Acne
Definition
Acne is a common skin disease characterized by pimples on the face, chest, and back. It occurs when the pores of the skin become clogged with oil, dead skin cells, and bacteria.
Description
Acne vulgaris, the medical term for common acne, is the most common skin disease. It affects nearly 17 million people in the United States. While acne can arise at any age, it usually begins at
puberty and worsens during adolescence. Nearly 85% of people develop acne at some time between the ages of 12-25 years. Up to 20% of women develop mild acne. It is also found in some newborns.
The sebaceous glands lie just beneath the skin's surface. They produce an oil called sebum, the skin's natural moisturizer. These glands and the hair follicles within which they are found are called sebaceous follicles. These follicles open onto the skin through pores. At puberty, increased levels of androgens (male hormones) cause the glands to produce too much sebum. When excess sebum combines with dead, sticky skin cells, a hard plug, or comedo, forms that blocks the pore. Mild noninflammatory acne consists of the two types of comedones, whiteheads and blackheads.
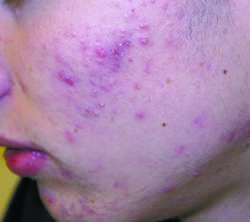
Moderate and severe inflammatory types of acne result after the plugged follicle is invaded by Propionibacterium acnes, a bacteria that normally lives on the skin. A pimple forms when the damaged follicle weakens and bursts open, releasing sebum, bacteria, and skin and white blood cells into the surrounding tissues. Inflamed pimples near the skin's surface are called papules; when deeper, they are called pustules. The most severe type of acne consists of cysts (closed sacs) and nodules (hard swellings). Scarring occurs when new skin cells are laid down to replace damaged cells.
The most common sites of acne are the face, chest, shoulders, and back since these are the parts of the body where the most sebaceous follicles are found.
Causes and symptoms
The exact cause of acne is unknown. Several risk factors have been identified:
- Age. Due to the hormonal changes they experience, teenagers are more likely to develop acne.
- Gender. Boys have more severe acne and develop it more often than girls.
- Disease. Hormonal disorders can complicate acne in girls.
- Heredity. Individuals with a family history of acne have greater susceptibility to the disease.
- Hormonal changes. Acne can flare up before menstruation, during pregnancy, and menopause.
- Diet. No foods cause acne, but certain foods may cause flare-ups.
- Drugs. Acne can be a side effect of drugs including tranquilizers, antidepressants, antibiotics, oral contraceptives, and anabolic steroids.
- Personal hygiene. Abrasive soaps, hard scrubbing, or picking at pimples will make them worse.
- Cosmetics. Oil-based makeup and hair sprays worsen acne.
- Environment. Exposure to oils and greases, polluted air, and sweating in hot weather aggravate acne.
- Stress. Emotional stress may contribute to acne.
Acne is usually not conspicuous, although inflamed lesions may cause
pain, tenderness,
itching, or swelling. The most troubling aspects of these lesions are the negative cosmetic effects and potential for scarring. Some people, especially teenagers, become emotionally upset about their condition, and have problems forming relationships or keeping jobs.
Diagnosis
Acne patients are often treated by family doctors. Complicated cases are referred to a dermatologist, a skin disease specialist, or an endocrinologist, a specialist who treats diseases of the body's endocrine (hormones and glands) system.
Key terms
Androgens — Male sex hormones that are linked with the development of acne.
Comedo — A hard plug composed of sebum and dead skin cells. The mildest type of acne.
Comedolytic — Drugs that break up comedones and open clogged pores.
Corticosteroids — A group of hormones produced by the adrenal glands with different functions, including regulation of fluid balance, androgen activity, and reaction to inflammation.
Estrogens — Hormones produced by the ovaries, the female sex glands.
Isotretinoin — A drug that decreases sebum production and dries up acne pimples.
Sebaceous follicles — A structure found within the skin that houses the oil-producing glands and hair follicles, where pimples form.
Sebum — An oily skin moisturizer produced by sebaceous glands.
Tretinoin — A drug that works by increasing the turnover (death and replacement) of skin cells.
