Chairs have created an<br />
additional avenue for excellent videos to be viewed by meeting attendees. You may view these<br />
videos in your hotel rooms on Thursday, Friday, and Saturday. Please turn to channel 57 (subject<br />
to change) in your Gaylord Hotel room to view the <strong>2010</strong> Video Channel Loop videos. The Video<br />
Channel Loop listing is available on page 148 of your program.<br />
12 th World Congress of Endoscopic Surgery 38
Thursday, April 15, <strong>2010</strong><br />
1:30 PM - 5:00 PM *Separate Registration Fee<br />
Single Port Access Surgery Hands-On Course<br />
Chair: Paul G. Curcillo II, M.D.; Co-Chair: Daniel J. Scott, M.D.<br />
**Offsite lab<br />
Location: Washington Institute of Surgical Endoscopy (WISE)<br />
The George Washington University Medical Center<br />
2300 I Street, NW, Ross Hall, Washington DC, 20037<br />
Shuttles for faculty and course registrants will depart at 12:30 PM from the Gaylord National Hotel and Convention Center.<br />
Go to the Group Bus Loading area, located at the Woodrow Wilson exit on the 2 nd level, opposite of guest parking.<br />
This session is designed to familiarize the participants with the developing field of Single Port Access surgery. Exposure to the tools, devices<br />
and techniques available will form the foundation for participants to begin to assimilate this technique into their practice.<br />
This course will consist of a hands-on lab in which participants will receive instruction by experts in various single port access<br />
laparoscopic techniques and procedures. Techniques for low-profile port layout and insertion, as well as the use of multi-port devices<br />
will be demonstrated with practice afforded. Participants will be supervised by experts and perform single port access laparoscopic<br />
cholecystectomy, fundoplication, adjustable gastric band placement, splenectomy and nephrectomy. Participants will have the opportunity<br />
to use a variety of specialized instrumentation, including novel imaging technologies, retraction devices, suturing instruments, and<br />
articulating devices. Lab stations will have a 1:3 faculty to participant ratio<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• Reproduce the various access techniques and identify the benefits and drawbacks of the multi-trocared vs. the multi-port devices<br />
• Identify and use the various instruments and tools that may facilitate single port access operations<br />
• Describe the operative strategies for performing single port access laparoscopic procedures (including – cholecstectomy, fundoplication,<br />
adjustable gastric band placement, splenectomy and nephrectomy)<br />
• Identify and be aware of the current data addressing the impact in terms of risks and benefits this new field is having on patients<br />
Schedule<br />
1:30 PM Introduction Paul G. Curcillo II, M.D. & Daniel J. Scott, M.D.<br />
1:35 PM Single Port Access Surgery: Techniques and Approaches<br />
1:35 PM OPUS – One Port Umbilical Access Prashanth Rao, M.D.<br />
1:45 PM Single Incision Surgery – Single Incision Laparoscopic Approach Homero Rivas, M.D.<br />
1:55 PM Single Incision Surgery – Single Port Access Approach Paul G. Curcillo II, M.D.<br />
2:05 PM Flexible Endoscopic Approach Julio Teixiera, M.D.<br />
2:15 PM Bariatric Considerations Daniel J. Scott, M.D.<br />
2:25 PM Access Device Considerations Abhay Rane, M.D.<br />
2:35 PM Hands On Lab<br />
Laparoscopic Cholecystectomy<br />
laparoscopic GE Jxn (Nissen / Banding)<br />
laparoscopic Splenectomy / Nephrectomy<br />
Lab Instructors:<br />
Casey Graybeal, M.D.<br />
Andrew Gumbs, M.D.<br />
Eric Hungness, M.D.<br />
Shuji Kitashiro, M.D.<br />
Abhay Rane, M.D.<br />
Prashanth Rao, M.D.<br />
Homero Rivas, M.D.<br />
Julio Teixiera, M.D.<br />
<strong>SAGES</strong> acknowledges educational grants in support of this World Congress course from:<br />
Applied Medical, Covidien, Ethicon Endo-Surgery, Inc., Karl Storz Endoscopy-America, Olympus and Stryker Endoscopy.<br />
12 th World Congress of Endoscopic Surgery<br />
<strong>SAGES</strong> acknowledges contributions in-kind in support of this World Congress course from:<br />
Aesculap, Allergan, Apple Medical, Applied Medical, Cambridge Endoscopy, Cambridge Health Alliance,<br />
Carefusion, Covidien, Davol Inc., a BARD Company, Ethicon Endo-Surgery, Inc., Karl Storz Endoscopy-America,<br />
Microline Surgical, Novare Surgical Systems, Olympus, Stryker Endoscopy, Surgiquest and Virtual Ports.<br />
Evaluation & CME Credit Claim<br />
Visit the kiosks next to registration to complete<br />
your online evaluation and CME credit form on-site.<br />
Attendees may print CME certificates two weeks<br />
after the conclusion of the meeting.<br />
The programs and lectures presented at the <strong>2010</strong> World<br />
Congress Meeting are copyrighted products of the Society<br />
of American Gastrointestinal and Endoscopic Surgeons.<br />
Any reproduction or rebroadcasting without the express<br />
written consent of <strong>SAGES</strong> is strictly prohibited.<br />
39 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Thursday, April 15, <strong>2010</strong><br />
1:30 PM - 5:00 PM *included in Registration SuperPass (Option A) or Registration Option B)<br />
MBA for Surgeons Panel: Asset Management and Protection for Surgeons<br />
Chair: Demetrius E. M. Litwin, M.D.; Co-Chair: Fredrick J. Brody, M.D.<br />
location: Potomac Ballroom C<br />
Description: The rapidly changing economics of practicing medicine will affect all of us. This practical session will help understand what<br />
changes you can make in your practice and investments to adjust to these turbulent times. The session will be full of practical, real-world<br />
advice and potential solutions to difficult financial problems you face on a daily basis.<br />
Objectives: At the conclusion of this session, participants will be able to:<br />
• Understand money management options during a practice lifetime.<br />
• Recognize and understand the fundamentals of investment principles during a practice lifetime.<br />
• Identify the importance of leadership in organizations.<br />
• Understand the importance of strategic planning exercises for high performance organizations.<br />
Schedule<br />
1:30PM Introduction Demetrius E. M. Litwin, M.D.; Fredrick Brody, M.D.<br />
Wealth Management, Asset Protection<br />
1:35PM Who to Entrust with Your Money and What Relationships Should You Have? David Field, CFA<br />
1:50PM Investing 101 – The Business School Perspective Bruce Behn, M.D.<br />
2:05PM Investing – Practical Tips Tim Pitney – Sapers & Wallack<br />
2:20PM Retirement, Insurance and Estate Management – Aviva Sapers – Sapers & Wallack<br />
How Much Do You Really Need and What Do You Do With It?<br />
2:45PM Discussion Panel & Questions<br />
3:15PM BREAK<br />
Leadership<br />
3:30PM Physician Executive MBA – What Can It Do For You? Mike Stahl, M.D.<br />
3:45PM The Leadership Moment – The Business School Perspective Bruce Behn, M.D.<br />
4:00PM The Leadership Moment – Practical Examples in the World of Surgery Isadore Lieberman, M.D.<br />
4:15PM Strategic Planning To Create High Performance Organizations Alec Glover, M.B.A.<br />
4:30PM Discussion Panel & Questions<br />
5:00PM Adjourn<br />
<strong>SAGES</strong> does NOT offer CME credits for this Panel<br />
1:30 PM - 5:00 PM **Separate Registration Fee<br />
Hands On Endolumenal/NOTES® Lab<br />
Chair: Santiago Horgan, M.D.; Co-Chair: Christopher C. Thompson, M.D.<br />
location: Maryland Ballroom B-D<br />
Description: This will be a multiple station hands-on course that will allow a technical experience in a variety of endolumenal procedures<br />
and technology. This will also include an introduction to NOTES® specifically, a transvaginal and transgastric peritoneal access, and<br />
transgastric closure. The latest endolumenal tissue fixation devices, energy application devices and intraluminal stents will be included.<br />
Participants should have basic endoscopic skills and be willing to try new procedures and use new technology.<br />
Objectives: At the conclusion of this session, participants will be able to:<br />
• Experience the use of modern endolumenal techniques for energy ablation (argon plasma coagulation, heater probe, BICAP, etc.) and<br />
stent placement<br />
• Demonstrate techniques for Endoscopic Mucosal Resection (EMR) and Endoscopic Submucosal Tunneling<br />
• Recognize the principles of endolumenal tissue fixation<br />
• Evaluate and practice transgastric and transvaginal approaches to peritoneal access (Natural Orifice Translumenal Endoscopic Surgery, NOTES®)<br />
• Demonstrate techniques for transgastric closure<br />
Schedule<br />
1:30 PM Introduction – Video Demonstration of Basic Technique Santiago Horgan, M.D. & Christopher C. Thompson, M.D.<br />
Barrett’s Ablation<br />
Steven Edmundowicz, M.D.<br />
Endoscopic Mucosal Resection (EMR) and<br />
Endoscopic Submucosal Tunneling<br />
Christopher J. Gostout, M.D. & Abraham Mathew, M.D., M.Sc.<br />
Endoscopic Revision for GERD<br />
Jeffrey W. Hazey, M.D.<br />
Intraluminal Stents: Placements and Removal, Colonic and Esophageal<br />
Jose Martinez, M.D.<br />
Treatment of Bleeding<br />
Bipan Chand, M.D.<br />
Endosuturing Techniques for GERD and Redo Bypass<br />
Garth Jacobsen, M.D.<br />
NOTES® Stations:<br />
Transgastric and Transvaginal Approaches to<br />
peritoneal Access and Transgastric Closure Techniques<br />
Marc Bessler, M.D., Brian J. Dunkin, M.D., Michael Marohn, M.D.,<br />
Jeffrey Marks, M.D., Patricia Sylla, M.D., Yoav Mintz, M.D.<br />
<strong>SAGES</strong> acknowledges educational grants in support of this World Congress course from:<br />
BÂRRX Medical, Boston Scientific, Covidien, Endogastric Solutions, Olympus and Stryker Endoscopy.<br />
<strong>SAGES</strong> acknowledges contributions in-kind in support of this World Congress course from:<br />
Alveolus Inc., Apollo Endosurgery, Aponos Medical Corp., BÂRRX Medical, Boston Scientific, Covidien, Davol Inc., a BARD Company,<br />
Endogastric Solutions, Endosim, Erbe, Karl Storz Endoscopy-America, Novare Surgical Systems, Olympus, US Endoscopy, Virtual Ports.<br />
12 th World Congress of Endoscopic Surgery 40
Thursday, April 15, <strong>2010</strong><br />
1:30 PM - 2:30 PM *included in Registration SuperPass (Option A) or Registration Option B<br />
Robotics Symposium: What’s New?<br />
Chair: Mehran Anvari, M.D.; Co-Chair: Jacques Marescaux, M.D.<br />
location: Potomac Ballroom B<br />
Description:<br />
Robotic surgery has the potential to become a significant force in the future of minimally invasive surgery.This session will demonstrate new<br />
applications of robotics with particular emphasis on the application to reduced port surgery and image-guided applications.<br />
Objectives: At the conclusion of this session, participants will be able to:<br />
• Highlight some of the new developments in application of robotics in surgery<br />
• Discuss the use of robotics in augmented reality and image guided surgery<br />
• Provide and overview of robotic development for NOTES® and single incision surgery<br />
Schedule<br />
1:30 PM Introduction Mehran Anvari, M.D. & Jacques Marescaux, M.D.<br />
1:35 PM Augmented Reality and Image Guided Robotic Surgery Luc Soler, M.D.<br />
1:45 PM New Applications of Surgical Robot Richard Satava, M.D.<br />
1:55 PM The EU ARAKNES Robotic System Sir Alfred Cuschieri, M.D.<br />
2:05 PM Flexible Robotic Platform for NOTES® or Single Incision Surgery Bernard Dallemagne, M.D.<br />
2:15 PM Discussion<br />
2:30 PM - 4:00 PM *included in Registration SuperPass (Option A) or Registration Option B)<br />
Metabolic Surgery Symposium: Current Status<br />
Chair: Philip R. Schauer, M.D.; Co-Chair: Francesco Rubino, M.D.<br />
location: Potomac Ballroom B<br />
Description:<br />
The metabolic syndrome is a worldwide problem – can it be solved by surgery? Internationally-renowned experts will discuss the relevant<br />
issues in this rapidly developing field.<br />
Objectives: At the conclusion of this session, participants will be able to:<br />
• Understand how to diagnose the various stages of Barrett’s<br />
• Understand the different minimally invasive treatment options available<br />
• Discuss new technologies and their impact on the management process<br />
Schedule<br />
2:30 PM Introduction Philip R. Schauer, M.D. & Francesco Rubino, M.D.<br />
2:35 PM Effect of Gastric Banding and Sleeve Gastrectomy on Metabolic Disease Alfonso Torquati, M.D.<br />
2:50 PM Effect of Bypass Procedures Philip R. Schauer, M.D.<br />
3:05 PM Mechanisms of Remission of Metabolic Disease David Cummings, M.D.<br />
3:20 PM The Diabetes Surgery Summit Guidelines for Surgical Treatment of Diabetes Francesco Rubino, M.D.<br />
3:35 PM The American Diabetes Association Guidelines for Surgical Treatment of Diabetes Sue Kirkman, M.D.<br />
3:50 PM Discussion<br />
<strong>SAGES</strong> acknowledges an educational grant in support of this World Congress panel from Covidien.<br />
12 th World Congress of Endoscopic Surgery<br />
4:00 PM - 5:30 PM *included in Registration SuperPass (Option A) or Registration Option B)<br />
Barrett’s Debate: How to Follow, How to Treat?<br />
Chair: John Hunter, M.D.; Co-Chair: Karl H. Fuchs, M.D.<br />
location: Potomac Ballroom B<br />
Description:<br />
Cancer in Barrett’s esophagus continues to be a serious worldwide problem. Can we identify the patients at high risk to impact this disease?<br />
This session will provide a critical update on strategies in the diagnosis and management of Barrett’s.<br />
Objectives: At the conclusion of this session, participants will be able to:<br />
• Understand how to diagnose the various stages of Barrett’s<br />
• Understand the different minimally invasive treatment options available<br />
• Discuss new technologies and their impact on the management process<br />
Schedule<br />
4:00 PM Introduction John Hunter, M.D. & Karl H. Fuchs, M.D.<br />
4:05 PM The Indications and Strategy for Screening and Surveillance of Barrett’s Esophagus Jeffrey Peters, M.D.<br />
4:20 PM Ablation Therapy – Who Should Have It and Who Should Do It? John Hunter, M.D.<br />
4:35 PM Endoscopic Mucosal Resection of Early Esophageal Neoplasia – The Current State of the Art Haruhiro Inoue, M.D.<br />
4:50 PM Limited Surgical Resection – or En-Bloc Karl H. Fuchs, M.D.<br />
5:05 PM Emerging Technology in the Diagnosis and Management of Barrett’s Esophagus Blair Jobe, M.D.<br />
5:20 PM Discussion<br />
41 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Thursday, April 15, <strong>2010</strong><br />
5:30 PM - 7:30 PM Free for any World Congress Attendee<br />
Industry Satellite Symposia (No Registration Required)<br />
Industry presentations will take place on Thursday evening, immediately following the Congress sessions. Three symposia on<br />
varying topics will be offered in the World Congress session rooms. Registration is FREE for any World Congress attendee. These<br />
events are not planned nor accredited for CME by <strong>SAGES</strong>.<br />
Boston Scientific – “Intraluminal Stents and the Surgeon –<br />
Who, What, Where, When and Why?”<br />
Location: Chesapeake D-E<br />
Boston Scientific invites you to join your colleagues for a presentation on the role of stents in managing malignant and benign disease. Topics<br />
covered will include emerging treatment algorithms, current clinical data, new stent technologies, and case experiences. A Q&A session will<br />
follow the presentation.<br />
Light refreshments will be provided as a courtesy for people attending this event. Due to restrictions imposed by Massachusetts and<br />
Vermont law, we ask that health care professionals who are licensed by Massachusetts or Vermont not partake of them. Thank you for your<br />
cooperation.<br />
This is a non-CME activity presented and supported by Boston Scientific.<br />
Covidien – “Insights into the Future of Surgical Stapling:<br />
Integrated Materials, Tri-Staple Technology, Powered Staplers”<br />
Location: Potomac Potomac D-4-5-6<br />
Presenters: Mark S. Soberman, MD, FACS, Moderator<br />
Aurora Pryor, MD, FACS<br />
Garrett M. Nash, MD, MPH<br />
Samer G. Mattar, MD, FACS<br />
This is a non-CME activity presented and supported by Covidien.<br />
Davol Inc., a BARD Company: “Advanced Endoscopic Technique for Abdominal Wall<br />
Reconstruction”<br />
Location: Maryland C<br />
Speaker: J. Scott Roth, MD, FACS<br />
Associate Professor of Surgery<br />
Chief, Gastrointestinal Surgery<br />
Director, Minimally Invasive Surgery<br />
University of Kentucky Medical Center<br />
Overview: Dr. J. Scott Roth from the University of Kentucky will discuss the evolution of the Component Separation Technique for complex<br />
abdominal wall reconstruction. Dr. Roth will walk the attendees through the evolution of his current technique for endoscopic assisted<br />
component separation, including the advantages of this technique over open component separation. Dr. Roth will also discuss such topics as<br />
patient selection for component separation and graft selection, as well as current clinical data on the procedure.<br />
This is a non-CME activity presented and supported by Davol Inc., a BARD Company.<br />
Ethicon Endo-Surgery, Inc.: “Minimally Invasive Surgery – Where is it Going?”<br />
Location: Potomac C-1-2-3<br />
Surgeons will be discussing the following topics:<br />
Advances in General Surgery: Santiago Horgan, MD<br />
Advances in Colorectal Surgery: Conor Delaney, MD<br />
Advances in Bariatric Surgery: Keith Zuccala, MD<br />
This is a non-CME activity presented and supported by Ethicon Endo-Surgery, Inc.<br />
Karl Storz Endoscopy-America, Inc.: “The Great Debate: S-PORTAL (Single Portal<br />
Access) Surgery vs. Mini-Laparoscopy”<br />
Location: Maryland A-1-2-3<br />
Dr. Jeffrey Ponsky (Case Western Reserve University, Cleveland, Ohio) will act as moderator as four representatives engage in the debate.<br />
Proponents of S-PORTAL –<br />
Dr. Paul Curcillo (Drexel University, Philadelphia, Pennsylvania)<br />
Professor Giovanni Dapri (Saint-Pierre University Hospital, Brussels, Belgium)<br />
Proponents of Mini-Laparoscopy –<br />
Dr. Michel Gagner (Mount Sinai Medical Center, Miami Beach, Florida)<br />
Dr. Joseph Mamazza (Ottawa Hospital, Ottawa, Canada)<br />
This is a non-CME activity presented and supported by Karl Storz Endoscopy-America.<br />
12 th World Congress of Endoscopic Surgery 42
12 th World Congress of Endoscopic Surgery<br />
Notes<br />
<strong>2010</strong> World Congress International Webcast Sessions<br />
To participate in the International Webcast Sessions, please visit:<br />
http://www.sages.org/meetings/annual_meeting/<strong>2010</strong>/<br />
Password: sages<br />
Friday, April 16, <strong>2010</strong><br />
TIME SESSION CHAIR (S)/SPEAKER<br />
8:00 am- 9:00 am Plenary Session C. Daniel Smith, MD & C. Jamieson, MD<br />
9:00 am - 9:30 am <strong>SAGES</strong> Presidential Address C. Daniel Smith, MD<br />
9:30 am - 10:00 m Gerald Marks Keynote Lecture Richard H. Bell, MD<br />
10:00 am - 11:00 am Symposium: NOTES® - Alive and Well, or RIP?<br />
12:30 pm - 2:30 pm Presidential Debates<br />
2:30 pm - 4:00 pm Panel: Single Port Access Surgery<br />
Saturday, April 17, <strong>2010</strong><br />
Chair: David W. Rattner, MD<br />
Co-chair: Venkat G. Rao, MD<br />
Chair: Daniel J. Deziel, MD<br />
Co-chair: Nathaniel Soper, MD<br />
Chair: Joel Leroy, MD<br />
Co-chair: Andrew A. Gumbs, MD<br />
TIME SESSION CHAIR (S)/SPEAKER<br />
7:00 am - 8:30 am Live from Afghanistan Session: Video Conference Military Coalition<br />
Chair: Steven P. Bowers, MD<br />
Co-chair: Richard M. Satava, MD<br />
8:30 am - 9:00 am Karl Storz Keynote Lecture Christopher J. Gostout, MD<br />
9:00 am - 9:30 am CAGS / Royal College of Surgeons Lecture Robert DiRaddo, Ph.D.<br />
9:30 am - 11:00 am Plenary Session II Moderators: J. Buyske, MD & A. Chousleb, MD<br />
<strong>SAGES</strong> gratefully acknowledges Covidien, Ethicon Endo-Surgery, Inc. and the <strong>SAGES</strong> Education & Research Foundation<br />
for their generous support towards the <strong>SAGES</strong> Global Proctoring Initiative.<br />
To fully comply with ACCME regulations, all World Congress attendees must have their badge<br />
scanned before entering any course or session room in order to receive CME credit for that event.<br />
12 th World Congress of Endoscopic Surgery 44
Friday, April 16, <strong>2010</strong><br />
Time Session Location<br />
Scientific Sessions & Panels<br />
7:00 AM - 8:00 AM Posters of Distinction Potomac Ballroom C<br />
8:00 AM - 9:00 AM SS02 Plenary Session 1 Potomac Ballroom A-B<br />
9:00 AM - 9:30 AM<br />
<strong>SAGES</strong> Presidential Address: Everyone Knows Plan A:<br />
Its All About Plan B<br />
Potomac Ballroom A-B<br />
C. Daniel Smith, M.D.<br />
9:30 AM - 10:00 AM<br />
Gerald Marks Lecture: The Making of a Surgeon – Revisited<br />
Richard H. Bell, M.D.<br />
Potomac Ballroom A-B<br />
10:00 AM - 2:30 PM Exhibits, Posters, Learning Center Open<br />
10:00 AM -11:00 AM<br />
Concurrent Sessions (accepted oral & video presentations)<br />
SS03 Solid Organ<br />
Maryland Ballroom B-D<br />
SS04 Basic Science<br />
Maryland Ballroom A<br />
10:00 AM - 11:00 AM Endolumenal Therapies Session Potomac Ballroom C<br />
10:00 AM - 11:00 AM NOTES® Symposium – Alive & Well or RIP? Potomac Ballroom A-B<br />
10:00 AM - 11:00 AM<br />
Laparoscopic Education Panel –<br />
Do MIS Fellowships Have a Future?<br />
Potomac Ballroom D<br />
11:00 AM - 12:30 PM Video Complications Luncheon:<br />
What Has Happened and What Do We Have to Do?<br />
Maryland Ballroom C<br />
12:30 PM - 1:30 PM<br />
Go Global Report from the Field Panel:<br />
Teaching Laparoscopic Surgery Abroad<br />
Maryland Ballroom A<br />
12:30 PM - 2:30 PM Peer Review Training Session Potomac Ballroom D<br />
12:30 PM - 2:30 PM <strong>SAGES</strong> Presidential Debates Potomac Ballroom A-B<br />
1:30 PM - 2:30 PM Conflict of Interest Panel Maryland Ballroom A<br />
2:30 PM - 5:30 PM Resident and Fellows Scientific Session Maryland Ballroom C<br />
2:30 PM - 4:00 PM Single Port Access Surgery Panel Potomac Ballroom A-B<br />
2:30 PM - 4:00 PM<br />
Concurrent Sessions<br />
SS05 Hepatobiliary/Pancreatic<br />
Maryland Ballroom B-D<br />
SS06 Hernia<br />
Potomac Ballroom D<br />
Concurrent Sessions<br />
SS07 Best of Video 2<br />
Maryland Ballroom B-D<br />
4:00 PM - 5:30 PM<br />
SS08 Education/Simulation<br />
Maryland Ballroom A<br />
SS09 NOTES®<br />
Potomac Ballroom D<br />
2:30 PM - 5:30 PM Emerging Technology Session Potomac Ballroom C<br />
6:00 PM - 7:00 PM<br />
Meet the Leadership Reception For Residents, Fellows & New<br />
Members<br />
Pose, 18-19th Floor<br />
12 th World Congress of Endoscopic Surgery<br />
Water Taxi Service<br />
In addition to cabs and rental cars, the National Harbor offers a fun and practical way to get to various<br />
destinations…a water taxi! Water taxi service is available to and from points around Washington D.C., Virginia<br />
and Maryland for your convenience. The Potomac Riverboat Company operates water taxi service between<br />
National Harbor and Old Town Alexandria, with additional boat service to Mount Vernon and Georgetown. Water<br />
taxis will run every half hour between National Harbor and Old Town Alexandria. There will be three daily trips to<br />
Georgetown’s Washington Harbor, and a single daily trip to George Washington’s Mount Vernon Estate. Ask the<br />
concierge for more information and about pricing.<br />
45 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Friday, April 16, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
Scientific Session Concurrent Sessions (accepted oral & video presentations)<br />
Description:<br />
This section of the World Congress includes panels with invited faculty who will speak on specific topics, and sessions of oral & video<br />
presentations of abstracts selected by the World Congress <strong>Program</strong> Committee.<br />
What Is Included:<br />
The Scientific Session is included in Registration SuperPass (Option A). Thursday sessions (concurrent only) are also included in Registration<br />
Option B. Friday/Saturday sessions and panels are included in Registration Option C. All fees include entrance to all didactic session rooms<br />
(not including hands-on course labs or lunches), <strong>Final</strong> <strong>Program</strong>, entrance to the Exhibit Hall, Learning Center, Posters, Digital Meeting Guide,<br />
continental breakfast & breaks, and lunch in the Exhibit Hall on Saturday.<br />
7:00 AM - 8:00 AM *Included in Registration SuperPass (Option A) or Registration Option C<br />
Posters of Distinction<br />
Moderators: Subhash U. Kini, M.D. & Melina C. Vassiliou, M.D.<br />
location: Potomac Ballroom C<br />
P001 EVALUATION OF THE SLEEVE GASTRECTOMY AS A SINGLE-STAGE TREATMENT OF MORBID OBESITY Philippe A Topart, MD, Cyril<br />
Chazelet, MD, Pierre Verhaeghe, MD FACS, Societe de Chirurgie Viscerale, Clinique de l’Anjou, Angers ; Clinique St Brice, Provins, Chirurgie<br />
Viscerale, CHU, Amiens, France<br />
P002 PATIENTS EXPECT TO LOSE MORE THAN AVERAGE WEIGHT AFTER BARIATRIC SURGERY Brad E Snyder, MD, Erik B Wilson, MD FACS,<br />
Todd Wilson, MD, Connie Klein, RN NP, University of Texas Health Sciences Center at Houston<br />
P003 ANASTOMOTIC LEAKS AFTER 899 LAPAROSCOPIC COLORECTAL SURGERIES:WAY TO AN OPTIMAL INTESTINAL ANASTOMOSIS<br />
Song Liang, MD PhD, Morris E Franklin Jr, MD FACS, The Texas Endosurgery Institute<br />
P004 SINGLE INCISION LAPAROSCOPIC GASTRIC BANDING: EVOLUTION TOWARDS SCARLESS SURGERY DURING 50 CONSECUTIVE<br />
CASES Sarah C Oltmann, MD, Lauren Mashaud, MD, Stephanie Morris, BS, Arsalla Islam, MD, Homero Rivas, MD MBA, Daniel J Scott, MD,<br />
Southwestern Center for Minimally Invasive Surgery, Department of Surgery, University of Texas Southwestern Medical Center, Dallas, TX<br />
P005 CLINICAL OUTCOMES OF ATYPICAL SYMPTOMS FOLLOWING LAPAROSCOPIC ANTIREFLUX SURGERY Shaun R Brown, DO, C.<br />
Prakash Gyawali, MD, Lora Melman, MD, Eric D Jenkins, MD, Julia Bader, PhD, Margaret M Frisella, RN, L. Michael Brunt, MD, J. Christopher<br />
Eagon, MD, Michael M Awad, MD PhD, Brent D Matthews, MD, Department of Surgery, Section of Minimally Invasive Surgery, Washington<br />
University School of Medicine, Saint Louis, MO<br />
P006 PREOPERATIVE ULTRASOUND AS A PREDICTOR OF GALLBLADDER EXTRACTION DURING TRANSGASTRIC NOTES<br />
CHOLECYSTECTOMY Byron F Santos, MD, Edward D Auyang, MD, Eric S Hungness, MD, Kush R Desai, MD, Edward S Chan, BA, Darren B van<br />
Beek, BS, Edward C Wang, PhD, Nathaniel J Soper, MD, Northwestern University, Department of Surgery<br />
P007 A COMPARISON OF PRE-OPERATIVE COMORBIDITIES AND POST-OPERATIVE OUTCOMES AMONG PATIENTS UNDERGOING<br />
LAPAROSCOPIC NISSEN FUNDOPLICAITON AT HIGH AND LOW VOLUME CENTERS Oliver A Varban, MD, Thomas McCoy, MS, Carl<br />
Westcott, MD, Wake Forest University Baptist Medical Center<br />
P008 102 CONSECUTIVE ROBOTIC ASSISTED MINIMALLY INVASIVE COLECTOMIES – AN OUTCOME AND TECHNICAL UPDATE Franziska<br />
Huettner, MD PhD, Paul E Pacheco, MD, Jamie L Doubet, RN BS, Michael J Ryan, MS, Danuta I Dynda, MD, David L Crawford, MD, Division of<br />
Minimally Invasive Surgery, Department of Surgery, University of Illinois College of Medicine at Peoria<br />
P009 238 LAPAROSCOPIC LEFT-SIDE COLORECTAL SURGERIES WITH N.O.S.E.: A 10-YEAR EXPERIENCE WITH TRANSANAL SPECIMEN<br />
EXTRACTION Morris E Franklin, Jr, MD FACS, Song Liang, MD PHD, The Texas Endosurgery Institute<br />
P010 SINGLE-INCISION LAPAROSCOPIC COLECTOMY FOR COLON CANCER: EXPERIENCE OF 35 CASES Bac H Nguyen, PhD, Thinh H<br />
Nguyen, MD, Viet V Ung, MD, University Medical Center at Ho Chi Minh City<br />
P011 SAFETY AND USEFULNESS OF LAPAROSCOPIC METHOD FOR TREATMENT OF PERITONITIS DUE TO ANASTOMOSIS SITE<br />
LEAKAGE AFTER RECTAL CANCER RESECTION Gyu-Seog Choi, MD, Kyoung-Hoon Lim, MD, Jun Seok Park, MD, You Seok Jang, MD, Soo-<br />
Han Jun, MD, Department of Surgery, School of Medicine, Kyungpook National University, Daegu, Korea<br />
P012 INDICATIONS, COMPLICATIONS AND LONG TERM OUTCOMES OF REMNANT GASTRECTOMY FOR GASTRO-GASTRIC FISTULA<br />
AFTER DIVIDED ROUX-EN-Y GASTRIC BYPASS FOR MORBID OBESITY Emeka Acholonu, Jeremy Eckstein, Sheetal Patel, Wasef Abu-Jaish,<br />
Samuel Szomstein, Raul Rosenthal, Cleveland Clinic Florida<br />
P013 NEEDLESCOPIC SURGERY: THE COSMETIC ALTERNATIVE TO SILS Morris E Franklin, MD, Karla Russek, MD, Jojy George, MD, Texas<br />
Endosurgery Institute<br />
P014 ROLE OF INTERLEUKIN-6 (IL-6) IN THE GROWTH OF CT26 COLORECTAL CANCER IN A MURINE MODEL Melissa A Donigan, BS, Heidi<br />
Bahna, MD, Bryan D Loh, MD, Laurie S Norcross, MD, John Aversa, DO, Paul R Williamson, MD, Samuel DeJesus, MD, Andrea Ferrara, MD,<br />
Joseph T Gallagher, MD, Cheryl H Baker, PhD, M. D. Anderson Cancer Center Orlando, University of Central Florida, Colon and Rectal Clinic of<br />
Orlando, Orlando Regional Medical Center<br />
P015 LAPAROSCOPIC LIVER SURGERY IN CANCER PATIENTS-EXPERIENCE AT A NATIONAL CANCER INSTITUTE Ronald Matteotti, MD,<br />
John Hoffman, MD, Elie Chouillard, MD, Veeraiah Siripurapu, MD, Andrew Gumbs, MD, FOX CHASE CANCER CENTER, Philadelphia-PA, USA<br />
P016 IS SURGERY A BETTER OPTION AS FIRST LINE TREATMENT FOR ACHALASIA?: A COMPARISON OF LAPAROSCOPIC<br />
ESOPHAGOMYOTOMY WITH FUNDOPLICATION AND ENDOSCOPIC DILATION Jason F Reynoso, MD, Manish M Tiwari, MD PhD MPH,<br />
Albert W Tsang, MD, Dmitry Oleynikov, MD, Department of Surgery, University of Nebraska Medical Center<br />
P017 PERFORMANCE RAMIFICATIONS OF SINGLE PORT LAPAROSCOPIC SURGERY: MEASURING DIFFERENCES IN TASK<br />
PERFORMANCE USING SIMULATION Nathan E Conway, MD, John R Romanelli, MD, Ron W Bush, BS, Neal E Seymour, MD, Baystate Medical<br />
Center, Tufts University School of Medicine, Springfield, MA<br />
12 th World Congress of Endoscopic Surgery 46
Friday, April 16, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
P018 ONCOLOGIC AND PERIOPERATIVE OUTCOMES OF LAPAROSCOPIC ASSISTED VS HAND-ASSISSTED VS OPEN RESECTIONS FOR<br />
RECTAL CANCER RESECTION: A CASE MATCH STUDY. Pornthape Prathanvanich, Jirawat Pattana Arun, Chucheep Sahakitrungruang,<br />
Puttarat Atithansakul, Arun Rojanasakul, Chulalongkorn University<br />
P019 “INCISIONLESS” LAPAROSCOPIC PROCTECTOMY: AN IDEAL NATURAL ORIFICE AND LAPAROSCOPIC SURGERY HYBRID John<br />
Marks, MD, Radu Nedelcoviciu, MD, Eileen Larkin, BA, Albert DeNittis, MD, Gerald Marks, MD, Lankenau Hospital and Institute for Medical<br />
Research: Section of Colorectal Surgery, Wynnewood, PA<br />
P020 COLORECTAL CANCER RISK REDUCTION IN INFLAMMATORY BOWEL DISEASE WITH AMINOSALICYLATE THERAPY: A META-<br />
ANALYSIS AND COMPARISON TO COLORECTAL CANCER RISK IN THE GENERAL POPULATION Omer Nasir, MD, Amit Kaul, MD, Tejwant<br />
Datta, MD, Maryanne Franco, M Gilson, MD, Michael Marohn, DO, Hien Nguyen, MD, Johns Hopkins University School of Medicine<br />
P021 CONVENTIONAL 4-PORT LAPAROSCOPIC CHOLECYSTECTOMY VERSUS SILS PORT LAPAROSCOPIC CHOLECYSTECTOMY-<br />
EARLY RESULTS OF THE FIRST PROSPECTIVE RANDOMIZED SHAM CONTROLLED TRIAL Jeffrey Marks, MD, Raymond Onders, MD,<br />
George DeNoto, MD, Berry Paraskeva, PhD, Homero Rivas, MD, Kurt Roberts, MD, Alexander Rosemurgy, MD, Sajani Shah, MD, Nathaniel<br />
Soper, MD, Roberto Tacchino, MD, University Hospitals Case Medical Center, North Shore University Hospital, Imperial College of London,<br />
UT Southwestern Medical Center, Yale New Haven Medical Center, Tampa General Hospital, Tufts Medical Center, Northwestern Memorial<br />
Hospital, Catholic U<br />
P022 COLON RESECTIONS IN AN ERA OF NONAGENARIANS: NSQIP PREDICTORS OF MORTALITY Dan Ruiz, MD, Alexander Kraev, MD,<br />
Darshak Shah, MD, Allapagan W Annamalai, MD, James W Turner, MD, Howard Tiszenkel, MD, New York Hospital Queens<br />
8:00 AM - 9:00 AM *Included in Registration SuperPass (Option A) or Registration Option C<br />
SS02 Plenary Session 1<br />
Moderators: C. Daniel Smith, MD & Christopher Jamieson, Md<br />
location: Potomac Ballroom A-B<br />
S001 MOST RECENT NATIONAL SURGICAL QUALITY IMPROVEMENT PROJECT DATA (NSQIP), COMPARISON OF LAPAROSCOPIC VS.<br />
OPEN COLON RESECTIONS Dan Ruiz, MD, Alexander Kraev, MD, Steven Nurkin, MD, Darshak Shah, MD, James W Turner, MD, Howard<br />
Tiszenkel, MD, New York Hospital Queens<br />
S002 INCISIONAL HERNIA – MIDLINE VS LOW TRANSVERSE INCISION: WHAT IS THE IDEAL INCISION FOR SPECIMEN EXTRACTION/<br />
HALS? Ashwin L deSouza, MS MRCSEd DNB FCPS MNAMS, Bastian Domajnko, MD, John J Park, MD, Slawomir J Marecik, MD, Leela M Prasad,<br />
MD MSSurg FRCSE FRCSC FACS FASCRS, Herand Abcarian, MD, Advocate Lutheran General Hospital, Park Ridge, Illinois<br />
S003 LIMITED VALUE OF HAPTICS IN VIRTUAL REALITY LAPAROSCOPIC CHOLECYSTECTOMY TRAINING Jonathan R Thompson, MD,<br />
Charles R Doarn, MBA, Matt J Roesch, Brian D Henry, MD, Timothy J Broderick, MD, University of Cincinnati, Department of Surgery<br />
V011 LAPAROSCOPIC REPAIR OF BOCHDALEK HERNIA Mohamad D Saad, DO, Jonathan Eng, MD, Frances Allocco, MD, Brian J Dunkin, MD,<br />
Patrick R Reardon, MD, The Methodist Hospital<br />
<strong>SAGES</strong> acknowledges our Diamond Level Donors for their support of this session:<br />
Covidien, Ethicon Endo-Surgery, Inc. and <strong>SAGES</strong> Education and Research Foundation<br />
12 th World Congress of Endoscopic Surgery<br />
9:00 AM - 9:30 AM *included in Registration SuperPass (Option A) or Registration Option C<br />
<strong>SAGES</strong> Presidential Address<br />
C. Daniel Smith, M.D.<br />
Professor and Chair, Department of Surgery, Surgeon in Chief, Mayo Clinic Florida, Jacksonville, FL<br />
Everyone Knows Plan A: Its All About Plan B<br />
Location: Potomac Ballroom A-B<br />
FLS Testing Available!<br />
Wednesday, April 14 - Saturday, April 17, <strong>2010</strong><br />
Location: Chesapeake Conference Rooms 7-9<br />
All testing appointments must be made by April 9 – no onsite appointments available<br />
Contact FLS@sages.org for more details or to schedule your test.<br />
To fully comply with ACCME regulations, all World Congress<br />
attendees must have their badge scanned before entering any<br />
course or session room in order to receive CME credit for that event.<br />
47 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Friday, April 16, <strong>2010</strong><br />
1994 Prof. Alex Walt<br />
1995 Prof. Kenneth Forde<br />
1996 Prof. John Wickham<br />
1997 Prof. Thomas Dent<br />
1998 Prof. Jacques J. Perissat<br />
1999 Prof. Michael Trede<br />
2000 Prof. Tom R. DeMeester<br />
2001 Prof. Layton F. Rikkers<br />
Scientific Sessions & Panels<br />
9:30 AM - 10:00 AM *included in Registration SuperPass (Option A) or Registration Option C<br />
Gerald Marks Lecture: The Making of a Surgeon – Revisited<br />
Richard H. Bell, M.D.<br />
Location: Potomac Ballroom A-B<br />
Assistant Executive Director, American Board of Surgery, Philadelphia, PA<br />
Richard H. Bell Jr., M.D. is the Assistant Executive Director of the American Board of Surgery.Dr. Bell earned his Bachelor’s degree at<br />
Princeton University and MD degree at Northwestern. He completed his general surgical residency at the University of Colorado<br />
Medical Center in Denver. Following military service, he served on the faculty at the University of California at San Diego and then as<br />
Associate Professor, then Chief of General Surgery at the University of Cincinnati College of Medicine. In 1994 he joined the<br />
University of Washington School of Medicine in Seattle as Vice Chair of Surgery and Chief of Surgery at the Seattle VA Medical<br />
Center. In 2000 he became the Loyal and Edith Davis Professor and Chair of the Department of Surgery at Northwestern University in Chicago.<br />
Dr. Bell is a Past President of the Association for Academic Surgery (AAS) and the Central Surgical Association. He has served as Vice-President<br />
of the Society of Surgery for the Alimentary Tract (SSAT) and is a past member of the Board of Governors of the American College of<br />
Surgeons.<br />
He has a long-standing interest in pancreatic diseases and pancreatic cancer. He has written more than 150 articles and book chapters<br />
and edited a major textbook in digestive tract surgery and a surgical handbook. He has served on the editorial boards of the Journal of<br />
Gastrointestinal Surgery, Surgery, and Pancreas.<br />
Dr. Bell was recruited to the American Board of Surgery in August, 2006 to head up an effort to define and implement a national curriculum<br />
for residency training in general surgery.<br />
<strong>SAGES</strong> acknowledges our Diamond and Platinum Level Donors for their support of this lecture:<br />
Diamond: Covidien, Ethicon Endo-Surgery, Inc. and <strong>SAGES</strong> Education and Research Foundation<br />
Platinum: Karl Storz Endoscopy, Olympus<br />
The Marks Lecture – A History<br />
1987 Prof. William Wolfe<br />
(not named Marks Lecture in ‘87)<br />
1988 Prof. Worth Boyce<br />
1989 Prof. Peter Cotton<br />
1990 Prof. Alfred Cuschieri<br />
1991 Prof. George Berci<br />
1992 Prof. Theodore Schrock<br />
1993 Prof. John Terblanche<br />
2002 Prof. Hans G. Beger<br />
2003 Prof. R. Scott Jones<br />
2004 Prof. Jeffrey L. Ponsky<br />
2005 Prof. Andrew L. Warshaw<br />
2006 Prof. Gregory V. Stiegmann<br />
2007 Prof. Lester Rosen<br />
2008 Prof. James “Butch” Rosser<br />
2009 Prof. John Cameron<br />
10:00 AM - 2:30 PM<br />
Exhibits, Posters, Learning Center Open<br />
<strong>2010</strong> Poster Session<br />
Posters will be on display, Thursday, Friday & Saturday.<br />
Poster presenters will be available for Q&A on Friday, from 11:15 AM - 12:15 PM<br />
<strong>SAGES</strong> acknowledges our Diamond and Platinum Level Donors for their support of the poster session:<br />
Diamond: Covidien, Ethicon Endo-Surgery, Inc. and <strong>SAGES</strong> Education and Research Foundation<br />
Platinum: Karl Storz Endoscopy, Olympus<br />
A Gentle Reminder About Safety/Security:<br />
We have taken every precaution to assure the safety and security of our guests and their possessions.<br />
However, we urge you to be aware and take simple steps to guard your possessions.<br />
– Do not leave your purse or briefcase unattended.<br />
– Do not leave your laptop, phone or other electronic devices on the floor or out of your sight in a darkened room<br />
– Be aware of your surroundings, in the Gaylord Hotel, in and around the National Harbor area and in Washington, DC.<br />
Have a safe & secure meeting!<br />
12 th World Congress of Endoscopic Surgery 48
12 th World Congress of Endoscopic Surgery<br />
Friday, April 16, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
10:00 AM -11:00 AM *included in Registration SuperPass (Option A) or Registration Option C<br />
Concurrent Sessions (accepted oral & video presentations)<br />
SS03 Solid Organ<br />
Location: Maryland Ballroom B-D<br />
Moderators: Amir Szold, MD & Allan Siperstein, MD<br />
S004 UTILIZATION OF LAPAROSCOPIC SPLENECTOMY: AN ANALYSIS FROM THE NATIONAL SURGICAL QUALITY IMPROVEMENT<br />
PROGRAM DATABASE Vikram Attaluri, MD, Philip I Niles, BA, Louisa W Chiu, MD, Eric D Hixson, MBA, Haris Khwaja, MD, Steven Rosenblatt,<br />
MD, J Michael Henderson, MD, Allan Siperstein, MD, Cleveland Clinic, Cleveland, OH USA; Case Western School of Medicine and<br />
Weatherhead School of Management, Cleveland, OH USA<br />
S005 LAPAROSCOPIC ADRENALECTOMY FOR LARGE TUMORS. SINGLE TEAM EXPERIENCE. Abhay N Dalvi, MS, Pinky M Thapar, MS, Vinay<br />
M Thapar, MS, Sameer A Rege, MS, Seth G S Medical College & KEM Hospital, Mumbai, INDIA<br />
V012 PNEUMORETROPERITONEUM: AN ALTERNATIVE APPROACH FOR COMPLETION ADRENALECTOMY IN A HOSTILE ABDOMEN<br />
David E Skarda, MD, Martin Walz, MD, Sayeed Ikramuddin, MD, University of Minnesota, Minneapolis, USA, Kliniken Essen-Mitte, Essen,<br />
Germany<br />
S006 COMPARISON OF OPEN LIVE DONOR NEPHRECTOMY, LAPAROSCOPIC LIVE DONOR NEPHRECTOMY, AND HAND-ASSISTED LIVE<br />
DONOR NEPHRECTOMY: A COST-EFFECTIVENESS ANALYSIS Derek E Moore, MD MPH, Matthew Landman, MD, Deonna Moore, MSN,<br />
Irene Feurer, PhD, C W Pinson, MD MBA, Vanderbilt University Medical Center<br />
S007 MULTICENTER COMPARISON OF INTERMEDIATE ONCOLOGIC OUTCOMES OF LAPAROSCOPIC PARTIAL NEPHRECTOMY AND<br />
RENAL CRYOABLATION Sean Stroup, MD, John Malcolm, MD, James L’Esperance, MD, Robert Wake, MD, Michael Fabrizio, MD, Ithaar H<br />
Derweesh, MD, University of California San Diego, University of Tennessee at Memphis Health Science Center, Eastern Virginia Medical<br />
School<br />
V013 LAPAROSCOPIC BILATERAL PARTIAL ADRENALECTOMY FOR HEREDITARY PHEOCHROMOCYTOMA William W Hope, MD, Stanton T<br />
Smith, MD, Damon E Sheneman, DO, Jorge Gonzalez, MD, Cyrus A Kotwall, MD, New Hanover Regional Medical Center<br />
SS04 Basic Science<br />
Location: Maryland Ballroom A<br />
Moderators: Steven Stain, MD & Frederick Greene, MD<br />
S008 REAL-TIME INTRAOPERATIVE DETECTION OF TISSUE HYPOXIA IN ENDOSCOPIC GASTROINTESTINAL SURGERY BY A NOVEL<br />
WIRELESS PULSE OXIMETER (WIPOX) Elliot L Servais, MD, Nabil P Rizk, MD, Luis Oliviera, MS, Marom Bikson, PhD, Valerie W Rusch, MD,<br />
Prasad S Adusumilli, MD, Department of Thoracic Surgery, Memorial Sloan-Kettering Cancer Center; Department of Biomedical Engineering,<br />
City College of New York<br />
S009 A PILOT STUDY OF USING MULTIPHOTON MICROSCOPY TO DIAGNOSE GASTRIC CANCER Jun Yan, MD, Gang Chen, MD, Jianxin<br />
Chen, PhD, Shuangmu Zhuo, PhD, Hui Yu, MD, Mingang Ying, MD, Fujian Provincial Tumor Hospital, Fuzhou, 350014, China<br />
S010 EFFICACY OF TURMERIC (CURCUMIN) IN PAIN AND POSTOPERATIVE FATIGUE AFTER LAPAROSCOPIC CHOLECYSTECTOMY<br />
– A DOUBLE BLIND, RANDOMIZED PLACEBO CONTROLLED STUDY Krishna A Agarwal, C D Tripathi, MD, Brij B Agarwal, MS, VMMC &<br />
Safdarjung Hospital, Dr. Agarwal’s Surgery & Yoga and Sir Ganga Ram Hospital, New Delhi, India<br />
S011 3-CCD (CHARGE COUPLED DEVICE) IMAGE ENHANCEMENT FOR BOWEL ISCHEMIA John C Graybill, MD, Nicole Crane, PhD, Susan<br />
M Gillern, MD, Eric A Elster, MD, Jonathan P Pearl, MD, Naval Medical Research Center; National Naval Medical Center; Walter Reed Army<br />
Medical Center<br />
S012 SENSING FORCES IN NATURAL ORIFICE SURGERY Ana Luisa Trejos, MASc, Shiva Jayaraman, MD, Rajni V Patel, PhD, Michael D Naish,<br />
PhD, Christopher M Schlachta, MD, Canadian Surgical Technologies & Advanced Robotics (CSTAR), Lawson Health Research Institute.<br />
Departments of Electrical and Computer Engineering, Mechanical and Materials Engineering, Surgery, The University of Western Ontario,<br />
London, Ontario, Canada<br />
S013 DOWNREGULATION OF LEPTIN AND RESISTIN EXPRESSION IN BLOOD FOLLOWING BARIATRIC SURGERY Claire Edwards, MD,<br />
A. Katharine Hindle, MD, Sidney Fu, MD PhD, Fred Brody, MD MBA, Dept. of Surgery, Dept. of Biochemistry & Molecular Biology and<br />
McCormick Genomics Center, George Washington University Medical Center, Washington, DC<br />
Interactive Sessions: Featuring Google Moderator!<br />
Back by popular demand, <strong>SAGES</strong> is increasing the number of interactive sessions available for the<br />
<strong>2010</strong> meeting. All Scientific Sessions occurring in the MAIN SESSION Room Friday & Saturday,<br />
April 16-17, <strong>2010</strong> will feature Google Moderator, enabling attendees to participate in the<br />
presentation as it occurs! The audience will help determine the direction of the discussion by rating<br />
the submitted comments and suggestions. Moderators will address the highest rated questions.<br />
The room will be equipped with WIFI connectivity. Please bring your laptop and/ or iPhone/<br />
Android/Blackberry (newest generation or with Opera Mini).<br />
12 th World Congress of Endoscopic Surgery 50
Friday, April 16, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
10:00 AM - 11:00 AM *included in Registration SuperPass (Option A) or Registration Option C<br />
Endolumenal Therapies Session<br />
Chair: Dean J. Mikami, M.D.; Co-Chair: Simon Bergman, M.D.<br />
location: Potomac Ballroom C<br />
With the emergence of new technology and the refinement of old techniques, the field of endoscopy has rapidly evolved from simple<br />
diagnostics to cutting edge therapeutics. In this session, international experts will share their experience with endolumenal therapies in the<br />
care and management of patients suffering from morbid obesity and diseases of the foregut.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• Discuss the effectiveness of new endoscopic modalities in the treatment of morbid obesity and foregut disease<br />
• Identify the patients (and diseases processes) that are best suited for therapeutic management via the endolumenal approach<br />
• Describe the proper techniques and potential complications of endolumenal therapies<br />
Schedule<br />
10:00 AM Introduction Dean J. Mikami, M.D. & Simon Bergman, M.D.<br />
10:05 AM Endolumenal Bariatrics: Revisional Techniques Sergio Roll, M.D.<br />
10:15 AM Endolumenal Foregut: Established and Upcoming Technology W. Scott Melvin, M.D.<br />
10:25 AM EMR and ESD: Techniques, Tips, and Tricks Daniel von Renteln, M.D.<br />
10:45 AM Discussion<br />
10:00 AM - 11:00 AM *included in Registration SuperPass (Option A) or Registration Option C<br />
NOTES® Symposium – Alive & Well or RIP?<br />
Chair: David W. Rattner, M.D.; Co-Chair: G. V. Rao, M.D.<br />
location: Potomac Ballroom A-B<br />
Description:<br />
While intense interest continues in the development of NOTES®, its place as a useful therapy remains to be defined. Is NOTES® alive and well?<br />
Is it sleeping? Is it dead? This session seeks to provide insight into the current state of NOTES® and its potential for the future.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• Understand recent developments in NOTES®<br />
• Discuss if, when and how NOTES® will be added to the surgical armamentarium<br />
Schedule<br />
10:00 AM Introduction David W. Ratther, M.D. & G. V. Rao, M.D.<br />
10:05 AM Endolumenal or Translumenal Surgery Jeffrey Marks, M.D.<br />
10:15 AM Time to Abandon NOTES® and Perfect Single Port Surgery Paul G. Curcillo, M.D.<br />
10:25 AM NOTES® – Steady Progress Has Been Made Eric Hungness, M.D.<br />
10:35 AM NOTES® in 2020 Yoav Mintz, M.D.<br />
10:45 AM Discussion<br />
<strong>SAGES</strong> acknowledges educational grants in support of this World Congress symposium from Covidien, Ethicon Endo-Surgery, Inc. and Olympus.<br />
10:00 AM - 11:00 AM<br />
Laparoscopic Education Panel –<br />
Do MIS Fellowships Have a Future?<br />
Chair: Bruce D. Schirmer, M.D.; Co-Chair: Joseph Mamazza, M.D.<br />
location: Potomac Ballroom D<br />
This debate format session will focus on the current state of MIS fellowships in training: are they compatible with strong general surgery<br />
training programs, or do they conflict with them? Does the current and planned future training experience of general surgery residents<br />
suggest MIS fellowships are still needed?<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• Quantify the current breadth and depth of MIS training done by finishing residents of U.S. training programs<br />
• Describe evidence-based studies which suggest numbers necessary to achieve competence in any given operative procedure<br />
• Compare and contrast examples of training programs which have encountered conflicts between residents and MIS fellows and those<br />
that have not<br />
• Describe the current state of MIS fellowships in North America and their role in MIS training for the General Surgeon<br />
Schedule<br />
10:00 AM Introduction Bruce D. Schirmer, M.D. & Joseph Mamazza M.D.<br />
10:05 AM Can Residents Become Fully Skilled MIS Surgeons During Their Training? YES Fady Balaa, M.D.<br />
10:15 AM Can Residents Become Fully Skilled MIS Surgeons During Their Training? NO Rebecca Minter, M.D.<br />
10:25 AM Can a Good MIS Fellowship Co-Exist with a Residency Designed to Train MIS Surgeons? YES Peter Hallowell, M.D.<br />
10:35 AM Can a Good MIS Fellowship Co-Exist with a Residency Designed to Train MIS Surgeons? NO Ronnie Clements, M.D.<br />
10:45 AM Discussion<br />
<strong>SAGES</strong> acknowledges an educational grant in support of this World Congress panel from Ethicon Endo-Surgery, Inc.<br />
51 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
Friday, April 16, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
11:00 AM - 12:30 PM **Separate Registration Fee: $55<br />
Video Complications Luncheon:<br />
What Has Happened and What Do We Have to Do?<br />
Chair: Bipan Chand, M.D.; Co-Chair: Manabu Yamamoto, M.D.<br />
location: Maryland Ballroom C<br />
In this Lunch Session participants will watch popular and rare complications during laparoscopic surgery and discuss its prevention and<br />
solution.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• List the popular/rare complications of laparoscopic surgery<br />
• Discuss how to manage and prevent the complications<br />
• Lessen the complications to obtain better patient outcomes<br />
Schedule<br />
11:00 AM Introduction Bipan Chand, M.D. & Manabu Yamamoto M.D.<br />
11:05 AM GERD Lee L. Swanstrom, M.D.<br />
11:13 AM ARS<br />
11:20 AM Colon Steve D. Wexner, M.D.<br />
11:28 AM ARS<br />
11:35 AM Liver Go Wakabayashi, M.D.<br />
11:43 AM ARS<br />
11:50 AM Bariatric Kazunori Kasama, M.D.<br />
11:58 AM ARS<br />
12:05 PM Hernia Edward Phillips, M.D.<br />
12:13 PM ARS<br />
12:20 PM Discussion<br />
<strong>SAGES</strong> acknowledges our Diamond Level Donors for their support of this session:<br />
Covidien, Ethicon Endo-Surgery, Inc. and <strong>SAGES</strong> Education and Research Foundation.<br />
12:30 PM - 1:30 PM *included in Registration SuperPass (Option A) or Registration Option C<br />
Global Report from the Field Panel:<br />
Teaching Laparoscopic Surgery Abroad<br />
Chair: Raul Rosenthal, M.D.; Co-Chair: Horacio Asbun M.D.<br />
location: Maryland Ballroom A<br />
As a result of <strong>SAGES</strong> growth and evolution, our society has become one of the world’s leaders in minimally invasive and endoscopic surgery.<br />
The practice and evolution of minimally invasive surgery has been enriched by <strong>SAGES</strong> members from around the globe, and it is important<br />
to analyze the challenges that have occurred outside the United States and how <strong>SAGES</strong> has participated in helping overcome adversity. The<br />
Global Initiative program was conceived to participate in basic and advanced surgical education worldwide. This symposium will highlight<br />
the achievements of the Global Initiative since its inception and highlight how surgeons manage some unusual disease processes in other<br />
parts of the world.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• Understand sentinel contributions made by <strong>SAGES</strong> members in minimally invasive surgery worldwide<br />
• Identify contributions made by <strong>SAGES</strong> and the Global Initiative in implementing Minimally Invasive Surgical techniques in other countries<br />
• Discuss the impact and application of minimally invasive surgical techniques in other parts of the world<br />
Schedule<br />
12:30PM Introduction Raul Rosenthal, M.D. & Horacio Asbun, M.D.<br />
12:35 PM Can We Help Address the Worldwide Burden of Surgical Disease? Ramon Berguer, M.D.<br />
12:45 PM Problems and Solutions When Dealing with Laparoscopic Equipment:<br />
humanitarian and Military Experiences<br />
Steve Bowers M.D.<br />
12:55 PM A Trainer Perspective: Peru Experience Allan Okrainec, M.D.<br />
1:05 PM A Trainee Perspective: Peru Experience Edmundo Dedios, M.D.<br />
1:15 PM Discussion<br />
Evaluation & CME Credit Claim<br />
Visit the kiosks next to registration to complete<br />
your online evaluation and CME credit form on-site.<br />
Attendees may print CME certificates two weeks<br />
after the conclusion of the meeting.<br />
The programs and lectures presented at the <strong>2010</strong> World<br />
Congress Meeting are copyrighted products of the Society<br />
of American Gastrointestinal and Endoscopic Surgeons.<br />
Any reproduction or rebroadcasting without the express<br />
written consent of <strong>SAGES</strong> is strictly prohibited.<br />
12 th World Congress of Endoscopic Surgery 52
Friday, April 16, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
12:30 PM - 2:30 PM *included in Registration SuperPass (Option A) or Registration Option C<br />
Peer Review Training Session<br />
Chair: Abe L. Fingerhut, M.D.; Co-Chair: Sir Alfred Cuschieri, M.D.<br />
location: Maryland Ballroom B-D<br />
The peer review process has been critical to the dissemination of up-to-date scientific knowledge and best practices in medicine. This session<br />
outlines the issues involved in the peer review process as well as the intent. There will be didactic lectures and an examination and critique of<br />
several papers previously published in Surgical Endoscopy to provide a practical example to session attendees.<br />
Objectives: At the conclusion of this session, participants will be able to:<br />
• Describe what the peer review process entails • Incorporate ways of doing peer review well<br />
• Understand the critical importance and intent of peer review • Identify ethical issues regarding the peer review process<br />
Schedule<br />
1:00 PM Introduction Abe L. Fingerhut, M.D. & Sir Alfred Cuschieri, M.D.<br />
1:05 PM What is Peer Review? Kenneth A. Forde, M.D.<br />
1:15 PM What Do We Need It? Sir Alfred Cuschieri, M.D.<br />
1:25 PM How Should It Be Done? Abe L. Fingerhut, M.D.<br />
1:35 PM How to Learn to Do It Well Mark A. Talamini, M.D.<br />
1:45 PM Ethical Issues Peter Crookes, M.D.<br />
1:55 PM Discussion<br />
2:10 PM Examples of Articles Published in Surgical Endoscopy Faculty<br />
2:45 PM Discussion<br />
12:30 PM - 2:30 PM *included in Registration SuperPass (Option A) or Registration Option C<br />
<strong>SAGES</strong> Presidential Debates<br />
Chair: Daniel J. Deziel, M.D.; Co-Chair: Nathaniel J. Soper, M.D.<br />
location: Potomac Ballroom A-B<br />
Description:<br />
This popular session will address practical and philosphical issues that are important to <strong>SAGES</strong> surgeons in an animated and entertaining<br />
format.<br />
Objectives: At the conclusion of this session, participants will be able to:<br />
• Understand the relevant applications of robotics in general surgery<br />
• Discuss the issues pertinent to laparoscopic repair of groin hernias<br />
• Appreciate the practical and ethical concerns about reimbursement for investigational procedures and about the omnipresent<br />
dissemination of minimal access surgery<br />
Schedule<br />
12:30 PM Introduction Daniel J. Deziel, M.D. & Nathaniel J. Soper, M.D.<br />
Robotics: A Real Role in GI Surgery<br />
12:35 PM “Right On” Mark A. Talamini, M.D.<br />
12:45 PM “No Way” David W. Rattner, M.D.<br />
12:55 PM Discussion<br />
For My Groin Hernia...<br />
1:00 PM “Laparoscopy is Lovely” Desmond H. Birkett, M.D.<br />
1:10 PM “Laparoscopy is Ludicrous” Greg V. Stiegmann, M.D.<br />
1:20 PM Discussion<br />
Should Investigational Procedures be Reimbursed?<br />
1:25 PM “Yes” Steven D. Wexner, M.D.<br />
1:35 PM “No” Jeffrey H. Peters, M.D.<br />
1:45 PM Discussion<br />
The Title Bout<br />
1:50 PM “Laparoscopy Must be Universal” Lee Swanstrom, M.D.<br />
2:00 PM “Laparoscopy Cannot be Universal” Kenneth A. Forde, M.D.<br />
2:10 PM Discussion<br />
<strong>SAGES</strong> acknowledges our Silver Level Donors for their support of this debate: Boston Scientific, Davol Inc., a BARD Company, Gore & Associates<br />
12 th World Congress of Endoscopic Surgery<br />
Hotel Video Loop<br />
Attention Guests at the Gaylord Hotel: The World Congress <strong>Program</strong> Chairs have created an<br />
additional avenue for excellent videos to be viewed by meeting attendees. You may view these<br />
videos in your hotel rooms on Thursday, Friday, and Saturday. Please turn to channel 57 (subject<br />
to change) in your Gaylord Hotel room to view the <strong>2010</strong> Video Channel Loop videos. The Video<br />
Channel Loop listing is available on page 148 of your program.<br />
53 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Friday, April 16, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
1:30 PM - 2:30 PM *included in Registration SuperPass (Option A) or Registration Option C<br />
Conflict of Interest Panel<br />
Chair: Steve Eubanks, M.D.; Co-Chair: Neely Panton, M.D.<br />
location: Maryland Ballroom A<br />
Description:<br />
This panel provides a well-rounded perspective of the current issues that revolve around Conflict of Interest. The topics covered outline not<br />
only the pros and cons of the newly set rules for Physician-Industry Relationships, but also define avenues for healthy partnerships amidst<br />
strict regulations.<br />
Objectives: At the conclusion of this session, participants will be able to:<br />
• Identify the new Conflict of Interest rules affecting Physician-Industry relationships<br />
• Understand the impetus for current rules and oversight<br />
• Integrate new approaches to managing Conflict of Interest rules<br />
• Utilize effective strategies for coping with Conflict of Interest rules<br />
Schedule<br />
1:30 PM Introduction Steve Eubanks, M.D. & Neely Panton, M.D.<br />
1:35 PM The Current Status of Physician-Industry Relationships and Conflict of Interest (COI) Rules Gerald M. Fried, M.D.<br />
1:45 PM Why Physician-Industry Relationships Require Strict Conflict of Interest (COI) Rules and Oversight Michael D. Holzman, M.D.<br />
1:55 PM How Excessive COI Rules are Killing Healthy Physician-Industry Relationships R. Larry Whelan, M.D.<br />
2:05 PM Surviving and Succeeding in an Era of Tightened COI Regulations Bruce D. Schirmer, M.D.<br />
2:15 PM Discussion<br />
2:30 PM - 5:30 PM *included in Registration SuperPass (Option A) or Registration Option C<br />
Resident and Fellows Scientific Session<br />
Chair: Gregory F. Dakin, M.D.; Co-Chair: Adheesh A. Sabnis, M.D.<br />
location: Maryland Ballroom C<br />
In this session, selected residents and fellows will have the opportunity to present their research to a panel of distinguished faculty – all prominent<br />
surgeon-scientists who contribute regularly to the field of minimally invasive surgery. The panel will discuss and critique each presentation with<br />
a particular focus on study design, methodology, and critical review of results. Speakers will be judged not only on the content and originality of<br />
their work but on their presentation skills as well. An award for the best scientific presentation will be given at the conclusion of the session.<br />
Objectives: At the conclusion of this session, participants will be able to:<br />
• Describe methodological pitfalls that detract from scientific studies<br />
• Identify solutions to these problems and apple them in order to improve study design<br />
• Optimize communication and transfer of information in the context of a 10 minute presentation<br />
• Recognize the depth and complexity of current research endeavors of surgeons-in-training<br />
Schedule<br />
2:30 PM Introduction Gregory F. Dakin, M.D. & Adheesh A. Sabnis, M.D.<br />
Discussion<br />
Frederick L. Greene, M.D., Bruce MacFadyen, Jr., M.D., William Barry Inabnet, M.D.,<br />
William Traverso, M.D., Christopher Jamieson, M.D.<br />
S093 SINGLE INCISION LAPAROSCOPIC CHOLECYSTECTOMIES COST COMPARISON Katie Love, MD, Michael P Meara, MD, Christopher A<br />
Durham, MD, Curtis E Bower, MD FACS, ECU Brody School of Medicine<br />
S094 SINGLE-INCISION LAPAROSCOPIC SURGERY (SILS) VERSUS STANDARD LAPAROSCOPIC SURGERY: A COMPARISON OF<br />
PERFORMANCE USING A SURGICAL SIMULATOR Byron F Santos, MD, Daniel H Enter, BA, Nathaniel J Soper, MD, Eric S Hungness, MD,<br />
Northwestern University, Department of Surgery<br />
S095 DOES SPEED MATTER? THE IMPACT OF OPERATIVE TIME ON OUTCOMES IN LAPAROSCOPIC SURGERY Timothy D Jackson, MD<br />
MPH, Jeffrey J Wannares, BS, Robert T Lancaster, MD MPH, David W Rattner, MD, Matthew M Hutter, MD MPH, The Codman Center for<br />
Clinical Effectiveness in Surgery, Massachusetts General Hospital, Boston, MA<br />
S096 MORTALITY RISK ASSOCIATED WITH INSURANCE DENIALS IN BARIATRIC SURGERY CANDIDATES Raghid S Bitar, MD, Mastafa<br />
Springston, Geoffrey P Kohn, MD, Lindsee E McPhail, MD, David W Overby, MD, Timothy M Farrell, MD, University of North Carolina at Chapel<br />
Hill<br />
S097 INTRAOPERATIVE COLONOSCOPIES WITH LAPAROSCOPIC ASSISTANCE REDUCES UNNECESSARY BOWEL RESECTIONS AND<br />
HOSPITILIZATION Donald M Davis, MD, Valentine Nfonsam, MD, Jorge E Marcet, MD, Jared C Frattini, MD, University of South Florida<br />
S098 IMPROVING SURGICAL TRAINING; THE USE OF FEEDBACK TO REDUCE ERRORS AND IMPROVE RETENTION DURING A<br />
SIMULATED SURGICAL PROCEDURE E Boyle, MRCS, M Al-Akash, MRCS, O Traynor, FRCS, AG Gallagher, PhD Bsc, ADK Hill, MD FRCS, PC<br />
Neary, MD FRCS, National Surgical Training Centre, RCSI, Dublin, Ireland<br />
S099 SAFETY OF LAPAROSCOPIC PARAESOPHAGEAL HERNIA REPAIR IN OCTOGENARIANS Heidi L Fitzgerald, MD, Gina L Adrales, MD,<br />
Thadeus L Trus, MD, Song Li, BA, William S Laycock, MD, Dartmouth Hitchcock Medical Center<br />
S100 A COMPARATIVE STUDY OF HAND-SEWN VERSUS STAPLED GASTROJEJUNAL ANASTOMOSIS IN LAPARASCOPIC ROUX-EN-Y<br />
GASTRIC BYPASS Amanda J Kravetz, MD, Subhash Reddy, MD, Shean Satgunam, MD, Panduranga Yenumula, MD, Michigan State University<br />
Department of Surgery<br />
S101 HOW RELIABLE IS LAPAROSCOPIC COLORECTAL SURGERY COMPARED TO OPEN SURGERY FOR OCTOGENARIANS? Rodrigo A<br />
Pinto, Dan Ruiz, Yair Edden, Eric G Weiss, Juan J Nogueras, Steven D Wexner, Cleveland Clinic Florida<br />
S102 BARRETT’S ESOPHAGUS TREATMENT DILEMMA: PILLS VERSUS OPERATION: STATISTICAL ANALYSIS AND COST/EFFECTIVENESS<br />
Victor Bochkarev, MD, Dmitry Oleynikov, MD, UNMC<br />
<strong>SAGES</strong> acknowledges an educational grant in support of this World Congress session from Ethicon Endo-Surgery, Inc.<br />
12 th World Congress of Endoscopic Surgery 54
Friday, April 16, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
2:30 PM - 4:00 PM *included in Registration SuperPass (Option A) or Registration Option C<br />
Single Port Access Surgery Panel<br />
Chair: Joel Leroy, M.D.; Co-Chair: Andrew A. Gumbs, M.D.<br />
location: Potomac Ballroom A-B<br />
Description:<br />
Reduced port surgery has generated a tremendous amount of excitement in the surgical community. However, its clinical benefits remain<br />
poorly defined. This session will provide an update on the latest developments in this rapidly evolving area.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• Trace the history and evolution of Single Port Access Surgery in the spectrum of Minimally Invasive Surgery<br />
• Identify the key concepts in getting Single Port Access and the steps necessary to safely perform appendectomy, cholecystectomy, and<br />
colectomies<br />
• Discuss the indications for Single Port Access surgery and when to convert to multiple port laparoscopy<br />
• Recognize oncologic principles and pitfalls specific to Single Port Access surgery and indications/contraindications to Single Port Access<br />
surgery in cancer patients<br />
Schedule<br />
2:30 PM Introduction Joel Leroy, M.D. & Andrew A. Gumbs, M.D.<br />
2:35 PM The History of Single Port Access Surgery and Basic Technical Principles Paul G. Curcillo, M.D.<br />
2:45 PM Single Port Access Appendectomy Elie Chouillard, M.D.<br />
2:55 PM Single port Cholecystectomy: Techniques and Overview of the Literature Prashanth Rao, M.D.<br />
3:05 PM Single Port Access Bariatric Surgery:<br />
Gastric Sleeves and Laparoscopic Adjustable Gastric Band Placement<br />
Marc Bessler, M.D.<br />
3:15 PM Colorectal Surgery with Single Port: Techniques and Overview of the Indications Feza Remzi, M.D.<br />
3:25 PM Single Port Access in Endocrine Surgery (Adrenal, Spleen, Thyroid?) Eduardo Targarona, M.D.<br />
3:35 PM Single Port Surgery: A Step to NOTES® Ronan Cahill, M.D.<br />
3:45 PM Discussion<br />
<strong>SAGES</strong> acknowledges educational grants in support of this World Congress panel from Covidien, Ethicon Endo-Surgery, Inc. and Olympus.<br />
2:30 PM - 4:00 PM *included in Registration SuperPass (Option A) or Registration Option C<br />
Concurrent Sessions<br />
SS05 Hepatobiliary/Pancreatic<br />
Location: Maryland Ballroom B-D<br />
Moderators: Namir Katkhouda, MD & Brice Gayet, MD<br />
S014 COMMON BILE DUCT EXPLORATION IN DECLINE: MAJORITY OF THESE PROCEDURES ARE DONE IN NON-TEACHING HOSPITALS<br />
IN THE US. Samuel Jacob, MD, Marek Rudnicki, MD PhD, Metropolitan Group Hospitals/University of Illinois Surgery Residency <strong>Program</strong><br />
Chicago, USA<br />
S015 DISPARITIES IN ACCESS TO BASIC LAPAROSCOPIC SURGERY AT U.S. ACADEMIC CENTERS Esteban Varela, MD FACS, Ninh Nguyen,<br />
MD FACS, Department of Surgery, Washington University in St. Louis<br />
S016 REAL-TIME FLUORESCENCE IMAGING OF BILIARY ANATOMY DURING LAPAROSCOPIC CHOLECYSTECTOMY Nobumi Tagaya,<br />
PhD, Aya Nakagawa, PhD, Akihito Abe, PHD, Yoshimi Iwasaki, PhD, Mitsugi Shimoda, PhD, Masato Kato, PhD, Keiichi Kubota, phD, Second<br />
Department of Surgery, Dokkyo Medical University, Tochigi, Japan<br />
V014 LAPAROSCOPIC LEFT HEPATECTOMY WITHOUT INFLOW OCCLUSION USING MODIFIED ANTERIOR APPROACH C Palanivelu, MCh<br />
FACS FRCS, P Senthilnathan, MS DNB MRCS, N Anand Vijai, MS, R Rohit, MS, P Praveen Raj, MS, GEM Hospital<br />
S017 INITIAL EXPERIENCES IN 70 CASES OF TOTALLY LAPAROSCOPIC LIVER RESECTION FOR HCC Nguyen Hoang Bac, PhD, Tran Cong<br />
Duy Long, MD, Nguyen Duc Thuan, MD, Le Tien Dat, MD, Medical University Center at Hochiminh city<br />
S018 LAPAROSCOPIC MANAGEMENT OF CBD STONES: AN INDIAN EXPERIENCE Jagdish Chander, MD, Pawanindra Lal,<br />
MDDNBFRCSEdFRCSGlasg, Anubhav Vindal, MD, Vinod K Ramteke, MD, Maulana Azad Medical College, New Delhi, India<br />
S019 GERIATRIC SURGERY: IMPACT OF AGE ON THE OPERATIVE DECISION IN GALLSTONE DISEASE Simon Bergman, MD MSc, Nadia<br />
Sourial, MSc, Shannon A Fraser, MD MSc, Wael C Hanna, MD, Isabelle Vedel, MSc, Michèle Monette, Gabriela Ghitulescu, MD, Issie Weissglas,<br />
MD, Johanne Monette, MD, Department of Surgery, Sir Mortimer B. Davis Jewish General Hospital, Montreal, QC; Solidage Research Group<br />
on Frailty and Aging, Montreal, QC; Division of Geriatric Medicine, Sir Mortimer B. Davis Jewish General Hospital<br />
S020 IS THE USE OF T-TUBE NECESSARY AFTER LAPAROSCOPIC CHOLEDOCHOTOMY? Ahmed R El-Geidie, MD, Gastroenterology Surgical<br />
Center, Mansoura University, Egypt<br />
S021 BILE DUCT INJURY AFTER LAPAROSCOPIC CHOLECYSTECTOMY IN HOSPITALS WITH AND WITHOUT SURGICAL TRAINING<br />
PROGRAMS. IS THERE A DIFFERENCE? Vincent L Harrison, MD, Thai H Pham, MD, Brian S Diggs, PhD, Alexander J Greenstein, MD, James P<br />
Dolan, MD, Brett C Sheppard, MD, John G Hunter, MD, Oregon Health & Science University<br />
SS06 Hernia<br />
Location: Potomac Ballroom D<br />
Moderators: William Laycock, MD & Minhua Zheng, MD<br />
S022 EVALUATION OF INTRAPERITONEAL PLACEMENT OF ABSORBABLE AND NONABSORBABLE BARRIER COATED MESH SECURED<br />
WITH FIBRIN SEALANT (NEW ZEALAND WHITE RABBIT MODEL) Eric D Jenkins, MD, Lora Melman, MD, Salil Desai, BA, Shaun R Brown,<br />
DO, Margaret M Frisella, RN, Corey R Deeken, PhD, Brent D Matthews, MD, Department of Surgery, Washington University, St. Louis, Missouri<br />
S023 A PROSPECTIVE RANDOMIZED STUDY COMPARING SUTURE MESH FIXATION VS TACKER MESH FIXATION FOR LAPAROSCOPIC<br />
REPAIR OF INCISIONAL AND VENTRAL HERNIAS Mahesh C Misra, MS FRCS, Virinder K Bansal, MS, Subodh Kumar, MS, Keerthi Y Rao,<br />
MBBS, Department of Surgical Disciplines, All India Institute of Medical Sciences, Ansari Nagar, New Delhi, India<br />
55 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
Friday, April 16, <strong>2010</strong><br />
12 th World Congress of Endoscopic Surgery 56<br />
Scientific Sessions & Panels<br />
S024 OPEN VERSUS ENDOSCOPIC COMPONENT SEPARATION – A COST EFFECTIVENESS ANALYSIS Karem C Harth, MD MHS, Conor P<br />
Delaney, MD PhD, Johnie Rose, MD, Michael J Rosen, MD, University Hospital at Case Medical Center<br />
V015 LAPAROSCOPIC LUMBAR HERNIA REPAIR WITH BONE ANCHOR FIXATION Vanessa P Ho, MD, Gregory F Dakin, MD, Weill Cornell<br />
Medical College-NewYork Presbyterian Hospital<br />
S025 OUTCOMES OF LAPAROSCOPIC VENTRAL HERNIA REPAIR WITH ROUTINE DEFECT CLOSURE USING “SHOELACING” TECHNIQUE<br />
Sean B Orenstein, MD, Julie Monteagudo, Jillian Fortier, Mun Jye Poi, MD, Yuri W Novitsky, MD, Connecticut Comprehensive Center for<br />
Hernia Repair, Department of Surgery, University of Connecticut Health Center, Farmington, Connecticut<br />
S026 OPEN TENSION-FREE MESH-PLUG VERSUS TRANSABDOMINAL PREPERITONEAL(TAPP) VERSUS TOTALLY<br />
EXTRAPERITONEAL(TEP) LAPAROSCOPIC TECHNIQUES FOR PRIMARY UNILATERAL INGUINAL HERNIA REPAIR: A PROSPECTIVE<br />
RANDOMIZED CONTROLLED TRIAL Ke Gong, MD, Nengwei Zhang, MD, Yiping LU, MD, Zhanzhi Zhang, MD, Dexiao Du, MD, Beijing<br />
Shijitan Hospital, Beijing, China<br />
S027 A COMPARISON OF OUTCOMES IN OPEN VERSUS LAPAROSCOPIC SURGICAL REPAIR OF RECURRENT INGUINAL HERNIAS<br />
Nilay R Shah, MD, Clayton T Hodges, BS, Vanchad R Memark, MD, Eric T Volckmann, MD, Clinton R Hall, MD, Bradley J Needleman, MD,<br />
Dean J Mikami, MD, Jeffrey W Hazey, MD, W. Scott Melvin, MD, Vimal K Narula, MD, Center for Minimally Invasive Surgery, Division of<br />
Gastrointestinal Surgery, The Ohio State University Medical Center, Columbus, Ohio, USA<br />
S028 30-DAY READMISSION AFTER VENTRAL HERNIA REPAIR: PREDICTABLE OR PREVENTABLE? Jeffrey A Blatnik, MD, Karem C Harth,<br />
MD MHS, Mark I Aeder, MD, Michael J Rosen, MD, Department of Surgery, University Hospitals Case Medical Center, Cleveland, OH<br />
V016 RECONSTRUCTION OF THE ANTERIOR ABDOMINAL WALL WITH BILATERAL ENDOSCOPIC COMPONENT SEPARATION,<br />
LAPAROSCOPIC ASSISTED MEDIALIZATION OF THE RECTUS AND LAPAROSCOPIC MESH PLACEMENT Jawaid Kalim, MD, Scott Philipp,<br />
MD, Archana Ramaswamy, MD, University of Missouri, Columbia<br />
4:00 PM - 5:30 PM<br />
Concurrent Sessions<br />
SS07 Best of Video 2<br />
Location: Maryland Ballroom B-D<br />
Moderators: Natan Zundel, MD & David Hazzan, MD<br />
V017 SINGLE INCISION LAPAROSCOPIC RIGHT COLECTOMY Wai Lun Law, MD, Joe Fan, MD, Jensen Poon, MD, The University of Hong Kong<br />
V018 LAPAROSCOPIC REPAIR OF TRAUMATIC FLANK HERNIA Mun Jye Poi, MD, Yuri W Novitsky, MD, University Of Connecticut Health<br />
Center, Farmington, Connecticut<br />
V019 LAPAROSCOPIC REPAIR OF A DUODENAL ATRESIA AND LADD’S PROCEDURE IN A NEONATE Steven S Rothenberg, MD, Rocky<br />
Mountain Hospital For Children<br />
V020 LAPAROSCOPIC REPAIR OF ACUTELY INCARCERATED PARAESOPHAGEAL HERNIA Elizabeth Honigsberg, MD, Barry Salky, MD FACS,<br />
The Mount Sinai Hospital, New York<br />
V021 GALLBLADDER VOLVULUS: A VIDEO CASE REPORT Justin K Lawrence, MD, Nikhil Pawa, MD, Matthew G Tutton, MD, Antonio<br />
Privitera, MD, Colchester University Hospital, UK<br />
V022 TOTALLY EXTRAPERITONEAL REPAIR OF A SPIGELIAN HERNIA Frances Allocco, MD, Patrick Reardon, MD, Mohamed Saad, DO, Brian<br />
Dunkin, MD, The Methodist Hospital<br />
V023 LAPAROSCOPIC RESECTION OF A PRESACRAL SCHWANNOMA. Alexander Ramirez, Samuel Szomstein, Raul Rosenthal, Cleveland<br />
Clinic Florida<br />
SS08 Education/Simulation<br />
Location: Maryland Ballroom A<br />
Moderators: Teodor Grantcharov, MD & Michael Nussbaum, MD<br />
S029 SURGEON IMPRESSIONS AND TECHNICAL DIFFICULTY ASSOCIATED WITH LAPARO-ENDOSCOPIC SINGLE-SITE SURGERY:<br />
A <strong>SAGES</strong> LEARNING CENTER STUDY Antonio O Castellvi, MD, Arsalla Islam, MD, Seifu T Tesfay, RN, Alejandro D Castellvi, BS, Andrew S<br />
Wright, MD, Daniel J Scott, MD, Spartanburg Regional Medical Center, UT Southwestern Medical Center, St. Matthews Medical School,<br />
University of Washington<br />
S030 TRENDS AND RESULTS OF THE FIRST FIVE YEARS OF FUNDAMENTALS OF LAPAROSCOPIC SURGERY (FLS) CERTIFICATION<br />
TESTING Allan Okrainec, MD, Nathaniel J Soper, MD, Lee L Swanstrom, MD, Gerald M Fried, MD, University of Toronto, Toronto, ON,<br />
Northwestern University Feinberg School of Medicine, Chicago, IL, Legacy Health System, Portland, OR, and McGill University, Montreal, QC<br />
S031 A NATIONAL TRAINING PROGRAM FOR LAPAROSCOPIC COLORECTAL SURGERY IN THE UK Danilo Miskovic, MD FRCS, Susannah<br />
M Wyles, MSc MRCS, Mark G Coleman, MD FRCS, George B Hanna, PhD FRCS, Department of Biosurgery and Surgical Technology, Imperial<br />
College London/UK for the National Training <strong>Program</strong>me for Laparoscopic Colorectal Surgery<br />
S032 ANALYSIS OF STANDARD MULTI-PORT VS. SINGLE SITE ACCESS FOR LAPAROSCOPIC SKILLS TRAINING AND ACQUISITION Daniel<br />
R Cox, BS, Wenjing Zeng, BS, L Michael Brunt, MD, Washington University School of Medicine<br />
S033 A DEFICIENCY IN KNOWLEDGE OF BASIC PRINCIPLES OF LAPAROSCOPY AMONG ATTENDEES OF AN ADVANCED LAPAROSCOPIC<br />
SURGERY COURSE Carlos A Menezes, MD, Daniel W Birch, MD, Andrey Vizhul, MD, Xinzhe Shi, MPH, Vadim Sherman*, MD, Shahzeer<br />
Karmali, MD, Centre for the Advancement of Minimally Invasive Surgery, University Of Alberta, Edmonton, Alberta, Canada; *Baylor College<br />
of Medicine, Houston, Texas, USA.<br />
S034 EVALUATION OF SURGICAL PERFORMANCE DURING LAPAROSCOPIC INCISIONAL HERNIA REPAIR- A MULTICENTER STUDY Iman<br />
Ghaderi, MD, Marilou Vaillancourt, MD, Liane S Feldman, Gideon Sroka, MD, Pepa A Kaneva, MS, Melina C Vassiliou, MD, Jacob Seagull, PhD,<br />
Erica Sutton, MD, Carlos Godinez, MD, Ivan George, BSc, Adrian E Park, MD, Ian Choy, MD, Allan Okrainec, MD, Rita, Steinberg-Bernstein<br />
Centre for Minimally Invasive Surgery, McGill University, Montreal, QC, University of Western Ontario, London, ON, University of Maryland,<br />
Baltimore, MD, University of Toronto, Toronto, ON, Carolinas Medical Center, Charlotte, NC<br />
S035 SEX ISN’T EVERYTHING: THE ROLE OF GENDER IN EARLY PERFORMANCE OF A FUNDAMENTAL LAPAROSCOPIC SKILL Nicoleta O<br />
Kolozsvari, MD, Amin Andalib, MD, Pepa Kaneva, MSc, Jiguo Cao, PhD, Liane S Feldman, MD, Gerald M Fried, MD, Steinberg-Bernstein Centre<br />
for Minimally Invasive Surgery and Innovation, McGill University, Montreal, Qc, Canada
Friday, April 16, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
S036 A NOVEL SENSORIZED INSTRUMENT-BASED MINIMALLY INVASIVE SURGERY (SIMIS) TOOL: INITIAL CONSTRUCT VALIDATION OF<br />
FORCE SENSING Shiva Jayaraman, MD MESc, Ana Luisa Trejos, MASc, Andrew C Lyle, Michael D Naish, PhD, Rajni V Patel, PhD, Christopher<br />
M Schlachta, MD, CSTAR (Canadian Surgical Technologies & Advanced Robotics), Lawson Health Research Institute and Department of<br />
Surgery, Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Ontario, Canada<br />
S037 MENTORED TRAINEES OBTAIN COMPARABLE OPERATIVE RESULTS TO EXPERTS IN COMPLEX LAPAROSCOPIC COLORECTAL<br />
SURGERY Federico Costantino, MD, Jacopo D’Agostino, MD, Cosimo Callari, MD, Joël Leroy, MD, Hurng-Sheng Wu, MD, Didier Mutter, MD,<br />
Jacques Marescaux, MD, IRCAD, University Hospital of Strasbourg, France - Show Chwan Memorial Hospital, Changhua, Taiwan<br />
SS09 NOTES®<br />
Location: Potomac Ballroom D<br />
Moderators: W. Scott Melvin, MD & Dean Mikami, MD<br />
S038 TRANSGASTRIC APPROACH DOES NOT INCREASE POSTOPERATIVE INFECTIONS OR COMPLICATIONS IN SWINE UTERINE HORN<br />
RESECTION Asghar Azadani, MD, Henrik Jonsson, MD, Maria Bergstrom, MD PhD, Per-Ola Park, MD PhD, Dept of Surgery, Sahlgrenska<br />
University Hospital, Gothenburg, Sweden, Dept of Surgery, South Alvsborg Hospital, Boras, Sweden<br />
S039 STUDY OF HUMAN PERITONEAL BACTERIAL CONTAMINATION AFTER NOTES TRANSGASTRIC AND TRANSVAGINAL<br />
CHOLECYSTECTOMY Silvana Perretta, MD, Bernard Dallemagne, MD, Pierre Allemann, MD, Gianfranco Donatelli, MD, Cosimo Callari,<br />
MD, Hurng-Shen Wu, MD, Jacques Marescaux, MD, IRCAD, University Hospital of Strasbourg, France - Show Chwan Memorial Hospital,<br />
Changhua, Taiwan<br />
S040 PROSPECTIVE RANDOMIZED TRIAL COMPARING LAPAROSCOPIC AND NOTES CHOLECYSTECTOMY: PRELIMINARY RESULTS<br />
Alberto R Ferreres, MD PhD MPH FACS, Anibal Rondán, MD, Santiago Horgan, MD, Julieta Paleari, MD, Mariano E Giménez, MD, Oscar O<br />
Laudanno, MD, Vicente P Gutiérrez, Department of Surgery. University of Buenos Aires<br />
V024 ENDOSCOPIC TRANSESOPHAGEAL MEDIASTINAL AND THORACIC LYMPH NODE DISSECTION WITH EN BLOC RESECTION (VIDEO<br />
SUBMISSION) Brian G Turner, MD, Denise W Gee, MD, Sevdenur Cizginer, MD, Min-Chan Kim, MD, Yusuf Konuk, MD, Mari Mino-Kenudson,<br />
MD, Patricia Sylla, MD, David W Rattner, MD, William R Brugge, MD FASGE, (1) Gastrointestinal Unit, Massachusetts General Hospital, (2)<br />
Department of Surgery, (3) Department of Pathology, Massachusetts General Hospital, Boston, MA<br />
S041 FIRST HUMAN EXPERIENCE WITH ENDOLUMINAL, ENDOSCOPIC GASTRIC BYPASS Bryan J Sandler, MD, C. Paul Swain, MD, Roberto<br />
Rumbaut, MD, Gustavo Torres, MD, Luis Morales, MD, Lizcelly Gonzales, MD, Santiago Horgan, MD, University of California, San Diego, San<br />
Diego, CA, USA; Imperial College of London, London, England; San Jose Tec de Monterrey, Monterrey, Mexico<br />
S042 ESOPHAGEAL STENT PLACEMENT PROVIDES SAFE CLOSURE FOLLOWING TRANSESOPHAGEAL ACCESS FOR NOTES® THORACIC<br />
PROCEDURES Brian G Turner, MD, Denise W Gee, MD, Min-Chan Kim, MD, Sevdenur Cizginer, MD, Mari Mino-Kenudson, MD, Patricia<br />
Sylla, MD, David W Rattner, MD, William R Brugge, MD FASGE, (1) Gastrointestinal Unit, Dept of Medicine, (2) Department of Surgery, (3)<br />
Department of Pathology, Massachusetts General Hospital, Boston, MA<br />
S043 QUANTITATIVE ERGONOMICS ASSESSMENT OF NOTES TECHNIQUES: A STUDY OF PHYSICAL WORKLOAD, BODY MOVEMENT<br />
AND POSTURE Gyusung Lee, PhD, Erica Sutton, MD, Yassar Youssef, MD, Tameka Clanton, MS, Adrian Park, MD, University of Maryland<br />
S044 PROSPECTIVE NON-RANDOMIZED STUDY OF ENDOSCOPIC TRANSVAGINAL CHOLECYSTECTOMY VERSUS LAPAROSCOPIC<br />
CHOLECYSTECTOMY José F Noguera, MD PhD, Angel Cuadrado, MD PhD, Carlos Dolz, MD, José M Olea, MD, Rafael Morales, MD, Luis C<br />
Lozano, MD, José C Vicens, MD, Hospital Son Llàtzer<br />
V025 LAPAROSCOPIC SLEEVE GASTRECTOMY AS A TREATMENT OPTION FOR ACUTE GASTRIC FUNDUS NECROSIS AFTER<br />
LAPROSCOPIC REDO PARAESOPHAGEAL HERNIA REPAIR AND SLIPPED REDO NISSEN FUNDOPLICATION Ismael Court, Omar Bellorin,<br />
Sheetal Patel, Samuel Szomstein, Raul J Rosenthal, Cleveland Clinic Florida<br />
12 th World Congress of Endoscopic Surgery<br />
Pencil us in for next year:<br />
CAGS Canadian Surgery Forum<br />
September 2 - 5, <strong>2010</strong>, Québec City Convention Centre, Canada<br />
<strong>SAGES</strong> Scientific Session & Postgraduate Course<br />
March 30 - April 2, 2011, San Antonio, Texas<br />
IMPORTANT AV INFORMATION:<br />
You may now upload your presentation on line at any point during the meeting. Please load your<br />
presentation online (http://sages.presentationman.com/) or on the show computer in the Speaker<br />
Prep room no later than 2 hours before your presentation.<br />
Please Note: Even if you have submitted your presentation online you must visit the Speaker Prep<br />
room to check in, your session moderator may not allow you to present if you do not.<br />
Speaker Prep Hours:<br />
4/13/10: 7:00 am - 5:00 pm<br />
4/14/10: 5:30 am - 5:00 pm<br />
4/15/10: 6:00 am - 5:00 pm<br />
4/16/10: 5:30 am - 5:30 pm<br />
4/17/10: 5:30 am - 5:00 pm<br />
57 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Friday, April 16, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
2:30 PM - 5:30 PM *included in Registration SuperPass (Option A) or Registration Option C<br />
Emerging Technology Session<br />
Chair: Steven D. Schwaitzberg, M.D.; Co-Chair: Alex Gandsas, M.D.<br />
location: Potomac Ballroom C<br />
For the 6th year, <strong>SAGES</strong>, as part of the <strong>SAGES</strong> Technology Initiative, will present the Emerging Technology Session. Surgeons, physicians,<br />
scientists from academic centers as well as industry are invited to submit abstracts for consideration. Submissions that reflect “late braking”,<br />
“cutting-edge” or novel information are greatly encouraged. Submission of preliminary results for new technologies is encouraged as well.<br />
<strong>SAGES</strong> does NOT offer CME for this session.<br />
ET01 NOVEL HANDHELD PET PROBES PROVIDE INTRAOPERATIVE LOCALIZATION OF MALIGNANT LYMPH NODES Segundo J Gonzalez,<br />
MD, Joyce Wong, MD, Lorena Gonzalez, MD, Peter Brader, MD, Mithat Gönen, Maureen Zakowski, MD, Yuman Fong, MD, Vivian Strong, MD,<br />
Departments of Surgery,1 Radiology,2 Pathology,3 and Epidemiology and Biostatistics,4; Memorial Sloan-Kettering Cancer Center, New<br />
York, NY, 10065 USA<br />
ET02 SINGLE CENTER EXPERIENCE WITH A NOVEL PURELY ENDOLUMINAL FUNDOPLICATION DEVICE Ozanan R Meireles, MD, Julietta<br />
Paleari, MD, Noam Belkind, MD, Kari Thompson, MD, Michael Sedrak, MD, Garth Jacobsen, MD, Mark A Talamini, MD, Santiago Horgan, MD,<br />
University of California-San Diego<br />
ET03 CLEANOSCOPE: A CLEAR IMAGE AT ALL TIMES Barry Salky, MD, Daniel Sherwin, Mr, Ori Nesher, Mr, Noam Danenberg, Mr, Gadi Lotan,<br />
MD, Cleanoscope, Ltd; The Mount Sinai Hospital, New York<br />
ET04 LAPAROSCOPIC INFRARED IMAGING – THE FUTURE VASCULAR MAP Noam Shussman, MD, Mahmoud Abu Gazala, MD, Avraham<br />
Schlager, MD, Ram Elazary, MD, Abed Khalaileh, MD, Gideon Zamir, MD, Avraham I Rivkind, MD FACS, Yoav Mintz, MD, Department of<br />
General Surgery, Hadassah Hebrew University Medical Center, Jerusalem, Israel<br />
ET05 TRANSGASTRIC SMALL BOWEL RESECTION WITH A NEW MULTITASKING PLATFORM ENDOSAMURAI(TM) Karl H Fuchs, Wolfram<br />
Breithaupt, title, Markus-Krankenhaus, Dept of Surgery<br />
ET06 A NOVEL FLEXIBLE BIPOLAR HEMOSTASIS FORCEPS (BELA, ETHICON ENDO-SURGERY, NOTES TOOLBOX) OVERCOMES THE<br />
CURRENT SHORTCOMINGS OF ENDOSCOPIC ZENKER´S DIVERTICULOTOMIES: AN EXPERIMENTAL MODEL. Erwin Rieder, MD, Danny V<br />
Martinec, BS, Christy M Dunst, MD, Lee L Swanstrom, MD, Dept. of Minimally Invasive Surgery, Legacy Health, Portland, OR<br />
ET07 INSERTABLE ROBOTIC EFFECTOR PLATFORM Dennis L Fowler, MD MPH, Peter Allen, PhD, Jayson Ding, PhD, Roger Goldman, BA,<br />
Austin Reiter, BA, Nabil Simaan, PhD, Columbia University<br />
ET08 INTRA-LUMINAL INJECTION OF FERROMAGNETIC GLUE-BASED MEDIA FOR BOWEL RETRACTION IN LAPAROSCOPIC SURGERY<br />
Z Wang, PhD, A W Brown, S I Brown, PhD, D Liu, L Wang, PhD MD, A Cuschieri, Professor, Institute for Medical Science and Technology,<br />
University of Dundee, UK<br />
ET09 “THE DUNDEE ENDOCONE”: A NEW REUSABLE SILS DEVICE Andrea Pietrabissa, MD, Mario Alessiani, MD, Andrea Peri, MD, Sandro<br />
Zonta, MD, Lorenzo Cobianchi, MD, Paolo Dionigi, MD, SI Brown, MD, TG Frank, MD, Alfred Cuschieri, MD, Department of Surgical Science,<br />
University of Pavia; Institute for Medical Science and Technology - Dundee U.K<br />
ET10 FLEXIBLE CO2 LASER AND SUBMUCOSAL GEL INJECTION FOR SAFE ENDOSCOPIC AND LAPAROSCOPIC SURGERY OF THE<br />
INTESTINES Joyce T Au, MD, Arjun Mittra, MD, Joyce Wong, MD, Iain Nixon, MD, Paula Ezell, DVM, Snehal Patel, MD, Yuman Fong, MD,<br />
Memorial Sloan Kettering Cancer Center<br />
ET11 TOWARDS INTRA OPERATIVE DIAGNOSIS OF MESENTERIC TISSUE OXYGENATION WITH HYPERSPECTRAL IMAGING David James,<br />
MRCS MBBS BSc, Vincent Sauvage, Neil T Clancy, James Clark, MRCS MBBS, Ara W Darzi, KBE FRCS FACS MD, Guang-Zhong Yang, PhD, Daniel<br />
S Elson, PhD, Dept. Biosurgery and Surgical Technology and Institute of Biomedical Engineering, Imperial College, London<br />
ET12 LAPAROSCOPIC INTESTINAL ANASTOMOSIS WITH THE CAIMAN LEKTRAFUSE DEVICE Dirk W Meijer, MD MSc PhD, H Jaap Bonjer,<br />
MD PhD, BRG, VUMC<br />
ET13 NOVEL METHODOLOGY FOR COMPARING TISSUE ANALOGS Jenna Turocy, John Hryb, Danyel Racenet, Andrew Miesse, Thomas<br />
Wenchell, Covidien<br />
ET14 BETA TESTING OF A V-BAND SIMULATOR Jamie D Adair, MD, Ganesh Sankaranarayanan, PhD, Tansel Halic, MS, Zhonghua Lu,<br />
MS, Woojin Ahn, PhD, Mark A Gromski, BA, Daniel B Jones, MD, Suvranu De, ScD, Beth Israel Deaconess Medical Center and Rensselaer<br />
Polytechnic Institute<br />
ET15 WIRELESS ENDOLUMINAL APPLICATION OF A MAGNETIC DRIVEN CAMERA Nicola Di Lorenzo, MD Phd, Arianna Menciassi, Prof,<br />
Pietro Valdastri, Eng Phd, Livia Cenci, MD, Luca Iezzi, Eng Phd, Achille Lucio Gaspari, Prof, Paolo Dario, Prof, Scuola superiore Sant’ Anna Pisa -<br />
Department of surgey-University of Rome Tor Vergata<br />
ET16 AUGMENTED REALITY SYSTEM FOR ENDOSCOPIC AND NOTES PROCEDURES Luc Soler, PhD, Vincent Agnus, PhD, Stephane<br />
Nicolau, PhD, Julien Waechter, Eng, Oliver Burckhardt, MD, Silvana Perretta, MD, Bernard Dallemagne, MD, Didier Mutter, MD PhD, Jacques<br />
Marescaux, MD, IRCAD<br />
ET17 360° IMMERSIVE PANOMORPH ENDOSCOPIC DEVICE: A NEW ADVANCED VISION SYSTEM CONCEPT Pierre Garneau, MD, Patrice<br />
Roulet, Pierre Konen, Mathieu Villegas, Simon Thibault, MSc PhD ing, Sacré-Coeur Hospital of Montreal, ImmerVision, Université Laval<br />
ET18 ROBOTIC TRANSAXILLARY THYROIDECTOMY: REPORT OF TWO CASES AND DESCRIPTION OF THE TECHNIQUE Katherine B<br />
Heiden, MD, Allan Siperstein, MD, Mira Milas, MD, Joyce Shin, MD, Jamie Mitchell, MD, Eren Berber, MD, Cleveland Clinic<br />
ET19 TRANS-ORAL ENDOSCOPIC RESTRICTIVE IMPLANT SYSTEM (TERIS) FOR THE TREATMENT OF MORBID OBESITY: A 12 MONTHS<br />
REVIEW OF SAFETY AND RESULTANT WEIGHT LOSS Fady Moustarah, MD MPH, Stéfane Lebel, MD, Laurent Beirtho, MD, Frédéric-Simon<br />
Hould, MD, Simon Biron, MD, Institut Universitaire de Cardiologie et de Pneumologie de Québec, Université Laval<br />
ET20 HEMORRHOIDAL LASER PROCEDURE (HELP) IN THE TREATMENT OF SYMPTOMATIC HEMORRHOIDS Paolo Giamundo, MD, Maria<br />
Geraci, MD, Livio Tibaldi, MD, Marco Valente, MD, Department of General Surgery -Hospital S. Spirito - Bra (CN) - ITALY<br />
12 th World Congress of Endoscopic Surgery 58
Friday, April 16, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
ET21 TRANSCOLONIC NOTES- PRELIMINARY HUMAN EXPERIENCE: NOTES TRANSRECTAL RECTOSIGMOID RESECTION AND TME<br />
Ricardo Zorron, Djalma Coelho, Luciana Flach, Fabiano Lemos, Moacyr Moreira, Priscila Oliveira, Alain Barbosa, Department of Surgery –<br />
University Hospital Teresópolis HCTCO-FESO;Hospital Municipal Lourenco Jorge, Rio de Janeiro, Brazil<br />
ET22 DUAL CONSOLE ROBOTIC SURGERY ENHANCES OPERATIVE TASK EFFICIENCY Michael M Awad, MD PhD, Eric Jenkins, MD, Lora<br />
Melman, MD, Brent Matthews, MD, Washington University in St. Louis - School of Medicine<br />
<strong>SAGES</strong> acknowledges our Gold Level Donors for their support of this World Congress session: Ascent Healthcare Solutions, Stryker Endoscopy<br />
Friday Evening<br />
6:00 PM - 7:00 PM<br />
Meet the Leadership Reception For<br />
Residents, Fellows & New Members<br />
Location: Pose, 18-19 th Floor<br />
Water Taxi Service<br />
In addition to cabs and rental cars, the National Harbor offers a fun and practical way to get to various<br />
destinations…a water taxi! Water taxi service is available to and from points around Washington D.C., Virginia<br />
and Maryland for your convenience. The Potomac Riverboat Company operates water taxi service between<br />
National Harbor and Old Town Alexandria, with additional boat service to Mount Vernon and Georgetown. Water<br />
taxis will run every half hour between National Harbor and Old Town Alexandria. There will be three daily trips to<br />
Georgetown’s Washington Harbor, and a single daily trip to George Washington’s Mount Vernon Estate. Ask the<br />
concierge for more information and about pricing.<br />
<strong>2010</strong> World Congress International Webcast Sessions<br />
To participate in the International Webcast Sessions, please visit:<br />
http://www.sages.org/meetings/annual_meeting/<strong>2010</strong>/<br />
Password: sages<br />
Friday, April 16, <strong>2010</strong><br />
TIME SESSION CHAIR (S)/SPEAKER<br />
8:00 am- 9:00 am Plenary Session C. Daniel Smith, MD & C. Jamieson, MD<br />
9:00 am - 9:30 am <strong>SAGES</strong> Presidential Address C. Daniel Smith, MD<br />
9:30 am - 10:00 m Gerald Marks Keynote Lecture Richard H. Bell, MD<br />
10:00 am - 11:00 am Symposium: NOTES® - Alive and Well, or RIP?<br />
12:30 pm - 2:30 pm Presidential Debates<br />
2:30 pm - 4:00 pm Panel: Single Port Access Surgery<br />
Saturday, April 17, <strong>2010</strong><br />
Chair: David W. Rattner, MD<br />
Co-chair: Venkat G. Rao, MD<br />
Chair: Daniel J. Deziel, MD<br />
Co-chair: Nathaniel Soper, MD<br />
Chair: Joel Leroy, MD<br />
Co-chair: Andrew A. Gumbs, MD<br />
TIME SESSION CHAIR (S)/SPEAKER<br />
7:00 am - 8:30 am Live from Afghanistan Session: Video Conference Military Coalition<br />
Chair: Steven P. Bowers, MD<br />
Co-chair: Richard M. Satava, MD<br />
8:30 am - 9:00 am Karl Storz Keynote Lecture Christopher J. Gostout, MD<br />
9:00 am - 9:30 am CAGS / Royal College of Surgeons Lecture Robert DiRaddo, Ph.D.<br />
9:30 am - 11:00 am Plenary Session II Moderators: J. Buyske, MD & A. Chousleb, MD<br />
12 th World Congress of Endoscopic Surgery<br />
<strong>SAGES</strong> gratefully acknowledges Covidien, Ethicon Endo-Surgery, Inc. and the <strong>SAGES</strong> Education & Research Foundation<br />
for their generous support towards the <strong>SAGES</strong> Global Proctoring Initiative.<br />
59 www.12thworldcongress.org
Saturday, April 17, <strong>2010</strong><br />
Time Session Location<br />
7:00 AM - 8:30 AM<br />
Live From Afghanistan Session:<br />
Video Conference Military Coalition<br />
Hernia Debates Panel:<br />
7:00 AM - 8:30 AM<br />
What Has Happened and What Do We Have to Do?<br />
Karl Storz Lecture: New Trends in Endoscopy – What<br />
8:30 AM - 9:00 AM Technology and Techniques are in it for You?<br />
Christopher J. Gostout, M.D.<br />
The Royal College of Physicians and<br />
9:00 AM - 9:30 AM Surgeons of Canada Lecture<br />
VR Systems for Surgical Oncology<br />
Robert DiRaddo, Ph.D.<br />
Scientific Sessions & Panels<br />
Potomac Ballroom A-B<br />
Potomac Ballroom C<br />
Potomac Ballroom A-B<br />
Potomac Ballroom A-B<br />
9:30 AM - 11:00 AM SS10 Plenary Session 2 Potomac Ballroom A-B<br />
10:00 AM - 1:00 PM<br />
Last Chance to Visit Exhibits, Posters, Learning Center<br />
Open – Please note 1:00 PM Closing Time!<br />
11:00 AM - 11:30 AM<br />
<strong>SAGES</strong> Annual General Membership Business Meeting<br />
All <strong>SAGES</strong> Members Encouraged to Attend!<br />
11:00 AM - 1:00 PM BREAK: Exhibits, Posters & Learning Center Open<br />
11:30 AM - 12:30 PM<br />
FREE Lunch in Exhibit Hall for all World Congress<br />
Scientific Session Registrants!<br />
11:30 AM - 1:00 PM<br />
Fellowship Council Luncheon<br />
The Future of Fellowships: How Will They Be Funded<br />
Prince George’s Exhibit Hall A-C<br />
Potomac Ballroom C<br />
Maryland Ballroom C<br />
1:00 PM - 3:00 PM “Uh Oh! What Now?” Video Panel Potomac Ballroom C<br />
1:00 PM - 3:00 PM CAGS Simulation in the Training of Surgeons Session Maryland Ballroom B-D<br />
1:00 PM - 3:00 PM FES Roll-Out Session Maryland Ballroom A<br />
1:00 PM - 5:00 PM Concurrent Sessions (accepted oral & video presentations)<br />
1:00 PM - 2:00 PM SS11 Robotics Maryland Ballroom B-D<br />
12 th World Congress of Endoscopic Surgery<br />
1:00 PM - 3:00 PM SS12 Bariatric Potomac Ballroom A-B<br />
2:00 PM - 3:00 PM SS13 Research Grant Presentations Maryland Ballroom B-D<br />
3:00 PM - 4:00 PM SS14 Complications/Ergonomics/Instruments Maryland Ballroom B-D<br />
3:00 PM - 5:00 PM SS15 Esophageal/Gastric Potomac Ballroom D<br />
3:00 PM - 5:00 PM SS16 Colorectal Potomac Ballroom C<br />
3:00 PM - 5:00 PM SS17 Best of Video 3 Potomac Ballroom A-B<br />
3:00 PM - 5:00 PM IFSES Surgical Education Around the World Panel Maryland Ballroom A<br />
7:30 PM - 11:00 PM<br />
World Congress Gala, Featuring Dinner &<br />
the International Sing-Off<br />
Shuttles begin departing at 7:15 PM at the Bus Pickup are of the Gaylord<br />
hotel ONLY. Go to the Group Bus Loading area, located at the Woodrow<br />
Wilson exit on the 2nd level, opposite of guest parking. Buses will circle all<br />
evening until the event ends.<br />
Newseum<br />
<strong>2010</strong> Poster Session<br />
Posters will be on display, Thursday, Friday & Saturday.<br />
Poster presenters will be available for Q&A on Friday, from 11:15 AM - 12:15 PM<br />
<strong>SAGES</strong> acknowledges our Diamond and Platinum Level Donors for their support of the poster session:<br />
Diamond: Covidien, Ethicon Endo-Surgery, Inc. and <strong>SAGES</strong> Education and Research Foundation<br />
Platinum: Karl Storz Endoscopy, Olympus<br />
61 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Saturday, April 17, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
7:00 AM - 8:30 AM *included in Registration SuperPass (Option A) or Registration Option C<br />
Live From Afghanistan Session:<br />
Video Conference Military Coalition<br />
Chair: COL (ret) Steven P. Bowers, M.D.; Co-Chair: COL (ret) Richard M. Satava, M.D.<br />
location: Potomac Ballroom A-B<br />
Description:<br />
The military has adapted laparoscopic and endoscopic technologies to the battlefield setting. This session will provide a unique window into<br />
how active duty military personnel use new surgical technologies in challenging environments.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• To understand how the military uses minimally invasive surgical techniques<br />
• To learn how surgery in challenging military environments differs from the elective setting<br />
Schedule<br />
7:00 AM Introduction<br />
7:05 AM Live from Salerno Afghanistan – Use of MIS and Endoscopy in the Field Hospital Josh Alley, M.D., USAF<br />
7:20 AM Live from Kandahar – Humanitarian Care and Care of Host Nationals Ron Brisebois, M.D., Canadian Forces<br />
7:35 AM Management of the Abdominal Wall in Combat Casualties Scott Rehrig, M.D., Army<br />
7:50 AM Military Battlefield Surgery Hon Ward Casscels, Immediate Assistant Secretary of Defense for Health Affairs<br />
8:20 AM Discussion<br />
7:00 AM - 8:30 AM *included in Registration SuperPass (Option A) or Registration Option C<br />
Hernia Debates Panel:<br />
What Has Happened and What Do We Have to Do?<br />
Chair: Guy R. Voeller, M.D.; Co-Chair: Edward H. Phillips, M.D.<br />
location: Potomac Ballroom C<br />
Description:<br />
Is laparoscopic therapy for the treatment of hernia better, worse, or equivalent to the open approach? This question remains incompletely<br />
answered even in 2009. This panel will address recent advances in the evaluation and treatment of inguinal, paraeshophageal, incisional and<br />
sportsman’s hernia.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• Learn treatment options for sportsman hernia<br />
• Learn the best surgical approach for paraesophageal hernia repair<br />
• Learn if mesh fixation is required for laparoscopic inguinal hernia repair<br />
• Learn if lapaoroscopic repair of incisional hernia adequately reconstructs the abdominal wall<br />
Schedule<br />
7:00 AM Introduction Guy R. Voeller, M.D. & Edward H. Phillips, M.D.<br />
Debate 1 – Biologic Mesh Should Be Widely Applied<br />
7:05 AM Biologic Mesh Should Be Widely Applied TBA<br />
7:15 AM Biologic Mesh Should NOT Be Widely Applied Shirin Towfigh, M.D.<br />
Debate 2 – Paraesophageal Hiatal Hernia<br />
7:25 AM Laparoscopic Approach is Preferred James D. Luketich, M.D.<br />
7:35 AM Open Thoracic Approach is Preferred Jeffrey Peters, M.D.<br />
Debate 3 – Fixation of Mesh for Laparoscopic Inguinal Hernia Repair<br />
7:45 AM Fixation of Mesh is Required Bruce Ramshaw, M.D.<br />
7:55 AM Fixation of Mesh is Not Required Craig Taylor, M.D.<br />
Debate 4 – Laparoscopic Repair of Incisional Hernia Cannot Adequately Reconstruct the Abdominal Wall<br />
8:05 AM Agree and Believe the Open Approach is Preferred Jean Bernard Flament, M.D.<br />
8:15 AM Disagree and Believe the Laparoscopic Approach is Preferred Michael J. Rosen, M.D.<br />
8:25 PM Discussion<br />
<strong>SAGES</strong> acknowledges educational grants in support of this World Congress panel from Covidien and Gore & Associates.<br />
12 th World Congress of Endoscopic Surgery 62
Saturday, April 17, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
8:30 AM - 9:00 AM *included in Registration SuperPass (Option A) or Registration Option C<br />
Karl Storz Lecture: New Trends in Endoscopy –<br />
What Technology and Techniques are in it for You? Location: Potomac Ballroom A-B<br />
Christopher J. Gostout, M.D.<br />
Mayo Clinic, Rochester, MN<br />
Associate Professor of Medicine, Mayo Clinic<br />
Dr. Gostout attended Medical School at the State University of New York, Brooklyn, NY and completed is residency at the Mayo<br />
Graduate School of Medicine, Mayo Clinic, Rochester, MN<br />
His clinical and research interests have been therapeutic endoscopy, gastroenterology and hepatology. His work in innovative<br />
flexible endoscopic procedures has made him a leader in his field. Dr. Gostout served as President, American Society for<br />
Gastrointestinal Endoscopy, in 2004-2005.<br />
He has 187 peer reviewed papers and has presented all over the world. He holds two US Patents<br />
- Apparatus and methods for internal surgical procedures 03-12-2009 and (2) Methods And<br />
- Systems For Performing Submucosal Medical Procedures 01-15-2009.<br />
His recent research protocols include: Function and comparative evaluation of flexible monopolar endoscopic scissors; Anatomical<br />
Considerations for NOTES® surgery<br />
9:00 AM - 9:30 AM *included in Registration SuperPass (Option A) or Registration Option C<br />
The Royal College of Physicians and Surgeons of Canada Lecture<br />
VR Systems for Surgical Oncology<br />
Location: Potomac Ballroom A-B<br />
Robert DiRaddo, Ph.D.<br />
Group Leader, Simulation of Deformable Materials<br />
National Research Council of Canada<br />
Robert DiRaddo graduated from McGill University in Engineering in the early 1980’s. He obtained his PhD in Engineering in the use<br />
of computer-systems for manufacturing processes. Dr DiRaddo worked in the petrochemical sector for several years, before joining<br />
the National Research Council of Canada (NRC). He currently leads a team working on the development of simulation technology<br />
for both industrial manufacturing operations and surgery. Since 2008 he has led a large pan-Canadian effort on the development<br />
of surgical simulation technology focused on surgical oncology. The program includes the participation of teaching hospitals from across<br />
Canada, from Halifax to Victoria. Part of Dr. Di Raddo’s project development includes a new simulator that lets neurosurgeons rehearse before<br />
operating--like pilots on a flight simulator. It is said that this idea could revolutionize how doctors train for and handle brain surgery. The<br />
prototype simulator developed by and several other research groups under his tutelage, gives surgeons a dry run in virtual reality before<br />
entering the operating room, potentially reducing mistakes.<br />
9:30 AM - 11:00 AM *included in Registration SuperPass (Option A) or Registration Option C<br />
SS10 Plenary Session 2<br />
Moderators: Jo Buyske, MD & Alberto Chousleb, M.D.<br />
location: Potomac Ballroom A-B<br />
S045 HIATAL MESH IS ASSOCIATED WITH MAJOR RESECTION AT REVISIONAL OPERATION. Michael Parker, MD, Jillian M Bray, MD MPH,<br />
Adam S Harris, MD, Erol V Belli, MD, Jason M Pfluke, MD, Susanne S Preissler, Horacio J Asbun, MD, C D Smith, MD, Steven P Bowers, MD,<br />
Mayo Clinic Florida, Jacksonville, FL, USA<br />
S046 SAFETY, EFFICACY AND COST-EFFECTIVENESS OF COMMON LAPAROSCOPIC PROCEDURES Manish M Tiwari, MD PhD MPH, Jason F<br />
Reynoso, MD, Albert W Tsang, MD, Dmitry Oleynikov, MD FACS, Department of Surgery, University of Nebraska Medical Center, Omaha, NE<br />
V026 THE FEAR OF TRANSGASTRIC CHOLECYSTECTOMY: MISINTERPRETATION OF THE BILIARY ANATOMY Silvana Perretta, MD, Bernard<br />
Dallemagne, MD, Gianfranco Donatelli, MD, Didier Mutter, MD, Pierre Allemann, MD, Hurng-Sheng Wu, MD, Jacques Marescaux, MD, IRCAD,<br />
University Hospital of Strasbourg, France - Show Chwan Memorial Hospital, Changhua, Taiwan<br />
S047 LIFETIME MEDICATION COST-SAVINGS FOR TREATING HYPERTENSION AND DIABETES AFTER GASTRIC BYPASS Saber Ghiassi, MD<br />
MPH, John Morton, MD MPH, Dan Eisenberg, MD MS, Stanford school of medicine and Palo Alto VA Health Care System<br />
S048 MINILAPROTOMY APPROACH TO PERFORATED DUODENAL ULCER Tomonori Ohsawa, MD, Toru Ishiguro, MD, Norimichi Okada, MD,<br />
Keiichiro Ishibashi, PhD, Norihiro Haga, PhD, Hideyuki Ishida, PhD, Department of Digestive Tract and General Surgery, Saitama Medical<br />
Center, Saitama Medical Schoo<br />
V027 LAPAROSCOPIC MEDIAN ARCUATE LIGAMENT RELEASE FOR CELIAC ARTERY DECOMPRESSION Arthur Rawlings, MD MDiv,<br />
Margaret Frisella, RN, L. Michael Brunt, MD, Washington University<br />
<strong>SAGES</strong> acknowledges our Diamond Level Donors for their support of this session:<br />
Covidien, Ethicon Endo-Surgery, Inc. and <strong>SAGES</strong> Education and Research Foundation.<br />
10:00 AM - 1:00 PM<br />
Last Chance to Visit Exhibits, Posters, Learning Center Open<br />
Please note 1:00 PM Closing Time!<br />
12 th World Congress of Endoscopic Surgery<br />
63 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Saturday, April 17, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
11:00 AM - 11:30 AM<br />
<strong>SAGES</strong> Annual General Membership Business Meeting<br />
All <strong>SAGES</strong> Members Encouraged to Attend!<br />
Location: Potomac Ballroom C<br />
Agenda<br />
President’s Introduction<br />
Report of Ballots, Explanation of Bylaws Changes, Introduction of new Officers/Board Members<br />
Committee Reports<br />
Finance/Assets<br />
development<br />
Membership<br />
legislative<br />
publications / Journal<br />
Guidelines<br />
Flexible Endoscopy<br />
Endolumenal Task Force / NOTES®<br />
Educational Resources<br />
resident Education<br />
Continuing Education<br />
FLS & FES<br />
research & Career Development<br />
Quality, Outcomes & Safety<br />
program<br />
Technology & Web Task Force<br />
Global Affairs<br />
Military Working Group<br />
liaison Groups (Bariatric, Ethics, Pediatric)<br />
advisory Groups (Business Development, Communications, Industry Relations)<br />
Remarks by Incoming President<br />
C. Daniel Smith, MD<br />
Adrian Park, MD<br />
Jo Buyske, MD<br />
11:00 AM - 1:00 PM<br />
BREAK: Exhibits, Posters & Learning Center Open<br />
11:30 AM - 12:30 PM<br />
FREE Lunch in Exhibit Hall for all<br />
World Congress Scientific Session Registrants!<br />
11:30 AM - 1:00 PM **Separate Registration Fee: $55<br />
Fellowship Council Luncheon<br />
The Future of Fellowships: How Will They Be Funded<br />
Chair: Adrian E. Park, M.D.; Co-Chair: Bruce D. Schirmer, M.D.<br />
location: Maryland Ballroom C<br />
Description:<br />
New guidelines in the funding of fellowships will pose great challenges to <strong>Program</strong> Directors and fellows alike. This session will bring our<br />
members up to date with the current status of fellowship funding and discuss options that may be available for the future.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• To understand the recent changes in industry that will affect fellowship funding<br />
• To learn of alternative funding approaches for MIS fellowships<br />
Schedule<br />
11:30 AM Introduction Adrian E. Park, M.D. & Bruce D. Schirmer, M.D.<br />
11:35 AM Non-ACGME Fellowships: How Many & What Types Are Out There?! Samer Matter, M.D.<br />
11:50 AM Current Funding of Non-ACGME Fellowships: A Variety of Options Daniel J. Scott, M.D.<br />
12:05 PM The Industry Perspective on Funding of Fellowships Pamela Martin (Ethicon) & Chuck Kennedy (Covidien)<br />
12:25 PM Discussion<br />
<strong>SAGES</strong> acknowledges an unrestricted educational grant in support of this session from Covidien.<br />
12 th World Congress of Endoscopic Surgery 64
Saturday, April 17, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
1:00 PM - 3:00 PM *included in Registration SuperPass (Option A) or Registration Option C<br />
“Uh Oh! What Now?” Video Panel<br />
Chair: David R. Urbach, M.D.; Co-Chair: David B. Earle, M.D.<br />
location: Potomac Ballroom C<br />
This panel invovles interactive case presentations with video and still photos of intraoperative findings. Both the audience and the expert<br />
panel will weigh in on solutions to the problems. The audience will be able to interact with an audience response system, and microphones<br />
on the floor. The moderator will poll the expert panel, and review recent, pertinent literature related to the topic.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• Develop a strategy for emergent conversion to open surgery<br />
• Resolve an intraoperative exposure during single port cholecystectomy<br />
• Improve operative exposure during single port cholecsystectomy<br />
• Understand and implement strategies for controlling hemorrhage laparoscopically<br />
Schedule<br />
1:00 PM Introduction David R. Urbach, M.D. & David B. Earle, M.D.<br />
1:05 PM Leaking Anastomosis After Gastric Bypass John Romanelli, M.D.<br />
1:20 PM Laparoscopic Treatment of Ruptured Diverticulitis Morris Franklin, M.D.<br />
1:35 PM Enhancing Operative Exposure During Gastric Bypass with Larger Liver Daniel Birch, M.D.<br />
1:50 PM Enhancing Operative Exposure During Single Port Cholecystectomy L. Michael Brunt, M.D.<br />
2:05 PM Difficult Fundus Mobilization and Bleeding Short Gastrics During Foregut Surgery Allan Okrainec, M.D.<br />
2:20 PM Rapid Conversion to Open Surgery – Pro Sports Team or Circus Circus? David Earle, M.D.<br />
2:35 PM Discussion<br />
1:00 PM - 3:00 PM *included in Registration SuperPass (Option A) or Registration Option C<br />
CAGS Simulation in the Training of Surgeons Session<br />
Chair: Liane S. Feldman, M.D.; Co-Chair: Teodor P. Grantcharov, M.D.<br />
location: Potomac Ballroom D<br />
While growing evidence supports the transfer of skills from the simulated to the operating room environment, barriers remain to its wide<br />
adoption and integration into clinical training practices. This session will review recent evidence supporting the use of simulation for surgical<br />
training (including integration in comprehensive curricula) and assessment (selection, certification, re-certification), as well as discuss current<br />
obstacles to implementation.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• Summarize the evidence supporting transfer of skills from the simulated to the operating room environment [competence]<br />
• List important factors required for effective teaching in the simulated environment [competence]<br />
• Integrate comprehensive simulation-based training and assessment curricula unto clinical training [performance]<br />
• Discuss what level of evidence is required for the use of simulation for certification [competence]<br />
• Apply the principles of objective assessment and evidence-based training to improve quality of surgical education at their center<br />
[outcomes]<br />
Schedule<br />
12:30 PM Introduction Liane S. Feldman, M.D. & Teodor P. Grantcharov, M.D.<br />
12:35 PM Transfer of Skills from the Simulation Lab to the Operation Room – What is the Evidence? Liane S. Feldman, M.D.<br />
12:50 PM How to Provide Effective Teaching in a Simulated Environment Karim Qayumi, M.D., Ph.D.<br />
1:05 PM Integrating Comprehensive Simulation-Based Curricula Into Clinical Training Teodor P. Grantcharov, M.D.<br />
1:20 PM Introducing Team Training Into Residency Training –<br />
What Can We Teach and How Can We Measure It?<br />
Daniel B. Jones, M.D.<br />
1:35 PM Simulation as a Tool for Certification – Are We Ready? Jo Buyske, M.D.<br />
1:50 PM Fulfilling the Promises of Simulation Training – What are the Obstacles? Carlos Pellegrini, M.D.<br />
2:05 PM Discussion<br />
12 th World Congress of Endoscopic Surgery<br />
Evaluation & CME Credit Claim<br />
Visit the kiosks next to registration to complete<br />
your online evaluation and CME credit form on-site.<br />
Attendees may print CME certificates two weeks<br />
after the conclusion of the meeting.<br />
The programs and lectures presented at the <strong>2010</strong> World<br />
Congress Meeting are copyrighted products of the Society<br />
of American Gastrointestinal and Endoscopic Surgeons.<br />
Any reproduction or rebroadcasting without the express<br />
written consent of <strong>SAGES</strong> is strictly prohibited.<br />
65 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Saturday, April 17, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
1:00 PM - 3:00 PM *included in Registration SuperPass (Option A) or Registration Option C<br />
FES Roll-Out Session<br />
Chair: Brian J. Dunkin, M.D.; Co-Chair: Jeffrey M. Marks, M.D.<br />
location: Maryland Ballroom A<br />
This session will introduce the new FES testing program – the first validated test of flexible endoscopy skills. FES is modeled after FLS<br />
(Fundamentals of Laparoscopic Surgery) with web-based reference material, a written examination, and a hands-on skills test. The process for<br />
developing FES, data on its validation, and plans for making it available to the medical community will be described.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• Recognize the current requirements for endoscopic training<br />
• Describe the components of FES<br />
• Define the overall goals of FES<br />
Schedule<br />
1:00 PM Introduction Brian J. Dunkin, M.D. & Jeffrey M. Marks, M.D.<br />
1:05 PM The Numbers Game – Current Requirements for Training & Credentialing in Flexible Endoscopy John Mellinger, M.D.<br />
1:20 PM Why Create FES? – Inspiration and Timeline Brian J. Dunkin, M.D.<br />
1:35 PM What is FES – Web-Based Didactic Material, Cognitive Exam, Hands-on Skills Test Jeffrey M. Marks, M.D.<br />
1:55 PM How was FES Validated? – Cognitive Exam Benjamin Poulose, M.D.<br />
2:10 PM How was FES Validated? – Hands-on Skills Test Melina Vassilou, M.D.<br />
2:25 PM Future of FES – Linking to Clinical Performance, Requirement in Surgery Training Gerald Fried, M.D.<br />
2:40 PM Discussion<br />
1:00 PM - 5:00 PM *included in Registration SuperPass (Option A) or Registration Option C<br />
Concurrent Sessions (accepted oral & video presentations)<br />
1:00 - 2:00 PM SS11 Robotics Location: Maryland Ballroom B-D<br />
Moderators: Mehran Anvari, MD & Alessio Pigazzi, MD<br />
S049 ROBOTIC GASTRECTOMIES OFFER A SOUND ONCOLOGIC SURGICAL ALTERNATIVE FOR THE TREATMENT OF EARLY GASTRIC<br />
CANCERS COMPARING FAVORABLY WITH LAPAROSCOPIC RESECTIONS Yanghee Woo, MD, Kazuki Inaba, MD, Woo Jin Hyung, MD PhD,<br />
Sung Hoon Noh, MD PhD, Yonsei University Health System, Seoul Korea. Columbia University Medical Center , NY NY USA<br />
S050 NEUROERGONOMIC ASSESSMENT OF THE ROBOTIC ENHANCEMENT OF MINIMALLY INVASIVE SURGERY David James, MRCS<br />
MBBS BScHons, Felipe Orihuela-Espina, PhD, Daniel R Leff, PhD MRCS MBBS, George Mylonas, Ka-Wai Kwok, Ara W Darzi, KBE MD FACS<br />
FRCS, Guang-Zhong Yang, PhD, Dept Biosurgery and Surgical Technology and Royal Wolfson Royal Wolfson Image Computing Laboratory,<br />
Imperial College London, United Kingdom<br />
S051 ROBOTIC GASTRIC BYPASS: THE FUTURE OF BARIATRIC SURGERY? Chan W Park, MD, Edward Lam, BS, Cedric Lorenzo, MD, Kenric<br />
Murayama, MD, Racquel Bueno, MD, University of Hawaii, Queen’s Medical Center<br />
S052 A COMPARISON OF SHORT-TERM OUTCOMES FOR OPEN, LAPAROSCOPIC, AND ROBOT-ASSISTED RECTAL RESECTION FOR<br />
CANCER Gyu-Seog Choi, MD, Jun Seok Park, MD, Kyoung Hoon Lim, MD, You Seok Jang, MD, Soo Han Jun, MD, Department of Surgery,<br />
School of Medicine, Kyungpook National University, Daegu, Korea<br />
S053 MULTI-FUNCTIONAL ROBOT FOR LAPAROENDOSCOPIC SINGLE-SITE SURGERY Amy C Lehman, MS, Tyler D Wortman, BS, Kyle W<br />
Strabala, MS, Nathan A Wood, MS, Manish M Tiwari, MD, Matthew R Goede, MD, Shane M Farritor, PhD, Dmitry Oleynikov, MD, University of<br />
Nebraska-Lincoln, University of Nebraska Medical Center<br />
S054 ROBOTIC VS. CONVENTIONAL LAPAROSCOPIC GASTRIC BANDING: A COMPARISON OF 407 CASES Paula K Edelson, BSc, Kristoffel<br />
R Dumon, MD, Seema S Sonnad, PhD, Bilal M Shafi, MD, Noel N Williams, MD, Bariatric Surgery <strong>Program</strong>, Deptartment of Surgery, University<br />
of Pennsylvania School of Medicine<br />
1:00 - 3:00 PM SS12 Bariatric Location: Potomac Ballroom A-B<br />
Moderators: William Richards, MD & Alfons Pomp, MD<br />
S055 PROPHYLACTIC INFERIOR VENA CAVA FILTERS IN HIGH-RISK BARIATRIC SURGERY Khashayar Vaziri, MD, John D Watson, BS, Amy P<br />
Harper, MSN ACNPBC, Juliet Lee, MD, Fred Brody, MD, Shawn Sarin, MD, Elizabeth A Ignacio, MD, Albert Chun, MD, Anthony C Venbrux, MD,<br />
Paul P Lin, MD, The George Washington University Medical Center<br />
S056 B-TYPE NATRIURETIC PEPTIDE INCREASES AFTER GASTRIC BYPASS AND CORRELATES TO WEIGHT LOSS Eric Changchien, MD,<br />
Gavitt A Woodard, BS, Tina H Boussard, PhD, John M Morton, MD MPH, Stanford University<br />
S057 LAGB WITH TRUNCAL VAGOTOMY: ANY INCREASED WEIGHT LOSS? Kristen R Earle, MD, Matt B Martin, MD, Moses H. Cone Hospital<br />
Systems, Central Carolina Surgery, PA<br />
V028 LAPAROSCOPIC GASTRIC ACCESS FOR ENDOSCOPIC RETROGRADE CHOLANGIOPANCREATOGRAPHY (ERCP) FOLLOWING ROUX-<br />
EN-Y GASTRIC BYPASS (RYGB) Sachin S Kukreja, MD, Matthew I Goldblatt, MD, James R Wallace, MD PhD, Froedtert Memorial Lutheran<br />
Hospital and the Medical College of Wisconsin<br />
S058 NUTRITIONAL EFFECT OF ORAL SUPPLEMENT ENRICHED IN BETA-HYDROXY-BETA -METHYLBUTYRATE, GLUTAMINE AND<br />
ARGININE ON RESTING METABOLIC RATE AFTER LAPAROSCOPIC GASTRIC BYPASS. R H Clements, MD, N Saraf, MPH, M Kakade, MPH, M<br />
White, RN, J Hackett, RN, Division of Gastrointestinal Surgery, University of Alabama at Birmingham, AL<br />
12 th World Congress of Endoscopic Surgery 66
Saturday, April 17, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
S059 DETERMINANTS OF RESOURCE UTILIZATION IN LAPAROSCOPIC ROUX-EN-Y GASTRIC BYPASS: A MULTICENTER ANALYSIS OF<br />
6322 PATIENTS Prateek K Gupta, MD, Himani Gupta, MD, Weldon J Miller, MS, Robert A Forse, MD PhD, Creighton University Medical Center<br />
S060 GASTROJEJUNOSTOMY STENOSIS FOLLOWING LAPAROSCOPIC ROUX-EN-Y GASTRIC BYPASS: 21 VS. 25-MM CIRCULAR<br />
STAPLER, A FOLLOW-UP STUDY OF LONG TERM WEIGHT LOSS. Carter T Smith, MD, Michael Garren, MD, Jon Gould, MD, University of<br />
Wisconsin School of Medicine and Public Health, Department of Surgery, Madison, WI, USA<br />
V029 SLEEVE GASTRECTOMY WITH ILEAL INTERPOSITION FOR TYPE 2 DIABETES Augusto C Tinoco, Luciana J El-Kadre, Renam Tinoco,<br />
São Jose do Avaí Hospital<br />
S061 EARLY GHRELIN AND GLP-1 CHANGES AFTER SLEEVE GASTRECTOMY IN DIABETIC OBESE PATIENTS. Nicola Basso, MD, Frida<br />
Leonetti, MD, Paola Mariani, MD, Mario Rizzello, PhD, Francesca Abbatini, MD, Giorgio Alessandri, MD, Giovanni Casella, MD, Danila<br />
Capoccia, MD, Gianluca Borgonuovo, MD, Maria L De Luca, MD, Policlinico “Umberto I”, University of Rome “Sapienza”<br />
S062 OUTCOMES OF LAPAROSCOPIC ROUX-EN-Y GASTRIC BYPASS AS A PRIMARY VERSUS REVISIONAL BARIATRIC SURGERY. Balaji<br />
Jangam, MD, Kristine M O’Hara, MD, Bruce Bernstein, PhD, Ravi Chhatrala, MD, Ioannis Raftopoulos, MD PhD FACS, Bariatric Center at Saint<br />
Francis Hospital and Medical Center, Hartford, CT.<br />
S063 LONG-TERM RESULTS AFTER LAPAROSCOPIC ADJUSTABLE GASTRIC BANDING IN ADOLESCENT PATIENTS. Gerd R Silberhumer,<br />
Karl Miller, Professor, Antonia Pump, Stefan Kriwanek, Professor, Kurt Widhalm, Professor, Gerhard Prager, Medical University Vienna, Austria;<br />
Department of Surgery<br />
V030 LAPAROSCOPIC RESECTION OF AN OCCLUDED ROUX LIMB Frances Allocco, MD, Patrick Reardon, MD, Brian Dunkin, MD, Mohamed<br />
Saad, DO, The Methodist Hospital<br />
2:00 - 3:00 PM SS13 Research Grant Presentations Location: Maryland Ballroom B-D<br />
Moderators: Aurora Pryor, MD & Tehemton Udwadia, MD<br />
S064 COLLAGEN TYPE I/III RATIO IN THE SUPPORTING LIGAMENTS OF THE GASTROESOPHAGEAL JUNCTION IN PATIENTS WITH<br />
PARAESOPHAGEAL HERNIAS Shaun R Brown, DO, Lora Melman, MD, Eric D Jenkins, MD, Corey R Deeken, PhD, Margaret M Frisella, RN,<br />
L. Michael Brunt, MD, J. Christopher Eagon, MD, Brent D Matthews, MD, Department of Surgery, Section of Minimally Invasive Surgery,<br />
Washington University School of Medicine, Saint Louis, MO. Discussant: Alfredo Carbonell, D.O.<br />
S065 IN VIVO FLUORESCENCE IMAGING OF STAPHYLOCOCCUS AUREUS BIOLOGIC MESH INFECTION – A 30 DAY ANALYSIS Karem C<br />
Harth, MD MHS, Ann-Marie Broome, PhD, Michael R Jacobs, MD PhD, Jeffrey A Blatnik, MD, Michael J Rosen, MD, University Hospitals Case<br />
Medical Center. Discussant: Yuri Novitsky, MD<br />
S066 FIBRIN GLUE FOR INTRAPERITONEAL LAPAROSCOPIC MESH FIXATION: A COMPARATIVE STUDY IN A SWINE MODEL Namir<br />
Katkhouda, MD, Tatyan Clarke, MD, Jeffrey Algra, MD, Bon C Cheng, BA, Rodney J Mason, MD, Maryam Balouch, BS, Helen J Sohn, MD,<br />
Ashkan Moazzez, MD, Jaisa Olasky, MD, Thomas V Berne, MD, USC Keck School of Medicine, Department of Surgery, Los Angeles, CA, USA.<br />
Discussant: Namir Katkhouda, MD<br />
S067 INITIAL EXPERIENCE WITH SENTINEL LYMPH NODE BIOPSY FOR ESOPHAGEAL CANCER Sarah K Thompson, MD, Dylan<br />
Bartholomeusz, MBBS MD, Peter G Devitt, MBBS, University of Adelaide, Royal Adelaide Hospital, South Australia, Australia.<br />
Discussant: John Hunter, MD<br />
S068 THE SELF-APPROXIMATING TRANSLUMENAL ACCESS TECHNIQUE (STAT) RELIABLY PERMITS TRANSGASTRIC ORGAN RESECTION<br />
AND RETRIEVAL Eric M Pauli, MD, Jegan Gopal, MD, Matthew T Moyer, MD, Abraham Mathew, MD, Randy S Haluck, MD, Ann M Rogers, MD,<br />
Penn State Milton S. Hershey Medical Center. Discussant: Mark Talamini, MD<br />
12 th World Congress of Endoscopic Surgery<br />
3:00 - 4:00 PM SS14 Complications/Ergonomics/Instruments Location: Maryland Ballroom B-D<br />
Moderators: Maurice Arregui, MD & Aaron Fink, MD<br />
S069 SHORT-STAY SURGERY: WHAT REALLY HAPPENS AFTER DISCHARGE? Tung T Tran, MD, Pepa Kaneva, MSc, Nancy E Mayo, PhD,<br />
Gerald M Fried, MD, Liane S Feldman, MD, Steinberg-Bernstein Centre for Minimally Invasive Surgery, McGill University, Montreal, Quebec,<br />
Canada<br />
V031 LAPAROSCOPIC HEPATICODUODENOSTOMY David J Kaczorowski, MD, Steven J Hughes, MD, University of Pittsburgh Medical Center<br />
S070 LAPAROSCOPIC APPENDECTOMY IS SAFE AND EFFICACIOUS IN THE ELDERLY: AN ANALYSIS USING THE NSQIP DATABASE.<br />
Michael J Kim, MD MA, Fergal J Fleming, MD, Douglas D Gunzler, MS MA, Susan Messing, MA MS, Rabih M Salloum, MD MPH, John R<br />
Monson, MD, University of Rochester<br />
V032 USE OF A NOVEL PERCUTANEOUS RETRACTION DEVICE AND MAGNETIC ANCHORING AND GUIDANCE SYSTEM (MAGS) HELPS<br />
RE-ESTABLISH THE CRITICAL VIEW AND IMPROVES SURGEON PERFORMANCE WHILE MIMICKING THE FOUR PORT TECHNIQUE IN<br />
SINGLE SITE LAPAROSCOPIC (SSL) CHOLECYSTECTOMY Rohan A Joseph, MD, Nilson A Salas, MD, Michael A Donovan, MS, Patrick R<br />
Reardon, MD, Barbara L Bass, MD, Brian J Dunkin, MD, Methodist Institute for Technology Innovation and Education (MITIE), Department<br />
of Surgery, The Methodist Hospital, Houston- TX<br />
S071 SINGLE SITE LAPAROSCOPIC (SSL) CHOLECYSTECTOMY IN HUMAN CADAVERS USING NOVEL PERCUTANEOUS RETRACTION<br />
AND A MAGNETIC ANCHORING AND GUIDANCE SYSTEM (MAGS): RE-ESTABLISHING THE CRITICAL VIEW Rohan A Joseph, MD, Nilson<br />
A Salas, MD, Michael A Donovan, MS, Patrick R Reardon, MD, Barbara L Bass, MD, Brian J Dunkin, MD, Methodist Institute for Technology<br />
Innovation and Education (MITIE), Department of Surgery, The Methodist Hospital,Houston- TX<br />
S072 LAPAROSCOPIC CHOLECYSTECTOMY POSES PHYSICAL INJURY RISK TO SURGEONS: ANALYSIS OF HAND TECHNIQUE AND<br />
STANDING POSITION Yassar Youssef, MD, Gyusung Lee, PhD, Carlos Godinez, MD, Erica Sutton, MD, Rosemary Klein, MA, Ivan George,<br />
Jacob Seagull, PhD, Adrian Park, MD, Sinai Hospital of Baltimore, MD, USA and University of Maryland Medical Center, Baltimore, MD, USA.<br />
67 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Saturday, April 17, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
3:00 - 5:00 PM SS15 Esophageal/Gastric Location: Potomac Ballroom D<br />
Moderators: Raul Rosenthal, MD & Estuardo Behrens, MD<br />
S073 EFFECTS OF NISSEN FUNDOPLICATION ON ABLATION OF BARRETT’S ESOPHAGUS WITH ENDOSCOPIC, ENDOLUMINAL<br />
RADIOFREQUENCY ABLATION Kathleen O’Connell, BS, Vic Velanovich, MD, Henry Ford Hospital, Detroit, Michigan<br />
S074 LAPARO-ENDOSCOPIC SINGLE SITE (LESS) HELLER MYOTOMY AND ANTERIOR FUNDOPLICATION FOR ACHALASIA Linda Barry,<br />
MD, Sharona B Ross, MD, Sujat Dahal, MD, Melissa Rosas, Chinyere Okpaleke, BS, Desiree Villadolid, MPH, Alexander S Rosemurgy, MD,<br />
Department of Surgery, University of South Florida, Tampa, Florida<br />
S075 DAY TO DAY DISCREPANCY IN BRAVO CAPSULE PH MONITORING: THE IMPACT OF MANOMETRIC PLACEMENT AND STATUS OF<br />
LOWER ESOPHAGEAL SPHINCTER Shahin Ayazi, MD, Jeffrey A Hagen, MD, Farzaneh Banki, MD, Joerg Zehetner, MD, Florian Augustin, MD,<br />
Helen J Sohn, MD, Steven R DeMeester, MD, John C Lipham, MD, Tom R DeMeester, MD, University of Southern California<br />
S076 REOPERATIVE ANTIREFLUX SURGERY FOR DYSPHAGIA Andras Legner, MD, Kazuto Tsuboi, MD, Lokesh Bathla, MD, Morrow E Lee, MD<br />
MS, Tommy Lee, MD, Sumeet K Mittal, MD FACS, Creighton University Medical Center Department of Surgery, Creighton University Medical<br />
Center Pulmonary and Critical Care Division<br />
S077 CAN DYSPHAGIA BE OBJECTIVELY CHARACTERIZED USING MULTICHANNEL INTRALUMINAL IMPEDANCE? Ushast Dhir, MD, Leena<br />
Khaitan, MD MPH, University Hospitals Case Medical Center<br />
V033 RECURRENT PARAESOPHAGEAL HERNIA WITH GASTROBRONCHIAL FISTULA: LAPAROSCOPIC REPAIR Brian P Jacob, MD, Anthony<br />
Vine, MD, Mark Reiner, MD, L. Brian Katz, MD, Mount Sinai Medical Center<br />
S078 LAPAROSCOPIC REPAIR OF LARGE HIATAL HERNIAS – IMPACT ON PULMONARY FUNCTION Jacqui C. Zhu, MBBS, Guillemo Becerril,<br />
MBBS, Gregory L. Falk, MBBS, Deptartment of Upper Gastrointestinal Surgery and Endosurgery, Concord Hospital<br />
S079 THE RISK OF RECURRENCE IN LAPAROSCOPY-ASSISTED RADICAL GASTRECTOMY Young-Joon Lee, PhD, Sang-Ho Jeong, MD,<br />
Soon-Tae Park, PhD, Sang-Kyung Choi, PhD, Soon-Chan Hong, PhD, Young-tae Joo, PhD, Chi-Young Jeong, MD, Hyeong-Gon Moon, MD,<br />
Woo-Song Ha, PhD, Department of Surgery, Gyeongsang National University Hospital, Gyeongnam Regional Cancer Center, Gyeongsang<br />
Institute of Health Sciences, Jinju, South Korea.<br />
S080 INTRAOPERATIVE INJECTION OF BUPIVACAINE TO THE DIAPHRAGMATIC CRURA SIGNIFICANTLY ELIMINATES THE NEED FOR<br />
OPIOIDS AFTER LAPAROSCOPIC NISSENS FUNDOPLICATION Ismail H Ozerhan, MD, Onur C Kutlu, MD, Yusuf Meker, MD, Sadettin Cetiner,<br />
MD, GATA Medical Academy Ankara Turkey, Etimesgut 600 Bed Army Hospital Etimesgut Ankara Turkey<br />
S081 OUTCOMES AFTER REPAIR OF THE INTRA-THORACIC STOMACH: OBJECTIVE FOLLOW-UP UP TO 5 YEARS Jai Bikhchandani, MD,<br />
Ona Gurney, F Yano, Tommy Lee, MD, Sumeet K Mittal, MD, Creighton University Medical Center<br />
S082 REOPERATIVE LAPAROSCOPIC PARAESOPHAGEAL HERNIORRAPHY CAN PRODUCE EXCELLENT OUTCOMES Albert W Tsang, MD,<br />
Manish M Tiwaria, MD PhD MPH, Jason F Reynoso, MD, Dmitry Oleynikov, MD, Department of Surgery, University of Nebraska Medical<br />
Center<br />
V034 TAILORED APPROACH TO MINIMALLY INVASIVE RESECTION OF GASTIRC GIST S. Al-Sabah, MD MBA, GM Fried, MD, MC Vassiliou,<br />
MD MEd, Y. Kurashima, MD PhD, LE Ferri, MD PhD, LS Feldman, MD, Steinberg- Bernstein Centre for Minimally Invasive Surgery and<br />
Innovation, McGill University Health Centre, Montreal, Canada<br />
3:00 - 5:00 PM SS16 Colorectal Location: Potomac Ballroom C<br />
Moderators: James Fleshman, MD & TBA<br />
S083 THE IMPACT OF SURGEON BEHAVIOR ON THE COST OF PERFORMING LAPAROSCOPIC APPENDECTOMY Ryan A Chandhoke, BS<br />
MS, Thomas Chu, BA, Paul C Smith, BA, Steven D Schwaitzberg, MD, Cambridge Health Alliance, Tufts University School of Medicine, Heller<br />
School for Social Policy & Management and Harvard Medical school<br />
S084 TRANSANAL ENDOSCOPIC MICROSURGERY VERSUS LAPAROSCOPIC RESECTIONS IN 100 T2-N0 RECTAL CANCERS FOLLOWING<br />
NEOADJUVANT TREATMENT: A PROSPECTIVE RANDOMIZED TRIAL WITH FIVE YEARS MINIMUM FOLLOW-UP Emanuele Lezoche,<br />
Professor Phd, Maddalena Baldarelli, MD, Massimiliano Rimini, MD, Alessandro Maria Paganini, Professor Phd, Roberto Campagnacci, MD,<br />
Mario Guerrieri, Professor, Department of Surgery University Politecnica delle Marche “Ancona” Italy<br />
S085 LAPAROSCOPIC VERSUS OPEN ELECTIVE SIGMOID RESECTION IN DIVERTICULAR DISEASE: SIX MONTHS FOLLOW-UP OF THE<br />
RANDOMIZED CONTROL SIGMA-TRIAL Bastiaan R Klarenbeek, MD, Roberto Bergamaschi, MD PhD FRCS, Alexander A Veenhof, MD,<br />
Donald L van der Peet, MD PhD, Wim T van der Broek, MD PhD, Elly S de Lange, PhD, Willem A Bemelman, MD PhD, Piet Heres, MD, Antonio<br />
M Lacy, MD PhD, Miguel A Cuesta, MD, VU University Medical Center, Amsterdam, The Netherlands; Forde Health System, Bergen University,<br />
Forde, Norway; Academic Medical Center, Amsterdam, The Netherlands; Waterland Hospital, Purmerend, The Netherlands; Hospital Clinic,<br />
Barcelona, Spain<br />
S086 TOTAL INTRACORPOREAL COLON SURGERY USING THE N.O.S.E. (NATURAL ORIFICE SPECIMEN EXTRACTION) TECHNIQUE. Morris<br />
E Franklin, MD, Karla Russek, MD, Allen Alvarez, MD, Texas Endosurgery Institute<br />
S087 SINGLE INCISION LAPAROSCOPIC TOTAL PROCTOCOLECTOMY WITH ILEOANAL ANASTOMOSIS: INITIAL OPERATIVE EXPERIENCE<br />
Daniel P Geisler, MD, Hasan T Kirat, MD, Feza H Remzi, MD, Department of Colorectal Surgery Cleveland Clinic Foundation<br />
V035 SINGLE PORT ANTERIOR RESECTION Hester Cheung, MD, Catherine Co, MD, Cliff Chung, MD, KK Yau, MD, Michael Li, Prof, Pamela<br />
Youde Nethersole Eastern Hospital<br />
S088 STAGED LAPAROSCOPIC ADJUVANT INTRAPERITONEAL CHEMOHYPERTHERMIA (IPCH) AFTER COMPLETE RESECTION FOR<br />
LOCALLY ADVANCED COLORECTAL OR GASTRIC CANCER Elie K Chouillard, MD, Poissy Medical Center (FRANCE)<br />
S089 A CASE CONTROL COMPARISON OF LAPAROSCOPIC (LX) AND OPEN (OP) APPROACH FOR THE SURGICAL MANAGEMENT OF<br />
SMALL BOWEL OBSTRUCTION (SBO) Eran Itzkowitz, MD, Yehuda Kariv, MD, Boaz Sagie, MD, Joseph Koriansky, MD, Joseph Klausner, MD,<br />
Tel Aviv Sourasky Medical Center, and Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel.<br />
12 th World Congress of Endoscopic Surgery 68
Saturday, April 17, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
S090 140 CASES EXPERIENCE OF SELF-EXPANDABLE METALIC STENT INSERTION FOR COLON AND RECTUM Yoshihisa Saida, MD,<br />
Toshiyuki Enomoto, MD, Kazuhiro Takabayashi, MD, Ayako Otsuji, MD, Yoichi Nakamura, MD, Miwa Katagiri, MD, Sayaka Nagao, MD, Shinya<br />
Kusachi, MD, Manabu Watanabe, MD, Koji ASAI, MD, Yasushi Okamoto, MD, Jiro Nagao, MD, Third Department of Surgery, Toho University<br />
Ohashi Medical Center<br />
S091 DO DIETARY SPICES IMPAIR THE PATIENT REPORTED OUTCOMES IN STAPLED HEMORRHOIDOPEXY ? A RANDOMIZED<br />
CONTROLLED STUDY Brij B Agarwal, MS, Kumar Manish, MBBS, Tapish Sahu, MBBS, Rathindra Sarangi, MS, Krishan C Mahajan, FRCS, Dr.<br />
Agarwal’s Surgery & Yoga and Sir Ganga Ram Hospital, New Delhi, India<br />
S092 IMPLEMENTATION OF COLONOSCOPIC PROCESS MEASURES: DOES IT IMPROVE QUALITY? Theodor Asgeirsson, MD, Anthony J<br />
Senagore, MD MBA FACS FASCRS, Martin A Luchtefeld, MD FASCRS, Spectrum Health Research, Michigan State University, Ferguson Clinic<br />
V036 THE ADVANTAGES OF LAPAROSCOPIC APPROACH FOR INTERSPHINCTERIC RESECTION M Hamada, MD, T Matsumura, MD, T<br />
Matsumoto, MD, F Teraishi, MD, K Ozaki, MD, T Nakamura, MD, Y Fukui, MD, Y Nishioka, MD, T Taniki, MD, T Horimi, MD, Kochi Health Sciences<br />
Center<br />
3:00 - 5:00 PM SS17 Best of Video 3 Location: Potomac Ballroom A-B<br />
Moderators: Roberto Gallardo, MD, Atul Madan, MD, Kenric Murayama, MD<br />
V037 LAPAROSCOPIC PARAESOPHAGEAL HERNIA REPAIR WITH BIOSYNTHETIC MESH AND COLLIS GASTROPLASTY Angel M Caban,<br />
MD, Daniel J Scott, MD FACS, UT Southwestern, Dallas Texas<br />
V038 LAPAROSCOPIC NISSEN FUNDOPLICATION: IT’S ROLE IN THE TREATMENT OF A FAILED ESOPHYX PROCEDURE Barry A Salky, MD<br />
FACS, The Mount Sinai Hospital, New York<br />
V039 LAPAROSCOPIC DUODENAL POLYPECTOMY WITH INTRAOPERATIVE ENDOSCOPY IN PEUTZ-JEGHERS SYNDROME Eugenius J<br />
Harvey, MBBS, Kervin Arroyo, MD, Blair Lewis, MD, Lester Katz, MD, Mount Sinai School of Medicine<br />
V040 SINGLE PORT ACCESS: A FEASIBLE ALTERNATIVE TO CONVENTIONAL LAPAROSCOPIC SPLENECTOMY EM Targarona, MD, C<br />
Balague, MD, L Pallares, MD, F Marinello, MD, C Rodriguez-Luppi, MD, C Martinez, MD, MP Hernandez, MD, M Trias, MD, Hospital Santpau,<br />
UAB, Barcelona, Spain.<br />
V041 USE OF A NOVEL, SELF-CONTAINED TISSUE RETRACTION DEVICE TO REDUCE TROCAR SITE NUMBER IN LAPAROSCOPIC AND<br />
NOTES-BASED SURGICAL PROCEDURES Trudie A Goers, MD, Richard A Pierce, MD PhD, Danny V Martinec, BS, Lee L Swanstrom, MD FACS,<br />
Legacy Health System, Portland, OR<br />
V042 AGAINST OCCAM’S RAZOR: TAP REPAIR OF RECURRENT INGUINAL HERNIA WITH CONCOMITANT INVERSION OF ORIGINAL<br />
POLYPROPYLENE PLUG Antonio D Lassaletta, MD, Erika Fellinger, MD, Steven D Schwaitzberg, MD FACS, Beth Israel Deaconess Medical<br />
Center, Cambridge Health Alliance, Harvard Medical School<br />
V043 LAPAROSCOPIC AND THORACOSCOPIC IVOR LEWIS ESOPHAGECTOMY Kazunori Sato, MD, Beemen N Khalil, MD, Pierre Theodore,<br />
MD, David Jablons, MD, Guilherme M Campos, MD, University of Wisconsin School of Medicine and Public Health and University of<br />
California San Francisco<br />
V044 LAPAROSCOPIC TREATMENT OF RECTOCELE BY ANTERIOR RECTOPEXY David Lechaux, PhD, Adrian Marius Nedelcu, Aurelie<br />
Lemarrec, MD, “Yves Le Foll’ Hospital - Saint Brieuc<br />
V045 LAPAROSCOPIC SPLEN-PANCREATECTOMY, FOR MUCINOUS PANCREATIC-CYST Jorge E Nefa, MD, Pablo E Omelanczuk, MD, Mario<br />
D Masrur, MD, Sergio E Bustos, MD, Surgical Service, Hospital Italiano, Mendoza-Argentina<br />
V046 LAPAROSCOPIC EXTIRPATION OF A FORK FROM THE DUODENUM Konrad W Karcz, MD, Birte Kulemann, MD, Gabriel J Seifert, MD,<br />
Hans J Schrag, MD, Simon Küsters, MD, Goran Marjanovic, MD, Jodok M Grüneberger, MD, Cheng Zhou, MD, Philipp Holzner, MD, Alexander<br />
Braun, MD, Videosurgery Division, Department of General and Abdominal Surgery, University Hospital Freiburg, Hugstetter Str 55, D-79106<br />
Freiburg, Germany<br />
12 th World Congress of Endoscopic Surgery<br />
FLS Testing Available!<br />
Wednesday, April 14 - Saturday, April 17, <strong>2010</strong><br />
Location: Chesapeake Conference Rooms 7-9<br />
All testing appointments must be made by April 9 – no onsite appointments available<br />
Contact FLS@sages.org for more details or to schedule your test.<br />
A Gentle Reminder About Safety/Security:<br />
We have taken every precaution to assure the safety and security of our guests and their possessions.<br />
However, we urge you to be aware and take simple steps to guard your possessions.<br />
– Do not leave your purse or briefcase unattended.<br />
– Do not leave your laptop, phone or other electronic devices on the floor or out of your sight in a darkened room<br />
– Be aware of your surroundings, in the Gaylord Hotel, in and around the National Harbor area and in Washington, DC.<br />
Have a safe & secure meeting!<br />
69 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Saturday, April 17, <strong>2010</strong><br />
Scientific Sessions & Panels<br />
3:00 PM - 5:00 PM *included in Registration SuperPass (Option A) or Registration Option C<br />
IFSES Surgical Education Around the World Panel<br />
Chair: Alberto Chousleb, M.D.; Co-Chair: Natan Zundel, M.D.; Co-Chair: Tatsuo Yamakawa<br />
Location: Maryland Ballroom A<br />
Description:<br />
Each member society of IFSES has educational challenges as related to laparoscopic/endoscopic surgery. This session will feature a variety<br />
of educational issues amongst our member societies. How do we compare with each other? Can we offer similar solutions from different<br />
backgrounds? This is an international, star-studded cast to peak your interest in education.<br />
Objectives:<br />
At the conclusion of this session, participants will be able to:<br />
• Realize the different ways and options for surgical education around the world<br />
• Explain how new technologies are being implemented and their impact in surgical training<br />
• Recognize what the widespread use of new technologies is in different parts of the world<br />
Schedule<br />
3:00 PM Introduction Alberto Chousleb, M.D. & Natan Zundel M.D.<br />
3:05 PM Telementoring and Telemedicine as an Educational Tool Mehran Anvari, M.D.<br />
3:15 PM Fellowship Training in the United States, Where Do We Stand? Steve Eubanks, M.D.<br />
3:25 PM Minimally Invasive Surgery Training in Latin America Samuel Shuchleib, M.D.<br />
3:35 PM How to Adapt Surgical Education to New Technology Sir Alfred Cuschieri, M.D.<br />
3:45 PM 3-D/Robotic Surgery as Emerging Technologies Current Applications and Near Future Expectation Seigo Kitano, M.D.<br />
3:55 PM Application of Advanced Minimally Invasive Techniques in Rural Areas Pradeep Chowbey, M.D.<br />
4:05 PM Discussion<br />
4:15 PM Training Residents Versus training Surgeons – Should They be Trained the Same? Michael Li, M.D.<br />
4:25 PM Should Single Incision Surgery, NOTES®, and Robotics Integrate the<br />
Current Surgical Curriculum or be Part of a Fellowship <strong>Program</strong>?<br />
Natan Zundel, M.D.<br />
4:35 PM What is the Role of International Surgical Societies in Education Gerald Marks, M.D.<br />
4:45 PM 1990 - <strong>2010</strong> Twenty Years of Minimally Invasive Surgery Extensive Development;<br />
present and Future of Their Educational <strong>Program</strong>s – A European Viewpoint<br />
Jacques Perissat, M.D.<br />
4:55 PM Discussion<br />
<strong>SAGES</strong> acknowledges educational grants in support of this World Congress panel from Covidien and Ethicon Endo-Surgery, Inc.<br />
Saturday Evening<br />
7:30 PM - 11:00 PM<br />
Don’t miss the World Congress Gala,<br />
Featuring Dinner & the International Sing-Off<br />
Location: Newseum. See page 94 for details.<br />
Shuttles begin departing at 7:15 PM at the Bus Pickup are of the Gaylord hotel ONLY.<br />
Go to the Group Bus Loading area, located at the Woodrow Wilson exit on the 2 nd level,<br />
opposite of guest parking. Buses will circle all evening until the event ends.<br />
To purchase tickets on-site, please visit the Registration Desk.<br />
12 th World Congress of Endoscopic Surgery 70
Presenting…<strong>SAGES</strong> Media Madness!<br />
<strong>SAGES</strong> iMAGES Library<br />
<strong>SAGES</strong> SUR<br />
The <strong>SAGES</strong> Image Resource Library<br />
i MAGES at <strong>SAGES</strong><br />
S-WIKI<br />
what does it do?<br />
what does it do?<br />
iMAGES provides <strong>SAGES</strong> Members with<br />
access to various digital images, photos<br />
and graphics. All images are donated by<br />
<strong>SAGES</strong> Members to be used by other<br />
<strong>SAGES</strong> Members to advance education<br />
and excellence in minimally invasive<br />
surgery.<br />
Content may be uploaded, shared, downloaded,<br />
edited and used for publication<br />
and presentation by any <strong>SAGES</strong> member<br />
as long as appropriate credit is given to<br />
<strong>SAGES</strong> and the original submitter(s).<br />
S-WIKI is a surgical “Wikipedia”<br />
editable by all <strong>SAGES</strong><br />
members.<br />
This has significant potential to<br />
become the most authoritative<br />
and frequently accesses<br />
surgical reference on the web.<br />
The <strong>SAGES</strong> Wiki will be open<br />
for public viewing but may be<br />
edited only by <strong>SAGES</strong><br />
membership.
