What are blasts?
Blasts are precursors to the mature, circulating blood cells such as neutrophils, monocytes, lymphocytes and erythrocytes. Blasts are usually found in low numbers in the bone marrow. They are not usually found in significant numbers in the blood.
Why do blasts matter?
Circulating blasts can be seen with severe infections, medications (e.g. granulocyte colony stimulating factor), bone marrow replacing processes and hematopoietic neoplasms.
Acute leukemia is the most important hematopoietic neoplasm to recognize because it can rapidly lead to death. Other hematopoietic neoplasms with circulating blasts include myelodysplastic syndromes and chronic myeloproliferative disorders.
What do blasts look like?
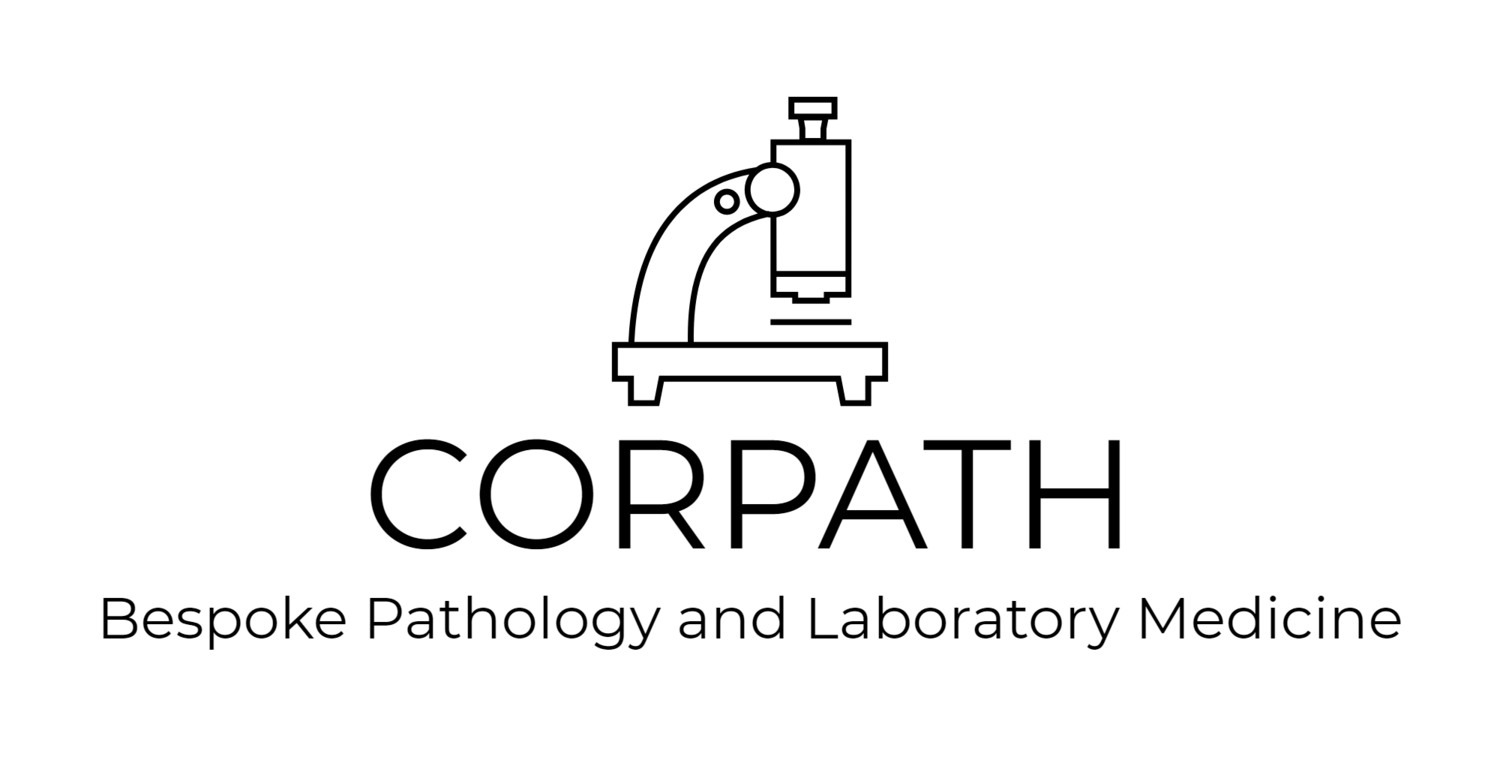
- No single characteristic identifies a blast. In general, blasts are cells that have a large nucleus, immature chromatin, a prominent nucleolus, scant cytoplasm and few or no cytoplasmic granules. Blasts may not have all of these features.
