Anthrax Lab Protocol - Office of Public Health Practice
Anthrax Lab Protocol - Office of Public Health Practice
Anthrax Lab Protocol - Office of Public Health Practice
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
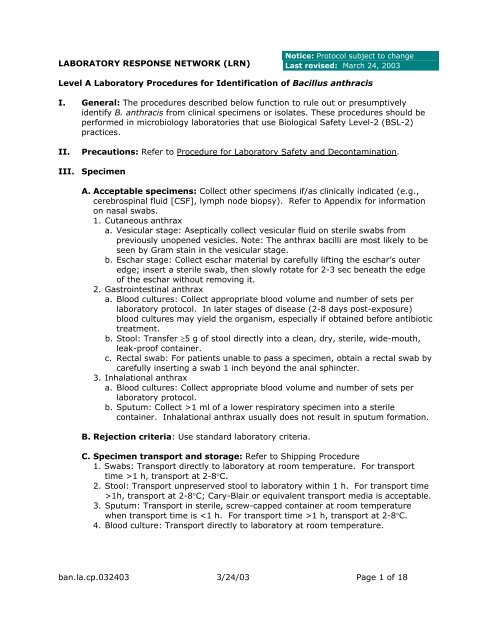
LABORATORY RESPONSE NETWORK (LRN)<br />
Notice: <strong>Protocol</strong> subject to change<br />
Last revised: March 24, 2003<br />
Level A <strong>Lab</strong>oratory Procedures for Identification <strong>of</strong> Bacillus anthracis<br />
I. General: The procedures described below function to rule out or presumptively<br />
identify B. anthracis from clinical specimens or isolates. These procedures should be<br />
performed in microbiology laboratories that use Biological Safety Level-2 (BSL-2)<br />
practices.<br />
II. Precautions: Refer to Procedure for <strong>Lab</strong>oratory Safety and Decontamination.<br />
III. Specimen<br />
A. Acceptable specimens: Collect other specimens if/as clinically indicated (e.g.,<br />
cerebrospinal fluid [CSF], lymph node biopsy). Refer to Appendix for information<br />
on nasal swabs.<br />
1. Cutaneous anthrax<br />
a. Vesicular stage: Aseptically collect vesicular fluid on sterile swabs from<br />
previously unopened vesicles. Note: The anthrax bacilli are most likely to be<br />
seen by Gram stain in the vesicular stage.<br />
b. Eschar stage: Collect eschar material by carefully lifting the eschar’s outer<br />
edge; insert a sterile swab, then slowly rotate for 2-3 sec beneath the edge<br />
<strong>of</strong> the eschar without removing it.<br />
2. Gastrointestinal anthrax<br />
a. Blood cultures: Collect appropriate blood volume and number <strong>of</strong> sets per<br />
laboratory protocol. In later stages <strong>of</strong> disease (2-8 days post-exposure)<br />
blood cultures may yield the organism, especially if obtained before antibiotic<br />
treatment.<br />
b. Stool: Transfer ≥5 g <strong>of</strong> stool directly into a clean, dry, sterile, wide-mouth,<br />
leak-pro<strong>of</strong> container.<br />
c. Rectal swab: For patients unable to pass a specimen, obtain a rectal swab by<br />
carefully inserting a swab 1 inch beyond the anal sphincter.<br />
3. Inhalational anthrax<br />
a. Blood cultures: Collect appropriate blood volume and number <strong>of</strong> sets per<br />
laboratory protocol.<br />
b. Sputum: Collect >1 ml <strong>of</strong> a lower respiratory specimen into a sterile<br />
container. Inhalational anthrax usually does not result in sputum formation.<br />
B. Rejection criteria: Use standard laboratory criteria.<br />
C. Specimen transport and storage: Refer to Shipping Procedure<br />
1. Swabs: Transport directly to laboratory at room temperature. For transport<br />
time >1 h, transport at 2-8°C.<br />
2. Stool: Transport unpreserved stool to laboratory within 1 h. For transport time<br />
>1h, transport at 2-8°C; Cary-Blair or equivalent transport media is acceptable.<br />
3. Sputum: Transport in sterile, screw-capped container at room temperature<br />
when transport time is 1 h, transport at 2-8°C.<br />
4. Blood culture: Transport directly to laboratory at room temperature.<br />
ban.la.cp.032403 3/24/03 Page 1 <strong>of</strong> 18
IV. Materials<br />
A. Reagents<br />
1. Gram stain reagents<br />
2. Catalase reagent (3% hydrogen peroxide)<br />
3. Motility media (or slide, coverslips, saline for wet mount)<br />
4. India ink (an optional test)<br />
5. Sterile saline<br />
B. Media<br />
1. 5% sheep blood agar (SBA) or equivalent<br />
2. Chocolate agar (CA)<br />