...Now available on sages.org<br />
GICAL WIKI<br />
<strong>SAGES</strong> Video Library<br />
tV<br />
Share your own videos<br />
with the Surgical Community.<br />
<strong>2010</strong><br />
sages.org<br />
what does it do?<br />
<strong>SAGES</strong> TV is a central “searchable and fully<br />
navigational” depository for <strong>SAGES</strong> related videos.<br />
<strong>SAGES</strong> members will be able to submit, view, and<br />
rate videos on the site.<br />
The <strong>SAGES</strong> Surgical WIKI<br />
<strong>SAGES</strong> TV is the new home for all official <strong>SAGES</strong><br />
videos including the existing the classic <strong>SAGES</strong><br />
video library and past <strong>SAGES</strong> meeting content.<br />
Features:<br />
· 305 free videos and counting<br />
· Narrated by leading laparoscopic surgeons<br />
· Free access with no registration required<br />
· Classic videos from 1995-2003<br />
· Keynote Lectures<br />
· <strong>SAGES</strong> PG Courses<br />
· And much more!!
12 th World Congress of Endoscopic Surgery<br />
<strong>2010</strong> Learning Center Chair: Allan Okrainec, M.D.; Co-Chair: Brian Jacob, M.D.<br />
Hours of Operation:<br />
Thursday, April 15, <strong>2010</strong> 10:00 AM - 2:30 PM<br />
Friday, April 16, <strong>2010</strong> 10:00 AM - 2:30 PM<br />
Saturday, April 17, <strong>2010</strong> 10:00 AM - 1:00 PM<br />
The Learning Center is a set of educational<br />
classrooms where attendees can gain<br />
knowledge and practice skills relevant to<br />
minimally invasive surgery. Station coordinators<br />
instruct individuals and small groups on topics<br />
that range from basic instrumentation to<br />
advanced laparoscopic skills. Participants may<br />
visit one or more stations that address their<br />
educational objectives and spend whatever<br />
time is necessary to meet their learning<br />
objectives<br />
1. Natural Orifice Transluminal<br />
Endoscopic Surgery (NOTES®)<br />
Coordinator: Kai Matthes, MD, PhD<br />
Natural Orifice Transluminal Endoscopic Surgery<br />
(NOTES®) is an emerging research area of<br />
minimally-invasive surgery. The development<br />
of new surgical procedures and devices can<br />
be simulated effectively in a training model.<br />
For the NOTES® Station of the <strong>SAGES</strong> learning<br />
center, a novel ex-vivo simulator is used to<br />
provide a realistic training experience using<br />
commercially available laparoscopic and flexible<br />
endoscopic devices. The ex-vivo model consist<br />
of a complete porcine peritoneal cavity explant,<br />
which is harvested from the meat production<br />
industry, thoroughly cleaned, embalmed and<br />
modified to closely resemble human anatomy.<br />
Real tissue provides a realistic tactile feedback,<br />
which is essential to assess and train new<br />
techniques such as NOTES®. Laparoscopic<br />
surgeons without flexible endoscopic<br />
experience can learn how to operate a flexible<br />
endoscope and how to establish transgastric,<br />
transvaginal or transcolonic access in order<br />
to perform a peritoneal exploration. For the<br />
more advanced ‘digestivists’ with flexible<br />
endoscopic experience, organ resection<br />
(appendectomy, cholecystectomy, distal<br />
pancreatectomy, nephrectomy, liver lobe<br />
resection, hysterectomy, oophorectomy)<br />
or gastrointestinal anastomosis techniques<br />
(gastrojejunostomy, partial gastrectomy,<br />
colectomy) will be simulated.<br />
Objectives:<br />
At the conclusion of this activity, the participant<br />
will be able to:<br />
• Perform transluminal access of the peritoneal<br />
cavity by using a transgastric, transcolonic<br />
or transvaginal approach using flexible<br />
endoscopes with or without laparoscopic<br />
assistance<br />
• Perform NOTES® appendectomy,<br />
cholecystectomy, distal pancreatectomy,<br />
nephrectomy, liver lobe resection,<br />
hysterectomy, oophorectomy<br />
• Perform a secure closure of the transluminal<br />
access port using various techniques such as<br />
t-tags, clips or sophisticated closure devices<br />
• Review the limitation of currently available<br />
standard endoscopic devices and the<br />
advantage of additional laparoscopic ports<br />
for visualization and retraction using a hybrid-<br />
NOTES® approach<br />
2. Single Incision Surgery:<br />
Entry Methods<br />
Coordinators: Gregg Kai Nishi, MD &<br />
Marina Kurian, MD<br />
Single incision or single port access is emerging<br />
as an optional technique for entry into the<br />
abdominal cavity to perform a variety of<br />
different laparoscopic procedures. To date,<br />
there is dominantly-preferred entry method,<br />
but instead a variety of options exist that<br />
include using multiple trocars through a single<br />
skin incision or using one of many specially<br />
designed single port access devices. At this<br />
station, you will become familiar with both<br />
options. A variety of low-profile trocars that<br />
are routinely used in single incision surgery<br />
will be available for use in an inanimate model.<br />
Additionally, you will be able to practice<br />
inserting and setting up a variety of single<br />
port access devices that are currently available<br />
for clinical use. By the end of your visit, you<br />
will be more familiarized with and more able<br />
to compare and contrast the different entry<br />
methods available to perform single incision<br />
surgery operations.<br />
Objectives:<br />
At the conclusion of this activity, the participant<br />
will be able to:<br />
• Compare and contrast different entry<br />
methods available to perform single incision<br />
surgery operations<br />
• Demonstrate how to insert and set up a<br />
variety of single port access devices<br />
3. Single Incision Surgery:<br />
Instruments & Techniques<br />
Coordinators: Brian Jacob, MD,<br />
Greg Dakin, MD, &<br />
Julio Teixeiria, MD<br />
In conjunction with the single incision<br />
surgery Entry Methods Station, at this station<br />
participants will gain experience with the ability<br />
to perform single incisions procedures. The<br />
highlight of this station will be an opportunity<br />
to suture using single incision techniques in a<br />
trainer box and then to compare your skill to<br />
traditional laparoscopic suturing. Both straight<br />
instruments and articulating instruments will<br />
be compared. In addition, you will learn to<br />
insert liver and gallbladder retractors, and then<br />
practice performing different single incision<br />
tasks like suturing, running bowel, or dissecting.<br />
Participants will have the opportunity to use a<br />
variety of single incision surgery instruments.<br />
In addition, at this station, experts in the<br />
various single incision surgery procedures like<br />
lap adjustable gastric banding, gallbladder,<br />
colon, and hernia, will be showing videos<br />
that demonstrate their techniques and offer a<br />
unique one-on-one opportunity to learn and<br />
ask questions.<br />
Objectives:<br />
At the conclusion of this activity, the participant<br />
will be able to:<br />
• Perform different single incisions tasks such as<br />
suturing, running bowel, or dissecting<br />
• Demonstrate how to insert and set up a<br />
variety of single port access devices<br />
4. Fundamentals of Laparoscopic<br />
Surgery<br />
Coordinator: Melina Vassiliou, MD<br />
This station will introduce participants to the<br />
Fundamentals of Laparoscopic Surgery (FLS)<br />
didactic and technical skills modules. FLS was<br />
designed to teach the physiology, fundamental<br />
knowledge, and technical skills required to<br />
perform basic laparoscopic surgery, and is a<br />
joint ACS-<strong>SAGES</strong> program. Participants will<br />
use the interactive web-based format and the<br />
lap trainer boxes to become familiar with the<br />
program while working on their laparoscopic<br />
knowledge and skills. This station will also give<br />
new program directors the opportunity to have<br />
hands-on time with the module and to learn<br />
about the Covidien Educational Fund.<br />
Objectives:<br />
At the conclusion of this activity, the participant<br />
will be able to:<br />
• Describe the components of the FLS program<br />
• Explain some of the preoperative,<br />
intraoperative, and postoperative<br />
considerations fundamental to laparoscopic<br />
surgery<br />
5. Fundamentals of Endoscopic<br />
Surgery<br />
Coordinators: Brian Dunkin, MD &<br />
Thadeus Trus, MD<br />
Come get hands-on experience in flexible<br />
endoscopy. This station will showcase the newly<br />
developed Fundamentals of Endoscopic Surgery<br />
(FES) testing platform (the flexible endoscopy<br />
equivalent of FLS) - the first validated hands-on<br />
test for gastrointestinal endoscopic skills. FES<br />
will be loaded on a Simbionix virtual reality<br />
simulator for you to “test drive”. <strong>Final</strong>ly, video<br />
based education material is available to review<br />
the new <strong>SAGES</strong> flexible endoscopy hands-on<br />
training curriculum and preview the developing<br />
FES website.<br />
This is your chance to practice your endoscopic<br />
skills with the help of expert proctors, or throw<br />
your hat into the ring to pit your skills against<br />
others in an FES shootout. The winner of the<br />
FES shootout will receive a <strong>SAGES</strong> Top 14 DVD<br />
video set.<br />
Objectives:<br />
At the conclusion of this activity, the participant<br />
will be able to:<br />
• Evaluate the FES manual skills testing module<br />
• Assess his/her flexible endoscopy skills<br />
• Develop basic endoscopic skills on virtual<br />
reality and real tissue simulation platforms<br />
• Evaluate the <strong>SAGES</strong> flexible endoscopy handson<br />
training curriculum<br />
12 th World Congress of Endoscopic Surgery 74
<strong>2010</strong> Learning Center<br />
6. Laparoscopic Ventral Hernia<br />
and Inguinal Hernia Repair<br />
Coordinator: Adrian Park, MD,<br />
Yo Kurashima, MD,<br />
Gerald Fried, MD<br />
The laparoscopic ventral hernia repair<br />
has become a very commonly performed<br />
procedure. Both virtual reality and box trainer<br />
hernia modules will allow participants to<br />
practice and become facile with this technique.<br />
This station will also feature new simulation<br />
models for laparoscopic inguinal hernia repair.<br />
Participants will gain experience with the steps<br />
of the procedures, as well as positioning and<br />
securing the mesh.<br />
Objectives:<br />
At the conclusion of this activity, the participant<br />
will be able to:<br />
• To learn normal anatomic relationships.<br />
• Practice mesh deployment and securing<br />
techniques.<br />
7. Suturing<br />
Coordinators: Zoltan Szabo, PhD &<br />
Neal Seymour, MD<br />
Participants receive intense hands-on suturing<br />
including intracorporeal techniques with<br />
instantaneous feedback. Laparoscopic tissue<br />
handling and complex suturing maneuvers will<br />
also be demonstrated. Virtual reality suturing<br />
simulators will be used to allow “virtual”<br />
suturing practice – no suture required, just a<br />
fancy videogame with needle driver handles<br />
instead of joysticks. Trainees will be able to<br />
compare their scores with established expert<br />
levels for both types of simulators.<br />
Objectives:<br />
At the conclusion of this activity, the participant<br />
will be able to:<br />
• To describe the key steps for intracorporeal<br />
suturing and knot-tying.<br />
• To practice intracorporeal suturing and<br />
knot-tying in inanimate and virtual reality<br />
environments.<br />
• To demonstrate proficiency compared to<br />
“experts”.<br />
8. Top Gun<br />
Coordinator: James “Butch” Rosser, MD<br />
The Top Gun Laparoscopic Skill Shootout Station<br />
will allow participants to establish and enhance<br />
basic laparoscopic skills and suturing ability.<br />
All participants can gain skill advancement<br />
no matter their baseline. The station will<br />
feature the validated “Rosser TOP GUN” skill<br />
development stations developed by Dr. Rosser<br />
and made famous at Yale. To date, over 6000<br />
surgeons have participated around the world.<br />
Instructors will show tactics and techniques<br />
that will transfer readily into the clinical<br />
environment. In addition, participants will be<br />
competing for slots in the Top Gun Shoot Out<br />
that will crown one <strong>SAGES</strong> <strong>2010</strong> TOP GUN.<br />
Objectives:<br />
At the conclusion of this activity, the participant<br />
will be able to:<br />
• To review the Rosser suturing algorithm and<br />
be able to list and recite<br />
• To perform dexterity skills and suturing<br />
excercises using the “Rosser TOP GUN” training<br />
stations<br />
• To perform with other surgeons in the Top<br />
Gun Shoot Out (no CME credits will be given<br />
for this competition)<br />
9. Laparoscopic Common Bile<br />
Duct Exploration<br />
Coordinator: Benjamin Poulose, MD,<br />
Brian Katz, MD<br />
At this station, participants will gain exposure<br />
to the laparoscopic transcystic method of<br />
common bile duct stone management. The<br />
station utilizes the latest in inanimate model<br />
technology to simulate an actual situation for<br />
the management and retrieval of common bile<br />
duct stones.<br />
Objectives:<br />
At the conclusion of this activity, the participant<br />
will be able to:<br />
• Identify the indications for laparoscopic<br />
common bile duct exploration.<br />
• Describe the necessary equipment utilized<br />
during laparoscopic transcystic common bile<br />
duct exploration including common bile duct<br />
access instrumentation, choledochoscopy,<br />
and stone retrieval methods.<br />
• Work as part of a simulated operating room<br />
team to perform laparoscopic transcystic<br />
common bile duct exploration.<br />
10. Intraoperative Ultrasound<br />
Coordinator: Leonardo Villegas, MD &<br />
David Sindram, MD<br />
This station will focus on Intraoperative<br />
Ultrasound techniques and applications.<br />
Participants will use the latest ultrasound<br />
technology with a new inanimate phantom<br />
that was developed to mimic the ultrasound<br />
properties of abdominal organs. Instructors will<br />
demonstrate and help participants perform<br />
intraoperative ultrasound for liver, biliary and<br />
pancreatic disease, as well as discuss their<br />
surgical applications.<br />
Objectives:<br />
• To describe basic ultrasonography techniques.<br />
• To describe how ultrasound may be used<br />
to diagnose and treat biliary and pancreatic<br />
disease.<br />
11. Laparoscopic Weight Loss<br />
Surgery<br />
Coordinator: Shanu Kothari, MD &<br />
John Morton, MD<br />
The learning curve for gaining proficiency in<br />
weight-loss procedures may be shortened<br />
with an effective simulator. The Laparoscopic<br />
Adjustable Gastric Band Simulator allows<br />
participants to introduce a laparoscopic<br />
adjustable band, “run” the tubing, place the<br />
band in its correct anatomic position, and fixate<br />
the port into the subcutaneous tissue. The<br />
technical aspects of laparoscopic adjustable<br />
gastric band placement may be enhanced by<br />
simulation and allow a greater preprocedural<br />
understanding for the trainee and expert alike.<br />
A virtual laparoscopic gastric bypass trainer will<br />
similarly allow for participants to familiarize<br />
themselves with the steps and techniques<br />
necessary to perform gastric bypass.<br />
Objectives:<br />
At the conclusion of this activity, the participant<br />
will be able to:<br />
• To review laparoscopic adjustable gastric<br />
band anatomy, structure, and function.<br />
• To describe the basic steps of placing a<br />
laparoscopic adjustable gastric band.<br />
• To explain the steps and techniques necessary<br />
to perform laparoscopic gastric bypass<br />
surgery.<br />
(Please note this does not meet the FDA<br />
requirements for qualifications to perform lap<br />
band surgery)<br />
12. Robotic Surgery<br />
Coordinators: Dmitry Oleynikov, MD &<br />
Matt Goede, MD<br />
Surgical robotic systems allow for the<br />
surgeon to comfortably sit at a console and<br />
ergonomically manipulate and control the<br />
robotic arms and instruments. This offers the<br />
surgeon increased range of motion, threedimensional<br />
imaging, the benefit of motion<br />
scaling, as well as eliminating tremor. The<br />
purpose of this station will be to all participants<br />
to have hands-on exposure to the latest<br />
technologies in robotic surgery. Participants<br />
will be able to perform various simulated tasks<br />
using a surgical robot. Additionally, new invivo<br />
robots, including deployable robotically<br />
controlled laparoscopic visualization systems<br />
will be demonstrated.<br />
Objectives:<br />
At the conclusion of this activity, the participant<br />
will be able to:<br />
• Perform various simulated tasks using a<br />
surgical robot<br />
• Identify latest technologies in robotic surgery<br />
13. Video Editing<br />
Coordinators: Adheesh Sabnis, MD,<br />
Yuri Novitsky, MD<br />
The presentation of surgical videos is now<br />
an integral component of scientific meetings<br />
both for educational reasons, as well as for the<br />
demonstration of new techniques. The purpose<br />
of this station will be to learn the basic tools<br />
needed for capturing video in the operating<br />
room, and become familiar with the various<br />
software available for video editing on both PC<br />
and Mac platforms. Participants will have the<br />
opportunity to perform basic video editing of<br />
short videos as the station.<br />
75 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
<strong>2010</strong> Learning Center<br />
Objectives:<br />
At the conclusion of this activity, the participant<br />
will be able to:<br />
• Identify basic tools needed to capture video<br />
in operating room<br />
• Perform basic video editing of short videos<br />
14. Team Simulations<br />
Coordinator: Shawn Tsuda, MD<br />
Team training is on the forefront of the<br />
surgical simulation revolution. Patient safety,<br />
health care cost, decreased training time, and<br />
advances in learning theory are driving forces<br />
for the optimization of multi-disciplinary team<br />
performance in a safe environment. This station<br />
will feature a mock endosuite that will allow<br />
surgeons to plan, execute, debrief, and improve<br />
upon best practices during surgery, with a focus<br />
on cost-containment, compliance, and quality<br />
of care.<br />
Objectives:<br />
At the conclusion of this activity, the participant<br />
will be able to:<br />
• utilize team-based concepts in optimizing<br />
time, compliance, performance, and quality<br />
during a common surgical procedure<br />
• become familiar with technology and<br />
techniques in team-based training, including<br />
video-capture and debriefing<br />
• simulate a laparoscopic cholecystectomy in a<br />
mock endosuite<br />
15. Patient Safety<br />
Coordinator: Gretchen Purcell Jackson, MD,<br />
PhD & Joshua Glenn, MD<br />
The last decade has seen increasing emphasis<br />
on patient safety and quality of care from<br />
government agencies, regulatory bodies,<br />
and payers. At this station, participants can<br />
explore a variety topics related to surgical<br />
<strong>SAGES</strong> acknowledges educational grants in support of this World Congress educational venue from:<br />
Aloka Ultrasound, B-K Medical Systems, Covidien and Olympus.<br />
patient safety including proper use of<br />
operative instrumentation, informed consent,<br />
care-team communications, and avoiding<br />
malpractice lawsuits through videos, webbased<br />
instructional modules, and interactive<br />
instruction.<br />
At the conclusion of this activity, the participant<br />
will be able to:<br />
• Identify critical patient safety issues relevant<br />
to the practicing surgeon<br />
• Enumerate educational resources for learning<br />
about surgical patient safety<br />
• Demonstrate competencies in one or more<br />
areas of patient safety<br />
<strong>SAGES</strong> acknowledges contributions in-kind in support of this World Congress educational venue from:<br />
3-DMED, Allergan, Aloka Ultrasound, Apollo Endosurgery, B-K Medical Systems, Cambridge Endoscopy, Carefusion,<br />
Covidien, Endosim, Ethicon Endo-Surgery, Inc., Ethicon Inc., Gore & Associates, Karl Storz Endoscopy-America, Kyoto Kagaku,<br />
Novare Surgical Systems, Olympus, Ovesco, Simbionix, Simulab and Stryker Endoscopy.<br />
d<br />
12 th World Congress of Endoscopic Surgery 76
World Congress Invited Faculty List<br />
Gina L. Adrales, MD, Assistant Professor,<br />
Dartmouth Medical School, Dartmouth-<br />
Hitchcock Medical Center, Lebanon, NH<br />
Luigi Angrisani, MD, Consultant surgeon,<br />
University of Naples Federico II, Laparoscopic<br />
Surgery Unit, S.Giovanni Bosco Hospital,<br />
Napoli, Italy<br />
Mehran Anvari, MD, Professor of Surgery,<br />
McMaster University, Hamilton, ON, Canada<br />
Maurice E. Arregui, MD, Chairman<br />
Department of General Surgery, Director of<br />
Adult MIS, Director of Fellowship in Advanced<br />
La, St. Vincent Hospital, Indianapolis, IN<br />
Horacio J. Asbun, MD, Director of<br />
Hepatobiliary and Pancreas <strong>Program</strong>, Mayo<br />
Clinic Florida, Mayo Clinic, Jacksonville, FL<br />
Sharon L. Bachman, MD, Assistant Professor<br />
of Clinical Surgery, University of Missouri,<br />
Columbia, MO<br />
Fady Kamal Balaa, MD, Assistant Professor<br />
of Surgery, University of Ottawa, The Ottawa<br />
Hospital, Ottawa, ON, Canada<br />
Katherine A. Barsness, MD, Assistant<br />
professor of Surgery, Northwestern<br />
University’s Feinberg School of Medicine,<br />
Attending physician, Pediatric Surgery,<br />
Northwestern University, Chicago, IL<br />
Bruce Behn, MD, Ergen Professor and CBER<br />
Faculty Fellow, The University of Tennessee,<br />
Knoxville, TN<br />
Estuardo J. Behrens, MD, FACS, General<br />
Surgeon / Bariatric Surgeon, Hospital de las<br />
Américas, Miami, FL<br />
Richard H. Bell, MD, Assistant Executive<br />
Director, The American Board of Surgery, Inc.,<br />
Philadelphia, PA<br />
Simon Bergman, MD, Assistant Professor<br />
of Surgery, McGill University, Faculty,<br />
Department of Surgery and Associate<br />
Member, Division of Gastroenterology, Sir<br />
Mortimer B Davis Jewish General Hospital,<br />
Montreal, PQ, Canada<br />
Ramon Berguer, MD, FACS, Clinical Professor<br />
of Surgery, University of California Davis, Chief<br />
of Surgery, Contra Costa Regional Medical<br />
Center, Martinez, CA<br />
Marc Bessler, MD, Assistant Professor of<br />
Surgery, Columbia University, Director<br />
Minimal Access Surgery Center, New York<br />
Presbyterian Hospital, New York, NY<br />
Daniel W. Birch, MD, Associate Professor<br />
of Surgery, University of Alberta, Medical<br />
Director, CAMIS, Royal Alexandra Hospital,<br />
Edmonton, AB, Canada<br />
Desmond H. Birkett, MD, Clinical Professor of<br />
Surgery, Tufts University School of Medicine,<br />
Chairman, Department of General Surgery,<br />
Lahey Clinic Medical Center, Burlington, MA<br />
Simon Biron, MD, Professor, Laval University,<br />
Director General Suregery Division, Laval<br />
University, Quebec City, Quebec, Canada<br />
Steven P. Bowers, MD, Assistant Professor,<br />
Mayo Clinic, Florida, Senior Associate<br />
Consultant, Mayo Clinic, Jacksonville, FL<br />
Fredrick J. Brody, MD, Associate Professor of<br />
Surgery, The George Washington University<br />
Medical Center, Director of Minimally Invasive<br />
Surgery, Washington, DC<br />
L. Michael Brunt, MD, Professor of Surgery,<br />
Washington University School of Medicine,<br />
Barnes-Jewish Hospital, St Louis, MO<br />
Matias Bruzoni, MD, Palo Alto, CA<br />
Luis E. Burbano, MD, Professor of Surgery,<br />
Metropolitan Hospital Quito, Ecuador, Quito,<br />
Ecuador<br />
Jo Buyske, MD, Adjunct Professor of Surgery,<br />
University of Pennsylvania School of Medicine,<br />
Associate Executive Director, American Board<br />
of Surgery, Philadelphia, PA<br />
Ronan A. Cahill, MD, Oxford Radcliffe<br />
Hospitals, John Radcliffe Hospital, Sh’llorgan,<br />
Dublin, Ireland<br />
Alfredo M. Carbonell, DO, Assistant<br />
Professor of Clinical Surgery, University of<br />
South Carolina School of Medicine, Division<br />
of Minimal Access and Bariatric Surgery,<br />
Greenville Hospital System University Medical<br />
Cent, Greenville, SC<br />
Bipan Chand, MD, Director of Surgical<br />
Endoscopy, Cleveland Clinic Foundation, Staff<br />
Surgeon, Cleveland Clinic Hospital, Cleveland,<br />
OH<br />
Elie Chouillard, MD, President,<br />
Intercontinental Society of Natural Orifice,<br />
Endoscopic, and Laproscopic Surgery<br />
(i-NOELS), Chief of Surgery, Poissy-Saint-<br />
Germain-En-Laye Medical Center, Poissy,<br />
France<br />
Elias Chousleb, MD, Clinical Fellow, Cleveland<br />
Clinic Florida, Hallandale Beach, FL<br />
Alberto Chousleb, MD, Chief Experimental<br />
Surgery, ABC Medical Center, Medical Director,<br />
ABC Medical Center, Mexico, Mexico City,<br />
Mexico<br />
Pradeep K. Chowbey, MD, Chief of Surgery,<br />
Director, Max Healthcare Institute, New Delhi,<br />
India<br />
W. Y. Chung, MD, Yonsei University College of<br />
Medicine, Seoul, Seodaemun-gu, South Korea<br />
Ronald Hanson Clements, MD, Professor of<br />
Surgery, University of Alabama-Birmingham,<br />
Director Bariatric Surgery, University Hospital,<br />
Nashville, TN<br />
Ricardo V. Cohen, MD, Director, The Center for<br />
the Surgical Treatment of Morbid Obesity and<br />
Metabolic Disorders, Baros Surgical Associates,<br />
Sao Paulo, Brazil<br />
Manolo Cortez, MD, Medical Doctor,<br />
International University of Ecuador, General<br />
& Bariatric Surgeon, Metropolitano Hospital,<br />
Quito, Ecuador<br />
David Cummings, MD, Professor of Medicine,<br />
University of Washington, Deputy Director,<br />
Diabetes Endocrinology Research Center,<br />
University of Washington, Seattle, WA<br />
Christopher Cunningham, MD, Consultant<br />
Colorectal Surgeon, Oxford Radcliffe<br />
Hospitals, Oxford, United Kingdom<br />
Paul G. Curcillo II, MD, Associate Professor &<br />
Vice Chairman of Surgery, Drexel University,<br />
Director, Robotics and Minimally Invasive<br />
Surgery, Flourtown, PA<br />
Alfred Cuschieri, MD, Professor Sir, University<br />
of Dundee, Sir Alfred, Institute for Medical<br />
Science and Technology, Dundee, Scotland,<br />
United Kingdom<br />
Allan Dackiw, MD, Assistant Professor of<br />
Surgery, Johns Hopkins University, Baltimore,<br />
MD<br />
Gregory F. Dakin, MD, Assistant Professor<br />
of Surgery, Weill Cornell Medical College,<br />
Attending Surgeon, New York Presbyterian<br />
Hospital, New York, NY<br />
Bernard Dallemagne, MD, Scientific<br />
Co-Director, Digestive Cancer Research<br />
Institute (IRCAD), MD, University Hospital of<br />
Strasbourg, Strasbourg - France, Strasbourg,<br />
France<br />
Aureo L. De Paula, MD, Hospital de<br />
Especialidades, Goiania, Goias, Brazil<br />
Edmundo Dedios Orozco, MD, General<br />
Surgeon, Universidad Nacional , Chief<br />
Surgeon, Hospital II EsSalud , Piura, Peru<br />
Conor P. Delaney, MD, PhD, Professor of<br />
Surgery, Case Western Reserve University,<br />
Chief, Division of Colorectal Surgery,<br />
University Hospitals Case Medical Center,<br />
Cleveland, OH<br />
Nicolas Demartines, MD, Professor , University<br />
of Lausanne, Switzerland, Chairman,<br />
University Hospital CHUV, Lausanne,<br />
Switzerland, Switzerland<br />
Daniel J. Deziel, MD, Professor of Surgery,<br />
Rush University, Senior Attending Surgeon,<br />
Rush University Medical Center, Chicago, IL<br />
Andre Dhoore, MD, Professor, University<br />
Hospital Leuven Belgium, UZ Gasthuisberg,<br />
Leuven, Belgium<br />
Robert DiRaddo, MD, Group Leader,<br />
Simulation of Deformable Materials, Industrial<br />
Materials Institute, National Research Council<br />
Canada, Boucherville, Québec, Canada<br />
Quan-Yang Duh, MD, Professor, University of<br />
California, San Francisco, Attending Surgeon,<br />
VA Medical Center, San Francisco, San<br />
Francisco, CA<br />
Brian J. Dunkin, MD, Professor of Clinical<br />
Surgery, Weill Cornell Medical College, Head,<br />
Section of Endoscopic Surgery, The Methodist<br />
Hospital, Houston, TX<br />
Sanjeev Dutta, MD, Assistant Professor,<br />
Stanford University, Lucile Packard Children’s<br />
Hospital, Stanford, CA<br />
12 th World Congress of Endoscopic Surgery<br />
77 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
World Congress Invited Faculty List<br />
David Bryan Earle, MD, Assistant Professor of<br />
Surgery, Tufts University School of Medicine,<br />
Director of Minimally Invasive Surgery,<br />
Baystate Medical Center, Springfield, MA<br />
Steven Edmundowicz, MD, Professor of<br />
Medicine, Washington University, Chief of<br />
Endoscopy, Barnes Jewish Hospital, St. Louis,<br />
MO<br />
Michael B. Edye, MD, FACS, Adjunct Associate<br />
Professor of Surgery, Mount Sinai School of<br />
Med, Attending, The Mount Sinai Hospital,<br />
New York, New York, NY<br />
Jonathan E. Efron, MD, Associate Professor<br />
of Surgery, Mayo Clinic College of Medicine,<br />
Consultant Surgeon, Mayo Clinic Arizona,<br />
Scottsdale, AZ<br />
Steve Eubanks, MD, Professor, University of<br />
Missouri- Columbia, University of Missouri-<br />
Columbia, Columbia, MO<br />
Liane S. Feldman, MD, Associate Professor of<br />
Surgery, McGill University, surgeon, McGill<br />
University Health Centre, Montreal, PQ,<br />
Canada<br />
Edward L. Felix, MD, Assistant Clinical<br />
Professor of Surgery UCSF, UCSF- Fresno,<br />
Director of Bariatric Surgery, Clovis Hospital,<br />
Fresno, CA<br />
John J. Feng, MD, Director, Bariatric Surgery,<br />
Sequoia Hospital, Redwood City, CA<br />
David Field, CFA, Chicago, IL<br />
Abe L. Fingerhut, MD, Professor, College<br />
de médecins de Paris, past chief of Surgery,<br />
Centre Hospitalier Intercommunal, Poissy,<br />
France<br />
Aaron S. Fink, MD, Professor, Department of<br />
Surgery, Emory University School of Medicine,<br />
VISN Chief Surgical Consultant, VAMC -<br />
Atlanta, Decatur, GA<br />
Jean Bernard Flament, MD, 1st Class<br />
Professor, University Hospital of Rheims, Staff<br />
Surgeon, Hopital Robert Debre, France<br />
James W. Fleshman, MD, Professor of Surgery,<br />
Chief Section of Colon and Rectal Surgery,<br />
Washington University in St. Louis, St Louis,<br />
MO<br />
Roberto Fogel, MD, Endoscopic Specialist,<br />
Jackson South Hospital, Miami, FL<br />
Kenneth A. Forde, MD, Jose M. Ferrer<br />
Professor Emeritus of Surgery, Columbia<br />
University, Dobbs Ferry, NY<br />
Dennis L. Fowler, MD, Professor of Clinical<br />
Surgery, Columbia University College of<br />
Physicians and Surgeons, NA, NA, Boston, MA<br />
Morris E. Franklin Jr, MD, Director, Texas<br />
Endosurgery Institute, General Surgeon,<br />
Southeast Baptist Hospital, San Antonio, TX<br />
Gerald M. Fried, MD, Adair Family Professor<br />
and Chairman, Department of Surgery, McGill<br />
University Faculty of Medicine, Surgeonin-Chief,<br />
McGill University Health Centre<br />
Hospitals, Montreal, PQ, Canada<br />
Karl H. Fuchs, MD, Prof. Dr., Goethe University<br />
Frankfu, Markus-Krankenhaus, Frankfurt,<br />
Germany<br />
Daniel J. Gagne, MD, Clinical Associate<br />
Professor of Surgery, Temple University School<br />
of Medicine, Director of Bariatric Surgery, The<br />
Western Pennsylvania Hospital, Pittsburgh, PA<br />
Michel Gagner, MD, Clinical Professor of<br />
Surgery, Florida International University,<br />
Chairman, Department of Surgery, Mount<br />
Sinai Medical Center, Scarsdale, NY<br />
Roberto Gallardo, MD, President of ALACE<br />
/ President of FECCAP, ALACE Asociación<br />
Latinoamericana de Cirujanos Endoscopistas<br />
AND FECCAP Federacion de Cirugia de<br />
Centroamerica y Panamá, Titular Surgeon,<br />
Sanatorio Nuestra Señora del Pilar , Ciudad De<br />
Guatemala, Guatemala<br />
Alex Gandsas, MD, Professor of Surgery,<br />
UMDNJ-SOM, Chairman, Department of<br />
Surgery, UMDNJ - SOM, Statford, NJ<br />
Brice Gayet, MD, Professor of surgery,<br />
Université Paris Descartes, Head of<br />
department, Institut Mutualiste Montsouris<br />
(IMM), Paris, France<br />
Daniel P. Geisler, MD, Associate Professor,<br />
Cleveland Clinic Foundation, Cleveland, OH<br />
Keith E. Georgeson, MD, Professor of Surgery,<br />
University of Alabama School of Medicine,<br />
Director, Division of Pediatric Surgery, The<br />
Children’s Hospital of Alabam, Birmingham, AL<br />
Alec Glover, MBA, Palo Alto, CA<br />
Matthew Randall Goede, MD, Assistant<br />
Professor of Surgery, University of Nebraska<br />
Medical Center, Omaha, NE<br />
Christopher J. Gostout, MD, Professor of<br />
Medicine, Mayo Clinic School of Medicine,<br />
Director of Developmental Endoscopy, Mayo<br />
Clinic, Rochester, MN<br />
Teodor P. Grantcharov, MD, Assistant<br />
Professor, University of Toronto, Staff Surgeon,<br />
St. Michael’s Hospital, Toronto, ON, Canada<br />
Casey J. Graybeal, MD, Northeast Georgia<br />
Medical Center, Gainesville, GA, Gainesville,<br />
GA<br />
Frederick L. Greene, MD, Clinical Professor of<br />
Surgery, University of North Carolina School of<br />
Medicine, Chairman, Department of Surgery,<br />
Carolinas Medical Center, Charlotte, NC<br />
Andrew A. Gumbs, MD, Assistant Professor<br />
of Surgery, Fox Chase Cancer Center, Director<br />
of Minimally Invasive HPB Surgery, Fox Chase<br />
Cancer Center, Philadelphia, PA<br />
Peter T. Hallowell, MD, Assistant Professor,<br />
University of Virginia, Staff, University of<br />
Virginia Health System, Charlottesville, VA<br />
Erik N. Hansen, MD, Senior Pediatric<br />
Surgery Resident, University of Alabama<br />
at Birmingham, The Children’s Hospital of<br />
Alabama, Birmingham, AL<br />
Carroll M. Harmon, MD, Professor of Surgery,<br />
Division of Pediatric Surgery, University of<br />
Alabama at Birmingham, Pediatric Surgeon,<br />
Children’s Hospital of Alabama, Birmingham,<br />
AL<br />
Kristi Lee Harold, MD, Associate Professor<br />
of Surgery, Mayo Clinic Arizona, Director<br />
of Minimally Invasive Surgery, Mayo Clinic<br />
Arizona, Phoenix, AZ<br />
Jeffrey W. Hazey, MD, Associate Professor of<br />
Surgery, The Ohio State University, Attending<br />
Surgeon, The Ohio State University Medical<br />
Center, Columbus, OH<br />
David Hazzan, MD, Director, Minimally<br />
Invasive Surgery, Carmel Medical Center,<br />
Haifa, Israel<br />
B. Todd Heniford, MD, Professor, University<br />
of North Carolina, Chief, Division of<br />
Gastrointestinal and Minimally Invasive<br />
Surgery, Carolinas Medical Center, Charlotte,<br />
NC<br />
Miguel Herrera, MD, Profesor of Endocrine<br />
/ Minimally Invasive Surgery, Universidad<br />
Nacional Autónoma de México, Attending<br />
Surgeon, Instituto Nacional de la Nutrición,<br />
Mexico DF, Mexico<br />
Daniel M. Herron, MD, Associate Professor<br />
of Surgery, Mount Sinai School of Medicine,<br />
Chief, Bariatric Surgery, Mount Sinai Medical<br />
Center, New York, NY<br />
Kelvin D. Higa, MD, Clinical Professor of<br />
Surgery, UCSF, Director of Minimally Invasive<br />
and Bariatric Surgery, Fresno Heart and<br />
Surgical Hospital, Fresno, CA<br />
Jacques M. Himpens, MD, Vinderhoute, OV,<br />
Belgium<br />
Michael D. Holzman, MD, Lester & Sara<br />
Jayne Williams, Chair of Academic Surgery;<br />
Associate Professor of Surgery, Vanderbilt<br />
University, Vanderbilt University Medical<br />
Center, Nashville, TN<br />
Santiago Horgan, MD, Professor of Surgery.,<br />
University of California San Diego, Director<br />
Minimally Invasive Surgery, UCSD Medical<br />
Center, San Diego, CA<br />
Eric Steven Hungness, MD, Assistant Professor<br />
of Surgery, Northwestern University, Chicago,<br />
IL<br />
John Hunter, MD, Mackenzie Professor and<br />
Chair, Dept. of Surgery, Oregon Health &<br />
Science University, Portland, OR<br />
Matthew M. Hutter, MD, Assistant Professor,<br />
Harvard Medical School, Director, Codman<br />
Center for Clinical Effectiveness in Surgery,<br />
Mass. General Hospital, Boston, MA<br />
Sayeed Ikramuddin, MD, Director, Bariatric<br />
Surgery, University of Minnesota, Co-Director,<br />
Center for Minimially Invasive Surgery,<br />
University of Minnesota, Minneapolis, MN<br />
William Barry Inabnet III, MD, FACS,<br />
Associate Professor of Clinical Surgery,<br />
Columbia University, New-York Presbyterian ,<br />
New York, NY<br />
12 th World Congress of Endoscopic Surgery 78
World Congress Invited Faculty List<br />
Haruhiro Inoue, MD, Professor, Digestive<br />
Disease Center, Showa University Northern<br />
Yokohama Hospital, Professor, Digestive<br />
Disease Center, Showa University Northern<br />
Yokhama Hospital, Japan<br />
Gretchen Purcell Jackson, MD, Assistant<br />
Professor of Surgery and Biomedical<br />
Informatics, Vanderbilt University, Assistant<br />
Professor of Surgery, Monroe Carell Jr.<br />
Children’s Hospital at Vanderbil, Nashville, TN<br />
Brian P. Jacob, MD, Attending, Assistant<br />
Clinical Professor of Surgery, Mt. Sinai<br />
Hospital, New York, NY<br />
Garth R. Jacobsen, MD, Assistant Professor,<br />
UCSD, Rancho Santa Fe, CA<br />
Christopher Jamieson, MD, Professor, Dept of<br />
Surgery., Dalhousie University, Staff Surgeon,<br />
Victoria General Hospital<br />
Blair A. Jobe, MD, Professor of Surgery ,<br />
University of Pittsburgh , Surgeon, UPMC<br />
Shadyside, Pittsburgh, PA<br />
Daniel Bougere Jones, MD, Associate<br />
Professor, Harvard Medical School, Chief,<br />
Minimally Invasive Surgical Services;<br />
Director,Simulation and Skills Center;<br />
Director, Ba, Beth Israel Deaconess Medical<br />
Center, Boston, MA, USA<br />
Matthew F. Kalady, MD, Staff Surgeon,<br />
Cleveland Clinic, Cleveland Heights, OH<br />
Timothy D. Kane, MD, Assistant Professor of<br />
Surgery, University of Pittsburgh School of<br />
Medicine, Pediatric Surgeon; Clinical Director<br />
/ Div. of Pediatric Gen. & Thoracic Surgery;<br />
Director, Minimall, Children’s Hospital of<br />
Pittsburgh of UPMC, Pittsburgh, PA<br />
Sergey V. Kantsevoy, MD, Director of<br />
Theapeutic Endoscopy, Institute for Digestive<br />
Health and Liver Disease, Mercy Medical<br />
Center, Baltimore, MD<br />
Kazunori Kasama, MD, Director, Dept of<br />
Weight Loss Surgery, Minimally Invasive<br />
Surgery Center, Yotsuya Medical Cube, Tokyo,<br />
Japan<br />
Zachary Kastenberg, MD, Surgical Resident,<br />
Surgical Resident, Stanford University Hospital<br />
and Clinics<br />
Namir Katkhouda, MD, Professor and Vice<br />
Chairman , University of Southern California,<br />
Chief, Division of General and Laparoscopic<br />
Surgery; Director, Bariatric surgery program,<br />
USC University hospital and LAC -USC Medical<br />
Cente, Los Angeles, CA<br />
L. Brian Katz, MD, Attending, Associate Clinical<br />
Professor, General and Laparoscopic Surgery,<br />
Mt. Sinai Hospital, New York, NY<br />
Nilton Kawahara, MD, Assistant Professor,<br />
MD PhD, University of Sao Paulo School of<br />
Medicine, General Surgeon, Hospital das<br />
Clinicas da FMUSP, Brazil<br />
Chuck Kennedy, Global VP Professional Affairs<br />
& Clinical Education, Covidien, Norwalk, CT<br />
Leena Khaitan, MD, Associate Professor of<br />
Surgery, University Hospitals, Case Medical<br />
Center, Director of Minimally Invasive and<br />
Bariatric Surgery, University Hospital, Geauga<br />
Medical Center, Chagrin Falls, OH<br />
Subhash U. Kini, MD, Asst. Professor Division<br />
of Laparoscopic Surgery, Mount Sinai Medical<br />
Center, Scarsdale, NY<br />
Sue Kirkman, MD, Vice President, Clinical<br />
Affairs, American Diabetes Association,<br />
Staff Physician, Washington Hospital Center,<br />
Indianapolis<br />
Seigo Kitano, MD, Professor, Department of<br />
Surgery I, Oita University Faculty of Medicine,<br />
Chairman, Oita University Hospital, Yufu,<br />
Japan<br />
Shuji Kitashiro, MD, Director of Surgery,<br />
Center for Digestive Disease, Tonan Hospital,<br />
Sapporo, Japan<br />
Shanu N. Kothari, MD, Director of Minimally<br />
Invasive Bariatric Surgery, Gundersen Clinic,<br />
Gundersen Lutheran, La Crosse, WI<br />
Yo Kurashima, MD, Research Fellow,<br />
Steinberg-Bernstein Center for Minimally<br />
Invasive Surgery, McGill University, Japan<br />
Marina Kurian, MD, Asst Professor of surgery,<br />
NYU School of Medicine, Attending Surgeon,<br />
NYU medical center, New York, NY<br />
Antonio M. Lacy, MD, Professor of<br />
Surgery, University of Barcelona, Chief of<br />
Gastrointestinal Surgery, Hospital Clínic,<br />
Barcelona, Spain<br />
Jacob C. Langer, MD, Professor of Surgery,<br />
University of Toronto, Chief, Paediatric General<br />
Surgery, Hospital for Sick Children, Toronto,<br />
ON, Canada<br />
James Lee, MD, Chief, Endocrine Surgery,<br />
Columbia University Medical Center, Assistant<br />
Professor of Surgery, New York Presbyterian<br />
Hospital- Columbia University, New York, NY<br />
Joel Leroy, MD, Associated Professor,<br />
University Hospital of Starsbourg, France,<br />
MD, University Hospital of Strasbourg, France,<br />
Strasbourg, Cedex, France<br />
Michael K.W. Li, MD, FRCS, FRCSE, FCSHK,<br />
FHKAM (Surgery), The University of Hong<br />
Kong, The Chinese University of Hong Kong,<br />
Chief of Service, Department of Surgery,<br />
Pamela Youde Nethersole Eastern Hospital,<br />
Hong Kong, China<br />
Isador Lieberman, MD, Professor of Surgery,<br />
Cleveland Clinic Lerner College of Medicine,<br />
Chairman Spine Department, Cleveland Clinic<br />
Florida, Weston, FL<br />
Demetrius E.M. Litwin, MD, Professor and<br />
Chairman, Department of Surgery, University<br />
of Massachusetts Medical School, Professor<br />
and Chairman, Department of Surgery, UMass<br />
Memorial, Worcester, MA<br />
Thom E. Lobe, MD, Professor, University of<br />
Tennessee Health Sciences Center, Memphis,<br />
TN, Blank Children’s Hospital, Des Moines, IA<br />
Kirk Allen Ludwig, MD, Associate Professor of<br />
Surgery, Medical College of Wisconsin, Chief<br />
of Colorectal Surgery, Froedtert Memorial<br />
Lutheran Hospital, Milwaukee, WI<br />
Markham C. Luke, MD, Clinical Deputy Office<br />
Director/Chief Medical Officer, Food and Drug<br />
Administration, HHS, Bethesda<br />
James D. Luketich, MD, Henry T. Bahnson<br />
Professor of Cardiothoracic Surgery, University<br />
of Pittsburgh, Chief, The Heart, Lung, and<br />
Esophageal Surgery Institute, University of<br />
Pittsburgh Medical Center, Pittsburgh, PA<br />
Bruce V. MacFadyen Jr, MD, Professor of<br />
Surgery, Medical College of Surgery, Chairman<br />
of Surgery, Medical College of Georgia<br />
Hospital, Augusta, GA<br />
Atul K. Madan, MD, Miami, FL<br />
Joseph Mamazza, MD, Chairman, Division<br />
of General Surgery, Director of Minimally<br />
Invasive Surgery, University of Ottawa, Chief<br />
General Surgery, The Ottawa Hospital, Ottawa,<br />
ON, Canada<br />
Jacques Marescaux, MD, Professor of Surgery,<br />
University Louis Pasteur Strasbourg, Chairman<br />
Department Digestive and Endocrine Surgery,<br />
University Hospital of Strasbourg, Strasbourg,<br />
France<br />
Gerald Marks, MD, Professor, Lankenau<br />
Institute for Medical Research, Surgeon,<br />
Section of Colorectal Surgery, Lankenau<br />
Hospital, Wynnewood, PA 19096, Wynnewood,<br />
PA<br />
Jeffrey M. Marks, MD, Associate Professor,<br />
Case Medical Center, Director of Surgical<br />
Endoscopy, University Hospital, Cleveland, OH<br />
John H. Marks, MD, Professor, Lankenau<br />
Institute for Medical Research, Chief, Section<br />
of Colorectal Surgery, Main Line Health<br />
System (3 hospitals), Wynnewood, PA<br />
Michael R. Marohn, MD, Associate Professor<br />
of Surgery, Johns Hopkins University School of<br />
Medicine, Director, Minimally Invasive Surgery<br />
Fellowship, Johns Hopkins, Baltimore, MD<br />
Pamela Martin, MD, Director of Medical<br />
Education, Ethicon Endo-Surgery<br />
Jose M. Martinez, MD, Assistant Professor of<br />
Surgery, University of Miami, Miller School<br />
of Medicine, Chief, Section of Surgical<br />
Endoscopy, Jackson Memorial Hospital,<br />
Miami, FL<br />
Abraham Mathew, MD, Associate Professor of<br />
Medicine, Penn State Hershey Medical Center,<br />
Director of Endoscopy, The Milton S Hershey<br />
Medical Center, Hershey, PA<br />
Samer G. Mattar, MD, Associate Professor of<br />
Surgery, Indiana University, Medical Director,<br />
Clarian Bariatrics, Clarian North Medical<br />
Center, Indianapolis, IN<br />
Kai Matthes, MD, Chief Resident, Harvard<br />
Medical School, Beth Israel Deaconess Medical<br />
Center, Berlin, MA<br />
12 th World Congress of Endoscopic Surgery<br />
79 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
World Congress Invited Faculty List<br />
Brent D. Matthews, MD, Professor of<br />
Surgery, Department of Surgery, Washington<br />
University in St Louis, Chief, Section of<br />
Minimally Invasive Surgery, Barnes-Jewish<br />
Hospital, St Louis, MO<br />
John D. Mellinger, MD, Professor of<br />
Surgery, Medical College of Georgia, Chief<br />
Gastrointestinal Surgery, Residency <strong>Program</strong><br />
Director, Medical College of Georgia, Augusta,<br />
GA<br />
W. Scott Melvin, MD, Professor of Surgery,<br />
The Ohio State University, Director, Center<br />
for Minimally Invasive Surgery, Tho Oho State<br />
University Medical Center, Columbus, OH<br />
Adam T. Meneghetti, MD, Assistant<br />
Professor, Director- Research, Education<br />
and Development, Centre of Excellence for<br />
Surgical Education and Innovation, University<br />
of British Columbia, Vancouver, BC, Canada<br />
Dean J. Mikami, MD, Assistant Professor of<br />
Surgery, The Ohio State University, Assistant<br />
Professor of Surgery, The Ohio State University<br />
Medical Center, Columbus, OH<br />
Bertrand Millat, MD, Head of Department<br />
of Surgery, Saint Eloi Hospital, Montpellier,<br />
France<br />
Karl A. Miller, MD, Associate Professor of<br />
Surgery, Hallein Clinic, General Surgeon,<br />
Bariatric Surgeon, Hallein Clinic, Hallein,<br />
Austria<br />
Rebecca Manget Minter, MD, Assistant<br />
Professor of Surgery, University of Michigan<br />
Department of Surgery, Ann Arbor, MI<br />
Yoav Mintz, MD, Senior Physician, Dept of<br />
General Surgery, Hadassah-Hebrew University<br />
Medical Center, Jerusalem, Israel<br />
John R.T. Monson, MD, Chief of Colorectal<br />
Surgery, Vice Chair of Dept of Surgery,<br />
University of Rochester Medical Center,<br />
Rochester, NY<br />
John M. Morton, MD, Associate Professor,<br />
Stanford University, Director of Bariatric<br />
Surgery and Surgical Quality, Stanford<br />
University Medical Center, Menlo Park, CA<br />
Kenric M. Murayama, MD, Professor of<br />
Surgery, Univ. of Pennsylvania, Chief of<br />
Surgery, Penn Presbyterian Medical Center,<br />
Philadelphia, PA<br />
Didier Mutter, MD, IRCAD/EITS Digestive and<br />
Endocrine Surgery, Strasbourg Cedex, France<br />
Leslie K. Nathanson, MD, VMO, Royal<br />
Brisbane Womens Hospital, Brisbane, QLD,<br />
Australia<br />
Ninh Tuan Nguyen, MD, Professor of Surgery,<br />
University of California Irvine Medical Center,<br />
Chief, Division of Gastrointestinal Surgery,<br />
University of California, Irvine Medical Center,<br />
Orange, CA<br />
Gregg K. Nishi, MD, Assistant Clinical Professor<br />
of Surgery, UCLA/Cedars-Sinai Medical Center,<br />
Director of Outcomes, Minimally Invasive<br />
Surgery, Cedars-Sinai Medical Center, Los<br />
Angeles, CA<br />
Yuri W. Novitsky, MD, Assistant Professor of<br />
Surgery, University of Connecticut School<br />
of Medicine, Chief, Laparoscopic Surgery;<br />
Director, Connecticut Comprehensive Center<br />
for Hernia Repair, University of Connecticut<br />
Health Center, Farmington, CT<br />
Michael S. Nussbaum, MD, Professor and<br />
Chair Department of Surgery, University of<br />
Florida College of Medicine - Jacksonville,<br />
Surgeon-in-Chief, Shands Jacksonville,<br />
Jacksonville, FL<br />
Brant K. Oelschlager, MD, Associate Professor,<br />
University of Washington Department of<br />
Surgery, Seattle, WA<br />
Allan E. Okrainec, MD, Assistant Professor,<br />
University of Toronto, Deputy Head, Division<br />
of General Surgery, Toronto Western Hospital -<br />
University Health Netwo, Toronto, ON, Canada<br />
Dmitry Oleynikov, MD, Associate profesor<br />
of surgery, University of Nebraska Medical<br />
Center, Director of Minimally Invasive and<br />
Computer Aided Surgery, nebraska medical<br />
center, Omaha, NE<br />
Raymond P. Onders, MD, Associate Professor<br />
of Surgery, Case Western Reserve University,<br />
Director of Minimally Invasive Surgery,<br />
University Hospitals Case Medical Center,<br />
Shaker Heights, OH<br />
Chinnasamy Palanivelu, MCH(GE), GEM<br />
Hospital and Research Center, Coimbatore,<br />
Tamil Nadu, India<br />
Juan P. Pantoja, MD, Attending Surgeon,<br />
Instituto Nacional de Ciencias Medicas<br />
y Nutricion Salvador Zubiran, Attending<br />
Surgeon, Instituto Nacional de Ciencias<br />
Medicas y Nutricion, Mexco DF, Mexico<br />
Neely Panton, MD, Clinical Professor, Head,<br />
Division of General Surgery, UBC, University<br />
of British Columbia, Head, Division of<br />
General Surgery, Vancouver General Hospital,<br />
Vancouver, Canada<br />
Adrian E. Park, MD, Campbell & Jeannette<br />
Plugge Professor of Surgery, University of<br />
Maryland, Head General Surgery, University of<br />
Maryland Medical Center, Baltimore, MD<br />
John J. Park, MD, Clinical Assistant Professor of<br />
Surgery, University of Illinois, Clinical Assistant<br />
Professor of Surgery, University of Illinois<br />
Medical Center, Park Ridge, IL<br />
Carlos A. Pellegrini, MD, The Henry N. Harkins<br />
Professor and Chair, University of Washington,<br />
Seattle, WA<br />
Jacques J. Perissat, MD, Professeur Emeritus,<br />
DETERCA Université Victor Ségalen Bordeaux<br />
II, Bordeaux, France<br />
Jeffrey H. Peters, MD, Professor & Chairman<br />
Department of Surgery, University of<br />
Rochester, Surgeon in Chief, Strong Memorial<br />
Hospital, Rochester, NY<br />
Edward H. Phillips, MD, Clinical Associate<br />
Professor of Surgery, University of Southern<br />
California, Los Angeles County Hospital,<br />
Executive Vice-Chairman, Department of<br />
Surgery, Cedars-Sinai Medical Center, Los<br />
Angeles, CA<br />
12 th World Congress of Endoscopic Surgery 80<br />
Alessio Pigazzi, MD, Assistant Professor of<br />
Surgery, City of Hope , City of Hope National<br />
Medical Center, Duarte, CA<br />
Tim Pitney, Vice President, Investment<br />
Advisory, Sapers & Wallack, Inc., Newton, MA<br />
Alfons Pomp, MD, Leon C. Hirsch Professor<br />
of Surgery, Weill Medical College of Cornell<br />
University, Attending Surgeon, New York<br />
Presbyterian Hospital, New York, NY<br />
Jeffrey L. Ponsky, MD, Professor and Chairman,<br />
Department of Surgery, Case Western Reserve<br />
University School of Medicine, Surgeonin-Chief,<br />
University Hospitals Case Medical<br />
Center, Moreland Hill, OH<br />
Benjamin K. Poulose, MD, MPH, Vanderbilt<br />
University, Assistant Professor, Surgery,<br />
Vanderbilt University Medical Center,<br />
Nashville, TN<br />
Rhonda J. Prewitt, MIS <strong>Program</strong> Associate, MIS<br />
Fellowship Coordinator, University Nebraska<br />
Medical Center, Omaha, NE<br />
Jose Manuel Prince, MD, Fellow, University<br />
of Pittsburgh, Fellow, Children’s Hospital of<br />
Pittsburgh, Pittsburgh, PA<br />
Aurora Dawn Pryor, MD, Associate Professor<br />
of Surgery, Duke University Medical Center,<br />
Division Chief, General Surgery, Durham<br />
Regional Hospital, Durham, NC<br />
Karim Qayumi, MD, Professor of Surgery<br />
Director of the Center of Excellence for<br />
Simulation Education & Innovation, University<br />
of BC, VGH, Vancouver General Hospital,<br />
Vancouver, B.C., Canada<br />
Sonia L. Ramamoorthy, MD, Assistant<br />
Professor of Surgery, UC San Diego Medical<br />
Ctr., UCSD Medical Center, La Jolla, CA<br />
Bruce J. Ramshaw, MD, Associate Professor,<br />
Surgery, University of Missouri, Chief, General<br />
Surgery, University of Missouri, Columbia, MO<br />
Abhay Rane, MD, Consultant Urological<br />
Surgeon, East Surrey Hospital, United Kingdom<br />
Prashanth Prabhakar Rao, MD, Chief, Dept. of<br />
MAS, Mamata Hospital, Dombivli (E), India<br />
G. V. Rao, MS, MAMS, Chief of GI and<br />
Minimally Invasive Surgery, Asian Institute of<br />
Gastroenterology, Director, Asian Institute of<br />
Gastroenterology, Sohajiguda, Hyderabad,<br />
India<br />
David W. Rattner, MD, Professor of Surgery,<br />
Harvard Medical School, Chief Division<br />
of General and Gastrointestinal Surgery,<br />
Massachusetts General Hospital, 15 Parkman<br />
St #460, MA<br />
Kevin M. Reavis, MD, Assistant Clinical<br />
Professor, University of California, Irvine<br />
Medical Center, Assistant Clinical Professor,<br />
University of California, Irvine Medical Center,<br />
Orange, CA<br />
Petachia Reissman, MD, Associate Professor<br />
of Surgery, Hebrew University School of<br />
Medicine Jerusalem, Israel, Chairman,<br />
Department of General Surgery, Shaare-Zedek<br />
Medical Center, Jerusalem, Israel, Jerusalem,<br />
Israel
World Congress Invited Faculty List<br />
Feza Remzi, MD, MD, FACS, FASCRS, Ed and<br />
Joey Chair in Colorectal Surgery, Chairman,<br />
Dept. of Colorectal Surgery, The Cleveland<br />
Clinic, Department of Colorectal Surgery, The<br />
Cleveland Clinic, Cleveland, OH<br />
Jose Ribamar Azevedo, MD, Doctor of<br />
General Surgery from Federal University of<br />
Rio de Janeiro-RJ-Brazil, Private, Teacher of<br />
General Surgery from Federal University of Rio<br />
de Janeiro-RJ-Brazil, Samaritano Hospital and<br />
Copa D’Or Hospital (both in Rio de Janeiro),<br />
Sao Paulo, Brazil<br />
William O. Richards, MD, Ingram Professor<br />
of Surgical Sciences, Vanderbilt University,<br />
Director of Center for Surgical Weight Loss,<br />
Vanderbilt University Medical Center, Mobile,<br />
AL<br />
E. Matt Ritter, MD, Chief, Minimally Invasive<br />
Surgery and Emerging Technologies Assistant<br />
Professor of Surgery, Uniformed Services<br />
University, Chief, Laparoscopic Surgery,<br />
National Naval Medical Center, Gaithersburg,<br />
MD<br />
Homero Rivas, MD, Assistant Professor,<br />
Stanford University, MD, MBA, FACS, Stanford<br />
University Medical Center, Dallas, TX<br />
Sergio Roll, MD, MD, PhD, Clinical Professor<br />
of Surgery, University Positivo-School of<br />
Medicine, Brazil, O. Cruz German Hospital, O.<br />
Cruz German Hospital, Sao Paulo, Brazil<br />
John R. Romanelli, MD, Assistant Professor of<br />
Surgery, Tufts University School of Medicine,<br />
Medical Director, Bariatric Surgery, Baystate<br />
Medical Center, Springfield, MA<br />
Michael J. Rosen, MD, Assistant Professor of<br />
Surgery, Case Medical Center, Chief, Division<br />
of Gastrointestinal and General Surgery,<br />
University Hospitals of Cleveland, Cleveland,<br />
OH<br />
Raul J. Rosenthal, MD, Associate Professor<br />
of Surgery, University of South Florida ,<br />
Chairman, Bariatric and metabolic Institute<br />
and Section Head of Minimally Invasive<br />
Surgery, Cleveland Clinic Florida, Weston, FL<br />
James B. Rosser Jr, MD, Professor of Clinical<br />
Surgery, Morehouse School of Medicine,<br />
Attending Surgeon, Grady Memorial Hospial,<br />
Spring, TX<br />
Francesco Rubino, MD, Associate Professor of<br />
Surgery, Weill-Cornell Medical College, Chief,<br />
Section of Gastrointestinal Metabolic Surgery,<br />
New York Presbyterian Hospital, Strasbourg,<br />
France<br />
Eric Rullier, MD, Professor of Surgery,<br />
University of Bordeaux, Chairman department<br />
of colorectal surgery, Saint-Andre Hospital,<br />
France<br />
Adheesh A. Sabnis, MD, Co-Driector of<br />
Minimally Invasive and Laparoscopic Surgery,<br />
Good Samaritan Hospital, Baltimore, MD<br />
Barry A. Salky, MD, Professor of Surgery;<br />
Division of Laparoscopic Surgery, Mount<br />
Sinai School of Medicine, Attending Surgeon,<br />
Mount Sinai Hospital, New York, NY<br />
Aviva Sapers, CEO, Sapers & Wallack, Inc.,<br />
Newton, MA<br />
Abeezar I. Sarela, MD, Honorary Senior<br />
Lecturer, The University of Leeds, Consultant<br />
in Upper GI & Bariatric Surgery, St James’s<br />
University Hospital, Leeds, United Kingdom<br />
Richard M. Satava, MD, Professor of Surgery,<br />
University of Washingotn Medical Center,<br />
Professor of Surgery, University of Washington<br />
Medical Center, Seattle, WA<br />
Philip R. Schauer, MD, Professor of Surgery,<br />
Lerner College of Medicine, Director,<br />
Advanced Laparoscopic & Bariatric Surgery,<br />
Clevleand Clinic, Cleveland, OH<br />
Bruce D. Schirmer, MD, Stephen H. Watts<br />
Professor of Surgery, University of Virginia<br />
Health System, Vice Chair, Department of<br />
Surgery, University of Virginia Health System,<br />
Charlottesville, VA<br />
Christopher M. Schlachta, MD, Associate<br />
Professor, Departments of Surgery and<br />
Oncology, University of Western Ontario,<br />
Medical Director, CSTAR (Canadian Surgical<br />
Technologies and Advanced Robotics),<br />
London Health Sciences Centre, London, ON,<br />
Canada<br />
Steven D. Schwaitzberg, MD, Associate<br />
Professor of Surgery, Harvard Medical School,<br />
Chief of Surgery, Cambridge Health Alliance,<br />
Cambridge, MA<br />
Daniel J. Scott, MD, Associate Professor of<br />
Surgery, University of Texas Southwestern<br />
Medical Center, Director, Southwestern Center<br />
for Minimally Invasive Surgery, Dallas, TX<br />
Carol E. Scott-Conner, MD, Professor, Division<br />
of Surgical Oncology and Endocrine Surgery,<br />
University of Iowa Hospitals & Clinics, Iowa<br />
City, IA<br />
Donna See, MD, Columbia University Science &<br />
Technology Ventures, New York, NY<br />
Don J. Selzer, MD, Associate Professor<br />
of Surgery, Indiana University School of<br />
Medicine, General Surgeon, Clarian Health<br />
Partners, Inc., Indianapolis, IN<br />
Neal E. Seymour, MD, Professor, Tufts<br />
University, Division Chief General Surgery,<br />
Baystate Medical Center, Springfield, MA<br />
Paresh C. Shah, MD, <strong>Program</strong> Director<br />
General Surgery, Lenox Hill Hospital, Chief<br />
of Laparoscopic Surgery, Lenox Hill Hospital,<br />
New York, NY<br />
Baiju R. Shah, CEO, BioEnterprise, Cleveland, OH<br />
Scott A. Shikora, MD, Professor of Surgery, Tufts<br />
University School of Medicine, Chief, Divisions<br />
of General, Bariatric and Minimally Invasive<br />
Surgery, Tufts Medical Center, Sharon, MA<br />
Samuel Shuchleib, MD, Professor, National<br />
University of Mexico, Executive Director, Latin<br />
American Federation of Surgical Societies,<br />
Mexico City, Mexico<br />
Allan E. Siperstein, MD, Professor of Surgery,<br />
Cleveland Clinic, Chair, Surgery Institute,<br />
Cleveland Clinic, Cleveland, OH<br />
C. Daniel Smith, MD, Professor and Chair,<br />
Mayo School of Medicine, Mayo Clinic -<br />
Florida, Jacksonville, FL<br />
Luc Soler, MD, Research Project Manager,<br />
IRCAD, Strasbourg, France<br />
Toyooki Sonoda, MD, Assistant Attending<br />
Surgeon, NewYork-Presbyterian Hospital/Weill<br />
Cornell Medical Center, Assistant Professor of<br />
Surgery, Weill Cornell Medical College, New<br />
York, NY<br />
Nathaniel J. Soper, MD, Loyal and Edith Davis<br />
Professor and Chair of Surgery, Northwestern<br />
University Feinberg School of Medicine,<br />
Surgeon-in-Chief, Northwestern Memorial<br />
Hospital, Chicago, IL<br />
Mike Stahl, MD, Distinguished Professor of<br />
Management, Director of Physician Executive<br />
MBA <strong>Program</strong>, University of Tennessee,<br />
Knoxville, TN<br />
Steven C. Stain, MD, Professor and Chair,<br />
Albany Medical College, Chief of Surgery,<br />
Albany Medical Center Hospital, Albany, NY<br />
Greg V. Stiegmann, MD, Professor of Surgery,<br />
University of Colorado Denver School of<br />
Medicine, Vice President Clinical Affairs,<br />
University of Colorado Hospital, Aurora, CO<br />
Vivian E.M. Strong, MD, Assistant Attending<br />
Surgeon, Memorial Sloan-Kettering Cancer<br />
Center, Assistant Professor of Surgery, Weill<br />
Medical College of Cornell University, New<br />
York, NY<br />
Lee L. Swanstrom, MD, Clinical Professor of<br />
Surgery, Oregon Health Sciences University,<br />
Director, Division of Minimally Invasive<br />
Surgery, Legacy Health System, Portland, OR<br />
Patricia Sylla, MD, Instructor in Surgery,<br />
Harvard University, Assistant in Surgery,<br />
Massachusetts General Hospital, Boston, MA<br />
Zoltan Szabo, PhD, Visiting Professor, Institute<br />
of Surgical Research, University of Szeged<br />
Medical School, Hungary, Director, MOET<br />
Institute, San Francisco, CA, San Francisco, CA<br />
Amir Szold, MD, Senior Lecturer, Sackler<br />
School of Medicine, Tel Aviv University,<br />
Department of Surgery B, Tel Aviv Sourasky<br />
Medical Center, Tel Aviv, Israel<br />
Mark A. Talamini, MD, Professor and<br />
Chairman, Department of Surgery, University<br />
of California, San Diego, Surgeon-in-Chief,<br />
UCSD Medical Center, San Diego, CA<br />
Eduardo Targarona, MD, Professor of Surgery,<br />
Autonomous University of Barcelona, Director<br />
Unit Gastrointestinal & Hematological Surgery,<br />
Hospital de Santpau, Barcelona, Spain<br />
Craig J. Taylor, MD, Dr, University of Sydney,<br />
Dr, Concord General Hospital, Balgowlah,<br />
NSW, Australia<br />
Julio A. Teixeira, MD, Associate Clinical<br />
professor of Surgery, Columbia University,<br />
Chief Division of Minimally :invasive Surgery,<br />
St.Luke’s-Roosevelt Hospital Center, New York,<br />
NY<br />
12 th World Congress of Endoscopic Surgery<br />
81 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
World Congress Invited Faculty List<br />
Michael H. Thomson, MD, Consultant<br />
in Pediatric Gastroenterology, Sheffield<br />
Childrens NHS Trust, Bristol, United Kingdom<br />
Christopher C. Thompson, MD, Assistant<br />
Professor of Medicine, Harvard Medical<br />
School, Director of Developmental Endoscopy,<br />
Brigham and Women’s Hospital, Boston, MA<br />
Augusto Almeida Tinoco, MD, Chief of<br />
Laparoscopic Surgery, Hospital Sao Jose do<br />
Avai, Itaperuna, Brazil<br />
Alfonso Torquati, MD, Associate Professor of<br />
Surgery, Duke University, Director Minimally<br />
Invasive Surgery Research, Durham, NC<br />
Shirin Towfigh, MD, Visiting Associate<br />
Professor of Clinical Surgery, Cedars-Sinai<br />
Medical Center, Los Angeles, CA<br />
L. William Traverso, MD, Clinical Professor of<br />
Surgery, University of Washington, Director<br />
Digestive Disease Institute - Pancreas Section,<br />
Virginia Mason Medical Center, Seattle, WA<br />
Thadeus L. Trus, MD, Associate Professor<br />
of Surgery, Dartmouth-Hitchcock Medical<br />
Center, Dartmouth-Hitchcock Medical Center,<br />
Lebanon, NH<br />
Shawn T. Tsuda, MD, Assistant Professor<br />
of Surgery, University of Nevada School of<br />
Medicine, Surgeon, University Health System,<br />
Las Vegas, NV<br />
Surendra M. Ugale, MD, Director of Metabolic<br />
& Advanced Laparoscopic Surgery, Kirloskar<br />
Hospital, Hyderabad, India<br />
David R. Urbach, MD, Associate Professor<br />
of Surgery and Health Policy, Management<br />
and Evaluation, University of Toronto, Staff<br />
Surgeon, University Health Network, Toronto,<br />
ON, Canada<br />
Melina C. Vassiliou, MD, Assistant Professor<br />
of Surgery, McGill University Health Centre,<br />
Assistant Professor of Surgery, Montreal<br />
General Hospital, Montreal, PQ, Canada<br />
Ashley Vernon, MD, Instructor, Harvard<br />
Medical School, Associate Surgeon, Brigham &<br />
Women’s Hospital, Boston, MA<br />
Leonardo Villegas, MD, General Surgery,<br />
UMKC, Durham, NC<br />
Anthony J. Vine, MD, Attending, Assistant<br />
Clinical Professor, General and Laparoscopic<br />
Surgery, Mt. Sinai Hospital, New York, NY<br />
Guy R. Voeller, MD, Professor of Surgery,<br />
University of Tennessee, Memphis, TN<br />
Daniel Von Renteln, MD, Department of<br />
Interdisciplinary Endoscopy, University<br />
Hospital Hamburg-Eppendorf, Hamburg,<br />
Germany<br />
Go Wakabayashi, MD, Professor and<br />
Chairman, Department of Surgery, Iwate<br />
Medical University, Surgeon-in-Chief, Iwate<br />
Medical University Hospital, Morioka-city,<br />
Japan<br />
Martin Walz, MD, Prof. Dr. Dr., University of<br />
Essen, Kliniken Essen-Mitte, Germany<br />
Eric Glenn Weiss, MD, Vice Chairman,<br />
Department of Colorectal Surgery, DIO &<br />
Chairman of Graduate Medical Education,<br />
Residency <strong>Program</strong> Director, Cleveland Clinic<br />
Florida, Weston, FL<br />
Steven D. Wexner, MD, Professor of Surgery,<br />
Ohio State University, Chief Academic Officer,<br />
Cleveland Clinic Florida, Weston, FL<br />
R. Larry Whelan, MD, Professor of Surgery,<br />
Columbia University, Chief Of Surgical<br />
Oncology, St. Luke’s Roosevelt HospitaL, New<br />
York, NY<br />
Mark H. Whiteford, MD, Clinical Associate<br />
Professor, Oregon Health & Science University,<br />
Director, Colorectal Surgery <strong>Program</strong>,<br />
Providence Portland Medical Center, Portland,<br />
OR<br />
Tatsuo Yamakawa, MD, Emeritus Professor<br />
of of Surgery, Teiyo University School of<br />
Medicine, Professor of Surgery, Teikyo<br />
Uiversity Hospita, at Mizonokuchi, Tokyo,<br />
Japan<br />
Manabu Yamamoto, MD, Director and<br />
Chairman, Adachi Kyosai Hospital, Tokyo,<br />
Japan<br />
Han-Kwang Yang, MD, Professor, Seoul<br />
National University College of Medicine,<br />
Professor, Seoul National University Hospital,<br />
South Korea<br />
Tonia M. Young-Fadok, MD, Professor of<br />
Surgery, Mayo Clinic, Chair, Division of Colon<br />
and Rectal Surgery, Mayo Clinic, Phoenix, AZ<br />
Natan Zundel, MD, Clinical Professor of<br />
Surgery, F I U, Miami Beach, FL<br />
12 th World Congress of Endoscopic Surgery 82
World Congress Faculty & Presenter Disclosures<br />
The following presenters, faculty, <strong>SAGES</strong> Board of Governors, <strong>Program</strong> and Continuing Education Committee Members do not have any relevant<br />
financial relationships or significant commercial interests associated with their participation at the <strong>2010</strong> World Congress meeting. If name is not listed<br />
below, please refer to the following pages.<br />
Brij B Agarwal<br />
Krishna A Agarwal<br />
Rajesh Aggarwal<br />
Craig T. Albanese<br />
Frances Allocco<br />
S. Al-Sabah<br />
Luigi Angrisani<br />
Chandrakanth Are<br />
Maurice E. Arregui<br />
Theodor Asgeirsson<br />
Vikram Attaluri<br />
Shahin Ayazi<br />
Asghar Azadani<br />
Jose Ribamar Azevedo<br />
Sharon L. Bachman<br />
Heidi Bahna<br />
Fady Kamal Balaa<br />
Virinder K Bansal<br />
Limaris Barrios<br />
Linda Barry<br />
Katherine A. Barsness<br />
Nicola Basso<br />
Bruce Behn<br />
Estuardo J. Behrens<br />
Richard H. Bell<br />
Simon Bergman<br />
Jai Bikhchandani<br />
Daniel W. Birch<br />
Simon Biron<br />
Raghid S Bitar<br />
James G. Bittner<br />
Victor Bochkarev<br />
Alexandre Bouchard<br />
Steven P. Bowers<br />
Matias Bruzoni<br />
Luis E. Burbano<br />
Angel M Caban<br />
Michael J. Cahalane<br />
Ronan A. Cahill<br />
Guilherme M Campos<br />
Antonio O Castellvi<br />
Rose S.M. Chan<br />
Bipan Chand<br />
Ryan A Chandhoke<br />
Eric Changchien<br />
Hester Cheung<br />
Gyu-Seog Choi<br />
Elie Chouillard<br />
Elie K Chouillard<br />
Alberto Chousleb<br />
Elias Chousleb<br />
Pradeep K. Chowbey<br />
W. Y. Chung<br />
Tatyan Clarke<br />
Ricardo V. Cohen<br />
Nathan E Conway<br />
Manolo Cortez<br />
Federico Costantino<br />
Ismael Court<br />
Angel Cuadrado<br />
Christopher Cunningham<br />
Sir Alfred Cuschieri<br />
Allan Dackiw<br />
Gregory F. Dakin<br />
Bernard Dallemagne<br />
Abhay N Dalvi<br />
Donald M Davis<br />
Aureo L. De Paula<br />
Edmundo Dedios Orozco<br />
Nicolas Demartines<br />
Ithaar H Derweesh<br />
Ashwin L deSouza<br />
Daniel J. Deziel<br />
Ushast Dhir<br />
Andre Dhoore<br />
Robert DiRaddo<br />
Quan-Yang Duh<br />
Kristen R Earle<br />
Paula K Edelson<br />
Claire Edwards<br />
Michael B. Edye<br />
Jonathan E. Efron<br />
Ahmed R El-Geidie<br />
Casey J. Grabeal<br />
Timothy M. Farrell<br />
Nicole M. Fearing<br />
John J. Feng<br />
Alberto R Ferreres<br />
David Field<br />
Abe L. Fingerhut<br />
Aaron S. Fink<br />
Heidi L Fitzgerald<br />
Jean Bernard Flament<br />
Roberto Fogel<br />
Kenneth A. Forde<br />
Morris E Franklin<br />
Karl H. Fuchs<br />
Daniel J. Gagne<br />
Roberto Gallardo<br />
Alex Gandsas<br />
Denise W. Gee<br />
Daniel P. Geisler<br />
Keith E. Georgeson<br />
Iman Ghaderi<br />
Saber Ghiassi<br />
Matthew Randall Goede<br />
Trudie A Goers<br />
Ke Gong<br />
Jon Gould<br />
Teodor P. Grantcharov<br />
John C Graybill<br />
Frederick L. Greene<br />
Andrew A. Gumbs<br />
Prateek K Gupta<br />
Peter T. Hallowell<br />
M Hamada<br />
Erik N. Hansen<br />
Kristi Lee Harold<br />
Vincent L Harrison<br />
Eugenius J Harvey<br />
David Hazzan<br />
Vanessa P Ho<br />
Elizabeth Honigsberg<br />
William W Hope<br />
John Hunter<br />
Matthew M. Hutter<br />
Haruhiro Inoue<br />
Takeaki Ishizawa<br />
Eran Itzkowitz<br />
Gretchen Purcell Jackson<br />
Timothy D Jackson<br />
Samuel Jacob<br />
Garth R. Jacobsen<br />
David James<br />
Christopher Jamieson<br />
Balaji Jangam<br />
Shiva Jayaraman<br />
David J Kaczorowski<br />
Matthew F. Kalady<br />
Jawaid Kalim<br />
Timothy D. Kane<br />
Sergey V. Kantsevoy<br />
Kazunori Kasama<br />
Zachary Kastenberg<br />
Nilton Kawahara<br />
Leena Khaitan<br />
Michael J Kim<br />
Subhash U. Kini<br />
Sue Kirkman<br />
Seigo Kitano<br />
Shuji Kitashiro<br />
Bastiaan R Klarenbeek<br />
Amanda J Kravetz<br />
Sachin S Kukreja<br />
Birte Kulemann<br />
Yo Kurashima<br />
Antonio M. Lacy<br />
Pawanindra Lal<br />
Jacob C. Langer<br />
Antonio D Lassaletta<br />
Wai Lun Law<br />
Gyusung Lee<br />
James Lee<br />
Young-Joon Lee<br />
Andras Legner<br />
Eli N. Lerner<br />
Joel Leroy<br />
Emanuele Lezoche<br />
Michael K.W. Li<br />
Song Liang<br />
Dimitrios A. Linos<br />
Demetrius E.M. Litwin<br />
Markham C. Luke<br />
Bruce V. MacFadyen Jr<br />
Atul K. Madan<br />
Jacques Marescaux<br />
Gerald Marks<br />
Michael R. Marohn<br />
Abraham Mathew<br />
Ronald Matteotti<br />
David A. McClusky<br />
Marian P. McDonald<br />
Stephen S. McNatt<br />
Adam T. Meneghetti<br />
Carlos A Menezes<br />
Bertrand Millat<br />
Karl A. Miller<br />
Rebecca Manget Minter<br />
Danilo Miskovic<br />
Derek E Moore<br />
John M. Morton<br />
Didier Mutter<br />
Omer Nasir<br />
Leslie K. Nathanson<br />
Adrian Marius Nedelcu<br />
Scott Quy Nguyen<br />
Thinh H Nguyen<br />
Juan J. Nogueras<br />
Michael S. Nussbaum<br />
Kathleen O’Connell<br />
Tomonori Ohsawa<br />
Allan Okrainec<br />
Pablo E Omelanczuk<br />
Sean B Orenstein<br />
Ismail H Ozerhan<br />
John T. Paige<br />
C Palanivelu<br />
Chinnasamy Palanivelu<br />
Juan P. Pantoja<br />
Chan W Park<br />
John J. Park<br />
Michael Parker<br />
Marco G. Patti<br />
Eric M Pauli<br />
Nikhil Pawa<br />
Suraj B Pawar<br />
Jacques J. Perissat<br />
Silvana Perretta<br />
Edward H. Phillips<br />
Alessio Pigazzi<br />
Rodrigo A Pinto<br />
Timothy Pitney<br />
Mun Jye Poi<br />
Benjamin K. Poulose<br />
Pornthape Prathanvanich<br />
Rhonda J. Prewitt<br />
Jose Manuel Prince<br />
Shailesh Puntambekar<br />
Karim Qayumi<br />
Abhay Rane<br />
G. V. Rao<br />
Prashanth Prabhakar Rao<br />
Petachia Reissman<br />
Feza Remzi<br />
Jason F Reynoso<br />
William S. Richardson<br />
Homero Rivas<br />
Sergio Roll<br />
John R. Romanelli<br />
Raul Rosenthal<br />
James B. Rosser Jr<br />
Dan Ruiz<br />
Eric Rullier<br />
Mohamad D Saad<br />
Adheesh A. Sabnis<br />
Aviva Sapers<br />
Abeezar I. Sarela<br />
Bruce D. Schirmer<br />
Wayne H. Schwesinger<br />
Carol E. Scott-Conner<br />
Donna See<br />
P Senthilnathan<br />
Elliot L Servais<br />
Paul A. Severson<br />
Neal E. Seymour<br />
Baiju R. Shah<br />
Scott A. Shikora<br />
Samuel Shuchleib<br />
Gerd R Silberhumer<br />
Allan E. Siperstein<br />
C. Daniel Smith<br />
Brad E Snyder<br />
Luc Soler<br />
Michael Stahl<br />
Steven C. Stain<br />
Vivian E.M. Strong<br />
Erica Sutton<br />
John F. Sweeney<br />
Nobumi Tagaya<br />
Eduardo Targarona<br />
EM Targarona<br />
Craig J. Taylor<br />
Sarah K Thompson<br />
Michael H. Thomson<br />
Augusto Almeida Tinoco<br />
Augusto c Tinoco<br />
Manish M Tiwari<br />
Shirin Towfigh<br />
L. William Traverso<br />
Albert W Tsang<br />
David R. Urbach<br />
Kent R. Van Sickle<br />
Oliver A Varban<br />
Esteban Varela<br />
Melina C. Vassiliou<br />
Khashayar Vaziri<br />
Ashley Vernon<br />
Leonardo Villegas<br />
Daniel Von Renteln<br />
Go Wakabayashi<br />
Martin Walz<br />
Carl J. Westcott<br />
Yanghee Woo<br />
Tatsuo Yamakawa<br />
Manabu Yamamoto<br />
Jun Yan<br />
Han-Kwang Yang<br />
Tonia M. Young-Fadok<br />
Yassar Youssef<br />
Jacqui C. Zhu<br />
12 th World Congress of Endoscopic Surgery<br />
83 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
World Congress Faculty & Presenter Disclosures<br />
The following presenters, faculty, <strong>SAGES</strong> Board of Governors, <strong>Program</strong> and Continuing Education Committee Members provided information indicating<br />
they have a financial relationship with a proprietary entity producing health care goods or services, with the exemption of non-profit or government<br />
organizations and non-health care related companies. (Financial relationships can include such things as grants or research support, employee,<br />
consultant, major stockholder, member of speaker’s bureau, etc.)<br />
Name Commercial Interest What was received For what role Other<br />
Gina L. Adrales WL Gore Honoraria Speaking/Teaching<br />
Ethicon Endosurgery Honoraria Speaking/Teaching<br />
Mehran Anvari<br />
Astra-Zeneca Honoraria Speaking/Teaching<br />
Enteromedics Honoraria Advisory Committee<br />
Ethicon Endosurgery Honoraria Advisory Committee<br />
Horacio J. Asbun Doctors Company Honoraria Consultant<br />
Ziad T. Awad Genzyme Biosurgery Honoraria Speaking/Teaching<br />
Simon Bergman<br />
Paladin Labs Consulting Fee Consulting<br />
Covidien Consulting Fee Consulting<br />
Ramon Berguer Ethicon Honoraria Speaking/Teaching<br />
Covidien Consulting Fee Consultant<br />
Marc Bessler<br />
Satiety Other Other Investigator in Trial<br />
GI Dynamics Consulting Fee Advisory Committee<br />
Olympus Consulting Fee Consultant<br />
Jeffrey A Blatnik<br />
LifeCell Honorarium Speaking and/or Teaching<br />
Covidien Honorarium Speaking and/or Teaching<br />
Ethicon Honoraria Other Educational grant<br />
Fredrick J. Brody Nutricia North America Consulting Fee Consultant<br />
Covidien<br />
Consulting Fee<br />
Muskuloskeletal Transplant<br />
Foundation<br />
Consulting Fee<br />
Consulting<br />
Shaun R Brown<br />
Ethicon EndoSurgery Consulting Fee Consulting<br />
Atrium Medical Consulting Fee Consulting<br />
Covidien Honoraria Speaking/Teaching<br />
Ethicon Endosurgery Honoraria Speaking/Teaching<br />
Ethicon Endosurgery Other Other<br />
L. Michael Brunt<br />
Karl Storz Endoscopy Other Other<br />
Lifecell Corp Other Other<br />
Stryker Honoraria Consultant<br />
Stryker Endoscopy Other Other<br />
Cook Medical Honoraria Speaking/Teaching<br />
American Board of Surgery Salary Employment<br />
Jo Buyske<br />
Sunstones Biotech Ownership Interest Other<br />
my spouse is chief<br />
scientific officer<br />
W.L. Gore and Associates Honoraria Speaking/Teaching<br />
Alfredo M. Carbonell W.L. Gore and Associates Consulting Fee Consultant<br />
Ethicon Inc. Consulting Fee Advisory Committee<br />
Abbott Ross Laboratories Other Financial Benefit Other Activities Grant/Financial Support<br />
Ronald Hanson<br />
Clements<br />
Cardinal Healthcare/<br />
Snowden-Pencer<br />
Honoraria<br />
Advisory Committee<br />
Covidien Consulting Fee Review Panel<br />
Olympus Consulting Fee Consultant<br />
Karl Storz Endoscopy Other Financial Benefit Other Activities<br />
Educational grant<br />
support<br />
Daniel R Cox<br />
Covidien Honorarium Speaking and/or Teaching<br />
Ethicon Endosurgery Honorarium Speaking and/or Teaching<br />
David L. Crawford Intuitive Surgical Honoraria Other Preceptor/Proctor<br />
Storz Honoraria Speaking/Teaching<br />
Paul G. Curcillo II<br />
Olympus Honoraria Speaking/Teaching<br />
Ethicon Honoraria Speaking/Teaching<br />
Microline Honoraria Speaking/Teaching<br />
Conor P. Delaney<br />
Covidien Honoraria Speaking/Teaching<br />
Adolor Honoraria Advisory Committee<br />
12 th World Congress of Endoscopic Surgery 84
World Congress Faculty & Presenter Disclosures<br />
Name Commercial Interest What was received For what role Other<br />
Brian J. Dunkin<br />
Covidien<br />
Consulting Fee<br />
Ethicon Consulting Fee Consultant<br />
Sanjeev Dutta<br />
Stryker Endoscopy Consulting Fee Consultant<br />
Novare Consulting Fee Advisory Committee<br />
Lifeguard Other Advisory Committee<br />
David Bryan Earle<br />
Covidien Other Other Fellowship Grant<br />
Atrium Medical Consulting Fee Consultant<br />
Surgiquest Honoraria Advisory Committee<br />
David W. Easter<br />
Cubist<br />
Honoraria<br />
MedWaves Other Advisory Committee<br />
Olympus Consulting Fee Consultant<br />
Steven Edmundowicz Boston Scientific Consulting Fee Advisory Committee<br />
BARRX Consulting Fee Speaking/Teaching<br />
Barosense Ownership Interest Other Major Stockholder<br />
Steve Eubanks<br />
Ethicon Other Other Grant Funding<br />
Stryker Other Other Grant Funding<br />
Transenterix Honoraria Advisory Committee<br />
Ethicon Canada Other Other<br />
Unrestricted Educational<br />
grant<br />
Liane S. Feldman Covidien Canada Consulting Fee Speaking/Teaching<br />
Covidien Canada Other Other<br />
Unrestricted education<br />
grant<br />
Paré Surgical Other Consultant<br />
Edward L. Felix<br />
Power Medical Consulting Fee Consultant<br />
Cardica Consulting Fee Consultant<br />
Covidien Honoraria Speaking/Teaching<br />
Dennis L. Fowler Applied Medical Ownership Interest Board Member<br />
W.L. Gore Other Advisory Committee<br />
Cook Consulting Fee Speaking/Teaching<br />
Morris E. Franklin Jr Covidien Honoraria Speaking/Teaching<br />
Stryker Other Advisory Committee<br />
Ethicon Honoraria Speaking/Teaching<br />
Synovis Other Consultant<br />
Ethicon Honoraria Speaking/Teaching<br />
Bariatric Times Honoraria Speaking/Teaching<br />
Michel Gagner<br />
Cine Med Inc. Honoraria Speaking/Teaching<br />
Gore Honoraria Speaking/Teaching<br />
Covidien Honoraria Speaking/Teaching<br />
Olympus Other Advisory Committee<br />
EndoMetabolic Solutions Ownership Interest Board Member<br />
Brice Gayet Olympus Consulting Fee Consultant<br />
Daniel P Geisler Covidien Consulting Fee Consulting<br />
Dpeartment of Surgery, Consulting Fee Consultant<br />
Alec Glover<br />
UMass-Memorial Medical Center/<br />
School<br />
Vysera Royalty Advisory Committee<br />
Christopher J. Gostout Softscope Medical Consulting Fee Consultant<br />
Apollo Endosurgery Royalty Advisory Committee<br />
Carroll M. Harmon Stryker Endoscopy Other Advisory Committee<br />
Karem C Harth<br />
Covidien Honorarium Consulting<br />
Lifecell Honorarium Consulting<br />
Stryker Endoscopy Other Other Research Grant<br />
Covidien Honoraria Speaking/Teaching<br />
Jeffrey W. Hazey<br />
Boston Scientific Other Other<br />
Fellowship funding<br />
support<br />
Ethicon Endosurgery Other Speaking/Teaching<br />
12 th World Congress of Endoscopic Surgery<br />
85 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
World Congress Faculty & Presenter Disclosures<br />
Name Commercial Interest What was received For what role Other<br />
MTF-Musculoskeletal Transplant<br />
Foundation<br />
Other Other Research Grant<br />
B. Todd Heniford WL Gore Other Other Research Grants<br />
Ethicon Endo Surgery Other Other Research Grant<br />
Ethicon, Inc. Other Speaking/Teaching<br />
Miguel Herrera<br />
Johnson & Johnson Medical Mexico Other Other Education grant<br />
Enteromedics Inc Other Other Research grant<br />
Covidien Other Other Educational grant<br />
Daniel M. Herron Gore Consulting Fee Consultant<br />
Hourglass Technology Consulting Fee Advisory Committee<br />
Kelvin D. Higa Surgiquest Other Advisory Committee<br />
Jacques M. Himpens<br />
Ethicon Consulting Fee Speaking/Teaching<br />
Covidien Consulting Fee Speaking/Teaching<br />
Michael D. Holzman UK Specialty Hospitals Consulting Fee Advisory Committee<br />
USGI Other Advisory Committee<br />
Stryker Other Consultant<br />
Olympus America Honoraria Consultant<br />
Santiago Horgan<br />
Novare Other Advisory Committee<br />
intuitive surgical Honoraria Speaking/Teaching<br />
Ethicon Endosurgery Honoraria Speaking/Teaching<br />
Ethicon<br />
Consulting Fee<br />
Valentx Other Advisory Committee<br />
Franziska Huettner Intuitive Honorarium Speaking and/or Teaching<br />
Boston Scientific Consulting Fee Consultant<br />
Eric Steven Hungness Olympus America Consulting Fee Consultant<br />
Terumo Consulting Fee Consultant<br />
Allergan Consulting Fee Consultant<br />
Sayeed Ikramuddin Covidien Consulting Fee Consultant<br />
Ethicon Endo-Surgery Honoraria Speaking/Teaching<br />
William Barry Inabnet<br />
III<br />
Covidien Other Other<br />
Covidien Honorarium Speaking and/or Teaching<br />
Brian P Jacob<br />
Ethicon Consulting Fee Consultant<br />
Covidien Honoraria Speaking/Teaching<br />
Ethicon EndoSurgery Consulting Fee Consulting<br />
Atrium Medical Consulting Fee Consulting<br />
Eric D Jenkins<br />
Muskuloskeletal Transplant<br />
Foundation<br />
Consulting Fee<br />
12 th World Congress of Endoscopic Surgery 86<br />
Consulting<br />
4th will be emailed to<br />
<strong>SAGES</strong> office<br />
Olympus Other Other research support<br />
Crospon Other Other research support<br />
Blair A. Jobe<br />
Sandhill Other Other research support<br />
Torax Medical Other Other research support<br />
Covidien Other Other Research<br />
Covidien<br />
Consulting Fee<br />
Access Surgical<br />
Royalty<br />
Daniel Bougere Jones<br />
Surgiquest<br />
Consulting Fee<br />
Cine-Med<br />
Royalty<br />
Ethicon<br />
Other<br />
Allergan<br />
Consulting Fee<br />
Rohan A Joseph<br />
Ethicon Endo Surgery Consulting Fee Consulting<br />
Ethicon Endo-Surgery Consulting Fee Consulting<br />
Ethicon Endosurgery Other Other<br />
Namir Katkhouda<br />
Ethicon Endosurgery Honoraria Consultant<br />
WL Gore Honoraria Speaking/Teaching<br />
Storz Consulting Fee Consultant<br />
L. Brian Katz Neat Stitch Ownership Interest Advisory Committee<br />
Chuck Kennedy Covidien Salary Employment
World Congress Faculty & Presenter Disclosures<br />
Name Commercial Interest What was received For what role Other<br />
Nicoleta O Kolozsvari Covidien Canada Other Financial Benefit Other Activities<br />
Unrestricted<br />
educational grant<br />
Covidien Consulting Fee Speaking/Teaching<br />
Shanu N. Kothari ValleyLab Consulting Fee Speaking/Teaching<br />
Lifecell Consulting Fee Consultant<br />
Marina Kurian<br />
Covidien Honoraria Speaking/Teaching<br />
Allergan Honoraria Speaking/Teaching<br />
Axiomed Spine Corp Royalty Consultant<br />
Isador Lieberman<br />
Mazor Surgical Royalty Consultant<br />
Merlot OrthopediX Royalty Board Member<br />
Stryker Spine Royalty Consultant<br />
Thom E. Lobe<br />
Visual Medical Solutions Ownership Interest Other Partner<br />
Neatstich Ownership Interest Board Member<br />
Katie Love Covidien Consulting Fee Consulting<br />
Kirk Allen Ludwig Applied Medical Honoraria Speaking/Teaching<br />
Stryker, Covidien, Axcan<br />
Speaking/Teaching<br />
Accuray Other Other<br />
Research Grant/Principal<br />
Invesitgator<br />
Intuitive Surgical, Boston Other Other Stock<br />
James D. Luketich<br />
Scientific, Covidien,<br />
Options/Recipient<br />
Stryker, Axcan,<br />
Covidien, Stryker and Other Other Research<br />
Oncotech<br />
Grant/Principal Investigator<br />
Covidien Other Other<br />
Minimally Invasive<br />
Surgery program<br />
Joseph Mamazza<br />
support<br />
Minimally Invasive<br />
Storz Other Other<br />
Surgery program<br />
support<br />
Ethicon Honoraria Consultant<br />
Covidien Consulting Fee Consultant<br />
Jeffrey M. Marks Olympus Consulting Fee Consultant<br />
WL Gore Consulting Fee Consultant<br />
Apollo Endusurgery Consulting Fee Advisory Committee<br />
SurgiQuest Honoraria Advisory Committee<br />
Wolf Consulting Fee Consultant<br />
Stryker Consulting Fee Consultant<br />
John H. Marks<br />
Glaxo Smith Kline Consulting Fee Consultant<br />
Covidien Honoraria Speaking/Teaching<br />
Covidien Consulting Fee Consultant<br />
Zassi Consulting Fee Consultant<br />
Pamela Martin Ethicon Endo-Surgery Salary Employment<br />
Transenterix Other Advisory Committee<br />
Ethicon Inc<br />
Other<br />
Boston Scientific Honoraria Speaking/Teaching<br />
Jose M. Martinez Lifecell Honoraria Speaking/Teaching<br />
Olympus Honoraria Speaking/Teaching<br />
Transenterix Consulting Fee Advisory Committee<br />
Covidien Other Speaking/Teaching<br />
Samer G. Mattar<br />
Ethicon Honoraria Speaking/Teaching<br />
Covidien Honoraria Speaking/Teaching<br />
Kai Matthes<br />
EndoSim, LLC Ownership Interest Management Position<br />
Olympus America Inc. Other Other equipment support<br />
WL Gore Honoraria Speaking/Teaching<br />
Atrium Medical Consulting Fee Consultant<br />
Brent D. Matthews Musculoskeletal Transplantation<br />
Foundation<br />
Consulting Fee<br />
Consultant<br />
Ethicon Endosurgery Other Speaking/Teaching<br />
12 th World Congress of Endoscopic Surgery<br />
87 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
World Congress Faculty & Presenter Disclosures<br />
Name Commercial Interest What was received For what role Other<br />
John D. Mellinger Gore Honoraria Speaking/Teaching<br />
Endogastric Solutions Other Advisory Committee<br />
Transenterix Other Advisory Committee<br />
Surgiquest Other Advisory Committee<br />
W. Scott Melvin<br />
Covidien Other Other<br />
research and training<br />
grants<br />
W L Gore Other Other research funding<br />
Stryker Consulting Fee Consultant<br />
Endogastric Solutions Honoraria Speaking/Teaching<br />
Dean J. Mikami Gore Consulting Fee Consultant<br />
Covidien Honoraria Speaking/Teaching<br />
EasyLap Consulting Fee Advisory Committee<br />
Yoav Mintz<br />
Virtual Ports Other Advisory Committee<br />
Lumenis Consulting Fee Consultant<br />
Ethicon Endosurgery Israel Honoraria Speaking/Teaching<br />
John R.T. Monson Covidien Honoraria Speaking/Teaching<br />
Kenric M. Murayama Covidien Honoraria Speaking/Teaching<br />
Stryker<br />
Honorarium<br />
Membership on Advisory<br />
Committees or Review Panels<br />
Radu Nedelcoviciu Covidien Honorarium Speaking and/or Teaching<br />
Adolor Honorarium Speaking and/or Teaching Surgiquest, Wolfe,<br />
Olympus<br />
Ninh Tuan Nguyen<br />
Surgiquest Other Consultant<br />
Covidien Honoraria Speaking/Teaching<br />
LifeCell Consulting Fee Speaking/Teaching<br />
Yuri W. Novitsky<br />
Nerites Consulting Fee Review Panel<br />
Davol, Inc Consulting Fee Consultant<br />
Covidien Consulting Fee Speaking/Teaching<br />
Cook Surgical Other Speaking/Teaching<br />
W.L. Gore Other Other Educational grants<br />
Torax Medical Other Other Research grant<br />
Brant K. Oelschlager<br />
Sandhill Scientific Other Other Educational grant<br />
Educational grants,<br />
Covidien Other Other<br />
research grants,<br />
honorarium<br />
Allan E. Okrainec Ethicon Honoraria Speaking/Teaching<br />
