Understanding Polycystic Ovary Syndrome (PCOS) can be both empowering and vital for many women. If you’ve ever wondered about PCOS symptoms that might indicate PCOS or are curious about the PCOS testing process, you’re in the right place.
In this article, we break down the fundamentals of how to test for PCOS, making the information accessible to anyone seeking insights into this common hormonal disorder. So, let’s dive in and unravel the mystery behind PCOS testing, empowering you with the knowledge you need for a proactive approach to your reproductive health.
Testing for PCOS: What You Need to Know
Understanding and testing for polycystic ovary syndrome is a pivotal step towards managing this prevalent hormonal disorder.
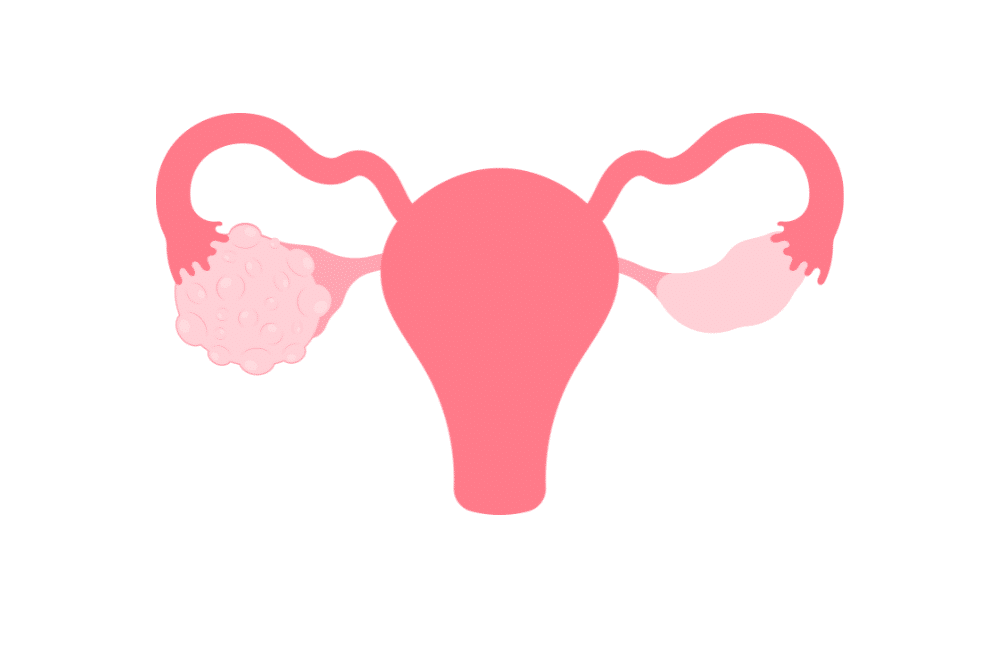
The process involves a comprehensive approach that begins with a discussion about your medical history. This conversation provides key insights into your situation, setting the stage for further examinations. A physical examination, including a pelvic exam, is the next step to check for physical signs such as enlarged ovaries or cysts (hence the term, polycystic ovaries).
Blood tests play a central role in the testing process, assessing hormone levels like testosterone, oestrogen, and luteinising hormone (LH). These tests offer valuable insights into potential hormonal imbalances associated with PCOS. Alongside blood tests, ultrasound imaging is employed to examine the ovaries, identifying the presence of cysts or other abnormalities. Additional tests may be conducted to rule out other potential causes, ensuring an accurate diagnosis. Understanding these testing procedures equips individuals with the knowledge to actively engage with healthcare providers, facilitating early detection and effective management of PCOS.
The Diagnosis Process: How to Determine if You Have PCOS
Navigating the diagnosis process for polycystic ovary syndrome involves several key steps aimed at uncovering whether this common hormonal disorder is affecting you. Let’s break down the process into simple terms, empowering you to understand how healthcare providers determine if you have PCOS.
1. Consultation and Medical History:
The journey begins with a discussion about your medical history. Your healthcare provider will ask about your menstrual cycle, symptoms, and any relevant health information. This conversation lays the groundwork for understanding your unique situation.
2. Physical Examination:
A physical examination is often conducted, including a pelvic exam. This step helps your healthcare provider check for any physical signs of PCOS, such as the size of the ovaries and the presence of cysts.
3. Blood Tests:
Blood tests are crucial for assessing hormone levels in your body. Elevated levels of testosterone, luteinising hormone (LH), and other hormones may indicate hormonal imbalances associated with PCOS. Additionally, metabolic markers like fasting insulin and glucose are often measured to provide a comprehensive picture.
4. Ultrasound Imaging:
Ultrasound is a non-invasive imaging technique used to examine the ovaries. Your healthcare provider will look for cysts or follicles on the ovaries, a key characteristic of PCOS.
5. Rule Out Other Conditions:
Sometimes, additional tests may be conducted to rule out other potential causes of your symptoms. This ensures an accurate diagnosis and allows a targeted approach to managing PCOS.
