Iris prolapse during cataract surgery (Figure 1) can lead to significant visual disability because it can result in iris transillumination defects, polycoria, partial mydriasis, and iridodialysis. These defects disrupt the iris’ ability to regulate the amount of light entering the eye (Figures 2–4). Patients with iris defects frequently complain of edge glare, halos, foggy vision, and washed-out images due to overexposure of the retina.
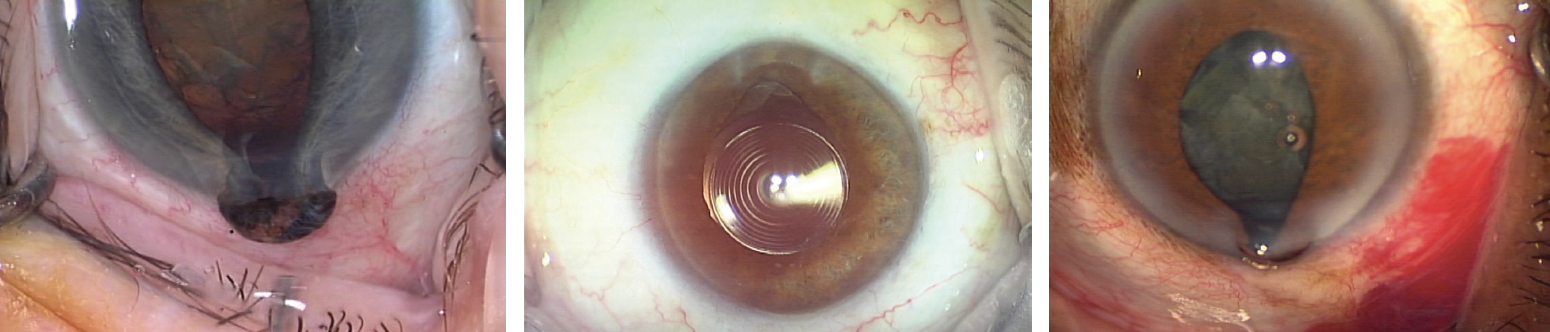
Figure 1. Examples of iris prolapse during cataract surgery.
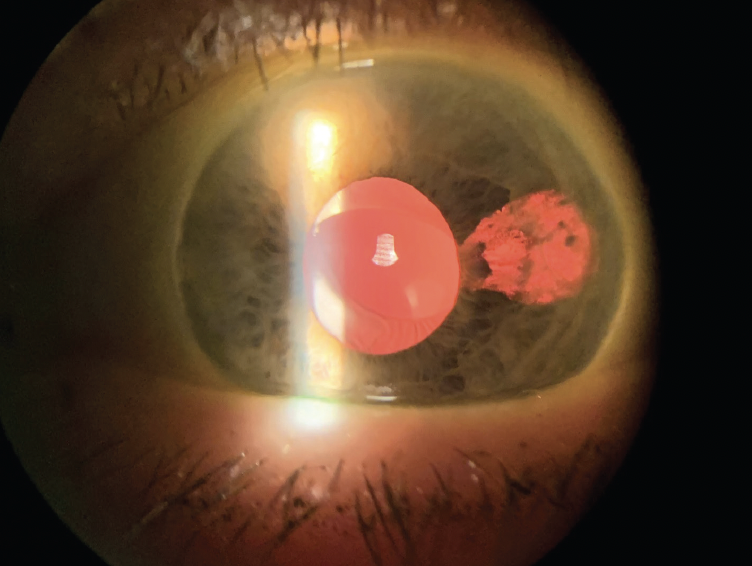
Figure 2. Subincisional iris transillumination defect.
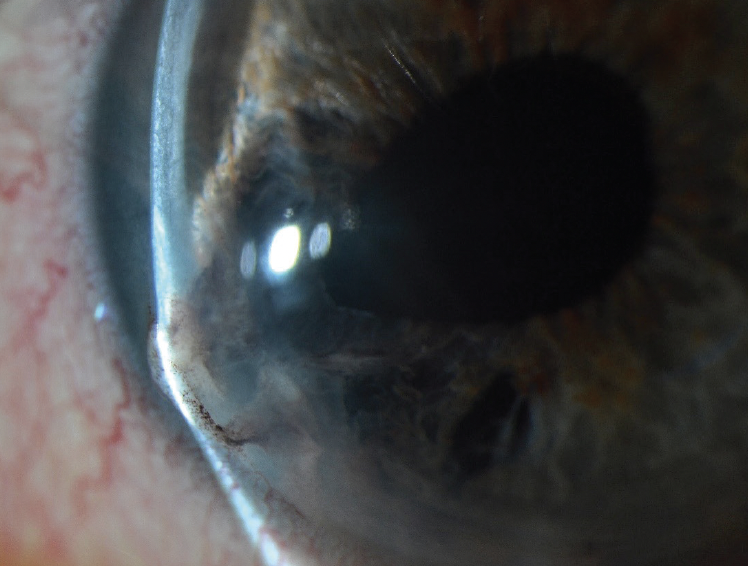
Figure 3. Iris extruding through the cataract incision, partial mydriasis, and transillumination defect.