Gore Other Other Research Grant<br />
life cell Honoraria Speaking/Teaching<br />
Dmitry Oleynikov Virtual Incision corp Ownership Interest Board Member<br />
Covidien Honoraria Speaking/Teaching<br />
Virtual Incision Corporation Ownership Interest Board Membership<br />
Ethicon<br />
Licensing agreement,<br />
research grants<br />
Sarah C Oltmann<br />
Allergan<br />
Speaking and/or Teaching<br />
Covidien Speaking and/or Teaching Research Grants<br />
Raymond P. Onders<br />
Covidian Consulting Fee Consultant<br />
Synapse Biomedical Ownership Interest Board Member<br />
Neely Panton<br />
Ethicon EndoSurgical Consulting Fee Advisory Committee<br />
Ethicon EndoSurgical Consulting Fee Consultant<br />
WL Gore Honoraria Consultant<br />
Adrian E. Park<br />
Surgiquest Honoraria Advisory Committee<br />
Stryker Endoscopy Honoraria Advisory Committee<br />
Apollo Endosurgery Other Advisory Committee<br />
12 th World Congress of Endoscopic Surgery 88
World Congress Faculty & Presenter Disclosures<br />
Name Commercial Interest What was received For what role Other<br />
Cook Other Other<br />
Received: Grant<br />
Role: PI<br />
Covidien (Spouse) Salary Employment<br />
Carlos A. Pellegrini<br />
METI Other Other<br />
Received:Grant<br />
Role:PI<br />
Stryker Other Other<br />
Received: Grant<br />
Role:PI<br />
MediGus Inc Other Other Grant Support<br />
Jeffrey H. Peters<br />
Ethicon Endosurgery Honoraria Advisory Committee<br />
Torax Inc Other Other Grant Support<br />
EndoVx Inc. Ownership Interest Consultant<br />
Covidien Honoraria Speaking/Teaching<br />
Alfons Pomp<br />
Ethicon Endosurgery Honoraria Speaking/Teaching<br />
W.L. Gore and Associates Honoraria Speaking/Teaching<br />
Jeffrey L. Ponsky US Endoscopy Consulting Fee Consultant<br />
Barosense Ownership Interest Advisory Committee<br />
Immersion Consulting Fee Consultant<br />
Aurora Dawn Pryor Synecor Consulting Fee Consultant<br />
TransEnterix Ownership Interest Advisory Committee<br />
Covidien Honoraria Speaking/Teaching<br />
Sonia L. Ramamoorthy Applied MEdical Honoraria Speaking/Teaching<br />
LifeCell Honoraria Speaking/Teaching<br />
MTF Consulting Fee Advisory Committee<br />
Bruce J. Ramshaw<br />
Atrium Other Other Research support<br />
Ethicon Honoraria Speaking/Teaching<br />
WL Gore Honoraria Speaking/Teaching<br />
Covidien Honoraria Speaking/Teaching<br />
David W. Rattner<br />
TransEnterix Honoraria Advisory Committee<br />
Olmpus Honoraria Speaking/Teaching<br />
Covidien Consulting Fee Speaking and/or Teaching Education Grant<br />
Arthur Rawlings<br />
Support<br />
Stryker Endoscopy Consulting Fee Speaking and/or Teaching Grant Support<br />
Ethicon Endosurgery Consulting Fee Speaking and/or Teaching Education Grant Support<br />
Gore Honoraria Speaking/Teaching<br />
Kevin M. Reavis Endogastric Solutions Honoraria Speaking/Teaching<br />
Covidien Honoraria Speaking/Teaching<br />
William O. Richards Covidien Honoraria Advisory Committee<br />
Covidien Other Other<br />
Unrestricted Educational<br />
Grants and Equipment<br />
via Henry M. Jackson<br />
Foundation<br />
ConMed Linvatec Other Other<br />
Video Imaging<br />
equipment for skills<br />
E. Matt Ritter<br />
training lab<br />
Ethicon Endosurgery Other Other<br />
Unrestricted Educational<br />
Grants and Equipment<br />
via Henry M. Jackson<br />
Foundation<br />
Henry M. Jackson Foundation Other Other<br />
Unrestricted Educational<br />
Grants<br />
Michael J. Rosen<br />
Lifecell Consulting Fee Consultant<br />
Covidien Consulting Fee Consultant<br />
Sinovys Consulting Fee Speaking/Teaching<br />
Karl Storz Endoscopy Consulting Fee Consultant<br />
Karl Storz Consulting Fee Speaking/Teaching<br />
Raul J. Rosenthal<br />
Ethicon Endosurgery Consulting Fee Consultant<br />
Ethicon Consulting Fee Speaking/Teaching<br />
Covidien Consulting Fee Speaking/Teaching<br />
Covidien Consulting Fee Consultant<br />
Synovis Consulting Fee Consultant<br />
89 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
World Congress Faculty & Presenter Disclosures<br />
Name Commercial Interest What was received For what role Other<br />
Steven S Rothenberg Storz Consulting Fee Consulting<br />
Francesco Rubino<br />
Covidien Consulting Fee Consultant<br />
Ethicon Honoraria Speaking/Teaching<br />
GI Dynamic Consulting Fee Consultant<br />
NGM Biotech Consulting Fee Advisory Committee<br />
Yoshihisa Saida Boston JAPAN Consulting Fee Consulting<br />
Barry A Salky<br />
NeatStitch, LTD<br />
Ownership Interest<br />
Membership on Advisory<br />
Committees or Review Panels,<br />
Board Member<br />
Cleanoscope, LTD Shares in Company Advisory Board<br />
Bryan J Sandler ValenTx Consulting Fee Consulting<br />
Ethicon Endosurgery Other Financial Benefit Speaking and/or Teaching Research funding for lab<br />
Ethicon Endosurgery Other Financial Benefit Contracted Research Research funding for lab<br />
Byron F Santos Covidien Honorarium Speaking and/or Teaching<br />
Karl Storz Other Financial Benefit Contracted Research Equipmnt for research<br />
Karl Storz Other Financial Benefit Contracted Research Received Equipment<br />
Richard M. Satava<br />
InTouch Technologies Ownership Interest Other own stock in company<br />
Karl Storz Consulting Fee Consultant<br />
SurgiQuest Ownership Interest Advisory Committee<br />
Ethicon Endosurgery Consulting Fee Advisory Committee<br />
Gore Consulting Fee Consultant<br />
Philip R. Schauer Covidien Honoraria Speaking/Teaching<br />
Barosense Ownership Interest Advisory Committee<br />
Bard-Davol Other Other Research Funding<br />
Stryker Consulting Fee Advisory Committee<br />
Christopher M.<br />
Schlachta<br />
Steven D.<br />
Schwaitzberg<br />
Daniel J. Scott<br />
Niazy M. Selim<br />
Don J. Selzer<br />
Nilay R Shah<br />
Johnson and Johnson Medical<br />
Products<br />
Consulting Fee<br />
Advisory Committee<br />
Ethicon Endosurgery Honoraria Speaking/Teaching<br />
Surgiquest Ownership Interest Advisory Committee<br />
Stryker Honoraria Advisory Committee<br />
Endocore Consulting Fee Independent Contractor<br />
MITI Ownership Interest Advisory Committee<br />
Cambridge Endo Ownership Interest Advisory Committee<br />
Neatstitch Ownership Interest Advisory Committee<br />
MMDI Consulting Fee Consultant<br />
Olympus Consulting Fee Consultant<br />
Accelerrated Technologies, Inc. Consulting Fee Consultant<br />
Covidien Other Other<br />
Sponsored research,<br />
advisory panel, teaching<br />
Ethicon Other Other sponsored research<br />
Magnetically Anchored Instruments IP Rights Other Co-inventor<br />
NeatStitch Consulting Fee Consultant<br />
Storz Other Other Equipment Grant<br />
Luxor Software Services, LLC Ownership Interest Other Owner<br />
Intuitive Surgical Honoraria Speaking/Teaching<br />
Cambridge Endo Ownership Interest Advisory Committee<br />
Cook Biotech, Inc. Salary Advisory Committee<br />
Covidien Other Other Educational Grant<br />
Elemental Healthcare /Cambridge<br />
Endo<br />
Honoraria<br />
Speaking/Teaching<br />
Ethicon Endosurgery Other Other Educational grant<br />
MMDI Other Financial Benefit Contracted Research<br />
Covidien Other Financial Benefit Contracted Research<br />
BarrX Other Financial Benefit Contracted Research<br />
12 th World Congress of Endoscopic Surgery 90
World Congress Faculty & Presenter Disclosures<br />
Name Commercial Interest What was received For what role Other<br />
Suturtek Ownership Interest Consultant<br />
transenterix Ownership Interest Consultant<br />
Paresh C. Shah Ventralfix Ownership Interest Management Position<br />
Covidien Consulting Fee Consultant<br />
Ethicon Consulting Fee Consultant<br />
David E Skarda<br />
Covidien Consulting Fee Speaking and/or Teaching<br />
Ethicon Consulting Fee Speaking and/or Teaching<br />
Olympus Honoraria Speaking/Teaching<br />
Toyooki Sonoda Applied Medical Honoraria Speaking/Teaching<br />
Tyco Honoraria Speaking/Teaching<br />
Terumo Honoraria Advisory Committee<br />
Nathaniel J. Soper<br />
TransEnterix Consulting Fee Advisory Committee<br />
Karl Storz Other Other<br />
equipment used for<br />
education and research<br />
Greg V. Stiegmann Valley Lab Honoraria Speaking/Teaching<br />
Lee L. Swanstrom<br />
Boston Scientific<br />
Other<br />
Ethicon Other Other education grants<br />
Patricia Sylla Covidien Consulting Fee Consultant<br />
Zoltan Szabo Karl Storz Endoscopy Royalty<br />
Surgica Structure<br />
Ownership Interest<br />
MST<br />
Consulting Fee<br />
Amir Szold<br />
Nicast<br />
Consulting Fee<br />
Niti Medical<br />
Consulting Fee<br />
Visionsense<br />
Other<br />
Virtual Ports<br />
IP Rights<br />
Apollo Endosurgery Other Consultant<br />
Mark A. Talamini<br />
Covidien Other Advisory Committee<br />
Max Endoscopy Other Advisory Committee<br />
Sanofi-Aventis Other Consultant<br />
Novare Consulting Fee Consultant<br />
Julio A. Teixeira<br />
Covidien Honoraria Speaking/Teaching<br />
Allergan Inc. Honoraria Advisory Committee<br />
Ethicon Endosurgery Consulting Fee Consultant<br />
USGI Medical Consulting Fee Consultant<br />
USGI Medical Honoraria Advisory Committee<br />
Power Medical Honoraria Advisory Committee<br />
Covidien Honoraria Advisory Committee<br />
Covidien Consulting Fee Consultant<br />
Boston Scientific Consulting Fee Consultant<br />
Christopher C.<br />
Thompson<br />
Bard Royalty Other Licensing Agreement<br />
Bard Other Other<br />
Grants for research<br />
support<br />
Bard Honoraria Consultant<br />
Bard Honoraria Advisory Committee<br />
Bard Consulting Fee Consultant<br />
Valentx Consulting Fee Consultant<br />
Jonathan R Thompson Ethicon Endosurgery Consulting Fee Consulting<br />
Allergan Other Financial Benefit Speaking and/or Teaching<br />
Kari Thompson Olympus Honorarium Consulting<br />
Ethicon Other Financial Benefit Speaking and/or Teaching<br />
Philippe A Topart<br />
ETHICON Honorarium Speaking and/or Teaching<br />
GORE Other Financial Benefit Other Activities<br />
Alfonso Torquati<br />
Duke<br />
Covidien Consulting Fee Advisory Committee<br />
12 th World Congress of Endoscopic Surgery<br />
91 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
World Congress Faculty & Presenter Disclosures<br />
Name Commercial Interest What was received For what role Other<br />
Tung T Tran Covidien Other Financial Benefit Other Activities<br />
Unrestricted educational<br />
grant<br />
Thadeus L. Trus<br />
Ethicon Endosurgery Other Other<br />
Boston Scientific Consulting Fee Consultant<br />
Shawn T. Tsuda<br />
Covidien Honoraria Speaking/Teaching<br />
Ethicon Honoraria Speaking/Teaching<br />
Surendra M. Ugale Ethicon Endosurgery Other Speaking/Teaching<br />
Anthony J. Vine Ethicon Endosurgery Consulting Fee Speaking/Teaching<br />
W.L. Gore Consulting Fee Consultant<br />
Guy R. Voeller<br />
Atrium Consulting Fee Consultant<br />
Covidien Honoraria Speaking/Teaching<br />
Davol Honoraria Speaking/Teaching<br />
Century Medical Incorporated Consulting Fee Consultant<br />
Signalomics Gmbh Consulting Fee Consultant<br />
Power Medical Interventions IP Rights Other inventor<br />
Niti Consulting Fee Consultant<br />
Neatstitch Ownership Interest Board Member<br />
Neatstitch Consulting Fee Consultant<br />
Medtronics Consulting Fee Consultant<br />
Karl Storz Endoscopy America IP Rights Other inventor<br />
Karl Storz Endoscopy America Consulting Fee Consultant<br />
Intuitive Surgical Ownership Interest Consultant<br />
Steven D. Wexner<br />
Renew Medical Consulting Fee Consultant<br />
Incontinence Devices Inc Consulting Fee Consultant<br />
EZ Surgical Ownership Interest Consultant<br />
EZ Surgical Consulting Fee Consultant<br />
Ethicon Inc Consulting Fee Consultant<br />
Unique Surgical Innovations Ownership Interest Management Position<br />
Covidien IP Rights Other inventor<br />
Advanced Surgical Innovations Ownership Interest Management Position<br />
Adolor/Glaxo Smith Kline Honoraria Speaking/Teaching<br />
SurgRX Consulting Fee Consultant<br />
SurgRX Ownership Interest Consultant<br />
Cr Bard Consulting Fee Consultant<br />
Bristol Meyers Squibb Other Other PI on Phase 1 Drug trial<br />
Olympus Corporation Honoraria Speaking/Teaching<br />
R. Larry Whelan Applied Medical Other Other multi-center study<br />
PolyE Pharma Corporation Other Other<br />
Murine and human study<br />
testing drug<br />
Sanofi Aventis Honoraria Speaking/Teaching<br />
Mark H. Whiteford Richard Wolf Medical Instruments Consulting Fee Consultant<br />
Applied Medical Honoraria Speaking/Teaching<br />
Natan Zundel<br />
Ethicon Endosurgery Honoraria Consultant<br />
Cinemed Honoraria Speaking/Teaching<br />
12 th World Congress of Endoscopic Surgery 92
Notes<br />
12 th World Congress of Endoscopic Surgery<br />
93 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
World Congress Social <strong>Program</strong>s<br />
Welcome Reception<br />
Date: Wednesday evening, April 14, <strong>2010</strong><br />
Time:<br />
Place:<br />
Fee:<br />
Dress:<br />
5:00 - 7:00 PM<br />
Prince George’s Exhibit Hall A-C<br />
No Fee for Registrants & registered guests.<br />
Ticketed Event.<br />
Business casual<br />
Special promotions, presentations and entertainment.<br />
Great food! Open bar!<br />
Note: Children under the age of 14 will not be permitted in the Exhibit Hall due to safety considerations.<br />
<strong>SAGES</strong> Meet the Leadership Reception<br />
for New <strong>SAGES</strong> Members<br />
Residents and Fellows<br />
Date: Friday Evening, April 16, <strong>2010</strong><br />
Time:<br />
Place:<br />
Dress:<br />
6:00 - 7:00 PM<br />
Gaylord Hotel, Pose 18 th -19 th floor<br />
Casual<br />
“All The News” World Congress Gala<br />
An Evening at “The Newseum”<br />
Dinner and Sing-Off<br />
Date: Saturday Evening, April 17, <strong>2010</strong><br />
Place:<br />
Time:<br />
Dress:<br />
Fee:<br />
Tickets:<br />
“The Newseum” Pennsylvania Ave & Sixth St. NW, Washington<br />
7:30 - 11:30 PM<br />
Business Casual<br />
Included in Registration for <strong>SAGES</strong> SuperPass (Option A), & registered guests.<br />
$140.00 (for additional guests and <strong>SAGES</strong> Registration Options B & C) available at Registration desk until Friday 5:00 PM<br />
Join us for an international evening at “The Newseum” – a museum of news that blends five centuries of news history with up-to-the-second<br />
technology and hands-on exhibits. As you enter you’ll see a 74-foot-high marble engraving of the First Amendment. With seven levels of<br />
galleries and theaters, The Newseum is a unique environment where we go behind the scenes to experience how and why news is made.<br />
Fabulous food by world renowned caterer Wolfgang Puck and plenty of bars.<br />
The evening will conclude with the World Congress International Sing-Off.<br />
12 th World Congress of Endoscopic Surgery 94
World Congress Tours<br />
Tour 1: Wonders of Washington<br />
Date: Thursday, April 15, <strong>2010</strong><br />
Time: Depart 9:00 AM – 4 1/2 hours<br />
Buses load beginning at 8:45 AM<br />
Fee:<br />
$50.00 per person<br />
Includes: Deluxe Climate-Controlled<br />
Motor coach D.C. Licensed,<br />
Uniformed Tour Guide, All<br />
Admissions and Appointments<br />
Washington, DC, is one of only three planned<br />
federal capitals. George Washington chose<br />
this site in 1790, and selected Pierre Charles<br />
L’Enfant to design the city as the capital for the<br />
new United States.<br />
One of the city’s finest tour guides will<br />
introduce you to the history, architecture<br />
and grandeur of Washington, DC. Engaging<br />
stories, little known facts, and trivia will be told<br />
as you explore the monuments, memorials<br />
and notable buildings. Drive by the The<br />
“Church of the Presidents”, the White House,<br />
Smithsonian Institution Complex and the<br />
Washington Monument. See the Capitol<br />
Dome and travel the inaugural parade<br />
route and see the FBI Building. Then stop at<br />
one of the most visited areas of the city, the<br />
National Park that boasts as its centerpieces<br />
the Lincoln, Vietnam War and Korean War<br />
Veterans Memorials. See the National World<br />
War II Memorial and walk where Martin Luther<br />
King gave his “I Have a Dream” speech. Enjoy a<br />
short ride along the Tidal Basin to the Jefferson<br />
and Franklin Delano Roosevelt Memorials.<br />
Tour 2: Where Fabulous Lives –<br />
Hillwood Museum and Gardens<br />
Date: Friday, April 16, <strong>2010</strong><br />
Time: Depart 9:00 AM – 5 hours<br />
Buses load beginning at 8:45 AM<br />
Fee:<br />
$105.00 per person<br />
Includes: Deluxe Climate-Controlled<br />
Motor coach, D.C. Licensed,<br />
Uniformed Tour Guide, Tour of<br />
Estate, All Admissions, Elegant<br />
lunch at Hillwood<br />
Travel to the former home of Marjorie<br />
Merriweather Post to experience the opulent<br />
lifestyle and aristocratic luxury of her 25-acre<br />
estate, known as Hillwood. Mrs. Post was the<br />
heiress of the Post cereal fortune and mother<br />
of famous actress Dina Merrill. She furnished<br />
her 40-room Georgian-Style Mansion with a<br />
collection of 18th and 19th century Russian<br />
and French decorative art, including Fabergé<br />
eggs, Russian Imperial icons, rare tapestries<br />
and priceless objects d’art. See period pieces<br />
from the reign of Catherine the Great and<br />
the nuptial crown worn by Empress Alexandra<br />
at her wedding to Nicolas II in 1894. A stroll<br />
through the lavish gardens and greenhouse will<br />
charm you. A Russian dacha (summer house)<br />
and Greenhouse shelters a stunning display<br />
of 5000 orchids. You will enjoy lunch in the<br />
beautiful café on the grounds of the estate.<br />
Tour 3: Washington’s<br />
Great Private Museums –<br />
The Kreeger and the Phillips<br />
Date: Saturday, April 17, <strong>2010</strong><br />
Time: Depart 9:30 AM – 6 hours<br />
Buses load beginning at 9:15 AM<br />
Fee:<br />
$95.00 per person<br />
Includes: Deluxe Climate-Controlled<br />
Motor coach, D.C. Licensed,<br />
Uniformed Tour Guide, Tours of<br />
Both Museums, All Admissions,<br />
(Lunch on your own)<br />
Begin with a docent-led tour of the Kreeger<br />
Museum. Renowned architect Philip Johnson,<br />
famous for such masterpieces as the pre-<br />
Columbian gallery at Dumbarton Oaks in<br />
Georgetown and the Lincoln Center in New<br />
York, designed this magnificent home for David<br />
Kreeger, the insurance magnate. Completed<br />
in 1967 the Kreeger is a Showcase for<br />
its collection of 19th- and 20th-century<br />
Masters, with more than 180 works by Picasso,<br />
Monet, Miro, Rodin and Kandinsky, as well<br />
as other contemporary artists. The 66-foot<br />
great hall was designed for chamber music<br />
ensembles where artists such as Isaac Stern<br />
have performed. The Phillips Collection was<br />
the first permanent museum of Modern art<br />
in the U.S. and served as the home of Duncan<br />
Phillips. This Georgian Revival Style Mansion<br />
boasts as the centerpiece of its collection,<br />
Renoir’s “Luncheon of the Boating Party”.<br />
This outstanding collection concentrates on<br />
French Impressionist, Post Impressionist and<br />
American Modernist paintings.<br />
12 th World Congress of Endoscopic Surgery<br />
Tour tickets<br />
may be<br />
purchased at<br />
Registration<br />
desk until tours<br />
are sold out<br />
FYI! Getting Around National Harbor:<br />
Water Taxi Service<br />
In addition to cabs and rental cars, the National Harbor offers a<br />
fun and practical way to get to various destinations…a water taxi!<br />
Water taxi service is available to and from points around Washington<br />
D.C., Virginia and Maryland for your convenience. The Potomac<br />
Riverboat Company operates water taxi service between National<br />
Harbor and Old Town Alexandria, with additional boat service to Mount<br />
Vernon and Georgetown. Water taxis will run every half hour between<br />
National Harbor and Old Town Alexandria. There will be three daily<br />
trips to Georgetown’s Washington Harbor, and a single daily trip to<br />
George Washington’s Mount Vernon Estate. Ask the concierge for more<br />
information.<br />
95 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Notes<br />
12 th World Congress of Endoscopic Surgery 96
Scientific Session Oral Abstracts<br />
S001<br />
MOST RECENT NATIONAL SURGICAL QUALITY IMPROVEMENT<br />
PROJECT DATA (NSQIP), COMPARISON OF LAPAROSCOPIC VS. OPEN<br />
COLON RESECTIONS Dan Ruiz, MD, Alexander Kraev, MD, Steven Nurkin,<br />
MD, Darshak Shah, MD, James W Turner, MD, Howard Tiszenkel, MD New<br />
York Hospital Queens<br />
BACKGROUND. The ACS National Surgical Quality Improvement <strong>Program</strong><br />
(ACS NSQIP) is the first nationally validated, risk-adjusted, outcomesbased<br />
program to measure and improve the quality of surgical care. The<br />
program employs a prospective, peer controlled, validated database<br />
to quantify 30-day risk-adjusted surgical outcomes, which allows valid<br />
comparison of outcomes among all hospitals in the program. The most<br />
recent 2008 National Surgical Quality Improvement Project (NSQIP)<br />
database, contains over 240,000 surgical cases.<br />
METHODS. The 2008 NSQIP database was queried for all patients<br />
undergoing colon resection. Patients were divided into laparoscopic and<br />
open groups based on CPT procedure codes. Difference in 30-day survival<br />
between subgroups was evaluated using Kaplan-Meier and logistic<br />
regression analysis. Pre-operative morbidity was compared using the<br />
unpaired t-test.<br />
RESULTS. There were 17224 patients who underwent colon resection in<br />
2008. Patients who underwent laparoscopic operation had a significantly<br />
better survival at thirty days over open (98.8% vs 94.7%, logrank p-value<br />
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
procedural tasks one time with haptics engaged at the default setting.<br />
The haptics trained group was sequentially trained to proficiency in the<br />
basic tasks and then performed each of the procedural tasks one time<br />
with haptics engaged. The non-haptics group used the same training<br />
protocol except haptics was disengaged. Proficiency was to previously<br />
published expert values. Each group was assessed in the performance<br />
of ten laparoscopic cholecystectomies (alternating with and without<br />
haptics). Performance was measured via automatically collected simulator<br />
data. Unpaired student t-test was used to compare the groups. A p value<br />
Scientific Session Oral Abstracts<br />
3 months after surgery. The mean follow up is 26 months. The series<br />
shows that mere size should not be considered as a contraindication<br />
to laparoscopic approach in large adrenal masses. Graded approach to<br />
LA1, adherence to strict anatomical principles, minimum handling of<br />
the tumor and dissection of the body away from the tumor is the key<br />
to success. We suggest that large adrenal masses should be tackled by<br />
experienced laparoscopic surgeons.<br />
1. Laparoscopic adrenalectomy:Gaining experience by graded approach.<br />
Dalvi A, Thapar P et al. J Minimal Access Surgery 2006;2:59-66<br />
S006<br />
COMPARISON OF OPEN LIVE DONOR NEPHRECTOMY, LAPAROSCOPIC<br />
LIVE DONOR NEPHRECTOMY, AND HAND-ASSISTED LIVE DONOR<br />
NEPHRECTOMY: A COST-EFFECTIVENESS ANALYSIS Derek E Moore, MD<br />
MPH, Matthew Landman, MD, Deonna Moore, MSN, Irene Feurer, PhD, C W<br />
Pinson, MD MBA Vanderbilt University Medical Center<br />
INTRODUCTION: Live donor kidney transplantation is the treatment of<br />
choice for end-stage renal failure. Open Donor Nephrectomy (ODN) was<br />
the standard until the introduction of Laparoscopic Donor Nephrectomy<br />
(LDN) in 1995. Hand-Assisted Laparoscopic Donor Nephrectomy<br />
(HALDN) was added shortly thereafter. While decreasing post-operative<br />
analgesic requirements and speeding return to normal activity, the<br />
laparoscopic techniques are associated with longer operative times and a<br />
minor increase in peri-operative complications. The aim of this study is to<br />
evaluate the cost-effectiveness of the different techniques.<br />
METHODS: A decision analytic model was created to simulate outcomes<br />
for donors undergoing ODN, LDN, and HALDN. Baseline values and<br />
ranges were determined from the SRTR database and a literature<br />
review. Sensitivity analyses were conducted to test model strength and<br />
parameter variability.<br />
RESULTS: Donors undergoing LDN and HALDN accrued less cost and had<br />
a superior quality of life when all factors were considered in this model.<br />
HALDN costs are lower $13,000 vs LDN $15,000 and ODN $17,000. HALDN<br />
was the dominant scenario in all models.<br />
CONCLUSIONS: By requiring less post-operative analgisia, returning<br />
to normal activity faster, and having a more favorable peri-operative<br />
complication rate; the HALDN was the more cost-effective procedure for<br />
live donor nephrectomy.<br />
S007<br />
MULTICENTER COMPARISON OF INTERMEDIATE ONCOLOGIC<br />
OUTCOMES OF LAPAROSCOPIC PARTIAL NEPHRECTOMY AND RENAL<br />
CRYOABLATION Sean Stroup, MD, John Malcolm, MD, James L’Esperance,<br />
MD, Robert Wake, MD, Michael Fabrizio, MD, Ithaar H Derweesh, MD<br />
University of California San Diego, University of Tennessee at Memphis<br />
Health Science Center, Eastern Virginia Medical School<br />
Introduction: The surgical paradigm for small renal masses has evolved<br />
towards less invasive nephron sparing intervention. While partial<br />
nephrectomy remains the gold standard for the management of most<br />
small renal masses, increasing experience with renal cryoablation has<br />
suggested a viable alternative with a favorable morbidity profile and good<br />
efficacy. We compare intermediate-term oncologic outcomes following<br />
laparoscopic partial nephrectomy (LPN) and renal cryoablation (RC) from<br />
a multi-center experience.<br />
Methods: We performed a retrospective review of our LPN and RC<br />
experience between 9/1998 and 3/2008. Patients with at least 6 months<br />
follow-up were included in the analysis. LPN was performed via a<br />
transperitoneal approach. RC was performed via a percutaneous or<br />
transperitoneal laparoscopic approach. Follow-up consisted of imaging<br />
and laboratory studies at regular intervals. Persistent mass enhancement<br />
or interval tumor growth was considered a treatment failure following<br />
RC, and repeat biopsy and retreatment were recommended. Residual<br />
enhancing tumor was evidence of treatment failure following LPN.<br />
Results: 119 patients (60%male, 39%black, mean BMI: 29.3) underwent<br />
RC with a mean follow-up of 29.5 months (range: 7-120). 123 patients<br />
(41%male, 34%black, mean BMI: 27.5) underwent LPN with a mean followup<br />
of 23.8 months (range: 7.7-74.6). Average patient age was 58 for LPN<br />
and 68 for RC (p
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
Conclusions: We have validated a novel wireless pulse oximeter capable<br />
of detecting intraoperative tissue hypoxia. A clinical trial in esophageal<br />
and gastric anastomotic surgery is planned in order to test the efficacy of<br />
the WiPOX in reducing anastomotic complications.<br />
S009<br />
A PILOT STUDY OF USING MULTIPHOTON MICROSCOPY TO DIAGNOSE<br />
GASTRIC CANCER Jun Yan, MD, Gang Chen, MD, Jianxin Chen, PhD,<br />
Shuangmu Zhuo, PhD, Hui Yu, MD, Mingang Ying, MD Fujian Provincial<br />
Tumor Hospital, Fuzhou, 350014, China<br />
Introduction: Using a combination of autofluorescence from cells<br />
and second harmonic generation signal from collagen, multiphoton<br />
microscopy (MPM) imaging can provide detailed information on<br />
tissue architecture and cellular morphology. The purpose of this<br />
study was to evaluate the feasibility of using MPM to diagnose gastric<br />
cancer, compared with gold standard hematoxylin-eosin (H-E) stained<br />
histopathology.<br />
Methods: A pilot study was performed between June 2009 and<br />
September 2009. 10 cases with gastric cancer confirmed by pre-op<br />
endoscopic biopsy underwent gastrectomy in Fujian Provincial Tumor<br />
Hospital. Each fresh specimen was opened by an attending pathologist.<br />
Cancer area and normal area in the specimen received examination<br />
under MPM in Key Laboratory of Optoelectronic Science and Technology<br />
for Medicine of Fujian University. After MPM examination, the same<br />
cancer area and the normal area in the specimen were received routing<br />
histopathological examination. MPM images and H-E stained images were<br />
compared by the same attending pathologist.<br />
Results: MPM images were acquired in two channels: broadband<br />
autofluorescence from cells, and second harmonic generation from tissue<br />
collagen. Cancer cells were identified in MPM images in the cancer area of<br />
10 specimens, which were confirmed by H-E stained slides. Normal area<br />
in 10 specimens didn’t have cancer cells in MPM images and H-E stained<br />
images.<br />
Conclusions: It is feasible to use Multiphoton microscopy to diagnose<br />
gastric cancer. With development and equipped into endoscopy,<br />
multiphoton microscopy maybe provide a real-time diagnosis without<br />
invasive biopsy for gastric cancer in the future.<br />
S010<br />
EFFICACY OF TURMERIC (CURCUMIN) IN PAIN AND POSTOPERATIVE<br />
FATIGUE AFTER LAPAROSCOPIC CHOLECYSTECTOMY - A DOUBLE<br />
BLIND, RANDOMIZED PLACEBO CONTROLLED STUDY Krishna A<br />
Agarwal, C D Tripathi, MD, Brij B Agarwal, MS VMMC & Safdarjung Hospital,<br />
Dr. Agarwal’s Surgery & Yoga and Sir Ganga Ram Hospital, New Delhi,<br />
India<br />
Objective of Study: Popularity of laparoscopic surgery owes largely<br />
to improved patient reported outcomes (PRO). Postoperative pain and<br />
fatigue are important indices of return to activity based quality of life<br />
PROs. Turmeric has been successfully used in India as a monotherapy<br />
for traumatic pain & fatigue. Curcumin, the active ingredient of turmeric<br />
has anti-inflammatory / anti-oxidant & tissue modulation / healing<br />
properties reported even at nanomolar levels without any toxicity & a<br />
wide therapeutic window. We studied the effect of curcumin on pain and<br />
postoperative fatigue in patients of Laparoscopic cholecystectomy (LC),<br />
an index Laparoscopic procedure.<br />
Methods and procedures: From July - September 2009 fifty unselected<br />
consecutive day care LC candidates were enrolled for this prospective,<br />
double blind randomized placebo (well matched & label blind) controlled<br />
study with ethics and informed consent protocol. Pregnant / lactating<br />
ladies, patient with psychosis/ neuropathic pain / alcohol or drug<br />
dependence / on self-administered analgesics /on regular analgesics or<br />
immunosuppressive or cytotoxic or steroid therapy were excluded.<br />
Any perioperative adverse event was the withdrawal criteria. A standard<br />
general anesthesia and perioperative analgesia protocol was followed for<br />
the LCs. No analgesic was prescribed at discharge except for either of the<br />
label blinded curcumin / placebo in 6 hourly dosage. Patients were asked<br />
to maintain pain / fatigue / any adverse event diaries based upon 100<br />
point visual analog scale (VAS) for pain and 10-point interval rating scale<br />
(IRS) for fatigue. Paracetamol 650 mg was the rescue analgesic. Patients<br />
were asked to record the number of tablets used during the 3 weeks.<br />
Patients were followed up on 3 rd day (D3), 1 st week (W1), 2 nd week (W2)<br />
and 3 rd week (W3) for prospective data. The random labels assigned were<br />
opened & entered for the corresponding patients only at the end of study<br />
for analysis.<br />
Results: The patients in the study (n=25) and the control group (n=25)<br />
were well matched for demographics, co-morbidity and gallbladder<br />
inflammation parameters. There was no withdrawal. All patients were pain<br />
free at W3 follow up. Analgesic tablet usage in 3 weeks was 7 (5-11) in the<br />
study group versus 39 (18-79) in the control group.<br />
12 th World Congress of Endoscopic Surgery 100
Scientific Session Oral Abstracts<br />
Table showing the mean (range) scores of post-operative pain & fatigue.<br />
Group Pain Scores Fatigue Scores<br />
D3 W1 W2 D3 W1 W2 W3<br />
Study 45(30-85) 15(10-25) 15(10-25) 6(4-10) 2(1-8) 1 0<br />
Control 40(35-80) 30(15-50) 32(18-56) 6(5-10) 5(4-9) 4(1-7) 1<br />
Conclusions: Turmeric (Curcumin) improves the postoperative pain &<br />
fatigue related PROs in patients of laparoscopic cholecystectomy. In view<br />
of encouraging results, benefits of a non-toxic common food ingredient<br />
i.e. turmeric (Curcumin) need to be studied in large, multi-centric, multiethnic<br />
studies.<br />
S011<br />
3-CCD (CHARGE COUPLED DEVICE) IMAGE ENHANCEMENT FOR<br />
BOWEL ISCHEMIA John C Graybill, MD, Nicole Crane, PhD, Susan M<br />
Gillern, MD, Eric A Elster, MD, Jonathan P Pearl, MD Naval Medical Research<br />
Center; National Naval Medical Center; Walter Reed Army Medical Center<br />
Introduction: Determination of bowel perfusion in cases of strangulating<br />
hernias, SMA occlusion, and other ischemic states is currently a subjective<br />
decision of surgeons. 3-CCD image enhancement allows objective and<br />
quantitative criteria to be included in a surgeon’s decision as to whether<br />
bowel resection is warranted secondary to ischemia. 3-CCD technology<br />
separates visible light into its three primary wavelength regions (red,<br />
green, and blue); by using an easily implemented mathematical<br />
algorithm, the amount of light detected by the red, green, and blue CCDs<br />
can be directly correlated with tissue oxygenation. We have previously<br />
demonstrated the utility of this approach in vessel identification, partial<br />
nephrectomy, donor nephrectomy, and now extend these studies to<br />
bowel ischemia.<br />
Materials and Methods: In a pilot study, two cases of ischemic bowel<br />
were analyzed using 3-CCD laparoscopic images and 3-CCD image<br />
enhancement. Ischemic bowel presented with lower values than healthy<br />
bowel. Watershed areas were then designated as either ischemic or<br />
well-perfused. To adjust for variations in brightness and clarity inherent<br />
to laparoscopic imaging, images were standardized such that fat always<br />
received a value of “1”. Fat is ubiquitous and well-perfused due to its<br />
numerous capillaries.<br />
Results: In this scenario, healthy bowel received a value of “0.727” while<br />
ischemic bowel received a value of “0.486,” with a p-value
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
medications. Post-operatively, mean leptin expression was decreased<br />
for all morbidly obese patients. However, this value was not significantly<br />
decreased (p=0.16). Post-operatively, mean resistin expression was<br />
unchanged for the entire cohort (p=0.36). However, resistin expression<br />
was significantly lower (p=0.05) after surgery in diabetic morbidly obese<br />
patients. Post-operative resistin expression in non-diabetic morbidly<br />
obese patients was not significantly different from pre-op values (p=0.32).<br />
Conclusions: This unique data shows that decreased gene expression<br />
of resistin and leptin may play a significant role in normalizing insulin<br />
resistance in morbidly obese patients following bariatric surgery. Also, this<br />
preliminary data suggests that modulation of resistin expression plays<br />
a role in diabetic obese patients and not necessarily in morbidly obese<br />
patients without T2D. Patient recruitment is ongoing to further elucidate<br />
these trends. Specific understanding of the pathways by which these<br />
adipocytokines contribute to both obesity and T2D could potentially lead<br />
to novel therapies for these conditions.<br />
S014<br />
COMMON BILE DUCT EXPLORATION IN DECLINE: MAJORITY OF<br />
THESE PROCEDURES ARE DONE IN NON-TEACHING HOSPITALS IN<br />
THE US. Samuel Jacob, MD, Marek Rudnicki, MD PhD Metropolitan Group<br />
Hospitals/University of Illinois Surgery Residency <strong>Program</strong> Chicago, USA<br />
BACKGROUND: Common bile duct (CBD) exploration used to be one<br />
of the relatively frequent procedures in armamentarium of the general<br />
surgeon. With raise of minimally invasive techniques one may expect<br />
diminished needs and fewer indications for that surgery.<br />
OBJECTIVE: The purpose of this study was to determine nationwide<br />
trends of cholecystectomy and common bile duct exploration over 10<br />
years period. In addition, this investigation was designed to evaluate<br />
utilization of these procedures in the teaching and non-teaching US<br />
Hospitals contributing to the National Inpatient Sample database.<br />
METHODS: The National Inpatient Sample from the Healthcare Cost and<br />
Utilization Project was analyzed for 1997-2007 nationwide trends for open<br />
and laparoscopic cholecystectomy using ICD-9 procedure codes 51.22,<br />
51.23 respectively, and exploration of CBD with and without CBD stone<br />
removal (51.41, 51.51). The data was subcategorized based on two main<br />
hospital characteristics: teaching or non-teaching hospitals. Analyzed<br />
data were weighted to provide national estimates. Statistical testing was<br />
performed using Z-test. The trends were studied using trendlines with<br />
R-square values as the coefficient of determination.<br />
RESULTS: Number of cholecystectomies did not change over the<br />
observed period and ranged from 442,260 in 1997 to 429,805 in<br />
2007 (R=0.0005). Open cholecystectomies declined from 138,116<br />
in 1997 to 86,582 in 2007 (p
Scientific Session Oral Abstracts<br />
S017<br />
INITIAL EXPERIENCES IN 70 CASES OF TOTALLY LAPAROSCOPIC LIVER<br />
RESECTION FOR HCC Nguyen Hoang Bac, PhD, Tran Cong Duy Long, MD,<br />
Nguyen Duc Thuan, MD, Le Tien Dat, MD Medical University Center at<br />
Hochiminh city<br />
Initial experiences in 70 cases of<br />
Totally Laparoscopic Liver resection for HCC<br />
Background: Laparoscopic surgery now is commonly applied for several<br />
kinds of different operations, but laparoscopic liver resection is still under<br />
survey. The objective of this study was to evaluate the feasibility and<br />
safety of this technique for HCC<br />
Patients and methods: Perspective and descriptive study. From Sep 2005<br />
to Feb 2008, we performed laparoscopic liver resections for 70 patients<br />
with HCC.The accompanied cirrhosis was in fifty two patients – 74% (51<br />
with Child A and 1 with Child B); mean tumor size 3.75 cm (2-10) and<br />
tumor locations were as follows:<br />
• 31 (44.3%) in left lateral segment,<br />
• 4 (5.7 %) in segment IVb,<br />
• 13 (18.6%) in segment V,<br />
• 12 (17.1%) in segment VI,<br />
• 2 (2.9%) in segment VII,<br />
• 1 (1.4%) in segment VIII<br />
• 3 (4.3%) in the posterior segments<br />
• 4 (5.7%) in segment V and VI<br />
Results: We performed 31 cases of one segmentectomy include:<br />
• 4 cases of segment II, 2 of segment III, 4 of segment IV, 8 of segment V,<br />
11 of segment VI, 1 of segment VII and 1 of segment VIII.<br />
There were 33 cases of bisegmentectomy include:<br />
• 24 (34.3%) cases of left lateral segmentectomies,<br />
• 3 (4.3%) posterior segmentectomy,<br />
• 6 (8.6%) V-VI bisegmentectomy.<br />
After Laparoscopic Diagnostic operation, three (4,3%) patients were<br />
not suitable for liver resection because of severe cirrhosis. One of them<br />
underwent RFA and 2 had TACE after operation.<br />
We had 3 (4.3%) patients converted to other procedures because<br />
of severe intraoperative bleeding. We converted to open operation<br />
after right hepatic vein was injured in one patient, or performed<br />
Minilaparotomy to control bleeding and continued to transect the<br />
parechymal laparoscopically in one, and converted to hand-assissted to<br />
define the tumor and divided the parechymal in the other.<br />
Mean operation time was 118 minutes (30-240).<br />
Mean Blood loss was 221 ml (0-1000ml) that required no blood<br />
transfusion.<br />
Hospital stay was 6.23 days (4-17 days).<br />
The Surgical margin less than 1cm was in 13 (18.5%) patients; from 1 to<br />
2cm was in 37 (61.5%) and more than 2cm in 14 (20%) patients. But we<br />
had only one positive surgical margin.<br />
There was no postoperative complication and no mortality.<br />
After 10-month follow-up (1–31 months) there are 3 recurrence cases and<br />
two of them can be reoperated (one open and 1 laparscopic operations).<br />
Conclusion: Laparoscopic liver resection is feasible and safe for selective<br />
patients with peripheral tumors located in the left lobe or in the segment<br />
IVb, V, VI, VII of the right liver.<br />
S018<br />
LAPAROSCOPIC MANAGEMENT OF CBD STONES: AN<br />
INDIAN EXPERIENCE Jagdish Chander, MD, Pawanindra Lal,<br />
MDDNBFRCSEdFRCSGlasg, Anubhav Vindal, MD, Vinod K Ramteke, MD<br />
Maulana Azad Medical College, New Delhi, India<br />
Introduction: India has a high incidence of gall stones and consequently<br />
of CBD stones (CBDS) which are very different from that seen in the west.<br />
It is not infrequent to see multiple, large, impacted stones in a hugely<br />
dilated CBD. Therefore many of these patients have been managed by<br />
open CBD exploration, even after advent of laparoscopic cholecystectomy<br />
(LC), since these large stones pose significant challenges for extraction by<br />
ERCP. This series presents the largest experience of managing CBDS using<br />
a laparoscopic approach from the Indian subcontinent.<br />
Material and Methods: Over the last 7 years, 150 patients of<br />
documented CBDS were treated laparoscopically in a single surgical unit<br />
at a tertiary care hospital in New Delhi. Of these 4 patients were managed<br />
through transcystic route and 140 through the trans-choledochal route.<br />
Of the latter, 29 patients were managed with a T-tube, 60 patients with<br />
an endobiliary stent, 31 patients had a primary closure of CBD, and 20<br />
had a choledochoduodenostomy. There were 6 conversions to open<br />
procedures.<br />
Results: There were 34 male and 116 female patients with age ranging<br />
from 15 to 72 years (mean of 46.9±12.4 years). The mean size of the CBD<br />
on ultrasound was 11.7±3.7mm (range of 4.0mm to 23.0mm) while that<br />
on MRCP was 13.8±4.7mm (range of 4.1mm to 30.0mm). The average<br />
number of stones extracted per patient was 7.5±11.8 with a range of<br />
1 to 70. The size of the extracted stones varied from 2mm to 30mm,<br />
with the average stone size being 11.5±4.8mm.The average duration of<br />
surgery was 139.9±26.3 min with a range of 90 to 205 min. The maximum<br />
duration was seen with conversion to open procedures followed by those<br />
with T-tube drainage. The mean intra-operative blood loss was 103.4±85.9<br />
ml (range 10 to 500 ml).<br />
In patients with T-tube drainage, the average duration for which the<br />
T-tube was kept was 13.1±5.0 days (range 9 to 36 days). There was one<br />
post-operative death (0.7%). Twenty three patients (15%) had nonfatal<br />
postoperative complications (25 events in total) ranging from minor<br />
complications like wound infection to more serious ones like bile leakage.<br />
There were 3 cases of retained stones (2%), all of which were managed<br />
effectively with post-operative ERCP.Post-operative stay ranged from 2 to<br />
33 days with an average of 4.6±4.1 days. The patients with conversion to<br />
open procedures had the longest stays, while those with primary closure<br />
had the shortest stays. 96% of the procedures could thus be completed by<br />
laparoscopic techniques.<br />
Conclusions: This study shows that for the subgroup of patients with<br />
multiple, large, impacted stones in a dilated CBD who were traditionally<br />
subjected to open CBD exploration owing to inefficiency of ERCP,<br />
minimally invasive procedure with its attendant benefits, in the form<br />
of laparoscopic CBD exploration (LCBDE) is highly effective and safe<br />
procedure. LCBDE when performed by an experienced surgeon results in<br />
no additional morbidity or mortality as compared to open surgery, with<br />
excellent success rates and 98% stone clearance from the CBD.<br />
S019<br />
GERIATRIC SURGERY: IMPACT OF AGE ON THE OPERATIVE DECISION<br />
IN GALLSTONE DISEASE Simon Bergman, MD MSc, Nadia Sourial, MSc,<br />
Shannon A Fraser, MD MSc, Wael C Hanna, MD, Isabelle Vedel, MSc,<br />
Michèle Monette, Gabriela Ghitulescu, MD, Issie Weissglas, MD, Johanne<br />
Monette, MD Department of Surgery, Sir Mortimer B. Davis Jewish General<br />
Hospital, Montreal, QC; Solidage Research Group on Frailty and Aging,<br />
Montreal, QC; Division of Geriatric Medicine, Sir Mortimer B. Davis Jewish<br />
General Hospital<br />
Introduction: Elderly patients with gallstone disease often present and<br />
are treated differently than their younger counterparts. We hypothesize<br />
that these differences also exist within age subgroups of elderly patients.<br />
The purpose of this study is to evaluate the relationship between age and<br />
disease severity and management of gallstone disease, and to identify the<br />
12 th World Congress of Endoscopic Surgery<br />
103 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
predictors of performing a cholecystectomy.<br />
Methods: This is a single institution retrospective chart review of hospital<br />
visits for patients ≥65 with biliary colic, cholecystitis, choledocholithiasis,<br />
cholangitis, or biliary pancreatitis, between April 2004 and April 2008. All<br />
prior visits for these patients were also reviewed. Disease severity<br />
outcomes were diagnosis (colic vs. complicated) at first visit, visit type<br />
(emergency department (ED) visit only vs. urgent admission vs. elective<br />
admission) and clinical severity score (calculated upon presentation to ED<br />
and based on temperature, pulse, BP, WBC, and symptom duration).<br />
Management outcomes were occurrence of cholecystectomy, occurrence<br />
of cholecystostomy tube, and admitting ward at first visit. Stratified age<br />
groups (Group 1: 65-75, Group 2: 75-85, and Group 3: ≥85) were compared<br />
using Mantel-Haenszel for proportions. Multivariable logistic regression<br />
was used to identify predictors of undergoing cholecystectomy.<br />
Results: 433 patients over 622 hospital visits were included in the analysis.<br />
Mean Charlson Comorbidity Index (CCI) for Group 1 (n=203), Group 2<br />
(n=169), and Group 3 (n=61) were 1.5±1.8, 2.2±2.1, and 2.3±1.9,<br />
respectively. Disease severity: At first visit, diagnosis was complicated<br />
disease in 34.0%, 63.1%, and 70.5% of patients (p
Scientific Session Oral Abstracts<br />
Conclusion: Our data suggest that bile duct injury rates are not<br />
influenced by the presence of a surgical training program. In addition,<br />
there were no significant differences in mortality for LC done at hospitals<br />
with surgical training programs when compared to hospitals without<br />
surgical training programs. There was a significant difference noted in<br />
admission type and conversion rates but this did not appear to affect the<br />
rate of bile duct injury.<br />
S022<br />
EVALUATION OF INTRAPERITONEAL PLACEMENT OF ABSORBABLE<br />
AND NONABSORBABLE BARRIER COATED MESH SECURED WITH<br />
FIBRIN SEALANT (NEW ZEALAND WHITE RABBIT MODEL) Eric D<br />
Jenkins, MD, Lora Melman, MD, Salil Desai, BA, Shaun R Brown, DO,<br />
Margaret M Frisella, RN, Corey R Deeken, PhD, Brent D Matthews, MD<br />
Department of Surgery, Washington University, St. Louis, Missouri<br />
Introduction: The purpose of this study is to evaluate the acute and<br />
chronic fixation strength of fibrin sealant as an alternative fixation method<br />
for laparoscopic ventral hernia repair (LVHR).<br />
Methods: Representative mesh types for LVHR included one<br />
nonabsorbable barrier mesh (Composix), and three absorbable barrier<br />
meshes (Sepramesh, Proceed and Parietex Composite). Macroporous<br />
polypropylene mesh (Prolite Ultra) served as control. Three methods of<br />
fixation were used, 0-polypropylene suture + fibrin sealant (ARTISS 4IU,<br />
Baxter Healthcare Corp.), fibrin sealant alone (ARTISS) or tacks alone, to<br />
secure 3x4cm pieces of mesh (n=10 each combination) to the peritoneal<br />
surface of New Zealand white rabbit abdominal wall. After 2 hours of<br />
incubation at 37C, specimens underwent acute testing, described below.<br />
Subsequently, a chronic phase was completed using the aforementioned<br />
fixation methods (n=10 each combination), where two 4x4cm pieces of<br />
mesh were secured intraperitoneally in each of 75 New Zealand white<br />
rabbits and survived eight weeks until sacrifice. A transparent grid overlay<br />
was utilized to measure mesh area and adhesion area. Adhesion tenacity<br />
was characterized using the Garrard adhesion scale. For both acute and<br />
chronic samples, a 3x3cm area of mesh-tissue interface underwent lap<br />
shear testing at a rate of 0.42mm/sec using a tensiometer (Instron 5542,<br />
Norwood, MA), for both acute and chronic samples. The maximum load<br />
sustained by the mesh-tissue construct was recorded as the acute fixation<br />
strength in Newtons (N). Data are given as means ± SEM. Statistical<br />
significance (p
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
impact of open versus endoscopic component separation in complex<br />
abdominal wall reconstruction.<br />
METHODS: All patients undergoing open and endoscopic CST between<br />
2005 and 2009 by a single surgeon at Case Medical Center were<br />
retrospectively identified. Length of stay and financial data were obtained<br />
for the primary admission. Direct and Indirect costs were evaluated. Direct<br />
costs were itemized as: operating room supplies/time, anesthesia, ICU,<br />
floor care, laboratory, imaging, pharmacy and supportive therapy. Median<br />
and interquartile ranges (IQR) were evaluated by Wilcoxon rank sum test<br />
with a p-value of
Scientific Session Oral Abstracts<br />
S027<br />
A COMPARISON OF OUTCOMES IN OPEN VERSUS LAPAROSCOPIC<br />
SURGICAL REPAIR OF RECURRENT INGUINAL HERNIAS Nilay R Shah,<br />
MD, Clayton T Hodges, BS, Vanchad R Memark, MD, Eric T Volckmann,<br />
MD, Clinton R Hall, MD, Bradley J Needleman, MD, Dean J Mikami, MD,<br />
Jeffrey W Hazey, MD, W. Scott Melvin, MD, Vimal K Narula, MD Center for<br />
Minimally Invasive Surgery, Division of Gastrointestinal Surgery, The Ohio<br />
State University Medical Center, Columbus, Ohio, USA<br />
Introduction: Inguinal hernia recurrence following surgical repair is a<br />
major concern. There are conflicting views in the surgical community<br />
regarding the best treatment approach to prevent recurrence. We report<br />
our experience with open and laparoscopic repair of recurrent inguinal<br />
hernias.<br />
Methods: After obtaining Institutional Review Board (IRB) approval, we<br />
retrospectively reviewed the charts of 98 patients who had surgical repair<br />
of recurrent inguinal hernias from January 2004 through July 2009. Repair<br />
techniques included open with mesh, transabdominal pre-peritoneal<br />
(TAPP), or totally extraperitoneal (TEP). Surgical variables and clinical<br />
outcomes were compared using Chi-square, Fisher’s exact, and Mann-<br />
Whitney U test.<br />
Results: Ninety-eight patients with a mean age of 55 years underwent<br />
either open mesh repair (N=16) or laparoscopic mesh repair (N=82) for<br />
recurrent inguinal hernias. Hernia recurrence was found on the right side<br />
in 51 patients, left in 41 patients, and bilaterally in 6 patients. The mean<br />
operative time was 75 minutes in the open repair and 66 minutes in the<br />
laparoscopic (TAPP or TEP) repair (p = 0.15). The mean follow-up was<br />
18.4 months. There were no re-recurrent hernias in the open group and 4<br />
(4.8%) re-recurrent hernias in the laparoscopic group (p=0.5). Two patients<br />
(12.5%) in the open group and 10 patients (12.1%) in the laparoscopic<br />
group had ongoing pain in the inguinal region (p=0.8). Five patients<br />
(31.3%) in the open group and 6 patients (7.3%) in the laparoscopic group<br />
had post-operative complications (p=0.02).<br />
Conclusions: Both the open and laparoscopic mesh approaches<br />
are acceptable in the treatment of recurrent inguinal hernias. In this<br />
retrospective review, there is no statistical difference in the re-recurrence<br />
rate between the two techniques. In this study, the complication rate in<br />
the open group is greater than in the laparoscopic group. Prospective,<br />
randomized multicenter clinical trials are required to determine the ideal<br />
approach for the treatment of recurrent inguinal hernias.<br />
S028<br />
30-DAY READMISSION AFTER VENTRAL HERNIA REPAIR:<br />
PREDICTABLE OR PREVENTABLE? Jeffrey A Blatnik, MD, Karem C Harth,<br />
MD MHS, Mark I Aeder, MD, Michael J Rosen, MD Department of Surgery,<br />
University Hospitals Case Medical Center, Cleveland, OH<br />
Introduction: Thirty-day readmission has become an increasingly<br />
scrutinized event in the field of surgery, especially in light of projected<br />
cuts in reimbursement. Our objective was to determine if any factors are<br />
predictive of 30-day readmission in patients undergoing ventral hernia<br />
repair.<br />
Methods: We retrospectively reviewed consecutive charts of patients<br />
who underwent laparoscopic or open ventral hernia repair from<br />
September 1st, 2005 through June 30th, 2009 by one surgeon at our<br />
institution. Perioperative variables included: age, gender, ASA score, BMI,<br />
# comorbidities (smoking, diabetes mellitus, COPD, immunosupression),<br />
number of prior abdominal surgeries, type of surgery and active<br />
abdominal infection at the time of surgery. The primary outcome measure<br />
was all cause 30-day readmission. Univariate analysis consisted of Mann-<br />
Whitney and Fischer’s or Chi-squared statistics. Multiple logistic regression<br />
was performed on significant variables followed by the likelihood ratio<br />
test to assess model significance. A p-value of
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
supported these impressions regarding increased technical difficulty,<br />
as LAP scores were significantly better than both LESS Straight and<br />
LESS Articulating scores. Furthermore, 59% indicated that articulating<br />
instruments did not help in performing the Peg task and the LESS Straight<br />
scores were significantly better than LESS Articulating scores. Despite<br />
these obstacles, 82% believe that LESS will be adopted by surgeons in<br />
the next 5 years, 97% believe that LESS will provide better cosmesis, and<br />
100% would offer LESS to their patients if appropriately trained.<br />
FLS PEG TRANSFER NORMALIZED SCORES<br />
LESS<br />
Conventional Laparoscopic Straight Instruments<br />
LESS<br />
Articulating<br />
Instruments<br />
N= 45 62.8 ± 62.1 34.6 ± 29.0* 18.9 ± 114.9*<br />
*p< 0.001 comparing LAP vs. LESS Straight, LAP vs. LESS Articulating, and LESS<br />
Straight vs. LESS Articulating; high scores indicate superior performance<br />
Conclusion: Despite the increased technical difficulty associated with a<br />
LESS approach, the majority of surgeons feel that LESS will be adopted.<br />
Further improvements in instrumentation and operative strategies<br />
are needed, in conjunction with robust training methods, including<br />
simulation, such that LESS procedures can be safely and efficiently<br />
performed.<br />
S030<br />
TRENDS AND RESULTS OF THE FIRST FIVE YEARS OF FUNDAMENTALS<br />
OF LAPAROSCOPIC SURGERY (FLS) CERTIFICATION TESTING Allan<br />
Okrainec, MD, Nathaniel J Soper, MD, Lee L Swanstrom, MD, Gerald M<br />
Fried, MD University of Toronto, Toronto, ON, Northwestern University<br />
Feinberg School of Medicine, Chicago, IL, Legacy Health System, Portland,<br />
OR, and McGill University, Montreal, QC<br />
Introduction: FLS is an educational program developed by the Society<br />
of American Gastrointestinal and Endoscopic Surgeons and endorsed by<br />
the American College of Surgeons. The goal of the FLS program is to teach<br />
and assess the basic cognitive and psychomotor skills required to perform<br />
laparoscopic surgery. The purpose of this study was to review the results<br />
from the first five years of FLS certification testing.<br />
Methods: FLS test data were prospectively collected for all participants<br />
taking the FLS certification examination since its inception. De-identified<br />
data were reviewed and analyzed using standard descriptive statistics.<br />
Results: The FLS examination was taken by 2189 participants between<br />
October 2004 and July 2009. There was a yearly increase in the number of<br />
individuals seeking FLS certification, with 13 participants tested in 2004,<br />
65 in 2005, 141 in 2006, 366 in 2007, 588 in 2008, and 1016 in the first 7<br />
months of 2009. Complete demographic information was available for<br />
approximately 1500 participants: 13% were junior residents (PGY 1-3),<br />
67% were senior residents (PGY 4-5) or fellows, and 20% were attending<br />
surgeons. A breakdown of participants by specialty revealed that 84%<br />
were general surgeons, 7% gynecologists, 2% urologists, and 7% were<br />
labeled as other. The mean (SD) score on the cognitive exam was 519<br />
(157) with a 93% pass rate. The mean score on the technical skills exam<br />
was 525 (117) with a 92% pass rate. After combining both scores, the<br />
overall FLS certification passing rate was 87%.<br />
Conclusions: The FLS certification exam has gained widespread<br />
acceptance among laparoscopic surgeons in training and practice with a<br />
marked increase in testing since the American Board of Surgery mandate<br />
for certification was announced. The overall pass rate of 87% on the<br />
examination approaches the target pass rate of 90%, established during<br />
the test-setting process.<br />
S031<br />
A NATIONAL TRAINING PROGRAM FOR LAPAROSCOPIC COLORECTAL<br />
SURGERY IN THE UK Danilo Miskovic, MD FRCS, Susannah M Wyles,<br />
MSc MRCS, Mark G Coleman, MD FRCS, George B Hanna, PhD FRCS<br />
Department of Biosurgery and Surgical Technology, Imperial College<br />
London/UK for the National Training <strong>Program</strong>me for Laparoscopic<br />
Colorectal Surgery<br />
Introduction: The aim of this study was to investigate the educational<br />
12 th World Congress of Endoscopic Surgery 108<br />
impact of a national training programme (NTP) for laparoscopic colorectal<br />
surgery by analysing peer- and self- assessments of trainers and trainees.<br />
Methods: Colorectal surgeons enrolled in the NTP (trainees) were trained<br />
in a series of individual live cases by expert laparoscopic surgeons<br />
(trainers). Trainers rated their trainees after each supervised case,<br />
using a Global Assessment Score form. Trainees completed a similar<br />
self-assessment form. The target score was set at 5 (=independent<br />
performance). Proficiency gain curves were analysed by CUSUM charts<br />
and interrater agreement by Bland Altman plots.<br />
Results: Analysis involved data of 252 cases (38 trainees and 20 trainers).<br />
The median number of training cases per trainee was 5.5 (range<br />
1-25). Trainers rated slightly higher then the trainees self-assessment<br />
[Variation +0.02 (2 SD=+/-1.3)]. On average the target score was reached<br />
approximately after case 15. A more detailed analysis of the CUSUM charts<br />
showed that theatre setup, exposure of the operating field, exteriorisation<br />
of the specimen and anastomosis was completed independently after<br />
five supervised sessions, whereas dissection of the vascular pedicle,<br />
mobilisation of the colon/ rectum took more than 15 procedures.<br />
Conclusions: These early results are supportive evidence for the efficacy<br />
of the National Training <strong>Program</strong>me in Laparoscopic Colorectal Surgery.<br />
Trainees scored themselves slightly lower than their trainers suggesting<br />
adequate insight. Furthermore, when planning training it should be noted<br />
that different stages of the operation are learnt at different rates.<br />
Figure: CUSUM chart of peer assessments by the trainer, with breakdown<br />
of the different components.<br />
S032<br />
ANALYSIS OF STANDARD MULTI-PORT VS. SINGLE SITE ACCESS FOR<br />
LAPAROSCOPIC SKILLS TRAINING AND ACQUISITION Daniel R Cox, BS,<br />
Wenjing Zeng, BS, L Michael Brunt, MD Washington University School of<br />
Medicine<br />
Introduction: Single site access (SSA) laparoscopy is gaining popularity<br />
but is more challenging to perform than laparoscopy using multiple<br />
separate port sites. This study examined the effect of standard multi-port<br />
(MP) laparoscopic skills training versus SSA training on laparoscopic skills<br />
acquisition and performance in surgically nave individuals.<br />
Methods: Forty end-of-first year medical students were randomized into<br />
two groups. Both groups were then trained on 4 laparoscopic drills (peg<br />
transfer [Peg], cobra rope [Rope], bean drop [Bean] and pattern cutting<br />
[Pattern]) using either a standard MP laparoscopic setup (Group 1) or an<br />
SSA skill approach (Group 2). Students then practiced the skills exclusively<br />
using the approach on which they were trained until a pre-determined<br />
proficiency level was reached. Training time to proficiency and number<br />
of repetitions (reps) for each drill were recorded. Each group then crossed<br />
over to the alternate approach where the sequence was repeated.<br />
Statistical analysis was performed using a two-tailed, unpaired t-test.<br />
Results: Mean skills times and numbers of repetitions to proficiency<br />
are in the table. Four students (3 in Gr. 1, one in Gr. 2) were unable to
Scientific Session Oral Abstracts<br />
complete the study. Total combined times to proficiency for the SSA and<br />
MP approaches was not significantly different between groups (Group<br />
1 MP 234.0 ± 114.9 min vs Group 2 SSA 216.4 ± 106.5 min, p=0.67). The<br />
MP-trained group took less time to reach proficiency on the standard<br />
MP setup than the SSA group did on the SSA approach (119.1 ± 69.7 min<br />
vs 178.0 ± 93.4 min, p=0.058) with significantly fewer repetitions (77.6 ±<br />
42.6 vs. 118.8 ± 54.3, p=0.027). When the SSA-trained group crossed over<br />
to the MP setup, they took significantly less time to reach proficiency for<br />
the MP setup than the standard MP-trained group (38.4 ± 29.4 min vs.<br />
119.1 ± 69.7 min; p=0.0013), reaching proficiency in a mean of only 26.9<br />
(range 11-65) total repetitions. Similarly, when the standard MP group<br />
crossed over to the SSA setup, they took significantly less time to reach<br />
proficiency with the SSA approach than the SSA-trained group (114.8<br />
±50.5 min vs. 178.0 ± 93.4 min, p=0.026) but with more total repetitions<br />
than was needed to achieve proficiency with the M-P approach (86.2±<br />
35.2 vs 77.6 ± 42.6, p= NS).<br />
Group Task Peg Peg Rope Rope Bean Bean Pattern Pattern Total Total<br />
Setup Time Reps Time Reps Time Reps Time Reps Time Reps<br />
1 (MP<br />
Trained<br />
MP 17.3 12.8 5.6 8.8 20.8 13.9 67.2 36.6 119.1 77.6<br />
1 SSA 35.4 29.6 8.8 13.1 21.3 14.2 51.7 29.7 114.8 86.2<br />
2 (SSA<br />
Trained<br />
SSA 53.9 38.2 13.8 19.3 29.2 19.6 81.9 42.1 178.0 118.8<br />
2 MP 5.4 4.5 0.8 1.4 4.9 3.2 28.4 18.7 38.4 26.9<br />
MP= multiport, SSA = Single site access<br />
Conclusions: Laparoscopic single site access skills training initially results<br />
in longer times and more repetitions to achieve proficiency than standard<br />
multi-port training, but the skills acquired transfer well to the multi-port<br />
approach. Both modalities should be used in training surgical residents<br />
for single incision laparoscopy in patients.<br />
S033<br />
A DEFICIENCY IN KNOWLEDGE OF BASIC PRINCIPLES OF<br />
LAPAROSCOPY AMONG ATTENDEES OF AN ADVANCED<br />
LAPAROSCOPIC SURGERY COURSE Carlos A Menezes, MD, Daniel W<br />
Birch, MD, Andrey Vizhul, MD, Xinzhe Shi, MPH, Vadim Sherman*, MD,<br />
Shahzeer Karmali, MD Centre for the Advancement of Minimally Invasive<br />
Surgery, University Of Alberta, Edmonton, Alberta, Canada; *Baylor<br />
College of Medicine, Houston, Texas, USA.<br />
Introduction: Advanced laparoscopic courses serve as a comprehensive<br />
and very popular Continuing Medical Education (CME) activity.<br />
Knowledge of basic laparoscopy is an assumed prerequisite for<br />
attendance at these courses.<br />
Objective: To determine the baseline laparoscopic knowledge of<br />
attendees at an advanced laparoscopic surgical course.<br />
Methods: A seventeen question exam was designed utilizing<br />
data from the basic laparoscopic quizzes on the Society of American<br />
Gastroenterological Surgeons (<strong>SAGES</strong>) website (www.sages.org/<br />
education/quiz). The questions covered four realms of basic laparoscopy:<br />
access, pneumoperitoneum, camera navigation and surgical<br />
instrumentation. The questionnare was distributed to all attendees at<br />
an advanced laparoscopic course at the 2009 Canadian Surgical Forum<br />
organized by the Canadian Association of General Surgeons.<br />
Results: Forty three respondents completed the survey. Fifty-three<br />
percent (53%) of responders had been in practice for more than 10<br />
years and 65% had over 5 years experience. Fifty five percent (55%)<br />
[24/43] of respondents listed laparoscopic courses as the sole means of<br />
laparoscopic training. Sixty-one percent (61%)[28/43] were performing<br />
>50 laparoscopic cases per year. The median score on the knowledge<br />
based questions was 70.6% [12/17]. In terms of overall score, respondents<br />
with more than 5 years experience performed similarly to respondents<br />
with less than 5 years experience (73% correct answers) [Figure<br />
1]. Interestingly, in sub-group analysis, respondents performed well in<br />
camera skills and pneumoperitoneum themed questions (84% correct<br />
answers) but faired poorly on questions pertaining to instrumentation or<br />
access (52% correct answers)[Figure 2].<br />
Conclusion: Basic laparoscopic knowledge among the attendees of an<br />
advanced laparoscopic course is sub-optimal. Review of basic principles<br />
of laparoscopy particularly pertaining to instrumentation and<br />
access should form part of these CME activities.<br />
S034<br />
EVALUATION OF SURGICAL PERFORMANCE DURING LAPAROSCOPIC<br />
INCISIONAL HERNIA REPAIR- A MULTICENTER STUDY Iman Ghaderi,<br />
MD, Marilou Vaillancourt, MD, Liane S Feldman, Gideon Sroka, MD, Pepa<br />
A Kaneva, MS, Melina C Vassiliou, MD, Jacob Seagull, PhD, Erica Sutton,<br />
MD, Carlos Godinez, MD, Ivan George, BSc, Adrian E Park, MD, Ian Choy,<br />
MD, Allan Okrainec, M Steinberg-Bernstein Centre for Minimally Invasive<br />
Surgery, McGill University, Montreal, QC, University of Western Ontario,<br />
London, ON, University of Maryland, Baltimore, MD, University of Toronto,<br />
Toronto, ON, Carolinas Medical Center, Charlotte, NC<br />
Introduction: Laparoscopic incisional hernia repair (LIHR) is a relatively<br />
common procedure yet requires advanced laparoscopic skills. There is no<br />
reliable or valid measure of performance during this procedure. The aim<br />
of this study was to develop a procedure-specific objective rating scale<br />
to assess performance of LIHR, and to evaluate its reliability and validity.<br />
Methods: The Global Operative Assessment of Laparoscopic Skills-<br />
Incisional Hernia Module (GOALS-IH) is a global rating scale developed<br />
by content experts consisting of 7 items evaluating the critical steps of<br />
LIHR (placement of trocars, adhesiolysis, estimation of size and shape of<br />
the mesh, introduction, orientation and positioning of the mesh, fixation<br />
of the mesh, knowledge and autonomy in the use of instruments, overall<br />
competence) each rated on a 5-point Likert scale (maximum possible<br />
score =35). During LIHR, 10 experienced and 12 intermediate level<br />
surgeons (PGY3 to 5) were evaluated at 4 University hospital centers<br />
by the attending, a trained observer and by self-assessment using the<br />
GOALS-IH, and by a previously validated 5-item general laparoscopic<br />
rating scale (GOALS). Interrater reliability was assessed by intraclass<br />
correlation (ICC), internal consistency of rating items by Cronbach’s<br />
alpha. Known-groups construct validity was assessed by t-test and by<br />
correlating the number of self-reported LIHR cases with total score;<br />
concurrent validity by correlating the procedure-specific rating scale with<br />
the GOALS general rating scale. Data are shown as mean (95% CI). Results:<br />
Interrater reliability for the total GOALS-IH score was 0.80 (0.56-0.92)<br />
between observer and attendings, 0.81 (0.58-0.92) between participants<br />
109 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
and attendings, and 0.89 (0.76-0.96) between participants and observer.<br />
Internal consistency was high, with Cronbach’s alpha 0.97. The correlation<br />
of each domain with total score ranged from 0.83 to 0.93. There was<br />
strong correlation between GOALS-IH and generic GOALS total scores<br />
(r =0.90, p
Scientific Session Oral Abstracts<br />
Materials and methods: Fourty-two LRHP were performed between<br />
2000 and 2008. The procedure was standardized by an expert in colorectal<br />
surgery. This included port placement, adhesiolysis, rectal stump<br />
management, splenic flexure mobilization, and colorectal anastomosis<br />
with early introduction of the anvil through the stoma. Trainee surgeons<br />
(experience inferior to 20 colorectal surgeries) were mentored by an<br />
expert surgeon (experience over 2,000 colorectal procedures). Operative<br />
time, conversion, complications and post-operative outcome were<br />
measured. The group of patients operated upon by the senior colorectal<br />
surgeon was compared to the group of patients operated upon by the<br />
trainee surgeons while being mentored by the senior surgeon.<br />
Results: Each group included 21 patients. All patients underwent LRHP<br />
successfully and no mortality occurred. No intra-operative significant<br />
difference was observed between the group of trainees and experts:<br />
operative time was of 131 minutes (range: 70-230) vs. 132 minutes<br />
(range: 60-240); conversion rate: 2 (1 ureteral injury in the trainee’s group,<br />
repaired intra-operatively and 1 difficult adhesiolysis in the expert’s<br />
group). Complications occurred in 6 patients (14%), 3 requiring reoperation<br />
(7%). Two complications occurred in the trainee’s group (1 early<br />
anastomotic stricture requiring re-operation, 1 late stenosis requiring<br />
endoscopic dilation). Four complications occurred in the expert’s group<br />
(two patients were re-operated upon during the first 30 days, 1 for a postoperative<br />
obstruction and 1 for an early post-operative fistula) and two<br />
were treated medically (1 port site infection, 1 rectorrhagia). The patient<br />
post-operative outcomes were comparable in both groups: oral intake: 3<br />
vs. 2 days; hospital stay: 6 vs. 7.5 days.<br />
Conclusion: Performing these difficult but standardized laparoscopic<br />
procedures offers the same results as when performed by trainees<br />
mentored by an expert surgeon, or carried out by an expert. The observed<br />
complication rate (14%) was comparable to that of experienced centres<br />
(131 to 48%2, including anastomotic leaks2; ureteral injury1, anastomotic<br />
strictures1,2 and re-operations (3.31 to 19%2). The expert mentoring does<br />
not prevent all intra-operative complications in challenging procedures,<br />
but can solve intra-operative technical problems that make the trainee<br />
more confident. Additionally, no intra-operative complication was<br />
encountered. Trainee mentoring and procedure standardization will<br />
probably increase their ability to perform more advanced procedures<br />
without any additional risk for the patient. Mentoring should be<br />
promoted as it can be performed locally or remotely through modern<br />
interactive technology.<br />
References<br />
1. Haughn C, Ju B, Uchal M, Arnaud JP, Reed JF, Bergamashi R.<br />
Complication rates after Hartmann’s reversal: open vs. laparoscopic<br />
approach. Dis Col Rect 2008;51:1232-1236.<br />
2. Aydin HN, Remzi FH, Tekkis PP, Fazio VW. Hartmann’s reversal is<br />
associated with high postoperative adverse effects. Dis Col Rect<br />
2005;48:2117-2126.<br />
S038<br />
TRANSGASTRIC APPROACH DOES NOT INCREASE POSTOPERATIVE<br />
INFECTIONS OR COMPLICATIONS IN SWINE UTERINE HORN<br />
RESECTION Asghar Azadani, MD, Henrik Jonsson, MD, Maria Bergstrom,<br />
MD PhD, Per-Ola Park, MD PhD Dept of Surgery, Sahlgrenska University<br />
Hospital, Gothenburg, Sweden, Dept of Surgery, South Alvsborg Hospital,<br />
Boras, Sweden<br />
Introduction: Doubts have been raised versus NOTES surgery concerning<br />
intra abdominal infectious complications. The aim of this study was to<br />
compare the postoperative course in open, laparoscopic and transgastric<br />
surgery, specially concerning infections and postop well being in a<br />
randomized porcine survival study.<br />
Methods & Procedures: 30 landrace pigs were randomized to open,<br />
laparoscopic or NOTES (transgastric) uterine horn resection with a survival<br />
time of 4 weeks. All animals were prepared with liquid diet for 2 days<br />
and fasted for 12 hours prior to surgery. They received a single dose of<br />
prophylactic antibiotics, Cefuroxim, at start of the procedure. No washing<br />
of the stomachs was performed in the transgastric group. All surgical<br />
procedures were performed by trained surgeons, NOTES operations<br />
were performed by trained surgical endoscpists. Open and laparoscopic<br />
surgery was performed using standard surgical techniques. Transgastric<br />
surgery was performed using the Olympus R-scope together with<br />
conventional endoscopic accessories. The gastric access site was closed<br />
using TAS T-tags (Ethicon Endosurgery). Peritoneal fluid was sampled for<br />
bacterial culture at the time of peritoneal access, prior to closure and at<br />
post mortem. The operating time and the postop time till standing up<br />
and eating were recorded. During the first postop week temperature<br />
and weight were recorded daily. Blood samples were taken every other<br />
day during one week and then every week until post mortem. CRP was<br />
analysed using porcine specific ELISA.<br />
Results: 27 animals survived until euthanised at 4 weeks. Three animals,<br />
one from each group, were euthanized earlier; one due to a hoof<br />
infection, one omental bleeding, one abdominal wound dehiscence. The<br />
operating time was significantly longer in the NOTES-group, mean 124<br />
min versus 35 min for lap surgery and 23 min for open surgery. However,<br />
the groups did not differ concerning postop time to standing up or<br />
eating, postop temperature or weight-gain.<br />
At post mortem 3/9 animals in the open surgery group had wound<br />
infections and 2/9 in the laparoscopic group. No intra abdominal<br />
infections were recorded in either group and there was no significant<br />
difference in bacterial cultures at any time-point. The CRP was equal prior<br />
to surgery and at its conclusion, but at postop day one the NOTES group<br />
had significantly lower CRP than open or lap surgery. From day 3 until day<br />
28 no differences were seen.<br />
Conclusion: Despite a long operating time the transgastrically operated<br />
animals recovered just as quickly as the other animals and showed no<br />
infectious complications. The lower CRP at day 1 indicates a reduced<br />
stress response in the NOTES group.<br />
S039<br />
STUDY OF HUMAN PERITONEAL BACTERIAL CONTAMINATION AFTER<br />
NOTES TRANSGASTRIC AND TRANSVAGINAL CHOLECYSTECTOMY<br />
Silvana PERRETTA, MD, Bernard DALLEMAGNE, MD, Pierre ALLEMANN,<br />
MD, Gianfranco DONATELLI, MD, Cosimo CALLARI, MD, Hurng-Shen WU,<br />
MD, Jacques MARESCAUX, MD IRCAD, University Hospital of Strasbourg,<br />
France - Show Chwan Memorial Hospital, Changhua, Taiwan<br />
Introduction: The recent literature has questioned the infectious risk of<br />
natural orifice translumenal endoscopic surgery (NOTES). One important<br />
requirement of this technique is the need to minimize the risk of eritoneal<br />
contamination.<br />
Our study examines the resultant microbial contamination of the human<br />
peritoneum after transgastric and transvaginal cholecystectomy.<br />
Methods and procedures: From April 2007 to September 2009,<br />
22 patients undergoing transgastric (n 11) and transvaginal (n 11)<br />
cholecystectomy for non complicated cholelithiasis were prospectively<br />
studied as part of a database approved by our Institutional Review<br />
Board. Intraoperative samplings of peritoneal fluid were collected before<br />
and after transgastric (n=11) and transvaginal (n=6/11) access and<br />
sent for anaerobic, aerobic and fungal cultures. Each sample was sent<br />
for bacterial colony counts, culture, and identification of species. No<br />
gastric decontamination was performed and the vagina was prepped<br />
with betadine. All patients received single-shot intraoperative antibiotic<br />
prophylaxis. Operative times, clinical course and biological parameters<br />
were recorded.<br />
Results: Patients undergoing cholecystectomy had peritoneal exposure<br />
after trasngastric access for an average of 150 minutes, versus 113<br />
minutes for patients undergoing transvaginal approach. Two of 11<br />
patients (18%) had evidence of novel bacterial contamination of the<br />
peritoneum after transgastric approach (Escherichia Coli and Staph.<br />
Coagulase -). No patient had a positive anaerobic culture or fungal culture<br />
from the peritoneum in the transvaginal group. Total operative time did<br />
not predict peritoneal contamination. No clinically significant infectious<br />
complications or leaks were noted at 30-day follow-up.<br />
Conclusions: Prolonged peritoneal exposure to gastric content<br />
demonstrates minimal contamination of the abdominal cavity and is<br />
without postoperative infectious significance. Transvaginal incision would<br />
effectively be a clean portal of entry for NOTES.<br />
111 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
S040<br />
PROSPECTIVE RANDOMIZED TRIAL COMPARING LAPAROSCOPIC AND<br />
NOTES CHOLECYSTECTOMY: PRELIMINARY RESULTS Alberto R Ferreres,<br />
MD PhD MPH FACS, Anibal Rondán, MD, Santiago Horgan, MD, Julieta<br />
Paleari, MD, Mariano E Giménez, MD, Oscar O Laudanno, MD, Vicente P<br />
Gutiérrez Department of Surgery. University of Buenos Aires<br />
Introduction: the feasibility of hybrid NOTES cholecystectomy has<br />
been demonstrated. The recommendations from the 4th International<br />
Conference on NOTES (Boston, 2009) encouraged randomized trials to<br />
prove the advantages of this approach.<br />
Methods: Between January and July 2009, a prospective randomized<br />
trial of hybrid NOTES cholecystectomy (H-NC) versus laparoscopic<br />
cholecystectomy (LC) for patients with symptomatic gallstone disease<br />
was undertaken in compliance with our IRB and Ethics Committee´s<br />
approval. Mean age was 42.5 years. The inclusion criteria specify: a)<br />
Age between 18 and 65 years, b) Previous pregnancy/ies, and negative<br />
pregnancy tests, c) Informed consent process, d) Symptomatic gallbladder<br />
stones with surgical indication, e) Absence of common bile obstruction,<br />
f) Body mass index below 25, j) Non relevant ultrasound findings. The<br />
patients were allocated randomly in 2 groups of 20 patients each: Group<br />
I (LC): a laparoscopic cholecystectomy was performed with a 3 5 mm<br />
trocars and in cases, an additional 2 mm forceps for retraction of the<br />
gallbladder fundus was used. Group II (H-NC): placement of a 5 mm<br />
umbilical trocar for insuflation and visualization, insertion of a 2 channel<br />
trocar through the right posterior vaginal cul de sac and introduction of a<br />
flexible videoendoscope (Olympus GIF-160) and long forceps and diverse<br />
instruments (Novare®). Disecction of the cystic elements (duct and artery)<br />
and the Calot´s triangle was performed with electrocautery, scissors and<br />
Maryland forceps through the umbilical port, in a laparoscopic fashion as<br />
well as the ligaclip instrument. Removal of the gallbladder through the<br />
vagina using an endoscopic loop placed at its neck. The access was closed<br />
with a running suture of absorbable vycril 2/0 from the vagina. Antibiotic<br />
prophylaxis was used with cefazolin 1g before anesthetic induction and<br />
post-operative analgesia was standardized for the 2 groups.<br />
Results: 1) the procedure was completed as intended in both groups,<br />
2) Mean operative time was 38 +/- 8.5 minutes for LC and 56 +/- 12 for<br />
H-NC, 3) Length of stay was similar for both groups, 4) No intraoperative<br />
complications were achieved, 5) In two of the H-NC an additional 2 mm<br />
forceps was required, 6) No infectious or parietal complications developed<br />
during follow-up, 7) Postoperative pain was less in the N-HC group as<br />
well as the need for additional painkiller medication, but not statistically<br />
significant, 8) Cosmetic results were excellent in the H-NC group, 9)<br />
Patients´ preferences were inclined to the H-NC procedure and 10) 9)<br />
Return to work was in average 39 hours earlier for the H-NC.<br />
Conclusions: Our initial results conclude that H-NC is superior to LC for<br />
less postoperative pain and better cosmetic results, though it is associated<br />
with longer operative time and additional instruments. Nonetheless,<br />
H- NC can be performed safely and has an excellent outcome and high<br />
patient acceptability, comparable to LC for the treatment of cholelithiasis<br />
and intraoperative complications and total hospital stay.<br />
S041<br />
FIRST HUMAN EXPERIENCE WITH ENDOLUMINAL, ENDOSCOPIC<br />
GASTRIC BYPASS Bryan J Sandler, MD, C. Paul Swain, MD, Roberto<br />
Rumbaut, MD, Gustavo Torres, MD, Luis Morales, MD, Lizcelly Gonzales,<br />
MD, Santiago Horgan, MD University of California, San Diego, San Diego,<br />
CA, USA; Imperial College of London, London, England; San Jose Tec de<br />
Monterrey, Monterrey, Mexico<br />
Introduction: Here we report the first human experience with an<br />
endoluminal, endoscopically delivered and retrieved gastro-duodenojejunal<br />
bypass sleeve (ValenTx, Inc. Carpinteria, CA), including the shortterm<br />
weight loss and changes in co-morbidities.<br />
Methods and Procedures: The gastro-duodeno-jejunal bypass sleeve<br />
(GJBS) is a 120cm sleeve secured at the esophago-gastric junction with<br />
endoscopic and laparoscopic techniques, and is designed to create<br />
an endoluminal gastro-duodeno-jejunal bypass. The patients are<br />
12 th World Congress of Endoscopic Surgery 112<br />
morbidly obese individuals who meet NIH criteria for bariatric surgery. A<br />
prospective, single-center, 12 week trial was designed. At the completion<br />
of this trial, the device was explanted with endoscopic retrieval. The<br />
primary endpoints were safety and incidence of adverse events. The<br />
secondary outcomes included the percentage of excess weight loss (EWL)<br />
and changes in co-morbidities, specifically glucose control, use of antihyperglycemics,<br />
and changes in hemoglobin A1C levels.<br />
Results: From July 2008 until September 2009, 24 patients were enrolled.<br />
The device was implanted, left in-situ, and then retrieved. The study<br />
included 7 men and 17 women with a mean pre-operative BMI of 41.0<br />
kg/m2. The GJBS was successfully delivered in 22 of the 24 patients (92%)<br />
and retrieved endoscopically in all 22 patients in whom it was implanted<br />
(100%). One patient was excluded pre-operatively secondary to failure<br />
to lose weight on the pre-op liquid diet. One device was not attempted<br />
endoscopically due to significant inflammation at the gastro-esophageal<br />
junction at the time of laparoscopic evaluation.<br />
In the first phase of the study, 12 patients had the device placed. Nine of<br />
these patients maintained the device for the full 12 weeks of the study.<br />
These patients had 39.9% excess weight loss at the completion of the<br />
study. In the second phase of the trial, 12 patients were enrolled; at eight<br />
weeks the EWL is 40.5%.<br />
Of the 22 patients with the device implanted, 17 have maintained it (77%).<br />
Nine patients completed the 12-week trial and eight are ongoing at 8<br />
weeks. The primary reason for early explantation of the device was early<br />
post-operative dysphagia.<br />
The seven patients with pre-operative diabetes mellitus all had normal<br />
blood glucose levels throughout the trial and none required antihyperglycemic<br />
medications. All seven patients with elevated Hemoglobin<br />
A1C levels pre-operatively showed improvement by the end of the trial.<br />
Conclusions: This trial demonstrates that the endoluminal gastroduodeno-jejunal<br />
bypass sleeve can achieve excellent weight loss at<br />
12 weeks. No patient safety issues were encountered. Adverse effects<br />
were minimal and resolved upon endoscopic device removal. Effective<br />
glycemic control was demonstrated through use of the device during the<br />
trial. Long-term results are needed.<br />
S042<br />
ESOPHAGEAL STENT PLACEMENT PROVIDES SAFE CLOSURE<br />
FOLLOWING TRANSESOPHAGEAL ACCESS FOR NOTES® THORACIC<br />
PROCEDURES Brian G Turner, MD, Denise W Gee, MD, Min-Chan Kim, MD,<br />
Sevdenur Cizginer, MD, Mari Mino-Kenudson, MD, Patricia Sylla, MD, David<br />
W Rattner, MD, William R Brugge, MD FASGE (1) Gastrointestinal Unit, Dept<br />
of Medicine, (2) Department of Surgery, (3) Department of Pathology,<br />
Massachusetts General Hospital, Boston, MA<br />
INTRODUCTION: Safe esophageal closure remains a challenge in<br />
transesophageal Natural Orifice Transluminal Endoscopic Surgery (NOTES)<br />
procedures. Suturing or t-tag devices are time consuming and risk organ<br />
injury due to their blind deployment. Endoclips are difficult to place in<br />
the narrow esophagus and submucosal tunneling techniques do not<br />
necessarily prevent leakage of esophageal contents into the mediastinum<br />
or thorax. In this survival animal series, we demonstrate safe esophageal<br />
closure with a prototype retrievable, anti-migration stent.<br />
METHODS: Nine Yorkshire swine underwent thoracic NOTES procedures.<br />
A double-channel gastroscope equipped with a mucosectomy<br />
device was used to create a small esophageal mucosal defect. A 5-cm<br />
submucosal tunnel was created and a needle-knife was used to incise<br />
the muscular esophageal wall and permit entry into the mediastinum<br />
and thorax. Mediastinoscopy and thoracoscopy were performed in all<br />
swine; lymphadenectomy was performed in 7 swine. A prototype small<br />
intestinal submucosal (surgiSIS®) covered stent was deployed over the<br />
mucosectomy site and tunnel. Three versions of the prototype stent were<br />
developed (Table 1). Pre-necropsy endoscopy was performed to confirm<br />
stent location and retrieve the stent. Explanted esophagi were sent to<br />
pathology for review.<br />
RESULTS: Esophageal stenting was successful in all animals. Stent<br />
placement took 15.8±5 min and no stent migration occurred in any swine.