3. MacConkey agar (MAC)<br />
4. Phenyl ethyl alcohol agar (PEA)<br />
5. Blood culture bottles<br />
6. Tubed motility media<br />
7. Tryptic soy broth (TSB), or equivalent<br />
8. Thioglycolate broth or equivalent<br />
C. Equipment/miscellaneous<br />
1. Blood culture instrument (optional)<br />
2. Light microscope with 10X, 40X and 100X objectives and 10X eyepiece<br />
3. Microscope slides and coverslips<br />
4. Disposable bacteriologic inoculating loops<br />
5. Incubator, 35-37 o C, ambient preferred (CO 2 enriched is acceptable)<br />
Disclaimer: Names <strong>of</strong> vendors or manufacturers are provided as examples <strong>of</strong><br />
suitable product sources; inclusion does not imply endorsement by the Centers for<br />
Disease Control and Prevention, the Department <strong>of</strong> <strong>Health</strong> and Human Services, the<br />
United States Army, or the Federal Bureau <strong>of</strong> Investigation.<br />
V. Quality control: Document all quality control results for the following tests per<br />
standard laboratory procedure/protocol.<br />
VI. Procedure: Refer to Fig. A1a and A1b.<br />
A. Stains and smears<br />
1. Gram stain<br />
a. Procedure: Perform Gram stain procedure/QC per standard laboratory<br />
protocol.<br />
b. Interpretation<br />
(1) B. anthracis is a large gram-positive rod (1-1.5 X 3-5 µm).<br />
(2) Blood and impression smears: Vegetative cells seen on Gram stain <strong>of</strong><br />
blood and impression smears are in short chains <strong>of</strong> 2-4 cells that are<br />
encapsulated, which may be seen on the Gram stain as clear zones<br />
around the bacilli. Spores are not present in clinical samples unless<br />
exposed to low CO 2 levels, such as those found in the atmosphere; higher<br />
CO 2 levels within the body inhibit sporulation. The presence <strong>of</strong> large<br />
encapsulated gram-positive rods in the blood is strongly presumptive for<br />
B. anthracis identification. Refer to Fig. A2.<br />
ban.la.cp.032403 3/24/03 Page 2 <strong>of</strong> 18
(3) Growth on SBA or equivalent medium: B. anthracis forms oval, centralto-subterminal<br />
spores (1 X 1.5 µm) on SBA that do not cause significant<br />
swelling <strong>of</strong> the cell; frequently occur as long chains <strong>of</strong> bacilli. However,<br />
cells from growth on SBA regardless <strong>of</strong> the incubation conditions<br />
(ambient atmosphere or CO 2 enriched) are not encapsulated. Refer to<br />
Fig. A3a and Fig. A3b.<br />
2. India Ink (optional procedure)<br />
a. Purpose. Used to improve visualization <strong>of</strong> encapsulated B. anthracis in clinical<br />
samples such as blood, blood culture bottles, or cerebrospinal fluid (CSF).<br />
b. Quality control<br />
(1) Positive control strain: Klebsiella pneumoniae (or laboratory validated<br />
equivalent) will demonstrate a well-defined clear zone on SBA.<br />
(2) Negative control strain: E. coli ATCC 25922 (or laboratory validated<br />
equivalent) will demonstrate no clear zone.<br />
(3) Method controls: Perform the test with suspensions <strong>of</strong> fresh cultures <strong>of</strong><br />
the control strains. Control strains should be assayed on each day <strong>of</strong><br />
testing.<br />
(4) Resolving out-<strong>of</strong>-control results: Check media, reagents, controls and<br />
equipment; replace or correct as appropriate. Document corrective<br />
actions and repeat test.<br />
c. Procedure<br />
(1) For the controls, transfer a small amount <strong>of</strong> growth (1 mm diameter)<br />