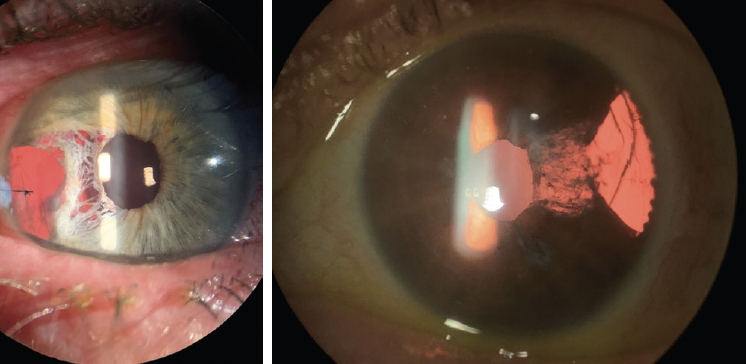
Figure 4. Transillumination defect, partial mydriasis, and iridodialysis.
The potential for iris prolapse exists during several steps of cataract surgery, but all occurrences arise from a sequential triad of elements I refer to as Hart’s triad. The elements are (1) a floppy iris, (2) wound gape, and (3) rapid outflow. They are the sine qua non of iris prolapse. Control any element of the triad completely, and iris prolapse cannot occur.
There are two important corollaries to the triad of iris prolapse. First, a floppy iris goes with the flow. As the pupil becomes progressively miotic, more of the iris is exposed to turbulence within the anterior chamber, akin to the effect of raising the sails on a sailboat on a windy day. Second, the closer the iris is located to the internal opening of the incisions, the more likely iris prolapse becomes. A patient with a shallow anterior chamber and a floppy iris is at much higher risk of iris prolapse than someone with a deep anterior chamber.
RISK FACTORS
The use of alpha blockers increases the risk of a floppy iris during cataract surgery. A negative history of the therapy does not rule out exposure to alpha blockers. I always suspect exposure in patients who report a history of prostate issues (including surgery) or urinary retention. Tamsulosin is routinely prescribed for kidney stones, prostatitis, and female voiding dysfunction. Numerous other drugs, moreover, have alpha-blocking activity.
Because the patient history cannot always predict who will develop intraoperative floppy iris syndrome (IFIS), recognizing its early clinical signs is important. A poorly dilating pupil despite maximal mydriatic drops is often the first clue. In this situation, fluid—usually Shugarcaine (9 mL BSS Plus [Alcon], 3 mL 4% nonpreserved lidocaine, and 4 mL 1:1000 bisulfite-free epinephrine)—may be directed at the pupillary margin at the outset of surgery. If the maneuver elicits iris billowing, IFIS can be expected throughout the case.
The relationship between the pupillary margin, iris, and internal openings of the incisions is crucial during hydrodissection—the first step when iris prolapse is likely to occur. Hydrodissection creates a pocket of balanced salt solution behind the cataract, causing the lens to prolapse anteriorly. Anterior displacement of the lens results in sudden shallowing of the anterior chamber followed immediately by the rapid outflow of OVD through the gaping incision. If the iris is floppy and in close proximity to the incision, iris prolapse can result. If iris prolapse is not recognized early and appropriately resolved, massive iris prolapse may result (watch a related video below).
Reversal of early iris prolapse during hydrodissection involves depressing the lens to release the fluid pocket from behind the cataract. This maneuver deepens the anterior chamber, moving the iris away from the internal openings of the incisions. After the anterior chamber has deepened, and iris prolapse is reversed, cataract surgery may proceed without the risk of iris prolapse as long as at least one of the three elements of the triad is under control (watch a related video below).
MANAGING THE TRIAD OF IRIS PROLAPSE
Unfortunately, no single method can control IFIS during every step of cataract surgery. Understanding how to control all three elements of the triad is therefore critical to reducing the chances of iris prolapse.
A floppy iris. As phacoemulsification proceeds, OVD erodes from the surface of the iris. When the unsupported iris is exposed to turbulence, the pupil initially responds with rapidly alternating dilation and constriction. With greater loss of OVD and exposure to turbulence, the iris starts to billow and then undergoes progressive miosis. A floppy iris may be managed in three ways (see Three Ways to Manage a Floppy Iris).
Wound gape. The incision gapes whenever an instrument that is smaller than the wound is inserted into the anterior chamber. Proper wound architecture is therefore crucial. If the incision is too large, it may be closed to the appropriate size with sutures. Poorly constructed wounds leak fluid excessively, destabilizing the anterior chamber and worsening IFIS by eroding OVD from the surface of the iris.
Poorly constructed wounds may also gape with high or low IOP because they are not self-sealing.
An often unrecognized, transient cause of wound gape is the introduction or removal of the tapered tip of a coaxial instrument into or from the main incision.