Acne has a characteristic appearance and is not difficult to diagnose. The doctor takes a complete medical history, including questions about skin care, diet, factors causing flare-ups, medication use, and prior treatment.
Physical examination includes the face, upper neck, chest, shoulders, back, and other affected areas. Under good lighting, the doctor determines what types and how many blemishes are present, whether they are inflamed, whether they are deep or superficial, and whether there is scarring or skin discoloration.
In teenagers, acne is often found on the forehead, nose, and chin. As people get older, acne tends to appear towards the outer part of the face. Adult women may have acne on their chins and around their mouths. The elderly may develop whiteheads and blackheads on the upper cheeks and skin around the eyes.
Laboratory tests are not done unless the patient appears to have a hormonal disorder or other medical problem. In this case, blood analyses or other tests may be ordered. Most insurance plans cover the costs of diagnosing and treating acne.
Treatment
Acne treatment consists of reducing sebum production, removing dead skin cells, and killing bacteria with topical drugs and oral medications. Treatment choice depends upon whether the acne is mild, moderate, or severe.
Drugs
TOPICAL DRUGS. Treatment for mild noninflammatory acne consists of reducing the formation of new comedones with topical tretinoin, benzoyl peroxide, adapalene, or salicylic acid. Tretinoin is especially effective because it increases turnover (death and replacement) of skin cells. When complicated by inflammation, topical antibiotics may be added to the treatment regimen. Improvement is usually seen in two to four weeks.
Topical medications are available as cream, gel, lotion, or pad preparations of varying strengths. They include
antibiotics (agents that kill bacteria), such as erythromycin, clindamycin (Cleocin-T), and meclocycline (Meclan); comedolytics (agents that loosen hard plugs and open pores) such as the vitamin A acid tretinoin (Retin-A), salicylic acid, adapalene (Differin), resorcinol, and sulfur. Drugs that act as both comedolytics and antibiotics, such as benzoyl peroxide, azelaic acid (Azelex), or benzoyl peroxide plus erythromycin (Benzamycin), are also used. These drugs may be used for months to years to achieve disease control.
After washing with mild soap, the drugs are applied alone or in combination, once or twice a day over the entire affected area of skin. Possible side effects include mild redness, peeling, irritation, dryness, and an increased sensitivity to sunlight that requires use of a sunscreen.
ORAL DRUGS. Oral antibiotics are taken daily for two to four months. The drugs used include tetracycline, erythromycin, minocycline (Minocin), doxycycline, clindamycin (Cleocin), and trimethoprim-sulfamethoxazole (Bactrim, Septra). Possible side effects include allergic reactions, stomach upset, vaginal yeast infections,
dizziness, and tooth discoloration.
The goal of treating moderate acne is to decrease inflammation and prevent new comedone formation. One effective treatment is topical tretinoin along with a topical or oral antibiotic. A combination of topical benzoyl peroxide and erythromycin is also very effective. Improvement is normally seen within four to six weeks, but treatment is maintained for at least two to four months.
A drug reserved for the treatment of severe acne, oral isotretinoin (Accutane), reduces sebum production and cell stickiness. It is the treatment of choice for severe acne with cysts and nodules, and is used with or without topical or oral antibiotics. Taken for four to five months, it provides long-term disease control in up to 60% of patients. If the acne reappears, another course of isotretinoin may be needed by about 20% of patients, while another 20% may do well with topical drugs or oral antibiotics. Side effects include temporary worsening of the acne, dry skin, nosebleeds, vision disorders, and elevated liver enzymes, blood fats and cholesterol. This drug must not be taken during pregnancy since it causes
birth defects.
Anti-androgens, drugs that inhibit androgen production, are used to treat women who are unresponsive to other therapies. Certain types of oral contraceptives (for example, Ortho-Tri-Cyclen) and female sex hormones (estrogens) reduce hormone activity in the ovaries. Other drugs, for example, spironolactone and corticosteroids, reduce hormone activity in the adrenal glands. Improvement may take up to four months.