Understanding this diagnosis process empowers you to actively participate in discussions with your healthcare provider. If you’re experiencing irregular periods, fertility issues, or other symptoms associated with PCOS, seeking professional guidance is crucial. Early detection and diagnosis lay the foundation for effective management, enabling you to take proactive steps towards your reproductive health.
Understanding PCOS Blood Test Results
Deciphering the results of blood tests for polycystic ovary syndrome is key to gaining insights into your hormonal health. These tests play a pivotal role in confirming or ruling out PCOS, and understanding the results empowers you to actively engage in your healthcare.
1. Testosterone Levels:
Elevated testosterone levels are a common marker of PCOS. Testosterone is a male sex hormone present in both males and females, but higher levels in females may indicate hormonal imbalances associated with PCOS.
2. Luteinising Hormone (LH):
An imbalance in LH levels may also be indicative of PCOS. Elevated LH levels, when compared to follicle-stimulating hormone (FSH), contribute to the hormonal irregularities associated with the syndrome.
3. Oestrogen Levels:
Oestrogen, a primary female sex hormone, is often evaluated. While not a definitive marker for PCOS, imbalances in oestrogen levels may contribute to symptoms and are considered in the overall assessment.
4. Fasting Insulin and Glucose:
Testing insulin and glucose levels provides insights into metabolic aspects associated with PCOS. Elevated levels may indicate insulin resistance, a common feature in individuals with PCOS, influencing both hormonal and metabolic functions.
Understanding these key parameters in your blood test results helps paint a clearer picture of your hormonal health. It’s important to note that a diagnosis isn’t solely based on a single test result but rather on a combination of factors. Your healthcare provider will interpret these results in the context of your medical history and other diagnostic measures.
How is PCOS Confirmed: Explained
Confirming the presence of polycystic ovarian syndrome involves a multi-faceted approach that combines various diagnostic tools. The process aims to provide a comprehensive understanding of an individual’s hormonal and reproductive health.
Firstly, your healthcare provider will discuss your medical history, focusing on menstrual cycles, symptoms, and relevant health information. Following this, a physical examination, including a pelvic exam, may be conducted to identify any physical signs associated with PCOS, such as enlarged ovaries or cysts.
Key diagnostic tools include blood tests to evaluate hormone levels, specifically assessing testosterone, oestrogen, and luteinising hormone (LH). Elevated levels of these hormones can be indicative of hormonal imbalances linked to PCOS. Ultrasound imaging is another component, enabling the visualisation of the ovaries to identify the presence of cysts or follicles.
To confirm a PCOS diagnosis, healthcare providers consider the collective results of these assessments and may also rule out other potential causes for similar symptoms. This comprehensive approach ensures a more accurate and personalised diagnosis, laying the foundation for tailored management strategies. Understanding how PCOS is confirmed empowers individuals to actively participate in their healthcare journey and make informed decisions about their reproductive well-being.
Detecting PCOS: Signs and Symptoms to Look Out For
Recognising the signs and symptoms of polycystic ovary syndrome is essential for early detection and proactive management. While the manifestations can vary from person to person, there are common indicators to be mindful of:
Irregular Menstrual Cycles: One of the hallmark signs of PCOS is irregular periods. This may include prolonged cycles, missed periods, or unpredictable bleeding, reflecting hormonal imbalances.
Excess Hair Growth (Hirsutism): PCOS can lead to increased levels of male hormones (androgens), resulting in hirsutism—excessive hair growth in areas where men typically grow hair, such as the face, chest, or back.
Acne and Oily Skin: Hormonal fluctuations associated with PCOS can be one of the causes of hormonal acne and excessively oily skin, impacting the complexion.
Weight Changes: Sudden weight gain, particularly around the abdomen, is a common symptom. PCOS can influence the body’s ability to regulate insulin, potentially leading to weight-related issues. Learn how to lose weight with PCOS.
Thinning Hair or Hair Loss: PCOS may cause thinning of the hair on the scalp or lead to male-pattern baldness due to hormonal imbalances.
Pelvic Pain: Some individuals with PCOS may experience discomfort or pain in the pelvic region, often associated with cysts on the ovaries.
Difficulty Getting Pregnant: PCOS can affect fertility by disrupting ovulation. Women with PCOS may face challenges in conceiving.
Being vigilant about these signs and symptoms is crucial, especially if you notice a combination of these indicators. If you suspect PCOS, seeking guidance from a healthcare professional is vital for accurate diagnosis and tailored management. Early detection empowers individuals to take proactive steps toward addressing PCOS-related challenges and optimising reproductive health.
How to Get Properly Diagnosed with PCOS
Achieving a proper diagnosis for polycystic ovary syndrome involves a collaborative effort between you and your healthcare provider. Here’s a guide on how to navigate the diagnostic process effectively:
1. Consultation and Communication:
Initiate an open and detailed conversation with your healthcare provider. Share information about your menstrual cycles, symptoms, and any relevant medical history. Clear communication sets the foundation for a thorough assessment.