from each control SBA plate (positive control = Klebsiella pneumoniae;<br />
negative control = Escherichia coli ATCC 25922) into 0.5 ml saline and<br />
mix.<br />
(2) For the unknowns, take 100 µl <strong>of</strong> sample (blood, CSF). Transfer 5-10 µl<br />
<strong>of</strong> unknown sample or control to a slide. Place a coverslip on the drop,<br />
and then add 5-10 µl <strong>of</strong> India ink to the edge <strong>of</strong> the coverslip. After the<br />
ink diffuses across the slide, view the cells using 100X oil immersion<br />
objective with oil on top <strong>of</strong> the coverslip.<br />
d. Interpretation<br />
(1) Positive result: The capsule will appear as a well-defined clear zone<br />
around the cells.<br />
(2) Negative result: No zone will be present.<br />
e. Reporting/actions<br />
(1) Clinical specimens with encapsulated (visualized with India ink), grampositive<br />
rods provide a presumptive identification <strong>of</strong> B. anthracis.<br />
(2) Every effort should be made to obtain an isolate for continued testing and<br />
referral to state public health laboratory.<br />
f. Limitations<br />
(1) Interpretation <strong>of</strong> results requires trained/experienced staff.<br />
(2) A negative test result should not be used to rule out B. anthracis.<br />
B. Cultures<br />
1. Inoculation and plating procedure: Inoculate and streak the following media for<br />
isolation <strong>of</strong> the respective specimen types. Note: Standard media should be used<br />
according to normal laboratory procedures.<br />
a. Blood cultures: Process following routine laboratory protocol.<br />
b. Cutaneous swab specimens: Plate directly on media used routinely for<br />
surface wounds such as SBA, MAC, and broth enrichment, and prepare<br />
smears for staining. Note: B. anthracis does not grow on MAC.<br />
ban.la.cp.032403 3/24/03 Page 3 <strong>of</strong> 18
c. Stool: Plate directly on appropriate media, such as PEA, SBA, and MAC.<br />
Note: B. anthracis does not grow on PEA.<br />
d. Sputum specimens: Plate directly on media used routinely, such as SBA, MAC,<br />
and CA, and prepare smears for staining.<br />
2. Incubation<br />
a. Temperature: 35-37°C<br />
b. Atmosphere: Ambient preferred<br />
c. Length <strong>of</strong> incubation: Hold primary plates for at least 3 days; read daily.<br />
Examine plates within 18-24 h <strong>of</strong> incubation. Growth <strong>of</strong> B. anthracis may<br />
be observed as early as 8 h after incubation.<br />
3. Colony characteristics <strong>of</strong> B. anthracis<br />
a. After incubation <strong>of</strong> SBA plates for 15-24 h at 35-37°C, well isolated colonies<br />
<strong>of</strong> B. anthracis are 2-5 mm in diameter. The flat or slightly convex colonies<br />
are irregularly round, with edges that are slightly undulate (irregular, wavy<br />
border), and have a ground-glass appearance. There may be <strong>of</strong>ten commashaped<br />
projections from the colony edge, producing the "Medusa-head"<br />
colony. Refer to Fig. A4.<br />
b. B. anthracis colonies on SBA usually have a tenacious consistency. When<br />
teased with a loop, the growth will stand up like beaten egg white; refer to<br />
Fig. A5. In contrast to colonies <strong>of</strong> B. cereus and B. thuringiensis, colonies <strong>of</strong><br />
B. anthracis are not β-hemolytic; refer to Fig. A6. However, weak hemolysis<br />
may be observed under areas <strong>of</strong> confluent growth in aging cultures and<br />
should not be confused with β-hemolysis.<br />