Scientific Session Oral Abstracts<br />
Pre-necropsy endoscopy revealed ingrowth of esophageal mucosa and<br />
erosion at the proximal portion of Stent A. Mucosal inflammation and<br />
erosion was observed at the proximal site of Stent B. No esophageal<br />
erosion or pressure damage from high radial forces was seen during<br />
stent retrieval in the swine receiving Stent C. On necropsy, swine 5 had<br />
a 0.5cm peri-esophageal abscess. Histology revealed a localized lesion<br />
at the esophageal exit site consisting of acute inflammatory cells in the<br />
esophageal wall in swine 4, 7, and 9. The mucosectomy site was partially<br />
healed in 3 swine and poorly healed in 6. All swine thrived clinically,<br />
except a brief period of mild lethargy in swine 9 on postoperative day 3.<br />
This particular swine improved with short-term antibiotic therapy. The<br />
submucosal tunnels were completely healed and no esophageal bleeding<br />
or stricture formation was observed in any swine. All swine survived<br />
13.8±0.4 days and gained weight in the postoperative period.<br />
CONCLUSION: Esophageal stenting provides safe closure for NOTES<br />
thoracic procedures, but may impede healing of the mucosectomy site.<br />
Table 1: Prototype Stent Specifications for Esophageal Closure<br />
Swine<br />
No<br />
Diameter<br />
Proximal<br />
Cage<br />
Diameter<br />
(body)<br />
Stent<br />
Length,<br />
mm<br />
Plastic<br />
covered<br />
proximal<br />
cage<br />
SIS/Plastic<br />
Covered<br />
body<br />
cage<br />
Stent A 1-5 45mm 28mm 80mm No Yes Yes<br />
Stent B 6-7 45mm 28mm 80mm Yes Yes Yes<br />
Stent C 8-9 37mm 22mm 65mm Yes Yes Yes<br />
S043<br />
Plastic<br />
covered<br />
distal cage<br />
QUANTITATIVE ERGONOMICS ASSESSMENT OF NOTES TECHNIQUES:<br />
A STUDY OF PHYSICAL WORKLOAD, BODY MOVEMENT AND POSTURE<br />
Gyusung Lee, PhD, Erica Sutton, MD, Yassar Youssef, MD, Tameka Clanton,<br />
MS, Adrian Park, MD University of Maryland<br />
Introduction: This study investigates through biomechanical analyses<br />
NOTES and laparoscopic physical workloads. Research confirms that<br />
surgeons experience physical symptoms due to the unfavorable<br />
ergonomics of MIS performance. The ergonomics of NOTES—potentially<br />
the next evolutionary surgical step—is only now being quantitatively and<br />
systematically assessed<br />
Methods and Procedures: Six surgeons with varying MIS experience<br />
were recruited for this IRB-approved study. Each participant performed<br />
two tasks 1) transferring rings between two sets of pegs by using two<br />
graspers; 2) transferring a triangle with attached eyelet between two<br />
circles by using a needle held by a needle driver. These tasks were<br />
performed using two surgical platforms: 1) traditional laparoscopy<br />
employing rigid instruments; 2) NOTES employing a dual-working<br />
channel flexible endoscope. With NOTES, the surgeon instructed an<br />
assistant in opening and closing the graspers. The NOTES approach was<br />
simulated by an upper torso mannequin placed at the trainer box front;<br />
an endoscope was introduced through the mannequin’s mouth. Motion<br />
capture, sixteen-channel electromyography (EMG), and force plate<br />
systems recorded biomechanical data. Integrated percentage maximum<br />
voluntary contraction (%MVC) obtained from EMG data collected<br />
throughout performance permitted identification of accumulated<br />
muscular workload. Mean %MVC was calculated for average muscular<br />
activation level. The postural stability demand (PSD) and the sway areas<br />
calculated from center of mass (COM) and center of pressure (COP)<br />
allowed postural sway quantification. A parallel study investigated<br />
surgical grasper force transfer mechanisms. Six electrodes placed on each<br />
subject’s forearm muscle groups and a force sensor located between each<br />
instrument’s jaws acquired data. Participants performed an opening/<br />
closing task using 1) two different-sized hemostats, 2) Maryland and Park<br />
laparoscopic graspers, and 3) endo-graspers and biopsy forceps. Force<br />
transfer was calculated by dividing &MVC by maximum tip force.<br />
Results: Integrated %MVC was substantially higher with NOTES<br />
performance (1305 %MVC) than with laparoscopy (375 %MVC) (p
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
S045<br />
HIATAL MESH IS ASSOCIATED WITH MAJOR RESECTION AT<br />
REVISIONAL OPERATION. Michael Parker, MD, Jillian M Bray, MD MPH,<br />
Adam S Harris, MD, Erol V Belli, MD, Jason M Pfluke, MD, Susanne S<br />
Preissler, Horacio J Asbun, MD, C D Smith, MD, Steven P Bowers, MD Mayo<br />
Clinic Florida, Jacksonville, FL, USA<br />
Introduction: The use of mesh to potentiate the hiatal closure during<br />
laparoscopic foregut surgery is increasing among surgeons, as some<br />
consider this the standard of care. Our objective is to evaluate the<br />
incidence of mesh removal during revisional foregut surgery and to<br />
examine the complications that can arise from the use of mesh near the<br />
esophageal hiatus. Our objective is to compare indications for surgery<br />
and perioperative outcomes between those patients with and without<br />
prior mesh hiatoplasty.<br />
Methods and Procedures: Our design is an IRB-approved retrospective<br />
cohort study from a single tertiary-care referral center. Between<br />
December 2006 and September 2009, sixty-nine (69) patients underwent<br />
revisional foregut surgery at the esophageal hiatus. Patients undergoing<br />
planned operations for obesity or achalasia were excluded from analysis.<br />
Of these sixty-nine (69) patients, ten (10) had previous hiatal mesh (PHM).<br />
Results: The patients in each group were similar with regard to age<br />
(range 17-76 yrs), BMI (range 17.7-48.1), and ASA (median 3). PHM and<br />
NM patients had similar rates (70% and 68%, respectively) and types<br />
of anatomic failure (misplaced, slipped, herniated and/or twisted<br />
fundoplication). There was no statistically significant difference in<br />
outcomes between PHM and NM patients with regard to estimated<br />
blood loss (430 cc vs. 105 cc, p=0.09), operative time (4.19 hrs vs. 2.74 hrs,<br />
p=0.07), blood transfusion (1.1 units vs. 0.2 units, p=0.29), or length of stay<br />
(6.2 days vs. 3.2 days, p=0.16). Of the ten PHM patients, four required a<br />
major resection with anastomosis, whereas only four of 59 required such a<br />
resection in the NM group. Therefore, the relative risk of requiring a major<br />
resection is 5.9 times as high in PHM patients as compared to NM patients<br />
(95% CI = 1.754, 19.84; p=0.01). The rate of major resection was similar<br />
between those patients with biological and permanent mesh.<br />
Conclusions: Our study demonstrates that the presence of mesh at<br />
the esophageal hiatus is associated with an increased risk of requiring<br />
a major resection during a revisional procedure. The pattern of failure<br />
was not different in patients with hiatal mesh, suggesting that the use of<br />
mesh at initial repair does not eliminate the potential need for revisional<br />
operation. Thus, when performing an initial hiatal hernia repair, the risk of<br />
increased hiatal hernia recurrence if not using mesh should be weighed<br />
against the potential risk of a subsequent major resection if using mesh.<br />
S046<br />
SAFETY, EFFICACY AND COST-EFFECTIVENESS OF COMMON<br />
LAPAROSCOPIC PROCEDURES Manish M Tiwari, MD PhD MPH, Jason<br />
F Reynoso, MD, Albert W Tsang, MD, Dmitry Oleynikov, MD FACS<br />
Department of Surgery, University of Nebraska Medical Center, Omaha,<br />
NE<br />
Introduction: Although several single-center studies on the outcomes of<br />
laparoscopic surgery have shown better surgical outcomes, a large multicenter<br />
study on outcomes of common laparoscopic surgical procedures<br />
has not been performed. The objective of this study was to retrospectively<br />
examine multi-center outcomes of common laparoscopic procedures.<br />
Methods: The University HealthSystem Consortium (UHC) is an alliance<br />
of more than 100 academic medical centers and nearly 200 affiliate<br />
hospitals. UHC’s Clinical Data Base / Resource Manager (CDB/RM) allows<br />
member hospitals to compare patient-level risk-adjusted outcomes<br />
for performance improvement purposes. This study is a multi-center,<br />
retrospective analysis of the outcomes of common surgical procedures<br />
using the UHC database. Three-year discharge data from the UHC<br />
database was accessed using International Classification of Diseases (ICD-<br />
9) codes for commonly performed surgical procedures between January<br />
2006 and December 2008. Discharge data on six common open (O) and<br />
laparoscopic (L) surgical procedures, including cholecystectomy (C),<br />
appendectomy (A), reflux surgery (RS), gastric bypass (GB), ventral hernia<br />
repair (VHR) and colectomy (CO) was collected. Main outcome measures<br />
analyzed were mortality, morbidity, 30-day readmission, intensive care<br />
unit (ICU) admission, length of ICU stay, overall length of hospital stay and<br />
costs.<br />
Results: A total of 207,984 patients underwent either open or<br />
laparoscopic surgery for one of the six surgical procedures included in<br />
the study. Lower mortality index, reduced length of stay and reduced<br />
costs were observed with laparoscopic procedures compared to open<br />
procedures. Patients in the laparoscopic group had lower mortality index<br />
(0.82 for LC vs. 1.01 for OC; 0.82 for LA vs. 0.85 for OA; 0.23 for LRS vs. 0.72<br />
for ORS; 0.68 for LGB vs. 0.95 for OGB; 0.00 for LVHR vs. 0.89 for OVHR;<br />
0.61 for LCO vs. 1.16 for OCO). Laparoscopic group showed significantly<br />
reduced length of stay (in days) for all six procedures (3.89 for LC vs. 10.11<br />
for OC; 2.26 for LA vs. 4.26 for OA; 2.94 for LRS vs. 7.38 for ORS; 2.62 for<br />
LGB vs. 5.95 for OGB; 3.71 for LVHR vs. 7.89 for OVHR; 7.13 for LCO vs.<br />
13.12 for OCO; p
Scientific Session Oral Abstracts<br />
S048<br />
MINILAPROTOMY APPROACH TO PERFORATED DUODENAL ULCER<br />
Tomonori Ohsawa, MD, Toru Ishiguro, MD, Norimichi Okada, MD, Keiichiro<br />
Ishibashi, phD, Norihiro Haga, PhD, Hideyuki Ishida, PhD Department of<br />
Digestive Tract and General Surgery, Saitama Medical Center, Saitama<br />
Medical Schoo<br />
Background and Purpose: Although the technical feasibility of<br />
laparoscopic approach to perforated duodenal ulcer is well established,<br />
this procedure has not been widely performed because of several<br />
limitations. This retrospective study was performed to clarify the<br />
feasibility, safety, and minimal invasiveness of a minilaparotomy for<br />
perforated duodenal ulcer. Patients and Methods: We retrospectively<br />
analyzed data on 40 patients with perforated duodenal ulcer, who<br />
were attempted to undergo simple closure and/or omentopexy via<br />
minilaparotomy (skin incision,
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
design was employed with subjects performing the task for 20 seconds<br />
followed by 30 seconds rest, repeated 5 times. Accuracy was determined<br />
by the distance from the tool tip to the target.<br />
Results: 21 right-handed novices completed the task with and<br />
without GCMC. Subjects were more accurate with GCMC assistance<br />
versus unassisted performance (p=0.008). Greater changes in cortical<br />
haemodynamics were observed with GCMC, with 8 fNIRS channels<br />
demonstrating statistically significant activity (?=5%) compared to zero<br />
channels without GCMC. The activation occurred in the medial prefrontal<br />
cortex.<br />
Conclusion: It has been demonstrated that GCMC enhances novice<br />
performance and that this requires greater medial prefrontal cortical<br />
activity. It is possible that in using GCMC, the user focussed more on<br />
the quality and accuracy of movement. In order to achieve this, the<br />
medial prefrontal cortex which is involved in performance monitoring,<br />
is recruited to a greater extent. This work demonstrates how changes<br />
in brain behaviour can be used to assess the impact of novel surgical<br />
technology.<br />
1 - Mylonas G.P. et al. MICCAI. 2008: 11, 676-683<br />
2 - Parasuraman R. Theoretical Issues in Ergonomics Science. 2003 4, 5-20<br />
S051<br />
ROBOTIC GASTRIC BYPASS: THE FUTURE OF BARIATRIC SURGERY?<br />
Chan W Park, MD, Edward Lam, BS, Cedric Lorenzo, MD, Kenric Murayama,<br />
MD, Racquel Bueno, MD University of Hawaii, Queen’s Medical Center<br />
Objective: Compare robotic versus laparoscopic roux-en-Y gastric bypass<br />
(RYGB) for the treatment of morbid obesity in a community hospital.<br />
Introduction: Since receiving Food and Drug Administration approval<br />
in 2000, surgery utilizing a robot (da Vinci® Surgical System) has been<br />
successfully performed in numerous procedures including RYGB.<br />
However, despite the proven safety profile, reported lower complication<br />
rates, and technical benefits of robotic surgery, only a few of the over 200<br />
robotic surgery centers in the United States have consistently applied this<br />
technology to RYGB. In addition, there are limited studies with relatively<br />
small sample sizes that have compared robotic vs. laparoscopic RYGB in<br />
the literature.<br />
Methods: Through a retrospective analysis of a prospectively collected<br />
database, we compared outcomes and complication rates of robotic vs.<br />
laparoscopic RYGB in the treatment of morbid obesity. All patients who<br />
underwent robotic RYGB performed through the Comprehensive Weight<br />
Management <strong>Program</strong> of Queen’s Medical Center (Honolulu, HI) between<br />
December 2006 to July 2009 were compared to a matched cohort of<br />
patients who received laparoscopic RYGB during the same study period.<br />
Outcomes data included weight loss, operative times, and hospital length<br />
of stay. All complications encountered by both groups were reported.<br />
Results: Eighty patients who underwent robotic RYGB were compared<br />
to 80 patients who received laparoscopic RYGB. Rate of weight loss and<br />
reduction in body mass index (BMI) over time were similar in both groups.<br />
There were no mortalities in either group. The robotic group experience a<br />
12.5% complication rate. Robotic complications included post-operative<br />
anemia (2 patients), marginal ulcer (2 patients), anastomotic stricture (4<br />
patients), and anastomotic leaks (2 patients). The laparoscopic group also<br />
experienced a 12.5% complication rate for a range of issues including<br />
wound infections (2 patients), anastomotic stricture/ulcer (2 patients),<br />
aspiration pneuomonia (1 patient), anastomotic leak (1 patient) requiring<br />
re-operation, small bowel obstruction (1 patient), etc. Hospital length<br />
of stay and operative times were similar in both groups, but there was a<br />
trend towards a shorter length of stay with robotic RYGB.<br />
female/<br />
male<br />
age<br />
(range)<br />
BMI<br />
(range)<br />
Robotic 59/21 44 (21-69)<br />
46.4 (33-<br />
75)<br />
Laparoscopic 52/28 44 (20-64)<br />
49 (35-<br />
87)<br />
Operative<br />
time<br />
length<br />
of stay<br />
174 2.9<br />
minutes days<br />
164 3.1<br />
minutes days<br />
complications<br />
12.5%<br />
12.5%<br />
Conclusion: Robotic RYGB is a safe and effective procedure for the<br />
surgical treatment of morbid obesity, and this approach can be utilized<br />
12 th World Congress of Endoscopic Surgery 116<br />
effectively in a community hospital setting. Robotic RYGB resulted in the<br />
same overall complication rate as the laparoscopic approach with a trend<br />
towards a shorter length of stay. Operative times decreased after the<br />
initial few robotic RYGB, and this may be due to a more favorable learning<br />
curve for robotic RYGB. Future studies comparing actual cost comparisons<br />
and analysis of outcomes are needed.<br />
S052<br />
A COMPARISON OF SHORT-TERM OUTCOMES FOR OPEN,<br />
LAPAROSCOPIC, AND ROBOT-ASSISTED RECTAL RESECTION FOR<br />
CANCER Gyu-Seog Choi, MD, Jun Seok Park, MD, Kyoung Hoon Lim, MD,<br />
You Seok Jang, MD, Soo Han Jun, MD Department of Surgery, School of<br />
Medicine, Kyungpook National University, Daegu, Korea<br />
Introduction: In recent years, robotic-assisted surgery using the da Vinci<br />
System ® has been proposed as an alternative to the traditional open or<br />
laparoscopic procedures. The aim of this study was to compare the shortterm<br />
outcomes for open, laparoscopic, and robot-assisted rectal resection<br />
for cancer.<br />
Methods: Two hundred sixty-three patients with rectal cancer who<br />
underwent curative resection between 2007 and 2009 were included.<br />
Patients were divided into an open surgery group (OPEN, n = 88), a<br />
laparoscopic surgery group (LAP, n = 123) and a robot-assisted group<br />
(ROBOT, n = 52). Data include operative time, length of recovery,<br />
methods of specimen extraction, quality of total mesorectal excision, and<br />
morbidity.<br />
Results: The mean operation time was 233.8 ± 59.2 for OPEN group,<br />
158.0 ± 49.2 for LAP group and 232.6 ± 52.4 for Robot group (p < 0.001).<br />
Patients from the LAP group and ROBOT group recovered significantly<br />
faster than those from the OPEN group (p < 0.05). The proportion of cases<br />
done by natural orifice surgery-intracorporeal anastomosis with transanal<br />
or transvaginal retrieval of specimens-were significantly higher in the<br />
ROBOT group (p < 0.001). There were no differences in specimen quality<br />
among the three groups, with distal resection margin, harvested lymph<br />
node, and circumferential margin. The overall complication rate in OPEN,<br />
LAP, and ROBT group were 20.5, 11.4, and 19.2% (p = 0.160).<br />
Conclusions: Robot-assisted rectal resection is equivalent to open and<br />
laparoscopy approach with respect to short-term outcomes. Furthermore,<br />
the technical advantages of robot surgical system are helpful to adopt a<br />
method of natural orifice surgery.<br />
S053<br />
MULTI-FUNCTIONAL ROBOT FOR LAPAROENDOSCOPIC SINGLE-SITE<br />
SURGERY Amy C Lehman, MS, Tyler D Wortman, BS, Kyle W Strabala, MS,<br />
Nathan A Wood, MS, Manish M Tiwari, MD, Matthew R Goede, MD, Shane<br />
M Farritor, PhD, Dmitry Oleynikov, MD University of Nebraska-Lincoln,<br />
University of Nebraska Medical Center<br />
Introduction: This study demonstrates the effectiveness of using a multifunctional<br />
miniature in vivo robot to perform complex tasks, such as<br />
intracorporeal suturing, through a single incision. Existing technologies<br />
for Laparoendoscopic Single-Site Surgery (LESS), such as articulating,<br />
bent, and flexible instrumentation, are limited in visualization and tissue<br />
manipulation capabilities by multiple tools working through a single<br />
access point. A robotic platform that is completely inserted into the<br />
peritoneal cavity through a single incision mitigates these constraints and<br />
provides a more intuitive approach than standard LESS methods.<br />
Methods: A robotic platform consisting of a miniature in vivo robot and<br />
a remote surgeon interface has been designed and built. The basic robot<br />
design consists of two arms each connected to a central body. The body<br />
of the robot contains a mounting assembly and a maneuverable camera<br />
pair that provides images to the remote surgeon interface. The robot arms<br />
have two degree-of freedom rotational shoulder and elbow joints. Each<br />
forearm is fitted with specialized grasper or cautery end effectors. These<br />
end effector tools can be interchanged depending on the particular task<br />
being performed. For example, when performing a cholecystectomy, the<br />
robot forearms are fitted with standard cautery and grasper end effectors.<br />
Then, for performing intracorporeal suturing, laparoscopic needle holders<br />
are used in place of the cautery and grasper end effectors. The surgeon
Scientific Session Oral Abstracts<br />
interface, located remotely within the operating room, consists of a<br />
monitor, a foot pedal for locking and clutching, and two PHANTOM Omni®<br />
(SensAble, Woburn, MA) devices for manipulation of the robot arms.<br />
Results: This robot has been demonstrated in multiple non-survival<br />
procedures in a porcine model, including three cholecystectomies.<br />
All procedures were performed at the University of Nebraska Medical<br />
Center with experimental protocols approved by the institutional review<br />
committee. For each procedure, the robot was inserted and then mated<br />
with a mounting rod that was advanced through the insertion incision.<br />
This rod was used with an external supporting assembly mounted<br />
to the rails of the operating table. The surgeon at the user interface<br />
manipulated the robot to perform the cholecystectomy, with stapling<br />
of the cystic duct and supplementary retraction being performed with<br />
standard laparoscopic tools that were advanced into the peritoneal cavity<br />
through the incision. At completion of the cholecystectomy, the robot<br />
was removed from the peritoneal cavity and then fitted with needle<br />
holder end effectors. The robot was then reintroduced into the peritoneal<br />
cavity to successfully perform intracorporeal suturing of the bowel. Also,<br />
students performed benchtop tasks using both the robot platform and<br />
standard LESS. The results showed that the tasks were performed faster<br />
and more accurately using the robot.<br />
Conclusions: The widespread adoption of NOTES and LESS for complex<br />
surgeries is dependent on the development of devices that provide<br />
a stable multi-tasking platform. A multi-functional robot provides a<br />
completely insertable platform that addresses the triangulation and<br />
visualization limitations of existing instrumentation for LESS. The two<br />
degree-of-freedom rotational elbow joint enhanced surgical dexterity and<br />
enabled the performance of the complex surgical task of intracorporeal<br />
suturing with access through a single incision.<br />
S054<br />
ROBOTIC VS. CONVENTIONAL LAPAROSCOPIC GASTRIC BANDING: A<br />
COMPARISON OF 407 CASES Paula K Edelson, BSc, Kristoffel R Dumon,<br />
MD, Seema S Sonnad, PhD, Bilal M Shafi, MD, Noel N Williams, MD Bariatric<br />
Surgery <strong>Program</strong>, Deptartment of Surgery, University of Pennsylvania<br />
School of Medicine<br />
INTRODUCTION: The current indications and rationale for using a<br />
robotic technique in bariatric surgery, specifically gastric banding,<br />
remain unclear. The objective of this study was to quantify the safety and<br />
potential benefits of this novel technology in the context of both patient<br />
and surgeon outcomes as compared to the conventional laparoscopic<br />
approach.<br />
METHODS AND PROCEDURES: A retrospective database of obese<br />
patients undergoing laparoscopic gastric banding (LGB) between<br />
December 2006 and June 2009 was examined. During this period<br />
407 consecutive patients underwent LGB: 287 robotically and 120<br />
conventionally. The procedures were performed by two primary surgeons<br />
in a teaching hospital setting. The conventional laparoscopic approach<br />
had been practiced since 2004, and the robotic approach had been<br />
practiced since 2006. Patient demographics, operative complications,<br />
operating times, and clinical outcomes were examined.<br />
RESULTS: The patients in the robotic and conventional cohorts did not<br />
vary significantly in demographic composition. The robotic cohort had<br />
a mean age of 47 ± 25 years, was 230/287 (80.1%) female and 57/287<br />
(19.9%) male and had a mean pre-operative Body Mass Index (BMI) of<br />
45.4 kg/m². The conventional cohort had a mean age of 45 ± 24 years,<br />
was 89/120 (74.2%) female and 31/120 (25.8%) male, and had a mean<br />
pre-operative BMI of 45.1 kg/m². The prevalence of pre-operative comorbidities<br />
was similar between the two groups: hypertension was 56%<br />
and 67%, hypercholesterolemia was 29% and 33%, sleep apnea was<br />
54% and 52%, diabetes mellitus was 28% and 33%, and osteoarthritis<br />
was 41% and 29% in the robotic and conventional cohorts respectively.<br />
The rates of intra-operative and post-operative complications did not<br />
differ significantly between the two approaches (Table 1). The length of<br />
post-operative hospital stay did not differ significantly between the two<br />
approaches (1.3 ± 2.7 days for both approaches). The operating time<br />
from incision to wound closure did not differ significantly between the<br />
two approaches (91.5 minutes vs. 92.1 minutes robotic and conventional<br />
respectively). However, for patients with a pre-operative BMI of ≥ 50 kg/<br />
m² (N = 89: 64 robotic, 25 conventional), the operating time is significantly<br />
lower using the robotic approach (91.3 ± 63.7 minutes, SD = 19.7 vs. 101.3<br />
± 49.7 minutes, SD = 23.7; p=0.04).<br />
CONCLUSIONS: In this series, robotic and conventional approaches were<br />
similar in intra-operative or post-operative complication rates, operating<br />
time, and length of post-op hospital stay. However, for patients with a<br />
pre-operative BMI of ≥ 50 kg/m², the operating time is significantly lower<br />
using the robotic approach despite the adoption of the new technique.<br />
These data suggest that the robotic approach is at least as safe as<br />
conventional laparoscopic approach, and that robotic approach should<br />
be considered for gastric banding candidates with BMI ≥ 50 kg/m².<br />
Table 1: Complications of robotic vs. conventional approaches<br />
Complication<br />
Robot (N=287)<br />
Conventional<br />
(N=119)<br />
Conversion to open 0 1<br />
Reoperation: Band removal or replacement 9 3<br />
Port removal or replacement 2 2<br />
Band slippage 8 3<br />
GI complaints not resulting in admission 28 10<br />
S055<br />
PROPHYLACTIC INFERIOR VENA CAVA FILTERS IN HIGH-RISK<br />
BARIATRIC SURGERY Khashayar Vaziri, MD, John D Watson, BS, Amy P<br />
Harper, MSN ACNPBC, Juliet Lee, MD, Fred Brody, MD, Shawn Sarin, MD,<br />
Elizabeth A Ignacio, MD, Albert Chun, MD, Anthony C Venbrux, MD, Paul P<br />
Lin, MD The George Washington University Medical Center<br />
Objective: High-risk patients are at significant risk for venous<br />
thromboembolism (VTE) and may benefit from the addition of retrievable<br />
inferior vena cava filters (rIVCF) to chemoprophylaxis. However, the<br />
optimal VTE prophylaxis has not been established in morbidly obese<br />
patients undergoing bariatric surgery. This observational study examines<br />
the use of rIVCFs in combination with chemoprophylaxis for high-risk<br />
bariatric surgery patients.<br />
Methods: A retrospective review was performed of all high-risk morbidly<br />
obese patients who underwent bariatric surgery between February 2007<br />
and July 2009. Patients were considered high-risk for the development of<br />
a peri-operative VTE if they had a prior history of VTE, a BMI ≥ 55 kg/m2,<br />
were severely immobile, or had preexisting hypercoaguable condition.<br />
All patients underwent a preoperative venous duplex study. RIVCF<br />
placement was performed preoperatively on the day of the bariatric<br />
procedure. Standard chemoprophylaxis was initiated preoperatively and<br />
continued throughout the hospital stay. Clinical, demographic, operative<br />
and postoperative data were recorded. A venogram was performed prior<br />
to removal of the rIVCFs.<br />
Results: Forty-four patients (12 men and 32 women) with a mean age<br />
of 47.9 ± 12.1 years and a mean BMI of 58 ± 9.5 kg/m2 underwent<br />
roux-en-y gastric bypass with concomitant rIVCF placement. Mean<br />
follow up was 184 days. One patient (2.3%) was found to have a deep<br />
venous thrombosis (DVT) on preoperative venous duplex. All patients<br />
received VTE chemoprophylaxis preoperatively and successful rIVCF<br />
placement. Indications for rIVCF placement were BMI (68%), history<br />
117 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
of prior VTE (30%), and/or severe immobility (2%). The operation<br />
was performed laparoscopically in 41 patients (93%). Three patients<br />
(two revisional surgeries and one conversion secondary to intestinal<br />
adhesions) underwent open gastric bypass. The mean operative time<br />
was 111.1 ± 30.2 minutes and the mean length of stay was 3.2 ± 1.2<br />
days. A postoperative venous duplex for the clinical suspicion of VTE was<br />
performed in four patients (9%), of which 2 were positive for the presence<br />
of a DVT. Retrieval was successful in 25 patients (57%). A venogram was<br />
performed prior to removal of each rIVCF. No significant thrombus was<br />
found, however, one filter had migrated to the right common iliac vein.<br />
Overall, there were two complications of rIVCF placement (4.5%), one<br />
during insertion and the other due to migration. One mortality (2%)<br />
occurred as the result of an arrhythmia; no pulmonary emboli were found.<br />
Conclusions: This study documents that rIVCFs in high-risk bariatric<br />
surgery patients is associated with a low incidence of DVT (4.5%) and<br />
filter-related complications (4.5%) without pulmonary emboli. However, a<br />
significant portion of patients continue to have their filters in place. Long<br />
term effects of rIVCFs in patients who do not undergo retrieval are largely<br />
unknown. These long term effects need further investigation in order to<br />
appreciate the true benefit of rIVCFs in this patient population.<br />
S056<br />
B-TYPE NATRIURETIC PEPTIDE INCREASES AFTER GASTRIC BYPASS<br />
AND CORRELATES TO WEIGHT LOSS Eric Changchien, MD, Gavitt A<br />
Woodard, BS, Tina H Boussard, PhD, John M Morton, MD MPH Stanford<br />
University<br />
Background: B-type natriuretic peptide (BNP) is a recognized serologic<br />
marker of heart failure and has been associated with cachexia of heart<br />
failure. In addition, BNP is positively correlated to adiponectin which is<br />
inversely correlated to weight gain. We are aware that gastric bypass leads<br />
to early satiety and increases in adiponectin. Our study hypothesis is that<br />
surgically induced weight loss will lead to an increase in BNP.<br />
Methods: At a single academic institution (2008-2009), we measured<br />
BNP in 100 consecutive gastric bypass patients preoperatively and at 12<br />
months postoperatively. All RNYGB surgeries were performed by a single<br />
surgeon with a 30cc pouch and a 100cm Roux limb. Post-operatively, all<br />
patients discontinued diuretics and statins. Weights and BNP levels were<br />
measured pre-op and at 3, 6 and 12 months and compared by a paired<br />
t-test of equal variance.<br />
Results: Preoperatively, patients were representative of a bariatric surgery<br />
population with an average BMI 47, age 43, % female (82), % history of<br />
coronary artery disease (5), % hypertension (56), % diabetes (37) and %<br />
Sleep Apnea (41). At 12 months post-op, patients had lost 86% of their<br />
excess weight. There were significant increases in BNP from pre-op (57)<br />
to post–op: 3 months (87) to 6 months (84) to 12 months (119). These<br />
increases in BNP correlated to post-operative weight loss.<br />
Conclusion: This novel study demonstrates that surgically induced<br />
weight loss leads to increases in B-type natriuretic peptide correlating to<br />
weight loss. This correlation of BNP and weight loss may potentially serve<br />
as an additional marker and mechanism for satiety.<br />
S057<br />
LAGB WITH TRUNCAL VAGOTOMY: ANY INCREASED WEIGHT LOSS?<br />
Kristen R Earle, MD, Matt B Martin, MD Moses H. Cone Hospital Systems,<br />
Central Carolina Surgery, PA<br />
Objective: Does truncal vagotomy enhance weight loss when combined<br />
with LAGB? Laparoscopic adjustable gastric banding (LAGB) causes<br />
weight loss primarily through a mechanical restrictive mechanism.<br />
The vagus nerve provides connections between the brain and the<br />
gut through afferent and hormonal signals that regulate fullness and<br />
satiation. Published studies demonstrate clinically significant weight loss<br />
in subjects undergoing open surgical truncal vagotomy for ulcer disease<br />
and morbid obesity. The primary objectives of this study were to evaluate<br />
the safety and efficacy of adding truncal vagotomy to LAGB and compare<br />
weight loss to LAGB alone.<br />
Methods: This open-label case controlled study was conducted at Central<br />
Carolina Surgery, PA, a private surgery practice in Greensboro, NC. Since<br />
May 2006, 47 subjects with Class II and III obesity underwent LAGB with<br />
12 th World Congress of Endoscopic Surgery 118<br />
truncal vagotomy. The anterior and posterior nerves were divided and<br />
resected just below the diaphragm and sent to pathology. The primary<br />
safety variable was the number of procedure-related adverse events. The<br />
primary efficacy variable was the percent excess weight loss (%EWL).<br />
Completeness of vagotomy was assessed by direct inspection, pathology<br />
confirmation and endoscopic Congo red testing after intravenous<br />
Baclofen stimulation. 47 cohorts who were matched for age, sex, and<br />
preop BMI were used for the ongoing comparison.<br />
Results: The average enrollment BMI was 45 and average age was 46.<br />
There were no intra-operative or unanticipated adverse events. All<br />
subjects were discharged in ≤ 24 hours. There was one case of incomplete<br />
vagotomy confirmed via pathology. The LAGB/Vagotomy group had an<br />
average 34.8 % excess weight loss at an average 17 months post op. The<br />
cohort group had an average weight loss of 38.5% of excess body weight<br />
at an average 21 months postop. All of the LAGB/vagotomy patients<br />
reported an absence of hunger; no diarrhea, gastric outlet obstruction, or<br />
dumping was seen.<br />
Conclusions: This data does not support the hypothesis that vagotomy<br />
when added to LAGB augments weight loss. None of the vagtomy<br />
patients had any of the complications usually attibuted to vagotomy<br />
without drainage.<br />
S058<br />
NUTRITIONAL EFFECT OF ORAL SUPPLEMENT ENRICHED IN BETA-<br />
HYDROXY-BETA -METHYLBUTYRATE, GLUTAMINE AND ARGININE ON<br />
RESTING METABOLIC RATE AFTER LAPAROSCOPIC GASTRIC BYPASS. R<br />
H Clements, MD, N Saraf, MPH, M Kakade, MPH, M White, RN, J Hackett, RN<br />
Division of Gastrointestinal Surgery, University of Alabama at Birmingham,<br />
AL<br />
Objective- To evaluate the nutritional effect of an oral supplement<br />
enriched in beta-hydroxy-beta-methylbutyrate, glutamine and arginine<br />
(HMB/Glu/Arg) on resting metabolic rate (RMR) following laparoscopic<br />
gastric bypass (LGB). Although, LGB is a highly effective approach to<br />
induce weight loss in morbid obesity, most patients regain 10-15% of this<br />
weight over time. Studies indicate, this is due to a decrease in RMR which<br />
is largely determined by loss in lean body mass (LBM) after LGB. There is<br />
evidence that HMB/Glu/Arg helps restore LBM in cachexia due to cancer<br />
and critically ill trauma patients. If this effect can help modulate RMR in<br />
bariatric patients, more stable weight maintenance may be achieved.<br />
Method- Patients scheduled to undergo LGB were randomized to an<br />
experimental arm receiving (HMB/Glu/Arg) and to a control arm not<br />
receiving it. The experimental group was required to consume 24g of<br />
supplement dissolved in water, twice daily and record their consumption.<br />
Primary outcomes of interest included weight loss, LBM determined<br />
by double emission x-ray aborptiometry (DXA) and RMR measured by<br />
indirect calorimetry. These were assessed at baseline, 2 and 8 week<br />
intervals.<br />
Results- 27 morbidly obese patients with mean age 46 + 8.5 years (78%<br />
Whites, 22% African Americans, 96% females) and mean BMI 43.2 +4.1 kg/<br />
m2 were enrolled. Paired t test was used to compare means in all subjects<br />
(N=27) and the results are depicted in the table below.<br />
Variable Baseline 8 week Change p value<br />
Weight(kg) 112.7 +11.8 96.8 +12.0 - 15.7 +2.6
Scientific Session Oral Abstracts<br />
Conclusion- There was a significant decrease in weight, BMI, LBM and<br />
RMR in all subjects after LGB, and these changes were not affected by the<br />
use of supplement. Potential preservation of LBM as a result of HMB/Glu/<br />
Arg requires further investigation. Its consumption (78cal/serving) did not<br />
adversely affect weight loss in the experimental group.<br />
S059<br />
DETERMINANTS OF RESOURCE UTILIZATION IN LAPAROSCOPIC<br />
ROUX-EN-Y GASTRIC BYPASS: A MULTICENTER ANALYSIS OF 6322<br />
PATIENTS Prateek K Gupta, MD, Himani Gupta, MD, Weldon J Miller, MS,<br />
Robert A Forse, MD PhD Creighton University Medical Center<br />
Objective: Treatment of chronic diseases such as obesity by resource<br />
intensive therapy such as Laparoscopic Roux-en-Y Gastric Bypass surgery<br />
(LRYGB) is associated with early increases in healthcare costs. With the<br />
increasing frequency of LRYGB being performed and the rising cost of<br />
health care, preoperative optimization may reduce resource utilization<br />
and these early costs. We sought to investigate the independent<br />
contributions of modifiable and non-modifiable factors to resource<br />
utilization in LRYGB.<br />
Methods: American College of Surgeons’ 2007 National Surgical Quality<br />
Improvement <strong>Program</strong> (NSQIP) database was used. 6322 patients of<br />
this multicenter (183 academic and private US hospitals participating),<br />
prospective database who underwent LRYGB were studied. Resource<br />
variables were operative time (OT), hospital length of stay (LOS), as<br />
well as occurrence of 17 postoperative complications comprising of<br />
wound infection, organ space infection, wound dehiscence, pneumonia,<br />
reintubation, on ventilator > 48 hours, pulmonary embolus, deep venous<br />
thrombosis, renal insufficiency, renal failure, stroke, coma, cardiac<br />
arrest, myocardial infarction, bleeding, sepsis and return to operating<br />
room. Bivariable and multivariable linear and logistic regressions were<br />
performed.<br />
Results: Mean age was 44.2±11.2 years. Mean BMI was 49.3±8.6.<br />
Male:female ratio was 1212:5126. Mean LOS was 2.59±2.88 days. Mean<br />
OT was 139.3±55.9 minutes. Being a male increased OT by 7.8 minutes<br />
(p
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
and after IVGTT . These changes are independent from the food passage<br />
through the gastro-intestinal tract or weight loss. The Ghrelin and GLP-1<br />
changes seem to be directly related to the fundus ablation.<br />
S062<br />
OUTCOMES OF LAPAROSCOPIC ROUX-EN-Y GASTRIC BYPASS AS A<br />
PRIMARY VERSUS REVISIONAL BARIATRIC SURGERY. Balaji Jangam,<br />
MD, Kristine M O’Hara, MD, Bruce Bernstein, PhD, Ravi Chhatrala, MD,<br />
Ioannis Raftopoulos, MD PhD FACS Bariatric Center at Saint Francis<br />
Hospital and Medical Center, Hartford, CT.<br />
BACKGROUND: The purpose of this study was to compare the outcomes<br />
of laparoscopic Roux-en-Y gastric bypass (LRYGB) as a primary (CG) versus<br />
revisional bariatric surgery (RBS).<br />
METHODS: Data of 514 consecutive patients who underwent LRYGB by<br />
one surgeon between August 2004 and June 2009 as primary (n=481,<br />
93.6%) or RBS (n=33, 6.4%) were compared. Collected data included age,<br />
body mass index (BMI), operative time (OT), length of hospital stay (LOS),<br />
conversion to open surgery, early (< 30 days), or late (> 30 days) major<br />
complications, % excess weight loss (%EWL), status of comorbidities<br />
including hypertension (HTN), diabetes (DM), gastro-esophageal reflux<br />
disease (GERD), obstructive sleep apnea (OSA) and dyslipidemia, as well<br />
as score change of SF-36 quality of life (QoL) questionnaire. Indications<br />
for RBS included inadequate weight loss (n=13), intractable GERD (n=12),<br />
weight regain (n=10), abdominal pain (n=6), intractable or perforated<br />
ulcer (n=3), and anastomotic stricture (n=1). RBS procedures included:<br />
1) conversion to Roux-en-Y gastric bypass of jejuno-ileal bypass (n=2),<br />
adjustable gastric band (n=5), sleeve gastrectomy (n=1), vertical<br />
banded gastroplasty (n=8), Nissen fundoplication (n=4), 2) revision of<br />
gastrojejunostomy (n=8), 3) Roux limb lengthening (n=5), 4) resection<br />
of Roux limb blind loop end (n=2) and 5) revision of gastric pouch (n=1).<br />
Differences in continuous and categorical variables between groups were<br />
explored with analysis of covariance (ANCOVA) and multinomial logistic<br />
regression respectively, both models adjusting for BMI, age and gender. P<br />
< 0.05 was considered significant.<br />
RESULTS: There was a significant difference between CG and RBS groups<br />
in relation to BMI (47.2 vs. 38.6 Kg/m2, p
Scientific Session Oral Abstracts<br />
Conclusion: Evaluation of the esophageal hiatus revealed that patients<br />
with Type III PEH have a different biologic environment in regards to<br />
collagen resulting in a higher collagen ratio (I/III) compared to control<br />
patients. Collagen Deficiency in the GE junction supporting ligaments<br />
does not appear to be an etiology of PEH formation.<br />
S065<br />
IN VIVO FLUORESCENCE IMAGING OF STAPHYLOCOCCUS AUREUS<br />
BIOLOGIC MESH INFECTION - A 30 DAY ANALYSIS Karem C Harth,<br />
MD MHS, Ann-Marie Broome, PhD, Michael R Jacobs, MD PhD, Jeffrey A<br />
Blatnik, MD, Michael J Rosen, MD University Hospitals Case Medical Center<br />
BACKGROUND: Infection in the setting of hernia repair poses a difficult<br />
challenge, and biologic mesh might perform favorably in this setting.<br />
The specific response of different biologic mesh constructs to infection is<br />
unclear. Using fluorescent-labeled bacteria and innovative in vivo imaging<br />
quantitative bacterial analysis, we evaluated the response of two biologic<br />
mesh prosthetics to staphylococcus aureus infection.<br />
METHODS: Twenty-four rats underwent creation of a chronic hernia.<br />
They were randomly assigned to underlay bridge repair with Permacol<br />
(cross linked porcine dermis) (n=12) or Surgisis (noncrosslinked porcine<br />
submucosa) (n=12). Half in each group were repaired in sterile fashion<br />
(clean cases; n=6) and half were inoculated with 10 4 CFU/ml of a clinical<br />
strain of green fluorescent protein (GFP) labeled Staphylococcus aureus<br />
(SA) (clean contaminated cases; n=6). Animals were allowed to survive<br />
30-days, euthanized and the explanted abdominal wall underwent<br />
immediate in vivo fluorescent imaging. A 6mm punch biopsy of both<br />
tissue and mesh was obtained after imaging. This was followed by<br />
homogenizing, serial diluting, plating in blood agar dishes, incubation<br />
for 24 hours at 37° C and CFU/gm estimates. Validation of our imaging<br />
was performed by in vitro fluorescence imaging of serial concentrations<br />
of GFP SA (10 3 – 10 8 CFU/ml) to determine the minimal level of GFP signal<br />
detection. Fisher’s exact statistic was performed.<br />
RESULTS: All animals survived 30 days following repair. CLEAN CASES:<br />
Culture results for both clean groups did not reveal evidence of infection<br />
(0 CFU/gm). CLEAN CONTAMINATED CASES: One of six (17%) Permacol<br />
animals had residual GFP SA infection (8 x 10 2 CFU/gm; n=1) while the<br />
remainder had no GFP SA (0 CFU/gm; n=5). Three of six (50%) Surgisis<br />
animals had residual GFP SA infection (1.3 x 10 2 CFU/gm; n=3) while the<br />
others had no detectable GFP SA infection (p-value = 0.55). IMAGING:<br />
In vivo imaging corroborated our low bacterial counts and was unable<br />
to detect presence of GFP SA or a difference in signal between clean<br />
contaminated cases of Permacol or Surgisis (0 RFU signal/group; n=12).<br />
IN VITRO VALIDATION: There was a positive linear correlation (R 2 = 0.9121;<br />
Y=715X+186) between imaging device signal and bacterial counts above<br />
a concentration of 10 5 CFU/ml. This was determined to be the lower limit<br />
of GFP SA detection with our in vivo fluorescence-imaging device.<br />
CONCLUSIONS: This study confirms that biologic mesh can tolerate clean<br />
contaminated situations. In these settings most animals were able to clear<br />
the bacterial contamination as demonstrated by low quantitative cultures<br />
and corroborated with in vivo fluorescent imaging. Further analysis as to<br />
the exact mechanism of bacterial clearance and biomechanical alterations<br />
of the mesh in infected fields is ongoing.<br />
S066<br />
FIBRIN GLUE FOR INTRAPERITONEAL LAPAROSCOPIC MESH<br />
FIXATION: A COMPARATIVE STUDY IN A SWINE MODEL Namir<br />
Katkhouda, MD, Tatyan Clarke, MD, Jeffrey Algra, MD, Bon C Cheng, BA,<br />
Rodney J Mason, MD, Maryam Balouch, BS, Helen J Sohn, MD, Ashkan<br />
Moazzez, MD, Jaisa Olasky, MD, Thomas V Berne, MD USC Keck School of<br />
Medicine, Department of Surgery, Los Angeles, CA, USA<br />
Introduction: A conventional method of mesh fixation in laparoscopic<br />
ventral hernia repair is transfascial sutures with tacks. This method has<br />
been associated with low recurrence rates, but yields significant morbidity<br />
from pain and bleeding. Fibrin glue has been used successfully in inguinal<br />
hernia repairs with decreased incidence of chronic pain without an<br />
increase in recurrence rates, but its utility is unknown for laparoscopic<br />
ventral hernia repairs. Our aim is to evaluate the efficacy of fibrin glue for<br />
laparoscopic mesh fixation to the anterior abdominal wall compared to<br />
other fixation methods.<br />
Methods and Procedures: Four different laparoscopic mesh fixation<br />
methods were randomly assigned to midline positions along the<br />
abdominal wall of 12 female pigs and compared: 1. fibrin glue only (GO),<br />
2. transfascial sutures with tacks (ST), 3. fibrin glue with tacks (GT), and<br />
4. tacks only (TO). At four weeks post-implantation, tensile strength,<br />
adhesions, migration, contraction, and buckling/folding were assessed<br />
using the Kruskal-Wallis one-way analysis by ranks test.<br />
Results: There were no significant differences in tensile strength,<br />
adhesions,<br />
or buckling/folding among the four fixation methods. A significant<br />
increase in mean migration (3.3 vs. 0.0mm, p=0.03) and percent<br />
contraction (28 vs. 14%, p=0.02) were identified in the GO group when<br />
compared to ST.<br />
GO GT TO ST p-value<br />
Tensile Stress<br />
N/m 2 x10 4 5.2 (1.8) 5.0 (2.0) 6.4 (2.2) 6.8 (1.3) NS<br />
mmHg 393 (132) 373 (149) 478 (165) 514 (99.0)<br />
Migration (mm) 3.3 (4.4) 0.8 (2.9) 0.4 (1.4) 0 p=0.03*<br />
Contraction (%) 28.0 (12.5) 18.9 (11.9) 17.2 (11.3) 14.2 (8.10) p=0.02*<br />
Buckling Score 0.42 (0.67) 0.75 (0.62) 0.58 (0.51) 0.50 (0.52) NS<br />
Adhesion Score 4.7 (4.0) 1.8 (3.0) 4.3 (3.7) 4.1 (4.3) NS<br />
All values are reported as mean (standard deviation); *p-value comparing<br />
GO to ST<br />
Conclusion: Mesh fixation using fibrin glue has comparable tensile<br />
strength and adhesion rate to sutures with tacks in the swine model.<br />
Increased contraction and migration rates associated with fibrin glue<br />
alone may be an issue and warrants further study. On the other hand,<br />
the GT group showed similar biomechanical characteristics as the<br />
other groups and may represent a reasonable alternative to the use of<br />
transfascial sutures.<br />
S067<br />
INITIAL EXPERIENCE WITH SENTINEL LYMPH NODE BIOPSY FOR<br />
ESOPHAGEAL CANCER Sarah K Thompson, MD, Dylan Bartholomeusz,<br />
MBBS MD, Peter G Devitt, MBBS University of Adelaide, Royal Adelaide<br />
Hospital, South Australia, Australia<br />
Introduction: There is emerging evidence that isolated tumor cells and<br />
micrometastases in lymph nodes have prognostic value in esophageal<br />
cancer. To facilitate a detailed examination of a limited number of<br />
lymph nodes by the pathologist, we report our initial experience with<br />
sentinel lymph node biopsy in patients undergoing resection for invasive<br />
esophageal cancer.<br />
121 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
S068<br />
THE SELF-APPROXIMATING TRANSLUMENAL ACCESS TECHNIQUE<br />
(STAT) RELIABLY PERMITS TRANSGASTRIC ORGAN RESECTION AND<br />
RETRIEVAL Eric M Pauli, MD, Jegan Gopal, MD, Matthew T Moyer, MD,<br />
Abraham Mathew, MD, Randy S Haluck, MD, Ann M Rogers, MD Penn State<br />
Milton S. Hershey Medical Center<br />
Introduction: Several studies have shown that the Self-Approximating<br />
Translumenal Access Technique (STAT) allows safe abdominal access<br />
and a reliable means of gastric closure for per-oral NOTES. Little is<br />
known, however, about the durability of the STAT tunnel under the<br />
mechanical forces required for organ resection and specimen retrieval.<br />
We hypothesized that simple extirpative abdominal operations (including<br />
specimen resection and retrieval) could be performed via STAT so that the<br />
tunnel would maintain its integrity for the conclusion of the procedure,<br />
permitting a secure gastrotomy closure.<br />
Methods: 14 domestic swine (mean wt 26kg) underwent transgastric<br />
organ resection (7 cholecystectomy, 7 left uterine horn resection).<br />
Abdominal access was obtained using STAT (as previously described) with<br />
the submucosal tunnel directed at the target organ. The resected surgical<br />
specimen, a fully inflated 2 cm endoscopic balloon and an 8x3x3cm<br />
manufactured ‘standard specimen’ (a simulated human gallbladder with<br />
large gallstone) were sequentially retrieved through the submucosal<br />
tunnel. Evaluation of tunnel integrity and an assessment of the ease of<br />
specimen extraction were performed following each retrieval. Physiologic,<br />
operative and clinical data were collected. All procedures were video<br />
recorded. After a two-week observation period, animals were euthanized<br />
and necropsy performed for documentation of gross findings.<br />
Results: The mean operative time was 4.1h (range 2.4-5.5hr). The mean<br />
abdominal access time (mucosal incision to serotomy) was 51min (range<br />
26-78). A mean tunnel length of 12cm (6-23cm) with a width 4cm (2.5-<br />
5cm) was created. The STAT tunnel remained fully intact in: 14/14 after<br />
organ resection and retrieval, 13/13 after balloon extraction and 11/14<br />
after standard specimen extraction. All three tears occurred early in our<br />
experience. Two small mucosal tears still permitted the STAT tunnel to<br />
be closed by standard endoscopic clip technique. One significant gastric<br />
tear required a single laparoscopic suture for secure closure. The ease<br />
in specimen extractions can be seen in Table 1. None of the standard<br />
specimens were able to be endoscopically delivered past the gastroesophageal<br />
junction (GEJ). Post-operatively all animals gained weight.<br />
One animal, sacrificed at post-operative day 12 due to lethargy, had a<br />
cystic duct leak and biloma. Other necropsy findings included: adhesions<br />
(4), bile leak (1), laparoscopic port site abscess (1), small submucosal<br />
abscess(1).<br />
Type of<br />
Specimen<br />
No<br />
Difficulty<br />
Mild<br />
Difficulty<br />
Moderate<br />
Difficulty<br />
Severe<br />
Difficulty<br />
Surgical Specimen 14 0 0 0<br />
Balloon 12 1 0 0<br />
Standard Specimen 7 0 3 4 (Early Cases)<br />
Conclusions: The submucosal tunnel created using STAT is capable of<br />
withstanding the mechanical forces of transgastric organ resection and<br />
retrieval. STAT also permitted the removal of rigid specimens (simulate<br />
large gallstone). None of these standard specimens could be delivered<br />
past the GEJ, suggesting that tunneling methods of transgastric access<br />
are not the size-limiting factor in per-oral specimen retrieval. One<br />
significant mucosal tear occurred early in the study, suggesting that there<br />
is a learning curve inherent in making the STAT tunnel wide enough to<br />
accommodate large, rigid specimens.<br />
S069<br />
SHORT-STAY SURGERY: WHAT REALLY HAPPENS AFTER DISCHARGE?<br />
Tung T Tran, MD, Pepa Kaneva, MSc, Nancy E Mayo, PhD, Gerald M Fried,<br />
MD, Liane S Feldman, MD Steinberg-Bernstein Centre for Minimally<br />
Invasive Surgery, McGill University, Montreal, Quebec, Canada<br />
Introduction: Innovations in surgery and perioperative care enable rapid<br />
hospital discharge after a variety of procedures. While length of hospital<br />
stay is commonly used as a surrogate outcome for surgical recovery, it<br />
12 th World Congress of Endoscopic Surgery 122<br />
is not applicable in the setting of short-stay surgery (
Scientific Session Oral Abstracts<br />
group compared to the laparoscopically treated group (median 4 days<br />
vs. 2 days, p < 0.05). Rates of incisional infections were also significantly<br />
higher in the open vs. the laparoscopic group (5.9% vs. 2.2%, p < 0.05).<br />
When controlling for other patient characteristics, open appendectomy<br />
was still significantly associated with a higher rate of incisional wound<br />
infection.<br />
Conclusion: Laparoscopic appendectomy in elderly patients is a<br />
safe procedure with regards to 30-day post-operative morbidity and<br />
demonstrates a benefit of decreased wound infection rates as compared<br />
to the open approach.<br />
S071<br />
SINGLE SITE LAPAROSCOPIC (SSL) CHOLECYSTECTOMY IN HUMAN<br />
CADAVERS USING NOVEL PERCUTANEOUS RETRACTION AND A<br />
MAGNETIC ANCHORING AND GUIDANCE SYSTEM (MAGS): RE-<br />
ESTABLISHING THE CRITICAL VIEW Rohan A Joseph, MD, Nilson A<br />
Salas, MD, Michael A Donovan, MS, Patrick R Reardon, MD, Barbara L Bass,<br />
MD, Brian J Dunkin, MD Methodist Institute for Technology Innovation<br />
and Education (MITIE), Department of Surgery, The Methodist<br />
Hospital,Houston- TX<br />
Introduction: SSL, though promising, introduces ergonomic challenges<br />
due to loss of instrument triangulation as obtained in conventional<br />
laparoscopy. This limitation makes establishing the critical view during<br />
dissection of the Triangle of Calot (TOC) difficult and has resulted in a<br />
variety of strategies to overcome the problem. This study investigates<br />
use of a novel percutaneous grasper that mimics a standard laparoscopic<br />
instrument and MAGS in aiding surgeons to perform SSL cholecystectomy<br />
more easily and with a technique that closely mimics four-port<br />
cholecystectomy.<br />
Methods: SSL cholecystectomy was performed on four female cadavers<br />
by an expert laparoscopic surgeon with limited experience in SSL. A<br />
15–18mm incision was made at the umbilicus and the MAGS introduced<br />
into the abdomen. MAGS consists of an oblong (7.8cm × 14mm) magnetic<br />
internal effector with a retractable monopolar cautery hook (6.3cm) and<br />
is coupled across the abdominal wall to an external hand-held magnet.<br />
By sliding the external magnet over the abdominal wall and applying<br />
external pressure, subtle motions of the hook can be achieved. Following<br />
MAGS introduction, a commercially available port comprised of a foam<br />
cuff and three 5mm trocars was placed. Next, the novel grasper was<br />
introduced percutaneously in the RUQ. The device’s 3mm transabdominal<br />
shaft is mated to a 5mm end effector intra-corporeally and can grasp<br />
tissue with the purchase and security of a standard laparoscopic<br />
instrument while providing 360° rotation and locking jaws. Retraction<br />
was accomplished using the percutaneous grasper to manipulate the<br />
fundus and a standard 5mm grasper through the umbilical port for the<br />
infundibulum. Dissection was done using a combination of the MAGS and<br />
a standard Maryland dissector. Total procedure time, time from procedure<br />
start to obtain a critical view of the TOC and clipping and dividing the<br />
cystic duct/ artery, time for dissection of the gall bladder from the liver<br />
bed, and thickness of the abdominal wall at the umbilicus were measured.<br />
A multi-institutional survey was also administered among surgeons<br />
having experience with these devices to gauge satisfaction.<br />
Results: The critical view was obtained in each case and all 4 procedures<br />
were completed successfully. Both devices performed optimally to<br />
allow smooth flow of the procedure. Mean procedure time was 40min<br />
(33-51min); time from procedure start to obtaining the critical view and<br />
clipping and dividing the cystic duct/ artery was 33 min (28-38min) and<br />
time for dissection of the gall bladder from the liver bed was 6.7min (3-<br />
13min). The mean abdominal wall thickness was 1.9cm (1.5-2cm). The<br />
survey found that MAGS increased surgeon satisfaction in performing SSL<br />
cholecystectomy by 73% (18% satisfaction standard SSL, 100% MAGS).<br />
Conclusions: The use of a novel graspers and MAGS overcomes the<br />
limitations of SSL cholecystectomy and improves surgeon dexterity.<br />
Making SSL feel more like traditional laparoscopy will enable a wider<br />
adoption of this procedure in the community.<br />
S072<br />
LAPAROSCOPIC CHOLECYSTECTOMY POSES PHYSICAL INJURY RISK<br />
TO SURGEONS: ANALYSIS OF HAND TECHNIQUE AND STANDING<br />
POSITION Yassar Youssef, MD, Gyusung Lee, PhD, Carlos Godinez, MD,<br />
Erica Sutton, MD, Rosemary Klein, MA, Ivan George, Jacob Seagull, PhD,<br />
Adrian Park, MD Sinai Hospital of Baltimore, MD, USA and University of<br />
Maryland Medical Center, Baltimore, MD, USA.<br />
Introduction: This study compares the effects of surgical techniques<br />
(one-handed versus two-handed) and surgeon’s standing position (sidestanding<br />
versus between-standing) during laparoscopic cholecystectomy<br />
(LC) and its outcomes on surgeons’ learning, performance, and<br />
ergonomics. There is little homogeneity in how to perform and train for<br />
LC. Variations in standing position (“American” or side-standing technique<br />
where the surgeon stands on the patient’s left versus “French” or betweenstanding<br />
technique where the surgeon stands between the patient’s<br />
legs) as well as hand technique (one-handed versus two-handed) exist.<br />
The two-handed technique refers to the surgeon providing his own<br />
exposure using one hand for dissection and the other for retraction while<br />
the assistant hold the camera. The one-handed technique refers to the<br />
situation during which the surgeon dissects with one hand and manages<br />
the camera with the other with the assistant helping in providing<br />
exposure and gallbladder retraction.<br />
Methods: Thirty-two LC procedures performed by a total of eight subjects<br />
on a virtual reality simulator were video recorded and analyzed. All<br />
eight subjects were right-handed. Each subject performed four different<br />
procedures so as individual assessment of the following methods was<br />
possible: one-handed/side-standing, one-handed/between-standing,<br />
two-handed/side-standing, and two-handed/between-standing. Physical<br />
ergonomics were evaluated using the Rapid Upper Limb Assessment<br />
(RULA) tool. Mental workload assessment was achieved through the use<br />
of the National Aeronautics and Space Administration-Task Load Index<br />
(NASA-TLX). Performance evaluation data generated by both the virtual<br />
reality simulator and a subjective survey were also analyzed.<br />
Results: The RULA scores for all procedures were statistically significantly<br />
better for the between-standing technique compared to the sidestanding<br />
technique. Regardless whether the technique used was one- or<br />
two-handed, the between-standing technique was associated with better<br />
ergonomics than the side-standing technique. The median RULA scores<br />
for different anatomical area was significantly worse for the upper arms<br />
and trunk in the side-standing position (upper arms: 3.5 – trunk: 3.5)<br />
when compared with the between-standing position (upper arms: 2 and<br />
trunk: 1.5). This showed that the main disadvantage of the side-standing<br />
position to be its detrimental effect on both the upper arms and trunk.<br />
There was no significant difference in other body parts including the<br />
lower arms, wrist, neck and legs.<br />
Using the NASA-TLX tool, the side-standing position was associated with<br />
statistically significantly higher effort, frustration, and physical demand<br />
(p< 0.05). The objective, simulator-generated performance metrics<br />
demonstrated no differences in either operative time or complication rate<br />
among the four methods for performing LC. Survey answers indicated the<br />
subjects’ choice to be the two-handed/between-standing technique as<br />
the best procedural method for teaching and standardization.<br />
Conclusion: Laparoscopic cholecystectomy poses a risk of physical injury<br />
to the surgeon. As it is currently commonly performed in the United<br />
States, the left side-standing position leads to increased physical demand<br />
and effort, thus resulting in ergonomically unsound operative conditions.<br />
Until further investigations are made, adopting the between-standing<br />
position deserves serious consideration as it presents the best short-term<br />
ergonomic alternative.<br />
12 th World Congress of Endoscopic Surgery<br />
123 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
S073<br />
EFFECTS OF NISSEN FUNDOPLICATION ON ABLATION OF BARRETT’S<br />
ESOPHAGUS WITH ENDOSCOPIC, ENDOLUMINAL RADIOFREQUENCY<br />
ABLATION Kathleen O’Connell, BS, Vic Velanovich, MD Henry Ford<br />
Hospital, Detroit, Michigan<br />
Background: Endoscopic, endoluminal radiofrequency ablation is<br />
achieving increasing acceptance as a mode of eliminating Barrett’s<br />
metaplasia and, thus, reducing the risk of developing esophageal<br />
adenocarcinoma. It is believed that reducing the exposure of the<br />
esophageal epithelium to acid is essential to achieve long-term ablation<br />
of Barrett’s esophagus. However, it is unclear whether the use of proton<br />
pump inhibitors or antireflux operations are more effective to accomplish<br />
this goal.<br />
Methods: A review of all patients who underwent endoscopic,<br />
endoluminal radiofrequency ablation with the BARRx device (BARRx<br />
Medical, Sunnyvale, CA) were reviewed for date of initial ablation,<br />
length of Barrett’s epithelium, presence or performance of a<br />
Nissen fundoplication, all follow-up endoscopy and treatment, and<br />
posttreatment biopsy results. Patients were categorizes by the presence<br />
of a Nissen fundoplication and presence of Barrett’s metaplasia or<br />
dysplasia by biopsy at least 12 months following ablation and at last<br />
endoscopic follow-up. Data was analyzed by Fisher’s exact test and the<br />
Mann-Whitney U-test.<br />
Results: Of 77 patients ablated, 47 had documented endoscopic followup<br />
at 12 months or longer following the ablation. Of these, 19 patients<br />
had Nissen fundoplications before, at the same time, or after ablation.<br />
The median length of Barrett’s epithelium, with interquartile range (IQR)<br />
was 3 (2-12) in patients with fundoplications compared to 3 (2-7) without<br />
fundoplications (p=NS). Median follow-up in months was 15 (12-24) in<br />
fundoplication patients compared to 12.5 (12-17) without (p=NS). One<br />
of 19 patients with fundoplications had persistent or recurrent Barrett’s<br />
epithelium, compared to 7 of 28 without fundoplications (p=0.03). Of<br />
patients without fundoplications, those who had persistent or recurrent<br />
Barrett’s had a median Barrett’s length of 10 cm (6-12 cm), compared to<br />
3 cm (2-5 cm) in patients who had ablated Barrett’s (p=0.03). Follow-up<br />
length was similar in those with ablated epithelium, 15 (12-19), compared<br />
to those with persistent or recurrent Barrett’s, 12 (12-13) (p=NS).<br />
Conclusions: Patients who had fundoplications in conjunction with<br />
endoluminal radiofrequency ablation were more likely to achieve<br />
durable ablation compared to patients who were treated with proton<br />
pump inhibitor therapy. It appears that patients with long-segment<br />
Barrett’s esophagus are at higher risk or persistent or recurrent Barrett’s<br />
metaplasia. Consideration for an antireflux operation should be<br />
given in patients with long-segment Barrett’s esophagus and planned<br />
endoluminal radiofrequency ablation.<br />
S074<br />
LAPARO-ENDOSCOPIC SINGLE SITE (LESS) HELLER MYOTOMY AND<br />
ANTERIOR FUNDOPLICATION FOR ACHALASIA Linda Barry, MD,<br />
Sharona B Ross, MD, Sujat Dahal, MD, Melissa Rosas, Chinyere Okpaleke,<br />
BS, Desiree Villadolid, MPH, Alexander S Rosemurgy, MD Department of<br />
Surgery, University of South Florida, Tampa, Florida<br />
Introduction: Laparo-Endoscopic Single Site (LESS) surgery is beginning<br />
to include advanced laparoscopic operations, such as Heller myotomy<br />
with anterior fundoplication. However, the feasibility and efficacy of LESS<br />
Heller myotomy and anterior fundoplication has not been established.<br />
This study was undertaken to evaluate our initial experience with LESS<br />
Heller myotomy and anterior fundoplication for achalasia.<br />
Methods: Transumbilical LESS Heller myotomy with concomitant anterior<br />
fundoplication for achalasia was undertaken in 51 patients since October<br />
2007. Outcomes, including operative time, complications, and length of<br />
stay were recorded and compared to an earlier consecutive contiguous<br />
group of 51 patients undergoing conventional multi-incision laparoscopic<br />
Heller myotomy with anterior fundoplication. Symptoms before and after<br />
myotomy were scored by patients using a Likert scale (0=never / not<br />
severe to 10=always / very severe). Data were analyzed using the Mann-<br />
Whitney test, Wilcoxon matched pairs test, and Fisher exact test, where<br />
12 th World Congress of Endoscopic Surgery 124<br />
appropriate. Data are presented as median (mean ± SD).<br />
Results: Patients undergoing LESS Heller myotomy vs. conventional<br />
laparoscopic Heller myotomy were similar in gender, age, BMI, blood<br />
loss, and length of hospital stay (Table). However, patients undergoing<br />
LESS Heller myotomies had operations of significantly longer duration.<br />
With LESS myotomy, 10 patients (20%) required an additional port /<br />
incision. No patients were converted to “open” operations. No patients<br />
had procedure specific complications. Symptom reduction was dramatic,<br />
satisfying, and similar after both LESS and conventional laparoscopic<br />
myotomy and fundoplication (Table). Patients undergoing Heller<br />
myotomy and anterior fundoplication using LESS approach had no<br />
apparent scars.<br />
Conventional lap<br />
Heller<br />
LESS Heller<br />
Patients (N): 51 51<br />
Gender: 25 m / 26 f 25 m / 26 f NS<br />
Age:<br />
50 years (52 years<br />
± 19.1)<br />
57 years (55<br />
years ± 16.0)<br />
NS<br />
BMI:<br />
24 kg/m 2 (24 kg/m 2<br />
± 4.2)<br />
25 kg/m2 (24<br />
kg/m2 ± 3.8)<br />
NS<br />
Length of Operation:<br />
106 min (109 min ± 133 min (131<br />
32.4)<br />
min ± 41.5)<br />
0.002<br />
Blood Loss:<br />
47 (
Scientific Session Oral Abstracts<br />
Results: The study population consisted of 310 patients with a median<br />
age of 52 (IQR:42-63). No significant difference was found between day 1<br />
and day 2 composite pH score (13.1, 14.4, p=0.66), this was also true for all<br />
the esophageal pH monitoring components (p>0.17). A strong correlation<br />
was found between composite pH score in day 1 and day 2 [r = 0.83 (95%<br />
CI: 0.79 - 0.86, p
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
S078<br />
LAPAROSCOPIC REPAIR OF LARGE HIATAL HERNIAS - IMPACT ON<br />
PULMONARY FUNCTION Jacqui C. Zhu, MBBS, Guillemo Becerril, MBBS,<br />
Gregory L. Falk, MBBS Deptartment of Upper Gastrointestinal Surgery and<br />
Endosurgery, Concord Hospital<br />
Introduction: This study is to examine the impact of laparoscopic repair<br />
of large hiatal hernia on patient’s respiratory function and quality of life.<br />
Methods: From 2004 to 2008, 30 consecutive patients with large<br />
paraesophageal hernia defined as >50% of stomach in the intrathoracic<br />
cavity with a minimum follow-up of 2 years were included in this<br />
study. All patients graded their dyspnoea severity as an index of 1=no<br />
dyspnoea, 2=dyspnoea with exertion, 3=dyspnoea with basic activities or<br />
4=dyspnoea at rest. All patients had a formal respiratory function test 1<br />
week prior and 3 months after their laparoscopic hiatal hernia repair. The<br />
patients had to rate their symptom severity and complete a quality of life<br />
questionnaire in the form of Gastrointestinal Quality of Life Index (GIQLI)<br />
preoperatively and then at 3-month, 6-month and thereafter yearly<br />
intervals postoperatively.<br />
Results: There were no hospital mortality and the morbidity rate was<br />
10%. In 26 patients with preoperative dyspnoea, 22 had complete<br />
resolution while the remaining 4 had experienced improvement in<br />
dyspnoea severity postoperatively. The mean dyspnoea severity index<br />
reduced from 2.4 to 1.3(p
Scientific Session Oral Abstracts<br />
Conclusion: Our series are of relatively limited number and our results<br />
need to be verified by larger series. In our double blinded study, pain<br />
control was easily achieved by NASIDs in the study group. The need<br />
for opioids were significantly higher in the control group as well as<br />
the VAS scores. We have found crural Bupivacaine injection to be an<br />
effective treatment for the management of perioperative pain in patients<br />
undergoing Laproscopic Nissens Fundoplication.<br />
S081<br />
OUTCOMES AFTER REPAIR OF THE INTRA-THORACIC STOMACH:<br />
OBJECTIVE FOLLOW-UP UP TO 5 YEARS Jai Bikhchandani, MD,<br />
Ona Gurney, F Yano, Tommy Lee, MD, Sumeet K Mittal, MD Creighton<br />
University Medical Center<br />
Introduction: Laparoscopic surgery is a viable treatment option for intrathoracic<br />
stomach (ITS); however doubts have been raised regarding its<br />
efficacy. Routine use of mesh has been advocated. The aim of this study is<br />
to look at long term objective and symptomatic outcomes after repair of<br />
ITS with selective use of mesh and fundoplication.<br />
Methods: A retrospective review of prospectively collected data was<br />
performed to identify patients who underwent surgical treatment of ITS<br />
from Jan 2004 to Sep 2008 at Creighton University Medical Center. ITS was<br />
defined as herniation of greater than 75% of the stomach into the chest<br />
on a barium swallow. A standardized foregut symptom questionnaire was<br />
administered along with contrast study at 1, 3 and 5 yrs post-surgery.<br />
Results: Sixty-nine patients with a mean age of 71.2 years (44-88) had<br />
surgical treatment of ITS. There were 46 (67%) females. There were 7<br />
trans-thoracic and 62 trans-abdominal repairs (59 laparoscopic and 3<br />
open conversions). There was one intra-op death due to bleeding. Antireflux<br />
surgery was performed in 38 patients (21 Nissen, 13 Toupet, 1 Dor<br />
and 3 Roux-en-Y gastric bypass). Of these 10 patients also had Collis<br />
gastroplasty for a short esophagus. In the remaining 30 patients excision<br />
of the hernia sac and crural repair was done. Mesh was used in 6 (8.7%)<br />
patients for crus reinforcement. Objective follow-up was available for<br />
89%, 76% and 75% at 1, 3 and 5 years respectively. There were 7% (4/59)<br />
radiological failures (one patient required emergent re-operation) within<br />
the first year. No additional recurrences were noted at 3 and 5 years. There<br />
was no significant difference in mean symptom and satisfaction scores or<br />
use of PPI between the patients with and without fundoplication. Mean<br />
satisfaction scores were 9.4, 9.0 and 9.3 at 1, 3 and 5 years respectively<br />
Conclusion: Laparoscopic repair of ITS is feasible, safe and durable with<br />
selective use of mesh and fundoplication and results in a high degree of<br />
patient satisfaction. Low recurrence rates at 1 year were achieved with no<br />
incremental failures up to 5 years. Longer follow-up with larger number of<br />
patients is needed to confirm these findings.<br />
S082<br />
REOPERATIVE LAPAROSCOPIC PARAESOPHAGEAL HERNIORRAPHY<br />
CAN PRODUCE EXCELLENT OUTCOMES Albert W Tsang, MD, Manish<br />
M Tiwaria, MD PhD MPH, Jason F Reynoso, MD, Dmitry Oleynikov, MD<br />
Department of Surgery, University of Nebraska Medical Center<br />
Introduction: Patients undergoing laparoscopic paraesophageal<br />
herniorraphy, either initial or recurrent, present with a myriad of<br />
esophageal and extra-esophageal symptoms. Given an overall recurrence<br />
rate of approximately 8%, reoperative paraesophageal herniorraphy is<br />
necessary on a significant number of patients. The goal of this study is to<br />
determine whether patients proceeding with laparoscopic reoperative<br />
paraesophageal herniorraphy experienced symptom resolution equal to<br />
or better than patients undergoing a first-time repair.<br />
Methods: A comprehensive, symptom frequency based clinical tool<br />
consisting of 24 esophageal and extra-esophageal reflux symptoms<br />
was developed and administered to patients undergoing an initial<br />
or reoperative paraesophageal herniorraphy between February 2002<br />
and September 2009. This was administered pre-operatively and<br />
post-operatively. From individual symptom scores, a composite score<br />
for esophageal reflux and extra-esophageal reflux was calculated. A<br />
retrospective analysis of patient records including history and physical<br />
examination, laboratory investigations, operative and post-operative<br />
follow-up progress notes was reviewed. Data on age, gender, twentyfour<br />
symptom frequencies, manometry results, pH testing results was<br />
collected and analyzed using appropriate statistical tests.<br />
Results: Patients included in the study had a mean age of 53.6 years<br />
and 57.4% of patients were female. Analysis of composite symptom<br />
scores of 195 patients demonstrated that paraesophageal herniorraphy<br />
results in a significant resolution of both esophageal (16.1 ± 8.5 preop<br />
vs. 3.5 ± 5.0 at 6 months post-op; p
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
reimbursements ranged from $264-$504 and $0-$545 respectively for<br />
patients discharged on day 1.<br />
The surgeon with the lowest average disposable cost per case ($329.18)<br />
utilized clips, pre-tied loops, and hand-ties as their predominant<br />
techniques. The surgeon with the highest average disposable cost per<br />
case ($552.33) predominantly used a linear stapler with 3 cartridges.<br />
DISCUSSION: Disposable costs incurred during each case frequently<br />
exceeded the hospital reimbursement. Currently, there is no scientific<br />
literature that suggests a superior surgical method for performing<br />
these portions of LA. Therefore additional costs are incurred without<br />
demonstrable clinical benefit. Practice amongst individual surgeons<br />
can be quite variable. This study suggests surgeons should review the<br />
cost implications of their practice and to find ways to provide the same<br />
effective care without unwarranted expenditures. Certain patients may<br />
present with complex pathology that merits individual approaches, yet<br />
routine LA procedures can be performed with less-expensive techniques<br />
that provide the same quality of care.<br />
S084<br />
TRANSANAL ENDOSCOPIC MICROSURGERY VERSUS LAPAROSCOPIC<br />
RESECTIONS IN 100 T2-N0 RECTAL CANCERS FOLLOWING<br />
NEOADJUVANT TREATMENT: A PROSPECTIVE RANDOMIZED TRIAL<br />
WITH FIVE YEARS MINIMUM FOLLOW-UP Emanuele Lezoche, Professor<br />
Phd, Maddalena Baldarelli, MD, Massimiliano Rimini, MD, Alessandro<br />
Maria Paganini, Professor Phd, Roberto Campagnacci, MD, Mario Guerrieri,<br />
Professor Department of Surgery University Politecnica delle Marche<br />
“Ancona” Italy<br />
Background: Aim of this study was to compare the oncological results of<br />
local excision performed with Transanal Endoscopic Microsurgery (TEM)<br />
versus Laparoscopic Resection (LR) with total mesorectal excision in the<br />
treatment of T2 N0, G1-2 rectal cancer following NT in both arms, with a 5<br />
years minimum follow-up.<br />
Methods: In the period comprised between April 1997 and April 2004,<br />
100 patients staged at admission as T2 N0, G1-2 rectal cancer with a<br />
tumour diameter lower than 3 cm and located within 6 cm from the anal<br />
verge were enrolled: 50 were randomized to TEM and 50 to LR. Patients in<br />
both groups were previously underwent high dose radiotherapy (5,040<br />
cGy in 28 fractions over 5 weeks) combined with continuous infusion of<br />
5-Flurouracil (200 mg/m2/day).<br />
Results: At minimum follow-up of 5 years 4 local recurrence (8.0 %) were<br />
observed after TEM and 3 (6 %) after LR . Distant metastases occurred<br />
in 2 (4%) case after TEM and in 2 (4%) pts after LR. The probability of<br />
disease-free survival at the end of follow-up was 91% in TEM group (95%<br />
Confidence Interval=79%-99%) and 93 % in LR group B (95% Confidence<br />
Interval=78%-99%).<br />
Conclusions: The study shows similar results between the two arms in<br />
terms of local recurrences, distant metastases and probability of survival<br />
for rectal cancer.<br />
S085<br />
LAPAROSCOPIC VERSUS OPEN ELECTIVE SIGMOID RESECTION<br />
IN DIVERTICULAR DISEASE: SIX MONTHS FOLLOW-UP OF THE<br />
RANDOMIZED CONTROL SIGMA-TRIAL Bastiaan R Klarenbeek, MD,<br />
Roberto Bergamaschi, MD PhD FRCS, Alexander A Veenhof, MD, Donald<br />
L van der Peet, MD PhD, Wim T van der Broek, MD PhD, Elly S de Lange,<br />
PhD, Willem A Bemelman, MD PhD, Piet Heres, MD, Antonio M Lacy,<br />
MD PhD, Miguel A Cues VU University Medical Center, Amsterdam, The<br />
Netherlands; Forde Health System, Bergen University, Forde, Norway;<br />
Academic Medical Center, Amsterdam, The Netherlands; Waterland<br />
Hospital, Purmerend, The Netherlands; Hospital Clinic, Barcelona, Spain<br />
Background: The short-term results of the Sigma-trial, comparing<br />
laparoscopic (LSR) versus open (OSR) elective sigmoid resection for<br />
diverticular disease, showed a 15.4% reduction in major complication<br />
rates, less pain, and shorter hospitalization at the cost of a longer<br />
operating time. Present data complements these results with six months<br />
follow-up.<br />
Methods: This was a prospective, multi-center, double-blind, parallelarm,<br />
randomized control trial, eligible patients were randomized to either<br />
LSR or OSR. Short-term results of the Sigma-trial have been published<br />
previously, methodological and operative details can be found in this<br />
original article. Patients attended the outpatient clinic six weeks and<br />
six months after surgery. Physical examination was carried out and the<br />
quality of life questionnaires were completed. In case of readmission,<br />
medical records were prospectively evaluated. Primary endpoints were<br />
mortality and late complications occurring between 30 days from surgery<br />
until six months postoperative.<br />
Results: From 2002 to 2006, 104 patients were randomized in five centers.<br />
All patients underwent the allocated intervention. 52 LSR patients were<br />
comparable to 52 OSR patients for gender, age, BMI, ASA grade, comorbid<br />
conditions, previous abdominal surgery, and indication for surgery.<br />
Conversion rate was 19.2%. LSR was associated with short-term benefits<br />
like a 15.4% reduction in major complication rates, less pain, and shorter<br />
hospitalization at the cost of a longer operating time. At six months<br />
follow up no significant differences in morbidity and mortality rates were<br />
found. Two patients died of cardiopulmonal causes (overall mortality 3%).<br />
Late complications (LSR 7 vs. 12 OSR; p = .205) consist of three incisional<br />
hernias, five times ileus, four fistulas, one abscess, two anastomotic<br />
stenoses and three recurrent episodes of diverticulitis. Nine of these<br />
patients underwent additional surgical interventions. Only 30% of ten<br />
ostomies were reversed during the follow-up period. The Short Form-36<br />
(SF-36) questionnaire showed significantly better quality of life for LSR at<br />
the six weeks follow-up, but at the six moths follow-up these differences<br />
were decreased.<br />
Conclusions: Six months follow-up showed an overall mortality rate of<br />
3% and a complication rate of 18%. No significant differences were found<br />
between LSR and OSR in terms of complications, re-interventions or<br />
ostomy reversal.<br />
S086<br />
TOTAL INTRACORPOREAL COLON SURGERY USING THE N.O.S.E.<br />
(NATURAL ORIFICE SPECIMEN EXTRACTION) TECHNIQUE. Morris E<br />
Franklin, MD, Karla Russek, MD, Allen Alvarez, MD Texas Endosurgery<br />
Institute<br />
Introduction: Laparoscopic surgery for colonic disease has experienced<br />
an increased utilization by surgeons owing to decreased morbidity, less<br />
pain, earlier ambulation, earlier bowel function, fewer complications,<br />
decreased narcotic use, and improved cosmesis compared with open<br />
colon surgery. The ability to perform a totally intracorporeal anastomosis<br />
will be an initial step to allow surgeons to perform natural orifice colon<br />
surgery in the future. Natural orifice specimen extraction eliminates<br />
the need for any enlargement of extraction abdominal incisions.<br />
The transvaginal site for specimen extraction is a safe alternative to<br />
transabdominal specimen extraction where enlargement of incisions are<br />
needed during laparoscopic colorectal surgery.<br />
Methods: The objective of this study was to report our experience with<br />
patients requiring a laparoscopic right hemicolectomy using a totally<br />
intracorporeal technique. We designed a nonrandomized prospective<br />
study of all consecutive female patients requiring a right hemicolectomy<br />
for both benign and malignant disease.<br />
Results: Forty-nine patients were entered into the study from December<br />
2007 to August 2009; 24 patients in the transvaginal (NOSE) group, and<br />
25 patients in the counter incision group. Mean age was 69.9 +/- 14.8.<br />
Operative time 159 +/- 27.1 min NOSE group vs 133.5 +/- 29 min counter<br />
incision group. Estimated blood loss was 83.3 +/- 14.4 mL NOSE group<br />
vs.133 +/- 65.5 mL. Length of hospital stay was similar at 5.5 +/- 2.5<br />
days NOSE group vs. 5.9 +/- 2.2 days. There was one intraoperative<br />
complication in the NOSE group (4.1%) and two minor postoperative<br />
complications (6.6%). There was one incisional hernia, one wound<br />
infection and two minor postoperative complications in the counter<br />
incisional group (13%). The overall complication rate was 8.3% for the<br />
NOSE group vs. 13% for the counter incision group.<br />
Conclusion: We consider the Natural orifice extraction approach after a<br />
laparoscopic right hemicolectomy to be feasible and safe.<br />
12 th World Congress of Endoscopic Surgery 128
Scientific Session Oral Abstracts<br />
S087<br />
SINGLE INCISION LAPAROSCOPIC TOTAL PROCTOCOLECTOMY WITH<br />
ILEOANAL ANASTOMOSIS: INITIAL OPERATIVE EXPERIENCE Daniel<br />
P Geisler, MD, Hasan T Kirat, MD, Feza H Remzi, MD Department of<br />
Colorectal Surgery Cleveland Clinic Foundation<br />
Introduction: Single incision laparoscopic surgery (SILS) has been<br />
described in the urologic, gynecologic, bariatric and, more recently,<br />
colorectal surgical literature. Single-port colectomies have only been<br />
described as case-reports. We herein describe our experience to date with<br />
the use of single incision laparoscopic surgery for total proctocolectomy<br />
with ileoanal anastomosis.<br />
Patients and Methods: All patients who have undergone SILS total<br />
proctocolectomy and ileoanal anastomosis were identified from an IRBapproved<br />
laparoscopic database. Data was collected via chart review. All<br />
procedures were performed with use of the 5mm Olympus EndoEye and<br />
traditional laparoscopic instruments.<br />
Results: 5 patients were identified between June 2009 and September<br />
2009. Mean age was 36 years (range 13 to 47). There were 3 males and 2<br />
females. Mean body mass index was 21.2 (range 15.5 to 25.9). Diagnoses<br />
included ulcerative colitis (n=4) and familial adenomatous polyposis<br />
(n=1). Mean American Society of Anesthesiologists score (ASA) was 2. 3 of<br />
the 5 patients had previous abdominal surgery. All 5 patients had a SILS<br />
(Covidien, Mansfield, MA) port placed at the planned ileostomy site. No<br />
other abdominal incisions were made. Average operative time was 219<br />
minutes (range 137 to 278). Average estimated blood loss was 117 mL.<br />
There were no conversions to either a conventional laparoscopic or an<br />
open procedure. Average time to return of bowel function was 2 days and<br />
average length of stay was 4 days (3-6). Post-operative complications<br />
included two patients that were admitted to an outside hospital on<br />
postoperative day 15 with partial small bowel obstructions at the stoma<br />
site. Both resolved with conservative management. Two patients had their<br />
ileostomies reversed at 4 weeks and 6 weeks postoperatively with the<br />
other three scheduled in the near future.<br />
Conclusion: SILS total proctocolectomy with ileoanal anastomosis is a safe<br />
minimally invasive technique. Additional studies are needed to compare<br />
SILS approach to conventional laparoscopy and open surgery with<br />
respect to operative times, convalescence and outcomes.<br />
S088<br />
STAGED LAPAROSCOPIC ADJUVANT INTRAPERITONEAL<br />
CHEMOHYPERTHERMIA (IPCH) AFTER COMPLETE RESECTION FOR<br />
LOCALLY ADVANCED COLORECTAL OR GASTRIC CANCER Elie K<br />
Chouillard, MD Poissy Medical Center (FRANCE)<br />
Purpose: Cytoreductive surgery followed by intraperitoneal<br />
chemohyperthermia (IPCH) is a promising treatment for patients with<br />
peritoneal malignancies. Usually, IPCH is performed concomitantly<br />
with cytoreductive surgery for peritoneal cancinomatosis (PC) or more<br />
occasionally as an adjuvant treatment after gastric resection for cancer. In<br />
this report, we describe our experience with staged adjuvant laparoscopic<br />
IPCH after complete resection in patients with advanced colorectal or<br />
gastric cancer.<br />
Methods: 25 patients underwent resection for colorectal (16 patients)<br />
or gastric cancer (9 patients) followed by staged laparoscopic IPCH.<br />
Operative technique, complications, as well as more than 2-year follow-up<br />
findings were assessed.<br />
Results: Mean intraperitonel temperature was 41.9° C. The homogeneity<br />
of the hyperthermia across the abdominal cavity was electronically<br />
maintained throughout the procedure by input and output flow<br />
regulation. No conversion to laparotomy was performed. No major<br />
operative incident was encountered.<br />
The mean hospital stay was 11 days (6-24). No 30-day mortality<br />
occurred. Five patients developed complications (20 %). One patient was<br />
reoperated (4 %).<br />
Mean follow-up was 30.5 months (24-49). Six patients died including<br />
4 of cancer related causes (distant metastases). 17 patients (68 %) had<br />
some form of second look laparoscopy or laparotomy and 4 patients had<br />
autopsy (16 %). All patients had PET scans every 6 months. No patient<br />
developed PC.<br />
Conclusion: Staged laparoscopic adjuvant IPCH after open or<br />
laparoscopic resection in selected patients with colorectal or gastric<br />
cancer is safe and feasible. After more than 2-year follow-up, no patient<br />
seemed to have developed PC. Additional survival data are still needed.<br />
S089<br />
A CASE CONTROL COMPARISON OF LAPAROSCOPIC (LX) AND OPEN<br />
(OP) APPROACH FOR THE SURGICAL MANAGEMENT OF SMALL<br />
BOWEL OBSTRUCTION (SBO) Eran Itzkowitz, MD, Yehuda Kariv, MD, Boaz<br />
Sagie, MD, Joseph Koriansky, MD, Joseph Klausner, MD Tel Aviv Sourasky<br />
Medical Center, and Sackler Faculty of Medicine, Tel Aviv University, Tel<br />
Aviv, Israel.<br />
Background: LX offers enhanced recovery and better cosmesis.<br />
Reduction in postoperative adhesions and incisional hernia rates<br />
are potential long term benefits. Previous studies have shown that<br />
laparoscopic management of SBO is feasible and associated with<br />
acceptable morbidity. However, rates of conversion to OP are higher than<br />
in other laparoscopic procedures. Data comparing short and long term<br />
results of LX and OP in SBO are limited.<br />
Objectives: To identify risk factors for conversion, investigate its<br />
consequences, and compare short and long term outcomes of LX and OP.<br />
Methods: Patients who were operated for a diagnosis of SBO in either<br />
an attempted LX or OP were retrospectively identified. Data collected<br />
included patients demographics and comorbidities, indication for surgery,<br />
operative details, and postoperative recovery. Long term data including<br />
recurrent SBO, reoperations, and incisional hernias were obtained using<br />
patient charts and a telephone survey. LX and OP patients were matched<br />
(1:1) for age and the extent of previous abdominal operations (no surgery;<br />
minor surgery; laparotomy; multiple laparotomies). Short and long term<br />
results in both groups were analyzed according to intension to treat.<br />
Results: From 1998 to 2007, 202 patients were operated for SBO (90<br />
attempted LX, 112 OP). Most common etiologies for SBO in the LX group<br />
included adhesions (85.5%), malignancy (2.2%), and internal hernia<br />
(2.2%). 29 (32%) patients in the LX group were converted to an open<br />
procedure. Causes of conversion were dense adhesions (31%), need for<br />
bowel resection (17%), unidentified etiology (24%), and iatrogenic injury<br />
(28%).<br />
Preoperative patient characteristics and the extent of previous surgery<br />
were not associated with conversion (previous laparotomy 27% vs. 18%,<br />
p=0.3, conversion vs. non-conversion, respectively).<br />
Patients converted from laparoscopy to open surgery had longer<br />
operations (92.0±28.7 vs. 48.7±22.0 min, p
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Oral Abstracts<br />
rate of postoperative complications (32% vs. 51%, p=0.03), and earlier<br />
passage of flatus (median postoperative day 2 vs. 3, p
Scientific Session Oral Abstracts<br />
Group Total Withdrawal Studied<br />
Pain,peri-anal burning/<br />
irritation<br />
AnalgesicTablets<br />
used in 3 Weeks<br />
D3 W1 W3 Mean Range<br />
Study 32 7 25 20 2 0 7 5-31<br />
Control 35 12 23 16 5 0 11 10-27<br />
Conclusion: Resumption of normal spicy diet has no adverse impact on<br />
patient reported outcomes in stapled hemorrhoidopexy. Its apparent<br />
benefits in the present study and its impact on patient reported quality of<br />
life need to be studied in larger studies.<br />
S092<br />
IMPLEMENTATION OF COLONOSCOPIC PROCESS<br />
MEASURES: DOES IT IMPROVE QUALITY? Theodor<br />
Asgeirsson, MD, Anthony J Senagore, MD MBA FACS FASCRS, Martin<br />
A Luchtefeld, MD FASCRS Spectrum Health Research, Michigan State<br />
University, Ferguson Clinic<br />
Purpose: Although screening colonoscopy has significantly reduced<br />
the incidence of colorectal cancer due to removal of clinically significant<br />
adenomatous polyps, the clinical benefit of removing micro adenomas is<br />
of unclear benefit. As a result basing the value of increasing withdrawal<br />
time on adenoma detection rate may not be a good surrogate quality<br />
indicator for colonoscopic cancer screening. The aim of this study was to<br />
compare colonoscopic screening prior to and after full implementation of<br />
6 minute withdrawal time. Specifically assess polyp detection rate (PDR)<br />
and adenoma detection rate (ADR) during both time frames and the<br />
incidence of interval cancers in the earlier study population.<br />
Methods: Data from all out-patient screening colonoscopies during the<br />
first 6 months of 2006 (pre 6 minute withdrawal) and 2009 (post 6 minute<br />
withdrawal) were reviewed. Pathology reports were correlated with<br />
endoscopic findings. A retrospective chart review was performed on all<br />
screening colonoscopies from 2006 to evaluate for primary diagnosis of<br />
colorectal cancer in the 3 year period after there screening. Chi-square<br />
and T-test was used for quantitative and categorical data respectively.<br />
Confidence interval was used to compare difference in proportions and<br />
repeated measures ANOVA for data with Poisson distribution. P value was<br />
set at 0.05<br />
Results: 900 screening colonoscopies were performed during the first 6<br />
months of ‘06 and 750 in ‘09. Mean age 58.7 vs 57.7 years (p0.05). Visualization was documented<br />
as good in over 99.5% of screening colonoscopies in both years. Neither<br />
PDR 14.9% vs 13.9% nor ADR 7.2% vs 9.6% were statistically significant<br />
between pre and post 6 minute withdrawal time, (p>0.05). Interval<br />
colorectal cancer rate at 3 years was 0%.<br />
Conclusion: The data indicate that implementation of the 6 minute<br />
withdrawal time did no significantly alter PDR or ADR. Importantly<br />
there was no incidence of interval colon cancer in the 3 years following<br />
a screening colonoscopy in the pre 6 minute withdrawal group. These<br />
results occurred in a population with a high rate of cecal intubation<br />
and removal of clinically significant adenomatous lesions. Therefore the<br />
optimal quality measure may be interval colon cancer incidence rather<br />
than reliance on surrogate measures not clearly tied to the desired<br />
outcome.<br />
12 th World Congress of Endoscopic Surgery<br />
131 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Residents/Fellows Scientific Abstracts<br />
S093<br />
SINGLE INCISION LAPAROSCOPIC CHOLECYSTECTOMIES COST<br />
COMPARISON Katie Love, MD, Michael P Meara, MD, Christopher A<br />
Durham, MD, Curtis E Bower, MD FACS ECU Brody School of Medicine<br />
Objective: Cholecystectomy performed using the Single Incision<br />
Laparoscopic Surgery (SILS) technique should not cost significantly<br />
more or less than standard multiport cholecystectomy. Single access<br />
techniques are becoming more common for a multitude of laparoscopic<br />
procedures. Criticism has revolved around potential costs associated with<br />
increased operative time and use of innovative equipment.<br />
Methods: Retrospective cost data was collected from the accounting<br />
records of a single institution. A direct comparison of standard multiport<br />
cholecystectomies to SILS cholecystectomies was conducted. Data on<br />
the SILS cases that were converted to multiport cholecystectomies was<br />
included. Total operating room (OR) cost (actual cost to the hospital for<br />
equipment, time, and personnel) and total OR charges (the “list” price, or<br />
what the patient was billed, for equipment, time, and personnel) were<br />
examined. Total hospital charges (OR charges plus hospital charges<br />
accrued in the perioperative period) were also included. Descriptive<br />
statistics were used to analyze the data with p-values of statistical<br />
significance 25 LAP operations but no SILS procedures. The SILS-experience group<br />
(SE) consisted of attending LAP surgeons who had also performed at<br />
least 5 SILS operations. Each subject performed standardized tasks from<br />
FLS including peg transfer (PEG), pattern cutting (CIRCLE), placement<br />
of ligating loop (LOOP), and intracorporeal suturing (SUTURE) using<br />
a standard, three-port, FLS box-trainer with standard laparoscopic<br />
instruments. For SILS, the subjects used an FLS box modified to accept<br />
a Covidien SILS Port with two working ports for instruments and one<br />
port for a 30-degree 5mm laparoscope. SILS tasks were performed with<br />
Covidien Roticulator instruments capable of unilateral articulation.<br />
12 th World Congress of Endoscopic Surgery 132<br />
SILS suturing was performed using a Covidien SILS Stitch (articulating<br />
Endostitch device). Performance of FLS tasks was graded using standard<br />
time and accuracy metrics. Individual task scores as well as overall<br />
laparoscopic FLS score (LS) and overall SILS FLS score (SS) were calculated<br />
for each participant, and normalized to previously published FLS scoring<br />
criteria used to distinguish competent (>54%) and non-competent<br />
surgeons (
Residents/Fellows Scientific Abstracts<br />
CONCLUSION: Increasing operative time was associated with increased<br />
odds of complications and so it appears that speed may matter in<br />
laparoscopic surgery. These analyses are limited in their inability to<br />
adjust completely for all patient factors, potential confounders and<br />
case complexity. Additional multivariate and hierarchical surgeon level<br />
analyses are required to examine this relationship further.<br />
S096<br />
MORTALITY RISK ASSOCIATED WITH INSURANCE DENIALS IN<br />
BARIATRIC SURGERY CANDIDATES Raghid S Bitar, MD, Mastafa<br />
Springston, Geoffrey P Kohn, MD, Lindsee E McPhail, MD, David W Overby,<br />
MD, Timothy M Farrell, MD University of North Carolina at Chapel Hill<br />
Introduction: Increasing numbers of Americans meet medical candidacy<br />
criteria for bariatric surgery; however many are denied or delayed<br />
because of absence of insurance benefits or administrative hurdles in the<br />
pre-approval process. In many cases, patients endure months of delay<br />
before coming to a surgical date or giving up. Since morbid obesity carries<br />
inherent medical risk, we set about to define the mortality rate among<br />
those patients who were deemed acceptable candidates by our surgeons<br />
but who were declined or delayed in the insurance process.<br />
Methods: Retrospective review of a single institution bariatric surgery<br />
database between June 2002 and December 2008 was performed. Of 538<br />
total patients who were deemed surgical candidates in our preoperative<br />
clinic, 114 were denied and did not undergo surgery (subject group)<br />
compared with 424 who came to operation (control group) during the<br />
same time frame. Following IRB approval, patient identifiers were used<br />
to query the Social Security death index to assess whether patients were<br />
dead or alive as of August 10, 2009. Survival analysis with Kaplan-Meier<br />
plot was performed using SPSS (SPSS Inc. Chicago, IL) with log-rank test<br />
for statistical significance.<br />
Results: The subject group and control group were similar<br />
demographically (85.3% vs 85.6% females, mean age 44.7 vs 45.9 years).<br />
Mean follow up was 44.3 (range 8-86) months for subjects and 44.5 (range<br />
4-108) months for controls. Two medical deaths occurred in the subject<br />
group and 12 deaths occurred in the surgical group. Of these, 3 occurred<br />
within 30 days of surgery for a perioperative mortality of 0.71%, but 9<br />
others died during extended follow-up. Cumulative survival analysis using<br />
Kaplan-Meier plot is shown below. Curves are statistically similar.<br />
Conclusions: About 21% of patients who satisfy medical and surgical<br />
criteria for bariatric surgery failed to achieve insurance approval and<br />
follow-through with operation at our institution. Among these, there was<br />
a 1.8% mortality rate over 44.3 months follow-up, which is similar to the<br />
risk in early postoperative surgical patients. Over time, those patients with<br />
insurance denials are expected to suffer increasing mortality, although<br />
our data do not yet demonstrate this separation in survival curves.<br />
Longitudinal studies are necessary.<br />
S097<br />
INTRAOPERATIVE COLONOSCOPIES WITH LAPAROSCOPIC<br />
ASSISTANCE REDUCES UNNECESSARY BOWEL RESECTIONS AND<br />
HOSPITILIZATION Donald M Davis, MD, Valentine Nfonsam, MD, Jorge E<br />
Marcet, MD, Jared C Frattini, MD University of South Florida<br />
Objective of the Study: Colonic polyps found during colonoscopy are<br />
typically biopsied or removed using cold or hot snares. At times it is very<br />
difficult to remove these polyps because they may be large or flat, risking<br />
bowel perforation in the process. In addition, access to the polyp may<br />
be difficult due to adhesion from previous surgeries, redundancy of the<br />
colon, or location of the polyp. Traditionally, these patients are referred to<br />
a surgeon for bowel resection. At our institution, repeat colonoscopies are<br />
performed in the operating room. If warranted, laparoscopic assistance<br />
is used for enhanced colonic visualization, mobilization of the bowel<br />
and take-down of adhesions if required. This allows access to polyps that<br />
we not previously accessible with traditional colonoscopy. We can be<br />
much more aggressive in our polypectomies due to the fact that any full<br />
thickness injuries can immediately be repaired laparoscopically. Through<br />
this process we believe unnecessary bowel resections and its associated<br />
complications have been avoided. We have therefore undertaken this<br />
retrospective review to demonstrate the safety and efficacy of perform<br />
intraoperative colonoscopies with laparoscopic assistance in patients with<br />
benign disease.<br />
Methods: The names of patients scheduled for intraoperative<br />
colonoscopies from 2001 through September 2009 were collected.<br />
The respective electronic medical records were then reviewed. The<br />
data obtained included age, gender, whether laparoscopic assistance<br />
was utilized, operation performed (if applicable), location of tumor,<br />
intraoperative and postoperative complications, and length of hospital<br />
stay. The demographics were then analyzed and the data was then<br />
compared between operative or nonoperative (including laparoscopic<br />
assisted colonoscopies) groups.<br />
Results: Between March 2001 and September 2009, 106 patients<br />
with a diagnosis of benign polyps by colonoscopy underwent repeat<br />
intraoperative colonoscopies. The average age was 65 (median 65) with<br />
56% male patients. Of these patients, 74 patients (70%) were successfully<br />
treated with colonoscopic polypectomy, 10 of which utilized laparoscopy<br />
for mobilization and positioning of the colon.<br />
Of the 32 operative patients (30%), there were 17 colectomies, 7<br />
cecectomies, 5 transanal excisions, 2 low anterior resections, and one<br />
colotomy with mass excision. In all but two of the operative patients,<br />
laparoscopic assistance was not needed during colonoscopy. These<br />
patients underwent formal resections due to size or appearance<br />
suspicious for malignancy. In the two patients who underwent<br />
laparoscopic assistance, one underwent formal resection after the polyp<br />
was determined to be cancerous, while the other could still not be<br />
adequately accessed even after mobilization.<br />
There was a significant difference in the length of hospital stay between<br />
these groups (p
12 th World Congress of Endoscopic Surgery<br />
Residents/Fellows Scientific Abstracts<br />
S098<br />
IMPROVING SURGICAL TRAINING; THE USE OF FEEDBACK TO REDUCE<br />
ERRORS AND IMPROVE RETENTION DURING A SIMULATED SURGICAL<br />
PROCEDURE E Boyle, MRCS, M Al-Akash, MRCS, O Traynor, FRCS, AG<br />
Gallagher, PhD Bsc, ADK Hill, MD FRCS, PC Neary, MD FRCS National<br />
Surgical Training Centre, RCSI, Dublin, Ireland<br />
Introduction: It is known that feedback enhances the learning process,<br />
although the optimal type and frequency of feedback is not established.<br />
The ProMIS hand-assisted laparoscopic colectomy (HALC) simulator uses<br />
a combination of virtual reality (VR) and and physical models of intraabdominal<br />
organs to simulate a left-sided hemicolectomy. It can be used<br />
to train surgeons to perform a complete procedure in a safe environment.<br />
The purpose of this study was to determine if giving trainees feedback<br />
during a training session would improve their performance.<br />
Methods: We tested 16 residents (Group 1) who performed 5 HALC<br />
procedures on the ProMIS simulator. Efficiency of instrument use and predefined<br />
intra operative error scores were assessed. Facilitators assisted<br />
their performance and answered questions when asked. A similar cohort<br />
of 12 trainee surgeons (Group 2) then performed the same 5 cases, but<br />
with standardized feedback and the chance to review errors after every<br />
procedure. Eight subjects in Group 2 completed retention testing which<br />
consisted of two further repetitions of the HALC procedure. Data were<br />
analyzed using SPSS version 15. Means were compared using Mann-<br />
Whitney-U tests, with a p-value of
Residents/Fellows Scientific Abstracts<br />
the average age was 42.67 in the stapled group. 87% were female and<br />
the average age was 43.45 in the hand-sewn group (p=0.68 and p=0.67<br />
for gender and age respectively). BMI was 48.06 in the stapled group and<br />
48.01 in the hand-sewn group (p=0.76). The rate of stricture formation<br />
in the stapled group was 8% (8/100) and 1% in the hand-sewn group,<br />
and this finding was statistically significant with a p value of 0.017. No<br />
statistical difference of stricture formation based on age (those younger<br />
than versus those older than 40 years) was noted between the two groups<br />
(p=0.88 and p=0.32 for the stapled and the hand-sewn anastomoses<br />
respectively). The average length of time from the operation to the<br />
EGD with balloon dilatation was 40.9 days in the stapled group and<br />
108 days in the hand-sewn group (p=0.004). One patient with a stapled<br />
anastomosis required 2 dilatations. Two patients in the stapled group had<br />
a GJ anastomotic leak (p=0.16) and did not require eventual dilatation. All<br />
patients were followed up for at least 4 months.<br />
CONCLUSION: The incidence of anastomotic stricture is significantly<br />
higher with a linear stapled technique compared to a hand-sewn<br />
gastrojejunal anastomosis in patients undergoing laparoscopic Roux-en<br />
-Y gastric bypass.<br />
S101<br />
HOW RELIABLE IS LAPAROSCOPIC COLORECTAL SURGERY COMPARED<br />
TO OPEN SURGERY FOR OCTOGENARIANS? Rodrigo A Pinto, Dan Ruiz,<br />
Yair Edden, Eric G Weiss, Juan J Nogueras, Steven D Wexner Cleveland<br />
Clinic Florida<br />
Background: Considering today’s increased longevity in the elderly<br />
population, and the increased size of that population major abdominal<br />
intervention is more frequently performed in octogenarians.<br />
Objective: To compare the surgical and postoperative outcomes of<br />
laparoscopic colorectal resections to open surgery in the octogenarian<br />
population.<br />
Methods: A retrospective analysis based on a prospectively maintained<br />
database of octogenarians who underwent laparoscopic or open elective<br />
colorectal resections from 2001 to 2008 was performed. Diagnosis,<br />
comorbidities, operative data and early postoperative complications were<br />
analyzed in this report.<br />
Results: One hundred ninety-nine octogenarians underwent colon<br />
resection. Laparotomy was performed in 116 patients (group I) and<br />
laparoscopic surgery in 83 (group II). The mean age was 84.3 vs. 84.7<br />
and the mean ASA score was 2.8 vs. 2.6 in groups I and II, respectively.<br />
Colorectal adenoma was the most common indication for surgery in both<br />
groups (77.6% vs. 54.2% in groups I and II, respectively) And right-hemi<br />
colectomy was the most frequently performed operation in group II (31%<br />
vs. 57.8% in groups I and II, respectively; p=0.0003). Open resections had<br />
a higher mean blood loss (286ml vs. 152ml, in groups I and II respectively;<br />
p=0.0002), and more patients required intraoperative transfusions<br />
(p=0.005), despite similar operative times. The conversion rate in the<br />
laparoscopic group was 25.3%. The laparoscopic patients had less overall<br />
complications, and clinical morbidity (p0.05) and mortality rates were 3.4% vs. 2.4% in groups I<br />
and II respectively.<br />
Conclusions: Laparoscopic colorectal resection is effective and safe for<br />
octogenarians with less blood loss and faster postoperative recovery<br />
associated with lower morbidity when compared to laparotomy.<br />
S102<br />
BARRETT’S ESOPHAGUS TREATMENT DILEMMA: PILLS VERSUS<br />
OPERATION: STATISTICAL ANALYSIS AND COST/EFFECTIVENESS Victor<br />
Bochkarev, MD, Dmitry Oleynikov, MD UNMC<br />
INTRODUCTION: Controversy over the management of barrett’s<br />
esophagus has been difficult to resolve due to the low incidence<br />
of progression to adenocarcinoma. A prospective study comparing<br />
thousands of patients with barretts esophagus randomized either into<br />
PPI or antireflux surgery group is costly and no likely to be perfomed. This<br />
study examined possible clinical outcomes of the two strategies and cost/<br />
effectiveness associated with treatment of Barrett’s esophagus.<br />
METHODS: A decision analysis tree (Markov Monte Carlo model) was<br />
used to track hypothetical cohort of patients with Barrett’s esophagus.<br />
The input variables were estimated by a pooled analysis of 74 published<br />
studies on a total of 23,368 patients. Possible clinical outcomes of the<br />
two treatment strategies, laparoscopic Antireflux procedure (LARP) vs.<br />
proton pump inhibitors (PPI), were analyzed. Cost/effectiveness ratio was<br />
calculated based on average cost and expected effectiveness of the two<br />
treatment strategies.<br />
RESULTS: Expected utility score for laparoscopic antireflux surgery<br />
was calculated to be .93 compared to that for PPI of .89. The model was<br />
sensitive to alterations in the probabilities of Regression, Progression<br />
and Death rates demonstrating preference to antireflux surgery over PPI<br />
alone. Cost/utility ratio for antireflux surgery was 38.9, and for PPI – 28.7,<br />
indicating favorable cost/effectiveness for PPI treatment.<br />
CONCLUSIONS: Our model, based on a comprehensive literature review,<br />
predicted that laparoscopic antireflux surgery was more effective strategy<br />
to achieve regression of Barrett’s esophagus. At the same time, PPI alone<br />
was less costly treatment strategy for patients with Barrett’s esophagus.<br />
12 th World Congress of Endoscopic Surgery<br />
135 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Video Abstracts<br />
V001<br />
IMPROVING FUNCTIONAL ESOPHAGEAL SURGERY WITH A “SMART”<br />
BOUGIE: ENDOFLIP® Silvana PERRETTA, MD, Bernard DALLEMAGNE,<br />
MD, Barry MACMAHON, MD, Jacopo D’AGOSTINO, MD, Hurng-Sheng WU,<br />
MD, Jacques MARESCAUX, MD IRCAD, University Hospital of Strasbourg,<br />
France - Show Chwan Memorial Hospital, Changhua, Taiwan<br />
Introduction: In order to improve the results of functional surgical<br />
procedures on the esophagus, the use of intraoperative esophageal<br />
manometry has been described to document the ablation of the lower<br />
esophageal sphincter (LES) high-pressure zone (HPZ) and to calibrate the<br />
pressure of the fundal wrap. An emerging physiology tool, the functional<br />
lumen imaging probe (Endoflip®, Crospon Ltd.), combines measurements<br />
of the EGJ resistance to distention and provides a geometrical<br />
reconstruction of the EGJ. The FLIP therefore represents a promising<br />
entirely new method to dynamically profile the EGJ that can show a live<br />
modification on EGJ capacity and diameter which would be of particular<br />
interest when performing functional operation on the esophagus such<br />
as antireflux procedures and Heller myotomy. Here we shows the clinical<br />
application of this emerging physiology tool in the surgical tratment of<br />
achalasia and GERD.<br />
Methods: The first case is that of a young woman with achalasia<br />
undergoing heller myotomy for persistent dysphagia after 2 failed<br />
endoscopic dilatation using the Endoflip® to follow the extend of<br />
the myotomy. The second case demonstrates its use to assess the<br />
configuration and quality of a posterior partial and Nissen fundoplication.<br />
In order to do this the EndoFLIP® catheter was placed transorally<br />
straddling the esophagogastric junction (EGJ). For the distension protocol<br />
the balloon was inflated to 30ml at a rate of 40ml per minute and data<br />
on 16 cross-sectional areas and pressure in the balloon was recorded.<br />
Two distensions were carried out at each stage of the procedure.<br />
Measurements were taken at the key steps of the heller myotomy and<br />
total and partial fundoplication .<br />
Results: Before the myotomy pressure in the balloon rose to 15 cmH20<br />
at a cross sectional area (CSA) of 25mm2 indicating that the EGJ is closed<br />
and tight. After dissection of the longitudinal muscle and the clasp fibres<br />
the pressure only rises to 8 cmH2O and the minimum CSA opens to 34<br />
mm2 indicating that the EGJ is now very compliant and flaccid. After the<br />
Heller wrap is complete the junction has become less compliant but it<br />
can open at its narrowest point to 35 mm2 at a pressure of 20 cmH2O.<br />
This suggests that the EGJ is tight but not as rigid as before so that<br />
when a bolus passes through it will stretch and open. The second part of<br />
the video demonstrates that the the Endoflip® acts as a “smart bougie”<br />
evaluating the orientation and position of a properly constructed floppy<br />
Nissen and posterior partial fundoplication.<br />
Conclusions: EndoFLIP can quantify changes in the distensibility of the<br />
EGJ. This “smart bougie” could be integrated into the surgical routine<br />
of esophageal functional surgery providing a good and immediate<br />
physiological visual feed-back of the surgical manoeuvres and could<br />
therefore improve outcome and facilitate surgical training and learning<br />
curve in this arena.<br />
V002<br />
REPAIR OF A HIATAL DEFECT USING A ROTATIONAL FALCIFORM<br />
FLAP Erica Sutton, MD, Adrian Park, MD University of Maryland School of<br />
Medicine<br />
Background: Closure of the hiatal defect in laparoscopic surgery of the<br />
foregut remains a challenging problem. Over the years, several materials<br />
have been used- varying compounds of nonabsorbable synthetics as<br />
well as absorbable biologic material. Yet, there is a high recurrence<br />
rate associated with primary closure and an unacceptably high rate of<br />
esophageal erosion and stricture associated with both synthetic and<br />
biologic material. Adding to the complexity of hiatal hernia repairs is<br />
the highly dynamic nature of the region, in which exists esophageal<br />
peristalsis and constant diaphragmatic excursion. We describe the use of<br />
the falciform ligament as a rotational flap for repair of such hiatal defects.<br />
Method: To create a rotational flap of the falciform ligament, ultrasonic<br />
dissection is used to detach the falciform from the anterior abdominal<br />
12 th World Congress of Endoscopic Surgery 136<br />
wall. Once fully mobilized, the flap is rotated to reach the esophageal<br />
hiatus. The flap is secured to the right crus using 2-3 interrupted sutures<br />
of 2-0 silk. On the left side, the flap is broadly attached to the diaphragm<br />
posteriorly and the crus anteriorly to provide overlapping coverage of the<br />
defect. Once the flap is sewn to the left crus, the flap completely covers<br />
the hiatal defect. As experience accrues, we are engaged in longitudinal<br />
follow-up.<br />
V003<br />
LAPAROSCOPIC CHOLECYSTECTOMY USING INTRAOPERATIVE<br />
FLUORESCENT CHOLANGIOGRAPHY Takeaki Ishizawa, MD PhD,<br />
Nobuhiro Harada, MD, Arata Muraoka, MD, Masayoshi Ijichi, MD PhD, Koji<br />
Kusaka, MD PhD, Masayuki Shibasaki, MD PhD, Yasutsugu Bandai, MD<br />
PhD, Norihiro Kokudo, MD PhD Department of Surgery, Central Hospital of<br />
Social Health Insurance<br />
OBJECTIVE: Although intraoperative cholangiography (IOC) has<br />
been recommended for avoiding bile duct injury during laparoscopic<br />
cholecystectomy (LC), radiographic IOC is time-consuming and the<br />
procedure itself may cause bile duct injury. We have developed a novel<br />
fluorescent cholangiography technique by applying the principle that<br />
indocyanine green (ICG) is excreted into bile and emits light with a peak<br />
wavelength of around 830 nm when illuminated with near-infrared<br />
light. The aim of this study was to evaluate the ability of fluorescent<br />
cholangiography to detect the bile duct anatomy during LC, especially in<br />
patients with accessory bile ducts.<br />
METHODS: In 43 patients undergoing laparoscopic cholecystectomy,<br />
ICG (2.5 mg) was intravenously injected before surgery. A fluorescent<br />
imaging system (prototype; Hamamatsu Photonics Co., Hamamatsu,<br />
Japan) comprised of a xenon light source and a laparoscope with a<br />
charge-coupled device camera, which can filter out light wavelengths<br />
below 810 nm, was utilized. Fluorescent cholangiography was performed<br />
before and during the dissection of the triangle of Calot by changing<br />
from color images to fluorescent images using a foot switch. The ability<br />
of fluorescent cholangiography to detect the bile duct anatomy was<br />
evaluated by comparing the fluorescent images with preoperative<br />
cholangiography findings.<br />
RESULTS: Fluorescent cholangiography delineated the cystic duct<br />
in all 43 patients and the cystic duct - common hepatic duct (CHD)<br />
junction in 41 patients prior to the dissection of the triangle of Calot<br />
(FIGURE). This technique also identified all the accessory bile ducts that<br />
were preoperatively diagnosed in 7 patients. We will present videos<br />
demonstrating the dissection of the triangle of Calot using fluorescent<br />
cholangiography in a patient with the normal bile duct anatomy and<br />
another two patients with an accessory hepatic duct draining the right<br />
lateral sector or the left paramedian sector of the liver and directly<br />
entering the CHD. No adverse reactions to the ICG or postoperative bile<br />
leaks were encountered.<br />
CONCLUSIONS: Fluorescent cholangiography enables real-time<br />
identification of accessory hepatic ducts as well as the cystic duct and<br />
the common hepatic duct during the dissection of the triangle of Calot.<br />
This safe and simple technique has the potential to become a standard<br />
practice for avoiding bile duct injury during LC, replacing conventional<br />
radiographic IOC.<br />
FIGURE<br />
Fluorescent cholangiography (A) before the dissection of the triangle of<br />
Calot clearly delineates the bile duct anatomy, which are unidentifiable on<br />
color images (B). Arrow shows the cystic duct - CHD junction.
Scientific Session Video Abstracts<br />
V004<br />
LAPAROSCOPIC D2 LYMPH NODE DISSECTION WITH TOTAL<br />
GASTRECTOMY AND HUNT LAWRENC JEJUNAL POUCH<br />
RECONSTRUCTION FOR CARCINOMA STOMACH C Palanivelu, MCh<br />
FACS FRCS, P Senthilnathan, MS DNB FRCS, S Rajapandian, MSFRCS, V<br />
Vaithiswaran, MS MRCS, R Sathiyamurthy, MS, P Praveen Raj, MS GEM<br />
Hospital<br />
Introduction: D2 lymph node dissection for early gastric cancer was<br />
popularized by the Japanese, though it is still controversial. The adequacy<br />