Oral
corticosteroids, or anti-inflammatory drugs, are the treatment of choice for an extremely severe, but rare type of destructive inflammatory acne called acne fulminans, found mostly in adolescent males. Acne conglobata, a more common form of severe inflammation, is characterized by numerous, deep, inflammatory nodules that heal with scarring. It is treated with oral isotretinoin and corticosteroids.
Other treatments
Several surgical or medical treatments are available to alleviate acne or the resulting scars:
- Comedone extraction. The comedo is removed from the pore with a special tool.
- Chemical peels. Glycolic acid is applied to peel off the top layer of skin to reduce scarring.
- Dermabrasion. The affected skin is frozen with a chemical spray, and removed by brushing or planing.
- Punch grafting. Deep scars are excised and the area repaired with small skin grafts.
- Intralesional injection. Corticosteroids are injected directly into inflamed pimples.
- Collagen injection. Shallow scars are elevated by collagen (protein) injections.
Alternative treatment
Alternative treatments for acne focus on proper cleansing to keep the skin oil-free; eating a well-balanced diet high in fiber, zinc, and raw foods; and avoiding alcohol, dairy products, smoking,
caffeine, sugar, processed foods, and foods high in iodine, such as salt. Supplementation with herbs such as burdock root (
Arctium lappa), red clover (
Trifolium pratense), and milk thistle (
Silybum marianum), and with nutrients such as essential fatty acids, vitamin B complex, zinc, vitamin A, and chromium is also recommended. Chinese herbal remedies used for acne include cnidium seed (
Cnidium monnieri) and honeysuckle flower (
Lonicera japonica). Wholistic physicians or nutritionists can recommend the proper amounts of these herbs.
Prognosis
Acne is not curable, although long-term control is achieved in up to 60% of patients treated with isotretinoin. It can be controlled by proper treatment, with improvement taking two or more months. Acne tends to reappear when treatment stops, but spontaneously improves over time. Inflammatory acne may leave scars that require further treatment.
Prevention
There are no sure ways to prevent acne, but the following steps may be taken to minimize flare-ups:
- gentle washing of affected areas once or twice every day
- avoid abrasive cleansers
- use noncomedogenic makeup and moisturizers
- shampoo often and wear hair off face
- eat a well-balanced diet, avoiding foods that trigger flare-ups
- unless told otherwise, give dry pimples a limited amount of sun exposure
- do not pick or squeeze blemishes
- reduce stress
Resources
Periodicals
Billings, Laura. "Getting Clear." Health Magazine (April 1997): 48-52.
Organizations
American Academy of Dermatology. 930 N. Meacham Road, P.O. Box 4014, Schaumburg, IL 60168-4014. (847) 330-0230. Fax: (847) 330-0050. http://www.aad.org.
Gale Encyclopedia of Medicine. Copyright 2008 The Gale Group, Inc. All rights reserved.
acne
[ak´ne] a disorder of the skin with eruption of papules or pustules; more particularly,
acne vulgaris.
acne congloba´ta (conglobate acne) severe acne, seen almost exclusively in males, with many comedones, marked by suppuration, cysts, sinuses, and scarring.
cystic acne acne with the formation of cysts enclosing a mixture of keratin and sebum in varying proportions.
acne ful´minans a rare form of severe
cystic acne seen in teenage boys, characterized by highly inflammatory nodules and plaques that undergo suppurative degeneration leaving ulcerations, fever, weight loss, anemia, leukocytosis, elevated erythrocyte sedimentation rate, and polyarthritis.
acne indura´ta a progression of papular acne, with deep-seated and destructive lesions that may produce severe scarring.
acne necro´tica milia´ris a rare and chronic form of folliculitis of the scalp, occurring principally in adults, with formation of tiny superficial pustules that are destroyed by scratching. See also
acne varioliformis.
acne neonato´rum acne vulgaris in infants, usually in males before 3 months of age, chiefly characterized by papules, pustules, and open and closed comedones on the face; it is thought to be due to hormonal stimulation of sebaceous glands. The affected child may be predisposed to more severe acne in adolescence.