Rapid outflow. In the presence of a floppy iris, wound gape can occur without iris prolapse if outflow is not rapid. Rapid outflow, however, most often results from rapid inflow into the eye and frequently occurs during hydrodissection or irrigation with a coaxial instrument (I/A or phaco tip) as it enters or exits the main incision. Rapid outflow can also occur owing to patient Valsalva maneuvers or a suprachoroidal hemorrhage. These are the points during cataract surgery when iris prolapse is most likely to occur.
One way to control rapid outflow is to avoid performing irrigation as a coaxial instrument enters or exits the main incision. Instead, irrigation begins only when the tapered portion of the irrigation sleeve is completely within the anterior chamber. A second method is to wait 1 full second in position 0 (no irrigation into the eye) before removing a coaxial instrument from the eye. This allows fluid to leak in a controlled way around the instrument, thereby reducing the pressure in the anterior chamber. If there is little or no outflow pressure, the iris will not prolapse.
No-touch iris repositioning. Iris prolapse occurs occasionally despite a cataract surgeon’s best efforts. Most often, damage to the iris is caused not by iris prolapse alone but by pushing or sweeping the iris with instruments in an effort to reposition the iris within the eye (Figure 5). The keys to avoiding iris trauma after iris prolapse are creating negative pressure in the anterior chamber and avoiding touching the prolapsed iris with any instrument.
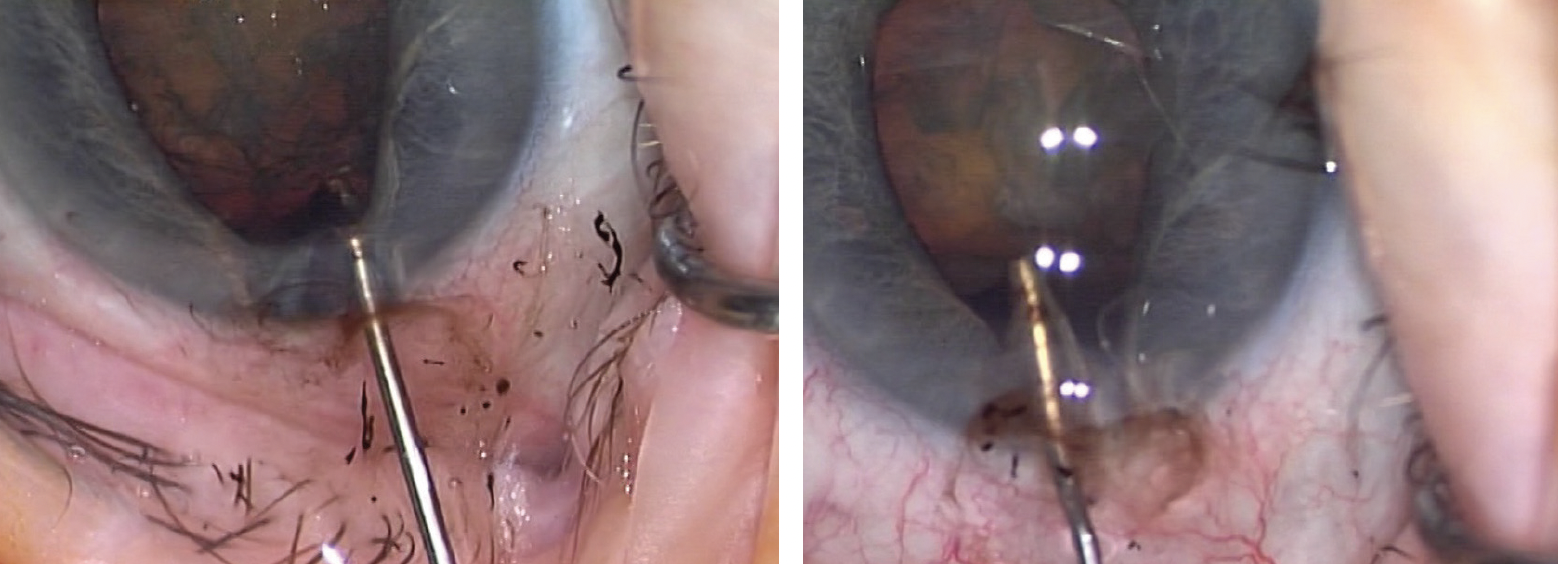
Figure 5. Pigment loss caused by pushing the iris with an instrument.
Creating negative pressure in the anterior chamber changes the direction of flow through the wound. When a prolapsed iris is exposed to negative pressure in the anterior chamber, the iris goes with the flow and moves back into its natural position without loss of pigment or pupillary function. Negative pressure can be created in the anterior chamber by aspirating aqueous through a paracentesis. Because the incisions are self-sealing, the iris may remain slightly trapped within the cornea. Gentle irrigation outside of the wound against the incarcerated tissue will release it without causing iris damage. The important point is to avoid touching the prolapsed iris with an instrument (watch a related video below).
CONCLUSION
The three sequential elements of iris prolapse are a floppy iris, wound gape, and rapid outflow. Controlling any element of the triad completely with the methods described here will prevent iris prolapse from occurring. If iris prolapse does occur, a no-touch iris repositioning technique can prevent iatrogenic iris trauma.