of laparoscopic node harvest remains doubtful. In this video, we present<br />
a laparoscopic D2 dissection with total gastrectomy and jejunal pouch<br />
anastamosis.<br />
Methods: The patient is placed supine with legs apart so that the surgeon<br />
stands between the legs. The dissection is commenced by disconnecting<br />
the greater omentum off the transverse colon, proceeding to clear the<br />
nodes at the splenic hilum (#10), gastrocolic (#6), nodes around superior<br />
mesenteric vein (#14v), and subpyloric nodes. Next, the duodenum was<br />
transected and the hepatoduodenal (#12a & 5), celiac axis (#9), and nodes<br />
around portal vein (#8p) were cleared. The nodes around left gastric<br />
artery (#7) were then cleared, and the dissection was continued up to the<br />
median arcuate ligament to clear nodes at the gastroesophageal junction<br />
(#1& 2). Nodes around the splenic artery (#11) were cleared. At this point,<br />
the esophagus is divided at the junction with a stapler. Esophagealpouch<br />
anastomosis was performed laparoscopically, while the pouch<br />
construction was done extracorporeally.<br />
Conclusion: Laparoscopic D2 dissection with total gastrectomy and<br />
jejunal pouch anastomosis is safe and feasible. It is comparable with the<br />
open technique regarding lymph node harvest and superior because of<br />
lower morbidity.<br />
V005<br />
TRANSCERVICAL VIDEOSCOPIC ESOPHAGEAL DISSECTION IN<br />
MINIMALLY INVASIVE ESOPHAGECTOMY Michael Parker, MD, Jason<br />
M Pfluke, MD, Kyle K Shaddix, MD, Leslie A Dowling, BS, Timothy A<br />
Woodward, MD, Horacio J Asbun, MD, C D Smith, MD, Steven P Bowers,<br />
MD Mayo Clinic Florida, Jacksonville, FL, USA<br />
Introduction: Currently, minimally invasive esophagectomy (MIE) is<br />
being performed using Video-Assisted Thoracoscopic Surgery (VATS) for<br />
mediastinal esophageal dissection. The VATS approach is still associated<br />
with pulmonary and cardiovascular morbidity, as well as incisional pain.<br />
This study investigates the feasibility of MIE using a single-incision<br />
transcervical videoscopic esophageal dissection (TVED). A simultaneous<br />
laparoscopic and transcervical videoscopic approach would allow MIE<br />
without the need for patient repositioning or single lung ventilation.<br />
Methods: Technical steps of the procedure include a standard cervical<br />
incision large enough to accommodate a modified hand-assisted access<br />
device. Cervical esophageal dissection was done in standard fashion.<br />
The modified access device was placed, and pneumomediastinum was<br />
established with laparoscopic trocars placed through the access port. The<br />
tracheoesophageal plane was developed above and below the thoracic<br />
inlet. Vagal nerves were identified, dissected, and divided distal to the<br />
recurrent branches. Standard minimally invasive laparoscopic techniques<br />
were used for the esophagogastric dissection routinely performed in<br />
MIE. Following specimen extraction, the animals were euthanized as per<br />
protocol.<br />
Results: A full circumferential dissection of the mediastinal esophagus<br />
was successfully accomplished in both animals using a single-incision<br />
TVED for MIE.<br />
Conclusions: Our research describes a novel approach for mediastinal<br />
dissection of the esophagus using a TVED approach that may avoid the<br />
potential morbidity of VATS while providing better visualization of the<br />
upper mediastinal esophagus when compared to the transabdominal,<br />
transhiatal approach.<br />
V006<br />
NOTES-ASSISTED TRASVAGINAL SPLENECTOMY: THE NEXT STEP FOR<br />
THE MINIMAL INVASIVE APPROACH TO THE SPLEEN EM Targarona,<br />
MD, C Gomez- Oliva, MD, R Rovira, MD, JC Pernas, MD, C Balague, MD,<br />
C Guarner-Argente, MD, S Sainz, MD, M Trias, MD Service of Surgery,<br />
Digestive Pathology, Gynecology and Radiology. Hospital de Sant Pau,<br />
UAB, Barcelona, Spain.<br />
Laparoscopic splenectomy (LS) is the gold standard for treatment of<br />
normal-medium sized spleens, but spleen morcellation and removal<br />
requires an enlargement of the wound port, specially for extraction of<br />
the intact spleen. Transvaginal extraction of the resected spleen was<br />
described in early 90’, but rarely used, and it didn’t avoid the use of<br />
multiple large diameter trocars (3-5 of 5-12 mm) trough the abdominal<br />
wound. NOTES description have favored hybrid less invasive approaches<br />
to the abdomen, but it has not been applied for spleen pathology. The<br />
Aim of this videopresentation is to show the technique used for a hybrid<br />
NOTES assisted transvaginal splenectomy:<br />
Case report and surgical technique: A 65 yrs. woman, multipara,<br />
without previous abdominal surgery diagnosed of a 6 cm multicystic<br />
splenic lesion. BMI: 30. Surgical steps: 1.- : Preoperative planning: Body<br />
CT in right lateral decubitus and 3D body reconstruction measuring the<br />
distance from the tip of the vagina to the splenic hilum (27,5 cm) . 2.-<br />
Table position: Patient placed in right decubitus with free access to the<br />
vulvar introitus. 3.- Pneumoperitoneum and 3 subcostal mininstruments<br />
ports (1 of 5 mm and 2 of 3 mm). 4.- Transvaginal 15 mm trocar insertion<br />
under laparoscopic control (5 mm scope), 5.- Insertion of a 13 mm<br />
colonoscope transvaginally for control of the dissection of the spleen<br />
with the subcostal instrumentation (Ucision and 3 mm instruments).<br />
6.- Transvaginal stapling transection of the splenic hilum with standard<br />
flexible tip 60 mm extralong (44 cm) endostapler (Ethicon). 7.- Insertion<br />
transvaginally of a bag (Endocatch II, Covidien) to recover the spleen, and<br />
extraction trough the Douglasl pouch. 8.- Closure of the vagina. Operative<br />
time was 180’, with uneventful recovery and discharge at 48 hrs.<br />
Conclusion: Transvaginal acces can be safely used for operative<br />
visualization, hilum transection and spleen removal, reducing at minimum<br />
the parietal wall trauma. Clinical, esthetic and functional advantages<br />
require further analysis.<br />
V007<br />
TOTAL ENDOSCOPIC GASTRIC BAND REMOVAL Kari Thompson, MD,<br />
Brian Wong, MD, Tom Savides, MD, Garth R Jacobsen, MD, Bryan Sandler,<br />
MD, Mark A Talamini, MD, Santiago Horgan, MD University of California,<br />
San Diego, San Diego, California, USA<br />
Introduction: Multiple surgical options are available for patients<br />
undergoing treatment for obesity. One of the most popular, due to short<br />
surgical times and low morbidity, is laparoscopic gastric band placement.<br />
Complications necessitating reoperation include prolapse and gastric<br />
band erosion. In our video we present a totally endoscopic removal of an<br />
eroded gastric band.<br />
Methods: A 61 year old female presented to bariatric surgery clinic with<br />
the complaint of abdominal pain. She had had a laparoscopic gastric<br />
band placed two years ago by a surgeon in Mexico. On endoscopy, the<br />
patient was found to have a complete erosion of her gastric band into<br />
her stomach. The patient was taken to the operating room and her port<br />
was first removed from her abdominal wall. Next, the endoscope was<br />
advanced into her stomach and the decision was made to remove the<br />
band endoscopically. An endoscopic guide wire was placed through a<br />
hole in the band that was easily accessed though the endoscope. An<br />
endoscopic snare then grasped the end of the wire, wrapping it around<br />
the band, and pulled it out of the patient’s mouth. An endoscopic<br />
lithotripsy overtube was then placed and the ends of the wire attached<br />
to the lithotripsy device. Using gentle pressure through the lithotripsy<br />
device, the band was divided. With the band completely divided, an<br />
end of the band was grasped using the endoscopic snare and removed<br />
through the patient’s mouth. On final endoscopy, the stomach showed no<br />
sign of perforation or bleeding.<br />
Results: The patient was kept overnight for observation and was<br />
137 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Video Abstracts<br />
discharged home on postoperative day 1. She had no perioperative<br />
complications. At one month follow up, she had no complaints.<br />
Conclusion: A total endoscopic removal of an eroded gastric band is<br />
important for a bariatric surgeon to have in their armamentarium due to<br />
the low morbidity of the procedure.<br />
V008<br />
LAPROSCOPIC COMPLETION RADICAL CHOLECYSTECTOMY Shailesh<br />
Puntambekar, MS, Seema Puntambekar, MD, Geetanjali Agarwal, MS,<br />
Neeraj Rayate, MS Galaxy-Care Laparoscopy Institute<br />
LAPROSCOPIC COMPLETION RADICAL CHOLECYSTECTOMY<br />
We describe a of a case of 60 years old female who underwent<br />
laparoscopic cholecystectomy elsewhere and incidentally on<br />
histopathology was diagnosed as adenocarcinomas of gall bladder<br />
with invasion up to the serosa. She was referred to our institute for<br />
laparoscopic completion radical cholecystectomy.<br />
Method : Five ports were placed with camera post at umbilicus (10mm<br />
0 degree ) 2 working ports a 10mm port placed at midline and5mm<br />
port placed in mid clavicular line and two 5mm ports for retraction<br />
one in epigastrium and one in subcoastal region in mid clavicular line.<br />
Laparoscopic segment 4A of liver was resected with total lymph nodal<br />
cleareance of the porta with excision of the cystic duct margin.<br />
Results : The operation time was 120 min and blood loss was 200 ml.<br />
Pathological examination revealed deposits of adenocarcinoma with<br />
moderate sclerosis. Lymph node at porta showed 8 positive nodes with 16<br />
lymph node harvested.<br />
Conclusion : Video shows that lap radical cholecystectomy is a feasible<br />
and oncological adequate treatment for carcinoma gall bladder.<br />
V009<br />
THORACOSCOPIC ESOPHAGECTOMY IN DORSOLATERAL POSITION :<br />
AN INNOVATIVE APPROACH - THE PAWAR TECHNIQUE Suraj B Pawar,<br />
MS FICS FAIS FMAS, Prashant Mullerpatan, MS FRCS, Reshma S Pawar,<br />
MBBS DGO Kolhapur Cancer Centre, India<br />
Aims: To assess the feasibility of Thoracoscopic Esophagectomy in the<br />
Dorso-Lateral position with the intention of reducing the disadvantages<br />
and increasing the benefits of lateral approach and prone approach which<br />
are the two conventional approaches.<br />
Methods : Thoracoscopic Esophagectomy is routinely performed in two<br />
positions. The left lateral decubitus position is the most commonly used<br />
position at most of the centres. However prone jack-knife position as<br />
described by Cushieri is another alternative.<br />
To combine the advantages and reduce the disadvantages of the two<br />
above mentioned positions we started performing this procedure in a<br />
Dorso-Lateral position since 1st October 2008 . This is a position midway<br />
between the Lateral and Prone position i.e. Left lateral position with an<br />
inclination making an angle of 45 degrees with the horizontal. Operating<br />
Surgeon and assistant are positioned anteriorly facing the ventral aspect<br />
of the patient. A three-port approach is taken with port placements in<br />
the 5th, 7th and 9th intercostals spaces in the posterior, mid and anterior<br />
axillary lines. Pneumothorax is created with CO2 pressure of 5 – 7 mm Hg.<br />
Although single lung ventilation is preferable the procedure can be done<br />
with routine dual lung ventilation with a 4th port being used to retract<br />
the lung if necessary.<br />
Esophagus is mobilized en-block with posterior mediastinal<br />
lymphadenectomy. The Azygous vein and right Bronchial artery are<br />
preferably preserved to maintain vascularity of right bronchus.<br />
Following this patient is turned supine and Stomach mobilization and<br />
coeliac dissection is done laparoscopically. Left neck incision is taken and<br />
esophagus is divided in the neck. Specimen is delivered in the abdomen<br />
and extra-corporeally through a mini-laparotomy. Gastric tube is prepared<br />
and brought in the neck through posterior mediastinum underneath the<br />
azygous vein and rt.bronchial artery for anastamosis in the neck.<br />
Results: In our experience of 24 cases, it was technically easier to do<br />
posterior mediastinal , especially the infra-azygous dissection in the<br />
dorso-lateral approach as compared to the lateral approach. Also bilateral<br />
recurrent laryngeal nerve lymph node dissection were carried out with<br />
12 th World Congress of Endoscopic Surgery 138<br />
technically the same ease as in lateral approach.<br />
The position kept the lung and blood away from the posterior<br />
mediastinum .<br />
One patient (4.16%) was converted to open procedure due to pulmonary<br />
adhesions. Duration of the thoracoscopic dissection was a mean 160<br />
min (100 – 250min) and thoracic blood loss was 100ml (50 – 300ml).<br />
Lymph nodes dissected were a median 19 (14-32). Anastamotic leak was<br />
seen in 2 patients (8.3%) both minor , which settled with conservative<br />
management. There was no mortality and the overall pulmonary<br />
complication rate was 21%.<br />
The video shows the procedure in the Dorso-Lateral Position as we<br />
routinely perform at our centre.<br />
Conclusion: Thoracoscopic Esophagectomy with Mediastinal<br />
Lymphadenectomy in the Dorso-Lateral position is a feasible , more<br />
convenient and a safe option which can combine the benefits of the<br />
conventional left lateral and prone approaches. Surgeon comfort is<br />
enhanced in terms of more comfortable operating position and improved<br />
ergonomics.<br />
V010<br />
SINGLE-INCISION LAPAROSCOPIC PROCTOCOLECTOMY WITH ILEAL<br />
J-POUCH-ANAL ANASTOMOSIS Alexandre Bouchard, MD, Jesse Lackey,<br />
SA, Tonia Young-Fadok, MD MS Mayo Clinic - Arizona<br />
Laparoscopic assisted proctocolectomy and ileoanal pouch-anal<br />
anastomosis is performed with multiple ports and an extraction incision.<br />
When compared to the traditional open procedure, the laparoscopic<br />
approach shortens the postoperative recovery and reduces adhesion<br />
formation.<br />
To further reduce the number of incisions and abdominal wall trauma,<br />
we used a single-incision device to perform this operation. This device<br />
permits the introduction of 3 instruments through the same small<br />
abdominal opening.<br />
This video presents a single-incision laparoscopic proctocolectomy with<br />
ileal J-pouch-anal anastomosis on a 19-year-old female with familial<br />
adenomatous polyposis syndrome. We introduced the single-incision<br />
device at the planned site for the diverting loop ileostomy.<br />
Key steps of the procedure demonstrated in this video are:<br />
1- Placement of single-port device via the planned ileostomy site.<br />
2- Establishment of the pneumoperitoneum and introduction of 3 trocars.<br />
3- Complete mobilization of the left and right colon with visualization and<br />
protection of duodenum, inferior vena cava and both ureters.<br />
4- Complete mobilization of the base of the terminal ileum to facilitate<br />
pouch creation.<br />
5- Complete rectal mobilization and transection at the pelvic floor.<br />
6- Ligation of the mesenteric vessels, using a bipolar device.<br />
7- Extraction of the specimen through the ileostomy site.<br />
8- Ileoanal J-pouch construction.<br />
9- Anastomosis.<br />
10- Diverting loop ileostomy<br />
At the end of the procedure, the only incision on the patient’s abdomen<br />
was that used for the diverting loop ileostomy. A single-incision<br />
proctocolectomy and ileoanal pouch-anal anastomosis is feasible, and can<br />
be performed safely.<br />
V011<br />
LAPAROSCOPIC REPAIR OF BOCHDALEK HERNIA Mohamad D Saad,<br />
DO, Jonathan Eng, MD, Frances Allocco, MD, Brian J Dunkin, MD, Patrick R<br />
Reardon, MD The Methodist Hospital<br />
Bochdalek hernia develops from mal-development in the fusion of the<br />
cephalic fold of the pleuroperitoneal membrane. It was first described<br />
by Bochdalek in 1848. It is most frequently diagnosed in neonates or<br />
children, while its presence in adult is rare. Perforation or necrosis of the<br />
involved organ is a feared complication and surgical repair constitutes the
Scientific Session Video Abstracts<br />
gold standard of treatment. Cadaveric examination discovered 1 in 7000.<br />
Yet, other attempts to study the incidence of Bochdalek hernia based on<br />
prospective CT studies found the incidence of about 13%.<br />
Here, we present a 42 year old male who presented with left flank pain,<br />
nausea, and vomiting. Initial CT was interpreted as upside down stomach<br />
and a hiatal hernia. During laparoscopy, the stomach, greater omentum,<br />
and the transverse colon were herniated through the defect into the right<br />
chest cavity. The defect measure about 13 cm in length. Fresh edges were<br />
initially obtained in order to anchor the mesh and the defect we closed<br />
primarily. A Gore-Tex soft mesh is placed with the ePTFE side facing the<br />
viscera.<br />
Post operatively, the patients symptoms resolved completely and was<br />
discharged the following day. Laparoscopic repair of Bochdalek hernia by<br />
closing the defect primarily and utilizing mesh is an effective and a safe<br />
approach.<br />
V012<br />
PNEUMORETROPERITONEUM: AN ALTERNATIVE APPROACH FOR<br />
COMPLETION ADRENALECTOMY IN A HOSTILE ABDOMEN David<br />
E Skarda, MD, Martin Walz, MD, Sayeed Ikramuddin, MD University of<br />
Minnesota, Minneapolis, USA, Kliniken Essen-Mitte, Essen, Germany<br />
A 43-year-old woman developed morning headaches, sweating,<br />
palpitations and uncontrolled hypertension for 12 months. She was<br />
known to have Von Hippel-Lindau and had previously had a left<br />
adrenalectomy in 1995 (open anterior approach) and a partial right<br />
adrenalectomy in 2000 (open lateral approach). She required an<br />
exploratory laparotomy in 1991 for a gunshot wound to the epigastrium.<br />
She suffered from type II diabetes mellitus, obesity (body mass index of<br />
42), hypothyroidism, gastritis, cirrhosis (Child’s-Pugh class A) and recurrent<br />
right renal stones.<br />
Her biochemical evaluation revealed elevated norepinephrine,<br />
normetanephrines, and vanillylmandelic acid. Computed tomography<br />
imaging revealed a heterogenous right adrenal mass (1.9 x 1.7 cm), bullet<br />
fragments in the right psoas, and absence of the right rectus abdominal<br />
muscle. Metaiodobenzylguanidine scan revealed a focal area of intense<br />
uptake within a retroperitoneal mass adjacent to the aorta and right<br />
kidney.<br />
We made the presumptive diagnosis of recurrent right<br />
pheochromocytoma and recommended right completion adrenalectomy.<br />
After preoperative blood pressure control with phenoxybenamine,<br />
propranolol and hydration, we performed a completion right<br />
adrenalectomy using a posterior retroperitoneoscopic approach. The<br />
operative time was 2.5 hours and our blood loss was less than 5 mL.<br />
Pathology revealed a 1 mm pheochromocytoma focus in a 3 x 2.5 cm<br />
specimen of normal adrenal gland, inflammatory tissue, and old surgical<br />
clips.<br />
The patient was discharged to home 3 days after her operation.<br />
Her symptoms resolved and she has required no antihypertensive<br />
medications.<br />
V013<br />
LAPAROSCOPIC BILATERAL PARTIAL ADRENALECTOMY FOR<br />
HEREDITARY PHEOCHROMOCYTOMA William W Hope, MD, Stanton T<br />
Smith, MD, Damon E Sheneman, DO, Jorge Gonzalez, MD, Cyrus A Kotwall,<br />
MD New Hanover Regional Medical Center<br />
Hereditary syndromes are responsible for a small number of<br />
pheochromocytomas. These hereditary pheochromocytomas are<br />
frequently bilateral and rarely malignant. Surgical treatment remains<br />
controversial secondary to the risk of Addisonian crisis and need<br />
for lifelong corticosteroid therapy associated with bilateral total<br />
adrenalectomy. Recently it has been reported that cortical sparing<br />
bilateral adrenalectomy is safe and can successfully avoid the need for<br />
replacement therapy.<br />
We present a case of a 21 year Hispanic male who presented with<br />
headaches, palpitations, and severe hypertension and was found to<br />
have bilateral pheochromocytomas by biochemical analysis, MIBG, and<br />
computed tomography scanning. The patient’s brother had previously<br />
undergone a right adrenalectomy and removal of extra adrenal<br />
pheochromocytoma. Patient underwent a laparoscopic bilateral cortical<br />
sparing adrenalectomy. The technique including pertinent positives,<br />
trocar placement, dissection, and method of excision are demonstrated.<br />
The patient had no postoperative morbidity and was discharged home<br />
on postoperative day 2. Pathology revealed a 23 gm/33 gm right cortical<br />
benign pheochromocytomas, both with low Ki67 proliferation indices.<br />
Two month follow-up ACTH stimulation test has shown normal 30 min<br />
aldosterone and 60 min cortisol stimulation levels. The patient has<br />
remained asymptomatic thus far, and has avoided the need for adrenal<br />
cortical replacement.<br />
Laparoscopic bilateral cortical sparing adrenalectomy is a safe, technically<br />
feasible treatment for hereditary pheochromocytoma. These patients<br />
must have long term follow-up including monitoring of the remnant<br />
gland for recurrence and yearly biochemical screening studies.<br />
V014<br />
LAPAROSCOPIC LEFT HEPATECTOMY WITHOUT INFLOW OCCLUSION<br />
USING MODIFIED ANTERIOR APPROACH C Palanivelu, MCh FACS FRCS,<br />
P Senthilnathan, MS DNB MRCS, N Anand Vijai, MS, R Rohit, MS, P Praveen<br />
Raj, MS GEM Hospital<br />
INTRODUCTION: Laparoscopic liver surgery requires high degree of<br />
anatomical knowledge, laparoscopic skills and technical know how of<br />
latest state of the art haemostatic and parenchymal split instruments,<br />
more so for major hepatic procedures like right hepatectomy .We describe<br />
the technique of laparoscopic left hepatectomy by anterior approach<br />
performed by single surgeon using two hand technique.<br />
METHOD: The patient is placed in modified lithotomy position and the<br />
surgeon stands between legs of the patient. We insert 6 ports and a<br />
hand port for parenchymal split or specimen retrieval. We begin with the<br />
division of falciform ligament and cystic duct and artery. Gall bladder is<br />
used to retract the liver cranially which exposes the porta hepatis. The left<br />
branch of hepatic artery, bile duct and portal vein dissected and divided,<br />
preserving branches to caudate lobe. Retrohepatic veins are then divided,<br />
followed by parenchymal division along the Cantlie’s line using different<br />
haemostatic and parenchymal splitting instruments which include<br />
ultrasonic shears, CUSA, Ligasure, clips and APC. As we reach the posterior<br />
surface of liver, left hepatic vein is dissected and divided using endoGIA<br />
stapler. <strong>Final</strong>ly, attachments of the left lobe are divided and specimen<br />
retrieved. The intra and post operative variables by this approach<br />
compares favorably with open approach.<br />
CONCLUSION: We conclude that laparoscopic left hepatectomy using<br />
modified anterior approach without inflow occlusionis safe and feasible,<br />
but should be performed only when expertise and equipments are<br />
available.<br />
V015<br />
LAPAROSCOPIC LUMBAR HERNIA REPAIR WITH BONE ANCHOR<br />
FIXATION Vanessa P Ho, MD, Gregory F Dakin, MD Weill Cornell Medical<br />
College-NewYork Presbyterian Hospital<br />
INTRODUCTION: Lumbar hernias are rare defects of the posterolateral<br />
abdominal wall. Surgical repair of lumbar hernias is challenging because<br />
they are bounded inferiorly by the iliac bone, which makes adequate<br />
mesh fixation difficult. We demonstrate a method of a laparoscopic<br />
lumbar hernia repair utilizing bone anchor fixation at the inferior border.<br />
METHODS: The patient is a 37-year old male with a history of motor<br />
vehicle collision who presented with a large left lumbar hernia and<br />
nonspecific abdominal pain. The patient had a Petit-type hernia, bordered<br />
by the external oblique muscle, the latissimus dorsi and the iliac crest. We<br />
opted to perform a laparoscopic mesh repair. Two Mitek GII QuickAnchor<br />
sutures were placed in the anterior superior iliac crest to provide inferior<br />
fixation of the mesh, with sufficient overlap of the mesh to prevent<br />
recurrence. The remainder of the mesh is fixed with standard laparoscopic<br />
tacks and transfascial sutures.<br />
RESULTS: The patient did well postoperatively and left the hospital on the<br />
first post-operative day. He has had no signs of recurrence at followup.<br />
12 th World Congress of Endoscopic Surgery<br />
139 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Video Abstracts<br />
CONCLUSIONS: The anatomic features of lumbar hernias creates several<br />
challenges. A number of surgical approaches have been described,<br />
including laparoscopic and open methods, as well as intraperitoneal<br />
and preperitoneal approaches and the use of flaps to cover the defects.<br />
However, limited fixation points for the mesh can lead to high recurrence<br />
rates. We demonstrated a method utilizing bone anchor fixation in a<br />
laparoscopic approach to overcome the challenge of inferior fixation.<br />
This provides a secure repair with good coverage of the defect, while<br />
maintaining the benefits of the minimally-invasive approach.<br />
V016<br />
RECONSTRUCTION OF THE ANTERIOR ABDOMINAL WALL WITH<br />
BILATERAL ENDOSCOPIC COMPONENT SEPARATION, LAPAROSCOPIC<br />
ASSISTED MEDIALIZATION OF THE RECTUS AND LAPAROSCOPIC<br />
MESH PLACEMENT Jawaid Kalim, MD, Scott Philipp, MD, Archana<br />
Ramaswamy, MD University of Missouri, Columbia<br />
Introduction: Standard laparoscopic repair of a large midline ventral<br />
hernia with mesh is frequently associated with seroma formation. In<br />
addition the rectus muscles cannot be medialized in large defects,<br />
thereby potentially leading to a less functional abdominal wall.<br />
We present a novel approach of repairing the midline abdominal wall<br />
defect while repairing the hernia laparoscopically with a mesh. We begin<br />
with bilateral endoscopic component separation and then medialize the<br />
rectus muscles with laparoscopically placed transfascial sutures. With<br />
bilateral component separation, we are able to completely close the hernia<br />
defect. We then reinforce the repair with a laparoscopically placed mesh.<br />
Method: A transverse skin incision is made two fingerbreadths below<br />
the costal margin at the anterior axillary line. The external oblique<br />
aponeurosis is identified and incised. A space is created between the<br />
external and internal oblique aponeurosis, by blunt finger dissection. A<br />
balloon dissector is then introduced in this space and further dissection<br />
is done under vision, with a 10mm 0-degree scope in the balloon. The<br />
balloon dissector is then removed and 10mm balloon port is placed.<br />
Carbon Dioxide is then insufflated into this space to a pressure of 12 to<br />
15mm of Hg. A 5mm port is placed inferiorly at the lateral aspect of the<br />
space created. The lateral border of the rectus sheath is identified and the<br />
external oblique aponeurosis one to two cm lateral to the rectus sheath is<br />
incised with a hook or scissors connected to electrocautery. Scarpa’s fascia<br />
is also incised to obtain additional release. The release incision extends<br />
from the pubic tubercle inferiorly to several centimeters above the<br />
costal margin superiorly. After completion of the myofascial release and<br />
advancement, this technique is repeated on the opposite side.<br />
We then enter the peritoneal cavity using the same skin incisions and<br />
pneumoperitoneum is created. After the hernia is reduced and all<br />
adhesions are taken down, we make tiny stab incisions in the midline<br />
and use transfascial sutures with laparoscopic assistance to bring the<br />
rectus sheath to the midline. After medialization of the rectus muscle,<br />
we proceed with laparoscopic placement and fixation of mesh in the<br />
standard fashion.<br />
Result: We have successfully performed this procedure on 4 patients and<br />
on follow up, have one small asymptomatic seroma with excellent patient<br />
satisfaction.<br />
V017<br />
SINGLE INCISION LAPAROSCOPIC RIGHT COLECTOMY Wai Lun Law,<br />
MD, Joe Fan, MD, Jensen Poon, MD The University of Hong Kong<br />
The video shows a single incision laparoscopic right colectomy for a<br />
patient with a big sessile polyp at the ascending colon, which could not<br />
be removed endoscopically.<br />
The patient was a 49-year-old lady with good past health. She underwent<br />
colonoscopy because of change in bowel habit. A 3-cm sessile polyp was<br />
found at the ascending colon and it could not be removed endoscopically.<br />
Biopsy of the polyp showed foci of intramucosal adenocarcinoma. She<br />
underwent a laparoscopic right colectomy using the single port. The<br />
video shows the operation and the operation was successfully performed<br />
and the patient recovered uneventfully.<br />
V018<br />
LAPAROSCOPIC REPAIR OF TRAUMATIC FLANK HERNIA Mun Jye<br />
Poi, MD, Yuri W Novitsky, MD University Of Connecticut Health Center,<br />
Farmington, Connecticut<br />
Introduction: Traumatic flank hernias are caused by a blunt abdominal<br />
trauma with resultant detachment of the oblique musculofascial<br />
complex at the iliac crest and/or costal margin. Given such proximity<br />
to the bony structures and essential absence of the healthy fascia to<br />
anchor the mesh, traumatic flank hernias represent a challenging surgical<br />
problem. Although laparoscopic repair of ventral hernias has become<br />
very common, laparoscopic approach to traumatic flank hernias has not<br />
been established well. We present a video detailing the technique of<br />
laparoscopic repair of traumatic flank hernia.<br />
Methods: The patient was placed in the decubitus position. Entrance<br />
to the abdomen was performed using Optiview trocar in the subcostal<br />
area. Operative steps included a complete reduction of the hernia sac,<br />
pre/retroperitoneal dissection to expose the entire lateral edge of a<br />
psoas muscle, defect closure with trans-abdominal sutures, wide mesh<br />
overlap, transabdominal suture fixation followed by the use of Mitek bone<br />
anchors.<br />
Results: The operative time was 180 minutes. Estimated blood loss was<br />
100ml. The defect size was 12 cm x 6 cm and the size of the mesh used<br />
was 20cm x 15cm. There were no perioperative complication. Hospital<br />
stay was 5 days. The patient returned to full activities by 1 month. At<br />
follow-up of 11 months, there was no recurrence.<br />
Conclusions: Laparoscopic approach to traumatic flank hernia is feasible<br />
and safe. It is associated with minimal hospital stay and fast functional<br />
recovery. The key components of our approach include wide pre/<br />
retro-peritoneal dissection with subsequent wide mesh coverage with<br />
mandatory fixation to bony structures using anchors/screws. We believe<br />
the laparoscopic approach should be considered for most patients with<br />
traumatic flank hernias.<br />
V019<br />
LAPAROSCOPIC REPAIR OF A DUODENAL ATRESIA AND LADD’S<br />
PROCEDURE IN A NEONATE Steven S Rothenberg, MD Rocky Mountain<br />
Hospital For Children<br />
Purpose: To demonstrate current refinements of technique in<br />
performing a duodenal anastomosis in a neonate with duodenal atresia.<br />
Methods: A 33 week premature infant with a prenatal diagnosis of<br />
Duodenal atresia was explored laparoscopically on day two of life for<br />
repair. The patients weight was 2 Kg. Two 3mm ports and one 4mm<br />
port were used for the procedure. The patient was also found to have<br />
malrotation at the time of surgery. The procedure consisted of a Ladd’s<br />
procedure and duodenoduodenostomy. Techniques of abdominal wall<br />
retraction sutures are demonstrated.<br />
Results: The procedure was completed successfully laparoscopically. The<br />
procedure took 60 minutes. An NG tube was used for 5 days and feeds<br />
were started on post-op day 6.<br />
Conclusion: This video demonstrates that a laparoscopic<br />
duodenoduodenostomy and Ladd’s procedure is efficacious and safe<br />
even in a small premature infant.<br />
V020<br />
LAPAROSCOPIC REPAIR OF ACUTELY INCARCERATED<br />
PARAESOPHAGEAL HERNIA Elizabeth Honigsberg, MD, Barry Salky, MD<br />
FACS The Mount Sinai Hospital, New York<br />
This is an 80 year old male who presented with acute incarceration<br />
of a known paraesophageal hernia. He was reduced by emergency<br />
endoscopy. The past history is significant for hypothyroidism and GERD,<br />
long standing. The video demostrates the amount of stomach that can<br />
necrose if this emergent condition is not operated quickly. The edema<br />
in the tissues, especially at the hernia sac/crural fiber junction, can make<br />
the dissection difficult. This is clearly demonstrated. The importance of<br />
adequate esophageal length is demonstrated, as well as why complete<br />
12 th World Congress of Endoscopic Surgery 140
Scientific Session Video Abstracts<br />
mobilization of the posterior attachments along with sac excision, are so<br />
important in acheiving reduction of the stomach. The proper dissection<br />
planes are demonstrated in this video. The technique of biodegradable<br />
mesh placement is shown.<br />
V021<br />
GALLBLADDER VOLVULUS: A VIDEO CASE REPORT Justin K Lawrence,<br />
MD, Nikhil Pawa, MD, Matthew G Tutton, MD, Antonio Privitera, MD<br />
Colchester University Hospital, UK<br />
Summary: We present a case report from September 2009 at our<br />
Laparoscopic Institution. The case attended as an emergency in an 84<br />
year old female. Initially treated under medical care with generalised<br />
abdominal pain, an abdominal ultrasound scan demonstrated an<br />
inflamed, thick-walled gallbladder and a diagnosis of cholecystitis<br />
was made. At laparoscopy, the gallbladder was clearly necrosed and<br />
seemingly torted. We proceeded to laparoscopic cholecystectomy and<br />
following literature review, felt that this would represent an interesting<br />
video case report.<br />
V022<br />
TOTALLY EXTRAPERITONEAL REPAIR OF A SPIGELIAN HERNIA Frances<br />
Allocco, MD, Patrick Reardon, MD, Mohamed Saad, DO, Brian Dunkin, MD<br />
The Methodist Hospital<br />
TOTALLY EXTRAPERITONEAL REPAIR OF A SPIGELIAN HERNIA<br />
Allocco, Frances MD; Reardon, Patrick MD; Saad, Mohamed MD; Dunkin,<br />
Brian MD<br />
Spigelian hernias are rare and account for up to 2% of abdominal wall<br />
hernias. In the past these were repaired using an open technique, but<br />
over the past two decades, there have been a growing number of reports<br />
of laparoscopic repairs. Over the past decade we have seen these reports<br />
to include totally extraperitoneal repairs.<br />
Here we present a video of a totally extraperitoneal repair of a Spigelian<br />
hernia and briefly review Spigelian hernias and their laparoscopic repair,<br />
based on review of the literature.<br />
The patient is a 65 year old female with a bulge in the right lower<br />
quadrant of her abdomen. She noted the bulge a year previous but did<br />
not seek medical attention at that time. Over the course of six months,<br />
she began experiencing occasional pain in the area which was becoming<br />
more frequent, and presented to us.<br />
Our plan was to perform a totally extraperitoneal repair of this hernia. At<br />
the beginning of the procedure we placed a 2mm trocar and insufflated<br />
the peritoneal cavity, and confirmed the hernia to be a Spigelian hernia.<br />
We then repaired the hernia using a totally extraperitoneal approach,<br />
using a 2mm and a 5mm port. After reducing the hernia sac we measured<br />
the defect to be 1.2 x 4 cm. Our dissection allowed for a 6 x 6 inch piece of<br />
mesh to be tacked in place. At the end of the procedure we re-insufflated<br />
the peritoneal cavity and saw our mesh lying completely flat.<br />
The patient went home the same day and was seen in follow-up with an<br />
intact repair and no further complaints.<br />
Spigelian hernias usually present in patients 40 to 80 years old. Physical<br />
exam correctly identifies approximately 50%, as many are interparietal<br />
hernias, and so do not present with a bulge. Most are 1 to 2 centimeters<br />
with a risk of incarceration as high as 24.1% and a strangulation risk of 2.4-<br />
14%. Recurrence is low for open and laparoscopic repair. Currently there is<br />
one prospective randomized controlled trial of open versus laparoscopic<br />
elective Spigelian hernia repair by Moreno-Egea et al in 2002. It showed<br />
decrease in morbidity and hospital stay and concluded TEP repair to offer<br />
the best results.<br />
Here we show how a Spigelian hernia can be laparoscopically diagnosed<br />
and treated with a totally extraperitoneal approach, using 2 and 5 mm<br />
ports, in a manner similar to an inguinal hernia repair.<br />
V023<br />
LAPAROSCOPIC RESECTION OF A PRESACRAL SCHWANNOMA.<br />
Alexander Ramirez, Samuel Szomstein, Raul Rosenthal Cleveland Clinic<br />
Florida<br />
Background: Benign shwannomas are tumors arising from the neural<br />
sheath of peripheral nerves (schwannoma cells).The Schwannoma is the<br />
most common benign retroperitoneal tumor in adults. Few cases have<br />
been reported in the presacral space. Complete resection is treatment of<br />
choice for these tumors. To our knowledge not many reports describe the<br />
laparoscopic approach for resection of this unusual neoplasm.<br />
Case report: This is a 27 year-old female that was presented in<br />
consultation after she had been diagnosed 2 years ago with a right<br />
adnexal paramedian mass. An MRI showed a mass in the presacral space<br />
measuring 4.3 x 4.4 x 4.4 cm with demonstrated low signal intensity<br />
and did blush with dye. After obtaining informed consent, the patient<br />
underwent a diagnostic laparoscopy and biopsy by a gynecologist.<br />
Pathology report showed spindle cell neoplasm, possibly a benign nerve<br />
sheath tumor. The patient underwent a re-laparoscopy. The pelvic and<br />
presacral space was opened by means of blunt and sharp dissection. The<br />
mass was dissected from attachments to the retroperitoneal area, placed<br />
in an Endobag and extracted through the enlarged infraumbilical trocar<br />
site. The peritoneal floor was suture closed with a running 2-0 Vycril<br />
suture.<br />
Results: No perioperative complication, the patient was discharged home<br />
on postoperative day three with an intact neurological exam.<br />
Conclusions: The laparoscopic approach appears to be a safe, feasible<br />
option to treat presacral schwannomas. The benefit of this approach was<br />
evident by achieving a complete resection of the tumor, short hospital<br />
stay, no complications and high patient satisfaction.<br />
V024<br />
ENDOSCOPIC TRANSESOPHAGEAL MEDIASTINAL AND THORACIC<br />
LYMPH NODE DISSECTION WITH EN BLOC RESECTION (VIDEO<br />
SUBMISSION) Brian G Turner, MD, Denise W Gee, MD, Sevdenur Cizginer,<br />
MD, Min-Chan Kim, MD, Yusuf Konuk, MD, Mari Mino-Kenudson, MD,<br />
Patricia Sylla, MD, David W Rattner, MD, William R Brugge, MD FASGE (1)<br />
Gastrointestinal Unit, Massachusetts General Hospital, (2) Department of<br />
Surgery, (3) Department of Pathology, Massachusetts General Hospital,<br />
Boston, MA<br />
This video demonstrates a novel, transesophageal endoscopic technique<br />
for mediastinal and thoracic lymph node dissection and en bloc<br />
lymphadenectomy using a Natural Orifice Transluminal Endoscopic<br />
Surgery (NOTES®) technique. Using a swine model, a double-channel<br />
gastroscope equipped with an endoscopic cap band mucosectomy<br />
device is used to create a small esophageal mucosal defect. Next, a<br />
short submucosal tunnel is created using the tip of the endoscope and<br />
closed biopsy forceps. A hook knife is then used to incise the muscular<br />
esophageal wall and to enter the mediastinum. Subsequently, endoscopic<br />
scissors are used to create a small hole in the visceral pleura and the<br />
endoscope is passed through it and into the thorax. Once in the thorax,<br />
the endoscope is carefully advanced up the thoracic wall and lymph<br />
node stations are identified high in the apex of the lung near the trachea.<br />
The parietal pleura overlying the target lymph node is then incised with<br />
the hook knife to better expose the lymph node. Prototype endoscopic<br />
Maryland dissectors are used to dissect the LN away from surrounding<br />
structures. Care is taken to preserve the lymph node architecture and to<br />
not damage the lymphovascular bundle. After lymph node dissection is<br />
complete, an electrocautery snare is placed around the entire node and<br />
closed around the lymphovascular bundle, while a second snare is used to<br />
secure the body of the lymph node and facilitate retrieval. This technique<br />
prevents the resected node from falling freely into the thoracic cavity<br />
where retrieval can be challenging. The lymph node is then removed<br />
by withdrawing the endoscope through the thorax, mediastinum,<br />
submucosal tunnel, esophagus and ultimately out of the natural orifice.<br />
Necropsy photos are shown demonstrating one of the surgical sites where<br />
a paratracheal node was removed. Histology slides also demonstrate the<br />
12 th World Congress of Endoscopic Surgery<br />
141 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Video Abstracts<br />
preserved, architecturally intact, lymph node specimens. The procedure<br />
is carried out with minimal bleeding and trauma to the lymph node. In<br />
summary, this video demonstrates that transesophageal NOTES® can<br />
accomplish mediastinal and thoracic lymph node dissection and resection<br />
and provide architecturally intact specimens for histologic examination.<br />
V025<br />
LAPAROSCOPIC SLEEVE GASTRECTOMY AS A TREATMENT OPTION<br />
FOR ACUTE GASTRIC FUNDUS NECROSIS AFTER LAPROSCOPIC REDO<br />
PARAESOPHAGEAL HERNIA REPAIR AND SLIPPED REDO NISSEN<br />
FUNDOPLICATION Ismael Court, Omar Bellorin, Sheetal Patel, Samuel<br />
Szomstein, Raul J Rosenthal Cleveland Clinic Florida<br />
Introduction: This video illustrates the use of laparoscopic techniques<br />
to resolve an acute gastric fundus necrosis after laparoscopic redo<br />
Paraesophageal Hernia Repair (PHR) and redo Nissen Fundoplication (NF)<br />
for a slipped NF.<br />
Case Report: A sixty six-year-old female 24 hours status post a redo<br />
procedure for recurrent paraesophageal hernia with slipped NF and<br />
high-grade dysphagia, who presents with CT Scan showing large pleural<br />
effusion, worsening of the respiratory status and an upper gastro<br />
intestinal series showing contrast extravasation. The patient underwent<br />
a diagnostic laparoscopy. During the procedure the fundoplication was<br />
taken down, identifying two areas of perforation of the gastric fundus,<br />
most likely due to ischemic necrosis. A 32-French Ewald tube was passed<br />
into the distal stomach, and with the aid of a green cartilage linear stapler,<br />
the stomach was vertically transected, and the gastric fundus resected.<br />
The staple line was reinforced with a running 2-0 absorbable suture and a<br />
sub hepatic drain was placed as well.<br />
Results: The patient tolerated the procedure well. The postoperative<br />
course was remarkable for a slow recovery of the pulmonary status.<br />
The patient was started on oral feeds on postoperative day # 3 and was<br />
discharged home on postoperative day #17. The long term follow-up and<br />
recovery were uneventful.<br />
Conclusion: Acute gastric necrosis after PHR and NF is an unusual<br />
complication resulting most likely due to an error in judgment. Early<br />
recognition and surgical treatment are paramount to decrease mortality.<br />
The laparoscopic approach and sleeve gastrectomy are feasible options in<br />
the management of this complication.<br />
V026<br />
THE FEAR OF TRANSGASTRIC CHOLECYSTECTOMY:<br />
MISINTERPRETATION OF THE BILIARY ANATOMY Silvana PERRETTA,<br />
MD, Bernard DALLEMAGNE, MD, Gianfranco DONATELLI, MD, Didier<br />
MUTTER, MD, Pierre ALLEMANN, MD, Hurng-Sheng WU, MD, Jacques<br />
MARESCAUX, MD IRCAD, University Hospital of Strasbourg, France - Show<br />
Chwan Memorial Hospital, Changhua, Taiwan<br />
Introduction: The prevention of major injury at cholecystectomy relies<br />
on the accurate dissection of the cystic duct and artery, and avoidance of<br />
major biliary and vascular structures.<br />
The advent of NOTES cholecystectomy has led to a new look and insights<br />
into biliary anatomy especially of the Calot’s triangle. Here we show the<br />
clinical case of a NOTES transgastric cholecystectomy for uncomplicated<br />
cholelithiasis, in which misinterpretation of biliary anatomy occurred.<br />
Methods and procedure: After induction of pneumoperitoneum using<br />
a Veress needle, a single 5mm transparietal port was introduced at the<br />
umbilicus to ascertain the feasibility of transgastric cholecystectomy<br />
ensure safe gastrotomy creation and closure, insufflation and monitoring<br />
of the pneumoperitoneum and to allow the use of a 5mm laparoscopic<br />
clip applier. Transgastric access was obtained using a double channel<br />
endoscope (KARL STORZ® Endoskope, Germany) under laparoscopic<br />
visual control. An endoscopic needle-knife was used to create a full<br />
thickness puncture on the anterior wall in the mid-body of the stomach<br />
expanded using a 18mm balloon dilator to allow passage of the 12mm<br />
gastroscope. The laparoscopic optic could then be switched to a 5mm<br />
laparoscopic grasper to expose the gallbladder. Dissection started using<br />
the endoscopic flexible tools at the junction between the infundibulum<br />
and what was thought to be the cystic duct. During the dissection the<br />
12 th World Congress of Endoscopic Surgery 142<br />
size and the orientation of the cystic duct appeared unclear. Decision was<br />
made to switch to a laparoscopic view to re-orient the dissection and<br />
define the correct planes. At this point we realized that the dissection<br />
of the triangle of Calot although started in close proximity to the<br />
gallbladder, was far to low and that we had mistaken the common bile<br />
duct with the cystic duct. Fortunately the dissection maneuvers had<br />
been performed with extreme care and no injury to the CBD occurred.<br />
Once the biliary anatomy was clarified the vision was switched back to<br />
the endoscope but a 2mm grasper was introduced to improve retraction.<br />
Cholecystectomy was performed in a standard fashion. A laparoscopic<br />
hook was used to skeletonized, the cystic duct and artery that were<br />
clipped using a laparoscopic clip applicator. At the end of the dissection,<br />
the operative site was checked to ensure haemostasis and biliostasis. The<br />
gallbladder was extracted through the gastrotomy under laparoscopic<br />
control and the gastrotomy closed with extracorporeal stitches by means<br />
of a 2mm laparoscope and a 3mm needle holder inserted side by side into<br />
the 5mm umbilical port.<br />
Conclusions: Specific anatomical distortions due to the NOTES technique,<br />
along lack of exposure,with the present methods of retraction tend to<br />
distort the Calot’s triangle by actually flattening it rather than opening<br />
it out. Their contribution in producing injury and a preventive strategy<br />
based need to be investigated . At this stage whenever the anatomy<br />
of the biliary tract is confusing as happened in this case, a temporary<br />
“conversion” to a laparoscopic view, more familiar to the surgeon’s eye and<br />
therefore clearer that will provide a better understanding of the location<br />
of the common bile duct in respect to the cystic duct.<br />
V027<br />
LAPAROSCOPIC MEDIAN ARCUATE LIGAMENT RELEASE FOR CELIAC<br />
ARTERY DECOMPRESSION Arthur Rawlings, MD MDiv, Margaret Frisella,<br />
RN, L. Michael Brunt, MD Washington University<br />
Median arcuate ligament syndrome is a rare cause of abdominal pain<br />
that results from the celiac artery being narrowed by the insertion of<br />
the muscle fibers of the diaphragm or fibrous bands of the celiac nerve<br />
plexus. Patients typically have symptoms of weight loss, postprandial<br />
abdominal pain, and nausea or vomiting. Operative management,<br />
laparoscopic or open, involves completely dividing these fibers to release<br />
the compression of the celiac artery. There have been few reports to date<br />
of laparoscopic treatment of this condition. In this video, laparoscopic<br />
release of the median arcuate ligament is shown in a 36 year old female<br />
who had a one year history of abdominal pain and a 35 pound weight<br />
loss resulting in a BMI of 17.5 kg/m 2 . The patient had a history of MALT<br />
lymphoma but an extensive workup was otherwise negative. She<br />
ultimately had an MR angiogram which showed a celiac artery stenosis<br />
with post-stenotic dilatation and collateral pancreatoduodenal vessels.<br />
Laparoscopic exploration and decompression of the celiac artery was<br />
performed. Intraoperative ultrasound showed improved flow in the celiac<br />
artery after decompression. The patient was discharged the day after<br />
surgery without any complications. At follow-up, her symptoms were<br />
significantly improved.<br />
V028<br />
LAPAROSCOPIC GASTRIC ACCESS FOR ENDOSCOPIC RETROGRADE<br />
CHOLANGIOPANCREATOGRAPHY (ERCP) FOLLOWING ROUX-EN-Y<br />
GASTRIC BYPASS (RYGB) Sachin S Kukreja, MD, Matthew I Goldblatt, MD,<br />
James R Wallace, MD PhD Froedtert Memorial Lutheran Hospital and the<br />
Medical College of Wisconsin<br />
Patients who have undergone roux-en-y gastric bypass may require upper<br />
endoscopic evaluation for a variety of reasons which may or may not<br />
be related to their surgical procedure. The ability to access the remnant<br />
stomach or biliary tree by the traditional transoral route may be only<br />
possible through specialized endoscopic or percutanous procedures, or<br />
even laparotomy due to the altered foregut anatomy. The following video<br />
demonstrates a method of accessing the gastric remnant and performing<br />
percutaneous Endoscopic Retrograde Cholangiopancreatography (ERCP)<br />
through a laparoscopic gastrostomy. Such an approach provides access to<br />
the papilla without the need for specialized equipment. In our particular<br />
patient, cholangiography and sphincterotomy were required for
Scientific Session Video Abstracts<br />
Sphincter of Oddi dysfunction; however, the approach could also be used<br />
to evaluate the biliary tree for evaluation of a multitude of either benign<br />
or malignant pathologies.<br />
V029<br />
SLEEVE GASTRECTOMY WITH ILEAL INTERPOSITION FOR TYPE 2<br />
DIABETES Augusto C. Tinoco, Luciana J El-Kadre, Renam Tinoco São Jose<br />
do Avaí Hospital<br />
This video shows technical details for the surgical treatment of type 2<br />
diabetes in a no-obese population . This surgery, sleeve gastrectomy with<br />
ileal interposition, was done under approved protocol in 20 patients. The<br />
principle used was the ileal-brake.<br />
V030<br />
LAPAROSCOPIC RESECTION OF AN OCCLUDED ROUX LIMB Frances<br />
Allocco, MD, Patrick Reardon, MD, Brian Dunkin, MD, Mohamed Saad, DO<br />
The Methodist Hospital<br />
Allocco, Frances MD; Reardon, Patrick MD; Dunkin, Brian MD; Saad,<br />
Mohamed MD<br />
The purpose of of our video is to present a patient who had a laparoscopic<br />
roux-en-Y gastric bypass, who years later developed occlusion of her<br />
roux limb. This is demonstrated endoscopically and was repaired<br />
laparoscopically.<br />
The patient is a 38 year old woman with a history of a laparoscopic rouxen-Y<br />
gastric bypass. She presented seven years later with nausea and<br />
vomiting. She had an open internal hernia repair at an outside hospital,<br />
but her symptoms persisted. She was treated by the author, with a<br />
laparoscopic lysis of adhesions. Following that surgery, her symptoms<br />
persisted. Preoperative endoscopy revealed severe ulceration with<br />
complete obstruction of the roux limb.<br />
We performed intraoperative endoscopy to confirm this and<br />
laparoscopically resected the occluded portion of the roux limb. We<br />
reanastomosed the distal end of the remaining roux limb distal to the<br />
previous jejunojejunostomy.<br />
In follow-up, the patient has done well and is tolerating a diet without any<br />
problems.<br />
This is a first report of an occluded roux limb after roux-en-Y gastric<br />
bypass. Bowel obstruction after gastric bypass has many etiologies,<br />
including internal hernias and adhesions, both of which this patient was<br />
surgically treated for. Obstruction may occur early or late. This patient<br />
presented years later with a complete obstruction of her roux limb from<br />
severe ulceration. Most ulcers in gastric bypass patients are marginal<br />
ulcers at the gastrojejunostomy and usually do not present years later.<br />
These can often be treated medically with proton pump inhibitors.<br />
If stenosis develops, it may be able to be managed endoscopically<br />
by dilation. Here endoscopy served as a helpful diagnostic tool and<br />
confirmed the location of the segment of bowel which we removed<br />
laparoscopically.<br />
V031<br />
LAPAROSCOPIC HEPATICODUODENOSTOMY David J Kaczorowski, MD,<br />
Steven J Hughes, MD University of Pittsburgh Medical Center<br />
INTRODUCION: Rapid weight loss following bariatric surgery can result<br />
in cholelithiasis and related complications, including choledocholithiasis.<br />
Furthermore, a Roux-en-Y gastric bypass can complicate the management<br />
of choledocholithiasis. CASE HISTORY: Here, we present the case of a<br />
72 year-old woman with a history of morbid obesity who underwent a<br />
Roux-en-Y gastric bypass and a cholecystectomy for cholelithiasis. She<br />
subsequently developed recurrent choledocholithiasis complicated<br />
by cholangitis, which was managed conservatively with the use of<br />
percutaneous transhepatic cholangiocatheter (PTC). She developed<br />
a biliary stricture secondary to false passage of a PTC and went on to<br />
suffer further episodes of cholangitis. After over a year and a half of<br />
further conservative management, she was offered a laparoscopic<br />
hepaticoduodenostomy.<br />
OPERATIVE COURSE: After placing trocars, dense omental adhesions<br />
were dissected from the undersurface of the liver. A liver retractor was<br />
then placed. The bile duct was then dissected circumferentially. Next, a<br />
ductotomy was made approximately 1 cm proximal to the insertion of<br />
the bile duct into the pancreatic head. The PTC catheter was grasped<br />
and pulled from the duct. The catheter was then cut so that it would<br />
retract back into the duct away from the intended site of anastomosis.<br />
A white load of the Endo GIA stapling device was used to divide the<br />
duct distal to the ductotomy. Next, an enterotomy was then created<br />
on the cephalad antimesenteric border of the duodenum. Using a 4-0<br />
PDS suture and diamond dust coated graspers, we performed a running<br />
hepaticoduodenostomy, starting on the duct side to allow forehand<br />
suturing. The right upper quadrant was irrigated and hemostasis was<br />
assured. The 12 mm trocar site and skin incisions were then closed.<br />
RESULTS: A postoperative cholangiogram revealed free passage of<br />
contrast into the duodenum. The patient did well and was discharged<br />
home on the third postoperative day.<br />
CONCLUSIONS: Laparoscopic hepaticoduodenostomy can serve as a safe<br />
and effective management option for patients with distal biliary strictures.<br />
V032<br />
USE OF A NOVEL PERCUTANEOUS RETRACTION DEVICE AND<br />
MAGNETIC ANCHORING AND GUIDANCE SYSTEM (MAGS) HELPS<br />
RE-ESTABLISH THE CRITICAL VIEW AND IMPROVES SURGEON<br />
PERFORMANCE WHILE MIMICKING THE FOUR PORT TECHNIQUE<br />
IN SINGLE SITE LAPAROSCOPIC (SSL) CHOLECYSTECTOMY Rohan<br />
A Joseph, MD, Nilson A Salas, MD, Michael A Donovan, MS, Patrick R<br />
Reardon, MD, Barbara L Bass, MD, Brian J Dunkin, MD Methodist Institute<br />
for Technology Innovation and Education (MITIE), Department of<br />
Surgery, The Methodist Hospital, Houston- TX<br />
Introduction: SSL, though promising, introduces ergonomic challenges<br />
due to loss of instrument triangulation as obtained in conventional<br />
laparoscopy. This limitation makes establishing the critical view during<br />
dissection of the Triangle of Calot (TOC) difficult and has resulted in a<br />
variety of strategies to overcome the problem. This study investigates<br />
use of a novel percutaneous grasper that mimics a standard laparoscopic<br />
instrument and MAGS in aiding surgeons to perform SSL cholecystectomy<br />
more easily and with a technique that closely mimics four-port<br />
cholecystectomy.<br />
Methods: SSL cholecystectomy was performed on four female cadavers<br />
by an expert laparoscopic surgeon with limited experience in SSL. A<br />
15–18mm incision was made at the umbilicus and the MAGS introduced<br />
into the abdomen. MAGS consists of an oblong (7.8cm × 14mm) magnetic<br />
internal effector with a retractable monopolar cautery hook (6.3cm) and<br />
is coupled across the abdominal wall to an external hand-held magnet.<br />
By sliding the external magnet over the abdominal wall and applying<br />
external pressure, subtle motions of the hook can be achieved. Following<br />
MAGS introduction, a commercially available port comprised of a foam<br />
cuff and three 5mm trocars was placed. Next, the novel grasper was<br />
introduced percutaneously in the RUQ. The device’s 3mm transabdominal<br />
shaft is mated to a 5mm end effector intra-corporeally and can grasp<br />
tissue with the purchase and security of a standard laparoscopic<br />
instrument while providing 360° rotation and locking jaws. Retraction<br />
was accomplished using the percutaneous grasper to manipulate the<br />
fundus and a standard 5mm grasper through the umbilical port for the<br />
infundibulum. Dissection was done using a combination of the MAGS and<br />
a standard Maryland dissector. Total procedure time, time from procedure<br />
start to obtain a critical view of the TOC and clipping and dividing the<br />
cystic duct/ artery, time for dissection of the gall bladder from the liver<br />
bed, and thickness of the abdominal wall at the umbilicus were measured.<br />
A multi-institutional survey was also administered among surgeons<br />
having experience with these devices to gauge satisfaction.<br />
Results: The critical view was obtained in each case and all 4 procedures<br />
were completed successfully. Both devices performed optimally to<br />
allow smooth flow of the procedure. Mean procedure time was 40min<br />
(33-51min); time from procedure start to obtaining the critical view and<br />
clipping and dividing the cystic duct/ artery was 33 min (28-38min) and<br />
time for dissection of the gall bladder from the liver bed was 6.7min (3-<br />
143 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Video Abstracts<br />
13min). The mean abdominal wall thickness was 1.9cm (1.5-2cm). The<br />
survey found that MAGS increased surgeon satisfaction in simplifying SSL<br />
cholecystectomy by 73% (18% satisfaction standard SSL, 100% MAGS).<br />
Conclusions: The use of a novel graspers and MAGS overcomes the<br />
limitations of SSL cholecystectomy and improves surgeon dexterity.<br />
Making SSL feel more like traditional laparoscopy will enable a wider<br />
adoption of this procedure in the community.<br />
V033<br />
RECURRENT PARAESOPHAGEAL HERNIA WITH GASTROBRONCHIAL<br />
FISTULA: LAPAROSCOPIC REPAIR Brian P Jacob, MD, Anthony Vine, MD,<br />
Mark Reiner, MD, L. Brian Katz, MD Mount Sinai Medical Center<br />
Introduction: The optimal method to manage a second recurrence of<br />
a paraesophageal hernia and a simultaneous gastrobronchial fistula<br />
is debatable. This video demonstrates a laparoscopic approach to this<br />
complex revisional operation performed on a 62 year old female who<br />
presented to our office with this diagnosis.<br />
History: This patient’s surgical history began with a laparoscopic<br />
paraesophageal hernia repair performed at an outside institution that<br />
recurred immediately. During the reoperation, there was a perforation to<br />
the stomach and esophagus that was managed using a left thoractomy<br />
to perform both the resection of the perforated portion of the stomach<br />
and a Nissen fundoplication. Recovery was prolonged by a left empyema<br />
and gastric fistula managed by a chest tube. The drainage stopped after<br />
2 months, but the patient continued to have symptoms of significant<br />
dysphagia and a 50 pound weight loss over 10 months. She then<br />
presented to our institution, where she also reported the history of a<br />
post-prandial cough for the past several months. An endoscpopy showed<br />
a benign ulcer in the stomach fundus but her upper GI series showed<br />
a second recurrence of a paraesophageal hernia with a slipped Nissen<br />
Fundoplication and a left gastrobronchial fistula.<br />
Results: The patient was managed with a laparoscopic revisional surgery.<br />
The video demonstates the adhesiolysis required in a reoperative<br />
situation as well as the identification and division of the gastrobronchial<br />
fistula. The previsous Nissen is then identified and taken down. The<br />
redundant fundus is resected, and finally the crural defect is repaired<br />
using standard laparoscopic techniques. The patient fortunately had<br />
an uneventful recovery and at her 3 month follow up visit reported no<br />
dysphagia and had already regained 15 pounds. A post operative upper<br />
GI demonstrates the results.<br />
Conclusion: Laparoscopic revisional foregut surgery is feasible, even in<br />
the setting of very complex situations such as what is demonstrated here<br />
with a second recurrence of a paraesophageal hernia with a herniated<br />
Nissen fundoplication and a gastrobronchial fistula. Using laparoscopic<br />
techniques in these complicated scenarios can provide the patients the<br />
known benefits of minimally invasive surgery.<br />
V034<br />
TAILORED APPROACH TO MINIMALLY INVASIVE RESECTION OF<br />
GASTIRC GIST S. Al-Sabah, MD MBA, GM Fried, MD, MC Vassiliou, MD<br />
MEd, Y. Kurashima, MD PhD, LE Ferri, MD PhD, LS Feldman, MD Steinberg-<br />
Bernstein Centre for Minimally Invasive Surgery and Innovation, McGill<br />
University Health Centre, Montreal, Canada<br />
The goal of surgical resection of gastric gastrointestinal stromal tumor<br />
(GIST) is to achieve a negative pathologic surgical margin while limiting<br />
morbidity. In most cases, nonanatomic wedge resections are sufficient.<br />
Laparoscopic surgery is an acceptable option as long as standard<br />
oncologic principles are followed, with multiple case series demonstrating<br />
similar oncological outcomes as open resection. Preoperative computed<br />
tomography (CT) scans, gastroscopy and endoscopic ultrasound allow<br />
for selection of a specific operative strategy based on tumor location, size<br />
and growth pattern. This video outlines a tailored approach for minimally<br />
invasive gastric GIST resection using five cases. The use of intraoperative<br />
endoscopy is highlighted as an adjunct, which helps in tumor localization,<br />
facilitates identification of tumor margins, and allows for verification<br />
of the integrity of the staple line post resection. In most cases, wedge<br />
resection is feasible. For GISTs with exophytic growth patterns, wedge<br />
12 th World Congress of Endoscopic Surgery 144<br />
resection may first require gastric mobilization. Transgastric resection<br />
is used for intraluminal posterior wall GISTs. Avoidance of direct<br />
tumor handling using stay sutures and endoloops is demonstrated. In<br />
conclusion, this video will demonstrate a selective approach and helpful<br />
hints for laparoscopic resection of gastric GIST.<br />
V035<br />
SINGLE PORT ANTERIOR RESECTION Hester Cheung, MD, Catherine<br />
Co, MD, Cliff Chung, MD, KK Yau, MD, Michael Li, Prof Pamela Youde<br />
Nethersole Eastern Hospital<br />
Objective: To determine the technical feasibility and clinical outcomes<br />
of laparoscopic anterior resection using combined single-port and<br />
endoluminal technique.<br />
Methods: A single port was placed at the umbilicus. Sigmoid colon was<br />
retracted using transabdominal sutures. After adequate mobilization, the<br />
colon was stapled distal to the lesion using non-cutting endo-stapler, and<br />
the rectum was opened distal to the staple line. The transanal endoscopic<br />
operation (TEO) device was placed transanally and the anvil of a circular<br />
stapler was then delivered via the device into the peritoneal cavity. The<br />
anvil was placed intraluminally via a colotomy made proximal to the<br />
lesion; following this the colon was transected above the colotomy site.<br />
The specimen was next delivered transanally via the TEO device. <strong>Final</strong>ly,<br />
the rectum was closed with endo-stapler and intra-corporeal side-to-end<br />
colorectal anastomosis was constructed using the circular stapler.<br />
Results: This technique was attempted in an 82 with an ulcerative<br />
tumor growth over the sigmoid colon. Single port anterior resection<br />
was performed. The operative time was 150 minutes. There was no intraoperative<br />
complication. The patient was discharged on post-operative<br />
day 6, with a maximum pain score of 2. Histological examination revealed<br />
T2N0 moderately differentiated adenocarinoma with 11 lymph nodes<br />
harvested.<br />
Conclusion: Laparoscopic anterior resection using this combined<br />
single-port and endoluminal technique is feasible for small lesions in the<br />
sigmoid colon or upper rectum. The technique avoids multiple trocar<br />
incisions and a minilaparotomy for specimen retrieval.<br />
V036<br />
THE ADVANTAGES OF LAPAROSCOPIC APPROACH FOR<br />
INTERSPHINCTERIC RESECTION M Hamada, MD, T Matsumura, MD, T<br />
Matsumoto, MD, F Teraishi, MD, K Ozaki, MD, T Nakamura, MD, Y Fukui, MD,<br />
Y Nishioka, MD, T Taniki, MD, T Horimi, MD Kochi Health Sciences Center<br />
Purpose: The most difficult steps of Intersphincteric resection (ISR)<br />
are circular dissection and separation of the internal sphincter muscle<br />
from the external sphincter and puborectalis by the perineal approach.<br />
Further dissection of the intersphincteric space by the abdominal<br />
approach may reduce the problems associated with the perineal<br />
approach. We present our techniques of Laparoscopic ISR using three<br />
cases of ISR for rectal tumor (Male /Female 2:1) by the video presentation.<br />
Presented Cases<br />
Case 1 is a 68-year-old male with a large, laterally spreading rectal<br />
adenoma.<br />
Case 2 is a 61-year-old male with rectal cancer whose tumor was located<br />
4.0 centimeter from the anal verge. Laparoscopic surgery was performed<br />
after neoadjuvant chemo-radiotherapy.<br />
Case 3 is a 71-year-old female with T1 rectal cancer whose tumor was<br />
located just above the dentate line. After dissecting the intersphincteric<br />
space, the prolapsing technique was useful in case it was a small-size<br />
tumor.<br />
Technique: In case of male patient, First, we dissected the rectum<br />
with the mesorectum to the anal hiatus, initially on the posterior side<br />
along the avascular plane. Second, we dissected Denonvilliers’ fascia<br />
and exposed the seminal vesicle.The third step was dissection of the<br />
lateral tissues followed by incision of Denonvilliers’ fascia with rectal wall<br />
exposure taking care not to injure the neurovascular bundle. It was easier<br />
to perform this step on the left side than on the right side. Along this<br />
dissection plane, we could reach the puborectalis, which was separated<br />
from the rectal wall, and we entered the intersphincteric space from the<br />
lateral side of the rectal wall. Dissection of the intersphincteric space
Scientific Session Video Abstracts<br />
should be performed in the posterior to anterior direction and to the<br />
anal side as much as possible. The final step was dissection of the hiatus<br />
ligament at the posterior side of the rectum. Nearly circular dissection of<br />
the interspincteric space could be completed.<br />
The difficulties associated with the perineal approach were reduced by<br />
this abdominal approach, and the tumor could be exteriorized easily.<br />
Results: Laparoscopic ISR with total mesorectal excision was performed<br />
in a total of 15 patients (10 males, 5 females). The median age was 60.5<br />
years. The T categories of the TNM classification of the rectal cancers were<br />
Tis 2, T1 1, T2 4, T3 8. The median distance from the anal verge to the<br />
tumor was 3.7 centimeter.The mean duration of surgery was 386 minutes.<br />
The mean blood loss was 108 miliiter, and mean postoperative hospital<br />
stay was 18 days. The diverting ileostomy was closed at a mean of 7.3<br />
postoperative months. No remarkable perioperative complication was<br />
encountered.<br />
Conclusion: laparoscopic ISR enabled us to reduce the difficulties<br />
associated with the perineal approach. An advantage of laparoscopic ISR<br />
was the ability to clearly visualize anatomical structures in the deep pelvic<br />
cavity.<br />
V037<br />
LAPAROSCOPIC PARAESOPHAGEAL HERNIA REPAIR WITH<br />
BIOSYNTHETIC MESH AND COLLIS GASTROPLASTY Angel M Caban,<br />
MD, Daniel J Scott, MD FACS UT Southwestern, Dallas Texas<br />
Surgical treatment of paraesophageal hernias has changed significantly<br />
in the last decade. Laparoscopy has decrease the risk associated with<br />
open surgery and today a larger number of high risk cases are being<br />
performed. The minimally invasive surgeon is faced with many challenges<br />
and controversies during these procedures. One of the major issues is<br />
recognition of a shortened esophagus, which affects only 3 to 5 percent<br />
of cases. Recognition of inadequate intraabdominal esophageal length<br />
is critical in providing effective treatment. Additionally, recent data<br />
support the use of a biosynthetic mesh buttress to decrease hernia<br />
recurrence rates. In this video we present a fifty year-old female with a<br />
giant paraesophageal hernia and a true short esophagus. A laparoscopic<br />
paraesophageal hernia repair with biosynthetic mesh and “wedge”<br />
Collis gastroplasty was performed. The patient was discharged home on<br />
postoperative day number five and at 6-month follow up demonstrate<br />
dramatic improvement in her symptoms and had no signs of recurrence.<br />
V038<br />
LAPAROSCOPIC NISSEN FUNDOPLICATION: IT’S ROLE IN THE<br />
TREATMENT OF A FAILED ESOPHYX PROCEDURE Barry A Salky, MD<br />
FACS The Mount Sinai Hospital, New York<br />
This is a 52 year old male, 9/11 responder who developed GERD and<br />
respiratory related issues from 9/11. He had a NDO plicator in 2006 with<br />
no effect, and an Esophex in November, 2008. This was complicated<br />
by abdominal pain, free air, and mediastinal air. He was treated<br />
conservatively and eventually responded over one week in hospital.<br />
However, the GERD increased markedly. He consented for a Nissen which<br />
was accomplished in June, 2009. At laparoscopy, the blue plastic pins<br />
where inserted through the esophagus, left crus of the diaphragm, and<br />
sometimes into the cardia of the stomach. Clearly, the hiatal hernia had<br />
not been reduced completely before the applications of the pins. This will<br />
be demonstrated in the video. The patient developed an abscess post<br />
operatively thought to be secondary to a sealed off perforation at one of<br />
the pin site. This is shown in the video. As IR could not drain the abscess,<br />
laparoscopic drainage was performed. This is shown in the video as well.<br />
The dissection was surprising difficult because of the fixation of the pins<br />
to the esophagus, crus and stomach. The construction of the Nissen,<br />
while shown, is not the thrust of this video.<br />
V039<br />
LAPAROSCOPIC DUODENAL POLYPECTOMY WITH INTRAOPERATIVE<br />
ENDOSCOPY IN PEUTZ-JEGHERS SYNDROME Eugenius J Harvey, MBBS,<br />
Kervin Arroyo, MD, Blair Lewis, MD, Lester Katz, MD Mount Sinai School of<br />
Medicine<br />
We present a video of a laparoscopic resection of a 6cm hamartomatous<br />
polyp arising from the 3rd part of the duodenum and intraoperative<br />
endoscopy in a 15 year old female with Peutz-Jeghers syndrome.<br />
The patient has a history of multiple small hamartomatous polyps<br />
removed endoscopically. She now presents with symptoms of<br />
intermittent postprandial abdominal pain. At upper endoscopy she was<br />
found to have a large pedunculated polyp arising from the third part of<br />
the duodenum which could not be endoscopically resected.<br />
A combined laparoscopic and endoscopic procedure was elected.<br />
Initial laparoscopy demonstrated a chronically dilated duodenum and<br />
proximal jejunum. An intraluminal mass was encountered in the proximal<br />
jejunum with a transition to normal jejunum distally. The remaining small<br />
bowel appeared normal.<br />
A transverse enterotomy was made in the dilated jejunum and the<br />
pedunculated polyp resected.<br />
An intraoperative upper endoscopy/ push enteroscopy was performed<br />
which demonstrated the base of the polyp in the duodenum and the<br />
closed enterotomy in the jejunum.<br />
Patients with benign polyposis syndromes often require multiple<br />
intestinal operations during their lifetime. The laparoscopic approach<br />
can minimize the adverse effects of multiple surgeries. Intraoperative<br />
endoscopy helps to assess the adequacy of resection, hemostasis and<br />
closure of the enterotomy or anastomosis.<br />
V040<br />
SINGLE PORT ACCESS: A FEASIBLE ALTERNATIVE TO CONVENTIONAL<br />
LAPAROSCOPIC SPLENECTOMY EM Targarona, MD, C Balague, MD, L<br />
Pallares, MD, F Marinello, MD, C Rodriguez-Luppi, MD, C Martinez, MD, MP<br />
Hernandez, MD, M Trias, MD Hospital Santpau, UAB, Barcelona, Spain.<br />
Laparoscopic approach is the gold standard for splenectomy . There<br />
is currently a trend to reduce the invasiveness of minimally invasive<br />
procedures. Single port access is alternative to NOTES but no reports have<br />
yet been published in relation to the spleen. AIM: To describe the SAP<br />
technique for splenectomy MAT. & METH.. 2 patients were approached<br />
by SAP: a 26-yr male diagnosed of IPT and a 45-yr male with recurrent<br />
Hodgkin disease. Surgical technique: It was divided into 5 steps: 1.-<br />
Patient position: standard right decubitus with the table flexed at the<br />
flank, 2. - Transumbilical trocar insertion: A 15 mm periumbilical incision<br />
and a flexible tip 10 mm HD scope through a 12 mm bladeless trocar<br />
bluntly introduced under optic contro. Two 5 mm trocar with a flexible<br />
corrugate shaft was inserted to the right and left. 3.- Splenic dissection.<br />
A 5 mm curved grasper used for TEM was placed through the left trocar<br />
and a 5 mm Ultracision on the right. Using this approach it was possible<br />
to mobilize the splenic colon flexure and to section the short vessels, The<br />
table was tilted to the left and the posterior spleno-renal attachments<br />
were freed. 4.- Splenic hilum transection: The flexible scope was retrieved<br />
and visual control was changed to a 5 mm scope introduced through<br />
the right 5 mm trocar. A 6 cm cartridge stapler was inserted through<br />
the 12 mm trocar and was applied several times to sever the splenic<br />
hilum. 5.- Spleen extraction. Once the spleen was completely free, a 15<br />
mm endobag was inserted, replacing the 12 mm trocar. The spleen was<br />
grasped and introduced in the bag and the spleen was morcellated The<br />
mean op time was 90’ and blood loss was minimal. Spleen weight was<br />
200 gr. and 450 gr..RESULTS: The postoperative course was uneventful.<br />
Both patients had minimal postoperative pain and scarring, and were<br />
discharged on the second postoperative day. CONCLUSIONS: SAP access<br />
can be safely used for operative visualization, hilum transection and<br />
spleen removal with conventional instrumentation, reducing parietal wall<br />
trauma to a minimum. The clinical, esthetic and functional advantages<br />
require further analysis.<br />
12 th World Congress of Endoscopic Surgery<br />
145 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Scientific Session Video Abstracts<br />
V041<br />
USE OF A NOVEL, SELF-CONTAINED TISSUE RETRACTION DEVICE<br />
TO REDUCE TROCAR SITE NUMBER IN LAPAROSCOPIC AND NOTES-<br />
BASED SURGICAL PROCEDURES Trudie A Goers, MD, Richard A Pierce,<br />
MD PhD, Danny V Martinec, BS, Lee L Swanstrom, MD FACS Legacy Health<br />
System, Portland, OR<br />
In an effort to make laparoscopic surgical procedures even less invasive,<br />
single port access and natural orifice transgastric endoscopic surgical<br />
(NOTES) approaches have been developed over the past several years.<br />
However, the need to maintain basic surgical working principles, such<br />
as proper tissue retraction to create tension and counter-tension, is<br />
still of critical importance if emerging techniques are to be successfully<br />
implemented. New self-retaining retraction devices that do not require<br />
dedicated trocar placement represent a technology that could help<br />
to bridge the gap between traditional laparoscopy and less invasive<br />
techniques. One such device (EndoGrab, Virtual Ports Ltd) utilizes a<br />
fully insertable, self-contained, double hook configuration to generate<br />
tissue retraction by providing a means of atraumatic tissue attachment<br />
between either 2 adjacent visceral structures or between the viscera and<br />
the abdominal wall. The device can be repositioned at will throughout<br />
the operative case, and allows for both the elimination of a dedicated<br />
transabdominal port and the need for active assistant retraction.<br />
Additionally, a flexible applicator will allow the device to be introduced<br />
through an overtube via a natural orifice. This video shows the use of the<br />
EndoGrab device in both basic and advanced laparoscopic procedures,<br />
as well as in a technically challenging NOTES operative case.<br />
When used in a laparoscopic cholecystectomy, the EndoGrab is<br />
introduced through a 5 mm port. One of four usual operating ports<br />
is eliminated such that only two working ports and a camera port are<br />
needed. The device allows for initial suspension of the fundus, and<br />
subsequently, the gall bladder body, from the abdominal wall above.<br />
Consequently, critical operating views of the structures within Calot’s<br />
triangle are well-visualized with the cephalad retraction provided by the<br />
device.<br />
Similarly, in more complex laparoscopic cases such as repair of<br />
paraesophageal hernia, the EndoGrab is again be used in lieu of<br />
placement of a port for assistant retraction. The device is placed on the<br />
stomach in various locations to allow for adequate visualization of critical<br />
structures during dissection, crural closure and fundoplication creation.<br />
Use of the EndoGrab allows the procedure to be completed with four<br />
rather than five incisions.<br />
Not only does the EndoGrab allow for the reduction in number<br />
of incisions, but in certain cases, it can help eliminate the need for<br />
transabdominal ports. With the continued development of NOTES<br />
equipment and technology, tools like the EndoGrab can play critical<br />
roles in procedures accomplished with access exclusively through<br />
natural orifices. Given that currently available NOTES platforms make<br />
lateral retraction and dissection of the gall bladder difficult during<br />
cholecystectomy, the EndoGrab serves a novel solution in this video.<br />
In conclusion, the EndoGrab represents a valuable technological<br />
advance that allows traditional laparoscopy to be done with fewer trocar<br />
sites, and may facilitate NOTES procedures in becoming truly externally<br />
incisionless.<br />
V042<br />
Because of her complaints of a mass protruding while her bladder was<br />
full, it was decided to perform a TAP repair so that the bladder could be<br />
filled and visualized during the operation. The patient had two concurrent<br />
issues noted intra-operatively: 1. Her full bladder was pushing the<br />
previously placed prolene plug, everting it through her repair and likely<br />
represented the mass which the patient was feeling. 2. In addition, there<br />
was a clear and separate recurrent left inguinal hernia just medial to the<br />
previous repair. There was no evidence of plug migration. We removed<br />
the plug, reduced her recurrent hernia and used a soft polyester mesh<br />
placed extra-peritoneally to cover both defects.<br />
V043<br />
LAPAROSCOPIC AND THORACOSCOPIC IVOR LEWIS<br />
ESOPHAGECTOMY Kazunori Sato, MD, Beemen N Khalil, MD, Pierre<br />
Theodore, MD, David Jablons, MD, Guilherme M Campos, MD University<br />
of Wisconsin School of Medicine and Public Health and University of<br />
California San Francisco<br />
Minimally invasive (MIS) Ivor-Lewis Esophagectomy is a technically<br />
challenging procedure, but series from expert centers have described<br />
its feasibility and safety. The benefit in terms of long-term oncologic<br />
outcomes is being investigated. The extent of MIS techniques has ranged<br />
from a laparoscopic abdominal component with a thoracotomy, minithoracotomy,<br />
or thoracoscopic component. This video describes the main<br />
steps of a MIS laparoscopic and thoracoscopic Ivor Lewis esophagectomy<br />
with upper abdominal and subcarinal lymph nodal dissection and<br />
the circular stapled anastomosis with the transoral anvil. We have<br />
performed MIS Ivor Lewis Esophagectomy in thirty-seven patients (mean<br />
age 67 years; range 45 to 85) with distal esophageal adenocarcinoma<br />
(n=29), squamous cell cancer (n=5), or high-grade dysplasia in Barrett’s<br />
Esophagus (n=3) between October 2007 and August 2009. The abdominal<br />
portion of the operation was completed laparoscopically in 30 patients<br />
(81.1%). The thoracic portion was completed using a mini-thoracotomy<br />
in 23 patients (62.2%) and thoracoscopic techniques in 14 (37.8%).<br />
Proximal and distal margins were negative in all patients. A median of<br />
15 lymph nodes (range 8 to 33) were dissected from each specimen,<br />
with a median of 3 (range 0 to 18) histologically positive nodes. No<br />
intra-operative technical failures of the anastomosis or deaths occurred.<br />
The average hospital stay was 11 days (range 7 to 30). Five patients had<br />
strictures (13.5%) and all were successfully treated with either two or<br />
three endoscopic dilations. One patient had an anastomotic leak that<br />
was successfully treated by re-operation and endoscopic stenting. The<br />
operation shown includes laparoscopic hiatal, distal esophageal, and<br />
gastroesophageal junction dissection and lymph nodal dissection of the<br />
porta-hepatis, left gastric artery, and supra-pancreatic lymph stations.<br />
Gastric conduit preparation was performed using multiple firings of<br />
a 4.8mm linear stapler. A pyloroplasty was performed and a feeding<br />
jejunostomy placed. The thoracic portion was completed using standard<br />
thoracoscopic ports and techniques and included mobilization of the<br />
esophagus from the esophageal bed, subcarinal lymph node dissection<br />
and transection of the most superior aspect of the thoracic esophagus<br />
at the level of the thoracic inlet with a 4.8mm linear stapler above the<br />
divided azygous vein. The esophagogastric anastomosis was performed<br />
using a 25mm anvil passed trans-orally, in a tilted position, and connected<br />
to a 90cm long PVC delivery tube through a small opening in the stapled<br />
esophageal stump. The anastomosis was completed by joining the anvil<br />
to a circular stapler (EEA 25mm with 4.8mm Staples) inserted into the<br />
gastric conduit. Then, the gastric conduit opening was closed using an<br />
additional firing of a 4.8mm linear stapler.<br />
While long-term oncologic outcomes are still being evaluated, MIS Ivor<br />
Lewis Esophagectomy is feasibe and seems safe in high volume centers. It<br />
also seems to offer superior visualization of the operative field in addition<br />
to the usual benefits of MIS techniques.<br />
AGAINST OCCAM’S RAZOR: TAP REPAIR OF RECURRENT<br />
INGUINAL HERNIA WITH CONCOMITANT INVERSION OF ORIGINAL<br />
POLYPROPYLENE PLUG Antonio D Lassaletta, MD, Erika Fellinger, MD,<br />
Steven D Schwaitzberg, MD FACS Beth Israel Deaconess Medical Center,<br />
Cambridge Health Alliance, Harvard Medical School<br />
The patient is a 42 year old female who had undergone an open left<br />
inguinal hernia repair 13 years ago. She presents to clinic with a 1 year V044<br />
history of a recurrent left groin mass in the area of her previous repair. LAPAROSCOPIC TREATMENT OF RECTOCELE BY ANTERIOR<br />
Interestingly, she states that at night when her bladder is full she feels a RECTOPEXY David LECHAUX, PhD, Adrian Marius NEDELCU, Aurelie<br />
hard mass protruding from her left groin. In addition, she has pain in the LEMARREC, MD “Yves Le Foll”’Hospital - Saint Brieuc<br />
area with straining or heavy lifting.<br />
The patient is a 53 yo F with stage III symptomatic rectocele.<br />
12 th World Congress of Endoscopic Surgery 146
Scientific Session Video Abstracts<br />
1. Installation/ Positioning<br />
The patient is in gynecological position. We used 4 trocars.<br />
2. Exposure to/of the operative field<br />
Thanks to a pronounced Trendelenburg position the sigmoid loop is<br />
retracted appropriately. The uterus is fixed on the anterior abdominal wall.<br />
Findings: Douglas pouch is enlarged. Excces peritoneum is excised<br />
allowing for the exposure of the pelvic floor.<br />
3. Dissection of the rectovaginal space<br />
We used an intravaginal buggy. The dissection was performed to the<br />
deepest part of the pelvic floor and lateral, to the pararectal fossa<br />
4. Promontorium approach<br />
There are 3 risks:<br />
- median sacral artery;<br />
- intervertebral disk;<br />
- the hypogastric plexus;<br />
In the same time the right ureter must be identified, being localized<br />
very close to the area of dissection. Scissor were used to make a 3-4 cm<br />
peritoneal incision<br />
5. Tunnelissation<br />
The blunt dissection was used to create a bridge/space/oppening<br />
between the promontorium and the Douglas pouch.<br />
6. Lower fixation of the prosthesis<br />
The prosthesis is 6/6 cm inferiorly and the superior part is 2,5 /9 cm.<br />
The fixation is performed with Protack device and with the help of an<br />
intralumenal finger.<br />
7. Fixing the prosthesis to posterior vaginal pouch/fornix is stretching /<br />
is putting tension on the posterior vaginal wall. We used an intravaginal<br />
finger for contrapressure<br />
7. Suspension to the posterior vaginal pouch(fund de sac post vaginal)<br />
allow (punerea in tensiune) a tension of posterior vaginal wall. 2 agrafes<br />
are put with the control of an intravaginal finger>>>.aici tre schimbat ca<br />
m-a apucat oboseala…sper ca totusi ai inteles<br />
8. Fixation to the promontorium<br />
Is realized by Protrack device avoiding the intervertebral disk.<br />
It’s about a technique without tension of the prosthesis<br />
9 Peritoneal closure<br />
Is performed using Vicryl 2/0 continuous suture both at the level of<br />
Douglas pouch and promontorium.<br />
No drainage, no naso gastric tube are needed.<br />
Postoperatively, first bowel movement was on day one which allows for<br />
progressive realimentation/ feeding. Hospital stay was 4 days.<br />
V045<br />
LAPAROSCOPIC SPLEN-PANCREATECTOMY, FOR MUCINOUS<br />
PANCREATIC-CYST Jorge E Nefa, MD, Pablo E Omelanczuk, MD, Mario<br />
D Masrur, MD, Sergio E Bustos, MD Surgical Service, Hospital Italiano,<br />
Mendoza-Argentina<br />
BACKGROUND: Among pancreatic cysts, mucinous cystadenoma,<br />
and intraductal papillary mucinous neoplasms have the potential for<br />
malignant transformation. Differentiation between benign and potentially<br />
malignant cysts remains difficult at the preoperative time. Majority<br />
of these tumors must be resected and the laparoscopic approach is<br />
nowadays a valid option.<br />
OBJECTIVE of this presentation was to show in a video the laparoscopic<br />
excision of a multiple pancreatic mucinous cyst. In this was necessary the<br />
simultaneous splenectomy.<br />
METHODS: A 54 years-old female was diagnosed for Pancreatic mucinous<br />
Cyst by CTA, NMR, PET Scan and Tumor Markers. Using four trocars the<br />
spleen and pancreatic Cysts were successfully removed. Pancreatic section<br />
was carried out using stapler. Both splenic artery and vein, were occluded<br />
by ligature and clips.<br />
RESULTS: The operating room time was 4 hours, transfusion of 500Ml<br />
of Red Cells was necessary. Hospital stay was 5 days. Pathologic study<br />
informed Adenocarcinoma mucinous of the pancreas.<br />
CONCLUSIONS: Simultaneous resection of pancreas and spleen is<br />
possible by Laparoscopy as many authors have reported.<br />
On the other hand, neither laboratory exams nor Imagines were able to<br />
confirm the malignant condition of the tumor at the preoperative time.<br />
V046<br />
LAPAROSCOPIC EXTIRPATION OF A FORK FROM THE DUODENUM<br />
Konrad W Karcz, MD, Birte Kulemann, MD, Gabriel J Seifert, MD, Hans<br />
J Schrag, MD, Simon Küsters, MD, Goran Marjanovic, MD, Jodok M<br />
Grüneberger, MD, Cheng Zhou, MD, Philipp Holzner, MD, Alexander<br />
Braun, MD Videosurgery Division, Department of General and Abdominal<br />
Surgery, University Hospital Freiburg, Hugstetter Str 55, D-79106 Freiburg,<br />
Germany<br />
BACKROUND: A woman who had accidentally swallowed a fork during a<br />
dinner party was admitted to our Department of General and Abdominal<br />
surgery. Different techniques have been described for removing foreign<br />
bodies (FB) from the stomach or the duodenum. Endoscopical techniques<br />
are widely and successfully used, but not in each case.<br />
Here, we present the laparoscopic retrieval of a 15 cm fork from the<br />
duodenal bulb.<br />
METHODS: A 23-year-old woman was admitted with progressive<br />
abdominal pain two weeks after swallowing a plastic fork while<br />
attempting to induce vomiting during a party.<br />
On the day of admission to our emergency room, she presented with<br />
leukocytosis, otherwise normal laboratory findings and mild epigastric<br />
tenderness without peritonism. She was afebrile with normal vital<br />
signs and had no significant events in her past medical history. Prior to<br />
admission, she ate normal meals.<br />
A routine X-ray examination did not show the expected FB. The<br />
preoperative upper endoscopy, on the other hand, showed a plastic fork,<br />
tines up, right behind the pylorus in the duodenal bulb: The tines were<br />
deeply buried in the wall of the intestine. The handle was irremovably<br />
lodged in the opposite part of the duodenum. In consequence, the<br />
indication for laparoscopic extirpation was given, especially due to<br />
uncertainty concerning further lesions or the presence of an abscess<br />
within the abdominal cavity. Perforating objects and objects larger than 7<br />
cm ought to be removed surgically to prevent oesophageal perforation.<br />
The patient was placed in supine position with the surgeon standing<br />
between her legs. Four trocars, two 10-mm and two 5-mm, were used<br />
(ApplyMedical, USA). We expected peritonitis and extreme tissue<br />
swelling with adhesions in the upper abdominal cavity, but only saw a<br />
slightly swollen duodenum with very few fibrin stripes and roughly 250<br />
ml of white, exudative, intraperitoneal fluid. The fork tines, which had<br />
perforated the duodenal bulb, could be seen. There were no liver injuries.<br />
The tines were held with a clamp, and the perforated intestinal wall was<br />
carefully dissected with the monopolar hug (STORZ, Germany) and later<br />
with the ACE Harmonic Scalpel (ETHICON, USA) due to bleeding.<br />
After the tines were freed, the 15cm plastic fork was extracted in proximal<br />
direction through the perforation injury. There was no severe necrosis,<br />
and debridement was not necessary. The bowel was irrigated and<br />
continuously sutured with 3-0 PDS.<br />
<strong>Final</strong>ly, the fork was retrieved without problems from the abdominal<br />
cavity through the 10mm trocar incision.<br />
RESULTS: Operating time was 60 minutes, blood loss estimated at<br />
roughly 100 ml with no blood transfusion. The patient’s postoperative<br />
course was uneventful. Hospital stay was 4 days. The patient tolerated<br />
a gradual reintroduction of liquid and solid foods; she was well and<br />
asymptomatic one year after the operation.<br />
CONCLUSION: A fork may be swallowed, but cannot spontaneously pass<br />
through the gastrointestinal tract. Early removal should be advised to<br />
avoid perforation and to minimize morbidity.<br />
Laparoscopic removal is a safe and feasible method of managing FBs that<br />
are not removable endoscopically.<br />
147 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
Video Channel Loop Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
V047 LAPBAND PLACEMENT WITH REPAIR OF INCIDENTAL HIATAL<br />
HERNIA USING CURVED LAPAROSCOPIC INSTRUMENTS THROUGH<br />
A SINGLE INCISION Shabirhusain S Abadin, MD MPH, Rami Lutfi, MD<br />
FACS, St. Joseph Resurrection Hospital<br />
V048 LAPAROSCOPIC REVISION OF GASTRIC BANDING TO ROUX-<br />
EN-Y GASTRIC BYPASS: TECHNICAL PEARLS. Maher El Chaar, MD,<br />
Neal Agee, MD, Dimitrios Stefanidis, MD, Gray Hughes, MD, Timothy<br />
Kuwada, MD, Keith Gersin, MD, Carolinas Medical Center, Division of<br />
Minimally Invasive and Bariatric Surgery<br />
V049 SIMULTANEOUS LAPAROSCOPY AND CO2 COLONOSCOPY FOR<br />
FULL-THICKNESS EXCISION OF A SUBMUCOSAL CECAL LESION<br />
Vanessa P Ho, MD, Anjali S Kumar, MD MPH, Jun Yan, MD, Olival de<br />
Oliveira, Jr., MD, Christopher W Towe, MD, Paul Basuk, MD, Jeffrey W<br />
Milsom, MD, New York Presbyterian Hospital- Weill Cornell Medical<br />
Center<br />
V050 SINGLE PORT LAPAROSCOPIC SIGMOIDECTOMY FOR<br />
SIGMOID VOLVULUS John Marks, MD, Eileen Larkin, BA, Rahila Essani,<br />
MD, Lankenau Hospital and Institute for Medical Research: Section of<br />
Colorectal Surgery, Wynnewood, PA<br />
V051 PERORAL ENDOSCOPIC SUBMUCOSAL PYLOROMYOTOMY<br />
IN IN ANIMAL MODEL FOR A NEW CONCEPT OF MINIMALLY<br />
INVASIVE SURGERY FOR PYLORIC STENOSIS Masaru Kawai, MD,<br />
Silvana Perretta, MD, Oliver Burckhardt, MD, Gianfranco Donatelli, MD,<br />
Bernard Dallemagne, MD, Hurng-Sheng Wu, MD, Jacques Marescaux,<br />
MD, IRCAD, University Hospital of Strasbourg, France - Show Chwan<br />
Memorial Hospital, Changhua, Taiwan<br />
V052 DS (DISK SUSPENSION) METHOD: NOVEL AND SAFE<br />
TECHNIQUE FOR THE RETRACTION OF THE LIVER IN<br />
LAPAROSCOPIC SURGERY Kazunori Shibao, MD PhD, Aiichiro Higure,<br />
MD PhD, Koji Yamaguchi, MD PhD, University of Occupational and<br />
Environmental Health<br />
V053 LAPAROSCOPIC RADICAL CHOLECYSTECTOMY AND ROUX-<br />
EN-Y CHOLEDOCHOJEJUNOSTOMY FOR GALLBLADDER CANCER<br />
Andrew A Gumbs, MD, John P Hoffman, MD, Fox Chase Cancer Center<br />
V054 LAPAROSCOPIC REDO HEPATICO-JEJUNOSTOMY FOR BILIARY<br />
STRICTURE AFTER OPEN HEPATICOJEJUNOSTOMY FOR CBD<br />
INJURY Mariano Palermo, MD PhD, Nelson Trelles, MD, Michel Gagner,<br />
MD FACS FRCSC, Department of Surgery, Mount Sinai Medical Center.<br />
Miami Beach, FL. USA.<br />
V055 SINGLE INCISION LAPAROSCOPIC SURGERY (SILS): BILATERAL<br />
TOTAL EXTRAPERITONEAL (TEP) INGUINAL HERNIA WITH<br />
SIMULTANEOUS UMBILICAL HERNIA REPAIR Brian P Jacob, MD,<br />
Catherine Madorin, MD, Anthony Vine, MD, Mark Reiner, MD, Mount<br />
Sinai Medical Center<br />
V056 DEGARENGEOT’S HERNIA: LAPAROSCOPIC REDUCTION,<br />
REPAIR & RESECTION OF AN INCARCERATED APPENDICEAL<br />
MUCOCELE David D Odell, MD, Alexandre Y Derevianko, MD,<br />
Benjamin E Schneider, MD, John T Mullen, MD, Beth Israel Deaconess<br />
Medical Center<br />
V057 LOOP SNARE TECHNIQUE FOR TRANSFASCIAL SUTURING Brian<br />
D Layton, DO, Carl J Westcott, MD, Wake Forest University<br />
V058 GALLBLADDER VOLVULUS: CASE REPORT AND REVIEW<br />
OF THE LITERATURE Terri R Martin, MD, Jennifer Keller, MD, John<br />
Martinie, MD, Carolinas Medical Center<br />
V059 THREE PORT ROBOTIC RIGHT HEMICOLECTOMY: A<br />
SYSTEMATIC APPROACH TO SET UP AND SURGERY Jeffrey A Neale,<br />
MD, Eric Szilagy, MD FACS FASCRS, Melissa Times, MD FACS FASCRS,<br />
Surya P M Nalamati, MD FACS, Henry Ford Health System<br />
V060 SINGLE-INCISION LAPAROSCOPIC SPLENECTOMY FOR ITP<br />
Bac H Nguyen, MD PhD, Tuan A Le Quan, MD, Thinh H Nguyen, MD,<br />
University Medical Center at Ho Chi Minh City<br />
V061 DIAGNOSIS AND TREATMENT OF OCCULT GI BLEEDING AFTER<br />
LAPAROSCOPIC ROUX-EN- Y GASTRIC BYPASS (LRYGB). A CASE<br />
REPORT OF A GIST AS BLEEDING SOURCE. Jesus E Hidalgo, Omar<br />
Bellorin, Ismael Court, Katharina Schmidt, Samuel Szomstein, Raul J<br />
Rosenthal, Cleveland Clinic Florida<br />
V062 LAPAROSCOPIC CONVERSION OF LAPAROSCOPIC<br />
ADJUSTABLE GASTRIC BANDING (LAGB) TO SLEEVE<br />
GASTRECTOMY (LSG) FOR MORBID OBESITY Omar Bellorin, Ismael<br />
Court, Samuel Szomstein, Raul J Rosenthal, Cleveland Clinic Florida<br />
V063 SINGLE-INCISION LAPAROSCOPIC SIGMOIDECTOMY FOR<br />
CANCER Bac H Nguyen, MD PhD, Thinh H Nguyen, MD, Khanh C<br />
Pham, MD, University Medical Center at Ho Chi Minh City<br />
V064 SINGLE INCISION LAPAROSCOPIC RIGHT HEMICOLECTOMY<br />
USING STANDARD LAPAROSCOPIC INSTRUMENTS Joshua A<br />
Waters, MD, Michael J Guzman, MD, Don J Selzer, MD, Bruce W Robb,<br />
MD, Eric A Wiebke, MD, Virgilio V George, MD, Indiana Univerisity<br />
Department of Surgery<br />
V065 ENDOSCOPIC TREATMENT FOR GASTRIC PERFORATION<br />
USING T-TAG AND PLASTIC PROTECTION CHAMBER Kiyoshi<br />
Hashiba, MD PhD, Sergio Roll, MD PhD, Pablo r Siqueira, MD, Marco<br />
A D`Assunção, MD, Horus A Brasil, MD, Hospital Sírio Libanês<br />
Endoscopic Unit. S.Paulo. Brazil.<br />
V066 LAPARO-ENDOSCOPIC SINGLE SITE (LESS) TOUPET<br />
FUNDOPLICATION WITH REDUCTION OF A GIANT HIATAL HERNIA<br />
Sharona B Ross, MD, Connor A Morton, BS, Desiree Villadolid, MPH,<br />
Sujat Dahal, MD, Linda K Barry, MD, Andy Roddenbery, MD, Alexander<br />
S Rosemurgy, MD, Department of Surgery, University of South Florida,<br />
Tampa, Florida<br />
V067 TOTAL LAPAROSCOPIC WHIPPLES<br />
PANCREATICODUODENECTOMY –EARLY EXPERIENCE WITH 3<br />
CASES Varghese Chalissery, MS FMAS, Alfie Kavalakat, MS DNB,<br />
Center for Laparoscopic Surgery&Minimallly Invasive Procedures,<br />
West Fort Hospital,Thrissur,Kerala,India<br />
V068 LAPARO-ENDOSCOPIC SINGLE SITE (LESS) PANCREATIC CYST<br />
ENUCLEATION Andy S Roddenbery, MD, Sharona B Ross, MD, Connor<br />
A Morton, BS, Leigh Ann Humphries, Harold Paul, BS, Alexander S<br />
Rosemurgy, MD, Department of Surgery, Tampa, Florida<br />
V069 LAPAROSCOPIC PARADUODENAL HERNIA REPAIR Faisal M<br />
Al-Mufarrej, MD, Jason Kasza, MD, Bruce Abell, MD, Frederick Brody,<br />
MDMBA, George Washington University Medical Center<br />
V070 LAPAROSCOPIC REMOVAL OF INGUINAL PLUG AND PATCH<br />
MESH FOR CHRONIC GROIN PAIN Jeffrey A Blatnik, MD, Michael J<br />
Rosen, MD, Department of Surgery, University Hospitals Case Medical<br />
Center, Cleveland, OH<br />
V071 LAPAROSCOPIC MEDIAN ARCUATE LIGAMENT RELEASE Mun<br />
Jye Poi, MD, Robert J. Lowe, MD, Pavlos K. Papasavas, MD, Darren S.<br />
Tishler, MD, Hartford Hospital , Hartford, Connecticut<br />
V072 ROBOTIC ASSISTED ESOPHAGECTOMY FOR TREATMENT OF<br />
ESOPHAGEAL HEMANGIOMA Philip WY Chiu, Prof, Anthony YB Teoh,<br />
Dr, Simon KH Wong, Dr, Tiffany CL Wong, Dr, Enders KW Ng, Prof, The<br />
Chinese University of Hong Kong<br />
V073 LAPAROSCOPIC SPLEEN PRESERVING DISTAL<br />
PANCREATECTOMY Shailesh P Puntambekar, MS, Geetanjali Agarwal,<br />
MS, Anjali Patil, MS, Sourabh Joshi, MS, Galaxy CARE Laparoscopy<br />
Institute<br />
V074 SURGICAL MANAGEMENT OF CHRONIC ABDOMINAL PAIN<br />
AFTER LAPAROSCOPIC ROUX-EN-Y GASTRIC BYPASS. Jeremy<br />
Eckstein, Sheetal Patel, Emeka Acholonu, Wasef Abu-Jaish, Alexander<br />
Ramirez, Samuel Szomstein, Raul Rosenthal, Cleveland Clinic Florida<br />
V075 HYBRID TRANSVAGINAL SLEEVE GASTRECTOMY Michel<br />
Gagner, MD FRCSC FACS, Florida International University<br />
12 th World Congress of Endoscopic Surgery 148
Video Channel Loop Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
V076 GELPOINTTM SINGLE INCISION INTRACORPOREAL<br />
ANASTOMOTIC TECHNIQUES Eric M Paul, MD, John Weaver, MD,<br />
Scott Davis, MD, Jahnavi Srinivasan, MD, John Sweeney, MD, Edward<br />
Lin, DO, Emory Endosurgery Unit<br />
V077 ENDOSCOPIC REMOVAL OF PARTIALLY ERODED ADJUSTABLE<br />
GASTRIC BAND WITH COMMON ENDO-HOUSEHOLD ITEMS<br />
Seiichi Kitahama, MD, Katayun Irani, MD, Valerie J Halpin, MD FACS,<br />
Lee L Swanström, MD PhD FACS, Legacy Good Samaritan Hospital,<br />
Portland, OR<br />
V078 SINGLE-INCISION LAPAROSCOPIC CHOLECYSTECTOMY USING<br />
NOVEL POWERED ARTICULATING INSTRUMENTS (TERUMO) Byron<br />
F Santos, MD, Nathaniel J Soper, MD, Eric S Hungness, Northwestern<br />
University, Department of Surgery<br />
V079 LAPAROSCOPIC TRANSHIATAL RESECTION OF ESOPHAGEAL<br />
DIVERTICULUM Kervin Arroyo, MD, John Harvey, MD, Daniel M<br />
Herron, MD, Michael Edye, MD, Mount Sinai School of Medicine<br />
V080 LAPAROSCOPIC REPAIR OF A COMMON BILE DUCT INJURY<br />
Elyssa J Feinberg, MD, Adam J Nadelson, MD, Diego R Camacho,<br />
MD FACS, Montefiore Medical Center, The Albert Einstein College of<br />
Medicine, Bronx, New York<br />
V081 SINGLE INCISION LAPAROSCOPIC PARTIAL HEPATECTOMY<br />
Juliana E Meyer, MD, Richard A Arenas, MD, Francis Cannizzo Jr., MD<br />
PhD, John R Romanelli, MD, Baystate Medical Center, Tufts University<br />
School of Medicine<br />
V082 LAPAROSCOPIC COMPONENT SEPARATION FOR INCISIONAL<br />
HERNIA REPAIR AND REMOVAL OF INFECTED MESH Dennis F Diaz,<br />
MD, John Scott Roth, MD, University of Kentucky Chandler Medical<br />
Center<br />
V083 SINGLE INCISION LAPAROSCOPIC RESECTION OF A GASTRIC<br />
GASTROINTESTINAL STROMAL TUMOR Philip Omotosho, MD,<br />
Christopher Myers, MD, Dana Portenier, MD, Duke University Medical<br />
Center<br />
V084 SINGLE PORT ACCESS LAPAROSCOPIC LOOP ILEOSTOMY;<br />
A FEASIBILITY STUDY Diana Cheng-Robles, Zuri Murrell, Rodrigo<br />
Alban, Som Kohanzadeh, Phillip Fleshner, Cedars Sinai Medical Center<br />
V085 LAPAROSCOPIC ROBOTIC POSTERIOR RETROPERITONEAL<br />
ADRENALECTOMY:TECHNICAL DETAILS Eren Berber, MD, Hizir<br />
Akyildiz, MD, Jamie Mitchell, MD, Mira Milas, MD, Allan Siperstein, MD,<br />
Cleveland Clinic<br />
V086 ENDOSCOPIC UNROOFING OF A POSTRAUMATIC SPLENIC<br />
CYST THROUGH A TRANSUMBILICAL SINGLE PORT ACCESS<br />
EM Targarona, MD, C Balague, MD, L Pallares, MD, F Marinello, D, C<br />
Rodriguez-Luppi, MD, L Estalella, MD, C Martinez, MD, MP Hernandez,<br />
MD, M Trias, M, Hospital Santpau, UAB, Barcelona, Spain.<br />
Videos in the Video Channel Loop<br />
can be viewed in the dedicated viewing area<br />
set up in the Exhibit Hall. The viewing area will be<br />
set up next to the Learning Center.<br />
12 th World Congress of Endoscopic Surgery<br />
Look for the hanging sign<br />
“<strong>2010</strong> Video Channel Loop Viewing Area.”<br />
Viewing hours are subject to the Exhibit Hall hours.<br />
149 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Posters of Distinction Abstracts<br />
P001<br />
EVALUATION OF THE SLEEVE GASTRECTOMY AS A SINGLE-STAGE<br />
TREATMENT OF MORBID OBESITY Philippe A Topart, MD, Cyril Chazelet,<br />
MD, Pierre Verhaeghe, MD FACS Societe de Chirurgie Viscerale, Clinique<br />
de l’Anjou, Angers ; Clinique St Brice, Provins, Chirurgie Viscerale, CHU,<br />
Amiens, France<br />
Objectives: A multicenter, retrospective study reviewed the current<br />
practice of the sleeve gastrectomy in Europe to assess the early<br />
postoperative outcome as well as the effect on weight loss.<br />
Methods and procedures<br />
446 sleeve gastrectomies were performed by 14 centers between<br />
September 2000 and October 2007. Operative data, postoperative<br />
outcomes as well as 2 year weight loss were reviewed.<br />
Results: The initial mean BMI of the patients was 46 (range 30-71) and<br />
their mean age 43 (18-70). 83% were women. 45% had at last 1 comorbid<br />
condition and 25% were gastric band failures. 99% of the procedures were<br />
performed laparoscopically with a 0.7% conversion rate. The sleeve was<br />
fashioned on a 34 to 50 Fr bougie. Methylene blue test was routine and<br />
25% of the patients kept a naso-gastric tube for 48 hours. The staple line<br />
was oversewn or reinforced with buttressing material in 263 patients. The<br />
mean operative time was 105 mn (30-550) without difference according<br />
to the BMI. The overall rate of complications was 16.7% with 5.3% major<br />
(19/20 were gastric leaks) but none were fatal. Although the leak rate was<br />
reduced with staple line reinforcement (0 vs 4.5%) and oversewing (3.3<br />
vs 6.3%), this was not significant and the only prognostic factor was the<br />
operation duration (p=0.03). The percentage of excess weight loss was<br />
stable after 1 year and 64% at 2 years. Male gender, comorbidities and BMI<br />
>50 significantly and adversely influenced weight loss.<br />
Conclusion: This large series demonstrates the safety of the sleeve<br />
gastrectomy. Although 2 year weight loss seems on par with gastric<br />
bypass, long term assessment is needed and limitating factors may exist.<br />
P002<br />
PATIENTS EXPECT TO LOSE MORE THAN AVERAGE WEIGHT AFTER<br />
BARIATRIC SURGERY Brad E Snyder, MD, Erik B Wilson, MD FACS, Todd<br />
Wilson, MD, Connie Klein, RN NP University of Texas Health Sciences<br />
Center at Houston<br />
Background: While most bariatric surgeons try to help patient achieve<br />
a realistic goal weight after surgery, patients are often disappointed<br />
that they have not reached “ideal” body weight. We propose that this is<br />
because patients begin the surgical process with inflated self expectations<br />
and set themselves up for disappointment.<br />
Methods and Procedures: At the University of Texas in Houston, we<br />
recorded the patient expected % excessive weights of 125 preoperative<br />
gastric banding patients and 36 gastric bypass patients. Frequencies of<br />
expected weight loss were graphed for different percentages of weight<br />
loss. Patient expectations were separated by gender and compared using<br />
Student’s t-test.<br />
Result: Despite abundant education about the procedure and the<br />
average weight loss for our patients in our program, patients drastically<br />
overestimated the %EWL they would obtain. In the banding group, 88 out<br />
of 125 patients (70%) expected to lose more than 80% excessive weight<br />
(EW). For the bypass group, 24 of the 36 (67%) patients expected to lose<br />
more than 90% EW. 82% of the banding group and 89% of the bypass<br />
group were women. Women had significantly higher expectations for<br />
weight loss than men for both banding and bypass (p
Posters of Distinction Abstracts<br />
P004<br />
SINGLE INCISION LAPAROSCOPIC GASTRIC BANDING: EVOLUTION<br />
TOWARDS SCARLESS SURGERY DURING 50 CONSECUTIVE CASES<br />
Sarah C Oltmann, MD, Lauren Mashaud, MD, Stephanie Morris, BS, Arsalla<br />
Islam, MD, Homero Rivas, MD MBA, Daniel J Scott, MD Southwestern<br />
Center for Minimally Invasive Surgery, Department of Surgery, University<br />
of Texas Southwestern Medical Center, Dallas, TX<br />
INTRODUCTION: Single incision laparoscopic surgery (SILS) may prove<br />
beneficial but techniques are still evolving. The purpose of this study was<br />
to assess outcomes associated with a SILS approach for adjustable gastric<br />
banding (AGB) for morbid obesity.<br />
METHODS: We conducted an IRB-approved retrospective review of our<br />
first 50 consecutive SILS AGB procedures attempted over an 18-month<br />
period. All patients were managed by a single attending surgeon at an<br />
academic center. A modified SILS approach was used in 44 cases, in which<br />
a separate subxyphoid incision was used for Nathanson liver retractor<br />
placement; a “pure” SILS approach, in which only a single incision was<br />
used for insertion of all laparoscopic instruments, was used in 6 cases.<br />
A Nathanson retractor was used in 45 cases and intracorporeal liver<br />
retraction was achieved using suture and/or umbilical tape in 5 cases.<br />
Operating instruments included straight and articulating tools placed<br />
through 3 separate working ports (n=48) or a multiport access device<br />
(n=2), via a LUQ (n=41) or umbilical (n=9) incision. Data are displayed as<br />
mean ± standard deviation, unless otherwise stated.<br />
RESULTS: Patient age was 41.4 years (range 18 – 69); 42 patients were<br />
female and 8 male. Pre-operative weight was 122 ± 22 kg, with a BMI of<br />
45.5 kg/m² (35 – 67). 28 patients had previous abdominal surgery, most<br />
commonly hysterectomy (n=10) or cholecystectomy (n=9). Operative<br />
time was 110 minutes (48 – 165), and 18 cases had additional procedures<br />
performed: 15 hiatal hernia repairs, 1 umbilical hernia repair, 1 EGD, and<br />
1 liver biopsy. Estimated blood loss was 23 cc ± 22. Incision length for<br />
working port(s) was 4.5 cm ± 0.9. In 4 cases, an additional port (separate<br />
from single-incision operative site) was required for placement of<br />
additional liver retractor (n=2), suction irrigator for bleeding (n=1), or<br />
additional grasper for retrogastric tunnel creation (n=1). There was one<br />
conversion to traditional 5-port laparoscopic approach in a patient with<br />
severe hepatomegaly, and no conversions to open. 4 complications (1<br />
major, 3 minor) were noted in 3 patients. The major complication was a<br />
mid-esophageal perforation secondary to calibration tube manipulation,<br />
successfully treated with esophageal stenting and left chest drainage.<br />
Minor complications included: gastric obstruction secondary to postop<br />
edema managed expectantly, a liver laceration treated with direct<br />
pressure, an upper extremity DVT secondary to PICC line for TPN in<br />
the esophageal perforation patient managed with line removal and<br />
anticoagulation. Routine POD 1 imaging was normal except in two cases,<br />
as noted above. Median hospital stay was 1 day (1-28). BMI reduction<br />
averaged 4.4 ± 3.8 kg/m2 over a mean follow-up of 6.8 ± 4 months.<br />
CONCLUSION: Although techniques are still evolving, SILS AGB appears<br />
to be feasible for achieving satisfactory band placement and safe from<br />
the viewpoint of intra-abdominal tissue manipulation. Continued work<br />
is needed to further improve operative strategies, determine relative<br />
benefit compared to traditional approaches, and to investigate long-term<br />
outcomes.<br />
P005<br />
CLINICAL OUTCOMES OF ATYPICAL SYMPTOMS FOLLOWING<br />
LAPAROSCOPIC ANTIREFLUX SURGERY Shaun R Brown, DO, C. Prakash<br />
Gyawali, MD, Lora Melman, MD, Eric D Jenkins, MD, Julia Bader, PhD,<br />
Margaret M Frisella, RN, L. Michael Brunt, MD, J. Christopher Eagon, MD,<br />
Michael M Awad, MD PhD, Brent D Matthews, MD Department of Surgery,<br />
Section of Minimally Invasive Surgery, Washington University School of<br />
Medicine, Saint Louis, MO<br />
Introduction: Gastroesophageal reflux disease (GERD) can manifest with<br />
both typical (heartburn, regurgitation) and atypical symptoms (cough,<br />
hoarseness, wheeze). While it is well established that antireflux surgery<br />
is effective in relieving typical symptoms, it is currently unclear whether<br />
atypical symptoms foreshadow a less satisfactory outcome following<br />
laparoscopic antireflux surgery (LARS). The purpose of this study is to<br />
critically analyze the clinical outcomes of atypical symptoms in patients<br />
undergoing LARS.<br />
Methods: Patients scheduled for LARS were prospectively enrolled in<br />
this IRB-approved study over a 5 year period. All subjects included in<br />
this study underwent preoperative high resolution manometry (HRM)<br />
and had evidence of GERD on an ambulatory pH study. For the purpose<br />
of this study, cough, wheeze and hoarseness were considered atypical<br />
symptoms. During preoperative and postoperative examinations, patients<br />
completed detailed foregut symptom questionnaires, using both 5-point<br />
Likert and 10-point visual analog scales (VAS) to document typical as well<br />
as atypical symptoms. Atypical symptom burden was calculated as a sum<br />
of VAS for the three atypical symptoms, termed the atypical score (ATS).<br />
HRM patterns were grouped into normal, spastic and hypomotile. Data<br />
are expressed as mean ± standard errors of mean. Statistical significance<br />
(p
12 th World Congress of Endoscopic Surgery<br />
Posters of Distinction Abstracts<br />
(LGS). Multiple logistic regression was performed to determine whether<br />
ultrasound findings and patient characteristics (age, BMI, and sex)<br />
predicted the ability of the specimen to pass through the overtube.<br />
Results: Specimens from 57 patients were examined. Forty-four<br />
patients (35 female, 9 male) had preoperative ultrasounds that were<br />
available for electronic review and were included in the analysis. Mean<br />
± standard deviation for age and BMI were 42 ± 12 years, and 32 ± 8 kg/<br />
m2. Ultrasound dimensions for gallbladder length, width, depth, and<br />
wall thickness were 80 ± 17mm, 35 ± 12mm, 28 ± 10mm, 3 ± 1mm.<br />
CBD diameter was 4 ± 2 mm. Gallstones were absent in 11 patients,<br />
and present in 35. In patients with gallstones, measurement of LGS<br />
was successful in 23 patients with a mean diameter of 12 ± 8mm. LGS<br />
was indeterminate (IGS) in the remaining 12 patients due to artifact<br />
from multiple stones. Eighteen gallbladders were perforated during<br />
the operation. Rate of passage for perforated versus intact gallbladders<br />
was not statistically different (40% v. 23%, p = 0.054 with Fisher’s exact<br />
test). Weight, BMI, LGS, and IGS were predictors of passage through the<br />
overtube on univariate logistic regression. However, only LGS (Odds ratio<br />
1.167, 95% confidence interval 1.023-1.332, p = 0.021) and IGS (Odds<br />
ratio 22.965, 95% confidence interval 1.986 – 265.629, p = 0.025) were<br />
significant predictors of passage on multivariate logistic regression.<br />
Passage rate was 80% when LGS < 10mm or no stones were present, 18%<br />
when LGS was greater than or equal to 10mm, and 8% with IGS (Pearson<br />
Chi-Square, p value < 0.001).<br />
Conclusion: Preoperative ultrasound findings predict gallbladder<br />
extraction during transgastric NOTES cholecystectomy. IGS, or LGS greater<br />
than or equal to 10mm should be considered relative contraindications to<br />
transgastric NOTES cholecystectomy.<br />
P007<br />
A COMPARISON OF PRE-OPERATIVE COMORBIDITIES AND<br />
POST-OPERATIVE OUTCOMES AMONG PATIENTS UNDERGOING<br />
LAPAROSCOPIC NISSEN FUNDOPLICAITON AT HIGH AND LOW<br />
VOLUME CENTERS Oliver A Varban, MD, Thomas McCoy, MS, Carl<br />
Westcott, MD Wake Forest University Baptist Medical Center<br />
Objective: Peer reviewed data is often published by single centers that<br />
are affiliated with teaching institutions with a high volume of cases.<br />
As operations grow in popularity, they are performed at a wide variety<br />
of institutions with the potential to produce inconsistent results. The<br />
purpose of this study is to compare pre-operative comorbidities and postoperative<br />
outcomes between patients that have undergone laparoscopic<br />
Nissen fundoplication (LNF) at high and low volume centers across North<br />
Carolina.<br />
Methods: This is a retrospective study using the North Carolina<br />
Hospital Association Patient Data System database. Selected patients<br />
include adults (>17 years old) that have undergone laparoscopic Nissen<br />
fundoplication for gastroesophageal reflux disease (GERD). Patients<br />
that underwent operative management for emergent purposes, or had<br />
associated diagnoses of esophageal cancer or achalasia were excluded<br />
from the study. High volume centers are defined as institutions that<br />
performed ten or more LNFs per year averaged over a period of four years.<br />
Comparative statistics are performed on a number of variables between<br />
high and low volume centers.<br />
Results: A total of 1019 patients underwent laparoscopic Nissen<br />
fundoplication for GERD in North Carolina between 2004 and 2008. High<br />
volume centers performed 530 LNFs (52%) while low volume centers<br />
performed 489 LNFs (48%). Patients at high volume centers were older<br />
(52.5 yo vs. 49.0 yo, p=0.019), had a higher incidence of diabetes (13.4%<br />
vs. 8.8%, p=0.026), chronic obstructive pulmonary disease (5.1% vs. 2 %,<br />
p=0.015), hyperlipidemia (9.6% vs. 4.7%, p=0.004) and cystic fibrosis (2.8%<br />
vs 0.8%, p=0.03). Patients with a history of transplantation were also more<br />
likely to undergo LNF at a high volume center (15.8% vs. 1.6%, p=3.1 x10-<br />
15). There were no deaths among the two groups and also no difference<br />
between median length of stay (2 days). Low volume centers had a higher<br />
incidence of intraoperative accidental puncture or laceration (3.3% vs.<br />
0.9%, p=0.017) while high volume centers had a higher incidence of<br />
pulmonary collapse (5.3% vs 2.5%, p=0.031).<br />
12 th World Congress of Endoscopic Surgery 152<br />
Conclusions: Patients undergoing LNF at high volume centers tend to be<br />
older and have more comorbidities than patients at low volume centers.<br />
Although there was a higher incidence of intraoperative accidental<br />
puncture or laceration among patients at the low volume centers, there<br />
was no difference between median length of stay and there was no<br />
associated mortality. Although patient selection and complications are<br />
different, overall outcomes are the same at high and low volume centers.<br />
P008<br />
102 CONSECUTIVE ROBOTIC ASSISTED MINIMALLY INVASIVE<br />
COLECTOMIES - AN OUTCOME AND TECHNICAL UPDATE Franziska<br />
Huettner, MD PhD, Paul E Pacheco, MD, Jamie L Doubet, RN BS, Michael<br />
J Ryan, MS, Danuta I Dynda, MD, David L Crawford, MD Division of<br />
Minimally Invasive Surgery, Department of Surgery, University of Illinois<br />
College of Medicine at Peoria<br />
Objective: The purpose of the study was to review 102 consecutive<br />
robotic-assisted laparoscopic colectomies at our institution. We evaluated<br />
the eight-year experience (2002–2009) of one minimally invasive surgery<br />
(MIS) fellowship trained surgeon using the da Vinci Telerobotic system.<br />