acne papulo´sa acne vulgaris with the formation of papules.
acne rosa´cea a form of acne in which the skin around each pustule is a rosy red; it is usually seen in persons over 25 years of age and is often psychogenic.
tropical acne (
acne tropica´lis) a severe type of
acne vulgaris seen in the tropics when the weather is hot and humid, characterized by large painful cysts, nodules, and pustules that lead to the formation of rounded abscesses and frequent scarring and tend to localize on the back, nape of the neck, buttocks, thighs, and upper arms and usually sparing the face. It tends to affect those who have had acne vulgaris at an earlier age.
acne variolifor´mis a rare condition with reddish-brown, papulopustular umbilicated lesions, usually on the brow and scalp; probably a deep variant of acne necrotica miliaris.
acne venena´ta acne produced by contact with any of numerous chemicals, including those used in cosmetic and grooming agents and in industry.
acne vulga´ris a chronic skin disorder usually seen in adolescents and young adults, in which there is increased production of sebum (oil) from the sebaceous glands and formation of
comedones (blackheads and
whiteheads) that plug the pores. Noninflammatory acne produces plugged follicles and a few pimples. Inflammatory acne is characterized by many pimples, pustules, nodules, and inflamed cysts. The lesions are found on the face, neck, chest, back, and shoulders.
Treatment. The noninflammatory lesions often respond to over-the-counter creams and lotions, but inflammatory lesions may require intensive and individualized medical treatment under the direction of a dermatologist. Acne is treated by both topical and systemic drugs; the one most frequently recommended is
benzoyl peroxide in a 5 or 10 per cent concentration. It is applied to the skin daily or as frequently as necessary to produce mild dryness of the skin. A mainstay for treatment of inflammatory acne continues to be oral
tetracycline, which is effective for most cases and safe even when taken for years. A relatively new systemic drug for severe, treatment-resistant acne is
isotretinoin (13-
cis-retinoic acid). It inhibits the secretion of sebum and alters the lipid composition of the skin surface. Isotretinoin is a teratogen; hence it is not given to pregnant women. It can also cause bone changes. Minor side effects include dry mouth and dry eyes. Another agent used against acne is
tretinoin (all-
trans-retinoic acid), which is applied topically to reduce the number of comedones and to prevent formation of inflammatory lesions.
Acne therapy can continue for months and even years. Patients who conscientiously follow the prescribed regimen greatly increase their chances for improvement and the prevention of permanent scarring and pitting of the skin.
When acne has left permanent, disfiguring scars, there are medical techniques that can remove or improve the blemishes. One method is planing with a rotary, high-speed brush. This removes the outer layer of pitted skin, leaving the growing layer and the layers containing the glands and hair follicles. New epithelium grows from the layers underneath; it is rosy at first and gradually becomes normal in color. The technique has also been used successfully in removing some types of disfigurations resulting from accidents. This so-called “sand-paper surgery” or dermabrasion is recommended only for selected cases of acne and results are not always satisfying.
Patient Care. Because patients with acne often have a lack of knowledge about the nature of their skin disorder, patient education is a major component of care. Additionally, the disorder often affects young people at a time when they are deeply concerned about their appearance and acceptance by their peers. Adolescents need to know that their concerns are taken seriously. Even though the disorder is not life-threatening, it can adversely affect one's self-image and self-esteem.
Laypersons often are misinformed about the cause and effects of acne. It is not a contagious disease, nor is it due to uncleanliness or poor personal hygiene. It is not caused or made worse by lack of sleep, constipation, masturbation, venereal disease, or by anger or hostility. Dietary indiscretion can sometimes contribute to the appearance of lesions, but there are very few people who can find a cause-effect relationship between certain foods they have eaten and the appearance of acne lesions. In general, cola drinks, chocolate, and fried foods need not be restricted or eliminated from the diet in hopes that acne can be avoided or cured. A well-balanced diet is all that is recommended for the management of acne.
Scrubbing the skin and using harsh soaps is not recommended because this only serves to damage the skin and predispose it to breakdown. A mild soap is as effective as special medicated soaps. If the hair is excessively oily, it may help to shampoo regularly and keep the hair off the face.
