Abstract
Purpose
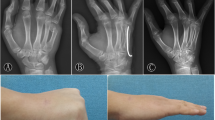
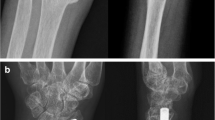
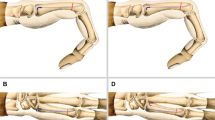
The purpose of this study was to evaluate the radiological and clinical outcomes of treatment of comminuted open fractures of the metacarpal bone (MCB) with associated injuries to soft tissues, tendons, and neurovascular structures using antegrade intramedullary nailing (AIN) at least 2 years postoperatively.
Methods
Between January 2008 and December 2017, a total of 27 patients who met the inclusion/exclusion criteria were included in this study. The inclusion criterion was open and comminuted fracture (with/without segmental bone defects). We evaluated simple radiograph and computed tomography (CT) findings and clinical conditions (visual analog scale [VAS] pain score and Disabilities of the Arm, Shoulder, and Hand [DASH] score), including active range of motion (ROM) at metacarpophalangeal joint (MP) and grip strength at final follow-up.
Results
The mean preoperative angulation was 29.63° ± 7.59° and the mean shortening was 9.30 ± 2.38 mm. Union was achieved at mean 12.3 weeks postoperatively, without any complications due to operative treatment. The dorsal angulation measured on the CT scans, shortening on simple radiographs was significantly improved (10.26 °± 3.19°, 0.52 ± 1.05 mm, respectively). The final VAS and DASH scores were 0.41 ± 0.64 and 3.6 ± 2.47, respectively, indicating satisfactory outcomes. The final ROM was 85.0° ± 3.67°. The mean final grip strength was 89.56 ± 5.69% relative to the normal side. A mean extension lag at the MP joint of 12° was noted in three patients; however, it was resolved by additional tenolysis.
Conclusions
AIN is a simple method for fixation of open comminuted metacarpal fractures accompanied by soft tissue injury. The simplicity of the method is beneficial for repairing associated injured structures and healing soft tissue. Minimized additional damage around the MCB during surgery and good stability resulted in satisfactory bony union with minimal angulation, shortening, and rotation.
Level of evidence
Level IV, Retrospective case series.



Similar content being viewed by others
References
Feehan LM, Sheps SB (2006) Incidence and demographics of hand fractures in British Columbia, Canada: a population-based study. J Hand Surg Am 31:1068–1074
Gajendran VK, Szabo RM, Myo GK et al (2009) Biomechanical comparison of double-row locking plates versus single- and double-row non-locking plates in a comminuted metacarpal fracture model. J Hand Surg Am 34:1851–1858
Kollitz KM, Hammert WC, Vedder NB et al (2014) Metacarpal fractures: treatment and complications. Hand (NY) 9:16–23
Sohn RC, Jahng KH, Curtiss SB et al (2008) Comparison of metacarpal plating methods. J Hand Surg Am 33:316–321
Hohendorff B, Unglaub F, Spies CK, Wegmann K, Müller LP, Ries C (2019) Operative Zugangswege an der Hand [Surgical approaches to the hand]. Oper Orthop Traumatol 31(5):372–383. https://doi.org/10.1007/s00064-019-0622-8 (Epub 2019 Jul 29. PMID: 31359070; in German)
Firoozbakhsh KK, Moneim MS, Howey T et al (1993) Comparative fatigue strengths and stabilities of metacarpal internal fixation techniques. J Hand Surg Am 18:1059–1068
Mann RJ, Black D, Constine R et al (1985) A quantitative comparison of metacarpal fracture stability with five different methods of internal fixation. J Hand Surg Am 10:1024–1028
Vanik RK, Weber RC, Matloub HS et al (1984) The comparative strengths of internal fixation techniques. J Hand Surg Am 9:216–221
Spies CK, Langer M, Hohendorff B, Müller LP, Oppermann J, Unglaub F (2019) Offene Reposition und Schrauben-/Plattenosteosynthese von Mittelhandfrakturen [Open reduction and screw/plate osteosynthesis of metacarpal fractures]. Oper Orthop Traumatol 31(5):422–432. https://doi.org/10.1007/s00064-019-00625-y (Epub 2019 Sep 5. PMID: 31486853; German)
Aykut S, Öztürk K, Özcan Ç et al (2015) Results of surgical treatment in metacarpal shaft fractures using low profile mini plates. Ulus Travma Acil Cerrahi Derg 21:279–284. https://doi.org/10.5505/tjtes.2015.01651
Cha SM, Shin HD, Kim YK (2019) Comparison of low-profile locking plate fixation versus antegrade intramedullary nailing for unstable metacarpal shaft fractures—a prospective comparative study. Injury 50:2252–2258. https://doi.org/10.1016/j.injury.2019.10.018 (Epub 2019 Oct 7)
Cha SM, Shin HD (2018) Antegrade intramedullary pinning in subacute fifth metacarpal neck fracture after failed conservative treatment: a prospective comparative study with acute fracture. Ann Plast Surg 80:347–352. https://doi.org/10.1097/SAP.0000000000001265