c. When examining primary growth media, it is important to compare the extent<br />
<strong>of</strong> growth on SBA plates with that on MAC. B. anthracis grows well on SBA<br />
but does not grow on MAC or PEA.<br />
d. B. anthracis grows rapidly; heavily inoculated areas may show growth within<br />
6-8 h and individual colonies may be detected within 12-15 h. This trait can<br />
be used to isolate B. anthracis from mixed cultures containing slower-growing<br />
organisms.<br />
4. Extent <strong>of</strong> identification: For the Level A laboratory, identification is limited to<br />
‘presumptive’ only (see section VII, below, for specific criteria/key<br />
characteristics).<br />
C. Motility test: Wet mount or motility medium<br />
1. Purpose: Used to determine motility <strong>of</strong> suspected isolates; B. anthracis is<br />
nonmotile. Two methods are given, the wet mount and the motility medium<br />
test.<br />
2. Wet mount procedure<br />
a. Deliver 2 drops (approximately 0.1 ml) <strong>of</strong> TSB, or equivalent, into a sterile<br />
glass tube. Using an inoculating loop, transfer a portion <strong>of</strong> the suspect colony<br />
from a 12-20 h culture and suspend the growth in the broth medium.<br />
b. Alternatively, a loopful <strong>of</strong> medium from a fresh broth culture can be used.<br />
c. Transfer 10 µl <strong>of</strong> the suspension to a microscope slide and overlay with a<br />
coverslip.<br />
d. Examine slide under a microscope using the 40X objective (total<br />
magnification 400X; may also be viewed at 1000X with oil objective).<br />
e. Discard slide(s) following standard laboratory procedures, such as into 0.5%<br />
hypochlorite solution.<br />
ban.la.cp.032403 3/24/03 Page 4 <strong>of</strong> 18
3. Motility medium test procedure<br />
a. Using a sterile inoculating needle, remove a portion <strong>of</strong> growth from an<br />
isolated, suspect colony after 18-24 h incubation.<br />
b. Inoculate the motility medium by carefully stabbing the needle 3-4 cm into<br />
the medium and then drawing the needle directly back out so that a single<br />
line <strong>of</strong> inoculum can be observed.<br />
c. Incubate the tube at 35-37°C in ambient atmosphere for 18-24 h.<br />
4. Interpretation <strong>of</strong> motility results: Lack <strong>of</strong> motility is unusual among Bacillus<br />
species and is therefore useful in the preliminary identification <strong>of</strong> B. anthracis<br />
isolates.<br />
a. Wet mount<br />
(1) Positive result: Motile organisms will be observed moving throughout<br />
the suspension. Observe that the movement may be sluggish/slower<br />
than that <strong>of</strong> the positive controls .<br />
(2) Negative result: Nonmotile organisms either do not move or move with<br />
Brownian motion.<br />
b. Motility test<br />
(1) Positive result: Motile organisms will form a diffuse growth zone around<br />
the inoculum stab.<br />
(2) Negative result: Nonmotile organisms, such as B. anthracis, will form a<br />
single line <strong>of</strong> growth that does not deviate from the original inoculum<br />
stab.<br />
5. Quality control<br />
a. Positive control strain: Pseudomonas aeruoginosa ATCC 35032 or laboratoryvalidated<br />
equivalent will demonstrate motility.<br />
b. Negative control strain: Acinetobacter spp. ATCC 49139 or laboratoryvalidated<br />
equivalent will show no motility<br />
c. Method controls: Perform the test with fresh cultures <strong>of</strong> the control strains<br />