Pimples and pustules should not be squeezed. This can press the sebum and accumulated debris more firmly into the clogged duct and increase the chance of inflammation and the spread of infection. Blackheads and whiteheads are best removed by applying a prescription medication that causes peeling of the skin.
Since the management of acne can go on for years, requiring periodic evaluation by a dermatologist, patients and their families will need continued support and encouragement. Patients taking prescription medications will need to know the expected results, any adverse reactions that might occur, their symptoms, and to whom they should be reported.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
acne
(ak'ne) [Ult. fr. acme] An inflammatory disease of the sebaceous follicles of the skin, marked by comedones, papules, and pustules. It is exceptionally common in puberty and adolescence. Acne usually affects the face, chest, back, and shoulders. In severe cases, cysts, nodules, and scarring occur. Synonym:
common acne;
acne vulgarisEtiology
The cause is unknown, but predisposing factors include hereditary tendencies and disturbances in the androgen-estrogen balance. Acne begins at puberty when the increased secretion of androgen in both males and females increases the size and activity of the pilosebaceous glands. Specific inciting factors may include food allergies, endocrine disorders, therapy with adrenal corticosteroid hormones, and psychogenic factors. Vitamin deficiencies, ingestion of halogens, and contact with chemicals such as tar and chlorinated hydrocarbons may be specific causative factors. The fact that bacteria are important once the disease is present is indicated by the successful results following antibiotic therapy. The lesions may become worse in women and girls before the menstrual period.
Symptoms
Acne vulgaris is marked by either papules, comedones with black centers (pustules), or hypertrophied nodules caused by overgrowth of connective tissue. In the indurative type, the lesions are deep-seated and cause scarring. The face, neck, and shoulders are common sites. Acne may be obstinate and recurrent.
Treatment
Treatments include skin cleansing, topical agents (e.g., azelaic acid or benzoyl peroxide or vitamin A derivatives), and oral or topical antibacterial drugs.
Patient care
The patient is instructed to wash the skin thoroughly but gently, avoiding intense scrubbing and skin abrasion; to keep hands away from the face and other sites of lesions; to limit the use of cosmetics; and to observe for, recognize, and avoid or modify predisposing factors that may cause exacerbations. The need to reduce sun exposure is explained, and the patient is advised to use a sunscreen agent when vitamin A acid or tetracycline is prescribed. Information is provided to fill knowledge gaps or correct misconceptions, and emotional support and understanding are offered, particularly if the patient is an adolescent. Patients (and others) need to be aware that extensive use of antibiotic treatment for acne increases the prevalence of antibiotic-resistant facial bacteria and can affect treatment response. Most improvement occurs during the first 6 weeks of therapy, whatever the regimen. More than half of all patients respond to therapy. Colonization with tetracycline-resistant propionibacteria diminishes response to all oral antibiotic regimens. Skin irritation as an adverse effect to treatment occurs most commonly with topical benzoyl peroxide alone, which is the most cost-effective treatment. Adding topical erythromycin may help reduce irritation and increase efficacy.
CAUTION!
Because of the teratogenicity of some acne medications (such as isotretinoin), pregnancy must be avoided during their use.
acne atrophica
Acne with residual pitting and scarring.
bromide acne
The characteristic acne caused by bromide.
acne ciliaris
Acne that affects the edges of the eyelids.
common acne
Acne.acne conglobata
Acne vulgaris with abscesses, cysts, and sinuses that leave scars.