Bland JM, Altman DG (1999) Measuring agreement in method comparison studies. Stat Methods Med Res 8:135–160
Beaton DE, Davis AM, Hudak P et al (2001) The DASH (disabilities of the arm, shoulder, and hand) outcome measure: What do we know about it now? Br J Hand Ther 6:109–118
Doro C, Hayden RJ, Louis DS (2006) Complex regional pain syndrome type I in the upper extremity. Clin Occup Environ Med 5:445–454
Norris BL, Lang G, Russell TAT et al (2018) Absolute versus relative fracture fixation: impact on fracture healing. J Orthop Trauma 32(Suppl 1):S12–S16. https://doi.org/10.1097/BOT.0000000000001124
Ring D (2006) Malunion and nonunion of the metacarpals and phalanges. Instr Course Lect 55:121–128 (Review)
Yamagiwa H, Endo N (2009) Bone fracture and the healing mechanisms. Histological aspect of fracture healing. Primary and secondary healing. Clin Calcium 19:627–633
Mirza A, Mirza J, Healy C et al (2018) Radiographic and clinical assessment of intramedullary nail fixation for the treatment of unstable metacarpal fractures. Hand (NY) 13(2):184–189. https://doi.org/10.1177/1558944717695747 (Epub 2017 Mar 15)
Dreyfuss D, Allon R, Izacson N et al (2019) A comparison of locking plates and intramedullary pinning for fixation of metacarpal shaft fractures. Hand (NY) 14(1):27–33. https://doi.org/10.1177/1558944718798854 (Epub 2018 Sep 7. PMID: 30192648; PMCID: PMC6346363)
Rocchi L, Merendi G, Mingarelli L et al (2018) Antegrade percutaneous intramedullary fixation technique for metacarpal fractures: prospective study on 150 cases. Tech Hand Up Extrem Surg 22(3):104–109. https://doi.org/10.1097/BTH.0000000000000198 (PMID: 29889155)
Eisenschenk A, Spitzmüller R, Güthoff C et al (2019) Single versus dual Kirschner wires for closed reduction and intramedullary nailing of displaced fractures of the fifth metacarpal neck (1–2 KiWi): a randomized controlled trial. Bone Joint J 101-B(10):1263–1271. https://doi.org/10.1302/0301-620X.101B10.BJJ-2019-0410.R1 (PMID: 31564142)
Chen KJ, Wang JP, Yin CY et al (2020) Fixation of fifth metacarpal neck fractures: a comparison of medial locking plates with intramedullary K-wires. J Hand Surg Eur 45(6):567–573. https://doi.org/10.1177/1753193419896518 (Epub 2020 Jan 14. PMID: 31937179)
Lazarus P, Hidalgo Diaz JJ, Xaxier F et al (2020) Transverse and oblique fractures of the diaphysis of the fifth metacarpal: surgical outcomes for antegrade intramedullary pinning versus combined antegrade and retrograde intramedullary pinning. Eur J Orthop Surg Traumatol 30(3):425–433. https://doi.org/10.1007/s00590-019-02587-0 (Epub 2019 Oct 30. PMID: 31667582)
Wood AM, Robertson GAJ, MacLeod K et al (2017) Epidemiology of open fractures in sport: one centre’s 15-year retrospective study. World J Orthop 8(7):545–552. https://doi.org/10.5312/wjo.v8.i7.545 (PMID: 28808625; PMCID: PMC5534403)
Tulipan JE, Ilyas AM (2016) Open fractures of the hand: review of pathogenesis and introduction of a new classification system. Orthop Clin North Am 7(1):245–251. https://doi.org/10.1016/j.ocl.2015.08.021 (PMID: 26614938)
Kamath JB, Jayasheelan N, Savur A et al (2016) Outcome of unstable fractures of metacarpal and phalangeal bones treated by bone tie. Indian J Orthop 50(3):316–321. https://doi.org/10.4103/0019-5413.181796 (PMID: 27293294; PMCID: PMC4885302)
Perren SM, Fernandez Dell’oca A, Regazzoni P (2017) Evolution of AO fracture treatment part 1: the internal fixator. Acta Chir Orthop Traumatol Cech 84(6):413–417 (PMID: 29351522)
Halawi MJ, Morwood MP (2015) Acute management of open fractures: an evidence-based review. Orthopedics 38(11):e1025–e1033. https://doi.org/10.3928/01477447-20151020-12
Drenth DJ, Klasen HJ (1998) External fixation for phalangeal and metacarpal fractures. J Bone Joint Surg Br 80(2):227–230
Pennig D, Gausepohl T, Mader K et al (2000) The use of minimally invasive fixation in fractures of the hand–the minifixator concept. Injury 31(Suppl 1):102–112
Shehadi SI (1991) External fixation of metacarpal and phalangeal fractures. J Hand Surg Am 16(3):544–550
Sochart DH, Paul AS (1995) A simple external fixator for use in metacarpal and phalangeal fractures: a technique paper. J Orthop Trauma 9(4):333–335
Funding
This work was supported by the research fund of Chungnam National University Hospital, 2019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by our institutional review board.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cha, S.M., Kang, J.W., Shin, H.D. et al. Antegrade intramedullary nailing in comminuted, open metacarpal bone fracture: maintenance of the length. Arch Orthop Trauma Surg 141, 1815–1823 (2021). https://doi.org/10.1007/s00402-021-03960-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03960-7