- Cell size - blasts are often medium to large cells. They are usually larger than a lymphocyte and at least the size of a monocyte.
- Large nucleus - most of the cell is taken up by the nucleus (a high nuclear to cytoplasmic ratio).
- Immature chromatin - the nuclear chromatin looks as if it composed of fine dots. One can visualize this chromatin as many tiny points made by the tip of a sharp pencil on a piece of paper. Monocyte chromatin is more linear and dark, looking like smudged pencil lines. Lymphocyte chromatin looks to be colored in heavy crayon.
- Prominent nucleolus.
- Conformable nuclear membrane - the nuclear membrane often conforms to the shape of the cytoplasmic membrane. The nucleus appears squishy. A lymphocyte nucleus appears rigid.
- Scant cytoplasm.
- Few to no cytoplasmic granules - blasts usually lack the numerous granules seen in mature granulocytes. Occasional granules may be present. Acute promyelocytic leukemia is an exception.
- Auer rods - orange-pink, needle-like cytoplasmic structures in blasts of myeloid lineage. These may be numerous in acute promyelocytic leukemia.
Diagnostic Criteria for Acute Leukemia
- 20% of more blasts in the peripheral blood or bone marrow OR
- The presence of a specific leukemia gene mutation.
Acute Promyelocytic Leukemia (APL)
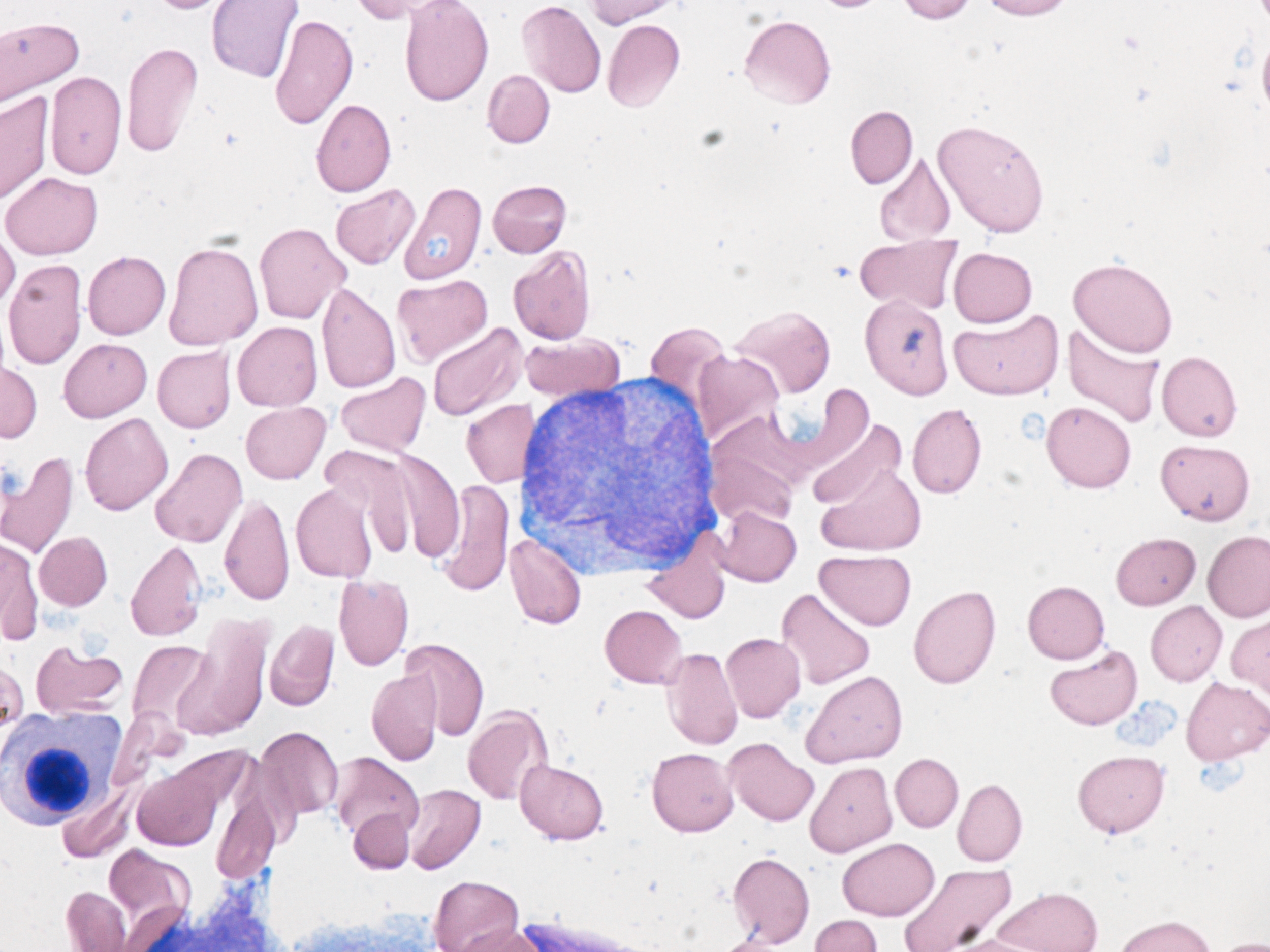
- Acute promyelocytic leukemia is important to recognize because it is often associated with disseminated intravascular coagulation (DIC) and has specific therapy (all-trans retinoic acid (ATRA; tretinoin)).
- The blasts in APL are large and have abundant cytoplasm. The nuclei are eccentric and often bilobed with a folded contour, immature chromatin, and a prominent nucleolus. The bilobed, folded nuclei look like two partially stacked, overlapping dishes. The cytoplasm has abundant purple cytoplasm. Some cells have multiple Auer rods. The golgi apparatus may be visible as an area of clearing near the nucleus.
- The microgranular variant of APL has no visible granules and less Auer rods.
- Also look for signs of DIC - schistocytes, elevated D-dimer, decreased fibrinogen, and prolonged PT and APTT.
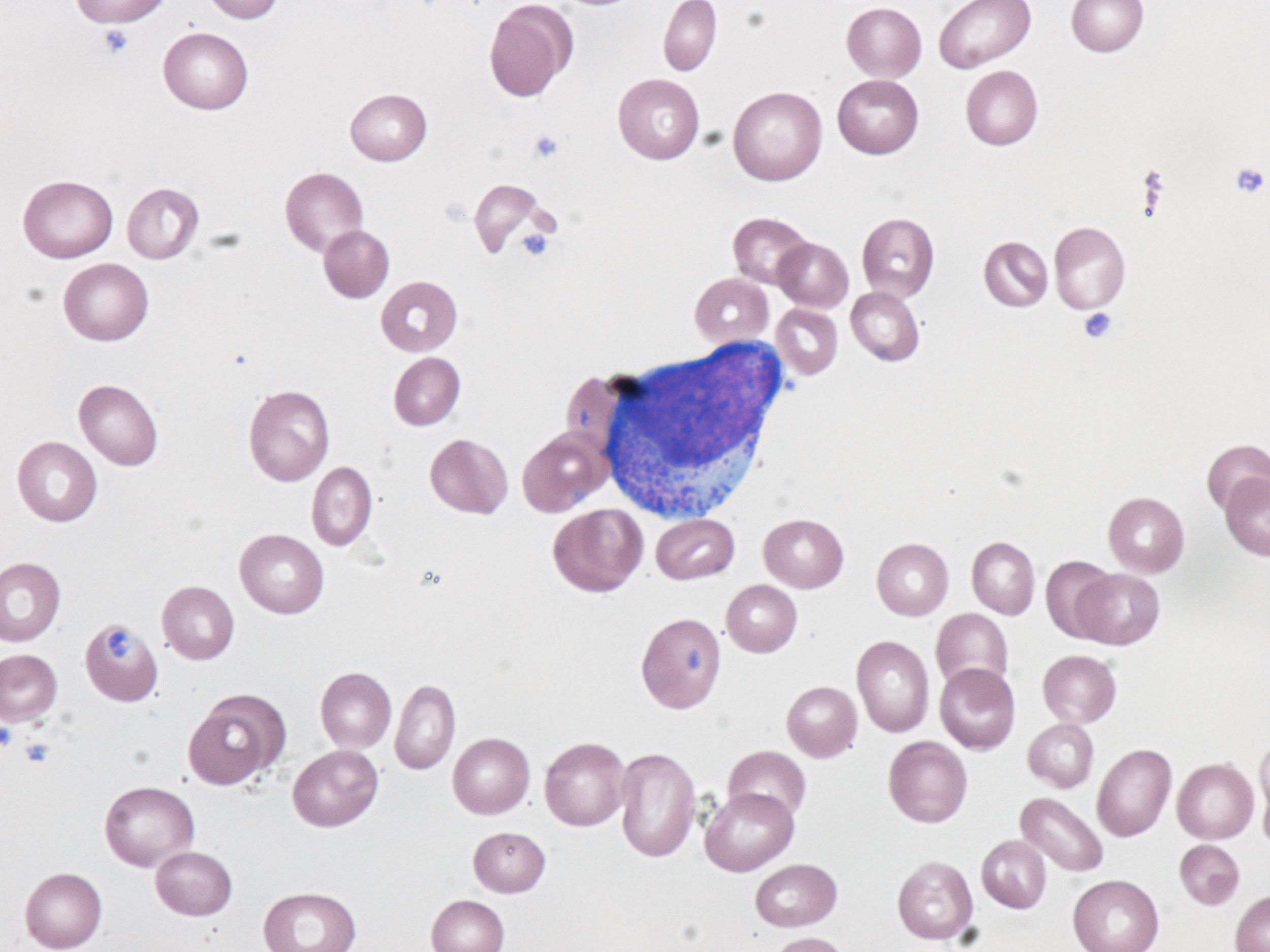
Acute Promyelocytic leukemia, microgranular variant
- Lacks the numerous visible granules typically seen in APL
- May be CD34 positive
Acute Monocytic Leukemia