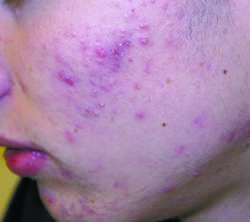

CYSTIC ACNE
cystic acne
Acne with cysts containing keratin and sebum. See:
illustrationTreatment
Isotretinoin, a vitamin A derivative, has been effective in treating this condition. For Caution concerning its use, See: isotretinoin
acne fulminans
A rare type of acne in teenage boys, marked by inflamed, tender, ulcerative, and crusting lesions of the upper trunk and face. It has a sudden onset and is accompanied by fever, leukocytosis, and an elevated sedimentation rate. About half of the cases have inflammation of several joints.
halogen acne
Acne due to exposure to halogens such as bromine, chlorine, or iodine.
acne indurata
Acne vulgaris with chronic, discolored, indurated surfaces.
keloid acne
Acne keloidalis nuchae .acne keloidalis nuchae
Chronic follicular infection of the skin at the occiput (base of the skull) and the neck. It occurs most often in men of African heritage and causes scars and thickening of the skin.
Synonym: keloid acneacne keratosa
Acne in which suppurating nodules crust over to form horny plugs. These occur at the corners of the mouth.
acne neonatorum
Acne occurring in newborns. It is common, appearing about the second to fourth week of life. Comedones, inflamed papules, and pustules may be seen (the latter yield staphylococcal species when cultured). The rash typically resolves spontaneously by the third or fourth month of life. Lesions are typically seen on the chin, cheeks, and forehead. Usually no treatment is required, but keratolytic agents may be used for severe cases.


ACNE PAPULOSA
acne papulosa
Acne characterized by formation of papules with very little inflammation. See: illustration
illustrationpetroleum acne
Acne that may occur in those who work with petroleum and oils.
acne pustulosa
Acne with pustule formation and subsequent deep scars.
acne rosacea
Rosacea.steroid acne
Acne caused by systemic or topical use of corticosteroid drugs.
summer acne
Acne that appears only in hot, humid weather or that is much worse in such weather. Although the exact cause is unknown, the condition is not caused by increased exposure to the sun's rays.
tropical acne
Severe acne caused by or aggravated by living in a hot, humid climate. The skin of the thorax, back, and legs is most commonly affected.
acne urticaria
An acneiform eruption of itching wheals.
acne varioliformis
Vesiculopustular folliculitis that occurs mostly on the temples and frontal margins of the scalp but may be seen on the chest, back, or nose.
acne vulgaris
Acne.Medical Dictionary, © 2009 Farlex and Partners
Patient discussion about acne
Q. what is the best treatment for acne vulgaris
A. The best treatment is what helps the SPECIFIC patients - never forget that treatments have their own side effect, so it's not necessarily the best to start with the strongest (but difficult to tolerate) option.
Generally, the widely used treatment for acne that doesn't respond to local treatment is retinoid, which are different forms of Vitamin A. There are several products, and they should require prescription by a doctor. They have side effects, some of them more problematic, and they require the use of contraceptives, but they are very efficient.
You can read more about it here: http://www.nlm.nih.gov/medlineplus/acne.html#cat3 and here: http://www.skincarephysicians.com/acnenet/treatingmoderatesevereacne.html)
Q. Does cow's milk cause acne? I'm 16 years old guy, and I have acne for several years now. Lately, although I treat it as my dermatologist instructs me, it seems I have more zits, particularly on my face.
My friend told it can be because for the last few months ago I've been drinking a cup of milk for breakfast (I almost didn't drink milk at all before that). Is it true? The acne really makes me miserable, and the last thing I want to do is to make it worse.
Thanks!!!
A. Regardless of what milk does to your acne, emotional stress can also make it worse, so first of all, try to relax- it'll make feel better and can also make your acne better, so it'll make you feel even better. Try to avoid milk for some time and see what helps you most. No one really proved milk has any influence on acne, so you shouldn't feel like you you're responsible for your acne.
Q. I have acne !!!! what can i do? no one looks at me? will it go a way??? i need Answer !!!! Help ! Help !!!! i'm a teenage and i suffer from bad , and i mean , bad Acne !!!! what can i do ? i tried almost everything the pharmacy has to offer and nothing worked , does anyone knows how to deal with bad acne ??? how will i grow through teenage with this ... thing !
someone Help
A. try proactive,a few of my family members use it it works for them.
More discussions about acneThis content is provided by iMedix and is subject to iMedix Terms. The Questions and Answers are not endorsed or recommended and are made available by patients, not doctors.