Colon procedures are 6th most commonly performed procedure of the<br />
senior author annually.<br />
Methods: An IRB approved retrospective review of prospectively<br />
collected data from 2002–2009 representing 102 colon operations<br />
was performed. Data analyzed were: procedure performed; indication<br />
for surgery; gender; age; body mass index (BMI); estimated blood loss<br />
(EBL); port setup time (PST); robot operating time (ROT); total case time<br />
(TCT); length of stay (LOS); complications; conversions; and resident<br />
involvement. Statistical Analysis using the Anova test was performed.<br />
The changes in technique and operative approach for right and sigmoid<br />
colectomy over the years were evaluated. The results were compared with<br />
the current literature.<br />
Results: One-hundred and two robotic colectomies, right (59) and<br />
sigmoid (43), were performed in 49 males and 53 females. Average patient<br />
age was 63.5 + 13.6 (22-86) years. Mean BMI was 27.4 + 4.3 (17.0-40.5) kg/<br />
m². Preoperative indications included: polyps (53); diverticular disease<br />
(27); cancer (19); and carcinoid (3). Mean total operative time for all cases<br />
was 219.6 ± 45.1 (50-380) min, with a mean robot time of 126.6 + 41.6<br />
(12-306) min. Operative times for right colectomies were: PST 32.4 ± 10.5<br />
(20-64) min; ROT 145.2 ± 39.6 (53-306) min; and TCT 212.3 ± 46.4 (50-380)<br />
min. Times for sigmoid colectomies were: PST 31.2 ± 9.6 (10-57) min; ROT<br />
101.2 ± 29.2 (12-165) min; and TCT 229.7 ± 41.6 (147-323) min. Mean EBL<br />
for right colectomies was 58.6 + 80.8 (15-500) ml and 77.6 + 54.7 (15-250)<br />
ml for left colectomies. Overall median length of stay for all patients was<br />
3 days with a range of 2 to 27 days. Complications occurred in 19 patients<br />
with an overall complication rate of 18.6%. Nine cases were converted –<br />
four to laparoscopic and five to open for a total conversion rate of 8.8%.<br />
Anastomotic leak occurred in one patient (0.98%). Residents PGY levels<br />
1-5 participated in 61 cases (59.8%).<br />
Conclusion: We demonstrate with this series that robotic colectomy is<br />
safe and feasible. Procedural sequence and technical alterations have<br />
been made that have improved efficiency. Senior author experience has<br />
allowed resident participation to evolve to the level of primary surgeon<br />
in both procedures. Our results compare favorably with other series in<br />
the robotic literature. Resident participation is critical if we hope to bring<br />
robotic procedures into the mainstream of surgical practice.<br />
P009<br />
238 LAPAROSCOPIC LEFT-SIDE COLORECTAL SURGERIES WITH<br />
N.O.S.E.: A 10-YEAR EXPERIENCE WITH TRANSANAL SPECIMEN<br />
EXTRACTION Morris E Franklin, Jr, MD FACS, Song Liang, MD PHD The<br />
Texas Endosurgery Institute<br />
BACKGOUND AND OBJECTIVE: Natural Orifice Specimen Extraction<br />
(NOSE) has been postulated as an alternative approach to deliver<br />
the resected specimen out of peritoneal cavity through an anatomic<br />
passage rather than any abdominal incision after laparoscopic<br />
colorectal resections. This prospective study focused on the patients<br />
who underwent various laparoscopic left-side colorectal surgeries<br />
with intracorporeal anastomosis and transanal specimen extraction at
Posters of Distinction Abstracts<br />
our institute in the past 10 years with the specific aim to investigate if<br />
transanal approach can be accepted as a safe and effective method for<br />
extracting the specimen from abdominal cavity in laparoscopic colorectal<br />
surgeries.<br />
METHODS: A prospectively designed database of a consecutive series<br />
of patients undergoing various laparoscopic colorectal surgeries with<br />
transanal specimen extraction for different left-side colonic as well<br />
rectal pathologies between April 1995 and May 2006 was analyzed<br />
on categories of age, gender, co-morbidities, preoperative diagnosis,<br />
indications for surgery, American Society of Anesthesiology Class,<br />
types of surgery, operating time, intraoperative blood loss, intra- and<br />
postoperative complications, tumor size, lymph node status, results of<br />
postoperative pathology, AJCC TMN Stage, length of hospitalization,<br />
cancer recurrence, and causes of death. Patient selection for laparoscopic<br />
colorectal surgeries with intracorporeal anastomosis and transanal<br />
specimen extraction was made on the basis of entities of diseases, size of<br />
the tumor, and distance of colorectal lesions to the anal verge.<br />
RESULTS: 238 various colorectal procedures including 6 left<br />
hemicolectomy (2.5%), 83 sigmoidectomy (34.9%), and 149 low anterior<br />
resection (62.6%) were completed laparoscopically with intracorporeal<br />
anastomosis (ICA) and transanal specimen extraction (TASE). The straight<br />
and circular surgical stapling devices including Endo-GIA and EEA were<br />
used to create anastomosis intracorporeally in all 238 laparoscopic<br />
colorectal resections. Pathological evaluation of all the surgical specimens<br />
demonstrated 167 malignant tumors with various AJCC TMN stages<br />
(70.2%) and 69 diverticulitis (29%). The operating time for laparoscopic<br />
colorectal resections with ICA and TASE was 157.3 +/- 51.4 minutes, blood<br />
loss during the surgeries was 96.8 +/- 76.5 ml, and distance from the lower<br />
edge of the lesion to the anal verge was measured to be 11.8+/- 8.2 cm.<br />
One patient developing postoperative anastomotic leakage with leak<br />
rate of 0.42%, and overall rate of major complications after the surgeries<br />
is 2.1%. The length of hospital stay was 6.9 +/- 2.8 days. 2-year followup<br />
showed the development of anal stenosis in 3 patients (2.0%) and<br />
erectile dysfunction in one patient (0.67%) after the procedures. Lastly 7<br />
out of 149 patients underwent laparoscopic low anterior resection with<br />
ICA and TASE were confirmed to have cancer recurrences with the 2-year<br />
local cancer recurrence rate of 4.7%, furthermore the patients having<br />
preopeative chemoradiation therapy had higher recurrence rate (11.3%)<br />
than that of the patients without (1.0%).<br />
CONCLUSIONS: As a bridge to NOTES, transanal specimen extraction in<br />
laparoscopic colorectal surgeries is a safe and effective approach with low<br />
local cancer recurrence and other long as well as short-term postoperative<br />
complication rates, suggesting it can be integrated into laparoscopic<br />
colorectal surgeries for left-side colorectal pathologies including cancer.<br />
More importantly, NOSE does not unnecessarily traumatize other<br />
normal organs.<br />
P010<br />
SINGLE-INCISION LAPAROSCOPIC COLECTOMY FOR COLON CANCER:<br />
EXPERIENCE OF 35 CASES Bac H Nguyen, PhD, Thinh H Nguyen, MD, Viet<br />
V Ung, MD University Medical Center at Ho Chi Minh City<br />
Objective: Single-port trans-umbilical laparoscopy has emerged as an<br />
attempt to further enhance cosmetic benefits and reduce morbidity<br />
of minimally invasive surgery. There were some reports about singleport<br />
laparoscopic colectomy in the world. However, this technique<br />
requires a specialized multichannel port for introducing laparoscope<br />
and articulating instruments. We present our preliminary experience of<br />
using conventional ports and straight instruments for performing singleincision<br />
laparoscopic colectomy (SILC).<br />
Methods: We inserted 3 ports (one 10-mm port and two 5-mm ports) at<br />
different places in midline through the 4cm umbilical incision. Using 450<br />
scope and conventional straight laparoscopic instruments, the dissection<br />
was performed in a medial-to-lateral fashion with extracorporeal<br />
anastomosis. This is a prospective study of consecutive 35 colon cancer<br />
patients who underwent SILC between May and September 2009.<br />
Results: There were 35 patients (16 males, 19 females); median age 59.1<br />
years. Right hemicolectomy was performed in 11 patients (31%), left<br />
hemicolectomy in 9 (26%), sigmoidectomy in 12 (34%), right and left<br />
colectomy for synchronous colon cancer in 2 (6%), left hemicolectomy<br />
and cholecystectomy in 1 (3%). The median operative time was 115 min<br />
(80-145). There was no conversion, no intraoperative complications or<br />
postoperative complications. The mean estimated blood loss was 10ml.<br />
All of patients had safe margin of resection. Overall morbidity rate was<br />
6.2%, with no significant difference between right hemicolectomy and left<br />
hemicolectomy or sigmoidectomy. The length of hospital stay was 5 days.<br />
Conclusions: Single-incision laparoscopic colectomy is technically feasible<br />
and safe. This technique may be an alternative for current specialized port<br />
and instruments. Greater numbers and a randomized controlled trial will<br />
be necessary to access the true benefit of this approach.<br />
P011<br />
SAFETY AND USEFULNESS OF LAPAROSCOPIC METHOD FOR<br />
TREATMENT OF PERITONITIS DUE TO ANASTOMOSIS SITE LEAKAGE<br />
AFTER RECTAL CANCER RESECTION Gyu-Seog Choi, MD, Kyoung-<br />
Hoon Lim, MD, Jun Seok Park, MD, You Seok Jang, MD, Soo-Han Jun,<br />
MD Department of Surgery, School of Medicine, Kyungpook National<br />
University, Daegu, Korea<br />
Introduction:In cases of peritonitis due to anastomosis site leakage<br />
after rectal cancer resection where surgical management was necessary,<br />
patients who have undergone open laparotomy and patients with<br />
laparoscopic exploration have been compared to determine safety and<br />
usefulness of laparoscopic method.<br />
Methods:Out of 1146 patients who have undergone rectal cancer<br />
resection excluding patients with AP, double primary maliganancy,<br />
preoerative ileostomy, and FAP, 97 patients who suffered anastomosis<br />
sited leakage have been compared and analyzed for peritonitis sx,<br />
operation method, operation time for second op, complication after<br />
operation, hospitalization time after second operation, and location of<br />
anastomosis. In case of open laparotomy, previous op wound was used,<br />
and in case of laparoscopy, only previous trocar sites were used, not mini<br />
laparotomy site. In reoperation, intra peritoneum irrigation was done in<br />
all patients, ileostomy was done in 47 patients, and 4 patients only did a<br />
simple closure without ileostomy. Of the 47 patients who had ileostomy,<br />
39 patients had only ileostomy, 6 patients had simple closure with<br />
ileostomy, and remaining 2 patients had reanastomosis with ileostomy.<br />
Results: Of the total 1146 patients, 97 patients had anastomosis site<br />
leakage, and 51 patients had peritonitis symptom requiring intra<br />
peritoneal irrigation. Patients who previously had open surgery<br />
done open laparotomy for reoperation, patients who previously had<br />
laparoscopic surgery done laparoscopy for reoperation. 21 patients<br />
had laparoscopy, 30 patients had open laparotomy. There were no<br />
difference in age, sex ration, or anastomosis location between two<br />
groups. Hospitalization time after reoperation in laparoscopy group<br />
was noticeably shorter than that of open laparotomy group (16.3±10.9<br />
days vs. 33.4 ± 19.7 days, p
12 th World Congress of Endoscopic Surgery<br />
Posters of Distinction Abstracts<br />
P012<br />
INDICATIONS, COMPLICATIONS AND LONG TERM OUTCOMES OF<br />
REMNANT GASTRECTOMY FOR GASTRO-GASTRIC FISTULA AFTER<br />
DIVIDED ROUX-EN-Y GASTRIC BYPASS FOR MORBID OBESITY Emeka<br />
Acholonu, Jeremy Eckstein, Sheetal Patel, Wasef Abu-Jaish, Samuel<br />
Szomstein, Raul Rosenthal Cleveland Clinic Florida<br />
Background: GGF is a rare complication after divided RYGBP for morbid<br />
obesity. Medical management has proved grossly ineffective. Less<br />
invasive methods like fibrin glue and sealants via an endoscopic approach<br />
have been reported with recurrence rates as high as 75 %.<br />
Method: After IRB approval and following HIPAA guidelines, we<br />
retrospectively analyzed our prospectively collected database for 2226<br />
patients that underwent LRG for GGF after divided RYGBP between April<br />
2001 and September 2008. RYGB divided were completed over this period<br />
as well as referred cases from outside institutions. The procedure entails<br />
dissecting out the pouch and remnant stomach, stapling off the GGF and<br />
transecting the remnant stomach at the antrum. A total of 60 cases were<br />
completed. Our patients were followed up 10 days, 2 months, 6 months<br />
and yearly after discharge.<br />
Results: There were 51 females (85%) and 9 males (15%). The age range<br />
was between 25 and 68 (average 45), the BMI ranged between 20 and<br />
58.7 (average 36.3).The most common indication for the procedure was<br />
pain, other indications include recurrent or persistent ulcers, weight<br />
regain, upper gastrointestinal bleed, intractable nausea and vomiting.<br />
10 (17%) of the procedures were converted to open. We did not regard<br />
conversion as a complication but as a judgment call, opting for safer<br />
treatment. There was a 15% complication rate (9 patients) and the most<br />
common complication was leakage from staple lines. Our cumulative long<br />
term outcome suggests most patients were satisfied with the results. 4<br />
patients (7%) complained of persistent unexplained pain. There has been<br />
no recurrence and there has been no mortality.<br />
Conclusions: LRG seems to be a safe, feasible and reliable option to<br />
treat GGF after divided RYGB, with significant relief of symptoms and<br />
acceptable perioperative morbidity.<br />
P013<br />
NEEDLESCOPIC SURGERY: THE COSMETIC ALTERNATIVE TO SILS Morris<br />
E Franklin, MD, Karla Russek, MD, Jojy George, MD Texas Endosurgery<br />
Institute<br />
Introduction: Minimally invasive procedures have revolutionized the<br />
art of surgical practice. Laparoscopic cholecystectomy (LC) is the gold<br />
standard for management of gall bladder disease. In an attempt to further<br />
improve on the benefits of the standard multiple incision LC, less invasive<br />
methods have been described, including smaller incisions, fewer incisions,<br />
and use of single incisions. Needlescopic cholecystectomy (NC) utilizes 2<br />
or 3 mm instruments and has been shown to provide improved cosmesis.<br />
Single incision is a newer approach to cholecystectomy, with theoretical<br />
advantage of improved cosmesis and reduced postoperative wound<br />
complications.<br />
Methods: All 404 operations at TEI were done by a single surgeon from<br />
1995-2008. 86% of subjects were female, and average age of all subjects<br />
was 41.9 years (range 14-82). Average BMI was 25.7 (range 16.4 -39.2).<br />
19.6 % of patients had previous abdominal surgery. Ultrasound findings<br />
most commonly was cholelithiasis; no patients had preoperative imaging<br />
indicating common duct stones, and only one patient was found to<br />
have a dilated (>1cm) CBD on preoperative ultrasound. We performed<br />
intraoperative cholangiograms on all patients regardless of preoperative<br />
diagnosis, laboratory values or ultrasound findings.<br />
Results: Only once was a CBD stone found on cholangiogram, and a<br />
CBDE, stone extraction and T-Tube placement was performed. Average<br />
operating time was 59.3 minutes (range 30- 200). One 200 minute<br />
operation required laparoscopic CBDE, accounting for the extended time.<br />
Average estimated intraoperative blood loss (EBL) was < 15 cc ( range<br />
0-50cc). 2% of cases required conversion to standard 5 mm LC and was<br />
completed without incident. Since 1995, only one patient presented with<br />
a hernia at the umbilical site. Otherwise, no wound, bile duct, bile leaks,<br />
bleeding complications or hernias have been identified.<br />
12 th World Congress of Endoscopic Surgery 154<br />
Conclusion: We propose that NC currently provides a better cosmetic<br />
result over standard LC and SILS cholecystectomy, with fewer theoretical<br />
and actual wound and hernia complications.<br />
P014<br />
ROLE OF INTERLEUKIN-6 (IL-6) IN THE GROWTH OF CT26 COLORECTAL<br />
CANCER IN A MURINE MODEL Melissa A Donigan, BS, Heidi Bahna,<br />
MD, Bryan D Loh, MD, Laurie S Norcross, MD, John Aversa, DO, Paul<br />
R Williamson, MD, Samuel DeJesus, MD, Andrea Ferrara, MD, Joseph<br />
T Gallagher, MD, Cheryl H Baker, PhD M. D. Anderson Cancer Center<br />
Orlando, University of Central Florida, Colon and Rectal Clinic of Orlando,<br />
Orlando Regional Medical Center<br />
PURPOSE: This study is designed to investigate the role of surgeryinduced<br />
levels of cytokines in affecting proliferation and migration of<br />
colon cancer cells. Clinical standards in the management of colon cancer<br />
and surgery-related differences in various cytokines have been predicted<br />
to correlate with the degree of trauma afflicted during surgery, ultimately<br />
impacting tumor growth and metastasis. Laparoscopic surgery is thought<br />
to stimulate less of an acute cytokine (IL-1β, TNF-α, IL-6) response<br />
than open surgery, thereby preserving normal immune function. The<br />
significance of the surgery-related differences in these cytokines may<br />
correlate with the degree of anterior abdominal wall trauma.<br />
METHODS: Murine colon cancer CT26 cells were incubated in the<br />
absence or presence of 1-10 uM recombinant mouse IL-6. Protein<br />
expression of IL-6 and its receptor (IL-6R) was measured and the cell<br />
proliferation/cell viability and migration was monitored by in vitro<br />
biological assays. In the first set of in vivo studies, non-tumor bearing<br />
Balb/c mice and Balb/c mice injected subcutaneously with CT26 cells<br />
received an open or laparoscopic surgery (LAS). Serum levels of IL-6<br />
were measured at 30 minutes, 2 hrs, 4 hrs, 6 hrs, 12 hrs, 24 hrs, and 48<br />
hrs following surgery. In a second set of murine studies, 10 Balb/c mice<br />
received either an intraperitoneal (i.p.) or a subcutaneous (s.c.) injection of<br />
1500 ng of recombinant mouse IL-6 immediately following s.c. injections<br />
of CT26 cells. Tumor growth was monitored by caliper measurements<br />
every three days for twenty-one days. Tumor-bearing mice that did not<br />
receive IL-6 injections served as controls.<br />
RESULTS: Colon cancer CT26 cells growing in vitro express low levels of<br />
IL-6 and IL-6R. CT26 cell proliferation and migration was not significantly<br />
increased in the presence of recombinant IL-6. There is a significant<br />
decrease in tumor take, size and volume of subcutaneously growing CT26<br />
cells in mice which received LAS surgery as compared to mice which<br />
received an open surgery, and control mice (no surgery). IL-6 levels in the<br />
open group peaked at 8 hours; in sharp contrast, IL-6 peaked in the LAS<br />
group at 4 hours. Interestingly, the peak (at their respective hours) in the<br />
open surgery group was significantly greater as compared to the LAS<br />
group. By 48 hours, the IL-6 levels for both groups normalized to baseline<br />
levels. Additionally, i.p. injection (and not the s.c. injection) of IL-6 into<br />
mice caused the most significant increase in tumor growth.<br />
CONCLUSION: These data suggest that surgery-induced (and not tumorderived)<br />
serum levels of IL-6 may play a crucial role in the in vivo growth<br />
of colon cancer. Understanding the differential effects of open versus<br />
laparoscopic surgery on the growth of colon cancer may significantly<br />
impact the immediate and long-term prognosis of colon cancer patients.<br />
P015<br />
LAPAROSCOPIC LIVER SURGERY IN CANCER PATIENTS-EXPERIENCE AT<br />
A NATIONAL CANCER INSTITUTE Ronald Matteotti, MD, John Hoffman,<br />
MD, Elie Chouillard, MD, Veeraiah Siripurapu, MD, Andrew Gumbs, MD<br />
FOX CHASE CANCER CENTER, Philadelphia-PA, USA<br />
Introduction: The oncological adequacy and safety of major liver<br />
resections is still uncertain. The aim of this retrospective analysis was to<br />
compare intraoperative data with final pathology and short-term clinical<br />
outcome.<br />
Methods:Patients undergoing laparoscopic liver surgery were<br />
retrospectively analysed using our tumor registry. Surgical and<br />
postsurgical outcomes were compared with final pathology. The data<br />
were statistically analyzed using ANOVA and Fisher’s Exact test.<br />
Results: Forty-nine consecutive liver procedures by a single surgeon
Posters of Distinction Abstracts<br />
were analyzed, of which 47 were attempted and 45 (96%) completed<br />
laparoscopically. Mean age was 62, mean BMI 27, average ASA was<br />
2. Fifteen underwent major resections (31%), 27 minor resections<br />
(56%) 7 (13%) underwent either an ablation or liver biopsy. The major<br />
hepatectomy group constituted of 5 laparoscopic left hepatectomies<br />
(33%), 10 right hepatectomies of which 8 were completed<br />
laparoscopically (80%). 95% of patients underwent additional procedures<br />
such as adhesiolysis, ablation or an additional wedge resection. In 4<br />
(9%) patients we encountered intraoperative complications, 2 required<br />
conversion. Our overall conversion rate was 4% and the reason for<br />
conversion was major bleeding from the parenchyma in one case, an<br />
IVC injury in another case, requiring a staged procedure. Two patients<br />
had diaphragm injuries that were repaired laparoscopically, the second<br />
patient also had an injury to the IVC that was repaired laparoscopcally.<br />
Twenty-two percent had a postoperative complication, mainly DVT,<br />
one pulmonary embolism, and ileus. We only encountered one postoperative<br />
bile leak. Lymph node dissection in the hepatoduodenal<br />
ligament was only necessary in 19% of the patients (n=9). We never used<br />
portal clamping and a drain was only placed in 19% of the patients (n=9).<br />
Preoperative embolization before major resections was done in 4% of the<br />
patients. Mean EBL was 403 cc, Mean operative time was 259 min.<br />
n Mean EBL Mean OR time<br />
Major resection 15 1000 cc 383 min<br />
Minor resection 27 90 cc 120 min<br />
Intraoperative obtained frozen sections were positive in 27% requiring<br />
re-resection during the same surgery. Thirty-six patients were given a<br />
diagnosis of malignancy upon final pathology. Margins were positive in<br />
1 (2%) patient. In 29 patients we were dealing with stage 4 disease, n=21<br />
being colorectal cancer metastatic to the liver.<br />
Size (mm) Volume (cc) Weight (gr) Distance tumor to margin (mm)<br />
111 925 605 14<br />
The mean hospital stay was 4.8 days. Thirty-day mortality was 0%. Four<br />
patients required intraoperative blood transfusion of 2 units of pRBCs.<br />
Infectious complications during hospital stay was only seen in n=1, an<br />
intra-abdominal abscess, requiring drainage by interventional radiology.<br />
Conclusions: Laparoscopic liver surgery at a major cancer center is safe,<br />
feasible and does not translate into more complications intraoperatively<br />
or postoperatively. Mean hospital stay, short term mortality are<br />
comparable to similar series in the literature, reporting open procedures.<br />
Most important, a laparoscopic approach does not violate oncological<br />
principles intraoperatively, tumor visualization is excellent and adequate<br />
margins can be obtained. Long-term follow up data will be needed to<br />
compare laparoscopy to an open approach in terms of survival and<br />
quality of life.<br />
P016<br />
IS SURGERY A BETTER OPTION AS FIRST LINE TREATMENT<br />
FOR ACHALASIA?: A COMPARISON OF LAPAROSCOPIC<br />
ESOPHAGOMYOTOMY WITH FUNDOPLICATION AND ENDOSCOPIC<br />
DILATION Jason F Reynoso, MD, Manish M Tiwari, MD PhD MPH, Albert<br />
W Tsang, MD, Dmitry Oleynikov, MD Department of Surgery, University of<br />
Nebraska Medical Center<br />
INTRODUCTION: Recent studies have shown laparoscopic<br />
esophagomyotomy with fundoplication (LM) to have superior long-term<br />
symptom relief and low rates of post-operative gastroesophageal reflux<br />
when compared to endoscopic dilation (ED). This study evaluates the<br />
morbidity, mortality and cost of treating achalasia with LM versus ED.<br />
METHODS: The University HealthSystem Consortium (UHC) is an alliance<br />
of more than 100 academic medical centers and nearly 200 affiliate<br />
hospitals. UHC’s Clinical Data Base / Resource Manager (CDB/RM) allows<br />
member hospitals to compare patient-level risk-adjusted outcomes for<br />
performance improvement purposes. The CDB/RM was queried using<br />
ICD-9 diagnosis and procedural codes for patients with achalasia who<br />
underwent LM (N=1,390) or ED (N=492) during a 37 month period<br />
between January 2006 and January 2009. Overall comorbidity, mortality,<br />
readmission rates, hospital cost and specific complications are assessed in<br />
this multicenter, retrospective study.<br />
RESULTS: Overall esophageal perforation rates for LM and ED were 0.4%<br />
and 2.4% (p
12 th World Congress of Endoscopic Surgery<br />
Posters of Distinction Abstracts<br />
laparoscopic study task as well as the more expert groups because of<br />
prior specific training on this task as part of their curriculum. However,<br />
their performance declined dramatically when confronted with the<br />
challenges of the single port task. These results strongly suggest a role for<br />
systematic lab-based single port training prior to clinical application, as is<br />
now done for conventional laparoscopy.<br />
P018<br />
ONCOLOGIC AND PERIOPERATIVE OUTCOMES OF LAPAROSCOPIC<br />
ASSISTED VS HAND-ASSISSTED VS OPEN RESECTIONS FOR<br />
RECTAL CANCER RESECTION: A CASE MATCH STUDY. PORNTHAPE<br />
PRATHANVANICH, JIRAWAT Pattana_arun, CHUCHEEP Sahakitrungruang,<br />
PUTTARAT Atithansakul, ARUN Rojanasakul CHULALONGKORN<br />
UNIVERSITY<br />
Purpose: Advances in surgical techniques and improvements in<br />
laparoscopic instruments have enabled most colorectal procedures to be<br />
performed by using the laparoscopic approach.Laparoscopic surgery of<br />
colon cancer has been accepted to be oncologically adequate compared<br />
with open resection.However,the situation in rectal cancer remains<br />
unclear,because anatomy and complex surgical procedures.There have<br />
been only a few reports compare Laparoscopic assisted vs Hand-Assissted<br />
vs Open resections for rectal cancer resection.<br />
This study is designed to analyze oncologic and perioperative outcomes<br />
for selected patients;match by staging who undergoing in these three<br />
access of surgery.<br />
Methods: A total of 114 patients with rectal cancer,who underwent<br />
surgery by the same surgical team(2006-2008) are prospectively<br />
analyzed;by select the same staging.38 patients are choosen in each<br />
group.<br />
One-way ANOVA,Pearson’s chi-square and Fisher’sExact test are used to<br />
compare differences in demographics and perioperative parameters.<br />
Results: Each groups are comparable regarding age,gender,tumor<br />
localization,and complications.Each groups have 2/upper,6/middle,30/<br />
low rectal cancer and 5/stage 0,3/stage I,13/stage IIA,3/stage IIIA,9/stage<br />
IIIB, 4/stage IIIC,1/stage IV. No mortality occurred in either group.Mean<br />
operative times are not difference significantly between open and HALS<br />
group(276 min/open vs 263 min/HALS, p = 0.546).But difference are found<br />
in these both groups with laparoscopic surgery(344 min/lap , p=0.002<br />
and 0.000 respectively).Not difference significantly are found in first<br />
bowel movement between minimal invasive surgery(2.5 day/lap vs 1.9<br />
day/ HALS , p = 0.128),but difference with open group(3.5 day/ open , p =<br />
0.02 and 0.00 respectively).The mean tumor size is 4.5 cm/open, 3.6 cm/<br />
lap and 4.2 cm/HALS.The mean tumor-free margin is 1.6 cm/open,1.8 cm/<br />
lap and 2.3 cm/HALS group. And the mean number of harvested lymph<br />
nodes is 19.4 /open, 17.5 /lap and 17.6 /HALS group. No wound recurrene<br />
is observed.<br />
Conclusions: Minimal invasive surgery is equivalent with conventional<br />
surgery in the treatment of rectal cancer and shows advantages of faster<br />
recovery. Especially in patients with low rectal cancer,minimally invasive<br />
surgery with exact preparation of the total mesorectal excision seems to<br />
be favorable compared with open access surgery.<br />
P019<br />
“INCISIONLESS” LAPAROSCOPIC PROCTECTOMY: AN IDEAL NATURAL<br />
ORIFICE AND LAPAROSCOPIC SURGERY HYBRID John Marks, MD, Radu<br />
Nedelcoviciu, MD, Eileen Larkin, BA, Albert DeNittis, MD, Gerald Marks,<br />
MD Lankenau Hospital and Institute for Medical Research: Section of<br />
Colorectal Surgery, Wynnewood, PA<br />
Introduction: To evaluate the safety and efficacy of laparoscopic<br />
proctectomy with per-anal delivery of the specimen for rectal cancer,<br />
avoiding an incision for specimen extraction while accomplishing<br />
sphincter preservation we review our experience.<br />
Methods: Between 2001 and 2009, in a prospective database, 51 patients<br />
with invasive adenocarcinoma of the rectum underwent laparoscopic<br />
total mesorectal excision (TME) with delivery of the specimen transanally<br />
without the need for an additional incision to remove the specimen.<br />
Patients undergoing APR were excluded. Demographics were as follows:<br />
men=33, women=18, mean level in the rectum=1.5 cm (-0.5-5.0 cm).<br />
Pretreatment T stage was T1=1, T2=11, T3=39. Mean size of cancer was 4.2<br />
cm (2-10 cm). Fixity of the tumor was: mobile=33, tethered=15, fixed=2.<br />
Patients receiving chemotherapy: N=44. Mean radiation dose was 5385<br />
(4500-8040cGy). Mean BMI=26.2 (17.4-47.5).<br />
Results: Mean follow up was 21.2 months (1.4-80.3 months). There were<br />
no perioperative mortalities. There were no laparoscopic conversions.<br />
Mean EBL was 302 cc (75-1900cc). Transfusion rate was 2.0%. The mean<br />
size for the largest incision was 1.9cm (1.2-3cm). The mean total length<br />
of all incisions was 4.6cm (1.8-8cm). All patients were protected with<br />
a temporary stoma. Overall morbidity rate was 31%, major morbidity<br />
rate was 5.8% and included pelvic abscess N=2, fistula N=1. Pathology<br />
was complete response = 21%. ypT stage : T0=11, T1=8, T2=17, T3=15.<br />
ypN positive=15; ypN negative=36. Local Recurrence rate (LR) was 2.0%.<br />
One patient had a positive margin, undergoing subsequently an APR.<br />
Permanent 5 year stoma rate was 86%.<br />
Conclusion: For distal rectal cancer in need of a coloanal anastomosis,<br />
“incisionless” laparoscopic TME using the natural orifice, per-anal route for<br />
specimen delivery is a safe and accomplishable technique with good early<br />
oncologic results. Long term follow up and multi-institutional studies will<br />
be required to establish the widespread applicability of this promising<br />
technique.<br />
P020<br />
COLORECTAL CANCER RISK REDUCTION IN INFLAMMATORY BOWEL<br />
DISEASE WITH AMINOSALICYLATE THERAPY: A META-ANALYSIS<br />
AND COMPARISON TO COLORECTAL CANCER RISK IN THE GENERAL<br />
POPULATION Omer Nasir, MD, Amit Kaul, MD, Tejwant Datta, MD,<br />
Maryanne Franco, M Gilson, MD, Michael Marohn, DO, Hien Nguyen, MD<br />
Johns Hopkins University School of Medicine<br />
Background: Worldwide, the incidence rates for inflammatory bowel<br />
disease (IBD) vary from 0.5 to 24.5 per 100,000 people (0.012%). It has<br />
been estimated that the risk of CRC in IBD patients increases by 0.5%<br />
per year after eight years of the disease. Many recent studies proposed<br />
aminosalicylates as chemopreventive agents for colorectal cancer (CRC)<br />
development in IBD.<br />
Objectives: The aim of the present study is to conduct a meta-analysis to<br />
evaluate CRC incidence rate reduction with the use of aminosalicylates<br />
in patients with IBD, and to compare it to CRC incidence in the general<br />
population.<br />
Methods: The PUBMED engine was utilized to search for relevant<br />
literature by use of specific search criteria and experts consult was sought<br />
where appropriate. All papers were scrutinized for 1) total sample size, 2)<br />
defined exposure to aminosalicylates, 3) total number of exposed and unexposed<br />
groups, and 4) CRC outcomes.<br />
Results: Three case-control studies from Europe satisfied our inclusion<br />
criteria, containing 236 cases of CRC and a total of 775 subjects<br />
(performed between the years 1965 and 2001). CRC incidence in patients<br />
not on aminosalicylates therapy was averaged to be 1.89%, while patients<br />
on aminosalicylates therapy had an average incidence of 0.67%. The<br />
European, age-adjusted CRC incidence rate was estimated to be 0.05%.<br />
Conclusion: Collective analysis showed a significant link between<br />
aminosalicylates and CRC incidence rates among IBD patients treated<br />
with aminosalicylates, compared to non-exposed IBD population. Pooled<br />
results of these studies support a three-fold reduction in CRC incidence<br />
in the treated IBD population. This reduction continues to approach a<br />
general population CRC incidence rate.<br />
However, these studies presented pre-immunomodulator therapy data.<br />
Moreover, publications continue to report varying degrees of benefit.<br />
Further studies, particularly in the United States, including prospective<br />
trials and cost-effectiveness analyses, need to be performed to develop<br />
an optimal strategy for the reduction of cancer risk in patients with IBD, as<br />
well as clarifying the synergistic role of immunomodulator therapy with<br />
anti-inflammatory treatment in reducing CRC risk.<br />
12 th World Congress of Endoscopic Surgery 156
Posters of Distinction Abstracts<br />
P021<br />
CONVENTIONAL 4-PORT LAPAROSCOPIC CHOLECYSTECTOMY<br />
VERSUS SILS PORT LAPAROSCOPIC CHOLECYSTECTOMY- EARLY<br />
RESULTS OF THE FIRST PROSPECTIVE RANDOMIZED SHAM<br />
CONTROLLED TRIAL Jeffrey Marks, MD, Raymond Onders, MD, George<br />
DeNoto, MD, Berry Paraskeva, PhD, Homero Rivas, MD, Kurt Roberts, MD,<br />
Alexander Rosemurgy, MD, Sajani Shah, MD, Nathaniel Soper, MD, Roberto<br />
Tacchino, MD University Hospitals Case Medical Center, North Shore<br />
University Hospital, Imperial College of London, UT Southwestern Medical<br />
Center, Yale New Haven Medical Center, Tampa General Hospital, Tufts<br />
Medical Center, Northwestern Memorial Hospital, Catholic U<br />
Introduction: Laparoscopic surgery through a single incision (SILS)<br />
aims to enhance the benefits of conventional minimally invasive surgery<br />
by reducing the number of required surgical incisions. To date, SILS<br />
has been utilized to accomplish cholecystectomy, gastric banding,<br />
Nissen fundoplication, appendectomy, nephrectomy, tubal ligation,<br />
gastric bypass, right colectomy, sleeve gastrectomy, and numerous<br />
other procedures. The initial experience with SILS suggests that it<br />
is technically feasible and safe and may offer select advantages over<br />
standard laparoscopic approaches. This is a preliminary report of an ongoing<br />
multi-institutional study which we believe is the first prospective<br />
randomized sham controlled trial, aimed at objectively analyzing the<br />
safety and efficacy of SILS Cholecystectomy.<br />
Methods: The study is designed to randomize 200 patients in a 3:2 SILS<br />
cholecystectomy vs conventional 4 port laparoscopic cholecystectomy<br />
(“4PLC”) ratio at 9 centers. All patients, regardless of randomized<br />
procedure, receive 4 bandages at conventional locations to achieve a<br />
sham design. Patients are blinded until the bandages are removed after<br />
completion of the 1 week pain evaluation. Patients are contacted by<br />
phone on days 1,3, and 5. Patients are seen in follow up at 1,2, 4, 12, and<br />
52 weeks post-operatively. Pain intensity numerical rating scale(PI-NRS),<br />
SF-8, and body image scoring are performed at each followup. In addition,<br />
analgesic usage, surgical complications, hernia development, and<br />
wound complications are recorded. Primary endpoints include feasibility,<br />
operative time, and EBL. Secondary endpoints include pain, cosmesis,<br />
and quality of life.<br />
Preliminary Results: Between April 2009 and September 2009 twenty<br />
five (25) patients, 15 SILS and 10 4PLC, have been enrolled and have<br />
completed their 1 month follow-up visit. No significant adverse events<br />
have occurred. One SILS case was converted to a 4PLC secondary<br />
to adhesions. The mean operative time (54.9 minutes for SILS vs. 51.5<br />
minutes for 4PLC) and mean intra-operative blood loss (16.2 ml vs.<br />
13.8 ml) have trended similar between groups. The postoperative Pain<br />
Intensity Numerical scores at various time points are trending similar<br />
between groups at all time points. Cosmesis was evaluated utilizing three<br />
questionnaires at 1 month follow-up. Patient derived body image data<br />
indicates a positive trend for SILS versus 4PLC. 68% of the total patient<br />
population would have SILS if they had to have the procedure again.<br />
Conclusion: In this prospective randomized sham controlled trial, early<br />
results are trending towards showing that SILS is a safe and effective<br />
procedure with select cosmetic advantages over conventional 4-port<br />
laparoscopic cholecystectomy. It is understood that the these are early<br />
results of a small patient population. On-going enrollment and follow-up<br />
will permit a more robust scientific analysis.<br />
P022<br />
COLON RESECTIONS IN AN ERA OF NONAGENARIANS: NSQIP<br />
PREDICTORS OF MORTALITY Dan Ruiz, MD, Alexander Kraev, MD,<br />
Darshak Shah, MD, Allapagan W Annamalai, MD, James W Turner, MD,<br />
Howard Tiszenkel, MD New York Hospital Queens<br />
BACKGROUND: Nonagenarians are a growing population often viewed<br />
as high-risk surgical candidates. This study aims to review mortality and<br />
predictors of adverse outcome in nonagenarians undergoing colon<br />
resection.The National Surgical Quality Improvement Project (NSQIP)<br />
database was used for the analysis.<br />
METHODS: The 2005-2008 NSQIP databases were reviewed for all<br />
patients over ninety years old who underwent colon resection. Logistic<br />
regression and then multi-iteration logistic regression analysis was used<br />
to identify univariate and multivariate predictors of mortality.<br />
RESULTS: The study evaluated 766 patients over ninety years old who<br />
underwent colon resection between years of 2005 and 2008. Overall<br />
mortality was 11.6%. Significant univariate predictors of mortality<br />
were: dyspnea at rest (p-value 0.014), having DNR order (p-value .005),<br />
history of angina (p-value 0.032), history of peripheral vascular disease<br />
(p-value .006), impaired sensorium (p-value .018), sepsis (p-value .008),<br />
septic shock (p-value .032), SIRS (p-value .022), and BUN (p-value .027).<br />
Risk adjusted multivariable predictors of mortality were dyspnea at rest<br />
(p-value .0205), having DNR order (p-value of .0091), history of peripheral<br />
vascular disease (p-value .0317), sepsis (p-value
12 th World Congress of Endoscopic Surgery<br />
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P023 LAPAROSCOPIC ROUX-EN-Y GASTRIC BYPASS WITH PRIMARY<br />
REPAIR FOR SYMPTOMATIC GIANT PARAESOPHAGEAL HERNIA IN<br />
MORBID OBESITY: KILLING TWO BIRDS WITH ONE STONE George<br />
Kasotakis, MD, Ranjan Sudan, MD, Sumeet Mittal, MD, Creighton<br />
University Medical Center, Omaha, NE; Duke Health Center, Durham, NC<br />
P024 WANDERING SPLEEN AFTER ROUX-EN-Y GASTRIC BYPASS Ziad y<br />
Fayad, MD, Ryan Hashem, Piotr Gorecki, MD, New York Methodist Hospital<br />
P025 LAPAROSCOPIC APPROACH TO REVISIONAL BARIATRIC<br />
SURGERY David M Lauter, MD, Troy P Houseworth, MD, Karen Baumann,<br />
RN, Institute for Laparoscopic Surgery, Overlake Hospital Medical Center<br />
P026 COMPUTED TOMOGRAPHY GUIDED PERCUTANEOUS<br />
GASTROSTOMY FOR MANAGEMENT OF ACUTE GASTRIC REMNANT<br />
LEAK FOLLOWING ROUX EN Y GASTRIC BYPASS Shahzeer Karmali,<br />
MD FRCSC, Daniel W Birch, MD FRCSC FACS, Vadim Sherman, MD FRCSC<br />
FACS, University of Alberta, Baylor College of Medicine<br />
P027 LAPAROSCOPIC GASTRIC BYPASS IN 1,692 PATIENTS.<br />
Constantine T Frantzides, MD PhD FACS, Atul Madan, MD, George<br />
Ayiomamitis, MD, Jennifer R Glover, MD, John Zografakis, MD FACS,<br />
Chicago Institute of Minimally Invasive Surgery<br />
P028 NINE STEPS TO FOLLOW FOR SAFE AND STANDARD APPROACH<br />
FOR LAPROSCOPIC PARAESOPHAGEAL HERNIA REPAIR. Ismael<br />
Court, Omar Bellorin, Samuel Szomstein, Raul Rosenthal, Cleveland<br />
Clinic Florida<br />
P029 IS THERE AN OPTIMAL GASTRIC BAND STOMA SIZE? John O’Dea,<br />
BE MED PhD CEng FIEI, Robert G Snow, FACOS, Crospon, Galway, Ireland;<br />
Specialty Surgery Center of Fort Worth, TX<br />
P030 ANCHORLESS, SUTURELESS PLACEMENT OF ADJUSTABLE<br />
GASTRIC BAND PORT FOR CONSISTENT, RELIABLE EASY PER-<br />
CUTANEOUS ACCESS. Philippe J Quilici, MD FACS, Alexander Tovar, MD,<br />
Carie McVay, MD, Providence St. Joseph Medical Center, Burbank. Cedars<br />
Sinai Medical Center, Los Angeles<br />
P031 SCLEROTHERAPY TREATMENT FOR WEIGHT GAIN WITH DILATED<br />
GASTRO-JEJUNOSTOMY FOLLOWING ROUX EN Y GASTRIC BYPASS:<br />
HOW MANY TREATMENTS? Mario P Morales, MD, J Stephen Scott, MD,<br />
Roger A de la Torre, MD, SSM DePaul Weight Loss Institute<br />
P032 IMPROVEMENTS IN OBESITY-RELATED CO-MORBIDITIES<br />
FOLLOWING BARIATRIC PROCEDURES IN CHINESE POPULATION<br />
Dennis Wong, FRACS, Kenneth Chau, MBBS, Cliff Chung, FRCS, Michael<br />
Li, FRCS, PAMELA YOUDE NETHERSOLE EASTERN HOSPITAL<br />
P033 GASTRIC POUCH DILATION VERSUS SLIPPED BAND: AN<br />
IMPORTANT DISTINCTION Daniel W Birch, MSc MD, Farzan Ali, MD,<br />
Shahzeer Karmali, MD, CAMIS, Royal Alexandra Hospital, University of<br />
Alberta<br />
P034 BARIATRIC SURGERY SIGNIFICANTLY IMPROVES BODY<br />
PROPORTION James B Wooldridge, MD, Khoi Du, MD, Laura Periou, RD,<br />
William S Richardson, MD, Ochsner Medical Center<br />
P035 COULD EARLY STRICTURE AFTER LAPAROSCOPIC GASTRIC<br />
BYPASS BE A RESULT OF SURGICAL TECHNIQUE, ANALYSIS OF 1760<br />
PATIENTS? I Hamdallah, MD, C David, MD, M Singh, MD, A Averbach,<br />
MD, K Singh, MD, Saint Agnes Hospital<br />
P036 MICROLAPAROSCOPIC GASTRIC BYPASS IS AS SAFE A<br />
TRADITIONAL LAPAROSCOPIC GASTRIC BYPASS Keith A Zuccala,<br />
MD, Laura H Choi, MD, Pierre F Saldinger, MD, Department of surgery,<br />
Danbury Hospital, Danbury, CT 06810<br />
P037 THE USE OF ONDANSETRON (ZOFRAN®) TO RELIEVE<br />
POSTOPERATIVE NAUSEA AND VOMITING AFTER INTRAGASTRIC<br />
BALLOON PLACEMENT: A RANDOMIZED CONTROLLED TRIAL Simon<br />
K.H. Wong, Dr, Wilfred LM Mui, Dr, Enders KW Ng, Dr, Prince of Wales<br />
Hosiptal, The Chinese University of Hong Kong<br />
P038 LAPAROSCOPIC SLEEVE GASTRECTOMY IN TYPE II DIABETIC<br />
PATIENTS; PROMISING EARLY RESULTS S N Wiebe, MD, D Klassen, MD,<br />
J Bonjer, MD, D Lawlor, RN, J Plowman, BSc, T Ransom, MD, M Vallis, PhD,<br />
J Ellsmere, MD, Departments of General Surgery and Medicine, Queen<br />
Elizabeth II Health Sciences Centre, Halifax, Nova Scotia, Canada<br />
P039 RESULTS OF LAPAROSCOPIC SLEEVE GASTRECTOMY Shahram<br />
Nazari, Dr, Semira Mousavi Khosroshahi, Dr, Hosain Khedmat, Dr, Erfan<br />
Hospital, Department of General and Laparoscopic surgery<br />
P040 LAPAROSCOPIC ROUX-EN- Y GASTRIC BYPASS(LRYGB) AND<br />
ADJUSTABLE GASTRIC BANDING(LAGB) FOR MORBIDLY OBESE<br />
PATIENTS IN KOREA : A SERIES OF 204 CASES Hong Lee, MD, Ho Youn,<br />
MD, Jun Lee, Eung Kim, MD, St. Mary’s Hospital, The Catholic University<br />
of Korea<br />
P041 IS THE SUB-LINGUAL ANALGESIC ROUTE OVERLOOKED IN THE<br />
POST-OPERATIVE BARIATRIC PATIENT Susannah M Wyles, MBBS MSc<br />
MRCS, M Harry Thompson, MBBS, Catherine Bradshaw, MBBS, Ahmed<br />
R Ahmed, BSc FRCS, Jonathan Cousins, BSc FRCA, Imperial College<br />
Healthcare London<br />
P042 BODY COMPOSITION: EARLY CHANGES AFTER WEIGHT LOSS<br />
INDUCED BY LAPAROSCOPIC GASTRIC BYPASS. R H Clements, MD,<br />
N Saraf, MPH, M Kakade, MPH, M White, RN, J Hackett, RN, Division<br />
of Gastrointestinal Surgery, University of Alabama at Birmingham,<br />
Birmingham, AL<br />
P043 SAGB TUBE INFECTION MIMICING ACUTE APPENDICITIS AFTER<br />
TUBE DECONECTION DUE TO INJECTION PORTE INFECTION – A CASE<br />
REPORT Toni Kolak, MD PhD, Josip Bakovic, MD, Igor Stipancic, MD PhD,<br />
Marijan Kolovrat, MD, Antonela Radic, MD, University hospital Dubrava;<br />
Department of colorectal surgery<br />
P044 A PROPOSED CLASSIFICATION SYSTEM FOR GASTRIC POUCH<br />
ENLARGEMENT ASSOCIATED WITH LAPAROSCOPICALLY PLACED<br />
ADJUSTABLE GASTRIC BANDS Bradley F Schwack, MD, Jeffrey q Allen,<br />
MD, Norton Healthcare<br />
P045 INTEGRATED BIOABSORBABLE TISSUE REINFORCEMENT IN<br />
LAPAROSCOPIC SLEEVE GASTRECTOMY Joshua B Alley, MD, Richard<br />
M Peterson, MD MPH, Michael Harnisch, MD, Stephen J Fenton, MD, San<br />
Antonio Military Medical Center, Lackland AFB / Fort Sam Houston, TX<br />
P046 LAPAROSCOPIC ROUX-EN-Y GASTRIC BYPASS USING 3 PORTS<br />
TECHNIQUE FOR TREATMENT OF MORBID OBESITY Haider A Al-<br />
Shurafa, MD, Abdullah Al-Masood, MD, Ali S Al-Mutairi, MD, Riyadh<br />
Military Hospiatl<br />
P047 TECHNIQUES FOR CLOSURE OF COMMON ENTEROTOMY OF<br />
THE JEJUNOJEJUNOSTOMY DURING GASTRIC BYPASS DETERMINES<br />
DEGREE OF ALIMENTARY LIMB NARROWING. Meena Theva, BS,<br />
Donald T Hess, MD, Brian Carmine, MD, Miguel Burch, MD, Boston<br />
University School of Medicine<br />
P048 COMPARISON OF STAPLE-LINE LEAKAGE AND HEMORRHAGE<br />
IN PATIENTS UNDERGOING LAPAROSCOPIC SLEEVE GASTRECTOMY<br />
WITH OR WITHOUT THE USE OF BIOABSORBABLE SEAMGUARD ®<br />
Todd E Simon, DO, Joshua A Scott, MD, Joel R Brockmeyer, MD, Farah A<br />
Husain, MD, Jim D Frizzi, MD, Yong U Choi, MD, Department of General<br />
Surgery, D.D. Eisenhower Army Medical Center, Ft. Gordon, GA<br />
P049 CO-MORBIDITIES RECUR WITH WEIGHT REGAIN AFTER INITIAL<br />
RESOLUTION POST-GASTRIC BYPASS Mohammed R Salabat, MD,<br />
Woody Denham, MD, Steven Haggerty, MD, Michael B Ujiki, NorthShore<br />
University Health System<br />
P050 OUTCOME ANALYSIS OF 100 PATIENTS UNDERGOING SINGLE-<br />
INCISION LAPAROSCOPIC ADJUSTABLE GASTRIC BANDING Gary S<br />
Schwartz, MD, Scott B Gmora, MD, Kevin McGill, MD, Deva Boone, MD,<br />
Justin D Blasberg, MD, Steven J Binenbaum, MD, Glenn J Forrester, MD,<br />
Scott J Belsley, MD, Julio A Teixeira, MD, St. Luke’s-Roosevelt Hospital<br />
Center, Columbia University College of Physicians and Surgeons<br />
P051 THE METABOLIC IMPACT OF BARIATRIC SURGERY: LESSONS<br />
LEARNED Gary S Schwartz, MD, Scott B Gmora, MD, Kevin McGill,<br />
MD, James J McGinty, MD, Scott J Belsley, MD, Laferrere B, MD, Julio A<br />
Teixeira, MD, St. Luke’s-Roosevelt Hospital Center, Columbia University<br />
College of Physicians and Surgeons<br />
P052 THE UTILITY OF LAPAROSCOPIC TRANSGASTRIC ACCESS IN THE<br />
ASSESSMENT AND TREATMENT OF THE GASTRIC BYPASS PATIENT<br />
Ursula D McMillian, MD, Keith Zuccala, MD, Danbury Hospital<br />
12 th World Congress of Endoscopic Surgery 158
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P053 IS EXTENDED POST-OPERATIVE MONITORING NECESSARY FOR<br />
MORBIDLY OBESE PATIENTS WITH OBSTRUCTIVE SLEEP APNEA<br />
UNDERGOING BARIATRIC SURGERY? Racquel S Bueno, MD FACS, Chan<br />
Park, MD, Edward Lam, Kenric Murayama, MD FACS, Cedric Lorenzo, MD,<br />
University of Hawaii, Queen’s Medical Center<br />
P054 PROGRESSIVE RESISTANCE TRAINING TO IMPROVE STRENGTH,<br />
FITNESS AND METABOLIC HEALTH IN WEIGHT LOSS SURGERY<br />
PATIENTS Jamie D Adair, MD, Samuel B Wollner, BA, Daniel B Jones, MD,<br />
Renee Miciek, MS, Benjamin Schneider, MD, George L Blackburn, MD<br />
PhD, Beth Israel Deaconess Hospital, Harvard Medical School<br />
P055 LAPAROSCOPIC SLEEVE GASTRECTOMY (SG) IMPROVES<br />
INSULIN SECRETION AND SENSITIVITY IN TYPE 2 DIABETIC OBESE<br />
PATIENTS Frida Leonetti, Danila Capoccia, Federica Coccia, Cristina<br />
Maglio, Francesca Abbatini, Paola Mariani, Nicola Basso, Policlinico<br />
“Umberto I”, University “Sapienza”<br />
P056 LAPAROSCOPIC PLICATION OF A GASTROJEJUNOSTOMY WITH<br />
ENDOSCOPIC GUIDANCE IN THE PORCINE MODEL Connie J Rossini,<br />
MD, Viriato M Fiallo, MD, Burritt L Haag, MD, Department of Surgery,<br />
Baystate Medical Center / Tufts University School of Medicine<br />
P057 DOES GENDER AFFECT EXCESS WEIGHT LOSS AFTER WEIGHT<br />
LOSS SURGERY? Maher El Chaar, MD, TImothy Kuwada, MD, Dimitrios<br />
Stefanidis, MD PhD, Keith Gersin, MD, Carolinas Medical Center<br />
P058 SILS PORT BARIATRIC SURGERY Ali Fardoun, MD, Fawaz Torab, Phd<br />
Associate Professor, Tawam Hospital<br />
P059 SILS, DILS AND THRILLS: AN EVALUATION OF SINGLE INCISION<br />
SURGERY IN LAPAROSCOPIC GASTRIC BANDING. P Ayoung-Chee,<br />
MD, H Hoang, MD, F Colonna, RN, C Magallanes, RN, G Rosario, RNP, A<br />
Finger, RPA, C Ren-Fielding, MD, G Fielding, MD, M Kurian, MD, NYU<br />
P060 DIAPHRAGMATIC HERNIATION OF GASTRIC REMNANT: RARE<br />
COMPLICATION Mohamed I Dahman, MD, Peter T Hallowell, MD,<br />
Bruce D Schirmer, MD, Department of Surgery, University of Virginia,<br />
Charlottesville, VA, USA<br />
P061 T2DM AND SLEEVE GASTRECTOMY : DIABETES DURATION AS<br />
PROGNOSTIC FACTOR OF CURE Giovanni Casella, Giorgio Alessandri,<br />
Francesca Abbatini, Mario Rizzello, Emanuele Soricelli, Danila Capoccia,<br />
Nicola Basso, Policlinico “Umberto I”, Università “Sapienza”<br />
P062 UNBUCKLING: A NEW TWO-STAGED APPROACH TO<br />
SYMPTOMATIC SLIPPAGE OF LAPAROSCOPIC ADJUSTABLE GASTRIC<br />
BANDS (LAGB) Eric A Sommer, MD, Amit Trivedi, MD, Douglas Ewing,<br />
MD, Garth Ballantyne, MD, Hans Schmidt, MD, Hackensack University<br />
Medical Center<br />
P063 LAPAROSCOPIC SLEEVE GASTRECTOMY (LSG) IN MORBIDLY<br />
OBESE – AN EARLY ASSESSMENT OF SAFETY AND EFFICACY Manish<br />
Singh, MD, Riny Karras, MD, Javeed Khan, MD, Kuldeep Singh, FACS,<br />
Andrew Averbach, FACS, Steve C David, MD, Saint Agnes Hospital ,<br />
Baltimore, MD<br />
P064 ROUTINE DRAIN PLACEMENT IN ROUX-EN-Y GASTRIC BYPASS:<br />
AN EXPANDED RETROSPECTIVE COMPARATIVE STUDY OF 755<br />
PATIENTS. Srinivas Kavuturu, MD, Daniel C Williams, MD, Randy s<br />
Haluck, MD, Timothy R Shope, MD, Ann M Rogers, MD, Penn State Milton<br />
S Hershey Medical Center<br />
P065 BARIATRIC SURGERY OUTCOMES FOR PATIENTS UNDERGOING<br />
PREOPERATIVE IVC FILTER PLACEMENT Tejwant S Datta, MD,<br />
Kimberley Steele, MD, Andrew D Shore, PhD, Thomas Magnuson, MD,<br />
Anne O Lidor, MD, Hien Nguyen, MD, Martin Makary, MD, Michael<br />
Schweitzer, MD, Johns Hopkins University School of Medicine<br />
P066 SUTURE LINE LEAKS AFTER LAPAROSCOPIC SLEEVE<br />
GASTRECTOMY : DIFFICULTIES OF MANAGEMENT MIGHT BE<br />
UNDERESTIMATED. Manish Singh, MD, Javeed Khan, MD, Nicholas c<br />
Tapazoglou, MD, Kuldeep Singh, FACS, Andrew Averbach, FACS, Steve c<br />
David, MD, Saint Agnes Hospital , Baltimore, MD<br />
P067 IS LAPAROSCOPIC SLEEVE GASTRECTOMY MORE SAFE AND<br />
EFFICACIOUS THAN LAPAROSCOPIC GASTRIC BANDING ? : A<br />
SHORT TERM REVIEW Manish Singh, MD, Nicholas s Tapazoglou, MD,<br />
Javeed Khan, MD, Steve c David, MD, Kuldeep Singh, FACS, Andrew<br />
Averbach, FACS, Saint Agnes Hospital , Baltimore, MD<br />
P068 REVIEW OF RYGB VERSUS FUNDOPLICATION FOR GERD IN<br />
OBESE PATIENTS M Cavaretta, MD, K Chinnappan, MD, J Gabrielsen,<br />
title, A Petrick, MD, Geisinger Medical Center<br />
P069 A NOVEL APPROACH TO FAILED VERTICAL BANDED<br />
GASTROPLASTY: LAPAROSCOPIC CONVERSION TO SLEEVE<br />
GASTRECTOMY John A Primomo, MD, Candace Y Williams-Covington,<br />
MD, Shazeer Karmali, MD, Vadim Sherman, MD, Baylor College of<br />
Medicine<br />
P070 GEOGRAPHICAL VARIATION IN INPATIENT MORTALITY AND<br />
LENGTH OF STAY AFTER LAPAROSCOPIC GASTRIC BYPASS Jennifer<br />
E Foster, MD, Sharon E Phillips, MSPH, D. Brandon Williams, MD, Michael<br />
D Holzman, MD MPH, Willie V Melvin, MD, Kristy L Kummerow, BS,<br />
Julia Shelton, MD, Benjamin K Poulose, MD MPH, Vanderbilt University<br />
Medical Center<br />
P071 FORCED GASTRIC WALL EROSION AND STAGED REMOVAL OF<br />
NONADJUSTABLE GASTRIC BANDS – A CASE SERIES Kanayochukwu<br />
J Aluka, MD, Todd D Wilson, MD, Brad E Snyder, MD, Sherman Yu, MD,<br />
Erik B Wilson, MD, University of Texas Health Science Center Houston,<br />
Houston, Texas<br />
P072 FEASIBILITY OF SIMULTANEOUS HIATAL HERNIA (HH) REPAIR<br />
AND LAPAROSCOPIC ADJUSTABLE GASTRIC BANDING (LAGB):<br />
CASE-IN-POINT PRESENTATION FOR PREVENTION OF DELAYED<br />
COMPLICATIONS. Gustavo Franco, MD, Murad Bani Hani, MD, Andrew<br />
Averbach, MD FACS, Saint Agnes Hospital. Baltimore, MD. USA.<br />
P073 DOES THE PATIENT CHOICE OF THE TYPE WEIGHT LOSS<br />
SURGERY AFFECT THE AMOUNT OF WEIGHT LOSS ACHIEVED<br />
PREOPERATIVELY ? Maher El Chaar, MD, Dimitrios Stefanidis, MD PhD,<br />
Keith Gersin, MD, Gray Hughes, MD, Timothy Kuwada, MD, Carolinas<br />
Medical Center, Division of Minimally Invasive Surgery and Bariatrics<br />
P074 CREATION OF A UNIVERSAL HEALTH SCORE Todd A Worley, MD,<br />
Brad E Snyder, MD, Kanayochukwu J Aluka, MD, Todd D Wilson, MD, Erik<br />
B Wilson, MD, University of Texas Health Science Center at Houston<br />
P075 DOES GASTRIC BYPASS RESOLVE CARDIAC COMORBIDITIES<br />
EQUALLY FOR THE OBESE VS SUPER OBESE? Eric Changchieng, MD,<br />
Gavitt A Woodard, BS, Sarah Miri, MD, Tina H Boussard, PhD, John M<br />
Morton, MD MPH, Stanford University<br />
P076 A SMALL POUCH LAPAROSCOPIC ADJUSTABLE GASTRIC<br />
BAND (HIGH BAND) IS ASSOCIATED WITH A LOWER INCIDENCE OF<br />
COMPLICATIONS. MIDTERM ANALYSIS OF 132 PATIENTS. Niazy M<br />
Selim, MD MBChB PhD FACS, Iris Dupanovic, University of Kansas<br />
P077 THE IMPACT OF PREVIOUS FUNDOPLICATION ON<br />
LAPAROSCOPIC GASTRIC BYPASS OUTCOMES Anna Ibele, MD,<br />
Michael Garren, MD, Jon Gould, MD, University of Wisconsin School of<br />
Medicine and Public Health, Department of Surgery<br />
P078 SINGLE PORT ACCESS FOR LAPAROSCOPIC ADJUSTABLE<br />
GASTRIC BANDING WITH REGULAR LAPAROSCOPIC INSTRUMENTS<br />
IS FEASIBLE AND ECONOMIC. Niazy M Selim, MD MBChB PhD FACS,<br />
University of Kansas<br />
P079 A COMBINED LAPRASCOPIC AND ENDOSCOPIC TECHNIQUE TO<br />
EVALUATE GASTRIC REMNANT AFTER GASTRIC BYPASS Neeraj Singh,<br />
MD, Artun Aksade, MD FACS, Easton Hospital, EAston,PA-18042<br />
P080 THE ASSOCIATION BETWEEN GERD AND LAPAROSCOPIC SLEEVE<br />
GASTRECTOMY Patrice R Carter, MD, Karl A LeBlanc, MD FACS, Mark<br />
G Hausmann, MD FACS, Kenneth P Kleinpeter, MD, Minimally Invasive<br />
Surgery Institute - The Surgeon’s Group of Baton Rouge<br />
P081 PATIENT PERCEPTIONS OF BAND ADJUSTMENTS AFTER<br />
LAPAROSCOPIC ADJUSTABLE GASTRIC BANDING Atul K Madan,<br />
MD, David S Tichansky, MD, Beverly Hills Surgery Center and Thomas<br />
Jefferson University<br />
12 th World Congress of Endoscopic Surgery<br />
159 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P082 LAPAROSCOPIC CHOLECYSTECTOMY ASSOCIATED WITH<br />
GASTRIC BYPASS SURGERY: A SAFE APPROACH FOR MORBID<br />
OBESITY PATIENTS? Carlos Alberto Lopera Ramírez, Jesús Vásquez<br />
Arango, Jean Pierre Vergnaud Córdoba, Sergio Díaz Rodríguez, Carmelo<br />
Díaz Pájaro, Universidad de Antioquia<br />
P083 GANGLIONEUROMA OF THE ADRENAL GLAND AND<br />
RETROPERITONEUM. A REPORT OF UNUSUAL CASE AND REVIEW<br />
OF THE LITERATURE Iswanto Sucandy, MD, Yasir M Akmal, MD, Joseph<br />
A Blansfield, MD, David G Sheldon, MD, William E Strodel, Geisinger<br />
Health System<br />
P084 THERMAL TISSUE FUSION: INTERACTION OF CONTROL<br />
PARAMETERS AND TISSUE EFFECTS Deogracias A Reyes, MD MMAS,<br />
Luisa Motta, MD, Lynda Cochrane, PhD, Chengli I Song, PhD, Stuart I<br />
Brown, PhD, Alfred Cuschieri, Prof, University of Dundee<br />
P085 THORACOSCOPIC SYMPATHETIC NERVE BLOCKING UNDER<br />
LOCAL ANESTHESIA WITH MAC: 114 CASES REPORT Shaohong Guo,<br />
MD, Jingjing Wang, Department of General Surgery,BenQHospital,<br />
Nanjing Medical University<br />
P086 CHOLECYSTECTOMY BY MICROLAPAROTOMY-AS THE<br />
PRECURSOR OF SINGLE INCISION LAPAROSCOPIC SURGERY-<br />
COMPARING TO STANDARD LAPAROSCOPIC CHOLECYSTECTOMY<br />
(IN HONOUR OF TWO HUNGARIAN SURGEONS) Istvan Gal, MD PhD,<br />
Zoltan Szabo, PhD, Miklos Czobel, MD, Gyorgy Weber, MD PhD, Telki<br />
International Private Hospital, Budapest-Telki,Hungary, M.O.E.T. Institute<br />
San Francisco, CA, USA, University of Szeged,Faculty of Medicine,<br />
Department of Surgery, Department of Surgical Research and Technique<br />
University Medical School of Pécs<br />
P087 CREATION OF A SLEEVE GASTRECTOMY MOUSE MODEL: A NEW<br />
TOOL IN THE EVALUATION OF THE BETA CELL PROLIFERATION AND<br />
GLUCOSE TOLERANCE EFFECTS OF BARIATRIC SURGERY Avraham<br />
Schlager, MD, Abed Khalaileh, MD, Seth Salpeter, Yuval Dor, PhD, Gideon<br />
Zamir, MD, New York University Medical Center, Hadassah-Hebrew<br />
University Medical Center<br />
P088 HUMAN VITAL AMNIOTIC MEMBRANE REDUCES ADHESIONS TO<br />
A POLYPROPYLENE MESH AND SUTURE FIXATION IN EXPERIMENTAL<br />
IPOM REPAIR IN RATS Alexander H Petter-Puchner, MD, René H<br />
Fortelny, MD, Simone Gruber-Blum, MD, Kathrin Mika, MD, Simone<br />
Hennerbichler, PhD, Heinz Redl, Prof, Ludwig Boltzmann Institute for<br />
Experimental and Clinical Traumatology, Vienna, Austria<br />
P089 ANALYSIS OF TISSUE DAMAGE CAUSED BY ULTRASONICALLY<br />
ACTIVATED DEVICE FOR LAPAROSCOPIC SURGERIES Hideki Hayashi,<br />
MD, Naomi Hioki, BA, Masaru Oya, MA, Tadashi Yamaguchi, PhD,<br />
Hiroyuki Hachiya, MD PhD, Toshiyuki Natsume, MD, Hiroshi Kawahira,<br />
MD, Hisahiro Matsubara, MD, Research Center for Frontier Medical<br />
Engineering, Chiba University, Chiba, Japan.<br />
P090 EMERGENCY SURGERY FOR COLONIC DIVERTICULITIS:<br />
DIFFERENCES BETWEEN RIGHT-SIDED AND LEFT-SIDED DISEASE IN<br />
AN ASIAN POPULATION Ker-Kan Tan, Jody Z Liu, Richard Sim, Tan Tock<br />
Seng Hospital, Singapore<br />
P091 INCISIONLESS LAPAROSCOPIC SURGERY FOR COLORECTAL<br />
CANCER ~HYBRID NOTES TECHNIQUE APPLIED TO TRADITIONAL<br />
LAPAROSCOPIC COLORECTAL RESECTION~ Goutaro Katsuno, MD<br />
PhD, Masaki Fukunaga, MD PhD, Hidenori Tsumura, MD PhD, Kunihiko<br />
Nagakari, MD PhD, Masahiko Sugano, MD PhD, Yoshifumi Lee, MD PhD,<br />
Shuichi Sakamoto, MD PhD, Masaru Suda, MD PhD, Yoshito Iida, MD<br />
PhD, Seiichiro Yoshikawa, MD PhD, Department of Surgery Juntendo<br />
Urayasu Hospital/Juntendo University<br />
P092 POST COLONOSCOPY COLONIC INTUSSUSCEPTION REDUCED<br />
VIA A LAPAROSCOPIC APPROACH: A CASE REPORT Mindy M Ho, MD,<br />
John J Park, MD, Leela M Prasad, MD, Metropolitan Group Hospitals<br />
General Surgery Residency, Lutheran General Hospital<br />
P093 LAPAROSCOPIC-ASSISTED RECTAL SURGERY USING THE SIMPLE<br />
RECTUM CATCHER DEVICE Akiyo Matsumoto, Kaida Arita, Masaki<br />
Tashiro, Hidenori Takahashi, Masaru Sugimoto, Junichi Kuramochi,<br />
Shinsuke Usui, Koji Ito, Noriaki Takiguchi, Susumu Hiranuma, Katsuhiro<br />
Sanada, Department of Surgery, Tsuchiura Kyodo General Hospital<br />
P094 LESS INVASIVE SURGERY ON THE PATIENTS WITH SEVERE<br />
CONSTIPATION INCLUDIING THE SPLENIC FLEXURE TYPE<br />
Hirotsugu Ohara, Yasuhiko Masuda, Fujieda Heisei Memorial Hospital<br />
P095 WHEN STAPLERS MISFIRE: ENDOSCOPIC RESCUE OF THE LOW<br />
PELVIC ANASTOMOSIS Rebecca A Levine, MD, Omar Kadro, MD, William<br />
Beaumont Hospital<br />
P096 TOTAL LAPAROSCOPIC REPAIR OF FOREIGN BODY<br />
PERFORATION OF JEJUNUM Floyd Herman, MD MSc, Nimitt Patel, MD,<br />
Marco Yung, MD MPH, Derick Christian, MD, St. Francis Medical Center,<br />
Seton Hall University School of Graduate Medical Education<br />
P097 3DCT NAVIGATION FOR SINGLE UMBILICAL INCISION<br />
LAPAROSCOPIC APPENDECTOMY Keiichi Fujino, MD PhD, Minoru<br />
Kakihara, MD PhD, Tamio Yamasaki, MD PhD, Hidekazu Yano, MD,<br />
Tonami Sato, MD, Hironori Tsujimoto, MD PhD, Takemaru Tanimizu, MD<br />
PhD, Nobuo Kugai, MD PhD, Department of General Medicine, National<br />
Defense Medical College Hospital, Japan<br />
P098 DOES THE RATIO OF LYMPH NODE HAS A NOTABLE<br />
PROGNOSTIC FACTOR ON THE SURVIVAL OF PATIENTS WITH STAGE<br />
III COLORECTAL CANCER Sezai Demirbas, MD, Nail Ersöz, MD, Ismail<br />
H Ozerhan, MD, Gokhan Yagci, MD, Mustafa T Ozer, MD, Ali Harlak, MD,<br />
Saadettin Cetiner, Prof Dr, Gulhane Mil. Medical Academy (GMMA)<br />
P099 CIRCULAR STAPLED TRANSANAL RECTAL RESECTION, A<br />
USEFUL TECHNIQUE IN TREATING RECTAL INTUSSUSCEPTION AND<br />
RECTOCELE. OUR EXPERIENCE OF A SINGLE CENTER WITH 23 CASES.<br />
Shahram Nazari, Dr, Semira Mousavi Khosroshahi, Dr, Omid Tahbaz, Dr,<br />
M. Towliat kashani, Dr, Ahmad Fanaie, Dr, Erfan Hospital, Department of<br />
General and Laparoscopic surgery<br />
P100 GASTROINTESTINAL BLEEDING IN HIV PATIENTS (5 YR STUDY)<br />
- A PARADIGM SHIFT IN THE ETIOLOGY Srinivas Kavuturu, MD,<br />
Anterpreet Singh, Daniel Farkas, MD, Vellore Parithivel, MD, John<br />
M Cosgrove, MD, Bronx Lebanon Hospital Center, Bronx, New York<br />
NY10457<br />
P101 SYNCHRONOUS APPENDICITIS AND UMBILICAL HERNIAL<br />
METASTASIS FROM CECAL ADENOCARCINOMA Shankar R Raman,<br />
MD MRCS, V Vattipally, MD, Daniel Farkas, MD FACS, John Cosgrove, MD<br />
FACS, Bronx-Lebanon Hospital Center<br />
P102 MINIMALLY INVASIVE MANAGEMENT OF JEJUNAL<br />
PERFORATION DUE TO ACCIDENTAL INGESTION OF KEBAB STICK IN<br />
INTOXICATED MORBIDLY OBESE PERSON Bala Thatigotla, MD, Vikram<br />
Vattipally, MD, Daniel Farkas, MDFACS, John M Cosgrove, MDFACS, Bronx<br />
Lebanon Hospital Center,Bronx,NY 10457,USA<br />
P103 SINGLE INCISION LAPAROSCOPIC COLECTOMY FOR NEOPLASMS<br />
OF THE COLON Michiya Kobayashi, MD PhD, Ken Dabanaka, MD, Ken<br />
Okamoto, MD PhD, Tsutomu Namikawa, MD PhD, Kazuhiro Hanazaki,<br />
MD PhD, Department of Human Health and Medical Sciences, Hospital<br />
Administration Section, Kochi Medical School<br />
P104 LAPAROSCOPIC COLECTOMY WITH RADICAL LYMPH NODE<br />
DISSECTION FOR TRANSVERSE COLON CANCER Yosuke Fukunaga,<br />
MD, Masao Kameyama, MD, Masayasu Kawasaki, MD, Hiroshi Sonoo,<br />
MD, Masashi Takemura, MD, Yushi Fujiwara, MD, Nagahisa Fjujio, MD,<br />
Masao Ogawa, MD, Koichi Demura, MD, Keiichi Yamazaki, MD, Tsuyoshi<br />
Ichikawa, MD, Tomoyuki Ueki, MD, Atsuo Ima, Bell-land General Hospital<br />
P105 FULL THICKNESS ENDOSCOPIC EXCISION OF A 3 CM<br />
LEIOMYOMA WITH ENDOCLIP REPAIR: A CASE REPORT. Amy L Levin,<br />
MD, Christine M Bouchard, MD, John J Park, MD, Advocate Lutheran<br />
General Hospital, Park Ridge, Illinois<br />
12 th World Congress of Endoscopic Surgery 160
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P106 MANTLE CELL LYMPHOMA OF THE GASTROINTESTINAL TRACT<br />
PRESENTING WITH MULTIPLE INTUSSUSCEPTIONS – CASE REPORT<br />
AND REVIEW OF LITERATURE Venkata K Kella, Radu Constantine, John<br />
M Cosgrove, Department of Surgery and Oncology, Bronx-Lebanon<br />
Hospital Center, Bronx, New York, USA<br />
P107 AN UNUSUAL CASE OF INTUSSUSCEPTION MASQUERADING AS<br />
RECTAL PROLAPSE. Phil V Bach, BSc, Daniel W Birch, MD, University of<br />
Alberta<br />
P108 UPDATED RESULTS OF DOUBLE TA TRANSECTION METHOD<br />
IN THE LAPAROSCOPE-ASSISTED ANTERIOR RESECTION OF THE<br />
RECTUM Fumihiro Uchikoshi, MD PhD, Yuko Yamagami, MD, Takahiko<br />
Tatsumi, MD PhD, Department of Surgery, Tatsumi clinic & Hospital<br />
P109 DOES AN ENLARGED EXTRACTION SITE AFFECT<br />
POSTOPERATIVE OUTCOMES AFTER LAPAROSCOPICALLY<br />
COMPLETED INTESTINAL RESECTION FOR CROHN’S DISEASE?<br />
Matteo Rottoli, MD, Luca Stocchi, MD, Daniel P Geisler, MD, Cleveland<br />
Clinic Foundation<br />
P110 PREOPERATIVE CHEMORADIATION FOLLOWED BY<br />
LAPAROSCOPIC INTERSPHINCTERIC RESECTION FOR LOW RECTAL<br />
CANCER Masanori Nishioka, Mitsuo Shimada, Nobuhiro Kurita,<br />
Takashi Iwata, Shinya Morimoto, Kozo Yoshikawa, Jun Higashijima, The<br />
University of Tokushima<br />
P111 COMPARISON OF SHORT TERM & LONG TERM FUNCTIONAL<br />
OUTCOMES AFTER LAPAROSCOPIC VS OPEN SURGERY FOR<br />
ULCERATIVE COLITIS – RESTORATIVE PROCTOCOLECTOMY ILEAL<br />
POUCH ANAL ANASTOMOSIS Haribhakti S P, MS DNB MCh, Soni H N, M<br />
S, Nagpal A P, MS, Haribhakti Surgical Hospital, Ahmedabad, India<br />
P112 A NEW STRATEGY FOR ADHESIVE BOWEL OBSTRUCTON USING<br />
LAPAROSCOPIC SURGERY AND BIOABSORBABLE MEMBRANE<br />
Hiroyuki Nagayama, MD, Yasuo Ishida, MD, Sumito Satou, MD,<br />
Junichi Ooga, MD, Toshiyuki Hatakeyama, MD, Department of<br />
surgery,Yokohama Asahi Central General Hospital<br />
P113 DGHAL WITH RECTO-ANAL-REPAIR MODIFICATION:<br />
FUNCTIONAL EVALUATION AND SAFETY ASSESSMENT OF A NEW<br />
MINIMALLY-INVASIVE METHOD OF TREATMENT OF ADVANCED<br />
HEMORRHOIDAL DISEASE. Piotr Walega, MD PhD, Michal Romaniszyn,<br />
MD, Jakub Kenig, MD PhD, Piotr Richter, MD PhD, Roman Herman, Prof,<br />
Wojciech Nowak, Prof, 3 rd Department of General Surgery, Jagiellonian<br />
University School of Medicine, Krakow, Poland<br />
P114 DEFINING MEASUREMENTS OF THE ILEOCOLIC AND INFERIOR<br />
MESENTERIC VESSELS BY CONTRAST-ENHANCED CT: IMPLICATIONS<br />
FOR VASCULAR PEDICLE LIGATION DURING COLECTOMY Jennifer D<br />
Rea, MD, Brent J Bose, MD, Nora Dobos, MD, Molly M Cone, MD, Karen<br />
E Deveney, MD, Kim C Lu, MD, Daniel O Herzig, MD, Oregon Health &<br />
Science University<br />
P115 DOES THE PRESENCE OF LAPAROSCOPIC COLORECTAL SURGERY<br />
CAPABILITY REFLECT GREATER PRESENCE OF OTHER HOSPITAL-<br />
LEVEL STRUCTURES OF CARE? Rahima N Nenshi, MD MSc, Binu Jacob,<br />
MSc, Kennedy Erin, MD PhD, Nancy Baxter, MD PhD, Rinku Sutradhar,<br />
PhD, David R Urbach, MD MSc, Department of Surgery, University Health<br />
Network<br />
P116 RISK FACTORS FOR ANASTOMOTIC LEAKAGAE AFTER<br />
LAPAROSCOPIC SURGERY FOR RECTOSIGMOIDAL AND RECTAL<br />
CANCER USING STAPLING TECHNIQUE Shin Fujita, MD, Takayuki<br />
Akasu, MD, Tomoya Funada, MD, Yoshihiro Moriya, MD, Seiichiro<br />
Yamamoto, MD PhD, National Cancer Center Hospital<br />
P117 LAPAROSCOPIC SURGERY IN COLORECTAL CANCERS:<br />
EXPERIENCE WITH 118 PATIENTS AT SINGLE INSTITUTION Shigeoki<br />
Hayashi, MD PhD, Minoru Matsuda, MD FACS, Motoo Yamagata, MD<br />
PhD, Ken Hagiwara, MD, Junko Sugiyama, MD, Tomoaki Takasugi, MD,<br />
Tadatoshi Takayama, MD PhD, Department of Digestive Surgery, Nihon<br />
University School of Medicine, Tokyo, Japan<br />
P118 FULL THICKNESS LAPAROENDOSCOPIC EXCISION (FLEX)<br />
PROCEDURE FOR LESIONS OF THE COLON AND STOMACH- A NOVEL<br />
TECHNIQUE Robin H Kennedy, MD, Ronan A Cahill, MD, Paul D Sibbons,<br />
FIBMS PhD, Chris Fraser, MD, St Marks Hospital, Harrow, UK; Oxford<br />
Radcliffe Hospitals, Oxford, UK, Northwick Park Biomedical Institution,<br />
Harrow UK.<br />
P119 LAPAROSCOPIC ANTERIOR RESECTION FOR RECTAL CANCER; A<br />
PROSPECTIVE FEASIBILITY STUDY Masafumi Inomata, MD, Yoshitake<br />
Ueda, MD, Manabu Togigamori, MD, Tsuyoshi Etoh, MD, Kazuhiro<br />
Yasuda, MD, Tsuyoshi Noguchi, MD, Norio Shiraishi,, MD, Seigo Kitano,<br />
Oita University Faculty of Medicine<br />
P120 LAPAROSCOPIC SURGERY FOR DUKES C COLORECTAL CANCER<br />
Takeshi Naitoh, MD, Atsushi Oyama, MD, Takashi Tsuchiya, MD, Hiroshi<br />
Honda, MD, Masaya Oikawa, MD, Tetsuya Kakita, MD, Department of<br />
Surgery, Sendai City Medical Center<br />
P121 TOTALLY LAPAROSCOPIC RIGHT HEMICOLECTOMY FOR CANCER<br />
Jordan B Lazarevic, MD, Vladimir Stajic, MD, Ivan Popovic, MD, City<br />
Hospital Valjevo<br />
P122 LAPAROSCOPIC HARTMAN’S COLOSTOMY REVERSAL Mohan<br />
Narasimhan, Kumar Palaniappan, Ramesh Ardhanari, Department of<br />
Surgery and Gastroenterology, Meenakshi Mission Hospital & Research<br />
Center, Madurai<br />
P123 STAPLED TRANSANAL RECTAL RESECTION (STARR) FOR<br />
OBSTRUCTIVE DEFECATION SYNDROME – A PROSPECTIVE STUDY<br />
WITH 6 MONTHS FOLLOW UP Brij B Agarwal, MS, Kumar Manish,<br />
MBBS, Rathindra Sarangi, MS, Krishan C Mahajan, FRCS, Dr. Agarwal’s<br />
Surgery & Yoga and Sir Ganga Ram Hospital, New Delhi, India<br />
P124 OUR EXPERIENCE OF TRANS UMBILICAL LAPAROSCOPIC<br />
APPENDECTOMY. Ibrahim Ahmed, FRCSI, Ibraheem Tunau, FRCSI,<br />
Elnazier Ibrahim, FRCSI, Alexander Lockley, MBCh, Thomas McEnery,<br />
Mohamed Salama, FRCSI, Vijaya Selvaraju, Our Lady’s Hospital, Navan,<br />
Ireland<br />
P125 SINGLE INCISION LAPAROSCOPIC COLECTOMY (SILC) FOR<br />
COLON CANCER Jun-ichi Tanaka, MD PhD, Gumpei Yoshimatsu, MD,<br />
Shunpei Mukai, MD, Kuniyasu Horikoshi, MD, Tomokatsu Omoto,<br />
MD, Shungo Endo, MD, Fumio Ishida, MD, Shin-ei Kudo, MD, Showa<br />
University Northern Yokohama Hospital<br />
P126 – Withdrawn.<br />
P127 EFFECT OF PRE-OPERATIVE RECTAL PREPARATION BY<br />
DIFFERENT METHODS ON OPERATIVE AND CLINICAL OUTCOMES<br />
OF STAPLED HEMORRHOIDOPEXY – A RANDOMIZED CONTROLLED<br />
STUDY Brij B Agarwal, MS, Kumar Manish, MBBS, Tapish Sahu, MBBS,<br />
Rathindra Sarangi, MS, Krishan C Mahajan, FRCS, Dr. Agarwal’s Surgery &<br />
Yoga and Sir Ganga Ram Hospital, New Delhi, India<br />
P128 IS MECHANICAL BOWEL PREPARATION NECESSARY FOR<br />
LAPAROSCOPIC COLON SURGERY Alex J Ky, MD, Ray Wong, MD, Erin<br />
Ly, BA, Mt Sinai Hospital<br />
P129 LAPAROSCOPIC SURGERY FOR COLONIC PERFORATION.<br />
ANALYSIS OF THREE CASES. Miguel J Garcia-Oria, MD PhD, Jose A<br />
Gazo, MD, Eduardo San Pio, MD, Jesus Merello, MD, Hospital Sanitas La<br />
Moraleja<br />
P130 SINGLE INCISION LAPAROSCOPIC SURGERY FOR RIGHT<br />
COLON PROCEDURES: A PROSPECTIVE ANALYSIS OF OUR INITIAL<br />
EXPERIENCE Maher El Chaar, MD, Gray Hughes, MD, Timothy Kuwada,<br />
MD, carolinas Medical Center, Division of Minimally Invasive Surgery<br />
P131 LAPAROSCOPIC TOTAL MESORECTAL EXCISION FOR MIDDLE<br />
AND LOW RECTAL ADENOCARCINOMA WITH OR WITHOUT<br />
SPHINCTER PRESERVATION: A PROSPECTIVE STUDY Elie K Chouillard,<br />
MD, Aziz Karaa, MD, Ziad Elrassi, MD, Andrew A Gumbs, Poissy Medical<br />
Center (France), Clinique de l’Yvette (France) and Fox Chase Cancer<br />
Center (USA)<br />
12 th World Congress of Endoscopic Surgery<br />
161 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P132 COMPARISON OF SHORT-TERM AND LONG-TERM OUTCOMES<br />
OF THE COLON-LIFTING METHOD AND STANDARD 5-PORTS<br />
LAPAROSCOPIC COLECTOMY FOR COLORECTAL CANCER: A CASE-<br />
MATCHED CONTROL STUDY Shoichi Fujii, MD PhD, Shigeru Yamagishi,<br />
MD PhD, Mitsuyoshi Ota, MD PhD, Yasushi Ichikawa, MD PhD, Shunichi<br />
Osada, MD PhD, Kazuteru Watanabe, MD PhD, Hirokazu Suwa, MD, Kenji<br />
Tatsumi, MD PhD, Yasuhiko Nagano, MD PhD, Takashi Oshima, MD PhD,<br />
Chikara Kunisaki, Prof, Department of Surgery, Gastroenterological<br />
Center, Yokohama City University<br />
P133 ONCOLOGICAL OUTCOME OF STAGE II/III COLON CANCER<br />
TREATED VIA MINILAPAROTOMY APPROACH Hideyuki Ishida, PhD,<br />
Toru Ishiguro, MD, Tomonori Ohsawa, MD, Norimichi Okada, PhD,<br />
Keiichiro Ishibashi, PhD, Norihiro Haga, PhD, Department of Digestive<br />
Tract and General Surgery, Saitama Medical Center, Saitama Medical<br />
School<br />
P134 PATTERN OF ARTERIAL BRANCHES CROSSING THE SUPERIOR<br />
MESENTERIC VEIN: ITS RELEVANCE TO LAPAROSCOPIC RIGHT<br />
HEMICOLECTOMY Tomonori Ohsawa, MD, Toru Ishiguro, MD, Keiichiro<br />
Ishibashi, PhD, Hideyuki Ishida, phD, Department of Digestive Tract and<br />
General Surgery, Saitama Medical Center, Saitama Medical School<br />
P135 ONE HEM-O-LOK CLIP IS ENOUGH TO SECURE THE BASE OF<br />
APPENDIX DURING LAPAROSCOPIC APPENDECTOMY. Samir<br />
Delibegovic, Ass Prof PhD, Department of surgery, University Clinci<br />
Center Tuzla<br />
P136 PELVIC PERITONIZATION AFTER LAPAROSCOPIC<br />
ABDOMINOPERINEAL RESECTION FOR LOW-RECTAL CARCINOMA<br />
Nikica Druzijanic, MD PhD, Zdravko Perko, MD PhD, Zenon Pogorelic, MD<br />
PhD, Damir Kraljevic, MD, Josko Juricic, MD, Kanito Bilan, MD, Dragan<br />
Krnic, MD, Department of surgery, University Hospital Split, Spinciceva 1,<br />
21000 Split, Croatia<br />
P137 SHORT-TERM RESULTS OF LAPAROSCOPIC INTERSPHINCTERIC<br />
RESECTION FOR VERY LOW RECTAL CANCER Masaaki Ito, MD, Yusuke<br />
Nishizawa, MD, Akihiro Kobayashi, Masanori Sugito, MD, Norio Saito,<br />
MD, Ntional Cancer Center Hospital East<br />
P138 EMERGENCY LAPAROSCOPIC COLORECTAL SURGERY— IS THE<br />
PAIN WORTH THE GAIN? Jim Khan, FRCS, Karim Muhammad, FRCS, Anil<br />
Hemandas, FRCS, Emma McGlone, Karen Flashman, BSc, Amjad Parvaiz,<br />
FRCS, Queen ALexandra Hospital, Portsmouth, UK<br />
P139 PROSPECTIVE COMPARISON OF SHORT-TERM OUTCOMES<br />
FOLLOWING LAPAROSCOPIC AND OPEN TOTAL MESORECTAL<br />
EXCISION FOR RECTAL CANCER Anil Hemandas, FRCS, Karim<br />
Muhammad, FRCS, Karen Flashman, BSc, Jim Khan, FRCS, Asha Senapati,<br />
FRCS, Daniel O’Leary, FRCS, Amjad Parvaiz, FRCS, Queen Alexandra<br />
Hospital, Portsmouth, UK.<br />
P140 EXPERIENCE OF SINGLE-INCISION LAPAROSCOPIC RECTAL<br />
ANTERIOR RESECTION Nobuhiro Ito, MD PhD, Hiroshi Nagata, MD<br />
PhD, Noiku Nakao, MD PhD, Hitoshi Inagaki, MD PhD, Toshiaki Nonami,<br />
MD PhD, Department of Gastroenterological Surgery, Aichi Medical<br />
University<br />
P141 OBESITY IS ASSOCIATED WITH INADEQUATE LYMPH NODE<br />
HARVEST IN LAPAROSCOPIC RIGHT HEMICOLECTOMY Matthew L<br />
Silviera, MD, Brian P Smith, MD, John Migaly, MD, Temple University<br />
Hospital, Philadelphia, PA, USA<br />
P142 PLASMA SOLUBLE VASCULAR ADHESION MOLECULE-1 LEVELS<br />
ARE PERSISTENTLY ELEVATED DURING THE FIRST MONTH AFTER<br />
COLORECTAL CANCER RESECTION HMC Shantha Kumara, PhD, X Yan,<br />
PhD, Sonali A C Herath, BS, A Nasar, MS, A Senagore, MD, R Baxter, BS,<br />
M Kalady, MD, RL Whelan, MD, Department of Surgery,Colon &Rectal<br />
Division,St.Luke Roosevelt Hospital Center, New York, NY,USA ,Colon &<br />
Rectal Surgery, Ferguson Clinic, Grand Rapids, MI, USA, Colon & Rectal<br />
Surgery,Cleveland Clinic, Cleveland,OH, USA<br />
P143 NUCLEOTIDE-GUIDED MESORECTAL EXCISION (NGME) DURING<br />
TEM FOR RECTAL CANCER: PRELIMINARY RESULTS Emanuele<br />
Lezoche, MD FACS, Giancarlo D’Ambrosio, MD, Alessandro M Paganini,<br />
MD PhD FACS, Mario Guerrieri, MD, Giovanni Lezoche, MD, Luciana<br />
Barchetti, MD, Bernardina Fabiani, MD, Pietro Ursi, MD, Daniele Scoglio,<br />
MD, Department of General Surgery, II Clinica Chirurgica, Università “La<br />
Sapienza”, Rome. *Azienda Ospedaliera Universitaria Ospedali Riuniti,<br />
Ancona, Italy.<br />
P144 ELEVATED LEVELS OF SOLUBLE VASCULAR ADHESION<br />
MOLECULE -1 IS ASSOCIATED WITH COLORECTAL CANCER HMC<br />
Shantha Kumara, PhD, Sonali A C Herath, BS, X Yan, PhD, V Cekic, RN, N<br />
Dujovny, MD, RL Whelan, MD, Department of Surgery, Colon & rectal<br />
Division, St.Lukes- Roosevelt Hospital Center,New York,NY,USA,Colon &<br />
Rectal Surgery,Ferguson Clinic, Grand Rapids, MI, USA.<br />
P145 TRANSANAL ENDOSCOPIC MICROSURGERY: A SINGLE<br />
INSTITUTION EXPERIENCE Joshua A Waters, MD, Jeffery S Browne, MD,<br />
Eric A Wiebke, MD, Bruce W Robb, MD, Virgilio V George, MD, Indiana<br />
University Department of Surgery<br />
P146 – Withdrawn.<br />
P147 LAPAROSCOPIC MANAGEMENT OF GENERALIZED PERITONITIS<br />
Jorge Fernandez-Alvarez, MD, Omar Pichardo, MD, Armando Baqueiro-<br />
Cendon, MD, Jose Manuel Gomez, MD, Francisco Terrazas, MD, Iker Leon,<br />
MD, Gonzalo Vargas, MD, Hospital Español De Mexico<br />
P148 SELF-EXPANDABLE METALLIC STENT IS A GOOD ALTERNATIVE<br />
TO SURGERY IN COLONIC OBSTRUCTION Maria Bergstrom, MD PhD,<br />
Eva Angenete, MD PhD, Dan Asplund, MD, Helena Lindegren, MD, Per-<br />
Ola Park, MD PhD, Dept of Surgery, Sahlgrenska University Hospital,<br />
Gothenburg, Sweden<br />
P149 TEACHING RESIDENTS LAPAROSCOPIC COLECTOMY;<br />
EXPERIENCE WITH 1069 CASES Candy K Anim, PGY, Vanessa Malit, PGY,<br />
Eben Strobos, PGY, Steve Fassler, Attending, Mark Zebley, Attending,<br />
Abington Memorial Hospital<br />
P150 LAPAROSCOPY-ASSISTED SURGERY FOR RECTO-SIGMOID<br />
TUMOR: A COMPARISON OF THE MEDIAL APPROACH AND LATERAL<br />
APPROACH. H Matsuoka, MD, T Mori, MD, T Masaki, MD, T Kobayashi,<br />
MD, K Sato, M Sugiyama, MD, Y Atomi, MD, Kyorin University<br />
P151 LAPAROSCOPIC TREATMENT OF CROHN’S DISEASE: A RESIDENT<br />
CASE? Nora Meenaghan, MD, Tiffany Stoddard, MD, Yassar Youssef, MD,<br />
Stephen M Kavic, MD, University of Maryland<br />
P152 PLASMA LEVELS OF PLACENTA GROWTH FACTOR (PLGF), A<br />
PROANGIOGENIC PROTEIN, ARE ELEVATED FOR 3 WEEKS AFTER<br />
MINIMALLY INVASIVE COLORECTAL CANCER RESECTION HMC<br />
Shantha Kumara, PhD, X Yan, PhD, D Feingold, MD, M Kalady, MD, N<br />
Dujovny, MD, RL Whelan, MD, Department of Surgery,Colon&Rectal<br />
Division,St.Lukes-Roosevelt Hospital,New York,NY,USA,Department<br />
of Surgery,Columbia University,New York,USA,Colon&Rectal<br />
Surgery,Cleveland Clinic,Cleveland,OH,USA,Colon&Rectal<br />
Surgery,Ferguson Clinic,Grand Rapid,MI,USA<br />
P153 ADULT INCIDENTAL INTUSSUSCEPTION – SINGLE INSTITUTE<br />
EXPERIENCE Venkata K Kella, SivaKumar Mahalingam, Ajay K Shah,<br />
Department of Surgery, Bronx Lebanon Hospital Center, Bronx New York<br />
10457<br />
P154 IS BODY MASS INDEX A FACTOR AFFECTING PEROPERATIVE<br />
AND EARLY POSTOPERATIVE COMPLICATIONS IN LAPAROSCOPIC<br />
RECTAL CANCER SURGERY? Erman Aytac, MD, Tayfun Karahasanoglu,<br />
MD, Ismail Hamzaoglu, MD, Bilgi Baca, MD, Istanbul University<br />
Cerrahpasa Medical School, Department of General Surgery, Istanbul,<br />
Turkey<br />
P155 WHAT ABOUT MINIMALLY INVASIVE SURGERY IN SENIOR<br />
COLORECTAL PATIENTS? Sandrine Ostermann, MD PhD, Pascal Bucher,<br />
MD, Pascal Gervaz, MD PD, Isabelle Neyroud, MD, Philippe Morel, Prof,<br />
Department of Surgery, University Hospital of Geneva (HUG); Geneva<br />
Cancer Registry, Geneva, Switzerland<br />
12 th World Congress of Endoscopic Surgery 162
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P156 COLONIC VOLVULUS: NOT ONLY A DISEASE OF THE ELDERLY<br />
Sebastian V Demyttenaere, MD, Jean-Michel Lavoie, BSc, Gabriella<br />
Ghitulescu, MD, Shannon Fraser, MD, Issie Weissglas, MD, Simon<br />
Bergman, MD, Department of Surgery, Saint Mary’s Hospital and Sir<br />
Mortimer B. Davis Jewish General Hospital, McGill University<br />
P157 SINGLE INCISION LAPAROSCOPIC COLECTOMY FOR NEOPLASIA:<br />
INITIAL OPERATIVE EXPERIENCE Kelly A Garrett, MD, Daniel Geisler,<br />
MD, Feza H Remzi, MD, Cleveland Clinic<br />
P158 ONCOLOGICAL OUTCOMES OF LAPAROSCOPIC COLON<br />
RESECTION FOR CANCER AFTER IMPLEMENTATION OF A FULL-TIME<br />
PRECEPTORSHIP Yasir M Akmal, MD, Carissa Bailey, Jeong-Heum Baek,<br />
MD PhD, Michelle Metchikian, Alessio Pigazzi, MD PhD, City of Hope<br />
National Medical Center, Department of General and Oncologic Surgery<br />
P159 LAPAROSCOPIC PRIMARY REPAIR OF COLONOSCOPIC<br />
PERFORATIONS J. R Salameh, MD, J. T Mayes, MD, Department<br />
of Surgery, Georgetown University, Washington, DC and Surgical<br />
Associates at Virginia Hospital Center, Arlington, VA<br />
P160 HAND ASSISTED LAPAROSCOPIC COLECTOMY: LOW<br />
CONVERSION RATE AND SHORT HOSPITAL STAY Constantinos<br />
Constantinou, MD, Paul Meade, MD, Jane Miller, RN, Geisinger Health<br />
System<br />
P161 WHAT IS THE COMPLIANCE WITH RECOMMENDED GUIDELINES<br />
FOR ENDOSCOPIC SURVEILLANCE AFTER COLON CANCER<br />
RESECTION? Rita A Brintzenhoff, MD, Amy E Lincourt, PhD, Dimitrios<br />
Stefanidis, MD PhD, B Todd Heniford, MD, Carolinas Medical Center<br />
P162 LONG-TERM OUTCOMES AFTER LAPAROSCOPIC VERSUS OPEN<br />
TOTAL MESORECTAL EXCISION FOR MID AND LOW RECTAL CANCER:<br />
A COMPARATIVE STUDY OF 259 CONSECUTIVE RESECTION BY A<br />
SINGLE SURGEON Taek-Gu Lee, MD, Duck-Woo Kim, phD, Sung-Bum<br />
Kang, phD, Department of Surgery Seoul National University Bundang<br />
Hospital, Seoul, Korea<br />
P163 USE OF A CLINICAL PATHWAY COMBINED WITH LAPAROSCOPY<br />
AS THE STANDARD OF CARE IN ACUTE APPENDICITIS Wijaya G<br />
Premaratne, Dr, Chatika Premaratne, Dr, Stephen Strahan, Dr, Thushara<br />
Dissanayake, Dr, Rohana Wanasinghe, Dr, Department of Surgery and<br />
Gastrointestinal Endoscopy Caboolture Hospital, Queensland Australia.<br />
P164 LAPAROSCOPIC RESECTION FOLLOWING STENT INSERTION FOR<br />
OBSTRUCTING COLORECTAL CANCER Wai Lun Law, MD, Joe Fan, MD,<br />
Jensen Poon, MD, Department of Surgery, The University of Hong Kong<br />
P165 ALVIMOPAN CAN REDUCE POSTOPERATIVE ILEUS AND<br />
HOSPITAL LENGTH STAY IN LAPAROSCOPIC COLON SURGERY<br />
Alia Abdulla, DO MPH, Gretchen Aquilina, DO, Roy Sandau, DO, John<br />
D’Emilia, MD, David Berg, MD, Larry Cohen, DO, Marc Neff, MD, UMDNJ,<br />
Department of Surgery<br />
P166 LAPAROSCOPIC GASTRECTOMY WITH COMPLETE D2<br />
LYMPH NODE DISSECTION CAN BE SAFELY PERFORMED IN OUR<br />
INSTITUTION Kohei Nakata, PhD, Eishi Nagai, PhD, Kenoki Ohuchida,<br />
Takao Ohtsuka, Hiroki Toma, Masao Tanaka, Department of Surgery and<br />
Oncology, Graduate School of Medical Sciences, Kyushu University<br />
P167 COMBINED LAPAROSCOPIC AND INTRAOPERATIVE<br />
ENTEROSCOPIC MANAGEMENT OF BENIGN INTESTINAL POLYPOSIS<br />
IN PEUTZ-JEGHERS SYNDROME – A CASE SERIES Eugenius J Harvey,<br />
MBBS, Kervin Arroyo, MD, Blair S Lewis, MD, Anthony J Vine, MD, Lester B<br />
Katz, MD, Mount Sinai School of Medicine<br />
P168 OUTCOME OF LAPAROSCOPIC RECTOPEXY VERSUS PERINEAL<br />
RECTOSIGMOIDECTOMY FOR FULL-THICKNESS RECTAL PROLAPSE<br />
IN ELDERLY Seung-Hyun Lee, Paryush Lakhtaria, Hong-Jae Jo, Steven D<br />
Wexner, Cleveland Clinic Florida<br />
P169 Assessment of the Outcomes of Hand-Assisted<br />
Laparoscopy vs. Laparoscopy in Elective Colorectal<br />
Surgery in Obese Patients – Are There Advantages?<br />
Kazuhiro Narita, Cesar Reategui, Sherief Shawki, Eric G Weiss, Juan G<br />
Nogueras, Steven D Wexner, Cleveland Clinic Florida<br />
P170 LAPAROSCOPIC REMOVAL OF AN INTRAABDOMINAL<br />
INTRAUTERINE DEVICE: CASE AND SYSTEMATIC REVIEW Derek Mok,<br />
MD, Daniel W Birch, MD FRCSC FACS, Christopher DeGara, MD FRCSC,<br />
Shahzeer Karmali, MD FRCSC, University of Alberta<br />
P171 HOSPITALIZATION COSTS OF LAPAROSCOPIC VS OPEN<br />
APPENDECTOMY: 5 YEAR EXPERIENCE. Jorge Cervantes, Carlos M<br />
Cardenas, Enrique R Jean, Sergio A Toledo, Adrian Murillo, Jose A Posada,<br />
Raul Lopez - Infante, Pablo D Murakami, Department Of Surgery, The<br />
American British Cowdray Medical Center, Mexico City.<br />
P172 LAPAROSCOPIC PRIMARY COMMON DUCT REPAIR:<br />
MANAGEMENT OF AN UNUSUAL COMPLICATION OF ERCP Alfred<br />
B Johnson, MD, Teresa Klainer, MD, Highland Community Hospital,<br />
Picayune, MS<br />
P173 PREOPERATIVE EVALUATION OF THE MAJOR BRANCHES OF<br />
THE MID HEPATIC VEIN AND PORTAL VEIN AT THE LIVER BED<br />
WITH THE DYNAMIC FLOW INVESTIGATION BY THE DOPPLER<br />
ULTRASONOGRAPHY TO AVOID THE BLEEDING FROM THE LIVER<br />
BED AT LAPAROSCOPIC CHOLECYSTECTOMY. Minoru Kakihara,<br />
MD PhD, Eiichi Sugasawa, MD PhD, Yoshiki Kajiwara, MD, Toshimichi<br />
Takigawa Phd, MD, Taichi Satou, MD, Nobuaki Kawarabayashi, MD PhD,<br />
Kazuo Hatsuse, MD PhD, Junji Yamamoto, MD PhD, Department of<br />
Surgery, National Defense Medical College, Japan.<br />
P174 DOES AN INCREASED BODY MASS INDEX (BMI) LEAD TO<br />
INCREASED RATES OF CONVERSION DURING LAPAROSCOPIC<br />
CHOLECYSTECTOMY? Daniel T Farkas, MD, Dovid S Moradi, BA, John M<br />
Cosgrove, MD, Bronx-Lebanon Hospital Center, Albert Einstein College<br />
of Medicine, Bronx, NY, USA.<br />
P175 MAJOR COMPLICATIONS OF LAPAROSCOPIC<br />
CHOLECYSTECTOMY ARE NOT NECESSARILY MEDICAL NEGLIGENCE<br />
– THE EVIDENCE IN SURGICAL LITERATURE. Manmohan Varma, MS,<br />
Kushal Varma, Medical Student, Private, Kanpur, India<br />
P176 THE ROLE OF BODY MASS INDEX AND VISCERAL FAT AREA IN<br />
COLORECTAL CANCER PATIENTS TREATED WITH LAPAROSCOPIC-<br />
ASSISTED SURGERY. Noriko Matsumoto, MD, Mitsuo Shimada, Prof,<br />
Nobuhiro Kurita, MD PhD, Takashi Iwata, MD PhD, Masanori Nishioka,<br />
MD PhD, Shinya Morimoto, MD PhD, Jun Higashijima, MD PhD,<br />
Tomohiko Miyatani, MD PhD, Toshihiro Nakao, MD, Oura Ryoko, MD,<br />
Masato Komatsu, MD, Hi, Department of Surgery, The University of<br />
Tokushima, Japan<br />
P177 THE CLINICAL RESERCH OF PREVENTION OF PANCREATIC<br />
LEAKAGE AND THE USEFULNESS OF FIBRIN GLUE AND POLYGLYCOL<br />
ACID FELT AFTER LAPAROSCOPIC ASSISTED GASTRECTOMY FOR<br />
GASTRIC CANCER Yuichiro Hiura, MD, Shuji Takiguchi, MD PhD, Makoto<br />
Yamasaki, MD PhD, Kiyokazu Nakajima, MD PhD, Hiroshi Miyata, MD<br />
PhD, Yoshiyuki Fujiwara, MD PhD, Masaki Mori, MD PhD, Yuichiro Doki,<br />
MD PhD, Osaka University, Graduate School of Medicine, Department of<br />
Gastroenterological Surgery<br />
P178 CAN CASE SELECTION MINIMISE CONVERSION RATE IN<br />
LAPAROSCOPIC COLORECTAL SURGERY? Susannah M Wyles, MBBS<br />
MSc MRCS, Danilo Miskovic, MD FRCS, Zhifang Ni, MSc, Ara W Darzi,<br />
FMedSci HonFREng KBE, George B Hanna, PhD FRCS, Biosurgery and<br />
Surgical Technology, Imperial College London<br />
P179 ACUTE PANCREATITIS AFTER ELECTIVE LAPAROSCOPIC<br />
CHOLECYSTECTOMY: RETROSPECTIVE STUDY JR Ramirez Gavidia,<br />
MD, P Raj, Cleveland Clinic Foundation<br />
P180 SPONTANEOUS RETROPERITONEAL HAEMATOMA CAUSED BY<br />
LUMBAR ARTERY BLEED. JR Ramirez Gavidia, P Raj, Clevelan Clinic<br />
Foundation<br />
P181 PREVENTION OF STOMAL COMPLICATIONS Madhav V Phadke,<br />
MD FACS, Lewis H Stocks, MD PhD FACS, Yeshwant G Phadke, MD FACS,<br />
WakeMed, Raleigh, NC affiliated with UNC Chapel Hill, NC, USA<br />
12 th World Congress of Endoscopic Surgery<br />
163 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P182 SURGEON-CONTROLLED FACTORS THAT REDUCE MONOPOLAR<br />
ELECTROSURGERY CAPACITIVE COUPLING DURING LAPAROSCOPY<br />
Thomas N Robinson, MD FACS, Katherine R Pavlovsky, MS, Heidi Looney,<br />
MS, Greg V Stiegmann, MD FACS, Francis T McGreevy, BS, University of<br />
Colorado School of Medicine, Denver, CO, USA.<br />
P183 COMPLICATIONS OF BARIATRIC SURGERY AND SOLUTION Dr Ali<br />
Fardoun, MD, Fawaz Torab, Phd associated prof, tawam UAE affiliated<br />
with John’s Hopkins<br />
P184 SAFETY OF OPEN TECHNIQUE FOR FIRST TROCAR PLACEMENT<br />
IN LAPAROSCOPIC SURGERY – A SERIES OF 6000 CASES Pawanindra<br />
Lal, MD, Rajeev Sharma, MD, Jagdish Chander, MD, Vinod K Ramteke,<br />
MD, Maulana Azad Medical College, New Delhi, India & Government<br />
Medical College, Chandigarh.<br />
P185 ESOPHAGEAL-PLEURAL FISTULA AFTER LAPAROSCOPIC SLEEVE<br />
GASTRECTOMY (LSG): SUCCESSFUL ENDOSCOPIC MANAGEMENT.<br />
Juan D Hernandez, MD, Hector Cardona, MD, Natan Zundel, Hospital<br />
Central de la Policía, Universidad de los Andes, Miami International<br />
University<br />
P186 COMMUNICATION PROBLEMS ACROSS SURGICAL PATIENTS’<br />
CARE PATHWAYS Kamal Nagpal, MD, Sonal Arora, MRCS, Helen Wong,<br />
MSc, Nick Sevdalis, PhD, Amit Vats, MRCS, Charles Vincent, PhD, Krishna<br />
Moorthy, FRCS, Department of Biosurgery and Surgical Technology,<br />
Imperial College, St Mary’s Hospital, Praed Street, London W21NY,<br />
United Kingdom.<br />
P187 PULMONARY EMBOLISM IN LAPAROSCOPIC<br />
CHOLECYSTECTOMY Prasanta Raj, MD MS FACS, Neilendu Kundu, MD,<br />
Andrew Smith, MD, Fairview Hospital / Cleveland Clinic Health Systems<br />
P188 EYE TRACKING AS A TOOL TO EVALUATE COLONOSCOPY SKILL<br />
Kazuhiko Shinohara, MD PhD, Yasushi Yamauchi, PhD, Tokyo University<br />
of Technology<br />
P189 HIGH FIDELITY RECONSTRUCTION OF HUMAN ANATOMY USING<br />
3 DIMENSIONAL PRINTING: PROOF OF CONCEPT Robert A Andrews,<br />
MD, Justin W Kung, MD, Theodore Korelitz, Scott R Johnson, MD, Daniel<br />
B Jones, MD, Beth Israel Deaconess Medical Center, Carl J Shapiro<br />
Simulation and Skills Center, Harvard Medical School<br />
P190 TRAINING MODEL FOR LAPAROSCOPIC COMMON BILE DUCT<br />
EXPLORATION. IMPACT IN THE IMPROVEMENT OF SURGICAL SKILLS.<br />
Alexis Sanchez, MD, Omaira Rodriguez, MD, Renata Sanchez, MD,<br />
Gustavo Benitez, MD, Omar Bellorin-Marin, MD, Samuel Szomstein, MD<br />
FACS, Universitary Hospital of Caracas, Central University of Venezuela,<br />
Caracas-Venezuela. Cleveland Clinic Florida, Weston-Florida<br />
P191 CROSS-PLATFORM ADAPTATION AND VALIDATION OF<br />
LAPAROSCOPIC SKILLS TASKS: SOME TASKS ARE ROBUST ACROSS<br />
PLATFORMS Daniel Box, BS, Rollin Nagel, PhD, David Way, MS, Alan E<br />
Harzman, MD, The Ohio State University, Columbus, Ohio, USA<br />
P192 RESULTS AND PERSPECTIVE TO THE FUTURE IN THE FIELD OF<br />
LAPAROSCOPIC CHOLECYSTECTOMY OF JAPANESE ENDOSCOPIC<br />
SURGICAL SKILL QUALIFICATION SYSTEM Sumio Matsumoto, PhD,<br />
Hiromi Tokumura, PhD, Yuichi Yamashita, PhD, Toshiyuki Mori, PhD,<br />
Masaki Kitajima, PhD, 1ESSQS Committee of the Japan Society for<br />
Endoscopic Surgery, Tokyo, Japan<br />
P193 FIVE YEAR EXPERIENCE OF THE LAPAROSCOPIC SKILL<br />
ACCREDITATION SYSTEM IN JAPAN Toshiyuki Mori, MD PhD, Yutaka<br />
Atomiu, MD PhD, Taizo Kimura, MD PhD, Masaki Kitazima, MD PhD,<br />
Department of Surgery, Kyorin University, Japan<br />
P194 ASSESSING THE VALIDITY OF SIMULATING THE FUNDAMENTALS<br />
OF LAPAROSCOPY (FLS) TASKS IN VIRTUAL REALITY Vanessa N Palter,<br />
MD, Neil Orzech, MD, Teodor P Grantcharov, MD PhD, The Wilson Centre<br />
and St Michael’s Hospital, Toronto, Canada<br />
P195 A NOVEL SENSORIZED INSTRUMENT-BASED MINIMALLY<br />
INVASIVE SURGERY (SIMIS) TOOL: INITIAL CONSTRUCT VALIDATION<br />
OF POSITION SENSING Shiva Jayaraman, MD MESc, Ana Luisa<br />
Trejos, MASc, Andrew C Lyle, Michael D Naish, PhD, Rajni V Patel, PhD,<br />
Christopher M Schlachta, MD, CSTAR (Canadian Surgical Technologies &<br />
Advanced Robotics), Lawson Health Research Institute and Department<br />
of Surgery, Schulich School of Medicine and Dentistry, The University of<br />
Western Ontario, London, Ontario, Canada<br />
P196 TELEMENTORING OF ENDOSCOPIC SUTURING USING THE<br />
ANNOTATION SYSTEM BETWEEN JAPAN AND THAILAND Kazuo<br />
Tanoue, MD PhD FACS, Satoshi Ieiri, MD PhD, Kozo Konishi, MD PhD,<br />
Kenoki Ohuchida, MD PhD, Manabu Onimaru, MD, Morimasa Tomikawa,<br />
MD PhD, Makoto Hashizume, MD PhD FACS, Department of Advanced<br />
Medicie and Innovative Technology<br />
P197 MENTORSHIP FOR PARTICIPANTS IN A LAPAROSCOPIC<br />
COLECTOMY COURSE Vanessa P Ho, MD, Koiana Trencheva, MS BSN,<br />
Sharon L Stein, MD, Jeffrey W Milsom, MD, Weill Cornell Medical College-<br />
NewYork Presbyterian Hospital<br />
P198 PORTABLE, SELF-PRACTICE LAPAROSCOPIC BOX TRAINERS<br />
UNDERUTILIZED BY SURGICAL TRAINEES Michael A Russo, MD, Shawn<br />
Tsuda, MD, University of Nevada School of Medicine<br />
P199 HOW DO WE MAKE DECSIONS REGARDING CANCER<br />
MANAGEMENT? Zhifang Ni, Miss, Kamran Ahmed, Mr, Laura<br />
Zimmermann, Miss, George Hanna, Prof, Imperial College London<br />
P200 SINGLE INCISION LAPAROSCOPIC SURGERY TRAINING COURSE:<br />
THE NEXT STEP IN SURGICAL EDUCATION Avraham Schlager, MD,<br />
Ram Elazary, MD, Abed Khalaileh, MD, Noam Shussman, MD, Gideon<br />
Zamir, MD, Avraham I Rivkind, MD, Yoav Mintz, MD, Hadassah-Hebrew<br />
University Center, New York University Medical Center<br />
P201 PLAYING NINTENDO® WII IMPROVES VIRTUAL REALITY<br />
LAPAROSCOPIC SIMULATOR PERFORMANCE Kellie K Middleton, MPH,<br />
John L Falcone, MD, Giselle G Hamad, MD FACS, Dana B Middleton,<br />
Travis M Hamilton, BS, University of Pittsburgh School of Medicine,<br />
University of Pittsburgh Medical Center<br />
P202 USE OF IMAGES TO ILLUSTRATE THE MEDICAL CONDITIONS IN<br />
THE OUTPATIENT CLINIC. R Vilallonga, PhD, Jm Fort, PhD, O Gonzalez,<br />
PhD, Ja Baena, PhD, M Armengol, PhD, Universitary Hospital Vall<br />
d’Hebron. Barcelona.<br />
P203 THE IMPACT OF A MENTOR ON THE EARLY LEARNING CURVE<br />
IN LAPAROSCOPIC COLORECTAL SURGERY Susannah M Wyles, MBBS<br />
MSc MRCS, Danilo Miskovic, MD FRCS, Zhifang Ni, MSc, Ara W Darzi,<br />
FMedSci HonFREng KBE, George B Hanna, PhD FRCS, Department of<br />
Biosurgery and Surgical Technology, Imperial College London<br />
P204 MEASURING PERFORMANCE USING THE GOALS-INCISIONAL<br />
HERNIA MODULE (GOALS-IH) Marilou Vaillancourt, MD, Iman Ghaderi,<br />
MD, Pepa Kaneva, MSc, Melina Vassiliou, MD, Nicole Koloszvari, MD,<br />
Gerald M Fried, MD, Liane S Feldman, MD, Steinberg-Bernstein Centre<br />
for Minimally Invasive Surgery & Innovation, McGill University, Montreal,<br />
Quebec, Canada<br />
P205 LAPAROSCOPIC APPENDECTOMY IS FEASIBLE AND SAFE IN<br />
SURGICAL TRAINING Ramon A Saade-Cardenas, MD, Maria E Aponte-<br />
Rueda, PhD MD, Miguel J Saade-Aure, PhD MD FACS, Gustavo A Benitez,<br />
MD, Salvador Navarrete-Aulestia, MD, Caracas University Hospital.<br />
Central University of Venezuela.Service of Surgery II-III<br />
P206 WEB BASED TELE-SIMULATION TRAINING Danny A Sherwinter,<br />
MD, Maimonides Simulation Center, Maimonides Medical Center,<br />
Brooklyn NY, USA<br />
P207 THE IMPACT OF VERBAL GUIDANCE ON LAPAROSCOPIC SKILLS<br />
TRAINING AND MULTI-TASKING PERFORMANCE Jamie Poolton, PhD,<br />
Joe Fan, MD, Rich S Master, PhD, Niv G Patil, MD Professor, Wai Lun Law,<br />
MD Professor, The University of Hong Kong<br />
12 th World Congress of Endoscopic Surgery 164
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P208 VIRTUAL REALITY SIMULATOR FOR THE TRAINING OF OPTICAL<br />
TROCAR ACCESS Michitaka Fujiwara, MD, Norifumi Ohashi, MD,<br />
Akimasa Nakao, MD, Masamichi Sakaguchi, PhD, Hiroki Hidaka, PhD,<br />
Hideo Fujimoto, PhD, Department of Surgery II, Graduate School of<br />
Medicine, Nagoya University, Graduate School of Engineering, Nagoya<br />
Institute of Technology<br />
P209 PROFICIENCY-BASED VIRTUAL REALITY LAPAROSCOPIC SKILLS<br />
TRAINING: A 7-YEAR EXPERIENCE Peter S Wu, MD, Ron W Bush, BS,<br />
Neal E Seymour, MD, Department of Surgery, Baystate Medical Center.<br />
Springfield, MA<br />
P210 THE FUNDAMENTALS OF LAPAROSCOPIC SURGERY (FLS)<br />
SIMULATOR AS A PLATFORM FOR EVALUATING SINGLE PORT<br />
LAPAROSCOPIC SURGERY AND ENABLING INSTRUMENTATION S.<br />
Al-Sabah, MD MBA, LS Feldman, MD, MC Vassiliou, MD MEd, PA Kaneva,<br />
MSc, GM Fried, MD, Steinberg- Bernstein Centre for Minimally Invasive<br />
Surgery and Innovation, McGill University Health Centre, Montreal,<br />
Canada<br />
P211 LAPAROSCOPE POSITION IMPACTS SURGEON EFFICIENCY AND<br />
WORKLOAD Paul N Montero, MD, Christina Acker, Dimitrios Stefanidis,<br />
MD PhD, B T Heniford, MD, Carolinas Laparoscopic and Advanced<br />
Surgery <strong>Program</strong>, Carolinas Medical Center<br />
P212 LAPAROSCOPIC FELLOWSHIP DOES NOT AFFECT GENERAL<br />
SURGERY RESIDENT EXPERIENCE Mohamed I Dahman, MD, Bruce D<br />
Schirmer, MD, Peter T Hallowell, MD, Department of Surgery, University<br />
of Virginia, Charlottesville, VA, USA<br />
P213 ENDOSCOPIC HARVESTING OF THE GRACILIS MUSCLE -<br />
EXPERIMENTAL STUDY IN A SWINE MODEL Alexandru I Blidisel, MD<br />
Phd, Lucian p Jiga, MD Phd, Laurentiu Sima, MD Phd, Octavian Cretu,<br />
MD Phd, Mihai Ionac, MD Phd, University Of Medicine and Pharmacy<br />
from Timisoara, Romania<br />
P214 LIVE CADAVERIC LAPAROSCOPY WITH LAPAROSCOPIC VIDEOS<br />
IN GROSS ANATOMY: INFLUENCE ON LEARNING AND CAREER<br />
CHOICE Sean B Orenstein, MD, Ean R Saberski, BS, Yuri W Novitsky, MD,<br />
University of Connecticut School of Medicine, Farmington, Connecticut<br />
P215 GILDING THE GOLDEN HOUR: USING M&M CONFERENCE DATA<br />
TO REFINE RESIDENT EDUCATION AND PATIENT SAFETY Stephen M<br />
Kavic, MD, Adrian Park, MD, University of Maryland<br />
P216 DOES A FELLOW’S INVOLVEMENT IN ADVANCED LAPAROSCOPIC<br />
PROCEDURES IMPROVE OUTCOMES? Jeffrey J Wannares, Timothy<br />
D Jackson, MD MPH, Robert T Lancaster, MD MPH, Matthew M Hutter,<br />
MD MPH FACS, The Codman Center for Clinical Effectiveness in Surgery,<br />
Massachusetts General Hospital<br />
P217 DOES A LAPAROSCOPIC SKILLS TRAINING CURRICULUM ON<br />
A VIRTUAL TRAINER IN A BUSY SURGICAL RESIDENCY PROGRAM<br />
NEED TO BE OPTIMIZED? Ben Selvan, MS, N. N Williams, MB BCh<br />
MCh FRCSI FRCSGen, Andrew S Resnick, MD, Jon B Morris, MD,<br />
Mayank Mittal, MRCS, K. R Dumon, MD, The Penn Medicine Clinical<br />
Simulation Center, Department of surgery, Hospital of University of<br />
Pennsylvania,Philedelphia.PA 19130<br />
P218 INCREASED VIDEO GAME EXPERIENCE RESULTS IN<br />
IMPROVED LAPAROSCOPY SKILLS: A PROSPECTIVE STUDY OF<br />
LAPAROSCOPICALLY NAIVE SUBJECTS Mark A Vitale, Wesley B<br />
Jones, MD, Jeff W Allen, MD, Gary C Vitale, MD, Department of Surgery,<br />
University of Louisville School of Medicine, Louisville, KY, USA<br />
P219 A RETROSPECTIVE STUDY CHALLENGES THE CONSTRUCT<br />
VALIDITY OF COLONOSCOPIC VIRTUAL TRAINING Ben Selvan, MS,<br />
K. R Dumon, MD, Jon B Morris, MD, Andrew S Resnick, MD, Mayank<br />
Mittal, MRCS, N. N Williams, MB BCh MCh FRCSI FRCSGen, The Penn<br />
Medicine Clinical Simulation Center , Department of Surgery, Hospital<br />
Of University of Pennsylvania, Philedelphia, PA 19130<br />
P220 TRAINING THE SURGEONS FOR COMPLEX SURGICAL UPPER<br />
GASTRO INTESTINAL AND COLORECTAL PROCEDURES IN UNITED<br />
KINGDOM Amir Nisar, FRCS, Glasg FRCSI FRCS, H Ali, J Gossage, Umerto<br />
Bracale, Oesophago Gastric Regional Unit, Maidstone and Tunbridge<br />
Wells Trust, Maidstone, Kent, England, United Kingdom<br />
P221 OBJECTIVE ASSESSMENT OF LAPAROSCOPIC SURGICAL SKILL<br />
USING THE DUAL-TASK APPROACH Adam T Meneghetti, MD, George<br />
Pachev, Valentyna Koval, Bin Zheng, MD, Karim Qayumi, MD, Ormond N<br />
Panton, MD, University of British Columbia<br />
P222 VALIDATION OF A NEW TRAINING CURRICULUM FOR BASIC<br />
LAPAROSCOPIC SKILLS Christian I Villeda-Sandoval, MD, David<br />
Velázquez-Fernández, MD PhD, Juan Pantoja, MD, Patricio Santillán-<br />
Doherty, MD, Miguel F Herrera, MD, Mauricio Sierra, MD, National<br />
Institute of Medical Sciences and nutrition “Salvador Zubirán”<br />
P223 INVESTIGATION OF THE RELATIONSHIP RISK FACTOR OF<br />
LAPAROSCOPIC ASSISTED GASTRECTOMY AND THE SKILL OF<br />
THE ASSISTANT OF OPERATION TEAM. Takashi Iwata, MD, Mitsuo<br />
Shimada, MD PhD FACS, Hideya Kashihara, MD, Jun Higanshijima, MD,<br />
Kozo Yoshikawa, MD, Shinaya Morimoto, MD, Masanori Nishioka, MD,<br />
Nobuhiro Kurita, MD, Department of Surgery, The Tokushima University<br />
P224 SURGICAL RESIDENT RETENTION OF FUNDAMENTALS OF<br />
LAPAROSCOPY (FLS) SKILLS Don J Selzer, MD, Daniel McKenna, MD,<br />
Jennifer Choi, MD, Laura Torbeck, PhD, Department of Surgery, Indiana<br />
University School of Medicine, Indianapolis, IN, USA<br />
P225 A MULTI-CENTER, SIMULATION-BASED SKILLS TRAINING<br />
COLLABORATIVE USING SHARED GI MENTOR II SYSTEMS:<br />
RESULTS FROM THE TEXAS ASSOCIATION OF SURGICAL SKILLS<br />
LABORATORIES (TASSL) FLEXIBLE ENDOSCOPY CURRICULUM Kent<br />
Van Sickle, MD, Lauren Buck, MD, Ross Willis, PhD, Alicia Mangram, MD,<br />
Michael S Truitt, MD, Mohsen Shabahang, MD PhD, Scott Thomas, MD,<br />
Lee Trombetta, MD, Brian Dunkin, MD, Daniel Scott, MD, UT Health<br />
Science Center San Antonio (UTHSCSA), Methodist Hospital, Dallas,TX<br />
(MHD), Texas A&M University, Temple, TX (TAMU), Brooke Army Medical<br />
Center, San Antonio, TX (BAMC), Methodist Hospital, Houston, TX, UT<br />
Southwestern, Dallas,TX (UTSW)<br />
P226 INDIVIDUALIZED SIMULATION USING 3D VIRTUAL REALITY<br />
IMAGE FACILITATES LEFT COLON CANCER SURGERY Norifumi Òhashi,<br />
MD, Michitaka Fujiwara, MD, Chie Tanaka, MD, Naoki Iwata, MD, Kensaku<br />
Mori, PhD, Goro Nakayama, MD, Masahiko Koike, MD, Yasuhiro Kodera,<br />
MD, Akimasa Nakao, MD, Department of Surgery II, Graduate School of<br />
Medicine, Nagoya University, Graduate School of Information Science,<br />
Nagoya University<br />
P227 VALIDATION OF A HIGH-FIDELITY NOTES SIMULATOR FOR<br />
TEAM TRAINING Shawn Tsuda, MD, Kai Matthes, MD, Charles St. Hill,<br />
MD, Alexandre Derevianko, MD, Tori Derevianko, Adnan Mohsin, Daniel<br />
Hashimoto, James Lau, MD, University of Nevada School of Medicine,<br />
Las Vegas, NV, USA; Beth Israel Deacones Medical Center, Boston, MA,<br />
USA, Boston University School of Medicine, Boston, MA, USA<br />
P228 IMPACT OF LEARNING STYLE IN NOVICES’ ACQUISITION OF<br />
MINIMALLY INVASIVE SURGICAL (MIS) BASIC SKILLS J Paige, MD, T<br />
Yang, MD, R Suleman, MD, S Chauvin, Ph D, J Alleyn, MD, M Brewer, MD,<br />
R Hoxsey, MD, Louisiana State University Health Sciences Center<br />
P229 EVALUATION OF NOTES® HANDS-ON COURSES BY SURGEONS AT<br />
THE <strong>SAGES</strong> ANNUAL MEETING LEARNING CENTER Mark A Gromski,<br />
BA, Fuad Alkhoury, MD, Suck-Ho Lee, MD PhD, Kai Matthes, MD PhD,<br />
Beth Israel Deaconess Medical Center, Harvard Medical School, Boston,<br />
MA and Hospital of Saint Raphael, Yale School of Medicine, New Haven,<br />
CT<br />
P230 PROGRAM OF BASIC TRAINING IN ENDOSCOPY FOR SURGEONS<br />
TO PERFORM NOTES Kiyoshi Hashiba, MD PhD, Sergio Roll, MD PhD,<br />
Pablo R Siqueira, MD, Marco A D`Assunção, MD, Jarbas M Farraco, MD,<br />
Institute of Teaching and Research of the Lebanese Syrian Hospital<br />
P231 THE USE OF REMOTE COMPUTER AUDIO-VIDEO PROCESSING<br />
TO CONDUCT SURGICAL FELLOWSHIP INTERVIEWS OF DEPLOYED<br />
PHYSICIANS. C V Chukwumah, MD, C Shega, M J Rosen, MD, L Khaitan,<br />
MD, J L Ponsky, MD, J M Marks, MD, University Hospitals Case Medical<br />
Center, Cleveland, Ohio,USA<br />
165 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P232 SURGICAL TECHNOLOGISTS DEMONSTRATE INITIAL<br />
PROFICIENCY AND POSITIVE IMPRESSIONS OF LAPAROSCOPIC<br />
AND ENDOSCOPIC SKILLS TRAINING Shawn Tsuda, MD, Samaan<br />
Sattarzadeh, Adnan Mohsin, Charles St. Hill, MD, Wright Jones, MD,<br />
James Lau, MD, University of Nevada School of Medicine, Las Vegas, NV,<br />
USA<br />
P233 CURRENT STATUS OF PERI-OPERATIVE TECHNICAL SKILL<br />
FEEDBACK – A NEEDS ASSESSMENT Don J Selzer, MD, Rahul Reddy, BS,<br />
Jennifer Choi, MD, Laura Torbeck, PhD, Department of Surgery, Indiana<br />
University School of Medicine, Indianapolis, IN, USA<br />
P234 VR TO OR PART II: THE EFFECT OF WARMUP ON OPERATIVE SKILLS<br />
IN THE OR Aaron Ashby, Kanav Kahol, PhD, Sumeet Kadakia, MD, John J<br />
Ferrara, MD FACS, Marshall L Smith, MD PhD, Richard M Satava, *Human<br />
Machine Symbiosis Laboratory, Department of Biomedical informatics,<br />
Arizona State University, Phoenix Arizona, +Banner Good Samaritan<br />
Medical Center, Phoenix, Arizona, ^Department of Surgery, University of<br />
Washington, Seattle Washington<br />
P235 NOTES IN EMERGENCY José F Noguera, MD PhD, Angel Cuadrado,<br />
MD PhD, Carlos Dolz, MD PhD, José M Olea, MD, Rafael Morales, MD,<br />
José C Vicens, MD, Luis Lozano, MD, Hospital Son Llàtzer<br />
P236 NOTES® STAPLED CYSTGASTROSTOMY –A NOVEL APPROACH<br />
FOR SURGICAL MANAGEMENT OF PANCREATIC PESUDOCYSTS<br />
Ratnakishore Pallapothu, MD, John Romanelli, MD, David Desilets,<br />
MDPhD, David Earle, MD, Baystate Medical Center, Tufts University<br />
School of Medicine, Springfield, MA<br />
P237 SINGLE INCISION PROCEDURE WITH CONVENTIONAL PORTS<br />
AND INSTRUMENTS Shailesh Puntambekar, MS, Galaxy-Care<br />
Laparoscopy Institute<br />
P238 HYBRID TRANSVAGINAL CHOLECYSTECTOMY Sanjeev K Singla,<br />
Dr, Sushil Budhiraja, Ravinder P Babra, Dayanand Medical College &<br />
Hospital, Ludhiana, India<br />
P239 FIRST CROATIAN TRANSVAGINAL LAPAROSCOPICALLY<br />
ASSISTED CHOLECYSTECTOMIES Zdravko Perko, Prof PhD, Radoslav<br />
Stipic, MD, Zoran Cala, Prof PhD, Zeljko Mimica, Prof PhD, Jasenka<br />
Kraljevic, MD, University Hospital and Medical School, Split, Croatia<br />
P240 NOTES PERITONEOSCOPY WITH CO2 INSUFFLATION SHOWS<br />
SIMILAR PHYSIOLOGIC STRESS AS STANDARD LAPAROSCOPY IN A<br />
SWINE MODEL. Erica A Moran, MD, Christopher J Gostout, MD, Juliane<br />
Bingener, MD, Department of Surgery, Mayo Clinic College of Medicine,<br />
Rochester, MN; Department of Medicine, Division of Gastroenterology<br />
and Hepatology, Developmental Endoscopy Unit, Mayo Clinic College of<br />
Medicine, Rochester, MN, United States.<br />
P241 TRANSORAL ENDOSCOPIC THYROIDECTOMY Nobumi Tagaya,<br />
PhD, Hiroyuki Oyama, MD, Keiichi Kubota, PhD, Second Department of<br />
Surgery, Dokkyo Medical University, Tochigi, Japan<br />
P242 NATURAL ORIFICE TRANSLUMENAL ENDOSCOPIC SURGERY<br />
(NOTES): A TECHNICAL REVIEW Edward D Auyang, MD, Daniel H Enter,<br />
BA, Byron F Santos, MD, Eric S Hungness, MD, Nathaniel J Soper, MD,<br />
Northwestern University, Department of Surgery<br />
P243 SURGEONS’ ATTITUDES TOWARDS NATURAL ORIFICE<br />
TRANSLUMENAL ENDOSCOPIC SURGERY Joe KM Fan, MD, Christine<br />
SY Lo, MD, Wai Lun Law, MD Professor, The University of Hong Kong,<br />
Hong KOng<br />
P244 TEMS USING SINGLE PORT INSTRUMENTS HJ Kim, MD, HM Cho,<br />
MD, SC Lee, MD, JK Shim, MD, IK Lee, MD, YS Lee, MD, ST Oh, MD, JG Kim,<br />
MD, Deparment of Surgery, The Catholic University of Korea<br />
P245 A NOVEL DEVICE FOR ENDOSCOPIC TRANSMURAL TISSUE<br />
FIXATION Kenneth Binmoeller, MD, Janak Shah, MD, California Pacific<br />
Medical Center<br />
12 th World Congress of Endoscopic Surgery 166<br />
P246 MAGNETIC CAUTERY DISSECTOR SUITABILITY FOR<br />
TRADITIONAL OR SINGLE SITE LAPAROSCOPIC CHOLECYSTECTOMY<br />
IN HUMAN CADAVER MODELS Lauren B Mashaud, MD, Emmanuel<br />
Eisenstein, BS, Deborah C Hogg, BS, Angel Caban, MD, Sara Best, MD, Jeff<br />
Cadedu, MD, Richard Bergs, MS, Heather Beardsley, PhD, Juan Paramo,<br />
Raul Fernandez, PhD, Daniel J Scott, MD, UT Southwestern Center for<br />
Minimally Invasive Surgery<br />
P247 SINGLE ACCESS TRANSVAGINAL NOTES LYMPHATIC MAPPING<br />
WITH COLONIC SENTINEL NODE BIOPSY IN A PORCINE MODEL Susan<br />
H Whang, MD, Jason Loewen, MD, Brent W Miedema, MD, Klaus Thaler,<br />
MD, University of Missouri, Department of General Surgery<br />
P248 INITIAL EXPERIENCE IN ECORES (ENDOSCOPIC COLORECTAL<br />
SURGERY) Ifesegun D Ayodeji, MD, Bas Govaert, MD, Nicole D Bouvy,<br />
MD PhD, Cor G Baeten, MD PhD, Marjolein L Smidt, MD PhD, Maastricht<br />
University Medical Center, Department of General surgery<br />
P249 SINGLE INCISION LAPAROSCOPIC COLORECTAL SURGERY: A<br />
PRELIMINARY EXPERIENCE Elie K Chouillard, MD, Andrew A Gumbs,<br />
MD, Poissy Medical Center (FRANCE) and Fox Chase Cancer Center (USA)<br />
P250 HYBRID NOTES SLEEVE GASTRECTOMY FOR MORBID OBESITY<br />
Elie K Chouillard, MD, Ziad Elrassi, MD, Poissy Medical Center (France)<br />
and Saint-Georges Hospital (Lebanon)<br />
P251 TWO HANDED ENDOSCOPIC ROBOT FOR USE IN NATURAL<br />
ORIFICE TRANSLUMENAL ENDOSCOPIC SURGERY (NOTES)<br />
TRANSABDOMINAL PRE-PERITONEAL (TAPP) INGUINAL<br />
HERNIORRHAPHY Danny A Sherwinter, MD, Department of minimally<br />
invasive Surgery, Maimonides Medical Center, Brooklyn N.Y.<br />
P252 CIRCUMFERENTIAL PERIUMBILICAL INCISION APPROACH FOR<br />
THE RESECTION OF T1N0 AND TIS COLON CANCER: RELEVANCE TO<br />
SINGLE PORT LAPAROSCOPIC SURGERY (SILS) Tomonori Ohsawa, MD,<br />
Hideyuki Ishida, PhD, Daijo Hashimoto*, PhD, Department of Digestive<br />
Tract and General Surgery and Hepatobiliary and Pancreatic and<br />
Pediatric Surgery*, Saitama Medical Center, Saitama Medical School<br />
P253 TRANSGASTRIC DIAGNOSTIC PERITONEOSCOPY WITH<br />
LAPAROSCOPIC ASSISTANCE USING A NOVEL FLEXIBLE TOOLBOX<br />
FOR ADVANCED MINIMALLY INVASIVE PROCEDURES: AN INITIAL<br />
EVALUATION Vanchad R Memark, MD, Nilay R Shah, MD, Peter N Nau,<br />
MD, Clinton R Hall, MD, Eric T Volckmann, MD, Rebecca R Dettorre, BA<br />
CCRC, Bradley J Needleman, MD, W. Scott Melvin, MD, Jeffrey W Hazey,<br />
MD, Center for Minimally Invasive Surgery, Division of Gastrointestinal<br />
Surgery, The Ohio State University Medical Center, Columbus, Ohio, USA<br />
P254 TRANSLUMENAL TRANSPARENT NAVIGATION BY OSIRIX GPS<br />
SYSTEM IN SINGLE INCISION LAPAROSCOPIC SURGERY AND NOTES<br />
Maki Sugimoto, MD PhD, Yoshinori Morita, MD PhD, Takeshi Azuma, MD<br />
PhD, Gastroenterology Kobe University, Veterans Affairs Palo Alto Health<br />
Care System, Stanford University<br />
P255 TOTAL TRANSVAGINAL APPENDECTOMY: LESS PAIN AND<br />
FASTER RECOVERY Kurt E Roberts, MD, Andrew J Duffy, MD, Dan Silasi,<br />
MD, Tom Rutherford, MD, Jeuse Saint Fleur, NP, Priya Jamidar, MD, Robert<br />
L Bell, MD, Department of Surgery, Yale School of Medicine.<br />
P256 PATIENTS AND SURGEONS PERCEPTIONS OF NATURAL<br />
ORIFICE TRANSLUMINAL ENDOSCOPIC SURGERY (NOTES), A<br />
SOUTHAMERICAN POINT OF VIEW. María Francisca Navarrete, MD,<br />
Alex Escalona, MD, Francisco Riquelme, Intern, Ignacio Cifuentes, MD,<br />
Pontificia Universidad Católica de Chile<br />
P257 SURGICAL ENTEROSCOPY: THE POTENTIAL FOR LESS INVASIVE<br />
SURGICAL INTERACTIONS BETWEEN LAPAROSCOPES AND<br />
INTRALUMENAL ENTEROSCOPES Per-Ola Park, MD PhD, Maria<br />
Bergstrom, MD PhD, Margherita Cadeddu, MD, Paul Swain, MD, Dept of<br />
Surgery, South Alvsborg Hospital, Boras, Sweden and Department of<br />
Surgical Oncology and Technology, Imperial College, London, United<br />
Kingdom<br />
P258 TRANSVAGINAL MA-NOS. CLINICAL EXPERIENCE IN MORBID<br />
OBESITY AND COLON CANCER S. Delgado, A. Ibarzabal, R. Corcelles, F.<br />
Higuera, N. Salgado, A.M. Lacy, Gastrointestinal Surgery Unit. Hospital<br />
Clínic. ICMDM. Barcelona.
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P259 SELF EXPANDING METAL STENTS FOR COMPLICATIONS OF<br />
RYGB: DO THE BENEFITS JUSTIFY THE RISKS? K Chinnappan, MD, M<br />
S Jean, MD, M Cavaretta, MD, J D Gabrielsen, MD FACS, A T Petrick, MD<br />
FACS, Geisinger Medical Center, Danville, PA, USA<br />
P260 AN EXPERIMENTAL STUDY OF THE EFFICACY OF NEW FLEXIBLE<br />
BIPOLAR FORCEPS (BELA) FOR HEMOSTASIS AND CYSTIC DUCT<br />
CLOSURE DURING CHOLECYSECTOMY Per-Ola Park, MD PhD, Asghar<br />
Azadani, MD, Henrik Jonsson, MD, Paul Swain, MD, Maria Bergstrom,<br />
MD PhD, Dept of Surgery, South Alvsborg Hospital, Boras, Sweden and<br />
Department of Surgery, Sahlgrenska University Hospital, Gothenburg,<br />
Sweden, and Department of Surgical Oncology and Technology,<br />
Imperial College, London, United Kingdom<br />
P261 RANDOMIZED STUDY COMPARING HEMODYNAMIC AND<br />
PULMONARY EFFECTS OF TRANSGASTRIC ENDOSCOPIC SURGERY<br />
WITH THE INSUFLATION OF CO2 AND AIR. A. Ibarzabal, B. Escobar, P.<br />
Taura, S. Delgado, N. Salgado, J. Mercadal, A. Alzaga, J. Rojas, A.M. Lacy,<br />
Gastrointestinal Surgery Unit. ICMDM. Hospital Clinic. Barcelona<br />
P262 RADICAL TRANSANAL ENDOSCOPIC MICROSURGEY (TEM):<br />
ENDOLUMINAL SURGERY FOR COMPLEX RECTAL LESIONS John<br />
Marks, MD, Rahila Essani, MD, Yusef Kudsi, MD, Eileen Larkin, BA,<br />
Lankenau Hospital and Institute for Medical Research: Section of<br />
Colorectal Surgery, Wynnewood, PA<br />
P263 SLEEVE GASTRECTOMY: COMPARISON BETWEEN NOTES, SINGLE<br />
PORT AND LAPAROSCOPIC APPROACH. INITIAL EXPERIENCE. A.<br />
Ibarzabal, S. Delgado, R. Corcelles, A.M. Lacy, Gastrointestinal Surgery<br />
Unit. ICMDM. Hospital Clinic. Barcelona.<br />
P264 ANTIREFLUX TRANSORAL INCISIONLESS FUNDOPLICATION<br />
USING ESOPHYX: THE NEW YORK EVIDENCE Shankar R Raman, MD<br />
MRCS, V Kella, Shawn Garber, MD FACS, Spencer Holover, MD FACS,<br />
John M Cosgrove, MD FACS, Bronx-Lebanon Hospital Center and Mercy<br />
Medical Center<br />
P265 LAPAROENDOSCOPIC SINGLE-SITE (LESS) CHOLECYSTECTOMY:<br />
RESULTS OF A PILOT RANDOMIZED TRIAL Marco Maria Lirici, MD,<br />
Francesco Corcione, MD, Andrea Domenico Califano, MD, B-M-M<br />
Hospital dpt. General and Thoracic Suregery - Reggio Calabria - Italy<br />
P266 NATURAL ORIFICE SURGERY: INITIAL BRAZILIAN EXPERIENCE<br />
UTILIZING THE STOMAPHYXTM DEVICE TO REDUCE GASTRIC<br />
POUCHES AND GASTROJEJUNOSTOMY ANASTOMOSIS (STOMA)<br />
AFTER ROUX-EN-Y GASTRIC BYPASS Sergio Roll, MD PhD, Marco A<br />
D`Assunção, MD, Bariatric Center Germany Hospital Oswaldo Cruz<br />
P267 EXPANDABLE GASTRIC PORT (EGP) FOR NOTES Kiyoshi Hashiba,<br />
MD PhD, Pablo R Siqueira, MD, Sergio Roll, MD PhD, Marco A D’Assunção,<br />
MD, Hospital Sírio Libanês Endoscopic Unit. S.Paulo Brazil.<br />
P268 ENDOLUMINAL FUNDOPLICATION (EFL) FOR THE TREATMENT<br />
OF GERD – FEASIBILITY STUDY OF A NEW TECHNIQUE IN PIGS.<br />
Sergio Roll, MD PhD, kiyoshi Hashiba, MD PhD, Pablo R Siqueira, MD,<br />
Marco A D`Assunção, MD, Hospital Sírio Libanês Endoscopic Unit.<br />
S.Paulo Brazil<br />
P269 NEW PLATFORM FOR A HYBRID N.O.T.E.S.TRANS-VAGINAL<br />
SLEEVE GASTRECTOMY Stephan R Myers, MD FACS, Riverside<br />
Methodist Hospital<br />
P270 COMBINING SINGLE INCISION LAPAROSCOPY AND NOTES<br />
TO MINIMIZE TRAUMA FOR ADVANCED PROCEDURES: GASTRIC<br />
BYPASS IN A PORCINE MODEL Monika E Hagen, MD MBA, Oliver<br />
J Wagner, Philippe Morel, MD PhD, Kari J Thompson, MD, Santiago<br />
Horgan, MD, Paul C Swain, Center for the Future of Surgery, Department<br />
of Surgery, University of California San Diego & Division of Digestive<br />
Surgery, University Hospital Geneva & Imperial College London<br />
P271 AN EX VIVO BACTERIOLOGIC STUDY COMPARING ANTISEPTIC<br />
TECHNIQUES FOR NATURAL ORIFICE TRANSLUMENAL ENDOSCOPIC<br />
SURGERY (NOTES) VIA THE GASTROINTESTINAL TRACT Marvin Ryou,<br />
MD, Ronen Hazan, PhD, Laurence Rahme, PhD, Christopher C Thompson,<br />
MD MSc FACG FASGE, Brigham and Women’s Hospital, Boston, MA, USA<br />
and Massachusetts General Hospital, Boston, MA, USA<br />
P272 EVALUATION OF COMMERCIALLY AVAILABLE PORT ACCESS<br />
DEVICES FOR SINGLE INCISION LAPAROSCOPIC SURGERY Daniel<br />
A Cusati, MD, Michael L Kendrick, MD, James M Swain, MD, Juliane<br />
Bingener, MD, Mayo Clinic Rochester<br />
P273 GALLBLADDER RETRACTION WITHOUT TRANSCUTANEOUS<br />
SUTURES DURING SINGLE-INCISION LAPAROSCOPIC<br />
CHOLECYSTECTOMY Eugene Rubach, MD FACS, Joanne McDevitt,<br />
RPAC, George DeNoto, MD FACS, Gary R Gecelter, MD FACS, St. Francis<br />
Hospital, Roslyn, NY; North Shore University Hospital, Manhasset, NY<br />
P274 OPTIMAL DESIGN OF INSTRUMENTS FOR SINGLE PORT<br />
LAPAROSCOPIC SURGERY USING MOTION ANALYSIS Yogesh V<br />
Kolwadkar, MD MCh Orth, Stuart I Brown, PhD, Rami J Abboud, Prof,<br />
Alfred Cuschieri, Prof Sir, Weijie Wang, PhD, University of Dundee<br />
P275 ERGONOMIC PERFORMANCE WITH CROSSED AND UNCROSSED<br />
INSTRUMENTS IN SINGLE PORT LAPAROSCOPIC SURGERY Roberto<br />
Rimonda, MD, Benjie Tang, MD, Stuart I Brown, PhD, Alfred Cuschieri,<br />
Prof, University of Dundee<br />
P276 GOING BACK TO OPEN TECHNIQUE ( FUNDUS FIRST ) SINGLE<br />
INCISION LAPAROSCOPIC CHOLECYSTECTOMY Shailesh P<br />
Puntambekar, MS, Galaxy-CARE Laparoscopy Institute<br />
P277 MANAGEMENT OF THE ULTRASONICALLY ACTIVATED SCALPEL<br />
HANDPIECE WITH SELF-CHECK “BME MODE”. Minoru Ishida(1), BA,<br />
Keisuke Kimura(1), Takashi Saitoh(1), Yuma Ebihara(2), MD PhD, Shunichi<br />
Okushiba(2), MD PhD, Hiroyuki Katoh(2), MD PhD, Tsukasa Iwakura(3),<br />
BA, (1)Department of Clinical Engineering KKR Sappro Medical Center<br />
Tonan Hospital Japan (2)Department of Surgery KKR Sappro Medical<br />
Center Tonan Hospital Japan (3)Department of Clinical Engineering<br />
Nikko kinen Hospital Japan<br />
P278 SINGLE-INCISION LAPAROSCOPIC CHOLECYSTECTOMY IN<br />
MODIFIED LITHOTOMY POSITION – IMPROVED ERGONOMICS FOR<br />
SURGEONS AND SURGICAL ASSISTANTS Eugene Rubach, MD FACS,<br />
Joanne McDevitt, RPAC, Vikraman Gunabushanam, MD, Nitin Mishra,<br />
MD, George DeNoto, MD FACS, Gary R Gecelter, MD FACS, St. Francis<br />
Hospital, Roslyn, NY; North Shore University Hospital, Manhasset, NY<br />
P279 SINGLE PORT ACCESS SURGERY: PERFORMANCE DIFFICULTY<br />
AND A POSSIBLE SOLUTION Zheng Bin, MD PhD, Thamer Al-Tayeb, MD,<br />
Young Sang Sohn, MD, Karim A Qayumi, MD PhD, Adam T Meneghetti,<br />
MD, Neely M Panton, MD, University of British Columbia<br />
P280 A NEW MULTI-VIEW (MV) RIGID LAPAROSCOPE Harmik J<br />
Soukiasian, MD, Edward H Phillips, MD FACS, Aydin H Pooli, MD, Toshiko<br />
Nobuto, MD, George Berci, MD FACS FRCS, Department of Surgery,<br />
Cedars-Sinai Medical Center, Los Angeles, CA<br />
P281 A COMPARISON OF INDEPENDENCE OF MOTION IN SINGLE PORT<br />
ACCESS TECHNIQUES Erica R Podolsky, MD, Paul G Curcillo, II MD FACS,<br />
Drexel University, College of Medicine, Department of Surgery<br />
P282 EFFECTS OF DIFFERENT TYPES OF STAPLE LINE<br />
REINFORCEMENT ON TISSUE HANDLING AND SLIPPAGE DURING<br />
LAPAROSCOPIC STAPLING Eric T Volckmann, MD, Ozgur Firat, MD, Nilay<br />
R Shah, MD, Dean J Mikami, MD, Clinton R Hall, MD, Vanchad R Memark,<br />
Bradley J Needleman, MD, Center for Minimally Invasive Surgery,<br />
Division of Gastrointestinal Surgery, The Ohio State University Medical<br />
Center, Columbus, Ohio, USA<br />
P283 APPLICATION OF HEM-O-LOK CLIP IN BASIC LAPAROSCOPIC<br />
PROCEDURES: A SINGLE CENTER EXPERIENCE ON 856 CASES AND<br />
REVIEW OF DATA FROM FOOD AND DRUG ADMINISTRATION Ali<br />
Aminian, MD, Faramarz Karimian, MD, Karamollah Toolabi, MD, Rasoul<br />
Mirsharifi, MD, Department of Surgery, Tehran University of Medical<br />
Sciences, Tehran, Iran<br />
P284 FIRST HUMAN EXPERIENCE WITH A NOVEL LAPAROSCOPIC<br />
PORT SITE CLOSURE DEVICE Bilal M Shafi, MD MSE, Scott Perryman,<br />
MD, Eric Thorsell, MSE, Gabriel Sanchez, MSE, Carlos Mery, MD MPH,<br />
Thomas Krummel, MD, John Morton, MD, Department of Surgery,<br />
Stanford University, Stanford, CA, Department of Surgery, University of<br />
Pennsylvania, Philadelphia, PA<br />
12 th World Congress of Endoscopic Surgery<br />
167 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P285 ESOPHAGECTOMY FOR ADENOCARCINOMA: COMPARISON OF<br />
MINIMALLY INVASIVE, TRANSHIATAL AND EN BLOC RESECTION<br />
TECHNIQUES Joerg Zehetner, MD, Steven R DeMeester, MD, Shahin<br />
Ayazi, MD, Patrick Kilday, MS, Florian Augustin, MD, Helen J Sohn,<br />
MD, John C Lipham, MD, Jeffrey A Hagen, MD, Tom R DeMeester, MD,<br />
Department of Surgery, University of Southern California<br />
P286 ENDOSCOPIC CLOSURE OF AN ESOPHAGOCUTANEOUS FISTULA<br />
USING A BIOABSORBABLE MATERIAL AND TISSUE GLUE Lonnie W<br />
Frei, MD, University of Mississippi Medical Center<br />
P287 OBESITY DOES NOT INCREASE OPERATIVE MORBIDITY FOR<br />
ESOPHAGEAL RESECTION Brittany L Willer, Stephanie G Worrell, MD,<br />
Sumeet K Mittal, MD, Seemal Mumtaz, MD, Creighton University Medical<br />
Center<br />
P288 TREATMENT CHOICES AND OUTCOMES OF PATIENTS WITH<br />
MANOMETRICALLY DIAGNOSED ACHALASIA Christian J Finley, MD<br />
MPH, Linda Miller, RN, Urbach David, MD MSc, Lorenzo Ferri, MD PhD,<br />
Gail Darling, MD, Division of Thoracic Surgery, Toronto General Hospital<br />
P289 COMPARISON OF THE EFFECT OF OBESITY ON LAPAROSCOPY-<br />
ASSISTED DISTAL GASTRECTOMY WITH THAT ON OPEN DISTAL<br />
GASTRECTOMY Hideki Kawamura, MD, Ryoichi Yokota, MD,<br />
Department of Surgery, JA Sapporo Kosei Hospital<br />
P290 A NOVEL LAPAROSCOPIC COMPRESSION ANASTOMOSIS CLIP<br />
(LAPCAC) FOR LAPAROSCOPIC GASTROENTEROANASTOMOSIS:<br />
Xinxiang Li, MD, Chengzhu Zheng, MD, Raul J Rosenthal, MD, Kai<br />
Yin, MD, Department of Colorectal Surgery, Fudan University Cancer<br />
Hospital<br />
P291 LAPAROSCOPIC SLEEVE RESECTION FOR NON-CANCEROUS<br />
GASTRIC TUMORS Gadiyaram Srikanth, MCh, Neel Shetty, MS, TLVD<br />
Prasad Babu, MCh, Sadiq S Sikora, MS, Manipal Institute of Liver and<br />
Digestive Diseases<br />
P292 POSTERIOR VAGUS NERVE WITHIN OR OUTSIDE NISSEN<br />
FUNDOPLICATION: DOES IT MATTER? Kazuto Tsuboi, MD, András<br />
Legner, MD, Tommy H Lee, MD, Fumiaki Yano, MD, Sumeet K Mittal, MD,<br />
Department of Surgery, Creighton University Medical Center, Omaha,<br />
Nebraska<br />
P293 DOES METASTATIC LYMPH NODE RATIO ACCEPT AS<br />
A PROGNOSTIC FACTOR IN THE PATIENTS UNDERWENT<br />
LYMPHADENECTOMY WITH LESS THAN 15 LYMPH NODES FOR<br />
GASTRIC CANCER? Sezai Demirbas, MD, Ilker Sucullu, MD, Ali I Filiz, MD,<br />
Mustafa T Ozer, MD, Kagan Coskun, MD, Nail Ersoz, MD, Gulhane Mil.<br />
Medical Academy (GMMA)<br />
P294 OUTCOMES OF LAPAROSCOPIC SURGERY FOR ESOPHAGEAL<br />
ACHALASIA IN 200 PATIENTS Fumiaki Yano, MD PhD, Nobuo Omura,<br />
MD PhD, Kazuto Tsuboi, MD, Masato Hoshino, MD, Seryon Yamamoto,<br />
MD, Syunsuke Akimoto, MD, Hideyuki Kashiwagi, MD PhD, Katsuhiko<br />
Yanaga, MD PhD, Department of Surgery, Jikei University School of<br />
Medicine, Tokyo, Japan<br />
P295 LAPAROSCOPIC TREATMENT OF A UNIQUE CASE OF LARGE<br />
SLIDING PARAESOPHAGEAL HIATAL HERNIA WITH INTRATHORACIC<br />
STOMACH AND ACHALASIA M R Jaber, MD, Ata Mazahiri, MD, Loma<br />
Linda University Medical Center<br />
P296 A PRELIMINARY STUDY ON PREOPERATIVE THREE-<br />
DIMENSIONAL SIMULATION USING MDCT FOR SINGLE PORT ACCESS<br />
SURGERY ON GIST Toshiyuki Natsume, MD PhD, Kiyohiko Shuto, MD<br />