using the same method as with unknowns. Control strains should be assayed<br />
on each day <strong>of</strong> testing.<br />
6. Resolving out-<strong>of</strong>-control results<br />
a. Check media, reagents, controls and equipment; replace or correct as<br />
appropriate. Document corrective actions and repeat test.<br />
b. Check purity and identity <strong>of</strong> control strains and repeat testing.<br />
VII. Interpretation and reporting<br />
A. Presumptive identification criteria: Refer to Table A1.<br />
1. Direct smears from clinical samples, such as blood, CSF, or skin lesion (eschar)<br />
material: Encapsulated gram-positive rods<br />
2. From growth on SBA or equivalent media: Large gram-positive rods (may<br />
stain gram-variable after 72 h <strong>of</strong> culture). Spores may be found in culture,<br />
under non-CO 2 atmosphere (but not on direct examination). Spores are<br />
nonswelling and oval-shaped.<br />
3. Rapid, aerobic growth, and tenacious colonies on sheep blood agar.<br />
4. Catalase positive<br />
5. Nonmotile: In addition to B. anthracis, B. cereus var. mycoides is nonmotile.<br />
6. Nonhemolytic on SBA, ground-glass appearance <strong>of</strong> colonies<br />
ban.la.cp.032403 3/24/03 Page 5 <strong>of</strong> 18
B. Rule out: While hemolysis, gram stain morphology, or motility can be used for<br />
rule out when the result provides clear evidence that the isolate is not B. anthracis<br />
(e.g., a clearly visible zone <strong>of</strong> beta hemolysis), a combination <strong>of</strong> two Level A tests is<br />
recommended for rule out.<br />
C. Reporting/action<br />
1. Consult with state public health laboratory director (or designate) if B. anthracis<br />
is suspected.<br />
2. General instruction and information<br />
a. Preserve original specimens pursuant to a potential criminal investigation and<br />
possible transfer to an appropriate LRN laboratory.<br />
b. Environmental/nonclinical samples and samples from announced events<br />
are not processed by Level A <strong>Lab</strong>oratory; submitter should contact the state<br />
public health laboratory directly.<br />
c. The state public health laboratory/state public health department will<br />
coordinate notification <strong>of</strong> local FBI agents as appropriate.<br />
d. Assist local law enforcement efforts in conjunction with guidance received<br />
from the state public health laboratory.<br />
e. The state public health laboratory/state public health department may<br />
request transfer <strong>of</strong> suspicious specimens prior to presumptive testing.<br />
f. FBI and state public health laboratory/state public health department will<br />
coordinate the transfer <strong>of</strong> isolates/specimens to a higher-level LRN laboratory<br />
as appropriate; refer to Shipping Procedure.<br />
3. Immediately notify state public health laboratory director (or designate) and<br />
state public health department epidemiologist/health <strong>of</strong>ficer if B. anthracis<br />
cannot be ruled out and a bioterrorist event is suspected.<br />
4. Immediately notify physician/infection control according to internal policies if B.<br />
anthracis cannot be ruled out.<br />
5. If B. anthracis is ruled out, proceed with efforts to identify using established<br />
procedures.<br />
VIII. References<br />
Brachman, P.S., and A.M. Friedlander. <strong>Anthrax</strong>, p. 729-739. In S.A. Plotkin and<br />
E.A. Mortimer, Jr. (ed), Vaccines. W.B. Saunders, Philadelphia, PA.<br />
Cieslak, T.J. and E.M. Eitzen, Jr. 1999. Clinical and epidemiologic principles <strong>of</strong><br />
