


Identifying the disease's stage (amount of spread) is critical for most forms of cancer. The size of the primary tumor and the extent of cancer's dissemination determine the stage. This can assist in determining a person's prognosis and treatment options.
Acute myeloid leukemia (AML), on the other hand, seldom results in tumor formation. It has expanded to other organs, such as the liver and spleen, and is typically prevalent throughout the bone marrow. As a result, unlike most other malignancies, AML is not staged. The prognosis for someone with AML is affected by various factors such as the patient's age, the subtype of AML (identified by lab tests), and the findings of additional lab tests.
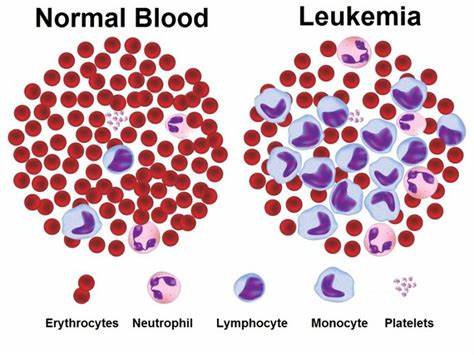
The subtypes of AML can be classified in a variety of ways. Despite the fact that all subtypes produce a reduction in normal blood cell counts, various forms of AML are linked to varied symptoms and issues. Furthermore, each subtype may respond to therapy in a unique way.
The morphology of Acute myeloid leukemia, or how malignant cells appear under a microscope, is the first characteristic to be identified. AML is categorized based on how closely it resembles a normal, immature white blood cell. The majority of patients with AML have a subtype known as myeloid leukemia, which implies the disease resides in the cells that generate neutrophils. Monoblastic or monocytic leukemia is a form of AML that affects others. The cells of monocytic leukemia appear like monocytes, which are white blood cells. Myeloblastic and monocytic cells can combine together to become leukemia cells. AML appears to be caused by cells that generate erythroid or megakaryocytic platelets, or cells that make red blood cells.
Knowing the subtype of acute myeloid leukemia is crucial since it can influence a patient's prognosis as well as the best therapy options. The acute promyelocytic leukemia (APL) subtype, for example, is frequently treated with medicines that aren't utilized for other AML subtypes. If you're not sure which subtype of Acute myeloid leukemia you have, talk to your doctor about it and how it may influence your treatment options.
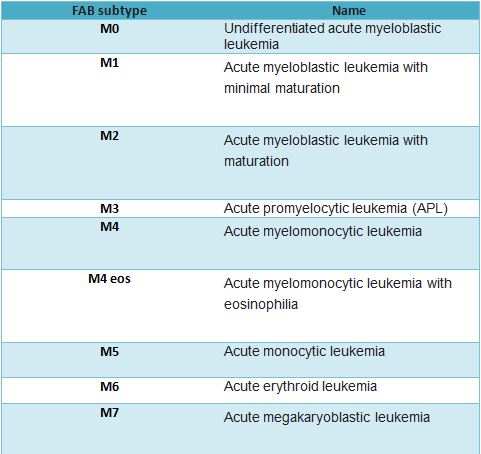
The French-American-British (FAB) classification and the updated World Health Organization (WHO) classification are two of the most often used classifications to divide AML into subtypes.
| S. no. | FAB sub-types | Name |
| 1. | M0 | Undifferentiated acute myeloblastic leukemia |
| 2. | M1 | Acute myeloblastic leukemia with minimal maturation |
| 3. | M2 | Acute myeloblastic leukemia with maturation |
| 4. | M3 | Acute promyelocytic leukemia (APL) |
| 5. | M4 | Acute myelomonocytic leukemia |
| 6. | M4 eos | Acute myelomonocytic leukemia with eosinophilia |
| 7. | M5 | Acute monocytic leukemia |
| 8. | M6 | Acute erythroid leukemia |
| 9. | M7 | Acute megakaryoblastic leukemia |
The categorization of AML by the World Health Organization (WHO) is as follows:
Although the FAB categorization system is useful, it ignores many of the variables that are now known to influence prognosis (outlook). Some of these characteristics are included in the World Health Organization (WHO) classification, which was most recently revised in 2016, in an attempt to properly define AML.
The WHO classifies AML into many categories: Certain genetic anomalies in AML (gene or chromosome changes)
Changes in AML caused by myelodysplasia
AML caused by chemotherapy or radiation treatments in the past
If acute myeloid leukemia isn't mentioned otherwise (This is comparable to the FAB categorization and covers instances with AML that do not fit into one of the aforementioned categories.)
Undifferentiated and biphenotypic acute leukemias are leukemias that contain both lymphocytic and myeloid characteristics but are not exclusively AML. Acute leukemias with mixed phenotypes are also known as mixed phenotype acute leukemias (MPALs)
Cytogenic:
The cytogenetic (chromosome) alterations identified in leukemia cells are also used to classify the disease. The appearance of AML cells and certain chromosomal alterations are closely linked. More significantly, chromosomal alterations may sometimes indicate how well intense treatment will work, which aids doctors in determining the best treatment options. The chance that therapy will work against the subtype of AML is typically classified by chromosomal abnormalities.
From 1 to 22, all chromosomes are numbered. The letters "p" and "q" relate to the "arms" or particular regions of the chromosome, whereas "X" and "Y" allude to sex chromosomes. AML is associated with a variety of genetic alterations, including:
The following are some of the most prevalent chromosomal changes:
Favorable. Abnormalities of chromosome 16 at bands p13 and q22 [t(16;16)(p13;q22), inv(16)(p13q22)] have been linked to better treatment outcomes. and a translocation [t(8;21)] between chromosomes 8 and 21.
Normal chromosomes with no alterations and a translocation between chromosomes 9 and 11 [t(9;11)] are two changes linked with a poor prognosis. Many additional subtypes, particularly those with one or more unique molecular alterations, are included in this category. Extra copies of chromosome 8 or trisomy 8 are sometimes classed as an intermediate risk compared to unfavorable risk (see below).
Unfavorable: Extra copies of chromosomes 8 or 13 [for example, trisomy 8 (+8)], deletion of all or part of chromosomes 5 or 7, complicated alterations on multiple chromosomes, and changes to chromosome 3 at band q26 are examples of chromosomal variations linked with less effective therapy or a poor likelihood of curing AML.
In general, positive changes are more prevalent in younger individuals, whereas negative changes are more likely in persons over 60. In each of these groups, the effectiveness of therapy still varies greatly. Treatment is effective in the long run for 50% to 60% of patients younger than 60 with favorable AML and fewer than 10% of patients younger than 60 with unfavorable AML. Patients above the age of 60 have a considerably poorer prognosis. Other parameters, such as the number of white blood cells, influence how effective therapy works. It's impossible to know with certainty how likely a person's treatment will be effective.
Rishi Kapoor's Incident:
This is ending up being an unfriendly circumstance for the nation and the Film Industry. Yesterday Irfan Khan and today Rishi Kumar, both nailed somewhere around a similar foe. Rishi Kapoor was an on-screen character who had gotten various honors in his career from being granted National Film Award for Best Child Artist for debut in Mera Naam Joker to winning Lifetime Achievement.
Award for the critical commitments he has made to the Hindi Film Industry. An on-screen character who was known for his glamourous career lost the fight against Acute Myeloid Leukaemia at the age of 67.
know more about it
https://zenonco.io/cancer/rishi-kapoor-acute-myeloid-leukaemia/