PhD, Tsuguaki Kohno, MD PhD, Gaku Ohira, MD PhD, Takayuki Tohma,<br />
MD PhD, Asami Sato, MD PhD, Hiroshige Saito, MD, Takumi Ohta, MD,<br />
Hiroshi Kawahira, MD PhD, Takashi Akai, MD PhD, Yoshihiro Nabeya, MD<br />
PhD, Hide, Department of Frontier Surgery, Chiba University Graduate<br />
School of Medicine, Research Center for Frontier Medical Engineering,<br />
Chiba University<br />
P297 THORACOSCOPIC TOTAL OESOPHAGECTOMY Shailesh<br />
Puntambekar, MS, Galaxy-Care Laparoscopy Institute<br />
P298 MINIMALLY INVASIVE ESOPHAGECTOMY FOR CLINICAL<br />
EARLY STAGE ESOPHAGEAL SQUAMOUS CELL CARCINOMA:<br />
THORACOSCOPY COMPARED WITH MEDIASTINOSCOPY ASSISTED<br />
Lijie Tan, MD, Mingxiang Feng, MD, Qun Wang, MD, Division of Thoracic<br />
Surgery, Zhong Shan Hospital, Fu Dan University<br />
P299 MINIMALLY INVASIVE ESOPHAGECTOMY FOR ESOPHAGEAL<br />
CANCER VERSUS OPEN THORACOABDOMINAL ESOPHAGECTOMY<br />
Hiroyuki Kitagawa, Michiya Kobayashi, Tsutomu Namikawa, Kochi<br />
Medical School<br />
P300 INITIAL OUTCOME OF LAPAROSCOPIC NISSEN<br />
FUNDOPLICATION: THAILAND EXPERIENCE Chadin Tharavej,<br />
MD, Patpong Navicharoen, MD, Poochong Timratana, MD, Suppa-at<br />
Pungpapong, MD, Suthep Udomsaweangsup, MD, Department of<br />
Surgery, Chulalongkorn University, Bangkok THAILAND<br />
P301 Withdrawn.<br />
P302 THE IMPACFT OF OBESITY AND HIATAL HERNIA ON THE LONG<br />
TERM RESULT OF LAPAROSCOPIC HELLER MYOTOMY Fawzi S Khayat,<br />
MD, Patricia Sylla, MD, David W Rattner, MD, Massachusetts General<br />
Hospital<br />
P303 TRANSORAL ESOPHAGO-GASTRIC PARTIAL FUNDOPLICATION<br />
FOR THE TREATMENT OF GASTROESOPHAGEAL REFLUX DISEASE<br />
(GERD): OPERATIVE FINDINGS AND SAFETY Reginald Bell, MD, Kate<br />
Freeman, NP MSN, Swedish Medical Center, Englewood CO<br />
P304 PERIOPERATIVE OUTCOMES OF SURGICAL PROCEDURES FOR<br />
RECURRENT GERD FOLLOWING NISSEN FUNDOPLICATION Sandeepa<br />
Musunuru, MD, Jon Gould, MD, University of Wisconsin School of<br />
Medicine and Public Health<br />
P305 OUTCOMES FOLLOWING LAPAROSCOPIC VS. ROBOTIC HELLER<br />
MYOTOMY Sandeepa Musunuru, MD, Jon Gould, MD, University of<br />
Wisconsin School of Medicine and Public Health<br />
P306 IDENTIFICATION OF RISK FACTORS FOR POST-OPERATIVE<br />
DYSPHAGIA AFTER LAPAROSCOPIC PRIMARY ANTI-REFLUX<br />
SURGERY Kazuto Tsuboi, MD, András Legner, MD, Tommy H Lee, MD,<br />
Fumiaki Yano, MD, Xiang Fang, PhD, Sumeet K Mittal, MD, Department<br />
of Surgery, Creighton University Medical Center, Omaha, Nebraska,<br />
Research and Compliance, Creighton University, Omaha, Nebraska<br />
P307 INTERSTITIAL LUNG DISEASE AND GASTROESOPHAGEAL<br />
REFLUX DISEASE: KEY ROLE OF ESOPHAGEAL FUNCTION TESTS<br />
IN THE DIAGNOSIS AND TREATMENT. Renato V Soares, MD, Anne<br />
Forsythe, RN, Kyle Hogarth, MD, Nadera Sweiss, MD, Irme Noth, MD,<br />
Marco G Patti, MD, University of Chicago<br />
P308 THE TRAINING OF OPERATING SURGEON IN LAPAROSCOPIC<br />
ASSISTED DISATAL GASTRECTOMY Kazuyoshi Yamamoto, MD,<br />
Shuji Takiguchi, MD PhD, Yuichiro Hiura, MD, Makoto Yamasaki, MD<br />
PhD, Hiroshi Miyata, MD PhD, Kiyokazu Nakajima, MD PhD, Yoshiyuki<br />
Fujiwara, MD PhD, Masaki Mori, MD PhD, Yuichiro Doki, MD PhD,<br />
Division of Gastroenterological Surgery, Department of Surgery,<br />
Graduate School of Medicine, Osaka University, Osaka, Japan<br />
P309 FEASIBILITY OF LAPAROSCOPIC DISTAL GASTRECTOMY FOR<br />
NON-CURATIVE GASTRIC CANCER FOLLOWING ENDOSCOPIC<br />
SUBMUCOSAL DISSECTION Yuma Ebihara, PhD, Shunichi Okushiba,<br />
PhD, Daisuke Miyasaka, PhD, Takeshi Sasaki, PhD, You Kawarada, PhD,<br />
Shuji Kitashiro, PhD, Hiroyuki Katoh, PhD, Department of Surgery, Tonan<br />
Hospital<br />
P310 CORRELATION BETWEEN INTRAOPERATIVE AND<br />
POSTOPERATIVE EVALUATION OF THE GASTRIC TUBE VIABLITY IN<br />
ESOPHAGECTOMY Katsunori Nishikawa, MD, Nobuyoshi Hanyuu, MD,<br />
Yujirou Tanaka, MD, Akira Matsumoto, MD, Yuichiro Tanishima, MD,<br />
Fumiaki Yano, MD, Hideyuki Kashiwagi, MD, Katsuhiko Yanaga, MD, Jikei<br />
University Department of Surgery<br />
12 th World Congress of Endoscopic Surgery 168
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P311 LAPAROSCOPIC GASTRECTOMY WITH D2 LYMPHADECTOMY<br />
FOR GASTRIC CANCER: IS IT STILL TIME-CONSUMING? Jun Yan,<br />
MD, Changhua Zhuo, MD, Yu Yao, MD, Hui Yu, MD, Weidong Zang, MD,<br />
Mingang Ying, MD, Fujian Provincial Tumor Hospital, Fuzhou, 350014,<br />
China<br />
P312 THE M,ANAGEMENT OF GASTROESOPHAGEAL REFLUX<br />
DISEASE-RELATED PULMONARY SYMPTOMS BY LAPAROSCOPIC<br />
FUNDOPLICATION Zhong-Gao Wang, MD, Ji Feng, MD, Ji-min Wu, MD,<br />
Yun-Gang Lai, MD, Xiang Gao, MD, Xiu Chen, MD, Herbert Dardik, MD,<br />
Ibrahim M Ibrahim, MD, Center for GERD of Er Pao General Hospital,<br />
Beijing, China and Englewood Hospital & Medical Center, Englewood, NJ<br />
P313 LUNG TRANSPLANT CANDIDATES MAY BENEFIT FROM ANTI-<br />
REFLUX SURGERY; DEMONSTRATON OF GASTROESOPHAGEAL<br />
REFLUX (GERD), ESOPHAGEAL MOTILITY DISORDERS AND<br />
ANATOMIC ABNORMALITIES IN THIS POPULATION Harmik J<br />
Soukiasian, MD, Jaclyn T Parker, MD, Edward H Phillips, MD FACS, Robert<br />
Tabrizi, MD, Sinan A Simsir, MD, Jeffrey L Conklin, MD, Esophageal And<br />
Thoracic/Foregut Surgery <strong>Program</strong>, Cedars – Sinai Medical Center. Los<br />
Angeles, CA<br />
P314 OVERCOMING BARRIERS TO DEVELOPMENT OF A MINIMALLY<br />
INVASIVE ESOPHAGECTOMY PROGRAM Kfir Ben-David, MD, Nicole A<br />
Kissane, MD, Georgios Rossidis, MD, Stephen R Grobmyer, MD, Juan C<br />
Cendan, MD, George A Sarosi, MD, Steven N Hochwald, MD, University of<br />
Florida College of Medicine. Gainesville, Florida.<br />
P315 HYBRID ESOPHAGECTOMY FOR ESOPHAGEAL CANCER:<br />
COMBINED THORACOSCOPIC AND MEDIASTINOSCOPIC<br />
ESOPHAGECTOMY. Y Izumi, PhD, A Miura, PhD, T Kato, MD, T Ryotokuji,<br />
MD, Tokyo Metropolitan Cancer and Infectious Disease Center,<br />
Komagome Hospital, Tokyo, Japan<br />
P316 LAPAROSCOPIC MANAGEMENT OF GASTROINTESTINAL<br />
STROMAL TUMOURS AT A CANADIAN INSTITUTION Jasmine C Lam,<br />
MD, Adam T Meneghetti, MD, Ormond N Panton, MD, University of<br />
British Columbia<br />
P317 LOWER LEVELS OF OCCASIONAL BLOOD GLUCOSE IN PATIENTS<br />
WITH BILLROTH I RECONSTRUCTION AFTER NOT VAGUS NERVE-<br />
SPARED LAPAROSCOY-ASSISTED DISTAL GASTRECTOMY. Hiroshi<br />
Kawahira, MD, Hideki Hayashi, MD, Toshiyuki Natsume, MD, Yoshihiro<br />
Nabeya, MD, Takashi Akai, MD, Hisahiro Matsubara, MD, Department of<br />
Frontier Surgery, Chiba University Graduate School of Medicine<br />
P318 EFFECTS OF EARLY ORAL FEEDING ON SURGICAL OUTCOMES<br />
AND RECOVERY AFTER LAPAROSCOPY-ASSISTED DISTAL<br />
GASTRECTOMY FOR EARLY GASTRIC CANCER: A NONRANDOMIZED<br />
STUDY. Shinya Asami, Hitoshi Idani, Hiroshi Sasaki, Kenjirou Kumano,<br />
Youhei Kurose, Shinichirou Kubo, Hiroki Nojima, Kanyu Nakano, Takashi<br />
Yoshioka, Masahiko Muro, Hitoshi Kin, Norihisa Takakura, Department of<br />
surgery, Fukuyama city hospital, Hiroshima, Japan<br />
P319 ESOPHAGO-GASTROSTOMY USING NARROW GASTRIC TUBE<br />
AFTER LAPAROSCOPY-ASSISTED PROXIMAL GASTRECTOMY Kenoki<br />
Ohuchida, MD PhD, Eishi Nagai, MD PhD, Kohei Nakata, MD PhD, Hideki<br />
Takanami, MD, Takao Ohtsuka, MD PhD, Hiroki Toma, MD PhD, Masao<br />
Tanaka, MD PhD FACS, Department of Surgery and Oncology, Kyushu<br />
University<br />
P320 LAPAROSCOPIC MANAGEMENT OF GASTRIC GIST Mohan<br />
Narasimhan, Kumar Palaniappan, Ramesh Ardhanari, Department of<br />
Surgery and Gastroenterology, Meenakshi Mission Hospital & Research<br />
Center, Madurai<br />
P321 COST COMPARISON OF LAPAROSCOPIC V/S OPEN<br />
GASTRECTOMY IN THE TREATMENT OF GASTRIC CANCER Pablo<br />
Becerra, MD, Ricardo Yañez, MD, Sergio Guzman, MD, Luis Ibanez, MD,<br />
Ricardo Funke, MD, Cristian Alvear, Alex Escalona, MD, Department of<br />
Digestive Surgery. Pontificia Universidad Católica de Chile<br />
P322 THE ROLE OF ENDOSCOPIC ULTRASOUND IN ASSESSING TUMOR<br />
RESPONSE AND STAGING POST NEOADJUVANT CHEMOTHERAPY IN<br />
ESOPHAGEAL CANCER Subhasis Misra, MD MS, Mark W Choi, BS, Alan<br />
S Livingstone, MD, Dido Franceschi, MD, Division of Surgical Oncology,<br />
Sylvester Comprehensive Cancer Center, University of Miami<br />
P323 SINGLE PORT ACCESS PARTIAL GASTRECTOMY FOR GASTRIC<br />
GIST. Ken Hagiwara, MD, Minoru Matsuda, MD FACS, Motoo Yamagata,<br />
MD, Shigeoki Hayashi, MD, Tadatoshi Takayama, MD, Division of<br />
digestive surgery, Nihon University School of medicine<br />
P324 ESOPHAGEAL RECONSTRUCTION USING BIOLOGICAL<br />
SCAFFOLDS IN A CLINICAL SETTING. Toshitaka Hoppo, MD PhD, Bart<br />
Witteman, MD, Adolfo E Badaloni, MD, Ricardo Casella, MD, Alejandro F<br />
Sanz, MD, Stephen F Badylak, DVM PhD MD, Blair A Jobe, MD, Alejandro<br />
Nieponice, MD, 1) Esophageal Surgery Institute, Fundacion Favaloro,<br />
Buenos Aires, Argentina. 2) The Heart, Lung and Esophageal Institute 3)<br />
McGowan Institute for Regenerative Medicine, University of Pittsburgh<br />
Medical Center, Pittsburgh, PA USA<br />
P325 ESD-ASSISTED LAPAROSCOPIC PARTIAL GASTRECTOMY<br />
FOR GASTRIC SUBMUCOSAL TUMOR Takashi Ogata, Hidenori<br />
Tomioka, Yusuke Murakoshi, So Katayanagi, Motohide Shimazu,<br />
Gastroenterological Surgery, Hachioji Medical Center, Tokyo Medical<br />
University, Tokyo, Japan<br />
P326 PARAESOPHAGEAL HIATAL HERNIA REPAIR USING GORE<br />
BIO-A TISSUE REINFORCEMENT, ONE YEAR FOLLOW UP DATA<br />
James M Massullo, MD, Tejinder P Singh, MD, Brian Binetti, MD, Ward<br />
Dunnican, MD, Albany Medical Center<br />
P327 LAPAROSCOPIC PARAESOPHAGEAL HERNIA REPAIR WITH<br />
HUMAN ACELLULAR DERMAL MATRIX CRUROPLASTY Dennis F Diaz,<br />
MD, John Scott Roth, MD, University of Kentucky Chandler Medical<br />
Center<br />
P328 LAPAROSCOPIC GASTROJEJUNOSTOMY FOR MALIGNANT<br />
GASTRIC OUTLET OBSTRUCTION. Norihito Wada, MD PhD, Yoshiro<br />
Saikawa, MD PhD, Rieko Nakamura, MD PhD, Takashi Ohyama, MD,<br />
Tsunehiro Takahashi, MD PhD, Hiroya Takeuchi, MD PhD, Yuko Kitagawa,<br />
MD PhD, Department of Surgery, School of Medicine, Keio University<br />
P329 STANDARDIZATION OF VIDEO-ASSISTED ESOPHAGECTOMY:<br />
HAND-ASSISTED THORACOSCOPIC SURGERY AS A SAFETY<br />
PROCEDURE Toshiaki Shichinohe, MD PhD, Shunichi Okushiba, MD PhD,<br />
You Kawarada, MD PhD, Shuji Kitashiro, MD PhD, Hiroto Manase, MD PhD,<br />
Kentaro Kato, MD PhD, Takahiro Tsuchikawa, MD PhD, Joe Matsumoto, MD<br />
PhD, Ryosuke Kawasaki, MD PhD, Eiichi Tanaka, MD PhD, Satosh, Surgical<br />
Oncology, Hokkaido University Graduate School of Medicine, Tonan<br />
Hospital, Asahikawa Redcross Hospital, Hokkaido, Japan<br />
P330 MEDIASTINOSCOPIC TRANSHIATAL ESOPHAGECTOMY FOR<br />
AN AGED PERSON WITH TYPE 4 THORACIC ESOPHAGEAL CANCER:<br />
REPORT OF A CASE T Ryotokuji, MD, Y Izumi, PhD, A Miura, PhD, T Kato,<br />
MD, K Ogawa, MD, okyo Metropolitan Cancer and Infectious Diseases<br />
Center, Komagome Hospital, Tokyo, JAPAN<br />
P331 COMPARATION BETWEEN LAPAROSCOPY ASSISTED<br />
GASTRECTOMY D2 LYMHP NODE DISSECTION AND OPEN<br />
PROCEDURE FOR GASTRIC CANCER IN COLOMBIA Jorge Alberto<br />
Bernal Mesa, Dr, Evelyn Astrid Dorado Alban, Dr Fellowship, Mario<br />
muñoz, Dr, Las Americas Oncology Institute<br />
P332 TRANASVAGINAL SPECIMEN EXTRACTION AFTER TOTALLY<br />
LAPAROSCOPIC SUBTOTAL GASTRECTOMY IN EARLY GASTRIC<br />
CANCER Young-Joon Lee, PhD, Sang-Ho Jeong, MD, Won-Joon Choi,<br />
PhD, Soon-Tae Park, PhD, Sang-Kyung Choi, PhD, Soon-Chan Hong, PhD,<br />
Young-tae Joo, PhD, Chi-Young Jeong, MD, Hyeong-Gon Moon, MD,<br />
Woo-Song Ha, PhD, Department of Surgery, Department of Obstetrics<br />
and Gynecology, Gyeongsang National University Hospital, Gyeongnam<br />
Regional Cancer Center,Gyeongsang Institute of Health Sciences, Jinju,<br />
South Korea.<br />
12 th World Congress of Endoscopic Surgery<br />
169 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P333 THE SAFETY OF BIOLOGIC MESH FOR LAPAROSCOPIC REPAIR<br />
OF LARGE, COMPLICATED HIATAL HERNIA Eelco Wassenaar, MD, Saad<br />
Shebrain, MD, Huseyin Sinan, MD, Valeria Martin, MD, Carlos Pellegrini,<br />
MD, Brant Oelschlager, MD, Center for Videoendoscopic Surgery,<br />
Department of Surgery, University of Washington<br />
P334 THE RISK OF COMBINED ORGAN RESECTION IN RADICAL<br />
GASTRECTOMY Sang-Ho Jeong, MD, Young-Joon Lee, PhD, Soon-Tae<br />
Park, PhD, Sang-Kyung Choi, PhD, Soon-Chan Hong, PhD, Young-tae<br />
Joo, PhD, Chi-Young Jeong, MD, Hyeong-Gon Moon, MD, Woo-Song Ha,<br />
PhD, Department Surgery of Gyeongsang National University Hospital,<br />
Gyeongnam Regional Cancer Center, Gyeongsang Institue of Health<br />
Sciences, Jinju, South Korea<br />
P335 DISTAL GASTRECTOMY WITH LAPAROSCOPIC ASSISTANCE FOR<br />
NON-OVERWEIGHT PATIENTS WITH T1N0 GASTRIC CANCER Hideyuki<br />
Ishida, PhD, Toru Ishiguro, MD, Norimichi Okada, PhD, Keiichiro Ishibashi,<br />
PhD, Norihiro Haga, PhD, Department of Digestive Tract and General<br />
Surgery, Saitama Medical Center, Saitama Medical School<br />
P336 FACTORS OF INCREASING BLOOD LOSS AND OPERATION TIME<br />
IN LAPAROSCOPIC ASSISTED DISTAL GASTRECTOMY Hisae Aoki, MD,<br />
Osamu Yanagida, MD PhD, Gen Nagao, MD, Nobutsugu Abe, MD PhD,<br />
Tadahiko Masaki, MD PhD, Toshiyuki Mori, MD PhD, Masanori Sugiyama,<br />
MD PhD, Yutaka Atomi, MD PhD, Kyorin University, School of Medicine<br />
P337 TOTALLY LAPAROSCOPIC TOTAL GASTRECTOMY WITH<br />
ESOPHAGOJEJUNOSTOMY USING LINER STAPLING DEVICES. Eishi<br />
nagai, MD PhD, Hiroki Toma, MD PhD, Kenoki Ouchida, MD PhD, Kohei<br />
Nakata, MD, Takao Otsuka, MD PhD, Shuji Shimizu, MD PhD, Masao<br />
Tanaka, MD PhD, Department of Surgery and Oncology, Graduate<br />
School of Medical Sciences, Kyushu University<br />
P338 LAPAROSCOPIC TRANSHIATAL APPROACH FOR SQUAMOUS<br />
CELL CARCINOMA OF THE LOWER THIRD OF THE ESOPHAGUS<br />
A Miura, PhD, Y Izumi, PhD, T Kato, MD, T Ryotokuji, MD, Tokyo<br />
Metropolitan Cancer and Infectious Disease Center, Komagome<br />
Hospital, Tokyo, Japan<br />
P339 TECHNIQUES OF ROUX-EN Y RECONSTRUCTION USING<br />
REVERSED RHO-SHAPED SIDE-TO-SIDE ESOPHAGO-JEJUNOSTOMY<br />
IN LAPAROSCOPY-ASSISTED TOTAL GASTRECTOMY (LATG) Norio<br />
Shiraishi, MD, Tyuyoshi Etoh, MD, Kazuhiro Yasuda, MD, Masafumi<br />
Inomata, MD, Seigo Kitano, MD, Department of Surgery I, Oita University<br />
Faculty of Medicine,<br />
P340 THE TOTAL NUMBER OF RESECTED LYMPH NODES HAS AN<br />
IMPACT ON SURVIVAL IN NODE-NEGATIVE ESOPHAGEAL CANCER<br />
Jacqui C. Zhu, MBBS, Guillemo Becerril, MBBS, Gregory L. Falk, MBBS,<br />
Deptartment of Upper Gastrointestinal Surgery and Endosurgery,<br />
Concord Hospital<br />
P341 LAPAROSCOPIC FUNDOPLICATION FOR GERD; EXPERIENCE<br />
FROM A TERTIARY CARE HOSPITAL IN INDIA. Pawanindra Lal, MD<br />
DNBFRCSEd FRCSGlasg, Nitin Leekha, MD, Rakesh Saini, MD, Jagdish<br />
Chander, MD, Vinod K Ramteke, MD, Department of Surgery, Maulana<br />
Azad Medical College, New Delhi, India<br />
P342 LAPAROSCOPIC FUNDOPLICATION FOR GASTRO-ESOPHAGEAL<br />
REFLUX DISEASE: A 10 YEAR EXPERIENCE Konstantinos Tsalis, Prof,<br />
Stavros Kalfadis, PhD, Konstantinos Blouhos, MD, Theofanis Maris, MD,<br />
Kyriakos Christodoulou, MD, Foteini Kordits, MD, Charalampos Lazaridis,<br />
Prof, D’ Surgical Department Aristotle University of Thessaloniki Greece<br />
P343 FEASIBILITY AND POST OPERATIVE OUTCOME OF MINIMALLY<br />
INVASIVE ESOPHAGECTOMY IN PATIENTS WHO RECEIVED<br />
NEOADJUVANT CHEMOTHERAPY FOR LOCALLY ADVANCED<br />
ESOPHAGEAL CANCER C Palanivelu, P Senthilnathan, MS DNB MRCS,<br />
V Vaithiswaran, MS MRCS, N Anand Vijai, MS, K.V Jaiganesh, MS, GEM<br />
Hospital<br />
P344 LYMPH NODE HARVEST IN MINIMALLY INVASIVE<br />
ESOPHAGECTOMY FOR ESOPHAGEAL CANCER C Palanivelu, MCh<br />
FACS FRCS, P S Rajan, MS FACS, S Rajapandian, MSFRCS, P Senthilnathan,<br />
MS DNB MRCS, R Rohit, MS, A.P Manoj Kumar, MS, V Vaithiswaran, MS<br />
MRCS, P Praveen Raj, MS, GEM Hospital<br />
P345 A NEW SYNTHETIC BIOABSORBABLE PROSTHETIC AND METHOD<br />
OF FIXATION FOR MESH REINFORCEMENT OF CRURAL CLOSURE<br />
DURING HIATAL HERNIA REPAIR Dan Wandrey, MD, Benjamin Powell,<br />
MD, Guy Voeller, MD, University of Tennessee Health Science Center,<br />
Memphis, TN<br />
P346 LAPAROSCOPIC GASTRECTOMY FOR CANCER Theodore Liakakos,<br />
MD, Evangelos P Misiakos, MD, Anastasios Macheras, MD, Dimitrios<br />
Bistarakis, MD, Paul Patapis, MD, Gabriel Karatzas, MD FACS, 3rd<br />
Department of Surgery-University of Athens School of Medicine<br />
P347 GASTRODUODENAL INTUSSUSCEPTION WITHOUT UNDERLYING<br />
MASS Matthew M Philp, MD, Daniel T Dempsey, MD, Colleen Gaughan,<br />
MD, Temple University Hospital<br />
P348 MINIMALLY INVASIVE ESOPHAGECTOMY IN A PATIENT WITH<br />
PORTAL HYPERTENSION. Scott J Keckler, MD, Colleen S Hupp, DO, Amit<br />
K Taggar, MD, Mazin F Al-kasspooles, MD, Niazy M Selim, MD MBChB<br />
PhD, University of Kansas Medical Center, Department of Surgery<br />
P349 ONCOLOGICAL ‘HOLY PLANE’ IN CHEST FOR OESOPHAGEAL<br />
CANCER RESECTION Amir Nisar, FRCSGlasg FRCSI FRCS, H Ali, John<br />
B Schofield, Regional Oesophago Gastric Cancer Unit, Maidstone and<br />
Tunbridge Wells Trust, Maidstone, Kent, England, United Kingdom<br />
P350 THREE “5MM” PORTS LAPAROSCOPIC NISSEN FUNDOPLICATION<br />
- THE LEAST INVASIVE SO FAR. Amir Nisar, FRCSGlag FRCSI FRCS, H Ali,<br />
U Bracale, Y Abdulaal, Oesophago Gastric Regional Unit, Maidstone and<br />
Tunbridge Wells Trust, Maidstone, Kent, England, United Kingdom<br />
P351 IMPACT OF A VISITING PRECEPTOR ON THE INSTITUTIONAL<br />
SURGICAL RESULTS OF LADG Shuji Takiguchi, MD, Yoshiyuki Fujiwara,<br />
MD, Makoto Yamasaki, MD, Hiroshi Miyata, MD, Kiyokazu Nakajima, MD,<br />
Mitsugu Sekimoto, MD, Masaki Mori, MD, Yuichiro Doki, MD, Osaka Univ.<br />
Dept. of Gastroenterological Surgery<br />
P352 HELLER’S MYOTOMY WITH RECONSTRUCTION OF THE<br />
ANGLE OF HIS IN ACHALASIA. IMPACT ON POSTOPERATIVE<br />
GASTROESOPHAGEAL REFLUX AND LES PRESSURE Juan F Molina,<br />
MD, Mauricio Sierra, MD, Federico López, MD, David Velázquez, MD PhD,<br />
Juan P Pantoja, MD, Miguel A Valdovinos, MD, Miguel F Herrera, MD PhD,<br />
Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán,<br />
Mexico City, Mexico<br />
P353 TOTALLY SUPINE LAPAROSCOPIC/THORACOSCOPIC IVOR LEWIS<br />
OESOPHAGECTOMY - A NOVEL TECHNIQUE Amir Nisar, FRCSGlasg<br />
FRCSI FRCS, Umberto Bracale, H Ali, Y Abdulaal, Oesophago Gastric<br />
Regional Unit, Maidstone and Tunbridge Wells Trust, Maidstone, Kent,<br />
England, United Kingdom<br />
P354 LAPAROSCOPIC REPAIR OF RECURRENT PARAESOPHAGEAL<br />
HERNIA: A RARE BUT SAFE PROCEDURE Marianne Franco, MD,<br />
Ariel Spencer, MD, Hien Nguyen, MD, Kimberley Steele, MD, Michael<br />
Schweitzer, MD, Michael Marohn, DO, Anne Lidor, MD MPH, Johns<br />
Hopkins Medical Institutions<br />
P355 LONG AND SHORT TERM RESULTS OF LESS INVASIVE SURGERY<br />
FOR STOMACH CANCER: LAPAROSCOPIC-ASSISTED DISTAL<br />
GASTRECTOMY WITH “SLIDING WINDOW METHOD (SWM)”.<br />
Takanobu Hoshino, MD PhD, Takashi Ishida, MD, Narihiro Cho, MD,<br />
Akio Odaka, MD PhD, Hashi Daijo, MD PhD, Saitama Medical University,<br />
Saitama Medical Center<br />
P356 GASTRIC DUPLICATION TREATED BY LAPAROSCOPIC GASTRIC<br />
PARTIAL RESECTION Yoo Shin Choi, MD, Beom Gyu Kim, MD, In Taik<br />
Chang, MD, Department of Surgery, College of Medicine, Chung-Ang<br />
University, Seoul, Korea<br />
P357 IMPROVEMENT AFTER LAPAROSCOPIC AND ENDOSCOPIC<br />
PYLOROPLASTY FOR GASTROPARESIS Michael L Hibbard, MD, Lee L<br />
Swanström, MD, Christy M Dunst, MD, The Oregon Clinic<br />
P358 TRANSORAL INCISIONLESS FUNDOPLICATION IMPROVES<br />
REFLUX SYMPTOMS IN LONG-TIME PPI USERS: A RETROSPECTIVE<br />
STUDY IN LIVINGSTON COUNTY, KENTUCKY William E Barnes, MD<br />
MBAFACS, Michael P Gavin, MD, Stephanie Mundy, RN, Livingston<br />
Hospital and Healthcare Services, Inc., Salem, KY<br />
12 th World Congress of Endoscopic Surgery 170
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P359 CLINICAL SIGNIFICANCE OF ENDOSCOPIC SURGERY FOR<br />
THORACIC ESOPHAGEAL CANCER AFTER NEOADJUVANT<br />
CHEMOTHERAPY Hiroki Toma, MD, Eishi Nagai, MD, Kenoki Ohuchida,<br />
MD, Takao Ohtsuka, MD, Shuji Shimizu, MD, Masao Tanaka, MD,<br />
Department of Surgery and Oncology<br />
P360 MINIMALLY INVASIVE ESOPHAGO- GASTRECTOMY (IVOR-<br />
LEWIS) A SERIES OF 13 PATIENTS C Palanivelu, MCh FRCS FACS, P<br />
Senthilnathan, MS DNB MRCS, V Vaithiswaran, MS MRCS, P Praveen Raj,<br />
MS, GEM hospital<br />
P361 MINIMALLY INVASIVE OESOPHAGECTOMY IN ENGLAND:<br />
TRENDS OF UTILISATION Kamal Nagpal, MD, Antonio Ivan Lazzarino,<br />
MD, Alex Bottle, PhD, Omar Faiz, FRCS, Krishna Moorthy, FRCS, Paul<br />
Aylin, FFPH, Department of Biosurgery and Surgical Technology,<br />
Imperial College, St Mary’s Hospital, Praed Street, London W21NY,<br />
United Kingdom.<br />
P362 LAPAROSCOPIC REVISIONAL FUNDOPLICATION WITH PRIMARY<br />
SUTURED CLOSURE AND PROSTHETIC REINFORCEMENT: A<br />
RETROSPECTIVE STUDY Sergio Roll, MD PhD, CEITEL - Center for<br />
Education, Inovation and Technology in EndoSurgery- Laparoscopy of<br />
Sao Paulo, Brazil.<br />
P363 LAPAROSCOPIC ANTI-REFLUX SURGERY AS A DEFINITIVE<br />
TREATMENT IN REFRACTORY UPPER AND LOWER RESPIRATORY<br />
TRACT DISEASES. A A Warsi, C P Armstrong, Bristol, U.K.<br />
P364 ESOPHAGEAL STENTING FOR IMMEDIATE PALLIATION OF<br />
SYMPTOMATIC THORACIC MALIGNANCIES Natasha M Rueth, MD,<br />
Darcy Shaw, MD, Shawn S Groth, MD, Jennifer Swanson, MD, Jonathan<br />
D’Cunha, MD PhD, Michael A Maddaus, MD, Rafael S Andrade, MD,<br />
University of Minnesota Department of Surgery, Division of Thoracic and<br />
Foregut Surgery, Minneapolis MN USA<br />
P365 ARE RURAL GENERAL SURGEONS PERFORMING VALID<br />
COLONOSCOPIES? Truman M Sasaki, MD FACS, Solo Practitioner<br />
P366 ENDOSCOPIC MANAGEMENT OF A RARE RIGHT COLON<br />
PERFORATION FROM A MIGRATED BILIARY STENT Logan Rawlins,<br />
MD, Linda Barney, MD, Wright State University, Dept of Surgery<br />
P367 FIRST REPORT OF SPRAY CRYOSURGERY DEPTH OF INJURY TO<br />
THE HUMAN ESOPHAGUS Afonso Ribeiro, MD, Dido Francerschi, MD,<br />
Pablo Bejarano, MD, Lynne Sparling, RN, Alan Livingstone, MD, Bach<br />
Ardalan, MD, University of Miami<br />
P368 SAFETY AND QUALITY OF COLONOSCOPY PERFORMED BY<br />
GENERAL SURGEONS Ibrahim Ahmed, FRCSI, Elnazier Ibrahim, FRCSI,<br />
Edrian Iskandar, MRCSI, Alexander Lockley, MBCh, Ibraheem Tunau,<br />
FRCSI, Mohamed Salama, FRCSI, Olumide Fagbeja, FRCSI, Our Lady’s<br />
Hospital, Navan, Ireland<br />
P369 SMALL-DOSE INDIA INK TATTOOING FOR PREOPERATIVE<br />
LOCALIZATION OF COLORECTAL TUMOR: A PILOT STUDY Mi Ri<br />
Hwang, MD, Dae Kyung Sohn, MD, Ji Won Park, MD, Byung Chang Kim,<br />
MD, Chang Won Hong, MD, Kyung Su Han, MD, Hee Jin Chang, MD,<br />
Jae Hwan Oh, MD, Center for Colorectal Cancer, Research Institute &<br />
Hospital, National Cancer Center<br />
P370 EARLY US EXPERIENCE WITH ENDOSCOPIC REMOVAL OF THE<br />
ORBERA SYSTEM® INTRAGASTRIC BALLOON. Mark A Fusco, MD,<br />
LifeShape Advanced Bariatrics Center of Florida, and Melbourne<br />
Internal Medicine Associates<br />
P371 ENDOSCOPIC STENT MANAGEMENT OF LEAKS AND<br />
ANASTOMOTIC STRICTURES AFTER FOREGUT SURGERY Panot<br />
Yimcharoen, MD, Fady Moustarah, MD MPH, Nabil Tarek, MD, Joseph<br />
Talarico, MD, Kibwe Weaver, MD, Fahed Sabagh, MD, Stacy Brethauer,<br />
MD, Philip Schauer, MD, Matthew Kroh, MD, Bipan Chand, MD, Bariatric<br />
& Metabolic Institute, Cleveland Clinic Foundation, Cleveland, OH<br />
P372 OUTCOME COMPLICATIONS OF PERCUTANEOUS ENDOSCOPIC<br />
GASTROSTOMY TUBE PLACEMENT IN SEVERLY MALNOURISHED<br />
PATIENTS Sammy D Eghbalieh, MD, Navid Eghbalieh, MD, Robert<br />
Brenes, MD, Michael S Ajemian, MD FACS, Saint Mary’s Healthcare<br />
Hospital System<br />
P373 A CASE SERIES OF TRANSMURAL PRESSURE NECROSIS FROM<br />
PROLONGED USE OF PEG TUBES Hamed Taheri, MD, Vijay Rastogi, MD<br />
FACS, Hani mourad, MD, Harjit Kohli, MD FACS, Easton Hospital<br />
P374 THE RELATIONSHIP BETWEEN POST-OPERATIVE ANATOMY AND<br />
ENDOSCOPIC STENT MIGRATION Gary S Schwartz, MD, Koji Park, MD,<br />
Scott B Gmora, MD, Kevin McGill, MD, Deva Boone, MD, Shahzad S Razi,<br />
MD, James J McGinty, MD, Faiz Y Bhora, MD, Scott J Belsley, MD, Julio A<br />
Teixeira, MD, St. Luke’s-Roosevelt Hospital Center, Columbia University<br />
College of Physicians and Surgeons<br />
P375 FLEXIBLE ENDOLOOP “ HAND MADE” Mohamed Seleem, PhD,<br />
Cairo University Faculty Of Medicine<br />
P376 EFFICACY OF A PROTOTYPE ENDOSCOPE WITH TWO<br />
DEFLECTING WORKING CHANNELS FOR ENDOSCOPIC SUBMUCOSAL<br />
DISSECTION (ESD): A PROSPECTIVE COMPARATIVE EX-VIVO STUDY<br />
Suck-Ho Lee, MD PhD, Mark A Gromski, BA, Alexandre Derevianko,<br />
MD, Daniel B Jones, MD MS FACS, Douglas K Pleskow, MD, Mandeep<br />
Sawhney, MD, Ram Chuttani, MD, Kai Matthes, MD PhD, Beth Israel<br />
Deaconess Medical Center and Harvard Medical School, Boston, MA<br />
P377 ONE STEP MANAGEMENT OF COMMON BILE DUCT STONES<br />
Matthew Johnson, MD, Charles R St. Hill, MD, Nabeel Arain, BA MSIV,<br />
Nathan Ozobia, MD FACS, University of Nevada School of Medicine,<br />
Department of Surgery<br />
P378 PNEUMATOSIS COLI FROM ENDOSCOPY: A CASE REPORT Kayla J<br />
Foertsch, MD, De Tran, MD, VA Fargo, ND<br />
P379 CONCURRNET USE OF SELF-EXPANDABLE BILIARY AND ENTERIC<br />
METAL STENTS FOR OBSTRUCTING INOPERABLE DUODENAL<br />
CANCER Diya I Alaedeen, MD, Jose M Martinez, MD, Cleveland Clinic<br />
Foundation, Fairview Hospital Department of Surgery, and * University<br />
of Miami School of Medicine, Department of Surgery, Division of<br />
Laparoendoscopic Surgery<br />
P380 ARE COLONOSCOPIES BY COLORECTAL SURGEONS ADEQUATE?<br />
Vincent Obias, MD, Grace Montenegro, MD, Bruce Orkin, MD, George<br />
Washington University<br />
P381 ENDOSCOPIC TREATMENT OF LARGE CHRONIC<br />
GASTROCUTANEOUS FISTULA AFTER BARIATRIC SURGERY USING<br />
A PARTIALLY COVERED METALLIC ESOPHAGEAL STENT Javier<br />
E Andrade, MD, Alberto R Iglesias, MD, Decio Carvalho, MD, Jose M<br />
Martinez, MD, University of Miami. Miller School of Medicine. DeWitt<br />
Daughtry Family Department of Surgery. Division of Laparoendoscopic<br />
and Bariatric Surgery. Miami, FL, USA.<br />
P382 THE VALUE OF ERCP IN THE MANAGEMENT OF COMPLEX LIVER<br />
INJURIES Charles R St. Hill, MD, Matthew Johnson, MD, Nabeel Arain,<br />
BA MSIV, Nathan Ozobia, MD FACS, University of Nevada School of<br />
Medicine, Department of Surgery, Las Vegas, Nevada<br />
P383 BARRETT’S ESOPHAGITIS IN PATIENTS UNDERGOING<br />
PREOPERATIVE SCREENING ENDOSCOPY FOR BARIATRIC SURGERY<br />
Atul K Madan, MD, Jose M Martinez, Alberto R Iglesias, MD, Scott T<br />
Hartnett, DO, Javier Andrade, MD, Beverly Hills Surgery Center and<br />
University of Miami<br />
P384 LAPAROSCOPIC SUBTOTAL CHOLECYSTECTOMY. A SAFE<br />
ALTERNATIVE! Gadiyaram Srikanth, MCh, Neel Shetty, MS, TLVD Prasad<br />
Babu, MCh, Sadiq S Sikora, MS, Manipa Institute of Liver and Digestive<br />
Surgery<br />
P385 SINGLE-STAGE LAPAROSCOPIC CBD EXPLORATION IMPROVES<br />
THE OUTCOME OF LC IN CURRENT LAPAROSCOPIC ERA. Shahram<br />
Nazari, Dr, Semira Mousavi Khosroshahi, Dr, Hosain Khedmat, Dr,<br />
Shahram Agah, Dr, Erfan Hospital, Department of General and<br />
Laparoscopic surgery<br />
P386 MINIMALLY INVASIVE CHOLECYSTECTOMY PROCEDURES – A<br />
REVIEW OF THE LITERATURE. Manmohan Varma, Ms, Kushal Varma,<br />
MedicalStudent, Private, Kanpur, India<br />
P387 LAP MANAGEMENT OF VARIOUS PANCREATIC TUMORS Shailseh<br />
Puntambekar, Galaxy Care Laparoscopy<br />
12 th World Congress of Endoscopic Surgery<br />
171 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P388 LAPAROSCOPIC CHOLECYSTECTOMY IN HIV POSITIVE PATIENTS:<br />
A CASE SERIES Daniel T Farkas, MD, Dovid S Moradi, BA, John M<br />
Cosgrove, MD, Bronx-Lebanon Hospital Center, Albert Einstein College<br />
of Medicine<br />
P389 TRANS-UMBILICAL SINGLE INCISION LAPAROSCOPIC<br />
CHOLECYSTECTOMY CONSIDERED ABOUT ECONOMIC EFFICIENCY<br />
Hidenori Fujii, MD PhD, Yosiyuki Kawakami, MD PhD, Toshiharu Aotake,<br />
MD PhD, Koiji Doi, MD PhD, Kei Hirose, MD, Hisaya Shirai, MD, Naoki<br />
Nagayoshi, MD, Atushi Ikeda, MD, Fumie Tanak, MD, Yuki Hirose, MD<br />
PhD, Fukui Red Cross Hospital<br />
P390 CLINICAL OUTCOMES COMPARED BETWEEN LAPAROSCOPIC<br />
AND OPEN DISTAL PANCREATECTOMY FOR BENIGN TUMORS Jun<br />
Chul Chung, MD PhD, Hyung Chul Kim, MD PhD, Chong Woo Chu, MD<br />
PhD, Department of Surgery, Soonchunhyang University College of<br />
Medicine,Soonchunhyang University Bucheon Hospital, Bucheon, Korea.<br />
P391 IN LAPAROSCOPIC DISTAL PANCREATECTOMY, PANCREATIC<br />
RESECTION USING HARMONIC SCALPEL Jun Chul Chung, MD PhD,<br />
Hyung Chul Kim, MD PhD, Chong Woo Chu, MD PhD, Department<br />
of Surgery, Soonchunhyang University College of Medicine,<br />
Soonchunhyang University Bucheon Hospital, Bucheon, Korea.<br />
P392 GASLESS SINGLE PORT LAPAROSCOPIC CHOLECYSTECTOMY<br />
Nobumi Tagaya, PhD, Akihito Abe, PhD, Keiichi Kubota, PhD, Second<br />
Department of Surgery, Dokkyo Medical University, Tochigi, Japan<br />
P393 MINIMALLY INVASIVE PANCREATIC NECROSECTOMY – HOW<br />
TO CHOOSE THE BEST APPROACH? Sanjiv P Haribhakti, Harshad<br />
Soni, Anish P Nagpal, Nitin Patel, Rahul Naik, Department of Surgical<br />
Gastroenterology and Advanced Laparoscopic Surgery, Haribhakti<br />
Surgical Hospital<br />
P394 FEASIBILITY OF LAPAROSCOPIC PORTAL VEIN LIGATION PRIOR<br />
TO MAJOR LIVER RESECTION Hitoshi Inagaki, MD, Tsuyoshi Kurokawa,<br />
MD, Tadashi Yokoyama, MD, Nobuhiro Ito, MD, Manabu Kikuchi, MD,<br />
Yasuhisa Yokoyama, MD, Toshiaki Nonami, MD, Department of Surgery,<br />
Yokoyama Hospital for Gastroenterological Diseases<br />
P395 LAPAROSCOPIC PANCREATIC SURGERY Nobumi Tagaya, PhD,<br />
Aya Nakagawa, PhD, Yukihiro Iso, PhD, Yoshimi Iwasaki, phD, Mitsugi<br />
Shimoda, PhD, Keiichi Kugota, PhD, Second Department of Surgery,<br />
Dokkyo Medical University, Tochigi, Japan<br />
P396 A PROSPECTIVE COHORT STUDY FOR SIMPLE NEW TECHNIQUE<br />
TWO-INCISION LAPAROSCOPIC CHOLECYSTECTOMY Pornthape<br />
Prathanvanich, Patpong Navicharern, Chadin Tharavej, Suthep<br />
Udomsawaengsup, Suppa-ut Suppa-ut, Chulalongkorn University<br />
P397 SINGLE PORT LAPAROSCOPIC CHOLECYSTECTOMY WITHOUT<br />
THE INDUCTION OF PNEUMOPERITONEUM Masashi Ihikawa, PhD,<br />
Takako Furukawa, Dr, Ayumi Kihara, Dr, Yutaka Matsuoka, Dr, Yoko<br />
Yamamura, Dr, Takuya Minato, Dr, Yasuhiro Yuasa, Dr, Toshihiro Ichimori,<br />
Dr, Suguru Kimura, PhD, Akihiro Sakata, PhD, Tokushima Red Cross<br />
Hospital<br />
P398 LAPAROSCOPIC LIVER RESECTION FOR HEPATOCELLULAR<br />
CARCINOMA IN PATIENTS WITH LIVER CIRRHOSIS Chung-Wei Lin,<br />
MD, Tzu-June Tsai, MD, Tsung-Yen Cheng, MD, Chii-Ming Chen, MD,<br />
Department of Surgery, Koo-Foundation Sun Yat-Sen Cancer Center,<br />
Taipei, Taiwan<br />
P399 LAPAROSCOPIC SURGERY FOR BILIARY TRACT CANCER Osamu<br />
Itano, MD PhD, Shingo Maeda, MD PhD, Naokazu Chiba, MD PhD,<br />
Takeyuki Wada, MD, Takashi Nakayama, MD, Hideki Ishikawa, MD PhD,<br />
Yasumasa Koyama, MD, Yuko Kitagawa, MD PhD, Endoscopic Surgery<br />
Center, Eiju General Hospital, Tokyo, Japan, Department of Surgery, Keio<br />
University, School of Medicine, Tokyo, Japan<br />
P400 BOUVERET’S SYNDROME: GALLSTONE ILEUS OF THE<br />
DUODENUM Katie Love, MD, Zachary P Englert, DO, Stephan Barrientos,<br />
MD, Mark D Marilley, MD, Curtis E Bower, MD FACS, ECU Department of<br />
Surgery, Brody School of Medicine<br />
P401 SINGLE INCISION LAPAROSCOPIC CHOLECYSTECTOMY WITH<br />
ROUTINE CHOLANGIOGRAM: REPORT OF 30 CASES Brendan G<br />
O’Connell, MD, Bruce Bernstein, PhD, Ibrahim M Daoud, MD, University<br />
of Connecticut, St. Francis Hospital and Medical Center, Hartford, CT<br />
P402 UMBILICAL SINGLE INCISION LAPAROSCOPIC<br />
CHOLECYSTECTOMY Alberto R Ferreres, MD PhD MPH FACS, Anibal<br />
Rondán, MD, Julieta Paleari, MD, Mariano E Giménez, MD, Vicente P<br />
Gutiérrez, MD FACS, Department of Surgery, University of Buenos Aires<br />
P403 LAPAROSCOPIC RESECTION OF THE LEFT LIVER: TECHNICAL<br />
REFINEMENTS FOR STANDARDIZATION Satoru Imura, MD, Mitsuo<br />
Shimada, MD PhD, Toru Utsunomiya, MD PhD, Yuji Morine, MD, Tetsuya<br />
Ikemoto, MD, Jun Hanaoka, MD, Shuichi Iwahashi, MD, Yu Saito, MD,<br />
Nobuhiro Kurita, MD, Hidenori Miyake, MD PhD, Department of Surgery,<br />
The University of Tokushima<br />
P404 LAPAROSOCPIC MANAGEMENT OF CYSTIC NEOPLASM OF<br />
PANCREAS Mohan Narasimhan, Sourav Kalia, Kumar Palaniappan,<br />
Ramesh Ardhanari, Department Of Surgery And Gastroenterology,<br />
Meenakshi Mission Hospital And Research Centre, Madurai<br />
P405 EMERGENCY LAPAROSCOPIC COMMON BILE DUCT<br />
EXPLORATION IN ACUTE CHOLANGITIS WITH COMMON BILE DUCT<br />
STONE PATIENTS. Koo Yong Hahn, MD, Jeong Hwan Keum, MD,<br />
Department of Surgery, Seongnam Central Hospital<br />
P406 THE CRITICAL VIEW OF SAFETY DURING SINGLE INCISION<br />
LAPAROSCOPIC CHOLECYSTECTOMY Hitoshi Idani, MD, Takashi<br />
Yoshioka, MD, Kenjiro Kumano, MD, Yohei Kurose, MD, Hiroki Nojima,<br />
MD, Shinichiro Kubo, MD, Hiroshi Sasaki, MD, Shinya Asami, MD, Nakano<br />
Kanyu, MD, Tetsumasa Yamashita, MD, Masahiko Muro, MD, Hitoshi Kin,<br />
MD, Norihisa Takakura,, Department of Surgery, Fukuyama City Hospital/<br />
Okayama University Graduate School of Medicne, Dentistry and<br />
pharmaceutical Sciences<br />
P407 CLINICAL OUTCOMES OF LAPAROSCOPIC CHOLECYSTECTOMY<br />
(WITHOUT ENERGISED DISSECTION) PERFORMED BY A BASIC<br />
SURGICAL TRAINEE OR A CONSULTANT-DOUBLE BLIND<br />
RANDOMIZED CONTROL STUDY Brij B Agarwal, MS, Lakshmi<br />
Jayaraman, MD, Ashish Mishra, MS, Rathindra Sarangi, MS, Krishan<br />
C Mahajan, FRCS, Dr. Agarwal’s Surgery & Yoga and Sir Ganga Ram<br />
Hospital, New Delhi, India<br />
P408 SYNCHRONOUS LAPAROSCOPIC TREATMENT OF LIVER HYDATID<br />
CYSTS AND CHOLELITHIASIS AFTER OBSTRUCTIVE ICTERUS Toni<br />
Kolak, MD PhD, Josip Bakovic, MD, Igor Stipancic, MD PhD, Mario Tadic,<br />
MD, Antonela Radic, MD, University hospital Dubrava; Department of<br />
colorectal surgery<br />
P409 INTRADUCTAL PAPILLARY MUCINOUS CARCINOMA WITH A<br />
RARE ATYPICAL FISTULIZATION TO ADJACENT STRUCTURES HN<br />
Aydin, MD, K Singh, MD, A Shiyab, MD, M Arregui, Department of MIS<br />
and Advanced Endoscopy, St. Vincent Hospital, Indianapolis IN USA<br />
P410 LAPAROSCOPIC LIVER RESECTION FOR HEPATOCELLULAR<br />
CARCINOMA Yang-Seok Koh, MD PhD, Jin Shick Seoung, MD, Young Hoi<br />
Hur, MD, Jung Chul Kim, MD PhD, Chol-Kyoon Cho, MD PhD, Hyun Jong<br />
Kim, MD PhD, Department of Surgery, Chonnam National University<br />
Hwasun Hospital<br />
P411 NOT JUST LITTLE STONES IN LITTLE ADULTS: BILIARY<br />
MICROLITHIASIS IN CHILDREN IS SUCCESSFULLY MANAGED<br />
WITH ENDOSCOPIC ULTRASOUND AND LAPAROSCOPIC<br />
CHOLECYSTECTOMY Lucas P Neff, MD, Girish Mishra, MD, John E<br />
Fortunato, MD, John K Petty, MD, Brenner Children’s Hospital/ Wake<br />
Forest University School of Medicine<br />
P412 LAPAROSCOPIC LIVER RESECTION: A SINGLE CENTER<br />
EXPERIENCE Kim Hohyun, MD, Park Eunkyu, MD, Seoung Jinshick,<br />
MD, Hur Younghoe, MD, Koh Yangseok, MD, Kim Jungchul, MD, Cho<br />
Cholkyoon, MD, Kim Hyunjong, MD, Department of surgery, Chonnam<br />
National University Hospital<br />
12 th World Congress of Endoscopic Surgery 172
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P413 CONVERSION FACTORS IN LAPAROSCOPIC CHOLECYSTECTOMY<br />
Tae Han Kim, Dr, Yoo Shin Choi, MD, Beom Gyu Kim, MD, Jun Seok Park,<br />
MD, Seong Jae Cha, MD, Sung Jun Park, MD, In Taik Chang, MD, Chungang<br />
university hospital<br />
P414 EFFECT OF YOGA ON THE SPEED OF CONVALESCENCE<br />
AFTER UNCOMPLICATED OUTPATIENT LAPAROSCOPIC<br />
CHOLECYSTECTOMY--A CASE CONTROLLED STUDY Brij B Agarwal,<br />
MS, Rathindra Sarangi, MS, Krishan C Mahajan, FRCS, Dr. Agarwal’s<br />
Surgery & Yoga and Sir Ganga Ram Hospital, New Delhi, India<br />
P415 UTILITIES OF PREOPERATIVE ASSESSMENT OF ABDOMINAL<br />
ADHESIONS USING ULTRASOUND SCANS IN THE LAPAROSCOPIC<br />
HEPATECTOMY Yuichiro Otsuka, MD, Masaru Tsuchiya, MD, Tetsuya<br />
Maeda, MD, Satoshi Yajima, MD, Takashi Suzuki, MD, Yorichika Kubota,<br />
MD, Masashi Watanabe, MD, Yoko Oshima, MD, Satoru Kagami, MD,<br />
Hironori Kaneko, PhD, Department of surgery (Omori), Toho university<br />
faculty of medicine, Tokyo, Japan<br />
P416 NECESSITY OF INTRAOPERATIVE CHOLANGIOGRAPHY DURING<br />
LAPAROSCOPIC CHOLECYSTECTOMY BASED ON ANALYSIS OF<br />
CASES OF PANCREATICOBILIARY DUCTAL MALJUNCTION WITHOUT<br />
COMMON BILE DUCT DILATATION Shoji Fukuyama, MD PhD, Hiromi<br />
Tokumura, MD PhD, Takashi Tsuchiya, MD PhD, Sendai Open Hospital,<br />
Department Of Surgery<br />
P417 PRELIMINARY EXPERIENCE OF LAPAROSCOPIC HEPATECTOMY<br />
IN HEPATOCELLULAR CARCINOMA Choon Hyuck D Kwon, MD, Gwan<br />
Chul Lee, MD, Jae Won Joh, MD PhD, Jin Seok Heo, MD PhD, Gum O<br />
Jung, MD, Ju Ik Moon, MD, Jong Man Kim, MD, Department of Surgery,<br />
Samsung Medical Center, Sungkyunkwan University<br />
P418 LONG TERM FOLLOW UP AFTER LAPAROSCOPIC NON-<br />
MALIGNANT PANCREATIC TUMOR SURGERY Emanuele Lezoche,<br />
MD FACS, Alessandro M Paganini, MD PhD FACS, Mario Guerrieri,<br />
MD, Giancarlo D’Ambrosio, MD, Maddalena Baldarelli, MD, Giovanni<br />
Lezoche, MD, Luciana Barchetti, MD, Massimiliano Rimini, MD, Daniele<br />
Scoglio, MD, Clinica Chirurgica e Tecnologie Avanzate, Department of<br />
Surgery “Paride Stefanini”, University of Rome “La Sapienza”, Rome, Italy.<br />
*Department of General Surgery, Università Politecnica delle Marche,<br />
“Umberto I” Hospital, Via Conca, Ancona, Italy<br />
P419 IMPACT OF HEALTH INSURANCE ON COMPLICATED<br />
CHOLEDOCHOLITHIASIS AND SAME-ADMISSION INTERVENTIONS<br />
K Kummerow, BS, J Shelton, MD, J Foster, MD, S Phillips, MSPH, M<br />
Holzman, MD MPH, K Sharp, MD, B Poulose, MD MPH, Vanderbilt<br />
University Medical Center<br />
P420 CARBON FOOTPRINT OF LAPAROSCOPIC CHOLECYSTECTOMY<br />
PERFORMED WITH OR WITHOUT ENERGIZED DISSECTION-A CASE<br />
CONTROLLED STUDY Krishna A Agarwal, Brij B Agarwal, Krishan C<br />
Mahajan, VMMC & Safdarjung Hospital, Dr. Agarwal’s Surgery & Yoga<br />
and Sir Ganga Ram Hospital, New Delhi, India<br />
P421 COMPARATIVE PATEINT REPORTED WELL BEING AFTER<br />
LAPAROSCOPIC CHOLECYSTECTOMY PERFORMED WITH OR<br />
WITHOUT ENERGISED DISSECTION-A CASE CONTROLLED STUDY Brij<br />
B Agarwal, MS, Krishan C Mahajan, FRCS, Dr. Agarwal’s Surgery & Yoga<br />
and Sir Ganga Ram Hospital, New Delhi, India<br />
P422 HAND-ASSISTED LAPAROSCOPIC AND TOTAL LAPAROSCOPIC<br />
PARTIAL HEPATECTOMY FOR HEPATOCELLULAR CARCINOMA – A<br />
COMPARATIVE STUDY Eric C.H. Lai, Chung Ngai Tang, George P.C. Yang,<br />
Oliver C.Y. Chan, Michael K.W. Li, Department of Surgery, Pamela Youde<br />
Nethersole Eastern Hospital, Hong Kong SAR, China<br />
P423 LAPAROSCOPIC LIVER RESECTION USING VASCULAR STAPLERS<br />
IN THE PORCINE MODEL Konstantinos G Tsalis*, Prof, Konstantinos<br />
Blouhos*, MD, George Vrakas*, MD, Ioannis Savvas×, Assist Prof,<br />
Timoleon Ralis×, Prof, Staavros Kalfadis*, PhD, Charalampos Lazaridis*,<br />
Prof, *D’ Surgical Department Medical School Aristotle University of<br />
Thessaloniki Greece<br />
P424 HOW RELIABLE IS LAPAROSCOPIC CHOLECYSTECTOMY IN<br />
ELDERLY PATIENTS? A RETROSPECTIVE ANALYSIS OF OUTCOMES.<br />
A. Ziya Anadol, MD FACS, Ekmel Tezel, MD PhD, Emin Ersoy, MD, Gazi<br />
University Department of Surgery<br />
P425 ON DEMAND TROCAR INSERTION FOR LAPAROSCOPIC<br />
CHOLECYSTECTOMY: TWO, THREE OR FOUR? A. Ziya Anadol, MD PhD,<br />
Gazi University School of Medicine<br />
P426 LAPAROSCOPIC LIVER RESECTIONS INCLUDING MAJOR<br />
HEPATECTOMIES- A TERTIARY CENTRE EXPERIENCE C Palanivelu,<br />
MCh FACS FRCS, P Senthilnathan, MS DNB MRCS, P S Rajan, MS FACS, R<br />
Rohit, MS, P Praveen Raj, MS, Atul Kumar Gupta, MS, Pinak Das Gupta,<br />
MS, GEM Hospital<br />
P427 SHORT TERM OUTCOME AFTER LAPAROSCOPIC RADICAL<br />
CHOLECYSTECTOMY FOR CARCINOMA OF THE GALL BLADDER<br />
C Palanivelu, MCh FACS FRCS, P Senthilnathan, MS DNB MRCS, V<br />
Vaithiswaran, MS MRCS, Charles William, MS, Pinak Das Gupta, MS, Atul<br />
Das Gupta, MS, C Chandramaliteeswaran, MS, GEM Hospital<br />
P428 SINGLE INCISION LAPAROSCOPIC CHOLECYSTECTOMY: THE<br />
FIRST 100 OUTPATIENTS Jose Erbella, MD, Gary Bunch, MD, Manatee<br />
Memorial Hospital<br />
P429 STAPLE LINE REINFORCEMENT IN LAPAROSCOPIC DISTAL<br />
PANCREATECTOMY Ezra N Teitelbaum, MD, Khashayar Vaziri, MD, Fred<br />
Brody, MD, Paul P Lin, MD, The George Washington University Medical<br />
Center<br />
P430 LAPAROSCOPIC VS OPEN LEFT (DISTAL) PANCREATECTOMY- A<br />
CASE-MATCHED COMPARATIVE STUDY. Srinivas Kavuturu, MD, Dustin<br />
Morrow, MD, Isabelle Deshaies, MD, Eric T Kimchi, MD, Kevin F Staveley-<br />
O’Carroll, MD PhD, Niraj J Gusani, MD MS, Penn State Milton S Hershey<br />
Medical Center<br />
P431 GALLBLADDER PERFORATION: INCREASED RISK IN A VA<br />
POPULATION ASSOCIATED WITH LOWER BODY MASS INDEX (BMI)<br />
Amit Parikh, DO, Kshitij Kakar, MD, Salvador Sordo, MD, Helenmari<br />
Merritt, DO, Kishore Malireddy, MD, Michelle K Savu, MD, The University<br />
of Texas Health Science Center at San Antonio<br />
P432 PREOPERATIVE PANCREATIC STENTING PRIOR TO<br />
PANCREATECTOMY FOR CHRONIC PANCREATITIS: A COMBINED<br />
ENDOSCOPIC AND SURGICAL APPROACH Wesley B Jones, MD, Mark<br />
A Vitale, Brian R Davis, MD, Roger M Galindo, MD, Daniel Makela, Gary<br />
C Vitale, MD, Department of Surgery, University of Louisville School of<br />
Medicine, Louisville, KY, USA<br />
P433 TOTALLY LAPAROSCOPIC HEPATECTOMY FOR HEPATOLITHIASIS<br />
Kuo-Hsin Chen, MD, Hsin-An Chen, MD, Jain-Ming Wu, MD, Chao-Chiang<br />
Tu, MD, Kuo- Hsiang Cheng, MD, Shin-Horng Huang, MD PhD, Division of<br />
General Surgery, Department of Surgery, Far-Eastern Memorial Hospital<br />
P434 – Withdrawn.<br />
P435 TOTALLY LAPAROSCOPIC ISOLATED CAUDATE HEPATECTOMY<br />
WITH SELECTIVE INFLOW CONTROL – CASE REPORT Shiu-Dong<br />
Chung, MD, Kuo-Hsin Chen, MD, Hsin-An Chen, MD, Jain-Ming Wu, MD,<br />
Chao-Chiang Tu, MD, Kuo- Hsiang Cheng, MD, Shin-Horng Huang, MD<br />
PhD, Department of Surgery, Far-Eastern Memorial Hospital, Taipei,<br />
Taiwan<br />
P436 LAPAROSOCPIC DISTAL PANCREATIC RESECTION Furuta kauznori,<br />
MD PhD, Ishii Kenichiro, MD PhD, Katagiri Hiroyuki, MD PhD, Takahashi<br />
Yoshihito, MD PhD, Watanabe Masahiko, MD PhD, Kitasato University<br />
P437 ROLE OF LAPAROSCOPIC HEPATECTOMY FOR HEPATOCELLULAR<br />
CARCINOMA Hironori Kaneko, MD, Yuichiro Otsuka, MD, Masaru<br />
Tsuchiya, MD, Akira Tamura, MD, Takayuki Suzuki, MD, Takashi<br />
Suzuki, MD, Yoko Oshima, MD, Yorichika Kubota, MD, Jun Ishii, MD,<br />
Shigeki Imamura, MD, Masashi Watanabe, MD, Hideaki Shimada, MD,<br />
Department of Surgery(Omori), , Toho university school of Medicine,<br />
Tokyo, Japan<br />
12 th World Congress of Endoscopic Surgery<br />
173 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P438 REPEATED LAPAROSCOPIC HEPATECTOMY FOR THE RECURRENT<br />
HEPATOCELLULAR CARCINOMA Hironori Kaneko, PhD, Masaru<br />
Tsuchiya, MD, Yuichiro Otsuka, MD, Akira Tamura, MD, Kunihiro<br />
Yamazaki, MD, Toshio Katagiri, MD, Tetsuya Maeda, MD, Satoru Kagami,<br />
MD, Yoshihisa Kubota, MD, Satoshi Matsuda, MD, Shigeki Imamura, MD,<br />
Yasuo Nagashima, MD, Department of Surgery(Omori), Toho University<br />
School of Medicine, Tokyo, Japan<br />
P439 USE OF COVERED METALLIC STENTS IN THE MANAGEMENT OF<br />
BENIGN BILIARY STRICTURES Javier E Andrade, MD, Decio Carvalho,<br />
MD, Alberto R Iglesias, MD, Jose M Martinez, MD, University of Miami<br />
Miller School of Medicine. DeWitt Daughtry Family Department of<br />
Surgery. Division of Laparoendoscopic and Bariatric Surgery. Miami, FL,<br />
USA.<br />
P440 LAPAROSCOPIC TRANSGASTRIC CYST GASTROSTOMY FOR AN<br />
UNRESECTABLE MUCINOUS CYST ADENOMA OF THE PANCREAS<br />
Venkata Kanthimathinathan, MD, J Andres Astudillo, MD, Ata Mazaheri,<br />
MD, Loma Linda University, Department of Surgery<br />
P441 LAPAROSCOPIC MANAGEMENT OF SYMPTOMATIC CYSTIC<br />
DISEASE OF THE LIVER Fumiki Kushihata, MD, Jota Watanabe, MD,<br />
Tetsuya Mizumoto, MD, Yoshikuni Nonenaga, MD, Akifumi Miyoshi, MD,<br />
Taiji Toyama, MD, Kazuo Honda, MD, Yasutsugu Takada, MD, Surgery,<br />
Ehime University School of medicine<br />
P442 A NEW APPLICATION OF BILIARY TRACT IDENTIFICATION<br />
BASED ON INDOCYANINE GREEN FLUORESCENT IMAGING AT<br />
LAPAROSCOPIC SURGERY Jota Watanabe, MD, Fumiki Kushihata, MD,<br />
Tetsuya Mizumoto, MD, Yoshikuni Yonenaga, MD, Akifumi Miyoshi, MD,<br />
Taiji Toyama, MD, Kazuo Honda, MD, Yasutsugu Takada, MD, Dept. of<br />
Surgery, Ehime University School of Medicine<br />
P443 SINGLE INCISION VENTRAL HERNIA REPAIR: THE INITIAL<br />
EXPERIENCE Katie M Love, MD, Curtis E Bower, MD FACS, ECU Brody<br />
School of Medicine<br />
P444 PHYSICOMECHANICAL EVALUATION OF ABSORBABLE<br />
AND NONABSORBABLE BARRIER COMPOSITE MESHES FOR<br />
LAPAROSCOPIC VENTRAL HERNIA REPAIR Corey R Deeken, PhD,<br />
Michael S Abdo, Margaret M Frisella, RN, Brent D Matthews, MD,<br />
Washington University School of Medicine<br />
P445 RESULTS OF LAPAROSCOPIC REPAIR OF PRIMARY AND<br />
RECURRENT INCISIONAL HERNIAS AT A SINGLE UK INSTITUTION<br />
Julian Sturt, MD FRCS, Christopher Liao, MD MRCS, Shivani<br />
Arulanandam, MD, Jyoti Sidhu, MD, Donald Menzies, MD FRCS, Roger<br />
Motson, MD FRCS, ICENI Centre, Colchester, United Kingdom<br />
P446 RARE CASE OF LAPAROSCOPIC REPAIR OF A STRANGULATED<br />
OBTURATOR HERNIA Ashraf A Sabe, MD, Mustapha Daoadi, MD, Sang<br />
Lee, MD, Praneetha Narahari, MD, Saint Vincent Hospital, Beth Israel<br />
Deaconess Medical Center, Harvard School of Medicine<br />
P447 LAPAROSCOPIC VENTRAL HERNIA IN THE ELDERLY: A SAFE<br />
OPTION Ashwin Kurian, MD, Sidhbh Gallagher, MD, Abhiman<br />
Cheeyandira, MD, Mary Hofmann, MD, Robert Josloff, MD, Abington<br />
Memorial Hospital<br />
P448 SIMULTANEOUS LAPAROSCOPIC HERNIOPLASTY AND<br />
LAPAROSCOPIC CHOLECYSTECTOMY Nobuhiro Ito, MD PhD, Noiku<br />
Nakao, MD PhD, Hiroshi Nagata, MD PhD, Hitoshi Inagaki, MD PhD,<br />
Toshiaki Nonami, MD PhD, Department of Gastroenterological Surgery,<br />
Aichi Medical University<br />
P449 PREDICTORS OF IN HOSPITAL LENGTH OF STAY AFTER<br />
LAPAROSCOPIC VENTRAL HERNIA REPAIR: A MULTI VARIATE<br />
LOGISTIC REGRESSION ANALYSIS. Ashwin A Kurian, MD, Sidhbh<br />
Gallagher, MD, Abhiman Cheeyandira, MD, Robert Josloff, MD, Abington<br />
Memorial Hospital<br />
P450 LAPAROSCOPIC REPAIR OF INCIDENTALLY FOUND SPIGELIAN<br />
HERNIAS: A CASE SERIES AND REVIEW OF LITERATURE Khanjan H<br />
Nagarsheth, MD, Henry S Nelson, MD, Todd Nickloes, DO, Greg Mancini,<br />
MD, Julio A Solla, MD, University of Tennessee Medical Center<br />
P451 MEANDERING EXTERNAL ILIAC ARTERY: A FREQUENT<br />
VASCULAR VARIANT FOUND DURING LAPAROSCOPIC INGUINAL<br />
HERNIA REPAIR Tiffany C Cox, MD, Jonathan P Pearl, MD, E. Matthew<br />
Ritter, MD, Departments of Surgery, National Naval Medical Center and<br />
the Uniformed Services University, Bethesda, Maryland<br />
P452 SINGLE-INCISION TOTALLY EXTRAPERITONEAL INGUINAL<br />
HERNIA REPAIR IS A USEFUL PRECURSOR TO MORE COMPLEX<br />
SINGLE-INCISION LAPAROSCOPIC OPERATIONS Jonathan P Pearl, MD,<br />
Uniformed Services University and National Naval Medical Center<br />
P453 LAPAROSCOPIC INCISIONAL HERNIA REPAIR: A RETROSPECTIVE<br />
REVIEW OF A MODIFIED TECHNIQUE Eugenia Kang, MD, Jonathan<br />
Svahn, MD, Kaiser Hospital- Oakland<br />
P454 USE OF LIGHT, PARTIALLY ABSORBABLE MESH IN OPEN<br />
INGUINAL HERNIA REPAIR REDUCES POST-OPERATIVE PAIN AND<br />
COMPLICATIONS: PRELIMINARY DATA WITH COUSIN 4D-DOME<br />
Andrew Morfesis, MD, Brian P Rose, Owen Drive Surgical Clinic of<br />
Fayetteville<br />
P455 POST-OPERATIVE CHRONIC PAIN AND RECURRENCE<br />
FOLLOWING LAPAROSCOPIC INGUINAL HERNIA REPAIR: TO STAPLE<br />
OR NOT TO STAPLE? Ibrahim M Daoud, MD, Vladimir P Daoud, MSc, St.<br />
Francis Hospital and Medical Center, Hartford, CT<br />
P456 LAPAROSCOPIC INGUINAL HERNIA REPAIR: A RETROSPECTIVE<br />
STUDY BASED ON THE 17-YEAR EXPERIENCE OF A SINGLE<br />
SURGEON. Ibrahim M Daoud, Vladimir P Daoud, MSc, St. Francis<br />
Hospital and Medical Center, Hartford, CT<br />
P457 PRECLINICAL EVALUATION OF NOVEL DESIGN FOR A<br />
RESORBABLE MESH FIXATION DEVICE Pullen Shnoda, DVM, Thomas<br />
Divilio, MD FACS, James W Oldham, PhD DABT, Timothy Muench, DVM<br />
PhD, Ethicon, Inc.<br />
P458 A PROSPECTIVE RANDOMIZED STUDY COMPARING<br />
LAPAROSCOPIC TOTALLY EXTRA PERITONEAL (TEP) REPAIR<br />
VERSUS TRANS ABDOMINAL PRE-PERITONEAL (TAPP) REPAIR FOR<br />
INGUINAL HERNIA REPAIR Mahesh C Misra, MS FRCS, Virinder K Bansal,<br />
MS, Subodh Kumar, MS, Asuri Krishna, MBBS, Department of Surgical<br />
Disciplines, All India Institute of Medical Sciences, New Delhi, India<br />
P459 – Withdrawn.<br />
P460 A COMPARATIVE BIOMECHANICAL EVALUATION OF HERNIA<br />
MESH FIXATION WITH FIBRIN SEALANT (FS) CONTAINING 4<br />
VS. 500 IU THROMBIN IN PIGS René H Fortelny, MD, A.H. Petter<br />
Puchner, MD, S. Blum, MD, J Ferguson, VD, J Brand, K Mika, MD, H Redl,<br />
PhD, II. Department of General Surgery, Wilhelminenspital, Vienna,<br />
Austria;Ludwig Boltzmann Institute for Experimental and Clinical<br />
Traumatology, Research Center of AUVA, Austrian Cluster for Tissue<br />
Regeneration, Vienna, Austria<br />
P461 THE IMPACT OF ATRAUMATIC FIBRIN SEALANT VS. STAPLE<br />
MESH FIXATION IN TAPP HERNIA REPAIR ON CHRONIC PAIN AND<br />
QUALITY OF LIFE – RESULTS OF A RANDOMIZED CONTROLLED<br />
STUDY René H Fortelny, MD, A.H. Petter Puchner, MD, Z. Khakpour, DI,<br />
C. May, MD, K. Mika, MD, K.S. Glaser, MD, H. Redl, PhD, II. Department of<br />
General Surgery, Wilhelminenspital, Vienna, Austria;Ludwig Boltzmann<br />
Institute for Experimental and Clinical Traumatology, Research Center<br />
of AUVA, Austrian Cluster for Tissue Regeneration, Vienna, Austria<br />
P462 POLYESTER COMPOSITE VERSUS PTFE IN LAPAROSCOPIC<br />
VENTRAL HERNIA REPAIR Modesto J Colon, MD, Dana Telem, MD, Scott<br />
Nguyen, MD, Edward Chin, MD FACS, Weber J Kaare, MD, Celia M Divino,<br />
MD FACS, The Mount Sinai Hospital, New York<br />
P463 EXPERIENCE OF SINGLE-SITE LAPAROSCOPIC HERNIOPLASTY<br />
Nobuhiro Ito, MD PhD, Hiroshi Nagata, MD PhD, Noiku Nakao, MD PhD,<br />
Hitoshi Inagaki, MD PhD, Toshiaki Nonami, MD PhD, Department of<br />
Gastroenterological Surgery, Aichi Medical University<br />
P464 COMPARISON OF LAPAROSCOPIC PRIMARY REPAIR AND OPEN<br />
REPAIR TECHNIQUES FOR SMALL VENTRAL HERNIAS. A. Ziya Anadol,<br />
MD FACS, Ekmel Tezel, MD PhD, Emin Ersoy, MD, Gazi University School<br />
of Medicine<br />
12 th World Congress of Endoscopic Surgery 174
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P465 LAPAROSCOPIC MANAGEMENT OF VARIOUS TYPES OF<br />
DIAPHRAGMATIC HERNIAS – A FIFTEEN YEARS EXPERIENCE FROM<br />
AN ADVANCE LAPAROSCOPIC CENTRE C Palanivelu, MCh FACS FRCS,<br />
S Rajapandian, MS FRCS, P Praveen Raj, MS, P Senthilnathan, MS DNB<br />
MRCS, R Kumaravel, MS, S Saravana Kumar, MS, GEM Hospital<br />
P466 LAPAROSCOPIC TRANSABDOMINAL PREPERITONEAL MESH<br />
REPAIR WITH SUTURED CLOSURE OF LOWER ABDOMINAL<br />
INCISIONAL HERNIA - A SINGLE CENTRE EXPERIENCE OF 15 CASES<br />
C Palanivelu, MCh FACS FRCS, P Senthilnathan, MS DNB MRCS, P S<br />
Rajan, MS FACS, V Vaithiswaran, MS MRCS, P Praveen Raj, MS, Alwar<br />
Ramanujam, MS, Atul Kumar Gupta, MS, GEM Hospital<br />
P467 LAPAROSCOPIC REPAIR OF LOSS OF DOMAIN INCISIONAL<br />
HERNIA COMBINING ENDOSCOPIC MYOFASCIAL ADVANCEMENT<br />
FLAPS, MEDIALIZATION OF THE RECTUS SHEATH, AND MESH<br />
REINFORCEMENT: A CASE SERIES Scott R Philipp, MD, Archana<br />
Ramaswamy, MD, University of Missouri - Columbia, Columbia, Missouri,<br />
USA<br />
P468 TOTALLY EXTRAPERITONEAL (TEP) SURGERY FOR INGUINAL<br />
HERNIA: SINGLE PORT ENDO-LAPAROSCOPIC SURGERY (SPES)<br />
VS STANDARD LAPAROSCOPIC SURGERY Michael M Lawenko,<br />
MD, Alembert Lee-Ong, MD, Javier Lopez-Gutierrez, MD, Sarah Chian,<br />
Davide Lomanto, MD, Minimally Invasive Surgical Centre, Department<br />
of Surgery, Yong Loo Lin School of Medicine, National University Health<br />
System - Singapore; Department of Sociology, Singapore Management<br />
University, Singapore<br />
P469 LAPAROSCOPIC TOTALLY EXTRAPERITONEAL PREPERITONEAL<br />
(TEPP) INGUINAL HERNIA REPAIR USING FETAL BOVINE DERMAL<br />
TISSUE (SURGIMEND). Joseph J Pietrafitta, MD, Fairview Northland<br />
Medical Center<br />
P470 LAPAROSCOPIC REPAIR OF ABDOMINAL WALL HERNIAS USING<br />
FETAL BOVINE DERMAL TISSUE (SURGIMEND). Joseph J Pietrafitta,<br />
MD, Fairview Northland Medical Center, Princeton, MN<br />
P471 TOTAL EXTRAPERITONEAL INGUINAL (TEP) HERNIORRHAPHY<br />
FOR PRIMARY INGUINAL HERNA: 3-YEAR EXPERIENCE OF A<br />
MINIMALLY INVASIVE FELLOWSHIP TRAINED SURGEON Beau<br />
Aldridge, Medical Student, Tejaswi Belavadi, Michael A Edwards, MD,<br />
Department of Surgery Gastrointestinal Section, Medical College of<br />
Georgia, Augusta, GA, USA<br />
P472 COMPARATIVE PATIENT REPORTED OUTCOMES IN<br />
LAPAROSCOPIC INTRAPERITONEAL ONLAY MESH REPAIR FOR<br />
VENTRAL HERNIA WITH OR WITHOUT DEFECT CLOSURE - A 9-YEAR<br />
FOLLOW UP CASE CONTROLLED STUDY Brij B Agarwal, MS, Sneh<br />
Agarwal, MS, Krishan C Mahajan, FRCS, Dr. Agarwal’s Surgery & Yoga, Sir<br />
Ganga Ram Hospital and Lady Hardinge Medical College, New Delhi,<br />
India<br />
P473 – Withdrawn.<br />
P474 SINGLE INCISION INTRACOPORAL LAPAROSCOPIC<br />
APPENDECTOMY: AN EARLY EXPERIENCE Elyssa J Feinberg, MD, David<br />
J O’Connor, MD, Prathiba Vemulapalli, MD, Diego Camacho, MD, Albert<br />
Einstein College of Medicine, Montefiore Medical Center<br />
P475 ANATOMIC THORACOSCOPIC LUNG SEGMENTECTOMY<br />
SIMULATED BY THREE-DIMENSIONAL COMPUTED TOMOGRAPHY<br />
ANGIOGRAPHY Hiroyuki Oizumi, PhD, Makoto Endoh, PhD, Jun<br />
Suzuki, MD, Ken Fukaya, MD, Mitsuaki Sadahiro, PhD, Department of<br />
Cardiovascular, Thoracic and Pediatric Surgery, , Yamagata University<br />
P476 LAPAROSCOPIC GASTROJEJUNOSTOMY FOR THE TREATMENT<br />
OF GASTRIC OUTLET OBSTRUCTION Linda P Zhang, MD, Parissa<br />
Tabrizian, MD, Dana Telem, MD, Scott Q Nguyen, MD, Celia Divino, MD,<br />
Mount Sinai School of Medicine<br />
P477 A SIMPLE ‘FUNDAL TRACTION SUTURE’ IN SINGLE INCISION<br />
LAPAROSCOPIC CHOLECYSTECTOMY Srikanth Gadiyaram, Dr, Neel<br />
Shetty, Dr, Manipal Institute of Liver and Digestive Diseases<br />
P478 THE FASHION OF INCISION AND TROCAR PLACEMENT FOR<br />
SINGLE PORT LAPAROSCOPIC CHOLECYSTECTOMY Atsushi Iida, MD<br />
PhD FACS, Kenji Koneri, MD, Kei Honda, MD, Takanori Goi, MD, Kanji<br />
Katayama, MD, Akio Yamaguchi, MD PhD, Gastroenterological surgery,<br />
University of Fukui, Fukui, Japan<br />
P479 THE FEASIBILITY OF LESS USING CONVENTIONAL<br />
LAPAROSCOPIC INSTRUMENTS. Modesto J Colon, MD, Dana Telem,<br />
MD, Scott Nguyen, MD FACS, Celia M Divino, MD FACS, Edward Chin, MD<br />
FACS, Mount Sinai Hospital<br />
P480 SILS USING STANDARD LAPAROSCOPIC INSTRUMENTS Shahram<br />
Nazari, Dr, Semira Mousavi Khosroshahi, Dr, Afshin Amini, Dr, Hosain<br />
Khedmat, Dr, Ahmad Fanaii, Dr, Erfan Hospital, Department of General<br />
and Laparoscopic surgery<br />
P481 LAPAROSCOPIC INFERIOR MESENTERIC ARTERY LIGATION<br />
PRIOR TO ENDOVASCULAR ABDOMINAL AORTIC ANEURYSM REPAIR<br />
Robert A Brenes, MD, Lucian Panait, MD, Jaime S Strachan, MD, Guiseppe<br />
Tripodi, MD FACS, Michael S Ajemian, MD FACS, Shady H Macaron, MD,<br />
Saint Mary’s Hospital, The Stanley J. Dudrick Department of Surgery,<br />
Waterbury, Connecticut<br />
P482 INITIAL EXPERIENCE IN SINGLE INCISION LAPAROSCOPIC<br />
SURGERY LEAD TO MODIFICATIONS AND DEDICATED TOOLS<br />
FOR COMPARABLE SAFETY TO STNADARD LAPAROSCOPY Noam<br />
Shussman, MD, Ram Elazary, MD, Abed Khalaileh, MD, Andrei Keidar, MD,<br />
Avraham I Rivkind, MD FACS, Yoav Mintz, MD, Department of Surgery,<br />
Hadassah-Hebrew University Medical Center, Jerusalem, Israel<br />
P483 ROBOTIC VERSUS LAPAROSCOPIC ADRENALECTOMY Hizir Y<br />
Akyildiz, MD, Allan Siperstein, MD, Mira Milas, MD, Jaime Mitchell, MD,<br />
Eren Berber, Cleveland Clinic<br />
P484 DAY CASE LAPAROSCOPIC SURGERY: HOW CAN WE IMPROVE<br />
? Ibrahim Ahmed, FRCSI, Elnazier Ibrahim, FRCSI, Mohamed Salama,<br />
FRCSI, Michelle Nolan, Alexander Lockley, MBCh, Noreen Kinsella, MSc,<br />
Our Lady’s Hospital, Navan, Ireland<br />
P485 OPINION SURVEY ON OPERATIVE MANAGEMENT OF<br />
ADHESIVE SMALL BOWEL OBSTRUCTION: LAPAROSCOPY VERSUS<br />
LAPAROTOMY IN THE STATE OF CONNECTICUT Tolutope O Oyasiji,<br />
MD, Scott W Helton, MD FACS, Hospital of Saint Raphael,1450 Chapel<br />
Street, New Haven, CT 06511<br />
P486 MINI-INCISION LAPARATOMY AS A ONE STAGE APPROACH IN<br />
MANAGEMENT OF COMPLICATED GALLSTONE DISEASE Abdulkadir<br />
Yakubu, MD, Viktor N Chernov, Professor, Rostov State Medical University<br />
P487 NEW EQUIPMENTS AND TECHNIQUES FOR VIDEO-ASSISTED<br />
THYROIDECTOMY USING LIFTING METHOD BY NEW RETRACTOR VIA<br />
AXILLARY APPROACH Koichi Kayano, MD PhD, Junichi Kohmoto, MD<br />
PhD, Hisao Mizutani, MD PhD, Motohisa Kojo, MD PhD, Satoshi Nishioka,<br />
MD PhD, Ako Central Hospital, Ako city, Japan<br />
P488 SINGLE PORT ACCESS CHOLECYSTECTOMY: SHORT-TERM<br />
OUTCOMES Shuji Kitashiro, Shunnichi Okushiba, Yo Kawarada, Yuma<br />
Ebihara, Tuyoshi Sasaki, Daisuke Miyasaka, Hiroyuki Katoh, tonan<br />
hospital<br />
P489 HYBRID NEEDLESCOPIC – SILS CHOLECYSTECTOMY VS<br />
LAPAROSCOPIC CHOLECYSTECTOMY: A PRELIMINARY COMPARISON<br />
IN ACUTE CHOLECYSTITIS Andreas Kiriakopoulos, MD, Dimitrios<br />
Tsakayannis, MD, Dimitrios Linos, MD, Hygeia Hospital, Athens, Greece<br />
P490 SINGLE PORT ACCESS SURGERY: EVALUATION OF ACCESS<br />
PLATFORMS, VERSATILITY AND FASCIAL DEFECTS Erica R Podolsky,<br />
MD, Paul G Curcillo, II MD FACS, Drexel University, College of Medicine,<br />
Department of Surgery<br />
P491 SINGLE-INCISION VERSUS CONVENTIONAL LAPAROSCOPIC<br />
APPENDICECTOMY: A COMPARATIVE STUDY Dennis Wong, FRACS,<br />
C N Shum, MRCS, H H Wong, MRCS, Kevin Yau, FRCS, Cliff Chung, FRCS,<br />
Michael Li, FRCS, Pamela Youde Nethersole Eastern Hospital<br />
12 th World Congress of Endoscopic Surgery<br />
175 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P492 TRANSUMBILICAL LAPAROSCOPIC ASSISTED APPENDECTOMY<br />
(TULAA) VERSUS CONVENTIONAL LAPAROSCOPIC APPENDECTOMY<br />
– PRELIMINARY RESULTS FROM A CASE CONTROL STUDY Robert<br />
Bergholz, MD, Ines Klein, Katharina Wenke, MD, Thomas Krebs, MD,<br />
Altona Children’s Hospital: Department of Pediatric Surgery, UKE -<br />
Medical School, Hamburg, Germany<br />
P493 LAPAROSCOPIC CHOLECYSTECTOMY FOR ASA III PATIENT’S<br />
IN DAY SURGERY. WHY NOT? Jonas Andriuškevicius, PhD, Zigmantas<br />
Urniežius, Dr, Tadas Pranckevicius, Dr, Martynas Jonkus, Dr, Department<br />
of Day Surgery, Kaunas district hospital, Kaunas, Lithuania<br />
P494 SINGLE PORT LAPAROSCOPIC SURGERY UNDER ABDOMINAL<br />
WALL LIFTING (LIFT-SPS) FOR APPENDECTOMY, HERNIA REPAIR,<br />
CHOLECYSTECTOMY Takashi Urushihara, PhD, Toshiyuki Itamoto,<br />
PhD, Hideki Nakahara, PhD, Yasuhiro Matugu, PhD, Toshihiko Kohashi,<br />
PhD, Takayuki Kadoya, PhD, Hiroyuki Egi, PhD, Ichiro Oomori, PhD,<br />
Department of General Surgery,Hiroshima Prefectural Hospital<br />
P495 DEVELOPMENT OF A NEW SURGICAL PROCEDURE, TWO-<br />
STEP TOTAL LAPAROSCOPIC HYSTERECTOMY COMBINED<br />
MYOMECTOMY(TTLH-CM), FOR DIFFICULT CASES OF LH Eiji Nishio,<br />
Yutaka Hirota, Akira Yasue, Haruki Nishizawa, Kazuhiko Tsukada, Yasuhiro<br />
Udagawa, Fujita Health UNIVERSITY SCHOOL OF MEDCINE<br />
P496 DIAGNOSTIC EFFICACY OF LAPAROSCOPIC BIOPSY FOR INTRA-<br />
ABDOMINAL LYMPHADENOPATHY S Wiebe, MD, D Klassen, MD,<br />
Queen Elizabeth II Health Sciences Centre, Halifax, Nova Scotia, Canada<br />
P497 MEASURING ESOPHAGOGASTRIC JUNCTION DISTENSIBILITY<br />
PERIOPERATIVELY AT HELLER MYOTOMY FOR ACHALASIA USING<br />
ENDOFLIP® Silvana Perretta, MD, Barry P McMahon, MSc PhD, Bernard<br />
Dallemagne, MD, 1. IRCAD-EITS,Department of Gastrointestinal and<br />
Endocrine Surgery, University of Strasborg, France 2. Dept of Medical<br />
Physics & Clinical Engineering, AMNCH, Dublin 24, Ireland<br />
P498 FINDING OF BRANCHES OF THE RECURRENT LARYNGEAL NERVE<br />
IN ENDOSCOPIC THYROIDECTOMY Yoshifumi Ikeda, MD, Junichi<br />
Takayama, MD, Naomi Morita, MD, Hiroshi Takami, MD, Department of<br />
Surgery, Teikyo University School of Medicine<br />
P499 SUPERIOR MESENTERIC ARTERY SYNDROME FOLLOWING<br />
LAPAROSCOPIC-ASSISTED PROCTOCOLECTOMY AND ILEAL<br />
J-POUCH-ANAL ANASTOMOSIS IN A PEDIATRIC PATIENT. Hamed<br />
Taheri, MD, Peter A Mattei, MD, The Children’s Hospital Of Philadelphia<br />
P500 LAPAROSCOPIC APPROACH FOR PHEOCROMOCYTOMA LARGER<br />
THEN 6 CM Roxana Ganescu, MD, Sorin Paun, MD PhD, Mircea Beuran,<br />
MD PhD, Mihaela Vartic, MD PhD, Diana Paun *, MD PhD, Constantin<br />
Dumitrache *, MD Phd, Emergency Hospital Bucharest Romania, *<br />
National Institute of Endocrinology C.I. Parhon<br />
P501 A DEVICE OF OPERATIVE METHOD FOR LAPAROSCOPIC<br />
SUBTOTAL HYSTERECTOMY. Akira Yasue, Eiji Nishio, Haruki Nishizawa,<br />
Kazuhiko Tsukada, Yutaka Hirota, Yasuhiro Udagawa, Dept. Obstetrics<br />
and Gynecology, Fujita Health University School of Medicine<br />
P502 THE INITIAL CANADIAN EXPERIENCE WITH SINGLE INCISION<br />
LAPAROSCOPIC SURGERY Benjamin D Teague, MBBS BA, Matthew<br />
S Butler, MD BSc, Pierre Y Garneau, MD, Clifford B Sample, MD, Anil<br />
Kapoor, MD, Margherita O Cadeddu, MD, Mehran Anvari, PhD, Centre<br />
for Minimal Access Surgery, St Josephs Healthcare ,McMaster University.<br />
Service de Chirurgie Générale, Hôpital du Sacré-Coeur de Montreal,<br />
Université de Montréal. Centre for Advancement of Minimally Invasive<br />
Surgery, University of Alberta. Canada.<br />
P503 LAPAROSCOPIC “SUDECK” SUTURE RECTOPEXY FOR ELDERLY<br />
PATIENTS Kengo Kanetaka, PhD MD, Yujo Kawashita, PhD MD,<br />
Shinichiro Ono, MD, Toru Iwata, PhD MD, Takashi Kanematsu, MD<br />
PhD, Department of Surgery, Nagasaki University, Graduate School of<br />
Biomedical Sciences<br />
P504 A NOVEL MINIMALLY INVASIVE TECHNIQUE FOR FORMING<br />
COMPRESSION GASTROJEJUNOSTOMY WITH IMMEDIATE<br />
DRAINAGE Benjamin D Teague, MBBS BA, Margherita O Cadeddu, MD,<br />
William D Fox, BSMT, Mehran Anvari, PhD, Paul Swain, MD, Centre for<br />
Minimal Access Surgery, St Joseph’s Healthcare, McMaster University,<br />
Hamilton, Ontario, Canada. Ethicon Endosurgery, Cincinnati, USA.<br />
Imperial College, London, UK.<br />
P505 INTRODUCER PEG (IPEG): THE TECHNIQUE FOR ENTERAL<br />
ACCESSING IN ADVANCED OROPHARYNGEAL CANCER PATIENT<br />
Suthep Udomsawaengsup, MD, Amarit Tansawet, MD, Suppa-ut<br />
Pungpapong, MD, Chadin Tharavej, MD, Patpong Navicharern, MD,<br />
Chula Minimally Invasive Surgery Center, Department of Surgery,<br />
Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand.<br />
P506 MANAGEMENT OF RETAINED GALLBLADDER/ CYSTIC DUCT<br />
REMNANT POST-CHOLECYSTECTOMY Sanjeev Singla, Dr, Varun Gupta,<br />
Dr, Sushil Budhiraja, Dr, Dayanand Medical College & Hospital, Ludhiana,<br />
India<br />
P507 LAPAROSCOPIC OMENTOPLASTY FOR BRONCHIAL STUMP<br />
REINFORCEMENT IN PNEUMONECTOMY PATIENT. Masanobu Hagiike,<br />
MD PhD, Tatsushi Inoe, MD, Minoru Ohshima, MD, Yasuyuki Suzuki, MD,<br />
Department of Gastroenterological surgery, Kagawa University, Japan<br />
P508 ENDOSCOPIC MANAGEMENT OF POST TRAUMATIC HEPATIC<br />
ARTERY ANEURYSM Varun Gupta, Sanjeev Singla, Sushil Budhiraja,<br />
Dayanand Medical College & Hospital, Ludhiana, India<br />
P509 USEFULNESS OF COAGULATING SHEARS IN SUBFASCIAL<br />
ENDOSCOPIC PERFORATOR VEIN SURGERY Akihito Abe, PhD, Nobumi<br />
Tagaya, PhD, Yuki Sakuraoka, MD, Masatsugu Tachibana, PhD, Kubota<br />
Keiichi, PhD, Second Department of Surgery, Dokkyo Medical University,<br />
Tochigi, Japan<br />
P510 SIMULTANOUS EMERGENCY AND ELECTIVE SURGERY IN A<br />
SINGLE LAPAROSCOPIC SESSION: IS IT SAFE ? Ibrahim Ahmed, FRCSI,<br />
Elnazier Ibrahim, FRCSI, Alexander Lockley, MBCh, Olumide Fagbeja,<br />
FRCSI, Saeed Khan, FRCSI, Our Lady’s Hospital, Navan, Ireland<br />
P511 CAMERA-LESS PERITONEAL ENTRY FOR UROLOGIC (C-PET)<br />
LAPAROSCOPY: DESCRIPTION OF A NOVEL TECHNIQUE Ricardo A<br />
Rendon, MD, Amit Rajguru, MD, William Carlson, MD, Griffeth W Tully,<br />
MD, Queen Elizabeth II Health Sciences Centre<br />
P512 A SCARLESS CHOLECYSTECTOMY MADE EASY BY THE HIDDEN<br />
SUPRAPUBIC APPROACH Angel Martinez-Munive, MD, Fernando<br />
Quijano-Orvananos, MD FACS, Rafael Padilla-Longoria, MD DSc FRCSC,<br />
ABC Medical Center IAP<br />
P513 DEVELOPMENT OF NEW METHODS AND DEVICES FOR FORMING<br />
MINIMALLY INVASIVE ANASTOMOSES - TOWARDS A COMPRESSION<br />
ENTERAL ANASTOMOSIS WITH IMMEDIATE DRAINAGE Margherita<br />
O Cadeddu, MD, Benjamin D Teague, MBBS BA, William D Fox, BSMT,<br />
Charles A Mosse, MD, Mehran Anvari, PhD, Paul Swain, MD, Centre for<br />
Minimal Access Surgery, St Joseph’s Healthcare, McMaster University,<br />
Hamilton, Canada. Ethicon Endosurgery, Cincinatti, USA. Imperial<br />
College, London, UK.<br />
P514 SCARLESS LAPAROSCOPIC APPENDECTOMY BY HIDDEN<br />
SUPRAPUBIC APPROACH Angel Martinez-Munive, MD, Fernando<br />
Quijano-Orvananos, MD FACS, Rafael Padilla-Longoria, MD DSc FRCSC,<br />
ABC Medical Center IAP<br />
P515 SINGLE INCISION ENDO-LAPAROSCOPIC SURGERY A<br />
PROSPECTIVE STUDY Michael M Lawenko, MD, Alembert Lee-Ong,<br />
MD, Javier Lopez-Gutierrez, MD, Charles Tan, MD, Yoke Fai Fong, MD,<br />
Jimmy So, MD, Cheah Wei Kit, MD, Davide Lomanto, MD, Minimally<br />
Invasive Surgical Centre, Department of Surgery, Yong Loo Lin School of<br />
Medicine, National University Health System - Singapore<br />
P516 PROSPECTIVE COMPARATIVE THERAPIES FOR PORTAL<br />
HYPERTENSION USING LAPAROSCOPY AND OPEN AZYGOPORTAL<br />
DISCONNECTION Yangwen Zhu, MD, Yuedong Wang, MD FACS, Zhijie<br />
Xie, MD, Xiaoli Zhan, MD, Zaiyuan Ye, MD, Department of General Surgery,<br />
Zhejiang Provincial People’s Hospital, Hangzhou 310014, China<br />
12 th World Congress of Endoscopic Surgery 176
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P517 SUMMARY OF FIVE CASES HALS-NEPHRECTOMY AND DISTAL<br />
PANCREATECTOMY: MINIMALLY INVASIVE APPROACH FOR<br />
DONOR OPERATION OF SIMULTANEOUS PANCREAS AND KIDNEY<br />
TRANSPLANT Naotake Akutsu, MD, Michihiro Maruyama, MD, Kenichi<br />
Saigo, MD, Chikara Iwashita, MD, Kazunori Otsuki, MD, Taihei Ito, MD,<br />
Takashi Kenmochi, MD, Department of Surgery, Chiba-East National<br />
Hospital, National Hospital Organization, Japan<br />
P518 COST SAVINGS ANALYSIS OF REUSABLE VERSUS DISPOSABLE<br />
TROCARS Tejwant S Datta, MD, Richard Lee, Marianne Franco, MD, Zaki<br />
Busbaih, MD, Amit Kaul, MD, Omer Nasir, MD, Anne O Lidor, MD, Hien<br />
Nguyen, MD, Michael R Marohn, DO, The Johns Hopkins University<br />
P519 LAPAROSCOPIC HYSTERECTOMY OF INTRALIGAMENTOUS<br />
FIBROIDS IN OUR HOSPITAL Haruki Nishizawa, Yutaka Hirota, Akira<br />
Yasue, Eiji Nishio, Kazuhiko Tsukada, Yasuhiro Udagawa, Department of<br />
Obstetrics and Gynecology, Fujita Health University School of Medicine<br />
P520 OUTCOMES OF SINGLE INCISION CHOLECYSTECTOMIES IN<br />
A NON-SELECT PATIENT GROUP Jacqueline J Wu, MD, Anthony L<br />
McCluney, MD, Anaeze C Offodile, MD, Ali Tavakkoli-zadeh, MD, Brigham<br />
and Women’s Hospital<br />
P521 SLEEVE GASTRECTOMY FOR THE TREATMENT OF DIABETIC<br />
GASTROPARESIS Melissa B Bagloo, MD, Aku Ude, MD, Marc Bessler, MD,<br />
New York Presbyterian Hospital<br />
P522 COMPUTER GUIDED SINGLE INCISION LAPAROSCOPIC<br />
SURGERY AND NOTES USING INTRAOPERATIVE MAGNETIC 3D GPS<br />
NAVIGATION SYSTEM Maki Sugimoto, MD PhD, Yoshinori Morita, MD<br />
PhD, Yuichiro Matsuoka, PhD, Hayato Yoshinaka, MD, Kagayaki Kuroda,<br />
PhD, Takeshi Azuma, MD Prof, Gastroenterology, Kobe University, Kobe,<br />
Hyogo, Japan, Veterans Affairs Palo Alto Health Care System, Stanford<br />
University, Palo Alto, CA, USA Molecular Imaging Research, Institute of<br />
Biomedical Research and Innovation, Kobe, Hyogo, Japan<br />
P523 LAPAROSCOPIC COMMON BILE DUCT EXPLORATION AND<br />
CURRENT MANAGEMENT OF COMMON BILE DUCT STONES.<br />
EXPERIENCE AT THE UNIVERSITARY HOSPITAL OF CARACAS-<br />
VENEZUELA Alexis Sanchez, MD, Omaira Rodriguez, MD, Renata<br />
Sanchez, MD, Gustavo Benitez, MD, Omar Bellorin-Marin, MD,<br />
Universitary Hospital of Caracas, Caracas-Venezuela. Central University<br />
of Venezuela<br />
P524 DIAGNOSTIC LAPAROSCOPY IS HELPFUL IN PERITONEAL<br />
DIALYSIS PATIENTS WITH ACUTE SCROTAL EDEMA Stephen Haggerty,<br />
MD, Jay Jorge, MD, NorthShore University Healthsystem, Evanston,<br />
Illinois, USA<br />
P525 A NEW APPROACH FOR LAPAROSCOPIC RESECTION OF<br />
SUBMUCOSAL TUMOR ON UPPER PORTION OF THE STOMACH Hun-<br />
Jin Kim, MD, Hoi-Won Kim, MD, Mi-Ran Jung, MD, Ho-Kun Kim, MD,<br />
Oh Cheong, MD, Young-Kyu Park, MD, Seong-Yeob Ryu, MD, Dong-Yi<br />
Kim, MD, Young-Jin Kim, MD, Division of Gastroenterologic Surgery,<br />
Department of Surgery, Chonnam National University Medical School.<br />
Gwangju, South Korea<br />
P526 FIRST EXPERIENCE OF SINGLE PORT ACCESSORY SPLENECTOMY<br />
IN PATIENT WITH AUTOIMMUNE HEMOLYTIC ANEMIA. Roman V<br />
Petrov, MD, Nikolaos Chandolias, MD, Paul T Singh, MD, Department of<br />
Surgery, Albany MedicalCenter<br />
P527 MULTICENTER EXPERIENCE WITH NON-ISCHEMIC<br />
LAPAROSCOPIC NEPHRON SPARING SURGERY UTILIZING HABIB<br />
4X BIPOLAR RADIOFREQUENCY ABLATION COAGULATOR Wassim<br />
M Bazzi, MD, Sijo Parekattil, MD, Mohamad Allaf, MD, Jared Berkowitz,<br />
MD, Hany Atalah, MD, Ithaar H Derweesh, MD, University of California<br />
San Diego, University of Florida, Gainesville and the Brady Urological<br />
Institute, Johns Hopkins University<br />
P528 PROSPECTIVE COMPARISON OF SINGLE SITE AND TRADITIONAL<br />
LAPAROSCOPY FOR UPPER URINARY TRACT SURGERY: INITIAL<br />
OUTCOMES Wassim M Bazzi, MD, Elana Godebu, MD, Jonathan<br />
Silberstein, MD, Ronald Im, MD, Kyoko Sakamoto, MD, Tracy M Downs,<br />
MD, Christopher J Kane, MD, Ithaar H Derweesh, MD, University of<br />
California San Diego, San Diego, CA, USA<br />
P529 SINGLE PORT LAPAROSCOPIC SURGERY FOR GASTRIC<br />
SUBMUCOSAL TUMOR USING OCTO(TM) PORT Seong-Yeob Ryu, MD,<br />
Hun-Jin Kim, MD, Hoi-Won Kim, MD, Mi-Ran Jung, MD, Ho-Kun Kim,<br />
MD, Oh Cheong, MD, Young-Kyu Park, MD, Jai-Kyun Joo, MD, Dong-Yi<br />
Kim, MD, Young-Jin Kim, MD, Division of Gastroenterologic Surgery,<br />
Department of Surgery, Chonnam National University Medical School.<br />
Gwangju, South Korea<br />
P530 LAPAROENDOSCOPIC SINGLE SITE SURGERY: A SINGLE<br />
INSTITUTION EXPERIENCE Michael J Guzman, MD, Joshua A Waters,<br />
MD, Don J Selzer, MD, Bruce W Robb, MD, Eric A Wiebke, MD MBA,<br />
Virgilio V George, MD, Indiana University School of Medicine<br />
P531 SINGLE INCISION LAPAROSCOPIC SURGERY: ONE SURGEON’S<br />
EXPERIENCE Kristine O’Hara, MD, Balaji Jangam, MD, Bruce Bernstein,<br />
PhD, Ibrahim M Daoud, MD, St. Francis Hospital and Medical Center,<br />
Hartford, CT<br />
P532 SINGLE INCISION LAPAROSCOPIC COLORECTAL SURGERY -<br />
INITIAL EXPERIENCES AND LEARNING CURVE Matthew S Butler,<br />
MD, Benjamin D Teague, MBBS BA, Federico Pampaloni, MD, Mehran<br />
Anvari, PhD, Centre for Minimal Access Surgery, St Joseph’s Healthcare,<br />
McMaster University, Hamilton, Ontario, Canada<br />
P533 SINGLE INCISION ACCESS CHOLECYSTECTOMY VS<br />
LAPAROSCOPIC Ali Fardoun, MD, Fawaz Torab, phd, Tawam<br />
P534 MIS TRAINING IN CANADA: THE STAFF SURGEONS’<br />
PERSPECTIVE. Alia P Qureshi, MD, Ashley Vergis, MD, Carolina M<br />
Jimenez C.M, Jessica Green, medical student, Aurora D Pryor, MD,<br />
Christopher Schlachta, MD, Allan Okrainec, MD, 1. University of Toronto,<br />
Department of Surgery, 2. University Health Network, Toronto Western<br />
Hospital 3. Duke Minimally Invasive Surgery at Durham Regional<br />
Hospital 4. University of Western Ontario<br />
P535 PAEDIATRIC LAPAROSCOPIC APPENDICECTOMY IN AN ADULT<br />
UNIT- A TEN YEAR EXPERIENCE Nikhil Pawa, MD, Justin K Lawrence,<br />
MD, Matthew G Tutton, MD, Tan Arulampalam, MD, Roger W Motson,<br />
MD, ICENI Centre, Colchester University Hospital, Colchester, UK<br />
P536 ENDOCRINE COMORBIDITIES AND LAPAROSCOPIC SURGERY<br />
FOR ADRENAL PATHOLOGY – OUR EXPERIENCE Roxana Ganescu, MD,<br />
Sorin Paun, MD PhD, Mircea Beuran, MD PhD, Mihaela Vartic, MD PhD,<br />
Diana Paun *, MD PhD, Constantin Dumitrache *, MD PhD, Emergency<br />
Hopsital Bucharest Romania. * National Institute of Endocrinology C. I.<br />
Parhon. Bucharest. Romania<br />
P537 SINGLE-INCISION LAPAROSCOPIC RIGHT HEMICOLECTOMY:<br />
SAFETY AND FEASIBILITY IN A SERIES OF 10 CONSECUTIVE CASES<br />
Diego I Ramos-Valadez, MD, Chirag B Patel, MSE, Madhu Ragupathi,<br />
MD, T. Bartley Pickron, MD, Eric M Haas, MD FACS, Division of Minimally<br />
Invasive Colon and Rectal Surgery, Department of Surgery, University of<br />
Texas Medical School at Houston, Houston, Texas<br />
P538 ADVANCED LAPAROENDOSCOPIC SINGLE SITE PROCEDURES<br />
Fernando Arias, MD FACS, Monica Rodriguez, Adolfo Torres, Jairo<br />
Dussan, Carlos Aguilar, MD, Daniel Carrillo, MD, Beatriz Angulo, Isabel<br />
Cañon, MD, Fundación SantaFe de Bogotá<br />
P539 SINGLE PORT CHOLECYSTECTOMY: SMALL SCAR, SHORT<br />
LEARNING CURVE Daniel Solomon, MD, Robert Bell, MD, Andrew Duffy,<br />
MD, Kurt Roberts, MD, Yale University School of Medicine<br />
P540 TRANSUMBILICAL MINIMALLY INVASIVE SURGERY (TUMIS): THE<br />
EARLY EXPERIENCE IN A TERTIARY CARE CENTER Candace Y Williams-<br />
Covington, MD, John A Primomo, MD, Vadim Sherman, MD, Baylor<br />
College of Medicine<br />
P541 SINGLE SITE WIRELESS LAPAROSCOPY IN ANIMAL MODEL<br />
Fernando Arias, MD FACS, Adolfo Torres, Jairo Dussan, Carlos Aguilar,<br />
MD, Beatriz Angulo, Pedro Merlano, Sara Vergara, Miguel Sarmiento,<br />
Fundación SantaFe de Bogotá<br />
P542 SINGLE INCISION LAPAROSCOPIC SPLENECTOMY: A CASE<br />
SERIES COMPARISON TO LAPAROSCOPIC SPLENECTOMY Michael<br />
G Doorly, MD, Brian Binetti, MD, Tejinder P Singh, MD, Albany Medical<br />
Center<br />
12 th World Congress of Endoscopic Surgery<br />
177 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P543 SINGLE PORT ENDO-LAPAROSCOPIC SURGERY (SPES) FOR<br />
MULTIPLE PROCEDURES Michael M Lawenko, MD, Javier Lopez-<br />
Gutierrez, MD, Alembert Lee-Ong, MD, Asim Shabbir, MD, James Mok,<br />
MD, Sarah Chian, Jimmy So, MD, Davide Lomanto, MD PhD, Minimally<br />
Invasive Surgical Centre, Department of Surgery, Yong Loo Lin School of<br />
Medicine, National University Health System - Singapore<br />
P544 DEFLECTABLE TIP LAPAROSCOPE DECREASES OPERATION<br />
TIME AND BLOOD LOSS DURING SINGLE INCISION LAPAROSCOPIC<br />
CHOLECYSTECTOMY. Mohammed R Salabat, MD, Woody Denham, MD,<br />
Jin Zhao, MD, Michael B Ujiki, NorthShore University Health System<br />
P545 BENEFITS OF LAPAROSCOPY FOR VENTRICULOPERITONEAL<br />
SHUNT PLACEMENT Yu Liang, MD, Anne Roberts, BS, Julie<br />
Monteagudo, BS, Sean B Orenstein, MD, Patrick B Senatus, MD, Hillary<br />
Onyiuke, MD, Yuri W Novitsky, MD, University of Connecticut Healh<br />
Center, Farmington, CT<br />
P546 CHOOSING THE COSMETICALLY SUPERIOR LAPAROSCOPIC<br />
ACCESSS TO THE ABDOMEN: THE IMPORTANCE OF THE NAVEL<br />
Monika E Hagen, MD MBA, Pouya Iranmanesh, MS, Oliver J Wagner,<br />
MG, Kari J Thompson, MD, Santiago Horgan, MD, Philippe Morel, PhD,<br />
Division of Digetsive Surgery, University Hospital Geneva & Center for<br />
the Future of Surgery, Department of Surgery, University of California<br />
San Diego<br />
P547 MENTORING FACILITATES ONCOLOGICALLY SOUND<br />
LAPAROSCOPIC COLON RESECTION A R Beaulieu, G K Kaban, MD<br />
FRCSC, Regina General Hospital, Regina Qu’Appelle Health District,<br />
University of Saskatchewan<br />
P548 CASE REPORT: GASTROINTESTINAL TRACT DUPLICATIONS<br />
TREATEMENT WITH LAPAROSCOPIC SURGERY Sergio Roll, MD PhD,<br />
German Hospital Oswaldo Cruz<br />
P549 INITIAL EXPERIENCE WITH SINGLE INCISION LAPAROSCOPIC<br />
SURGERY Emanuel Sporn, MD, Sebastian Roka, MD, Erwin Rieder, MD,<br />
Johannes Zacherl, MD, Gerhard Prager, MD, Department of Surgery -<br />
Medical University of Vienna<br />
P550 ACCEPTANCE OF SINGLE PORT ENDOSCOPIC SURGERY (SPES),<br />
NOTES AND LAPAROSCOPIC SURGERY IN A COHORT OF SURGICAL<br />
PATIENTS Javier Lopez Gutierrez, MD, Michael Lawenko, MD, Alembert<br />
Lee Ong, MD, Sarah Chian, Davide Lomanto, MD PhD, Minimally Invasive<br />
Surgical Centre, Dept.Surgery, National University Health System,<br />
National University of Singapore. Singapore Management University,<br />
Department of Sociology, Singapore. CMN 20 de Noviembre, ISSSTE,<br />
Mexico.<br />
P551 PICTORIAL DOCUMENTATION OF LAPAROSCOPIC<br />
CHOLECYSTECTOMY Prasanta Raj, MD MS FACS, Neilendu Kundu, MD,<br />
Fairview Hospital / Cleveland Clinic Health Systems<br />
P552 THE CURRENT STATUS OF LAPARO-ENDOSCOPIC SINGLE-<br />
SITE SURGERY (LESS) ACROSS SURGICAL DISCIPLINES, A SINGLE<br />
INSTITUTION’S EXPERIENCE. J Taylor, N Hubbard, R Atkins, N Mishra,<br />
V Gunabushanam, M Schwartz, N Wainganker, M Ostrowitz, D Eschete,<br />
E Rubach, L Richstone, L Kavoussi, L Gellman, D Gadaleta, H Zemon, M<br />
Nimaroff, G DeNoto, Northshore/LIJ Health System<br />
P553 ROBOTIC POSTERIOR RETROPERITONEAL ADRENALECTOMY:<br />
INITIAL REPORT Eren Berber, MD, Hizir Akyildiz, MD, Jamie Mitchell, MD,<br />
Mira Milas, MD, Allan E Siperstein, Cleveland Clinic<br />
P554 ROBOTIC-ASSISTED THYROIDECTOMY USING A GASLESS<br />
TRANSAXILLARY APPROACH: A PRELIMINARY EXPERIENCE Dimitrios<br />
Linos, MD, Andreas Kiriakopoulos, MD, Efthimios Poulios, MD, Hygeia<br />
Hospital, Athens, Greece<br />
P555 LAPAROSCOPIC SPLENECTOMY: CONVENTIONAL VERSUS<br />
ROBOTIC APPROACH: A COMPARATIVE STUDY Roberta Gelmini (1),<br />
MD PhD, Chiara Franzoni (1), MD, Alessandro Spaziani (2), MD, Alberto<br />
Patriti (2), MD, Luciano Casciola (2), MD, Massimo Saviano (1), MD PhD,<br />
University of Modena and RE - Dept. of Surgery(1) S. Matteo degli<br />
Infermi Hospital Spoleto - Dept of Surgery (2) ITALY<br />
P556 ENHANCING ROBOT-ASSISTED FUNDAMENTAL SURGICAL<br />
PROFICIENCY USING PORTABLE VIRTUAL SIMULATOR Jung H<br />
Chien, Irene H Suh, Mukul Mukherjee, PhD, Shi-Hyun Park, PhD, Dmitry<br />
Oleynikov, MD, Ka-Chun Siu, PhD, University of Nebraska Medical Center<br />
P557 ROBOTIC FOREGUT SURGERY: ONE SURGEON’S EXPERIENCE<br />
WITH NISSEN FUNDOPLICTION, ESOPHAGOMYOTOMY, AND HIATAL<br />
HERNIA REPAIR Robin A Alley, MD, Franziska Huettner, MD PhD, Jamie<br />
Doubet, RN, Michael J Ryan, MS, Danuta I Dynda, MD, David L Crawford,<br />
MD, University of Illinois College of Medicine, Peoria, IL<br />
P558 COMPARISON BETWEEN ROBOTIC AND LAPAROSCOPIC<br />
GASTRECTOMY WITH EXTRAPERIGASTRIC LYMPHNODE<br />
DISSECTION FOR ADVANCED GASTRIC CANCER Kazuki Inaba, MD,<br />
Geon-Ung Heo, MD, Woo Jin Hyung, MD PhD, Sung Hoon Noh, MD PhD,<br />
Department of Surgery, Yonsei University College of Medicine<br />
P559 ROBOTIC VERSUS LAPAROSCOPIC TOTAL MESORECTAL<br />
EXCISION OF RECTAL CANCER. A COMPARATIVE STUDY OF<br />
ONCOLOGICAL SAFETY AND SHORT-TERM OUTCOMES PP Bianchi,<br />
MD, C Ceriani, MD, A Locatelli, MD, B Andreoni, MD, Unit of Minimally-<br />
Invasive Surgery. European Institute of Oncology. Milano. Italy<br />
P560 FEASIBILITY OF TRANSVAGINAL PERITONEOSCOPY USING<br />
NOVEL ARTICULATED STEREO-LAPAROSCOPE ROBOT. Mikael<br />
Sodergren, MRCS, James Clark, MRCS, David Noonan, MSc, Jianzhong<br />
Shang, PhD, Christopher Payne, MSc, David James, MRCS, Thanos<br />
Athanasiou, PhD, Teare Julian, MD, Ara Darzi, FRCS KBE, Yang Guang-<br />
Zhong, PhD, Department of Biosurgery and Surgical Technology and the<br />
Institute of Biomedical Engineering; Imperial College London, UK.<br />
P561 A NOVEL ARTICULATED ROBOTIC LAPAROSCOPE FOR SINGLE<br />
INCISION AND NATURAL ORIFICE SURGICAL APPLICATIONS;<br />
PRELIMINARY USABILITY TRIALS IN A LIVE PORCINE MODEL. James<br />
Clark, MRCS, Mikael Sodergren, MRCS, David Noonan, MSc, Shang<br />
Jianzhong, PhD, Christopher Payne, MSc, David James, MRCS, Julian<br />
Teare, MD, Thanos Athanasiou, PhD, Ara Darzi, FRCS KBE, Yang Guang-<br />
Zhong, PhD, Department of Biosurgery and Surgical Technology and the<br />
Institute of Biomedical Engineering; Imperial College London, UK.<br />
P562 LAPAROBOTIC APPROACH TO ADRENALECTOMY Emil Shakov,<br />
MD, Anusak Yiengpruksawan, MD, Atthaphorn Trakarnsanga, MD,<br />
Shankar Raman, MD, The Valley Hospital<br />
P563 ROBOTIC-ASSISTED LAPAROSCOPIC SURGERY FOR<br />
DIVERTICULITIS: EXPERIENCE IN 19 CONSECUTIVE CASES AND A<br />
REVIEW OF THE LITERATURE Madhu Ragupathi, MD, Diego I Ramos-<br />
Valadez, MD, Chirag B Patel, MSE, Eric M Haas, MD FACS, Division of<br />
Minimally Invasive Colon and Rectal Surgery, Department of Surgery,<br />
University of Texas Medical School at Houston, Houston, Texas<br />
P564 STEPWISE PROGRESSION TO TOTALLY ROBOTIC BYPASS<br />
Arundathi Rao, MD, Erik B Wilson, MD, Brad Snyder, MD, Eduardo Parra-<br />
Davila, MD FACS FACCRS, Keith C Kim, MD, Department of Bariatric<br />
Surgery at Florida Hospital Celebration Health<br />
P565 ROBOTIC NISSEN FUNDOPLICATION REVISION Niazy m Selim, MD<br />
MBChB PhD FACS, Tamer Dabous, MD, University of Kansas<br />
P566 LEARNING CURVE FOR ROBOTIC-ASSISTED LAPAROSCOPIC<br />
COLORECTAL SURGERY OF THE PELVIS: ANALYSIS OF 50<br />
CONSECUTIVE CASES Chirag B Patel, MSE, Diego I Ramos-Valadez,<br />
MD, Madhu Ragupathi, MD, Malak Bokhari, MD, Eric M Haas, MD FACS,<br />
Division of Minimally Invasive Colon and Rectal Surgery, Department of<br />
Surgery, University of Texas Medical School at Houston, Houston, Texas<br />
P567 CASE REPORT: LAPAROSCOPIC ADRENALECTOMY FOR<br />
BILATERAL METACHRONOUS ALDOSTERONOMAS Piotr Gorecki, MD,<br />
Philippe Rizek, MSc, Aristid Lindenmayer, MD, Sabita Moktan, MD, New<br />
York Methodist Hospital, Brooklyn, NY<br />
P568 COMBINED ANTERIOR AND POSTERIOR APPROACH FOR<br />
STAPLESS LAPAROSCOPIC SPLENECTOMY; TOWARDS SAFE<br />
AND ECONOMIC LAPAROSCOPIC SPLENECTOMY Ahmed A Nada,<br />
AProfessor, Ayman El Samadoni, AProfessor, Amr Mohsen, Professor,<br />
Department of surgery, Faculty of Medicine, Cairo University, Egypt<br />
12 th World Congress of Endoscopic Surgery 178
<strong>2010</strong> Poster Listing<br />
Full abstract texts available in the Electronic Meeting Guide<br />
P569 A REVIEW OF PERIOPERATIVE COMPLICATIONS IN 120<br />
CONSECUTIVE COMMUNITY BASED LAPAROSCOPIC DONOR<br />
NEPHRECTOMIES John F Lazar, MD, Harold Yang, MD PhD, Harrisburg<br />
Hospital<br />
P570 LAPAROSCOPIC MANAGEMENT OF CYSTIC LESIONS OF SPLEEN<br />
Mohan Narasimhan, Kumar Palaniappan, Sourav Kalia, Ramesh<br />
Ardhanari, Department of surgery and Gastroenterology, Meenakshi<br />
Mission Hospital & Research Center, Madurai<br />
P571 A LARGE SINGLE INSTITUTION CASE SERIES OF LAPAROSCOPIC<br />
SPLENECTOMY FOR BENIGN AND MALIGNANT SPLENIC MASSES<br />
Haris Khwaja, MD DPhil, Fady Moustarah, MD MPH, Joseph Talarico, MD,<br />
Tamara Kindelan, MD, Nabil Tariq, MD, Vikram Attaluri, MD, Bipan Chand,<br />
MD, Matthew Kroh, MD, Stacy Brethauer, MD, Tomasz Rogula, MD, Philip<br />
Schauer, MD, Steven Rosenblatt, MD, Surgery Institute, Cleveland Clinic<br />
Foundation, Cleveland, Ohio<br />
P572 LAPAROSCOPIC SPLENECTOMY IN TRAUMA: BENEFIT OR<br />
BURDEN? Lucian Panait, MD, Tifany T Fancher, MD, Stanley J Dudrick,<br />
MD, Michael S Ajemian, MD, Saint Mary’s Hospital, Waterbury, CT<br />
P573 MINIMALLY INVASIVE DONOR NEPHRECTOMY USING A SUPRA-<br />
PUBIC APPROACH: INITIAL CLINICAL EXPERIENCE Ajai Khanna, MD<br />
PhD, Monika E Hagen, Santiago Horgan, MD, Section of Transplant<br />
Surgery, Center for the Future of Surgery, Department of Surgery,<br />
University of California San Diego<br />
P574 STANDARDIZED TRANS-ABDOMINAL SUTURING WITH THE<br />
IMESH STITCHER DEVICE Daniel R Marcus MD, Bruce Ramshaw MD,<br />
Yoav Mintz MD, Izhak Fabian, Nir Altman, Ofir Rimer, St Johns Health<br />
Center, Santa Monica CA, University Of Missouri, Columbia , Missouri,<br />
Hadassah Medical Center, Jerusalem, Israel<br />
12 th World Congress of Endoscopic Surgery<br />
179 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Emerging Technology Oral Abstracts<br />
ET01<br />
NOVEL HANDHELD PET PROBES PROVIDE INTRAOPERATIVE<br />
LOCALIZATION OF MALIGNANT LYMPH NODES Segundo J Gonzalez,<br />
MD, Joyce Wong, MD, Lorena Gonzalez, MD, Peter Brader, MD, Mithat<br />
Gönen, Maureen Zakowski, MD, Yuman Fong, MD, Vivian Strong, MD<br />
Departments of Surgery,1 Radiology,2 Pathology,3 and Epidemiology and<br />
Biostatistics,4; Memorial Sloan-Kettering Cancer Center, New York, NY,<br />
10065 USA<br />
Introduction: Positron emission tomography (PET) scanning is a helpful<br />
preoperative modality to detect sites of malignancy, however, for<br />
identification of smaller deposits such as suspicious lymph nodes it is<br />
not as reliable. A tool to identify such nodes intraoperatively may aid in<br />
improving sampling quality, provide better staging, and decrease overall<br />
intraoperative time. We investigated the ability of a novel, minimally<br />
invasive tool to localize these suspicious nodes intraoperatively.<br />
Methods: Ten female rats were inoculated with a lymphogenic tumor line<br />
and followed weekly with PET scan studies using 18F-2-fluoro-2-deoxy-<br />
D-glucose (18F-FDG) radiotracer. When suspicious nodes were found,<br />
animals were sacrificed for tissue harvesting, intraoperative radiotracer<br />
uptake counts, and later pathological analysis of these nodal tissues. The<br />
amount of radiation uptake was analyzed as tumor to background ratio<br />
(TBR) for its correction with the background uptake within each animal.<br />
Results: The intraoperative probe was used to guide dissections and<br />
select high risk nodes based on their specific radiotracer uptake. A total of<br />
52 nodes were harvested, eight of these being suspicious on preoperative<br />
PET scan studies. Using a TBR of 2.5, the intraoperative probes were<br />
able to localize all suspicious nodes previously seen on PET scan. Both<br />
gamma (sensitivity: 100%; specificity: 86%; positive predictive value (PPV):<br />
57%; negative predictive value (NPV): 100%) and beta (sensitivity: 88%;<br />
specificity: 91%; positive predictive value (PPV): 64%; negative predictive<br />
value (NPV): 98%) probes showed an excellent area under the curve (AUC)<br />
in the receiver operating characteristic analysis (ROC). Gamma probe had<br />
an AUC of 0.911 (95% C.I.:0.83-0.99), and beta had an AUC of 0.98 (95%<br />
C.I.: 0.94-1.0). Furthermore, its ability to specifically detect malignant<br />
nodes was also analyzed, with comparable statistical results.<br />
Conclusion: This novel tool reliably localized suspicious nodes identified<br />
on PET scan, which were subsequently confirmed malignant on histology.<br />
This device may be used synergistically with the PET scan exam to<br />
maximize intraoperative nodal selection and sampling.<br />
ET02<br />
SINGLE CENTER EXPERIENCE WITH A NOVEL PURELY ENDOLUMINAL<br />
FUNDOPLICATION DEVICE Ozanan R Meireles, MD, Julietta Paleari,<br />
MD, Noam Belkind, MD, Kari Thompson, MD, Michael Sedrak, MD, Garth<br />
Jacobsen, MD, Mark A Talamini, MD, Santiago Horgan, MD University of<br />
California-San Diego<br />
Background: Gastroesophageal reflux disease (GERD) has a high<br />
prevalence in the Western World. The surgical treatment of GERD has<br />
evolved from open surgery to robotic assisted anti-reflux operations,<br />
offering patients less invasive treatment options while improving<br />
outcomes. In trying to deliver the similar outcomes of laparoscopic<br />
surgery with less invasive approaches, endoluminal techniques have<br />
emerged as promising alternatives. This study aims to assess the safety<br />
and efficacy of a novel, computer monitored flexible endoluminal<br />
stapling system for the treatment of GERD. Methods: Under IRB approval,<br />
patients with history of GERD for at least 2 years, confirmed with 24h<br />
pH acid exposure test, and currently taking PPIs with significant relief of<br />
symptoms are being enrolled in our clinical trial. The exclusion criteria<br />
includes presence of hiatal hernia greater than 3 cm, Type III hiatal hernia<br />
of any size, presence of Barrett’s esophagus or grade IV esophagitis,<br />
esophageal stricture and any anatomical abnormality of the esophagus.<br />
A flexible endoscopic stapling system placed through the mouth was<br />
used under general anesthesia. Using a computer monitored system for<br />
stapling, an endoscopic fundoplications was created.<br />
Results: Four patients underwent endoscopic fundoplication. The<br />
average operative time was 78.75 minutes. The length of hospital stay<br />
was 1 day for all patients. No peri-operative complication occurred. All<br />
patients experienced relief of symptoms immediately after surgery.<br />
Conclusion: Our preliminary data demonstrates that purely endoluminal<br />
fundoplication is feasible, and that this novel flexible endoluminal<br />
stapling device is safe for human use. This system has the advantage<br />
of recreating key steps of conventional fundoplications with the<br />
unquestionable benefit of being much less invasive. Endoluminal<br />
therapies for GERD are promising, yet challenging, alternatives<br />
to laparoscopic fundoplications. Although our preliminary data<br />
demonstrates favorable results, a larger sample size is being gathered in<br />
coordination with other institutions in order to power a multi-centered<br />
study. Furthermore, long term outcomes must be obtained before<br />
considering this approach as the procedure of choice for the treatment of<br />
GERD.<br />
ET03<br />
CLEANOSCOPE: A CLEAR IMAGE AT ALL TIMES Barry Salky, MD, Daniel<br />
Sherwin, Mr, Ori Nesher, Mr, Noam Danenberg, Mr, Gadi Lotan, MD<br />
Cleanoscope, Ltd; The Mount Sinai Hospital, New York<br />
Objective: This device is designed to keep the view through a<br />
laparoscope or flexible endoscope clear at all times.<br />
Description: A rapidly spining optical disc(3000/minute) has been<br />
developed which does not allow liquids or solid particles to adhere to it.<br />
At present, it is designed to fit as an overtube. The overtube is made of a<br />
type of stainless steel that has FDA approval for medical procedures. The<br />
device can be incorporated into a laparoscope or flexible endoscope at<br />
the factory level, which, of course, would obviate an overtube. The optical<br />
disc spins rapidly, but this can not be detected by the hman ey or the<br />
image on the LCD/CRT. The device is patented.<br />
Results: Blood, iodine, fat, stool or other solid debris does not adhere<br />
to it. When the laparoscope passes through the trocar, the visual field<br />
remains clear at all times. Because of the heat generated by the motor/<br />
disc, fogging is no longer an issue.<br />
Conclusions: A completely clear video field is important in the<br />
performance of both basic and advanced laparoscopic and endoscopic<br />
surgery. This device keeps the video field clear at all times, and it will<br />
obviate taking the laparoscope out to clean it. In terms of flexible<br />
endoscopy, the channel now used for irrigation to clean the lens could be<br />
redesigned and made larger. That could benefit NOTES procedures.<br />
12 th World Congress of Endoscopic Surgery 180
Emerging Technology Oral Abstracts<br />
ET04<br />
LAPAROSCOPIC INFRARED IMAGING - THE FUTURE VASCULAR MAP<br />
Noam Shussman, MD, Mahmoud Abu Gazala, MD, Avraham Schlager,<br />
MD, Ram Elazary, MD, Abed Khalaileh, MD, Gideon Zamir, MD, Avraham<br />
I Rivkind, MD FACS, Yoav Mintz, MD Department of General Surgery,<br />
Hadassah Hebrew University Medical Center, Jerusalem, Israel<br />
OBJECTIVE: one of the major disadvantages of minimally invasive surgery<br />
(MIS) is the lack of palpation. Surgeons spend much time during surgery<br />
in order to locate the blood vessels, either to secure them or divide them<br />
safely. Recently due to the introduction of Single Port Access Surgery<br />
and NOTES this is further accentuated. Infrared (IR) detection has already<br />
shown promise in its ability to map out vascular structures during open<br />
surgery. The aim of this study, however, was to evaluate the performance<br />
of IR detectors inside the peritoneal cavity to localize blood vessels during<br />
laparoscopic procedures.<br />
DESCRIPTION OF TECHNOLOGY: IR radiation is composed of<br />
electromagnetic waves with a lower frequency and longer wavelength<br />
than that of visible light. Measurement of the IR emissions is a highly<br />
sensitive method of detecting discrepancies in thermal energy, or<br />
temperature. Because blood vessels are naturally warmer than their<br />
surroundings, IR detection can be highly effective in identifying and<br />
mapping out their course. In recent years, IR detection has been<br />
used successfully for this purpose in open surgery. Nevertheless, this<br />
technology has yet to be employed in laparoscopic surgery, where<br />
its contribution would be greatest, for a number of reasons: Firstly, IR<br />
detectors at present are too large to be introduced into the abdomen<br />
via a standard trocar and IR radiation cannot be transmitted through<br />
standard laparoscopic lenses. Secondly, because the closed insufflated<br />
abdomen does not allow heat loss, there has been concern that there<br />
would not be sufficient temperature discrepancy between blood vessels<br />
and their surrounding tissue to allow sensitive discrimination of the<br />
vasculature. We have developed a method to introduce detectors into<br />
a closed abdomen and test the sensitivity of their detection in the<br />
laparoscopic environment.<br />
PRELIMINARY RESULTS: We performed a feasibility study using this<br />
technology on live porcine models. After insertion of IR detectors into the<br />
insufflated abdomen we performed a series of laparoscopic procedures.<br />
During these operations we evaluated the ability of the IR detector to<br />
identify blood vessels as well as the effects of local and systemic changes<br />
in temperature. The IR detector successfully identified concealed blood<br />
vessels as well as acute bleeding. While cool lavage as well as insufflation<br />
of the peritoneal cavity with room temperature CO 2<br />
accentuated IR<br />
detection of blood vessels, warm CO 2<br />
and systemic temperature changes<br />
did not affect IR detection. Additionally, localized heating of tissue on the<br />
operative field using electro-cautery did not interfere with IR sensitivity.<br />
CONCLUSIONS AND FUTURE DIRECTIONS: Laparoscopic IR imaging is<br />
a feasible method of blood vessel detection in laparoscopic procedures.<br />
Use of IR blood vessel detection in laparoscopy has a potential to enable<br />
safer surgery and reduced operative times. The technique and video clips<br />
will be demonstrated. Fusion of IR imaging with the standard laparoscopic<br />
view is currently being developed to allow real time vessel mapping<br />
during laparoscopic surgery.<br />
ET05<br />
TRANSGASTRIC SMALL BOWEL RESECTION WITH A NEW<br />
MULTITASKING PLATFORM ENDOSAMURAI(TM) Karl H Fuchs, title,<br />
Wolfram Breithaupt, title Markus-Krankenhaus, Dept of Surgery<br />
Introduction: Recently NOTES-techniques in gastro-intestinal endoscopy<br />
and surgery are carefully introduced in clinical practice. It emerges that<br />
future therapeutic endoscopes should enable the operator to perform<br />
surgical task like suturing with a steerable stabile platform. A new<br />
prototype of a multitasking platform (EndoSAMURAI, Olympus Medical<br />
Systems Corporation, Tokyo, Japan) could fulfil these criteria and was<br />
tested by our team.<br />
Aim: The purpose of this study was the evaluation of this new prototype<br />
in an animal model using transgastric small bowel resection with<br />
laparoscopic assistance.<br />
Methods: In a porcine model small bowel resection was performed via<br />
the transgastric route using a needle knife gastrotomy and laparoscopic<br />
port assistance for stapler application. After resection an end-to-end<br />
interrupted sutured small bowel anastomosis were performed. After<br />
completion of the hand-sutured anastomosis with the EndoSAMURAI<br />
platform the experiment was terminated. The segment of small bowel,<br />
carrying the anastomosis, was again resected and air leak pressure and<br />
bursting pressure were measured in the laboratory using perfusion<br />
manometry. The bowel segment with the anastomosis was kept in<br />
a water bath and air was insufflated at 1ml/sec via an independent<br />
channel into the bowel lumen. Pressure values were recorded when an<br />
air leak occurred during rising intraluminal pressure. The experiment<br />
was terminated, after the bursting pressure was recorded, when air was<br />
abruptly insufflated with 50 ml/sec.<br />
Results: in total 7 animals were operated with a median body weight<br />
of 30 kg. All end-to-end anastomsis were completed. Total time of the<br />
procedure from skin incision for the assisting trocard until completion<br />
of the anastomosis was median 100 min (70-125). The median time for<br />
anstomosis was 90 min. Leak pressures: 50 mmHg (19-68). The results<br />
show that end-to-end small bowel anastomosis can be sutured in<br />
sufficient quality.<br />
Conclusion: The new prototype can be used for anastomotic suturing<br />
with a sufficient quality. These results and the technical experience are<br />
very promising to use this tool in the future for safe surgical endoscopic<br />
performance.<br />
ET06<br />
A NOVEL FLEXIBLE BIPOLAR HEMOSTASIS FORCEPS (BELA, ETHICON<br />
ENDO-SURGERY, NOTES TOOLBOX) OVERCOMES THE CURRENT<br />
SHORTCOMINGS OF ENDOSCOPIC ZENKER’S DIVERTICULOTOMIES:<br />
AN EXPERIMENTAL MODEL. Erwin Rieder, MD, Danny V Martinec, BS,<br />
Christy M Dunst, MD, Lee L Swanstrom, MD Dept. of Minimally Invasive<br />
Surgery, Legacy Health, Portland, OR<br />
Objective: Zenker´s diverticulum (ZD) is the most common type of<br />
diverticulum in the upper gastrointestinal tract. Treatment is indicated for<br />
symptomatic patients as complications such as carcinoma, aspiration or<br />
stenosis of the upper esophagus can occur. Common treatments are open<br />
surgical diverticulectomy and rigid endoscopic myotomy, using an endo-<br />
GIA stapler. This endoscopic alternative is relatively minimally invasive<br />
but is not applicable to all patients due to anatomic reasons. It also may<br />
have a higher failure rate due to the incomplete division of the stapleline.<br />
Flexible endoscopy has been described for diverticulotomy, and may<br />
have advantages over the rigid approach as it can be performed without<br />
general-anesthesia or the need for hyperextension of the neck. Different<br />
techniques such as needle-knife incision or argon plasma coagulation<br />
have been used for division of the septum between the diverticulum and<br />
the esophagus. These techniques are associated with a longer learning<br />
curve, which is difficult to achieve given the overall rarity of this condition.<br />
The danger inherent in the flexible approach is that division of the septum<br />
is not accompanied by sealing of the pouch and esophageal mucosa.<br />
This can lead either to clinical recurrence, mediastinal emphysema<br />
and infection or bleeding. We hypothesized that recent developments<br />
evolving from natural orifice transluminal endoscopic surgery (NOTES)<br />
techniques might strongly facilitate and simultaneously assure precise<br />
and safe endoscopic diverticulotomy.<br />
Methods: As the pig has a normal pharyngeal diverticulum (PD) that is<br />
identical to a human ZD from the endoscopic perspective, this model<br />
was used to perform diverticulotomy. A double-channel endoscope was<br />
inserted into the pharyngeal diverticulum of an intubated pig, which<br />
permits excellent viewing of the septum along with the esophageal<br />
lumen. The PD septum was dissected to the inferior border using a<br />
Flexible Bipolar Hemostasis Forceps (BELA, prototype instrument,<br />
Ethicon Endo-Surgery) providing intermittent coagulation and cutting.<br />
The septum can simultaneously be stabilized with a standard flexible<br />
endoscopic grasper, if necessary.<br />
Results: The PD could be easily visualized. Due to the small size of the<br />
BELA, the septum could be precisely dissected to the end of the inferior<br />
border, which is often not possible with the current standard endoscopic<br />
181 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
Emerging Technology Oral Abstracts<br />
procedure such as the use of a rigid endo-GIA stapler. In contrast to<br />
needle knife dissection, the BELA can easily be readjusted prior to any<br />
tissue dissection. As otherwise inevitable movements or tension while<br />
dissecting are not necessary and additionally energy is only applied on<br />
the tissue to be divided due to isolated branches, dissection is much more<br />
precise. The coapting or “tissue welding” characteristics of the bipolar<br />
technology were also valuable to fuse the esophageal and pouch-mucosa<br />
together and prevent leaks. Although no esophageal protection was used<br />
no complication occurred. The whole dissection of the septum took 16<br />
minutes.<br />
Conclusion: The use of the flexible bipolar hemostasis forceps (“BELA”)<br />
for endoscopic Zenker´s diverticulotomy could be a quicker and safer<br />
approach compared to needle knife dissection. This novel tool can<br />
significantly facilitate performance of endoscopists and may make flexible<br />
endoscopy the preferred method of Zenkers ablation.<br />
ET07<br />
INSERTABLE ROBOTIC EFFECTOR PLATFORM Dennis L Fowler, MD MPH,<br />
Peter Allen, PhD, Jayson Ding, PhD, Roger Goldman, BA, Austin Reiter, BA,<br />
Nabil Simaan, PhD Columbia University<br />
Objective of Device: The objectives of developing this technology are<br />
1) to reduce the invasiveness of surgery by converting access to either a<br />
single incision or a natural orifice, 2) to make it easier for surgeons to learn<br />
minimally invasive techniques with a manageable, computer-assisted<br />
platform, and 3) to reduce the overall cost and size of a robotic platform<br />
for minimally invasive surgery.<br />
Description of the Technology: The device includes robotic and<br />
control hardware, software, and a standard PC for operator interface.<br />
The hardware is a 15 mm diameter device that is inserted into the body<br />
cavity through a single site. When inserted into a body cavity, the device<br />
uses its 21 degrees of freedom to deploy a camera module containing<br />
two cameras for stereoscopic imaging and two dexterous snake-like<br />
robotic arms. The camera module and dexterous arms are motor-driven<br />
and are controlled by a surgeon using a telemanipulation interface or<br />
by the software itself using sensory information from the cameras. The<br />
controller software includes modules for moving the cameras and tools;<br />
advanced, novel, image processing software for optimally displaying<br />
and using the images from the cameras; and software to integrate the<br />
sensory information from the cameras with the controller software so as<br />
to manage the overall functionality of the device.<br />
Preliminary Results: We have measured and video-recorded the<br />
performance of the prototype in an inanimate model for study and<br />
presentation. In initial testing the system effectively controls the<br />
movement of the camera module by tracking the movement of the tool<br />
controlled by the surgeon’s dominant hand. The surgeon effectively<br />
controls the tools using the master manipulator.<br />
Conclusions/Future Directions: The camera module will autonomously<br />
follow one of the instruments, enabling the surgeon to be free to control<br />
only the tools. Future activities include refining the software; enhancing<br />
instrument performance by adding new functionality to existing tools as<br />
well as adding new instruments; and proceeding with animal trials.<br />
ET08<br />
INTRA-LUMINAL INJECTION OF FERROMAGNETIC GLUE-BASED MEDIA<br />
FOR BOWEL RETRACTION IN LAPAROSCOPIC SURGERY Z Wang, PhD,<br />
A W Brown, S I Brown, PhD, D Liu, L Wang, PhD MD, A Cuschieri, Professor<br />
Institute for Medical Science and Technology, University of Dundee, UK<br />
Objective Safe and effective manipulation of soft tissue during<br />
laparoscopic and other minimal access surgical procedures can be<br />
enabled by use of electromagnetic force. Previously we reported<br />
two approaches for tissue ferro-magnetisation, e.g. mucosal surface<br />
magnetisation using adhesives and sub-mucosal injection of magnetic<br />
media. This presentation describes a new method of ferro-magnetisation<br />
of a bowel segment for its magnetic retraction which overcomes the low<br />
retraction force limitation of the previously reported approaches.<br />
Method stainless steel microparticles were dispersed in cyanoacrylate<br />
liquid and injected intra-lumenally to form a coagulum attached to<br />
the inner (mucosal) aspect of the bowel wall using an ex-vivo porcine<br />
bowel model. The coagulum was then retracted towards a magnetic<br />
probe which was located external to the bowel wall. The probe was<br />
made of small magnet discs, and the magnetic force could be varied by<br />
changing the number of the stacked discs. Finite element method (FEM)<br />
was used to analyze the magnetic field and force exerted by the intralumenal<br />
magnetic coagulum for optimization of the probe design. The<br />
characteristics of the magnetic glue were investigated to ensure that the<br />
maximal retraction force could be delivered reliably and that the media<br />
could be injected without difficulty. Biocompatibility of the implanted<br />
ferromagnetic coagulum was preliminarily assessed by in-vitro cell culture<br />
toxicity studies.<br />
Results Using the ex-vivo porcine bowel loops, a large volume of<br />
magnetic media with a microparticle concentration of up to 2 g/mL was<br />
injected into the bowel lumen, and a range of magnetic retraction force<br />
was generated for manipulating the bowel. This was compared to grip<br />
retraction by forceps which resulted in significantly higher stress on the<br />
grasped bowel tissue. A low bond force between the coagulum and<br />
mucosal layer was found to facilitate removal of the coagulum from the<br />
bowel wall after surgical procedure. In-vivo, any residual ferromagnetic<br />
material from the intraluminal coagulum would be eliminated following<br />
the return of bowel function after surgery. The tendency for the<br />
microparticles to aggregate within the syringe was investigated by<br />
varying the viscosity of the cyanoacrylate liquid and concentration of the<br />
magnetic media. The cell culture tests indicated that the magnetic media<br />
based on medical grade cyanoacrylate were not cytotoxic.<br />
Conclusions Glue based intra-lumenal ferromagnetic coagula for<br />
magnetic retraction of bowel were realized in this ex-vivo porcine bowel<br />
model. The optimal magnet probe design and ferromagnetic implanted<br />
materials were investigated and identified using both FEM analysis and<br />
simulated surgical procedures. We previously reported mucosal retraction<br />
using glued media on the tissue surface and found that there was a low<br />
bond-strength between the mucosal and the magnetic coagulum. The<br />
present development based on use of intra-lumenal ferromagnetic gluebased<br />
media overcomes this problem and utilizes the maximal magnetic<br />
attraction potential by holding the bowel wall segment and retracting<br />
it towards a magnetic probe external to the bowel wall. Intra-luminal<br />
injection of ferromagnetic coagula appears to be a promising method for<br />
safe and effective magnetic bowel retraction.<br />
ET09<br />
“THE DUNDEE ENDOCONE”: A NEW REUSABLE SILS DEVICE Andrea<br />
Pietrabissa, MD, Mario Alessiani, MD, Andrea Peri, MD, Sandro Zonta, MD,<br />
Lorenzo Cobianchi, MD, Paolo Dionigi, MD, SI Brown, MD, TG Frank, MD,<br />
Alfred Cuschieri, MD Department of Surgical Science, University of Pavia;<br />
Institute for Medical Science and Technology - Dundee U.K<br />
Objective of the technology or device: Dundee EndoCone is a new<br />
device for SILS (Single Incision Laparoscopic Surgery) created at the<br />
Institute for Medical Science and Technology in Dundee U.K. with the<br />
industrial partnership of Karl Storz Gmbh. The challenge was to create<br />
a low cost SILS device which allows the surgeon to perform advanced<br />
surgical procedures using up to three instruments and the camera at<br />
the same time, through a single port of acceptable size. Most currently<br />
commercially available devices only allow the insertion of 2 operating<br />
instruments and the optics.<br />
Description of the technology and method of its use or application:<br />
The device consists of a waisted metallic cone with an extra-abdominal<br />
diameter of 45mm which tapers to a cylindrical section (30mm diameter)<br />
for insertion through the abdominal parieties into the previously<br />
insufflated peritoneal cavity. The device has a removable cap (bulkhead)<br />
with 8 valved ports: 6 - 5mm, 1 - 10mm and 1 - 12 mm for use of staplers.<br />
Insertion into the peritoneal cavity is achieved through a vertical 30mm<br />
umbilical incision by a clockwise screwing action. The device has a<br />
dedicated long Hopkins 5mm telescope which enables the camera person<br />
to manoeuvre the camera without encroaching on the operating space<br />
of the surgeon. The system enables the use of 4 instruments (including<br />
optic) at any one time. It overcomes the problem of triangulation,<br />
12 th World Congress of Endoscopic Surgery 182
Emerging Technology Oral Abstracts<br />
typical of SILS by use of specifically designed single and double curved<br />
instruments. Provided the specimen is small the bulkhead is removed<br />
for extraction, with the cone in situ, thus providing protection of the<br />
abdominal wall during the extraction.<br />
Initial clinical experience: Our initial clinical experience with the<br />
EndoCone includes SILS cholecystectomies and colectomy. The additional<br />
grasper of the EndoCone enables the necessary exposure and tension<br />
during active dissection not possible with current SILS devices. This<br />
facilitates execution of the procedure and control of any bleeding.<br />
All gallbladder specimens (n =2) were removed by simple removal<br />
of the bulkhead with the cone providing complete protection to the<br />
abdominal walls. For bulky specimens such as colectomy for colon<br />
cancer, the EndoCone is replaced by a protective circular plastic drape.<br />
Following extracorporeal reconstruction, the EndoCone is replaced for<br />
final inspection. All patients had a smooth post-operative course with no<br />
complications and required minimal analgesic medication in view of their<br />
low pain scores.<br />
Conclusions/ Future directions: The initial experience with the first<br />
generation EndoCone has been entirely favourable in terms of ease of<br />
execution and operating times. The feedback from these clinical results<br />
will be used to make fine tuning adjustments to the EndoCone operating<br />
system for SILS. The changes envisaged included a flexible waist to<br />
improve manoeuvrability and a range of disposable bulkheads depending<br />
on the requirements of specific operations.<br />
ET10<br />
FLEXIBLE CO2 LASER AND SUBMUCOSAL GEL INJECTION FOR SAFE<br />
ENDOSCOPIC AND LAPAROSCOPIC SURGERY OF THE INTESTINES<br />
Joyce T Au, MD, Arjun Mittra, MD, Joyce Wong, MD, Iain Nixon, MD, Paula<br />
Ezell, DVM, Snehal Patel, MD, Yuman Fong, MD Memorial Sloan Kettering<br />
Cancer Center<br />
OBJECTIVE: The CO2 laser’s unique wavelength of 10.6 μm has the<br />
advantage of being readily absorbed by water but historically limited<br />
it to line-of-sight procedures. Through recent technological advances,<br />
a flexible CO2 laser fiber has been developed and holds promise for<br />
endoluminal and laparoscopic surgery. In this study, we examined<br />
whether injection of a water-based gel in the submucosal space will allow<br />
safe dissection of the intestines using the flexible CO2 laser and enhance<br />
potential of this tool for endoluminal and laparoscopic surgery.<br />
METHODS: Using an ex vivo model with porcine intestines, spot and<br />
linear burning was performed with the flexible CO2 laser fiber at different<br />
power settings until transmural perforation. Additionally, excisions of<br />
mucosal patches were performed by submucosal dissection with and<br />
without submucosal injections of a water-based gel.<br />
RESULTS: With spot burning at 5 W, none of the specimens were<br />
perforated by 5 minutes which was the maximum recorded time. The time<br />
to perforation was significantly shorter at 10 W (mean=6 sec, p
12 th World Congress of Endoscopic Surgery<br />
Emerging Technology Oral Abstracts<br />
Further work is needed to study the effect of curvature of the tissue<br />
on the signal, the pattern of tissue oxygen saturation associated with<br />
development of ischemia, and how this influences surgical outcomes, e.g.<br />
anastomotic leak rate.<br />
ET12<br />
LAPAROSCOPIC INTESTINAL ANASTOMOSIS WITH THE CAIMAN<br />
LEKTRAFUSE DEVICE Dirk W Meijer, MD MSc PhD, H Jaap Bonjer, MD PhD<br />
BRG, VUMC<br />
Objective of the technology/device. Laparoscopic Intestinal Anastomosis<br />
with the Lektrafuse Caiman Device, without sutures or staples.<br />
Description of the technology and method of its use or application.<br />
The Aragon Surgical Lektrafuse Caiman laparoscopic instrument is a<br />
dedicated bipolar electrosurgical instrument intended for use in general<br />
surgical and gynecologic laparoscopic procedures where ligation<br />
and division of vessels is desired. The instrument creates a seal by the<br />
application of bipolar electrosurgical RF energy (coagulation) to vascular<br />
structure (vessels) and tissue interposed between the jaws of the device.<br />
A cutting blade is activated for the division of tissue. The device can be<br />
used on vessels up to 7mm in diameter and non-vascular tissue that fits<br />
between the jaws of the instrument.<br />
A challenging application is the creation of an intestinal anastomosis.<br />
This would be an attractive alternative to a stapled anastomosis. This was<br />
investigated in a side-to-side intestinal anastomosis in the mid-jejunum in<br />
2 pigs. The Aragon Lektrafuse system was used for intestinal transection<br />
and side-to-side intestinal anastomosis. Animals were sacrificed 20<br />
days postoperatively. The anastomosis and surrounding tissues were<br />
explanted and preserved in 10% neutral buffered formalin (NBF). Formalin<br />
fixed tissues were then trimmed, routinely processed in alcohol and<br />
xylene, embedded in paraffin, sectioned at 4-6 microns, and stained<br />
with hematoxylin and eosin (H&E) for routine microscopic evaluation.<br />
Trichrome stain was used on some sections to demonstrate fibrosis.<br />
Preliminary results. Grossly, a discrete anastomotic site was difficult to<br />
discern. The degree of fibrous adhesions forming around the anastomotic<br />
site was considered within normal limits as compared to side-to-side<br />
anastomosis performed with surgical staples. At the anastomotic site was<br />
a small discrete zone of fibrosis creating a stable adhesion and fusion<br />
between the conjoining loops of intestine. Furthermore, there was normal<br />
regeneration and growth of the mucosal lining over the anastomotic site.<br />
Conclusions and Future directions. This study demonstrates that small<br />
bowel anastomosis is feasible with the Caiman instrument. This very<br />
promising technique is evaluated in further detail to determine suitability<br />
for use in patients.<br />
ET13<br />
NOVEL METHODOLOGY FOR COMPARING TISSUE ANALOGS Jenna<br />
Turocy, John Hryb, Danyel Racenet, Andrew Miesse, Thomas Wenchell,<br />
Covidien<br />
Objective: To compare the compressive properties and penetration<br />
resistances of various tissue analogs to organic tissue using a powered<br />
stapling device.<br />
Technology and Method: An important step in the development of any<br />
medical device is frequent testing to evaluate device performance. While<br />
the need for a more realistic, consistent and humane testing material is<br />
not new, the development of the powered stapling device allows for a<br />
more accurate analysis our testing material. Current engineering tests<br />
for surgical staplers are performed in foam, polymeric materials, in vivo<br />
and ex vivo animal tissue and cadaver tissue. With many different options<br />
available, it is imperative that standardized tissue analogs be used for<br />
different physiological tissues. Recently, a synthetic tissue was developed<br />
to mimic the mechanical, structural, and visco-elastic properties of living<br />
tissue. To test the mimicry of the tissue analogs, device performance on<br />
versions of this media will be analyzed using electric current profiles. The<br />
electric current the powered stapling device draws as it clamps, staples<br />
and transects the media can be recorded with high resolution. The electric<br />
current is directly related to the torque in the device motor and can be<br />
12 th World Congress of Endoscopic Surgery 184<br />
translated into the linear force required to compress and penetrate the<br />
test media. The compressive force and penetration resistance can be used<br />
to determine a tissue analog’s similarity to organic tissue.<br />
Preliminary Results:<br />
Graph 1. Above are the electric current profiles recorded during firing a<br />
linear stapling reload with a powered stapling device on synthetic and<br />
in vivo canine tissue. The peaks in the current profile correspond to the<br />
formation of a staple.<br />
Conclusions/Future Directions: In the future, a synthetic tissue promises<br />
to provide a more realistic testing media than foam and a humane and<br />
more consistent testing media than live animals. Results from this testing<br />
will be used to modify the synthetic tissue to more accurately reflect<br />
the compression and penetration properties seen in organic tissue.<br />
The media’s relaxation rate and strain under compression will also be<br />
measured using a material compression testing machine. In the future,<br />
the testing will be expanded to study different tissue types as well<br />
introduce more variables such as age, sex, weight and disease state of<br />
tissue.<br />
ET14<br />
BETA TESTING OF A V-BAND SIMULATOR Jamie D Adair, MD, Ganesh<br />
Sankaranarayanan, PhD, Tansel Halic, MS, Zhonghua Lu, MS, Woojin Ahn,<br />
PhD, Mark A Gromski, BA, Daniel B Jones, MD, Suvranu De, ScD Beth Israel<br />
Deaconess Medical Center and Rensselaer Polytechnic Institute<br />
Background: The Laparoscopic Adjustable Gastric Band (LAGB) is an<br />
adjustable and reversible surgical weight loss procedure and the second<br />
most common weight loss procedure in the United States. The objective<br />
of our study was to evaluate the face, content and construct validity of a<br />
V-Band simulator that we have developed.<br />
Methods: Twenty eight subjects participated in the study and were<br />
categorized into two groups, experts (PGY 5/fellows/faculty) and novice<br />
(4th year medical students and PGY1-4). There were 13 subjects in the<br />
expert group and 15 in the novice group. Face and content validity was<br />
assessed using a 5-point Likert scale questionnaire. The face validity<br />
questions assessed subjects on the realism of the simulated procedure,<br />
haptic feedback, and videoendoscopic instrument movement. Content<br />
validity was evaluated by experts and consisted of a questionnaire on<br />
the usefulness of the V-Band trainer for training residents/surgeons<br />