anthrax. Emerg. Infect. Dis. 5:552-555.<br />
Dutz, W. and E. Kohout. 1971. <strong>Anthrax</strong>. Pathol. Annu. 6:209-248.<br />
Gilchrist, M.J.R., W.P. McKinney, J.M. Miller, and A.S. Weissfeld. 2000.<br />
Cumitech 33, <strong>Lab</strong>oratory Safety, management , and diagnosis <strong>of</strong> biological agents<br />
associated with bioterrorism. Coordinating ed., J.W. Snyder. ASM Press, Washington,<br />
D.C.<br />
Lew, D. P. 2000. Bacillus anthracis (<strong>Anthrax</strong>). p. 2215-2220. In G. L. Mandell, J.E.<br />
Bennett, and R. Dolin (ed), Principles and <strong>Practice</strong> <strong>of</strong> Infectious Disease, 5 th ed.<br />
Churchill Livingston, Philadelphia, PA.<br />
ban.la.cp.032403 3/24/03 Page 6 <strong>of</strong> 18
Logan, N.A. and P.C. Turnbull. 1999. Bacillus and recently derived genera, p. 357-<br />
369. In P.R. Murray, E.J. Baron, M.A. Pfaller, F.C. Tenover, and R.H. Yolken (ed)<br />
manual <strong>of</strong> Clinical Microbiology, 7 th ed. American Society for Microbiology,<br />
Washington, D.C.<br />
ban.la.cp.032403 3/24/03 Page 7 <strong>of</strong> 18
Figure A1a. Flowchart <strong>of</strong> B. anthracis Level A procedures.<br />
ban.la.cp.032403 3/24/03 Page 8 <strong>of</strong> 18
an.la.cp.032403 3/24/03 Page 9 <strong>of</strong> 18
Figure A2. Gram stain <strong>of</strong> B. anthracis in rhesus monkey blood, magnification 1000X<br />
ban.la.cp.032403 3/24/03 Page 10 <strong>of</strong> 18
Figure A3a. Gram stain <strong>of</strong> B. anthracis from SBA, magnification 1000X<br />
ban.la.cp.032403 3/24/03 Page 11 <strong>of</strong> 18
Figure A3b. Gram stain <strong>of</strong> B. anthracis with spores, magnification 1000X<br />
ban.la.cp.032403 3/24/03 Page 12 <strong>of</strong> 18
Figure A4. B. anthracis colony morphology; overnight cultures on SBA.<br />
ban.la.cp.032403 3/24/03 Page 13 <strong>of</strong> 18
Figure A5. Tenacious colonies <strong>of</strong> B. anthracis on SBA<br />
ban.la.cp.032403 3/24/03 Page 14 <strong>of</strong> 18
Figure A6. B. anthracis and B. cereus colony morphology; overnight cultures <strong>of</strong> B. cereus<br />
(left side <strong>of</strong> plate) and B. anthracis (right side) on SBA.<br />
ban.la.cp.032403 3/24/03 Page 15 <strong>of</strong> 18
Table A1. Presumptive identification <strong>of</strong> B. anthracis<br />
<strong>Lab</strong><br />
Level<br />
Type <strong>of</strong> sample<br />
Presumptive identification<br />
Characteristic<br />
Method<br />
A Clinical sample 1. Gram-positive rods<br />
Gram stain<br />
AND<br />
2. Capsule<br />
India ink stain<br />
A Isolate 1 Spore-former<br />
Gram stain<br />
AND<br />
2. Colony morphology<br />
Observation on SBA<br />
AND<br />
3. Nonhemolytic<br />
Observation on SBA<br />
AND<br />
4. Nonmotile<br />
Motility medium or<br />
Wet mount<br />
ban.la.cp.032403 3/24/03 Page 16 <strong>of</strong> 18
IX. Appendix: Nasal specimens for Bacillus anthracis screening<br />
A. General: Nasal specimens (nares culture) should ONLY be used to support a<br />
confirmed exposure to B. anthracis or during an ongoing epidemiologic<br />
investigation. Gram stain <strong>of</strong> nasal specimens for B. anthracis spores is not<br />
recommended. Refer to limitations section below.<br />
B. Materials: Swab (Dacron, rayon or other synthetic swabs are preferred over cotton)<br />
and transport medium for culture.<br />
C. Procedure<br />
1. Selection<br />
a. The specimen <strong>of</strong> choice is a swab specimen taken at least 1 cm inside the<br />