- Acute monocytic leukemia presents with leukocytosis and monocytosis. The number of blasts in the peripheral blood is variable - there can be no blasts or many. Immature monocytes and promonocytes may be present. The diagnosis requires 20% blasts or promonocytes in the peripheral blood or bone marrow (blasts + promonocytes >= 20%).
- Based on the peripheral blood findings the differential diagnosis includes chronic myelomonocytic leukemia. Bone marrow biopsy is often required to distinguish between the two entities.
- Monoblasts are medium-sized with scant to moderate amounts of cytoplasm with a few, scattered, fine lilac granules. The nuclei are oval to slightly folded with immature chromatin and variably prominent nucleoli.
- Acute monocytic leukemia may show gum infiltration.
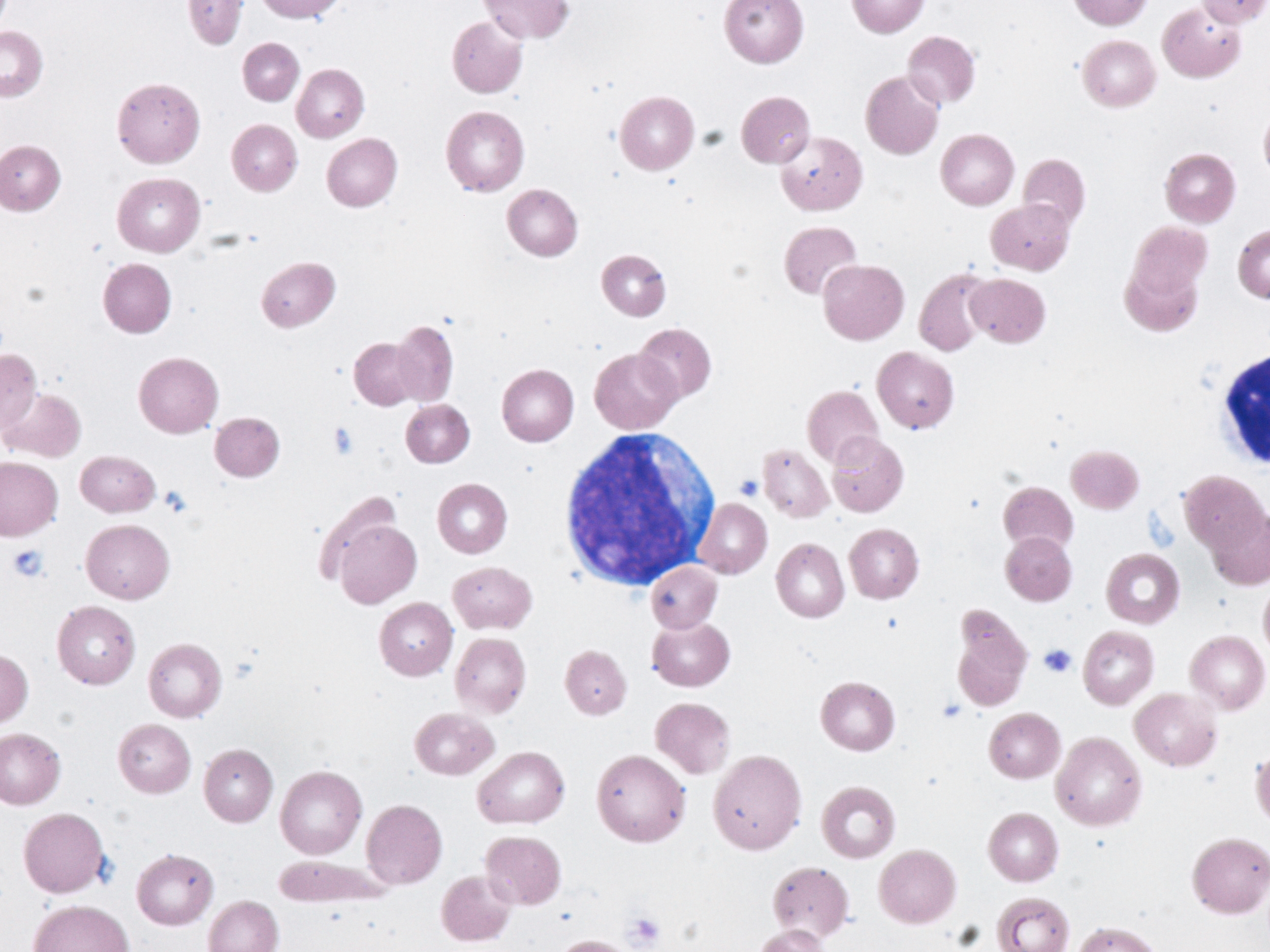
Lymphoblastic Leukemia
- Lymphoblasts are small to medium-sized with scant agranular cytoplasm, oval nuclei, immature chromatin and variably prominent nucleoli.
- Lymphoblasts can be difficult to tell from lymphocytes. Lymphoblast exhibit a squishy contour and may show cells that consist almost entirely of nucleus. Flow cytometry is required in difficult cases.
The complete blood count (CBC) is critical in the evaluation of peripheral blood smears.
There are a lot of numbers. Focus on the parameters white blood cell count (WBC), hemoglobin (Hb) and platelet count (PLT).
Look at the strength of the signal. The more parameters that are abnormal the more you should be worried. The more an individual parameter is abnormal, the more you should be worried. For example only mild anemia (WBC normal, Hb slightly decreased, PLT normal; not too worried) vs. severe pancytopenia (WBC markedly decreased, Hb markedly decreased, PLT marked decreased; worried).
20% or more blasts means acute leukemia. There can be less than 20% blasts in the peripheral blood and more than 20% in the bone marrow.
Below are some differential diagnoses based on the CBC and WBC differential
Leukocytosis and ≥20% blasts
- Acute leukemia
Leukopenia and ≥20% blasts
- Acute leukemia
Leukocytosis and 1-19% blasts
- Acute leukemia
- Myeloproliferative neoplasm (e.g. chronic myeloid leukemia (CML))
- Myeloproliferative/myelodysplastic neoplasm
- Reactive (e.g. severe infection, G-CSF therapy)
Leukopenia and 1-19% blasts
- Acute leukemia
- Myelodysplastic syndrome
- Chemotherapy (if not too many blasts)
- Severe infection (if not too many blasts)
Leukocytosis and monocytosis
- Acute monocytic leukemia.
- Chronic myelomonocytic leukemia (CMML).
- Reactive (e.g. infection)