and for potential LAGB certification. Construct validity was assessed by<br />
computing normalized individual scores for dissection of structures using<br />
electrocautery and band placement. An average score based on these<br />
two tasks was also calculated to determine a total score for the entire<br />
simulator procedure. Penalties were accorded to the number of times the<br />
band was dropped and the size of the perforations made in the stomach<br />
and esophagus.<br />
Results: Face validity results revealed an average rating of more than 3.0<br />
for realism. Visual display and tools/interface obtained a higher average<br />
rating of 4.0 and 4.07, respectively. Mann-Whitney U test between the two<br />
groups showed no significant difference indicating a general agreement<br />
between experts and novices.<br />
Content validity results show that the experts overwhelmingly agree that<br />
the V-Band simulator will be a useful trainer for residents/surgeons before<br />
their operating room experience (mean score of 4.5). They also agreed
Emerging Technology Oral Abstracts<br />
that it could potentially be used for certification of the procedure (mean<br />
score of 3.4). Construct validity (Table 1) was tested by using the Mann-<br />
Whitney U test between the two groups. The results show that the virtual<br />
LAGB simulator was able to differentiate between expert and novice<br />
groups.<br />
Table 1.<br />
Scoring Parameter Experts Experts Novice Novice<br />
Mann-Whitney<br />
U Test<br />
Lap-Band Placement 85.06 12.01 51.18 27.30 0.0003<br />
Electrocautery 81.49 24.26 62.41 17.74 0.0061<br />
Total Score 81.93 17.02 51.13 25.35 0.0002<br />
Conclusion: The V-Band simulator demonstrated excellent face, content<br />
and construct validity. We plan to add additional tasks of the procedure<br />
such as securing the band using gastro-gastric imbrications. To our<br />
knowledge, this is the first virtual reality simulator with haptic feedback<br />
developed for training surgeons and surgical residents in the LAGB<br />
procedure.<br />
ET15<br />
WIRELESS ENDOLUMINAL APPLICATION OF A MAGNETIC DRIVEN<br />
CAMERA Nicola Di Lorenzo, MD Phd, Arianna Menciassi, Prof, Pietro<br />
Valdastri, Eng Phd, Livia Cenci, MD, Luca Iezzi, Eng Phd, Achille Lucio<br />
Gaspari, Prof, Paolo Dario, Prof Scuola superiore Sant’ Anna Pisa -<br />
Department of surgey-University of Rome Tor Vergata<br />
Objective of technology or device. The use of magnetic fields to control<br />
and steer assistive and operative devices is increasing in endoluminal and<br />
transluminal surgical operations.<br />
The single port access is the future of surgery, thus allowing surgical<br />
procedures through a single incision.<br />
A promising technology is the Magnetic Internal Mechanism (MIM) control<br />
of diagnostic or surgical instruments deployed inside the patient’s body.<br />
A wireless controllable endoscopic capsule was developed as a proof<br />
of concept equipped with one electromagnetic motor moving two<br />
permanent magnets, coupled with an external sources of magnetic field<br />
for coarse positioning and stabilization of the device.<br />
The objective of our study was to assess the feasibility and functionality of<br />
a wireless miniaturized mechanism based on magnetic forces for precise<br />
camera steering and orientation.<br />
Description of technology and method of its use or application. MIM<br />
works jointly with an external static magnetic field source both for the<br />
coarse positioning and for stabilization.<br />
MIM capsule’s body has a cylindrical shape with a diameter of 15 mm and<br />
length of 48 mm and it incorporates one electromagnetic direct current<br />
brushless motor, two small permanent magnets diametrically magnetized<br />
and an electronic circuit for wireless motor control.<br />
In order to prove the concept of on line control of vision, a real time wired<br />
camera was incorporated in the device.<br />
The overall capsule weight is 14,4 g.<br />
This mechanism would allow to maximize the number of tools with respect<br />
of access port while in endoscopic practice magnetized camera system can<br />
be introduced by natural orifices and oriented by magnetic means.<br />
By adding an internal degree of freedom it would be possible to move the<br />
device relatively to the surrounding tissue more effectively and reliably.<br />
We performed 3 sets of test with MIM: a bench test in free space, a<br />
phantom with porcine gastrointestinal tract inserted, and two in vivo<br />
experiments with a 30 kg female domestic pig.<br />
Preliminary results. A fine navigation and rotation was achieved in all<br />
tests keeping an external magnet approximately 10 cm distant from the<br />
capsule.<br />
MIM allowed the capsule to identify several marks previously placed<br />
inside the cavity.<br />
Once the operative location has been reached, fine orientation and<br />
steering of the visual field can be obtained by actuating the in board<br />
motor without any further modification of the external magnetic field.<br />
Conclusion. We report the feasibility and effectiveness of the synergic<br />
use of the external static magnetic field and single internal wireless<br />
actuator to move small permanent magnets on board the capsule in<br />
order to achieve wirelessly controllable and precise camera steering<br />
intrabdominally.<br />
The concept is applicable to wireless capsule endoscopy as to other<br />
instrumentation for laparoscopy or endoluminal and transluminal<br />
procedures.<br />
ET16<br />
AUGMENTED REALITY SYSTEM FOR ENDOSCOPIC AND NOTES<br />
PROCEDURES Luc Soler, PhD, Vincent Agnus, PhD, Stephane Nicolau, PhD,<br />
Julien Waechter, Eng, Oliver Burckhardt, MD, Silvana Perretta, MD, Bernard<br />
Dallemagne, MD, Didier Mutter, MD PhD, Jacques Marescaux, MD IRCAD<br />
Objective: Endoluminal and Transluminal surgeries are known as<br />
complex procedures due to long articulated instruments on which no<br />
direct view is obtainable. Instrument direction, location and shape are<br />
thus difficult to estimate. Currently available systems can only overcome<br />
the shape obstacle by providing a 3D virtual view of the scope. To add<br />
direction and location, we have developed a new system named METRIS<br />
that provides a real-time 3D view of the flexible endoscope mixed to the<br />
patient’s real image. METRIS can also add the preoperative 3D modelling<br />
of patient organs to this augmented reality view.<br />
Material and methods: Based on the NDI Aurora© device, we have<br />
designed a 1.20m long and 2.2mm wide flexible tube containing eight<br />
8mm by 1mm 5 degree of freedom electromagnetic coils placed all along<br />
its length. This electromagnetic Aurora 5DOF shaped tool© developed by<br />
NDI can be sterilized in autoclave and is small enough to be introduced<br />
in the operative channels of almost all flexible endoscopes. From<br />
the spatial position and direction provided by Aurora©, our software<br />
computes the 3D shape of the tool by using a spline modelling. It can<br />
also provide the distance between two locations of the tool’s tip. To add<br />
the patient’s direction and location data linked to his position, we use an<br />
optical tracking of a fiducial tag stuck on the Aurora device by using an<br />
Augmented Reality Library (ARL) that we have developed. A conventional<br />
OP-room camera (scialitic or external camera) is linked through a Firewire<br />
port to a laptop integrating an OpenGL Graphic card. ARL calibration,<br />
registration and tracking algorithms then allow to fuse patient video<br />
view provided by the camera to the 3D shape virtual view of the flexible<br />
catheter. When available, a preoperative 3D modelling of the patient<br />
performed from a CT-scan or MRI using the VR-Anat© software developed<br />
by IRCAD, can be superimposed on the same video providing the patient’s<br />
virtual transparent view.<br />
Validation: Our preclinical validation was performed on pigs using<br />
Karl Storz flexible endoscopic devices. In colonoscopy, the endoscope<br />
loop can be avoided by 3D representation, thus reducing colonic<br />
perforation risks. We also demonstrated that METRIS provides a<br />
1mm accuracy of polyp sizes. Additionally, METRIS was evaluated to<br />
estimate the best NOTES path and gastrotomy position for transgastric<br />
cholecystectomy. Combined with Augmented Reality, it simplifies the<br />
NOTES scope navigation through anatomical structures and endoscope<br />
3D visualization.<br />
Conclusion: The METRIS system is a reusable sterizable system adjustable<br />
to any endoscopic system with an operative channel larger than 2.3mm.<br />
The 3D shape of an endoscope along with its direction and position<br />
are provided. It can also be passed through the endoscope’s tip to<br />
measure tumor sizes accurately. In this way, typical NOTES difficulties<br />
are diminished when combined to augmented reality. The next step will<br />
consist in validating these first preclinical tests clinically.<br />
ET17<br />
360° IMMERSIVE PANOMORPH ENDOSCOPIC DEVICE: A NEW<br />
ADVANCED VISION SYSTEM CONCEPT Pierre Garneau, MD, Patrice<br />
Roulet, Pierre Konen, Mathieu Villegas, Simon Thibault, MSc PhD ing<br />
Sacré-Coeur Hospital of Montreal, ImmerVision, Université Laval<br />
Minimally-invasive surgical procedures and medical examination<br />
procedures now require increasingly sophisticated devices to help<br />
explore a patient’s internal organs. Fortunately, recent advances in<br />
optic miniaturization and improvements in sensor size and resolution<br />
have led to the development of superior and smaller videoscopes for<br />
185 www.12thworldcongress.org<br />
12 th World Congress of Endoscopic Surgery
12 th World Congress of Endoscopic Surgery<br />
Emerging Technology Oral Abstracts<br />
certain medical imaging procedures. In fact, these ultra-modern visual<br />
instruments benefit from sensor miniaturization with an increased<br />
resolution of up to 1.3 megapixels (HD).<br />
Even with such high-resolution capacity, though, endoscopic vision<br />
is quite different from human vision in the context of open surgery,<br />
especially as regards field-of-view (Fig. 1). Existing endoscopic devices<br />
don’t address common limitations, including the afore-mentioned poor<br />
field-of-view, a limited range of motion, loss of depth perception and the<br />
need for counter-intuitive camera manipulation.<br />
This paper presents an innovative approach using a wide-angle 180°<br />
field-of-view panomorph lens and corresponding visualization software,<br />
designed specifically for endoscopy procedures.<br />
The new panomorph endoscopy application is based on replicating as<br />
closely as possible the parameters of human vision. As an example, it<br />
features a wide field-of-view (>140°) and the ability to increase angular<br />
resolution when and where required. This allows video capture of the full<br />
body cavity (Fig. 2).<br />
The device’s visualization software processes 360° panomorph endoscopic<br />
images from various distortion-free points of view, mimicking real-world<br />
proportions and actual geometrical information. With this visualization<br />
software, it is possible for a surgeon to customize views best suited<br />
to his/her psychomotor skills, physical position, and any extenuating<br />
circumstances, without having to physically manipulate the endoscope.<br />
In addition, the surgeon can arrange different points of view on several<br />
screens, to enable a global overview of the complete procedure.<br />
To further illustrate this advantage, we cite a possible scenario from a<br />
typical cholecystectomy procedure. Using our new device, the video feed<br />
from a panomorph laparoscope would allow the insertion of laparoscopic<br />
tools into the patient’s abdominal cavity without any camera movement<br />
and without losing the images of the surgical procedure underway.<br />
This is a considerable benefit during any unforeseen difficulties, such as<br />
intraoperative bleeding. Without adjusting the panomorph endoscope,<br />
the surgeon can simultaneously oversee any active bleeding and continue<br />
monitoring his/her surgical instruments, simply by using different views<br />
from the same immersive panomorph endoscopic video.<br />
In summary, the use of the new panomorph endoscopy device for both<br />
diagnostic and minimally-invasive surgical applications has the potential<br />
to:<br />
- enhance depth perception;<br />
- reduce procedure time;<br />
- decrease manipulation of tools and endoscope; and<br />
- provide more intuitive viewing and a superior user interface.<br />
Just as importantly, though, it will help the surgeon see more, and see it<br />
all simultaneously, for a true “big picture”.<br />
Just as advancements in minimally-invasive surgery, such as singleincision<br />
laparoscopic surgery (SILS), are forcing the progression of<br />
imaging technology, this newly developed “panomorph” device may<br />
make these procedures more efficient, with the added potential to<br />
increase procedural safety and cost-effectiveness.<br />
ET18<br />
ROBOTIC TRANSAXILLARY THYROIDECTOMY: REPORT OF TWO CASES<br />
AND DESCRIPTION OF THE TECHNIQUE Katherine B Heiden, MD, Allan<br />
Siperstein, MD, Mira Milas, MD, Joyce Shin, MD, Jamie Mitchell, MD, Eren<br />
Berber, MD Cleveland Clinic<br />
Objective: Various techniques for minimally invasive thyroid surgery<br />
have been described over the last decade. These techniques have<br />
significant limitations due to two-dimensional view and awkward<br />
endoscopic instrumentation. Robotic surgical technology was developed<br />
to overcome these limitations. In this case report and submitted video,<br />
we are describing and demonstrating the operative technique for robotic<br />
transaxillary thyroid lobectomy.<br />
Description: The procedure is performed by creating a subcutaneous<br />
flap from the axilla to the thyroid bed. The operative field is established<br />
using a specially designed retractor to lift the strap muscles anteriorly,<br />
exposing the thyroid. The entire procedure is completed using a robotic<br />
grasper, camera, and Harmonic scalpel inserted from the axillary incision,<br />
in addition to a robotic grasper inserted through a separate 8 mm<br />
parasternal incision.<br />
Results: In our initial two cases, we demonstrate that robotic transaxillary<br />
surgery is technically feasible, avoids a neck scar, and offers quality threedimensional<br />
vision of the recurrent laryngeal nerve and parathyroid<br />
glands.<br />
ET19<br />
TRANS-ORAL ENDOSCOPIC RESTRICTIVE IMPLANT SYSTEM (TERIS)<br />
FOR THE TREATMENT OF MORBID OBESITY: A 12 MONTHS REVIEW<br />
OF SAFETY AND RESULTANT WEIGHT LOSS Fady Moustarah, MD MPH,<br />
Stéfane Lebel, MD, Laurent Beirtho, MD, Frédéric-Simon Hould, MD, Simon<br />
Biron, MD Institut Universitaire de Cardiologie et de Pneumologie de<br />
Québec, Université Laval<br />
Introduction: An endoluminal natural orifice approach designed to<br />
produce gastric restriction and weight loss is currently under investigation<br />
at our Centre. A 12 month review of the safety profile, device tolerance,<br />
and resultant weight loss observed with the use of the Trans-oral<br />
Endoscopic Restrictive Implant System (TERIS) is presented.<br />
Methods: The TERIS procedure consists of two stages: 1) Endoscopic<br />
placement of 5 silicone anchors in the proximal stomach forming<br />
gastric plications, and 2) implantation of a restrictive silicone membrane<br />
(restrictor device) held in place by the previously inserted anchors. A<br />
registered randomized study is ongoing and compares a single stage<br />
procedure with simultaneous placement of the anchors and restrictor<br />
element (group 1) to a two stage procedure, where the anchors are placed<br />
6weeks before the restrictor is implanted (group 2). Each patient is then<br />
followed for a minimum of six months, at which time the device is either<br />
removed or kept in place as requested and tolerated by the patient.<br />
Results: The last patient in our randomized series of 12 patients (6 per<br />
group) was recruited and treated with TERIS in February 2009. There is no<br />
difference in initial pretreatment BMI between groups. In our total sample,<br />
male to female ratio is 1:3, and mean initial weight is 120±5 Kg. Mean<br />
initial age and BMI are 39 yrs (range: 29-52 yrs) and 43.7 Kg/m2 (range:<br />
38-48 Kg/m2), respectively. One year follow up data will be available for<br />
8 patients by February <strong>2010</strong>. Four patients exited the study before 12<br />
months. There is no statistically significant difference in weight or BMI<br />
between groups 1 and 2 at 6 or 12 months (p>0.05). Mean weight and<br />
BMI are, however, significantly less at both 6 and 12 months compared<br />
to values at the time of restrictor implantation (p
Emerging Technology Oral Abstracts<br />
Conclusion: Using TERIS for the treatment of morbid obesity will<br />
be described and presented by video. Early results demonstrate<br />
the feasibility of using TERIS clinically to promote significant weight<br />
loss in our sample at 12 months. Moreover, while there appears to be<br />
no difference in weight loss after one or two stage implantation of the<br />
system, simultaneously implanting the device components (anchors and<br />
restrictor) under general anesthesia in one endoscopic session is well<br />
tolerated by patients.<br />
ET20<br />
HEMORRHOIDAL LASER PROCEDURE (HELP) IN THE TREATMENT OF<br />
SYMPTOMATIC HEMORRHOIDS Paolo Giamundo, MD, Maria Geraci,<br />
MD, Livio Tibaldi, MD, Marco Valente, MD Department of General Surgery<br />
-Hospital S. Spirito - Bra (CN) - ITALY<br />
INTRODUCTION: Doppler-guided hemorrhoidal artery ligation, also<br />
known as THD or HAL-Doppler, represents an innovative approach that<br />
has captured the interest of many surgeons. It is based on the selective<br />
suture of the terminal branches of the superior rectal artery arteries that<br />
feed the hemorrhoidal plexus through a Doppler-guided identification.<br />
The technique seems to be successful and less painful than traditional<br />
surgery for hemorrhoids. The HeLP Laser procedure,described by the<br />
Authors follows the same rationale of THD/HAL Doppler procedure.<br />
980 nm Diode Laser has several different applications in the medical field.<br />
When used on the mucosa of the anal canal it causes shrinkage of tissue.<br />
The depth and width of tissue shrinkage can be regulated by the power<br />
and duration of Laser beam.<br />
Through a 600 micron conic fiber, five laser pulsed shots generated at<br />
a power of 13 Watt with a duration of 1.2 seconds each and a pause of<br />
0.6 seconds, causes shrinkage of mucosa and submucosa to a depth of<br />
approximately 5 mm and a width of 4 mm .<br />
Terminal branches of superior hemorrhoidal arteries in the anal canal, if<br />
precisely identified through a Doppler signal, can be consequently closed<br />
with the use of this Laser.<br />
PATIENTS and METHODS: A special proctoscope has been specifically<br />
designed for this nonexcisional technique.<br />
The proctoscope has a small window that allows introducing a Doppler<br />
probe whose function is to identify terminal branches of hemorrhoidal<br />
arteries.<br />
Approximately 4 cm above the dentate line, all branches of the superior<br />
hemorrhoidal arteries (usually 8-12) are recognized through a clockwise<br />
rotation of the proctoscope. Once identified, all arteries are progressively<br />
fulgurated through a Laser fiber which replaces the Doppler probe in<br />
the small window of the proctoscope. Effective closure of arterial flow is<br />
confirmed by the absence of Doppler-signal after the Laser shots.<br />
The procedure does not require anesthesia and can be performed as<br />
ambulatory treatment.<br />
Twenty Patients (12 males) with 2nd- 3rd degree symptomatic<br />
hemorrhoids have been treated with the described technique.<br />
RESULTS: Necrosis of the terminal hemorrhoidal arteries caused a<br />
progressive shrinkage of haemorrhoidal cushions and also a partial<br />
reduction of mucosal internal prolapse through shrinkage of mucosal/<br />
submucosal tissue.<br />
The procedure resulted to be successful in terms of improved symptoms<br />
in 95% of cases at a median follow-up of 6 months. No major adverse<br />
effects or complications were reported.<br />
Bleeding was observed intraoperatively in two cases. In one case surgical<br />
hemostasis was necessary. Minor pain requiring medication was reported<br />
in three cases(two intraoperatively).<br />
CONCLUSIONS: Doppler-guided closure of terminal branches of superior<br />
haemorrhoidal arteries with Diode-Laser represents a new proposal of<br />
mini-invasive treatment for patients suffering from 2nd and 3rd degree<br />
haemorrhoids without severe mucosal prolapse.<br />
This technique, if compared with previously described procedures, has<br />
several potential advantages: it is almost painless, it does not need<br />
anaesthesia, is technically easy to perform, has low morbidity rate and can<br />
be performed in a outpatients environment.<br />
ET21<br />
TRANSCOLONIC NOTES- PRELIMINARY HUMAN EXPERIENCE: NOTES<br />
TRANSRECTAL RECTOSIGMOID RESECTION AND TME Ricardo Zorron,<br />
Djalma Coelho, Luciana Flach, Fabiano Lemos, Moacyr Moreira, Priscila<br />
Oliveira, Alain Barbosa Department of Surgery - University Hospital<br />
Teresópolis HCTCO-FESO;Hospital Municipal Lourenco Jorge, Rio de<br />
Janeiro, Brazil<br />
Objectives: Clinical natural orifice surgery has been applied for<br />
abdominal surgery in recent years, using either a transvaginal or a<br />
transgastric access to perform the procedures. Despite potential<br />
advantages of using transcolonic NOTES to treat colorectal diseases, it<br />
was since now not yet clinically applied. The study describes the first<br />
successful series of human application of transcolonic NOTES access in the<br />
literature, in a new oncologic transrectal TME procedure for rectal cancer.<br />
Methods: Curative oncologic resection was indicated for 3 patients<br />
with diagnosed rectal adenocarcinoma at middle third of the rectum.<br />
IRB approval was obtained at the institution for the study, and the<br />
patients signed informed consent. Total mesorectal resection and<br />
rectosigmoidectomy with lymphadenectomy was performed using a<br />
posterior transcolonic access 3cm from the anal verge (Perirectal NOTES<br />
Access-PNA), and mesorectal dissection was achieved using flexible<br />
colonoscope and endoscopic instrumentation. In two cases, single port<br />
access was directly inserted in the rectum, and dissection was progressed<br />
proximally using LESS visualization. Laparoscopic assistance was used<br />
for IMA ligation and left colon mobilization. The specimen was extracted<br />
transanally, and stappled transorificial anastomosis was performed.<br />
Results: 3 patients were submitted to Transcolonic NOTES. Operative time<br />
was a mean of 350 min, no intraoperative complications occurred. The<br />
postoperative course at 15 days was uneventful, with resumption of oral<br />
diet on the second or third postoperative day. Pain scores were low for<br />
this initial casuistic.<br />
Conclusion: Successful first human series report on Transcolonic NOTES<br />
potentially brings new fronteers and future wider applications for<br />
minimally invasive surgery. The treatment of colorectal diseases through<br />
a flexible Perirectal NOTES Access (PNA) is a promising new approach<br />
besides existing laparoscopic and open surgery to improve patient care.<br />
ET22<br />
DUAL CONSOLE ROBOTIC SURGERY ENHANCES OPERATIVE TASK<br />
EFFICIENCY Michael M Awad, MD PhD, Eric Jenkins, MD, Lora Melman,<br />
MD, Brent Matthews, MD Washington University in St. Louis - School of<br />
Medicine<br />
OBJECTIVE - Robotic surgery has transformed the way in which<br />
laparoscopic surgery is conducted. However, it is still largely performed<br />
by a surgeon operating independently with little or no assistance. This<br />
potentially detracts from the efficiency that a skilled assistant may<br />
provide during complex procedures. The dual console for the da Vinci<br />
Si robot (Intuitive Surgical, Inc.) is an emerging technology that allows a<br />
second operator to provide real-time robotic assistance, possibly resulting<br />
in improved intra-operative efficiency. The potential benefits of the dual<br />
console have not been evaluated to date.<br />
METHODS - Surgeons with varying levels of laparoscopic and robotic<br />
experience were asked to perform four tasks using the single console or<br />
the dual console of the da Vinci Si robot. Surgeons who performed more<br />
than 100 laparoscopic procedures a year were considered ‘advanced’<br />
and all others were considered ‘novice.” Surgeons who performed more<br />
than 50 robotic procedures a year were considered ‘advanced’ and all<br />
others were considered ‘novice.’ The four timed tasks were: (1) FLS-style<br />
pattern cutting, (2) tension suturing, (3) hand-sewn bowel anastomosis,<br />
and (4) crural closure with mesh. Study subjects were asked to rate on a<br />
Likert scale the ease of performing each task using the single vs the dual<br />
console.<br />
RESULTS - Task performance was significantly improved when the<br />
dual console was employed compared to the single console. Surgeons<br />
universally rated the dual console as easier to use than the single console<br />
12 th World Congress of Endoscopic Surgery<br />
187 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Emerging Technology Oral Abstracts<br />
for all tasks. Differences in task performance were particularly pronounced<br />
for novice laparoscopic surgeons compared to advanced surgeons. There<br />
was an improvement in task performance even for advanced robotic<br />
surgeons when using the dual console.<br />
CONCLUSIONS / FUTURE STUDIES - The use of the dual console<br />
provided significant advantages in operative task efficiency for novice and<br />
advanced laparoscopic and robotic surgeons alike. The dual console adds<br />
significant costs to the institution. These costs may be partially recouped<br />
by reduced operative procedure times. Future studies will be needed to<br />
see if this advantage is realized in patient procedures.<br />
12 th World Congress of Endoscopic Surgery 188
Emerging Technology Poster Listings<br />
Full abstract texts available in the Electronic Meeting Guide<br />
ETP01 TRANSUMBILICAL CHOLECYSTECTOMY WITH FLEXIBLE<br />
ENDOSCOPE (NOTES–SILS), PRELIMINARY CLINICAL EXPERIENCE.<br />
José F Noguera, MD PhD, Angel Cuadrado, MD PhD, José M Olea, MD,<br />
Rafael Morales, MD, José C Vicens, MD, Hospital Son Llàtzer<br />
ETP02 NOVEL SIMULATOR FOR LAPAROSCOPIC INGUINAL HERNIA<br />
Yo Kurashima, MD PhD, Salman Al-Sabah, MD, Pepa Kaneva, MSc,<br />
Liane Feldman, MD, Gerald Fried, MD, Melina Vassiliou, MD, Steinberg-<br />
Bernstein Center for Minimally Invasive Surgery & Innovation, McGill<br />
University<br />
ETP03 FEASIBILITY OF A 3-D IMAGE-GUIDANCE SYSTEM FOR<br />
LAPAROSCOPIC LIVER RESECTION Shiva Jayaraman, MD MESc, Logan<br />
W Clements, PhD, James D Stefansic, PhD, Robert L Galloway, PhD,<br />
William R Jarnagin, MD, Hepatopancreatobiliary Service, Department<br />
of Surgery, Memorial Sloan-Kettering Cancer Center; Pathfinder<br />
Therapeutics Inc; Department of Biomedical Engineering, Vanderbilt<br />
University<br />
ETP04 A NOVEL RETRACTION INSTRUMENT IMPROVES THE SAFETY<br />
OF SINGLE INCISION LAPAROSCOPIC CHOLECYSTECTOMY Danny A<br />
Sherwinter, MD, Department of Minimally Invasive Surgery, Maimonides<br />
Medical Center<br />
ETP05 A NOVEL INSUFFLATING GUIDE-WIRE FOR TRANSGASTRIC<br />
NOTES Kiyokazu Nakajima, MD, Toshirou Nishida, MD, Tsuyoshi<br />
Takahashi, MD, Yoshihito Souma, MD, Masaki Mori, MD, Yuichiro Doki,<br />
MD, Osaka University Graduate School of Medicine, Osaka, Japan<br />
ETP06 SINGLE INCISION LAPAROSCOPIC SURGERY WITH A NOVEL<br />
PORT CAMERA SYSTEM Jonathan Schoen, MD, Benjamin S Terry,<br />
Zachary Mills, Aditya Bhave, Mark E Rentschler, PhD PE, University of<br />
Colorado at Boulder, University of Colorado at Denver<br />
ETP07 EFFECTS OF INCREASED LAPAROSCOPE COMPLEXITY ON<br />
MANEUVERABILITY AND PROFICIENCY Eric D Jenkins, MD, Michael<br />
Yip, BS, Lora Melman, MD, Margaret M Frisella, RN, Brent D Matthews,<br />
MD, Department of Surgery, Washington University, St Louis, Missouri<br />
ETP08 MINIATURE CAMERA FOR ENHANCED VISUALIZATION FOR<br />
SIMIS AND NOTES Mahmoud Abu Gazala, MD, Noam Shussman, MD,<br />
Avraham Schlager, MD, Ram Elazary, MD, Oleg Ponomarenko, MD, Abed<br />
Khalaileh, MD, Avraham I Rivkind, MD FACS, Yoav Mintz, MD, Hadassah<br />
Ein Kerem Medical Center<br />
ETP09 SIMULATING OPEN ABDOMINAL AORTIC ANEURYSM REPAIR:<br />
HIGH FIDELITY TEAM TRAINING AND EVALUATION FOR RESIDENTS<br />
Daniel A Hashimoto, BA, Ben Selvan, MD, Peter R McCombs, MD,<br />
Kristoffel Dumon, MD, Joseph Palmieri, MSEd, Josef Luba, Andrew S<br />
Resnick, MD, Noel N Williams, MD FRCSI, University of Pennsylvania<br />
School of Medicine, Penn Surgery Simulation, Philadelphia VAMC<br />
ETP10 A NEW METHOD FOR BOWEL ANASTOMOSIS BY SEALING Dirk<br />
W Meijer, MD MSc PhD, Jaap H Bonjer, MD PhD, BRG VUMC<br />
ETP11 CO2 LASER ENERGY FLEXIBLE TOOLS FOR MIS, NOTES<br />
AND SINGLE PORT SURGERY Oleg Ponomarenko, MD, Mahmoud<br />
Mahmoud Abu-Gazale, MD, Abed Khalaileh, MD, Ram Elazary, MD, Noam<br />
Shussman, MD, Avraham I Rivkind, MD, Yoav Mintz, MD, Department of<br />
Surgery, Hadassah Hebrew University Medical Center, Jerusalem, Israel<br />
ETP12 USE OF FLOSHIELD TO PREVENT LENS REMOVAL DURING<br />
SURGERY Wayne Poll, MD, Riverside Methodist Hospital<br />
ETP13 ENDOSCOPIC TRANSGASTRIC SUTURE CLOSURE Farid Kehdy,<br />
MD, Kenny King, Lindsay Strotman, Erica Wells, Guruprasad Giridharan,<br />
PhD, University of Louisville<br />
ETP14 A NEW METHOD FOR DETECTING COLORECTAL CANCER<br />
David Nasralla, MD MRCS, C Ferrett, MD FRCR, B George, MD FRCS, A<br />
Loktionov, PhD, Lywood H, MD, John Radcliffe Hospital, Oxford, UK;<br />
Colonix Medical, Cambridge, UK<br />
ETP15 MINIMALLY INVASIVE TUMOR ABLATION: A NEW ENDOSCOPIC<br />
APPROACH WITH THE ENDOVE DEVICE Declan M Soden, PhD, Patrick<br />
Forde, PhD, Gerald C O’Sullivan, MD, Cork Cancer Research Centre, UCC<br />
ETP16 OUTCOMES OF THORACOSCOPY FOR MYASTHENIA GRAVIS<br />
Vladimir N Nikishov, MD PhD, Eugeny I Sigal, MD PhD, Albert M Sigal,<br />
MD, Azat G Latipov, MD PhD, Tom L Sharapov, MD, Clinical Cancer<br />
Center, Kazan, Russia<br />
ETP17 THE LEARNING CURVE FOR SINGLE PORT INTRACORPOREAL<br />
SUTURE IN A MODIFIED FLS SIMULATOR S. Al-Sabah, MD MBA, MC.<br />
Vassiliou, MD, PA. Kaneva, MSc, R. Ribeiro, MD, Y. Kurashima, MD, GM<br />
Fried, MD, LS Feldman, MD, Steinberg-Bernstein Centre for Minimally<br />
Invasive Surgery and Innovation, McGill University Health Centre,<br />
Montreal, Canada<br />
ETP18 ENDOSCOPIC INFRARED COAGULATION: BROAD RANGE<br />
OF NOVEL AND PRACTICAL UTILITY RANGING FROM INTERNAL<br />
HEMORRHOIDS TO NOTES Elisabeth C McLemore, MD, Sonia<br />
Ramamoorthy, MD, Mark A Talamini, MD, University of California San<br />
Diego<br />
ETP19 TECHNIQUES OF RADIOFREQUENCY-ASSISTED PRE-<br />
COAGULATION IN LAPAROSCOPIC LIVER RESECTION Hizir Y Akyildiz,<br />
MD, Morris Stiff, MD, Frederico Aucejo, MD, John Fung, MD, Eren Berber,<br />
MD, Cleveland Clinic General Surgery Department<br />
ETP20 TOWARDS SPHINCTER OF ODDI-PRESERVING AND T-TUBE FREE<br />
LAPAROSCOPIC COMMON BILE DUCT EXPLORATION Shuo-Dong Wu,<br />
MD PhD, Chun-Chih Chen, MD, Ying Fan, MD MS, Ernest A Siwo, MD, The<br />
Department of Biliary and Vascular Surgery, Shengjing Hospital of China<br />
Medical University<br />
ETP21 ROBOTIC SINGLE PORT LAPAROSCOPIC CHOLECYSTECTOMY<br />
Sherry M Wren, MD, Myriam J Curet, MD, Stanford University School of<br />
Medicine and Palo Alto Veterans Health Care System<br />
ETP22 SUTURE RETRACTION TECHNIQUES: ELIMINATING PORTS TO<br />
FACILITATE BASIC AND COMPLEX SINGLE INCISION LAPAROSCOPIC<br />
SURGERY Daniel J Rosen, MD, Jenny Choi, MD, Marc Bessler, MD,<br />
Columbia University Medical Center, Beth Israel Medical Center<br />
ETP23 AN INSTRUMENTED SURGICAL TOOL FOR RELIABLE ISCHEMIA<br />
DETECTION Philip Roan, Andrew S Wright, MD, Mika Sinanan, MD<br />
PhD, Blake Hannaford, PhD, University of Washington: Department of<br />
Electrical Engineering, Department of Surgery<br />
ETP24 A VIRTUAL REALITY SIMULATOR FOR THE LAPAROSCOPIC<br />
EXAMINATION OF THE SMALL INTESTINES Matthew Johnson, MD,<br />
Tony Rubin, Anders Larsson, Shawn Tsuda, MD, University of Nevada<br />
School of Medicine<br />
ETP25 NEW TRANSVAGINAL PORT SYSTEM FOR RIGID AND FLEXIBLE<br />
NOTES CHOLECYSTECTOMY- HUMAN EXPERIENCE Ricardo Zorron,<br />
Marcos Filgueiras, Daniel Leal, Eduardo Kanaan, Priscila Oliveira, Gustavo<br />
Lessa, Henrique Phillips, Department of Surgery – University Hospital<br />
Teresópolis HCTCO-FESO;Hospital Municipal Lourenco Jorge, Rio de<br />
Janeiro, Brazil<br />
ETP26 IMPULSIVE HEAT DEPOSITION (IHD) LASER AND ITS POTENTIAL<br />
USE IN SURGERY AND ENDOSCOPY E Dubcenco, MD, T Grantcharov,<br />
MD, C J Streutker, MD, D Kraemer, M L Cowan, N N Baxter, MD, O D<br />
Rotstein, MD, RJ D Miller, J P Baker, St. Michael’s Hospital; Keenan<br />
Research Centre in the Li Ka Shing Knowledge Institute; University of<br />
Toronto; Toronto, Ontario, Canada<br />
ETP27 SINGLE INCISION LAPAROSCOPIC COMBINED PARTIAL<br />
GASTRECTOMY ,DISTAL PANCRECTOMY AND PARTIAL COLECTOMY<br />
: THE FIRST ONE CASE Shuo-Dong Wu, MD PhD, Ying Fan, MD MS, Yang<br />
Su, MD PhD, The Department of Biliary and Vascular Surgery, Shengjing<br />
Hospital of China Medical University<br />
ETP28 SINGLE PORT SURGERY ON PROMIS SIMULATOR Donncha Ryan,<br />
Fiona Slevin, Nicolas Sezille, Derek Cassidy, Haptica Inc., Boston<br />
ETP29 BETWEEN LAP AND LESS: THE EVOLUTION OF<br />
MICROLAPAROSCOPY Ralf Kleemann, PhD, Thomas Aue, Philippe Hall,<br />
MD PhD, Olympus Winter & Ibe<br />
12 th World Congress of Endoscopic Surgery<br />
189 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Emerging Technology Poster Listings<br />
Full abstract texts available in the Electronic Meeting Guide<br />
ETP30 MULTI-SCREEN, HANDS-FREE POINTER SYSTEM FOR TRAINING<br />
IN MINIMALLY INVASIVE SURGERY C D Ward, MESc, A L Trejos, MASc,<br />
M D Naish, PhD, R V Patel, PhD PEng, C M Schlachta, MD, Canadian<br />
Surgical Technologies and Advanced Robotics (CSTAR)<br />
ETP31 SINGLE PORT ACESS SURGERY 2.0 Paul G Curcillo II, MD, Erica<br />
R Podolsky, MD, Stephanie A King, MD, Drexel University College of<br />
Medicine<br />
ETP32 ASSESSMENT OF MULTI-SPECTRAL IMAGING FOR ENHANCED<br />
VISUALIZATION IN MINIMALLY INVASIVE SURGERY Matthew Field,<br />
Duncan Clarke, PhD, W B Seales, PhD, University of Kentucky<br />
ETP33 A RANDOMIZED CONTROL STUDY TO COMPARE A NEW<br />
VALVELESS TROCAR WITH A CONVENTIONAL TROCAR IN MORBIDLY<br />
OBESE PATIENTS Clinton Hall, MD, Nilay Shah, MD, Eric Volckmann, MD,<br />
Vanchad Memark, MD, Alexandar Haas, BS, W. Scott Melvin, MD, Dean<br />
Mikami, MD, Bradley Needleman, MD, Center for Minimally Invasive<br />
Surgery, Department of Surgery, The Ohio State University Medical<br />
Center, Columbus, Ohio<br />
ETP34 NITINOL COMPRESSION ANASTOMOSIS RING FOR<br />
RESTORATION OF INTESTINAL CONTINUITY AFTER RECTO-SIGMOID<br />
RESECTIONS. Dan Shteinberg, MD, Gideon Sroka, MD MSc, Foad<br />
Misharky, RN, Ibrahim Matter, MD, Department of General Surgery,Bnai-<br />
Zion Medical Center, Haifa, Israel.<br />
ETP35 NOTES CADAVERIC HYBRID SMALL BOWEL RESECTION:<br />
IMPROVED TECHNIQUE USING A NOVEL STEERABLE TROCAR,<br />
FLEXIBLE POWERED STAPLER, MAGNETIC CAMERA, AND<br />
INTERNALLY-ASSEMBLED PERCUTANEOUS INSTRUMENTS Byron F<br />
Santos, MD, Eric S Hungness, MD, Northwestern University, Department<br />
of Surgery<br />
ETP36 CADAVERIC SINGLE-SITE LAPAROSCOPIC CHOLECYSTECTOMY<br />
USING NOVEL ARTICULATING INSTRUMENTS, MAGNETIC<br />
ELECTROCAUTERY, AND INTERNALLY-ASSEMBLED PERCUTANEOUS<br />
INSTRUMENTS Byron F Santos, MD, Eric S Hungness, Northwestern<br />
University, Department of Surgery<br />
ETP37 COMPARISON OF N.O.T.E.S. AND LAPAROSCOPIC SURGICAL<br />
MOTION CHARACTERISTICS Balazs I Lengyel, MD, Dan E Azagury, MD,<br />
Marvin Ryou, MD, Sohail N Shaikh, MD, Raul E San Jose, PhD, Michele B<br />
Ryan, MS, Keith Obstein, MD, Vaibhav D Patil, MD, Jayender Jagadeesan,<br />
PhD, Christopher C Thompson, MD MHES, Kirby G Vosburgh, PhD,<br />
Brigham and Women’s Hospital / Harvard Medical School<br />
ETP38 VIRTUAL MEASURING OF ANATOMICAL STRUCTURES IN 3D<br />
DIGITAL MEDICAL IMAGE DATA FOR LAPAROSCOPIC SURGICAL<br />
PLANNING Marisol Martinez Escobar, MS, Catherine Peloquin, MS,<br />
Kenneth Kopecky, MS, Jung-Leng Foo, PhD, Eliot Winer, PhD, Thom Lobe,<br />
MD, Iowa State University & Blank Children’s Hospital<br />
ETP39 UTILITY OF MAGNETIC RESONANCE ENTEROGRAPHY IN<br />
SURGICAL DECISION-MAKING FOR CROHN’S DISEASE Anjali S<br />
Kumar, MD MPH, Raman Battish, MD, Duncan P Yoder, MD, Reena<br />
Chhitwal, MD, Kevin Olden, MD, James D McFadden, MD, Thomas Stahl,<br />
MD, Washington Hospital Center - Departments of Gastroenterology,<br />
Radiology, and Colon & Rectal Surgery<br />
ETP40 A NOVEL LAPAROSCOPIC BOX TRAINER WITH INTEGRATED<br />
FORCE AND POSITIONING SENSORS Timothy Kowalewski, Andrew<br />
S Wright, MD, Jacob Rosen, PhD, Blake Hannaford, PhD, University of<br />
Washington<br />
ETP41 OSIRIX SURGICAL NAVIGATION SYSTEM USING IMAGE<br />
OVERLAY IN NOTES AND SINGLE PORT ENDOSCOPIC SURGERY<br />
Maki Sugimoto, MD PhD, Takeshi Azuma, Prof, Gastroenterology Kobe<br />
University Graduate School of Medicine<br />
ETP42 EVALUATION OF THE EFFICACY OF LIGASURETM DEVICES IN<br />
SEALING OF LUNG PARENCHYMA Rebecca Coulson, Ms, Kimberly<br />
Martin, BS, Kimberly Krugman, MS, Ned Cosgriff, MD, Covidien Energy<br />
Based Devices Boulder, Co<br />
ETP43 THE SELF-APPROXIMATING TRANSLUMENAL ACCESS<br />
TECHNIQUE (STAT) FOR NOTES HELLER MYOTOMY IN A HUMAN<br />
CADAVER Jegan Gopal, MD, Eric M Pauli, MD, Randy S Haluck, MD,<br />
Matthew M Moyer, MD, Sami S Tannouri, MS, Brooke B Ancrile, PhD,<br />
Ann M Rogers, MD, Abraham Mathew, MD, Penn State Hershey Medical<br />
Center, Hershey, PA<br />
ETP44 OPTIMIZED ABLATION AND PROBE PLACEMENT VIA<br />
MATHEMATICAL MORPHOLOGY Brady King, Luke Reisner, Madhu<br />
Prasad, MD, Abhilash Pandya, PhD, Electrical and Computer Engineering,<br />
Wayne State University, Detroit, MI; Department of Surgery, Henry Ford<br />
Hospital, Detroit, MI<br />
ETP45 HIGH TEMPERATURE SUPERCONDUCTOR MAGNETIC<br />
INSTRUMENTATION FOR NATURAL ORIFICE TRANSLUMINAL<br />
ENDOSCOPIC SURGERY (N.O.T.E.S.) AND OTHER LIMITED ACCESS<br />
SURGICAL OPERATIONS Ronan A Cahill, MD, Richard P Lewin, PhD,<br />
Neil J Mortensen, MD, Harry Jones, PhD, Department of Colorectal<br />
Surgery, Oxford Radcliffe Hospitals, Oxford, UK & Clarendon Laboratory,<br />
Department of Physics. Oxford University, Oxford, UK.<br />
ETP46 COST EFFECTIVE SIMULATION BASED ENDOCRINE SURGERY<br />
TRAINING MODULE Mayank K Mittal, MD MRCS, Ben Selvan, MD MS,<br />
K R Dumon, MD, A S Resnick, MD, N N Williams, MD, J B Morris, MD, R R<br />
Kelz, MD MSCE, Penn Medicine Clinical Simulation Center, Philadelphia<br />
ETP47 A DEVICE SYSTEM FOR EFFICIENT LAPAROSCOPIC AND SILS<br />
VENTRAL HERNIA REPAIR Bruce Ramshaw, MD, Andrew J Duffy, MD,<br />
Einat Duvdevany, Daniel Marcus, MD, Yoav Mintz, MD, Guy Voeller, MD,<br />
Halifax Medical Center<br />
ETP48 EARLY RESULTS OF LOTUS (LAPAROSCOPIC OPERATING BY<br />
TORSIONAL ULTRASOUND) IN LAPAROSCOPIC LIVER RESECTION<br />
Neil W Pearce, DM FRCS, Mohammad Abu Hilal, MD FRCS, *Steven M<br />
Young, DPhil ARCS, Dept of Surgery, Southampton University Hospitals,<br />
Southampton, UK. *SRA Developments, Ashburton, Devon, UK<br />
ETP49 REAL-TIME 3D VISUALIZATION OF ORGAN DEFORMATIONS IN<br />
MINIMUM INVASIVE SURGERY Dan Wang, Ahmed H Tewfik, PhD, Bruce<br />
Hammer, PhD, Timothy Kinney, MD, Eric Jensen, MD, Juliane Bingener-<br />
Casey, MD, Bradley Erickson, MD, University of Minnesota<br />
ETP50 USE OF THE SUMO PROCEDURE FOR ENDOSCOPIC<br />
SUBMUCOSAL RESECTION OF SUPERFICIAL ESOPHAGEAL LESIONS<br />
Richard A Pierce, MD PhD, Danny V Martinec, BS, Christy M Dunst, MD,<br />
Lee L Swanstrom, MD, Legacy Health System, Division of Minimally<br />
Invasive Surgery, Portland, OR, USA<br />
ETP51 LAPAROSCOPIC SINGLE PORT INTRACORPREAL SUTURING:<br />
TIPS AND TRICKS S. Al-Sabah, MD MBA, R. Ribeiro, MD, Y. Kurashima,<br />
MD, MC Vassiliou, MD, GM Fried, MD, LS Feldman, MD, Steinberg-<br />
Bernstein Centre for Minimally Invasive Surgery and Innovation, McGill<br />
University Health Centre<br />
ETP52 TRANS-GASTRIC ENDO-ORGAN RESECTION OF GASTRO-<br />
ESOPHAGEAL JUNCTION ADENOCARCINOMA. Aru Panwar, MD,<br />
Tommy H Lee, MD, Charles Filipi, MD, Sumeet Mittal, MD, Division of<br />
esophageal surgery, Department of surgery, Creighton University,<br />
Omaha, Nebraska, USA<br />
ETP53 ACCELERATED WOUND HEALING WITH TOPICALLY DELIVERED<br />
DISSOVED OXYGEN Andrew Slemp, MD, Alan Dine, BSN, Bruce Gibbins,<br />
PhD, Carillion Wound Care Clinic, Acrymed Inc.<br />
ETP54 CURVED INSTRUMENTS FOR SINGLE PORT LAPAROSCOPY: THE<br />
WAY TO GO? Nicole Bouvy, Rob Strijkers, Sofie Fransen, Sanne Botden,<br />
MD PhD, LAurents Stassen, MD PhD, Maastricht University Medical<br />
Center<br />
ETP55 DEVELOPMENT OF A MODIFIED SKILLS TRAINER FOR SINGLE<br />
INCISION LAPAROSCOPY Andrew S Wright, MD, Saurabh Khandelwal,<br />
MD, Brant K Oelschlager, MD, University of Washington<br />
12 th World Congress of Endoscopic Surgery 190
Emerging Technology Poster Listings<br />
Full abstract texts available in the Electronic Meeting Guide<br />
ETP56 NATURAL ORIFICE TRANSLUMINAL ENDOSCOPIC SURGERY<br />
(NOTES) DISTAL PANCREATECTOMY IN A PORCINE SURVIVAL<br />
MODEL USING A TRANSVAGINAL APPROACH. Linda Barry, MD,<br />
Seaborn A Roddenbery, MD, Alexander Rosemurgy, MD, Sujat Dahal,<br />
MD, Sharona B Ross, MD, Leo Ondrovic, PhD, University of South Florida<br />
Department of Surgery<br />
ETP57 USE OF TYLE PRO SYSTEM FOR INTRAOPERATIVE NAVIGATION<br />
DURING ROBOTIC SURGERY Savvas Hiridis, MD, Konstantinos<br />
Kostantinidis, MD PhD, Pericles J Chrysoheris, MD, Athens Medical<br />
Center<br />
ETP58 TRACKING LAPAROSCOPIC ULTRASOUND PROBE IMPROVES<br />
SURGEON PERFORMANCE: EARLY CLINICAL EXPERIENCE James<br />
Ellsmere, MD, Jeffery Stoll, PhD, Raúl San José Estépar, PhD, Kirby<br />
Vosburgh, PhD, Dalhousie University, Halifax NS and Massachusetts<br />
General Hospital and Brigham and Women’s Hospitals, Boston MA<br />
ETP59 CLOSURE OF A FULL THICKNESS GASTRIC MUCOSAL<br />
DEFECT WITH THE APOLLO ENDOSURGERY, INC. OVERSTITCHTM<br />
ENDOSCOPIC SUTURING SYSTEM (ESS). Chike V Chukwumah, MD,<br />
Jeffrey M Marks, MD, University Hospitals Case Medical Center<br />
ETP60 TRANSORAL INCISIONLESS FUNDOPLICATION IS EFFECTIVE<br />
FOR THE TREATMENT OF CHRONIC GERD PATIENTS WITH THERAPY-<br />
RESISTANT SYMPTOMS Kevin M Hoddinott, MD, Madeline Williams,<br />
CRNFA, Monroe Regional Medical Center, Ocala, Florida<br />
12 th World Congress of Endoscopic Surgery<br />
191 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Notes<br />
12 th World Congress of Endoscopic Surgery 192
Exhibit Hall Floor Plan<br />
CONCESSIONS<br />
20'<br />
20'<br />
20'<br />
848<br />
748 749<br />
648 649<br />
548 549<br />
449<br />
20'<br />
349<br />
20'<br />
20'<br />
847<br />
846<br />
746 747<br />
646 647<br />
546 547<br />
447<br />
446<br />
347<br />
147 247<br />
LEARNING<br />
CENTER<br />
ENTRANCE<br />
20'<br />
842 843<br />
742 743<br />
20'<br />
642<br />
543<br />
542<br />
20'<br />
20'<br />
342<br />
243<br />
143<br />
840 841<br />
740 741<br />
641<br />
640<br />
541<br />
540<br />
441<br />
341<br />
340<br />
241<br />
141<br />
839<br />
139<br />
20'<br />
20'<br />
837<br />
20'<br />
736<br />
20'<br />
20' 20'<br />
20'<br />
237 336 337 436<br />
20'<br />
835<br />
735<br />
734<br />
635<br />
634<br />
535<br />
435<br />
235 334 335 434<br />
20'<br />
20'<br />
40'<br />
20'<br />
333<br />
233<br />
131<br />
ENTRANCE<br />
831<br />
20'<br />
730<br />
20'<br />
430<br />
331<br />
40'<br />
829<br />
727<br />
728<br />
629<br />
40'<br />
30'<br />
827<br />
726<br />
20'<br />
20'<br />
40'<br />
30'<br />
825<br />
20'<br />
724<br />
625<br />
425<br />
823<br />
723<br />
C<br />
323<br />
123<br />
60'<br />
30'<br />
50'<br />
20'<br />
819<br />
20'<br />
20'<br />
817<br />
717<br />
60'<br />
117<br />
50'<br />
20'<br />
30'<br />
20'<br />
813<br />
20'<br />
20'<br />
811<br />
711<br />
411<br />
213<br />
111<br />
193 www.12thworldcongress.org<br />
Inventory as of 03/10/201<br />
Size<br />
100<br />
200<br />
400<br />
600<br />
900<br />
1,600<br />
2,500<br />
3,600<br />
Dimension<br />
10'x10'<br />
10'x20'<br />
20'x20'<br />
20'x30'<br />
30'x30'<br />
40'x40'<br />
50'x50'<br />
60'x60'<br />
40'<br />
706<br />
20'<br />
606<br />
507<br />
506<br />
20'<br />
406<br />
306 307<br />
20' 20'<br />
40'<br />
20'<br />
605<br />
604<br />
505<br />
504<br />
405<br />
20' 20' 20'<br />
205<br />
204<br />
702<br />
603<br />
602<br />
503<br />
502<br />
402 403<br />
302 303<br />
203<br />
202<br />
Totals:<br />
700<br />
**174 DOUBLE SIDED<br />
9900 Business Parkway<br />
Lanham, Md 20706<br />
12 th World Congress of Endoscopic Surgery<br />
03.10.<strong>2010</strong><br />
<strong>SAGES</strong> & CAGS 12TH WORLD CONGRESS OF ENDOSCOPIC SURGERY<br />
APRIL 14-17, <strong>2010</strong><br />
GAYLORD NATIONAL RESORT & CONVENTION CENTER - PRINCE GEORGE'S BALLROOMS A-D<br />
NATIONAL HARBOR, MD<br />
EVERY EFFORT HAS BEEN MADE TO ENSURE THE ACCURACY OF ALL INFORMATION CONTAINED ON THIS FLOORPLAN. HOWEVER, NO WARRANTIES, EITHER EXPRESSED OF IMPLIED, ARE MADE WITH RESPECT TO THIS FLOORPLAN. IF THE LOCATION OF BUILDING COLUMNS, UTILITIES<br />
OR OTHER ARCHITECTURAL COMPONENTS OF THE FACILITY IS A CONSIDERATION IN THE CONSTRUCTION OR USAGE OF AN EXHIBIT, IT IS THE SOLE RESPONSIBILITY OF THE EXHIBITOR TO PHYSICALLY INSPECT THE FACILITY TO VERIFY ALL DIMENSION AND LOCATIONS.<br />
COPYRIGHT 2000, FREEMAN DECORATING CO., ALL RIGHTS RESERVED.
12 th World Congress of Endoscopic Surgery<br />
Exhibitor Profiles<br />
3-Dmed #604<br />
255 Industrial Drive<br />
Franklin, OH 45005<br />
Tel: 937-746-2901<br />
Fax: 937-746-5071<br />
Website: www.3-dmed.com<br />
3-Dmed is the innovator and manufacturer<br />
of the Minimally Invasive Training System<br />
(MITS) that provides a creative environment<br />
to practice and teach laparoscopic skills,<br />
procedures, camera navigation, and instrument<br />
demonstration. 3-Dmed MITS is a complete and<br />
portable system that is the best value for your<br />
budget.<br />
Residents can practice on the MITS to acquire<br />
the FLS skills. Try the New FLS Practice Board<br />
and other models.<br />
AESCULAP, INC. #111<br />
3773 Corporate Parkway, Center Valley, PA<br />
18034<br />
Tel: (800)258-1946 ext. 5247<br />
Fax: (610)791-6884<br />
Website: www.aesculapusa.com<br />
Aesculap is a leading manufacturer and supplier<br />
of handheld instruments for minimally invasive<br />
surgery. These laparoscopic instruments<br />
combine precision craftsmanship with modern<br />
materials and design. Precise performance<br />
makes Aesculap laparoscopic instruments the<br />
instrument of choice for today’s and tomorrow’s<br />
surgery.<br />
AGENCY FOR MEDICAL<br />
INNOVATIONS, INC. #648<br />
20 Main Street, Suite 205<br />
Natick, MA 01760<br />
Tel: 508-655-1200<br />
Fax: 508-655-0012<br />
Website: www.amisurgical.com<br />
The (DG)HAL/RAR Doppler guided Hemorrhoid<br />
Arterial Ligation/Recto Anal Repair System is the<br />
first system to utilize minimally invasive surgical<br />
techniques to treat the source of hemorrhoidal<br />
disease without surgical excision, stapling or<br />
banding. Additional products include Facia<br />
cutter and gastric band cutter.<br />
ALACE-SOBRACIL <strong>2010</strong> #829<br />
Rua do Carmo, 6 – 601 Centro<br />
Rio de Janeiro 20011-020 - Brazil<br />
Tel: 55-21-2215-4476<br />
Website: www.alacesobracil<strong>2010</strong>.com<br />
ALLERGAN #723<br />
2525 Dupont Drive<br />
Irvine, CA 92612<br />
Tel: 714-246-4500<br />
Fax: 714-246-4971<br />
Website: www.allergan.com<br />
Allergan has joined the effort to fight the<br />
growing obesity epidemic with the LAP-BAND®<br />
Adjustable Gastric Banding System, the first<br />
minimally invasive surgical approach approved<br />
in the United States by the FDA, to help patients<br />
achieve sustained weight loss, realize their goals<br />
for healthy living, and reduce obesity-related<br />
risks.<br />
ALOKA ULTRASOUND #605<br />
10 Fairfield Boulevard<br />
Wallingford, CT 06942<br />
Tel: (203) 269-5088<br />
Toll Free: (800) 872-5652<br />
Fax: (203) 269-6075<br />
Website: www.aloka.com<br />
Aloka’s commitment to ultrasound offers a<br />
range of consoles and transducers to meet<br />
surgeons needs. Recognized for our image<br />
quality, system reliability and intuitive use of<br />
cutting edge technology, Aloka remains the<br />
standard in the field of ultrasound for surgeons.<br />
AMERICAN COLLEGE OF<br />
SURGEONS #549<br />
Bariatric Surgery Center<br />
Network (ACS BSCN) Accreditation <strong>Program</strong><br />
633 North Saint Clair Street<br />
Chicago, IL 60611<br />
Tel: 312-202-5000<br />
Fax: 312-202-5063<br />
Website: www.acsbscn.org<br />
The American College of Surgeons continues its<br />
dedication to quality improvement through the<br />
Bariatric Surgery Center Network Accreditation<br />
<strong>Program</strong>. The ACS BSCN accredits facilities that<br />
have undergone an independent, rigorous<br />
peer evaluation in accordance with nationally<br />
recognized bariatric standards and participate<br />
in the program’s longitudinal outcomes<br />
database. Please visit booth 549 for information<br />
regarding program standards and enrollment.<br />
APOLLO ENDOSURGERY # 634<br />
7000 Bee Caves Rd, Suite 250, Austin, TX 78746<br />
Phone: 512-328-9990<br />
Fax: 512-328-9994<br />
Website: www.apolloendo.com<br />
Apollo Endosurgery is...Revolutionizing<br />
Patient Care through the Evolution of Flexible<br />
Surgery through the development of flexible<br />
endoscopic surgical tools. Our collaboration<br />
with physicians, providers, and the healthcare<br />
community is critical to delivering the future of<br />
advanced minimally invasive care.<br />
ARAGON SURGICAL #730<br />
1810 Embarcadero Road, Suite B<br />
Palo Alto, CA 94303<br />
Tel: 650-543-3100<br />
Fax: 650-318-1857<br />
Website: www.aragonsurgical.com<br />
Aragon Surgical is dedicated to pioneering<br />
utilization of its proprietary Lektrafuse<br />
technology in applications unmet by current<br />
RF tissue and vessel sealing devices. Aragon<br />
Surgical’s unique instruments are designed<br />
to help general and gynecologic surgeons in<br />
laparoscopic and open procedures.<br />
ARMY MEDICAL RECRUITING<br />
#717<br />
Munoz Building #206 - 9th Cavalry Reg. Ave.<br />
Ft Knox, KY 40121<br />
Tel: 502-626-0856; 502-626-1981<br />
Fax: 502-626-0854<br />
Website: www.healthcare.goarmy.com<br />
ARROW MARKET RESEARCh<br />
#347<br />
One Meridian Boulevard<br />
Wyomissing, PA 19610<br />
Arrow Market Research is a market research<br />
firm gathering qualitative and quantitative<br />
information for use within the medical device<br />
surgical market. Incentives will be provided for<br />
your valued opinion.<br />
ASCENT HEALTHCARE<br />
SOLUTIONS #117<br />
10232 S. 51st Street<br />
Phoenix, AZ 85044<br />
Tel: 800-887-9073<br />
Fax: 480-763-5320<br />
Website: www.ascenths.com<br />
Ascent is a medical device company leading<br />
the industry’s pursuit of more sustainable and<br />
responsible use of resources in healthcare<br />
through reprocessing and other programs.<br />
ATRIUM MEDICAL<br />
CORPORATION #446<br />
5 Wentworth Drive<br />
Hudson, NH 03051<br />
Tel: 603-880-1433<br />
Fax: 603-386-6266<br />
Website: www.atriummedical.com<br />
Atrium’s C-QUR Mesh family of hernia<br />
products combine our industry-leading<br />
ProLite polypropylene with a proprietary<br />
Omega 3 fatty acid absorbable coating.<br />
Pre-clinical studies demonstrate minimized<br />
tissue attachment and significant reduction<br />
in inflammation, resulting in a well healed,<br />
reinforced repair.<br />
12 th World Congress of Endoscopic Surgery 194
Exhibitor Profiles<br />
AUTOMATED MEDICAL<br />
PRODUCTS CORPORATion<br />
#502<br />
P.O. Box 2508<br />
Edison, NJ 08818<br />
Tel: 732-602-7717<br />
Fax: 732-602-7706<br />
Website: www.ironintern.com<br />
Automated Medical Products Corp offers the<br />
Iron Intern® Available for use in laparoscopic<br />
and open surgery. The Iron Intern® Stieber<br />
Rib Grip Kit provides superior exposure in the<br />
abdomen and serves liver transplants.<br />
BARIATRIC TIMES #827<br />
Matrix Medical Communications<br />
1595 Paoli Pike, Suite 103<br />
West Chester, PA 19380<br />
Tel: 866-325-9907<br />
Fax: 484-266-0726 Fax<br />
Website: www.Bariatrictimes.com<br />
Please stop by Booth 827 to pick up the recent<br />
issue of Bariatric Times and receive discounts<br />
on our educational textbooks, including<br />
the recently published Weight Loss Surgery:<br />
A Multidisciplinary Approach, edited by Drs.<br />
Raul Rosenthal and Dan Jones. New for <strong>2010</strong>:<br />
International attendees can register to receive a<br />
complimentary subscription to Bariatric Times<br />
International Edition, published exclusively in<br />
digital format.<br />
BÂRRX MEDICAL, INC. #702<br />
540 Oakmead Parkway<br />
Sunnyvale, CA 94085<br />
Tel: 408-328-7300<br />
Fax. 408-328-7395<br />
Website: www.barrx.com<br />
Developed by BÂRRX Medical, Inc. the HALO<br />
System provides a uniform and controlled<br />
ablation effect, removing the diseased tissue<br />
and allowing regrowth of normal cells for the<br />
treatment of Barrett’s esophagus, radiation<br />
proctitis and gastric antral vascular ectasia<br />
(GAVE).<br />
B-K MEDICAL SYSTEMS, INC.<br />
#436<br />
8 Centennial Drive<br />
Peabody, MA 01960<br />
Tel: 978-326-1300<br />
Fax: 978-326-1399<br />
Website: www.bkmed.com<br />
Designed for surgeons and to suit the OR,<br />
the Pro Focus UltraView has a wide range<br />
of specialized surgical transducers for<br />
percutaneous, laparoscopic and intraoperative<br />
scanning. With the mobile Flex Focus for breast<br />
scanning, you can afford to see everything.<br />
B-LINE MEDICAL #233<br />
1300 19th Street. NW, Suite 100<br />
Washington, DC 20036<br />
Tel: 301-768-4461<br />
Fax: 202-223-1171<br />
Website: www.blinemedical.com/<br />
B-Line Medical is a software firm specializing<br />
in web-based solutions for recording and<br />
assessment of simulation-based medical<br />
training. B-Line Medical’s SimCapture® and<br />
SimBridge® products are currently used in over<br />
100 top hospitals, medical schools and nursing<br />
programs in 6 different countries.<br />
BOSTON SCIENTIFIC, INC. #405<br />
100 Boston Scientific Way<br />
Marlboro, MA 01752<br />
Tel: 508 683 4000<br />
Website: www.bostonscientific.com<br />
BSC Endoscopy develops a broad spectrum of<br />
diagnostic and therapeutic devices for a variety<br />
of digestive diseases throughout the GI tract.<br />
We are committed to innovation, collaboration<br />
and less invasive, more efficient procedures that<br />
contribute to better patient outcomes.<br />
BUFFALO FILTER #547<br />
595 Commerce Drive<br />
Buffalo, NY 14228<br />
Tel: 716-835-7000<br />
Fax: 716-835-3414<br />
Website: www.buffalofilter.com<br />
Buffalo Filter® is a medical device manufacturer<br />
with a primary focus on manufacturing and<br />
engineering products for the evacuation and<br />
filtration of hazardous smoke plume generated<br />
during laser/electrosurgical procedures.<br />
Products include: surgical smoke evacuators,<br />
ULPA/HEPA replacement filters.<br />
CAE HEALTHCARE #842<br />
8585 Cote de Liesse<br />
Montreal, Quebec H4T 1G6 – Canada<br />
Tel: 514-341-6780<br />
Website: www.cae.com<br />
CALMOSEPTINE, INC. #307<br />
16602 Burke Lane<br />
Huntington Beach, CA 92647-4536<br />
Tel: (714) 840 - 3405<br />
Fax: (714) 840 – 9810<br />
Website: www.calmoseptine.com<br />
Calmoseptine Ointment is a multi-purpose<br />
moisture barrier that protects and helps<br />
heal skin irritations from moisture, such as<br />
urinary and fecal incontinence. Calmoseptine<br />
Ointment temporarily relieves discomfort and<br />
itching. Free samples at our booth!<br />
CANADIAN ASSOCIATION OF<br />
GENERAL SURGEONS (CAGS)<br />
#823<br />
774 Echo Drive<br />
Ottawa, ON K1S 5N8 - Canada<br />
Tel: 613-730-6280<br />
Fax: 613-730-1116<br />
Website: www.cags-accg.ca<br />
The Canadian Association of General Surgeons<br />
strives to be the voice of General Surgery across<br />
Canada by promoting the training, education,<br />
continuing professional development,<br />
thoughtful practice and research essential to<br />
exemplary surgical care.<br />
CAREFUSION #247<br />
3750 Torrey View Court<br />
San Diego, CA 92130<br />
Phone: 888-876-4287<br />
Website: www.carefusion.com<br />
CareFusion brings technology and<br />
intelligence together to help make the care<br />
process easier for caregivers and safer for<br />
patients. Our clinically proven products and<br />
services help reduce medication errors and<br />
healthcare-associated infections. Our portfolio<br />
encompasses some of the most trusted brands<br />
in healthcare, including Alaris®, ChloraPrep®,<br />
Nicolet, Pyxis® and V. Mueller®.<br />
CINE-MED, INC. #303<br />
127 Main Street N<br />
Woodbury, CT 06798<br />
Tel: 203-263-0006<br />
Fax: 203-263-4839<br />
Website: www.cine-med.com<br />
Ciné-Med partners with <strong>SAGES</strong> to produce and<br />
distribute the <strong>SAGES</strong> video library, including<br />
<strong>SAGES</strong> Grand Rounds, Postgraduate Courses,<br />
Top 14, and the <strong>SAGES</strong> Pearls series. Stop by<br />
booth #303 for more information and to view<br />
samples of these videos and more.<br />
CONMED CORPORATION #441<br />
525 French Road, Utica NY 13502<br />
Tel: 800-448-6506<br />
Fax: 800-438-3051<br />
Website: www.conmed.com<br />
CONMED specializes in Arthroscopy,<br />
Electrosurgery, Endoscopy, Imaging, Integrated<br />
Systems, Patient Care and Powered Instruments<br />
that are sold worldwide through its family of<br />
companies (CONMED & Linvatec).<br />
12 th World Congress of Endoscopic Surgery<br />
195 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Exhibitor Profiles<br />
COOK MEDICAL #402<br />
750 Daniels Way<br />
Bloomington, IN 47404<br />
Tel: 800-457-4500<br />
Fax: 800-554-8335<br />
Website: www.cookmedical.com<br />
Cook Medical was one of the first companies<br />
to help popularize interventional medicine,<br />
pioneering many of the devices now commonly<br />
used worldwide to perform minimally invasive<br />
medical procedures.<br />
COOPER SURGICAL #746<br />
95 Corporate Drive<br />
Trumbull, CT 06611<br />
Tel: 203-601-5200<br />
Fax 203-601-4741<br />
www.coopersurgical.com<br />
CooperSurgical is the leading provider of<br />
medical devices and procedure oriented<br />
solutions that result in improved health care<br />
delivery to women regardless of clinical<br />
setting. The company targets products that aid<br />
clinicians in the management and treatment<br />
of the broad spectrum of women’s health care<br />
issues that occur throughout her life.<br />
COVIDIEN #411<br />
150 Glover Avenue<br />
Norwalk, CT 06850<br />
Tel: 800-722-8772<br />
Fax: 888-636-1002<br />
Website: www.covidien.com<br />
Covidien is a leading global healthcare<br />
company that creates innovative solutions for<br />
better patient outcomes and delivers value<br />
through clinical leadership and excellence.<br />
Covidien manufactures a range of industryleading<br />
products in five segments including<br />
Surgical and Energy-based Devices.<br />
CROSPON INC. #505<br />
3rd Floor, 701 Palomar Airport Road<br />
Carlsbad, CA 92011<br />
Tel: 760-931-4801<br />
Fax: 760-931-4804<br />
Website: www.crospon.com<br />
The Crospon EndoFLIP imaging system is used<br />
intra-operatively and/or during endoscopy<br />
to assess stoma diameter for the purpose of<br />
optimizing the adjustment of all gastric bands.<br />
The company has CE Mark approval in Europe<br />
for the use of EndoFLIP for diameter, pressure<br />
and volume measurements in the upper<br />
gastrointestinal tract.<br />
DalimSurgNET CORP. #202<br />
B-708 Woolim Blue Nine<br />
240-21 Yeomchang-dong, Gangseo-gu<br />
Seoul, 157779 Korea<br />
Tel: +82-2-335-1651<br />
Fax: +82-2-323-1651<br />
Website: www.dalimsurg.net<br />
www.octo-port.com<br />
The DalimSurgNET aims to be the most<br />
innovative medical device company, and our<br />
vision is to be the global medical solution<br />
provider for sincere patient care. The OCTOTM<br />
Port is intended to use multiple instruments<br />
and endoscope through a single incision during<br />
the advanced minimally invasive laparoscopic<br />
surgery.<br />
DAVOL INC.,<br />
A BARD COMPANY #435<br />
100 Crossings Boulevard<br />
Warwick, RI 02886<br />
Tel: 800-556-6275<br />
Fax: 401-825-8759<br />
Website: www.davol.com<br />
Davol, a BARD Company, is the market leader in<br />
hernia repair, offering a broad range of unique<br />
synthetic and biologic implants for laparoscopic<br />
and open approaches. Additionally, the NEW<br />
PermaFix and SorbaFix Fixation Systems<br />
provides strong, consistent, and reliable fixation<br />
with both permanent and fully absorbable<br />
fasteners.<br />
EASY-LAP LTD. #205<br />
POB 128<br />
Kfar Truman, Israel, 73150<br />
Tel: +972-52-6717051<br />
Fax: +972-77-6<strong>2010</strong>03<br />
Website: www.easy-lap.com<br />
Easy-Lap’s vision is to enable widespread use of<br />
laparoscopy through devices that shorten the<br />
learning curve, reduce laparoscopic procedure<br />
time, optimize technique, and minimize<br />
complications. Easy-Lap’s *iMESH Hernia Kit<br />
* offers an intelligent path to laparoscopic<br />
success in hernia repair.<br />
ELSEVIER/SAUNDERS/MOSBy<br />
#602<br />
8701 Ivyberry Way<br />
Gaithersburg, MD 20886<br />
Tel: 240-277-3081<br />
Fax: 301-527-9248<br />
Website: www.elsevierhealth.com<br />
Elsevier is one of the world’s leading publisher<br />
of medical books and periodicals. Please stop by<br />
our booth during The World Congress to see the<br />
latest titles on display.<br />
ENCISION INC. #337<br />
6797 Winchester Circle<br />
Boulder, CO 80301<br />
Tel: 303-444-2600<br />
Fax: 303-444-2693<br />
Website: www.encision.com<br />
Encision’s ACTIVE ELECTRODE MONITORING<br />
system is a laparoscopic safety system that<br />
continuously monitors Encision’s monopolar<br />
laparoscopic instruments during surgery to<br />
eliminate the risk of stray energy burn injury to<br />
patients during laparoscopy.<br />
ENDOCHOICE #334<br />
11800 Wills Road, Suite 100<br />
Alpharetta, GA 30009<br />
Tel: 888-682-3636<br />
Fax: 866-567-8218<br />
Website: www.endochoice.com<br />
Welcome to EndoChoice - delivering a<br />
diverse portfolio of GI supplies, diagnostics,<br />
equipment and devices. Launching at <strong>SAGES</strong><br />
are: the revolutionary BONASTENT® - the most<br />
advanced GI stenting platform; and Exagen® IBD<br />
and IBS genomic tests.<br />
The company strives to exceed expectations<br />
through its exemplary customer care, superior<br />
products and easy online ordering. For more<br />
information, call 888-682-ENDO (3636) or visit<br />
www.EndoChoice.com.<br />
ENDOCONTROL #540<br />
5, Avenue du Grand Sablon<br />
38700 La Tronche<br />
+33 (0) 4 76 63 75 82<br />
+33 (0) 4 76 54 95 61<br />
Website: www.endocontrol-medical.com<br />
EndoControl is an innovative company<br />
specializing in the development of robotic<br />
surgical solutions for endoscopic surgery. It<br />
markets a range of products including ViKY®, a<br />
robotic assistant for laparoscopic, pelviscopic<br />
and thoracoscopic surgery.<br />
ENDOGASTRIC SOLUTIONS<br />
#629<br />
555 Twin Dolphin Drive, Suite 620<br />
Redwood City, CA 94065<br />
Tel: 650-226-2225<br />
Fax: 650-226-2201<br />
Website: www.endogastricsolutions.com<br />
EndoGastric Solutions, (EGS) is the pioneer<br />
in incisionless surgical procedures for the<br />
treatment of upper gastrointestinal diseases.<br />
TIF (Transoral Incisionless Fundoplication) with<br />
EGS’ EsophyX device creates a valve between<br />
the stomach and esophagus, reduces hiatal<br />
hernia, and restores the anatomy to reduce/<br />
prevent gastroesophageal reflux.<br />
12 th World Congress of Endoscopic Surgery 196
Exhibitor Profiles<br />
ETHICON ENDO-SURGERY, INC.<br />
#213<br />
4545 Creek Road<br />
Cincinnati, Ohio 45242<br />
Tel: 800-USE-ENDO<br />
Fax: 800-873-3636<br />
Website: www.ethiconendo.com<br />
Ethicon Endo-Surgery, Inc. develops<br />
and markets advanced medical devices<br />
for minimally invasive and open surgical<br />
procedures. The company focuses on<br />
procedure-enabling devices for the<br />
interventional diagnosis and treatment of<br />
conditions in general and bariatric surgery,<br />
as well as gastrointestinal health, plastic<br />
surgery, orthopedics, gynecology, and surgical<br />
oncology.<br />
ETHOS SURGICAL #546<br />
2065 NW Miller Road, Suite 301<br />
Portland, OR 92779<br />
Tel: 440-289-9788<br />
Website: www.ethos-surgical.com<br />
GENERAL SURGERY NEWS #507<br />
545 West 45th Street<br />
New York, NY 10036<br />
Tel: 212-957-5300<br />
Fax: 212-957-7230<br />
Website: www.generalsurgerynews.com<br />
General Surgery News is a monthly newspaper<br />
designed to keep general surgeons abreast<br />
of the latest developments in the field. The<br />
publication features extensive meeting<br />
coverage, analysis of journal articles,<br />
educational reviews, and information on new<br />
drugs and products.<br />
GORE & ASSOCIATES, INC. #711<br />
Medical Products Division<br />
301 Airport Road / P. O. Box 1408<br />
Elkton, MD 21922<br />
Tel: 410-506-8283<br />
FAX: 410-506-8221<br />
Website: www.davol.com<br />
Gore Medical Products Division has provided<br />
creative therapeutic solutions to complex<br />
medical problems for three decades. The<br />
extensive Gore Medical family of products<br />
includes vascular grafts, endovascular and<br />
interventional devices, surgical materials for<br />
hernia repair, soft tissue reconstruction, staple<br />
line reinforcement, and sutures for use in<br />
vascular, cardiac and general surgery.<br />
H & H SURGICAL<br />
TECHNOLOGIES #504<br />
4437 Robertson Road<br />
Madison, WI 53714<br />
Tel: 608-222-2776<br />
Fax: 608-222-2604<br />
Website: www.hhsurgical.com<br />
H+H Surgical Technologies is a leader in preowned<br />
medical equipment sales. We specialize<br />
in flexible endoscopy, laparoscopy and related<br />
instrumentation. We are dedicated to providing<br />
high quality and customer satisfaction. We feel<br />
that our prices are unbeatable and we stand<br />
behind every piece.<br />
HAPTICA INC #606<br />
101 Federal Street, Suite 1900<br />
Boston, MA, 02110<br />
Tel: +1 617 342 7270<br />
Fax: +1 617 342 7080<br />
Website: www.haptica.com<br />
Haptica’s award-winning ProMIST Surgical<br />
Simulator is the best validated simulator for<br />
training in laparoscopic skills and procedures.<br />
ProMIS’ ‘mixed reality’ approach has been<br />
shown to be better than VR and preferred by<br />
users. Haptica also develops custom simulation<br />
solutions to accelerate uptake of new surgical<br />
devices<br />
HCA - HOSPITAL CORPORATION<br />
OF AMERICA #447<br />
2 Maryland Farms, Suite 200<br />
Brentwood, TN 37027<br />
Tel: 615.372.5196<br />
Fax: 866.789.2288<br />
Website: www.hcahealthcare.com<br />
HCA owns and operates 163 healthcare<br />
facilities in 20 states with opportunities<br />
coast to coast. HCA was one of the nation’s<br />
first hospital companies. We strive to deliver<br />
quality healthcare that meets the needs of the<br />
communities we serve.<br />
HRA RESEARCH #724<br />
400 Lanidex Plaza<br />
Parsippany, N J 07054<br />
Tel: 973-240-1200<br />
Website: www.hraresearch.com<br />
Our team of experienced interviewers will be<br />
distributing carefully developed questionnaires.<br />
We’ll be gathering the answers to vital<br />
marketing and clinical questions- answers that<br />
can affect the introduction of new products<br />
or the continuation of existing healthcare<br />
products and services.<br />
INTEGRA SURGICAL #406<br />
311 Enterprise Drive, Plainsboro, NJ 08536<br />
Tel: 609-275-0500<br />
Fax: 609-799-3297<br />
Website: www.integra-ls.com<br />
Integra Surgical is a leader in quality surgical<br />
instrumentation for laparoscopic, general,<br />
cardiovascular, neurosurgery, orthopedic,<br />
plastic and reconstructive surgery. Products<br />
include surgical instrumentation from Jarit® ,<br />
Ruggles-Redmond and Padgett Instruments®,<br />
CIMS® Consulting Services, Luxtec® Xenon<br />
illumination and digital video recording<br />
systems, fiber optic cables, surgical loupes, and<br />
Omni-Tract® table-mounted retractor systems.<br />
INTERNATIONAL CONGRESS OF<br />
ENDOSCOPY (ICE 2011) #839<br />
C/O Hanser Service GmbH<br />
PaulsBorner Str. 44<br />
Berlin 14133 – Germany<br />
Tel: +4913033006690<br />
Fax: +4913013057391<br />
Website: www.ICE2011.org<br />
IFSES - INTERNATIONAL #740<br />
FEDERATION OF SOCIETIES OF<br />
ENDOSCOPIC SURGEONS<br />
Providencia # 1043, Col.<br />
Del Valle, Mexico City 03100<br />
Tel: + 52 + 55 + 5559-5332<br />
Fax: + 52 + 55 + 5559-6468<br />
Website: www.ifses.org<br />
IFSES, the International Federation of Societies<br />
of Endoscopic Surgeons will host in 2012 the<br />
13th World Congress of Endoscopic Surgery<br />
in Mexico. We will be pleased to welcome you<br />
in this wonderful country, cradle of ancient<br />
civilizations, full of beautiful places, cultural<br />
heritage, typical gastronomy and charming<br />
people.<br />
INTUITIVE SURGICAL, INC. #123<br />
1266 Kifer Road<br />
Sunnyvale, CA 94086<br />
Tel: 408-523-2100<br />
Fax: 408-523-1390<br />
Website: www.intuitivesurgical.com<br />
Intuitive Surgical, Inc., is the global technology<br />
leader in robotic-assisted, minimally invasive<br />
surgery. The Company’s da Vinci® Surgical<br />
System enables general surgeons to offer a new,<br />
minimally invasive approach to patients.<br />
12 th World Congress of Endoscopic Surgery<br />
197 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Exhibitor Profiles<br />
KARL STORZ ENDOSCOPY-<br />
AMERICA #323<br />
2151 E Grand Ave<br />
El Segundo, CA 90245<br />
Phone: 424- 218-8100<br />
Website: www.ksea.com<br />
KARL STORZ provides minimally invasive<br />
solutions for virtually every surgical specialty. .<br />
Among these innovative products is our Image<br />
1® FULL HD platform, which acquires and<br />
displays wide 16:9 1080p60 images, providing<br />
the optimal viewing experience necessary for<br />
minimally invasive surgery.<br />
KIMBERLY-CLARK HEALTHCARE<br />
#541<br />
1400 Holcomb Bridge Road<br />
Rosswell, GA 30076<br />
Tel: 770-587-8000<br />
Website: www.kchealthcare.com<br />
LEXION MEDICAL, INC. #635<br />
5000 Township Parkway<br />
St. Paul, MN 55110-5865<br />
Tel: 877-9LEXION<br />
Fax: 651-635-0090<br />
Website: www.lexionmedical.com<br />
LEXION Medical, a leader of innovative medical<br />
technologies improving patient safety, offers<br />
the Insuflow® Laparoscopic Gas Conditioning<br />
Systems for minimally invasive surgery,<br />
including thoracoscopic, laparoscopic and<br />
endoscopic vein harvesting surgical procedures<br />
and PneuVIEW® XE Laparoscopic Smoke<br />
Elimination System.<br />
LIFECELL #302<br />
1 Millennium Way<br />
Branchburg, NJ 08876<br />
Telephone; 908-947-1100<br />
Fax: 908-947-1200<br />
Website: www.lifecell.com<br />
LifeCell engineers both AlloDerm®<br />
Regenerative Tissue Matrix and Strattice<br />
Reconstructive Tissue Matrix used in hernia<br />
repair, breast reconstruction and breast plastic<br />
surgery revisions. They support regeneration<br />
through rapid revascularization, cell<br />
repopulation and white cell migration.<br />
LIMBS & THINGS, INC. #542<br />
PO Box 15669<br />
Savannah, GA 31416<br />
Tel: 912-629-0357<br />
Fax: 912- 629-0358<br />
Website: www.GOLIMBS.com<br />
Limbs & Things works hard to be your sole<br />
source for medical training models and medical<br />
simulators, providing medical education task<br />
training models for critical care, diagnostic skills,<br />
venipuncture, surgical simulation, Ob/Gyn,<br />
suturing, minor surgery, soft tissue injection,<br />
vascular surgery and many other medical<br />
simulation subjects.<br />
LIPPINCOTT WILLIAMS &<br />
WILKINS #837<br />
202 9th Street SE<br />
Washington, DC 20003<br />
Tel./Fax: 202-543-8710<br />
Website: www.lww.com<br />
Lippincott Williams & Wilkins publishes medical<br />
books, journals and software.<br />
MARKET ACCESS PARTNERS<br />
#641<br />
3236 Meadowview Road<br />
Evergreen, CO 80439<br />
Tel: 303-526-1900<br />
Fax: 303-526-7920<br />
Website: www.marketaccesspartners.com<br />
Market Access Partners provides market<br />
research consulting to the medical device and<br />
pharmaceutical industries. We use innovative<br />
qualitative and quantitative methodologies<br />
to research opinions of physicians, nurses and<br />
patients. We offer a management-oriented<br />
approach to product development and<br />
marketing.<br />
MARY ANN LIEBERT, INC.,<br />
PUBLISHERS #434<br />
140 Huguenot Street<br />
New Rochelle, NY 10801<br />
Tel: 914-740-2100<br />
Fax: 914-740-2101<br />
Website: www.liebertpub.com<br />
Mary Ann Liebert, Inc., publishes authoritative,<br />
peer-reviewed journals in new and promising<br />
areas of science and biomedical research<br />
including Bariatric Nursing and Surgical Patient<br />
Care. With bariatric surgical procedures<br />
increasing, this is the must-have journal for<br />
optimal patient care.<br />
MASIMO CORPORATION #333<br />
40 Parker<br />
Irvine, CA<br />
Tel: (949) 297-7534<br />
Website: www.masimo.com<br />
MEDERI THERAPEUTICS INC.<br />
#331<br />
8 Sound Shore Drive, Suite 304<br />
Tel: 203-930-9900<br />
Fax: 203-869-1013<br />
Website: www.mederitherapeutics.com<br />
Mederi Therapeutics manufactures and<br />
markets innovative medical devices that<br />
deliver radiofrequency energy to treat diseases<br />
affecting the human digestive system. The first<br />
two products — Secca, for bowel incontinence<br />
and Stretta, for GERD — have demonstrated<br />
clinical effectiveness in numerous studies. All<br />
Mederi therapies are outpatient, minimally<br />
invasive and promote rapid recovery for<br />
patients.<br />
MEDIFLEX SURGICAL<br />
PRODUCTS #603<br />
250 Gibbs Road<br />
Islandia, NY 11749<br />
Tel: 800-879-7575<br />
Fax: 631-582-8487<br />
Website: www.mediflex.com<br />
Visit Mediflex (Booth 603) to see the newest<br />
Holders/Positioners for Laparoscopy, the<br />
largest selection of Nathanson Hooks and our<br />
complete line of Laparoscopic Instruments and<br />
Disposables. And, if you do Bariatrics, come see<br />
how the AWEL device can help you.<br />
MEDTRONIC, INC. #403<br />
8200 Coral Sea Street NE<br />
Mounds View, MN 55112<br />
Tel: 763-528-9970<br />
Fax: 651-367-2476<br />
Website: www.medtronic.com<br />
At Medtronic, we’re committed to Innovating<br />
for Life by pushing the boundaries of medical<br />
technology and actually changing the way<br />
the world treats chronic disease. Medtronic’s<br />
U-CLIP® Device simplifies suturing by<br />
eliminating knot-tying and suture management<br />
in open, robotic and endoscopic procedures.<br />
MICROLINE SURGICAL #341<br />
800 Cummings Center, #166T<br />
800 Cummings Center #157X<br />
Beverly, MA 01915<br />
Tel: 978-922-9810<br />
Fax: 978-922-9209<br />
Website: www.microlinesurgical.com<br />
Microline Surgical develops and manufactures<br />
precision laparoscopic reposable instruments<br />
unsurpassed in precision, performance and<br />
reliability. Starion Instruments employs the<br />
direct transfer of thermal energy and pressure<br />
to simultaneously seal and divide tissue. Starion<br />
is a wholly owned subsidiary of Microline<br />
MINNESOTA MEDICAL<br />
DEVELOPMENT, INC. #449<br />
14305 21ST Avenue North, Suite 100<br />
Plymouth, MN 55447<br />
Tel: 763-354-7100<br />
Fax: 765-354-7101<br />
Website: www.2mdinc.com<br />
Minnesota Medical Development will feature<br />
the innovative Rebound HRD and Rebound<br />
HRD-V, a family of self-expanding Nitinol<br />
framed hernia repair devices designed for<br />
laparoscopic and open repair of inguinal and<br />
ventral hernias. The Rebound HRD ushers in a<br />
new era for surgical hernia repair.<br />
12 th World Congress of Endoscopic Surgery 198
Exhibitor Profiles<br />
NASHVILLE SURGICAL<br />
INSTRUMENTS #506<br />
2005 Kumar Lane<br />
Springfield, TN 37172<br />
Tel: 615-382-4996<br />
Fax: 615-382-4199<br />
Website: www.NashvilleSurg.com<br />
Kumar PRE-VIEW* Cholangiography Clamp and<br />
Kumar PRE-VIEW* Cholangiography Catheters<br />
allow Cystic Duct Marking to Prevent Common<br />
Bile Duct Injury. There is No Cystic Duct<br />
Cannulation! Kumar T-ANCHORS* Hernia Set<br />
allows easy laparoscopic Hernia Mesh Fixation<br />
by eliminating the need to grasp and feed<br />
sutures with Suture Passer. May be used with<br />
any brand of mesh.<br />
* Trademark and Patent<br />
NEATSTITCH #734<br />
800 East Leigh Street<br />
Richmond, VA 23219<br />
Tel: (804) 828-6884<br />
Website: www.neatstitch.com<br />
NeatStitch has developed the NeatClose<br />
system, which is the first fully automated<br />
port closure device for laparoscopic surgery.<br />
This system combines safety, ease of use and<br />
significantly reduced port closure time.<br />
NEW DIRECTION SYSTEM #819<br />
821 East Gate Drive<br />
Mount Laurel, NJ 08054<br />
Telephone: 866-494-1216<br />
Fax: 856-778-4439<br />
Website: www.newdirectionsystem.com<br />
Robard Corporation provides best-in-class<br />
nutritional solutions for successful weight<br />
management to surgeons and physicians<br />
nationwide. Partner your surgical technique<br />
with our turnkey medically-supervised system<br />
(New Direction) to provide patients with<br />
preoperative preparation, decreased surgical<br />
complications, and enhanced post-op weight<br />
loss.<br />
NEW WAVE SURGICAL Corp<br />
#342<br />
3700 NW 124th Avenue, Ste. 135<br />
Coral Springs, Florida 33065<br />
Tel: 866-346-8883<br />
Fax: 866-586-6793<br />
Website: www.newwavesurgical.com<br />
New Wave Surgical offers cutting-edge devices<br />
that increase the safety and efficiency of<br />
laparoscopic surgery.<br />
NOVARE SURGICAL SYSTEMS,<br />
INC. #535<br />
10440 Bubb Road, Suite A<br />
Cupertino, CA 95014<br />
Phone: 877-668-2730<br />
Fax: 408-873-3168<br />
Website: www.novaresurgical.com<br />
RealHand® High Dexterity (HD) Instruments<br />
continue to advance minimally invasive<br />
surgery including applications in Single Port<br />
Surgery and NOTES. RealHand delivers greater<br />
dexterity and surgical control with 7 degrees of<br />
freedom of movement and tactile feedback in<br />
convenient hand-held instruments.<br />
NOVUS INSURANCE COMpany<br />
#335<br />
Risk Retention Group<br />
3000 Bayport Drive, Suite 300<br />
Tampa, FL 33607<br />
Tel. 888-490-5185<br />
Fax 866-955-9831<br />
Website: www.NovusMD.com<br />
Novus Insurance Company is the medical<br />
malpractice solution for bariatric and general<br />
surgeons! Novus was created by surgeons<br />
for surgeons. Our goal is to provide stable<br />
insurance premiums while reducing your<br />
liability risk. Visit Booth #335 or our website:<br />
www.NovusMD.com.<br />
NOVUS SCIENTIFIC, INC. #649<br />
1030 Turnpike Street<br />
Canton, MA 02021<br />
Tel: 877- 211-4339<br />
Fax: 781- 713-4717<br />
Website: www.novusscientific.com<br />
OASYS HEALTHCARE<br />
CORPORATION #741<br />
191 Main Street North<br />
Uxbridge, Ontario L9P 1C3 - Canada<br />
Tel: 905-852-3399<br />
Fax: 905-852-3323<br />
Website: www.oasyshealthcare.com<br />
OASYS Healthcare integrates audio, video and<br />
control systems for the medical marketplace.<br />
Our solutions include OR Control, Telemedicine,<br />
digital signage and video monitoring<br />
systems. All OASYS systems are designed using<br />
the latest open platform, non-proprietary<br />
technology.<br />
OLYMPUS #425<br />
3500 Corporate Parkway<br />
Center Valley, PA 18034<br />
Tel: 484-896-5000<br />
Fax: 484-896-5133<br />
Website: www.olympusamerica.com<br />
Olympus, which incorporates surgical market<br />
leader Gyrus ACMI, develops solutions for<br />
healthcare professionals that help improve<br />
outcomes and enhance quality of life for their<br />
patients. By enabling less invasive procedures,<br />
innovative diagnostic and therapeutic<br />
endoscopy and early stage cancer evaluation<br />
and treatments, Olympus is transforming the<br />
future of healthcare.<br />
OVESCO ENDOSCOPY AG #235<br />
Dorfackerstr. 26<br />
72074 Tuebingen - Germany<br />
Mailing address: service@ovesco.com<br />
Tel: +49 (0)7071 98979-160<br />
Fax: +49 (0)7071 98979-260<br />
Website: www.ovesco.com<br />
Ovesco Endoscopy AG develops, manufactures<br />
and markets innovative products for the<br />
treatment of gastrointestinal disease: The<br />
OTSC® Over-The-Scope-Clip for gastrointestinal<br />
hemostasis and endoscopic digestive organ<br />
wall closure and application aids such as the<br />
OTSC® Anchor and the OTSC® Twin Grasper®.<br />
PARÉ SURGICAL INC. #706<br />
7332 S. Alton Way, Suite H<br />
Centennial, CO 80112<br />
Tel: 303-689-0187<br />
Fax: 303-689-0579<br />
Website: www.PareSurgical.com<br />
Innovative suturing technology for<br />
advanced Laparoscopic, Single Port and Flexible<br />
Endoscopic procedures. Disposable or reusable<br />
system delivers a pre-tied locking Roeder knot<br />
for secure tissue approximation, ligation or<br />
fixation. Quik-Stitch is ideal for gastric band<br />
placement and gastric bypass, especially for<br />
over-sewing staple lines. Quik-Stitch does not<br />
require triangulation. Perfect for all Single Port<br />
Procedures.<br />
During Flexible Endoscopic Procedures,<br />
gi-Stitch readily achieves serosa to serosa tissue<br />
penetration to tighten the dilated stoma of a<br />
gastric bypass. Delivered through the 2.8mm<br />
operating channel, the 2.6mm gi-Loop provides<br />
the capability to ligate vessels or ducts utilizing<br />
suture with the pre-tied locking Roeder knot.<br />
12 th World Congress of Endoscopic Surgery<br />
199 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Exhibitor Profiles<br />
PATTON SURGICAL #340<br />
6300 Bridgepoint Parkway<br />
Building Two, Suite 420<br />
Austin, TX 78730<br />
Tel: 512-329-0469<br />
Fax: 512-328-9113<br />
Website: www.pattonsurgical.com<br />
Patton Surgical improves patient care through<br />
advancements in surgical instrumentation. The<br />
PassPort® Double-Shielded Trocar, endorsed by<br />
renowned laparoscopic surgeons worldwide,<br />
provides superior protection and control and<br />
drastically reduces the risk of catastrophic vessel<br />
and organ injury associated with laparoscopic<br />
procedures.<br />
PERKINS HEALTHCARE<br />
TECHNOLOGIES #835<br />
700 International Parkway Suite 100<br />
Richardson, TX 75081<br />
Tel: 214.828.4545<br />
Fax: 214.827.6319<br />
Website: www.Perkins-HT.com<br />
Perkins Healthcare Technologies has earned the<br />
reputation of developing and manufacturing<br />
high quality medical products and solutions<br />
to meet the growing demand for video<br />
distribution and advanced visualization<br />
products in the clinical environment.<br />
RICHARD WOLF MEDICAL<br />
INSTRUMENTS #727 & #825<br />
353 Corporate Woods Parkway<br />
Vernon Hills, IL 60061<br />
Phone: 847.913.1113<br />
Fax: 847.913.6959<br />
Website: www.richardwolfusa.com<br />
Richard Wolf Medical Instruments (RWMIC)<br />
manufactures and distributes laparoscopic<br />
and thoracoscopic instruments. RWMIC<br />
also manufactures scopes, insufflators and<br />
a complete line of instruments and optics<br />
designed specifically for bariatric and colorectal<br />
surgery. RWMIC offers the only stereoscope on<br />
the market, designed specifically for Transanal<br />
Endoscopic Microsurgery.<br />
SAINT VINCENT HEALTH<br />
SYSTEM #728<br />
232 West 25th Street<br />
Erie, PA 16544<br />
Tel: (814) 452-7822<br />
Website: www.svhs.org<br />
SIERRA SCIENTIFIC<br />
INSTRUMENTS # 811<br />
5757 W. Century Blvd., Ste 660<br />
Los Angeles, CA 90045<br />
Tel: 310-641-8492<br />
Fax: 310-872-5558<br />
Website: www.sierrainst.com<br />
SSI produces high-resolution solid-state<br />
manometry systems for gastrointestinal motility<br />
studies. Our ManoScan 360T High-Resolution<br />
Manometry System has advanced diagnostic<br />
technology that makes manometry simple,<br />
accurate and complete. An average esophageal<br />
study can be done in 10 minutes or less.<br />
SIMBIONIX USA CORPORATion<br />
#430<br />
7100 Euclid Avenue, Suite 180<br />
Cleveland, OH 44103<br />
Tel: +216 229 2040<br />
Fax: +216 229 2070<br />
Website: www.simbionix.com<br />
Simbionix is a global leader in medical<br />
simulation and education technologies.<br />
Simbionix LAP Mentor and GI Mentor<br />
provide advanced simulation experience of<br />
complete MIS procedures. Simbionix was<br />
selected by <strong>SAGES</strong> to develop web-based<br />
didactic material and hands-on exam for the<br />
FES <strong>Program</strong>.<br />
SONY ELECTRONICS, INC. #131<br />
1 Sony Drive<br />
Park Ridge, NJ 07656<br />
Tel: 201-930-1000<br />
Website: www.sony.com/medical<br />
Sony Electronics is a leading provider of<br />
innovative medical imaging products. Our<br />
offerings include High Definition cameras,<br />
displays, capture systems and printers. Sony’s<br />
medical group is recognized for its commitment<br />
to fine-tuning its products to meet the<br />
demands for healthcare professionals.<br />
SPECIALTY SURGICAL<br />
INSTRUMENTATION #813<br />
200 River Hills Drive<br />
Nashville, TN 37210<br />
Tel: 615-883-9090<br />
Fax: 615-883-9107<br />
Website: www.specsurg.com<br />
SSI Ultra surgical instruments are handcrafted<br />
by the finest surgical instrument makers in<br />
Germany, individually inspected to maintain<br />
the highest standards of quality. SSI Ultra<br />
serves the surgical specialties of Neuro/Spine<br />
Orthopedics, Eye, ENT, Plastics Cardio/Peripheral<br />
Vascular, General GYN, Laparoscopic surgeries.<br />
SPRINGER #503<br />
233 Spring Street<br />
New York, NY 10013<br />
Tel: 212-460-1600<br />
Fax: 212-460-1575<br />
Website: www.springer.com<br />
Springer offers an increasing number of cuttingedge<br />
Surgery titles written by highly qualified<br />
experts. Visit our booth and browse books<br />
and journals on the newest developments<br />
in Surgery, including Surgical Endoscopy, the<br />
Official Journal of <strong>SAGES</strong> and EAES.<br />
STRYKER ENDOSCOPY #700<br />
5900 Optical Court<br />
San Jose, CA 95138<br />
Tel: 800-624-4422<br />
Fax: 800-729-2917<br />
Website: www.stryker.com<br />
Stryker Corporation is one of the world’s<br />
leading medical technology companies with<br />
the most broadly based range of products in<br />
orthopaedics and a significant presence in<br />
other medical specialties.<br />
SUPER BRUSH, LLC #843<br />
800 Worcester Street<br />
Springfield, MA 01151<br />
Tel: 413-543-1442<br />
Fax: 413- 543-1523<br />
Website: www.superbrush.com<br />
SURGICAL PRODUCTS<br />
MAGAZINE #726<br />
199 East Badger Road, Suite 201<br />
Madison, WI 53713<br />
Tel: 973-920-7789<br />
Fax: 608-274-6454<br />
Website: www.surgicalproductsmag.com<br />
Surgical Products, a monthly product news<br />
magazine, is the leading source for cuttingedge<br />
surgical product information to 60,000<br />
surgeons and other medical and purchasing<br />
professionals in hospitals and surgi-centers<br />
across the country. Surgical Products is<br />
available in both hard and digital editions. The<br />
publication is complemented by a stable of<br />
online offerings including a weekly Surgical<br />
Focus On enewsletter, e-product showcase<br />
and custom-designed, audience-directed<br />
E-Marketing blasts.<br />
SURGICAL SCIENCE, INC. #306<br />
7760 France Ave South, Suite 1100<br />
Minneapolis, MN 55435<br />
Tel: 612-810-1474<br />
Fax: 888-737-1648<br />
Website: www.surgical-science.com<br />
Surgical Science has been a market leader<br />
in Virtual Reality Laparoscopic Simulation<br />
since 2001. With a strong focus on usability,<br />
applicability in clinical education, and<br />
advanced technology, the LapSim® System<br />
continues to be in high demand among surgical<br />
professionals worldwide.<br />
12 th World Congress of Endoscopic Surgery 200
Exhibitor Profiles<br />
SURGIQUEST #847<br />
12 Cascade Blvd. – Suite 2B<br />
Orange, CT 06477<br />
Tel: 203-799-2400<br />
Website: www.surgiquest.com<br />
SurgiQuest, founded May 2006, creates<br />
innovative technology for minimally invasive<br />
surgery. SurgiQuest’s AirSeal access<br />
system presents significant technological<br />
breakthroughs in minimally invasive surgery.<br />
The AirSeal system provides unobstructed<br />
access to abdominal cavity and reduces<br />
variations of intra-abdominal pressure.<br />
SurgiQuest’s unique approach to MIS enables<br />
improved single incision surgery and many new<br />
instrument platforms.<br />
SYNAPSE BIOMEDICAL, INC.<br />
#336<br />
300 Artino Street<br />
Oberlin, OH 44074<br />
Tel: 440-774-2488<br />
Fax: 440-774-2572<br />
Website: www.synapsebiomedical.com<br />
Synapse Biomedical Inc., a neurostimulation<br />
company, markets the NeuRx Diaphragm<br />
Pacing System (DPS). The system is designed<br />
for laparoscopic implantation to address<br />
respiratory insufficiency or chronic ventilator<br />
dependency in high spinal cord injury and ALS<br />
(Lou Gehrig’s disease) patients.<br />
SYNOVIS SURGICAL<br />
INNOVATIONS #625<br />
2575 University Avenue W<br />
St Paul, MN 55114<br />
Tel: 1-800-255-4018<br />
Fax: 1-651-642-9018<br />
Website: www.synovissurgical.com<br />
Synovis Surgical Innovations, a division of<br />
Synovis Life Technologies, Inc., will feature<br />
Veritas® Collagen Matrix, a biomaterial for soft<br />
tissue repair that is rapidly revascularized and<br />
repopulated by surrounding host tissue. Synovis<br />
will also display Peri-Strips Dry® with Veritas®<br />
Collagen Matrix, its biologic circular and linear<br />
staple line reinforcement, for gastric, small<br />
bowel and mesentery applications.<br />
TEI BIOSCIENCES INC. #647<br />
7 Elkins St., Boston, MA 02127 USA<br />
Tel: Toll Free 800-524-0022; or 617-268-1616<br />
Fax: 617-268-3282<br />
Website: www.teibio.com<br />
TEI Biosciences is a leading, privatelyheld<br />
biomedical company with expertise<br />
in regenerative medicine that develops<br />
biologic products for soft tissue repair and<br />
reinforcement applications - from plastic<br />
and reconstructive surgery, abdominal wall<br />
reconstruction and hernia repair, and wound<br />
management.<br />
TUEBINGEN SCIENTIFIC<br />
MEDICAL GMBH #237<br />
Dorfackerstr. 26<br />
72074 Tuebingen - Germany<br />
Tel: +49 (0)7071 98979-140<br />
Fax: +49 (0)7071 97979-240<br />
Website: www.tuebingen-scientific.com<br />
Tuebingen Scientific Medical GmbH develops,<br />
produces and markets instruments<br />
and accessories for minimally invasive<br />
surgery. Our mission is to create products that<br />
significantly improve endoscopic surgery and<br />
match up with today’s economic reality in the<br />
hospital industry.<br />
ULTIMATE ESCAPES LUXURY<br />
DESTINATION CLUBS #742<br />
3501 W. Vine Street, Ste. 225<br />
Kissimmee, FL 34741<br />
Telephone: 1-877-955-1900<br />
Fax: 407-483-1936<br />
Website – www.UltimateEscapes.com<br />
Ultimate Escapes is a private club that gives you<br />
and your family a lifetime of “once-in-a-lifetime”<br />
vacation experiences. Similar to a traditional<br />
country club, Ultimate Escapes members pay<br />
a onetime membership fee and annual dues<br />
for access to over 130 private multi-milliondollar<br />
vacation residences and more than 140<br />
luxury resort hotels in over 150 destinations<br />
worldwide! Our Escape Planners assist you<br />
with complete pre-trip planning and at your<br />
destination, a Local Private Host offers 5-star<br />
concierge service and helps you feel completely<br />
at home. Memberships start at $70,000.<br />
UNIVERSITY OF MISSOURI<br />
HEALTH CARE #831<br />
One Hospital Drive; MC414 McHaney Hall<br />
Columbia, MO 65212<br />
Tel: 573-882-5609<br />
Fax: 573-884-4611<br />
The Department of Surgery at the University<br />
of Missouri is currently recruiting for excellent<br />
surgeons with fellowship or advanced training<br />
in minimally invasive surgery, laparoscopic<br />
techniques, and robotic procedures.<br />
THE UNIVERSITY OF<br />
TENNESSEE #548<br />
PHYSICIAN EXECUTIVE MBA PROGRAM<br />
916 Volunteer Boulevard<br />
608 Stokely Management Center<br />
Knoxville, TN 37996-0562<br />
Tel: (865) 974-1772<br />
Fax: (864) 974-0929<br />
Website: www.pemba.utk.edu<br />
The Physician Executive MBA at The University<br />
of Tennessee is the #1 preferred program<br />
exclusively for physicians. It is an internationally<br />
accredited one-year-long MBA, delivered via<br />
distance education and campus residency<br />
periods, offered exclusively for physicians<br />
seeking leadership skills<br />
VIRTUAL PORTS, LTD. #203<br />
800 E. Leigh Stree<br />
Richmond, VA 23219<br />
Tel: 804-827-8231<br />
Fax: 804-828-8566<br />
Website: www.virtual-ports.com<br />
Virtual Ports’ products are designed to reduce<br />
the number of “ports” needed for a surgery and<br />
medical staff required for a procedure. These<br />
products reduce the risk of complications,<br />
recovery time, scarring andoverall cost while<br />
allowing the surgeon more control.<br />
12 th World Congress of Endoscopic Surgery<br />
201 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Index of Faculty and Presenters<br />
Jamie D. Adair ..................................... 58<br />
Gina L. Adrales ................................... 33<br />
Brij B Agarwal ..................................... 69<br />
Krishna A.Agarwal ............................ 50<br />
Frances Allocco .............................56,67<br />
S. Al-Sabah ........................................... 68<br />
Luigi Angrisani ................................... 20<br />
Mehran Anvari .......................41, 66, 70<br />
Maurice E. Arregui ............................ 67<br />
Horacio J. Asbun ......................... 19, 52<br />
Theodor Asgeirsson ......................... 69<br />
Vikram Attaluri ................................... 50<br />
Joyce T. Au ........................................... 58<br />
Michael M. Awad ............................... 59<br />
Shahin Ayazi ........................................ 68<br />
Asghar Azadani .................................. 57<br />
Heidi Bahna ......................................... 46<br />
Fady Kamal Balaa .............................. 51<br />
Virinder K. Bansal .............................. 55<br />
Linda Barry .......................................... 68<br />
Katherine A. Barsness ...................... 28<br />
Nicola Basso ........................................ 67<br />
Bruce Behn .......................................... 40<br />
Estuardo J. Behrens .......................... 68<br />
Richard Bell ......................................... 48<br />
Simon Bergman .......................... 51, 55<br />
Ramon Berguer .................................. 52<br />
Marc Bessler ...........................20, 40, 55<br />
Jai Bikhchandani ............................... 68<br />
Daniel W. Birch ............................ 27, 65<br />
Desmond H. Birkett .......................... 53<br />
S. Biron .................................................. 20<br />
Raghid S. Bitar .................................... 54<br />
Jeffrey A. Blatnik ................................ 56<br />
Victor Bochkarev ............................... 54<br />
Alexandre Bouchard ........................ 35<br />
Steven P. Bowers ...................33, 52, 62<br />
E. Boyle .................................................. 54<br />
Fredrick J. Brody ......................... 35, 40<br />
Shaun R. Brown ........................... 46, 67<br />
L. Michael Brunt .......................... 35, 65<br />
Matias Bruzoni ................................... 28<br />
Luis E. Burbano .................................. 33<br />
Jo Buyske ...................................... 63, 65<br />
Angel M. Caban ................................. 69<br />
Ronan A. Cahill ................................... 55<br />
Guilherme M. Campos .................... 69<br />
Alfredo M. Carbonell ................. 33, 67<br />
Antonio O. Castellvi .......................... 56<br />
Bipan Chand ................................ 40, 52<br />
Ryan A. Chandhoke .......................... 68<br />
George Chang .................................... 18<br />
Eric Changchien ................................ 66<br />
Hester Cheung ................................... 68<br />
Gyu-Seog Choi ............................ 46, 66<br />
Elie K. Chouillard ........................ 55, 68<br />
Elie Chouilliard ............................ 55, 68<br />
Alberto Chousleb ....................... 63, 70<br />
Elias Chousleb .................................... 27<br />
Pradeep K. Chowbey ...........27, 33, 70<br />
W. Y. Chung .......................................... 19<br />
Tatyan Clarke ...................................... 67<br />
Ronald Hanson Clements ....... 51, 66<br />
Ricardo V. Cohen ............................... 20<br />
Tran Cong Duy Long ........................ 55<br />
Nathan E. Conway ............................. 46<br />
Manolo Cortez .................................... 20<br />
Federico Costantino ......................... 57<br />
Ismael Court ........................................ 57<br />
Daniel R. Cox ....................................... 56<br />
Peter Crookes ..................................... 53<br />
Angel Cuadrado ................................ 57<br />
David Cummings .............................. 41<br />
Paul G. Curcillo II ............33, 39, 51, 55<br />
Alfred Cuschieri ....................41, 53, 70<br />
Allan Dackiw ....................................... 19<br />
Gregory F. Dakin ......................... 54, 74<br />
Bernard Dallemagne ........................ 41<br />
Abhay N. Dalvi .................................... 50<br />
Donald Davis ...................................... 54<br />
Aureo L. De Paula .............................. 27<br />
Edmundo Dedios Orozco ............... 52<br />
Conor P. Delaney ........................ 18, 36<br />
Nicolas Demartines .......................... 19<br />
Ithaar H. Derweesh ........................... 50<br />
Ashwin L. deSouza ............................ 47<br />
Daniel J. Deziel ................................... 53<br />
Ushast Dhir .......................................... 68<br />
Andre Dhoore ..................................... 36<br />
Nicola Di Lorenzo .............................. 58<br />
Robert DiRaddo ................................. 63<br />
John Dixon .......................................... 20<br />
Quan-Yang Duh ................................. 19<br />
Brian J. Dunkin ......................40, 66, 74<br />
Sanjeev Dutta ..................................... 28<br />
David Bryan Earle .............................. 65<br />
Kristen R. Earle .................................... 66<br />
Paula K. Edelson ................................. 66<br />
Steven Edmundowicz ...................... 40<br />
Claire Edwards .................................... 50<br />
Michael B. Edye .................................. 33<br />
Jonathan E. Efron .............................. 18<br />
Ahmed R. El-Geidie ........................... 55<br />
Steve Eubanks ............................. 54, 70<br />
Liane S. Feldman ........................ 35, 65<br />
Edward L. Felix ................................... 27<br />
John J. Feng ........................................ 32<br />
Alberto R. Ferreres ............................ 57<br />
David Field ........................................... 40<br />
Abe L. Fingerhut ......................... 33, 53<br />
Aaron S. Fink ....................................... 67<br />
Heidi L. Fitzgerald ............................. 54<br />
Jean Bernard Flament ..................... 62<br />
James W. Fleshman .......................... 68<br />
Roberto Fogel ..................................... 20<br />
Kenneth A. Forde .............................. 53<br />
Dennis L. Fowler ......................... 36, 58<br />
Morris E. Franklin, Jr. ...........46, 65, 68<br />
Gerald M. Fried ...............34, 54, 66, 75<br />
Karl H Fuchs ................................. 41, 58<br />
Daniel J. Gagne .................................. 35<br />
Michel Gagner .................................... 20<br />
Roberto Gallardo ............................... 69<br />
Alex Gandsas ...................................... 58<br />
Pierre Garneau ................................... 58<br />
Brice Gayet .............................19, 33, 55<br />
Denise W. Gee ..................................... 57<br />
Daniel P. Geisler ....................18, 36, 68<br />
Keith E. Georgeson ........................... 36<br />
Iman Ghaderi ...................................... 56<br />
Saber Ghiassi ...................................... 63<br />
Paolo Giamundo ............................... 58<br />
Joshua Glenn ...................................... 76<br />
Alec Glover .......................................... 40<br />
Matthew Randall Goede .......... 32, 75<br />
Trudie A. Goers ................................... 69<br />
Ke Gong ................................................ 56<br />
Segundo J. Gonzalez ........................ 58<br />
Christopher J. Gostout ............. 40, 63<br />
Jon Gould ............................................. 67<br />
Teodor P. Grantcharov .............. 56, 65<br />
Casey J. Graybeal ............................... 39<br />
John C. Graybill .................................. 50<br />
Frederick L. Greene .................... 50, 54<br />
Andrew A. Gumbs ................19, 39, 55<br />
Prateek K. Gupta ................................ 67<br />
Peter T. Hallowell ............................... 51<br />
M. Hamada .......................................... 69<br />
Erik N. Hansen .................................... 28<br />
Paul Hansen ........................................ 24<br />
Carroll M. Harmon ............................. 28<br />
Kristi Lee Harold ................................ 33<br />
Vincent L. Harrison ........................... 55<br />
Karem C. Harth ............................ 56, 67<br />
Eugenius J. Harvey ............................ 69<br />
Jeffrey W. Hazey ................................. 40<br />
David Hazzan ...................................... 56<br />
Katherine B. Heiden ......................... 58<br />
B. Todd Heniford ................................ 33<br />
Miguel Herrera ................................... 19<br />
Kelvin D. Higa ..................................... 27<br />
Jacques M. Himpens ........................ 20<br />
Vanessa P. Ho ...................................... 56<br />
Michael D. Holzman ......................... 54<br />
Elizabeth Honigsberg ...................... 56<br />
William W. Hope ................................ 50<br />
Santiago Horgan ............................... 40<br />
Franziska Huettner ........................... 46<br />
Eric Steven Hungness ............... 39, 51<br />
John Hunter ................................. 41, 67<br />
Matthew M. Hutter ........................... 20<br />
Sayeed Ikramuddin .......................... 19<br />
William Barry Inabnet III .......... 19, 54<br />
Haruhiro Inoue ............................ 19, 41<br />
Takeaki Ishizawa ................................ 35<br />
Eran Itzkowitz ..................................... 68<br />
Gretchen Purcell Jackson ............... 76<br />
Timothy D. Jackson ......................... 54<br />
Brian P. Jacob ............................... 68, 74<br />
Samuel Jacob ..................................... 55<br />
Garth R. Jacobsen ............................. 40<br />
David James ................................. 58, 66<br />
Christopher Jamieson .............. 47, 54<br />
Balaji Jangam ..................................... 67<br />
Shiva Jayaraman ......................... 50, 57<br />
Eric D. Jenkins ..................................... 55<br />
Blair A. Jobe ......................................... 41<br />
Daniel Bougere Jones ...................... 65<br />
Rohan A. Joseph ................................ 67<br />
David J. Kaczorowski ........................ 67<br />
Matthew F. Kalady ............................. 18<br />
Jawaid Kalim ....................................... 18<br />
Timothy D. Kane ................................ 28<br />
Sergey V. Kantsevoy ......................... 32<br />
Kazunori Kasama ........................ 27, 52<br />
Zachary Kastenberg ......................... 28<br />
Namir Katkhouda ....................... 55, 67<br />
L. Brian Katz ......................................... 75<br />
Nilton Kawahara ................................ 27<br />
Chuck Kennedy .................................. 64<br />
Michael J. Kim ..................................... 67<br />
Subhash U. Kini .................................. 46<br />
Sue Kirkman ........................................ 41<br />
Seigo Kitano ................................. 19, 70<br />
Shuji Kitashiro .................................... 39<br />
Bastiaan R. Klarenbeek ............. 24, 68<br />
Nicoleta O. Kolozsvari ...................... 56<br />
Shanu N. Kothari ........................ 32, 75<br />
Amanda J. Kravetz ............................ 54<br />
Sachin S. Kukreja ............................... 66<br />
Birte Kulemann .................................. 69<br />
Yo Kurashima ...................................... 75<br />
Marina Kurian .............................. 27, 74<br />
Antonio M. Lacy ................................. 20<br />
Pawanindra Lal ................................... 55<br />
Jacob C. Langer .................................. 28<br />
Antonio D. Lassaletta ....................... 69<br />
Wai Lun Law ........................................ 56<br />
William Laycock ................................. 55<br />
Gyusung Lee ................................ 57, 68<br />
James Lee ............................................ 19<br />
Andras Legner .................................... 68<br />
Joel Leroy ...................................... 19, 55<br />
Emanuele Lezoche ........................... 68<br />
Michael K.W. Li ................................... 70<br />
Isadore Lieberman ............................ 40<br />
Song Liang .......................................... 46<br />
Demetrius E.M. Litwin ..................... 40<br />
Thom E. Lobe ...................................... 28<br />
Katie Love ............................................ 54<br />
Kirk Allen Ludwig .............................. 36<br />
Markham C. Luke .............................. 36<br />
James D. Luketich ............................. 62<br />
Bruce V. MacFadyen Jr. .................... 54<br />
Joseph Mamazza ............................... 51<br />
Jacques Marescaux .................... 25, 41<br />
Gerald Marks ................................ 21, 70<br />
Jeffrey M. Marks ......35, 40, 47, 51, 66<br />
John H. Marks ..................................... 36<br />
Michael R. Marohn ............................ 40<br />
Ian Martin ............................................. 33<br />
Pamela Martin .................................... 64<br />
Jose M. Martinez ................................ 40<br />
Abraham Mathew ............................ 40<br />
Samer G. Mattar ................................. 64<br />
Ronald Matteotti ............................... 46<br />
Kai Matthes ......................................... 74<br />
Brent D. Matthews ............................ 33<br />
Dirk W. Meijer ...................................... 58<br />
Ozanan R. Meireles ........................... 58<br />
John D. Mellinger .............................. 66<br />
W. Scott Melvin ........................... 51, 57<br />
Adam T. Meneghetti ......................... 27<br />
Carlos A. Menezes ............................. 56<br />
Dean J. Mikami ............................ 51, 57<br />
Bertrend Millat ................................... 33<br />
Karl A. Miller ........................................ 20<br />
Rebecca Manget Minter ................. 51<br />
Yoav Mintz .................................... 40, 51<br />
Danilo Miskovic ................................. 56<br />
John R.T. Monson .............................. 36<br />
Derek E. Moore ................................... 50<br />
John M. Morton ................................. 75<br />
Fady Moustarah ................................. 58<br />
Erica Moran ......................................... 22<br />
Kenric M. Murayama ........................ 69<br />
Didier Mutter ...................................... 35<br />
Omer Nasir<br />
Radu Nedelcoviciu ............................ 47<br />
Adrian Marius Nedelcub ................. 69<br />
Ninh Tuan Nguyen ............................ 20<br />
Thinh H Nguyen ................................ 46<br />
12 th World Congress of Endoscopic Surgery 202
Index of Faculty and Presenters<br />
Gregg K. Nishi ..................................... 74<br />
Yuri W. Novitsky ....................33, 67, 75<br />
Michael S. Nussbaum ...................... 56<br />
David O’Brien ...................................... 18<br />
Kathleen O’Connell .......................... 68<br />
Tomonori Ohsawa ............................ 63<br />
Allan E. Okrainec ....34, 52, 56, 65, 74<br />
Dmitry Oleynikov .................32, 66, 75<br />
Sarah C. Oltmann .............................. 46<br />
Pablo E. Omelanczuk ....................... 69<br />
Raymond P. Onders .......................... 36<br />
Sean B. Orenstein .............................. 56<br />
Ismail H. Ozerhan .............................. 68<br />
Chinnasamy Palanivelu ............ 27, 35<br />
Juan P. Pantoja ................................... 19<br />
Neely Panton ...................................... 54<br />
Adrian E. Park ............................... 64, 75<br />
Chan W. Park ....................................... 66<br />
John J. Park .......................................... 18<br />
Michael Parker ............................. 35, 63<br />
Eric M. Pauli ......................................... 67<br />
Nikhil Pawa .......................................... 56<br />
Suraj B. Pawar ..................................... 35<br />
Jonathan Pearl ................................... 34<br />
Carlos A. Pellegrini ............................ 65<br />
Jacques J. Perissat ............................. 70<br />
Silvana Perretta .....................35, 57, 63<br />
Jeffrey H. Peters ....................41, 53, 62<br />
Edward H. Phillips ...................... 52, 62<br />
Andrea Pietrabissa ............................ 58<br />
Alessio Pigazzi .................................... 66<br />
Rodrigo A. Pinto ................................ 54<br />
Tim Pitney ............................................ 40<br />
Mun Jye Poi ......................................... 56<br />
Alfons Pomp ................................ 20, 66<br />
Jeffrey L. Ponsky ................................ 28<br />
Benjamin K. Poulose ................. 66, 75<br />
Pornthape Prathanvanich .............. 47<br />
Rhonda J. Prewitt .............................. 32<br />
Jose Manuel Prince ........................... 28<br />
Aurora Dawn Pryor ........................... 67<br />
Shailesh Puntambekar .................... 35<br />
Karim Qayumi ..................................... 65<br />
Sonia L. Ramamoorthy .................... 18<br />
Bruce J. Ramshaw ............................. 62<br />
Abhay Rane ......................................... 39<br />
G. V. Rao ................................................ 51<br />
Prashanth Prabhakar Rao ........ 39, 55<br />
David W. Rattner ......................... 51, 53<br />
Arthur Rawlings ................................. 63<br />
Petachia Reissman ............................ 36<br />
Feza Remzi ........................................... 55<br />
Jason F. Reynoso ................................ 46<br />
J. Ribamar ............................................. 27<br />
William O. Richards ........................... 66<br />
Erwin Rieder ........................................ 58<br />
E. Matt Ritter ....................................... 34<br />
Homero Rivas ..................................... 39<br />
Sergio Roll ............................................ 51<br />
John R. Romanelli ...................... 32, 65<br />
Michael J. Rosen ......................... 33, 62<br />
Raul J. Rosenthal ....20, 46, 52, 56, 68<br />
James B. Rosser Jr. ............................. 75<br />
Steven S. Rothenberg ...................... 28<br />
Francesco Rubino .............................. 41<br />
Dan Ruiz ............................................... 47<br />
Eric Rullier ............................................ 19<br />
Mohamad D Saad ............................. 47<br />
Adheesh A. Sabnis ..................... 54, 75<br />
Yoshihisa Saida .................................. 69<br />
Barry A. Salky ............................... 58, 69<br />
Bryan J. Sandler ................................. 57<br />
Byron F. Santos ............................ 46, 54<br />
Aviva Sapers ........................................ 40<br />
Abeezar I. Sarela ................................ 19<br />
Richard M. Satava .................19, 41, 62<br />
Philip R. Schauer ................................ 41<br />
Bruce D. Schirmer .................51, 54, 64<br />
Steven D. Schwaitzberg ........... 19, 58<br />
Daniel J. Scott .............................. 39, 64<br />
Carol E. Scott-Conner ....................... 24<br />
Donna See ........................................... 36<br />
Don J. Selzer ........................................ 35<br />
P Senthilnathan ................................. 55<br />
Elliot L. Servais ................................... 50<br />
Neal E. Seymour ................................. 75<br />
Baiju R. Shah ....................................... 36<br />
Nilay R. Shah ....................................... 56<br />
Paresh C. Shah .................................... 27<br />
Scott A. Shikora .................................. 20<br />
Samuel Shuchleib ............................. 70<br />
Noam Shussman ............................... 58<br />
Gerd R. Silberhumer ......................... 67<br />
Allan E. Siperstein ...................... 19, 50<br />
David E. Skarda .................................. 50<br />
C. Daniel Smith .................................. 47<br />
Brad E. Snyder .................................... 46<br />
Luc Soler ........................................ 41, 58<br />
Toyooki Sonoda ................................. 36<br />
Nathaniel J. Soper ................25, 34, 53<br />
Mike Stahl ............................................ 40<br />
Steven C. Stain ................................... 50<br />
Greg V. Stiegmann ............................ 53<br />
Sharon Stein ........................................ 18<br />
Vivian E.M. Strong ...................... 19, 22<br />
Erica Sutton ......................................... 35<br />
Lee L. Swanstrom ..........28, 34, 52, 53<br />
Patricia Sylla ........................................ 40<br />
Zoltan Szabo ....................................... 75<br />
Amir Szold .................................... 20, 50<br />
Nobumi Tagaya .................................. 55<br />
Mark A. Talamini ......................... 53, 67<br />
Eduardo Targarona ..............35, 55, 69<br />
Craig J. Taylor ...................................... 62<br />
Julio A. Teixeira ......................20, 39, 74<br />
Christopher C. Thompson ....... 20, 40<br />
Jonathan R. Thompson ................... 47<br />
Kari Thompson ................................... 35<br />
Michael H. Thompson ...................... 28<br />
Sarah K. Thompson .......................... 67<br />
Augusto Almeida Tinoco ......... 33, 67<br />
Manish M. Tiwari ................................ 63<br />
Philippe A. Topart .............................. 46<br />
Alfonso Torquati ......................... 20, 41<br />
Shirin Towfigh ............................. 33, 62<br />
Tung T. Tran ......................................... 67<br />
L. William Traverso ..................... 33, 54<br />
Thadeus L. Trus .................................. 74<br />
Albert W. Tsang .................................. 68<br />
Shawn T. Tsuda ............................ 34, 76<br />
Jenna Turocy ....................................... 58<br />
Tehemton Udwadia .......................... 67<br />
Surendra M. Ugale ..................... 27, 33<br />
David R. Urbach ................................. 65<br />
Oliver A. Varban ................................. 46<br />
Esteban Varela .................................... 55<br />
Melina C. Vassiliou ........34, 46, 66, 74<br />
Khashayar Vaziri ................................. 66<br />
Ashley Vernon .................................... 34<br />
Leonardo Villegas .............................. 75<br />
Anthony J. Vine .................................. 27<br />
Guy R. Voeller ...................................... 62<br />
Daniel Von Renteln ........................... 51<br />
Go Wakabayashi ................................ 52<br />
Martin Walz ......................................... 19<br />
Z. Wang ................................................. 58<br />
Eric Glenn Weiss ................................. 36<br />
Steven D. Wexner .................52, 53, 68<br />
R. Larry Whelan ........................... 19, 54<br />
Mark H. Whiteford ............................. 18<br />
Yanghee Woo ..................................... 66<br />
Tatsuo Yamakawa .............................. 52<br />
Manabu Yamamoto .......................... 52<br />
Jun Yan .................................................. 50<br />
Han-Kwang Yang ............................... 19<br />
Laurence Yee ....................................... 18<br />
Tonia M. Young-Fadok ..................... 36<br />
Yassar Youssef ..................................... 67<br />
Basil Yurcisin II .................................... 22<br />
Minhua Zheng ................................... 55<br />
Jacqui C. Zhu ...................................... 68<br />
Ricardo Zorron ................................... 59<br />
Natan Zundel ............................... 56, 70<br />
12 th World Congress of Endoscopic Surgery<br />
203 www.12thworldcongress.org
12 th World Congress of Endoscopic Surgery<br />
Notes<br />
12 th World Congress of Endoscopic Surgery 204