2. Physical Examination:
Your healthcare provider may conduct a physical examination, including a pelvic exam, to check for physical signs such as enlarged ovaries or cysts. This helps in narrowing down potential causes for your symptoms.
3. Blood Tests:
Hormone levels can help diagnose PCOS. Blood tests, specifically measuring testosterone, oestrogen, and luteinising hormone (LH), provide insights into hormonal imbalances. Additionally, markers like fasting insulin and glucose are often assessed to understand metabolic aspects.
4. Ultrasound Imaging:
Ultrasound imaging is utilised to visualise the ovaries. This non-invasive technique helps identify the presence of cysts or follicles, contributing to the confirmation of a PCOS diagnosis.
5. Comprehensive Assessment:
A comprehensive approach involves considering the collective results of medical history, physical examination, blood tests, and ultrasound imaging. This helps rule out other potential causes and ensures an accurate diagnosis tailored to your situation.
6. Consulting a Specialist:
In some cases, your healthcare provider may refer you to a specialist, such as a reproductive endocrinologist or a gynaecologist with expertise in hormonal disorders, for further evaluation and management.
7. Ongoing Communication:
Establish ongoing communication with your healthcare provider. This facilitates a collaborative approach to managing PCOS, allowing adjustments in your treatment plan as needed.
By actively participating in the diagnostic process and maintaining open communication with your healthcare team, you empower yourself to navigate PCOS with informed decision-making. Remember, early detection and a proactive approach to management can significantly improve outcomes for individuals with PCOS.
Testing Methods for PCOS: What to Expect
When undergoing testing for polycystic ovary syndrome, you can anticipate a comprehensive evaluation encompassing various methods to gain a holistic understanding of reproductive health.
The process typically begins with a detailed medical history discussion, focusing on menstrual patterns, symptoms, and relevant health information. Following this, a physical examination, including a pelvic exam, may be conducted to identify any physical signs indicative of PCOS, such as enlarged ovaries or cysts.
Blood tests are integral to the diagnostic process, assessing hormone levels such as testosterone, oestrogen, and luteinising hormone (LH). These tests contribute valuable insights into hormonal imbalances associated with PCOS. Ultrasound imaging further aids in the assessment by providing a visual examination of the ovaries, helping identify the presence of cysts or follicles. Combining these testing methods allows for a comprehensive diagnosis, ensuring that individuals receive tailored insights into their hormonal and reproductive health, paving the way for effective management strategies.
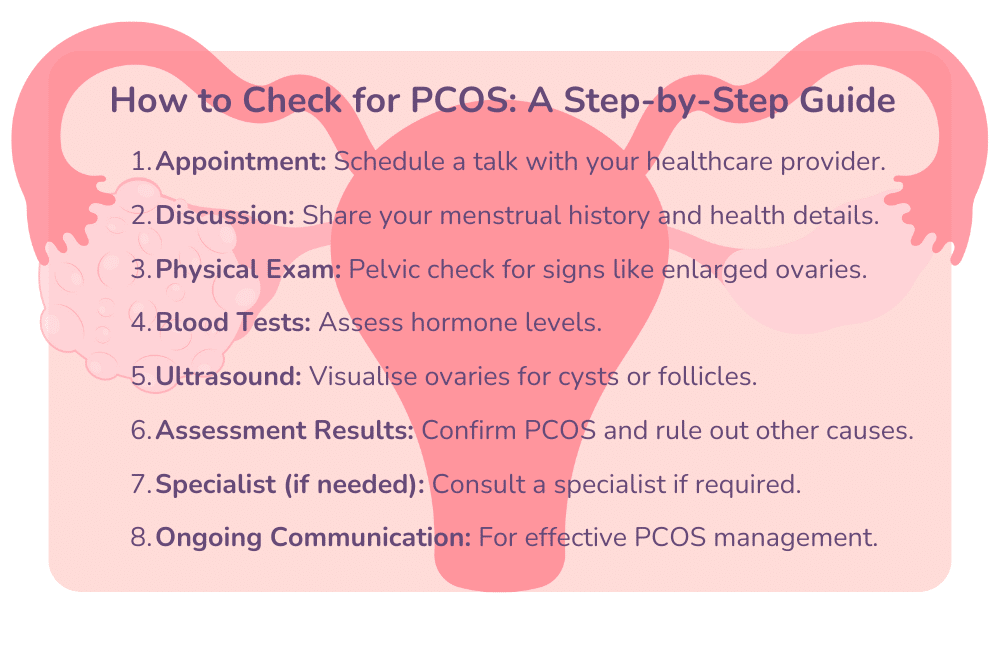
How to Check for PCOS: A Step-by-Step Guide
Empower yourself by taking proactive steps to assess your reproductive health with this actionable, step-by-step guide on checking for PCOS.