nares.<br />
b. Lesions in the nose require samples from the advancing margin <strong>of</strong> the lesions.<br />
2. Method<br />
a. Carefully insert the moistened swab (saline, sterile water) at least 1 cm into<br />
the<br />
nares.<br />
b. Firmly sample the inside <strong>of</strong> the nares by rotating the swab and leaving it in<br />
place for 10 to 15 sec.<br />
c. Withdraw the swab, insert it into its transport container, and submit the<br />
sampling unit to the laboratory for culture.<br />
3. <strong>Lab</strong>eling<br />
a. <strong>Lab</strong>el the swab container with patient information.<br />
b. Indicate, if possible, the degree or likelihood <strong>of</strong> exposure.<br />
4. Transport<br />
a. Transport the specimen to the laboratory as soon as possible.<br />
b. Do not refrigerate specimens for culture.<br />
5. Culture: Heat Shock<br />
a. Remove the swab from transport container and place it into 1.5 ml <strong>of</strong> sterile<br />
saline or a nutrient broth such as trypticase soy broth, brain heart infusion<br />
broth, or equivalent. Vigorously twist the swab, and recap the tube.<br />
b. Leave the swab in the tube. Place the broth suspension into a 65 o C water bath<br />
for 30 min.<br />
c. Plate 100-200 µl <strong>of</strong> broth on 5% sheep blood agar plate and incubate at<br />
35-37 o C for 18-24 h. Many B. anthracis will have visible growth in 12-18 h;<br />
observe for characteristics <strong>of</strong> B. anthracis.<br />
D. Interpretation: Observe colony morphology for typical Bacillus colonies, look for<br />
lack <strong>of</strong> hemolysis, perform Gram stain, and evaluate for B. anthracis characteristics<br />
as described in the Level A laboratory protocol.<br />
E. Reporting: If B. anthracis cannot be ruled out, submit the isolate to the state public<br />
health laboratory/department for confirmation. Refer to Level A reporting.<br />
F. Limitations: Nasal cultures taken to evaluate for the presence <strong>of</strong> anthrax spore<br />
have not been evaluated for sensitivity or specificity. Nasopharyngeal and throat<br />
specimens are not recommended for anthrax screens and should not be submitted.<br />
Nasal cultures are NOT recommended for screening those who are asymptomatic and<br />
without known exposure.<br />
ban.la.cp.032403 3/24/03 Page 17 <strong>of</strong> 18
G. Procedure Notes<br />
1. Anterior nares cultures, without an indication <strong>of</strong> the presence <strong>of</strong> a lesion, are<br />
routinely examined only for presence <strong>of</strong> Staphylococcus aureus and β-hemolytic<br />
streptococci. Because <strong>of</strong> the unknown sensitivity <strong>of</strong> this method for detecting B.<br />
anthracis spores, interpret negative results with caution.<br />
2. Anterior nares cultures cannot be used to predict a subsequent infection with B.<br />
anthracis, and should not be submitted in lieu <strong>of</strong> blood and other appropriate<br />
specimens from symptomatic patients.<br />
3. Anaerobic cultures are not done on nasal specimens. B. anthracis produces<br />
spores in culture only when grown in air.<br />
4. Nasal swabs may also be plated directly onto sheep blood agar prior to or without<br />
heat shocking, however normal nasal flora may overgrow very low numbers <strong>of</strong><br />
Bacillus colonies.<br />
5. Pediatric needs: Use the same procedure substituting a small fine-wire or<br />
nasopharyngeal swab to sample the anterior nares.<br />
ban.la.cp.032403 3/24/03 Page 18 <strong>of</strong> 18